Professional Documents
Culture Documents
Blood Banking Prelims
Blood Banking Prelims
Uploaded by
TriciaLeeCopyright:
Available Formats
You might also like
- Medical Student Clinical Assessment Form: (Mm/dd/yy) (Mm/dd/yy)Document4 pagesMedical Student Clinical Assessment Form: (Mm/dd/yy) (Mm/dd/yy)Natasha Reddy0% (1)
- Biochem 10A Lab QuestionsDocument6 pagesBiochem 10A Lab QuestionsPaul A IBattledaily Scavella100% (1)
- CHEM A 14B COMP Qual - Anions PDFDocument6 pagesCHEM A 14B COMP Qual - Anions PDFxerxeshakaNo ratings yet
- 1 Erythrocytic DisordersDocument6 pages1 Erythrocytic DisorderschippaiqweqweNo ratings yet
- Week 3 - Primary HemostasisDocument4 pagesWeek 3 - Primary HemostasisRubenne Miles ElagasNo ratings yet
- COMSATS Institute of Information Technology Abbottabad: Course Outline - Semester Fall 2019Document4 pagesCOMSATS Institute of Information Technology Abbottabad: Course Outline - Semester Fall 2019Haider AliNo ratings yet
- X y X y M M D : Pre-Calculus QUIZ NO. 1 (Prerequisite Skills)Document2 pagesX y X y M M D : Pre-Calculus QUIZ NO. 1 (Prerequisite Skills)Mikee VillanuevaNo ratings yet
- Prelims BitsDocument121 pagesPrelims BitsSaurav SumanNo ratings yet
- Inorganic and Organic Chemistry Prelims ReviewerDocument33 pagesInorganic and Organic Chemistry Prelims ReviewerMary Ann C RecañaNo ratings yet
- Anaphy Lecture Midterm ExamDocument5 pagesAnaphy Lecture Midterm ExamBulajyo Pangngay JolinaNo ratings yet
- CHEM 2402 Midterm 1 AnswersDocument4 pagesCHEM 2402 Midterm 1 AnswersDaniel Alexander Black100% (1)
- PreCalculus Quiz #1Document1 pagePreCalculus Quiz #1Ana Marie ValenzuelaNo ratings yet
- (Practical Exam) Physiology Lab Practical Cheat ShitDocument11 pages(Practical Exam) Physiology Lab Practical Cheat ShitKeesha RiveraNo ratings yet
- Departmental Syllabus For MAT 284, Business Calculus. Spring 2014Document4 pagesDepartmental Syllabus For MAT 284, Business Calculus. Spring 2014Anonymous bZTdTpLNo ratings yet
- Pre-Calculus HomeworkDocument7 pagesPre-Calculus Homeworkapi-205958356No ratings yet
- Pre-Algebra Ch.11 Quiz 2Document3 pagesPre-Algebra Ch.11 Quiz 2KaitlynNo ratings yet
- 30 Min QUIZ On Circle Parabola EllipseDocument2 pages30 Min QUIZ On Circle Parabola EllipseLeopold LasetNo ratings yet
- Pre-Calculus Quiz 3Document2 pagesPre-Calculus Quiz 3Kim VillanuevaNo ratings yet
- Pre-Calculus Quiz 1Document1 pagePre-Calculus Quiz 1Kim VillanuevaNo ratings yet
- Prelim Exam Schedule 1st Sem 2021 2022Document2 pagesPrelim Exam Schedule 1st Sem 2021 2022Carylle FontanillaNo ratings yet
- Prelim-Course Details Prelim CoverageDocument21 pagesPrelim-Course Details Prelim CoverageMary Claire SomeraNo ratings yet
- Grade 7 Math Challenge QuizDocument3 pagesGrade 7 Math Challenge QuizScottNo ratings yet
- Differential CalculusDocument4 pagesDifferential CalculusIsiahTanEdquibanNo ratings yet
- AnaPhy Midterm PointersDocument1 pageAnaPhy Midterm PointersAmielsimon NgoNo ratings yet
- Inorganic and Organic Chemistry Prelims ReviewerDocument33 pagesInorganic and Organic Chemistry Prelims ReviewerMary Ann C RecañaNo ratings yet
- Anaphy Lab MidtermsDocument32 pagesAnaphy Lab Midtermsjoseph manansalaNo ratings yet
- 2013 Midterm 3Document16 pages2013 Midterm 3billbyoag123No ratings yet
- Unit 4Document117 pagesUnit 4Soc Sci0% (1)
- Organic Chemistry Midterm 1epox+mech+keyDocument1 pageOrganic Chemistry Midterm 1epox+mech+keyNorma Leticia RamosNo ratings yet
- K101PracEx4 SP19 KeyDocument10 pagesK101PracEx4 SP19 KeyBraxton PhillipsNo ratings yet
- Pre-Calculus Quiz 3Document1 pagePre-Calculus Quiz 3Kim VillanuevaNo ratings yet
- PreCalculus Quiz #1Document1 pagePreCalculus Quiz #1Ana ValenzuelaNo ratings yet
- Chemistry Quiz Grade 7Document4 pagesChemistry Quiz Grade 7menma funNo ratings yet
- Hematology 1 MidtermsDocument31 pagesHematology 1 Midtermsella SyNo ratings yet
- Earthsci PrelimsDocument6 pagesEarthsci PrelimsKrisha DimailigNo ratings yet
- 1.02 Physiology Trans - Muscle PhysiologyDocument10 pages1.02 Physiology Trans - Muscle PhysiologyMineTagraNo ratings yet
- AP Biology Final Exam ReviewDocument1 pageAP Biology Final Exam Reviewrobertclee1234No ratings yet
- Comsats University Islamabad, Abbottabad Campus Afghan Students "Zero Semester" Biology Quiz Mcqs Name - Reg# - Time: 40 MinDocument3 pagesComsats University Islamabad, Abbottabad Campus Afghan Students "Zero Semester" Biology Quiz Mcqs Name - Reg# - Time: 40 Minanon_572243106No ratings yet
- Biology C - Lesson 1 - Circulatory SystemDocument46 pagesBiology C - Lesson 1 - Circulatory SystemMuhammad Azrie0% (1)
- Assignment 4 (Spectroscopy) : CH CH CH CCH O CH CH CH CH ODocument1 pageAssignment 4 (Spectroscopy) : CH CH CH CCH O CH CH CH CH OIbrahim MuhamadNo ratings yet
- General Chemistry Quiz - PrelimDocument5 pagesGeneral Chemistry Quiz - PrelimRochelle Anne Abad BandaNo ratings yet
- Chemistry QuizDocument6 pagesChemistry QuizlimananthonyNo ratings yet
- Multiple True False Past Year CompilationDocument9 pagesMultiple True False Past Year CompilationBrendaJooYeeNo ratings yet
- Altfragen Biostatistics ColloquiumDocument10 pagesAltfragen Biostatistics ColloquiumMolly McMillan100% (1)
- CLS Aipmt-15-16 XIII Che Study-Package-1 Set-1 Chapter-1 001Document26 pagesCLS Aipmt-15-16 XIII Che Study-Package-1 Set-1 Chapter-1 001Mudit Goel97% (29)
- Chemistry QuizDocument2 pagesChemistry Quizanon_572243106No ratings yet
- Hello WordDocument9 pagesHello WordRicardo CamargoNo ratings yet
- Che 323 Problem Set 6: Electrochemistry March 12, 2014 Engr. May V. Tampus ConceptsDocument1 pageChe 323 Problem Set 6: Electrochemistry March 12, 2014 Engr. May V. Tampus ConceptsLouie G NavaltaNo ratings yet
- Exam # 2 Chemistry 208, Organic Chemistry I Spring 2016: Your Name: - Laboratory SectionDocument6 pagesExam # 2 Chemistry 208, Organic Chemistry I Spring 2016: Your Name: - Laboratory SectionHieyeNo ratings yet
- PhyChem Quiz 3 and ProfEng Quiz 2 1Document5 pagesPhyChem Quiz 3 and ProfEng Quiz 2 1Krizzi Dizon GarciaNo ratings yet
- NMATDocument8 pagesNMATmariesklodowskaNo ratings yet
- Biology Lecture Exams: Scarlet RedDocument2 pagesBiology Lecture Exams: Scarlet RedEmsii DelfinoNo ratings yet
- Thin-Layer Chromatography: CHM 112 Lab Procedure 2Document17 pagesThin-Layer Chromatography: CHM 112 Lab Procedure 2zynab123No ratings yet
- Lecture 11 - AROMATIC COMPOUNDSDocument71 pagesLecture 11 - AROMATIC COMPOUNDSapi-19824406No ratings yet
- Sample Biology AssignmentDocument3 pagesSample Biology AssignmentSkyler RossNo ratings yet
- University of Santo TomasDocument5 pagesUniversity of Santo TomasJanine MontaNo ratings yet
- Ana Chem FinalsDocument8 pagesAna Chem FinalsLouisiana SollestreNo ratings yet
- Organic Chemistry Practice MidtermDocument7 pagesOrganic Chemistry Practice MidtermAmy HanNo ratings yet
- Heart Dissection Lab Report GuideDocument6 pagesHeart Dissection Lab Report Guideelorenzana0511100% (1)
- The RH Blood Group System: Tudy ID NswersDocument2 pagesThe RH Blood Group System: Tudy ID NswersChatie PipitNo ratings yet
- M 4Document19 pagesM 4Ritika JangraNo ratings yet
- A Field Manual of Camel Diseases Traditional and Modern Health Care For The DromedaryDocument273 pagesA Field Manual of Camel Diseases Traditional and Modern Health Care For The DromedaryHenrique100% (3)
- States Atty Press Release: Kathleen Savio's Death Ruled HomicideDocument2 pagesStates Atty Press Release: Kathleen Savio's Death Ruled HomicideJustice Café100% (2)
- Abordul Laparoscopic Pentru Testicule Nepalpabile Aspecte Tehnice Si RezultateDocument6 pagesAbordul Laparoscopic Pentru Testicule Nepalpabile Aspecte Tehnice Si RezultateAlexandra NechiforNo ratings yet
- Acls Guidelines 2015Document31 pagesAcls Guidelines 2015AgilNoviarAlvirosaNo ratings yet
- Diseases of The Spinal CordDocument15 pagesDiseases of The Spinal CordBai Aishwayra Haylee DalidigNo ratings yet
- Diathesis Stress Model - Zuckerman1999Document21 pagesDiathesis Stress Model - Zuckerman1999Paulina100% (1)
- Journal GastroenterologyDocument14 pagesJournal GastroenterologySusilo PrihrantoNo ratings yet
- Intra Oral ExaminationDocument14 pagesIntra Oral ExaminationpriyaNo ratings yet
- CDC Proposal On Male Circumcision: December 2, 2014Document73 pagesCDC Proposal On Male Circumcision: December 2, 2014Matthew Keys100% (3)
- Disprin UploadDocument13 pagesDisprin Uploadgoved2100% (1)
- Alternative Medicine Literature ReviewDocument8 pagesAlternative Medicine Literature Reviewea85vjdw100% (1)
- YadgirDocument6 pagesYadgirHashir PvNo ratings yet
- Buku BiomedikDocument4 pagesBuku BiomedikAchmad Bagus Dwi SNo ratings yet
- 3Document13 pages3Urologi Unpad Februari 2023No ratings yet
- LVS Chronic Pain WsDocument49 pagesLVS Chronic Pain WsdtncorreoNo ratings yet
- Venix Trifold BrochureDocument2 pagesVenix Trifold BrochureCherry San DiegoNo ratings yet
- Anna Garcia Death Timeline 1Document19 pagesAnna Garcia Death Timeline 1api-245176779No ratings yet
- Bronchial HygieneDocument37 pagesBronchial HygieneRayan MohhamadNo ratings yet
- Adrenaline (Anaethesia Tutorial of The Week)Document8 pagesAdrenaline (Anaethesia Tutorial of The Week)Raisa AriesthaNo ratings yet
- Migraine Diagnosis and TreatmentDocument19 pagesMigraine Diagnosis and TreatmentMagdalila Pua RosalesNo ratings yet
- Case Study - Intestinal Resection and Anastomosis in A DogDocument13 pagesCase Study - Intestinal Resection and Anastomosis in A Dogapi-301746262No ratings yet
- Prof Djoko Plenary PDFDocument23 pagesProf Djoko Plenary PDFbagir_dm10No ratings yet
- Drugs Used in AnaesthesiaDocument32 pagesDrugs Used in Anaesthesiav_vijayakanth7656100% (2)
- Bedside Teaching in Clinical MedicineDocument3 pagesBedside Teaching in Clinical Medicineawatif mahadiNo ratings yet
- Diabetes Mellitus Aticle ApthaDocument6 pagesDiabetes Mellitus Aticle ApthaRahul KirkNo ratings yet
- ACLS DrugsDocument16 pagesACLS Drugstostc100% (2)
- Risk Assessment CompletedDocument1 pageRisk Assessment Completedapi-410227491No ratings yet
- What Is SciaticaDocument2 pagesWhat Is Sciaticaha hoangNo ratings yet
Blood Banking Prelims
Blood Banking Prelims
Uploaded by
TriciaLeeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Banking Prelims
Blood Banking Prelims
Uploaded by
TriciaLeeCopyright:
Available Formats
Rh Blood Group System
- 2nd most important Blood Group System after
ABO
- Greatest clinical importance in Hemolytic
Disease of the Newborn (erythroblastosis
fetalis) and Transfusion Reactions
- 50 Rh antigens ( Rh1 -> Rh57)
- Come from Rhesus monkey - 85% Agglutinated = Rh (+)
- Most common based on antigenicity: - 15% Non-agglutinated = Rh (-)
D>c>E>C>e - Ab in Female = Anti-Rh
- D – primary antigen, would be Rh(+) or Rh(-) - Ab in Rabbit = Anti-LW
due to this no matter what
- Location: C. Weiner and Peter
Non-glycosylated protein on RBC membrane - Rh(-) who received Rh(+) blood are compatible
(Chromosome 1) along with
1. genes for elliptocytosis 4 NOMENCLATURES
2. 6-phosphoglucoronic dehydrogenase 1. Fischer-Race – DCE Terminology
3. phosphoglucomutase 2. Weiner – rH, Hr
4. phosphopyruvate hydratase 3. Rosenfield – Alpha/Numeric
- no glucose moity 4. ISBT – Numeric
- Autosomal dominant Fisher-Race
- Difficulty in describing structure - 3 closely linked genes that can be inherited
- 174,000 MW compound from each parent has 3 closely linked loci that
carry the Rh genes
HISTORY - Crossing over is rare cause they are closely
- Discovered by Blood Transfusion linked
A. (1939) Levine and Stetson - MNSS
- Antibody of D Antigen (Anti-D) - CDE -> cde
- In serum of woman whose fetus had HDN Weiner
(second birth) - 1 gene at a single locus controls the entire Rh
- Mother is Rh(-), Father is Rh(+) system
B. (1940) Landsteiner and Weiner - D – Rh0
-Identified the Rh Blood Group System - C – RhI
- E – RhII
- c – hrI
Rh RBC - e – hrII
- Has agglutinogen w/c is made up of 3 blood
factors
Rabbit - Antigen – subscript
Rosenfield
Produce Anti-Rh - Aims to bridge the confusion between first 2
antibodies - A number in chronological discovery
against Rh RBC - No genetic basis
- Presence or absence only of Ag
- D–1
Ab reaction - C–2
- E–3
with human - e–4
RBC
1 Pagkatipunan 3A-MT S.Y. 2014-2015
- c–5 - E – 004003
ISBT (International Society for Blood Transfusions) - c – 004004
- 6 numerical numbers - e – 004005
- 004 = Rh
- D – 004001
- C – 004002
2 Pagkatipunan 3A-MT S.Y. 2014-2015
Possible Fisher-Race Weiner Gene Agglutinogen 3 blood Rosenfield
combinations Shorthand or Ag factors
Dce Dce Ro Rho Rho Rho, hrI, hrII Rh 1, -2, -3, 4,
5
DCe DCe R1 Rh1 Rh1 Rho, rhI, hrII Rh 1, 2, -3, -4,
5
DcE DcE R2 Rh2 Rh2 Rho, hrI, rhII Rh 1, -2, 3, 4,
-5
DCE DCE Rz Rhz Rhz Rho, rhI, rhII Rh 1, 2, 3, -4,
-5
dce dce r rh rh hri, hrii Rh -1, -2, -3,
4, 5
dCe dCe rI rhI rhI rhi,hrii Rh -1, 2, -3,
-4, 5
dcE dcE rII rhII rhII hri,rhii Rh -1, -2, 3, 4,
-5
dCE dCE rY rhY rhY rhi,rhii Rh -1, 2, 3, -4,
-5
Variants of Rh
- Cu
- Cf
- Cw
- Eu
- Du – Weakened expression of D-Antigen
(Blacks>Caucasians) detectable only by Indirect
Method. It is few in number
- D+w is the phenotype 2. Partial or Mosaic
- Because Rh is a low MW compound (174,000
Mechanisms of Weak D Antigen daltons), it is said that the D-antigen is a mosaic
structure composed of 4 fragments and if one part
or others is/are missing, it shows weak expression of
1. c-Trans
D-antigen.
- C is in cis position with D
A position
- if C is in trans B A weak
it causes B D
C D D
D d D d
No Weak D Weak D with Anti-C
C Cis c Trans
c C Disadvantage – if you are Rh(-), you can receive only
e E Rh(-)
e E
3. Genetic Weak D
Normal Weak-D - All fragments are present but only in few number
and thus weakly expressed.
2 types of Du
3 Pagkatipunan 3A-MT S.Y. 2014-2015
1. Low Grade 1. Regulator Type – Mutation in Rh AG thus there is
- Direct product of inherited gene detectable only by Rh AG in RBC but has normal complement of Rh D
IAG, and can be passed unto future generations. and Rh CE
2. High Grade 2. Amorphic Type - Mutation in Rh CE, Deletion in Rh
- Cannot be passed unto future generations, rarely D, Normal Rh AG
need Anti-globulin test
General Characteristics of Rh Antibodies
1. Majority are IgG (1 and 3 most significant)
2. Not natural antibodies but immune antibodies
3. React best at 37C
4. Crosses placenta
5. Do not bind complement
6. Do not react in saline solution
7. Commonly found antibodies in
3 Genes that control Rh expression immunocompromised patients = Anti-D and Anti-G
1. Rh D – Presence of D antigen (Chromosome 1) (Abs found in immunized patients)
2. Rh CE – Presence of C, E, c, and e antigen
(Chromosome 1)
3. RhAG – Rh Associated glycoprotein, coexpressor
(Chromosome 6)
- Expresses Rh AG but by itself does not 3 Varieties of Rh Antibodies
display any antigen 1. 1st Order – Saline agglutinins, Bivalent, Complete
- If there is a mutation in this gene = Missing – React in Saline medium
or alteration of Rh D and Rh CE 2. 2nd Order – Albumin reacting, Monovalent,
Incomplete – React in protein medium
3. 3rd Order – Typical antibodies, Anti-globulin
Unusual Phenotypes of Rh
antibodies – React in antiglobulin medium
1. Rh Deleted – no C and E (D _ _ / D _ _ )
2. Rh Null – none at all ( _ _ _ / _ _ _ )
3. Rh Moderate – weak expression Different Anti Sera to detect Rh Antigens
1. Anti-C
1. Anti-E
Effects of no presence of D, C, E, c, and e
2. Anti-c
3. Anti-e
Rh Deleted Rh Null 4. Anti-D
RBC Normal Spherocytes,
morphology Stomatocytes Types of Anti Sera to detect Rh Antigens
Rh Antigens Increase D per No D, C, E, c,
RBC and e
1. Low Protein Based
In vivo survival Normal (120 Reduced 2. High Protein Based
days) 3. Saline Based
Effect Impaired N and 4. Chemically Modified
K ion transport 5. Monoclonal
Hemolytic 6. Polyclonal
Anemia
Decrease OFT
❖ Saline Reactive Anti-sera
- Low Protein Based
- Has IgM
Genetic Mechanisms of Rh Null Syndrome - Can test red cells coated with IgG
- Cannot detect weak D
4 Pagkatipunan 3A-MT S.Y. 2014-2015
- Requires long incubation time (30-60mins)
❖ Chemically Modified IgG Sera
- Low protein based
- No high MW potentiators
- Can be used for slide and tube
- Antibody molecules are treated with
reducing agents
❖ Modified Tube Anti-D
- Contains
1. IgG Direct Anti-globulin Test
2. High Concentration of protein (20-30% - In-vivo reaction
Serum Albumin) - It is not normal in the body to have
3. Macromolecular additives – Dextran, sensitization
Polyvinyl Pyrollidone - Detects antibodies for Hemolytic Disease of
the Newborn as Maternal Anti-D coats fetal
RBC
- Used to demonstrate in vivo coating of red
cells with antibodies or complement, in
particular IgG and C3d.
- Cephalexin – Causes sensitization of RBC X
and Y
Anti Globulin Test - Expected in patients with: Hemolytic
- Used to detect incomplete or non- Disease of the newborn, Drug Induced
agglutinating antibodies Hemolytic Anemia, Autoimmune Hemolytic
- Tool to detect IgG, 7s, or complement. Anemia, and Hemolytic Transfusion
- Not reactive in saline or high protein Reaction.
medium Indirect Anti-globulin Test
- Principle – Anti globulin agglutinate with - Detects presence of unexpected antibodies
cells with gamma globulin in the patient’s serum that are able to coat
antigens in type “O” red cells in vitro (in
vitro sensitization)
- It primarily detects antibodies other than
RBC IgG the naturally occurring anti-A and anti-B.
IgG coated cells or sensitized - It is useful in detecting weak variants of D
RBCs antigens, red cell phenotyping, in antibody
screening, and identification and in minor
crossmatching.
Anti-globulin types
- React at 37 C
- Polyspecific – Polyclonals – can agglutinate
Importance:
with IgG and anti-complement (Anti-C3D)
1. Du Testing
- Monospecific – Monoclonals – specific for
2. Compatibility Testing
only one
3. Antibody Screening Test
- These bridge together to agglutinize
4. RBC Phenotyping
sensitized RBC
5. Investigation of Transfusion
Reaction
6. Antibody Titration
Sensitized RBC Anti-globulin
5 Pagkatipunan 3A-MT S.Y. 2014-2015
Factors affecting Anti-globulin Test 3. Antibody Screening – Detects presence or
1. Ratio of serum to cells absence of unexpected antibodies.
- Higher ratio, higher sensitivity - Done in women with previous
- Minimum ratio is 40:1 (2 drops serum and pregnancy and patients with
1 drop 5% RCS) previous transfusions
- If the reaction of the antibody is weak -> 4. Compatibility Testing
133:1 (4 drops serum and 1 drop 5% RCS) - Major – Patient Serum, Donor Red Cell
2. Reaction Medium – Enhances Ag-Ab rxn - Minor – Patient Red Cell, Donor Serum
- Albumin – allows sensitized cell to come - Antibody in serum that can destroy
closer in contact (2 drops serum, 2 drops transfused red cells
albumin, 1 drop 3-5% RCS) - Tests if transfused red cells can survive in
- LISS (Low Ionic Strength Solution) – vivo
Enhances antibody uptake and reduces - Transfusion Reaction
incubation time (2 drops serum, 2 drops
LISS, 1 drop 3-5% RCS) Autologous Transfusion
- Polyethylene Glycol – water soluble polymer - Own blood is transfused to self
used as an additive which increase antibody - Surgical procedures
uptake by removing water thus increasing
antibody concentration Preferred specimen – Fresh, not less than 48 hours,
3. Incubation Time – LISS 10-15 minutes only not inactivated serum or plasma
4. Temperature Blood of donor and recipient must be kept at 1-6°C
5. Washing – 3 times with NSS, inadequate at minimum for 7 days first.
washing and excess NSS – False (-) IV Tube Patient – Do not get blood cause it is diluted,
6. Centrifuge can’t detect weak antibodies
7. Manner of reading result Solution: Stop IV for 5-10 minutes, extract 10mL and
8. Reagents used discard, use the specimen after.
Compatibility Testing
- Also called crossmatching
- Composed of procedures intended for
safest blood transfusion
- ABO and Rh Blood groups of donor and
recipient must be compatible
Important because: Different Serological Tests For Cross Matching
1. Ensures max benefits to intended 1. Immediate Spin Saline Cross Match – Sole
recipient cross match, Simplest
2. Prevent transfusion reaction that - Mix, centri, dislodge, interpret
might happen to the recipient due - Only for no clinically significant antibodies,
to antibodies test for ABO incompatibility
2. Abbreviated Cross Match – Type and screen
Compatibility Testing for Homologous Transfusions coupled with Immediate Spin
1. ABO Typing – Direct or Indirect - For ABO, Rh, and unexpected antibodies
2. Rh Typing – Direct 3. Anti Human Globulin Cross Match
6 Pagkatipunan 3A-MT S.Y. 2014-2015
4. Computed Cross Match – use computer for 2. Panagglutination – spontaneous clumping
final check, only when there is no clinically of cells against given serum caused by:
significant antibodies. - bacteriologic (20°C Thomsen Friedenrich)
- non-bacteriologic (37°C, Acute Hemolytic
Broad Spectrum Compatibility Anemia, Rare specific antibodies)
- Method of Choice 4. Prozone
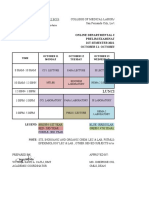
- Phases 5. Polyagglutination
1. Protein or Immediate Spin 6. Wharton’s Jelly
- For ABO, Cold antibodies, and Prozone Rh 7. Ag-Ab degradation
M MA N NA
Procedure to Shorten Compatibility Time
1. LISS
2. Enhancing Agents
- Albumin
-Papin
-Trypsin
2 drops patient serum 2 drops patient serum 2 drops patient red cell 2 drops patient red cell
-Polybrene Polycation
2drops donor red cell 2drops donor red cell 2drops donor serum 2drops donor serum
-2% RCS of donor
2 drops BSA 2drops BSA
- Centri, dislodge, interpret. If no
agglutination, use MA or NA and proceed to
next step.
2. Thermo or 37°C
- 37°C for 10 mins. Centri, dislodge, interpret.
If no agglutination, proceed to next step.
3. AHG
- Wash three times with NSS, add AHG. If no
agglutination:
- Add 1 drop check cells (Cells with IgG) and
should be 4+
Criteria of a Universal Donor
- Titer is less than 1:50
- If titer is high, remove the plasma and give
the RBC
- Use Witebsky substance to neutralize
naturally occurring anti-A and anti-B but not
immune anti-A and anti-B
1. A substance – from Hog’s stomach
2. B substance – from Horse’s stomach
Rh without previous immunization – no
anti-D
Rh with previous immunization – has anti-D
Problems
1. Rouleaux
7 Pagkatipunan 3A-MT S.Y. 2014-2015
You might also like
- Medical Student Clinical Assessment Form: (Mm/dd/yy) (Mm/dd/yy)Document4 pagesMedical Student Clinical Assessment Form: (Mm/dd/yy) (Mm/dd/yy)Natasha Reddy0% (1)
- Biochem 10A Lab QuestionsDocument6 pagesBiochem 10A Lab QuestionsPaul A IBattledaily Scavella100% (1)
- CHEM A 14B COMP Qual - Anions PDFDocument6 pagesCHEM A 14B COMP Qual - Anions PDFxerxeshakaNo ratings yet
- 1 Erythrocytic DisordersDocument6 pages1 Erythrocytic DisorderschippaiqweqweNo ratings yet
- Week 3 - Primary HemostasisDocument4 pagesWeek 3 - Primary HemostasisRubenne Miles ElagasNo ratings yet
- COMSATS Institute of Information Technology Abbottabad: Course Outline - Semester Fall 2019Document4 pagesCOMSATS Institute of Information Technology Abbottabad: Course Outline - Semester Fall 2019Haider AliNo ratings yet
- X y X y M M D : Pre-Calculus QUIZ NO. 1 (Prerequisite Skills)Document2 pagesX y X y M M D : Pre-Calculus QUIZ NO. 1 (Prerequisite Skills)Mikee VillanuevaNo ratings yet
- Prelims BitsDocument121 pagesPrelims BitsSaurav SumanNo ratings yet
- Inorganic and Organic Chemistry Prelims ReviewerDocument33 pagesInorganic and Organic Chemistry Prelims ReviewerMary Ann C RecañaNo ratings yet
- Anaphy Lecture Midterm ExamDocument5 pagesAnaphy Lecture Midterm ExamBulajyo Pangngay JolinaNo ratings yet
- CHEM 2402 Midterm 1 AnswersDocument4 pagesCHEM 2402 Midterm 1 AnswersDaniel Alexander Black100% (1)
- PreCalculus Quiz #1Document1 pagePreCalculus Quiz #1Ana Marie ValenzuelaNo ratings yet
- (Practical Exam) Physiology Lab Practical Cheat ShitDocument11 pages(Practical Exam) Physiology Lab Practical Cheat ShitKeesha RiveraNo ratings yet
- Departmental Syllabus For MAT 284, Business Calculus. Spring 2014Document4 pagesDepartmental Syllabus For MAT 284, Business Calculus. Spring 2014Anonymous bZTdTpLNo ratings yet
- Pre-Calculus HomeworkDocument7 pagesPre-Calculus Homeworkapi-205958356No ratings yet
- Pre-Algebra Ch.11 Quiz 2Document3 pagesPre-Algebra Ch.11 Quiz 2KaitlynNo ratings yet
- 30 Min QUIZ On Circle Parabola EllipseDocument2 pages30 Min QUIZ On Circle Parabola EllipseLeopold LasetNo ratings yet
- Pre-Calculus Quiz 3Document2 pagesPre-Calculus Quiz 3Kim VillanuevaNo ratings yet
- Pre-Calculus Quiz 1Document1 pagePre-Calculus Quiz 1Kim VillanuevaNo ratings yet
- Prelim Exam Schedule 1st Sem 2021 2022Document2 pagesPrelim Exam Schedule 1st Sem 2021 2022Carylle FontanillaNo ratings yet
- Prelim-Course Details Prelim CoverageDocument21 pagesPrelim-Course Details Prelim CoverageMary Claire SomeraNo ratings yet
- Grade 7 Math Challenge QuizDocument3 pagesGrade 7 Math Challenge QuizScottNo ratings yet
- Differential CalculusDocument4 pagesDifferential CalculusIsiahTanEdquibanNo ratings yet
- AnaPhy Midterm PointersDocument1 pageAnaPhy Midterm PointersAmielsimon NgoNo ratings yet
- Inorganic and Organic Chemistry Prelims ReviewerDocument33 pagesInorganic and Organic Chemistry Prelims ReviewerMary Ann C RecañaNo ratings yet
- Anaphy Lab MidtermsDocument32 pagesAnaphy Lab Midtermsjoseph manansalaNo ratings yet
- 2013 Midterm 3Document16 pages2013 Midterm 3billbyoag123No ratings yet
- Unit 4Document117 pagesUnit 4Soc Sci0% (1)
- Organic Chemistry Midterm 1epox+mech+keyDocument1 pageOrganic Chemistry Midterm 1epox+mech+keyNorma Leticia RamosNo ratings yet
- K101PracEx4 SP19 KeyDocument10 pagesK101PracEx4 SP19 KeyBraxton PhillipsNo ratings yet
- Pre-Calculus Quiz 3Document1 pagePre-Calculus Quiz 3Kim VillanuevaNo ratings yet
- PreCalculus Quiz #1Document1 pagePreCalculus Quiz #1Ana ValenzuelaNo ratings yet
- Chemistry Quiz Grade 7Document4 pagesChemistry Quiz Grade 7menma funNo ratings yet
- Hematology 1 MidtermsDocument31 pagesHematology 1 Midtermsella SyNo ratings yet
- Earthsci PrelimsDocument6 pagesEarthsci PrelimsKrisha DimailigNo ratings yet
- 1.02 Physiology Trans - Muscle PhysiologyDocument10 pages1.02 Physiology Trans - Muscle PhysiologyMineTagraNo ratings yet
- AP Biology Final Exam ReviewDocument1 pageAP Biology Final Exam Reviewrobertclee1234No ratings yet
- Comsats University Islamabad, Abbottabad Campus Afghan Students "Zero Semester" Biology Quiz Mcqs Name - Reg# - Time: 40 MinDocument3 pagesComsats University Islamabad, Abbottabad Campus Afghan Students "Zero Semester" Biology Quiz Mcqs Name - Reg# - Time: 40 Minanon_572243106No ratings yet
- Biology C - Lesson 1 - Circulatory SystemDocument46 pagesBiology C - Lesson 1 - Circulatory SystemMuhammad Azrie0% (1)
- Assignment 4 (Spectroscopy) : CH CH CH CCH O CH CH CH CH ODocument1 pageAssignment 4 (Spectroscopy) : CH CH CH CCH O CH CH CH CH OIbrahim MuhamadNo ratings yet
- General Chemistry Quiz - PrelimDocument5 pagesGeneral Chemistry Quiz - PrelimRochelle Anne Abad BandaNo ratings yet
- Chemistry QuizDocument6 pagesChemistry QuizlimananthonyNo ratings yet
- Multiple True False Past Year CompilationDocument9 pagesMultiple True False Past Year CompilationBrendaJooYeeNo ratings yet
- Altfragen Biostatistics ColloquiumDocument10 pagesAltfragen Biostatistics ColloquiumMolly McMillan100% (1)
- CLS Aipmt-15-16 XIII Che Study-Package-1 Set-1 Chapter-1 001Document26 pagesCLS Aipmt-15-16 XIII Che Study-Package-1 Set-1 Chapter-1 001Mudit Goel97% (29)
- Chemistry QuizDocument2 pagesChemistry Quizanon_572243106No ratings yet
- Hello WordDocument9 pagesHello WordRicardo CamargoNo ratings yet
- Che 323 Problem Set 6: Electrochemistry March 12, 2014 Engr. May V. Tampus ConceptsDocument1 pageChe 323 Problem Set 6: Electrochemistry March 12, 2014 Engr. May V. Tampus ConceptsLouie G NavaltaNo ratings yet
- Exam # 2 Chemistry 208, Organic Chemistry I Spring 2016: Your Name: - Laboratory SectionDocument6 pagesExam # 2 Chemistry 208, Organic Chemistry I Spring 2016: Your Name: - Laboratory SectionHieyeNo ratings yet
- PhyChem Quiz 3 and ProfEng Quiz 2 1Document5 pagesPhyChem Quiz 3 and ProfEng Quiz 2 1Krizzi Dizon GarciaNo ratings yet
- NMATDocument8 pagesNMATmariesklodowskaNo ratings yet
- Biology Lecture Exams: Scarlet RedDocument2 pagesBiology Lecture Exams: Scarlet RedEmsii DelfinoNo ratings yet
- Thin-Layer Chromatography: CHM 112 Lab Procedure 2Document17 pagesThin-Layer Chromatography: CHM 112 Lab Procedure 2zynab123No ratings yet
- Lecture 11 - AROMATIC COMPOUNDSDocument71 pagesLecture 11 - AROMATIC COMPOUNDSapi-19824406No ratings yet
- Sample Biology AssignmentDocument3 pagesSample Biology AssignmentSkyler RossNo ratings yet
- University of Santo TomasDocument5 pagesUniversity of Santo TomasJanine MontaNo ratings yet
- Ana Chem FinalsDocument8 pagesAna Chem FinalsLouisiana SollestreNo ratings yet
- Organic Chemistry Practice MidtermDocument7 pagesOrganic Chemistry Practice MidtermAmy HanNo ratings yet
- Heart Dissection Lab Report GuideDocument6 pagesHeart Dissection Lab Report Guideelorenzana0511100% (1)
- The RH Blood Group System: Tudy ID NswersDocument2 pagesThe RH Blood Group System: Tudy ID NswersChatie PipitNo ratings yet
- M 4Document19 pagesM 4Ritika JangraNo ratings yet
- A Field Manual of Camel Diseases Traditional and Modern Health Care For The DromedaryDocument273 pagesA Field Manual of Camel Diseases Traditional and Modern Health Care For The DromedaryHenrique100% (3)
- States Atty Press Release: Kathleen Savio's Death Ruled HomicideDocument2 pagesStates Atty Press Release: Kathleen Savio's Death Ruled HomicideJustice Café100% (2)
- Abordul Laparoscopic Pentru Testicule Nepalpabile Aspecte Tehnice Si RezultateDocument6 pagesAbordul Laparoscopic Pentru Testicule Nepalpabile Aspecte Tehnice Si RezultateAlexandra NechiforNo ratings yet
- Acls Guidelines 2015Document31 pagesAcls Guidelines 2015AgilNoviarAlvirosaNo ratings yet
- Diseases of The Spinal CordDocument15 pagesDiseases of The Spinal CordBai Aishwayra Haylee DalidigNo ratings yet
- Diathesis Stress Model - Zuckerman1999Document21 pagesDiathesis Stress Model - Zuckerman1999Paulina100% (1)
- Journal GastroenterologyDocument14 pagesJournal GastroenterologySusilo PrihrantoNo ratings yet
- Intra Oral ExaminationDocument14 pagesIntra Oral ExaminationpriyaNo ratings yet
- CDC Proposal On Male Circumcision: December 2, 2014Document73 pagesCDC Proposal On Male Circumcision: December 2, 2014Matthew Keys100% (3)
- Disprin UploadDocument13 pagesDisprin Uploadgoved2100% (1)
- Alternative Medicine Literature ReviewDocument8 pagesAlternative Medicine Literature Reviewea85vjdw100% (1)
- YadgirDocument6 pagesYadgirHashir PvNo ratings yet
- Buku BiomedikDocument4 pagesBuku BiomedikAchmad Bagus Dwi SNo ratings yet
- 3Document13 pages3Urologi Unpad Februari 2023No ratings yet
- LVS Chronic Pain WsDocument49 pagesLVS Chronic Pain WsdtncorreoNo ratings yet
- Venix Trifold BrochureDocument2 pagesVenix Trifold BrochureCherry San DiegoNo ratings yet
- Anna Garcia Death Timeline 1Document19 pagesAnna Garcia Death Timeline 1api-245176779No ratings yet
- Bronchial HygieneDocument37 pagesBronchial HygieneRayan MohhamadNo ratings yet
- Adrenaline (Anaethesia Tutorial of The Week)Document8 pagesAdrenaline (Anaethesia Tutorial of The Week)Raisa AriesthaNo ratings yet
- Migraine Diagnosis and TreatmentDocument19 pagesMigraine Diagnosis and TreatmentMagdalila Pua RosalesNo ratings yet
- Case Study - Intestinal Resection and Anastomosis in A DogDocument13 pagesCase Study - Intestinal Resection and Anastomosis in A Dogapi-301746262No ratings yet
- Prof Djoko Plenary PDFDocument23 pagesProf Djoko Plenary PDFbagir_dm10No ratings yet
- Drugs Used in AnaesthesiaDocument32 pagesDrugs Used in Anaesthesiav_vijayakanth7656100% (2)
- Bedside Teaching in Clinical MedicineDocument3 pagesBedside Teaching in Clinical Medicineawatif mahadiNo ratings yet
- Diabetes Mellitus Aticle ApthaDocument6 pagesDiabetes Mellitus Aticle ApthaRahul KirkNo ratings yet
- ACLS DrugsDocument16 pagesACLS Drugstostc100% (2)
- Risk Assessment CompletedDocument1 pageRisk Assessment Completedapi-410227491No ratings yet
- What Is SciaticaDocument2 pagesWhat Is Sciaticaha hoangNo ratings yet