Professional Documents
Culture Documents
Gynecologic Surgery: Cesarean Delivery
Gynecologic Surgery: Cesarean Delivery
Uploaded by
cesaliapOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gynecologic Surgery: Cesarean Delivery
Gynecologic Surgery: Cesarean Delivery
Uploaded by
cesaliapCopyright:
Available Formats
Gynecologic Surgery C
190 Cesarean Delivery
Thomas R. Moore
BACKGROUND annually in the United States alone, 100,000 live births. Maternal morbidities as-
making it is the most common surgical sociated with cesarean birth depend on the
Defi nition and History procedure performed on women today. indication for surgical delivery, but include
increased risk of endometritis (up to 20%),
The origin of the term cesarean is unclear,
but the legend of Julius Caesar’s “cesarean” INDICATIONS wound infections, increased blood loss, need
for transfusion (up to 7%), throm-boembolic
birth is unlikely to be true. In those ancient Cesarean delivery may be indicated for fetal events, anesthetic complications, and surgical
times, cesarean delivery was universally fa- and/or maternal reasons, such as failure to complications with damage to bowel,
tal, and Caesar’s mother was known to have progress in labor, fetal malpresentation, pla- bladder, and major pelvic blood vessels.
lived for many years after his birth. The term centa previa, nonreassuring fetal monitor-ing Morbidity is highest in emergency cesarean
may have derived from the Latin words (category II or III by the American Col-lege birth, especially after prolonged labor and/or
caedere (to cut), and caesons (the term for of Obstetricians and Gynecologists (ACOG) ruptured membranes.
children delivered by cesarean), or from the guidelines), suspected macrosomia (greater
Roman law known as Lex Cesare, which than 5,000 g or 4,500 g if diabetic), active
mandated postmortem delivery so the mother infections like herpes simplex virus or high SUBSEQUENT OUTCOMES
and infant could be buried sep-arately. The viral load HIV, vertical uterine incisions from
term “cesarean section” is re-dundant, previous deliveries, and certain fetal Long-term morbidities commonly attrib-uted
derived from the Latin words cae-dere and anomalies such as severe fetal hydrocepha- to cesarean delivery include uterine scar
secare, which both mean “to cut.” lus or fetal neck masses. The majority of ce- dehiscence or rupture, fetal demise and
The evolution of the current surgical sareans are still primary with repeat cesar-ean expulsion from a uterine scar, placenta previa
technique is of interest. Maternal mortality as an indication for 37.5% of all cesarean with or without accreta, increased surgical
rates for cesarean birth prior to the 20th births in 1997. A most controversial topic to- complications from adhesions, bowel
century approached 100% owing to the al- day is the “cesarean-on-demand”—elective, obstruction, bladder injury, and in-creased
most universal uterine sepsis that followed. patient-choice cesarean birth. There are data blood loss during future surgery. Uterine
Consequently, very few cesareans were per- suggesting less urinary incontinence and rupture occurs in subsequent preg-nancy less
formed. Cesarean delivery was combined pelvic organ prolapse after elective ce-sarean, than 1% if a low-transverse uter-ine incision
with hysterectomy in the late 19th century in but the slightly increased morbidity and was done, and up to 12% if a prior vertical
an effort to reduce infection and thus prevent mortality associated with surgical deliv-ery classical uterine incision was performed.
maternal death. Although one in-novation make the risk/benefit ratio for elective Uterine rupture may be an as-ymptomatic
(the “Porro” technique) involved suturing the cesarean difficult to quantify. There is cur- uterine “window” with mini-mal
edges of the uterine incision to the abdominal rently no standard recommendation regard- consequences or may be a catastrophic
wall, allowing the lochia to drain externally ing patient-choice cesarean. ACOG states, expulsion of the fetus into the abdomen with
significantly reduced post-partum sepsis and “Although the evidence does not support the subsequent fetal demise. If risk factors such
death; it was not until well into the 20th routine recommendation of elective cesar-ean as a previous classical uterine incision,
century that advances in surgical suture delivery, we believe that it does support a extensive myomectomy, or more than two
material, aseptic technique, anesthetic physician’s decision to accede to an in- previous low-transverse uterine incisions are
advances, the low-transverse in-cision, and formed patient’s request for such a delivery” present, repeat cesarean delivery prior to the
antibiotics improved the safety of cesarean (ACOG Committee Opinion on Ethics 2003). onset of labor is usually recom-mended. If a
delivery. As a result, cesarean delivery rates vaginal birth after cesarean delivery (VBAC)
is considered, an appropri-ate support team
in the United States increased from 4.5% of
all deliveries in 1965 to 16.5% in 1980 to
RISKS of anesthesiologist, nurse, and pediatrician
24.5% in 1988 to 32% in 2007. Ce-sarean Currently, cesarean delivery has an overall must be available in case an immediate
rates still vary widely with geo-graphic area low maternal mortality and morbidity but is abdominal delivery during labor is necessary.
and type of hospital (i.e., teach-ing vs. still significantly elevated over vaginal deliv- Women undergoing VBAC must be properly
nonteaching). Currently, over 1 million ery. The current cesarean mortality rate in the informed about the potential risks/benefits of
cesarean deliveries are performed United States ranges from 6.1 to 22 per vaginal versus
2013
You might also like
- Cesarian Section Case PresentationDocument26 pagesCesarian Section Case PresentationMae Azores86% (51)
- Nebosh Idip Unit B: B1 Managing Occupational Health 2017Document44 pagesNebosh Idip Unit B: B1 Managing Occupational Health 2017francis100% (1)
- Cap 26 - 1Document26 pagesCap 26 - 1Nancy GuamanNo ratings yet
- Cesarean Delivery: History of The Procedure: The Exact Origin of The Term Cesarean Is Unclear. TheDocument18 pagesCesarean Delivery: History of The Procedure: The Exact Origin of The Term Cesarean Is Unclear. TheCaro Lina Lina100% (1)
- Case StudyDocument7 pagesCase Studymark kennethNo ratings yet
- Obstetricia Iii Placenta AcretaDocument22 pagesObstetricia Iii Placenta AcretaHugo GutiérrezNo ratings yet
- Complications of Caesarean Section: ReviewDocument8 pagesComplications of Caesarean Section: ReviewDesi Purnamasari YanwarNo ratings yet
- Elective Primary Cesarean Delivery: Sounding BoardDocument6 pagesElective Primary Cesarean Delivery: Sounding BoardNicole Grace VillegasNo ratings yet
- Cesarean SectionDocument110 pagesCesarean SectionyordiNo ratings yet
- Disease Intity CsDocument7 pagesDisease Intity CsMary Rose LinatocNo ratings yet
- IntroductionDocument13 pagesIntroductionpurityobotNo ratings yet
- Abnormal PlacentationDocument9 pagesAbnormal PlacentationJack BladeNo ratings yet
- Cesarean Section or Vaginal Delivery in The 21st CenturyDocument2 pagesCesarean Section or Vaginal Delivery in The 21st CenturyLailaNo ratings yet
- Identifying Risk Factors For Uterine RuptureDocument15 pagesIdentifying Risk Factors For Uterine RuptureSakena NurzaNo ratings yet
- Safe Prevention of The Primary CS DeliveryDocument19 pagesSafe Prevention of The Primary CS DeliveryCleoGomezNo ratings yet
- Chapter TwoDocument7 pagesChapter Twohanixasan2002No ratings yet
- Silver 2015Document15 pagesSilver 2015Farlinda AlyaNo ratings yet
- Articulo 8Document15 pagesArticulo 8Monica ReyesNo ratings yet
- Cesarean SectionDocument139 pagesCesarean SectionMisganaw WorkuNo ratings yet
- Caesareans Section Scar Ectopic Pregnancy: An Emerging ChallengeDocument24 pagesCaesareans Section Scar Ectopic Pregnancy: An Emerging Challengenighshift serialsleeperNo ratings yet
- History: Records of The Grand HistorianDocument7 pagesHistory: Records of The Grand HistorianMarienel FuertesNo ratings yet
- EArl Case StudyDocument35 pagesEArl Case StudyAna LuisaNo ratings yet
- Planned Elective Cesarean Section: A Reasonable Choice For Some Women?Document2 pagesPlanned Elective Cesarean Section: A Reasonable Choice For Some Women?miss betawiNo ratings yet
- Caesarian Section: Case PresentationDocument23 pagesCaesarian Section: Case PresentationRiza Angela BarazanNo ratings yet
- Indication For CsDocument20 pagesIndication For CsSandiNo ratings yet
- Caserian SectionDocument100 pagesCaserian SectionsindhujojoNo ratings yet
- Placenta Previa PDFDocument15 pagesPlacenta Previa PDFDamaris GonzálezNo ratings yet
- Cesarean Section Trends and Outcomes in Jinja Regional Referral Hospital A Retrospective AnalysisDocument12 pagesCesarean Section Trends and Outcomes in Jinja Regional Referral Hospital A Retrospective AnalysisKIU PUBLICATION AND EXTENSIONNo ratings yet
- Committee Opinion: Placenta AccretaDocument5 pagesCommittee Opinion: Placenta AccretaagungNo ratings yet
- Jurnal Plasenta Akreta PDFDocument5 pagesJurnal Plasenta Akreta PDFfatqur28No ratings yet
- Trial of Labor After Cesarean (TOLAC)Document16 pagesTrial of Labor After Cesarean (TOLAC)Ricko Handen UriaNo ratings yet
- Sutura CesareasDocument10 pagesSutura CesareasalexNo ratings yet
- Committee Opinion: Placenta AccretaDocument5 pagesCommittee Opinion: Placenta AccretabebetteryesyoucanNo ratings yet
- VBACDocument3 pagesVBACAileen GoNo ratings yet
- Case Study Placenta AccretaDocument6 pagesCase Study Placenta AccretaBecca MirandaNo ratings yet
- Premature Rupture ofDocument4 pagesPremature Rupture ofEllyna EkaNo ratings yet
- Committee Opinion: Scheduled Cesarean Delivery and The Prevention of Vertical Transmission of HIV InfectionDocument4 pagesCommittee Opinion: Scheduled Cesarean Delivery and The Prevention of Vertical Transmission of HIV InfectionHerry SasukeNo ratings yet
- Thesis On Ectopic Pregnancy in IndiaDocument7 pagesThesis On Ectopic Pregnancy in Indiaynwtcpwff100% (2)
- Cesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDocument9 pagesCesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDinorah MarcelaNo ratings yet
- 11 Abnormal PlacentationDocument29 pages11 Abnormal PlacentationMaria Gabriela CristanchoNo ratings yet
- Society For Maternal-Fetal Medicine (SMFM) Consult Series #49: Cesarean Scar PregnancyDocument13 pagesSociety For Maternal-Fetal Medicine (SMFM) Consult Series #49: Cesarean Scar PregnancyTandyo TriasmoroNo ratings yet
- Acreta 2014Document12 pagesAcreta 2014pshz92No ratings yet
- Managing Placenta Accreta: Incidence and PathophysiologyDocument9 pagesManaging Placenta Accreta: Incidence and PathophysiologyAslesa Wangpathi PagehgiriNo ratings yet
- EctopicwDocument9 pagesEctopicwdrnunungNo ratings yet
- Predicting Cesarean Section AnDocument5 pagesPredicting Cesarean Section AnKEANNA ZURRIAGANo ratings yet
- IOSRPHRDocument3 pagesIOSRPHRIOSR Journal of PharmacyNo ratings yet
- C-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Document7 pagesC-Obs 38 Planned Vaginal Birth After C-Section New Jul 10Aris SugiatnoNo ratings yet
- Reading Part A CaesareanDocument6 pagesReading Part A Caesareanfernanda1rondelliNo ratings yet
- Cesarean Section Vbac: January, 2009Document43 pagesCesarean Section Vbac: January, 2009DanduuNo ratings yet
- The Back Alley Revisited: Sepsis After Attempted Self-Induced AbortionDocument3 pagesThe Back Alley Revisited: Sepsis After Attempted Self-Induced Abortionmila nurmalaNo ratings yet
- Prevencion CesareaDocument19 pagesPrevencion CesareaNatalia MartínezNo ratings yet
- Khing Journal...Document5 pagesKhing Journal...Khing AbatNo ratings yet
- Caesarean Section at Full Dilatation: Incidence, Impact and Current ManagementDocument20 pagesCaesarean Section at Full Dilatation: Incidence, Impact and Current ManagementAbdur RaheemNo ratings yet
- Vaginal Birth After Caeserean Section: BY Seun ODocument24 pagesVaginal Birth After Caeserean Section: BY Seun OOlaiya OluwaseunNo ratings yet
- Article 262063-PrintDocument15 pagesArticle 262063-PrintAhsan AuliyaNo ratings yet
- Moxibustion To Correct A Breech Presentation of The Fetus Author IDEASSDocument13 pagesMoxibustion To Correct A Breech Presentation of The Fetus Author IDEASSVraciul din VeciniNo ratings yet
- Vesico-Vaginal Fistulas in Developing Countries: P.HiltonDocument11 pagesVesico-Vaginal Fistulas in Developing Countries: P.HiltonRakha Sulthan SalimNo ratings yet
- C Cection 8Document43 pagesC Cection 8blatchujosephNo ratings yet
- Jurnal Obgyn 2018 2Document15 pagesJurnal Obgyn 2018 2aulNo ratings yet
- 2015 Sep Embarazo Múltiple - Vía Del Parto.Document13 pages2015 Sep Embarazo Múltiple - Vía Del Parto.Alexander Gonzalez BarturenNo ratings yet
- Atypical Breast Proliferative Lesions and Benign Breast DiseaseFrom EverandAtypical Breast Proliferative Lesions and Benign Breast DiseaseFarin AmersiNo ratings yet
- Tabel Perhitungan McuaDocument8 pagesTabel Perhitungan McuacesaliapNo ratings yet
- Part IX: Vascular Surgery: Renal and Spinal Cord ProtectionDocument1 pagePart IX: Vascular Surgery: Renal and Spinal Cord ProtectioncesaliapNo ratings yet
- Diagnostic Management of The Clinically Localized Ovarian MassDocument1 pageDiagnostic Management of The Clinically Localized Ovarian MasscesaliapNo ratings yet
- Vertebral Arteries: Common Carotid, Internal Carotid, and External Carotid ArteriesDocument1 pageVertebral Arteries: Common Carotid, Internal Carotid, and External Carotid ArteriescesaliapNo ratings yet
- Generations of The Plug-and-Patch Repair: Its Development and Lessons From HistoryDocument1 pageGenerations of The Plug-and-Patch Repair: Its Development and Lessons From HistorycesaliapNo ratings yet
- Results of A Personal Series: Femoral VesselsDocument1 pageResults of A Personal Series: Femoral VesselscesaliapNo ratings yet
- Part VIII: Nongastrointestinal Transabdominal Surgery: Intraperitoneal Mesh RepairDocument1 pagePart VIII: Nongastrointestinal Transabdominal Surgery: Intraperitoneal Mesh RepaircesaliapNo ratings yet
- Been Abandoned in Favor of Hetero-/ortho-Topic Pouches.: Heterotopic Continent DiversionDocument1 pageBeen Abandoned in Favor of Hetero-/ortho-Topic Pouches.: Heterotopic Continent DiversioncesaliapNo ratings yet
- Chapter 193: Surgical Management of Ovarian Carcinoma: Sup. Rectal A. and VDocument1 pageChapter 193: Surgical Management of Ovarian Carcinoma: Sup. Rectal A. and VcesaliapNo ratings yet
- Part VIII: Nongastrointestinal Transabdominal SurgeryDocument1 pagePart VIII: Nongastrointestinal Transabdominal SurgerycesaliapNo ratings yet
- Cooper Ligament Repair of Groin Hernias: Robb H. RutledgeDocument1 pageCooper Ligament Repair of Groin Hernias: Robb H. RutledgecesaliapNo ratings yet
- Part VIII: Nongastrointestinal Transabdominal SurgeryDocument1 pagePart VIII: Nongastrointestinal Transabdominal SurgerycesaliapNo ratings yet
- Ileal Pouches: Chapter 189: Supravesical Urinary DiversionDocument1 pageIleal Pouches: Chapter 189: Supravesical Urinary DiversioncesaliapNo ratings yet
- Remove Them Within A Week. Mainz Neobladder: Chapter 189: Supravesical Urinary DiversionDocument1 pageRemove Them Within A Week. Mainz Neobladder: Chapter 189: Supravesical Urinary DiversioncesaliapNo ratings yet
- Page 2087Document1 pagePage 2087cesaliapNo ratings yet
- Page 2089Document1 pagePage 2089cesaliapNo ratings yet
- Supravesical Urinary Diversion: Badrinath Konety and Sean P. ElliottDocument1 pageSupravesical Urinary Diversion: Badrinath Konety and Sean P. ElliottcesaliapNo ratings yet
- Pencarian Bukti IlmiahDocument2 pagesPencarian Bukti IlmiahcesaliapNo ratings yet
- Cagayan de Oro CityDocument6 pagesCagayan de Oro CityRaymond AbejuelaNo ratings yet
- How Physical Education Contribute To Young People's Physical Activity Level?Document2 pagesHow Physical Education Contribute To Young People's Physical Activity Level?Jessica Alcala Dela TorreNo ratings yet
- English Research PaperDocument6 pagesEnglish Research Paperapi-390838152No ratings yet
- COVID-19-Return To Work-Workplace Hygiene PolicyDocument2 pagesCOVID-19-Return To Work-Workplace Hygiene PolicyNilamSanjeev Kumar SinghNo ratings yet
- Time Table FCCS OB 13 - 14 Maret SbyDocument4 pagesTime Table FCCS OB 13 - 14 Maret SbyLina SusantiNo ratings yet
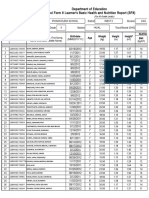
- Department of Education School Form 8 Learner's Basic Health and Nutrition Report (SF8)Document4 pagesDepartment of Education School Form 8 Learner's Basic Health and Nutrition Report (SF8)Roxan DosdosNo ratings yet
- Tribal Health in IndiaDocument14 pagesTribal Health in IndiaGautam G JNo ratings yet
- Sharfaa Ahmad Current ResumeDocument2 pagesSharfaa Ahmad Current Resumeapi-302596118No ratings yet
- Preparing Military Installations For Pandemic Infl Uenza Through Tabletop ExercisesDocument7 pagesPreparing Military Installations For Pandemic Infl Uenza Through Tabletop ExercisesEduardo Sousa SantosNo ratings yet
- Maternal Death Review: Need For Taking It UpDocument18 pagesMaternal Death Review: Need For Taking It UpPrabir Kumar ChatterjeeNo ratings yet
- RubelaDocument11 pagesRubelaMuhammad YusriNo ratings yet
- 2020 Article 363Document8 pages2020 Article 363RIAN NUGRAHANo ratings yet
- Task 11 EQUIPMENT MAINTENANCE SCHEDULEDocument1 pageTask 11 EQUIPMENT MAINTENANCE SCHEDULEMary Mel GarciaNo ratings yet
- Data Individu 1033017Document14 pagesData Individu 1033017Setyowati DwiNo ratings yet
- Criteria Donor of BloodDocument3 pagesCriteria Donor of Bloodapi-269388039No ratings yet
- Nurse Np1 Board CramsheetDocument8 pagesNurse Np1 Board CramsheetZero TwoNo ratings yet
- Infant and Young Child Feeding (IYCF) Practices in Udupi District, KarnatakaDocument7 pagesInfant and Young Child Feeding (IYCF) Practices in Udupi District, KarnatakaANna Laila Mardiana RNo ratings yet
- Neonatal SepsisDocument10 pagesNeonatal SepsisClaudelí GonzalezNo ratings yet
- Knowledge and Practices of Nurses in Infection Prevention and Control Within A Tertiary Care HospitalDocument4 pagesKnowledge and Practices of Nurses in Infection Prevention and Control Within A Tertiary Care HospitalAnonymous TzvMOnNo ratings yet
- Cermin Dunia Kedokteran, No 151. 2006. P: 14-17: Daftar PustakaDocument2 pagesCermin Dunia Kedokteran, No 151. 2006. P: 14-17: Daftar PustakaLaila Kurnia PramonoNo ratings yet
- Cosh CERT - FACILITATORDocument7 pagesCosh CERT - FACILITATORRedentor B. Rayla100% (1)
- Sex EducationDocument2 pagesSex EducationPatricia Bawiin †No ratings yet
- 11 - Recurrent UTI TOG 2020Document7 pages11 - Recurrent UTI TOG 2020Anna JuniedNo ratings yet
- ICD 10 CM Official Coding Gudance Interim Advice Coronavirus Feb 20 2020 PDFDocument3 pagesICD 10 CM Official Coding Gudance Interim Advice Coronavirus Feb 20 2020 PDFSumiwaty PanNo ratings yet
- Syndromic Management of STDsDocument13 pagesSyndromic Management of STDsMeenachi S100% (1)
- 15-17 - 7-PDF - Community Medicine With Recent Advances - 3 PDFDocument3 pages15-17 - 7-PDF - Community Medicine With Recent Advances - 3 PDFdwimahesaputraNo ratings yet
- Folder 10 BNAPDocument5 pagesFolder 10 BNAPRUDIRICK SIMBILINGNo ratings yet
- Hamilton County Infant Mortality RatesDocument3 pagesHamilton County Infant Mortality RatesWCPO 9 NewsNo ratings yet
- Standard Precautions 1Document34 pagesStandard Precautions 1Melody LandichoNo ratings yet