Professional Documents
Culture Documents
100%(1)100% found this document useful (1 vote)
199 viewsHematology Reviewer
Hematology Reviewer
Uploaded by
Abigail PunoThis document defines hematology and describes the blood system and its components. It discusses hematopoiesis, the development of blood cells, and the microanatomy of the bone marrow where blood cell formation takes place. It also outlines the different blood cell lines, how stem cells are studied to understand hematopoiesis, and the metabolism and energy requirements of red blood cells.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- Patient SafetyDocument8 pagesPatient SafetyKelly J Wilson0% (1)
- RENR Pass Paper With Answers August 4Document20 pagesRENR Pass Paper With Answers August 4Lateisha Ragguette100% (4)
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Microbio Lab 8Document4 pagesMicrobio Lab 8api-3743217100% (5)
- Inclusions HematologyDocument3 pagesInclusions HematologyMurreh100% (3)
- Step 2 NotesDocument202 pagesStep 2 NotesNaved Rahman100% (2)
- PB Assist +: Probiotic Defense FormulaDocument4 pagesPB Assist +: Probiotic Defense FormulaEduardo TakemuraNo ratings yet
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CDocument10 pagesRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- HematologyDocument5 pagesHematologyIvy Jan OcateNo ratings yet
- Top 10 AnemiasDocument24 pagesTop 10 AnemiasSim M ChangNo ratings yet
- Disorders of Iron Kinetics and Heme MetabolismDocument12 pagesDisorders of Iron Kinetics and Heme MetabolismJoanne JardinNo ratings yet
- HematologyDocument42 pagesHematologyadaako100% (8)
- Hematology PDFDocument46 pagesHematology PDFGiannis GkouzionisNo ratings yet
- Chapter 1: An Overview of Clinical LaboratoryDocument13 pagesChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Hematology 2 Lecture Notes Platelet Quantitative DisordersDocument10 pagesHematology 2 Lecture Notes Platelet Quantitative DisorderscccomayogNo ratings yet
- Aubf Questions With AnswersDocument16 pagesAubf Questions With AnswersFenyl Isis GuigayomaNo ratings yet
- Blood BankDocument32 pagesBlood Bankpikachu100% (1)
- Immunology Serology Review COMPLETEDocument30 pagesImmunology Serology Review COMPLETEEuliz G.100% (1)
- Clinical Chemistry Notes (Blanked) - ABI PDFDocument34 pagesClinical Chemistry Notes (Blanked) - ABI PDFAnya IgnacioNo ratings yet
- Immunology & Serology: Preliminaries: Romie Solacito, MLS3CDocument12 pagesImmunology & Serology: Preliminaries: Romie Solacito, MLS3CRomie Solacito100% (2)
- CHEM 2 CH 29 Review QuestionsDocument2 pagesCHEM 2 CH 29 Review QuestionsthrowawyNo ratings yet
- Serologic Tests Part 1Document4 pagesSerologic Tests Part 1Joshua TrinidadNo ratings yet
- Hematology Tables Morphology of RBCsDocument5 pagesHematology Tables Morphology of RBCsGlydenne Glaire Poncardas GayamNo ratings yet
- Must To Know HemaDocument44 pagesMust To Know HemaKaycee Gretz LorescaNo ratings yet
- Clinical Chemistry 2Document6 pagesClinical Chemistry 2Romie SolacitoNo ratings yet
- RBC MorphologyDocument9 pagesRBC MorphologybiancsNo ratings yet
- LN Hematology MLT FinalDocument549 pagesLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Compatibility Testing - BloodDocument5 pagesCompatibility Testing - BloodMunish DograNo ratings yet
- Summary in Histopath (Stain)Document15 pagesSummary in Histopath (Stain)Bless MarieNo ratings yet
- Correctly: IncorrectlyDocument70 pagesCorrectly: IncorrectlyDjdjjd Siisus100% (1)
- 05 HaematologyDocument9 pages05 HaematologyMayur WakchaureNo ratings yet
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 pagesA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNo ratings yet
- RBC AnomaliesDocument10 pagesRBC AnomaliesSHUPATUSSAINo ratings yet
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Clinical Chemistry (Lecture) - PrelimsDocument12 pagesClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- Maximo Lemar CMDocument31 pagesMaximo Lemar CMAdrian MaterumNo ratings yet
- HematologyDocument28 pagesHematologyGNiqM0% (1)
- Clin Path Lab 6 UrinalysisDocument5 pagesClin Path Lab 6 Urinalysisapi-3743217100% (6)
- Blood ComponentsDocument51 pagesBlood ComponentsMandy A. Delfin100% (1)
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- AUB - Microscopic Analysis of UrineDocument4 pagesAUB - Microscopic Analysis of UrineJeanne Rodiño100% (1)
- GeneralDocument31 pagesGeneralpikachu100% (1)
- MUST To KNOW in Blood Banking 1Document19 pagesMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- Hematology ReviewerDocument10 pagesHematology ReviewerAldren BeliberNo ratings yet
- Week 2 Chemical Examination of UrineDocument44 pagesWeek 2 Chemical Examination of UrineDayledaniel SorvetoNo ratings yet
- CBC Reviewer Anaphy LabDocument9 pagesCBC Reviewer Anaphy LabARVINE JUSTINE CORPUZNo ratings yet
- Hematology Final ExamDocument20 pagesHematology Final ExamAlon GoldfainerNo ratings yet
- Clinical Chemistry Board ReviewDocument14 pagesClinical Chemistry Board ReviewWellaBaylasNo ratings yet
- Red Blood Cells "Best Module Ever"Document4 pagesRed Blood Cells "Best Module Ever"Jose Emmanuel Dolor100% (1)
- Blood Banking Course BookDocument2 pagesBlood Banking Course BookShukr Wesman BlbasNo ratings yet
- Chapter 13 Rodaks HematologyDocument10 pagesChapter 13 Rodaks HematologyRALPH JAN T. RIONo ratings yet
- Recall 1Document4 pagesRecall 1pikachuNo ratings yet
- MUST To KNOW in Medical Technology Laws EthicsDocument2 pagesMUST To KNOW in Medical Technology Laws Ethicsjohnkuys75% (4)
- Liver Function (Clinical Chemistry)Document11 pagesLiver Function (Clinical Chemistry)Patricia Perfecto100% (1)
- Post Lab 01-09Document7 pagesPost Lab 01-09Patrick ParconNo ratings yet
- CSMLS Exam Guide Notes (Referrence Range)Document4 pagesCSMLS Exam Guide Notes (Referrence Range)software4us.2023No ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Fast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsFrom EverandFast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Multiple Choice Questions for Haematology and Core Medical TraineesFrom EverandMultiple Choice Questions for Haematology and Core Medical TraineesNo ratings yet
- Differentiate Between With AnswersDocument14 pagesDifferentiate Between With AnswersStephy SojanNo ratings yet
- ANUGRAH DHARMA HISTORY Duta Berkat Revisi 2 GambarDocument71 pagesANUGRAH DHARMA HISTORY Duta Berkat Revisi 2 GambarAndri aryanataNo ratings yet
- Opthalmology Short NotesDocument14 pagesOpthalmology Short NotesChristine Nancy Ng100% (1)
- Mild Cognitive Impairment - Beyond Controversies, Towards A Consensus: Report of The International Working Group On Mild Cognitive ImpairmentDocument7 pagesMild Cognitive Impairment - Beyond Controversies, Towards A Consensus: Report of The International Working Group On Mild Cognitive ImpairmentRoxana SanduNo ratings yet
- NCP Epidural HemDocument32 pagesNCP Epidural HemKatrina PonceNo ratings yet
- Literature Review-3Document5 pagesLiterature Review-3api-519320140No ratings yet
- The Korean 4 Point SystemDocument1 pageThe Korean 4 Point SystemHuib SalomonsNo ratings yet
- Basic Counseling Skills For Addiction Professionals: Module 1-Training IntroductionDocument36 pagesBasic Counseling Skills For Addiction Professionals: Module 1-Training IntroductionlissarlissaaNo ratings yet
- Surgical Diseases of The EsophagusDocument35 pagesSurgical Diseases of The Esophagusmogesie1995No ratings yet
- Improvement of The Rubber Dam FrameDocument3 pagesImprovement of The Rubber Dam FrameTiagoNo ratings yet
- What Is Pancreatic Cancer?: Primary-MetastaticDocument2 pagesWhat Is Pancreatic Cancer?: Primary-MetastaticValiant BaybayNo ratings yet
- Q2 Health9 Drug ScenarioDocument54 pagesQ2 Health9 Drug Scenarionova rhea garciaNo ratings yet
- Chapter 47 Diabetes Mellitus PDFDocument14 pagesChapter 47 Diabetes Mellitus PDFRLLT100% (1)
- Immediate Newborn Care: The First 90 Minutes: Preparing For The Birth (Continued)Document33 pagesImmediate Newborn Care: The First 90 Minutes: Preparing For The Birth (Continued)Zimm RrrrNo ratings yet
- Mov3. GENERAL - UMN (Pyramidal) & LMN DisordersDocument9 pagesMov3. GENERAL - UMN (Pyramidal) & LMN DisordersherlambangkusumoNo ratings yet
- Body Temperature and How To Measure ItDocument6 pagesBody Temperature and How To Measure ItMeyin LowNo ratings yet
- KARDEXDocument2 pagesKARDEXNicole Audrey JoaquinNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument6 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyAhmed AliNo ratings yet
- Medical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusDocument90 pagesMedical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusJonalynCollodChewacheoNo ratings yet
- Answer: C) End Tidal CO: - Total Comments: 0Document16 pagesAnswer: C) End Tidal CO: - Total Comments: 0Mysheb SS100% (1)
- Diabetes and Virgin Coconut Oil DR Bruce FifeDocument3 pagesDiabetes and Virgin Coconut Oil DR Bruce Fifepetri_jv100% (1)
- What Is Acute BronchitisDocument11 pagesWhat Is Acute BronchitisKerri-DojhnHallNo ratings yet
- Radionic CardsDocument2 pagesRadionic CardsRoberta & Thomas NormanNo ratings yet
- Lipo Stab Il Injection TechniqueDocument3 pagesLipo Stab Il Injection TechniqueMIAPISNo ratings yet
- International Guide To Prescribing Psychotropic Medication For The Management of Problem Behaviours in Adults With Intellectual DisabilitiesDocument6 pagesInternational Guide To Prescribing Psychotropic Medication For The Management of Problem Behaviours in Adults With Intellectual DisabilitiesShalawatyAbdkarimNo ratings yet
- Galson MENTALHEALTHMATTERS 2009Document4 pagesGalson MENTALHEALTHMATTERS 2009PSNo ratings yet
Hematology Reviewer
Hematology Reviewer
Uploaded by
Abigail Puno100%(1)100% found this document useful (1 vote)
199 views4 pagesThis document defines hematology and describes the blood system and its components. It discusses hematopoiesis, the development of blood cells, and the microanatomy of the bone marrow where blood cell formation takes place. It also outlines the different blood cell lines, how stem cells are studied to understand hematopoiesis, and the metabolism and energy requirements of red blood cells.
Original Description:
Diseases
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document defines hematology and describes the blood system and its components. It discusses hematopoiesis, the development of blood cells, and the microanatomy of the bone marrow where blood cell formation takes place. It also outlines the different blood cell lines, how stem cells are studied to understand hematopoiesis, and the metabolism and energy requirements of red blood cells.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
100%(1)100% found this document useful (1 vote)
199 views4 pagesHematology Reviewer
Hematology Reviewer
Uploaded by
Abigail PunoThis document defines hematology and describes the blood system and its components. It discusses hematopoiesis, the development of blood cells, and the microanatomy of the bone marrow where blood cell formation takes place. It also outlines the different blood cell lines, how stem cells are studied to understand hematopoiesis, and the metabolism and energy requirements of red blood cells.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 4
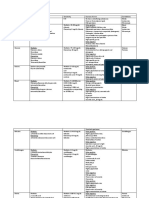
DEFINITION AND SCOPE OF HEMATOLOGY HEMATOPOIESIS
FUNCTIONS OF THE BLOOD SYSTEM DEVELOPMENT
1. Transport 1. Erythropoiesis
2. Temperature regulation 2. Leukopoiesis
3. Immunity 3. Thrombopoiesis
4. Communication
5. Defense MORPHOGENESIS
a. ONTOGENY: embryonic development
BLOOD COMPONENTS 1. Primitive (mesenchymal cells)
1. LIQUID: Plasma 55% i. Yolk sac: 3rd-4th week
a. Water 2. Definitive
b. Electrolytes i. Liver: 3rd month, main
c. Plasma proteins ii. Spleen: 3rd month
i. Acc. to function: enzymes, antibodies, iii. Bone marrow: starts at 4th, main
coag, fibrinolytic by 6th month
ii. Acc. to structure: simple & complex iv. Lymph nodes & thymus: 4th,
proteins secondary source of lymphocytes MICROANATOMY OF THE BONE MARROW
iii. Acc. to water solubility: albumins, throughout life Mesenchymal cells stem cell for connective
globulins tissues and blood cells
Major Functions 3. Notes: Hemocytoblasts pluripotent (give rise to all
o Transport: carrier proteins Liver and spleen: has residual blood cell lines), contained only in the bone
o Regulation of water movement: albumin hematopoietic capacity, revert to marrow after birth
o Coagulation: fibrinogen, fibrinolytic factors embryonic role if needed Foramina ducts where arteries enter the bone
o Immunoglobulins (antibodies): γ Medullary hematopoiesis: in bone Sinusoids substitute for capillary beds
o Inflammation marrow, all bones til 25 26 Wheel with spokes (sinusoids) and a central hub
2. SOLID onwards, happen in flat bones (vein) bone marrow cross-section
a. Red Blood Cells (erythrocytes) 45% Extramedullary hematopoiesis: Marrow stroma where blood cell formation take
b. White Blood Cells (leukocytes) <1% outside bone marrow lymph place (extravascular)
i. Granulocytes (acc to cytoplasmic nodes, liver, spleen Sinusoidal wall layers
granules) b. PHYLOGENY: evolution o Endothelial cells (internal)
1. Neutrophils c. HISTOLOGY: maturation o Basement membrane (middle)
2. Eosinophils Undifferentiated mesenchymal reticular cell o Adventitial reticular cells (outer)
3. Basophils pluripotent stem cell (hemocytoblast) myeloid, o Where the reticulocyte squeeze out and
ii. Lymphocytes (acc to fxn) lymphoid nucleus is removed circulation
1. B cells plasma cells Bone marrow
2. T cells o Red marrow hematopoietic tissue, ribs
a. Cytotoxic T-cells and sternum of young adults
b. Helper T cells o Yellow marrow fatty tissue, increased
c. Natural Killer Cells as a person ages, long bones of adults
3. Monocytes
c. Platelets (thrombocytes) <1%
TWO METHODS OF BONE MARROW STUDY BLOOD CELL LINES HB, BLOOD TRANSPORT
1. Aspiration Lymphoid-myeloid CFU
Needle inserted posterior iliac crest (adult)/ tibia o Lymphoid-CFU
(infant) small quantity of tissue smeared, Pre-B cell B cell plasma cell
fixed, stained and examined Pre-T cell
Disturbs bone marrow architecture for types NK cell
and number of cells Helper T cell
2. Biopsy Cytotoxic T cell
Biopsy needle into iliac crest Piece of bone o GEMM-CFU (Granulocyte-Erythrocyte-
marrow fixed, embedded in paraffin, examined magakaryocyte-monocyte)
Traumatic and dangerous better picture of the Erythroid-CFU RBC
real structure Granulocyte-monocyte-CFU
G-CFU neutrophil
STUDYING STEM CELLS & HEMATOPOEISIS M-CFU monocyte
Colony-Forming Units: identify and count stem cells then macrophage
o Hematologically empty mice bone Eosinophilic-CFU Eosinophil
marrow cells undifferentiated Basophil-CFU Basophil
myeloid or lymphoid SC Megakaryocyte-CFU platelets
Stem Cell Kinetics
Characteristics
o Self-maintaining divide into daughter
cells with parent capabilities
o Can differentiate
Renewal Theories
o Asymmetric cell division
o Replacement by progeny of other
pluripotent stem cells
Cytokinetics
o Study of the method by which blood cells
proliferate (constantly dividing and proliferate on demand)
Mass or size (total #)
Maturation
Life span
Turnover rate Growth Factors
o Colony Stimulating Factors (CSF)
GM-CSF: G-CSF, M-CSF
o Interleukins: IL-3, IL-4, IL-5, IL-6, IL-7, IL-9
o Erythropoeitin (EPO)
Cytokine, secreted by the kidney in response
to cellular hypoxia (non-steady state)
stimulates red blood cell production in the
bone marrow
METABOLISM AND FATE OF RBC RBC GLUCOSE-CONVERSION PATHWAYS:
RBCs get energy only from GLUCOSE Anaerobic Glycolysis 1. Embden-Meyerhof (EM) Pathway (Anaerobic
(ATP) and Pentose Phosphate Pathway (NADPH) Pathway)
Utilizes 90-95% of all the glucose
ENERGY REQUIREMENTS OF RBC Supplies 75% of the cell’s energy
Energy required for: Produce:
1. Keeping cation (Na, Ca) pumps going o All the ATP (2ATPs/ glucose mol)
2. Generation of NAD+ needed to produce NADH o NADH
- NADH: (a) provides NADH the energy for o 2,3 BPG
conversion of pyruvate to lactate; (b) helps in Why anaerobic RBC lack mitochondria,
regulation of the methemoglobin reduction prevent aerobic oxidation glucose &
system pyruvate
3. Generation of NADP+ needed to produce NADPH Phosphorylation: before glucose is broken
- NADPH: (a) generated via PPP (or Pentose down, ATP ADP
Monophosphate shunt/ Hexose Glucose pyruvate
monophosphate shunt) (b) major energy source Net gain: 2 ATP, 2 NADH (reduced, energy-
in keeping Hb in reduced state (Fe2+, if Fe3+, carrying)
cannot transport oxygen) 2. Hexose monophosphate shunt (HMS)/ Pentose
4. Generation of 2,3 BPG Phosphate Pathway (PPP)
- 2,3 BPG: essential ingredient for proper Utilizes 5-10% of the glucose
functioning of Hb as oxygen carrier Supplies 25% of the potential energy of
5. Maintenance of RBC shape (biconcave discs) the cell
Produce: All NADPH
GLUCOSE METABOLISM IN RBCS
NADP NADPH (involves enzyme G6PD)
Energy molecules:
NADPH
1. ATP
o Keep glutathione in reduced-state
a. Run the cationic pumps (Na+ & Ca+) to maintain
o Reduced-gluta major role in
the osmotic balance of erythrocytes
prolonging life of RBCs (~120days)
b. Keep the cell membrane in good shape
o Any defect in PPP early RBC
by ensuring proper lipid turnover
hemolysis
by phosphorylation of membrane proteins
c. providing phosphates needed to prime the
Embden-Meyerhof pathway (anaerobic
SURVIVAL
pathway)
d. contributing the active phosphates (NADH
NADPH)
2. NADH: antioxidant function reduces hydrogen
peroxide
3. NADPH: antioxidant function reduces
glutathione
Classification of Anemia
1. MORPHOLOGY B. Impairment in the maturation of new RBCs
I. Size (MCV): normo/macro/microcytic 1. Macrocytic-normochromic
II. Hb concentration (MCHC): a. Folic acid deficiency (Megaloblastic
normo/hypo/hyperchromic anemia)
A. Normocytic-normochromic b. Vitamin B12 deficiency (Megaloblastic
1. Bleeding anemia)
2. Bone marrow failure 2. Microcytic-hypochromic
- Hypo-proliferation of hematopoietic stem a. Iron deficiency (Iron deficiency
cells in the bone marrow (aplastic anemias, anemia)
anemia of chronic renal failure, b. unavailability of iron to blast cells
myelophthisic anemia) (anemia of chronic disease)
3. Toxic depression of the bone marrow c. impaired heme synthesis
(hemolytic anemias) (sideroblastic anemia)
B. Microcytic-hypochromic d. impaired globin synthesis
1. Iron deficiency anemia (thalassemia syndromes)
2. Sideroblastic anemia II. II. Increased RBC loss
C. Macrocytic- normochromic A. Hemorrhage: acute or chronic
1. Megaloblastic anemia B. Intravascular hemolysis
2. Certain hemolytic anemias 1. Hereditary factors
a. Defects in RBC membrane (hereditary
2. ETIOLOGY spherocytosis/elliptocytosis)
I. Decreased RBC production b. Defect in RBC metabolism (G-6-PD
A. Decreased proliferation deficiency anemia)
1. Decreased EPO c. Abnormal Hgb production (sickle cell
a. Impaired production by the kidney anemia, HbC disease, HbD disease,
(anemia of renal failure) HbE disease)
b. low oxygen requirement (anemia of 2. Acquired accelerated hemolysis
endocrine disease) a. Activation of the immune system
c. impaired stem cell response to EPO (hemolytic anemia)
2. Bone marrow damage/defect b. Physical factors (red cell
a. replacement of normal marrow by fragmentation syndromes)
tumor (Myelophthisic anemia) c. Chemical agents (various forms of
b. replacement of normal marrow by hemolytic anemia)
cancerous cell line (anemia d. Microorganisms (various forms of
associated with myeloproliferative anemia e.g. anemia of malaria)
disease) e. Secondary to other diseases (various
c. damage to bone marrow by physical, forms of anemia e.g. anemia of
chemical or infectious agents (aplastic hepatic failure)
anemia) f. Sensitivity to complement
d. inherited bone marrow defect (paroxysmal nocturnal
(Fanconi’s anemia) hemoglobinuria)
You might also like
- Patient SafetyDocument8 pagesPatient SafetyKelly J Wilson0% (1)
- RENR Pass Paper With Answers August 4Document20 pagesRENR Pass Paper With Answers August 4Lateisha Ragguette100% (4)
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Microbio Lab 8Document4 pagesMicrobio Lab 8api-3743217100% (5)
- Inclusions HematologyDocument3 pagesInclusions HematologyMurreh100% (3)
- Step 2 NotesDocument202 pagesStep 2 NotesNaved Rahman100% (2)
- PB Assist +: Probiotic Defense FormulaDocument4 pagesPB Assist +: Probiotic Defense FormulaEduardo TakemuraNo ratings yet
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CDocument10 pagesRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- HematologyDocument5 pagesHematologyIvy Jan OcateNo ratings yet
- Top 10 AnemiasDocument24 pagesTop 10 AnemiasSim M ChangNo ratings yet
- Disorders of Iron Kinetics and Heme MetabolismDocument12 pagesDisorders of Iron Kinetics and Heme MetabolismJoanne JardinNo ratings yet
- HematologyDocument42 pagesHematologyadaako100% (8)
- Hematology PDFDocument46 pagesHematology PDFGiannis GkouzionisNo ratings yet
- Chapter 1: An Overview of Clinical LaboratoryDocument13 pagesChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Hematology 2 Lecture Notes Platelet Quantitative DisordersDocument10 pagesHematology 2 Lecture Notes Platelet Quantitative DisorderscccomayogNo ratings yet
- Aubf Questions With AnswersDocument16 pagesAubf Questions With AnswersFenyl Isis GuigayomaNo ratings yet
- Blood BankDocument32 pagesBlood Bankpikachu100% (1)
- Immunology Serology Review COMPLETEDocument30 pagesImmunology Serology Review COMPLETEEuliz G.100% (1)
- Clinical Chemistry Notes (Blanked) - ABI PDFDocument34 pagesClinical Chemistry Notes (Blanked) - ABI PDFAnya IgnacioNo ratings yet
- Immunology & Serology: Preliminaries: Romie Solacito, MLS3CDocument12 pagesImmunology & Serology: Preliminaries: Romie Solacito, MLS3CRomie Solacito100% (2)
- CHEM 2 CH 29 Review QuestionsDocument2 pagesCHEM 2 CH 29 Review QuestionsthrowawyNo ratings yet
- Serologic Tests Part 1Document4 pagesSerologic Tests Part 1Joshua TrinidadNo ratings yet
- Hematology Tables Morphology of RBCsDocument5 pagesHematology Tables Morphology of RBCsGlydenne Glaire Poncardas GayamNo ratings yet
- Must To Know HemaDocument44 pagesMust To Know HemaKaycee Gretz LorescaNo ratings yet
- Clinical Chemistry 2Document6 pagesClinical Chemistry 2Romie SolacitoNo ratings yet
- RBC MorphologyDocument9 pagesRBC MorphologybiancsNo ratings yet
- LN Hematology MLT FinalDocument549 pagesLN Hematology MLT FinalMahfuzur Rahman100% (3)
- Compatibility Testing - BloodDocument5 pagesCompatibility Testing - BloodMunish DograNo ratings yet
- Summary in Histopath (Stain)Document15 pagesSummary in Histopath (Stain)Bless MarieNo ratings yet
- Correctly: IncorrectlyDocument70 pagesCorrectly: IncorrectlyDjdjjd Siisus100% (1)
- 05 HaematologyDocument9 pages05 HaematologyMayur WakchaureNo ratings yet
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 pagesA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNo ratings yet
- RBC AnomaliesDocument10 pagesRBC AnomaliesSHUPATUSSAINo ratings yet
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Clinical Chemistry (Lecture) - PrelimsDocument12 pagesClinical Chemistry (Lecture) - Prelimsisprikitik3100% (1)
- Maximo Lemar CMDocument31 pagesMaximo Lemar CMAdrian MaterumNo ratings yet
- HematologyDocument28 pagesHematologyGNiqM0% (1)
- Clin Path Lab 6 UrinalysisDocument5 pagesClin Path Lab 6 Urinalysisapi-3743217100% (6)
- Blood ComponentsDocument51 pagesBlood ComponentsMandy A. Delfin100% (1)
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- AUB - Microscopic Analysis of UrineDocument4 pagesAUB - Microscopic Analysis of UrineJeanne Rodiño100% (1)
- GeneralDocument31 pagesGeneralpikachu100% (1)
- MUST To KNOW in Blood Banking 1Document19 pagesMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- Hematology ReviewerDocument10 pagesHematology ReviewerAldren BeliberNo ratings yet
- Week 2 Chemical Examination of UrineDocument44 pagesWeek 2 Chemical Examination of UrineDayledaniel SorvetoNo ratings yet
- CBC Reviewer Anaphy LabDocument9 pagesCBC Reviewer Anaphy LabARVINE JUSTINE CORPUZNo ratings yet
- Hematology Final ExamDocument20 pagesHematology Final ExamAlon GoldfainerNo ratings yet
- Clinical Chemistry Board ReviewDocument14 pagesClinical Chemistry Board ReviewWellaBaylasNo ratings yet
- Red Blood Cells "Best Module Ever"Document4 pagesRed Blood Cells "Best Module Ever"Jose Emmanuel Dolor100% (1)
- Blood Banking Course BookDocument2 pagesBlood Banking Course BookShukr Wesman BlbasNo ratings yet
- Chapter 13 Rodaks HematologyDocument10 pagesChapter 13 Rodaks HematologyRALPH JAN T. RIONo ratings yet
- Recall 1Document4 pagesRecall 1pikachuNo ratings yet
- MUST To KNOW in Medical Technology Laws EthicsDocument2 pagesMUST To KNOW in Medical Technology Laws Ethicsjohnkuys75% (4)
- Liver Function (Clinical Chemistry)Document11 pagesLiver Function (Clinical Chemistry)Patricia Perfecto100% (1)
- Post Lab 01-09Document7 pagesPost Lab 01-09Patrick ParconNo ratings yet
- CSMLS Exam Guide Notes (Referrence Range)Document4 pagesCSMLS Exam Guide Notes (Referrence Range)software4us.2023No ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- Fast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsFrom EverandFast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Multiple Choice Questions for Haematology and Core Medical TraineesFrom EverandMultiple Choice Questions for Haematology and Core Medical TraineesNo ratings yet
- Differentiate Between With AnswersDocument14 pagesDifferentiate Between With AnswersStephy SojanNo ratings yet
- ANUGRAH DHARMA HISTORY Duta Berkat Revisi 2 GambarDocument71 pagesANUGRAH DHARMA HISTORY Duta Berkat Revisi 2 GambarAndri aryanataNo ratings yet
- Opthalmology Short NotesDocument14 pagesOpthalmology Short NotesChristine Nancy Ng100% (1)
- Mild Cognitive Impairment - Beyond Controversies, Towards A Consensus: Report of The International Working Group On Mild Cognitive ImpairmentDocument7 pagesMild Cognitive Impairment - Beyond Controversies, Towards A Consensus: Report of The International Working Group On Mild Cognitive ImpairmentRoxana SanduNo ratings yet
- NCP Epidural HemDocument32 pagesNCP Epidural HemKatrina PonceNo ratings yet
- Literature Review-3Document5 pagesLiterature Review-3api-519320140No ratings yet
- The Korean 4 Point SystemDocument1 pageThe Korean 4 Point SystemHuib SalomonsNo ratings yet
- Basic Counseling Skills For Addiction Professionals: Module 1-Training IntroductionDocument36 pagesBasic Counseling Skills For Addiction Professionals: Module 1-Training IntroductionlissarlissaaNo ratings yet
- Surgical Diseases of The EsophagusDocument35 pagesSurgical Diseases of The Esophagusmogesie1995No ratings yet
- Improvement of The Rubber Dam FrameDocument3 pagesImprovement of The Rubber Dam FrameTiagoNo ratings yet
- What Is Pancreatic Cancer?: Primary-MetastaticDocument2 pagesWhat Is Pancreatic Cancer?: Primary-MetastaticValiant BaybayNo ratings yet
- Q2 Health9 Drug ScenarioDocument54 pagesQ2 Health9 Drug Scenarionova rhea garciaNo ratings yet
- Chapter 47 Diabetes Mellitus PDFDocument14 pagesChapter 47 Diabetes Mellitus PDFRLLT100% (1)
- Immediate Newborn Care: The First 90 Minutes: Preparing For The Birth (Continued)Document33 pagesImmediate Newborn Care: The First 90 Minutes: Preparing For The Birth (Continued)Zimm RrrrNo ratings yet
- Mov3. GENERAL - UMN (Pyramidal) & LMN DisordersDocument9 pagesMov3. GENERAL - UMN (Pyramidal) & LMN DisordersherlambangkusumoNo ratings yet
- Body Temperature and How To Measure ItDocument6 pagesBody Temperature and How To Measure ItMeyin LowNo ratings yet
- KARDEXDocument2 pagesKARDEXNicole Audrey JoaquinNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument6 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyAhmed AliNo ratings yet
- Medical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusDocument90 pagesMedical-Surgical Nursing Care: Caring For Clients With Diabetes MellitusJonalynCollodChewacheoNo ratings yet
- Answer: C) End Tidal CO: - Total Comments: 0Document16 pagesAnswer: C) End Tidal CO: - Total Comments: 0Mysheb SS100% (1)
- Diabetes and Virgin Coconut Oil DR Bruce FifeDocument3 pagesDiabetes and Virgin Coconut Oil DR Bruce Fifepetri_jv100% (1)
- What Is Acute BronchitisDocument11 pagesWhat Is Acute BronchitisKerri-DojhnHallNo ratings yet
- Radionic CardsDocument2 pagesRadionic CardsRoberta & Thomas NormanNo ratings yet
- Lipo Stab Il Injection TechniqueDocument3 pagesLipo Stab Il Injection TechniqueMIAPISNo ratings yet
- International Guide To Prescribing Psychotropic Medication For The Management of Problem Behaviours in Adults With Intellectual DisabilitiesDocument6 pagesInternational Guide To Prescribing Psychotropic Medication For The Management of Problem Behaviours in Adults With Intellectual DisabilitiesShalawatyAbdkarimNo ratings yet
- Galson MENTALHEALTHMATTERS 2009Document4 pagesGalson MENTALHEALTHMATTERS 2009PSNo ratings yet