Professional Documents
Culture Documents
Propofol and Children What We Know and What We Do Not Know PDF
Propofol and Children What We Know and What We Do Not Know PDF
Uploaded by
Alexey Zamora BetancourtCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Comfort - Nursing Test QuestionsDocument57 pagesComfort - Nursing Test QuestionsRNStudent1100% (1)
- ERAS - Personal StatementDocument1 pageERAS - Personal StatementfewNo ratings yet
- Grand Case NP 1 Laparoscopic CholecystectomyDocument21 pagesGrand Case NP 1 Laparoscopic CholecystectomyFarida Paula R. SevillaNo ratings yet
- Hospital DepartmentsDocument16 pagesHospital DepartmentsfictoriaNo ratings yet
- Maternity Nursing Lecture NotesDocument198 pagesMaternity Nursing Lecture Notesprogramgrabber75% (4)
- CH 46 Complications of AnaesthesiaDocument29 pagesCH 46 Complications of AnaesthesiaChristian LeepoNo ratings yet
- Mandibular Nerve Block (Other Techniques)Document24 pagesMandibular Nerve Block (Other Techniques)daw022100% (2)
- Jurnal AnalgesikDocument7 pagesJurnal AnalgesikAnung IndrasNo ratings yet
- Spinal Anes Drug StudyDocument12 pagesSpinal Anes Drug StudyNicosia Mae FerrerNo ratings yet
- Case 10 (Post-Operative Pain Management & Complication)Document10 pagesCase 10 (Post-Operative Pain Management & Complication)ReddyNo ratings yet
- General Anaesthesia: Adityadeb Ghosh B. Pharm Guru Nanak Institute of Pharmaceutical Science and Technology, Kolkata, INDocument19 pagesGeneral Anaesthesia: Adityadeb Ghosh B. Pharm Guru Nanak Institute of Pharmaceutical Science and Technology, Kolkata, INSunetraNo ratings yet
- Drugs Used For Nervous System DisordersDocument95 pagesDrugs Used For Nervous System DisordersLaiba zamanNo ratings yet
- Hershey Board Certification Review Outline Study Guide: Jonathan M. Singer, D.P.MDocument9 pagesHershey Board Certification Review Outline Study Guide: Jonathan M. Singer, D.P.MpoddataNo ratings yet
- M206 Research Summary PDFDocument12 pagesM206 Research Summary PDFPeter CabinianNo ratings yet
- Mysheet: Requirement Id Requirement Name Referred by Name Date of Application Source of ApplicationDocument17 pagesMysheet: Requirement Id Requirement Name Referred by Name Date of Application Source of ApplicationMohd SaifNo ratings yet
- Dexamethasone Deep Dive PDFDocument1 pageDexamethasone Deep Dive PDFRizky TiensNo ratings yet
- What Is Dilation and Curettage (D&C) ?Document3 pagesWhat Is Dilation and Curettage (D&C) ?jaroh_20No ratings yet
- A Ciegas - Josh MalermanDocument6 pagesA Ciegas - Josh MalermanRooyValenciaNo ratings yet
- Preoperative Assessment of The Patient With Heart Disease Case FileDocument2 pagesPreoperative Assessment of The Patient With Heart Disease Case Filehttps://medical-phd.blogspot.comNo ratings yet
- BPL Catlogue Updated With 3dDocument24 pagesBPL Catlogue Updated With 3dcpt abbasNo ratings yet
- PassAMCQ Study Companion 21Document30 pagesPassAMCQ Study Companion 21nitesawakeningNo ratings yet
- Airway AssessmentDocument58 pagesAirway AssessmentSanjit Singh100% (3)
- Physiology of Pregnancy: Learning ObjectivesDocument5 pagesPhysiology of Pregnancy: Learning ObjectivesBaiiqDelaYulianingtyasNo ratings yet
- KPI - Foruth EditionDocument30 pagesKPI - Foruth EditionAnonymous qUra8Vr0SNo ratings yet
- Perioperative NursingDocument108 pagesPerioperative NursingKrishna Faith P. DelaraNo ratings yet
- Learn About CataractsDocument41 pagesLearn About CataractsRizkyAgustriaNo ratings yet
- Local Anesthesia Isolation in Ped DentDocument7 pagesLocal Anesthesia Isolation in Ped DentnazishNo ratings yet
- Psycho Cybernetics Summary PDF by THBDocument30 pagesPsycho Cybernetics Summary PDF by THBpritish satpathyNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakajhuvanNo ratings yet
- Comparative Pharmacology of The Ketamine IsomersDocument7 pagesComparative Pharmacology of The Ketamine IsomersCharlosNo ratings yet
Propofol and Children What We Know and What We Do Not Know PDF
Propofol and Children What We Know and What We Do Not Know PDF
Uploaded by
Alexey Zamora BetancourtOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Propofol and Children What We Know and What We Do Not Know PDF
Propofol and Children What We Know and What We Do Not Know PDF
Uploaded by
Alexey Zamora BetancourtCopyright:
Available Formats
Pediatric Anesthesia ISSN 1155-5645
REVIEW ARTICLE
Propofol and children – what we know and what we do not
know
Ann E. Rigby-Jones & J. Robert Sneyd
Anaesthesia Research Group, Peninsula Medical School, Peninsula College of Medicine & Dentistry, University of Plymouth, Plymouth, UK
Keywords Summary
propofol; children; pharmacokinetics;
pharmacodynamics The pharmacokinetics of propofol are relatively well described in the pedia-
tric population. Recent work has confirmed the validity of allometric scal-
Correspondence ing for predicting propofol disposition across different species and for
Dr. Ann E. Rigby-Jones, describing pediatric ontogenesis. In the first year of life, allometric models
Anaesthesia Research Group, Peninsula
require adjustment to reflect ontogeny of maturation. Pharmacodynamic
Medical School, Peninsula College of
Medicine & Dentistry, University of
data for propofol in children are scarcer, because of practical difficulties in
Plymouth, N31, ITTC Building, Tamar data collection and the limitations of currently available depth of anesthe-
Science Park, Derriford, Plymouth PL6 8BX, sia monitors for pediatric use. Hence, questions relating to the comparative
UK sensitivity of children to propofol, and differences in time to peak effect
Email: ann.rigby-jones@pms.ac.uk relative to adults, remain unanswered. Keo half-lives have been determined
for pediatric kinetic models using time to peak effect techniques but are
Section Editor: Brian Anderson
not currently incorporated into commercially available target-controlled
Accepted 13 October 2010
infusion pumps.
doi:10.1111/j.1460-9592.2010.03454.x
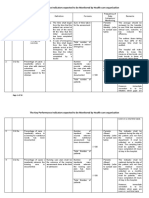
netic simulation. Figure 1 compares the concentration
Pediatric pharmacokinetics
versus time profile resulting from a 1-h propofol
The pharmacokinetics of propofol are relatively well infusion (4 mgÆkg)1Æh)1) administered to an adult
described in children, having been investigated in [Diprifusor kinetics (1,13)] or to a 20-kg child [Kataria
healthy children (1–5), children with biliary atresia (3), kinetics (5)]. The larger central compartment volume
small children suffering from burns (6), critically ill in children results in markedly reduced propofol
ventilated (7,8) and nonventilated children (9) and neo- plasma concentrations, relative to the adult.
nates (10,11). Propofol disposition is generally best
described by a 3-compartment mamillary model, with
Disentangling covariate effects
a rapidly equilibrating central compartment, a second
larger peripheral compartment and a third, very large The evaluation of drug disposition in heterogeneous
peripheral compartment. Propofol pharmacokinetics patients groups, such as those encountered in the
are altered in children, compared to adults. Compara- pediatric ICU, can be complicated by the presence of
tive analyses have demonstrated that on a per kilo- confounding factors. How can one separate the influ-
gram body weight basis, children demonstrate ences that critical illness may have on pharmaco-
increased clearance and larger volumes of distribution kinetics from the affects of body size and maturity?
relative to adults. In particular, the volume of the cen- Body size and age are usually well correlated in pedia-
tral compartment is much greater than in adults (12). tric populations. Allometric scaling is a useful and
Consequently, children require higher induction and well-supported (14) approach to disentangle body size
maintenance doses than adults to achieve the same effects from other correlated covariables, such as age,
propofol blood concentration. in pediatric populations. Allometric scaling relates
The influence of the larger central compartment body mass to metabolic rate (and hence to drug clear-
volume in children can be explored using pharmacoki- ance) using Kleiber’s Law. In 1932, Kleiber (15)
Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd 247
Propofol kinetics and dynamics in children A.E. Rigby-Jones and J.R. Sneyd
demonstrated that basal metabolic rate was propor- account for, age-related differences in pharmacoki-
tional to body mass raised to the power 0.75 and that netics.
this relationship applied to animals ranging in size
from a mouse to a whale. When deriving pharmacoki-
Propofol in neonates
netic data from pediatric populations, if weight is
selected as a initial covariate and the three-quarter The work of Allegaert and colleagues in recent years
power relationship applied a priori (to clearance para- has done much to inform propofol disposition and
meters; volume parameters are scaled to the power of 1), metabolism in term and preterm neonates. Allegaert
this allows the influence of secondary covariates, which (11) described markedly reduced clearance in a group
may be correlated to weight, e.g. age, to be examined of nine neonates (4–25 days postnatal age) after bolus
(16). injection of propofol. After appropriate allometric
Knibbe et al. (17) explored the application of allo- scaling to 70 kg to allow comparison, the clearance
metric scaling to propofol pharmacokinetic parameters value was approximately 32%, and the volume of dis-
obtained from rats, children (aged from 1 to 5 years), tribution at steady state was approximately 44% of the
and adults. This work demonstrated the validity of the corresponding values previously reported in infants.
allometric approach for predicting drug disposition Scaled propofol clearance rates approach adult values
across different species and for describing within-spe- within the first 3 months to 1 year of life (6,19), mir-
cies ontogenesis, Figure 2. roring ontogenic development of hepatic enzyme sys-
A recent publication by the same group has focused tems (20).
on defining the human body weight range for which For infants and older children, the inclusion of body
allometric scaling can accurately be applied to predict weight alone as a model covariate accounts for much
propofol clearance (18). Allometric scaling alone could of the observed interindividual variability in propofol
accurately predict propofol clearance in children older pharmacokinetics (5,8,9,19). Allegaert has demon-
than 2 years. However, adjustment of the model to strated that for neonates, postmenstrual and postnatal
reflect maturation was required to predict clearance in age as markers of maturity, rather than body weight,
children younger than 24 months, a demonstration were the most influential factors, with the youngest
that simple allometric scaling reveals, but does not babies having the smallest clearance values. Anderson
(21) further explored this finding, combining Alle-
gaert’s neonatal clearance data with clearance values
derived from older children (5,6) and adults (13,22,23).
A sigmoid Emax model was then applied to describe
the maturation profile, Figure 3. In this analysis, the
maturation half-time was calculated as 44 weeks.
Anderson highlights the need for additional study of
propofol disposition in infants to fully characterize the
maturation profile in the first 2 years of life.
Pediatric critical care and propofol infusion syndrome
(PRIS)
PRIS was first described in the literature in 1992 (24).
Shortly after, the syndrome was defined by Bray (25)
as a sudden onset of treatment-resistant bradycardia
leading to asystole, combined with at least one of the
following symptoms: lipemic plasma, clinically
enlarged or fat infiltrated liver, metabolic acidosis or
rhabdomylosis. The syndrome was associated with
Figure 1 Simulation of the concentration vs time profile resulting long-duration (more than 48 h), high-dose (more than
from a 1-h propofol infusion (4 mgÆkg)1Æh)1) administered to a 20-kg
4 mgÆkg)1Æh)1) propofol infusions in children under
child, using three different pharmacokinetic models. Diprifusor
kinetics (adult) (1,13), Kataria (pediatric) (5), and Rigby-Jones (pedia-
12 years old. In 2001, reports of the same propofol-
tric, postcardiac surgery) (8). The Diprifusor kinetics are linearly related syndrome occurring in adult ICU patients (26)
weight-scaled, hence the predicted profile shown would apply to led to the UK Commission on Human Medicines (then
any given body weight, adult or child. Commission on Safety of Medicines) to recommend
248 Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd
A.E. Rigby-Jones and J.R. Sneyd Propofol kinetics and dynamics in children
Figure 2 Evidence for applicability of allometric scaling of propofol ment (lower right) of propofol vs body weight in rats (bolus injec-
pharmacokinetic parameters. Plots show clearance (upper left), tion), children (postcardiac surgery, 6-h infusion), and adults (post-
intercompartmental clearance (upper right), volume of the central CABG, 5-h infusion). Figure from Knibbe et al. (17).
compartment (lower left), and volume of the peripheral compart-
that propofol infusion rates for sedation did not Eight years later, what have we learned about PRIS?
exceed 4 mgÆkg)1Æh)1(27). In the following year, the We know that it is a real phenomenon, with the con-
same committee announced the contraindication of sistency of clinical reports of the syndrome, the dose-
propofol for the sedation of critically ill children (28). dependency, and the temporal association with propo-
fol administration cited as reasons to strongly support
a causal relationship (29). Plausible mechanisms have
been suggested supporting the implication of the lipid
component of currently availably propofol formula-
tions in the pathology of the syndrome (30,31).
Whether a lipid-free propofol formulation, such as fos-
propofol, would decrease the risk of PRIS, or avoid it
entirely, is as yet unknown. However, the potential for
direct toxicity related to propofol itself, rather than the
vehicle, would remain (32).
In recent years, use of propofol sedation in critically
ill children in the United Kingdom has been extremely
limited in line with current recommendations (33). The
knowledge base regarding the disposition of propofol
in the critical care population is hence based on studies
carried out prior to the 2002 contraindication. Reed
Figure 3 Propofol clearance rates, scaled to 70kg, derived from
et al. (7) were first to study propofol disposition in a
neonates, children, and adults. The solid line describes the matura-
tion process as a sigmoid Emax function of postmenstrual age. Alle-
critically ill pediatric population, ranging from neo-
gaert (10) hypothesizes that the influence of postnatal age (PNA) nates to children aged 15 years. They concluded that
on clearance reflects ontogeny of glucuronidation activity during the the pharmacokinetics were not dissimilar to studies of
first week of postnatal life. Figure from Anderson (21). healthy children but described substantial inter-patient
Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd 249
Propofol kinetics and dynamics in children A.E. Rigby-Jones and J.R. Sneyd
variability that could not be attributed to age or other The Paedfusor model was prospectively validated in
demographic effects. Rigby-Jones et al. (8) described 29 children (1–15 years) undergoing cardiac surgery or
altered kinetics in very small babies (because of cardiac catheterization procedures (34). In this small
increased peripheral distribution volume) and reduced study, the Paedfusor model’s predictive performance
metabolic clearance in children recovering from cardiac was well within acceptable limits for clinical use. A
surgery, both findings leading to prolonged propofol formal prospective analysis of the predictive perfor-
elimination times, see Figure 2. Body weight was the mance of the Kataria model in children has not been
most influential model covariate and although a broad published to date. However, a study by Rigouzzo and
age range was studied (1 week to 12 years), no addi- colleagues involved TCI administration of propofol to
tional influence of age could be supported. In a non- children (aged 6–13 years) using the Kataria model.
ventilated, postneurosurgical, pediatric population (9), Blood samples for propofol plasma assay were col-
propofol clearance values were reported to be twice as lected (36). It was reported that measured concentra-
high as those previously described in pediatric inten- tions of propofol were consistently higher than those
sive care unit (PICU) patients (8), emphasizing the predicted by the Kataria model and that the margin of
impact that mechanical ventilation and cardiac bypass error increased with the increasing propofol concentra-
have on propofol elimination during postoperative tion.
sedation. The original analyses leading to the derivation of
the Kataria and Paedfusor models were based on phar-
macokinetic data only. However, values for Ke0 and
Pediatric propofol target-controlled infusion (TCI)
the blood–brain equilibration rate constant have been
There are at least two pediatric pharmacokinetic mod- retrospectively generated for both models using the
els for propofol available for use in commercially time to peak effect (tpeak) (37) technique (38). Tpeak is
available TCI pumps: the Paedfusor (34,35) and the a model-independent pharmacodynamic parameter
Kataria kinetic set (5). The Kataria model is based on that can be used to calculate a Ke0 value for a given
data from 53 healthy children, ranging in age from pharmacokinetic set, after administration of a submax-
three to 11 years. Mean postdose sampling duration imal dose. The Ke0 value derived is one that accurately
was 214 min (range 52–811). The Paedfusor pharmaco- predicts tpeak (37). Muñoz’s analysis revealed that the
kinetic set was derived as a preliminary model (pre- peak effect of propofol in children (132 s) occurs far
sumably based on pediatric data only) by Schuttler later than in adults (80 s). The explanation offered for
and Ihmsen (12) during their development of a phar- this finding is that, relative to adults (Schnider model),
macokinetic model based on pooled data from both simulations using the pediatric model demonstrate a
adults and children. In Schuttler’s analysis, pediatric much slower initial decline in plasma propofol concen-
data comprised 96 children aged from 2 to 11 years, trations, Figure 4. As the postbolus tpeak is the conse-
including the patient population on which Kataria’s quence of both decreasing plasma concentration and
model was based (5) and data from two further pedia- increasing effect site concentration, this is a plausible
tric studies (1,2). mechanism.
Figure 4 The unit disposition function of plasma vs time profile centration, and a larger variability related to patient age, is
simulation with the Schnider model (adults) (22) and both the observed with the pediatric models. Figure from Munoz et al.
Kataria and Paedfusor models. A shallower decline in plasma con- (38).
250 Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd
A.E. Rigby-Jones and J.R. Sneyd Propofol kinetics and dynamics in children
The experimentally derived tpeak value of 132 s impact that stimulation required as part of a scoring
extrapolated to a Ke0 value for the Kataria model of system may have on the underlying depth of sedation.
0.41 min)1 and for the Paedfusor model, 0.91 min)1. Additionally, researchers are unlikely to be able to
However, current commercially available TCI devices study single-drug effects in children. Hence, there is a
incorporating the Kataria and Paedfusor models do need for pragmatism regarding the concomitant
not include Ke0, i.e. plasma is the target of the infu- administration of other drugs with sedating effects
sion, rather than the effect site, thus depriving pedia- when evaluating propofol pharmacodynamics, such as
tric populations from the superior control offered by maintaining opioids infusions at a constant rate, so
effect site targeting systems (39–41). adjunct drug contribution to pharmacodynamic effects
are at least unchanging after a period of equilibration
(45). In another strategy to deal with multiple drug
Pediatric pharmacodynamics (PD)
effects, Jeleazcov et al. (46) assumed additive interac-
While the pharmacokinetics of propofol in the pedia- tions between propofol and co-administered opioids to
tric population are reasonably well described, there is derive pharmacodynamic parameter values for each
a relative paucity of pharmacodynamic data (9,38,42). drug based on their combined sedative effect, when
measured using bispectral index (BIS). They studied 59
children aged from 1 to 16 years undergoing general
Limitations of pediatric PD studies
surgery. A two-stage pharmacodynamic analysis
Undertaking pharmacodynamic studies can be very revealed an age-dependency of the Ke0 value for pro-
difficult in children and particularly so in intensive pofol, with Ke0 decreasing with increasing age. Tpeak,
care medicine. In a ‘real life’ scenario, rather than a however, showed a trend of increasing with age. These
controlled volunteer study in adults, it is often diffi- findings may reflect true age-dependent differences in
cult or impossible to obtain data describing a full propofol pharmacodynamics. Cortinez et al. (42) have
drug concentration versus effect profile. This is suggested that children may be more sensitive to pro-
required for adequately quantifying hysteresis and pofol than adults, based on higher calculated CE50
hence the derivation of Ke0. Arterial blood, the gold- values in adults than in children (3–11 years), resulting
standard matrix for sampling during PK–PD studies from a study examining auditory evoked potentials
of rapidly acting drug compounds, is highly unlikely (AEP) following a submaximal bolus propofol dose.
to be available for children outside of critical care. However, a second study by the same group which
The insertion of a peripheral arterial line in children determined propofol effect site concentrations at BIS
purely for research purposes is classified as high risk value = 50 in adults and in children aged 3–11 did
and cannot be justified (43); further, arterial line not demonstrate significant differences in propofol
insertion is typically carried out after induction of requirements (47). In contrast, Rigouzzo et al. (36)
anesthesia, and the opportunity to populate the rising suggested that children may be less sensitive than
phase of the hysteresis loop is lost. The use of venous adults to propofol. In their study of 45 children
blood sampling during pediatric pharmacodynamic (6–13 years) and 45 adults anaesthetized with TCI pro-
studies of intravenous sedative-hypnotics presents a pofol, children demonstrated higher measured and pre-
limitation that can in part be overcome by careful dicted propofol plasma concentrations at a BIS value
study design, such as the incorporation of equilibra- of 50 than the adult patients. Conflicting results from
tion stages to accompanying changes in infusion rate. such studies may be in part related to the choice of
This stabilizes arterial and venous blood concentra- depth of anesthesia monitor and differences in the
tions and minimizes arterio-venous differences as far pharmacokinetic models used to administer propofol
as possible. and/or predict effect site concentrations.
The use of intermittent pharmacodynamic markers, Recently, a second smaller study by Rigouzzo et al.
such as sedation scores, can also make it more difficult (48) attempted to identify the best model for describing
to capture rapidly changing drug effects. However, for propofol PK–PD in prepubertal children. Propofol
extended continuous infusion studies, COMFORT was administered to prepubertal children (n = 16,
scores (44) can provide useful information and have 6–12 years) by TCI using the Kataria model (5) and to
been successfully utilized as pharmacodynamic markers adults and postpubertal children (n = 13, 13–35 years)
for the development of complex but clinically informa- using the Schnider model (49). BIS was used as an
tive models of propofol pharmacodynamics (9). Other effect measure. The recorded BIS data from the prepu-
limitations of sedation scoring as a pharmacodynamic bertal group were then compared to predicted propofol
marker are inter- and intra-observer variance and the concentrations generated using several pharmacoki-
Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd 251
Propofol kinetics and dynamics in children A.E. Rigby-Jones and J.R. Sneyd
netic models; the Kataria model used to administer Prospective BIS monitoring of children (n = 12, 1–
propofol but also the Marsh (1), Schuttler (12) and 12 years) in PICU was performed to investigate the
Schnider models, to evaluate which model best incidence of over-sedation and periods of potential
described the data. BIS data from the postpubertal/ awareness during neuromuscular blockade (56). Chil-
adult cohort was compared to predicted concentrations dren were sedated with either midazolam or propofol
generated by the Schnider model only. The analysis infusions, with supplemental doses of midazolam, fen-
revealed that the prepubertal BIS vs predicted propofol tanyl, or morphine provided if additional sedation was
concentration was best described by the adult Schnider deemed necessary, based on physiological parameters.
model, so in a second stage of the analysis, the two The BIS monitor was concealed from clinical staff.
cohorts were pooled so that the influence of puberty During the 476 h of sedation studied, over-sedation
on propofol pharmacodynamic parameter estimates (BIS < 50) occurred 35% of the time, and under-seda-
could be examined. The authors hypothesize that the tion (periods of potential awareness, BIS > 71) com-
lack of early sampling in the studies that led to the prised 8% of the time. Over-sedation was more likely
derivation of the pediatric models tested may explain to occur in patients sedated with propofol, than with
their perceived weakness at describing the initial phase midazolam (P < 0.0001). There are several limitations
of propofol distribution kinetics, and hence the effect to this study, not least the small cohort and the
on BIS. Additionally, the Schnider model is unique assumption that BIS is a ‘gold standard’ measure of
among those explored in Rigouzzo’s analysis in that sedation in the patients studied. However, the study
both age and lean body mass are included as covari- results suggest the need for a larger prospective trial to
ates, thus allowing a more precise tailoring of indivi- establish the benefit of BIS-titrated sedation in pedia-
dual predicted propofol concentrations. Analysis of the tric patients during the use of neuromuscular blocking
pooled data from both cohorts using the Schnider agents.
model revealed that pubertal status was a significant Recently, Tirel et al. (57) used TCI propofol to eval-
pharmacodynamic model covariate with both KeO and uate the relationship between age and BIS values, in a
Ce50 varying between children and adults. The typical group of children aged from 3 to 15 years. Target pro-
value of Ce50 was around 20% higher in children than pofol plasma concentrations were held at 6, 4, and
in adults. Tpeak was subsequently derived and found to 2 lgÆmL)1 during periods without surgical stimulation
be significantly shorter in children at 0.71 min [0.37– to allow collection of BIS and raw EEG. In this study,
1.64] median [range] vs 1.73 [1.4–2.68] min in adults. there was no statistically significant difference in BIS
This is in contrast to the findings by Munoz (38), values at 4 and 6 lgÆmL)1. BIS values at 2 lgÆmL)1
which the authors suggest may relate to differences in were significantly different to those achieved at the
effect measure (BIS vs AEP) and methodological dif- higher target concentrations but were also correlated
ferences, including the use of different pharmacokinetic with the age of the children (r2 = 0.66), with the high-
models. The shorter Tpeak in younger children supports est BIS values being recorded in the youngest children.
the findings of Jeleacov and colleagues (46). Tirel et al. suggest this may reflect a true pharmacody-
namic difference between younger and older children
or could be influenced by the underlying pharmacoki-
Propofol, BIS, and children
netics. The Kataria model used for TCI does not
The technology of BIS monitoring is based on an algo- include age as a covariate after it was demonstrated
rithm developed from adults, hence its usefulness as a that its inclusion only marginally improved the model.
measure of anesthetic depth in children, and particu- Park et al. (58) investigated the relationship between
larly in infants, has long been questioned (50). Subse- BIS values and predicted plasma propofol concentra-
quent studies evaluating the relationship between the tions in 30 children aged from 2 to 7 years during
bispectral index and established sedation measures emergence from anesthesia. The Marsh model was
such as the Observer’s Assessment of Alertness/Seda- used to administer TCI propofol (1). On completion of
tion (OAA/S) and the University of Michigan Sedation surgery, the target propofol concentration was reduced
Scale (UMSS) have provided evidence that BIS moni- from 3 lgÆmL)1 in 0.2 lgÆmL)1-steps and BIS values
toring can be a useful measure of intravenous sedation were recorded. The authors concluded that BIS was
in children older than 2 years (51,52). Currently, evi- correlated with predicted propofol concentration dur-
dence to suggest that any of the alternative depth of ing emergence from anesthesia but that the correlation
anesthesia monitors is more or less suitable than BIS was weaker than that observed with an adult popula-
for use in children is limited (53–55). tion. Additionally, there was substantial interindividual
252 Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd
A.E. Rigby-Jones and J.R. Sneyd Propofol kinetics and dynamics in children
variability in the recorded BIS values at each predicted of much needed research in the neonatal population in
concentration. recent years. In addition, based on demonstration of
These studies suggest caution when using BIS to the applicability and limitations of allometric scaling,
titrate propofol infusions in children and demonstrate there is now better understanding of the mechanisms
a lack of sensitivity of the BIS system to discriminate and predictability of changes in propofol pharmaco-
at deep sedation levels in children. kinetics from birth to maturity.
Given the practical restrictions described, and the
continued lack of a gold-standard depth of anesthesia
Conclusion
monitor for children, it is not surprising that much
This review has sought to identify current gaps in the remains to be elucidated regarding the pharmacody-
knowledge base of propofol use in the pediatric popu- namics of propofol in the pediatric population. Indeed,
lation, in particular, aspects relating to drug disposi- the knowledge base relating to adult propofol pharma-
tion and pharmacodynamic effect. codynamics has its own limitations, with genuine dis-
There are comprehensive data describing propofol agreement about the most appropriate values for time
disposition across the pediatric age range, as a result to peak effect and t1/2keO (59,60).
References
1 Marsh B, White M, Morton N et al. Phar- 10 Allegaert K, Peeters MY, Verbesselt R et al. 20 Alcorn J, McNamara PJ. Ontogeny of hepa-
macokinetic model driven infusion of pro- Inter-individual variability in propofol phar- tic and renal systemic clearance pathways in
pofol in children. Br J Anaesth 1991; 67: macokinetics in preterm and term neonates. infants: part I. Clin Pharmacokinet 2002; 41:
41–48. Br J Anaesth 2007; 99: 864–870. 959–998.
2 Saint-Maurice C, Cockshott ID, Douglas EJ 11 Allegaert K, de Hoon J, Verbesselt R et al. 21 Anderson BJ. Pediatric models for adult tar-
et al. Pharmacokinetics of propofol in Maturational pharmacokinetics of single get-controlled infusion pumps. Pediatr
young children after a single dose. Br J intravenous bolus of propofol. Pediatr Anesth 2010; 20: 223–232.
Anaesth 1989; 63: 667–670. Anesth 2007; 17: 1028–1034. 22 Schnider TW, Minto CF, Shafer SL et al.
3 Raoof AA, van Obbergh LJ, Verbeeck RK. 12 Schuttler J, Ihmsen H. Population pharma- The influence of age on propofol pharmaco-
Propofol pharmacokinetics in children with cokinetics of propofol: a multicenter study. dynamics. Anesthesiology 1999; 90: 1502–
biliary atresia. Br J Anaesth 1995; 74: 46– Anesthesiology 2000; 92: 727–738. 1516.
49. 13 Gepts E, Camu F, Cockshott ID et al. Dis- 23 Struys MM, Coppens MJ, De Neve N et al.
4 Jones RD, Chan K, Andrew LJ. Pharmaco- position of propofol administered as con- Influence of administration rate on propofol
kinetics of propofol in children. Br J stant rate intravenous infusions in humans. plasma-effect site equilibration. Anesthesiol-
Anaesth 1990; 65: 661–667. Anesth Analg 1987; 66: 1256–1263. ogy 2007; 107: 386–396.
5 Kataria BK, Ved SA, Nicodemus HF et al. 14 Anderson BJ, Allegaert K, Holford NH. 24 Parke TJ, Stevens JE, Rice AS et al. Meta-
The pharmacokinetics of propofol in chil- Population clinical pharmacology of chil- bolic acidosis and fatal myocardial failure
dren using three different data analysis dren: modelling covariate effects. Eur J after propofol infusion in children: five case
approaches. Anesthesiology 1994; 80: 104– Pediatr 2006; 165: 819–829. reports. BMJ 1992; 305: 613–616.
122. 15 Kleiber M. Body size and metabolism. Hil- 25 Bray RJ. Propofol infusion syndrome in
6 Murat I, Billard V, Vernois J et al. Pharma- gardia 1932; 6: 315–333. children. Paediatr Anaesth 1998; 8: 491–499.
cokinetics of propofol after a single dose in 16 Anderson BJ, Holford NH. Mechanistic 26 Cremer OL, Moons KG, Bouman EA et al.
children aged 1–3 years with minor burns. basis of using body size and maturation to Long-term propofol infusion and cardiac
Comparison of three data analysis predict clearance in humans. Drug Metab failure in adult head-injured patients. Lancet
approaches. Anesthesiology 1996; 84: 526– Pharmacokinet 2009; 24: 25–36. 2001; 357: 117–118.
532. 17 Knibbe CA, Zuideveld KP, Aarts LP et al. 27 MCA/CSM. Long term, high dose propofol
7 Reed MD, Yamashita TS, Marx CM et al. Allometric relationships between the phar- (Diprivan) infusion. Curr Probl Pharmacov-
A pharmacokinetically based propofol dos- macokinetics of propofol in rats, children igilence 2001; 27: 6.
ing strategy for sedation of the critically ill, and adults. Br J Clin Pharmacol 2005; 59: 28 MCA/CSM. Clarification: propofol (Dipri-
mechanically ventilated pediatric patient. 705–711. van) infusion contraindication. Curr Probl
Crit Care Med 1996; 24: 1473–1481. 18 Peeters MY, Allegaert K, Blusse van Oud- Pharmacovigilence 2002; 28: 6.
8 Rigby-Jones AE, Nolan JA, Priston MJ Alblas HJ et al. Prediction of propofol 29 Fudickar A, Bein B. Propofol infusion syn-
et al. Pharmacokinetics of propofol clearance in children from an allometric drome: update of clinical manifestation and
infusions in critically ill neonates, infants, model developed in rats, children and adults pathophysiology. Minerva Anestesiol 2009;
and children in an intensive care unit. versus a 0.75 fixed-exponent allometric 75: 339–344.
Anesthesiology 2002; 97: 1393–1400. model. Clin Pharmacokinet 2010; 49: 269– 30 Wolf A, Weir P, Segar P et al. Impaired
9 Peeters MY, Prins SA, Knibbe CA et al. 275. fatty acid oxidation in propofol infusion
Propofol pharmacokinetics and pharmaco- 19 Shangguan WN, Lian Q, Aarons L et al. syndrome. Lancet 2001; 357: 606–607.
dynamics for depth of sedation in nonventi- Pharmacokinetics of a single bolus of pro- 31 Withington DE, Decell MK, Al Ayed T. A
lated infants after major craniofacial pofol in Chinese children of different ages. case of propofol toxicity: further evidence
surgery. Anesthesiology 2006; 104: 466–474. Anesthesiology 2006; 104: 27–32. for a causal mechanism. Pediatr Anesth
2004; 14: 505–508.
Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd 253
Propofol kinetics and dynamics in children A.E. Rigby-Jones and J.R. Sneyd
32 Schenkman KA, Yan S. Propofol controlled target-controlled infusion for pro- 50 Watcha MF. Investigations of the bispectral
impairment of mitochondrial respiration in pofol. Anesthesiology 2000; 92: 399–406. index monitor in pediatric anesthesia: first
isolated perfused guinea pig hearts 41 Mortier E, Struys M. Effect site modelling things first. Anesth Analg 2001; 92: 805–807.
determined by reflectance spectroscopy. and its application in TCI. Acta Anaesthe- 51 Sadhasivam S, Ganesh A, Robison A et al.
Crit Care Med 2000; 28: 172– siol Belg 2000; 51: 149–152. Validation of the bispectral index monitor
177. 42 Cortinez LI, Munoz HR, Lopez R. Pharma- for measuring the depth of sedation in chil-
33 Jenkins IA, Playfor SD, Bevan C et al. Cur- codynamics of propofol in children and dren. Anesth Analg 2006; 102: 383–388.
rent United Kingdom sedation practice in adults: comparison based on the auditory 52 Overly FL, Wright RO, Connor FA Jr et al.
pediatric intensive care. Pediatr Anaesth evoked potentials index. Rev Esp Anestesiol Bispectral analysis during pediatric proce-
2007; 17: 675–683. Reanim 2006; 53: 289–296. dural sedation. Pediatr Emerg Care 2005;
34 Absalom A, Amutike D, Lal A et al. Accu- 43 Hull D. Guidelines for the ethical conduct 21: 6–11.
racy of the ‘Paedfusor’ in children under- of medical research in children. Arch Dis 53 Davidson AJ. Monitoring the anaesthetic
going cardiac surgery or catheterization. Br Child 2000; 82: 177–182. depth in children – an update. Curr Opin
J Anaesth 2003; 91: 507–513. 44 Marx CM, Smith PG, Lowrie LH et al. Anaesthesiol 2007; 20: 236–243.
35 Absalom A, Kenny G. ‘Paedfusor’ pharma- Optimal sedation of mechanically ventilated 54 Wallenborn J, Kluba K, Olthoff D. Com-
cokinetic data set. Br J Anaesth 2005; 95: pediatric critical care patients. Crit Care parative evaluation of Bispectral Index and
110. Med 1994; 22: 163–170. Narcotrend Index in children below 5 years
36 Rigouzzo A, Girault L, Louvet N et al. The 45 Murray DM, Thorne GC, Rigby-Jones AE of age. Pediatr Anesth 2007; 17: 140–147.
relationship between bispectral index and et al. Electroencephalograph variables, drug 55 Klockars JG, Hiller A, Ranta S et al. Spec-
propofol during target-controlled infusion concentrations and sedation scores in chil- tral entropy as a measure of hypnosis in
anesthesia: a comparative study between dren emerging from propofol infusion children. Anesthesiology 2006; 104: 708–717.
children and young adults. Anesth Analg anaesthesia. Pediatr Anesth 2004; 14: 143– 56 Tobias JD, Grindstaff R. Bispectral index
2008; 106: 1109–1116. 151. monitoring during the administration of
37 Minto CF, Schnider TW, Gregg KM et al. 46 Jeleazcov C, Ihmsen H, Schmidt J et al. neuromuscular blocking agents in the pedia-
Using the time of maximum effect site con- Pharmacodynamic modelling of the bispec- tric intensive care unit patient. J Intensive
centration to combine pharmacokinetics and tral index response to propofol-based anaes- Care Med 2005; 20: 233–237.
pharmacodynamics. Anesthesiology 2003; 99: thesia during general surgery in children. Br 57 Tirel O, Wodey E, Harris R et al. Variation
324–333. J Anaesth 2008; 100: 509–516. of bispectral index under TIVA with propo-
38 Munoz HR, Cortinez LI, Ibacache ME et 47 Munoz HR, Cortinez LI, Ibacache ME fol in a paediatric population. Br J Anaesth
al. Estimation of the plasma effect site equi- et al. Effect site concentrations of propofol 2008; 100: 82–87.
libration rate constant (ke0) of propofol in producing hypnosis in children and adults: 58 Park HJ, Kim YL, Kim CS et al. Changes
children using the time to peak effect: com- comparison using the bispectral index. Acta of bispectral index during recovery from
parison with adults. Anesthesiology 2004; Anaesthesiol Scand 2006; 50: 882–887. general anesthesia with 2% propofol and
101: 1269–1274. 48 Rigouzzo A, Servin F, Constant I. Pharma- remifentanil in children. Pediatr Anesth
39 Wakeling HG, Zimmerman JB, Howell S cokinetic-pharmacodynamic modeling of 2007; 17: 353–357.
et al. Targeting effect compartment or cen- propofol in children. Anesthesiology 2010; 59 WorldSIVA. Open TCI Initiative http://
tral compartment concentration of propofol: 113: 343–352. opentci.org/doku.php. Accessed 8 Novem-
what predicts loss of consciousness? 49 Schnider TW, Minto CF, Gambus PL et al. ber, 2010.
Anesthesiology 1999; 90: 92–97. The influence of method of administration 60 Absalom AR, Mani V, De Smet T et al.
40 Struys MM, De Smet T, Depoorter B et al. and covariates on the pharmacokinetics of Pharmacokinetic models for propofol–defin-
Comparison of plasma compartment versus propofol in adult volunteers. Anesthesiology ing and illuminating the devil in the detail.
two methods for effect compartment – 1998; 88: 1170–1182. Br J Anaesth 2009; 103: 26–37.
254 Pediatric Anesthesia 21 (2011) 247–254 ª 2010 Blackwell Publishing Ltd
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Comfort - Nursing Test QuestionsDocument57 pagesComfort - Nursing Test QuestionsRNStudent1100% (1)
- ERAS - Personal StatementDocument1 pageERAS - Personal StatementfewNo ratings yet
- Grand Case NP 1 Laparoscopic CholecystectomyDocument21 pagesGrand Case NP 1 Laparoscopic CholecystectomyFarida Paula R. SevillaNo ratings yet
- Hospital DepartmentsDocument16 pagesHospital DepartmentsfictoriaNo ratings yet
- Maternity Nursing Lecture NotesDocument198 pagesMaternity Nursing Lecture Notesprogramgrabber75% (4)
- CH 46 Complications of AnaesthesiaDocument29 pagesCH 46 Complications of AnaesthesiaChristian LeepoNo ratings yet
- Mandibular Nerve Block (Other Techniques)Document24 pagesMandibular Nerve Block (Other Techniques)daw022100% (2)
- Jurnal AnalgesikDocument7 pagesJurnal AnalgesikAnung IndrasNo ratings yet
- Spinal Anes Drug StudyDocument12 pagesSpinal Anes Drug StudyNicosia Mae FerrerNo ratings yet
- Case 10 (Post-Operative Pain Management & Complication)Document10 pagesCase 10 (Post-Operative Pain Management & Complication)ReddyNo ratings yet
- General Anaesthesia: Adityadeb Ghosh B. Pharm Guru Nanak Institute of Pharmaceutical Science and Technology, Kolkata, INDocument19 pagesGeneral Anaesthesia: Adityadeb Ghosh B. Pharm Guru Nanak Institute of Pharmaceutical Science and Technology, Kolkata, INSunetraNo ratings yet
- Drugs Used For Nervous System DisordersDocument95 pagesDrugs Used For Nervous System DisordersLaiba zamanNo ratings yet
- Hershey Board Certification Review Outline Study Guide: Jonathan M. Singer, D.P.MDocument9 pagesHershey Board Certification Review Outline Study Guide: Jonathan M. Singer, D.P.MpoddataNo ratings yet
- M206 Research Summary PDFDocument12 pagesM206 Research Summary PDFPeter CabinianNo ratings yet
- Mysheet: Requirement Id Requirement Name Referred by Name Date of Application Source of ApplicationDocument17 pagesMysheet: Requirement Id Requirement Name Referred by Name Date of Application Source of ApplicationMohd SaifNo ratings yet
- Dexamethasone Deep Dive PDFDocument1 pageDexamethasone Deep Dive PDFRizky TiensNo ratings yet
- What Is Dilation and Curettage (D&C) ?Document3 pagesWhat Is Dilation and Curettage (D&C) ?jaroh_20No ratings yet
- A Ciegas - Josh MalermanDocument6 pagesA Ciegas - Josh MalermanRooyValenciaNo ratings yet
- Preoperative Assessment of The Patient With Heart Disease Case FileDocument2 pagesPreoperative Assessment of The Patient With Heart Disease Case Filehttps://medical-phd.blogspot.comNo ratings yet
- BPL Catlogue Updated With 3dDocument24 pagesBPL Catlogue Updated With 3dcpt abbasNo ratings yet
- PassAMCQ Study Companion 21Document30 pagesPassAMCQ Study Companion 21nitesawakeningNo ratings yet
- Airway AssessmentDocument58 pagesAirway AssessmentSanjit Singh100% (3)
- Physiology of Pregnancy: Learning ObjectivesDocument5 pagesPhysiology of Pregnancy: Learning ObjectivesBaiiqDelaYulianingtyasNo ratings yet
- KPI - Foruth EditionDocument30 pagesKPI - Foruth EditionAnonymous qUra8Vr0SNo ratings yet
- Perioperative NursingDocument108 pagesPerioperative NursingKrishna Faith P. DelaraNo ratings yet
- Learn About CataractsDocument41 pagesLearn About CataractsRizkyAgustriaNo ratings yet
- Local Anesthesia Isolation in Ped DentDocument7 pagesLocal Anesthesia Isolation in Ped DentnazishNo ratings yet
- Psycho Cybernetics Summary PDF by THBDocument30 pagesPsycho Cybernetics Summary PDF by THBpritish satpathyNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakajhuvanNo ratings yet
- Comparative Pharmacology of The Ketamine IsomersDocument7 pagesComparative Pharmacology of The Ketamine IsomersCharlosNo ratings yet