Professional Documents
Culture Documents
Armitage2005 PDF
Armitage2005 PDF
Uploaded by
ahmedOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Armitage2005 PDF
Armitage2005 PDF
Uploaded by
ahmedCopyright:
Available Formats
Staging Non-Hodgkin Lymphoma
Staging Non-Hodgkin Lymphoma
James O. Armitage, MD
Dr. Armitage is Professor, Depart-
ment of Internal Medicine, Joe ABSTRACT Non-Hodgkin Lymphomas are always treatable and frequently curable malignan-
Shapiro Distinguished Chair of On- cies. However, choosing the most appropriate therapy requires accurate diagnosis and a
cology, University of Nebraska Med-
icine Center, Omaha, NE. careful staging evaluation. New patients with non-Hodgkin Lymphoma should have their tumors
This article is available online at classified using the World Health Organization classification. The specific choice of therapy is
http://CAonline.AmCancerSoc.org
dependent on a careful staging evaluation. Patients with non-Hodgkin Lymphoma are assigned
an anatomic stage using the Ann Arbor system. However, patients should also be classified
using the International Prognostic Index. New insights into the biology of the lymphomas in the
coming years might well improve our ability to evaluate patients and choose therapy. (CA Cancer J Clin 2005;55:368–376.)
© American Cancer Society, Inc., 2005.
INTRODUCTION
The development of staging was an important advance in the care of patients with cancer. The concepts of staging
were developed during the 20th century and were formalized in the United States by the establishment of the
American Joint Commission on Cancer in 1959. Although anatomic stage (ie, the specific sites of involvement by
the cancer) was the initial focus of staging, for some cancers other factors are considered. Symptoms, the
differentiation of the tumor, and the results of specific laboratory tests are now included in assigning stage to certain
cancers. Staging accomplishes several important goals in cancer management. These include choosing the best
therapy, allowing an accurate prognosis to be given to the patient and their family, and accurately stratifying patients
to make clinical research and quality assessment possible. In addition, knowing the sites of involvement at diagnosis
makes it possible to accurately restage at the end of therapy and document a complete remission.
Assigning a stage to a newly diagnosed patient with non-Hodgkin Lymphoma is no less important than for other
cancers. However, the development of a staging system for non-Hodgkin Lymphoma has been a difficult and
complicated process. This is, at least in part, due to the heterogeneous nature of illnesses encompassed in the term
“non-Hodgkin Lymphoma.” Lymphoid malignancies are generally classified as leukemia if they involve primarily the
blood and bone marrow and as lymphoma if they present as tumors in lymph nodes or other organs. However, almost
all lymphoid malignancies can have either presentation and some are almost equally likely to present as a leukemia
or lymphoma. In addition, immune system malignancies represent a spectrum from some of the most indolent
malignancies (eg, some mucosa-associated lymphoid tissue [MALT] lymphomas) to the most rapidly progressive
human cancers (eg, Burkitt lymphoma).
The first system widely utilized for staging non-Hodgkin Lymphomas was actually developed for staging Hodgkin
disease and is referred to as the Ann Arbor Staging System.1 Although primarily an anatomic staging system, the Ann
Arbor stages are modified by the presence or absence of systemic symptoms. It was adjusted over the years for the
use in staging Hodgkin disease,2 but still represents a backbone of the staging system recommended today
for non-Hodgkin Lymphomas. However, recognition that the Ann Arbor system does not subdivide some types of
non-Hodgkin Lymphomas in a clinically useful way, and the recognition that other factors are important in
predicting treatment outcome, led to the development of the International Prognostic Index in 1993.3 The
recommendation for the evaluation of a new patient diagnosed with non-Hodgkin Lymphoma currently involves
application of both these systems.
The current recommendations for staging non-Hodgkin Lymphoma adopted by the American Joint Commission
on Cancer are published in the Cancer Staging Manual, sixth edition.4 These have been developed by a committee
368 CA A Cancer Journal for Clinicians
CA Cancer J Clin 2005;55:368–376
of experts and are reviewed on a regular basis. TABLE 1 American Joint Committee on Cancer
Lymphoma Task Force Members
The membership of the committee on staging
lymphoid neoplasms can be found in Table 1. Member Location
James O. Armitage, MD, Chair Nebraska
Fernando Cabanillas, MD Puerto Rico
CLASSIFICATION OF NON-HODGKIN LYMPHOMA Inez Evans, CTR, RHIT North Carolina
Richard I. Fisher, MD Illinois
Our ability to classify patients with non- Mary K. Gospodarowicz, MD Canada
Nancy Harris, MD Massachusetts
Hodgkin Lymphomas into clinically useful Richard T. Hoppe, MD California
groupings has steadily improved as our under- Robert A. Kyle, MD Minnesota
standing of the biology of the immune system Michael LeBlanc, PhD Washington
Andrew Lister, MD England
has advanced. The use of histopathology to John Sandlund, MD Tennessee
diagnose malignancies and the discovery of the Dennis D. Weisenburger, MD Nebraska
John W. Yarbro, MD Missouri
Reed Sternberg cell early in the 20th century
allowed a distinction between Hodgkin disease
and the other lymphomas grouped together as
overexpressing the associated Bcl-1 protein led
non-Hodgkin Lymphoma. Gall and Mallory
to the acceptance of mantle cell lymphoma as a
proposed a widely used system for subclassify-
specific diagnosis.11 The discovery of CD30
ing the non-Hodgkin Lymphomas in the
(formerly Ki-1) and the recognition that some
1940s.5 However, this system had limited clin-
malignancies marked by CD30 had a t(2;5) and
ical utility. Henry Rappaport used the presence
overexpression of the ALK protein led to the
or absence of a follicular growth pattern and
acceptance of anaplastic large T/null cell lym-
the size and shape of cells to devise the first
phoma as a distinct clinical entity.12–16 Also,
classification system with striking clinical util-
the description of small B-cell lymphomas oc-
ity.6 However, subsequent recognition that
lymphomas were all tumors of lymphocytes curring in association with epithelial tissue,
and that there were different subsets of lym- sometimes developing in association with spe-
phocytes (ie, B, T, and NK cells) led to new cific infections, led to acceptance of the con-
systems. The most popular of these were the cept of MALT lymphomas.17,18 Of course, the
Lukes-Collins classification in the United prototype MALT lymphoma occurs in the
States7 and the Kiel classification in Europe.8,9 stomach and is usually associated with infection
The use of multiple systems of classification by Helicobacter pylori. None of these new lym-
throughout the world posed serious difficulties phomas fit easily into a preexisting category in
for therapeutic research. It was difficult or im- the widely used classification systems and, in
possible to compare the results of therapeutic fact, generally were found in several different
trials when different systems of classification categories.
were utilized. To solve this problem, the In the 1990s, a group of hematopathologists
Working Formulation was developed as a proposed a new system to take into account
compromise system.10 The Working Formula- advances in understanding the biology of the
tion adopted some aspects of the Rappaport immune system and the recognition of these
Classification, the Lukes-Collins Classification, newly accepted subtypes of non-Hodgkin
and Kiel Classification and was the primary Lymphoma, termed the Revised European
system used in publications in much of the American Lymphoma (REAL) classification.19
1980s and 1990s. However, it never became as Diagnoses in the REAL classification were
popular in Europe as in North America. The based on morphology, immunology, and clin-
1980s and 1990s also saw striking advances in ical characteristics. Study of the REAL classifi-
our understanding of biology of the immune cation showed that it was clinically relevant and
system and recognition that some lymphomas more reproducible than previous systems.20
didn’t fit easily into the existing categories. The The concepts embodied in the REAL classifi-
study of lymphomas carrying the t(11;14) and cation were used to develop the World Health
Volume 55 Y Number 6 Y November/December 2005 369
Staging Non-Hodgkin Lymphoma
Organization (WHO) classification of lym- extra lymphatic tumor. Large cutting needle
phoma that is currently the gold standard biopsies are an alternative in selected cases
throughout the world.21 where excisional biopsy is difficult or danger-
The WHO classification is presented in Ta- ous. Fine-needle aspirates are not appropriate
ble 2. It subdivides tumors into those of B-cell and should not be the basis for primary diag-
versus T/NK-cell origin and those with an nosis of non-Hodgkin Lymphoma and the sub-
immature or blastic appearance versus those sequent choice of therapy.22
developing from more mature stages of lym-
phoid development. The latter tumors, in the
case of T-cell lymphomas, were referred to as ANN ARBOR STAGING
“peripheral” T-cell lymphomas. Today, the
first step in evaluation of any patient with non- Although originally developed for staging
Hodgkin Lymphoma should be classification of patients with Hodgkin disease, the Ann Arbor
their tumor in the World Health Organization staging system provides the basis for anatomic
classification. This should include the per- staging in non-Hodgkin Lymphomas as well.
formance of immunophenotyping and might However, the use of the Ann Arbor staging
require cytogenetics, fluorescent in situ hybrid- system for non-Hodgkin Lymphomas has a
ization (FISH), antigen receptor gene rear- number of shortcomings. These relate in large
rangement studies, and other investigations. If part to the different pattern of disease seen in
at all possible, this should be done by an expe- the non-Hodgkin Lymphomas as opposed to
rienced hematopathologist working with an Hodgkin disease. For example, primary extra-
excisional biopsy of an affected lymph node or nodal Hodgkin disease is rare, but a primary
TABLE 2 World Health Organization Classification of Lymphoid Neoplasms
B-cell neoplasms
Precursor B-cell neoplasm
Precursor B-lymphoblastic leukemia/lymphoma (precursor B-cell acute lymphoblastic leukemia)
Mature (peripheral) B-cell neoplasms
B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma
B-cell prolymphocytic leukemia
Lymphoplasmacytic lymphoma
Splenic marginal zone B-cell lymphoma (with or without villous lymphocytes)
Hairy cell leukemia
Plasma cell myeloma/plasmacytoma
Extranodal marginal zone B-cell lymphoma (with or without monocytoid B cells)
Nodal marginal zone B-cell lymphoma (with or without monocytoid B cells)
Follicular lymphoma
Mantle cell lymphoma
Diffuse large B-cell lymphoma
Burkitt lymphoma/Burkitt cell leukemia
T-cell and NK-cell neoplasms
Precursor T-cell neoplasm
Precursor T-lymphoblastic lymphoma/leukemia (precursor T-cell acute lymphoblastic leukemia)
Mature (peripheral) T/NK-cell neoplasma
T-cell prolymphocytic leukemia
T-cell granular lymphocytic leukemia
Aggressive NK-cell leukemia
Adult T-cell lymphoma/leukemia (HTLV1⫹)
Extranodal NK/T-cell lymphoma, nasal type
Enteropathy-type T-cell lymphoma
Hepatosplenic gamma delta T-cell lymphoma
Subcutaneous panniculitis-like T-cell lymphoma
Mycosis fungoides/Sezary syndrome
Anaplastic large cell lymphoma, T/null cell, primary cutaneous type
Peripheral T-cell lymphoma, not otherwise characterized
Angioimmunoblastic T-cell lymphoma
Anaplastic large cell lymphoma, T/null cell, primary systemic type
370 CA A Cancer Journal for Clinicians
CA Cancer J Clin 2005;55:368–376
extra nodal site is frequently seen in certain tion with regional lymph node involvement
types of non-Hodgkin Lymphomas and is al- with or without involvement of other lymph
ways the case in MALT lymphomas. In addi- node regions on the same side of the diaphragm
tion, some types of non-Hodgkin Lymphoma (IIE). The number of regions involved may be
(eg, small lymphocytic lymphoma and mantle indicated by a subscript, for example, II3. Stage
cell lymphoma) have bone-marrow involve- III: Involvement of lymph node regions on
ment in the majority of patients, placing a both sides of the diaphragm (III), which also
disproportionally high number of patients in may be accompanied by extralymphatic exten-
the highest stage. Despite these shortcomings, sion in association with adjacent lymph node
the Ann Arbor staging classification remains the involvement (IIIE) or by involvement of the
best method available for anatomic staging of spleen (IIIS) or both (IIIE,S). Stage IV: Diffuse
non-Hodgkin Lymphomas and has been uni- or disseminated involvement of one or more
versally adopted for this purpose. extralymphatic organs, with or without associ-
The Ann Arbor staging system divides pa- ated lymph node involvement; or isolated ex-
tients into four stages based on localized dis- tralymphatic organ involvement in the absence
ease, multiple sites of disease on one or the of adjacent regional lymph node involvement,
other side of the diaphragm, lymphatic disease but in conjunction with disease in distant
on both sides of the diaphragm, and dissemi- site(s). Any involvement of the liver or bone
nated extranodal disease (Table 3). Localized marrow, or nodular involvement of the lung(s)
extranodal sites of involvement are recognized is always Stage IV. The location of Stage IV
by a subscript E. disease is identified further by specifying site
The definition of these stages as found in the according to the notations listed for Stage III.
Cancer Staging Manual is as follows: Stage I: The distinction between Stage I and Stage II
Involvement of a single lymph node region (I), involvement is based not on individual lymph
or localized involvement of a single extralym- nodes but on what are termed as “lymph node
phatic organ or site in the absence of any lymph regions.” Lymph node regions were defined at
node involvement (IE) (rare in Hodgkin dis- the Rye Symposium in 1965 and have been
ease). Stage II: Involvement of two or more accepted by convention since that time. The
lymph node regions on the same side of the lymph node regions include right cervical (in-
diaphragm (II), or localized involvement of a cluding cervical, supraclavicular, occipital, and
single extralymphatic organ or site in associa- preauricular lymph nodes), left cervical, right
TABLE 3 Ann Arbor Classification and the Cotswold Modifications
Stage Features
I Involvement of a single lymph node region or lymphoid structure (eg, spleen, thymus, Waldeyer’s ring)
II Involvement of two or more lymph node regions on the same side of the diaphragm
III Involvement of lymph regions or structures on both sides of the diaphragm
IV Involvement of extranodal site(s) beyond that designated E
For all stages
A No symptoms
B Fever (⬎38oC), drenching sweats, weight loss (10% body weight over 6 months)
For Stages I to III
E Involvement of a single, extranodal site contiguous or proximal to known nodal site
Cotswold modifications
Massive mediastinal disease has been defined by the Cotswold meeting as a thoracic ratio of maximun transverse
mass diameter greater than or equal to 33% of the internal transverse thoracic diameter measured at the T5/6
intervertebral disc level on chest radiography.
The number of anatomic regions involved should be indicated by a subscript (eg, II3)
Stage III may be subdivided into: III1, with or without plenic, hilar, celiac, or portal nodes;III2, with para-aortic, iliac,
mesenteric nodes
Staging should be identified as clinical stage (CS) or pathologic stage (PS)
A new category of response to therapy, unconfirmed/uncertain complete remission (CR) can be introduced
because of the persistent radiologic abnormalities of uncertain significance
Volume 55 Y Number 6 Y November/December 2005 371
Staging Non-Hodgkin Lymphoma
axillary, left axillary, right infraclavicular, left opsy. The basic staging and investigation for a
infraclavicular, mediastinal, hilar, periaortic, mes- patient with non-Hodgkin Lymphoma in-
sentary, right pelvic, left pelvic, right inguinal cludes all these studies with images usually ob-
femoral, and left inguinal femoral. Multiple tained using computed tomography (CT)
lymph nodes palpable in one of these regions scans. In patients unable to safely undergo a CT
would be Stage I, and involvement of two of scan, magnetic resonance imaging studies are
these regions but on one side of the diaphragm often substituted. Recent advances in func-
would represent Stage II. Unlike Hodgkin dis- tional imaging using positron emission tomog-
ease, it is not uncommon for non-Hodgkin Lym- raphy scans have expanded the possibilities for
phoma to involve other lymph node sites not imaging in non-Hodgkin Lymphoma. How-
included in the core sites from the original Ann ever, clear definitions of what constitutes a site
Arbor classification. These might include epitrao- of involvement and whether or not positron
clear, popliteal, internal mammary, occipital, sub- emission tomography scans can substitute for
mental, perauricular, and other small lymph node CT scans are a point for debate and investiga-
areas. Each of these could also be considered a tion. Patients at high risk for central nervous
separate lymph node site and used in the distinc- system involvement should have a lumbar
tion between Stage I and Stage II. puncture and cerebrospinal fluid cy-
The designation of Stage IV disease implies tology performed. Bone marrow biopsy is a
disseminated disease involving extranodal sites. standard part of the clinical investigation.
However, by convention, involvement of the However, what is an appropriate bone marrow
bone marrow, liver, pleura, and cerebrospinal biopsy has been a point of disagreement, with
fluid are always considered Stage IV even if the some experts saying that bilateral biopsies are
disease is isolated to that organ. Lymphatic necessary. The most important part of a bone
involvement in a draining area from a primary marrow biopsy is obtaining an adequate core
extranodal lymphoma should be designated as for histological evaluation (ie, at least 15 to 20
IIE (eg, a thyroid lymphoma with cervical mm). Whether this is done with one or mul-
lymph node involvement). Lymphoma extend- tiple punctures probably does not matter. Bi-
ing beyond the lymph node capsule involving opsy of other sites (ie, beyond the initial
adjacent organs should also receive the E suffix excisional biopsy on which the diagnosis was
and not be called Stage IV (eg, lymphoma in based) would normally only be done if the
mediastinal lymph nodes growing directly into results might modify therapy.
adjacent lung). It is true that unusual cases In the past there has been debate on how
might lead to debate about the appropriate large a lymph node needed to be for it to be
assignment of Stage IIE or Stage IV, and some- considered abnormal. By convention, lymph
times even experts can disagree about which nodes greater than 1.5 cm in maximum diam-
would be most appropriate. eter are now considered abnormal and assumed
Anatomic staging in non-Hodgkin Lym- to be involved by disease. Documenting
phoma can be done using history, physical ex- splenic involvement lymphoma can be prob-
amination, laboratory studies, and images, in lematic but is usually done by identifying pal-
addition to definitive proof of involvement of a pably enlarged spleens or focal defects seen on
particular site from biopsy. As a practical point, imaging studies. Liver involvement is usually
most patients are assigned their stage based on demonstrated by multiple defects on imaging
the results of noninvasive studies rather than studies consistent with involvement by neo-
having biopsies to document each apparent site plasm or by liver biopsy. The presence of a
of involvement. palpable liver or abnormal liver chemistries
Appropriate clinical staging includes: a care- should not be used alone to assume involve-
ful recording of history and physical examina- ment of the liver by lymphoma. Lung involve-
tion; appropriate images of the chest, abdomen, ment is usually documented by presence of
and pelvis; blood chemistry measurements; characteristic imaging abnormalities. On occa-
complete blood count; and bone marrow bi- sion, lung biopsy may be necessary to clarify
372 CA A Cancer Journal for Clinicians
CA Cancer J Clin 2005;55:368–376
equivocal cases. Clinical involvement of the are not localized and the ability to better assess
brain can be documented by characteristic im- the majority of patients for treatment decisions
aging abnormalities in a patient with lym- and to stratify patients in clinical trials is ex-
phoma known to metastasize to the brain. tremely important. In 1993, the International
However, this is an unusual situation. More Non-Hodgkin Lymphoma Prognostic Index
commonly, primary brain lymphomas require was published.3 This was the result of an inter-
biopsy to document their presence. national collaboration involving more than
Although more useful in Hodgkin disease, 2,000 patients with aggressive non-Hodgkin
the Ann Arbor Staging system also designates Lymphoma who were treated with an anthra-
patients as either being suffix A or B. Designa- cycline-based combination chemotherapy reg-
tion as A indicates the absence of unexplained imen. Although originally intended for the use
fever with temperature greater than 38°C, in patients with aggressive lymphomas, this in-
dex has utility for all types of non-Hodgkin
drenching night sweats requiring the change of
Lymphoma and has been widely applied.
bedclothes, and unexplained weight loss of
Results of the International Prognostic In-
more than 10% in the 6 months before diag-
dex study showed that five factors were
nosis.
roughly equal in power in predicting treatment
outcome (Table 4). These included age greater
INTERNATIONAL PROGNOSTIC INDEX
or less than 60 years, Ann Arbor Stage I and II
versus Stage III or IV, none or one versus two
The Ann Arbor Staging system does not or more sites of extranodal involvement by
adequately provide prognostic information for lymphoma, an Eastern Cooperative Oncology
many subtypes of non-Hodgkin Lymphoma Group performance status (Table 5) of Grade 0
and is far from optimal for making treatment or 1 versus Grade 2 or greater, and a normal
decisions. Knowing when the disease is local- versus elevated lactate dehydrogenase (LDH).
The number of adverse prognostic factors (ie,
ized is an important factor for all types of lym-
age ⬎ 60 years, advanced stage, two or more
phoma, but most non-Hodgkin Lymphomas
extranodal sites, poor performance status, or
elevated LDH) could be simply summed be-
TABLE 4 International Prognostic Index cause each had approximately the same power
Prognostic Factors
in predicting treatment outcome. Thus, a score
Age ⬎ 60 years of 0 to 5 was possible. The original publication
Performance status ⬎ 2 suggested the patients be lumped into groups
Lactate dehydrogenase 1⫻ normal
Extranodal sites ⬎ 2 with a low risk (ie, score of 0 or 1), low
Stage III or IV intermediate risk (score of 2), a high interme-
Risk Category (Factors) diate group (score of 3), and a high risk (score
Low (0 or 1)
Low-intermediate (2) of 4 or 5). In the original study and in previous
High-intermediate (3) experience, there is a highly significant impact
High (4 or 5)
on chances to achieve a remission, remain in
TABLE 5 Eastern Cooperative Oncology Group Performance Status*
Grade Description
0 Fully active, able to carry on all predisease performance without restriction
1 Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature (eg, light housework,
office work)
2 Ambulatory and capable of all self-care but unable to carry out any work activities. Up and about more than 50% of waking hours
3 Capable of only limited self-care, confined to bed or chair more than 50% of waking hours
4 Completely disabled. Cannot carry on any self-care. Totally confined to bed or chair
5 Dead
*As published in Oken, et al.23
Volume 55 Y Number 6 Y November/December 2005 373
Staging Non-Hodgkin Lymphoma
TABLE 6 International Prognostic Index
Five-year
Complete Relapse-free Five-year
Number of Response Rate Survival Overall Survival
Risk Factors (%) (%) (%)
All patients*
Low 0 or 1 87 70 73
Low intermediate 2 67 50 51
High intermediate 3 55 49 43
High 4 or 5 44 40 26
Age-adjusted index, patients ⱕ60 years†
Low 0 92 86 83
Low intermediate 1 78 66 69
High intermediate 2 57 53 46
High 3 46 58 32
*Adverse factors: age ⬎ 60 years, increasing lactate dehydrogenase, performance status 2 to 4, more than one extranodal
site, Ann Arbor Stage III or IV.
†Adverse factors: elevated lactate dehydrogenase, performance status 2 to 4, Ann Arbor Stage III or IV.
remission, and overall survival based on the
International Prognostic Index score. For ex-
ample, patients in the low-risk group in the
original publication had an 87% complete
remission rate and an overall survival of 73%
at 5 years versus a 44% complete remission
rate and 26% survival at 5 years in the high-
risk group (Table 6).3
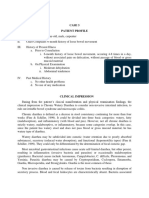
Particularly important was documentation
that the International Prognostic Index score
was able to subdivide patients in Ann Arbor
Stage II, III, and IV (Figure 1). The dramatic
difference in treatment outcome for patients
with the same Ann Arbor Stage found by
utilizing the International Prognostic Index
undoubtedly explains wide discrepancies in
the results of some previous clinical trials.
For example, in Phase II trials, several che-
motherapy regimens seemed to be superior
to cyclophosphamide, doxorubicin, vincris-
tine, and prednisone in the treatment of ag-
gressive lymphoma24 –26 but yielded the same
outcome in a head-to-head Phase III trial.27
In retrospect, the earlier studies almost cer-
tainly treated patients with a better progno-
sis, although the stages were similar.
The International Prognostic Index is pre-
sented in Table 4. This should be calculated on
FIGURE 1 The International Prognostic Index Score every new patient with non-Hodgkin Lym-
Identifies Patients With Differing Prognoses in Patients
With Ann Arbor Stage II, III, and IV Aggressive Non-
phoma and will have an important impact on
Hodgkin Lymphoma. the treatment decision.
374 CA A Cancer Journal for Clinicians
CA Cancer J Clin 2005;55:368–376
THE FUTURE The primary site of origin of a non-Hodgkin
Lymphoma almost certainly affects the biological
There will be further advances in our ability characteristics of the malignancy. There is no
to evaluate patients with non-Hodgkin Lym- reason to believe that diffuse large B-cell lym-
phoma. An obvious possibility, and one that is phoma originating in different sites of the body
currently being tested, is to have different sys- would have the same behavior any more than we
tems for different subsets of patients. For ex- would think that all squamous cell carcinomas,
ample, the International Prognostic Index has a regardless of origin, would have the same behav-
modification for patients younger than and
ior. It is possible that different types of evaluations
older than 60 years old (Table 5).3 A new
would be appropriate for tumors originating in
system has been developed for patients with
different parts of the body.
follicular lymphoma (ie, the Follicular Lym-
The most important factor likely to change
phoma Prognostic Index) to take into account
the way we evaluate patients with lymphoma is
differences between these patients and those
with diffuse aggressive non-Hodgkin Lympho- the rapidly expanding knowledge about gene
ma.28 The American College of Surgeons Stag- expression patterns and protein expression.29,30
ing Manual presents different systems for It is possible to imagine a time when the only
children with non-Hodgkin Lymphoma that evaluation of a new patient with lymphoma
are widely used by pediatric oncologists and that would be required would be identification
one for patients with cutaneous T-cell lympho- of the expression of certain key proteins. If
ma.4 drugs that specifically targeted these proteins
None of the systems currently in use for were available, and they could cure most or all
evaluation of adult patients with non-Hodgkin patients, other evaluation could be superfluous.
Lymphoma account for the presence of a bulky Although certainly a goal for the future, it is
mass. This probably relates the lack of uniform not impossible that we could reach this point.
data collection about the maximum tumor di- Whatever the future holds, at the present
ameter in previous studies. However, the pres- time an accurate staging evaluation is key to the
ence of a very large mass is a predictor of poor management of a patient with newly diagnosed
treatment outcome, and clinicians often take non-Hodgkin Lymphoma. Careful application
very bulky sites of disease into account by of the systems described in this paper will lead
adding radiotherapy to that site. to the best possible treatment outcome.
REFERENCES 7. Lukes RJ, Collins RD. Immunologic charac- 12. Stein H, Mason DY, Gerdes J, et al. The
terization of human malignant lymphomas. expression of the Hodgkin’s disease associated
1. Carbone PP, Kaplan HS, Musshoff K, et al.
Cancer 1974;34(4 Suppl):1488 –1503. antigen Ki-1 in reactive and neoplastic lym-
Report of the committee on Hodgkin’s disease stag-
8. Lennert K, Stein H. Malignant Lymphomas phoid tissue: evidence that Reed-Sternberg
ing classification. Cancer Res 1971;31:1860–1861.
Other than Hodgkin’s Disease: Histology, Cytol- cells and histiocytic malignancies are derived
2. Lister TA, Crowther D, Sutcliffe SB, et al. from activated lymphoid cells. Blood 1985;66:
ogy, Ultrastructure, Immunology. New York:
Report of a committee convened to discuss the Springer-Verlag; 1978. 848–858.
evaluation and staging of patients with Hodgkin’s
9. Lennert K, Stein H, Kaiserling E. Cytological 13. Kaneko Y, Frizzera G, Edamura S, et al. A
disease: Cotswolds meeting. J Clin Oncol 1989;
and functional criteria for the classification of novel translocation, t(2;5)(p23;q35), in child-
7:1630–1636.
malignant lymphomata. Br J Cancer 1975;31 hood phagocytic large T-cell lymphoma mim-
3. A predictive model for aggressive non- (Suppl 2):29 – 43. icking malignant histiocytosis. Blood 1989;73:
Hodgkin’s lymphoma. The International Non- 806–813.
Hodgkin’s Lymphoma Prognostic Factors Project. 10. National Cancer Institute sponsored
study of classifications of non-Hodgkin’s 14. Rimokh R, Magaud JP, Berger F, et al. A
N Engl J Med 1993;329:987–994.
lymphomas: summary and description of a translocation involving a specific breakpoint (q35)
4. AJCC Cancer Staging Manual. 6th ed. New working formulation for clinical usage. on chromosome 5 is characteristic of anaplastic
York: Springer; 2002. The Non-Hodgkin’s Lymphoma Pathologic large cell lymphoma (‘Ki-1 lymphoma’). Br J
5. Gall E, Mallory T. Malignant lymphoma. A clin- Classification Project. Cancer 1982;49:2112– Haematol 1989;71:31–36.
icopathologic survey of 618 cases. Am J Pathol 2135. 15. Bitter MA, Franklin WA, Larson RA, et al.
1942;18:381. 11. Rimokh R, Berger F, Delsol G, et al. Rear- Morphology in Ki-1(CD30)-positive non-
6. Hicks EB, Rappaport H, Winter WJ. Follic- rangement and overexpression of the BCL-1/ Hodgkin’s lymphoma is correlated with clinical
ular lymphoma; a re-evaluation of its position in PRAD-1 gene in intermediate lymphocytic features and the presence of a unique chromo-
the scheme of malignant lymphoma, based on a lymphomas and in t(11q13)-bearing leukemias. somal abnormality, t(2;5)(p23;q35). Am J Surg
survey of 253 cases. Cancer 1956;9:792–821. Blood 1993;81:3063–3067. Pathol 1990;14:305–316.
Volume 55 Y Number 6 Y November/December 2005 375
Staging Non-Hodgkin Lymphoma
16. Mason DY, Bastard C, Rimokh R, et al. 21. Pathology and Genetics of Tumours of 26. Shipp MA, Yeap BY, Harrington DP, et al.
CD30-positive large cell lymphomas (‘Ki-1 lym- Haematopoietic and Lymphoid Tissues, in Jaffe The m-BACOD combination chemotherapy regi-
phoma’) are associated with a chromosomal trans- E, Harris N, Stein H, Vardiman J (eds). World men in large-cell lymphoma: analysis of the com-
location involving 5q35 [see comments]. Br J Health Organization Classification of Tumors. pleted trial and comparison with the M-BACOD
Haematol 1990;74:161–168. Lyon: IARC Press; 2001. regimen. J Clin Oncol 1990;8:84–93.
17. Isaacson P, Wright DH. Malignant lym- 22. Hehn ST, Grogan TM, Miller TP. Utility of 27. Fisher RI, Gaynor ER, Dahlberg S, et al.
phoma of mucosa-associated lymphoid tissue. A fine-needle aspiration as a diagnostic technique in Comparison of a standard regimen (CHOP) with
distinctive type of B-cell lymphoma. Cancer lymphoma. J Clin Oncol 2004;22:3046 –3052. three intensive chemotherapy regimens for ad-
1983;52:1410–1416. 23. Oken MM, Creech RH, Tormey DC, et al. vanced non-Hodgkin’s lymphoma. N Engl J Med
Toxicity and response criteria of the Eastern Co- 1993;328:1002–1006.
18. Isaacson P, Wright DH. Extranodal malig-
operative Oncology Group. Am J Clin Oncol 28. Solal-Celigny P, Roy P, Colombat P, et al.
nant lymphoma arising from mucosa-associated
1982;5:649 – 655. Follicular lymphoma international prognostic in-
lymphoid tissue. Cancer 1984;53:2515–2524. dex. Blood 2004;104:1258–1265.
24. Longo DL, DeVita VT, Jr., Duffey, PL,
19. Harris NL, Jaffe ES, Stein H, et al. A revised et al. Superiority of ProMACE-CytaBOM over 29. Rosenwald A, Wright G, Chan WC, et al.
European-American classification of lymphoid neo- ProMACE-MOPP in the treatment of ad- The use of molecular profiling to predict survival
plasms: a proposal from the International Lym- vanced diffuse aggressive lymphoma: results of after chemotherapy for diffuse large-B-cell lym-
phoma Study Group. Blood 1994;84:1361–1392. a prospective randomized trial. J Clin Oncol phoma. N Engl J Med 2002;346:1937–1947.
20. The non-Hodgkin’s Lymphoma classification 1991;9:25–38. 30. Shipp MA, Ross KN, Tamayo P, et al. Dif-
project: a clinical evaluation of the International 25. Klimo P, Connors JM. MACOP-B chemo- fuse large B-cell lymphoma outcome prediction
Lymphoma Study Group classification of non- therapy for the treatment of diffuse large-cell by gene-expression profiling and supervised ma-
Hodgkin’s lymphoma. Blood 1997;89:3909 –3918. lymphoma. Ann Intern Med 1985;102:596–602. chine learning. Nat Med 2002;8:68–74.
376 CA A Cancer Journal for Clinicians
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- RxPrep 6-8 Week Study Review ScheduleDocument5 pagesRxPrep 6-8 Week Study Review ScheduleKilva Eratul100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Sel&Ass&Pae&Lis&Car&1 STDocument198 pagesSel&Ass&Pae&Lis&Car&1 STali tida100% (1)
- NCP: Chronic Obstructive Pulmonary Disease and AsthmaDocument15 pagesNCP: Chronic Obstructive Pulmonary Disease and AsthmaJavie100% (5)
- 25 RDSDocument7 pages25 RDSFinty ArfianNo ratings yet
- Neurology Clerkship UWORLD: Brain TumoursDocument13 pagesNeurology Clerkship UWORLD: Brain TumoursHaadi AliNo ratings yet
- Brain TumorsDocument2 pagesBrain TumorsScott McElroyNo ratings yet
- 1-CBC InterpretationDocument10 pages1-CBC Interpretationمصطفي خندقاويNo ratings yet
- Researching Alzheimer's Medicines - Setbacks and Stepping StonesDocument20 pagesResearching Alzheimer's Medicines - Setbacks and Stepping StonesOscar EspinozaNo ratings yet
- Leishmaniasis: Dr. Kazi Shihab Uddin Mbbs MRCP (Uk) Associate Professor & HOD Department of Internal MedicineDocument20 pagesLeishmaniasis: Dr. Kazi Shihab Uddin Mbbs MRCP (Uk) Associate Professor & HOD Department of Internal MedicineSHIHAB UDDIN KAZINo ratings yet
- Folinic AcidDocument1 pageFolinic AcidMuhammad ArsalanNo ratings yet
- Background of The StudyDocument7 pagesBackground of The StudyVern LeStrangeNo ratings yet
- Signs NotesDocument22 pagesSigns NotesVaidehi guptaNo ratings yet
- Herpes Simplex Type-1 Virus Infection (2003)Document16 pagesHerpes Simplex Type-1 Virus Infection (2003)Aron RonalNo ratings yet
- FMGE JUNE-2109 Questions: AriseDocument20 pagesFMGE JUNE-2109 Questions: AriseSugithaTamilarasanNo ratings yet
- Kawasaki Disease-NcpDocument5 pagesKawasaki Disease-NcpBelen SoleroNo ratings yet
- Pathophysiology CVA (Final2)Document10 pagesPathophysiology CVA (Final2)Jayselle Costes FelipeNo ratings yet
- HeparinDocument6 pagesHeparinFrank Asiedu AduseiNo ratings yet
- Mixed Group: Name: Age: Sex: Weight: Address: OccupationDocument23 pagesMixed Group: Name: Age: Sex: Weight: Address: OccupationKristian Karl Bautista Kiw-isNo ratings yet
- Stroke Differential Diagnosis and Mimics Part 1Document11 pagesStroke Differential Diagnosis and Mimics Part 1AnthoNo ratings yet
- The 90 Day Program To Beat Candida Restore Vibrant HealthDocument136 pagesThe 90 Day Program To Beat Candida Restore Vibrant HealthMihaela NNo ratings yet
- Peptic Ulcer Disease UpdatedDocument19 pagesPeptic Ulcer Disease UpdatedKiara GovenderNo ratings yet
- Ovariancancer 161007042738Document63 pagesOvariancancer 161007042738Syahmi YahyaNo ratings yet
- Practice Essentials: Abruptio PlacentaeDocument2 pagesPractice Essentials: Abruptio PlacentaeNurnajwa PahimiNo ratings yet
- Case Study - Parkinson'S Disease: Clinical Pharmacy & Therapeutics 1Document13 pagesCase Study - Parkinson'S Disease: Clinical Pharmacy & Therapeutics 1Jenesis Cairo CuaresmaNo ratings yet
- HydronephrosisDocument2 pagesHydronephrosisStefan ZemoraNo ratings yet
- 2024-Article Text-6560-1-10-20230128Document4 pages2024-Article Text-6560-1-10-20230128Adniana NareswariNo ratings yet
- Anemia OsamaDocument57 pagesAnemia Osamaosamafoud7710No ratings yet
- Note DR Ikhwan SaniDocument39 pagesNote DR Ikhwan SaniShutter Man100% (1)
- Para PBL CompleteDocument9 pagesPara PBL CompleteMerill Harrelson LibanNo ratings yet
- XXX. MCQ Cardiovascular System Book 315-336Document19 pagesXXX. MCQ Cardiovascular System Book 315-336Maria OnofreiNo ratings yet