Professional Documents
Culture Documents
NigJCardiol14115-1209864 032138
NigJCardiol14115-1209864 032138
Uploaded by
Timotius Gatma Buntori PurbaCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- Mind Pump - Reverse-Dieting-101-ebook-finalProofDocument57 pagesMind Pump - Reverse-Dieting-101-ebook-finalProofa350jamesNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- TMC CatalogDocument35 pagesTMC CatalogAdriano Guedes100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Fundamentals Exam ADocument38 pagesFundamentals Exam APatrice Miller100% (3)
- Shannon Sovndal Fitness CyclingDocument224 pagesShannon Sovndal Fitness CyclingJuan Antonio100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hamer Conflict DiseaseDocument2 pagesHamer Conflict DiseasemoninistorNo ratings yet
- What Are Gallstones?: Lemuel Jay A. Segovia Grade 8-Peace Science Q4M1Document4 pagesWhat Are Gallstones?: Lemuel Jay A. Segovia Grade 8-Peace Science Q4M1Zarah Joyce SegoviaNo ratings yet
- BMI Grade 10Document24 pagesBMI Grade 10Bry Mon Gacelo RosaNo ratings yet
- Of Burning Fat: While You SleepDocument16 pagesOf Burning Fat: While You SleepMcel PadiernosNo ratings yet
- How To Write A 8-10 Page Research PaperDocument8 pagesHow To Write A 8-10 Page Research Paperjpkoptplg100% (1)
- Hhs Lower Body Lesson Plan Leg DayDocument3 pagesHhs Lower Body Lesson Plan Leg Dayapi-481363865No ratings yet
- Scoring Short Ipaq April04Document9 pagesScoring Short Ipaq April04AmirAmiriNo ratings yet
- Salty EggDocument7 pagesSalty EggAndi Fildah YakubNo ratings yet
- Health IssuesDocument13 pagesHealth IssuesTarquin TomadaNo ratings yet
- Biology f212 Mixed Question PaperDocument198 pagesBiology f212 Mixed Question Paperapi-275024237No ratings yet
- Analytical Exposition Text 2Document3 pagesAnalytical Exposition Text 2lnanurulizzatiNo ratings yet
- PE LM Gr8Document204 pagesPE LM Gr8Princess Diloy Costa100% (1)
- Food Labels ExerciseDocument20 pagesFood Labels ExerciseAnonymous h2EnKyDbNo ratings yet
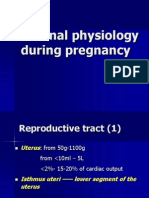
- Maternal Physiology During PregnancyDocument28 pagesMaternal Physiology During PregnancyPutra MahautamaNo ratings yet
- B Plan 9Document130 pagesB Plan 9Suhasini IyerNo ratings yet
- Mock Research Paper - FinalDocument4 pagesMock Research Paper - Finalapi-251159778No ratings yet
- Death by VeganismDocument3 pagesDeath by VeganismrocosanaNo ratings yet
- Chocolate LectureDocument9 pagesChocolate LectureShane HintonNo ratings yet
- Endocrine System GlandsDocument40 pagesEndocrine System GlandsSolita PorteriaNo ratings yet
- Taller de InglesDocument24 pagesTaller de InglesManuela Henao0% (2)
- The Role of Dialysis Nurse On Nutritional Therapy of DialysisDocument6 pagesThe Role of Dialysis Nurse On Nutritional Therapy of DialysisAryoNo ratings yet
- Cola Drink Are Bad For Your HealthDocument4 pagesCola Drink Are Bad For Your HealthLydia AfzanNo ratings yet
- ?overview of Secondary Prevention of Ischemic Stroke - UpToDateDocument40 pages?overview of Secondary Prevention of Ischemic Stroke - UpToDateJorgeNo ratings yet
- DM in Pregnancy PDFDocument89 pagesDM in Pregnancy PDFMichael Angelo BrinezNo ratings yet
- Weight Loss Energy Medicine Tips ChartDocument3 pagesWeight Loss Energy Medicine Tips ChartBreslo100% (1)
NigJCardiol14115-1209864 032138
NigJCardiol14115-1209864 032138
Uploaded by
Timotius Gatma Buntori PurbaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NigJCardiol14115-1209864 032138
NigJCardiol14115-1209864 032138
Uploaded by
Timotius Gatma Buntori PurbaCopyright:
Available Formats
[Downloaded free from http://www.nigjcardiol.org on Monday, January 13, 2020, IP: 114.122.10.
167]
Review Article
The eighth Joint National Committee on the prevention,
detection, evaluation, and treatment of high blood pressure
(Joint National Committee‑8) report: Matters arising
Ogba Joseph Ukpabi, Iheanyi Damian Ewelike
Department of Internal Medicine, Federal Medical Centre, Umuahia, Abia State, Nigeria
Abstract America’s Joint National Committee (JNC) on the prevention, detection, evaluation, and treatment of high
blood pressure is one of the foremost regional regulatory bodies on the management of hypertension.
Its latest report (JNC‑8) of 2014 has attracted a lot of strong criticisms. The aim of this review is to offer a
summarized insight into the different opinions that have trailed its process and content since its publication.
Keywords: Hypertension guidelines, Joint National Committee‑7, Joint National Committee‑8, matters arising
Address for correspondence: Dr. Ogba Joseph Ukpabi, Department of Internal Medicine, Federal Medical Center, Umuahia, Abia State, Nigeria.
E‑mail: ojukpabi@yahoo.com
INTRODUCTION hypertension and recommend guidelines. The WHO
and ISH expect Regional and National Societies to adapt
Worldwide, 7.6 million premature deaths (about 13.5% of the and evolve suitable guidelines based on evidence from
total) and 92 million disability‑adjusted life years – 60% of local studies as well as peculiar regional and national
the global total – were attributed to high blood pressure (BP) circumstances. America’s Joint National Committee (JNC)
in 2001.[1] Hypertension affects 65 million Americans.[2] The on the prevention, detection, evaluation, and treatment of
United States (US) between 1999 and 2004 had an overall high BP is one of the foremost regional regulatory bodies
prevalence of 29.3%,[3] and between 2001 and 2011 in on the management of hypertension.
Nigeria, it is put at 22.5%.[4] Control of hypertension is
even more important in Nigeria considering that about 80% JOINT NATIONAL COMMITTEE‑8
of the attributable burden occurred in low‑income and RECOMMENDATIONS
middle‑income economies and over half occurred in people
aged 45–69 years.[1] Most of the disease burden caused by high The latest review of the management of hypertension
BP is borne by low‑income and middle‑income countries, by by the JNC was published in 2014 as JNC‑8. Table 1
people in middle age, and by people with prehypertension.[1] contains summaries of the report.[6] Evidence for their
According to the World Health Organization (WHO), Nigeria recommendations was drawn from randomized control
is considered a middle‑income economy.[5] trials (RCTs).[6] Evidence quality and recommendations
were graded based on their effect on important outcomes.
At the global level, the WHO and International Society James et al. commenting on JNC‑8 stated that the work set
of Hypertension (ISH) regulate the management of
This is an open access article distributed under the terms of the Creative Commons
Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak,
Access this article online and build upon the work non‑commercially, as long as the author is credited and the
Quick Response Code: new creations are licensed under the identical terms.
Website:
www.nigjcardiol.org For reprints contact: reprints@medknow.com
How to cite this article: Ukpabi OJ, Ewelike ID. The eighth joint national
DOI: committee on the prevention, detection, evaluation, and treatment of high
10.4103/0189-7969.201909 blood pressure (joint national committee-8) report: Matters arising. Nig J
Cardiol 2017;14:15-8.
© 2017 Nigerian Journal of Cardiology | Published by Wolters Kluwer - Medknow 15
[Downloaded free from http://www.nigjcardiol.org on Monday, January 13, 2020, IP: 114.122.10.167]
Ukpabi and Ewelike: Matters arising from JNC‑8
out to synthesize the latest available scientific evidence and Table 1: The summaries of Joint National Committee‑8
update existing clinical recommendations on hypertension recommendations
control in order to minimize patients’ risk for cardiovascular Recommendation 1
In the general population aged ≥60 years, initiate pharmacologic
and other complications. treatment to lower BP at SBP ≥150 mmHg or DBP≥90 mmHg and
treat to a goal SBP <150 mmHg and goal DBP<90 mmHg (strong
Reactions recommendation ‑ Grade A)
Corollary recommendation
In JNC‑8, the critical questions and review criteria
In the general population aged ≥60 years, if pharmacologic treatment
were defined by an expert panel with input from the for high BP results in lower achieved SBP (e.g., <140 mmHg) and
methodology team, followed by initial systematic review by treatment is well tolerated and without adverse effects on health
or quality of life, treatment does not need to be adjusted (expert
methodologists restricted to RCT evidence.[6,7] Subsequent opinion ‑ Grade E)
review of RCT evidence and recommendations were Recommendation 2
made by the panel according to the standard protocol.[6,7] In the general population <60 years, initiate pharmacologic treatment
to lower BP at DBP ≥90 mmHg and treat to a goal DBP <90 mmHg. (for
In JNC‑7, methodology was based on nonsystematic ages 30-59 years, strong recommendation ‑ Grade A; for ages
literature review by an expert committee including a range 18-29 years, expert opinion ‑ Grade E)
of study designs, and recommendations were made based Recommendation 3
In the general population <60 years, initiate pharmacologic treatment
on consensus.[7,8] This change is said to be an improvement to lower BP at SBP ≥140 mmHg and treat to a goal SBP <140 mmHg
on the previous process of the past JNCs.[9] (expert opinion ‑ Grade E)
Recommendation 4
In the population aged ≥18 years with CKD, initiate pharmacologic
However, JNC‑8 report remains a guide not a law and it is treatment to lower BP at SBP ≥140 mmHg or DBP ≥90 mmHg and
not meant to substitute clinical judgment.[6,10] This supports treat to goal SBP <140 mmHg and goal DBP <90 mmHg
the opinion of some critics that it is not given that clinical (expert Opinion ‑ Grade E)
Recommendation 5
practice guidelines benefit patients.[11] In the population aged ≥18 years with diabetes, initiate
pharmacologic treatment to lower BP at SBP≥140 mmHg or DBP ≥90
Despite all the work, 6 of 11 recommendations had to be mmHg and treat to a goal SBP<140 mmHg and goal DBP <90 mmHg
(expert opinion ‑ Grade E)
based on expert opinions (Grade E).[6,10]
Recommendation 6
In the general non‑Black population, including those with diabetes,
In June 2013, the National Heart Lung and Blood initial antihypertensive treatment should include a thiazide‑type
Institute (NHLBI) announced its decision to discontinue diuretic, CCB, ACEI, or ARB (moderate recommendation ‑ Grade B)
Recommendation 7
developing clinical guidelines including those in process; In the general Black population, including those with diabetes,
instead, they would develop systematic reviews and work initial antihypertensive treatment should include a thiazide‑type
diuretic or CCB (For general Black population: moderate
with external stakeholders in developing guidelines.[12]
recommendation – Grade B; For Black patients with diabetes: weak
NHLBI neither did endorse JNC‑8 nor did any US federal recommendation – Grade C)
agency.[6] JNC‑7 which was a review by 39 professional, Recommendation 8
In the population aged ≥18 years with CKD, initial (or add‑on)
public, and voluntary organizations and seven federal antihypertensive treatment should include an ACEI or ARB to
agencies had wide acceptance. In contrast, JNC‑8 was a improve kidney outcomes. This applies to all CKD patients with
review by selected 16 individual experts and five federal hypertension regardless of race or diabetes status (moderate
recommendation ‑ Grade B)
agencies.[13] Recommendation 9
The main objective of hypertension treatment is to attain and maintain
Uncertain confidence toward the JNC‑8 started after the goal BP. If goal BP is not reached within a month of treatment, increase
NHBLI made that announcement and turned the guideline the dose of the initial drug or add a second drug from one of the classes
in recommendation 6 (thiazide‑type diuretic, CCB, ACEI, or ARB).
development process to the American Heart Association The clinician should continue to assess BP and adjust the treatment
and American College of Cardiology, but both associations regimen until goal BP is reached. If goal BP cannot be reached with
two drugs, add and titrate a third drug from the list provided. Do not
with this new mandate did not review the JNC‑8 report
use an ACEI and an ARB together in the same patient. If goal BP cannot
before its publication.[9] be reached using only the drugs in recommendation 6 because of a
contraindication or the need to use more than three drugs to reach goal
There still remains the issue of nonagreeability on BP BP, antihypertensive drugs from other classes can be used. Referral to
a hypertension specialist may be indicated for patients in whom goal
targets for the commencement of antihypertensive which BP cannot be attained using the above strategy or for the management
leaves the clinician to use their best judgment for their of complicated patients for whom additional clinical consultation is
needed (expert opinion ‑ Grade E)
individual patients.[6,10,14] The 2013 European Society of
Hypertension/European Society of Cardiology (ESH/ BP ‑ Blood pressure; SBP ‑ Systolic blood pressure; DBP ‑ Diastolic
blood pressure; CKD ‑ Chronic kidney disease; CCB ‑ Calcium
ESC) guidelines for the management of arterial channel blocker; ACEI ‑ Angiotensin‑converting enzyme inhibitor;
hypertension agreed with recommendation 1 of the ARB ‑ Angiotensin receptor blocker
16 Nigerian Journal of Cardiology | Volume 14 | Issue 1 | January-June 2017
[Downloaded free from http://www.nigjcardiol.org on Monday, January 13, 2020, IP: 114.122.10.167]
Ukpabi and Ewelike: Matters arising from JNC‑8
JNC‑8,[15] following the findings of Hypertension in Financial support and sponsorship
the Very Elderly Trial.[16] The 2013 ESH/ESC further Nil.
suggested that for elderly people <80 years of age who
are fit and can tolerate it considering a systolic BP (SBP) Conflicts of interest
of <140 mmHg goal would also be beneficial. There is a There are no conflicts of interest.
similar additional consideration in the recommendation
REFERENCES
1 of JNC‑8, but it has no age upper limit.[6] The SBP
cutoff for initiation of therapy and goal in the general 1. Lawes CM, Vander Hoorn S, Rodgers A; International Society of
population 60 years and above is the most important Hypertension. Global burden of blood‑pressure‑related disease, 2001.
source of disagreement. [17,18] The South African Lancet 2008;371:1513‑8.
2. Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The
Hypertension Practice Guideline 2014 out‑rightly rejected
burden of adult hypertension in the United States 1999 to 2000: A
recommendation 1 of the JNC‑8[19] and others expressed rising tide. Hypertension 2004;44:398‑404.
concern regarding the recommendation.[13] Some would 3. Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence,
consider this recommendation the most controversial[13] awareness, treatment, and control of hypertension among United
States adults 1999‑2004. Hypertension 2007;49:69‑75.
while another angle to the controversy would be that there 4. Ogah OS, Okpechi I, Chukwuonye II, Akinyemi JO, Onwubere BJ,
were no Blacks in the two major studies – the Valsartan Falase AO, et al. Blood pressure, prevalence of hypertension and
in Elderly Isolated Systolic Hypertension[20] and JATOS[21] hypertension related complications in Nigerian Africans: A review.
trials – used. World J Cardiol 2012;4:327‑40.
5. Country and Lending Groups | Data. The World Bank; 2015. Available
from: http://www.data.worldbank.org. [Last accessed on 2016 Jun 29].
The fourth recommendation did not reflect the 6. James PA, Oparil S, Carter BL, Cushman WC, Dennison‑Himmelfarb C,
comprehensive advice of the expert committee in its Handler J, et al. 2014 evidence‑based guideline for the management
discussion on BP management in patients with chronic of high blood pressure in adults: Report from the panel members
appointed to the Eight Joint National Committee (JNC 8). JAMA
kidney disease and proteinuria (especially in the elderly).[6,13]
2014;311:507‑20.
7. Mahajan R. Joint National Committee 8 report: How it differs from
There are also objections to fifth recommendation citing JNC 7. Int J Appl Basic Med Res 2014;4:61‑2.
strict criteria for inclusion of studies as an obstacle to 8. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA,
flexibility,[13] and this recommendation is in conflict with Izzo JL Jr., et al. Seventh report of the Joint National Committee
on prevention, detection, evaluation, and treatment of high blood
Kidney Disease: Improving Global Outcomes guideline,[22] pressure. Hypertension 2003;42:1206‑52.
American Diabetic Association, [23] and ESH/ESC 9. Sox HC. Assessing the trustworthiness of the guideline for
guideline[15] on BP goals in patients with diabetes. management of high blood pressure in adults. JAMA 2014;311:472‑4.
10. Black HR. JNC 8 Reviewed. Medscape Cardiology; 2013. Available
from: http://www.medscape.com/viewarticle/818018_5. [Last
The last recommendation failed to say what the qualification accessed on 2016 Jun 29].
of the hypertension specialist should be.[13] 11. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical
guidelines: Potential benefits, limitations, and harms of clinical
CONCLUSION guidelines. BMJ 1999;318:527‑30.
12. Gibbons GH, Shurin SB, Mensah GA, Lauer MS. Refocusing the agenda
The JNC‑8 has been strongly criticized, especially the first on cardiovascular guidelines: An announcement from the National
Heart, Lung, and Blood Institute. Circulation 2013;128:1713‑5.
recommendation which happens to bear a Grade A level 13. Reisin E, Harris RC, Rahman M. Commentary on the 2014 BP
of confidence.[6] The process was more in agreement with guidelines from the panel appointed to the Eighth Joint National
the Institute of Medicine guidelines than the previous Committee (JNC 8). J Am Soc Nephrol 2014;25:2419‑24.
JNC, but it has come under criticism for excluding 14. Hernandez‑Vila E. A review of the JNC 8 blood pressure guideline.
Tex Heart Inst J 2015;42:226‑8.
too many publications and having to work with too 15. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M,
few publications (especially for recommendation 1) in et al. 2013 ESH/ESC guidelines for the management of arterial
coming up with their final recommendations.[10,13,17,18] hypertension: The task force for the management of arterial
hypertension of the European Society of Hypertension (ESH)
Global guidelines need to be more complementary and
and of the European Society of Cardiology (ESC). Eur Heart J
fundamentally reflect similar viewpoints. It is belated 2013;34:2159‑219.
for Sub‑Saharan Africa to come up with an international 16. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D,
guideline on hypertension since we carry a large burden et al. Treatment of hypertension in patients 80 years of age or older.
N Engl J Med 2008;358:1887‑98.
of the diseases attributable to hypertension and some 17. Krakoff LR, Gillespie RL, Ferdinand KC, Fergus IV, Akinboboye O,
of these recommendations are based on studies which Williams KA, et al. 2014 hypertension recommendations from the
excluded Blacks. Eighth Joint National Committee panel members raise concerns
Nigerian Journal of Cardiology | Volume 14 | Issue 1 | January-June 2017 17
[Downloaded free from http://www.nigjcardiol.org on Monday, January 13, 2020, IP: 114.122.10.167]
Ukpabi and Ewelike: Matters arising from JNC‑8
for elderly black and female populations. J Am Coll Cardiol Rationale and design. Hypertens Res 2004;27:657‑61.
2014;64:394‑402. 21. JATOS Study Group. Principal results of the Japanese trial to
18. Wr i g h t J T J r. , F i n e L J, L a ck l a n d D T, O g e d e g b e G, assess optimal systolic blood pressure in elderly hypertensive
Dennison Himmelfarb CR. Evidence supporting a systolic blood patients (JATOS). Hypertens Res 2008;31:2115‑27.
pressure goal of less than 150 mm Hg in patients aged 60 years or 22. Kidney Disease: Improving Global Outcomes Blood Pressure Work
older: The minority view. Ann Intern Med 2014;160:499‑503. Group. KDIGO clinical practice guidelines for the management of
19. Seedat YK, Rayner BL; Southern African Hypertension Society. South blood pressure in chronic kidney disease. Kidney Int 2012;2:337‑414.
African hypertension guideline 2011. S Afr Med J 2011;102(1 Pt 2):57‑83. 23. American Diabetes Association. Standards of Medical Care in
20. Ogihara T, Saruta T, Matsuoka H, Shimamoto K, Fujita T, Shimada K, Diabetes – 2013. Diabetes Care. Available from: http://www.care.
et al. valsartan in elderly isolated systolic hypertension (VALISH) study: diabetesjournals.org. [Last accessed on 2016 Jun 29].
18 Nigerian Journal of Cardiology | Volume 14 | Issue 1 | January-June 2017
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- Mind Pump - Reverse-Dieting-101-ebook-finalProofDocument57 pagesMind Pump - Reverse-Dieting-101-ebook-finalProofa350jamesNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- TMC CatalogDocument35 pagesTMC CatalogAdriano Guedes100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Fundamentals Exam ADocument38 pagesFundamentals Exam APatrice Miller100% (3)
- Shannon Sovndal Fitness CyclingDocument224 pagesShannon Sovndal Fitness CyclingJuan Antonio100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hamer Conflict DiseaseDocument2 pagesHamer Conflict DiseasemoninistorNo ratings yet
- What Are Gallstones?: Lemuel Jay A. Segovia Grade 8-Peace Science Q4M1Document4 pagesWhat Are Gallstones?: Lemuel Jay A. Segovia Grade 8-Peace Science Q4M1Zarah Joyce SegoviaNo ratings yet
- BMI Grade 10Document24 pagesBMI Grade 10Bry Mon Gacelo RosaNo ratings yet
- Of Burning Fat: While You SleepDocument16 pagesOf Burning Fat: While You SleepMcel PadiernosNo ratings yet
- How To Write A 8-10 Page Research PaperDocument8 pagesHow To Write A 8-10 Page Research Paperjpkoptplg100% (1)
- Hhs Lower Body Lesson Plan Leg DayDocument3 pagesHhs Lower Body Lesson Plan Leg Dayapi-481363865No ratings yet
- Scoring Short Ipaq April04Document9 pagesScoring Short Ipaq April04AmirAmiriNo ratings yet
- Salty EggDocument7 pagesSalty EggAndi Fildah YakubNo ratings yet
- Health IssuesDocument13 pagesHealth IssuesTarquin TomadaNo ratings yet
- Biology f212 Mixed Question PaperDocument198 pagesBiology f212 Mixed Question Paperapi-275024237No ratings yet
- Analytical Exposition Text 2Document3 pagesAnalytical Exposition Text 2lnanurulizzatiNo ratings yet
- PE LM Gr8Document204 pagesPE LM Gr8Princess Diloy Costa100% (1)
- Food Labels ExerciseDocument20 pagesFood Labels ExerciseAnonymous h2EnKyDbNo ratings yet
- Maternal Physiology During PregnancyDocument28 pagesMaternal Physiology During PregnancyPutra MahautamaNo ratings yet
- B Plan 9Document130 pagesB Plan 9Suhasini IyerNo ratings yet
- Mock Research Paper - FinalDocument4 pagesMock Research Paper - Finalapi-251159778No ratings yet
- Death by VeganismDocument3 pagesDeath by VeganismrocosanaNo ratings yet
- Chocolate LectureDocument9 pagesChocolate LectureShane HintonNo ratings yet
- Endocrine System GlandsDocument40 pagesEndocrine System GlandsSolita PorteriaNo ratings yet
- Taller de InglesDocument24 pagesTaller de InglesManuela Henao0% (2)
- The Role of Dialysis Nurse On Nutritional Therapy of DialysisDocument6 pagesThe Role of Dialysis Nurse On Nutritional Therapy of DialysisAryoNo ratings yet
- Cola Drink Are Bad For Your HealthDocument4 pagesCola Drink Are Bad For Your HealthLydia AfzanNo ratings yet
- ?overview of Secondary Prevention of Ischemic Stroke - UpToDateDocument40 pages?overview of Secondary Prevention of Ischemic Stroke - UpToDateJorgeNo ratings yet
- DM in Pregnancy PDFDocument89 pagesDM in Pregnancy PDFMichael Angelo BrinezNo ratings yet
- Weight Loss Energy Medicine Tips ChartDocument3 pagesWeight Loss Energy Medicine Tips ChartBreslo100% (1)