Professional Documents
Culture Documents
NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy
NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy
Uploaded by
Sapna thakurCopyright:
Available Formats
You might also like
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNo ratings yet
- Risk For Acute ConfusionDocument2 pagesRisk For Acute ConfusionChar PereaNo ratings yet
- Impaired Liver FunctionDocument1 pageImpaired Liver FunctionShop Dzubiri Here75% (4)
- NCPDocument1 pageNCPhaniehaehae100% (1)
- NCP - Fluid RetentionDocument3 pagesNCP - Fluid RetentionMichelle Teodoro100% (1)
- Nursing Care Plan2 CVADocument4 pagesNursing Care Plan2 CVAhermesdave1No ratings yet
- BPH NCPDocument1 pageBPH NCPJayson BenitezNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- NCP: Acute GastroenteritisDocument3 pagesNCP: Acute GastroenteritishauteanicoleNo ratings yet
- NCP DobDocument1 pageNCP DobsarahAcristobalNo ratings yet
- NCP For RS-HF (Cor PulmonaleDocument5 pagesNCP For RS-HF (Cor PulmonaleMika Saldaña100% (1)
- EdemaDocument2 pagesEdemaVirus50% (2)
- NCPDocument2 pagesNCPDidith AbanNo ratings yet
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionMitsika AnadiaNo ratings yet
- Acute Pain OsteosarcomaDocument8 pagesAcute Pain OsteosarcomaMaryjoy Gabriellee De La Cruz100% (1)
- NCP Liver CirrosisDocument2 pagesNCP Liver CirrosisRosebud RoseNo ratings yet
- Cues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale EvaluationDocument4 pagesCues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale EvaluationEjie Boy Isaga100% (1)
- Impaired Urinary EliminationDocument3 pagesImpaired Urinary EliminationAgcopra MtchNo ratings yet
- Nursing Care Plan Student Nurse: Diestro, Angela Mae BSN 2BDocument3 pagesNursing Care Plan Student Nurse: Diestro, Angela Mae BSN 2BAngela Mae DiestroNo ratings yet
- Risk For Ineffective Airway Clearance 1Document8 pagesRisk For Ineffective Airway Clearance 1kint manlangitNo ratings yet
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonNo ratings yet
- Nursing Care Plan: Cues/Clues Nursing Diagnosis Rationale Objectives Nursing Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Cues/Clues Nursing Diagnosis Rationale Objectives Nursing Intervention Rationale EvaluationJennirose JingNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDocument1 pageNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationJhevilin RM100% (1)
- Patty NCP HyperthermiaDocument4 pagesPatty NCP HyperthermiaPatricia Jean FaeldoneaNo ratings yet
- Nursing Care Plan: Subjective Data " GoalDocument2 pagesNursing Care Plan: Subjective Data " GoalJay VillasotoNo ratings yet
- 2 Acute Pain Chronic Renal Failure Nursing Care PlansDocument5 pages2 Acute Pain Chronic Renal Failure Nursing Care Plansjustin_saneNo ratings yet
- NCP - Patient With Endotracheal TubeDocument1 pageNCP - Patient With Endotracheal TubeSelwynVillamorPatenteNo ratings yet
- NCP 1Document5 pagesNCP 1Denisse Shazz Mae MaretNo ratings yet
- NCP RiskDocument3 pagesNCP RiskMaricar Azolae MascualNo ratings yet
- Pleural EffusionDocument5 pagesPleural EffusionTerizla MobileNo ratings yet
- NCP LocDocument2 pagesNCP LocMel RodolfoNo ratings yet
- Nursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale EvaluationDocument1 pageNursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale Evaluationeihjay-bravo-8041No ratings yet
- NCP - Altered Tissue PerfusionDocument2 pagesNCP - Altered Tissue PerfusionLeigh Kristel Andrion0% (1)
- "Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientDocument2 pages"Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientMussaib Mushtaq100% (1)
- Word Ncp.......... TetanusDocument3 pagesWord Ncp.......... TetanusYvounne Ananias Bautista RNNo ratings yet
- Amlodipine CPDocument2 pagesAmlodipine CPRose EchevarriaNo ratings yet
- CKD NCPDocument4 pagesCKD NCPArlene Macatangay100% (1)
- Nursing Care Plan TB MeningitisDocument2 pagesNursing Care Plan TB Meningitisderic74% (19)
- Anxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationDocument2 pagesAnxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationmonaNo ratings yet
- NCP HemoDocument2 pagesNCP HemoJigs HechNo ratings yet
- Nursing Care Plan Renal FailureDocument2 pagesNursing Care Plan Renal FailureMark Jason Rabadan100% (1)
- NCPDocument4 pagesNCPEsther RefuncionNo ratings yet
- NCP - Risk For Infection - DMDocument3 pagesNCP - Risk For Infection - DMcessi18100% (1)
- Chronic Renal Failure Nursing Care PlanDocument6 pagesChronic Renal Failure Nursing Care PlanRuva Oscass JimmyNo ratings yet
- NCP - Activity IntoleranceDocument4 pagesNCP - Activity IntoleranceRoyce Vincent TizonNo ratings yet
- Nursing Care Plan - CancerDocument3 pagesNursing Care Plan - CancerChristineAla0% (1)
- NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyDocument3 pagesNCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyAngie MandeoyaNo ratings yet
- Nursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPDocument2 pagesNursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPLP Benoza100% (2)
- Final NCPDocument13 pagesFinal NCPBAGUIO CATSNo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationElla EvangelistaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationYzel Vasquez AdavanNo ratings yet
- Impaired Gas Exchange PneumoniaDocument2 pagesImpaired Gas Exchange PneumoniaShanice BedecirNo ratings yet
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 pagesAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresNo ratings yet
- NCPDocument7 pagesNCPRuth MontebonNo ratings yet
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- CopdDocument6 pagesCopdapi-3717941100% (2)
- Cu 4Document3 pagesCu 4Paul SahagunNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationTrisha SuazoNo ratings yet
- Nursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationDocument10 pagesNursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationGuile RilleraNo ratings yet
- Critical Incident TechniqueDocument15 pagesCritical Incident TechniqueSapna thakurNo ratings yet
- Role-Play: Administering HPV Vaccine Safely and CorrectlyDocument4 pagesRole-Play: Administering HPV Vaccine Safely and CorrectlySapna thakurNo ratings yet
- Peritoneal Dialysis Procedure: Amy Neufeldt, RN, BSCN, William J. Lawton, Md. July 2015 Mbingo Baptist HospitalDocument5 pagesPeritoneal Dialysis Procedure: Amy Neufeldt, RN, BSCN, William J. Lawton, Md. July 2015 Mbingo Baptist HospitalSapna thakurNo ratings yet
- 07.03.53 Mechanical VentilationDocument3 pages07.03.53 Mechanical VentilationSapna thakurNo ratings yet
- Sapan ThakurDocument1 pageSapan ThakurSapna thakurNo ratings yet
- Shimla Nursing College AnnadaleDocument9 pagesShimla Nursing College AnnadaleSapna thakurNo ratings yet
- Lumbar PunctureDocument1 pageLumbar PunctureSapna thakurNo ratings yet
- M.SC - Nursing 1st Year PDFDocument5 pagesM.SC - Nursing 1st Year PDFSapna thakur100% (2)
- Sub: Request To Postpone My Advanced Nursing Practice ExamDocument1 pageSub: Request To Postpone My Advanced Nursing Practice ExamSapna thakurNo ratings yet
- Play Therapy and Children With Intellectual Disability: D.Rathnakumar Open AccessDocument8 pagesPlay Therapy and Children With Intellectual Disability: D.Rathnakumar Open AccessSapna thakurNo ratings yet
- KalaivanicDocument117 pagesKalaivanicSapna thakurNo ratings yet
- 1986 7992 1 PBDocument8 pages1986 7992 1 PBSapna thakurNo ratings yet
- Central Reserve Police Force: 1 Paste Latest Passport Size Colour Photograph 2Document13 pagesCentral Reserve Police Force: 1 Paste Latest Passport Size Colour Photograph 2Sapna thakurNo ratings yet
- KMC For Premature Babies: Esearch RticleDocument6 pagesKMC For Premature Babies: Esearch RticleSapna thakurNo ratings yet
- Psychiatry: Section ofDocument12 pagesPsychiatry: Section ofSapna thakurNo ratings yet
- Video Game Violence and The Effects On Children - A Review of The PDFDocument24 pagesVideo Game Violence and The Effects On Children - A Review of The PDFSapna thakurNo ratings yet
- Hiv Aids QuizDocument1 pageHiv Aids QuizSapna thakurNo ratings yet
- Role of Pediatric NurseDocument11 pagesRole of Pediatric NurseSapna thakur100% (5)
- Assessment and Management of High Risk NeonateDocument14 pagesAssessment and Management of High Risk NeonateSapna thakur50% (2)
- Assessment and Management of High Risk NeonateDocument14 pagesAssessment and Management of High Risk NeonateSapna thakur50% (2)
- WHO International Bibliography of KMC PDFDocument84 pagesWHO International Bibliography of KMC PDFSapna thakurNo ratings yet
- Anemia Management in CKDDocument50 pagesAnemia Management in CKDAnonymous eYNrPrlNo ratings yet
- Quality of Life in HemodialysisDocument176 pagesQuality of Life in HemodialysisSebastian Amadeuz Esipindow SipayungNo ratings yet
- 10 Myths About FrusemideDocument4 pages10 Myths About FrusemideABARCA RENTERIA MARIANANo ratings yet
- Renal Failure - The FactsDocument282 pagesRenal Failure - The FactsJosé RamírezNo ratings yet
- IHFG Part B Renal Dialysis UnitDocument18 pagesIHFG Part B Renal Dialysis Unitmorton1472No ratings yet
- Stroke PDFDocument67 pagesStroke PDFBadrul MunirNo ratings yet
- Recent Advances in HypertensionDocument6 pagesRecent Advances in Hypertensionrudi saputraNo ratings yet
- Nej MC 2201160Document3 pagesNej MC 2201160Πάνος ΣταγήςNo ratings yet
- Gordon Feldman at 01 - 14 - 2023 09 - 19 PMDocument5 pagesGordon Feldman at 01 - 14 - 2023 09 - 19 PMschoolgirl7796No ratings yet
- Acute Cardiorenal Syndrome An UpdateDocument10 pagesAcute Cardiorenal Syndrome An UpdateErika Jiménez De LaraNo ratings yet
- Case Presentation - Acute Kidney InjuryDocument5 pagesCase Presentation - Acute Kidney InjuryC KandasamyNo ratings yet
- Adrian Covic, Mehmet Kanbay, Edgar V. Lerma (Eds.) - Dyslipidemias in Kidney Disease (2014, Springer-Verlag New York) PDFDocument325 pagesAdrian Covic, Mehmet Kanbay, Edgar V. Lerma (Eds.) - Dyslipidemias in Kidney Disease (2014, Springer-Verlag New York) PDFAndrada BararNo ratings yet
- Small Animal Clinical NutritionDocument8 pagesSmall Animal Clinical NutritionJairo PereiraNo ratings yet
- 8.3 Acute Kidney Injury - March 16 - Dr. Austria.Document6 pages8.3 Acute Kidney Injury - March 16 - Dr. Austria.Jess PeltraNo ratings yet
- (MED 2) S04 T02 Acute Kidney InjuryDocument16 pages(MED 2) S04 T02 Acute Kidney InjurySheila Lyn LacsonNo ratings yet
- Foods and Diet For Chronic Kidney DiseaseDocument10 pagesFoods and Diet For Chronic Kidney DiseaseChella Taz BoneetaNo ratings yet
- Medical-Surgical Nursing Exam 31 NLE Pre-Board (100 Items)Document16 pagesMedical-Surgical Nursing Exam 31 NLE Pre-Board (100 Items)Mimi Vee100% (2)
- ESRDDocument10 pagesESRDKayle Irah CaburnayNo ratings yet
- FNP 799 - DNP Project Manuscript - Morgan AtchisonDocument52 pagesFNP 799 - DNP Project Manuscript - Morgan Atchisonapi-577207555No ratings yet
- Iron SucroseDocument14 pagesIron SucroseTejaswi J DamerlaNo ratings yet
- LinksDocument24 pagesLinksTrisNo ratings yet
- Hypertension GuidelinesDocument33 pagesHypertension GuidelinesTika wahyuNo ratings yet
- Chronic Kidney Disease (CKD) : Diabetes High Blood Pressure Responsible For Up To Two-Thirds GlomerulonephritisDocument6 pagesChronic Kidney Disease (CKD) : Diabetes High Blood Pressure Responsible For Up To Two-Thirds GlomerulonephritisKyle Ü D. CunanersNo ratings yet
- 2014 JNC 8 HypertensionDocument2 pages2014 JNC 8 Hypertensionaudreynabilaf100% (1)
- Rounding NegashDocument4 pagesRounding NegashkaldamtewNo ratings yet
- Email Id For Mailing The AnswersheetDocument7 pagesEmail Id For Mailing The AnswersheetSankalp PariharNo ratings yet
- Immune Dysfunction and Risk of Infection in CKD - 2019Document8 pagesImmune Dysfunction and Risk of Infection in CKD - 2019Lú VillalobosNo ratings yet
- Akizawa 2009Document9 pagesAkizawa 2009PROF. ERWIN M. GLOBIO, MSITNo ratings yet
- Case Report - CC - Uraemic EncephalopathyDocument11 pagesCase Report - CC - Uraemic EncephalopathyM CubedNo ratings yet
- 1.1 AkiDocument89 pages1.1 Akilibentadesse57No ratings yet
NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy
NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy
Uploaded by
Sapna thakurOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy
NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy
Uploaded by
Sapna thakurCopyright:
Available Formats
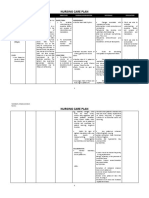
Patient’s Diagnosis: CHRONIC KIDNEY DISEASE probably secondary to DM Nephropathy
Short Background: Chronic kidney disease (CKD) occurs when one suffers from gradual and usually permanent loss of kidney function over time. With loss of kidney function, there is an
accumulation of water; waste; and toxic substances, in the body, that are normally excreted by the kidney. Glomerular Filtration Rate (GFR), the measure of the kidney's function,
determines the severity or stage of the disease (whereas Stage 5 CKD is considered Renal Failure due to gradual loss of GFR, GFR < 15: needs dialysis). CKD often develops from 1Diabetes
(stenosis/ischemic), 2Hypertension (microvascular damage), 3Glomerulonephritis (post-infection), or 4Nephrotoxicity (medications).
Assessment Nursing Scientific Explanation of Planning Interventions Rationale Evaluation
Diagnosis the Problem
Subjective: Ineffective Impaired GFR results into Goal: Collaborative:
Breathing Pattern fluid overload. With fluid Establish Spontaneous, non- 1. Administer humid Oxygen 1. To help patient get
Patient is not r/t impending volume excess, venous Labored Breathing (8-10Lpm) as ordered. adequate oxygen despite
able to verbalize. pulmonary pressure is more likely to of DOB.
congestion d/t cause both circulatory and Short Term: 2. Assist in Manual 2. To assist patient on
impaired GFR and pulmonary congestion. The After 4 hours of nursing Ventilation via ET Tube. respiration and to ensure
fluid retention or patient may possibly interventions, patient will be adequate tidal volume.
respiratory manifests fatigue, able to reduce labored and
Objective:
muscle weakness dyspnea, tachypnea, difficult breathing and
> Deep, fast, noisy
breathing d/t physical stress. muscle weakness establish a respiratory rate
(including diaphragm), or of less than 30cpm.
> RR 33cpm sputum production that
Independent:
are related to pulmonary Long Term: 1. To check and reassess
> Crackles heard 1. Monitor and record vital
congestion. Physical stress After 5 days of nursing vital function changes
on inspiration signs.
also impacts pulmonary interventions, patient will be (Respiration).
functioning. able to demonstrate non-
> SaO2 99%
labored and spontaneous 2. Assess for lung sounds. 2. To identify extent of
> BP Diabetic, there is a breathing. fluid accumulation in the
140/100mmhg possibility that sugar respiratory system.
crystallization has occurred
> PR 80bpm and leads to renal artery 3. To facilitate
3. Position on moderate high
stenosis or a microvascular gravitational expansion of
> T 37.0 C complication due to back rest.
the lungs to decrease
viscosity. inspiratory effort.
> Diaphoretic, cold
clammy skin
4. Maintain calm and non- 4. To avoid stressors and
> Unresponsive; stimulating environment. let patient regain strength
may be due to by manipulation of
fatigue/weakness. environment.
> Increased
respiratory 5. Suction secretions PRN. 5. To facilitate airway
secretions. clearance and reduce
effort from DOB.
CELESTINO, JOHN CHRISTOPHER S.
WUP SN’13 senior block 04
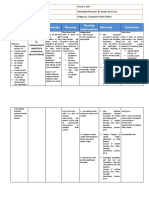
Patient’s Diagnosis: CHRONIC KIDNEY DISEASE probably secondary to DM Nephropathy
Priority Problem: (Priority 1) Ineffective Breathing Pattern
Assessment Nursing Scientific Explanation of Planning Interventions Rationale Evaluation
Diagnosis the Problem
Subjective: Fluid Volume Renal disorder impairs Goal: Collaborative: Collaborative:
Excess R/T glomerular filtration that Reduce Fluid Volume 1. Administer loop diuretics 1. Diuretics reduce fluid
Patient is not decrease resulted to fluid overload. Excess, output more (Furosemide/Lasix) as ordered. volume by helping kidney
able to verbalize. Glomerular With fluid volume excess, than input. excrete urine and sodium.
filtration Rate and hydrostatic pressure is 2. Assist in specimen extraction for 2. To prepare patient for
sodium retention. higher than the usual serum analysis (Serum Electrolytes/ possible lab orders..
Short Term:
pushing excess fluids into RBS or FBS) and urine analysis
After 4 hours of
the interstitial spaces, (BUN/Crea).
Objective: nursing interventions,
causes venous return, 3. CBG Test as ordered. 3. To determine the
> Anuria patient will be able to
leading the patient to have efficacy of DM regimen.
avoid recurrence of
> BP 140/100mahg edema, weight gain,
fluid excess Independent: Independent:
pulmonary congestion and
1. Monitor and record vital signs 1. To check and reassess
> RR 27cpm HPN at the same time due
vital function changes
to decrease GFR, nephron
> PR 80bpm Long Term: (Circulation).
hypertrophied leading to
After 5 days of 2. Auscultate breath sounds 2. To determine extent of
decrease ability of the
> T 37.0 C nursing intervention fluid excess.
kidney to concentrate
the patient will 3. Record occurrence of dyspnea 3. To check possible
> Peripheral Edema urine and impaired
manifest stabilize fluid respiratory complications
excretion of fluid thus
volume, I & O, normal (pulmonary congestion).
> Diaphoretic, cold leading to oliguria/anuria.
VS, stable weight,
clammy skin
and free from signs of 4. Review lab data like BUN, 4. To monitor kidney
With associated DM, there
> Unresponsive; edema. Creatinine, Serum electrolyte. function and fluid
is a possibility that sugar
may be due to crystallization has occurred
fatigue/weakness.
retention (electrolyte
and leads to renal artery compensation).
> Increased stenosis or a microvascular
respiratory complication due to
5. Record I&O accurately and 5. To determine fluid
secretions. viscosity of blood.
calculate fluid volume balance retention and kidney
> CBG 126mg/dL function (GFR).
6. Weigh client 6. Increasing weight may
indicate fluid retention.
7. Encourage quiet, restful 7. To allow patient cope
atmosphere. with stressors naturally.
Main Problem: (Priority 2) Fluid Volume Excess
CELESTINO, JOHN CHRISTOPHER S.
WUP SN’13 senior block 04
Patient’s Diagnosis: CHRONIC KIDNEY DISEASE probably secondary to DM Nephropathy
Manifestation Problem: (Priority 3) Risk for Impaired Skin Integrity
CELESTINO, JOHN CHRISTOPHER S.
WUP SN’13 senior block 04
Patient’s Diagnosis: CHRONIC KIDNEY DISEASE probably secondary to DM Nephropathy
Assessment Nursing Scientific Explanation of Planning Interventions Rationale Evaluation
Diagnosis the Problem
Subjective: Risk for Impaired Due to fluid retention, fluid Goal: Collaborative:
Skin Integrity r/t accumulates and fluid Prevent Risks on Developing 1. Ferrous Sulfate (Iron 1. To help body regulate
Patient is not edema and shifts from intracellular Skin Breakdown. supplement) as ordered. RBC in the
able to verbalize. prolonged bed rest compartment to absence/lacking of
d/t extracellular compartment Short Term: hormone erythropoietin.
causing escape of fluid to After 4 hours of nursing 2. Update Lab Findings for 2. To evaluate efficacy of
the tissues (edema). With interventions, patient will be CBC (RBC, Hgb, Hct). treatment/prophylaxis for
associated complications of able to remove potential anemia regimen.
Objective:
anemia, skin nutrition threats that may lead to
> Peripheral Edema
would be crucial and may poor skin integrity. 3. CBG T.I.D. as ordered. 3. To determine
> Prolonged bed have easily broken off. hyperglycemia that
rest Long Term: makes blood viscous and
DM could cause high blood After 5 days of nursing induces the risk for
> Pallor sugar levels and leads to interventions, patient will be infection.
viscosity of blood that also able to identify and avoid
> Hgb impairs nutrition of skin or factors that lead to skin Independent:
reduction of blood cells to breakdown.
> Diaphoretic, cold 1. Assess skin appearance 1. To determine edema or
clammy skin capillaries.
(color, texture, erythema that indicates
temperature). possible bed sore.
> Unresponsive;
may be due to
fatigue/weakness. 2. Turn patient side to side 2. To make pressure
every 2 hours if possible. equal when lying to avoid
> CBG 126mg/dL unilateral skin tissue
blood insufficiency.
3. Maintain crease-free bed 3. To avoid skin irritation
linen. from crease.
4. Maintain a clean, 4. To avoid risk for skin
therapeutic environment. injury and infection.
CELESTINO, JOHN CHRISTOPHER S.
WUP SN’13 senior block 04
You might also like
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNo ratings yet
- Risk For Acute ConfusionDocument2 pagesRisk For Acute ConfusionChar PereaNo ratings yet
- Impaired Liver FunctionDocument1 pageImpaired Liver FunctionShop Dzubiri Here75% (4)
- NCPDocument1 pageNCPhaniehaehae100% (1)
- NCP - Fluid RetentionDocument3 pagesNCP - Fluid RetentionMichelle Teodoro100% (1)
- Nursing Care Plan2 CVADocument4 pagesNursing Care Plan2 CVAhermesdave1No ratings yet
- BPH NCPDocument1 pageBPH NCPJayson BenitezNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- NCP: Acute GastroenteritisDocument3 pagesNCP: Acute GastroenteritishauteanicoleNo ratings yet
- NCP DobDocument1 pageNCP DobsarahAcristobalNo ratings yet
- NCP For RS-HF (Cor PulmonaleDocument5 pagesNCP For RS-HF (Cor PulmonaleMika Saldaña100% (1)
- EdemaDocument2 pagesEdemaVirus50% (2)
- NCPDocument2 pagesNCPDidith AbanNo ratings yet
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionMitsika AnadiaNo ratings yet
- Acute Pain OsteosarcomaDocument8 pagesAcute Pain OsteosarcomaMaryjoy Gabriellee De La Cruz100% (1)
- NCP Liver CirrosisDocument2 pagesNCP Liver CirrosisRosebud RoseNo ratings yet
- Cues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale EvaluationDocument4 pagesCues/Data Nursing Diagnosis Scientific Basis Goals of Care Nursing Interventions Rationale EvaluationEjie Boy Isaga100% (1)
- Impaired Urinary EliminationDocument3 pagesImpaired Urinary EliminationAgcopra MtchNo ratings yet
- Nursing Care Plan Student Nurse: Diestro, Angela Mae BSN 2BDocument3 pagesNursing Care Plan Student Nurse: Diestro, Angela Mae BSN 2BAngela Mae DiestroNo ratings yet
- Risk For Ineffective Airway Clearance 1Document8 pagesRisk For Ineffective Airway Clearance 1kint manlangitNo ratings yet
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonNo ratings yet
- Nursing Care Plan: Cues/Clues Nursing Diagnosis Rationale Objectives Nursing Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Cues/Clues Nursing Diagnosis Rationale Objectives Nursing Intervention Rationale EvaluationJennirose JingNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDocument1 pageNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationJhevilin RM100% (1)
- Patty NCP HyperthermiaDocument4 pagesPatty NCP HyperthermiaPatricia Jean FaeldoneaNo ratings yet
- Nursing Care Plan: Subjective Data " GoalDocument2 pagesNursing Care Plan: Subjective Data " GoalJay VillasotoNo ratings yet
- 2 Acute Pain Chronic Renal Failure Nursing Care PlansDocument5 pages2 Acute Pain Chronic Renal Failure Nursing Care Plansjustin_saneNo ratings yet
- NCP - Patient With Endotracheal TubeDocument1 pageNCP - Patient With Endotracheal TubeSelwynVillamorPatenteNo ratings yet
- NCP 1Document5 pagesNCP 1Denisse Shazz Mae MaretNo ratings yet
- NCP RiskDocument3 pagesNCP RiskMaricar Azolae MascualNo ratings yet
- Pleural EffusionDocument5 pagesPleural EffusionTerizla MobileNo ratings yet
- NCP LocDocument2 pagesNCP LocMel RodolfoNo ratings yet
- Nursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale EvaluationDocument1 pageNursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale Evaluationeihjay-bravo-8041No ratings yet
- NCP - Altered Tissue PerfusionDocument2 pagesNCP - Altered Tissue PerfusionLeigh Kristel Andrion0% (1)
- "Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientDocument2 pages"Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientMussaib Mushtaq100% (1)
- Word Ncp.......... TetanusDocument3 pagesWord Ncp.......... TetanusYvounne Ananias Bautista RNNo ratings yet
- Amlodipine CPDocument2 pagesAmlodipine CPRose EchevarriaNo ratings yet
- CKD NCPDocument4 pagesCKD NCPArlene Macatangay100% (1)
- Nursing Care Plan TB MeningitisDocument2 pagesNursing Care Plan TB Meningitisderic74% (19)
- Anxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationDocument2 pagesAnxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationmonaNo ratings yet
- NCP HemoDocument2 pagesNCP HemoJigs HechNo ratings yet
- Nursing Care Plan Renal FailureDocument2 pagesNursing Care Plan Renal FailureMark Jason Rabadan100% (1)
- NCPDocument4 pagesNCPEsther RefuncionNo ratings yet
- NCP - Risk For Infection - DMDocument3 pagesNCP - Risk For Infection - DMcessi18100% (1)
- Chronic Renal Failure Nursing Care PlanDocument6 pagesChronic Renal Failure Nursing Care PlanRuva Oscass JimmyNo ratings yet
- NCP - Activity IntoleranceDocument4 pagesNCP - Activity IntoleranceRoyce Vincent TizonNo ratings yet
- Nursing Care Plan - CancerDocument3 pagesNursing Care Plan - CancerChristineAla0% (1)
- NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyDocument3 pagesNCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyAngie MandeoyaNo ratings yet
- Nursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPDocument2 pagesNursing Care Plan Ineffective Airway Clearance Related To Tracheobronchial Secretions CAPLP Benoza100% (2)
- Final NCPDocument13 pagesFinal NCPBAGUIO CATSNo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationElla EvangelistaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationYzel Vasquez AdavanNo ratings yet
- Impaired Gas Exchange PneumoniaDocument2 pagesImpaired Gas Exchange PneumoniaShanice BedecirNo ratings yet
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 pagesAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresNo ratings yet
- NCPDocument7 pagesNCPRuth MontebonNo ratings yet
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- CopdDocument6 pagesCopdapi-3717941100% (2)
- Cu 4Document3 pagesCu 4Paul SahagunNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationTrisha SuazoNo ratings yet
- Nursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationDocument10 pagesNursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationGuile RilleraNo ratings yet
- Critical Incident TechniqueDocument15 pagesCritical Incident TechniqueSapna thakurNo ratings yet
- Role-Play: Administering HPV Vaccine Safely and CorrectlyDocument4 pagesRole-Play: Administering HPV Vaccine Safely and CorrectlySapna thakurNo ratings yet
- Peritoneal Dialysis Procedure: Amy Neufeldt, RN, BSCN, William J. Lawton, Md. July 2015 Mbingo Baptist HospitalDocument5 pagesPeritoneal Dialysis Procedure: Amy Neufeldt, RN, BSCN, William J. Lawton, Md. July 2015 Mbingo Baptist HospitalSapna thakurNo ratings yet
- 07.03.53 Mechanical VentilationDocument3 pages07.03.53 Mechanical VentilationSapna thakurNo ratings yet
- Sapan ThakurDocument1 pageSapan ThakurSapna thakurNo ratings yet
- Shimla Nursing College AnnadaleDocument9 pagesShimla Nursing College AnnadaleSapna thakurNo ratings yet
- Lumbar PunctureDocument1 pageLumbar PunctureSapna thakurNo ratings yet
- M.SC - Nursing 1st Year PDFDocument5 pagesM.SC - Nursing 1st Year PDFSapna thakur100% (2)
- Sub: Request To Postpone My Advanced Nursing Practice ExamDocument1 pageSub: Request To Postpone My Advanced Nursing Practice ExamSapna thakurNo ratings yet
- Play Therapy and Children With Intellectual Disability: D.Rathnakumar Open AccessDocument8 pagesPlay Therapy and Children With Intellectual Disability: D.Rathnakumar Open AccessSapna thakurNo ratings yet
- KalaivanicDocument117 pagesKalaivanicSapna thakurNo ratings yet
- 1986 7992 1 PBDocument8 pages1986 7992 1 PBSapna thakurNo ratings yet
- Central Reserve Police Force: 1 Paste Latest Passport Size Colour Photograph 2Document13 pagesCentral Reserve Police Force: 1 Paste Latest Passport Size Colour Photograph 2Sapna thakurNo ratings yet
- KMC For Premature Babies: Esearch RticleDocument6 pagesKMC For Premature Babies: Esearch RticleSapna thakurNo ratings yet
- Psychiatry: Section ofDocument12 pagesPsychiatry: Section ofSapna thakurNo ratings yet
- Video Game Violence and The Effects On Children - A Review of The PDFDocument24 pagesVideo Game Violence and The Effects On Children - A Review of The PDFSapna thakurNo ratings yet
- Hiv Aids QuizDocument1 pageHiv Aids QuizSapna thakurNo ratings yet
- Role of Pediatric NurseDocument11 pagesRole of Pediatric NurseSapna thakur100% (5)
- Assessment and Management of High Risk NeonateDocument14 pagesAssessment and Management of High Risk NeonateSapna thakur50% (2)
- Assessment and Management of High Risk NeonateDocument14 pagesAssessment and Management of High Risk NeonateSapna thakur50% (2)
- WHO International Bibliography of KMC PDFDocument84 pagesWHO International Bibliography of KMC PDFSapna thakurNo ratings yet
- Anemia Management in CKDDocument50 pagesAnemia Management in CKDAnonymous eYNrPrlNo ratings yet
- Quality of Life in HemodialysisDocument176 pagesQuality of Life in HemodialysisSebastian Amadeuz Esipindow SipayungNo ratings yet
- 10 Myths About FrusemideDocument4 pages10 Myths About FrusemideABARCA RENTERIA MARIANANo ratings yet
- Renal Failure - The FactsDocument282 pagesRenal Failure - The FactsJosé RamírezNo ratings yet
- IHFG Part B Renal Dialysis UnitDocument18 pagesIHFG Part B Renal Dialysis Unitmorton1472No ratings yet
- Stroke PDFDocument67 pagesStroke PDFBadrul MunirNo ratings yet
- Recent Advances in HypertensionDocument6 pagesRecent Advances in Hypertensionrudi saputraNo ratings yet
- Nej MC 2201160Document3 pagesNej MC 2201160Πάνος ΣταγήςNo ratings yet
- Gordon Feldman at 01 - 14 - 2023 09 - 19 PMDocument5 pagesGordon Feldman at 01 - 14 - 2023 09 - 19 PMschoolgirl7796No ratings yet
- Acute Cardiorenal Syndrome An UpdateDocument10 pagesAcute Cardiorenal Syndrome An UpdateErika Jiménez De LaraNo ratings yet
- Case Presentation - Acute Kidney InjuryDocument5 pagesCase Presentation - Acute Kidney InjuryC KandasamyNo ratings yet
- Adrian Covic, Mehmet Kanbay, Edgar V. Lerma (Eds.) - Dyslipidemias in Kidney Disease (2014, Springer-Verlag New York) PDFDocument325 pagesAdrian Covic, Mehmet Kanbay, Edgar V. Lerma (Eds.) - Dyslipidemias in Kidney Disease (2014, Springer-Verlag New York) PDFAndrada BararNo ratings yet
- Small Animal Clinical NutritionDocument8 pagesSmall Animal Clinical NutritionJairo PereiraNo ratings yet
- 8.3 Acute Kidney Injury - March 16 - Dr. Austria.Document6 pages8.3 Acute Kidney Injury - March 16 - Dr. Austria.Jess PeltraNo ratings yet
- (MED 2) S04 T02 Acute Kidney InjuryDocument16 pages(MED 2) S04 T02 Acute Kidney InjurySheila Lyn LacsonNo ratings yet
- Foods and Diet For Chronic Kidney DiseaseDocument10 pagesFoods and Diet For Chronic Kidney DiseaseChella Taz BoneetaNo ratings yet
- Medical-Surgical Nursing Exam 31 NLE Pre-Board (100 Items)Document16 pagesMedical-Surgical Nursing Exam 31 NLE Pre-Board (100 Items)Mimi Vee100% (2)
- ESRDDocument10 pagesESRDKayle Irah CaburnayNo ratings yet
- FNP 799 - DNP Project Manuscript - Morgan AtchisonDocument52 pagesFNP 799 - DNP Project Manuscript - Morgan Atchisonapi-577207555No ratings yet
- Iron SucroseDocument14 pagesIron SucroseTejaswi J DamerlaNo ratings yet
- LinksDocument24 pagesLinksTrisNo ratings yet
- Hypertension GuidelinesDocument33 pagesHypertension GuidelinesTika wahyuNo ratings yet
- Chronic Kidney Disease (CKD) : Diabetes High Blood Pressure Responsible For Up To Two-Thirds GlomerulonephritisDocument6 pagesChronic Kidney Disease (CKD) : Diabetes High Blood Pressure Responsible For Up To Two-Thirds GlomerulonephritisKyle Ü D. CunanersNo ratings yet
- 2014 JNC 8 HypertensionDocument2 pages2014 JNC 8 Hypertensionaudreynabilaf100% (1)
- Rounding NegashDocument4 pagesRounding NegashkaldamtewNo ratings yet
- Email Id For Mailing The AnswersheetDocument7 pagesEmail Id For Mailing The AnswersheetSankalp PariharNo ratings yet
- Immune Dysfunction and Risk of Infection in CKD - 2019Document8 pagesImmune Dysfunction and Risk of Infection in CKD - 2019Lú VillalobosNo ratings yet
- Akizawa 2009Document9 pagesAkizawa 2009PROF. ERWIN M. GLOBIO, MSITNo ratings yet
- Case Report - CC - Uraemic EncephalopathyDocument11 pagesCase Report - CC - Uraemic EncephalopathyM CubedNo ratings yet
- 1.1 AkiDocument89 pages1.1 Akilibentadesse57No ratings yet