Professional Documents
Culture Documents
Appi Ajp 2013 13010058 PDF
Appi Ajp 2013 13010058 PDF
Uploaded by
Rania EOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Appi Ajp 2013 13010058 PDF
Appi Ajp 2013 13010058 PDF
Uploaded by
Rania ECopyright:
Available Formats
Commentary
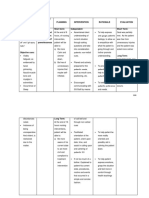
DSM-5 Sleep-Wake Disorders Classification:
Overview for Use in Clinical Practice
T he goal of the DSM-5 sleep-wake disorders classification was, from the outset,
to facilitate the differential diagnosis of sleep-wake complaints, given their ubiquity
in psychiatric practice, and to clarify when referral to a sleep disorders specialist is
appropriate.
The classification encompasses 10 disorders or disorder groups: insomnia dis-
order, hypersomnolence disorder, narcolepsy, breathing-related sleep disorders,
circadian rhythm sleep disorders, non-REM (NREM) sleep arousal disorders, night-
mare disorder, REM sleep behavior disorder, restless legs syndrome, and substance-
or medication-induced sleep disorder.
The core features of each disorder relate to the patient’s dissatisfaction regard-
ing the quality, timing, and amount of sleep with resulting daytime distress and
impairment.
In some disorders (e.g., insomnia disorder), the DSM-5 Sleep-Wake Disorders Work
Group took a lumping approach, while in others (e.g., narcolepsy/hypocretin de-
ficiency) we used a splitting approach,
reflecting the availability of validators
derived from epidemiological, neuro-
Sleep is by the brain, of the brain,
biological, and intervention research. and for the brain.
In all cases, however, the DSM-5 sleep-
wake chapter provides both categorical and dimensional approaches to diagnosis
and severity in order to facilitate measurement-based care in general mental health
and medical or pediatric settings. The focus on measurement-based care is fun-
damental to the goals of the sleep-wake disorders classification.
Clinical Relevance
Sleep disorders are often accompanied by depression, anxiety, and cognitive
changes that must be addressed in treatment planning and management. Sleep
disorders are also established risk factors for the subsequent development of com-
mon mental illnesses and may represent the prodromal expression of an episode of
mental illness, allowing the possibility of early intervention to preempt or attenuate
a full-blown episode.
In addition, sleep disturbances furnish a clinically useful indicator of medical
and neurological disorders that often coexist with depression and other common
mental disorders. Sleep-wake complaints can provide clinically actionable clues
in breathing-related sleep disorders, disorders of the heart and lungs (e.g., con-
gestive heart failure and chronic obstructive pulmonary disease), neurodegen-
erative disorders (Alzheimer’s disease or Parkinson’s disease), and disorders of
the musculoskeletal system. Each of these is characterized by prominent sleep-
wake complaints and each is frequently accompanied by depression and anxiety
disorders.
This article is featured in this month’s AJP Audio
Am J Psychiatry 170:10, October 2013 ajp.psychiatryonline.org 1099
COMMENTARY
Conversely, mental health clinicians should also understand that some medical
disorders may not only disturb sleep (as in the examples above) but may themselves
be worsened during sleep. Thus, some patients may experience apneas or ECG ar-
rhythmias during REM sleep, confusional arousals with dementing illness, or REM
sleep behavior disorder in alpha synucleinopathies such as Parkinson’s disease.
Clinical Utility of Dimensional Assessment
In addition to diagnostic criteria for categorical assessment, the DSM-5 sleep
classification also supports dimensional assessment for several reasons, primarily
to capture severity and to facilitate measurement-based clinical care in the ser-
vice of personalized medicine. Dimensional assessments are also useful for cap-
turing behaviors that may contribute to the pathogenesis and persistence of sleep
disorders, including poor sleep-wake hygiene practices. Finally, dimensional
assessments of severity allow correlation with, and exploration of, underlying
neurobiological issues such as genetic liability, hyperarousal, and circadian dys-
rhythmias. Particularly useful examples of dimensional measures amenable to
office-based practice and bedside care include the NIH Patient Reported Outcomes
Measurement Information System (http://www.nihpromis.org) and self-report in-
ventories of sleep quality (e.g., the Pittsburgh Sleep Quality Index and the Insomnia
Severity Scale).
Biological Validators of Diagnosis
The use of biological validators is now embedded in the DSM-5 classification of
sleep-wake disorders, and this represents a major change from DSM-IV. Examples
with particular relevance to clinical psychiatric practice, where the existence of
laboratory measures is essential to diagnostic confirmation, include disorders of
excessive sleepiness (e.g., narcolepsy/hypocretin deficiency), breathing-related
sleep disorders, REM sleep behavior disorder, and some NREM parasomnia dis-
orders of arousals.
A Practical Approach for Dealing With Comorbidity
The DSM-5 sleep-wake disorders classification has moved away from the caus-
al attributions that were inherent in the logic of DSM-IV. In order to underscore
the reality that patients in psychiatric and general medical practice frequently
have sleep disorders that warrant an independent clinical condition, DSM-5 calls
for clinicians to specify comorbid conditions, medical and psychiatric, that are
present. The aim is simply to acknowledge the bidirectional and interactive effects
between sleep disorders and coexisting medical and psychiatric illnesses.
An example from clinical practice will serve to illustrate this point. A psychiatrist
may be treating a patient with major depression and prominent insomnia com-
plaints. The DSM-IV classification would have specified “sleep disorder related to
another mental disorder.” In DSM-5, however, the clinician is asked to consider
whether the patient has an insomnia disorder (or a disorder of hypersomnolence)
in addition to a mood disorder. This question frequently arises in cases where
treatment of the mental disorder has led to improvement, but sleep-wake dis-
turbance persists. By diagnosing both major depressive disorder and, when ap-
propriate, insomnia disorder or hypersomnolence disorder (i.e., concurrently
specifying the two coexisting conditions), the management and treatment plan can
address both issues. Unless the sleep complaint is also addressed, the patient will
be at higher risk for failure to achieve remission and to suffer a relapsing, recurrent
course of depression.
1100 ajp.psychiatryonline.org Am J Psychiatry 170:10, October 2013
COMMENTARY
This conceptualization reflects a paradigm change that is now widely accepted
in the field of sleep medicine and that holds great relevance for psychiatric practice.
It moves away from the need to make causal attributions between coexisting dis-
orders and only requires specifying clinical comorbidities that may have relevance
to comprehensive treatment planning (1, 2).
Referral to Sleep Medicine Specialists
DSM-5 also provides guidance, in the text accompanying the diagnostic criteria,
as to when referral to a sleep medicine specialist is appropriate. Such referral is
indicated for severe daytime sleepiness, when patients may be placed in harm’s
way; if the patient has risk factors for sleep apnea (e.g., sleepiness during the day,
snoring, and obesity); for unusual or dangerous behaviors during sleep (e.g., REM
sleep behavior disorder); in cases of insomnia that do not respond to usual be-
havioral or pharmacological approaches; and finally, for atypical symptoms or
treatment refractoriness.
Summary
Mental health clinicians should appreciate that sleep is a fundamental hu-
man behavior and that inadequate sleep has adverse medical, psychiatric, and
psychosocial consequences. Sleep disturbances interact with common mental
disorders; the two are mutually exacerbating, and both must be appropriately ad-
dressed to ensure optimal outcomes for our patients. Sleep is by the brain, of the
brain, and for the brain.
References
1. National Institutes of Health: National Institutes of Health state of the science conference statement on
manifestations and management of chronic insomnia in adults, June 13–15, 2005. Sleep 2005; 28:1049–1057
2. Ohayon MM, Dauvilliers Y, Reynolds CF III: Operational definitions and algorithms for excessive sleepiness in
the general population: implications for the DSM-5 nosology. Arch Gen Psychiatry 2012; 69:71–79
CHARLES F. REYNOLDS III, M.D.
RUTH O’HARA, PH.D.
From the Department of Psychiatry and Behavioral Science, Sierra-Pacific Mental Illness Education and
Clinical Center, Stanford University School of Medicine, Calif. Dr. Reynolds is Chair of and Dr. O’Hara is a
member of the DSM-5 Sleep-Wake Disorders Work Group. Address correspondence to Dr. Reynolds
(ReynoldsCF@upmc.edu). Commentary accepted for publication March 2013 (doi: 10.1176/appi.ajp.2013.
13010058).
Dr. Reynolds has received board member fees from the American Association of Geriatric Psychiatry Editorial
Review Board; support from the American Association for Geriatric Psychiatry, the American Foundation for
Suicide Prevention, the Center for Medicare and Medicaid Services, the Commonwealth of Pennsylvania, the
John A. Hartford Foundation, the National Center for Minority Health Disparities, the National Heart Lung and
Blood Institute, the National Institute on Aging, NIH, NIMH, and the Patient Centered Outcomes Research
Institute; grant support from Bristol-Myers Squibb, Eli Lilly, Forest Labs, NIH (grants P60 MD000207, P30
MH090333, UL1RR024153, and UL1TR000005), and Pfizer; and licensing fees from psychometric analysis of
the Pittsburgh Sleep Quality Index, PRO10050447; Dr. Freedman has reviewed this commentary and found no
evidence of influence from these relationships. Dr. O’Hara reports no financial relationships with commercial
interests.
Supported by NIH grant P30 MH090333, the University of Pittsburgh Medical Center Endowment in Geriatric
Psychiatry (to Dr. Reynolds), and the Simons Foundation Autism Research Initiative grant 177986 (to Dr.
O’Hara).
Am J Psychiatry 170:10, October 2013 ajp.psychiatryonline.org 1101
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Unlearn Your Anxiety and Depression The First Five Chapters - A Self-GuidedDocument166 pagesUnlearn Your Anxiety and Depression The First Five Chapters - A Self-GuidedHeather Venitucci100% (9)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hose Tree Person (HTP)Document43 pagesHose Tree Person (HTP)mhrizvi_1279% (33)
- Sheri Van Dijk - Relationship Skills 101 For Teens PDFDocument209 pagesSheri Van Dijk - Relationship Skills 101 For Teens PDFWesley Riann50% (2)
- Prognosis For Ambulation in Cerebral Palsy: A Population-Based StudyDocument10 pagesPrognosis For Ambulation in Cerebral Palsy: A Population-Based StudyRania ENo ratings yet
- The Association Between Blotting Paper Application and Severity of Acne Vulgaris Among Medical StudentsDocument5 pagesThe Association Between Blotting Paper Application and Severity of Acne Vulgaris Among Medical StudentsRania ENo ratings yet
- 217 222CicatricialEctropionDocument7 pages217 222CicatricialEctropionRania ENo ratings yet
- PNTD 0004627 PDFDocument17 pagesPNTD 0004627 PDFRania ENo ratings yet
- Impact of Trichiasis Surgery On Daily Living: A Longitudinal Study in EthiopiaDocument23 pagesImpact of Trichiasis Surgery On Daily Living: A Longitudinal Study in EthiopiaRania ENo ratings yet
- Algorithm For The Management of Ectropion Through Medial and Lateral CanthopexyDocument9 pagesAlgorithm For The Management of Ectropion Through Medial and Lateral CanthopexyRania ENo ratings yet
- Predictors of Trachomatous Trichiasis Surgery OutcomeDocument13 pagesPredictors of Trachomatous Trichiasis Surgery OutcomeRania ENo ratings yet
- Morbili Pada Dewasa: February 2018Document4 pagesMorbili Pada Dewasa: February 2018Rania ENo ratings yet
- Fat Suppression in 3 Tesla MRI For Musculoskeletal Imaging: Techniques and PitfallsDocument33 pagesFat Suppression in 3 Tesla MRI For Musculoskeletal Imaging: Techniques and PitfallsRania ENo ratings yet
- 9 Fat Suppression TechniquesDocument5 pages9 Fat Suppression TechniquesRania ENo ratings yet
- Pi Is 0015028216554612Document2 pagesPi Is 0015028216554612Rania ENo ratings yet
- Speech Problems.Document10 pagesSpeech Problems.Alexander RoblesNo ratings yet
- Behaviourist Learning TheoryDocument10 pagesBehaviourist Learning TheoryCindy TsenNo ratings yet
- Big Five Personality Test ReportDocument3 pagesBig Five Personality Test Reportapi-562187732100% (1)
- Psyc1001 Lecture 1 Summary NotesDocument3 pagesPsyc1001 Lecture 1 Summary NotesDeadly ChillerNo ratings yet
- Humpty DumptyDocument14 pagesHumpty DumptyRicardo GarciaNo ratings yet
- KAP Assignment 1Document5 pagesKAP Assignment 1WanSyamNo ratings yet
- Motivation Resources and ActivitiesDocument18 pagesMotivation Resources and ActivitiesMaria Felisadae Lorenzo-RomanNo ratings yet
- 02 Neurobiologia de La AdiccionDocument25 pages02 Neurobiologia de La AdiccionZaira Camila CriolloNo ratings yet
- Mood ChartDocument2 pagesMood ChartMaria100% (1)
- NCP Depression Version 2Document4 pagesNCP Depression Version 2'SheenMarkReal'No ratings yet
- Cognitive OutcomesDocument13 pagesCognitive Outcomesgunawan djayaNo ratings yet
- Psychotherapy With Older AdultsDocument9 pagesPsychotherapy With Older AdultsMF LeblancNo ratings yet
- Eating Disorders Are Not An Illness Eating Disorders Are UncommonDocument5 pagesEating Disorders Are Not An Illness Eating Disorders Are UncommonRahi PatelNo ratings yet
- Care Plan 27 Bipolar Disorder, Manic Episode: Risk For Other-Directed ViolenceDocument11 pagesCare Plan 27 Bipolar Disorder, Manic Episode: Risk For Other-Directed ViolencesaraNo ratings yet
- Managing Negative or Unhelpful Thoughts: So How Do Thoughts Work?Document5 pagesManaging Negative or Unhelpful Thoughts: So How Do Thoughts Work?Adrienn Krisztina VargaNo ratings yet
- 2 - 4 - Module 4.2 - The Positive (PEA) and Negative (NEA) Emotional AttractorsDocument5 pages2 - 4 - Module 4.2 - The Positive (PEA) and Negative (NEA) Emotional AttractorsBraassociate AdvisoryNo ratings yet
- Cognitive Behavior Therapy For Panic Disorder.Document6 pagesCognitive Behavior Therapy For Panic Disorder.Brian HarrisNo ratings yet
- Final AslDocument11 pagesFinal Aslapi-512908107No ratings yet
- Tajdisk v3 Article ListDocument96 pagesTajdisk v3 Article ListMircea RaduNo ratings yet
- Common Psychiatric DisordersDocument3 pagesCommon Psychiatric DisordersWaheedullah AhmadiNo ratings yet
- Multiple Personality Disorder: Is It Fact or Fiction?: Deguzman 1Document10 pagesMultiple Personality Disorder: Is It Fact or Fiction?: Deguzman 1Eliza Philline De GuzmanNo ratings yet
- 01Document2 pages01BellaNo ratings yet
- Efficacy of Structured Yoga InterventionDocument6 pagesEfficacy of Structured Yoga InterventionJanardhan NNo ratings yet
- Hizon 2 NCP 1 Npi I Am SamDocument5 pagesHizon 2 NCP 1 Npi I Am SamDan HizonNo ratings yet
- Assessment 1Document13 pagesAssessment 1api-297389221100% (1)
- Chap13 Coping With Social AnxietyDocument18 pagesChap13 Coping With Social AnxietyLouise Gleeson100% (1)
- Theoretical Framework and Application-Cindy Ransom Reality Therapy Reflection EssayDocument17 pagesTheoretical Framework and Application-Cindy Ransom Reality Therapy Reflection EssayTan Li Li0% (1)