Professional Documents
Culture Documents
A 23yearold Woman With Panic Disorder Treated With Psychodynamic 1996 PDF
A 23yearold Woman With Panic Disorder Treated With Psychodynamic 1996 PDF
Uploaded by
hectorCopyright:
Available Formats
You might also like
- BrochureDocument2 pagesBrochureapi-375895852No ratings yet
- Internal Medicine Progress Note TemplateDocument2 pagesInternal Medicine Progress Note Templatehector100% (1)
- Development of A Tool To Assess Suicide Potential Among Filipino YouthDocument34 pagesDevelopment of A Tool To Assess Suicide Potential Among Filipino YouthMaria Theresa Deluna Macairan100% (1)
- CASE 7 Somatic Symptom DisorderDocument11 pagesCASE 7 Somatic Symptom DisorderApril AstilloNo ratings yet
- The Sentence Completion Test SSCT Rating Sheet: Stand Up For Himself Instead of Just Saying "Yes" To My Mother AlwaysDocument6 pagesThe Sentence Completion Test SSCT Rating Sheet: Stand Up For Himself Instead of Just Saying "Yes" To My Mother AlwaysRonald Bartolome0% (1)
- Case Presentation 3Document4 pagesCase Presentation 3api-285918237No ratings yet
- Case PresentationDocument33 pagesCase PresentationPratima ThakurNo ratings yet
- Allport's Theory of PersonalityDocument13 pagesAllport's Theory of PersonalityNiharika SpencerNo ratings yet
- Unit 3 The Thematic Apperception Test and Children S Pperception T TDocument16 pagesUnit 3 The Thematic Apperception Test and Children S Pperception T TAhmad Sameer AlamNo ratings yet
- Case Study Prac RevisedDocument13 pagesCase Study Prac Revised20172428 YASHICA GEHLOT100% (1)
- SAMPLE Outline PanicDocument3 pagesSAMPLE Outline PanicdexNo ratings yet
- Expectation From CounsellorsDocument27 pagesExpectation From CounsellorsAkriti SrivastavaNo ratings yet
- Psychology 3E: Saundra K. Ciccarelli, J. Noland WhiteDocument40 pagesPsychology 3E: Saundra K. Ciccarelli, J. Noland WhiteJansen WongNo ratings yet
- Delmundo 2019 - FinalDocument9 pagesDelmundo 2019 - FinalCall me PinguNo ratings yet
- TatDocument4 pagesTatlove148No ratings yet
- A Case Study of A Patient Suffering From Major Depressive DisorderDocument5 pagesA Case Study of A Patient Suffering From Major Depressive Disorderdennis ndegeNo ratings yet
- Karen Horney: Psychoanalytic Social TheoryDocument10 pagesKaren Horney: Psychoanalytic Social TheoryGabriel Lance Ivan ManaitNo ratings yet
- 2nd Testing of The Mentally Retarded PopulationDocument20 pages2nd Testing of The Mentally Retarded PopulationHoorya HashmiNo ratings yet
- Case Study of Social PhobiaDocument1 pageCase Study of Social PhobiaSarah KhairinaNo ratings yet
- Sullivan's Interpersonal TheoryDocument12 pagesSullivan's Interpersonal TheorySumam NeveenNo ratings yet
- SSCTDocument13 pagesSSCTMeharNo ratings yet
- Contemporary PsychologyDocument4 pagesContemporary PsychologyZunair IlyasNo ratings yet
- Aiss Write UpDocument4 pagesAiss Write UpDNo ratings yet
- MA in Psychology - Clinical Psychology (Thesis) .FEUDocument1 pageMA in Psychology - Clinical Psychology (Thesis) .FEUPaul Anthony PascualNo ratings yet
- Chapter 2 Barlow and DurandDocument18 pagesChapter 2 Barlow and DurandSharemax Holdings, Inc.No ratings yet
- Aiman 019309 Peace Psychologyassignment 1Document8 pagesAiman 019309 Peace Psychologyassignment 1Fatima MalikNo ratings yet
- MCQ Questions in Psychology: Described by Adler As HavingDocument7 pagesMCQ Questions in Psychology: Described by Adler As HavingDana AhmedNo ratings yet
- Rotter and MischellDocument3 pagesRotter and MischellangeluNo ratings yet
- Marie Jahoda: Current Concepts of Positive Mental HealthDocument32 pagesMarie Jahoda: Current Concepts of Positive Mental Healthrewv vhiNo ratings yet
- DPC Field Report CompletedDocument36 pagesDPC Field Report Completedraman_bhoomi9910No ratings yet
- Case ReportDocument16 pagesCase ReportSabbir ThePsychoExpressNo ratings yet
- Lived Experiences of Mental Health Service Frontliners Amidst The COVID-19 PandemicDocument14 pagesLived Experiences of Mental Health Service Frontliners Amidst The COVID-19 PandemicPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Psychodynamic and Behavioural Approach To Rehabilitation CounsellingDocument32 pagesPsychodynamic and Behavioural Approach To Rehabilitation CounsellingphakeynishaNo ratings yet
- A Case of Social PhobiaDocument3 pagesA Case of Social PhobiaFaRaz MemOnNo ratings yet
- Psych Case StudyDocument11 pagesPsych Case Studyapi-546513658No ratings yet
- Unit V Personality PDFDocument15 pagesUnit V Personality PDFOmprakash SwamiNo ratings yet
- Stress and Coping NotesDocument10 pagesStress and Coping Notesrashi100% (1)
- Harry SullivanDocument17 pagesHarry SullivanStephanie Joy Escala100% (1)
- Harry Stack SullivanDocument4 pagesHarry Stack SullivanMichal Gail100% (2)
- 1.4 Personality DisordersDocument11 pages1.4 Personality DisordersDomalaon, Princess Sophia B.No ratings yet
- Practical-2 - Eysenck's Personality QuestionnaireDocument18 pagesPractical-2 - Eysenck's Personality QuestionnairegitikaNo ratings yet
- Thematic Apperception TestDocument4 pagesThematic Apperception TestSahil MushafNo ratings yet
- Anxiety Case StudyDocument3 pagesAnxiety Case StudyJennaNo ratings yet
- Psych Assessment Chapter 12Document5 pagesPsych Assessment Chapter 12Marjorie VillarosaNo ratings yet
- Personality Disorders Lesson PlanDocument17 pagesPersonality Disorders Lesson Planapi-284104206No ratings yet
- Mood Disorders - DepressionDocument58 pagesMood Disorders - Depressionmaha abdallahNo ratings yet
- Unit 5 Family InfluencesDocument25 pagesUnit 5 Family Influencesshubhii1997No ratings yet
- I. Overview of Cognitive Social Learning TheoryDocument4 pagesI. Overview of Cognitive Social Learning TheorynitinandsubahNo ratings yet
- Case Study - Mental Status ExaminationDocument5 pagesCase Study - Mental Status ExaminationSrivathsanNo ratings yet
- Physical and Mental AssessmentDocument3 pagesPhysical and Mental AssessmentAlexis FurtonNo ratings yet
- Transpersonal Psychology in The BhagavadDocument9 pagesTranspersonal Psychology in The BhagavadNavneet DhimanNo ratings yet
- Personality DisordersDocument35 pagesPersonality DisordersMonika JosephNo ratings yet
- Clinical Psychology R's Case RecordDocument22 pagesClinical Psychology R's Case RecordSwati Tiwari Life CoachNo ratings yet
- Personality DisordersDocument4 pagesPersonality DisordersAngela Abigail AbingNo ratings yet
- Case AnalysisDocument29 pagesCase AnalysisSuji.TNo ratings yet
- Chapter 6 Somatic-Symptom-and-Related-Disorders-and-Dissociative-DisordersDocument3 pagesChapter 6 Somatic-Symptom-and-Related-Disorders-and-Dissociative-DisordersAnnie SumacotNo ratings yet
- Existential Psychotherapy (Logotherapy) : Bes3148 Theories of Personality Viktor FranklDocument4 pagesExistential Psychotherapy (Logotherapy) : Bes3148 Theories of Personality Viktor FranklNarona MaurenNo ratings yet
- Assignment # 3, Group 4, Clinical Psychology IIDocument9 pagesAssignment # 3, Group 4, Clinical Psychology IIFatima MalikNo ratings yet
- Kinetic Family and Human Figure Drawings of Child and AdolescentDocument310 pagesKinetic Family and Human Figure Drawings of Child and AdolescentBotoi Tabita-LoisNo ratings yet
- Case Analysis EtiologyDocument2 pagesCase Analysis EtiologyKaren LerioNo ratings yet
- Scientific American Mind November/December 2009Document8 pagesScientific American Mind November/December 2009AprilMartelNo ratings yet
- General Internal Medicine In-Training ObjectivesDocument18 pagesGeneral Internal Medicine In-Training ObjectiveshectorNo ratings yet
- Endocrinology In-Training ObjectivesDocument12 pagesEndocrinology In-Training ObjectiveshectorNo ratings yet
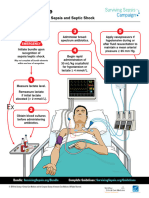
- Surviving Sepsis Campaign Hour 1 Bundle 220414 142741Document5 pagesSurviving Sepsis Campaign Hour 1 Bundle 220414 142741hectorNo ratings yet
- Episode ListDocument25 pagesEpisode ListhectorNo ratings yet
- Metabolism With Triphasic Oral Contraceptive Formulations Containing Norgestimate or LevonorgestrelDocument6 pagesMetabolism With Triphasic Oral Contraceptive Formulations Containing Norgestimate or LevonorgestrelhectorNo ratings yet
- U.S. Selected Practice Recommendations For Contraceptive Use, 2016 MMWRDocument60 pagesU.S. Selected Practice Recommendations For Contraceptive Use, 2016 MMWRhectorNo ratings yet
- 60 Affirmations For PeaceDocument21 pages60 Affirmations For PeacehectorNo ratings yet
- Gauthier 1992Document6 pagesGauthier 1992hectorNo ratings yet
- Blood Pressure Log 02Document1 pageBlood Pressure Log 02hectorNo ratings yet
- Clinical Reasoning Guide FormDocument3 pagesClinical Reasoning Guide FormhectorNo ratings yet
- Glasgow Coma Scale (With Explanations)Document1 pageGlasgow Coma Scale (With Explanations)hectorNo ratings yet
- A Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfilesDocument4 pagesA Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfileshectorNo ratings yet
- 050 Bonus GratitudeDocument9 pages050 Bonus GratitudehectorNo ratings yet
- ACGMECLERNational Report Findings 2019Document132 pagesACGMECLERNational Report Findings 2019hectorNo ratings yet
- The AOA Guide:: How To Succeed in The Third-Year ClerkshipsDocument25 pagesThe AOA Guide:: How To Succeed in The Third-Year Clerkshipshector100% (1)
- Assignments Report: Saved ProgramsDocument16 pagesAssignments Report: Saved ProgramshectorNo ratings yet
- 060 Bonus LawOfCauseAndEffectDocument1 page060 Bonus LawOfCauseAndEffecthectorNo ratings yet
- SketchyIM Check List PDFDocument5 pagesSketchyIM Check List PDFhectorNo ratings yet
- Purpose, V Purpose, V Purpose, V Purpose, V Purpose, Vision, Ision, Ision, Ision, Ision, Goals Goals Goals Goals GoalsDocument9 pagesPurpose, V Purpose, V Purpose, V Purpose, V Purpose, Vision, Ision, Ision, Ision, Ision, Goals Goals Goals Goals GoalshectorNo ratings yet
- Fibromyalgia: Basic InformationDocument5 pagesFibromyalgia: Basic InformationhectorNo ratings yet
- The Law of Gender: Be Patient! All Ideas Move Into Form in The Right TimeDocument1 pageThe Law of Gender: Be Patient! All Ideas Move Into Form in The Right TimehectorNo ratings yet
- 056 Bonus RelativityDocument1 page056 Bonus RelativityhectorNo ratings yet
- 008 ASereneMind PDFDocument2 pages008 ASereneMind PDFhectorNo ratings yet
A 23yearold Woman With Panic Disorder Treated With Psychodynamic 1996 PDF
A 23yearold Woman With Panic Disorder Treated With Psychodynamic 1996 PDF
Uploaded by
hectorOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A 23yearold Woman With Panic Disorder Treated With Psychodynamic 1996 PDF
A 23yearold Woman With Panic Disorder Treated With Psychodynamic 1996 PDF
Uploaded by
hectorCopyright:
Available Formats
Clinical Case Conference
A 23-Year-Old Woman With Panic Disorder
Treated With Psychodynamic Psychotherapy
Barbara Mitrod, M.D., Fredric N. Busch, M.D., Eric Hollander, M.D.,
Andrew Aronson, M.D., and Larry Siever, M.D.
professional who had never sought psychi-
T his
namic
case illustrates
factors in
psychody-
panic disor-
lasted for 20 minutes and then gradually
abated over the better part of an hour. Ms. atric help.
A did not think of her panic as a reason for
den, which is increasingly viewed as seeking psychiatric treatment. She did not Social History
a neurobiological disorder. The pa- have agoraphobia but lived with a chronic,
tient was managed with psychody- vague sense of severe anxiety, accompanied Ms. A functioned fairly well in spite of her
namic psychotherapy alone with by the fantasy that she was “doomed.” She symptoms. She high aver-
performed in the
had no specific phobias. age range in school, but achieving at this
complete resolution of her panic The symptom that caused Ms. A the most level required tremendous effort and anxi-
symptoms. Although the patient’s distress was her chronic difficulty negotiat. ety, despite her obvious superior intellect.
panic resolved within 2 months af- ing relationships with others. Beginning She had friends, but her relationships
ten she began twice-weekly psycho- with her earliest relationships with her par- tended not to last, so that she frequently felt
ents and older sister in childhood, Ms. A hurt and left out.
therapy, she remained in therapy
found herself in interpersonal situations in Her first experience away from home was
for an additional 22 months after which she felt abused and demeaned, either after 1 0th grade, when she attended a pro-
the resolution of hen panic disorder emotionally or physically. In high school gram for high school students abroad. Al-
and made major gains in her char- and college she had often felt belittled by though she had longed to be in this program,
friends and boyfriends. Currently, these is- several days after she arrived in the new
actenological problems.
sues recurred in the context of her relation- country she suddenly felt “very lonely and
ship with her fianc#{233} and her interactions strange” and desperately longed to return
(;UINICAI. Vl(;NFTTE (l)r. Milnod) with colleagues at graduate school. In the home. She felt that to do so would represent
course of these stormy relationships, Ms. A a terrible personal failure. She managed to
would become so agitated and panicked remain in the program but began a romance
Chief Complaint
that she was often violent. In the middle of with a fellow student who was attracted to
fights with her fianc#{233}, for example, she her but for whom she herself felt no attrac-
Ms. A, a 23-year-old single, white Jewish
would find herself hitting him and running tion, “just so I didn’t miss home so badly.”
graduate student, presented in a state of ex-
out of the apartment dressed in insufficient In contrast, the transition to college had
treme anxiety and emotional upheaval. Re-
clothing in the middle of the night. She had been less anxiety provoking.
cently her relationship with her boyfriend
no vegetative symptoms. She had no history She first had sexual intercourse with a
had become increasingly violent, and at the
of depression, mania, psychosis, or sub- boyfriend in college. Ms. A experienced the
time of presentation she had just begun
stance abuse. She had never been suicidal. sexual encounter as “frightening and revolt-
graduate school and moved to a new city.
Ms. A’s medical history was considered ing,” not having anticipated how upset she
Of greater concern to her, she had just made
noncontributory. would become. In recalling the event, she
the decision to marry her boyfriend.
said that the most distressing thing had been
Family History that she had bled on her bed. She terminated
Past Psychiatric History this relationship soon after this experience.
Ms. A’s mother had been in a Nazi con-
Ms. A reported that, starting in the second centration camp in Europe during World Mental Status Examination
grade, she had experienced frequent panic War II and had witnessed the public murder
attacks with prominent tachypnea, tachy- of her own family by the Nazis before that. A thin, attractive young woman, Ms. A
cardia, and a sense of loss of balance, ac- The mother had an episodic, uncharacter- was engaging and thoughtful throughout
companied by the idea that she was losing ized psychotic disorder that periodically her initial evaluation. She used measured
her mind. The attacks occurred frequently, emerged, making her “wild.” She screamed language to describe her dramatic experi-
usually several times per week. They usually uncontrollably at these times and behaved ences with her family and fianc#{233}. Her Ian-
in a frightening, erratic, and highly sexual- guage was in marked contrast to her voice,
Received Sept. 20, 1995; revision received ized manner. She had never sought psychi- which was noticeably dramatic and loud.
I)ec. 6, 1995; accepted Feh. 6, 1996. Fromii atric treatment. She gave the immediate impression of being
the 1)epartmiient (If Psychiatry, Mount Sinai Ms. A’s father, a teacher, had been diag- interested in understanding herself better
School (if Medmcmmie, New York. Address re- nosed as having bipolar disorder and had and seemed anxious. She displayed a full
print requests to l)r. Mmlrod, Pavmie Whmtmiey been treated successfully with ECT and lith- range of affect, which was appropriate to
Clinic, Stmite 3N, 445 Fast 68th St., New ium during Ms. A’s late adolescence. the content of her discussion. She seemed
York, NY I 0021. Ms. A’s older sister was a high-achieving very bright and had a good vocabulary and
698 Am] Psychiatry 153:5, May 1996
(IiNI(Al. (;AsF CONFERENCE
facility for explaining her ideas. Her thoughts
were well organized, and she displayed no FIGURE 1. Multiaxial DSM-IV Diagnosis for a Patient With Panic Disorder
evidence of psychosis or suicidality. Her and Characterological Problems
cognitive function was intact.
Axis I
Formulation Pamimc disorder without agoraphohma
Axis II
Ms. A was described as a 23-year-old Pensomiality disorder not otherwise specified, with horderlmne and sadoniasochmstic
daughter of a concentration camp survivor featu nes
with a longstanding history of panic disor- Axis III
der and prominent characterological prob- Noncontnmbutony
lems that engendered stormy functioning Axis IV
in school and in interpersonal relation- Severe problems (exposure to two psychotic parents, recent move to a stramige cmt ,
ships. Her DSM-IV multiaxial diagnosis is starting graduate school, and becoming engaged to he married)
shown in figure 1. Axis V
55
Course in Treatment
Ms. A was treated with psychodynamic
rooms or public buses. As I began to ques- school, but his studies were in an unrelated
psychotherapy alone for a variety of rea-
tion her about the feelings that she was field and he could not understand her com-
sons. Because she did not seek treatment for
aware of during the attacks, and during sex, plex questions, although he often tried. Even
panic symptoms but, rather, sought help in
it became clear that she had always avoided though she partly knew that she was asking
the management of her intense emotional
thinking about them. She said that she was something impossible of him, Ms. A always
states, the violence in her love life, and her
afraid that if she put too much time into had the feeling that he could help her if he
high background level of anxiety and “con-
trying to understand the irrational part of wanted to. She felt that, like her father, he
fusion,” treatments aimed solely at panic re-
herself, she would discover that she was was saying that he just could not be both-
mission were not feltto be sufficient. She did
“crazy,” like her mother. She gradually be- ered. Intense fights ensued. She angrily in-
not want to take psychiatric medications,
gan to say that she often did not want to suIted B at these times. Once, when Ms. A
which reminded her of her impaired father.
have sex when her fianc#{233}
wanted to and that had been deriding him for his stupidity and
Additionally, she felt demeaned by the con-
she often found herself extremely and, to lack of interest, B became so angry with her
sideration of a behavioral plan, which she
her mind, unaccountably angry at her fianc#{233} that he hit her while she was having a panic
felt implied she was seen as not bright
at these times. She knew that he loved her, attack. After he hit her, she felt calmer,
enough to engage in insight-oriented psy-
and he certainly was not trying to be mean. which later frightened her.
chotherapy. It became clear fairly rapidly in In treatment, Ms. A said that her relation-
Ms. A later reported that since I had be-
the course of the psychotherapy that her
gun to ask her about these times, she had ship with B reminded her of her childhood
panic attacks were closely intertwined with
become aware for the first time of fantasies relationship with her sister, who had often
her characterological difficulties and, in
that she had previously managed to ignore. beat Ms. A when they had been left alone
particular, were intimately tied to her sense In particular, she found herself frequently together. These had been very fearful times
of being abandoned and her sadomasochis imagining physically beating her fianc#{233}, for her. Her sister had forced her to clean
tic preoccupations. With the use of psy- the house and then would hit her if the
knocking him unconscious with a lamp, for
chodynamic psychotherapy, I was able to example. These images occurred to her in house was not clean enough. Ms. A had felt
address Ms. A’s acute sense of not being brief flashes, which she studiously avoided. unable to tell her parents about these
cared for as it emerged in the developing She found these ideas sexually arousing, and events. She had frequently had panic attacks
transference within 6 weeks of the begin- in the course of the psychotherapy she dis- when she had been alone with her sister as
ning of treatment. Her panic attacks remit-
covered that she was able to achieve orgasm a child.
ted in the context of that work, as will be only when she thought about these things. As this material emerged, Ms. A’s panic
elaborated. She experienced panic attacks at the same attacks increased in frequency. “I never
Ms. A’s treatment began with exploration time, with the prominent fantasy that she considered that my panic attacks were any-
of her panic attacks. The first panic attack was passing out and that no one would care thing I couldn’t handle, but since you’ve
she had ever experienced occurred before a or notice. She found this extreme degree of been focusing on them so much, they’ve just
mathematics test in second grade, which she anxiety exciting. Ms. A reported highly gotten worse and worse. They are a problem
was convinced that she would fail. Ms. A charged trips to her parents’ basement, now, I can’t function!” she complained.
had longstanding concerns that she was stu- where they kept their books (with pictures I pointed out to her that it seemed as
pid, although she had always been success- in them) about the Holocaust. She had se- though she felt that her worsening symp-
ful academically. She attributed this feeling cretly read these books as a child. They gave toms were the fault of her treatment, and
in part to the fact that she always compared her “a sick and excited feeling, but I couldn’t Ms. A agreed.
herself with her sister, who was 3 years stop going back.” She often thought of her “I wonder if you have been feeling similar
older than Ms. A and had been outstand- mother and what her mother must have things here in treatment with me as you feel
ingly successful in school and had won many lived through in the concentration camp. with B, and as you felt with your father as a
prizes. Ms. A had turned to her father for Her mother had told Ms. A that she had been child; that you desperately need help and
help with her school work, but this had raped repeatedly by the guards in the con- that I don’t care, or can’t be bothered to
proved to be a bigger problem than the work centration camp and that this was how she help you.”
itself. He was distracted and disorganized, had managed to stay alive. Ms. A recalled “I think I do feel that,” she said, sadly.
and she always had the feeling that he could staring for long hours at the emaciated bod- “I hate this.” Later in that session, she be-
not be bothered to understand her. She ies of the Jews in the pictures. “Everything gan to laugh about the idea that I was “her
wound up feeling rejected by him and hope- was life and death for me from an early age,” problem.”
less about herself and her mind. she said. After this exchange, which came after 6
At the time of her initial evaluation, Ms. While she recalled these childhood weeks of close focus on Ms. A’s panic, her
A was having panic attacks while studying events, Ms. A also described more details panic attacks suddenly, entirely disap-
and, in addition, almost every time that she about her relationship with B, her fianc#{233}. peared for the firsttime since her childhood.
and her fianc#{233}
had sex. She also had panic She often turned to B for help in under- Ms. A’s psychotherapy continued for 2 more
attacks in unexpected places, such as class- standing her work. B was also in graduate years, during which time her panic attacks
Anz I Ps)’cbzatrv 153:5, Ma)’ I 996 699
CLiNICAL. CASE CONFERENCE
never recurred. Ms. A moved to another city Famiiily amid twin sttmdmes amid biological persomialitv dis(irder, omie pr(imiiinemit
after her graduation. She elected not to re- challenge studies suggest that there are c(Inipomiemit of which was high anxiety
sume psychotherapy there. Her panic at- both state- and tra it-related vtmlmicrabili- with pamiic attacks? There is also a
tacks have not recurred for the ensuing 7
ties iii panic disorder amid have led to the questiomi (if the presence of posttrau-
years, according to a follow-up telephone
developmiiemit (if provisiomial biological miiatic stress disorder (PTSI)). Was the
conversation.
Although to my knowledge no systematic Iii(idels (3, 4). Taken together with stud- pamiic really just (IOC segmiiemit of PTSI),
studies of psychodynamic psychotherapy ies describing patients’ respomises to psy- or was it traumiiatmcallv induced panic
for the treatment of panic disorder have chopha rniacologic, prescri Pt i se cogn m- attacks?
been performed, the literature contains tive behavioral, and nomiprescniptmve The miiore comii(irhid comidmtmomis a pa-
many case reports of successful treatment of psychotherapeutic strategies (3, 5, 6), this tient has, the more difficult the treat-
panic disorder with psychodynamic psycho- evidence permits formulatiomi of an imite- Iiiemit and the more amicillary services
therapy (1, 2). In this case, Ms. A’s panic at- grated model of panic disorder, which needed for symptomii relief. Nis. A does
tacks emerged in the context of frightening comiipnises a spectrum of illmiess. not appear to have had omilv clear-cut
rageful feelings that she experienced as be-
At one end (If the spectrum, pamiic dis- pamimc disorder that responded to psy-
ing out of control and potentially danger-
order appears to be more biologically choanalytically oniemited psvchother-
ous. She had experienced this same set of
feelings toward her father and toward B, driven, while omi the other cud ofthe spec- apy. She is a unique imidividual who had
when she felt abandoned by them. The sense trumii it cami he seen as largely psychologi- (I iii iJ(i persomiality disorder that miiay
that her rage was dangerous was reinforced cally dnivemi. Neither a unitary biological have comitnmhuted to her panic synip-
by the physical fights that occurred between mior psychological lesion is suggested in t(iiiiS, amid treatmliemit for her should
Ms. A and her sister and later with B. Her the pathogenesis. Preva iling cognitive he- has’e heemi tailored dmffereiitly froni that
terrifying fantasies had their origin in her havioral models descni he a fumidamenta I, for someone with only panic attacks, iii
readings about the Holocaust and in the cOiiditi(Iiied, catastrophic miiisperceptmomi which case the treatniemit of choice
sense of chaos and danger that character-
(If interoceptive bodily cues (5, 7, 8). Iii would miot necessarily he psychoamia-
ized her household when she was a child.
The association of her rage with exciting, sa- a simplified version of the classical psy- lyticall oriented psychotherapy.
domasochistic sexual fantasies initially choanalytic model of psychological Klein has referred to the “ false suffo-
made herless willing to relinquish her symp- symptom formation, amixiety develops in catiomi alarmii” as a hallmiiark of pamiic
toms, or to consider her frequent panic at- response to au intermial threat constituted disorder ( 1 1 ). ()mie of the fotmr svmp-
tacks as a problem, as her experiences of ex- by an objectionable affect, idea, or fami- t(Iiiis of Ms. A’s panic attacks was a
citement and danger, rage, and anxiety tasy. There is clear evidemice of the effi- sense of suffocation. Another charac-
merged. She had successfully managed to ig- cacy of verbal therapeutics iii panic dms- tenistic clinical symiiptom is a rapid crc-
nore her violent, sadistic fantasies before order, at least in the short term, which scendo (if anxiety, whether the anxiety
entering psychotherapy. The safety of the
suggests a salutary effect ofexpenience on emerges Omit of the blue or iii respomise
therapeutic relationship allowed these feel-
biology (5, 9, 10). This case is a stnmkimig t(i triggering factors. Clearly, the in-
ings to be experienced consciously in the
transference, where they intensified and her instance in which an imiipressively favor- creased heart rate, the feeling of losimig
symptoms temporarily worsened. In this able, sustained outcome seemns related to control, the loss (If balance, and the
situation they could be carefully explored a therapeutic strategy that targeted a feeling (If peril support the diagnosis of
and interpreted, allowing her to have a deeper psychological structure of pamiic. panic disorder.
greater sense of safety and control over her The symptom structure may be said A n tmniber (If hiologica I miiechamiismiis
feelings. This enabled her to relinquish her tO have been the catastrophic elabora- can comitril mte t(i pamiic, mncltmdimig carhomi
panic attacks, which to her represented a tion of an idea or impulse of particular dioxide hypersensitivity, locus ceruleus
somatic, masochistic communication of her
meaning for the patient, triggered as amid serotonergic hypersemisitivity, amid
rage and sense of isolation. In addition, the
she began to fail to nianage or avoid hypersensitivity to s(Idiumii lactate. An-
process of psychotherapy allowed her to re-
evaluate her fantasized representations of these memital contents. The therapeutic other important miiechiamiismii niay lie re-
others as abandoning. strategy was based on a model of psy- lated to traumiiatmcallv imiduced intrusive,
This patient remained in twice-weekly chopathology that conceptualizes symp- persistemit, amid repetitive amixiery states.
psychotherapy for 2 years after the disap- t(imflS iS being connected with umiderly- Fimially, the issue of separatiomi anxiety
pearance of her panic attacks, during which ing character. should be highlighted. Withmmi the course
time she gained a great deal of self-confi- The therapeutic mechanmsmii of action (if Nis. A’s treatmiient, omie of the points
dence and broke off her engagement to B. seemiis to have been the toleratiomi of the that emerged was her sense of ahandomi-
The sadomasochistic features of her fantasy
experience (If frightenimig amid violent ment, which seemiied to trigger pamiic. In
life remained a central focus of the work of
famitasies, previously avoided amid tin- retrospective studies it has been demon-
her psychotherapy.
manageable. These were presented in a strated that niany adults with pamiic dis-
graded manner iii the treatmiiemit, facili- order have a history of early separatiomi
DISCUSSION tating recognition, defimiition, comiipre- amixiety ( 12). The fact that Ms. A’s panic
hension, and ultimately miiamiagememit in attacks started in the secomid grade raises
Dr. Aronson conscious awaremiess. the questmomi (If a history of separation
amixiety. Sepa ration amixiety is au inipor-
Panic disorder is an excellent exam- Dr. Hal/tinder tam-It symptom that iiiay have been ad-
pie of a psychobiological disorder. A dressed iii psychoamialytmc treatmemit in
wealth of data have accumiiulated as to A key question in this discussiomi is this case amid niav have heemi a factor in
the important comitrihutiomis of pedi- whether this case represents true panic the resolution of the panic attacks.
gree, biological vulnerability, amid expe- disorder. Did this patient have panic After the diagmiosis is made, the secomid
rience. The latter tWo factors often seem disorder in additiomi to a comorbid phase of treatniemit for pamimc disorder is
t(I imiteract in a fashiomi that provides personality disorder (borderline per- education. Patiemits must he taught ah(iut
striking examples of the deforniimig ef- sonality disorder with sadoniasochmstmc the catmses (if panic disorder, amid then
fects of experience (In hiolog . features)? Or did she pnimiiarily have there mieeds t(I he educatiomi about differ-
700 Am j Psychiatry l 53:5, May l 996
CLINICAL CASE CONFERENCE
ent treatment approaches. This patient panic symptoms,
ignoring other char- cidation of some transference issues, al-
declined medication and behavioral then- acterological or environmental factors lowed for the emergence and reevalu-
apy. With more aggressive psychoeduca- that contribute to their current distress. ation of these experiences of danger in
tion, she might have been persuaded to In my experience, most panic patients the context of the relationship with the
accept some targeted, rapidly effective report having experienced major trauma therapist. This case vividly demonstrates
treatment for panic. in their lives. Panic attacks that appear why psychodynamic psychotherapy
Ms. A’s panic attacks occurred within “out of the blue” are often found on should be carefully considered as a means
the context of personality disorder. Anxi- closer inspection to occur in the context to reduce vulnerability to panic.
ety is a common target symptom in treat- of particular stresses that trigger intense It is well known that panic patients
ing personality disorders. In a study by affective reactions of sadness, anxiety, continue to struggle with the intense af-
Johnson et al. (13), there was a high rate and rage. In a sense, we distinguish panic fects of rage, anxiety, and loneliness af-
of suicide attempts among patients with from PTSD on the basis of the type of ter the initial symptom reduction that
panic disorder. This finding has been trauma the patient experienced and on can be achieved with brief, panic-fo-
questioned because panic disorder pa- the presence of a certain degree of intru- cused treatments. Therapists may well
tients who attend anxiety disorder clinics sive thoughts. The distinction may be be enacting their countertransferential
do not have high rates of suicide at- somewhat arbitrary. feelings of wishing to avoid pain by fo-
tempts. The question is whether the epi- Although these views have been devel- cusing on panic alone.
demiologic study by Johnson et al. was oped from a series of case studies such as
measuring panic in the context of person- this one, a pilot study was done at the Dr. Siever
ality the high rate of sui-
disorders; if 5(1, Payne Whitney Clinic to systematically
cide attempts may have been attributable assess some of the aforementioned issues How are these different diagnoses or
to the presence of comorbid personality ( 14, 15). Psychodynamic interviews were symptoms related to each other? Does
disorder rather than to the panic disorder conducted with nine consecutive patients this list of comorbid diagnoses imply
itself. who presented to the Payne Whitney that they are independent entities? Can
Clinic anxiety disorder clinic and met the we think of pathophysiologic models
Dr. Busch DSM-III-R criteria for panic disorder. that might help us to understand the in-
These interviews revealed that identifi- terrelationship of the different symp-
This case is a highly informative exam- able, meaningful stressors, which were toms of these comorbid diagnoses in a
pIe of psychodynamic pa-
treatment of a experienced as threats to important rela- way that would inform the selection of
tient with panic disorder. Although to my tionships, preceded the onset of panic in appropriate treatments for patients like
knowledge there has been no systematic all ofthe patients. The patients described this one?
study of the psychodynamic treatment of growing up in frightening households, One question that has been raised is,
panic, the literature contains many re- with parents they viewed as temperamen- “Are these true panic attacks?” The ar-
ports of cases in which it was successful. tal, controlling, and demanding. Most of guments that this is not a typical case of
In addition, early excitement about the these patients described chronic difficul- panic disorder are 1) agoraphobia is
long-term efficacy of short-term medica- ties with acknowledging and expressing not present and 2) there are preexisting
non and cognitive behavioral treatments angry feelings. They reported having ma- stressors, which may often occur in
has been tempered by reports of relapse jon, longstanding problems in their rela- panic disorder but are not considered
or other persistent symptoms following tionships and at their jobs. A systematic prototypic in some categorical views of
these treatments. study (16) comparing defense mecha- the disorder. The fact that Ms. A was
In mm’ view, Dr. Hollander is stressing nisms in panic patients and dysthymic pa- the daughter of a Holocaust survivor
false dichotomies that interfere with tients revealed that the panic patients fre- may have profound implications that
more complex conceptualizations of quently employed reaction formation could influence our understanding of
panic disorder that are necessary for re- and undoing, defense mechanisms that this patient. How much of what we are
fining treatments aimed at vulnerability represent patients’ attempts to modulate seeing can be understood as personality
tO panic. The dichotomies are I ) that anger. It is my view that these charac- disorder, or even PTSD, rather than
panic disorder exists independently from terohogical and affective vulnerabilities panic disorder? If the symptoms are re-
underlying personality predisposition provide an important area of exploration viewed, however, they include classic
and 2) that PTSD is unrelated to panic for treatment aimed at the reduction of symptoms of panic disorder, such as
disorder. We have a tendency to dichoto- vulnerability to panic recurrence. tachypnea, tachycardia, and the feeling
mize syndronies along the lines of specific Psychodynamic psychotherapy, with of impending doom. Therefore, these
DSM-IV diagnoses and then describe pa- its emphasis on development
the role of episodes probably do represent panic
tients as having comorhid conditions. and intrapsychic conflict in symptom attacks, and the diagnosis appears to be
These diagnostic splits reduce the focus causation, is well suited to address these warranted.
omi how various symptom constellations areas of vulnerability. As described in the According to DSM-IV, Ms. A is de-
or personality predispositions may inter- clinical vignette, psychodynamic psycho- scnibed in terms of her comorbid diag-
act with each other. therapy focused on the aspects ofMs. A’s noses. At another level, by formulating
Many patients with panic disorder symptoms that were unique to her, and what the relationships between these
do not meet the criteria for an axis II it carefully explored the meaning of those different diagnoses might be, we can
personality disorder, but with most pa- symptoms. Ms. A’s panic attacks were reach a more unified understanding of
tients, as with Ms. A, panic symptoms found to be closely associated with arous- the case. Her central emotional issues
are embedded in a set of charactero- ing and frightening violent fantasies and were her fears of separation, abandon-
logical predispositions that lead to vul- with a perception of others as abandon- ment, and abuse. How were these is-
nerahility to panic onset and recur- ing in need. Other techniques
times of sues interconnected in this offspring of
rence. Patients often are unaware of employed, including the exploration of a Holocaust survivor, who appears to
these links and complain primarily of some unconscious processes and the elu- have been sensitive to separation and
Am J Psychiatry l53:5, May I 996 701
CLINICAL CASE CONFERENCE
vulnerable to affective and anxiety Her innate vulnerabilities and the medication treatment. Medication can
symptoms? Her father’s diagnosis of enormous trauma and stressors she ex- be helpful, even if the causes are not ge-
bipolar disorder suggests a genetic vul- perienced may have sensitized her inter- netic and the psychological effects of
nerabihity, as affective illness can be fa- nal alarm system. With the internaliza- environmental antecedents are great.
milially associated with panic disorder. tion of her anger and separation fears, Ms. A responded well to psychody-
These vulnerabilities played out in the alarm system becomes easily over- namic psychotherapy without medica-
the context of her particular develop- whelmed in the face of events that reso- non. An alternative approach would
mental history. One wonders what the nate with the earlier traumas, and panic have been to pursue the option of medi-
nature of her relationship with her attacks ensue. cation, the best-validated treatment op-
mother was. Often, one finds histories Panic attacks used to be called “anxi- tion, by further exploring the patient’s
of separation anxiety in patients with ety attacks,” which were often treated resistance to it. Her resistance may
early-onset panic. In Holocaust survi- with psychodynamic therapy focusing have been connected with her father’s
vors and their offspring, there is often a on the dynamics of the precipitant illness. For some patients, the act of
powerful dynamic involving the survi- events. Now that we understand some taking medication may seem to them to
von’s fear of losing his or her child. The of the biological basis of panic disor- invalidate their experience of having
fear of any kind of separation, which der, in which there are repetitive, fre- been a victim, and to take medication
raises the threat of death or loss, may quent panic attacks, often in the con- might imply that they are not victims
be transmitted in the family. text of agoraphobia and in many cases and, instead, are defective. These issues
Another dynamic is that of the con- without easily elicited triggers for the can be addressed actively in psycho-
densation of physical abuse, violence, specific attack, we have found effec- therapy. Even if medication proves
sexual abuse, and sexual excitement, tive pharmacologic treatment for the unnecessary because of improvement
which are embodied in the mother’s re- disorder. The kind of developmental during the course of the therapy, a dis-
counting of her rape experience. Ac- trauma that Ms. A must have experi- cussion of the feelings and resistances
cording to Dr. Rachel Yehuda, overt enced clearly sensitized her to environ- involving medication can he useful. Ms.
acknowledgment and discussion of this mental stress. This does not mean that A, had she taken medications, might
kind of rape experience with one’s chil- the panic attacks were not real, nor have experienced symptom relief any-
dren is rather unusual (R. Yehuda, does it mean that they might not have way, perhaps sooner, without diminu-
personal communication, 1995). This responded to medication. It might tion of the psychotherapeutic work.
case report provides little information point to a more favorable outcome of We cannot retrospectively evaluate
about Ms. A’s mother, but her “crazy using a psychodynamic intervention, these alternative scripts.
episodes” suggest the possibility of since Ms. A could analyze her experi- For this patient, the opportunity to
problems with affective boundaries and ence and bring insight to bear on it, as reexpenience some of her dreaded fan-
impulse control. Her open discussion opposed to viscerally experiencing panic tasies in a safe environment brought
of these experiences might represent an attacks that had become relatively them to light and was useful in allow-
inability to control her impulse to tell autonomous of any psychologic event. ing her to free herself of her incapacitat-
her children explicit details that could As a Holocaust survivor’s daughter, ing panic attacks. This case provides a
only be terribly confusing and upset- this patient is an example of a victim good example of the multiple influ-
ting for them. When Ms. A was grow- who becomes the abuser in her violent ences on the development of panic dis-
ing up, she may have wanted to turn to fantasies. This dynamic can be seemi in order and demonstrates that sometimes
her father, who seemed to have been the context of personality disorders, a psychotherapeutic intervention can
somewhat distracted, preoccupied, and such as borderline personality disorder. make dramatic inroads. With someone
depressed himself. Her father was A victim/abuser cycle is common among like this patient, even with medication
someone with whom Ms. A may have people who have grown up in families one would recommend some kind of
identified in terms of her own possible where there are such charged histories. psychotherapy. However, the “etiol-
affective vulnerabilities. She may have Some of Ms. A’s early symptoms, for ogy” of the disorder does not necessar-
developed a sense that she could not en- example, studying for a test and being ily dictate which treatment will work,
gage him and that he was not very in- afraid she would fail, may also have in- nor does the treatment’s efficacy neces-
terested in her, experiences that she volved fear of success, because success sarily identify the etiology of the disor-
later replicated with her fianc#{233}. might have seemed to be equivalent to der in some simplistic fashion.
During her early years, Ms. A devel- separation, and that was prohibited by
oped an active fantasy life, with both sex- Ms. A’s mother or the family. These are Dr. Milrod
ual and aggressive fantasies. She went to speculations.
the basement and looked at books of the In planning treatment for this pa- I will clarify sonic clinical points.
Holocaust and formed highly primitive, tient, we would have to consider the This patient, like so many panic pa-
sadomasochistic ideas about the nature following points: the mother’s Holo- tients, experienced
her panic attacks as
of sexual relationships, which were both caust experience is an obviously pro- coming “out (If the blue” until we were
arousing and highly disturbing. These ex- found environmental issue. The family able to explore them in treatment. She
periences likely had a profound impact history of bipolar illness on the other had a long history of separation anxiety
on her development. It is somewhat sun- hand speaks to genetic influences. The disorder but no longer met the DSM-
prising that she was not more disturbed work by Yehuda et al. (17) on the off- III-R criteria at the time that I treated
than she was. Indeed, the worst difficul- spring of Holocaust survivors showed her as an adult. However, separations
ties she had were in her relationship with profound biological changes and sensi- in the context of the therapeutic rela-
her fianc#{233},
which inevitably involved in- tization to stress, in a manner similar to tionship were difficult for her to toler-
timacy, and the reexperiencing of sexual that found in the parents who were the ate, demonstrating that the dynamism
and aggressive feelings that were con- survivors themselves. Such environ- was still alive for her and was an active
nected with some of her earlier fantasies. mental determinants do not preclude agent in the psychotherapy. In her
702 Am] Psychiatry 153:5, May 1996
CLINICAL CASE CONFERENCE
cally minded. All ofthese attributes made chemical overview of models and mecha-
childhood, every separation, particu-
nisms. Br J Psychiatry I 992; 160:165-178
larly when she started school, had been her a good candidate for this form of
4. Targum S: Panic attack frequency and vulner-
experienced as a crisis. At the time that treatment, and these characteristics like- ability to anxiogenic challenge studies.
I was treating her, she could no longer wise would have made a more superficial Psychiatry Res 1 992; 36:75-83
stand to he around her family. She was approach to her symptoms less meaning- 5. (;raske M, Waikar S: Panic disorder, in Hand-
hook of Prescriptive Treatments for Adults.
very frightened by the gravity of the ful to her.
Edited by Hersen M, Ammerman R. New
psychopathology in both of her par-
York, Plenum, 1994, pp 135-155
ents, and this was important in her re- Dr. Siever 6. Shear MK: Cognitive behavioral treatment
fusal of medication and in her down- compared with nonprescriptive treatment of
playing of her panic. Historically, thiscase is ofinterest. 5ev- panic disorder. Arch Gen Psychmatry 1994;
S I :395-401
The question of what protective fac- eral decades ago,
in the heyday of ana-
7. MargrafJ: Sodium lactate infusions and panic
tors permitted her to be as healthy as lytically oriented therapy, patients like attacks: a review and critique. Psychosom
she was brings up interesting issues this were seen as enacting neurotic con- Med 1986; 48:23-51
about the management of trauma. flicts and experiencing anxiety attacks re- 8. Clark D: Cognitive approach to panic. Behav
Why are some people less vulnerable to hated to those conflicts, and they were Res Ther 1986; 24:461-470
9. Shear MK: Cognitive behavioral therapy for
circumstances that would be over- treated with psychodynamic interven- panic: an open study. J Nerv Ment Dis 1991;
whelming to others? This patient’s tions that often lasted longer than this 179:468-472
older sister was the phobic companion treatment. Then psychiatrists became 10. Shear MK, Fyer AJ, Ball G, Josephson 5, Fitz-
of their mother. Her sister was a higher aware that one could focus on symptoms patrick M, Gitlin B, Frances A, Gorman J,
Liebowitz M, Klein MF: Vulnerability to so-
achiever than the patient. She was por- of repeated panic attacks, especially in dium lactate in panic disorder patients given
trayed as rigid by Ms. A, and her pres- the context of agoraphobia, and inter- cognitive-behavioral therapy. Am J Psychia-
ence permitted Ms. A to escape some of vene successfully with medication. Dr. try 1991; 148:795-797
the intensity that characterized the sis- Milrod is suggesting coming back to a I 1 . Klein DF: False suffocation alarms, spontane-
0U5 panics, and related conditions: an integra-
ter’s relationship to their mother. psychodynamic approach distinct from tive hypothesis. Arch Gen Psychiatry 1993;
I do not agree with the view that the the classical analytic approach. What re- 50:306-317
treatment of choice for a patient with mains to be seen is whether for patients 12. Hollander E, Simeon D, Gorman J: Anxiety
very severe panic disorder with ago- disorders, in American Psychiatric Press Text-
panic is necessarily medication or cogni- with
book of Psychiatry, 2nd ed. Edited by Hales
tive behavioral therapy. This was a pa- raphobia, a short-term psychodynamic RE, Yudofsky SC, Talbott SA. Washington,
tient with panic in the context of some approach without medication is going to DC, American Psychiatric Press, 1994, pp
degree of personality dysfunction, al- be effective. Part of the reason medica- 495-564
though in my experience many panic pa- tions became popular is that traditional 13. Johnson J, Weissman MM, Klerman GL:
Panic disorder, comorhidity, and suicide at-
tients have characterological underpin- psychodynamic therapy for patients with tempts. Arch Gen Psychiatry 1990; 47:805-
nings that affect the development of their severe, apparently autonomous, panic 808
panic. Ms. A’s symptoms responded rap- disorder was not that successful. Part of 14. Busch FN, Cooper AM, Klerman GL, Penzer
idly to psychodynamic psychotherapy. the refinement of determining which ap- RJ, Shapiro T, Shear MK: Neurophysiologi-
cal, cognitive-behavioral, and psychoanalytic
Medication management of panic disor- proaches are going to prove to be suitable approaches to panic disorder: toward an inte-
der also takes several weeks to be effec- will likely be connected with better iden- gration. Psychoanal Inquiry 1991; 11:316-
tive. Many psychoanalysts and psy- tification ofwhich diagnostic conditions, 332
chodynamic psychiatrists have observed 15. Shear MK, Cooper AM, Klerman GL, Busch
as well as other patient characteristics,
EN, Shapiro T: A psychodynamic model of
rapid symptomatic response of patients make a specific patient more or less ame- panic disorder. Am J Psychiatry 1993; 150:
with panic disorder to psychodynamic nable to a successful outcome with dif- 859-866
psychotherapy ( 1 , 2, 18). ferent therapeutic interventions. There 1 6. Busch FN, Shear MK, Cooper AM, Shapiro T,
Certain personality characteristics of are fewer data on differential treatment Leon AC: An empirical study of defense
mechanisms mn panic disorder. J Nerv Ment
this patient made her a good candidate than we would like. Dis 1995; 183:299-303
for psychodynamic psychotherapy. 17. Yehuda R, SchmeidlenJ, Elkin A, Houshmand
From our first meeting, she demonstrated E, Siever L, Binder-Brynes K, Wainberg M,
a tremendous curiosity about herself, Aferiat D, Lehman A, Guo LS, Yang RK:
REFERENCES
Phenomenology and psychobiology of the
and she was motivated to understand intergenerational response to trauma, in In-
herself. She thought about things that 1 . Milnod B, Shear MK: Psychodynamic treat- ternational Handbook of Multigenerational
were said in treatment and made connec- ment of panic: three case histories. Hosp Legacies (if Trauma. Edited by Danelli Y.
tions. She explored historical details as Community Psychiatry 1991; 42:31 1-3 12 New York, Plenum (in press)
2. Milrod B, Shear MK: Dynamic treatment of 1 8. Milrod B: The continued usefulness of psy-
they emerged. She was a bright, verbal
panic disorder: a review. J Nerv Ment Dis choanalysis in the treatment armamentarium
woman who was able to put complicated 1991; 179:741-743 for panic disorder. J Am Psychoanal Assoc
feelings into words. She was psychologi- 3. Nutt I), lawson C: Panmc attacks: a neuno- 1995; 43:151-1 62
Am ] Psychiatry 153:5, May 1996 703
You might also like
- BrochureDocument2 pagesBrochureapi-375895852No ratings yet
- Internal Medicine Progress Note TemplateDocument2 pagesInternal Medicine Progress Note Templatehector100% (1)
- Development of A Tool To Assess Suicide Potential Among Filipino YouthDocument34 pagesDevelopment of A Tool To Assess Suicide Potential Among Filipino YouthMaria Theresa Deluna Macairan100% (1)
- CASE 7 Somatic Symptom DisorderDocument11 pagesCASE 7 Somatic Symptom DisorderApril AstilloNo ratings yet
- The Sentence Completion Test SSCT Rating Sheet: Stand Up For Himself Instead of Just Saying "Yes" To My Mother AlwaysDocument6 pagesThe Sentence Completion Test SSCT Rating Sheet: Stand Up For Himself Instead of Just Saying "Yes" To My Mother AlwaysRonald Bartolome0% (1)
- Case Presentation 3Document4 pagesCase Presentation 3api-285918237No ratings yet
- Case PresentationDocument33 pagesCase PresentationPratima ThakurNo ratings yet
- Allport's Theory of PersonalityDocument13 pagesAllport's Theory of PersonalityNiharika SpencerNo ratings yet
- Unit 3 The Thematic Apperception Test and Children S Pperception T TDocument16 pagesUnit 3 The Thematic Apperception Test and Children S Pperception T TAhmad Sameer AlamNo ratings yet
- Case Study Prac RevisedDocument13 pagesCase Study Prac Revised20172428 YASHICA GEHLOT100% (1)
- SAMPLE Outline PanicDocument3 pagesSAMPLE Outline PanicdexNo ratings yet
- Expectation From CounsellorsDocument27 pagesExpectation From CounsellorsAkriti SrivastavaNo ratings yet
- Psychology 3E: Saundra K. Ciccarelli, J. Noland WhiteDocument40 pagesPsychology 3E: Saundra K. Ciccarelli, J. Noland WhiteJansen WongNo ratings yet
- Delmundo 2019 - FinalDocument9 pagesDelmundo 2019 - FinalCall me PinguNo ratings yet
- TatDocument4 pagesTatlove148No ratings yet
- A Case Study of A Patient Suffering From Major Depressive DisorderDocument5 pagesA Case Study of A Patient Suffering From Major Depressive Disorderdennis ndegeNo ratings yet
- Karen Horney: Psychoanalytic Social TheoryDocument10 pagesKaren Horney: Psychoanalytic Social TheoryGabriel Lance Ivan ManaitNo ratings yet
- 2nd Testing of The Mentally Retarded PopulationDocument20 pages2nd Testing of The Mentally Retarded PopulationHoorya HashmiNo ratings yet
- Case Study of Social PhobiaDocument1 pageCase Study of Social PhobiaSarah KhairinaNo ratings yet
- Sullivan's Interpersonal TheoryDocument12 pagesSullivan's Interpersonal TheorySumam NeveenNo ratings yet
- SSCTDocument13 pagesSSCTMeharNo ratings yet
- Contemporary PsychologyDocument4 pagesContemporary PsychologyZunair IlyasNo ratings yet
- Aiss Write UpDocument4 pagesAiss Write UpDNo ratings yet
- MA in Psychology - Clinical Psychology (Thesis) .FEUDocument1 pageMA in Psychology - Clinical Psychology (Thesis) .FEUPaul Anthony PascualNo ratings yet
- Chapter 2 Barlow and DurandDocument18 pagesChapter 2 Barlow and DurandSharemax Holdings, Inc.No ratings yet
- Aiman 019309 Peace Psychologyassignment 1Document8 pagesAiman 019309 Peace Psychologyassignment 1Fatima MalikNo ratings yet
- MCQ Questions in Psychology: Described by Adler As HavingDocument7 pagesMCQ Questions in Psychology: Described by Adler As HavingDana AhmedNo ratings yet
- Rotter and MischellDocument3 pagesRotter and MischellangeluNo ratings yet
- Marie Jahoda: Current Concepts of Positive Mental HealthDocument32 pagesMarie Jahoda: Current Concepts of Positive Mental Healthrewv vhiNo ratings yet
- DPC Field Report CompletedDocument36 pagesDPC Field Report Completedraman_bhoomi9910No ratings yet
- Case ReportDocument16 pagesCase ReportSabbir ThePsychoExpressNo ratings yet
- Lived Experiences of Mental Health Service Frontliners Amidst The COVID-19 PandemicDocument14 pagesLived Experiences of Mental Health Service Frontliners Amidst The COVID-19 PandemicPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Psychodynamic and Behavioural Approach To Rehabilitation CounsellingDocument32 pagesPsychodynamic and Behavioural Approach To Rehabilitation CounsellingphakeynishaNo ratings yet
- A Case of Social PhobiaDocument3 pagesA Case of Social PhobiaFaRaz MemOnNo ratings yet
- Psych Case StudyDocument11 pagesPsych Case Studyapi-546513658No ratings yet
- Unit V Personality PDFDocument15 pagesUnit V Personality PDFOmprakash SwamiNo ratings yet
- Stress and Coping NotesDocument10 pagesStress and Coping Notesrashi100% (1)
- Harry SullivanDocument17 pagesHarry SullivanStephanie Joy Escala100% (1)
- Harry Stack SullivanDocument4 pagesHarry Stack SullivanMichal Gail100% (2)
- 1.4 Personality DisordersDocument11 pages1.4 Personality DisordersDomalaon, Princess Sophia B.No ratings yet
- Practical-2 - Eysenck's Personality QuestionnaireDocument18 pagesPractical-2 - Eysenck's Personality QuestionnairegitikaNo ratings yet
- Thematic Apperception TestDocument4 pagesThematic Apperception TestSahil MushafNo ratings yet
- Anxiety Case StudyDocument3 pagesAnxiety Case StudyJennaNo ratings yet
- Psych Assessment Chapter 12Document5 pagesPsych Assessment Chapter 12Marjorie VillarosaNo ratings yet
- Personality Disorders Lesson PlanDocument17 pagesPersonality Disorders Lesson Planapi-284104206No ratings yet
- Mood Disorders - DepressionDocument58 pagesMood Disorders - Depressionmaha abdallahNo ratings yet
- Unit 5 Family InfluencesDocument25 pagesUnit 5 Family Influencesshubhii1997No ratings yet
- I. Overview of Cognitive Social Learning TheoryDocument4 pagesI. Overview of Cognitive Social Learning TheorynitinandsubahNo ratings yet
- Case Study - Mental Status ExaminationDocument5 pagesCase Study - Mental Status ExaminationSrivathsanNo ratings yet
- Physical and Mental AssessmentDocument3 pagesPhysical and Mental AssessmentAlexis FurtonNo ratings yet
- Transpersonal Psychology in The BhagavadDocument9 pagesTranspersonal Psychology in The BhagavadNavneet DhimanNo ratings yet
- Personality DisordersDocument35 pagesPersonality DisordersMonika JosephNo ratings yet
- Clinical Psychology R's Case RecordDocument22 pagesClinical Psychology R's Case RecordSwati Tiwari Life CoachNo ratings yet
- Personality DisordersDocument4 pagesPersonality DisordersAngela Abigail AbingNo ratings yet
- Case AnalysisDocument29 pagesCase AnalysisSuji.TNo ratings yet
- Chapter 6 Somatic-Symptom-and-Related-Disorders-and-Dissociative-DisordersDocument3 pagesChapter 6 Somatic-Symptom-and-Related-Disorders-and-Dissociative-DisordersAnnie SumacotNo ratings yet
- Existential Psychotherapy (Logotherapy) : Bes3148 Theories of Personality Viktor FranklDocument4 pagesExistential Psychotherapy (Logotherapy) : Bes3148 Theories of Personality Viktor FranklNarona MaurenNo ratings yet
- Assignment # 3, Group 4, Clinical Psychology IIDocument9 pagesAssignment # 3, Group 4, Clinical Psychology IIFatima MalikNo ratings yet
- Kinetic Family and Human Figure Drawings of Child and AdolescentDocument310 pagesKinetic Family and Human Figure Drawings of Child and AdolescentBotoi Tabita-LoisNo ratings yet
- Case Analysis EtiologyDocument2 pagesCase Analysis EtiologyKaren LerioNo ratings yet
- Scientific American Mind November/December 2009Document8 pagesScientific American Mind November/December 2009AprilMartelNo ratings yet
- General Internal Medicine In-Training ObjectivesDocument18 pagesGeneral Internal Medicine In-Training ObjectiveshectorNo ratings yet
- Endocrinology In-Training ObjectivesDocument12 pagesEndocrinology In-Training ObjectiveshectorNo ratings yet
- Surviving Sepsis Campaign Hour 1 Bundle 220414 142741Document5 pagesSurviving Sepsis Campaign Hour 1 Bundle 220414 142741hectorNo ratings yet
- Episode ListDocument25 pagesEpisode ListhectorNo ratings yet
- Metabolism With Triphasic Oral Contraceptive Formulations Containing Norgestimate or LevonorgestrelDocument6 pagesMetabolism With Triphasic Oral Contraceptive Formulations Containing Norgestimate or LevonorgestrelhectorNo ratings yet
- U.S. Selected Practice Recommendations For Contraceptive Use, 2016 MMWRDocument60 pagesU.S. Selected Practice Recommendations For Contraceptive Use, 2016 MMWRhectorNo ratings yet
- 60 Affirmations For PeaceDocument21 pages60 Affirmations For PeacehectorNo ratings yet
- Gauthier 1992Document6 pagesGauthier 1992hectorNo ratings yet
- Blood Pressure Log 02Document1 pageBlood Pressure Log 02hectorNo ratings yet
- Clinical Reasoning Guide FormDocument3 pagesClinical Reasoning Guide FormhectorNo ratings yet
- Glasgow Coma Scale (With Explanations)Document1 pageGlasgow Coma Scale (With Explanations)hectorNo ratings yet
- A Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfilesDocument4 pagesA Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfileshectorNo ratings yet
- 050 Bonus GratitudeDocument9 pages050 Bonus GratitudehectorNo ratings yet
- ACGMECLERNational Report Findings 2019Document132 pagesACGMECLERNational Report Findings 2019hectorNo ratings yet
- The AOA Guide:: How To Succeed in The Third-Year ClerkshipsDocument25 pagesThe AOA Guide:: How To Succeed in The Third-Year Clerkshipshector100% (1)
- Assignments Report: Saved ProgramsDocument16 pagesAssignments Report: Saved ProgramshectorNo ratings yet
- 060 Bonus LawOfCauseAndEffectDocument1 page060 Bonus LawOfCauseAndEffecthectorNo ratings yet
- SketchyIM Check List PDFDocument5 pagesSketchyIM Check List PDFhectorNo ratings yet
- Purpose, V Purpose, V Purpose, V Purpose, V Purpose, Vision, Ision, Ision, Ision, Ision, Goals Goals Goals Goals GoalsDocument9 pagesPurpose, V Purpose, V Purpose, V Purpose, V Purpose, Vision, Ision, Ision, Ision, Ision, Goals Goals Goals Goals GoalshectorNo ratings yet
- Fibromyalgia: Basic InformationDocument5 pagesFibromyalgia: Basic InformationhectorNo ratings yet
- The Law of Gender: Be Patient! All Ideas Move Into Form in The Right TimeDocument1 pageThe Law of Gender: Be Patient! All Ideas Move Into Form in The Right TimehectorNo ratings yet
- 056 Bonus RelativityDocument1 page056 Bonus RelativityhectorNo ratings yet
- 008 ASereneMind PDFDocument2 pages008 ASereneMind PDFhectorNo ratings yet