Professional Documents
Culture Documents
NCP Acute Pain
NCP Acute Pain
Uploaded by
Dyanne BOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Acute Pain
NCP Acute Pain
Uploaded by
Dyanne BCopyright:
Available Formats
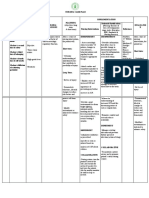
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
S: “mejo Acute Pain Report pain is 1. Document location 1. Aids in evaluating After 12 hours of
kumikirot kirot relieved or and intensity of pain need for and nursing
yung sugat controlled. (scale of 0–10). effectiveness of intervention, goal
ko” Appear relaxed 2. Investigate changes interventions.
and able to rest in pain 2. Changes may was met as
O: Amputated and sleep characteristics— indicate developing manifested by:
left leg appropriately. numbness and complications,
Verbalize tingling. such as necrosis or Patient reports pain
understanding 3. Elevate affected infection. is relieved and
Restless controlled.
of phantom part by raising foot
pain and of bed slightly or 3. Lessens edema
(+) Facial Grimace methods to using a pillow or formation by Patient is relaxed
provide relief. sling for upper-limb enhancing venous and able to rest and
BP = 140 / amputation. return; reduces sleep appropriately.
70mmHg muscle fatigue and
skin or tissue Patient is able to
Pulse:110 bpm 4. Provide or promote pressure. Note: verbalizes the
general comfort After initial 24 understanding of
measures (e.g., hours and in phantom pain and
frequent turn- ing, absence of edema, methods to provide
back rub) and residual limb may relief.
diversional be extended and
activities. kept flat.
Encourage use of
stress management 4. Refocuses
techniques, such as attention, promotes
deep-breathing relaxation, may
exer- cises, enhance coping
visualization and abilities, and may
guided imagery, decrease
and Therapeutic occurrence of
Touch. phantom-limb pain.
5. Investigate reports 5. May indicate
of progressive or developing
poorly localized compartment
pain unrelieved by syndrome,
analgesics. especially following
traumatic injury.
6. Acknowledge reality (Refer to CP:
of residual limb pain Fractures; ND: risk
and phantom pain for Peripheral
and that various Neurovascular
modalities will be Dysfunction.)
tried for pain relief.
6. Residual limb pain
is believed to come
from injuries to
nerves at the
amputation site. At
the ends of these
injured nerve fi
neuromas send out
pain impulses in a
random fashion, or
when trapped as in
7. Collaborative excessive
Administer compression by
medications, as other tissues such
indicated, such as as muscle, or in
the following: the development of
the infectious
Opioid analgesics, process. In
for example, contrast, phantom
morphine sulfate pain is thought to
(Astramorph, MS originate in the part
Contin), Fentanyl of the brain that
patch; combination controlled the limb
agents: oxycodone before it was
with acetaminophen amputated. So the
(Percocet); and client experiences
anti-inflammatory pain and sensation
agents, for as if the limb were
example, still in place.
acetaminophen
(Tylenol) and 7. Phantom pain is
ibuprofen (Motrin) often described as
Antidepressants, for crushing, grinding,
example, or burning. It can
amitriptyline (Elavil), occur immediately
nortripty- line or may not start for
(Pamelor), and several weeks.
duloxetine Note: Phantom
(Cymbalta); pain is not well
antiseizure drugs, relieved by
for example, traditional pain
carbamazepine medications.
(Tegretol),
gabapentin
(Neurontin), and 8. Many medications
pregabalin (Lyrica); and routes of
sedatives/anti- administration may
anxiety agents, for be used.
example, diazepam In acute postamputation
(Valium) and pain, opioid analgesics are
alprazolam (Xanax); the mainstay of pain
and local/regional management to reduce
anesthetics, for pain and muscle spasms.
example, nova-
caine (Marcaine) 9. As surgical pain
and ropivacaine subsides, other
(Naropin) medications will be
added to manage
8. Instruct in, and more long-term
monitor use of, conditions; for
patient-controlled example,
analgesia (PCA). antidepressants
and antiseizure
9. Refer to medications
interdisciplinary appear to help with
providers as neurotic pain
appropriate—pain associated with
management phantom pain and
specialist, physical sensations.
therapist,
prosthetist,
orthopedic surgeon,
and neurosurgeon. 10. PCA provides for
10. Discuss and continuous and
monitor use of timely drug
transcutaneous administration,
electrical nerve preventing
stimulation (TENS) fluctuations in pain
of the residual limb. level and muscle
tension and
spasms associated
with surgical
procedures.
11. A multidisciplinary
approach is
required, and many
therapy modalities
may be needed
both in the acute
and the long-term
management of
pain.
For some
individuals, a
TENS unit may
help to treat
retractable
phantom limb pain,
especially in
combination with
medica- tions for
neuropathic pain.
Note: Stimulation
of the intact
(opposite) limb is
often more
effective. Indeed,
an increase in
phantom pain has
occassionally been
reported when
TENS unit has
been applied to
residual limb.
You might also like
- Spinal Injury Nursing Care PlanDocument2 pagesSpinal Injury Nursing Care PlanPatricia OrtegaNo ratings yet
- Patriarca, Janna Mae H. Nursing Care Plan Client: Mr. YingDocument1 pagePatriarca, Janna Mae H. Nursing Care Plan Client: Mr. Yingjanna mae patriarca100% (2)
- Spinal Cord Injury NCPDocument2 pagesSpinal Cord Injury NCPEmmanuelRodriguez100% (1)
- Pantoprazole DrugDocument1 pagePantoprazole Drugman12No ratings yet
- NCPDocument2 pagesNCPsphinx809100% (2)
- Pre-Operative (Incision & Drainage of Abscess)Document6 pagesPre-Operative (Incision & Drainage of Abscess)Eunice MañalacNo ratings yet
- Vergara, Valerie G. Drug Study (Ma'Am Dean)Document3 pagesVergara, Valerie G. Drug Study (Ma'Am Dean)Valerie VergaraNo ratings yet
- Drug Classification Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationsDocument2 pagesDrug Classification Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationsFranz Earl Niño AlbesaNo ratings yet
- Drug Study Vit B ComplexDocument2 pagesDrug Study Vit B Complexbekbekk cabahugNo ratings yet
- CHAPTER 5 Nursing Care PlanDocument5 pagesCHAPTER 5 Nursing Care PlanMiguelito Galagar GultianoNo ratings yet
- NURSING CARE PLAN Problem Body Weakness Nursing Diagnosis Impaired PhysicalDocument1 pageNURSING CARE PLAN Problem Body Weakness Nursing Diagnosis Impaired Physicalmitchie riveraNo ratings yet
- Activity IntoleranceDocument2 pagesActivity IntoleranceSenyorita KHaye100% (4)
- Oraa, Jamie - Drug Study Surgical WardDocument1 pageOraa, Jamie - Drug Study Surgical WardJamie LeeNo ratings yet
- J.Paquit NCP ECCEDocument7 pagesJ.Paquit NCP ECCEJon Gab Paquit100% (1)
- TramadolDocument1 pageTramadolAi RouNo ratings yet
- Activity IntoleranceDocument2 pagesActivity IntolerancedohbleNo ratings yet
- BiperidenDocument1 pageBiperidenMFQ.RN100% (2)
- NCP For Ruptured AppendicitisDocument2 pagesNCP For Ruptured AppendicitisJansen Arquilita RiveraNo ratings yet
- NCPDocument1 pageNCPJ. ishtelleNo ratings yet
- Learning Guide: Ngeles Niversity OundationDocument9 pagesLearning Guide: Ngeles Niversity OundationNYCA GRACIA TUAZONNo ratings yet
- NCP Epidural HemDocument32 pagesNCP Epidural HemKatrina PonceNo ratings yet
- NCP Pot Riskforinjury EncephalitisDocument3 pagesNCP Pot Riskforinjury Encephalitisaila angNo ratings yet
- Nursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale EvaluationDocument1 pageNursing Care Plan: Cues Problem Scientific Reason Nursing Intervention Rationale Evaluationeihjay-bravo-8041No ratings yet
- Rena LogDocument1 pageRena LogRhika Mae Flores Valdez0% (1)
- NCP - OsteosarcomaDocument5 pagesNCP - OsteosarcomaNelson Lacsamana100% (1)
- NCP Liver CirrosisDocument2 pagesNCP Liver CirrosisRosebud RoseNo ratings yet
- Cad NCPDocument1 pageCad NCPKrizzia Mae F. MayoresNo ratings yet
- NCP Acute Pain RT CancerDocument3 pagesNCP Acute Pain RT CancerCharissa Magistrado De LeonNo ratings yet
- Nursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationDocument1 pageNursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationJaylord Verazon100% (1)
- Drug Study For FractureDocument4 pagesDrug Study For FractureitsmeayaNo ratings yet
- Atropine SulfateDocument1 pageAtropine SulfateTrishaaMayolNo ratings yet
- Drug Study Stugeron and Kalium DuruleDocument1 pageDrug Study Stugeron and Kalium DuruleawesomedawnNo ratings yet
- NCP - Acute Pain Related To EdemaDocument2 pagesNCP - Acute Pain Related To EdemaChenime Añana0% (1)
- NCP LocDocument2 pagesNCP LocMel RodolfoNo ratings yet
- NCP Myoma 2003Document2 pagesNCP Myoma 2003grace ecм мendozaNo ratings yet
- Impaired MobilityDocument3 pagesImpaired MobilityYeana AlonNo ratings yet
- FATIGUE NCP Que Fransis A.Document4 pagesFATIGUE NCP Que Fransis A.Irene Grace BalcuevaNo ratings yet
- NCP Total Hip ReplacementDocument11 pagesNCP Total Hip ReplacementDoneva Lyn MedinaNo ratings yet
- Nursing Care Plan SeizureDocument2 pagesNursing Care Plan Seizuretimie_reyes100% (1)
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- Calcium Gluconate Drug StudyDocument4 pagesCalcium Gluconate Drug StudyAngelou Joefred CongresoNo ratings yet
- Drug StudyDocument1 pageDrug StudySheryll Anne MolartoNo ratings yet
- Nahco3 Vancomycin AmlodipineDocument3 pagesNahco3 Vancomycin AmlodipineShan Dave TupasNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway ClearancePatrick Arvin Ballesteros BarcarseNo ratings yet
- Solu CortefDocument1 pageSolu CortefKristine YoungNo ratings yet
- Drug Study RopivacaineDocument2 pagesDrug Study Ropivacainerica sebabillonesNo ratings yet
- Nursing Care Plan NCP Group 3 Fatigue ..Document2 pagesNursing Care Plan NCP Group 3 Fatigue ..Aerron Severus Secano ShuldbergNo ratings yet
- System Normal Abnormal Remarks Vital SignsDocument3 pagesSystem Normal Abnormal Remarks Vital SignsJM RomiasNo ratings yet
- Brand Name: Diamicron Generic Name: Gliclazide Indication: For Non-Insulin DependentDocument2 pagesBrand Name: Diamicron Generic Name: Gliclazide Indication: For Non-Insulin DependentianecunarNo ratings yet
- Drug Study Drug Name Mechanism of Action Dosage Indication Contraindication Side Effects Nursing InterventionsDocument5 pagesDrug Study Drug Name Mechanism of Action Dosage Indication Contraindication Side Effects Nursing InterventionsYvonne AgathaNo ratings yet
- Drug StudyDocument4 pagesDrug StudyPam RomeroNo ratings yet
- Therabloc DrugDocument2 pagesTherabloc DrugMsOrangeNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- Grand Case NP 2 Laparoscopic CholecystectomyDocument10 pagesGrand Case NP 2 Laparoscopic CholecystectomyFarida Paula R. SevillaNo ratings yet
- Ncp. Acute PainDocument4 pagesNcp. Acute PainNathalie SamonteNo ratings yet
- Assessments Nursing Diagnosis Planning Interventions Rationale EvaluationDocument12 pagesAssessments Nursing Diagnosis Planning Interventions Rationale EvaluationAsniah Hadjiadatu AbdullahNo ratings yet
- Sabalo NCP 1Document2 pagesSabalo NCP 1baby_doll05062003No ratings yet
- Nursing Care Plan: Cues Nursing Diagnosis Pathophysiology Obje Ctive Expected Outcome Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Cues Nursing Diagnosis Pathophysiology Obje Ctive Expected Outcome Interventions Rationale EvaluationBuhkz Hermoso100% (1)
- Carry Out The Doctor's Order (E.g. Kardex, Meds Chart, Tickets)Document8 pagesCarry Out The Doctor's Order (E.g. Kardex, Meds Chart, Tickets)Yosef OxinioNo ratings yet
- Nursing Care Plan Mrs. Patao Ob Ward, GSGH Assessment SubjectiveDocument3 pagesNursing Care Plan Mrs. Patao Ob Ward, GSGH Assessment Subjectiveraizelc100% (2)