Professional Documents
Culture Documents
Recent Developmental in Biology Repair
Recent Developmental in Biology Repair
Uploaded by
Aby SuryaCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Injury: Ianiv Klaber, Pablo Besa, Felipe Sandoval, Daniel Lobos, Tomas Zamora, Daniel Schweitzer, Julio UrrutiaDocument4 pagesInjury: Ianiv Klaber, Pablo Besa, Felipe Sandoval, Daniel Lobos, Tomas Zamora, Daniel Schweitzer, Julio UrrutiaAby SuryaNo ratings yet
- Rotator Cuff Syndrome: October 2018Document16 pagesRotator Cuff Syndrome: October 2018Aby SuryaNo ratings yet
- Kulkarni2012 PDFDocument7 pagesKulkarni2012 PDFAby SuryaNo ratings yet
- Posterior Knee Dislocation: I I e MDocument2 pagesPosterior Knee Dislocation: I I e MAby SuryaNo ratings yet
- FFFFDocument4 pagesFFFFAby SuryaNo ratings yet
- Wjem 11 103 PDFDocument2 pagesWjem 11 103 PDFAby SuryaNo ratings yet
- Pneumothorax: An Update: ReviewDocument5 pagesPneumothorax: An Update: ReviewAby SuryaNo ratings yet
- Jurnal AutismDocument10 pagesJurnal AutismAby SuryaNo ratings yet
- P-342 Poster: Abstracts of The 25th Annual Meeting of ESHRE, Amsterdam, The Netherlands, 28 June - 1 July, 2009Document1 pageP-342 Poster: Abstracts of The 25th Annual Meeting of ESHRE, Amsterdam, The Netherlands, 28 June - 1 July, 2009Aby SuryaNo ratings yet
- Otolaryngology - Head and Neck Surgery: Clinical Practice Guideline: Acute Otitis ExternaDocument21 pagesOtolaryngology - Head and Neck Surgery: Clinical Practice Guideline: Acute Otitis ExternaAby SuryaNo ratings yet
- Richard W. Titball, E. Diane Williamson.2007.: WWW - Cdc.gov/ncidod/dvbid/plague/index - HTMDocument1 pageRichard W. Titball, E. Diane Williamson.2007.: WWW - Cdc.gov/ncidod/dvbid/plague/index - HTMAby SuryaNo ratings yet
- Acute Otitis Externa in Children: Child Health UpdateDocument3 pagesAcute Otitis Externa in Children: Child Health UpdateAby SuryaNo ratings yet
- Principles of Bone GraftingDocument6 pagesPrinciples of Bone GraftingJayanth Perumal100% (2)
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
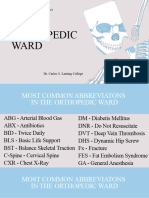
- Orthopedic-Ward-Abbrev CC FX NI-Lecture 20230830Document30 pagesOrthopedic-Ward-Abbrev CC FX NI-Lecture 20230830Yong VillafriaNo ratings yet
- Internal & External Fixation-NEWDocument23 pagesInternal & External Fixation-NEWaeruginoNo ratings yet
- ORP - Handout - English - Principles of Fracture Fixation - v2Document11 pagesORP - Handout - English - Principles of Fracture Fixation - v2Mohamad RamadanNo ratings yet
- Stages in The Healing of A Bone FractureDocument10 pagesStages in The Healing of A Bone FractureMagdalena PranataNo ratings yet
- Fracture Mandible PDFDocument120 pagesFracture Mandible PDFMorohai DoinaNo ratings yet
- Reviews: Fracture Healing: Mechanisms and InterventionsDocument10 pagesReviews: Fracture Healing: Mechanisms and InterventionsFatrika DewiNo ratings yet
- Orthopedic Hardware in Trauma - A Guided Tour For The Radiologist - Part 1Document15 pagesOrthopedic Hardware in Trauma - A Guided Tour For The Radiologist - Part 1Marcia MejíaNo ratings yet
- K. Adwar. Internal Fixation of #S.Document32 pagesK. Adwar. Internal Fixation of #S.Fathy AlhallagNo ratings yet
- DR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiDocument34 pagesDR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiAnjani Kumar JhaNo ratings yet
- Fracture HealingDocument23 pagesFracture Healingjomari dvNo ratings yet
- 1.1 Biology of Bone HealingDocument32 pages1.1 Biology of Bone HealingCristian CumpănăNo ratings yet
- Outline of Fracture Management & ComplicationDocument24 pagesOutline of Fracture Management & Complicationmsarwar100% (1)
- FractureDocument125 pagesFractureKlara Devina VanessaNo ratings yet
- Orthopedic Nursing CareDocument41 pagesOrthopedic Nursing CareIrfan Ners MaulanaNo ratings yet
- 19 Musculoskeletal System DR - FallerDocument27 pages19 Musculoskeletal System DR - FallerFranz Earl Niño AlbesaNo ratings yet
- Surgery (Ortho) NotesDocument155 pagesSurgery (Ortho) NotesprestigeuniversaltradingNo ratings yet
- Dsem TRM 0714 0109 3 - LRDocument88 pagesDsem TRM 0714 0109 3 - LRbagus lazuardiNo ratings yet
- Collagen and Hydroxyapatite Scaffolds Activate DisDocument15 pagesCollagen and Hydroxyapatite Scaffolds Activate DisIsworo RukmiNo ratings yet
- Paper 3 Surgery Not Answered Till 2022Document288 pagesPaper 3 Surgery Not Answered Till 2022NEMO2322No ratings yet
- (Download PDF) Fracture Management For Primary Care Updated Edition M Patrice Eiff Online Ebook All Chapter PDFDocument42 pages(Download PDF) Fracture Management For Primary Care Updated Edition M Patrice Eiff Online Ebook All Chapter PDFfreddie.branson694100% (13)
- Fracture Healing SsDocument2 pagesFracture Healing SsIndra SyafaatNo ratings yet
- Cutaneous Wound HealingDocument78 pagesCutaneous Wound HealingClaudio Luis VenturiniNo ratings yet
- Fracture Reduction and FixationDocument271 pagesFracture Reduction and FixationJAMPIER MORERANo ratings yet
- 1 Principles of Internal Fixation: 1.1.1 Mechanical Properties of BoneDocument29 pages1 Principles of Internal Fixation: 1.1.1 Mechanical Properties of BoneCarlos CalderonNo ratings yet
- AO Basic 2015 Relative StabilityDocument23 pagesAO Basic 2015 Relative StabilitySolidet VasimNo ratings yet
- Case Study GROUP 10Document22 pagesCase Study GROUP 10CreativeWorldwideNo ratings yet
- Management of Mandible FracturesDocument52 pagesManagement of Mandible FracturesAndykaYayanSetiawanNo ratings yet
- Robbins 7th Ed - Chapter 3 - Tissue Renewal & Repair (2) Flashcards by Heli Sinnpson - BrainscapeDocument12 pagesRobbins 7th Ed - Chapter 3 - Tissue Renewal & Repair (2) Flashcards by Heli Sinnpson - BrainscapeCarlos MaingeNo ratings yet
Recent Developmental in Biology Repair
Recent Developmental in Biology Repair
Uploaded by
Aby SuryaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Recent Developmental in Biology Repair
Recent Developmental in Biology Repair
Uploaded by
Aby SuryaCopyright:
Available Formats
Perspectives on Modern Orthopaedics
Recent Developments in the
Biology of Fracture Repair
Francois N. K. Kwong, MD Abstract
Mitchel B. Harris, MD Fracture repair is dependent on local and systemic molecular and
cellular processes. During fracture repair, mesenchymal stem cells
are systemically recruited to the fracture site, and cytokines are
released from the fracture site into the vascular system. In a
significant minority of fractures, healing delays result from adverse
clinical factors that interfere with these processes. Extrinsic
factors, such as aging and smoking, adversely affect the molecular
and cellular processes occurring locally in the fracture site.
Fracture fixation affects healing through local changes in the
biologic signaling within the fracture callus. Current biologic
treatment of fractures includes the local application of
Perspectives on Modern Orthopaedics osteoinductive bone morphogenetic proteins (ie, BMP-2, BMP-7)
articles provide an objective appraisal of and cell-based therapies. Although clinical results with bone
new or controversial techniques or areas
morphogenetic proteins have been satisfactory, they have not been
of investigation in orthopaedic surgery.
as impressive as those reported in animal studies. Further
Dr. Kwong is Research Fellow, Center understanding of the biology of fracture repair may lead to
for Molecular Orthopaedics, Brigham
improved treatment modalities.
and Women’s Hospital, Harvard Medical
School, Boston, MA. Dr. Harris is
F
Associate Professor of Orthopaedic racture healing is a highly effi- Fracture healing may be seen as
Surgery, Harvard Medical School, and cient repair process resulting in both a local and a systemic process
Chief, Orthopaedic Trauma Service, newly formed bone, similar in qual- (Figures 1 and 2). There are local mo-
Brigham and Women’s Hospital, ity to the original tissue. However, lecular and cellular signaling path-
Partners Orthopaedic Trauma Service,
in a small but significant number of ways, and evidence is emerging of
Boston, MA.
instances, adverse conditions impair the systemic recruitment of mesen-
None of the following authors or a this process, causing significant chymal stem cells (MSCs) to the
member of their immediate families has morbidity. Because fractures are fracture site. Extrinsic factors, such
received anything of value from or owns common in the general population, as drugs and aging, influence local
stock in a commercial company or delayed healing and nonunion are processes to alter the outcome of
institution related directly or indirectly to significant health care issues. Thus, fractures, while the biomechanics of
the subject of this article: Dr. Kwong and there remains a need to develop fracture fixation affect the biology of
Dr. Harris. treatment methods that enhance fracture healing.
Reprint requests: Dr. Kwong, Center for
fracture healing and improve out-
Molecular Orthopaedics, Room BLI comes.
Pathophysiology of
044, 221 Longwood Avenue, Boston, Biologic methods of bone regener-
Delayed Fracture
MA 02115. ation will continue to have an in-
Healing and Nonunion
creasing role in the treatment of
J Am Acad Orthop Surg 2008;16:619- fractures. To further develop these Bone regeneration depends on three
625 methods, knowledge of the patho- essential elements: progenitor cells,
Copyright 2008 by the American logic changes in the fracture repair growth factors (osteoinduction), and
Academy of Orthopaedic Surgeons. process that lead to delayed union or the appropriate milieu (osteoconduc-
nonunion is important. tion). Delayed fracture repair and
Volume 16, Number 11, November 2008 619
Recent Developments in the Biology of Fracture Repair
Figure 1 nonunion can result from a lack of to the fracture site and/or by affect-
osteoprogenitor cells, insufficient ing the local osteoinductive signals.
osteoinductive growth factors, or a Nonunions are commonly classi-
defective milieu, or, more common- fied on radiographs as hypertrophic
ly, a combination of these factors. or atrophic. Hypotrophic nonunion
Disease or other adverse factors may is generally thought to be the result
delay fracture healing by affecting of mechanical instability and is
one or more of these elements. treated by restoring stability, usu-
For example, a critical-sized bone ally by skeletal fixation. Atrophic
defect (ie, one that does not heal nonunion is thought to result from
spontaneously because of its size) biologic causes, principally poor vas-
would result in the absence of hu- cularization, and is treated by resto-
man MSCs (hMSCs) within the de- ration of the osteogenic potential,
fect, a lack of osteoinductive signals, with resection of fibrous tissue and
and a milieu that is nonconducive to bone grafting or some other method
healing. Excess motion at the frac- of osteoinduction. Both groups of
ture site impairs both the molecular nonunion contain fibrous tissue, fi-
and cellular processes within the de- brocartilage, and adipose tissue,
fect. Hypoxia affects osteogenic dif- which are not normally present in
ferentiation of hMSCs by reducing healing fractures.2 The hypertrophic
the number of viable cells and alter- group also has hyaline cartilage and
ing the molecular signals pro- bone in varying proportions.
Illustration demonstrating molecular duced.1 Blood supply is important to
signaling. Fracture repair depends on fracture repair as blood provides nu-
molecular processes occurring both
Local Molecular
trients and oxygen for cell survival,
locally and systemically. BMPs = bone Signaling
and blood vessels are the route for
morphogenetic proteins, IGF-1 = inflammatory and osteoprogenitor Osteoinductive Molecules
insulin-like growth factor-1, NSAIDs =
cells that are recruited to the frac- Fracture repair is regulated by
nonsteroidal anti-inflammatory drugs,
ture site. Systemic factors may affect several growth factors with varying
TGF-β = transforming growth factor-β,
- = inhibits fracture repair by reducing the num- osteogenic potential, such as trans-
ber of osteoprogenitor cells recruited forming growth factor-β, platelet-
Figure 2
Illustrations of cellular signaling and the role of mesenchymal stem cells (MSCs) in fracture healing. A, Source of MSCs.
B, Action of MSCs within fracture callus. BMPs = bone morphogenetic proteins
620 Journal of the American Academy of Orthopaedic Surgeons
Francois N. K. Kwong, MD, and Mitchel B. Harris, MD
derived growth factor, insulin-like have already demonstrated the pos- cause for this difference remains un-
growth factor-1, and bone morphoge- itive effect of the application of clear. Clinically, poor fracture heal-
netic protein (BMP). Of these, BMP BMPs on the outcome of fractures ing in humans may be associated
appears to be among the most conse- and nonunions. Because a review of with adverse factors not present in
quential. BMP was discovered and all available evidence is beyond the animal studies. For example, soft-
named by Urist3 in 1965; he also first scope of this article, we will focus on tissue coverage of the fracture may
described the phenomenon of os- the treatment of segmental bone de- not be adequate. The initial dose of
teoinduction. Urist observed new fects in patients because this allows BMPs given to human subjects (7 mg
bone formation occurring locally in a direct comparison with the studies of BMP-7 and 2 g of collagen carrier,
rodents after they were given intra- of BMPs in animals. or 12 mg of rhBMP-2 and collagen
muscular implantation of bone cyl- In most clinical studies of the sponge) was much higher than in the
inders decalcified with hydrochloric treatment of segmental bone de- animal studies. Because the release
acid. This phenomenon was attrib- fects, BMPs have been used in con- of BMP inhibitors depends on the ex-
uted to the presence of a protein, junction with allograft or autograft tracellular level of BMPs, it is postu-
BMP, in bone matrix. Since that dis- bone. Jones et al8 demonstrated that lated that this higher concentration
covery, at least 16 different human a combination of BMP-2 and al- of BMPs leads to the expression of
BMPs have been identified. These lograft bone was equivalent to autol- several BMP antagonists, which fur-
proteins affect cells and tissues in- ogous bone for the treatment of seg- ther limits their efficacy and reduc-
volved in the repair process in a mental bone defects. In that study, es the rate of bone healing. It is also
number of ways, including the re- patients with a tibial diaphyseal speculated that BMP receptors in an-
cruitment of MSCs from surround- fracture and a residual cortical de- imals and humans are different in
ing tissues to the fracture site, fol- fect were randomly assigned to re- their degree of responsiveness to the
lowed by their proliferation and ceive either autogenous bone graft BMP molecules.
differentiation into chondrocytes or allograft with an onlay applica-
and osteoblasts, invasion of blood tion of recombinant human BMP-2 Role of BMPs and
vessels, and, ultimately, bone forma- (rhBMP-2). Radiographic and func- Their Inhibitors in
tion. All of these effects are mediat- tional outcomes were similar in Fracture Healing
ed by the binding of BMPs to specif- both groups. To date, the only pub- The activity of BMPs can be lim-
ic transmembrane receptors on lished clinical study on the treat- ited by several antagonists, which
hMSCs, active osteoblasts, and ma- ment of segmental defects with bind to them and interfere with their
ture chondrocytes as well as to the BMPs alone (with a nonosteocon- ability to induce receptor activation.
subsequent activation of various in- ductive carrier matrix only) in hu- One of the most characterized BMP
tracellular messenger systems.4 mans showed healing of critical- inhibitors is noggin, a protein that
sized fibular defects in patients binds to both BMP-2 and BMP-7 and
Therapeutic Application undergoing opening wedge high tib- antagonizes their actions by prevent-
of BMPs ial osteotomy with fibulectomy.9 ing binding with their membrane
Extensive animal data have dem- RhBMP-7 bound to collagen type receptors.10 Its expression by osteo-
onstrated the potential of BMPs to 1 sponge induced bony union in five blasts is induced by BMP-2,10 imply-
induce healing of critical-sized (ie, of six patients with a critical-sized ing that BMP-2 and noggin are in-
large) bone defects.5-7 In animal mod- fibular defect, whereas there was no volved in a negative feedback loop
els, BMPs alone (with their carrier healing in any of the six patients during bone formation. This may
matrix) have been shown to induce treated with the type 1 collagen car- provide a physiologic mechanism
rapid bone bridging of a defect. The rier only. Despite these favorable re- that prevents overexposure of osteo-
quality of the repair tissue was sults, no large studies have been blasts to BMP signaling.
equivalent to or better than that ob- done on the use of BMPs alone in The balance between BMPs and
tained with autologous bone graft- humans. their inhibitors is likely to be a crit-
ing, the standard treatment for bone The pace of healing of segmental ical determinant of fracture healing,
defects and nonunions in clinical defects treated with BMPs differs with a decreased expression of BMPs
practice.6,7 At present, only BMP-2 significantly among species. Seg- and/or a relative increase of BMP an-
(Infuse; Medtronic Sofamor Danek, mental defects in large animals tagonists adversely affecting healing.
Memphis, TN) and BMP-7 (OP-1 Im- treated with BMPs alone healed in In a rat model of fracture nonunion,
plant; Stryker Biotech, Hopkinton, <3 months,5,6 whereas in humans, a downregulation of the gene expres-
MA) have been approved by the US critical tibial defects treated with al- sion of BMPs was demonstrated.11 In
Food and Drug Administration for lograft bone and BMP-2 required ≥6 an animal model of atrophic non-
clinical use. Several clinical studies months to achieve bony union.8 The union, reversal of this decreased ex-
Volume 16, Number 11, November 2008 621
Recent Developments in the Biology of Fracture Repair
pression of osteoinductive factors, this has not yet been specifically were recruited only locally. Howev-
induced by an early local injection of demonstrated in fractures. MSCs are er, a systemic mobilization and re-
rhBMP-7, prevented the develop- thought to be recruited locally from cruitment of osteoblastic precursors
ment of nonunion.12 The expression the cortex, bone marrow, perios- to the fracture site from the periph-
of chordin, a BMP antagonist with a teum, and external soft tissues (Fig- eral circulation have now been dem-
mode of action similar to that of ure 2). The relative contribution of onstrated in several recent studies.
noggin, was upregulated in an ani- MSCs from each tissue is uncertain In a rabbit ulnar osteotomy model, it
mal model of fracture nonunion,11 but is thought to depend on the local was demonstrated that some osteo-
suggesting that downregulation of parameters present at the injured tis- blasts involved in fracture healing
chordin in a fracture nonunion has sue, such as growth factors, oxygen were systemically mobilized and re-
the potential of improving bone gradient, and mechanical stability. cruited to the fracture from remote
healing. The clinical relevance of muscle as a bone marrow sites.20 Shen et al21
In normally healing fractures, the source of progenitor cells during demonstrated in a murine model
balance between BMPs and their in- fracture repair has been the subject that, following systemic injection of
hibitors can also be manipulated to of several recent studies.16,17 MSCs, osteoprogenitor cells local-
hasten repair. This would involve The presence in muscle of a pop- ized to the fracture callus.
the addition of the osteoinductive ulation of adult stem cells that can These studies have implications
factors (eg, BMP-2), inhibition of the differentiate into cells of different for the development of future cell-
activity of BMP inhibitors, or a com- lineages has been suspected for some based therapies for fracture healing.
bination of both methods. So far, bi- time based on two observations. Cell-based therapies are needed
ologic methods of enhancing bone First, muscle has the potential to when insufficient cells are present
regeneration have centered on the turn into bone, as occurs during het- within a fracture callus (eg, segmen-
promotion of osteoinduction via the erotopic ossification. Second, the tal defect). In such a situation, even
delivery of BMPs. However, it was original description of osteoinduc- when all of the osteoprogenitor cells
recently demonstrated that noggin tion by Urist3 has been attributed to at the site of fracture are working to
or chordin suppression can acceler- the effects of BMPs on progenitor the maximum, there will be no bony
ate osteogenesis in vitro13,14 and that cells within muscle tissue. Howev- union, nor will any osteoinductive
noggin knockdown increased the er, the isolation of the relevant MSC agents be effective because maximal
rate of intramembranous ossifica- population from this tissue is rela- osteogenesis per cell is already oc-
tion in an animal model.14 We be- tively recent.16 Clinically, the impor- curring. In a level III study (case-
lieve that these findings will be ex- tance of muscle as a source of os- control), Hernigou et al22 demon-
tended to fracture healing and that teoprogenitor cells is underlined by strated the clinical effectiveness of
blockade of the activity of BMP in- the poor outcome of fractures in local percutaneous injection of bone
hibitors may provide a novel strate- which muscle has been devitalized, marrow aspirate in treating tibial
gy for expediting fracture repair. although this poor outcome is often nonunions. We believe that the stud-
attributed to the coexisting damage ies mentioned here suggest that it
to the periosteal blood supply. Mus- might be possible to develop cell-
Local Cellular Signaling
cle resection significantly reduces based therapies in which cells are
Complete fracture healing requires callus formation and the biome- systemically administered and local-
that a sufficient number of hMSCs chanical properties of the healed ized to the site of injury.
differentiate into chondrocytes and bone, while a muscle crush does not Evidence is emerging that distant
osteoblasts, as well as other cells of significantly affect bone healing.18 skeletal sites can be affected in re-
the mesenchymal lineage, such as Conversely, heterotopic ossification sponse to a local bone injury.23 An
adipocytes, and stromal and endo- in acetabular fractures has been re- increased osteogenic response has
thelial cells. In addition to differen- duced as surgeons have become been detected in sites distant from
tiation, the trophic, or nutritional, more aggressive in débriding injured the fracture in animal models.23 This
activity of MSCs in the repair of oth- and necrotic muscle from the surgi- may result from the release of
er tissues is now well established.15 cal field.19 growth factors (eg, transforming
This refers to the capacity of MSCs growth factor-β, insulin-like growth
to secrete growth factors, which factor-1) from the fracture site into
Systemic Recruitment
stimulate blood vessel formation the systemic circulation, as shown
of Cells and Molecular
and the proliferation of other local in a clinical study.24 It is not known
Signaling
MSCs.15 It is postulated that MSCs whether the level of these factors in
exert a trophic activity in the early Traditionally, it was thought that serum reflects the repair activity of
stages of fracture repair, although the cells involved in fracture repair the fracture.
622 Journal of the American Academy of Orthopaedic Surgeons
Francois N. K. Kwong, MD, and Mitchel B. Harris, MD
Systemic Factors and pair. Delayed fracture healing in the (P < 0.05) longer by 4 weeks than in
elderly may be caused by differences nonsmokers.32 This effect may be
Local Fracture Healing
in molecular signaling locally with- mediated by either nicotine or some
It is widely accepted that extrinsic in the fracture callus as well as to other, yet undefined components in
factors have an influence on the out- systemic factors. Meyer et al28 re- cigarette smoke,33 or both.
come of fracture healing. However, it ported a decreased expression of In animal models, nicotine has
is often difficult to isolate the role of BMP-2 and Indian hedgehog (a factor been shown to delay cellular differen-
a particular systemic factor in clini- related to endochondral callus for- tiation into chondrocytes and to slow
cal situations. For example, impaired mation) in fracture calluses of older the physiologic transition from car-
fracture healing in the elderly may be rats. Noggin expression was not tilaginous callus to bone.34 It is also
related to age, osteoporosis, drugs, changed with age. However, the de- highly likely that the compromise of
malnutrition, and/or anemia. Evi- crease in expression of BMP-2 im- microcirculation secondary to nico-
dence gained from animal models as plies that the BMP inhibitor predom- tine causes a delay in fracture repair.
well as recently uncovered cellular inated over BMP-2 in older rats. It remains to be seen whether the
and molecular processes have led to Hormonal differences with aging deleterious effects of smoking are re-
better understanding of the role of may also be a factor. Sera obtained versible with smoking cessation and
systemic factors. from aged donors are less potent in- whether BMPs can improve healing
ducers of osteoblast differentiation of in smokers. These questions should
Nonsteroidal hMSC than are sera obtained from be investigated using animal models
Anti-inflammatory Drugs young donors.29 These effects were of fracture healing and smoking.
During fracture repair, the en- specific for osteoblast differentiation
zyme cyclooxygenase-2 (COX-2) is because no donor age differences in
Influence of Fracture
activated to produce prostaglandins, the ability to support differentiation
Fixation
which are needed during inflamma- of other cell types were observed.
tion and are critical for starting the Short-term bone marrow cultures es- The local mechanical forces on a
osteogenic response.25 Nonsteroidal tablished from young and old donors fracture resulting in movement at
anti-inflammatory drugs (NSAIDs) contain similar numbers of hMSCs the fracture site are critical factors in
inhibit COX-2, dramatically reduc- and exhibit similar proliferation the success of fracture repair. Excess
ing prostaglandin production, and rates.30 In addition, the capacity of motion can delay healing; casting
therefore have the potential to nega- hMSC to differentiate into osteo- and fracture fixation aim to provide
tively affect fracture repair. Al- blasts and adipocytes was main- a mechanical environment in which
though results in various animal tained irrespective of donor age.31 strains are decreased to avoid de-
studies have been conflicting, it is These studies suggest that there are layed union or nonunion. However,
generally accepted that NSAIDs im- no intrinsic defects in hMSCs with some movement, referred to as mi-
pair fracture healing in animal mod- aging and that extrinsic factors cromotion, is beneficial to fracture
els in which a high dose has been ad- present in the aging environment of healing. Different fractures and dif-
ministered.26 This inhibitory effect hMSCs may be responsible for the ferent areas of the skeleton respond
is most potent during the early phase impaired osteoblast functions seen differently to mechanical forces and
of healing, thereby underlining the with aging. resultant strains. Yet precisely how
importance of the initial inflamma- These observations need further these changes in local mechanical
tory reaction.26 investigation. If poor fracture repair loading result in a cartilaginous cal-
Although it is not known in in the elderly is related to impaired lus or intramembranous ossification
which clinical situations NSAIDs in osteoinductive signals rather than to remains speculative. The influence
high local concentrations will affect differences in the cellular compo- of the mechanical environment on
early-phase fracture healing, admin- nent of the healing fractures, then the fracture repair can be viewed at
istration of NSAIDs has been associ- the elderly patient with trauma is three levels: tissue, cellular, and mo-
ated with delayed union and pseud- more likely to benefit from an os- lecular.
arthrosis.27 The inhibitory effect of teoinductive agent, such as BMP-2, Tissue differentiation requires
COX-2 blockade in vitro has been than from cell-based therapies. mechanical stability. In an animal
shown to be reversed by the admin- model, Claes et al35 demonstrated a
istration of BMP-2.28 Smoking strong association between fracture
Smoking has an adverse effect on stability and the spatial distribution
Age fracture healing. In one study, the of newly formed blood vessels and
Aging is an independent factor time to union for tibial fractures specific tissue formation. It was also
that negatively affects fracture re- among smokers was significantly independently demonstrated in an
Volume 16, Number 11, November 2008 623
Recent Developments in the Biology of Fracture Repair
animal model that increased stabil- gamma in bone marrow stromal 2. Reed AA, Joyner CJ, Brownlow HC,
ity affected endochondral ossifica- cells, a mediator that favors adipo- Simpson AH: Human atrophic frac-
ture non-unions are not avascular.
tion by decreasing the overall genesis over osteogenesis.41 However,
J Orthop Res 2002;20:593-599.
amount of cartilage that formed at compression can also stimulate BMP 3. Urist MR: Bone: Formation by autoin-
the fracture site.36 This was thought production and decrease noggin pro- duction. Science 1965;150:893-899.
to be secondary to an increase in the duction, thereby stimulating the in 4. Kloen P, Di Paola M, Borens O, et al:
rate of maturation of chondrocytes vitro differentiation of human osteo- BMP signaling components are ex-
during the endochondral ossification blastic cells.42 These studies indicate pressed in human fracture callus.
stage of fracture healing. Conversely, Bone 2003;33:362-371.
that the same changes in molecular
5. Cook SD, Salkeld SL, Brinker MR,
orthopaedic surgeons often observe signaling can be induced by different Wolfe MW, Rueger DC: Use of an os-
an increase in the size of fracture types of forces acting on the progen- teoinductive biomaterial (rhOP-1) in
callus with increased movement itor cells in various circumstances. healing large segmental bone defects.
around the fracture. Endochondral J Orthop Trauma 1998;12:407-412.
ossification is also affected by the 6. Gerhart TN, Kirker-Head CA, Kriz
type of intermittent forces applied to Summary MJ, et al: Healing segmental femoral
the fracture site. In a rat model of defects in sheep using recombinant
Significant advances have been
human bone morphogenetic protein.
healing osteotomy, intermittent ten- made in the understanding of the bi- Clin Orthop Relat Res 1993;293:
sile strains stimulated endochondral ology of fracture healing. In particu- 317-326.
ossification, as opposed to compres- lar, it is now understood that frac- 7. Sciadini MF, Johnson KD: Evaluation
sive strains, which favored direct in- ture repair is not only a local of recombinant human bone morpho-
tramembranous ossification.37 genetic protein-2 as a bone-graft sub-
phenomenon but is itself under the
stitute in a canine segmental defect
The method of fracture fixation influence of extrinsic factors. Ad- model. J Orthop Res 2000;18:289-
also has an effect on the biology of verse local and systemic clinical fac- 302.
the healing callus. In a murine mod- tors can affect the molecular and cel- 8. Jones AL, Bucholz RW, Bosse MJ, et al:
el of femoral fracture healing, the lular processes involved and can lead Recombinant human BMP-2 and al-
fracture callus was significantly larg- lograft compared with autogenous
to delayed fracture repair and non-
bone graft for reconstruction of dia-
er with intramedullary nail fixation union. The management of these physeal tibial fractures with cortical
than with plate fixation.38 The healing problems remains challeng- defects: A randomized, controlled tri-
changes in gene expression follow- ing, despite the introduction of ther- al. J Bone Joint Surg Am 2006;88:
ing each fixation procedure were apeutic BMPs and other biologic 1431-1441.
similar and occurred after the same 9. Geesink RG, Hoefnagels NH, Bulstra
methods of bone regeneration. Fur-
SK: Osteogenic activity of OP-1 bone
postoperative time interval. Howev- ther understanding of the patho- morphogenetic protein (BMP-7) in a
er, the intramedullary group had sig- physiology of fracture repair is need- human fibular defect. J Bone Joint
nificantly greater expression of genes ed to develop improved treatment Surg Br 1999;81:710-718.
related to cartilage, cell division, and strategies targeted to the molecular 10. Abe E, Yamamoto M, Taguchi Y, et al:
inflammation (P < 0.05 for all), and Essential requirement of BMPs-2/4
and cellular processes affected in
for both osteoblast and osteoclast for-
there was greater expression of genes specific clinical conditions. mation in murine bone marrow cul-
related to macrophage activity in the tures from adult mice: Antagonism by
plate group than in the nail group noggin. J Bone Miner Res 2000;15:
(P < 0.001). References 663-673.
Osteoprogenitor cells have the ca- 11. Niikura T, Hak DJ, Reddi AH: Global
Evidence-based Medicine: Referenc-
gene profiling reveals a downregula-
pacity to detect their mechanical en- es 9, 19, 22, 24, and 32 are level I/II tion of BMP gene expression in exper-
vironment and modify their rate of prospective, randomized studies. imental atrophic nonunions com-
differentiation, a process mediated The remaining references are case- pared to standard healing fractures.
via effects on the BMP signal- control cohort studies, basic re- J Orthop Res 2006;24:1463-1471.
ing pathway. Cyclic stretching of 12. Makino T, Hak DJ, Hazelwood SJ,
search studies, or expert opinion.
Curtiss S, Reddi AH: Prevention of
hMSCs or osteoblastic precursor cells
Citation numbers printed in bold atrophic nonunion development by
in a collagen matrix increased their recombinant human bone morphoge-
proliferation and osteogenic differen- type indicate references published
netic protein-7. J Orthop Res 2005;
tiation,39,40 a phenomenon associated within the past 5 years. 23:632-638.
with an increase in BMP-2 pro- 13. Kwong FN, Richardson SM, Evans CH:
1. Potier E, Ferreira E, Andriamanalijaona Chordin knockdown enhances the os-
duction. This increase in osteogenic
R, et al: Hypoxia affects mesenchymal teogenic differentiation of human mes-
differentiation may also be mediated stromal cell osteogenic differentiation enchymal stem cells. Arthritis Res
by the downregulation of peroxi- and angiogenic factor expression. Ther 2008;10:R65.
some proliferator–activated receptor Bone 2007;40:1078-1087. 14. Wan DC, Pomerantz JH, Brunet LJ,
624 Journal of the American Academy of Orthopaedic Surgeons
Francois N. K. Kwong, MD, and Mitchel B. Harris, MD
et al: Noggin suppression enhances in are increased in the systemic circula- Sandell LJ: Smoking delays chondro-
vitro osteogenesis and accelerates in tion during bone callus healing. genesis in a mouse model of closed
vivo bone formation. J Biol Chem J Orthop Res 2003;21:320-325. tibial fracture healing. J Orthop Res
2007;282:26450-26459. 25. Zhang X, Schwarz EM, Young DA, Pu- 2006;24:2150-2158.
15. Caplan AI: Adult mesenchymal stem zas JE, Rosier RN, O’Keefe RJ: 35. Claes L, Eckert-Hübner K, Augat P:
cells for tissue engineering versus re- Cyclooxygenase-2 regulates mesen- The effect of mechanical stability on
generative medicine. J Cell Physiol chymal cell differentiation into the local vascularization and tissue differ-
2007;213:341-347. osteoblast lineage and is critically in- entiation in callus healing. J Orthop
16. Jankowski RJ, Huard J: Myogenic cel- volved in bone repair. J Clin Invest Res 2002;20:1099-1105.
lular transplantation and regenera- 2002;109:1405-1415. 36. Le AX, Miclau T, Hu D, Helms JA:
tion: Sorting through progenitor het- 26. Simon AM, Manigrasso MB, O’Connor Molecular aspects of healing in stabi-
erogeneity. Panminerva Med 2004; JP: Cyclo-oxygenase 2 function is es- lized and non-stabilized fractures.
46:81-91. sential for bone fracture healing. J Orthop Res 2001;19:78-84.
17. Gates CB, Karthikeyan T, Fu F, Huard J Bone Miner Res 2002;17:963-976. 37. Smith-Adaline EA, Volkman SK, Ig-
J: Regenerative medicine for the mus- 27. Giannoudis PV, MacDonald DA, Mat- nelzi MA Jr, Slade J, Platte S, Gold-
culoskeletal system based on muscle- thews SJ, Smith RM, Furlong AJ, De stein SA: Mechanical environment al-
derived stem cells. J Am Acad Boer P: Nonunion of the femoral diaph- ters tissue formation patterns during
Orthop Surg 2008;16:68-76. ysis: The influence of reaming and non- fracture repair. J Orthop Res 2004;22:
18. Utvåg SE, Grundnes O, Rindal DB, steroidal anti-inflammatory drugs. 1079-1085.
Reikerås O: Influence of extensive J Bone Joint Surg Br 2000;82:655-658. 38. Heiner DE, Meyer MH, Frick SL,
muscle injury on fracture healing in 28. Meyer RA Jr, Meyer MH, Tenholder Kellam JF, Fiechtl J, Meyer RA Jr: Gene
rat tibia. J Orthop Trauma 2003;17: M, Wondracek S, Wasserman R, Garg- expression during fracture healing in
430-435. es P: Gene expression in older rats rats comparing intramedullary fixation
19. Rath EM, Russell GV Jr, Washington with delayed union of femoral frac- to plate fixation by DNA microarray.
WJ, Routt ML Jr: Gluteus minimus tures. J Bone Joint Surg Am 2003;85: J Orthop Trauma 2006;20:27-38.
necrotic muscle debridement dimin- 1243-1254. 39. Ignatius A, Blessing H, Liedert A, et al:
ishes heterotopic ossification after 29. Abdallah BM, Haack-Sørensen M, Tissue engineering of bone: Effects of
acetabular fracture fixation. Injury Fink T, Kassem M: Inhibition of os- mechanical strain on osteoblastic
2002;33:751-756. teoblast differentiation but not adipo- cells in type I collagen matrices.
20. Shirley D, Marsh D, Jordan G, Mc- cyte differentiation of mesenchymal Biomaterials 2005;26:311-318.
Quaid S, Li G: Systemic recruitment stem cells by sera obtained from aged 40. Sumanasinghe RD, Bernacki SH, Lo-
of osteoblastic cells in fracture heal- females. Bone 2006;39:181-188. boa EG: Osteogenic differentiation of
ing. J Orthop Res 2005;23:1013-1021. 30. Stenderup K, Justesen J, Eriksen EF, human mesenchymal stem cells in
21. Shen FH, Visger JM, Balian G, Hur- Rattan SI, Kassem M: Number and collagen matrices: Effect of uniaxial
witz SR, Diduch DR: Systemically proliferative capacity of osteogenic cyclic tensile strain on bone morpho-
administered mesenchymal stromal stem cells are maintained during ag- genetic protein (BMP-2) mRNA ex-
cells transduced with insulin-like ing and in patients with osteoporosis. pression. Tissue Eng 2006;12:3459-
growth factor-I localize to a fracture J Bone Miner Res 2001;16:1120-1129. 3465.
site and potentiate healing. J Orthop 31. Justesen J, Stenderup K, Eriksen EF, 41. David V, Martin A, Lafage-Proust
Trauma 2002;16:651-659. Kassem M: Maintenance of osteoblas- MH, et al: Mechanical loading down-
22. Hernigou P, Poignard A, Beaujean F, tic and adipocytic differentiation po- regulates peroxisome proliferator-
Rouard H: Percutaneous autologous tential with age and osteoporosis in activated receptor gamma in bone
bone-marrow grafting for nonunions: human marrow stromal cell cultures. marrow stromal cells and favors os-
Influence of the number and concen- Calcif Tissue Int 2002;71:36-44. teoblastogenesis at the expense of ad-
tration of progenitor cells. J Bone 32. Adams CI, Keating JF, Court-Brown ipogenesis. Endocrinology 2007;148:
Joint Surg Am 2005;87:1430-1437. CM: Cigarette smoking and open tib- 2553-2562.
23. Einhorn TA, Simon G, Devlin VJ, ial fractures. Injury 2001;32:61-65. 42. Mitsui N, Suzuki N, Maeno M, et al:
Warman J, Sidhu SP, Vigorita VJ: The 33. Skott M, Andreassen TT, Ulrich- Optimal compressive force induces
osteogenic response to distant skele- Vinther M, et al: Tobacco extract but bone formation via increasing bone
tal injury. J Bone Joint Surg Am 1990; not nicotine impairs the mechanical morphogenetic proteins production
72:1374-1378. strength of fracture healing in rats. and decreasing their antagonists pro-
24. Kaspar D, Neidlinger-Wilke C, Hol- J Orthop Res 2006;24:1472-1479. duction by Saos-2 cells. Life Sci 2006;
bein O, Claes L, Ignatius A: Mitogens 34. El-Zawawy HB, Gill CS, Wright RW, 78:2697-2706.
Volume 16, Number 11, November 2008 625
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Injury: Ianiv Klaber, Pablo Besa, Felipe Sandoval, Daniel Lobos, Tomas Zamora, Daniel Schweitzer, Julio UrrutiaDocument4 pagesInjury: Ianiv Klaber, Pablo Besa, Felipe Sandoval, Daniel Lobos, Tomas Zamora, Daniel Schweitzer, Julio UrrutiaAby SuryaNo ratings yet
- Rotator Cuff Syndrome: October 2018Document16 pagesRotator Cuff Syndrome: October 2018Aby SuryaNo ratings yet
- Kulkarni2012 PDFDocument7 pagesKulkarni2012 PDFAby SuryaNo ratings yet
- Posterior Knee Dislocation: I I e MDocument2 pagesPosterior Knee Dislocation: I I e MAby SuryaNo ratings yet
- FFFFDocument4 pagesFFFFAby SuryaNo ratings yet
- Wjem 11 103 PDFDocument2 pagesWjem 11 103 PDFAby SuryaNo ratings yet
- Pneumothorax: An Update: ReviewDocument5 pagesPneumothorax: An Update: ReviewAby SuryaNo ratings yet
- Jurnal AutismDocument10 pagesJurnal AutismAby SuryaNo ratings yet
- P-342 Poster: Abstracts of The 25th Annual Meeting of ESHRE, Amsterdam, The Netherlands, 28 June - 1 July, 2009Document1 pageP-342 Poster: Abstracts of The 25th Annual Meeting of ESHRE, Amsterdam, The Netherlands, 28 June - 1 July, 2009Aby SuryaNo ratings yet
- Otolaryngology - Head and Neck Surgery: Clinical Practice Guideline: Acute Otitis ExternaDocument21 pagesOtolaryngology - Head and Neck Surgery: Clinical Practice Guideline: Acute Otitis ExternaAby SuryaNo ratings yet
- Richard W. Titball, E. Diane Williamson.2007.: WWW - Cdc.gov/ncidod/dvbid/plague/index - HTMDocument1 pageRichard W. Titball, E. Diane Williamson.2007.: WWW - Cdc.gov/ncidod/dvbid/plague/index - HTMAby SuryaNo ratings yet
- Acute Otitis Externa in Children: Child Health UpdateDocument3 pagesAcute Otitis Externa in Children: Child Health UpdateAby SuryaNo ratings yet
- Principles of Bone GraftingDocument6 pagesPrinciples of Bone GraftingJayanth Perumal100% (2)
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
- Orthopedic-Ward-Abbrev CC FX NI-Lecture 20230830Document30 pagesOrthopedic-Ward-Abbrev CC FX NI-Lecture 20230830Yong VillafriaNo ratings yet
- Internal & External Fixation-NEWDocument23 pagesInternal & External Fixation-NEWaeruginoNo ratings yet
- ORP - Handout - English - Principles of Fracture Fixation - v2Document11 pagesORP - Handout - English - Principles of Fracture Fixation - v2Mohamad RamadanNo ratings yet
- Stages in The Healing of A Bone FractureDocument10 pagesStages in The Healing of A Bone FractureMagdalena PranataNo ratings yet
- Fracture Mandible PDFDocument120 pagesFracture Mandible PDFMorohai DoinaNo ratings yet
- Reviews: Fracture Healing: Mechanisms and InterventionsDocument10 pagesReviews: Fracture Healing: Mechanisms and InterventionsFatrika DewiNo ratings yet
- Orthopedic Hardware in Trauma - A Guided Tour For The Radiologist - Part 1Document15 pagesOrthopedic Hardware in Trauma - A Guided Tour For The Radiologist - Part 1Marcia MejíaNo ratings yet
- K. Adwar. Internal Fixation of #S.Document32 pagesK. Adwar. Internal Fixation of #S.Fathy AlhallagNo ratings yet
- DR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiDocument34 pagesDR Himanshu Gaur: Consultant Orthopaedic, Joint Replacement & Arthroscopy (Sports Injury) Surgeon BCIMS, New DelhiAnjani Kumar JhaNo ratings yet
- Fracture HealingDocument23 pagesFracture Healingjomari dvNo ratings yet
- 1.1 Biology of Bone HealingDocument32 pages1.1 Biology of Bone HealingCristian CumpănăNo ratings yet
- Outline of Fracture Management & ComplicationDocument24 pagesOutline of Fracture Management & Complicationmsarwar100% (1)
- FractureDocument125 pagesFractureKlara Devina VanessaNo ratings yet
- Orthopedic Nursing CareDocument41 pagesOrthopedic Nursing CareIrfan Ners MaulanaNo ratings yet
- 19 Musculoskeletal System DR - FallerDocument27 pages19 Musculoskeletal System DR - FallerFranz Earl Niño AlbesaNo ratings yet
- Surgery (Ortho) NotesDocument155 pagesSurgery (Ortho) NotesprestigeuniversaltradingNo ratings yet
- Dsem TRM 0714 0109 3 - LRDocument88 pagesDsem TRM 0714 0109 3 - LRbagus lazuardiNo ratings yet
- Collagen and Hydroxyapatite Scaffolds Activate DisDocument15 pagesCollagen and Hydroxyapatite Scaffolds Activate DisIsworo RukmiNo ratings yet
- Paper 3 Surgery Not Answered Till 2022Document288 pagesPaper 3 Surgery Not Answered Till 2022NEMO2322No ratings yet
- (Download PDF) Fracture Management For Primary Care Updated Edition M Patrice Eiff Online Ebook All Chapter PDFDocument42 pages(Download PDF) Fracture Management For Primary Care Updated Edition M Patrice Eiff Online Ebook All Chapter PDFfreddie.branson694100% (13)
- Fracture Healing SsDocument2 pagesFracture Healing SsIndra SyafaatNo ratings yet
- Cutaneous Wound HealingDocument78 pagesCutaneous Wound HealingClaudio Luis VenturiniNo ratings yet
- Fracture Reduction and FixationDocument271 pagesFracture Reduction and FixationJAMPIER MORERANo ratings yet
- 1 Principles of Internal Fixation: 1.1.1 Mechanical Properties of BoneDocument29 pages1 Principles of Internal Fixation: 1.1.1 Mechanical Properties of BoneCarlos CalderonNo ratings yet
- AO Basic 2015 Relative StabilityDocument23 pagesAO Basic 2015 Relative StabilitySolidet VasimNo ratings yet
- Case Study GROUP 10Document22 pagesCase Study GROUP 10CreativeWorldwideNo ratings yet
- Management of Mandible FracturesDocument52 pagesManagement of Mandible FracturesAndykaYayanSetiawanNo ratings yet
- Robbins 7th Ed - Chapter 3 - Tissue Renewal & Repair (2) Flashcards by Heli Sinnpson - BrainscapeDocument12 pagesRobbins 7th Ed - Chapter 3 - Tissue Renewal & Repair (2) Flashcards by Heli Sinnpson - BrainscapeCarlos MaingeNo ratings yet