Professional Documents
Culture Documents
Mishra and Rao Seshadri Unpacking The Discourse On Uhc in India
Mishra and Rao Seshadri Unpacking The Discourse On Uhc in India
Uploaded by
rajsandhu250 ratings0% found this document useful (0 votes)
23 views7 pagesOriginal Title
mishra-and-rao-seshadri-unpacking-the-discourse-on-uhc-in-india
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
23 views7 pagesMishra and Rao Seshadri Unpacking The Discourse On Uhc in India
Mishra and Rao Seshadri Unpacking The Discourse On Uhc in India
Uploaded by
rajsandhu25Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 7
THEMES AND DEBATES
Unpacking the discourse on universal health
coverage in India
Arima Mishra Ph.D; Shreelata Rao Seshdari Ph.D
Abstract to as UHC) has been acknowledged as the most
Since the World Health Report 2010, universal important public health goal worldwide. Though this
health coverage has received increased policy goal has been widely acclaimed and reinforced in
attention worldwide. Though the goal of achieving several national and international forums, the
universal health coverage has been widely contours of the debate are disparate. This
acclaimed and is reinforced in several national and commentary seeks to unpack the discourse on UHC
international forums, the contours of the debate have in the context of India and argue that the recent
been disparate. Endorsing this global call, India like attention given to achieving UHC needs to focus on
many other low and middle income countries, “public” (population level) and “health” rather than
embarked on the path to achieve universal health on individualized medical care.
coverage by proposing several health sector reforms.
Though universal health coverage has received The call for UHC in India: An unfinished policy
significant political attention in the country, there is agenda?
a danger of limiting the debate to a question of Resonating with the global call, India has
financing and providing of medical services. We expressed its political commitment to achieve
argue that the current debate about universal health universal health coverage by 2020. The Government
coverage should draw critical attention to (re) of India set up the High Level Expert Group
prioritization of primary healthcare, health system (HLEG) in 2010 to develop a road map for
governance, and health equity. We must keep health operationalizing the UHC vision. The HLEG report
and its determinants in mind rather than medical has been heralded as a landmark document in health
care alone. Key words: universal health coverage, policy.1 Evoking principles of equity and
primary healthcare, governance, equity, India. universality in healthcare, it has generated a vibrant
political debate in India around the UHC vision.
Introduction In order to contextualize the current UHC
Margaret Chen, in her address to the World discourse in India, it is pertinent to ask if UHC is
Health Assembly in 2012, stated that universal really a new policy agenda. The World Health
health coverage is the single most powerful concept Report (2013)2 traces the current expression of UHC
that public health has to offer. Following the as a descendant of the Alma Ata declaration on
resolution of the 58th World Health Assembly in “Health for All.” Both these movements, as the
2005, Universal Health Coverage (hereafter referred report notes, underscore the aspiration of
“enjoyment of the highest attainable standard of
Arima Mishra. Ph.D, School of Development, Azim
health.” A historical analysis of the current UHC
Premji University, Bangalore, India debates in India is essential before any fresh
E-mail: arima.mishra@apu.edu.in recommendations on UHC are contemplated. The
Shreelata Rao Seshadri, Ph.D idea of UHC as a means of ensuring health for all
School of Development, Azim Premji University, was first expressed in India prior to the country’s
Bangalore, India Independence. The Health Survey and Development
E-mail: shreelata. seshadri@apu.edu.in Committee Report popularly known as the Bhore
Submitted: 5/31/2014 Committee Report (1946) has been considered as
Revised: 9/16/2014 India’s most comprehensive and detailed health
Accepted: 6/13/2015
policy and planning document.3 The Bhore
Conflict of interest: None
Peer-reviewed: Yes
Social Medicine (www.socialmedicine.info) - 86 - Volume 9, Number 2, October 2015
committee recommended a National Health Service public health facilities suffer from severe resource
to ensure universal health coverage through a constraints and fail to deliver quality healthcare. To
comprehensive state run health service. More add to this multi-level hierarchical public health
importantly, the National Health Service was service structure, there is a large private sector in
designed to offer both curative and preventive health, which is both unregulated and extremely
services to individual patients and health promotion varied. It includes traditional healers dispensing
for the population as a whole. The Commission homegrown remedies, practitioners of traditional
discussed the promotion of healthy environments at Indian Systems of Medicine, pharmacists, doctors in
home, in the workplace, and beyond. Acknow- solo practice, nursing homes, and highly sophis-
ledging rural-urban disparities, the Commission ticated tertiary care centers. Eighty percent of
proposed a decentralized health structure which outpatient care is provided by the private sector; this
would place health services close to the people; this means high out of pocket expenditure for the poor
would ensure their maximum use by the community. and marginalized.
The spirit of the Bhore committee report and the Despite some health gains in the recent past with
consequent Alma Ata Declaration (1978) was regard to reductions in maternal and child mortality
reflected in the first Indian National Health Policy in as well as improvements in life expectancy, health
1983. Critiquing the curative model of healthcare, outcomes in India continue to belie the
this policy reiterated the goal of providing universal, achievements of its consistent 6% economic growth
comprehensive primary healthcare services relevant in the past decade. Not only is India lagging behind
to the actual needs and priorities of the community.4 many countries at comparable levels of GDP per
Despite its progressive intentions, the 1983 policy capita, it is also clear now that several of the
fell far short of realizing its stated goals. The Millennium Development Goals for health will not
liberalization of the economy in the early 1990s was be achieved (with the current Infant Mortality Rate
accompanied by growth of the private sector with and Maternal Mortality Ratio at 47/1000 and
rare or ineffective regulations. Public investment in 212/100,000 respectively as against the targets of
the health system was as low as 0.9% of the Gross 28/1000 and 109/100,000 by 2005).5 There are
Domestic Product until 2005 when it was raised to a significant regional and inter-state differences
meagre 1.4%. Thus, chronic underfinancing, the within the country; substantial differences in health
absence of political prioritization/leadership on the outcomes based on gender and socio-economic class
social sector including health, the continued focus remain. For example, the infant mortality rate was
on disease specific programs, and an unregulated, 82 per 1000 live births in the poorest wealth quintile
rapidly blossoming private sector meant that UHC and 34 per 1000 live births in the richest wealth
remained an unrealized aspiration. quintile in 2005–06. Further, the mortality rate in
Opting for a strategy of providing selective children younger than 5 years who are born to
primary healthcare – considered more affordable mothers with no education compared with those
and feasible than comprehensive primary healthcare with more than 5 years of education was 106/1000
– India developed a large number of “vertical” live births and 49/1000 live births, respectively,
disease control programs that are financed and during period from 1995–96 to 2005–06.6 In terms
managed from the central level; these also known as of inter-state differences, maternal mortality ratio is
“Centrally Sponsored Schemes.” These programs as high as 390 in the state of Assam while southern
are directed at diseases of public health importance, states like Kerala and Tamil Nadu have 87 and 92
including inter alia reproductive and child health, respectively.7
HIV/AIDS, tuberculosis, malaria, cataract blindness, Hence, the discussion of UHC in India is very
and leprosy. They are managed, implemented, and timely given the dismal situation of poor access to
monitored by complex organizational arrangements affordable services, poor quality of care, and
at central, state, district, and community levels. inequity in health status. But how does this call aim
At the state level, public health services are to revive the unrealized agenda of universal
provided by an extensive network of primary, comprehensive health reflected in the Bhore
secondary, and tertiary health facilities, each with its Committee Report (1946) and the Alma Ata
own service guidelines and staffing pattern. Despite Declaration (which India like many other countries
such an elaborate organizational structure, most wholeheartedly endorsed in 1978)?
Social Medicine (www.socialmedicine.info) - 87 - Volume 9, Number 2, October 2015
Health for All to Universal Health Coverage coverage at secondary and tertiary levels for specific
Despite an apparent continuity between the Alma ailments.8 These principles set it apart from the
Ata declaration and the current UHC call, these Alma Ata discourse on Health for All which was
seem different on some fundamental grounds.8 The premised on the principles of a robust public health
differences pertain as much to the role of the state system (in financing and provisioning) and
vis-a-vis the private sector in financing and comprehensive primary healthcare.
provisioning of healthcare as to the notion of public The semantics of “comprehensive primary
health itself. Although set within an economic healthcare” (covering all aspects of care responding
climate of neo-liberal reforms, exponential growth to community needs and addressing social
of a private sector in health and widening disparities determinants of health) and “coverage” (provision
in healthcare, the UHC discourse focuses only on of a defined package of services to the population)
redressing financial hardship in obtaining indicate differences in approaches to health planning
healthcare. Catastrophic expenditure in healthcare itself (bottom-up/top-down). In this regard, it runs
has thus been the entry point for the recent UHC counter to the National Rural Health Mission
agenda. (NRHM) agenda that sought to carry out
The WHO identifies three key dimensions of “architectural corrections” in the public health
coverage: population, services, and cost. This has system in rural areas. By revitalising the primary
led to a lot of discussion around provision of a healthcare approach, the NRHM launched in 2005,
“package” of services through expansions in sought to strengthen comprehensive primary
insurance coverage. As stated above, catastrophic healthcare through inter-sectoral actions, integration
expenditure has been a hard reality in India and of earlier vertical health programs, and bringing the
there is no denying the fact that high out of pocket public (community) back into public health through
expenditure is an important deterrent to accessing recruitment of village level health workers, health
quality healthcare. UHC seeks to check this and nutrition outreach sessions, village level health
unwarranted financial catastrophe. Yet reducing planning and community monitoring.13 The UHC
UHC to financing healthcare is only part of the story debate needs to be integrally linked with the NRHM
and at best an unhealthy one. There is plenty of and strengthen the political commitment to ensure
evidence to show the pitfalls of responding to high healthcare that is comprehensive, integrated, and
healthcare costs through expanding insurance accessible to all.
coverage via schemes like the Rashtriya Swasthya Health for All is predicated on participation: of
Bima Yojana (RSBY, introduced in 2008).9-11 Such people, of communities, and of their political repre-
schemes have received greater support in the 12th sentatives at the local and state levels. This has been
Five Year Plan including the current Draft National supported by the 73rd Amendment to the Con-
Health Policy (2015).12 stitution in India, and subsequently reinforced in the
The HLEG in its report has rightly cautioned design and implementation of the NRHM. Health
against relying on insurance schemes as way to has long been peripheral on the political agenda in
implement UHC; there is a danger of fragmenting India. The UHC debate so far involves only the
healthcare through underinvestment in primary care, “Center” (the national level); but how this agenda
preventive care, health promotion, and rehabilitative fits into the political vision and priorities of different
care while fostering the institutions of secondary states in India is not yet clear. This is significant: the
and tertiary care. Other dangers of course include provision of health services in India’s federal
the indirect growth of private sector healthcare governance structure is the responsibility of
delivery using public financing. In a setting where individual states and without sufficient political will
the large, heterogeneous private health sector is of these states, India would have difficulty
mostly unregulated, such schemes would ironically achieving UHC. A goal like UHC cannot afford to
promote the very set of problems which they try to rest in a top-down planning mode. In fact one of the
redress: high cost of care and variations in quality. major critiques of the HLEG report is its inadequate
The insurance model of UHC initiatives rests on the appreciation of the fundamental rift between top-
fundamental principle of separating financing and down planning perspectives and demands of
provisioning (public finance with private practical and functioning UHC services.14-15
provisioning of healthcare) and the privileging of Continuing dialogue on the architecture and
Social Medicine (www.socialmedicine.info) - 88 - Volume 9, Number 2, October 2015
operationalization of UHC with different states in to be central to the UHC discourse (thus addressing
India is imperative. equity upfront), the UHC dialogue needs to go
beyond the health sector alone to align itself with
Equity lens in UHC other campaigns on the right to food or water “to
If UHC is about financing services to ensure create a broad people’s movement in the social
universality in accessibility and affordability, how sector.”8 The UHC debate in this context needs to
have inequalities in health been addressed in the be aligned with the comprehensive report of the
current debates on UHC? Does ensuring universal WHO Commission on Social Determinants of
coverage to health services translate in equity in Health (2008).17 While inter-sectoral actions in
population health? health are the way forward, the health sector itself
Financial barriers are only one of several could do a lot to address social determinants of
constraints that determine access to quality health including changes in clinical practice,
healthcare. Coverage as a term is inadequate to advocacy, education and training, and employment
address issues of equity as it does not necessarily conditions of health-sector workers.18-20 In his recent
encompass universal access to health, Access is plea for the inclusion of social determinants of
determined by factors such as physical accessibility, health in the current universal health coverage
financial affordability, and acceptability. There are debate and to address equity upfront, Marmot
also broader social determinants of health, and proposed using a monitoring framework for
healthcare is only one aspect of population health. measurements of health and healthcare indicators by
Inequalities and their impact on access to healthcare socio-economic status, age, geographical distri-
need to be more sharply addressed in the structure of bution or even education as markers of health
UHC. inequity.19 He cautioned that if a country is serious
Clearly, there are two distinct dimensions to about not merely ensuring universal access to health
inequality: the first has to do with the social services but equity in population health, it needs to
determinants of health. Studies of inequalities in work on the structural drivers of health inequity.
access to healthcare and healthcare outcomes, Another important dimension of inequity are the
though widely acknowledged in public health, are disparities in service provision. Inequalities in the
spoken of more in terms of “associations” (caste, distribution of human resources (along with absolute
class, age, gender) that impact healthcare access and shortage) have been a recurring problem in
outcome. An analytical understanding of how such accessing quality healthcare in India. India currently
inequalities translate into inequitable access, has 6.5 doctors per 10000 people, less than half the
vulnerability, and poor health outcomes is required. global average of 14.2 per 10000 people. Regional
Such an understanding would then inform the design inequalities are large and the distribution of
of mechanisms and processes through which health personnel is uneven in India. States like Tamil
inequities could be addressed. In this regard, the Nadu, Karnataka, Delhi, and Goa have a much
World Health Report (2013) rightly underscores the higher proportion of health personnel than states like
importance of research in informing relevant paths Haryana, Bihar and Uttar Pradesh.21 Though NRHM
to achieve universal health coverage. The goal is has sought to redress these to some extent,
universal but the many solutions and paths to the specifically in select states in the rural areas, UHC
goal need to be local.2 The paths to UHC need to be needs to further support these efforts by revisiting
cautiously nurtured to ensure that in the name of the quality of medical education, the development of
universality, it does not reinforce already existing better protocols and guidelines for service provision
inequalities.16 and care, and equipping personnel with the skills to
The HLEG both in its definition and in the report provide care with an equity lens. Narayan and
has devoted space to social determinants of health Narayan lament the HLEG’s inadequate attention to
both in terms of structural locations (caste, class, practical concerns like incentivising health providers
gender) and as well to plea for broader investments to work in disadvantaged areas, ensuring that
in cross-sectoral domains like food, sanitation, water continuing medical education supports the goal of
and housing. However like many other aspects of UHC, and developing health promotion strategies to
the report, modalities of implementation are far tackle health disparities.14
from clear. In order for social determinants of health Emphasis on human resources needs to be given
Social Medicine (www.socialmedicine.info) - 89 - Volume 9, Number 2, October 2015
a different dimension and focus: kinds of people, more constructive and collaborative manner. They
kinds of training, specific needs of different require a much more intense and informed debate
locations. Attention to these matters will lead to a than that which has surfaced in the current UHC
more people-centred health system. Lack of such a discourse. The strongest critique of the HLEG so far
vision shifts the focus of discussion to insurance and is its uncritical silence about the private sector
coverage rather than people per se. Without this which has fostered an increasingly powerful
discussion, UHC becomes simply an economic corporatization of healthcare with influence on
question of implementing financial and management health policies at the local, state, and national levels
solutions.21 Cautioning on a similar global trend, etc.14,15,23 The reason for such concern lies in the fact
Kutzin argues that discussions of financing that UHC discourse operates in the context of a
mechanisms in UHC need to be centrally linked to deeply entrenched commercialized private sector in
health system objectives and goals, namely equity in healthcare that privileges “individual responsibility
health, equity in finance and responsiveness of the and choice” over social solidarity raises ethical
system to the entire population.22 He rightly pleads dilemmas for designing a health service that is
for “getting the unit of analysis right” in the UHC universal and equitable.”22 The current and future
debate. We must focus the debates on UHC on directions of operationalizing UHC goal need to
questions of population and health system, rather engage with the power dynamics of this sector as
than on individual financing schemes to ensure regulation is not a technical but rather a political
coverage and utilization. question. In the absence of this discussion, current
public-private partnership arrangements in
Health system governance healthcare will be fraught with malpractice and
As is well known, the current state of public abuse of health financing mechanisms, over-
health in India is attributed to a large extent to poor medicalization of care, over-prescription of
governance of both the public and private health treatment services, and greater social exclusion of
sectors. How the UHC debate addresses this issue is vulnerable communities. Evidence on some of the
critical for retaining momentum and achieving its insurance programs has already indicated such
goal. Though the increasingly diverse private sector trends.9
cannot be ignored and needs to be roped in to
achieve this shared goal, it is important to work out Conclusion
effective mechanisms for an ideal mix of both If UHC is serious about ensuring the rights of all
public and private participation with well-defined Indian citizens to health, the predominant language
accountability mechanisms and processes. A much of commerce and finance needs to embrace a “social
more informed debate on what would work best in logic” that focuses on the “public” and on “health.”
24-25
terms of practical mechanisms of public-private mix It has long been acknowledged that a model that
is required. What have been the experiences so far focuses on health without considering its social
in the Public-Private Partnerships experiments? determinants is cost-intensive and not sustainable. It
How are lessons from such experiments fed into the would be a missed opportunity if we restrict UHC to
UHC debates? How could regulation and financial coverage and to curative healthcare alone.
accountability be enhanced in the private sector Though discussed in the context of India, this
considering that mainstream approaches to regulate concern is expressed widely as part of the global
private sector don’t work? What could be alternative movement on UHC.26 UHC is a shared goal and the
innovative mechanisms to regulate and govern the paths to achieve this goal traverse through
private sector? What have been the experiences of continuing and intense dialogues among different
different states on private sector regulations? We stakeholders in the society: political parties, policy
need to understand the differences between public makers, research and academic community, civil
and private health sectors and the power dynamics society and community. Such multi-pronged
within the private sector taking into account the dialogues are an imperative to construct a
huge diversity that is typical of this sector. However “progressive hegemony” around the concept of
within these frameworks of difference, what fruitful UHC.15 Experiences of other countries show that a
partnerships can be created and how can they help strong political commitment to health as a social
each other? These questions need to be explored in a goal, upholding strong values of equity, political
Social Medicine (www.socialmedicine.info) - 90 - Volume 9, Number 2, October 2015
participation and community involvement, go a long Economic and Political Weekly. 2011 Dec XLVI
way in ensuring health for all. India needs to fall (49):38-42.
back on these experiences to garner strong political 10. Dasgupta M, Muraleedharan VR Universal health
will to recognize UHC as a social and political goal coverage: Reform of the Government system better
than quality health insurance. Economic and Political
and a basic human right.
Weekly. 2014 XLIX (35):29-32.
11. Sodhi C, Rabbani, A. Health service system in India:
References Is insurance the way forward? Economic and Political
1. The Planning Commission. High Level Expert Group Weekly. 2014 XLIX (35):26-28.
on Universal Health Coverage. [Internet] New Delhi: 12. Ministry of Health and Family Welfare. National
Government of India. 2011. 323 p. Available from: Health Policy 2015 Draft. [Internet] New Delhi:
http://planningcommission.nic.in/reports/genrep/rep_ Ministry of Health & Family Welfare; 2014 Dec;
uhc0812.pdf Available at:
2. World Health Organization. World Health Report http://www.thehinducentre.com/multimedia/archive/0
2013: Research for universal health coverage. 2263/Draft_National_Hea_2263179a.pdf
Geneva: WHO; 2013 [cited 2015 Oct 10] 146 p. 13. Government of India (2005) The National Rural
Available from: Health Mission – Mission Document available from:
http://apps.who.int/iris/bitstream/10665/85761/2/978 http://www.nird.org.in/brgf/doc/Rural%20HealthMiss
9240690837_eng.pdf?ua=1 ion_Document.pdf
3. Health Survey and Development Committee. Report 14. Narayan R, Narayan T. Editorial: Universal health
of the Health and Development Committee survey. coverage for India: Now is the time to move beyond
Government of India. Calcutta: Government of India rhetoric and get the action right. BMJ 2012:344:e2247
Press; 1946 [cited 2015 Oct 10] 232 p. Available 15. Srivastan R, Shatrugna V. Political Challenges to
from: universal access to healthcare. Economic and Political
http://sihfwrajasthan.com/Reports/bhore%20Commit Weekly. 2012 Feb. XLVII(8).
tee%20Report%20VOL-1%20.pdf 16. Gwatkin, DR, Alex E. Universal health coverage:
4. Ministry of Health and Family Welfare. National Friend or foe of health equity. The Lancet. 2010 Jun,
Health Policy. New Delhi: Government of India, 377(9784):2160-2161.
1983 17. Commission on Social Determinants of Health.
5. Office of the Registrar General, India. Sample Closing the gap in a generation: health equity through
Registration Bulletin 2012. New Delhi: Office of the action on the social determinants of health. Final
Registrar General; 2013 [cited 2013 May 18] Report of the Commission on Social Determinants of
available from: Health. Geneva:World Health Organization. 2008.
http://censusindia.gov.in/vital_statistics/SRS_Bulleti 18. Marmot, M. Universal health coverage and social
ns/SRS_Bulletin-2010-2012.pdf determinants of health, The Lancet, 2013 Oct
6. Balarajan, Y, Selvaraja, Subramanian, S.V. 382(9900):1227-1228.
Healthcare and equity in India, The Lancet, Special 19. Farmer, P., Nizeye, B. et al. Structural Violence and
Issue on Call for Action on Universal Health Clinical Medicine. PLoS Medicine 2006 3(10):1686-
Coverage. 2011 377(9664):510-515 1691.
7. Office of the Registrar General. Special Bulletin on 20. Wong ST, Browne AJ, Varcoe C, Lavoie J, Smye V,
Maternal Mortality in India 2007-09. [Internet] New et al. Enhancing measurement of primary health care
Delhi: Office of the Registrar General 2011. [cited indicators using an equity lens: An ethnographic
2013 May 18] 4 p. Available from: study. International Journal for Equity in Health. 2011
http://www.censusindia.gov.in/vital_statistics/SRS_ [cited 2014 Apr 20] 10(38). Available from:
Bulletins/Final-MMR%20Bulletin-2007- http://www.equityhealthj.com/content/10/1/38
09_070711.pdf 21. Kollannur A. Editorial: Will India deliver on
8. Sengupta A. Universal healthcare in India: Making it universal health coverage? British Medical Journal.
public, making it a reality. Occasional Paper No. 19 2013, 347:f5621.
[Internet] Ontario: Municipal Services Project; 2013 22. Kutzin J. Health financing for universal health
May [cited 2015 Oct 15]. 23 p. Available from: coverage and health system performance: Concepts
http://www.municipalservicesproject.org/sites/munic and implications for policy, WHO Bulletin, 2013 91:
ipalservicesproject.org/files/publications/Sengupta_ 602-611.
Universal_Health_Care_in_India_Making_it_Public 23. Baru R. A limiting perspective on universal health
_May2013.pdf coverage. Economic and Political Weekly. 2012 Feb
XLVII(8).
9. Shatrugna V, Shukla R, Srivatsan, R. Aarogyashri
healthcare Model: Advantage private sector,
Social Medicine (www.socialmedicine.info) - 91 - Volume 9, Number 2, October 2015
24. Sengupta, A, Belanger Dumontier Health for All 25. Sengupta A, Vandana P. Developing a truly universal
in India: Public, not “packaged”, Global Health Indian Health System: The problem of replacing
Check, 2013 available from: “Health for All” to “Universal access to care”. Social
http://www.globalhealthcheck.org/?author=49.or Medicine, 2011 6(2):69-72.
g/?p=1440 26. Latko B. et al. Comment: The growing movement for
universal health coverage. [Intenet] The Lancet, 2010
Jun, 377, June 25 377(9784):2161-2163.
Social Medicine (www.socialmedicine.info) - 92 - Volume 9, Number 2, October 2015
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- KDIGO 2023 CKD Guideline Public Review Draft 5 July 2023Document339 pagesKDIGO 2023 CKD Guideline Public Review Draft 5 July 2023oscar coreaNo ratings yet
- Asme PCC-2 - 2022 HighlightedDocument112 pagesAsme PCC-2 - 2022 HighlightedAhmed Shakir67% (3)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Rtac IomDocument130 pagesRtac Iomfarshan296015No ratings yet
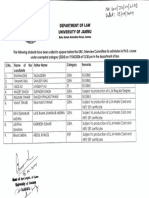
- PH.D Exempted Category in LawDocument1 pagePH.D Exempted Category in Lawrajsandhu25No ratings yet
- Notification AC 2024-2027Document3 pagesNotification AC 2024-2027rajsandhu25No ratings yet
- DSW Pre Summit Y20 Univ LevelDocument2 pagesDSW Pre Summit Y20 Univ Levelrajsandhu25No ratings yet
- Decision 16052007 11Document8 pagesDecision 16052007 11rajsandhu25No ratings yet
- JU-PG Admission (CUET-PG-2023) Notification-01-EDocument2 pagesJU-PG Admission (CUET-PG-2023) Notification-01-Erajsandhu25No ratings yet
- LM 101Document326 pagesLM 101rajsandhu25No ratings yet
- RFP - Legal Literacy and Legal Awarness Programme-DISHA 2021Document45 pagesRFP - Legal Literacy and Legal Awarness Programme-DISHA 2021rajsandhu25No ratings yet
- Terms and Conditions of Lenskart VoucherDocument1 pageTerms and Conditions of Lenskart Voucherrajsandhu25No ratings yet
- Zoology (OBC)Document1 pageZoology (OBC)rajsandhu25No ratings yet
- Central Information Commission, Baba Gangnath Marg, MunirkaDocument12 pagesCentral Information Commission, Baba Gangnath Marg, Munirkarajsandhu25No ratings yet
- Status RCP Courtcases 25.2.2015RCP PDFDocument3 pagesStatus RCP Courtcases 25.2.2015RCP PDFrajsandhu25No ratings yet
- Cic-Decisions: Work Shop On RTI ActDocument51 pagesCic-Decisions: Work Shop On RTI Actrajsandhu25No ratings yet
- Central Information CommissionDocument3 pagesCentral Information Commissionrajsandhu25No ratings yet
- Salient Features of National Health Policy 2017Document7 pagesSalient Features of National Health Policy 2017rajsandhu25No ratings yet
- Legal Rights of Refugees in IndiaDocument124 pagesLegal Rights of Refugees in Indiarajsandhu25No ratings yet
- Because Anno Domini Means "In The Year of The LordDocument1 pageBecause Anno Domini Means "In The Year of The Lordrajsandhu25No ratings yet
- Marketing-Plan-Ken Andrei L.Document4 pagesMarketing-Plan-Ken Andrei L.Kyle LapuzNo ratings yet
- 11-Try-In and Cementation of CrownsDocument10 pages11-Try-In and Cementation of CrownsElias EspinozaNo ratings yet
- Distemper VaccineDocument13 pagesDistemper VaccineAlberto ChongNo ratings yet
- Sexuality, Class and Role in 19th-Century America. Ch. E. RosenbergDocument24 pagesSexuality, Class and Role in 19th-Century America. Ch. E. RosenbergJosé Luis Caballero MartínezNo ratings yet
- Time Management at WorkplaceDocument10 pagesTime Management at WorkplaceStudy Material100% (1)
- Bar On Emotional Quotient InventoryDocument26 pagesBar On Emotional Quotient InventoryVANSHAJ JHA100% (1)
- Fitness & Wellness Industry in IndiaDocument12 pagesFitness & Wellness Industry in IndiaPrince SinghNo ratings yet
- Family Friendly UK Resource Sample Policy: Maternity, Adoption and Parental Leave PolicyDocument3 pagesFamily Friendly UK Resource Sample Policy: Maternity, Adoption and Parental Leave PolicycobbymarkNo ratings yet
- Chapter 3 ExercisesDocument4 pagesChapter 3 ExercisesK60 NGUYỄN THỊ HƯƠNG QUỲNHNo ratings yet
- Methas Arunnart MDDocument38 pagesMethas Arunnart MDjackie funtanillaNo ratings yet
- 1.seema Sanghi, "The Handbook of Competency Mapping: Understanding, Designing and Implementing Competency Model in An Organization"Document24 pages1.seema Sanghi, "The Handbook of Competency Mapping: Understanding, Designing and Implementing Competency Model in An Organization"Arun Ajith100% (1)
- Office of The Punong BarangayDocument4 pagesOffice of The Punong BarangayDona JojuicoNo ratings yet
- Legend: Wind Speed Hazard (M/S)Document1 pageLegend: Wind Speed Hazard (M/S)peshoaNo ratings yet
- Base Line Reform Updated MahideremariamDocument2 pagesBase Line Reform Updated MahideremariamDebrie YalewNo ratings yet
- The Truth About Cocaine and CrackDocument15 pagesThe Truth About Cocaine and Crackapi-616433899No ratings yet
- Fady Magdy Selim Fahmy: EducationDocument4 pagesFady Magdy Selim Fahmy: Educationfido30No ratings yet
- Mental Health of High Preformance AthletesDocument7 pagesMental Health of High Preformance AthletesKayla WorachekNo ratings yet
- RLYXU2 LP Easy-To-Use GuideDocument26 pagesRLYXU2 LP Easy-To-Use GuidePopescu MihaelaNo ratings yet
- STG 4thDocument1,239 pagesSTG 4thFentahun workieNo ratings yet
- Patient Specific Functional Scale PDFDocument1 pagePatient Specific Functional Scale PDFabhimanyu thakurNo ratings yet
- Rekap QCDocument13 pagesRekap QCWidy PrastiantoNo ratings yet
- DLL P.E. Q3 Week 1&2Document3 pagesDLL P.E. Q3 Week 1&2Vernadette HidalgoNo ratings yet
- Resume Maggy 2023Document1 pageResume Maggy 2023api-666488835No ratings yet
- Smidt (2009) - The Kirkpatrick Model, A Useful Tool For Evaluating Training OutcomesDocument10 pagesSmidt (2009) - The Kirkpatrick Model, A Useful Tool For Evaluating Training OutcomesLyra PuspaNo ratings yet
- Labsheet Fitting OfficialDocument11 pagesLabsheet Fitting OfficialSeb testaccountNo ratings yet
- Safety Officer Application - BWCDocument4 pagesSafety Officer Application - BWCBer Salazar JrNo ratings yet
- E Communication PDFDocument5 pagesE Communication PDFKhris Espinili AlgaraNo ratings yet