Professional Documents
Culture Documents
10 1016@j Ijom 2013 07 654
10 1016@j Ijom 2013 07 654
Uploaded by
DrGurkirpal Singh MarwahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1016@j Ijom 2013 07 654
10 1016@j Ijom 2013 07 654
Uploaded by
DrGurkirpal Singh MarwahCopyright:
Available Formats
21st ICOMS 2013 - Abstracts: Oral Papers 1355
T33.OR001 T33.OR003
Description of six trigeminal neurinomas with different location and extension. Analyze of
differents surgical approaches
T33.Skull Base Surgery
A. Encinas Bascones 1,∗ , T. Garcia 2 , S. Rosón 3 , C. Colmenero Ruiz 3
Trans-oral posterior maxillary craniofacial surgery to place a sphenopalatine ganglion (SPG) 1 Hospital Clinico San Carlos, Spain
neurostimulator for treatment of chronic cluster headache (CCH): pathway studies – Hamburg, 2 Hospital Universitario de la Princesa, Spain
Germany surgical experience 3 Private Practice, Madrid, Spain
A.T. Assaf 1,∗ , M. Blessmann 1 , J. Klatt 1 , P. Pohlenz 1 , T. Jürgens 2 , M. Heiland 1 , A. May 2
Objectives: To analyze the surgical management of six trigeminal neurinomas and the different
1 Department of Oral and Maxillofacial Surgery, University Medical Center Hamburg Eppendorf, approaches performed by our neurosurgery and maxillofacial team.
Martinistrasse 52, 20246 Hamburg, Germany Material and methods: We present six cases of trigeminal neurinoma with a massive involve-
2 Department of Systems Neuroscience, University Medical Center Hamburg Eppendorf, Martinis- ment of the skull base. The tumours presented extension to the infratemporal fossa and the masticatory
trasse 52, 20246 Hamburg, Germany space. All cases presented invasion of the cavernous sinus. One case demonstrated an invasion of the
infratemporal fossa, another the posterior fossa and one case growed along the third trigeminal branch
Aim: A new trans-oral surgical approach to the SPG has gained importance due to a new neu- to the lower lip.
rostimulation therapy for the treatment of CCH, which is in clinical trials currently. In our center, we Discussion: The surgical approach was a facial translocation in four cases and a preauricular-
have evaluated the morbidity of this approach for the treatment of CCH. subtemporal approach in two cases. Mandibular osteotomies were performed in five cases. The skull
Methods: Patients meeting the criteria for CCH were implanted with a miniaturized neurostim- base defect was reconstructed in four cases with a temporalis muscle flap and in two cases with a
ulator using a minimally invasive trans-oral technique in the dorsal mid facial region as a part of either rectus abdominis myocutaneous microvascular flap. All cases had a total tumour excision. Only two
the Pathway CH-1 study or the Pathway CH Registry. All patients were implanted under general anes- complications were observed: eyelid retraction and facial paresis. After a postoperative follow-up of
thesia with the use of intraoperative 3D CT imaging. Surgical follow-up examinations were performed 10 years, any tumoural recurrences were observed (0%). One patient died of malignant transformation
to assess adverse events related to the surgical procedure for implanting the neurostimulator. to neurosarcoma.
Results: 11 patients, 9 male and 2 female, with a mean age of 45 years of age, ranged 20–67 years Conclusions: Radical surgery is associated with an excellent clinical outcome and a good long-
of age with CCH were implanted with the ATI Neurostimulator. Most patients (10 of 11) experienced term tumour control.
typical side effects from this type of surgery, including post surgical swelling and loss of sensation in
the surgical area with an average time to resolution of 68.9 days, range 3–220 days, and 56.6 days,
http://dx.doi.org/10.1016/j.ijom.2013.07.655
range 31–94 days, respectively. Three patients experienced neurostimulation revision procedures, two
due to misplacement of the Neurostimulator lead and one due to lack of efficacy. Efficacy from the T33.OR004
implanted ATI Neurostimulator has been very good, of the 7 patients that have been implanted for 1
year, 6 have responded to SPG stimulation. Three achieve pain relief in >50% of acute headaches and Sphenopalatine ganglion (SPG) neurostimulator placement for treatment of severe headaches
3 experience a >50% reduction in headache frequency with SPG stimulation at one year. using a trans-oral posterior maxillary approach
Conclusion: The trans-oral surgical approach for implantation of the neurostimulator for SPG
stimulation to treat CCH has surgical morbidity consistent with the morbidity reported for other S. Hillerup 2,∗ , M. Puche 3 , M. Blessmann 4 , O. Müller 5 , A. Wilmont 7 , P. Pohlenz 4 ,
trans-oral procedures. D.Fontaine 6 , A. Caparso 1 , F. Papay 8
1 Autonomic Technologies, Inc., United States
http://dx.doi.org/10.1016/j.ijom.2013.07.653 2 Department of Oral and Maxillofacial Surgery, Rigshospitalet and Dental School, University of
Copenhagen, Copenhagen, Denmark
T33.OR002 3 Department of Oral and Maxillofacial Surgery, University of Valencia, Valencia, Spain
4 Department of Oral and Maxillofacial Surgery, University Medical Center Hamburg-Eppendorf,
Approximation to facial translocation: surgical approach to nasosinusal tumours with skull
Hamburg, Germany
base involvement 5 Department of Neurosurgery, University Hospital Essen, Essen, Germany
6 Department of Neurosurgery, Hôpital Pasteur, Nice, France
A. De Pablo García-Cuenca ∗ , D. Malet Hernández, C. Bescós Atín
7 Department of Maxillofacial Head and Neck, Plastic and Reconstructive Surgery – CHR de la
Hospital Vall D’Hebrón, Department of Oral and Maxillofacial Surgery, Spain Citadelle, Liège University, Liège, Belgium
8 Dermatology and Plastic Surgery Institute, Institute Chair, Cleveland Clinic, Cleveland, OH, United
Introduction: The facial translocation approach provides a good surgical exposure and tridi- States
mensional resection of tumours located in the nasopharynx and skull base. Our aim is to present our
case series to show the surgical field obtained by facial translocation combined with other resections. Background and objectives: The SPG plays a primary role in the pathogenesis of pain and
Materials and methods: A retrospective revision is presented of the facial translocation cases autonomic symptoms associated with primary headaches. Our objective is to analyze the results from
(standard or either associated to maxillectomy and/or orbital exenteration) performed by our Depart- the initial surgical experiences.
ment. The cases included required this approach for nasosinusal tumour ablation, benign or malignant, Methods: Patients were implanted with a miniaturized neurostimulator using a minimally inva-
with skull base involvement. sive trans-oral technique under general anaesthesia. The neurostimulator, which consists of an integral
Results: A total of 11 cases are presented, including 8 malignant tumours (4 sarcomas, 1 adenoid lead, body and fixation plate, is implanted such that the distal lead is within the pterygopalatine fossa
cystic carcinoma, 2 squamous cell carcinomas, and 1 basosquamous carcinoma) and 3 benign (1 and the fixation plate is anchored on the zygomaticomaxillary buttress.
fibrous dysplasia, 1 ameloblastoma, 1 cylindroma). 8 cases included a maxillectomy and in 7 cases Results: Ninety patients have undergone implantation of the ATITM Neurostimulator. Surgeries
and orbital exanteration was performed. have been performed by 14 surgeons; 97% of cases have resulted in successful implantation and no
Conclusions: Facial translocation is indicated for resection of big benign and malignant low infections resulting in explants occurred. With experience, the absolute time and standard deviation of
grade tumours affecting the nasosinusal territory with skull base involvement. Its main disadvantage the surgical duration is reduced by a third. Typical post surgical adverse events were reported, including
is the lack of cervical neurovascular control, and it can produce aesthetic sequelae. sensory nerve dysfunction and pain, in most patients. These surgical sequelae are typically mild and
Key words: facial translocation; nasosinusal tumours; skull base resolve within 90 days. These sequelae and their severities have decreased since the introduction of
a new surgical instrument.
Conclusions: The initial experience with this procedure has shown an acceptable safety profile
http://dx.doi.org/10.1016/j.ijom.2013.07.654
and risk-benefit profile for patients who suffer from severe, medically intractable headaches.
http://dx.doi.org/10.1016/j.ijom.2013.07.656
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- NICU - Policies, Procedures and ProtocolsDocument190 pagesNICU - Policies, Procedures and Protocolskrishnasree100% (3)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Тести, розділені за темамиDocument361 pagesТести, розділені за темамиАнна Олексіївна ГайченкоNo ratings yet
- Management of Epistaxis in Patients On Anti-Platelet And/ or Anticoagulant MedicationDocument6 pagesManagement of Epistaxis in Patients On Anti-Platelet And/ or Anticoagulant MedicationDrGurkirpal Singh MarwahNo ratings yet
- Organic Vapour List PDFDocument1 pageOrganic Vapour List PDFDrGurkirpal Singh MarwahNo ratings yet
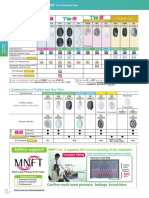
- Reusable & Disposable Respirator For Particle: Japanese Government StandardsDocument1 pageReusable & Disposable Respirator For Particle: Japanese Government StandardsDrGurkirpal Singh MarwahNo ratings yet
- Coulthard 2006Document1 pageCoulthard 2006DrGurkirpal Singh MarwahNo ratings yet
- Reusable Respirator: Particle FilterDocument1 pageReusable Respirator: Particle FilterDrGurkirpal Singh MarwahNo ratings yet
- 1 s2.0 S0901502709009941 MainDocument6 pages1 s2.0 S0901502709009941 MainDrGurkirpal Singh MarwahNo ratings yet
- Code For Identification of Gas-Mask Canisters: United States Department of LaborDocument9 pagesCode For Identification of Gas-Mask Canisters: United States Department of LaborDrGurkirpal Singh MarwahNo ratings yet
- Flexible Contribution Tenure With 25 Years of Protection: HSBC Takaful Future SmartDocument6 pagesFlexible Contribution Tenure With 25 Years of Protection: HSBC Takaful Future SmartmiazainuddinNo ratings yet
- Cerebral Palsy Research PaperDocument6 pagesCerebral Palsy Research Paperapi-354964737No ratings yet
- Best Gallbladder Removal Surgery in Pune - Kaizen Gastro CareDocument3 pagesBest Gallbladder Removal Surgery in Pune - Kaizen Gastro CareKaizen Gastro CareNo ratings yet
- A Study On Molecular Diagnosis of Theileria Species Infection by PCR Amplification in Sheep and Goats in Multan, PakistanDocument10 pagesA Study On Molecular Diagnosis of Theileria Species Infection by PCR Amplification in Sheep and Goats in Multan, PakistanAhmad RazaNo ratings yet
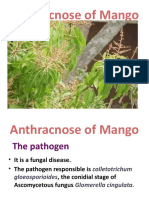
- Anthracnose of MangnoDocument22 pagesAnthracnose of MangnoLINTA JOSEPHNo ratings yet
- TheileriosisDocument10 pagesTheileriosisSomesh SharmaNo ratings yet
- Hypertension CaseDocument3 pagesHypertension CaseArnold Christian QuilonNo ratings yet
- Prevalence of Hypoalbuminemia in Outpatients With HIV/AIDS: ArticleDocument5 pagesPrevalence of Hypoalbuminemia in Outpatients With HIV/AIDS: ArticleMUHAMMAD BAGIR ALJUFRINo ratings yet
- Effectiveness of Proprioceptive Neuromuscular FacilitationDocument4 pagesEffectiveness of Proprioceptive Neuromuscular FacilitationMuhajir AjiNo ratings yet
- Bombay Hospital: Medical CertificateDocument1 pageBombay Hospital: Medical CertificateSandeep ShahNo ratings yet
- اختصارات المندوه ObstetricsDocument11 pagesاختصارات المندوه ObstetricssamyNo ratings yet
- Libro Ciencia y TecnologiaDocument173 pagesLibro Ciencia y TecnologiaLorenzo FuentesNo ratings yet
- MICP211 LEC - CombinedDocument40 pagesMICP211 LEC - CombinedJULIANA NICOLE TUIBUENNo ratings yet
- Clinical Reasoning Assessment For Thinking Effectively CRAFTeDocument4 pagesClinical Reasoning Assessment For Thinking Effectively CRAFTejohn smithNo ratings yet
- Biochemistry Papers MSUDocument20 pagesBiochemistry Papers MSUShiv BhattNo ratings yet
- CAS-GEC04 Module5 Mortality-and-Fertility RPZubietoDocument4 pagesCAS-GEC04 Module5 Mortality-and-Fertility RPZubietoArvie TVNo ratings yet
- AnemiaDocument2 pagesAnemiaLazeh MeNo ratings yet
- Chapter 25 The Child With Cardiovascular DysfunctionDocument20 pagesChapter 25 The Child With Cardiovascular DysfunctionJill Hill100% (3)
- Peripheral Nerve Repair and Reconstruction PDFDocument9 pagesPeripheral Nerve Repair and Reconstruction PDFDea Alberta SNo ratings yet
- Avian InfluenzaDocument9 pagesAvian Influenzajazz100% (1)
- Plagiarism Checker X Originality Report: Similarity Found: 12%Document10 pagesPlagiarism Checker X Originality Report: Similarity Found: 12%Project DevelopmentNo ratings yet
- Vsim Nursing Assignment #1: Toua Xiong 501 Pathophysiology and Pharmacology Gelsey Jian University of Maryland School of Nursing 9/14/18Document7 pagesVsim Nursing Assignment #1: Toua Xiong 501 Pathophysiology and Pharmacology Gelsey Jian University of Maryland School of Nursing 9/14/18Gelsey Gelsinator JianNo ratings yet
- Nhls Handbook 2019Document337 pagesNhls Handbook 2019xhdrv7nvdrNo ratings yet
- Understanding The Circulatory SystemDocument7 pagesUnderstanding The Circulatory SystempiknameripNo ratings yet
- Antibiotics IN Maxillofacial Surgery: Presenter: Dr. Venu G.RDocument92 pagesAntibiotics IN Maxillofacial Surgery: Presenter: Dr. Venu G.RkatnevNo ratings yet
- Max Lab ReportDocument8 pagesMax Lab ReportKallu PrasadNo ratings yet
- Qdoc - Tips Urology Mcqs For Posgraduate ExamDocument62 pagesQdoc - Tips Urology Mcqs For Posgraduate ExamDALIANo ratings yet
- Nausea, Vomiting in Pregnancy & Hyperemesis Gravidarum, UPDATE 2024Document30 pagesNausea, Vomiting in Pregnancy & Hyperemesis Gravidarum, UPDATE 2024patsilwalNo ratings yet