Professional Documents
Culture Documents
3d Zygoma Reduction
3d Zygoma Reduction
Uploaded by
Rudolf KiraljOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
3d Zygoma Reduction
3d Zygoma Reduction
Uploaded by
Rudolf KiraljCopyright:
Available Formats
HEAD AND NECK SURGERY
Three-Dimensional Approach to Zygoma Reduction
Review of 221 Patients Over 7 Years
Minbum Kang, MD
focusing on reducing complications while achieving good results have
Background: Zygoma reduction is commonly performed in Asian patients be-
been developed. In the present study, a new surgical technique involving
cause a broad face is considered stubborn in appearance and unattractive. Con-
an L-shaped ostectomy pattern with a 3-dimensional approach to zygoma
sequently, a number of different techniques have been developed for zygoma
reduction was developed. In this surgical technique, the surgeon ap-
reduction, the majority of which involve simple manipulations. However, no con-
proaches the bone via intraoral and preauricular incisions and performs
sensus has been reached on the optimal method. In the present report, we intro-
a small L-shaped ostectomy. The bone segment is moved forward, in-
duce a new method involving ostectomy and fixation that uses a 3-dimensional
ward, and upward, and then fixed with an L-shaped miniplate and screws
approach to zygoma reduction.
(see Video 1, http://links.lww.com/SAP/A140). In the present study, we
Methods: From 2007 to 2013, 221 Korean patients (39 men, 182 women)
assessed the surgical outcomes and complications of this new surgical
underwent zygoma reduction using this technique. The bone was accessed via
technique in 221 Korean patients.
an intraoral and preauricular incision and removed in the body area using a small
L-shaped osteotome through bone cutting in the arch area. The zygoma was
moved anteriorly, medially, and caudally, and then fixed with a miniplate and screws. PATIENTS AND METHODS
Results: All patients were followed up for over 6 months and asked whether they From 2007 to 2013, 221 Korean patients (39 men, 182 women;
were satisfied with the results. Four patients (1.8%) required further reduction age range, 19–62 years) underwent zygoma reduction using this tech-
and underwent a reoperation, but all were eventually satisfied. Two patients nique (Table 1). Of these, 167 patients underwent zygoma reduction
(0.9%) experienced overcorrection with a sunken area around the zygoma, which alone, and 54 patients underwent additional procedures (Table 2). None
was corrected with autologous fat grafting after 6 months. Two patients complained of the patients had a history of trauma, and there were no secondary
of sensory changes around the upper lip, which resolved within 6 months. Two cases. Before surgery, frontal, profile, and lateral view photographs
patients experienced dizziness, temporomandibular joint pain, infection, and/or and cephalometric radiographs (Water's view and submentovertical
cheek drooping. view) were obtained. Then, surgical plans were established based
Conclusions: This new surgical technique causes less frequent and less pro- on evaluation of these radiographs and photographs (see Video 2,
nounced cheek drooping and requires less bone stepping, resulting in greater http://links.lww.com/SAP/A140). All surgeries were performed under
patient satisfaction. general anesthesia. The preauricular incision was accurately planned
Key Words: zygoma reduction, malar reduction, facial contouring, to protect the frontal branch of the facial nerve. After injection of
facial bone reduction 0.25% lidocaine mixed with epinephrine (1:100,000) at the incision
sites, a preauricular incision was made and extended into the perios-
(Ann Plast Surg 2016;76: 51–56) teum using a Mosquito dissector. Complete subperiosteal dissection
was performed from the posterior arch to the body area. After careful
confirmation of complete dissection, an upper labiobuccal vestibular
I n Asia, individuals with a wide and short face (mesocephalic features)
often prefer to have a slender one because a prominent zygomatic
complex is considered to contribute to an unattractive, stubborn, and
incision was made from the bilateral canine fossae to the first molars.
Thereafter, periosteal dissection was performed via this incision medi-
aged appearance. Since Onizuka et al.1 first described a surgical tech- ally up to the inferior orbital nerve and superiorly up to the lateral or-
nique based on chiseling and shaving via an intraoral incision, a number bital rim with the upper portion of the zygoma body (Fig. 1). For the
of different surgical techniques have been developed for reducing malar anterior part of the insertion, the masseter muscle was detached using
bone volume.1–10 Current surgical methods can be divided based on electrocautery. After complete dissection of the zygoma body, the surgi-
the following aspects: (1) type of approach: coronal incision,3 intraoral cal outline was marked with a pencil. Thereafter, parallel osteotomy was
incision,4,6,7,9–11 or a combination of intraoral and preauricular inci- performed using a reciprocating saw (bone segment width, 4–6 mm).
sions5,8; and (2) type of ostectomy: parallel,5 large L-shaped,6,8 or small After 2 oblique osteotomies and 1 vertical osteotomy, the bone segment
L-shaped.11,12 Other aspects include shaving or grinding,7 involvement was removed. Two-point fixations with an L-shaped miniplate and
of a greenstick fracture,4 and type of bone fixation.9,10 Most surgeons screws were performed in the zygoma area. The arch under the
perform zygoma reduction using simple manipulations to avoid scarring, preauricular incision was fully cut and detached using an osteotome.
facial nerve injury, and cheek drooping; thus, a number of techniques Thereafter, the bone segment was moved anteriorly, medially, and cau-
dally, and repositioning was confirmed. In the body area, complete
bony contact was accomplished, and 2 additional screws were fixed
(Fig. 2). Wound closure was performed using 3-0 chromic sutures after
Received November 12, 2014, and accepted for publication, after revision April 14, 2015. saline irrigation. Compressive dressing was applied for 3 days. Most
From the Romian Plastic Surgery Clinic, Seoul, Republic of Korea. patients were discharged 4 or 5 hours postoperatively, but some were
Conflicts of interest and sources of funding: none declared. admitted for 1 day if they experienced pain or bleeding.
Reprints: Minbum Kang, MD, Romian Plastic Surgery, Clinic 8F, Glass
Tower, 406 Gangnam-daero, Gangnam-gu, Seoul 135-080, Republic of
Korea. E-mail: minbum.kang@gmail.com.
Minbum Kang designed the study, analyzed the data, and wrote the article.
RESULTS
Supplemental digital content is available for this article. Direct URL citations appear in All patients were followed up for over 6 months and asked
the printed text and are provided in the HTML and PDF versions of this article on whether they were satisfied with the results. Four patients (1.8%) re-
the journal's Web site (www.annalsplasticsurgery.com).
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
quired further reduction and underwent a reoperation at 6 months or
ISSN: 0148-7043/16/7601–0051 more after the primary operation. These patients reported subsequent
DOI: 10.1097/SAP.0000000000000548 satisfaction. Two patients (0.9%) experienced overcorrection with a
Annals of Plastic Surgery • Volume 76, Number 1, January 2016 www.annalsplasticsurgery.com 51
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Kang Annals of Plastic Surgery • Volume 76, Number 1, January 2016
Current surgical methods can be divided according to approach,
TABLE 1. Patient Classification Based on Age and Sex (n) osteotomy sites, fixation sites, and materials used.
The use of 3 approaches has been reported: coronal, intraoral,
Age, y Male Female Total and a combination of intraoral and external. Coronal approaches2 offer
<20 0 4 4 the advantage of reduction of the upper part of the zygoma and wide
21–30 23 84 107 exposure.11 If needed, a forehead lift can be performed concomitantly.
31–40 11 60 71 However, a coronal approach cannot be used to manage the inferior part
of the zygoma and may potentially result in a scalp scar. Kim and Seul6
41–50 4 25 29
and Gui et al11 reduced the zygoma body via an intraoral approach
51–60 0 9 9 alone, but the part of the body that was ostectomized differed. Kim
>60 1 0 1 and Seul5 included the inferior part of the maxilla, which can provide
Total 39 182 221 the maxillary sinus opening, but has fixation problems due to the thin
anterior wall. Gui et al11 removed the bone in the upper part of the
maxilla and zygoma body, and performed an osteotomy with 1 oblique
sunken area around the zygoma area, which was corrected with auto- osteotomy line and 2 vertical osteotomy lines. Our method is similar to
logous fat grafting at 6 months after surgery. One patient had pain in this previous study with respect to the part of bone that is ostectomized.
the temporomandibular joint area for 7 months, which resolved with However, we also removed the more posterior part after 2 oblique
mouth-opening exercises. Two patients experienced dizziness, were osteotomy lines and 1 vertical osteotomy line. Moreover, we used a
transferred to the ear, nose, and throat clinic, and were confirmed to preauricular incision for cutting the posterior part of the arch (Fig. 2).
have tinnitus. One patient developed an infection in an oral wound The anterior part of the masseter muscle detachment is essential for
and received intravenous ceftriaxone treatment for 1 week. Two patients providing an area for fixation. Many other surgeons have reported
experienced a sensory deficit around the upper lip, which resolved after methods using intraoral and preauricular incisions.4,5,8,12 Parallel
6 months. One patient complained of cheek drooping, but no other pro- ostectomy5 or shaving4 has been performed using an intraoral incision.
cedure was required (Table 3). Yang and Chung4 introduced a technique using a greenstick fracture
and preauricular fixation with miniplates and screws. Risk of facial
nerve injury is increased with this method; however, limitations with
CASE REPORTS respect to reduction are present, particularly with the body area. Lee
et al9 introduced a blind technique with rasping and sawing. Yang and
Case 1 Chung4 and Lee et al9 both reported use of a greenstick fracture in
A 25-year-old woman complained of a broad face that resulted in the body area. These techniques did not include fixation after bone
a masculine appearance. She underwent angle resection and tubercles cutting or the need for a greenstick fracture, but are associated with
excision concomitant with zygoma reduction. She was satisfied with the following issues: (1) nonunion or malunion can occur after bone
the results (Figs. 3, 4). cutting; (2) greenstick fracture is difficult to accurately perform until
the surgeon has acquired considerable experience with the technique;
Case 2 and (3) evidence of worsened sensory problems and nerve damage
from the fixation materials has been observed.
A 32-year-old woman complained of a prominent zygoma and The concept of malar reduction has changed from rasping and
facial angle, an antimongolian slant and epicanthus, and a flat forehead. rotation4,7,10 to body repositioning.11–13 Wide periosteal elevation is
She underwent mandible angle resection with tubercles excision, lateral thought to be a cause of cheek drooping. However, in the present study,
and medial canthoplasty, and autologous fat grafting of the forehead the zygoma was moved upward, forward, and inward after full periosteal
and nose. She was satisfied with the results (Figs. 5, 6). elevation, suggesting that wide periosteal elevation can be performed
without a high incidence of this complication. Gui et al11 reported min-
Case 3 imal periosteal dissection, short operating time, and wearing elastic fa-
A 22-year-old woman complained of a prominent zygoma and cial dressing as 3 factors to help avoid cheek drooping. However, face
flat nose. She underwent zygoma reduction and augmentation rhino-
plasty with a silicone implant. She was satisfied with the results (Fig. 7).
DISCUSSION
In Asia, reduction malarplasty has been performed increasingly
over the past decade. The aim of this procedure is to obtain softer and
rounder facial contours. Since Onizuka et al.1 reported bone shaving
via an intraoral incision, many other methods have been introduced.
TABLE 2. Patient Classification According to Surgeries Performed
Concomitantly With Zygoma Reduction (n)
No concomitant surgeries 167
Angle resection, tubercles excision 6
Angle resection 14
Rhinoplasty 33
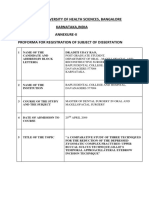
Angle resection, rhinoplasty 1 FIGURE 1. The periosteal dissection area, marked using a blue
pencil, is noted during zygoma reduction.
52 www.annalsplasticsurgery.com © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Annals of Plastic Surgery • Volume 76, Number 1, January 2016 Zygoma Reduction for Facial Contouring
FIGURE 2. Three-dimensional aspects of the operative procedure for zygoma reduction. A, Ostectomy of the malar area with 2 vertical
lines and an oblique line. B, Fixation of a small L-shaped miniplate before preauricular osteotomy. C, Fixation with screws after
preauricular osteotomy. D, Movement of the zygoma anteriorly, medially, and caudally.
lifting was required in 5.3% of patients in this previous study. Only incision. The present technique used a preauricular incision for full dis-
1 patient (0.45%) in the present study underwent face lifting despite un- section of the outer periosteum and accurate oblique bone cutting. An-
dergoing full periosteal dissection. This difference could be the result other option for avoiding cheek drooping is removal of buccal fat.
of differing direction of bone interventions between studies. In particu- In summary, this new technique has several essential features:
lar, Gui et al11 moved the bone downward, and used only an intraoral (1) full elevation of the outer periosteum of the zygoma; (2) masseter
FIGURE 3. (above) Preoperative views of a 25-year-old patient who complained of a broad face that resulted in a masculine impression.
She underwent a combination of zygoma reduction and angle resection with tubercles excision. (Below) Six-month postoperative
view. Smooth facial lines were achieved without any complaints.
© 2015 Wolters Kluwer Health, Inc. All rights reserved. www.annalsplasticsurgery.com 53
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Kang Annals of Plastic Surgery • Volume 76, Number 1, January 2016
FIGURE 4. (Left) Preoperative and postoperative submental view. (Right) Preoperative and postoperative Water's view.
FIGURE 5. (Above) Preoperative views of a 32-year-old patient who complained of a prominent zygoma and facial angle, an
antimongolian slant and epicanthus, and a flat forehead. She underwent angle resection of the mandible with tubercles excision,
lateral and medial canthoplasty, and autologous fat grafting of the forehead and nose. She was satisfied with the results. (Below)
One-year postoperative views.
54 www.annalsplasticsurgery.com © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Annals of Plastic Surgery • Volume 76, Number 1, January 2016 Zygoma Reduction for Facial Contouring
FIGURE 6. (Left) Preoperative and postoperative submental view. (Right) Preoperative and postoperative Water's view.
FIGURE 7. (Above) Preoperative views of a 22-year-old patient who complained of a prominent zygoma and flat nose. She underwent
zygoma reduction and augmentation rhinoplasty with a silicone implant. She was satisfied with the results. (Below) One-year
postoperative views.
© 2015 Wolters Kluwer Health, Inc. All rights reserved. www.annalsplasticsurgery.com 55
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Kang Annals of Plastic Surgery • Volume 76, Number 1, January 2016
ACKNOWLEDGMENT
TABLE 3. Complications During the Postoperative Period Informed consent was received for publication of the figures in
this article.
Complication (<6 mo) No. Patients Treatment
Bleeding 0 Admission for 1 day REFERENCES
TMJ pain 1 None 1. Onizuka T, Watanabe K, Takasu K, et al. Reduction malarplasty. Aesthetic Plast
Dizziness (tinnitus) 2 Transfer to ENT clinic Surg. 1983;7:121–125.
Infection 1 Daily IV antibiotic treatment for 3 d 2. Satoh K, Watanabe K. Correction of prominent zygomata by tripod osteotomy of
the malar bone. Ann Plast Surg. 1993;31:462–465.
Sensory change 2 None 3. Satoh K, Ohkubo F, Tsukagoshi T. Consideration of operative procedures for
Undercorrection 4 Revision zygomatic reduction in Orientals: based on a consecutive series of 28 clinical
Cheek drooping 1 None cases. Plast Reconstr Surg. 1995;96:1298–1306.
Bone nonunion 0 None 4. Yang DB, Chung JY. Infracture technique for reduction malarplasty with a short
preauricular incision. Plast Reconstr Surg. 2004;113:1253–1263.
Overcorrection 2 Fat graft 5. Sumiya N, Kondo S, Ito Y, et al. Reduction malarplasty. Plast Reconstr Surg.
1997;100:461–467.
ENT, ear, nose, throat; IV, intravenous; TMJ, temporomandibular joint.
6. Kim YH, Seul JH. Reduction malarplasty through an intraoral incision: a new
method. Plast Reconstr Surg. 2000;106:1514–1519.
7. Lee JG, Park YW. Intraoral approach for reduction malarplasty: a simple method.
muscle insertion site detachment for miniplate fixation; (3) 2 vertical Plast Reconstr Surg. 2003;111:453–460.
osteotomy lines that need to be in parallel; (4) movement of the poste- 8. Lee KC, Ha SU, Park JM, et al. Reduction malarplasty by 3-mm percutaneous
rior bone upward, forward, and inward (Fig. 2); and (5) removal of the osteotomy. Aesthetic Plast Surg. 2006;30:333–341.
buccal fat, if needed. Of note, this technique has several potential dis- 9. Lee HY, Yang HJ, Cho YN. Minimally invasive zygoma reduction. Plast Reconstr
Surg. 2006;117:1972–1979.
advantages, including preauricular osteotomy site malunion and bone
10. Hwang YJ, Jeon JY, Lee MS. A simple method of reduction malarplasty. Plast
widening in the malar area. Reconstr Surg. 1997;99:348–355.
11. Wang T, Gui L, Tang X, et al. Reduction malarplasty with a new L-shaped
osteotomy through an intraoral approach: retrospective study of 418 cases. Plast
CONCLUSIONS Reconstr Surg. 2008;124:1245–1253.
12. Ma YQ, Zhu SS, Li JH, et al. Reduction malarplasty using an L-shaped
The concept of this new technique is bone rearrangement after osteotomy through intraoral and sideburns incisions. Aesthetic Plast Surg.
ostectomy. There was no evidence to indicate that this technique re- 2011;35:237–241.
sulted in increased scarring, nerve damage, or dissatisfaction compared 13. Mendelson BC, Muzaffar AR, Adams WP Jr. Surgical anatomy of the midcheek
with other techniques. and malar mounds. Plast Reconstr Surg. 2002;110:885–896.
56 www.annalsplasticsurgery.com © 2015 Wolters Kluwer Health, Inc. All rights reserved.
Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved.
You might also like
- Nonsurgical Rhinoplasty With Polydioxanone Threads and FillersDocument8 pagesNonsurgical Rhinoplasty With Polydioxanone Threads and FillersRaphaela TravassosNo ratings yet
- A New Method To Eliminate The Risk of Maxillary Sinusitis With Zygomatic ImplantsDocument9 pagesA New Method To Eliminate The Risk of Maxillary Sinusitis With Zygomatic ImplantsCaioSelaimenNo ratings yet
- Genioplasty Oral SurgeryDocument45 pagesGenioplasty Oral SurgeryFourthMolar.com100% (2)
- Internal Nasal ValveDocument6 pagesInternal Nasal ValveAmmar EidNo ratings yet
- Sun 2015Document5 pagesSun 2015febyan yohanesNo ratings yet
- Modified Gap Arthroplasty and Myrhaugs Incision As A Treatment Option in Management of Temporomandibular Joint Ankylosis A Study of 10 CasesDocument6 pagesModified Gap Arthroplasty and Myrhaugs Incision As A Treatment Option in Management of Temporomandibular Joint Ankylosis A Study of 10 CasesS EllurNo ratings yet
- Cios 3 217 PDFDocument8 pagesCios 3 217 PDFantonio ferrerNo ratings yet
- Gliding Mentoplasty PDFDocument8 pagesGliding Mentoplasty PDFedmundo_mr3888No ratings yet
- Comparison of A New, Minimally Invasive Strabismus Surgery Technique With The Usual Limbal Approach For Rectus Muscle Recession and PlicationDocument7 pagesComparison of A New, Minimally Invasive Strabismus Surgery Technique With The Usual Limbal Approach For Rectus Muscle Recession and PlicationvikrizkaNo ratings yet
- EndoBL + Face RatioDocument8 pagesEndoBL + Face Ratiodrkorn.ophNo ratings yet
- Successful Treatment of Intraorbital Lymphangioma With Tissue Fibrin GlueDocument3 pagesSuccessful Treatment of Intraorbital Lymphangioma With Tissue Fibrin GlueIRANo ratings yet
- Root CoverageDocument4 pagesRoot CoverageRobins DhakalNo ratings yet
- 2015 Article 7Document7 pages2015 Article 7TikaZyka16No ratings yet
- Surgical Correction of Gynecomastia With Minimal Scarring: Multimediamanuscript AestheticDocument5 pagesSurgical Correction of Gynecomastia With Minimal Scarring: Multimediamanuscript AestheticAngga Putra Kusuma KusumaNo ratings yet
- Results and Complications of Alveolar Distraction Osteogenesis To Enhance Vertical Bone HeightDocument7 pagesResults and Complications of Alveolar Distraction Osteogenesis To Enhance Vertical Bone HeightKeval ModiNo ratings yet
- Using The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout FracturesDocument4 pagesUsing The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout Fracturesstoia_sebiNo ratings yet
- Facial Rejuve Arion Whit Fine ThreadsDocument6 pagesFacial Rejuve Arion Whit Fine Threads7rayosomonishangoNo ratings yet
- Kim (2021)Document8 pagesKim (2021)Caio GonçalvesNo ratings yet
- Kim 2015Document6 pagesKim 2015Juliana Gomes BarretoNo ratings yet
- 19 - Capítulo 4.2 - 5-Choi e Colaboradores 2022Document9 pages19 - Capítulo 4.2 - 5-Choi e Colaboradores 2022CharleneNo ratings yet
- HFM Free Flap Versus Fat GraftingDocument10 pagesHFM Free Flap Versus Fat GraftingNelson LowNo ratings yet
- Treatment of Condylar Fractures With An Intraoral ApproachDocument26 pagesTreatment of Condylar Fractures With An Intraoral Approachdhiraj.2367No ratings yet
- Techniques in Lower Extremity Reconstruction With SupermicrosurgeryDocument5 pagesTechniques in Lower Extremity Reconstruction With SupermicrosurgeryManny TrujilloNo ratings yet
- Jandrol 112 016444Document7 pagesJandrol 112 016444Павел ГичакNo ratings yet
- Modified Incision For Maxillectomy: Our ExperienceDocument4 pagesModified Incision For Maxillectomy: Our Experiencedarmayanti ibnuNo ratings yet
- Surgical Stent and C-Arm Guided Reduction andDocument5 pagesSurgical Stent and C-Arm Guided Reduction andkityamuwesiNo ratings yet
- HKDJ 0401Document4 pagesHKDJ 0401Yiu Kai WongNo ratings yet
- SJAMS 43B 750 754 Thesis Tibial PlateauDocument5 pagesSJAMS 43B 750 754 Thesis Tibial PlateauNisheshJainNo ratings yet
- Cleaning and Shaping 2006 FinalDocument9 pagesCleaning and Shaping 2006 Finaldhiraj.2367No ratings yet
- Ishida 2016Document9 pagesIshida 2016stoia_sebiNo ratings yet
- 18 TH JC - SindhuDocument8 pages18 TH JC - SindhuDadi SindhuNo ratings yet
- Wang 2019Document10 pagesWang 2019Hải Dương MinhNo ratings yet
- JC - Endoscopic Techniques in OralDocument33 pagesJC - Endoscopic Techniques in OralNarla SusheelNo ratings yet
- Young KyunDocument6 pagesYoung Kyunodontologia uvNo ratings yet
- Guidelines For Single-Stage Correction of TMJ Ankylosis, Facial Asymmetry and OSA in AdultsDocument9 pagesGuidelines For Single-Stage Correction of TMJ Ankylosis, Facial Asymmetry and OSA in Adultsmehak malhotraNo ratings yet
- Short Nose Correction-By Man Koon SuhDocument4 pagesShort Nose Correction-By Man Koon SuhJW整形医院(JW plastic surgery)No ratings yet
- Endoscopic Endonasal Approaches To The Craniovertebral Junction The Otolaryngologist's Perspective, Schwartz 2020Document6 pagesEndoscopic Endonasal Approaches To The Craniovertebral Junction The Otolaryngologist's Perspective, Schwartz 2020CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- C-Arm Assisted Zygoma Fracture Repair: A Critical Analysis of The First 20 CasesDocument8 pagesC-Arm Assisted Zygoma Fracture Repair: A Critical Analysis of The First 20 CasesYeison HidalgoNo ratings yet
- Long-Term Changes of The Anterior Palatal Alveolar Bone After Treatment With Bialveolar Protrusion, Evaluated With Computed TomographyDocument10 pagesLong-Term Changes of The Anterior Palatal Alveolar Bone After Treatment With Bialveolar Protrusion, Evaluated With Computed TomographyMonojit DuttaNo ratings yet
- Aesth Plast Surg - 2019 - 43 - 652-657Document6 pagesAesth Plast Surg - 2019 - 43 - 652-657HemerobibliotecaHospitalNo ratings yet
- Coccygectomy Z PlastyDocument5 pagesCoccygectomy Z PlastyJayesh BhanushaliNo ratings yet
- Kjod 51 3 145Document12 pagesKjod 51 3 145Fabio RibeiroNo ratings yet
- Two Bilateral Zygomatic Implants Placed and Immediately Loaded A Retrospective Chart Review With Up-To-54-Month Follow-UpDocument5 pagesTwo Bilateral Zygomatic Implants Placed and Immediately Loaded A Retrospective Chart Review With Up-To-54-Month Follow-UpBagis Emre Gul100% (1)
- Juergen Zix 2007Document6 pagesJuergen Zix 2007Arindom ChangmaiNo ratings yet
- Declerck 2011Document4 pagesDeclerck 2011ortodoncia 2022No ratings yet
- Treatment of Nipple Hypertrophy by A Simplified Reduction TechniqueDocument7 pagesTreatment of Nipple Hypertrophy by A Simplified Reduction TechniqueАндрей ПетровNo ratings yet
- Frenectomy Z PlastyDocument4 pagesFrenectomy Z Plastyantonio dlNo ratings yet
- OSRM ProximalDocument9 pagesOSRM ProximalÂngelo Rosso LlantadaNo ratings yet
- Cheek FlapDocument4 pagesCheek FlapDae AhmadNo ratings yet
- Ymj 53 642Document7 pagesYmj 53 642Yohana VeronicaNo ratings yet
- EDJ - Volume 62 - Issue Issue 1 - January (Oral Surgery) - Pages 955-958Document4 pagesEDJ - Volume 62 - Issue Issue 1 - January (Oral Surgery) - Pages 955-958Mohammed FaroukNo ratings yet
- Park 2012Document6 pagesPark 2012Yassin SalahNo ratings yet
- Use of Allograft in Skeletally Immature Patients For Calcaneal Neck Lengthening OsteotomyDocument5 pagesUse of Allograft in Skeletally Immature Patients For Calcaneal Neck Lengthening OsteotomyMonem ShakeerNo ratings yet
- Robotic Thyroidectomy by A Gasless Unilateral Axillo-Breast or Axillary Approach: Our Early ExperiencesDocument8 pagesRobotic Thyroidectomy by A Gasless Unilateral Axillo-Breast or Axillary Approach: Our Early ExperiencesAzia MaeNo ratings yet
- Lumbal Spinal Stenosis ODI ScoreDocument10 pagesLumbal Spinal Stenosis ODI ScoreTusan SidhartaNo ratings yet
- Elmo Zen 2015Document6 pagesElmo Zen 2015EstebanEduardo MarinNo ratings yet
- Double Barrel Fibula FlapDocument9 pagesDouble Barrel Fibula FlapAlvaro RivCalleNo ratings yet
- Aps 39 345Document9 pagesAps 39 345isabelNo ratings yet
- Gox 8 E2920Document5 pagesGox 8 E2920Erik BrooksNo ratings yet
- Initial Experience With Application of Single Layer Modified Kugel Mesh For Inguinal Hernia Repair: Case Series of 72 Consecutive PatientsDocument6 pagesInitial Experience With Application of Single Layer Modified Kugel Mesh For Inguinal Hernia Repair: Case Series of 72 Consecutive Patientsnur hasnahNo ratings yet
- Zygomatic Implants: Optimization and InnovationFrom EverandZygomatic Implants: Optimization and InnovationJames ChowNo ratings yet
- Finding The Bond Angle in Tetrahedral-Shaped Molecule: Christopher J. KawaDocument2 pagesFinding The Bond Angle in Tetrahedral-Shaped Molecule: Christopher J. KawaRudolf KiraljNo ratings yet
- Tetrahedron ElementsDocument12 pagesTetrahedron ElementsRudolf KiraljNo ratings yet
- Tetrakis (Tri-Tert-Butylsilyl) - Tetuahedvo-Tetrasilane (Tbu, Si), Si, The First Molecular Silicon Com-Pound With A Si, TetrahedronDocument3 pagesTetrakis (Tri-Tert-Butylsilyl) - Tetuahedvo-Tetrasilane (Tbu, Si), Si, The First Molecular Silicon Com-Pound With A Si, TetrahedronRudolf KiraljNo ratings yet
- Bliamptis 1968Document3 pagesBliamptis 1968Rudolf KiraljNo ratings yet
- Of Sodium: Influence of Phenol On The Habit Chloride CrystalsDocument6 pagesOf Sodium: Influence of Phenol On The Habit Chloride CrystalsRudolf KiraljNo ratings yet
- White p4Document4 pagesWhite p4Rudolf KiraljNo ratings yet
- PloymerptDocument20 pagesPloymerptRudolf KiraljNo ratings yet
- Iniern T Ohd Journd of Spectromet&and Ion P&y&Document9 pagesIniern T Ohd Journd of Spectromet&and Ion P&y&Rudolf KiraljNo ratings yet
- On The Planar Periodic Table: Tidjani NégadiDocument6 pagesOn The Planar Periodic Table: Tidjani NégadiRudolf KiraljNo ratings yet
- Campesino Romeo1982Document5 pagesCampesino Romeo1982Rudolf KiraljNo ratings yet
- Hopper-Like Single Crystals of Sodium Chloride Grown at The Interface of Metastable Water DropletsDocument4 pagesHopper-Like Single Crystals of Sodium Chloride Grown at The Interface of Metastable Water DropletsRudolf KiraljNo ratings yet
- Kolafa 1995Document15 pagesKolafa 1995Rudolf KiraljNo ratings yet
- Sasaki 2006Document4 pagesSasaki 2006Rudolf KiraljNo ratings yet
- Further Data On The Preparation of Extremely Pure Sodium Chloride CrystalsDocument10 pagesFurther Data On The Preparation of Extremely Pure Sodium Chloride CrystalsRudolf KiraljNo ratings yet
- Medjugorje 2010Document21 pagesMedjugorje 2010Rudolf KiraljNo ratings yet
- 266 2012 Article 9904Document9 pages266 2012 Article 9904Rudolf KiraljNo ratings yet
- Aging': Perceptual Motor Skih, 4 1Document6 pagesAging': Perceptual Motor Skih, 4 1Rudolf KiraljNo ratings yet
- The Crystal and Molecular Structure of Naphthalene. I. X-Ray MeasurementsDocument6 pagesThe Crystal and Molecular Structure of Naphthalene. I. X-Ray MeasurementsRudolf KiraljNo ratings yet
- ,radioactive Halos: X 5541 Robert GentryDocument16 pages,radioactive Halos: X 5541 Robert GentryRudolf KiraljNo ratings yet
- Formation of Regularly Arrayed Fines On Surface of Sodium Chloride CrystalsDocument4 pagesFormation of Regularly Arrayed Fines On Surface of Sodium Chloride CrystalsRudolf KiraljNo ratings yet
- Chemical Physics Letters: Hugo J. Bohórquez, Russell J. BoydDocument5 pagesChemical Physics Letters: Hugo J. Bohórquez, Russell J. BoydRudolf KiraljNo ratings yet
- Fossil Alpha-Recoil Analysis Certain Variant: RadioactiveDocument3 pagesFossil Alpha-Recoil Analysis Certain Variant: RadioactiveRudolf KiraljNo ratings yet
- Ebiomedicine: R. Fernández Del Río, M.E. O'Hara, A. Holt, P. Pemberton, T. Shah, T. Whitehouse, C.A. MayhewDocument8 pagesEbiomedicine: R. Fernández Del Río, M.E. O'Hara, A. Holt, P. Pemberton, T. Shah, T. Whitehouse, C.A. MayhewRudolf KiraljNo ratings yet
- 3D Periodic TableDocument38 pages3D Periodic TableRudolf KiraljNo ratings yet
- Teaching Electron Configuration The Musical WayDocument4 pagesTeaching Electron Configuration The Musical WayRudolf KiraljNo ratings yet
- cs2 MetabolismDocument6 pagescs2 MetabolismRudolf KiraljNo ratings yet
- Effects of Relativistic Motion of Electrons On The Chemistry of Gold and PlatinumDocument11 pagesEffects of Relativistic Motion of Electrons On The Chemistry of Gold and PlatinumRudolf KiraljNo ratings yet
- The Evolution of Seeds: New Phytologist June 2010Document16 pagesThe Evolution of Seeds: New Phytologist June 2010Rudolf KiraljNo ratings yet
- Psychogenic Itch: Reviewarticle OpenaccessDocument8 pagesPsychogenic Itch: Reviewarticle OpenaccessRudolf KiraljNo ratings yet
- Do General Chemistry Textbooks Facilitate Conceptual Understanding?Document2 pagesDo General Chemistry Textbooks Facilitate Conceptual Understanding?Rudolf KiraljNo ratings yet
- Filler Rhinoplasty: Evidence, Outcomes, and ComplicationsDocument3 pagesFiller Rhinoplasty: Evidence, Outcomes, and ComplicationsАндрей ПетровNo ratings yet
- Body Dysmorphic Disorder in AestheticDocument5 pagesBody Dysmorphic Disorder in AestheticPaula ArenasNo ratings yet
- The Role of Polycaprolactone in Asian RhinoplastyDocument4 pagesThe Role of Polycaprolactone in Asian RhinoplastyfatinfatharaniNo ratings yet
- Toriumi Et Al 2023 Auricular Composite Graft Survival in RhinoplastyDocument11 pagesToriumi Et Al 2023 Auricular Composite Graft Survival in RhinoplastydrapatriciacieloorlNo ratings yet
- Resume - Sara GhorbaniDocument4 pagesResume - Sara Ghorbaniarian tejaratNo ratings yet
- AdamRouilly Products Catalogue 2018Document44 pagesAdamRouilly Products Catalogue 2018NGUYEN HUU TRUONG TruongNo ratings yet
- The Spreader Flap in Primary Rhinoplasty: BackgroundDocument8 pagesThe Spreader Flap in Primary Rhinoplasty: BackgroundAlex Rolando SuntaxiNo ratings yet
- Rhinoplasty: Edited by Michael J. BrennerDocument158 pagesRhinoplasty: Edited by Michael J. BrennerSang TrầnNo ratings yet
- A Complete Subperichondrial Dissection Technique For Rhinoplasty With Management of The Nasal LigamentsDocument11 pagesA Complete Subperichondrial Dissection Technique For Rhinoplasty With Management of The Nasal LigamentsМаратNo ratings yet
- Whole Face Approach With Hyaluronic Acid FillersDocument11 pagesWhole Face Approach With Hyaluronic Acid Fillersalh basharNo ratings yet
- Glabellar Flaps For Reconstruction of Skin DefectsDocument6 pagesGlabellar Flaps For Reconstruction of Skin Defectslaljadeff12No ratings yet
- (03241750 - Acta Medica Bulgarica) Non-Surgical Correction of Nasal Dorsum and Tip in Primary CasesDocument4 pages(03241750 - Acta Medica Bulgarica) Non-Surgical Correction of Nasal Dorsum and Tip in Primary CasesTeodorNo ratings yet
- IncisionsDocument25 pagesIncisionspriya_edwin100% (1)
- 3d Zygoma ReductionDocument6 pages3d Zygoma ReductionRudolf KiraljNo ratings yet
- Deviated Nasal Septum 2Document62 pagesDeviated Nasal Septum 2Mukundan Subramanian100% (1)
- Otolaryngology - Head and Neck Surgery: Fracture Patterns of The Nasal SeptumDocument6 pagesOtolaryngology - Head and Neck Surgery: Fracture Patterns of The Nasal SeptumEduardo Cantu GarzaNo ratings yet
- Else Vier 2012 Plastic SurgeryDocument17 pagesElse Vier 2012 Plastic SurgerysabistonNo ratings yet
- Facial Danger Zones: DR - Mahmoud Gh. Fakiha, DescDocument29 pagesFacial Danger Zones: DR - Mahmoud Gh. Fakiha, DescIrfanHadiWijayaNo ratings yet
- Turbinate HypertrophyDocument8 pagesTurbinate HypertrophyNurhayati Akila JNNo ratings yet
- Clinical Practice Guideline For The Use of Fillers in Non Surgical RhinoplastyDocument25 pagesClinical Practice Guideline For The Use of Fillers in Non Surgical RhinoplastyDachi DavitashviliNo ratings yet
- 23 Sur Deviated Nasal SeptumDocument3 pages23 Sur Deviated Nasal SeptumSardar jiNo ratings yet
- ENT InstrumentsDocument71 pagesENT InstrumentsPragnya MeduriNo ratings yet
- The Sceptical Patriot Chapter 1 ExcerptDocument55 pagesThe Sceptical Patriot Chapter 1 ExcerptMission201516No ratings yet
- Specific Complications Associated With Non-Surgical RhinoplastyDocument4 pagesSpecific Complications Associated With Non-Surgical RhinoplastyKerlida SantosNo ratings yet
- OMFSCNA - 422septoplasty With RhinoplastyDocument10 pagesOMFSCNA - 422septoplasty With RhinoplastySooraj SNo ratings yet
- Dorsal Preservation: The Push Down Technique ReassessedDocument15 pagesDorsal Preservation: The Push Down Technique ReassessedPatricioMartinFragolaNo ratings yet
- Prof. DR. M. Thaufiq S. Boesoirie, Dr. Sp. THT - KL, (K) - TERBARUDocument14 pagesProf. DR. M. Thaufiq S. Boesoirie, Dr. Sp. THT - KL, (K) - TERBARUalpriani patrasNo ratings yet
- Photogrammetric Facial Analysis of AttractiveDocument6 pagesPhotogrammetric Facial Analysis of AttractiveTôn Thất Đam TriềuNo ratings yet