Professional Documents
Culture Documents
The Element of Surprise
The Element of Surprise
Uploaded by
mariacarmenstoicaCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mock TherapyDocument7 pagesMock TherapyElizabeth Marie RiveraNo ratings yet
- Transcendental Meditation and Treatment For Post-TraumaticDocument2 pagesTranscendental Meditation and Treatment For Post-TraumaticmariacarmenstoicaNo ratings yet
- Specific PhobiasDocument9 pagesSpecific PhobiasmariacarmenstoicaNo ratings yet
- Richard GallianoDocument3 pagesRichard Gallianomariacarmenstoica0% (1)
- Case Histories: Bipolar DisorderDocument1 pageCase Histories: Bipolar DisordermariacarmenstoicaNo ratings yet
- GriegDocument7 pagesGriegmariacarmenstoica0% (1)
- Oral and Genital Ulcers in Behçet's Disease: Images in Clinical MedicineDocument1 pageOral and Genital Ulcers in Behçet's Disease: Images in Clinical MedicinemariacarmenstoicaNo ratings yet
- Oboseala Final 229Document67 pagesOboseala Final 229mariacarmenstoicaNo ratings yet
- 6 DAYS Home Functional FitnessDocument2 pages6 DAYS Home Functional FitnessNaobi IrenNo ratings yet
- History of Health ReformDocument21 pagesHistory of Health ReformHihiNo ratings yet
- Vol 6 Suppissue1Document7 pagesVol 6 Suppissue1spiridon_andrei2011No ratings yet
- Surgery Compilation PDFDocument92 pagesSurgery Compilation PDFDivine SangutanNo ratings yet
- UntitledDocument515 pagesUntitledKimberly 007No ratings yet
- Life Skills Syllabus 12 Grade: Alignment With Curriculum Goals Alignment With Curriculum GoalsDocument3 pagesLife Skills Syllabus 12 Grade: Alignment With Curriculum Goals Alignment With Curriculum GoalsGardimar MontañezNo ratings yet
- Physical Education and Health 11: Learning Activity Sheet (Week 5-6) Personal Safety Background InformationDocument4 pagesPhysical Education and Health 11: Learning Activity Sheet (Week 5-6) Personal Safety Background InformationRheena-Ann Dupale PadillaNo ratings yet
- Personalized Medicine - A Biological Approach To Patient Treatment - FDADocument5 pagesPersonalized Medicine - A Biological Approach To Patient Treatment - FDAAditya DebnathNo ratings yet
- BasicScienceYear10textbook PDFDocument133 pagesBasicScienceYear10textbook PDFDove PaeaNo ratings yet
- ELLIOTT - Pursued by Happiness and Beaten Senseless Prozac and The American DreamDocument6 pagesELLIOTT - Pursued by Happiness and Beaten Senseless Prozac and The American Dreamrachel.avivNo ratings yet
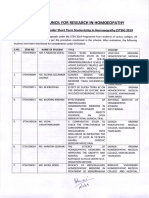
- Central Council For: in HomoeopathyDocument18 pagesCentral Council For: in Homoeopathy9891233665No ratings yet
- Kaizene 2 EditeDocument53 pagesKaizene 2 EditeHabteNo ratings yet
- BMRCL - SOP For WorksDocument3 pagesBMRCL - SOP For WorksravindraNo ratings yet
- Jeanine Avalos Resume 2Document2 pagesJeanine Avalos Resume 2api-644273888No ratings yet
- Occupational Health and Safety Management and TurnoverDocument6 pagesOccupational Health and Safety Management and TurnoverAngelica Maria Torregroza EspinosaNo ratings yet
- Accessibility Audit: by Dr. Parag NarkhedeDocument27 pagesAccessibility Audit: by Dr. Parag NarkhedeRadhika AgarwalNo ratings yet
- Epilepsy Syndromes in Children - UpToDateDocument26 pagesEpilepsy Syndromes in Children - UpToDatecapt_zoeNo ratings yet
- Cancer - 2005 - Van Gogh - The Efficacy of Voice Therapy in Patients After Treatment For Early Glottic CarcinomaDocument11 pagesCancer - 2005 - Van Gogh - The Efficacy of Voice Therapy in Patients After Treatment For Early Glottic CarcinomaNathalia Dos ReisNo ratings yet
- Submission Date First Name Last NameDocument45 pagesSubmission Date First Name Last NamejohnmarcNo ratings yet
- Eq and CQ Paragraph FormDocument18 pagesEq and CQ Paragraph FormmichaellanicpaculbzNo ratings yet
- Career Paths - Mediator (INFP) Personality - 16personalities Part06Document3 pagesCareer Paths - Mediator (INFP) Personality - 16personalities Part06CATIA VALERIA FERRAGENS E SELANTESNo ratings yet
- Sexual Assault TraumaDocument6 pagesSexual Assault TraumaYó MegaNo ratings yet
- SoP - MIT Media LabsDocument3 pagesSoP - MIT Media LabsAbhilash SreekumarNo ratings yet
- Catherine Mae Ledesma ACT2socioDocument2 pagesCatherine Mae Ledesma ACT2socioChris BryantNo ratings yet
- Relative Clauses - Future TenseDocument6 pagesRelative Clauses - Future TenseJose Jaime SaldarriagaNo ratings yet
- ND 211-Meal ManagementDocument18 pagesND 211-Meal ManagementMash JumahariNo ratings yet
- Cetaphil Pink Cleanser: (666) View More View More View MoreDocument1 pageCetaphil Pink Cleanser: (666) View More View More View MoreNUR AFATIN RAHMAT BINTI SARIF MoeNo ratings yet
- 5S (Methodology) - WikipediaDocument4 pages5S (Methodology) - WikipediaBORRELNo ratings yet
- Factors Associated With Sleep Quality Among Undergraduate Students at A Malaysian Public UniversityDocument19 pagesFactors Associated With Sleep Quality Among Undergraduate Students at A Malaysian Public UniversityHayati RaisNo ratings yet
The Element of Surprise
The Element of Surprise
Uploaded by
mariacarmenstoicaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Element of Surprise
The Element of Surprise
Uploaded by
mariacarmenstoicaCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
Clinical Problem-Solving
Caren G. Solomon, M.D., M.P.H., Editor
The Element of Surprise
Mounica Vallurupalli, M.D., Sanjay Divakaran, M.D., Aric Parnes, M.D.,
Bruce D. Levy, M.D., and Joseph Loscalzo, M.D., Ph.D.
In this Journal feature, information about a real patient is presented in stages (boldface type) to an expert
clinician, who responds to the information by sharing relevant background and reasoning with the reader
(regular type). The authors’ commentary follows.
A 64-year-old woman presented to the emergency department with fatigue and From the Department of Medicine,
shortness of breath. Her symptoms had begun 3 months earlier. During the past few Brigham and Women’s Hospital, and Har-
vard Medical School — both in Boston.
weeks, she had had worsening shortness of breath when walking short distances Address reprint requests to Dr. Levy at the
and climbing stairs. She had no chest discomfort or palpitations; she had a dry cough Department of Medicine, Brigham and
but no fevers, chills, or sweats. She had had two falls after feeling lightheaded but did Women’s Hospital, 75 Francis St., Boston,
MA 02115, or at blevy@bwh.harvard.edu.
not strike her head or lose consciousness. She reported no numbness in the legs, gait
imbalance, or weakness. N Engl J Med 2019;381:1365-71.
DOI: 10.1056/NEJMcps1811547
Copyright © 2019 Massachusetts Medical Society.
Fatigue is a common problem with a broad differential diagnosis. The patient
should be asked about muscular weakness or excessive sleepiness. Her exertional
dyspnea arouses concern about a cardiovascular or pulmonary cause. Her falls and
lightheadedness suggest the possibility of low intravascular volume, possibly sec-
ondary to anemia, third spacing of fluid (loss of intravascular fluid into the inter-
stitium), or poor oral intake. Clinical history and examination results can be used
to differentiate between syncope and falls related to neurologic or gait dysfunction.
The patient had a history of migraines, depression, supraventricular tachycardia, and
alcohol use disorder but reported having stopped alcohol consumption 3 years before
presentation. Her medications included escitalopram (20 mg daily) and a regimen
for migraines — metoclopramide (10 mg four times a day as needed), sumatriptan
(100 mg orally as needed), and verapamil (240 mg nightly). She had no known aller-
gies. She had a history of 17.5 pack-years of cigarette smoking and had quit 3 years
before presentation.
The patient’s history of supraventricular tachycardia arouses concern about a ma-
lignant tachyarrhythmia contributing to her presentation. Her former tobacco use
raises her risk of pulmonary disorders, including chronic obstructive pulmonary
disease and lung cancer.
On further evaluation, the patient reported daily episodes of nausea for 3 months
before presentation. She attributed the nausea to migraines, and metoclopramide
had provided some relief. She reported poor appetite, loose stools (up to three times
daily), and a weight loss of 5.5 kg (12 lb). She reported no hematochezia, melena, or
abdominal pain. She did not have nocturnal diarrhea or associate loose stools with
particular foods. Previously, she had had regular, well-formed bowel movements
n engl j med 381;14 nejm.org October 3, 2019 1365
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
every other day. She had had an unremarkable count was 72.8% neutrophils, 10.1% lympho-
colonoscopy 3 years earlier. cytes, 16.1% monocytes, 0.5% eosinophils, and
0.5% immature granulocytes. The mean corpus-
The presence of nausea relieved by metoclo- cular volume was 112 fl (normal range, 80 to 95).
pramide raises suspicion for gastroparesis; how- The red-cell distribution width was 18.6% (nor-
ever, gastroparesis is not associated with chronic mal range, 11.5 to 14.5), and the reticulocyte
diarrhea. Chronic diarrhea is often unrelated to count 0.7%. The patient received 3 units of packed
infectious causes in an immunocompetent host red cells on admission, which resulted in an in-
and can be due to secretory, osmotic, or malab- crease in her hemoglobin level from 3.8 g to 6.4 g
sorptive causes. The clinical history is most con- per deciliter. Several days later, she received an
sistent with malabsorption, which typically leads additional 2 units of packed red cells, which elicit-
to weight loss; loose, foul-smelling stools; and ed an appropriate response.
mild gastrointestinal symptoms (anorexia, flatu-
lence, and abdominal discomfort). Severe macrocytic anemia and leukopenia can
result from impaired marrow production or in-
On physical examination, the patient was afe- creased destruction of red cells in the peripheral
brile (with a temperature of 36.3°C); the heart blood. The inappropriately low reticulocyte count
rate was 91 beats per minute, the blood pressure suggests impaired marrow production. Potential
96/51 mm Hg, and the oxygen saturation 100% causes of macrocytic anemia include megalo-
while she was breathing ambient air. She was blastic anemia (most commonly due to vitamin B12
thin and appeared fatigued. She had conjunctival or folate deficiency or medications that result in
pallor. There was no cervical or supraclavicular impaired DNA synthesis, such as methotrexate,
lymphadenopathy. Her heart rate and rhythm azathioprine, or hydroxyurea), primary bone mar-
were regular, and there was a grade 2/6 systolic row disorders (myelodysplastic syndrome [MDS],
flow murmur. Jugular venous pressure was not aplastic anemia, and leukemia), liver disease,
elevated. Her lungs were clear on auscultation, long-term alcohol use, and hypothyroidism. Leu-
and her abdomen was soft, nontender, and non- kopenia with a macrocytic anemia can be seen
distended, without hepatosplenomegaly. She had in patients with primary bone marrow diseases,
no edema in the legs and no bruising or petechiae. megaloblastic anemia, medication-related effects,
There was no clubbing or cyanosis of the feet or and copper deficiency.
hands. The gait was normal, strength was intact
in the legs and arms, and proprioception and sen- The peripheral-blood smear showed macrocyto-
sation to light touch and temperature were nor- sis and anisocytosis but no schistocytes or sphe-
mal. The deep tendon reflexes were 2+ through- rocytes. There was a low number of white cells,
out. The Babinski sign was absent. She reported and the neutrophils were noted to be hypolobu-
feeling lightheaded when rising from a seated lated (Fig. 1). The platelets were normal in num-
position to standing, but there was no orthostatic ber, size, and granulation.
change in blood pressure.
Bilobed neutrophils are suggestive of pseudo-
The patient’s examination arouses concern about Pelger–Huët anomaly (acquired Pelger–Huët
intravascular volume depletion, whereas conjunc- anomaly). They can be seen in patients with
tival pallor raises suspicion for anemia. She does MDS, acute myeloid leukemia, and toxic effects
not have evidence of volume overload or a pri- of drug therapy.
mary pulmonary process.
The lactate dehydrogenase level was 168 U per
The sodium level was 133 mmol per liter, the urea liter (normal range, 135 to 225), the iron level
nitrogen level 15 mg per deciliter (5.4 mmol per 176 μg per deciliter (32 μmol per liter) (normal
liter), and the creatinine level 1.2 mg per deciliter range, 37 to 158 μg per deciliter [7 to 28 μmol per
(106 μmol per liter). The white-cell count was liter]), the total iron-binding capacity 275 μg per
1990 per cubic millimeter, the hemoglobin level deciliter (49 μmol per liter) (normal range, 220 to
3.8 g per deciliter, and the platelet count 214,000 460 μg per deciliter [39 to 82 μmol per liter]), the
per cubic millimeter. The white-cell differential ferritin level 914 μg per liter (normal range, 10 to
1366 n engl j med 381;14 nejm.org October 3, 2019
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
Clinical Problem-Solving
170), the vitamin B12 level 281 pg per milliliter A
(210 pmol per liter) (normal range, 250 to 900 pg
per milliliter [180 to 660 pmol per liter]), and the
folate level 11.9 ng per milliliter (27 nmol per liter)
(normal range, >5.2 ng per milliliter [>12 nmol
per liter]). The homocysteine level was 8 μmol per
liter (normal range, 5 to 12), and the methylmalo-
nic acid level 0.11 nmol per liter (normal range,
<0.40). A direct antiglobulin test (Coombs’ test)
was negative. The thyrotropin level was 2.28 mIU
per milliliter (normal range, 0.50 to 5.70). A com-
plete blood count from 5 months earlier showed
a white-cell count of 7610 per cubic millimeter, a
hemoglobin level of 11.9 g per deciliter, and a
platelet count of 235,000 per cubic millimeter.
The normal level of lactate dehydrogenase, low
reticulocyte count, and negative Coombs’ test B
argue against hemolysis. The iron studies do not
indicate iron deficiency. The vitamin B12 level is
near the lower limit of the normal range, but the
absence of elevation in the methylmalonic acid
and homocysteine levels is inconsistent with vita-
min B12 deficiency. Bone marrow examination is
warranted to determine the cause of the pro-
found anemia and leukopenia; I am concerned
about an underlying marrow disorder, particular-
ly MDS, given the pseudo-Pelger–Huët anomaly.
The patient underwent a bone marrow biopsy
(Fig. 2A through 2E). The aspirate smear showed
vacuoles in myeloid and erythroid precursors. The
percentage of blasts was not elevated. An iron
stain revealed occasional ringed sideroblasts. The
biopsy specimen showed a normocellular mar- Figure 1. Blood Specimens.
row with relative myeloid hyperplasia, a low A peripheral-blood smear at low magnification (Panel A) shows evidence
number of erythroid elements, a high number of of hypochromia. At higher magnification (Panel B), a representative hypo-
immature myeloid precursors, and focal dysmega- lobulated polymorphonuclear granulocyte (arrow) is noted, along with
karyopoiesis. Karyotyping and next-generation macrocytosis, anisocytosis, and hypochromia.
sequencing of the marrow aspirate were normal.
Myeloid hyperplasia, ringed sideroblasts, a high medications including methotrexate and azathio-
number of immature myeloid precursors, and prine. Ringed sideroblasts are a morphologic
mild dysplasia can be seen in patients with MDS; finding associated with abnormal iron seques-
however, a diagnosis of MDS is unlikely given tration in the mitochondria and are also seen in
the absence of clonal cytogenetic or molecular patients with toxic effects of lead exposure, alco-
alterations. There are nonclonal processes that hol use disorder, vitamin B6 deficiency, and cop-
can mimic the dysplasia seen in MDS and be per deficiency. The combination of multilineage
associated with cytopenias, including nutrient dysplasia, ringed sideroblasts, and vacuoles in
deficiencies (vitamin B12, folate, or copper), auto- myeloid and erythroid progenitors has been as-
immune diseases such as systemic lupus erythe- sociated with copper deficiency. Copper levels
matosus or rheumatoid arthritis, and effects of should be assessed in this patient, along with
n engl j med 381;14 nejm.org October 3, 2019 1367
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A B
C D E
Figure 2. Bone Marrow Specimens.
In Panel A, the core biopsy specimen shows 50% cellularity, normocellular to mildly hypercellular for the patient’s
age. In Panel B, a high number of immature myeloid precursors with mild myeloid predominance and a relative de-
crease in erythroid maturation are noted. In Panel C, closer examination of the bone marrow core reveals atypical,
small hypolobulated megakaryocytes (arrow) with a high nuclear-to-cytoplasmic ratio. In Panels D and E, cytoplas-
mic vacuoles (arrows) are noted in erythroid and myeloid precursors, respectively.
zinc levels, because zinc excess can contribute to prompt an evaluation for malabsorptive causes,
copper deficiency. and additional history should be obtained to
determine a source of excess zinc consumption.
Zinc and copper levels were assessed. The zinc
level was 247 μg per deciliter (37.8 μmol per liter) The patient reported no use of zinc-containing
(normal range, 66 to 110 μg per deciliter [10.1 to lozenges, supplements, denture creams, or mouth-
16.8 μmol per liter]), and the copper level was washes. Owing to the finding of copper defi-
less than 10 μg per deciliter (<1.6 μmol per liter) ciency and her history of loose stools, nausea, and
(normal range, 75 to 145 μg per deciliter [11.8 to weight loss, the patient underwent esophagogas-
22.8 μmol per liter]). troduodenoscopy (EGD), which revealed a nor-
mal esophagus, diffusely erythematous mucosa
Severe copper deficiency manifests with severe in the gastric body and gastric antrum, and dif-
hematologic or neurologic abnormalities. The fusely scalloped mucosa in the entire examined
findings of anemia, leukopenia, and dysplastic duodenum (Fig. 3A and 3B). Biopsy specimens
changes in the bone marrow are consistent with of the gastric body and the duodenum were ob-
copper deficiency. Common causes of copper tained. The duodenal biopsy (Fig. 4A and 4B) re-
deficiency include malnutrition, impaired absorp- vealed mucosa with partial villous blunting and a
tion, and excess zinc consumption. The patient’s high number of intraepithelial lymphocytes (>50
history of weight loss and loose stools should per 100 enterocytes).
1368 n engl j med 381;14 nejm.org October 3, 2019
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
Clinical Problem-Solving
A A
B
B
Figure 4. Duodenal Specimens.
Figure 3. Esophagogastroduodenoscopic Images. A duodenal-biopsy specimen obtained at the time of
Panel A shows a scalloped appearance in the duodenal diagnosis (Panel A) shows duodenal mucosa with par-
bulb (arrow). Panel B shows a smooth appearance of tial villous blunting and a high number of intraepithelial
the duodenum (arrow), a finding suggestive of loss lymphocytes (>50 per 100 enterocytes). A duodenal-
of villi in segment 2 of the duodenum. biopsy specimen obtained 6 months after the initiation
of a gluten-free diet (Panel B) shows improvement in
villous blunting and no increase in the number of intra-
epithelial lymphocytes.
The patient had no history of excess zinc intake.
Zinc uptake contributes to copper deficiency by
promoting the production of metallothionein in These findings confirm the diagnosis of celiac
enterocytes, which sequesters copper in entero- disease. Treatment of celiac disease involves care-
cytes. The patient’s EGD and biopsy results are ful lifelong adherence to a gluten-free diet. Long-
suggestive of celiac disease. Tissue transgluta- term complications that are associated with
minase (tTG) IgA antibody testing, which has uncontrolled celiac disease include nutritional
high sensitivity and specificity for the diagnosis deficiencies, anemia, low bone mineral density,
of celiac disease, is recommended to further and an increased risk of enteropathy-associated
evaluate the patient. T-cell lymphoma in the small bowel. The absence
of excess copper in the enterocytes suggests that
The patient’s levels of tTG IgA and IgG antibodies this patient’s level of zinc excess was not a pri-
were elevated, at 68 CU (normal range, 0 to 19) mary contributor to her copper deficiency.
and 28 CU (normal range, 0 to 19), respectively.
Copper staining was performed on the patient’s Over a period of 2 weeks, the patient’s anemia re-
duodenal-biopsy specimen and did not reveal any sponded to 2 mg of intravenous copper chloride
excess copper in the enterocytes. administered daily for eight doses. The hemoglo-
n engl j med 381;14 nejm.org October 3, 2019 1369
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
bin level increased from 7.7 g to 10.1 g per decili- C om men ta r y
ter. However, she had worsening hypoxemia at
rest. She had spontaneous desaturations to 89% This patient presented with fatigue, shortness
on pulse oximetry and was given oxygen supple- of breath, weight loss, nausea, and loose stools.
mentation at a rate of 2 liters per minute by nasal Further evaluation showed macrocytic anemia
cannula; the rate was increased to 6 liters per and leukopenia, leading to a diagnosis of copper
minute over a period of 2 days. Computed tomog- deficiency and then of celiac disease. Her course
raphy (CT) of the chest revealed mild bilateral in- was complicated by pulmonary compromise re-
terstitial and alveolar edema. She was treated with lated to alveolar hemorrhage that was attributed
diuretics for the presumptive diagnosis of volume to the Lane–Hamilton syndrome. Overall, mal-
overload from blood transfusions earlier in the absorption that was related to celiac disease led
course of illness. A follow-up chest CT after ade- to severe copper deficiency.
quate diuresis revealed gradual worsening with an Copper deficiency is rare in the Western world.
increase in peribronchial and subpleural ground- There are abundant sources of dietary copper,
glass opacities as well as interlobular septal thick- including dried legumes, whole grains, nuts,
ening throughout both lungs, particularly in the raisins, meat, fish, and poultry. Copper is ab-
upper lobes. In terms of symptoms, she continued sorbed in the upper gastrointestinal tract by
to have a dry cough and remained hypoxemic. She copper transporter 1 (CTR1), which is expressed
underwent bronchoscopy with serial lavages, on the luminal surface of the duodenum. Copper
which yielded progressively higher red-cell counts deficiency occurs in persons with a history of
(tube 1 had 1950 red cells per microliter, tube 2 gastric bypass surgery, other causes of malab-
had 2960, and tube 3 had 9650), findings that sorption, or zinc overload and in those who re-
were consistent with alveolar hemorrhage. Hemo- ceive parenteral nutrition exclusively. Acquired
siderin-laden macrophages were detected. copper deficiency has both hematologic mani-
festations, which are typically reversible, and
The patient’s bronchoscopy results arouse con- neurologic manifestations, which are unlikely to
cern about pulmonary hemosiderosis. This con- be reversed. Hematologic manifestations include
dition is most often identified in persons who anemia, neutropenia, and (in rare cases) throm-
have had recurrent episodes of diffuse alveolar bocytopenia. The anemia can be normocytic,
hemorrhage. In this patient’s case, an additional microcytic, or macrocytic; the cause of this
consideration is pulmonary hemosiderosis asso- variation is unknown. Bone marrow evaluation
ciated with celiac disease, or the Lane–Hamilton often reveals a high number of immature myeloid
syndrome. precursors, dysplasia, and ringed sideroblasts.
These findings can lead to a misdiagnosis of
The patient’s overall presentation was thought to MDS.1,2 Neurologic findings include myelopathy
be consistent with diffuse alveolar hemorrhage affecting the dorsal columns, similar to that of
and pulmonary hemosiderosis associated with vitamin B12 deficiency, as well as peripheral neu-
celiac disease. She received counseling from a ropathy and hyporeflexia. Patients can present
nutritionist regarding maintenance of a gluten- with spastic gait and sensory ataxia.3
free diet. Her anemia and leukopenia resolved This patient was noted to have an elevated
several weeks after intravenous copper supple- zinc level. Excess zinc impairs copper absorption
mentation, and she received maintenance therapy by sequestering copper in enterocytes, which are
with oral copper gluconate (2 mg daily). A gluten- then sloughed off. However, an elevated zinc
free diet resulted in a reduction in gastrointestinal level has been reported in persons with copper
and respiratory symptoms, and repeat chest radi- deficiency even in the absence of excess ingestion
ography showed improvement in bilateral patchy of zinc, for unclear reasons.4 Duodenal-biopsy
interstitial opacities 4 weeks later and complete specimens in this patient did not show excess
resolution 12 weeks after initial imaging. copper in the enterocytes, which suggests that
1370 n engl j med 381;14 nejm.org October 3, 2019
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
Clinical Problem-Solving
zinc excess was not a major contributor to her tient also had idiopathic pulmonary hemosidero-
copper deficiency. sis, a rare complication of celiac disease named
The mechanisms of cytopenias that are medi- the Lane–Hamilton syndrome.11 A gluten-free diet
ated by copper deficiency are incompletely under- can reverse pulmonary hemosiderosis; glucocor-
stood. Copper is an important cofactor for several ticoids are used in more symptomatic patients.12
enzymes, including hephaestin, ceruloplasmin, The present case highlights the importance
and cytochrome c oxidase. All three enzymes of considering copper deficiency in patients with
have oxidase functions important in iron trans- dysplasia and cytopenias, with or without a myelo
port and heme synthesis.2,5 The leukopenia in neuropathy. Recognition that this patient was
copper deficiency appears to be related to im- copper deficient led to the diagnosis of celiac
paired self-renewal and differentiation blockade disease, and the combination of copper replace-
in CD34+ progenitor cells.6-8 ment and a gluten-free diet resulted in marked
Copper deficiency has been reported as a clinical improvement.
complication of celiac disease in several case Disclosure forms provided by the authors are available with
series.4,9,10 Like vitamin B12 deficiency, copper the full text of this article at NEJM.org.
We thank our colleague Vignesh Shanmugam, M.D., for as-
deficiency should be considered in persons with sistance with obtaining the bone marrow and intestinal histo-
leukopenia, anemia, or a myelopathy. This pa- pathological images for this case.
References
1. Lazarchick J. Update on anemia and ED, Shirali AC. An element of unsteadiness. childhood celiac disease. Acta Haematol
neutropenia in copper deficiency. Curr N Engl J Med 2017;377:1379-85. 2004;111:211-4.
Opin Hematol 2012;19:58-60. 6. Gregg XT, Reddy V, Prchal JT. Copper 10. Botero-López JE, Araya M, Parada A,
2. Jaiser SR, Winston GP. Copper defi- deficiency masquerading as myelodys- et al. Micronutrient deficiencies in pa-
ciency myelopathy. J Neurol 2010;257:869- plastic syndrome. Blood 2002;100:1493-5. tients with typical and atypical celiac dis-
81. 7. Huff JD, Keung YK, Thakuri M, et al. ease. J Pediatr Gastroenterol Nutr 2011;53:
3. Sato M, Gitlin JD. Mechanisms of Copper deficiency causes reversible myelo 265-70.
copper incorporation during the biosyn- dysplasia. Am J Hematol 2007;82:625-30. 11. Lane DJ, Hamilton WS. Idiopathic
thesis of human ceruloplasmin. J Biol 8. Villalba A, Osorio J, Freiria C, et al. steatorrhoea and idiopathic pulmonary
Chem 1991;266:5128-34. Copper deficiency: a cause of misdiag haemosiderosis. Br Med J 1971;2:89-90.
4. Halfdanarson TR, Kumar N, Hogan nosis of myelodysplastic syndrome. Ann 12. Kumar N. Copper deficiency myelopa-
WJ, Murray JA. Copper deficiency in celiac Hematol 2018;97:1737-8. thy (human swayback). Mayo Clin Proc
disease. J Clin Gastroenterol 2009;43:162-4. 9. Fisgin T, Yarali N, Duru F, Usta B, 2006;81:1371-84.
5. Saly DL, Brewster UC, Sze GK, Louis Kara A. Hematologic manifestation of Copyright © 2019 Massachusetts Medical Society.
clinical problem-solving series
The Journal welcomes submissions of manuscripts for the Clinical Problem-Solving
series. This regular feature considers the step-by-step process of clinical decision
making. For more information, please see authors.nejm.org.
n engl j med 381;14 nejm.org October 3, 2019 1371
The New England Journal of Medicine
Downloaded from nejm.org on October 4, 2019. For personal use only. No other uses without permission.
Copyright © 2019 Massachusetts Medical Society. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5823)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mock TherapyDocument7 pagesMock TherapyElizabeth Marie RiveraNo ratings yet
- Transcendental Meditation and Treatment For Post-TraumaticDocument2 pagesTranscendental Meditation and Treatment For Post-TraumaticmariacarmenstoicaNo ratings yet
- Specific PhobiasDocument9 pagesSpecific PhobiasmariacarmenstoicaNo ratings yet
- Richard GallianoDocument3 pagesRichard Gallianomariacarmenstoica0% (1)
- Case Histories: Bipolar DisorderDocument1 pageCase Histories: Bipolar DisordermariacarmenstoicaNo ratings yet
- GriegDocument7 pagesGriegmariacarmenstoica0% (1)
- Oral and Genital Ulcers in Behçet's Disease: Images in Clinical MedicineDocument1 pageOral and Genital Ulcers in Behçet's Disease: Images in Clinical MedicinemariacarmenstoicaNo ratings yet
- Oboseala Final 229Document67 pagesOboseala Final 229mariacarmenstoicaNo ratings yet
- 6 DAYS Home Functional FitnessDocument2 pages6 DAYS Home Functional FitnessNaobi IrenNo ratings yet
- History of Health ReformDocument21 pagesHistory of Health ReformHihiNo ratings yet
- Vol 6 Suppissue1Document7 pagesVol 6 Suppissue1spiridon_andrei2011No ratings yet
- Surgery Compilation PDFDocument92 pagesSurgery Compilation PDFDivine SangutanNo ratings yet
- UntitledDocument515 pagesUntitledKimberly 007No ratings yet
- Life Skills Syllabus 12 Grade: Alignment With Curriculum Goals Alignment With Curriculum GoalsDocument3 pagesLife Skills Syllabus 12 Grade: Alignment With Curriculum Goals Alignment With Curriculum GoalsGardimar MontañezNo ratings yet
- Physical Education and Health 11: Learning Activity Sheet (Week 5-6) Personal Safety Background InformationDocument4 pagesPhysical Education and Health 11: Learning Activity Sheet (Week 5-6) Personal Safety Background InformationRheena-Ann Dupale PadillaNo ratings yet
- Personalized Medicine - A Biological Approach To Patient Treatment - FDADocument5 pagesPersonalized Medicine - A Biological Approach To Patient Treatment - FDAAditya DebnathNo ratings yet
- BasicScienceYear10textbook PDFDocument133 pagesBasicScienceYear10textbook PDFDove PaeaNo ratings yet
- ELLIOTT - Pursued by Happiness and Beaten Senseless Prozac and The American DreamDocument6 pagesELLIOTT - Pursued by Happiness and Beaten Senseless Prozac and The American Dreamrachel.avivNo ratings yet
- Central Council For: in HomoeopathyDocument18 pagesCentral Council For: in Homoeopathy9891233665No ratings yet
- Kaizene 2 EditeDocument53 pagesKaizene 2 EditeHabteNo ratings yet
- BMRCL - SOP For WorksDocument3 pagesBMRCL - SOP For WorksravindraNo ratings yet
- Jeanine Avalos Resume 2Document2 pagesJeanine Avalos Resume 2api-644273888No ratings yet
- Occupational Health and Safety Management and TurnoverDocument6 pagesOccupational Health and Safety Management and TurnoverAngelica Maria Torregroza EspinosaNo ratings yet
- Accessibility Audit: by Dr. Parag NarkhedeDocument27 pagesAccessibility Audit: by Dr. Parag NarkhedeRadhika AgarwalNo ratings yet
- Epilepsy Syndromes in Children - UpToDateDocument26 pagesEpilepsy Syndromes in Children - UpToDatecapt_zoeNo ratings yet
- Cancer - 2005 - Van Gogh - The Efficacy of Voice Therapy in Patients After Treatment For Early Glottic CarcinomaDocument11 pagesCancer - 2005 - Van Gogh - The Efficacy of Voice Therapy in Patients After Treatment For Early Glottic CarcinomaNathalia Dos ReisNo ratings yet
- Submission Date First Name Last NameDocument45 pagesSubmission Date First Name Last NamejohnmarcNo ratings yet
- Eq and CQ Paragraph FormDocument18 pagesEq and CQ Paragraph FormmichaellanicpaculbzNo ratings yet
- Career Paths - Mediator (INFP) Personality - 16personalities Part06Document3 pagesCareer Paths - Mediator (INFP) Personality - 16personalities Part06CATIA VALERIA FERRAGENS E SELANTESNo ratings yet
- Sexual Assault TraumaDocument6 pagesSexual Assault TraumaYó MegaNo ratings yet
- SoP - MIT Media LabsDocument3 pagesSoP - MIT Media LabsAbhilash SreekumarNo ratings yet
- Catherine Mae Ledesma ACT2socioDocument2 pagesCatherine Mae Ledesma ACT2socioChris BryantNo ratings yet
- Relative Clauses - Future TenseDocument6 pagesRelative Clauses - Future TenseJose Jaime SaldarriagaNo ratings yet
- ND 211-Meal ManagementDocument18 pagesND 211-Meal ManagementMash JumahariNo ratings yet
- Cetaphil Pink Cleanser: (666) View More View More View MoreDocument1 pageCetaphil Pink Cleanser: (666) View More View More View MoreNUR AFATIN RAHMAT BINTI SARIF MoeNo ratings yet
- 5S (Methodology) - WikipediaDocument4 pages5S (Methodology) - WikipediaBORRELNo ratings yet
- Factors Associated With Sleep Quality Among Undergraduate Students at A Malaysian Public UniversityDocument19 pagesFactors Associated With Sleep Quality Among Undergraduate Students at A Malaysian Public UniversityHayati RaisNo ratings yet