Professional Documents
Culture Documents
Tube Feeding Handouts 102819
Tube Feeding Handouts 102819
Uploaded by
MariaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tube Feeding Handouts 102819
Tube Feeding Handouts 102819
Uploaded by
MariaCopyright:
Available Formats
TUBE FEEDING
In tube feeding, a formula passes through a small tube that connects directly to
part of the patient’s digestive system (the body system that processes food).
The formula is a liquid that contains the nutrients that your patient needs.
Your patient’s doctor, nurse or dietitian will help figure out which type of tube
feeding is best.
This staff member will also decide how long the patient will need tube feeding.
While most patient need tube feeding for only a few days, others need it the
entire time they are having treatments, sometimes longer.
Unless a doctor, nurse or dietitian tells you otherwise, the patient may take part
in meals and eat some regular foods.
Sometimes, the patient may receive medicines through the feeding tube.
The methods for placing the tube are simple and fairly painless. Your patient’s
doctor will use one of these five ways to connect the tube to either the stomach or
the small intestine:
• A nasogastric tube (NG tube) passes through the nose, down the throat and to the
stomach.
• A nasojejunal tube (NJ tube) passes through the nose, down the throat, through the
stomach and to the small intestine.
Nasogastric Tube
Nasojejunal Tube
• A gastrostomy tube (G tube) passes through a small cut in the skin directly into the
stomach.
• A gastroenteric or transgastric jejunal tube (GJ tube) passes through a cut in the skin
directly into the stomach and extends into the small intestine
Gastroenteric or Transgastric Jejunal Tube
Why would you need to consider tube feeding?
difficulties chewing and swallowing your food
reduced hand and arm control making it difficult to get food to your mouth
weight loss due to eating less and muscle wasting
dehydration and constipation due to drinking less
changes to your sense of taste or reduced appetite
lack of energy caused by eating too few calories
food and liquid passing into the lungs, causing coughing or choking (known as
aspiration, this can cause chest infections).
ENTERAL FEEDING
Pertains to the delivery of food and nutrients either orally or by the tube directly
into the GIT. It is used on patients with a functioning GIT but unable to ingest
required nutrients orally or for patients with impaired digesting capacity or
unable to absorb nutrients.
Types of enteral formulation
1. Ready-to-use Formulations
1. Nutritionally complete formulation can be used alone and provides
total needs in a specified volume of formula.
2. Modular Formulation provides different forms of individual
nutrients to supplement existing formulas.
3. Combined formulation meets therapeutic needs.
2. Tube Feedings may be prepared from regular foods
2. Standard Tube Feeding is fiber-free and high in cholesterol, fat and sugar. It is
milk based, sugar, and soft cooked eggs.
3. Blenderized Tube Feeding are soft diet allowances which be blenderized easily.
Complications:
1. Mechanical
1. Nasopharyngeal irritation (ice chips, topical anesthetic and
decongestant)
2. Luminal obstructi0n (Flush, Replace Tube.)
3. Mucosal erosions (Reposition tube, ice water lavage; Remove
Tube.)
4. Tube displacement (Replace Tube)
5. Aspiration (Discontinue tube feeding)
2. Gastrointestinal
1. Cramping/distention (Change formula; Reduce infusion rate)
2. Vomiting/diarrhea (Dilute formula; Reduce infusion rate,
antidiarrheal agents)
3. Constipation (Promote sufficient fluids and fibers; Encourage
patient activity)
3. Metabolic
1. Hypertonic dehydration (Increase free water)
2. Glucose intolerance (Reduce infusion rate; Give
insulin)
3. Cardiac failure (Reduce sodium content; fluid
restriction)
4. Renal Failure (Decrease phosphate, magnesium,
potassium, protein restriction, essential amino acids
solution)
5. Hepatic encephalopathy (Decrease amount of
protein.)
Modes Of Feeding
Bolus feeding entails administration of 200–400 ml of feed down a feeding tube over
15–60 minutes at regular intervals.
The technique may cause bloating and diarrhea and bolus delivery into the
jejunum can cause a ‘‘dumping’’ type syndrome and should therefore be avoided
Bolus feeding can be performed using a 50 ml syringe, either with or without the
plunger
If the latter is removed, the syringe can be hung up to allow gravity feeding.
Continuous feedings are usually delivered using a pump at a constant infusion
rate over an established number of hours during the day and/or at night.
Continuous infusions over 24 hours are often better tolerated by critically ill
patients.
Cycled continuous feedings over a decreased number of hours throughout the
day (e.g., 20 hours of infusion with 4 hours “off”) allow freedom for
developmental activities and stimulation of hunger and thirst in infants.
Continuous overnight feedings may facilitate the development of hunger and
thirst during the day for children able to feed orally.
Overnight continuous feedings into the stomach are not routinely recommended
for children under one year of age or any child at risk for reflux and aspiration.
Continuous infusions must be used for infusions into the jejunum. For home
patients, financial support for a pump is available only if the infusion time is
equal to or greater than 6 hours per 24 hour period.
PARENTERAL FEEDING
Parenteral nutrition means feeding someone via their blood stream
‘intravenously’, TPN means feeding a patient solely via the intravenous route.
INDICATIONS
When patient gastrointestinal tract is paralyzed and nonfunctional, as in the case
of small bowel obstruction
When >7 days of nothing-by-mouth (NPO) status is anticipated, as in the case of
inflammatory bowel disease, patients with an acute exacerbation, critically ill
patients and so on
When the baby’s gut is too immature or has congenital malformations
When the patient is suffering from chronic diarrhea and vomiting or is extremely
undernourished and needs to have surgery, chemotherapy and so on
When patients with bowel anastomosis develop anastomotic leaks in the early
postoperative period
COMPLICATIONS OF TPN
Subtle deterioration of the overall clinical well-being of the patient may be the
first clue that a TPN-related complication has occurred.
The catheter insertion site infection should be ruled out as the first possibility.
In case of any tenderness, redness, drainage, warmth or other inflammatory
signs at the site of insertion, a fresh catheter should be re-sited at a different site
and the tip of the present catheter along with a wound swab should be sent for
culture and sensitivity tests.
Differentiation between the systemic inflammatory response syndrome and the
actual infection remains a difficult task, although preliminary evidence suggests
that new markers such as procalcitonin may be valuable in some circumstances
Short-term potential adverse effects of PN include: infection, hyperglycemia,
hepatic steatosis, essential fatty acid deficiency, electrolyte abnormalities,
acidbase disturbances, hypertriglyceridemia, bacterial translocation and
compromise of gut integrity.
The symptoms of essential fatty acid deficiency include dermatitis, alopecia, poor
wound healing, increased platelet aggregation, increased capillary fragility and
hepatic dysfunction.
Re-feeding syndrome characterized by hypophospatemia, hypomagnesemia,
hypokalaemia and hyperinsulinemia may be observed in patients kept NPO for
greater than 7 – 10 days, chronic alcoholics and those with severe systemic
derangements on initiation of TPN.
Correction of electrolyte abnormalities, administration of thiamine in alcoholics
and a regular check of electrolyte levels may help to prevent this re-feeding
syndrome.
You might also like
- Competency Test 1Document16 pagesCompetency Test 1AnneMarie Nashwinter Sylvester0% (1)
- Pretest FinalDocument2 pagesPretest FinalMatthew Pina0% (1)
- Perineal CareDocument3 pagesPerineal CareNikko Rafael RobillosNo ratings yet
- The Ethic of Care: A Moral Compass for Canadian Nursing Practice - Revised EditionFrom EverandThe Ethic of Care: A Moral Compass for Canadian Nursing Practice - Revised EditionNo ratings yet
- Pyloric Stenosis CaseDocument54 pagesPyloric Stenosis CaseMaria0% (1)
- Lab Policies Sysmex XS 1000i Procedure Lab 1501 PDFDocument26 pagesLab Policies Sysmex XS 1000i Procedure Lab 1501 PDFakiNo ratings yet
- NCLEX (Valerie) PDFDocument18 pagesNCLEX (Valerie) PDFValerie Orengo100% (1)
- Position S: Pratiksha RaiDocument49 pagesPosition S: Pratiksha RaiJoanne Cristie TolopiaNo ratings yet
- Principles in Preparing For A Home A VisitDocument14 pagesPrinciples in Preparing For A Home A VisitLawrence NemirNo ratings yet
- End-of-Life Care For The Newly Licensed Practical Nurse: State of Nebraska Transition GrantDocument8 pagesEnd-of-Life Care For The Newly Licensed Practical Nurse: State of Nebraska Transition GrantGee YorkNo ratings yet
- Admission Nursing AssessmentDocument20 pagesAdmission Nursing AssessmentKhaskheli NusratNo ratings yet
- Bathing On Adult or Pediatric ClientDocument25 pagesBathing On Adult or Pediatric Clientkto12No ratings yet
- HPPDocument28 pagesHPPVfinNo ratings yet
- COVID-19 Guidance For Home Care CHHA LHCSA HospiceDocument3 pagesCOVID-19 Guidance For Home Care CHHA LHCSA HospiceOANo ratings yet
- PositionsDocument16 pagesPositionsdenver matonNo ratings yet
- Assessing The AbdomenDocument18 pagesAssessing The Abdomenmartinezrose32No ratings yet
- IV TherapyDocument15 pagesIV TherapyJojebelle Kate Iyog-cabanlet100% (1)
- Updated Nurses Role in Organ DonationDocument7 pagesUpdated Nurses Role in Organ Donationapi-401168581No ratings yet
- Chapter 45 CanvasDocument49 pagesChapter 45 CanvasSheNo ratings yet
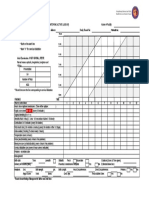
- Partograph: (Use This Form For Monitoring Active Labour)Document1 pagePartograph: (Use This Form For Monitoring Active Labour)Omar Khalif Amad PendatunNo ratings yet
- Nursing Documentation StandardsDocument27 pagesNursing Documentation StandardsVany Ogin100% (1)
- Colostomy CareDocument4 pagesColostomy CareRhenzes HaraNo ratings yet
- Palliative CareDocument12 pagesPalliative CareSonya VanceNo ratings yet
- AM CareDocument14 pagesAM CareMila Canoza HerreraNo ratings yet
- Bladder Care PostpartumDocument11 pagesBladder Care PostpartumAji NugrozzNo ratings yet
- Nutritional Guidelines For FilipinosDocument4 pagesNutritional Guidelines For FilipinosMademoiselle Kayetty67% (3)
- 2.2.2.A FoodLabelsFDocument5 pages2.2.2.A FoodLabelsFMarjaan KhanNo ratings yet
- Family Health AssessmentDocument23 pagesFamily Health AssessmentPatrick Poculan100% (1)
- Nursing Care Management During LaborDocument13 pagesNursing Care Management During LaborRoxane AquillanNo ratings yet
- Administering A Tube Feeding Preparation 1. Assess:: University of Eastern PhilippinesDocument4 pagesAdministering A Tube Feeding Preparation 1. Assess:: University of Eastern PhilippinesJerika Shane MañosoNo ratings yet
- Family Assessment ChecklistDocument5 pagesFamily Assessment ChecklistPauPauNo ratings yet
- CNA Body Mechanics Bed Making Comfort CareDocument32 pagesCNA Body Mechanics Bed Making Comfort CareFaith VaughnNo ratings yet
- Special Senses EYEDocument27 pagesSpecial Senses EYENadiabloshii NadiabloshiiNo ratings yet
- Ostomy CareDocument3 pagesOstomy CareKit ChanNo ratings yet
- Perioperative Nursing ModuleDocument2 pagesPerioperative Nursing ModulerosanowardNo ratings yet
- Personal Hygiene: IntroductionDocument12 pagesPersonal Hygiene: Introductionamar patelNo ratings yet
- Moving A Patient in Bed Moving Up Logrolling and Turning To SidesDocument4 pagesMoving A Patient in Bed Moving Up Logrolling and Turning To SidesJohn Paul BelenNo ratings yet
- Ethics in PediatricsDocument20 pagesEthics in PediatricsCruz YrNo ratings yet
- ColostomyDocument4 pagesColostomyleslie_macasaetNo ratings yet
- Muscle Strength TestingDocument3 pagesMuscle Strength TestingGiselle Chloe Baluya ico100% (1)
- Nursing Care During Labor and Pain Management2015Document51 pagesNursing Care During Labor and Pain Management2015christopher ebarbNo ratings yet
- Please Perform A Upper Limb MOTOR Neurological Examination. After 5 Minutes I Will Ask You Some QuestionsDocument2 pagesPlease Perform A Upper Limb MOTOR Neurological Examination. After 5 Minutes I Will Ask You Some QuestionsMu AbNo ratings yet
- H&S in The Home Care Enviornment - Lap - 301Document93 pagesH&S in The Home Care Enviornment - Lap - 301Jafar KhanNo ratings yet
- Reading Food Labels LPDocument11 pagesReading Food Labels LPapi-272272803No ratings yet
- Cushings SyndromeDocument51 pagesCushings SyndromeTina TalmadgeNo ratings yet
- NCM 101 Assessing Male GenitaliaDocument13 pagesNCM 101 Assessing Male GenitaliaKIM KALIBAYNo ratings yet
- International Council of NursesDocument4 pagesInternational Council of NursesKram Perez100% (3)
- StomaDocument37 pagesStomaAndryHarisNo ratings yet
- Constipation 508Document12 pagesConstipation 508Shishir Kumar SinghNo ratings yet
- Colostomy CareDocument34 pagesColostomy CareTolemre Emre100% (1)
- Bricsinnursingeducation PDFDocument6 pagesBricsinnursingeducation PDFshaikNo ratings yet
- Assessing AbdomenDocument115 pagesAssessing AbdomenKris TinaNo ratings yet
- 8 Common Charting Mistakes To Avoi1aDocument4 pages8 Common Charting Mistakes To Avoi1aEggy PascualNo ratings yet
- IvtDocument32 pagesIvtArlhona Juana RagoNo ratings yet
- ERCPDocument2 pagesERCPClariz TolentinoNo ratings yet
- Enteral Feeding: Gastric Versus Post-Pyloric: Table 1Document22 pagesEnteral Feeding: Gastric Versus Post-Pyloric: Table 1tasmeow23No ratings yet
- HeimlichDocument6 pagesHeimlichErryl Justine AdvinculaNo ratings yet
- A Comparative Analysis of The Philippine Nursing Curriculum From Other Countries.Document8 pagesA Comparative Analysis of The Philippine Nursing Curriculum From Other Countries.Alvin SantiagoNo ratings yet
- Home Health NursingDocument16 pagesHome Health NursingSathish Rajamani100% (1)
- Alterations in Nutrition and GastrointestinalDocument7 pagesAlterations in Nutrition and GastrointestinalChriszanie CruzNo ratings yet
- Nursing Home Visitation - COVID-19v2Document7 pagesNursing Home Visitation - COVID-19v2Sinclair Broadcast Group - EugeneNo ratings yet
- Renal Calculi: Urolithiasis, Nephrolithiasis, Renal StoneDocument18 pagesRenal Calculi: Urolithiasis, Nephrolithiasis, Renal StonerohitNo ratings yet
- Humanism, Nursing, Communication and Holistic Care: a Position Paper: Position PaperFrom EverandHumanism, Nursing, Communication and Holistic Care: a Position Paper: Position PaperNo ratings yet
- Drug Study OBDocument5 pagesDrug Study OBMariaNo ratings yet
- Date Performed: Final Grade: Clinical InstructorDocument2 pagesDate Performed: Final Grade: Clinical InstructorMariaNo ratings yet
- FNCP CHNDocument4 pagesFNCP CHNMariaNo ratings yet
- Community Awareness Public Health Laws: Term PaperDocument9 pagesCommunity Awareness Public Health Laws: Term PaperMariaNo ratings yet
- Bukidnon State University College of Nursing Malaybalay City BukidnonDocument3 pagesBukidnon State University College of Nursing Malaybalay City BukidnonMariaNo ratings yet
- Erythromycins PDFDocument3 pagesErythromycins PDFMariaNo ratings yet
- PHARMACOLOGY Anti Microbial DrugsDocument17 pagesPHARMACOLOGY Anti Microbial DrugsLeilani Sablan100% (2)
- Heath Assessment ToolDocument8 pagesHeath Assessment ToolHouda Hayek100% (1)
- Basic Rules in TranscriptionDocument6 pagesBasic Rules in TranscriptionJepoy Olivo100% (3)
- Test Bank For Medical Genetics 4th Edition Lynn B JordeDocument8 pagesTest Bank For Medical Genetics 4th Edition Lynn B Jorderoytuyenbau100% (1)
- Curs 14 Boala Lyme 2Document63 pagesCurs 14 Boala Lyme 2n1u1s1h1100% (1)
- Anaemia Among Pregnant Women Prevalence and DeterminantsDocument4 pagesAnaemia Among Pregnant Women Prevalence and DeterminantsKIU PUBLICATION AND EXTENSIONNo ratings yet
- What Is GKI, Glucose Ketone Index Calculate It KETO-MOJODocument1 pageWhat Is GKI, Glucose Ketone Index Calculate It KETO-MOJOsbtxbprm29No ratings yet
- Emergency First ResponseDocument34 pagesEmergency First ResponseColt AntipuestoNo ratings yet
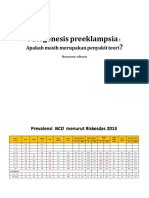
- Patogenesis Preeklampsia - Apakah Masih Merupakan Penyakit Teori PDFDocument49 pagesPatogenesis Preeklampsia - Apakah Masih Merupakan Penyakit Teori PDFFellita Ratri ANo ratings yet
- Psychiatry History & Suicide Risk Assessment TemplatesDocument32 pagesPsychiatry History & Suicide Risk Assessment TemplatesDuncan Jackson100% (2)
- AHW3e - Level 2 - Unit Test 8aDocument3 pagesAHW3e - Level 2 - Unit Test 8aDorian FarinangoNo ratings yet
- To Study The Effect of Lockdown On Physical, Mental and Emotional Health of Common PeopleDocument9 pagesTo Study The Effect of Lockdown On Physical, Mental and Emotional Health of Common PeopleInternational Journal of Innovative Science and Research Technology100% (1)
- PCE ReportDocument27 pagesPCE ReportNikhil ThosarNo ratings yet
- The Rising Menace of Smog: Time To Act Now: EditorialDocument2 pagesThe Rising Menace of Smog: Time To Act Now: EditorialBusiness RazaNo ratings yet
- First Aid - NotesDocument10 pagesFirst Aid - NotesRoisin McdonnellNo ratings yet
- Neuropsychiatric Symptoms in Lupus: PaperDocument3 pagesNeuropsychiatric Symptoms in Lupus: PaperCarolina MuñozNo ratings yet
- Health Awareness and Life Skills KCADocument17 pagesHealth Awareness and Life Skills KCAAdelite sabiriNo ratings yet
- CHCAGE001 Facilitate The Empowerment of Older People: Learner GuideDocument168 pagesCHCAGE001 Facilitate The Empowerment of Older People: Learner GuidemaxsalNo ratings yet
- Aspecte Radiologice in SarcoidozaDocument67 pagesAspecte Radiologice in SarcoidozaBianca Balas MafteiNo ratings yet
- Mtlaws LectureDocument6 pagesMtlaws LectureAhnorrei PavlaskaNo ratings yet
- Conference Paper TitleDocument4 pagesConference Paper Titleshivamsaidane09No ratings yet
- Emp09 PDFDocument5 pagesEmp09 PDFKarthik SNo ratings yet
- Ajtj3770052-050224 2662Document1 pageAjtj3770052-050224 2662desilvamnimeshNo ratings yet
- DAV Public School, Hehal, Ranchi Monday Test, Class-XI M.M-25 Subject-English Time - 1 HourDocument3 pagesDAV Public School, Hehal, Ranchi Monday Test, Class-XI M.M-25 Subject-English Time - 1 HourSHIVAM KUMAR SINGHNo ratings yet
- 6.clean Air Act RA8749-Revised Engr. Henry SorianoDocument100 pages6.clean Air Act RA8749-Revised Engr. Henry SorianoVinz SelabeNo ratings yet
- CARAIG, Jorgie D. BSCE 3-3-Reflection PaperDocument1 pageCARAIG, Jorgie D. BSCE 3-3-Reflection PaperJorgieNo ratings yet
- 11 - Chapter 2 PDFDocument74 pages11 - Chapter 2 PDFDev RayNo ratings yet
- Sovenier 2023Document492 pagesSovenier 2023kumarvikas32290No ratings yet