Professional Documents
Culture Documents
A Randomised Controlled Trial of Motivational Interviewing For Smoking Cessation
A Randomised Controlled Trial of Motivational Interviewing For Smoking Cessation
Uploaded by
jamie carpioOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Randomised Controlled Trial of Motivational Interviewing For Smoking Cessation
A Randomised Controlled Trial of Motivational Interviewing For Smoking Cessation
Uploaded by
jamie carpioCopyright:
Available Formats
R Soria, A Legido, C Escolano, et al
A randomised controlled trial
of motivational interviewing
for smoking cessation
Raimundo Soria, Almudena Legido, Concepión Escolano, Ana López Yeste
and Julio Montoya
INTRODUCTION
ABSTRACT Smoking is the main cause of preventable death in
Background developed countries.1 The natural history of
Motivational interviewing is a technique used to untreated smoking involves an increased probability
promote change in addictive behaviour, initially used to
of cardiovascular, respiratory and neoplastic
treat alcoholism. Despite this, its effectiveness has not
been sufficiently demonstrated for giving up smoking. diseases. Every year, tobacco causes 3.5 million
Aim deaths throughout the world.
The aim of the study was to establish whether In Spain, every year 56 000 people die from
motivational interviewing, compared with anti-smoking diseases directly related to smoking.2 According to the
advice, is more effective for giving up the habit.
2001 National Public Health Survey, the prevalence of
Design of study
smoking in the Spanish population over 16 years of
Randomised controlled trial.
age was 34.4% in that year. Compared with the figures
Setting
Primary care in Albecete, Spain. obtained in 1987, when the prevalence was 38.4%, a
Method slight drop in smoking in Spain can be found.3 In men,
Random experimental study of 200 smokers assigned smoking has gone down from 55% in 1987 to 42.1%
to two types of interventions: anti-smoking advice (n = in 2001. During the same period the habit in women
86) and motivational interviewing (n = 114). Subjects in
increased from 23 to 27.2%.
both groups were offered bupropion when nicotine
dependency was high (Fagerström score >7). The Within the sphere of primary health care, treatment
success rate was evaluated by intention to treat; point of tobacco addiction is one of the main challenges,
prevalence abstinence was measured 6 and 12 months in both primary and secondary prevention.
post intervention by personal testimony, confirmed by
However, since utilisation by the general
means of CO-oximetry (value < 6ppm).
population of primary healthcare consultations is
Results
The measure of effectiveness of the treatment for high (it is estimated that 75% of Spaniards consult
giving up smoking after both 6 and 12 months, showed their doctor at least once a year), with average
that the motivational interviewing action was 5.2 times frequency of 5.5 consultations per person yearly, this
higher than anti-smoking advice (18.4 % compared to
gives the GP and the health service numerous
3.4%; 95% confidence interval = 1.63 to 17.13).
opportunities to deal with tobacco addiction.4
Conclusion
The results of our study show that motivational There are many types of interventions to aid in
interviewing is more effective than brief advice for smoking cessation:5 anti-smoking advice given by
giving up smoking. doctors, structured actions in clinic consultations, self-
Keywords
clinical trial; motivation; motivational interviewing;
psychological techniques; smoking; treatment
effectiveness
R Soria, MBBS; A Legido, MBBS; C Escolano, MBBS;
A López Yeste, MBBS, Albacete, Zone I Health Centre, Spain.
J Montoya, MBBS, Albacete, Zone IV Health Centre, Spain.
Address for correspondence
Almudena Legido, Calle los Refranes no 17, Albacete, Spain.
E-mail: allegido17@hotmail.com
Submitted: 15 June 2005; Editor’s response: 4 January 2006;
final acceptance: 12 April 2006.
©British Journal of General Practice 2006; 56: 768–774.
768 British Journal of General Practice, October 2006
Original Papers
help materials, nicotine substitutes, antidepressants
and anxiolytics, aversion therapies, acupuncture and
hypnotherapy.
How this fits in
Smoking is the main cause of preventable death in developed countries.
Research into smoking by primary health care has,
Motivational interviewing is a useful tool for promoting change in addictive
given its feasibility, traditionally been based on
behaviour, although there is not sufficient proof of its effectiveness for smoking
medical anti-smoking advice. It has been shown that
cessation. Evidence from this trial indicates that motivational interviewing may be
brief medical advice is somewhat effective in a useful intervention for giving up smoking in primary healthcare settings.
promoting smoking cessation. Pooled data from 17
studies of brief advice versus no advice (or routine
care) revealed a small but significant increase in the interviews, versus anti-smoking advice for smoking
odds of quitting (odds ratio [OR] = 1.74, 95% cessation, at 6 and 12 months post intervention.
confidence interval [CI] = 1.48 to 2.05) following brief
advice. This equates to an absolute difference in the METHOD
quit rate of 2.5% between those receiving physician This is a randomised experimental study to assess
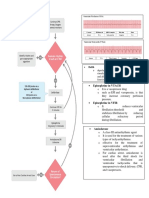
advice and those receiving routine care only. More two actions: advice versus MI (Figure 1).
intensive advice may result in slightly higher rates of
quitting. There is insufficient evidence to determine Physicians
whether use of aids or providing follow-up support The two categories of interventions, as well as all
after offering the advice increases the quit rates any initial and follow-up data collection and measures,
further.6 were conducted by five family physicians working
The apparent low efficacy is offset by the high within the Spanish Public Health Care System in two
number of smokers who may receive this treatment different Health Centres in the city of Albacete. Both
action, through minimum effort on the part of the Centres attend to an urban population of
physician. approximately 48 000 persons each, 13% of whom
More recently, recommendations from various are older than 65 years of age. The five doctors are
agencies (WHO 20017 and CDC 20008) indicate the members of the permanent staff in their respective
need to include motivational interviewing (MI) in the centres, each one assigned to attend a roster of 1900 Figure 1. Flow diagram of
treatment of smoking. patients over the age of 14 years. trial.
MI, a technique described by Miller in 1983,
initially used for treating alcoholism,9,10 is useful for
promoting change in addictive behaviour. It is a 200 smokers (patients)
patient-centred medical interview focused on Random allocation
examination and resolution of ambivalences
regarding unhealthy behaviours or habits. The
Brief advice Motivational
basic idea of this technique is that it is the patient n = 86 interviewing, n = 114
who reflects on and expresses their problems and
desire to change. The MI techniques allow the GP
to bring about an increase in the patient’s
First session First session
motivation, taking into account what their base
History of smoking Motivational History of smoking
motivational level is and always respecting their Stage of change
Stage of change interviewing sessions:
final decisions without penalising them. Brief advice 1. n = 26 (22.8%) First motivational
2. n = 50 (43.9%) interview
Prochaska11 et al, studying processes of change in
3. n = 38 (33.3%)
people who had given up smoking, found that they
were going through a series of stages, each one
characterised by a particular mental attitude and
level of motivational readiness. At present, the Six months Six months
Attendance n = 74 (86%) Attendance n = 87 (76.3%)
process of giving up smoking is studied mainly by No responsea n = 12 (14%) No responsea n = 27 (23.7%)
following the model that these authors put forward.
Most of the studies published using MI as a tool in
the treatment of addictive behaviour deal with
alcohol dependence. Nonetheless, numerous Twelve months Twelve months
Attendance n = 77 (89.5%) Attendance n = 97 (85.1%)
studies have applied the technique to tobacco No responsea n = 9 (10.5%) No responsea n = 17 (14.9%)
addiction, though few of them compare
effectiveness of MI with brief advice.12 a
Some of the patients who did not attend follow-up at 6 months were located for
The aim of the current study is to compare the follow-up at 12 months and vice-versa.
effectiveness in smokers of three motivational
British Journal of General Practice, October 2006 769
R Soria, A Legido, C Escolano, et al
The five GPs had been given specific training in MI Intervention
techniques by means of role-playing and video After opening the envelope, patients in both groups
recordings, in order to establish and combine the were given verbal and written information about the
basic contents, both of the brief individual action study’s purpose, aims and procedures.
(anti-smoking advice) and the MI action. The personal details of each patient were then
collected (age, sex, educational level, employment),
Participants variables relating to tobacco consumption (presence
All subjects in this study were patients on the rosters of disease related to tobacco consumption — chronic
of the five physician–investigators described above. obstructive pulmonary disease (COPD) and
200 active smoker patients between the ages of 15 ischaemic heart disease — number of cigarettes
and 75 years were recruited during regular visits to smoked a day, age when the patient started smoking,
their respective GPs, for whatever reason. None of years smoking) and stage of change, according to the
the subjects had been recipients of pre-selection five stages of change described by Prochaska-
cards nor publicity regarding the trial, nor were they DiClemente:11 precontemplative, contemplative,
chosen for the study with respect to any particular action, maintenance and relapse.
pathology. The degree of nicotine dependency was assessed
A smoker was considered to be any person who by Fagerström’s test.13 Depending on the result that
replied ‘yes’ to the question: Do you smoke? each smoker gives to each question, a certain mark
Patients were recruited over a period of is obtained, that may vary from 0–10 points.
23 months; informed consent was requested from all A degree of slight dependency is considered when
those taking part in the trial. Exclusion criteria were the test varies from 0 to 3 points; moderate
existence of severe psychiatric disorder, a terminal dependency is from 4 to 6 points; a severe degree of
illness or drug-addiction, or age <15 or >75 years. dependency is 7 points or over.
The smokers participating in the study were In all patients, the level of carbon monoxide in the
assessed over a total period of 1 year, and follow- air expired at the start of the study was measured by
ups of the effectiveness of the interventions were means of a micro smokerlyser carbon monoxide (CO)
conducted after 6 and 12 months post intervention. monitor14 (Bedfont Technical Instruments Ltd). CO
values were used as abstinence markers, 6 and
Sample size calculation 12 months after the action. Figures of ≥10 ppm of
Calculation of the sample size was made by CO indicate smokers; 6–10 ppm sporadic smokers,
considering an effectiveness in giving up smoking of and <6 ppm, non-smokers.15
5% with anti-smoking advice and of 20% with MI, In the same first consultation, following data
that is to say a relative effectiveness four times collection and CO measurements, the action
higher for MI over advice. Two groups of 100 assigned to each subject case was carried out.
subjects were necessary (α risk level of 0.05% and Patients receiving anti-smoking advice were
90% capacity to detect the difference existing given one intervention session consisting of a
between groups). personal talk by their physician, lasting
approximately 3 minutes. The dangers of smoking
Randomisation sequence generation were explained, as well as the advantages of giving
The patients were randomly assigned to either one of it up. The information given in all advice
the actions groups by means of a non-block table of consultations was the same and in accordance with
random numbers. The assignment sequence the recommendations of the Smoking Department
established resulted in one group of 86 patients of the Spanish Pneumology and Chest Surgery
receiving brief advice and another of 114 subjects Association (SEPAR).16
assigned to MI. Patients assigned to MI were given the first of a
Two hundred non-transparent sealed envelopes total of three 20–minute interviews conducted in the
containing the interventions (either brief advice or MI) physician’s office. There was no established protocol
were prepared. Before the start of daily for time lapse between interviews; rather,
consultations, the GPs conducting the interventions appointments for the subsequent session were set
would extract one of the envelopes, not knowing the up with the GP at the patient’s convenience.
type of action it contained. The first smoker patient Patients in both intervention groups showing high
who attended the consultation would be offered the nicotine-dependency (Fagerström’s test scores of
possibility of taking part in the study. If they accepted ≥7), were offered the possibility of concurrent
and signed the informed consent form, the envelope treatment with bupropion, the first non-nicotine
would be opened, upon which the GP would learn of medication approved for treating tobacco
the patient’s group assignment. dependence.17
770 British Journal of General Practice, October 2006
Original Papers
Outcome measures
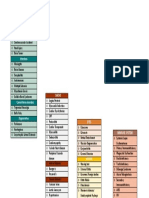
Table 1. Baseline characteristics of the smokers in both
All patients were contacted at 6 and 12 months post
actions.
intervention for follow-up appointments. Smoking
habits were assessed 6 and 12 months post Motivational Advice
intervention, by measuring number of cigarettes Action Interviewing n = 114 n = 86
smoked a day, the degree of nicotine dependency Mean age in years (SD) 38.58 (12.17) 38.44 (12.37)
according to Fagerström’s test, stage of change, as Women (%) 51.8 53.5
well as level of CO in expired air in all those taking Mean age in years when 16.31 (3.70) 17.13 (5.11)
part in the MI group and in those in the advice group started smoking (SD)
who reported abstinence. Smokers in active 86.0 75.6
The final primary variable measured was success employment (%)
index, namely point prevalence of abstinence at 6 and Mean number of years 21.40 (12.29) 19.94 (12.15)
12 months post intervention. Abstinence was of consumption (SD)
subjectively ascertained by means of direct personal Mean number of cigarettes 19.40 (10.26) 17.47 (10.24)
testimony, and objectively confirmed by obtaining smoked a day (SD)
values of less than 6 ppm of CO in expired air Mean CO-oximetry (SD) 15.40 (9.00) 15.10 (10.03)
(reference value acknowledged as a cut-off point Mean Fagerström’s test score (SD) 4.16 (2.71) 3.87 (2.59)
between smokers and non-smokers). Failure of COPD (%) 8.8 4.7
abstinence was defined as continuation of the Ischaemic heart disease (%) 2.6 1.2
smoking habit or non-attendance of follow-ups to Precontemplative stage (%) 56.1 70.9
confirm abstinence. Contemplative stage (%) 36.8 27.9
Decision stage (%) 7.0 1.2
Statistical analysis
COPD = coronary obstructive pulmonary disease.
Statistical analysis was made in blind form, without
knowing the identification labels of the groups that
were compared. The results were analysed using (range = 16–75 years), with a slight predominance of
SPSS. First of all, a description was made of the women over men (52.5 versus 47.5%).
variables studied in both groups, comparing the Only 7% of smokers had been diagnosed with
distribution of the determining factors that may have COPD and 2% with ischaemic heart disease. The
affected the final result, and then a comparison was majority (80.8%) of subjects were in active
made of the proportion of successes by means of the employment, while 19.2% were unemployed or
χ2 test. retired. The average age for starting smoking was
In order to evaluate the modifying variables of the 16 years. Average consumption was 18 cigarettes a
effect and avoid confusion factors, recourse was day and the average smoking period was 20 years
made to multivariant analysis, constructing a logistic (range = 1–55 years). The average score in
regression model by the step-by-step inclusion Fagerström’s test was 4.04. The level of CO in
method, in which the dependent variable was the expired air at the start of the study was 15.27 ppm.
success or failure of the anti-smoking action, after Regarding the degree of motivation according to the
both 6 and 12 months. classification of stages of change, 63.5% of smokers
The trial was analysed by intention to treat, were in a precontemplative stage at the start of the
evaluating each subject in the study group to which study, 32.4% in a contemplative stage and 4.1% had
they were randomly assigned. The extent of the taken the decision to give up smoking. In patients
therapeutic effect and the accuracy in its estimation assigned to advice, 70.9, 27.9 and 1.2% were in the
was considered, calculating the reduction in relative precontemplative, contemplative and determined
risk, the reduction in absolute risk and the absolute stages, respectively, with P = 0.04. In the MI group,
increase in benefit, as well as the number of patients 56.1, 36.8 and 7% were in the above-mentioned
it would be necessary to treat in order to avoid a stages, respectively.
negative result. Patients in this study with high physical
The study was approved by the medical research dependency levels (that is; Fagerström’s test scores
ethics committee of the Albacete University Hospital of ≥7) were offered the possibility of using bupropion
Complex (Spain) on 3 April 2003. as an adjunct medical treatment. This medication
was to be self-financed by the patient. Only 2.5%
RESULTS (five patients) began bupropion use; these five
Demographic and smoking characteristics patients were assigned to the MI intervention.
The baseline characteristics of the two groups are Patient adherence to the MI intervention was as
shown in Table 1. Patients’ average age was 38 years follows: 26 (22.8%) smokers attended the first
British Journal of General Practice, October 2006 771
R Soria, A Legido, C Escolano, et al
changes, without imposition or blame by the
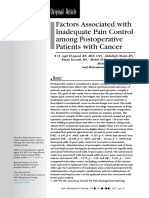
Table 2. Effectiveness of actions to give up smoking after 6
and 12 months. physician. Repeated advice, on the other hand, may
be perceived as preaching, with subsequent risk of
Motivational damaging the doctor–patient relationship and
Advice Interviewing
producing contrary behaviour.18
n = 86 n = 114 P OR 95% CI NNT
Abstinence after 3 (3.5) 21(18.4) 0.00 6.25 1.8-21.71 7
Comparison with existing literature
6 months (%)a
Abstinence after 3 (3.5) 21(18.4) 0.001 6.25 1.8-21.71 7 Until now, there has been limited evidence that MI
12 months (%)a and stage-of-change based interventions are
a
The fact that identical abstinence figures were obtained at 6 and 12 months in both groups
effective for smoking cessation.19 The use of these
was purely coincidental. NNT = number needed to treat. OR = odds ratio. methods has therefore not been justified in routine
care by family physicians. Brief advice, however,
interviewing only, 50 (43.9%) attended two interviews about which more has been published, has been
and 38 (33.3%) patients kept all three appointments. more extensively employed in clinical practice.6
A previous study conducted in a primary care
Effectiveness setting by Butler et al12 comparing effectiveness of MI
The measure of effectiveness of smoking cessation versus brief advice for smoking cessation in 536
treatment at both 6 and 12 months post smokers not selected for any other pathology,
intervention showed that the action based on MI showed moderately higher success for the stage-
was 5.28 times more successful than anti-smoking based intervention. At 6 months post intervention,
advice (Table 2; odds ratio [OR] = 6.25, 95% CI = significant differences between groups in scores on
1.8 to 21.7 at both 6 and 12 months).The fact that self-reported abstinence in the previous 24 hours
identical abstinence figures were obtained at 6 and were found (OR = 2.86, 95% CI = 1.21 to 6.76).
12 months in both patient groups was purely However, the odds of abandonment of the smoking
coincidental, given that some patients who did not habit at 6 months were considerably higher in our
respond at 6 months to confirm abstinence, did so study for the MI group (OR = 7.65, 95% CI = 2.18 to
at 12 months and vice versa. 26.84) than in the Butler trial.12
The absolute increase in benefit was 14.9% (95% Our relatively high abstinence levels for the MI
CI = 6.8 to 23%) and the number of smokers intervention may be partly attributed to the fact that
necessary to treat was 7 (95% CI = 5 to 15). the GPs conducting the interviews in our study
Regarding attendance of follow-up, 12 patients were the patients’ regular family physicians. The GP
from the advice group and 27 patients from the MI registrars in the Butler et al study12 (resident
group did not attend the first follow-up at 6 months doctors) trained in MI techniques were not the
post intervention. At 12 months, nine advice and 17 patients’ habitual physicians; thus, although
MI subjects did not attend appointments. In the perhaps more enthusiastic, their experience and
logistic regression model, after both 6 and knowledge of the study subjects would have been
12 months, the action appeared as a variable more limited. Moreover, patients tend to respond
independently associated with smoking cessation. more positively to doctors with whom they have
No confusion factors or effect-modifying variables maintained enduring doctor–patient relationships.
were found. The probability of giving up the habit Another difference between the current study and
was 7.6 times greater in the MI group after the Butler trial lies in the intensity of the MI
6 months (OR = 7.65, 95% CI = 2.18 to 26.84) and intervention. Our patients were scheduled for three
6.9 times greater after 12 months (OR = 6.91, 95% MI consultations, whereas in the Butler study, they
CI = 1.98 to 24.15). were exposed to only one interview. Therefore,
repeated stage of change based interventions may
DISCUSSION be more effective than a single consultation.
Summary of main findings Other interventions reviewed by Lancaster and
The primary objective of this study was to Stead20 of a similar nature to MI, such as individual
determine whether MI was a more effective anti- behavioural counselling, have shown a certain
smoking intervention than brief advice. Our results efficacy, with a reported OR of abandonment of the
show that MI is more effective than brief advice for smoking habit of 1.56 (95% CI = 1.32 to 1.84). Once
smoking cessation in a primary care setting. Higher again, however, the OR we report are considerably
levels of abstinence in the MI group may be higher. These differences in results may be due to
attributed, in part, to the patient-centred nature of the nature of stage-based interventions, as
the stage based intervention, where smokers previously described, and/or to the fact that in the
actively involve themselves in making habit behavioural counselling studies reviewed, sessions
772 British Journal of General Practice, October 2006
Original Papers
were administered by a trained therapist unknown opposed to a block table, resulting in unbalanced
to the patient. group sizes of 114 MI patients and 86 belonging to
the advice group.
Strengths and limitations of the study
This is a study of the development and evaluation of Implications for future research
a motivational interviewing intervention for primary The unusually high OR of abandonment of the
care use only. In our trial, patients were recruited smoking habit obtained in our study by the MI
during a regular visit to their GP for whatever reason intervention, raises several questions for future
and were not selected for any type of disease. No research. Since the current study was conducted in
prior advertisements were issued regarding the trial a general practice setting with GPs familiar to
and subjects had not received pre-selections cards. patients, comparisons should be made with stage-
Therefore a more realistic assessment of the based techniques carried out by therapists
effectiveness of the intervention variable could be unconnected to subjects, in specific tobacco
made under normal conditions experienced by GPs addiction treatment consultations.
and their patients on a daily basis. The MI group in our study received three treatment
The design of our study presents several sessions, whereas patients in the advice group were
limitations. As part of our efforts to evaluate the exposed to only one consultation with the GP,
efficacy of MI in the normal course of a GP’s daily suggesting that intensity of the intervention, rather
practice, adolescents as young as 15 years of age than efficacy of stage-based therapy and MI, may be
were included in the trial, given the reality that family responsible for higher abstinence levels. Further
physicians in Spain attend patients over the age of investigations are needed to compare effectiveness
14 years (minors of 14 years and younger are treated of more brief tailored MI interventions with brief
by paediatricians). The drawback to the admittance advice and to evaluate whether single session MI
of young adolescent smokers in the study lies with interventions are as effective as repeated ones.
the fact that they have not had sufficient time to It may also be of interest to ascertain from which
develop established nicotine dependency, thus stage of change anti-smoking therapy is most likely to
increasing their chances of successful quitting. be successful. The cost-effectiveness of MI
For ethical reasons, patients in our study with high compared to other interventions should also be
nicotine dependency were offered bupropion as investigated, since application of the method requires
adjunct therapy (five patients from the MI group training of physicians and extra consultation time.
accepted). It is well-demonstrated that this therapy is
effective for smoking cessation, increasing quitting Funding body
odds by 1.5–2 times, independent of setting.17 Research project financed by the Department of Health,
Health Science Institute of the Government of the
Therefore, these patients should probably have been Autonomous Communities of Castille – La Mancha,(Spain)
excluded from the trial, as they may potentially have according to the decision taken at the meeting of 19
February 2003 (D. O. C. M. number 21)
skewed results in favour of the MI intervention.
Ethics committee
Regarding patient characteristics at the outset of
Project approved by the Medical Research Ethics
the study, the two groups were not homogeneous Committee of the Albacete Health Service,(Spain) taking
with respect to the variable ‘stage of change.’ A into consideration that the aforesaid project was in
accordance with the essential ethical standards used in this
greater number of MI patients than advice patients field, as recorded in minutes no. 05/03 of the Medical
were classified as belonging to a contemplative or Research Ethics Committee meeting in Albacete held on
3 April 2003
decision stage (Table 1), thus favouring more
successful outcomes in the MI group. However, it is Competing interests
The authors have stated that there are none
also possible that since stage of change was
Acknowledgements
determined following group assignation of subjects, We wish to thank all the patients who worked with us and
GPs tended to overestimate the motivation of were involved in the project. Special thanks go to Dr. López
Torres for his impartial cooperation as scientific advisor.
patients belonging to the MI group. Ideally, data
collection from smokers and classification of stage of
REFERENCES
change should have been performed by an 1. Peto R, López AD, Boreham J, et al. Mortality from tobacco in
independent investigator before randomisation and developed countries: indirect estimation from national vital
statistics. Lancet 1992; 339: 1268–1278.
group assignation of patients. However, our wish to
2. Banegas Banegas JR, Diez Gañan L, Rodríguez-Artalejo F, et al.
be pragmatic and produce minimal alterations in the Mortalidad atribuible al tabaquismo en España en 1998.
course of our consultations did not allow us to (Smoking-attributable deaths in Spain in 1998). Med Clin (Barc)
2001; 117: 692–694.
proceed in this way.
3. Ministerio de Sanidad y Consumo. Encuesta Nacional de Salud de
Lastly, patient randomisation was achieved by España 1997. Madrid: Ministerio de Sanidad y Consumo, 1999.
applying a non-block table of random numbers as 4. Alonso JM, Magro R, Martínez JA, Sanz N. Tabaco y atención
British Journal of General Practice, October 2006 773
R Soria, A Legido, C Escolano, et al
primaria. En: Comité Nacional para la Prevención del Tabaquismo.
El Libro Blanco sobre el tabaquismo en España. (Tobacco and
Primary Care. In: National Committee Smoking Prevention. White
Paper about Smoking in Spain). Barcelona: Glosa SL, 1998.
5. Lancaster T, Stead L, Silagy C, Sowden A. Effectiveness of actions
to help people stop smoking: findings from the Cochrane Library.
BMJ 2000; 321: 355–358.
6. Lancaster T, Stead LF. Physician advice for smoking cessation
[review]. Cochrane Database Syst Rev 2004; Issue 4: CD000165.
7. World Health Organisation. Evidence-based recommendations on
the treatment of tobacco dependency. Copenhagen: WHO, 2001.
8. Centres for Disease Control and Prevention. Strategies for
reducing exposure to environmental tobacco smoke, increasing
tobacco-use cessation and reducing initiation in communities and
health-care systems. A report on recommendations of the Task
Force on Community Preventive Services. MMWR 2000; 49(RR-
12): 1–11.
9. Miller WR. Motivational interviewing with problem drinkers.
Behavioural Psychotherapy 1983; 11: 147–172.
10. Miller WR, Rollnick S. Motivational interviewing: preparing people
to change addictive behaviour. Barcelona: Ed Paidós; 1999.
11. Prochaska JO, DiClemente CC. Stages and processes of self-change
of smoking: toward an integrative model of change. J Consult Clin
Psychol 1983; 51(3): 390–395.
12. Butler C, Rollnick S, Cohen D, et al. Motivational consulting versus
brief advice for smokers in general practice: a randomised trial. Br
J Gen Pract 1999; 49: 611–616.
13. Fagerström KO, Schneider NG. Measuring nicotine dependence: a
review of the Fagerström Tolerance Questionnaire. J Behav Med
1989; 12: 159–182.
14. Jarvis M J, Russell MAH, Saloojee Y. Expired air carbon monoxide:
a simple breath test of tobacco smoke intake. BMJ 1980; 281:
484–485.
15. Russell MAH, Merriman R, Stapleton J, Taylor W. Effect of
nicotine chewing gum as an adjunct to general practitioner advice
against smoking. BMJ 1983; 287: 1782–1785.
16. Jiménez CA, Solano S, González de Vega JM, et al. Tratamiento del
tabaquismo. En: Recomendaciones SEPAR. (Treatment of tobacco
dependency. In: SEPAR Recommendations). Barcelona: Doyma,
1998: 421–436.
17. Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking
cessation. Cochrane Database Syst Rev 2004; Issue 4: CD000031.
18. Butler CC, Pill R, Stott NC. Qualitative study of patients’
perceptions of doctors’ advice to give up smoking: implications for
opportunistic health promotion. BMJ 1998; 316: 1878–1881.
19. Riemsma RP, Pattenden J, Bridle C, et al. Systematic review of the
effectiveness of stage based interventions to promote smoking
cessation. BMJ 2003; 326: 1175–1177.
20. Lancaster T, Stead LF. Individual behavioural counselling for
smoking cessation. Cochrane Database Syst Rev 2005; Issue 2:
CD001292.
774 British Journal of General Practice, October 2006
You might also like
- Jake - MH TeamDocument1 pageJake - MH Teamjamie carpioNo ratings yet
- Aversive Smoking For Smoking CessationDocument22 pagesAversive Smoking For Smoking Cessation77felixNo ratings yet
- Clinical Hypnosis For Smoking CessationDocument9 pagesClinical Hypnosis For Smoking Cessationamad90100% (1)
- Putting Evidence Into Practice Smoking CessationDocument48 pagesPutting Evidence Into Practice Smoking CessationXinyi LiewNo ratings yet
- Intervention For Smoking ReductionDocument15 pagesIntervention For Smoking Reductionben mwanziaNo ratings yet
- Passed and Cleared' - Former Tobacco Smokers' Experience in Quitting SmokingDocument9 pagesPassed and Cleared' - Former Tobacco Smokers' Experience in Quitting SmokingzikriNo ratings yet
- Jurnal Metode Konseling Dalam Membantu Mengurangi Kecanduan RokokDocument5 pagesJurnal Metode Konseling Dalam Membantu Mengurangi Kecanduan RokokNina MarliatiNo ratings yet
- Efektifitas Terapi Akupresur Terhadap Upaya Berhenti Merokok Di Desa Sungai Terap Kecamatan Kumpeh UluDocument8 pagesEfektifitas Terapi Akupresur Terhadap Upaya Berhenti Merokok Di Desa Sungai Terap Kecamatan Kumpeh UluOktia Rahmi100% (1)
- Factors Relating To Failure To Quit Smoking A Prospective Cohort StudyDocument7 pagesFactors Relating To Failure To Quit Smoking A Prospective Cohort StudySilas SilvaNo ratings yet
- Does A Population-Based Multi-Factorial Lifestyle Intervention Increase Social Inequality in SmokingDocument9 pagesDoes A Population-Based Multi-Factorial Lifestyle Intervention Increase Social Inequality in SmokingIr. Nyoman MahardikaNo ratings yet
- Cesation For Mild Intelectual Singh 2013Document10 pagesCesation For Mild Intelectual Singh 2013alejandroNo ratings yet
- Jurnal 1.4 yDocument20 pagesJurnal 1.4 yAmbarsari HamidahNo ratings yet
- Evaluation of Smoking Cessation Success in AdultsDocument8 pagesEvaluation of Smoking Cessation Success in AdultsSISNo ratings yet
- Jurnal Metode Konseling Dalam Membantu Mengurangi Kecanduan Rokok-DikonversiDocument5 pagesJurnal Metode Konseling Dalam Membantu Mengurangi Kecanduan Rokok-DikonversiNina MarliatiNo ratings yet
- A Game For SmokersDocument4 pagesA Game For SmokerstifaniNo ratings yet
- Aspek Neurologi Hipnoterapi Untuk Penghentian Merokok: Neurogical Aspects of Hypnotherapy For Smoking CessationDocument9 pagesAspek Neurologi Hipnoterapi Untuk Penghentian Merokok: Neurogical Aspects of Hypnotherapy For Smoking CessationSulaiman Noer FaiezyNo ratings yet
- Psychological Features of Smokers: Askin Gu Lsen MD and Bu Lent Uygur MDDocument6 pagesPsychological Features of Smokers: Askin Gu Lsen MD and Bu Lent Uygur MDMarianaNo ratings yet
- Tobacco Cessation Treatment PlanDocument7 pagesTobacco Cessation Treatment PlanyellowishmustardNo ratings yet
- The Effectiveness of Different Treatment Methods To Curb Smoking AddictionDocument15 pagesThe Effectiveness of Different Treatment Methods To Curb Smoking AddictionAzreZephyrNo ratings yet
- 9721 Smoking Cessaton Newsletter 1981Document8 pages9721 Smoking Cessaton Newsletter 1981Julia PurperaNo ratings yet
- Jurnal StopSmoking! PDFDocument21 pagesJurnal StopSmoking! PDFIbrahim JutNo ratings yet
- Research Paper-2Document9 pagesResearch Paper-2api-741551545No ratings yet
- Antidepresivos y PesoDocument11 pagesAntidepresivos y Pesogtellez25No ratings yet
- Hynoterapi Untuk Berhenti Merokok PDFDocument14 pagesHynoterapi Untuk Berhenti Merokok PDFsri subektiNo ratings yet
- AJGP 10 2019 Focus Manger Lifestyle Interventions Mental Health WEBDocument4 pagesAJGP 10 2019 Focus Manger Lifestyle Interventions Mental Health WEBisitugasnandasekarbuanaNo ratings yet
- Tobacco Cessation in India: Labani Satyanarayana, Smita Asthana, Sumedha Mohan, Gourav PopliDocument3 pagesTobacco Cessation in India: Labani Satyanarayana, Smita Asthana, Sumedha Mohan, Gourav PopliHakim ShaikhNo ratings yet
- Dapus Referat No.4Document7 pagesDapus Referat No.4Muhammad AkrimNo ratings yet
- Smoking Cessation Nursing InterventionsDocument12 pagesSmoking Cessation Nursing Interventionsapi-741272284No ratings yet
- Smoking in Psychiatric Hospitals: What Is The Role of Nursing Staff?Document5 pagesSmoking in Psychiatric Hospitals: What Is The Role of Nursing Staff?International Journal of Innovative Science and Research TechnologyNo ratings yet
- Rajiv Gandhi University of Health Sciences, Bangalore, KarnatakaDocument26 pagesRajiv Gandhi University of Health Sciences, Bangalore, KarnatakaAmit TamboliNo ratings yet
- Nursing Research Paper Final DraftDocument15 pagesNursing Research Paper Final Draftapi-593455086No ratings yet
- Psychological Effect F NicotineDocument6 pagesPsychological Effect F NicotinehelfiNo ratings yet
- 2018 HuanDocument8 pages2018 HuanRahul GoyalNo ratings yet
- Q 3 Cdy HKB PHBXM 5 WN QX VW XG PDocument8 pagesQ 3 Cdy HKB PHBXM 5 WN QX VW XG P517wangyiqiNo ratings yet
- Walid Sarhan F. R. C. PsychDocument46 pagesWalid Sarhan F. R. C. PsychFree Escort ServiceNo ratings yet
- Accepted ManuscriptDocument40 pagesAccepted ManuscriptsueffximenaNo ratings yet
- Smoking Cessation or Reduction With Nicotine Replacement Therapy: A Placebo-Controlled Double Blind Trial With Nicotine Gum and InhalerDocument28 pagesSmoking Cessation or Reduction With Nicotine Replacement Therapy: A Placebo-Controlled Double Blind Trial With Nicotine Gum and InhalerSigit Harya HutamaNo ratings yet
- Contemporary Clinical TrialsDocument8 pagesContemporary Clinical TrialsAzisahhNo ratings yet
- Cooper 2019Document16 pagesCooper 2019Lee HaeunNo ratings yet
- RelapseDocument10 pagesRelapseEmil Eduardo Julio RamosNo ratings yet
- Cannabis Medicina Basada en Evidencia EspañaDocument6 pagesCannabis Medicina Basada en Evidencia EspañaCarla AndradeNo ratings yet
- AbstractreadingDocument2 pagesAbstractreadingapi-341690050No ratings yet
- Health Consequences of Sustained Smoking Cessation FinalDocument5 pagesHealth Consequences of Sustained Smoking Cessation FinalAmin Mohamed Amin DemerdashNo ratings yet
- Epidemiological Characteristics, Safety and Efficacy of Medical Cannabis inDocument7 pagesEpidemiological Characteristics, Safety and Efficacy of Medical Cannabis inDanielNo ratings yet
- Journal Analysis-RESKI NURUL AFIFAHDocument6 pagesJournal Analysis-RESKI NURUL AFIFAHResky Nurul AfifaNo ratings yet
- Tatarsky+Marlatt 2010Document6 pagesTatarsky+Marlatt 2010Iyari LovegoodNo ratings yet
- File 1491650685 PDFDocument10 pagesFile 1491650685 PDFAngga PratamaNo ratings yet
- Dong Liu WuDocument29 pagesDong Liu WuJohn Vincent Consul CameroNo ratings yet
- How To Encourage To Stop SmokingDocument12 pagesHow To Encourage To Stop SmokingSamNo ratings yet
- Dawley 1975Document4 pagesDawley 1975Noor ChahayaNo ratings yet
- A Randomized, Multicentre, Open-Label, Comparative Trial of Disulfuram, Naltrexone, and Acamprosate in The Treatment of Alcohol DependenceDocument9 pagesA Randomized, Multicentre, Open-Label, Comparative Trial of Disulfuram, Naltrexone, and Acamprosate in The Treatment of Alcohol DependenceAlexander ColeNo ratings yet
- Pembelajaran Penyakit Terkait Perilaku Merokok Dan Edukasi Untuk Berhenti Merokok Di Pendidikan Dokter Fakultas Kedokteran UgmDocument16 pagesPembelajaran Penyakit Terkait Perilaku Merokok Dan Edukasi Untuk Berhenti Merokok Di Pendidikan Dokter Fakultas Kedokteran UgmkiranaNo ratings yet
- Pepito, Rjay cls#3Document8 pagesPepito, Rjay cls#3PEPITO, ARJAY F.No ratings yet
- Comparison of Topiramate and Naltroxene For Treatment of Alcohol DependenceDocument8 pagesComparison of Topiramate and Naltroxene For Treatment of Alcohol Dependencejgwatson1979No ratings yet
- Fneur 10 01145Document9 pagesFneur 10 01145ivoroNo ratings yet
- A Population Level Analysis of Changes in AustraliDocument17 pagesA Population Level Analysis of Changes in AustraliYuning tyas Nursyah FitriNo ratings yet
- J Jpsychires 2010 06 006Document7 pagesJ Jpsychires 2010 06 006Lumeiko LukaNo ratings yet
- Prevalence of Tobacco and Cigarette Consumption and Their Relationship Between Psychological Behaviour - A Narrative ReviewDocument6 pagesPrevalence of Tobacco and Cigarette Consumption and Their Relationship Between Psychological Behaviour - A Narrative ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Drug and Alcohol DependenceDocument7 pagesDrug and Alcohol DependenceNur Melizza, S.Kep., NsNo ratings yet
- Developing and Implementing A Smoking Cessation Intervention in Primary Care in NepalDocument1 pageDeveloping and Implementing A Smoking Cessation Intervention in Primary Care in NepalCOMDIS-HSDNo ratings yet
- Motivasi Berhenti Merokok Pada Perokok Dewasa Muda Berdasarkan Transtheoretical Model (TTM)Document8 pagesMotivasi Berhenti Merokok Pada Perokok Dewasa Muda Berdasarkan Transtheoretical Model (TTM)ari edogawaNo ratings yet
- Culture and Sensitivity: InhalationDocument3 pagesCulture and Sensitivity: Inhalationjamie carpioNo ratings yet
- Mari Andrew: Am I There Yet?: The Loop-De-Loop, Zigzagging Journey To AdulthoodDocument4 pagesMari Andrew: Am I There Yet?: The Loop-De-Loop, Zigzagging Journey To Adulthoodjamie carpioNo ratings yet
- RowariwudujiladekodazelaDocument3 pagesRowariwudujiladekodazelajamie carpioNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 4jamie carpioNo ratings yet
- Cardiovascular Disorders: Types of DysrythmiasDocument3 pagesCardiovascular Disorders: Types of Dysrythmiasjamie carpioNo ratings yet
- Brunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 6Document1 pageBrunner and Suddarth's Textbook of Medical-Surgical Nursing 12th Ed. (Dragged) 6jamie carpioNo ratings yet
- Jake PetersonDocument1 pageJake Petersonjamie carpioNo ratings yet
- Public Health Community Health Nursing: Goal: To Enable EveryDocument10 pagesPublic Health Community Health Nursing: Goal: To Enable Everyjamie carpioNo ratings yet
- Code MNGTDocument3 pagesCode MNGTjamie carpioNo ratings yet
- Paid Maternity Leave Claiming Personal Exemptions National Immunization DayDocument2 pagesPaid Maternity Leave Claiming Personal Exemptions National Immunization Dayjamie carpioNo ratings yet
- Hepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis GDocument9 pagesHepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis Gjamie carpioNo ratings yet
- MS TopicsDocument1 pageMS Topicsjamie carpioNo ratings yet
- El Aqoul2017Document9 pagesEl Aqoul2017jamie carpioNo ratings yet
- Nusing NCP Blood Transfusion NCP: Total Parenteral NutriDocument2 pagesNusing NCP Blood Transfusion NCP: Total Parenteral Nutrijamie carpioNo ratings yet
- Rapid Rehabilitation Nursing in Postoperative Patients With Colorectal Cancer and Quality of LifeDocument8 pagesRapid Rehabilitation Nursing in Postoperative Patients With Colorectal Cancer and Quality of Lifejamie carpioNo ratings yet
- Communication Competency: The Topic of Lifelong Learning For Nurse Managers in HospitalsDocument7 pagesCommunication Competency: The Topic of Lifelong Learning For Nurse Managers in Hospitalsjamie carpioNo ratings yet
- CONCEPTSDocument1 pageCONCEPTSjamie carpioNo ratings yet
- Family Nursing Care PlanDocument34 pagesFamily Nursing Care Planjamie carpioNo ratings yet
- OBSTETRICSDocument4 pagesOBSTETRICSjamie carpioNo ratings yet
- Citation 336796047Document1 pageCitation 336796047jamie carpioNo ratings yet
- Electronic Physician (ISSN: 2008-5842) : 1.1. BackgroundDocument10 pagesElectronic Physician (ISSN: 2008-5842) : 1.1. Backgroundjamie carpioNo ratings yet
- 2012 PatrickWilliams SDTandMI IJBNPADocument12 pages2012 PatrickWilliams SDTandMI IJBNPATitis Retno Sawitri SawitriNo ratings yet
- Boanerges: LewisDocument1 pageBoanerges: Lewisapi-245244824No ratings yet
- Groundswell Room To Breathe Full Report 2016Document35 pagesGroundswell Room To Breathe Full Report 2016Maria MirabelaNo ratings yet
- Smoking Secnav 5100 - 13cDocument8 pagesSmoking Secnav 5100 - 13cWill BorrallNo ratings yet
- Example of A Healthy Meal Plan For A 45 Year Old ManDocument12 pagesExample of A Healthy Meal Plan For A 45 Year Old ManzyloexNo ratings yet
- NURS FPX 6026 Assessment 3 Population Health Policy AdvocacyDocument4 pagesNURS FPX 6026 Assessment 3 Population Health Policy AdvocacyEmma WatsonNo ratings yet
- Final Thesis Topic About Sin Tax LawDocument11 pagesFinal Thesis Topic About Sin Tax LawRomnick JesalvaNo ratings yet
- Potential Therapeutic Effects of PsilocybinDocument7 pagesPotential Therapeutic Effects of Psilocybindaniel_jose_skateNo ratings yet
- Market Research TRAIN LAWDocument60 pagesMarket Research TRAIN LAWRusselNo ratings yet
- Effect of VareniclineDocument8 pagesEffect of VareniclineDANIELA GUARDO CARMONA ESTUDIANTENo ratings yet
- Research Paper About Smoking in The PhilippinesDocument8 pagesResearch Paper About Smoking in The Philippinesefj02jba100% (1)
- Note GuideDocument2 pagesNote GuideDemetrius Hobgood0% (1)
- Final Draft of Smoking Cessation Poster TemplateDocument1 pageFinal Draft of Smoking Cessation Poster Templateapi-540025326No ratings yet
- Amanda B.'s Story - Real Stories - Tips From Former Smokers - CDCDocument4 pagesAmanda B.'s Story - Real Stories - Tips From Former Smokers - CDCalex SimpsonNo ratings yet
- Northwest Queens Community Health ProfileDocument16 pagesNorthwest Queens Community Health ProfileAlicia FernandezNo ratings yet
- Name: Shrushti Shah Class: 11 B Roll No.: 43 Subject: Biology Topic: How Cigarettes Affect Your Health?Document23 pagesName: Shrushti Shah Class: 11 B Roll No.: 43 Subject: Biology Topic: How Cigarettes Affect Your Health?AHMED NAEEM 2No ratings yet
- Hypnosis Scripts ExamplesDocument8 pagesHypnosis Scripts Exampleserich70No ratings yet
- Text For Number 1-5 Teenagers Smoke: Riventus Xiipa1Document3 pagesText For Number 1-5 Teenagers Smoke: Riventus Xiipa1zzzzjrjaNo ratings yet
- Best Pulmonologist in DelhiDocument3 pagesBest Pulmonologist in DelhiDr Vikas MittalNo ratings yet
- Test 30Document8 pagesTest 30Hùng Thân NguyênNo ratings yet
- Writing Letter FormatDocument8 pagesWriting Letter FormatIggy GalganoNo ratings yet
- Tobacco CessationDocument45 pagesTobacco CessationGhada El-moghlyNo ratings yet
- Directed Writing ArticleDocument2 pagesDirected Writing ArticleAhmad Ismail71% (7)
- Truth Initiative Statement On Harm Reduction FinalDocument13 pagesTruth Initiative Statement On Harm Reduction FinalBrent StaffordNo ratings yet
- Stage of Change-Questions and StrategiesDocument2 pagesStage of Change-Questions and Strategiespharmacist2000No ratings yet
- Plan of Care For Ineffective Air Way 1Document6 pagesPlan of Care For Ineffective Air Way 1LisaNo ratings yet
- Smoking, Smoking CessationDocument5 pagesSmoking, Smoking CessationNikhilNo ratings yet
- Harm Reduction Strategy PDFDocument184 pagesHarm Reduction Strategy PDFArjumand AdilNo ratings yet
- Smoking Cessation in RSNDocument5 pagesSmoking Cessation in RSNtonylee24No ratings yet