Professional Documents
Culture Documents
Verma 2017
Verma 2017
Uploaded by
Vinh Quy VoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Verma 2017
Verma 2017
Uploaded by
Vinh Quy VoCopyright:
Available Formats
Opinion
VIEWPOINT
The Metabolodiuretic Promise of Sodium-
Dependent Glucose Cotransporter 2 Inhibition
The Search for the Sweet Spot in Heart Failure
Subodh Verma, MD, Clinical trials often yield surprising results, and in the changes. In addition, it has been speculated that SGLT2
PhD contemporary era, undoubtedly, the Empagliflozin inhibition may serve as a metabolic modulator pro-
Division of Cardiac Removal of Excess of Glucose Outcome (EMPA-REG moting improved cardiac substrate use and overall
Surgery, Department of
OUTCOME) trial stands out as one such example.1,2 No energetics.4,5 Accordingly, SGLT2 inhibition mediated in-
Surgery, St Michael’s
Hospital, University of one could have predicted that a sodium-dependent glu- creases in ketone bodies and may provide a more energy-
Toronto, Toronto, cose cotransporter 2 (SGLT2) inhibitor, which works to efficient source of adenosine triphosphate than other
Ontario, Canada. promote urinary glucose excretion as a treatment ap- conventional substrates. Although no specific data on
proach to hyperglycemia, would cut all-cause mortality measures of left ventricular structure and function are
John J. V. McMurray,
by about one-third in patients with type 2 diabetes. Just available from the EMPA-REG OUTCOME study, such
BSc (Hons), MB ChB
(Hons), MD as surprising were the observations that the reductions studies are currently under way (clinicaltrials.gov
British Heart in mortality were possibly driven by a reduction in heart NCT02998970). A small case series also demonstrates
Foundation failure as opposed to atherothrombotic events. De- that short-term treatment caused a marked reduction
Cardiovascular
Research Centre, spite these salutary clinical effects, the physiological in left ventricular mass index while also improving mea-
University of Glasgow, mechanisms responsible for these benefits are not yet sures of diastolic dysfunction.6
Glasgow, United known. The time frame of the effect precludes a glucose- The putative renal protective effects and their
Kingdom.
mediated effect, and furthermore, many other equally biological basis must also be addressed. In EMPA-REG
or more effective antihyperglycemic therapies are not OUTCOME, patients treated with empagliflozin had a
David Z. I. Cherney,
MD, PhD associated with reduced heart failure. The remarkable 39% reduction in the composite renal end point of pro-
Division of Nephrology, renal benefits noted in the trial were also surprising.2 Be- gression to macroalbuminuria, doubling of creatinine
Department of cause the glycosuric effects of SGLT2 inhibition are de- level, renal replacement therapy, or renal death.2 Many
Medicine, Toronto
pendent on the amount of filtered glucose and there- of the physiological changes associated with SGLT2 in-
General Hospital,
University of Toronto, fore diminished in participants with low glomerular hibition may be renal-protective including lowering of
Toronto, Ontario, filtration rate, it was surprising to note that treatment blood pressure, hemoglobin A1c level, and plasma uric
Canada. with empagliflozin resulted in a marked approximately acid level. In addition to these changes outside of the kid-
40% reduction in proteinuria and doubling of serum cre- ney, SGLT2 inhibition is associated with decreases in in-
atinine in the absence of marked differences in glyce- traglomerular pressure and hyperfiltration, likely inde-
mia. While the scientific community struggles to under- pendent of systemic circulatory effects, glycemia, or
stand the biologic basis and clinical implications of these weight. These direct intrarenal hemodynamic effects
observations, several questions related to EMPA-REG have been most widely attributed to vasoconstriction of
OUTCOME have come into focus: can SGLT2 inhibitors the afferent renal arteriole in response to increased so-
be used to treat heart failure as opposed to prevent heart dium chloride delivery to the macula densa, an effect
failure in diabetes? Can SGLT2 inhibitors be a treat- called tubuloglomerular feedback. The decline in glo-
ment for heart failure in patients without type 2 diabe- merular hypertension is also likely to be responsible for
tes? It is also tempting to ask whether SGLT2 inhibitors the antiproteinuric effect of SGLT2 inhibitors because the
will emerge as primary renoprotective strategies irre- 30% to 40% decline in urinary albumin-to-creatinine ra-
spective of glycemic or baseline renal status. tio is mostly independent of changes in blood pressure
Regarding mechanism(s) that might underlie the and hemoglobin A1c level.7
marked reductions in heart failure hospitalizations, the The final issue that requires reflection is whether the
prevailing thought is that these may be mediated at least cardio-renal benefits of these agents can be observed in
in part through effects on volume status.3 It is hypoth- euglycemic individuals without diabetes. The effect of
esized that osmotic diuresis accompanied by sustained SGLT2 inhibition on renal hemodynamic parameters and
Corresponding
natriuresis may result in a reduction in preload and over- hence proteinuria is most closely associated with natri-
Author: Subodh
Verma, MD, PhD, all myocardial strain. The effect of this might be particu- uresis leading to tubuloglomerular feedback, rather than
FRCSC, FAHA, Division larly relevant in the setting of patients with diastolic dys- glycosuria, and the antiproteinuric effects of these agents
of Cardiac Surgery, function who may function on a steeper Frank-Starling are seen across the spectrum of estimated glomerular fil-
Department of Surgery,
St Michael's Hospital,
curve, making them particularly sensitive to changes in tration rate, down to chronic kidney disease stage 4, al-
University of Toronto, intravascular volume. Diabetes is associated with an im- though hemoglobin A1c level–lowering and glycosuria ef-
30 Bond St, Bond paired natriuretic response, diminished atrial natri- fects are attenuated. In addition, other proximal tubular
Wing, Ste 8-003,
uretic peptide, and blunted cyclic guanine mono- diuretic agents, such as acetazolamide, reduce renal hy-
Toronto, ON M5B 1W8,
Canada (vermasu phosphate response to volume expansion, and patients perfiltration in patients without diabetes. This observa-
@smh.ca). with diabetes are very susceptible to sodium-volume tion suggests that tubuloglomerular feedback is an
jamacardiology.com (Reprinted) JAMA Cardiology Published online June 21, 2017 E1
© 2017 American Medical Association. All rights reserved.
Downloaded From: http://cardiology.jamanetwork.com/ by a Columbia University User on 07/02/2017
Opinion Viewpoint
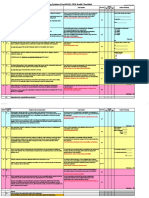
Figure. Proposed Mechanism of Cardiorenal Protection With Sodium-Dependent Glucose
Cotransporter 2 (SGLT2) Inhibitors
Afferent
arteriole Normal
ATP Efferent
arteriole
Myocardial Afferent arteriolar dilatation
energetics
β-hydroxybutyrate Intraglomerular pressure
(ketone body) Na+/glucose cotransport At the level of the kidney, SGLT2
inhibition promotes glycosuria and
natriuresis. It also promotes afferent
arterioral constriction resulting in a
decrease in intraglomerular pressure.
Afterload A reduction in preload and resultant
left ventricular (LV) wall stress
SGLT2 inhibitors cause improves overall LV filling conditions.
afferent arteriolar
Additionally, metabolic effects of
constriction
SGLT2 inhibition to improve
LV wall myocardial energetics and reduce
stress afterload have also been proposed as
cardioprotective mechanisms.
ATP indicates adenosine
Diuresis triphosphate.
Natriuresis
Preload Glycosuria This figure was specifically
Proteinuria commissioned for this article and has
not been reproduced in any form in
any media format. Figure created by
M. Gail Rudakevich, BSc, MScBMC.
important regulator of glomerular filtration rate and renal risk, regard- tients who have heart failure with reduced and preserved ejection
less of ambient glucose levels. For cardiovascular benefits, natriuresis fraction. Similarly, dapagliflozin is being studied in dedicated stud-
leading to contraction of plasma volume, rather than glycosuria, is a ies to evaluate efficacy in heart failure (clinicaltrials.gov:
strong candidate that may mediate the reduction of hospitalizations NCT01730534) and renal preservation (clinicaltrials.gov:
for heart failure. Because sodium, rather than glucose, is likely to be an NCT03036150). It is important to emphasize that whereas the
important physiological factor that is common to both renal and car- hypothesis emerged in the potential prevention of heart failure in pa-
diovascularbenefitswithSGLT2inhibition,itishasbeensuggestedthat tients with diabetes, whether an osmotic diuretic will work in the
cardiorenal benefits with SGLT2 inhibitors may extend to patients who treatment of established heart failure, who will be treated with
do not have diabetes.7 loop diuretics remains to be seen. As we await the results of these
Whether SGLT2 inhibitors will be used in the treatment of heart trials, we need to develop appropriate terminology to describe
failure and renal disease remains to be seen, but large, ongoing out- this class of agents. Accordingly, based on physiological data, we
come trials in these populations will inform us whether we have hit suggest that SGLT2 inhibitors be considered as metabolodiuretic
the “sweet spot” or not. Indeed, empagliflozin is being studied in pa- agents (Figure).
ARTICLE INFORMATION boards organized by Novartis and Sanofi-Aventis. and progression of kidney disease in type 2
Published Online: June 21, 2017. Dr Cherney has received consulting and/or diabetes. N Engl J Med. 2016;375(4):323-334.
doi:10.1001/jamacardio.2017.1891 speaker's honoraria from AstraZeneca, Boehringer 3. Sattar N, McLaren J, Kristensen SL, Preiss D,
Ingelheim, Eli Lilly, Janssen, Sanofi, Merck, and McMurray JJ. SGLT2 Inhibition and cardiovascular
Conflict of Interest Disclosures: All authors have Mitsubishi-Tanabe and research support from events. Diabetologia. 2016;59(7):1333-1339.
completed and submitted the ICMJE Form for Merck, AstraZeneca, and Boehringer Ingelheim.
Disclosure of Potential Conflicts of Interest. Dr 4. Ferrannini E, Mark M, Mayoux E. CV protection
Verma has received speaker’s honoraria from Additional Contributions: We thank Hwee Teoh, in the EMPA-REG OUTCOME trial. Diabetes Care.
AstraZeneca, Boehringer Ingelheim, Eli Lilly, and PhD, St Michael’s Hospital, for assisting with 2016;39(7):1108-1114.
Janssen and research support from AstraZeneca editing. No compensation was received for such 5. Lopaschuk GD, Verma S. Empagliflozin’s fuel
and Boehringer Ingelheim. Dr McMurray reports contributions. hypothesis. Cell Metab. 2016;24(2):200-202.
that his employer, Glasgow University, paid for his 6. Verma S, Garg A, Yan AT, et al. Effect of
participation in clinical trial committees by Abbvie, REFERENCES
empagliflozin on left ventricular mass and diastolic
AstraZeneca, Amgen, Bayer, Bristol-Myers Squibb, 1. Zinman B, Wanner C, Lachin JM, et al; EMPA-REG function in individuals with diabetes Diabetes Care.
Dalcor, GlaxoSmithKline, Merck, Novartis, OUTCOME Investigators. Empagliflozin, 2016;39(12):e212-e213.
Resverlogix, Stealth, and Theracos. In addition, his cardiovascular outcomes, and mortality in type 2 7. Cherney D, Lund SS, Perkins BA, et al. The effect
travel and accommodation have been paid to diabetes. N Engl J Med. 2015;373(22):2117-2128. of sodium glucose cotransporter 2 inhibition with
attend meetings related to some of the clinical trials 2. Wanner C, Inzucchi SE, Lachin JM, et al; empagliflozin on microalbuminuria and
funded by these sponsors. Dr McMurray’s employer EMPA-REG OUTCOME Investigators. Empagliflozin macroalbuminuria in patients with type 2 diabetes.
has also been paid for his attendance at advisory Diabetologia. 2016;59(9):1860-1870.
E2 JAMA Cardiology Published online June 21, 2017 (Reprinted) jamacardiology.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: http://cardiology.jamanetwork.com/ by a Columbia University User on 07/02/2017
You might also like
- Palliative Sedation Therapy in The Last Weeks of Life: A Literature Review and Recommendations For StandardsDocument19 pagesPalliative Sedation Therapy in The Last Weeks of Life: A Literature Review and Recommendations For StandardsMárcia MatosNo ratings yet
- SGLT2 Inhibitors. Mechanisms of Cardiovascular Benefit Beyond Glycaemic ControlDocument12 pagesSGLT2 Inhibitors. Mechanisms of Cardiovascular Benefit Beyond Glycaemic ControlEdgardo Vargas AlvarezNo ratings yet
- Sodium Glucose Cotransporter 2 Inhibitors in The Treatment of Diabetes MellitusDocument21 pagesSodium Glucose Cotransporter 2 Inhibitors in The Treatment of Diabetes MellitusWENDY JOHANA HENRIQUEZ SEGURA ESTUDIANTE ACTIVONo ratings yet
- Sodium Glucose Cotransporter 2 Inhibitors in The Treatment of Diabetes MellitusDocument21 pagesSodium Glucose Cotransporter 2 Inhibitors in The Treatment of Diabetes MellitusManuel PérezNo ratings yet
- Cardiovascular Protection by Sodium Glucose Cotransp 2017 The American JournDocument10 pagesCardiovascular Protection by Sodium Glucose Cotransp 2017 The American JournAlina PopaNo ratings yet
- Prescribing SGLT2 Inhibitors in Patients With CKD Expanding Indications and Practical ConsiderationsDocument14 pagesPrescribing SGLT2 Inhibitors in Patients With CKD Expanding Indications and Practical ConsiderationsJorge Alejandro SañudoNo ratings yet
- SGLTi - OrthostaticDocument8 pagesSGLTi - OrthostaticdipanNo ratings yet
- The Actions of SGLT2 Inhibitors On Metabolism, Renal Function and Blood PressureDocument10 pagesThe Actions of SGLT2 Inhibitors On Metabolism, Renal Function and Blood PressureLucian SiriteanuNo ratings yet
- Kidney News Article p14 - 9Document3 pagesKidney News Article p14 - 9hossein kasiriNo ratings yet
- GLP1 Renal 1Document11 pagesGLP1 Renal 1miguelcontreraszambranoNo ratings yet
- The Actions of SGLT2 Inhibitors On Metabolism, Renal Function and Blood PressureDocument19 pagesThe Actions of SGLT2 Inhibitors On Metabolism, Renal Function and Blood PressureIndri AswariNo ratings yet
- Los SGLT2Document11 pagesLos SGLT2David AriasNo ratings yet
- SGLT2 Inhibitors and Their Antiarrhythmic PropertiesDocument13 pagesSGLT2 Inhibitors and Their Antiarrhythmic PropertiesKardio - Akhmad IsnaNo ratings yet
- Sodium GlucoseDocument20 pagesSodium GlucoseYati Nurul HashfiNo ratings yet
- Cardio Diabetes 3Document15 pagesCardio Diabetes 3miguel contrerasNo ratings yet
- Euglycaemic Diabetic Ketoacidosis As A Complication of SGLT-2 Inhibitors. Epidemiology, Pathophysiology, and TreatmentDocument11 pagesEuglycaemic Diabetic Ketoacidosis As A Complication of SGLT-2 Inhibitors. Epidemiology, Pathophysiology, and Treatmentmaria arenas de itaNo ratings yet
- SGLT2 iNHIBITORDocument6 pagesSGLT2 iNHIBITORHninNo ratings yet
- Isglt2 Nefirits LupicaDocument2 pagesIsglt2 Nefirits LupicaAldo Amed Montaño SalinasNo ratings yet
- Sglt2 Inhibitor - PDF 25Document7 pagesSglt2 Inhibitor - PDF 25JaganNo ratings yet
- Sglt2i HFpEFDocument9 pagesSglt2i HFpEFlakshminivas PingaliNo ratings yet
- Sodium-Glucose Co Transport InhibitorsDocument19 pagesSodium-Glucose Co Transport InhibitorsMuhammad Bilal100% (1)
- SGLT 2 Inhibitors in Heart Failure A Review of Current EvidenceDocument9 pagesSGLT 2 Inhibitors in Heart Failure A Review of Current EvidenceAbdulrahmanNo ratings yet
- Effects of Sodium Glucose CotransporterDocument18 pagesEffects of Sodium Glucose CotransporterGustavo TeixeiraNo ratings yet
- Nej MR A 2115011Document11 pagesNej MR A 2115011LETICIA CRISTINO FRANCISCONo ratings yet
- ISGLT2 Revi3w Nejm2022Document11 pagesISGLT2 Revi3w Nejm2022salvado moyanoNo ratings yet
- Document 36 (2) .Doc NewDocument34 pagesDocument 36 (2) .Doc NewPraveen PuthuparambilNo ratings yet
- SGLT2Document8 pagesSGLT2ESTEBAN ALEJANDRO PERALTA ROJASNo ratings yet
- Dapa Aki ElectrolytesDocument13 pagesDapa Aki Electrolyteslakshminivas PingaliNo ratings yet
- Nephron Protection in Diabetic Kidney DiseaseDocument3 pagesNephron Protection in Diabetic Kidney Diseasekhangsiean89No ratings yet
- Top 3 PDFDocument2 pagesTop 3 PDFPablo SánchezNo ratings yet
- DAPA-HF Full PublicationDocument13 pagesDAPA-HF Full PublicationPutra AchmadNo ratings yet
- SGLT2 Inhibitors and MechanismsDocument7 pagesSGLT2 Inhibitors and MechanismseswaynedNo ratings yet
- PIIS2590059523000122Document7 pagesPIIS2590059523000122abo_youssof20047438No ratings yet
- GliffozinasDocument11 pagesGliffozinasArahiMaflaNo ratings yet
- Cardio Diabetes 4Document15 pagesCardio Diabetes 4miguel contrerasNo ratings yet
- Top 2 PDFDocument8 pagesTop 2 PDFPablo SánchezNo ratings yet
- Inhibition of Sodium-Glucose Cotransporter 2 To Slow The Progression of Chronic Kidney DiseaseDocument11 pagesInhibition of Sodium-Glucose Cotransporter 2 To Slow The Progression of Chronic Kidney DiseaseLevi PNo ratings yet
- Glycaemic Control and Blood Glucose Lowering AgentDocument23 pagesGlycaemic Control and Blood Glucose Lowering AgentIrsa SevenfoldismNo ratings yet
- Packer 2017Document5 pagesPacker 2017Olivia Chandra DeviNo ratings yet
- Proteinuria in Diabetic Kidney Disease: A Mechanistic ViewpointDocument15 pagesProteinuria in Diabetic Kidney Disease: A Mechanistic ViewpointangelramonrNo ratings yet
- Ijms 21 07833Document25 pagesIjms 21 07833Zerrae CBTNo ratings yet
- SGLT2 Inhibitors For Non-Diabetic Kidney Disease: Drugs To Treat CKD That Also Improve GlycaemiaDocument6 pagesSGLT2 Inhibitors For Non-Diabetic Kidney Disease: Drugs To Treat CKD That Also Improve GlycaemiaAdeliaNo ratings yet
- SezaiDocument13 pagesSezaigarry.soloanNo ratings yet
- EMPA-REG OUTCOME - The Endocrinologist's Point of ViewDocument6 pagesEMPA-REG OUTCOME - The Endocrinologist's Point of ViewTony Miguel Saba SabaNo ratings yet
- Circulationaha 123 064346Document19 pagesCirculationaha 123 064346niranjan reddyNo ratings yet
- SGLT 2Document11 pagesSGLT 2Macarena SainzNo ratings yet
- Treatment of Nephrotic Syndrome, RetrospectionDocument4 pagesTreatment of Nephrotic Syndrome, RetrospectionTim Engineer HD RSUD Dr. SoetomoNo ratings yet
- Mechanisms of Blood Pressure Reduction With Sodium GlucoseDocument4 pagesMechanisms of Blood Pressure Reduction With Sodium GlucoseArturo GuerreroNo ratings yet
- Cardiovascular Benefi Ts of SGLT2Document10 pagesCardiovascular Benefi Ts of SGLT2GVRNo ratings yet
- Aldosterone Blockade in CKD - Emphasis On PharmacologyDocument10 pagesAldosterone Blockade in CKD - Emphasis On PharmacologyAndrey KulakovNo ratings yet
- Antiplatelet Therapy in Flow Diversion-2019Document6 pagesAntiplatelet Therapy in Flow Diversion-2019ariNo ratings yet
- Euglycemic Ketoacidosis As A Complication of SGLT2Document8 pagesEuglycemic Ketoacidosis As A Complication of SGLT2Mila UlfiaNo ratings yet
- PIIS1053077018310437Document5 pagesPIIS1053077018310437andi rahmatNo ratings yet
- Is Age Accumulation A Therapeutic Target For Diabetic Complications?Document3 pagesIs Age Accumulation A Therapeutic Target For Diabetic Complications?Makhyan JibrilNo ratings yet
- Statins Do More Than Just Lower Cholesterol: ViewpointDocument4 pagesStatins Do More Than Just Lower Cholesterol: ViewpointTavo Martínez CanoNo ratings yet
- Sodium-Glucose Co-Transporter 2 Inhibitors - 2024Document15 pagesSodium-Glucose Co-Transporter 2 Inhibitors - 2024Kenny RuizNo ratings yet
- Hanefeld 2008Document11 pagesHanefeld 2008Hạ TrúNo ratings yet
- Diagnosis and Treatment of Digoxin Toxicity: Review ArticleDocument3 pagesDiagnosis and Treatment of Digoxin Toxicity: Review ArticleJameela FayezNo ratings yet
- 429 FullDocument2 pages429 FullSheldon SilvaNo ratings yet
- Cardiorenal Protection in Diabetic Kidney Disease: Review ArticleDocument14 pagesCardiorenal Protection in Diabetic Kidney Disease: Review ArticleveraNo ratings yet
- 2021 Expert Decision Pathway For HFrEF Treatment Optimization - American College of CardiologyDocument4 pages2021 Expert Decision Pathway For HFrEF Treatment Optimization - American College of CardiologyVinh Quy VoNo ratings yet
- The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II) : A Randomised TrialDocument5 pagesThe Cardiac Insufficiency Bisoprolol Study II (CIBIS-II) : A Randomised TrialVinh Quy VoNo ratings yet
- Empagliflozin in Heart Failure With A Preserved Ejection FractionDocument11 pagesEmpagliflozin in Heart Failure With A Preserved Ejection FractionVinh Quy VoNo ratings yet
- Olivier Hanon MD - Laure Caillard MD - Edouard Chaussade MD - Intza Hernandorena MD - Clemence Boully MDDocument8 pagesOlivier Hanon MD - Laure Caillard MD - Edouard Chaussade MD - Intza Hernandorena MD - Clemence Boully MDVinh Quy VoNo ratings yet
- Poulter2019 Article EfficacyAndSafetyOfIncremental (1225)Document11 pagesPoulter2019 Article EfficacyAndSafetyOfIncremental (1225)Vinh Quy VoNo ratings yet
- The Future of Us Healthcare Whats Next For The Industry Post Covid 19Document13 pagesThe Future of Us Healthcare Whats Next For The Industry Post Covid 19miltechinsightsNo ratings yet
- Kumho 1712 - SDS - EngDocument12 pagesKumho 1712 - SDS - EngMahmood Anwar ShadNo ratings yet
- "Shivashri", # 17, Manoj Hieghts, Near Sukruthi Public School, Vidyanagar, Hubli, Karnataka - 580031Document15 pages"Shivashri", # 17, Manoj Hieghts, Near Sukruthi Public School, Vidyanagar, Hubli, Karnataka - 580031Dr Meenakshi ParwaniNo ratings yet
- Subjective Data: Short Term Goal: IndependentDocument1 pageSubjective Data: Short Term Goal: IndependentVanetNo ratings yet
- World Obesity Atlas 2022Document289 pagesWorld Obesity Atlas 2022brunoencubaNo ratings yet
- RainforestHerbs BrochureDocument11 pagesRainforestHerbs BrochureErlena RahimNo ratings yet
- Prac 11 TDPDocument2 pagesPrac 11 TDPAravindhNo ratings yet
- Fieldwork Risk Assessment (Low Risk Activities) Fieldwork Project DetailsDocument3 pagesFieldwork Risk Assessment (Low Risk Activities) Fieldwork Project DetailsDiyoke HenryNo ratings yet
- Open Letter To Mayor-Elect Wu - Mass and CassDocument2 pagesOpen Letter To Mayor-Elect Wu - Mass and Cassdialynn dwyerNo ratings yet
- STOK250921Document36 pagesSTOK250921Martha AdinataNo ratings yet
- Sodium Hypochlorite 6 % MSDSDocument5 pagesSodium Hypochlorite 6 % MSDScataztropherNo ratings yet
- Vs July2014 View#7Document51 pagesVs July2014 View#7binhnguyen2145849No ratings yet
- MSDS Butyl CellosolveENDocument11 pagesMSDS Butyl CellosolveENthu hoaiNo ratings yet
- Ai Mon Chai Sudu Tomai Valobasi, Ai Mon Chai Sudu Tomar Kacha Aasi, Ai Mon Chai Tumar Mukher Akto Hasi, Ai Mon Chai Sudu Thakte Tumar Pasapasi!Document6 pagesAi Mon Chai Sudu Tomai Valobasi, Ai Mon Chai Sudu Tomar Kacha Aasi, Ai Mon Chai Tumar Mukher Akto Hasi, Ai Mon Chai Sudu Thakte Tumar Pasapasi!Subhajit_Mitra_7902No ratings yet
- Interpretasi Foto AbdomenDocument96 pagesInterpretasi Foto AbdomenGaluh EkaNo ratings yet
- Construction Safety Audit Scoring System (Consass) 2020 Audit ChecklistDocument30 pagesConstruction Safety Audit Scoring System (Consass) 2020 Audit ChecklistThee BouyyNo ratings yet
- Teen MothersDocument17 pagesTeen Motherskato chrisNo ratings yet
- Pidato Bahasa InggrisDocument10 pagesPidato Bahasa InggrisYustino JbNo ratings yet
- DM - Guidelines On The Roll-Out of Catch-Up and SIA For OPV 2024Document19 pagesDM - Guidelines On The Roll-Out of Catch-Up and SIA For OPV 20246ctqt746cp100% (1)
- Art of Urethral Reconstruction PDFDocument192 pagesArt of Urethral Reconstruction PDFWilfredo Antonio Olave BenitezNo ratings yet
- Stressors, Affectivity, and Self - Efficacy As Predictors of Librarians' Thriving at WorkDocument12 pagesStressors, Affectivity, and Self - Efficacy As Predictors of Librarians' Thriving at WorkIOER International Multidisciplinary Research Journal ( IIMRJ)No ratings yet
- NCP Kenezo, Female 17Document2 pagesNCP Kenezo, Female 17labanesstephanyNo ratings yet
- 20230321-Sdb-Grameen America-WestDocument23 pages20230321-Sdb-Grameen America-WestBassel HassanNo ratings yet
- Programs National Commission On Indigenous PeoplesDocument1 pagePrograms National Commission On Indigenous PeoplesDesiree Jolly Dela CruzNo ratings yet
- Workplace Safety ProcedureDocument12 pagesWorkplace Safety ProcedureLindsay CandolitaNo ratings yet
- Canine Impaction-A Review of The Prevalence, Etiology, Diagnosis and TreatmentDocument26 pagesCanine Impaction-A Review of The Prevalence, Etiology, Diagnosis and TreatmentAnil MarnaNo ratings yet
- Practical Neurosidom Elizaga 6yymbDocument22 pagesPractical Neurosidom Elizaga 6yymbAlina AbinetNo ratings yet
- Report On DamsDocument46 pagesReport On DamsNoli CorralNo ratings yet
- 4 Community Resource DirectoryDocument6 pages4 Community Resource DirectoryWonder LustNo ratings yet