Professional Documents
Culture Documents
Cardiology Flash Cards
Cardiology Flash Cards
Uploaded by
Rodrigo Fonseca0 ratings0% found this document useful (0 votes)
309 views5 pages1. The TIMI and GRACE scores are used to assess mortality in patients with ST elevation myocardial infarction (STEMI).
2. Heart failure goals include a cardiac index >2.2, pulmonary capillary wedge pressure <18 mmHg, mean arterial pressure >60 mmHg, and systemic vascular resistance <800 dynes·sec·cm−5.
3. Paroxysmal atrial fibrillation lasts less than 7 days, persistent lasts 7 days to 1 year, and permanent lasts over 1 year.
Original Description:
Flashcards
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. The TIMI and GRACE scores are used to assess mortality in patients with ST elevation myocardial infarction (STEMI).
2. Heart failure goals include a cardiac index >2.2, pulmonary capillary wedge pressure <18 mmHg, mean arterial pressure >60 mmHg, and systemic vascular resistance <800 dynes·sec·cm−5.
3. Paroxysmal atrial fibrillation lasts less than 7 days, persistent lasts 7 days to 1 year, and permanent lasts over 1 year.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
309 views5 pagesCardiology Flash Cards
Cardiology Flash Cards
Uploaded by
Rodrigo Fonseca1. The TIMI and GRACE scores are used to assess mortality in patients with ST elevation myocardial infarction (STEMI).
2. Heart failure goals include a cardiac index >2.2, pulmonary capillary wedge pressure <18 mmHg, mean arterial pressure >60 mmHg, and systemic vascular resistance <800 dynes·sec·cm−5.
3. Paroxysmal atrial fibrillation lasts less than 7 days, persistent lasts 7 days to 1 year, and permanent lasts over 1 year.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 5
CARDIOLOGY
STEMI Mortality Scores TIMI Score and GRACE Score
Heart failure goals (CI, PCWP, MAP, CI >2.2, PCWP <18, MAP >60, SVR <800
SVR)
Difference between interval and Intervals have waves, segments don’t
segment
AFib suppression Amiodarone
AFib prophylaxis after CABG Amiodaron
VTach characteristics Regular rhythm, wide QRS
Time needed with triple anticoagulation It is only recommended for one month: 2 antiplatelets + oral anticoagulants
after PCI
Difference between paroxysmal, Paroxysmal <7 days, Persistent 7 days – 1 year, Permanent >1 year
persistent and permanent AFib
Echo “BART” Blue – Away, Red – Towards
Bubble study interpretation <4 beats: shunt, 4-7: indeterminant, >7: pulmonary shunt
Indication to lower apixaban dose to 2.5 >80 yo, Cr >1.5, Weight: <60 kg
mg BID instead of 5 mg BID
Sever Aortic Stenosis Criteria Mean Gradient: 40, Vmax: 400 cm, Area: < 1 cm
Wall abnormalities in Takatsubo There is hypokinesis at the point of the ventricle and hyperkinesia at the base.
cardiomyopathy Reverse Takatsubo: other way around
Echo characteristic of mitral valve in Posterior leaflet is fixed. Looks like a “hockey stick”
rheumatic disease
Indication to increase furosemide dose If in the morning you weigh >3 lbs more than the previous day. Take 20 additional
at home mgs.
Prophylaxis for Bicuspid Aortic Valve Not indicated
Digoxin effectivity during exercise Digoxin only works with HR at rest, will not improve function during periods of
exercise
New HTN Classification Elevated BP: 120-129/80, Stage 1 HTN: 130-139/80-89, Stage 2 HTN: >140/>90
BP Goal for PX with CV Risk >10 and 130/90 (plus TX for risk factors)
HTN
COPD most common arrhythmia Multifocal atrial tachycardia
Most common SVT AVNRT
ST changes in pericarditis ST elevations WITHOUT reciprocal ST depressions
Definition of Low Voltage in EKG <5 mV in limb leads; <10 mV in precordial leads
Hypertrophic cardiomyopathy EKG Dager Q waver (v5-v6) + high voltaje
characteristics
Q differences in infarction vs Infarction Q >40 ms; hypertrophy Q <40 ms
hypertrophy
Contrainidicated medications in WPW NO ß-blockers; would inhibit AV node that controls rate = arrhythmia
TX for WPW Procainamide
Effects on afterload or preload of Handgrip increases afterload, Valsalva decreases preload, squatting increases
handgrip, Valsalva, squatting preload and afterload
Defect in left-right dynein results in… Dextrocardia (Kartagener SX)
>QT interval increases risk for… Torsades de Pointes
Congenital >QT interval causes Romano Ward (AD) and Jowell and Lange-Nielsen (AR, deafness)
SCN5A mutacion Brugada syndrome
Bundle of Kent Accessory conduction of WPW Sx
Recombination form of BNP Nesiritide
Drugs used in pharmacological stress Dipyridamole, regadenoson
test
Culture (-) endocarditis HACEK (Haemophilus, aggregaticobacter, cardiobacterium, eikenella, kingella),
bartonella, Coxiella
Hemodynamic parameter to use in HF MAP (normal 65-75), NOT BP
PWP in pulmonary edema >20 mmHg
Normal pressure ranges in Central venos 3-8, RV 15-30/3-8, PA 15-30/4-12, PV (wedge) 2-15, LV (100-140/3-
cardiovascular system 12)
CHA2DS2 Vasc CHF, Htn, Age (65-74 1 pt, >75 2 pts), diabetes, previous stroke, vascular disease,
female. >1 consider anticoagulation, ≥ 2 mandatory
WPW predisposes to .. AVRT
Selective pulmonary vasodialtors (NOT Prostaciclins (epoprostenol, iloprost, treprostinil), nitric oxide, PDE-5 inhibitores,
for left HF) endotelin antagonists (bosentan, dorusentan)
Cause of redunces BNP Obesity
Levosimendan Calcium sensitizer for management of acutely decompensated HF
Indications for cardiac EF <35%, NHYA III-IV, maxium medical TX, QRS >120 ms (LBBB)
resynchronization therapy
ß-blockers used in HF Bisoprolol, metoprolol, carvedilol (alpha + beta); PX has to be euvolemic
PX population for eplerenone use Diabetics or post-MI
TX for pulmonar edema O2, morphine, diurectics, when systolic BP >90-100 give vasodilators
(nitroglycerine, nitroprussiate), inotropic meds, aortic balloon, ß-blockers/calcium
antagonists cardioversion
EKG criteria ventricular Hypertrophy Tall Rs in V5-V6, deep Ss in V1-V2 (Sokolow index >35 mm, Lewis index >17 mm)
Drugs contraindicated before stress ß blockers, non-DHP calcium channel blockers, amiodarone, sotalol, digoxin,
tests: nitrates
Meds contraindicated in vasospastic Aspirin, non-selective ß blockers, sumatriptan
angina
If used, Ca channel blockers in HF must ACE-inhibitors; they tend to be avoided in HF. DHF for aortic insufficiency,
be used with .. verapamil/diltiazem for hypertrophic cardiomyopathy
Verapamil increases toxicity for… Digoxin
Trunetazidine use Protect cells from free radicals after isquemia
Echo criteria for diastolic dysfunction Small E wave; EA ration ≤0.8 (normal is 0.8-2)
Advantages of milrinone vs dobutamine Milrinone can be used in the presence of ß blockers but dobutamine is easier to
titrate
EKG if tachycardia does not come from Wide QRS
SA node
Meds that decrease mortality post-MI ß blockers
Pericarditis EKG Global ST segmental elevation (sensitive), PR depression (specific), pericardial
effusion (low voltage + electrical alternans)
TX of symptomatic antidromic AVRT Procainamide IV (definitive: radiocatheter ablation)
TX of symptomatic orthodromic AVRT Vagal maneuvers – AV nodal blocking agents (adenosine > verapamil). If
hemodynamically unstable = cardioversion.
Medication CI in WPW due to increased Digoxin
risk of V fib
Dopamine doses and effects Low: 0.5-2 µg/kg/min (renal + splenic vasodilation), Medium: 2-6 µg/kg/min
(inotropic + cronotropic), High >10 µg/kg/min (vasoconstriction)
Changes in PR interval with increased Shorter PR interval (atrial T wave can be seen after QRS altering J point = do not
HR confuse with ST depression)
Formulas to correct QT interval Bazetts and Hodges formulas.
QRS Axis Normal: positive I and II / leftward: positive in I, negative II / rightward: negative I,
positive aVF / extreme: negative I and aVF
Right deviation EKG causes RV hypertrophy, RBBB left posterior fascicular block, WPW, lateral wall SX
Left deviation EKG causes LV hypertrophy, LBBB, left anterior fascicular block, hyperpotasemia, inferior wal
MI
Possible normal negative P waves Always in aVR, sometimes III, V1
Normal QT interval <0.45 in men, <0.46 women
Causes of T wave inversion Isquemia, Brugada SX, arrythmogenic, right ventricular cardiomyopathy
EKG aneurysm Persisten ST elevation post MI (>3 weeks); can also be result of dyskinetic wall
Causes of short QT Hypercalemia, hypercalcemia, digitalis use
Tall T waves causes Hyperkalemia (>10 mm in precordial, >5 mm in limbs), early MI, LBB, LVH
Prominent U waves Hypocalemia, bradycardia, intracranial hemorrhage, class 1A and 3 antiarrythmics
EKF left anterior fasciscular block Left axis deviation, QRS negative II, III and aVF (r, deep S), aVL: small q, tall R
AFib prophylaxis after CABG Amiodarone; it can also be used to suppress the arrhythmia
TX to reduce degree of chronic cardiac Colchicine
tamponade
Triple anticoagulation therapy indication Only recommended for 1 month post-stent placement; then you drop aspirin and
continue for a year
Reverse agent dabigatran Idarucizumab
EKG Mi Criteria ST elevation at J point in two contiguous leads of ≥0.1 mV in leads, EXCEPT: 1)
V2-V3 ≥0.2 mV in men ≥40 years or ≥0.25 mV in <40 years or ≥0.15 in women / 2)
posterior STEMI V1-V3 depression (posterior EKG would show elevation in V7-V9)
KDIGO Acute Kidney Injury Criteria Increase of Cr ≥0.3 mg/dl within 48 hrs, increase CR to ≥1.5 x baseline within 7
days, urine volume <0.5 ml/kg/hr for 6 hours
Shones SX Supravalvular mitral membrane (parachute mitral valve, inserted to only 1 papillary
muscle) + subaortic stenosis + coarctation of the aorta
Williams SX Intellectual disability / learning problmes (visual-spacial) + facial abnormalities +
cardiovascular abdormalities (supravalvular aortic stenosis)
Spironolactone in HF recommendation NYHA clasee II – IV + EF <35% OR PX post-STEMI with therapeutic doses of ACE
inhibitors and ARBA + LVEF <40% + symptomatic HF or DM
Labs contraindications for K >5.0 mEq or GFR <30
spironolactone
TIMI Scores % of mortality risk at 14 days post-MI
GRACE Score Estimates admission and 6 month mortality for PX w/ acute coronary syndrome
Killip Class Stratify mortality post-MI first 30 days. I – no signs (6%), II – rales on crackels, S3,
increased JV pressure (17%), III – acute pulmonary edema (38%), IV – cardiogenic
shock or hypotension + peripheral vasoconstriction (81%)
Scarbossa criteria SX MI in PX with LBBB; concordant ST elevation >1 mm in leads with positive QRS
complex (5 pts) / concordant ST depression >1 mm in V1-V3 (3 pts), excessively
discordant ST elevation >5 mm (25%) in leads aVR QRS complex
You might also like
- Acute PancreatitisDocument31 pagesAcute PancreatitisAmoroso, Marian Corneth D.No ratings yet
- Pathophysiology LeptospirosisDocument1 pagePathophysiology Leptospirosisjeoffrey_castro100% (3)
- Lang 10 EditionDocument235 pagesLang 10 Editionraju niraulaNo ratings yet
- Pharmacology Main DrugsDocument14 pagesPharmacology Main DrugsSabir KhanNo ratings yet
- Cardiac 1.03 Hemodynamic ValuesDocument1 pageCardiac 1.03 Hemodynamic ValuesEdelwiess Marie CayetanoNo ratings yet
- Step 2 CK NotesDocument95 pagesStep 2 CK NotesKevin Yang100% (3)
- Electrolytes ImbalancesDocument4 pagesElectrolytes ImbalancesPeter John Ruiz100% (1)
- Mechanism of Action For Each Class of AntiDocument146 pagesMechanism of Action For Each Class of AntiReynaldo RiveraNo ratings yet
- A New Way of Mnemonics - Hypertension-cough-asthma-NSAID - WMDocument26 pagesA New Way of Mnemonics - Hypertension-cough-asthma-NSAID - WMKartik Mendiratta100% (1)
- Northern Ireland Management of Infection Guidelines For Primary and Community Care 2016Document48 pagesNorthern Ireland Management of Infection Guidelines For Primary and Community Care 2016dreneavalentinstefanNo ratings yet
- Labs 1.19 ABG AnalysisDocument1 pageLabs 1.19 ABG AnalysisMonica GonzalezNo ratings yet
- Finished Ekg Study GuideDocument4 pagesFinished Ekg Study Guideapi-652914452No ratings yet
- Abx FinalDocument3 pagesAbx Finalyanks1120No ratings yet
- Antihypotensive Drugs: Roger Joseph Ii Ramos Jecino, RN, M.DDocument28 pagesAntihypotensive Drugs: Roger Joseph Ii Ramos Jecino, RN, M.DFranz Earl Niño AlbesaNo ratings yet
- Pre Assessment Diabetes Nursing CareDocument4 pagesPre Assessment Diabetes Nursing CareHabib UllahNo ratings yet
- 1 - Internal Medicine UKIDocument128 pages1 - Internal Medicine UKILewishoppusNo ratings yet
- ChemotherapyDocument11 pagesChemotherapyNedaAbdullahNo ratings yet
- Clinical Use of Monoclonal Antibodies: Abciximab Infliximab TrastuzumabDocument15 pagesClinical Use of Monoclonal Antibodies: Abciximab Infliximab TrastuzumabAndleeb ImranNo ratings yet
- Basic Ecg: - Department of Medicine BIMC Hospital 2013Document60 pagesBasic Ecg: - Department of Medicine BIMC Hospital 2013LexadkNo ratings yet
- Transport of Critically Ill Adults 2011Document1 pageTransport of Critically Ill Adults 2011velocity25No ratings yet
- Complication of MI (Myocardial Infarction)Document2 pagesComplication of MI (Myocardial Infarction)Zahid QamarNo ratings yet
- Adult Tachycardia With A Pulse Algorithm: Doses/DetailsDocument1 pageAdult Tachycardia With A Pulse Algorithm: Doses/DetailsAlexis HospitalNo ratings yet
- Assessment of The Chest and LungsDocument46 pagesAssessment of The Chest and LungsSumathi GopinathNo ratings yet
- Drug Toxicity and PoisoningDocument12 pagesDrug Toxicity and PoisoningPAULA MARIE MERCADO LLIDONo ratings yet
- MCQ 1. Heart Sound Heart Sound S1 S2Document7 pagesMCQ 1. Heart Sound Heart Sound S1 S2Atirah AaNo ratings yet
- (Pha) Le 5Document19 pages(Pha) Le 5Gabby TanNo ratings yet
- Cardiovascular DisordersDocument9 pagesCardiovascular DisordersChristine Evan HoNo ratings yet
- Disorders of The BoneDocument2 pagesDisorders of The BoneRPh Krishna Chandra JagritNo ratings yet
- Heart Failure Express Card HMCDocument2 pagesHeart Failure Express Card HMCalexNo ratings yet
- CTSP Case 2 - Hypoglycemia and HyperglycemiaDocument2 pagesCTSP Case 2 - Hypoglycemia and HyperglycemiaVanessa HermioneNo ratings yet
- Normal Laboratory Values With Nursing Consideration - UsnganDocument8 pagesNormal Laboratory Values With Nursing Consideration - UsnganPrincess Nasima M. UsnganNo ratings yet
- Classification of The DrugsDocument50 pagesClassification of The DrugsGlena SalamNo ratings yet
- This Study Resource Was: System DisorderDocument1 pageThis Study Resource Was: System DisorderDeo FactuarNo ratings yet
- Asthma + COPDDocument60 pagesAsthma + COPDNur HasanahNo ratings yet
- Clinical Skills Handbook 2015 MEDN40060 2Document66 pagesClinical Skills Handbook 2015 MEDN40060 2Wilson KhawNo ratings yet
- Antiarrhythmic Drugs - AMBOSS TWODocument6 pagesAntiarrhythmic Drugs - AMBOSS TWOOpio IsaacNo ratings yet
- Drug Succinylcholine Atracurium Cis-Atracurium Rocuronium Vecuronium Pancuronium ED95 Intubating Dose Onset Duration MetabolismDocument1 pageDrug Succinylcholine Atracurium Cis-Atracurium Rocuronium Vecuronium Pancuronium ED95 Intubating Dose Onset Duration MetabolismMarshallMcGoughNo ratings yet
- Vasoactive Agents For Adult Septic Shock: An Update and ReviewDocument10 pagesVasoactive Agents For Adult Septic Shock: An Update and ReviewntnquynhproNo ratings yet
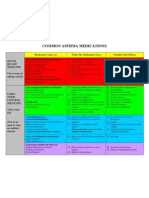
- Common Asthma MedicationsDocument1 pageCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyNo ratings yet
- A-Autonomic Drugs: 1) CholinergicDocument28 pagesA-Autonomic Drugs: 1) CholinergicMahmoud Ahmed MahmoudNo ratings yet
- First Part Exam - October 2020Document16 pagesFirst Part Exam - October 2020hassan mohamedNo ratings yet
- Anti-Arrhythmic Agents For Pharmacy PDFDocument41 pagesAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaNo ratings yet
- Ch-13 Drugs Used in Heart FailureDocument49 pagesCh-13 Drugs Used in Heart FailureShabrin SadikhNo ratings yet
- H&P GuideDocument7 pagesH&P GuideTBWPNo ratings yet
- 50 Most Commonly Prescribed Medications 02Document4 pages50 Most Commonly Prescribed Medications 02Jelly BeanNo ratings yet
- Abg InterpretationDocument1 pageAbg InterpretationPrincess EspadaNo ratings yet
- Sedative-Hypnotic Drugs - AMBOSSDocument8 pagesSedative-Hypnotic Drugs - AMBOSSRuva Oscass JimmyNo ratings yet
- Approach To Comatose Child: DR G.VenkateshDocument83 pagesApproach To Comatose Child: DR G.VenkateshG VenkateshNo ratings yet
- Diabetes and Complications: When Documenting Diabetes, It's Important To Note The FollowingDocument2 pagesDiabetes and Complications: When Documenting Diabetes, It's Important To Note The Followingmeikaizen100% (1)
- PREM AlgorithmsDocument20 pagesPREM AlgorithmsalexNo ratings yet
- Common Bacteria by Site of Infection: Mouth Skin/Soft Tissue Bone and JointDocument72 pagesCommon Bacteria by Site of Infection: Mouth Skin/Soft Tissue Bone and JointMuthia FadhilaNo ratings yet
- RespiratoryDocument4 pagesRespiratoryHaliana IzatiNo ratings yet
- Medicine Epidemiology (MedicalBooksVN - Com)Document34 pagesMedicine Epidemiology (MedicalBooksVN - Com)Jonathan AiresNo ratings yet
- Cardiovascular Pharmacology PDFDocument85 pagesCardiovascular Pharmacology PDFAhmed Shihab AhmedNo ratings yet
- Review Handouts For Medical Pharmacology: Terriann Crisp, PH.DDocument28 pagesReview Handouts For Medical Pharmacology: Terriann Crisp, PH.Dmus zaharaNo ratings yet
- Guideline Pneumothorax PDFDocument1 pageGuideline Pneumothorax PDFRhapsody KarnovinandaNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- Tachy/賸)Document28 pagesTachy/賸)Jason LinNo ratings yet
- Basic EKG RefresherDocument57 pagesBasic EKG RefresherJane Andrea Christiano DjianzonieNo ratings yet
- Heldt (2013) - Chapter 2 Mathematical Modeling of Physiological SystemsDocument21 pagesHeldt (2013) - Chapter 2 Mathematical Modeling of Physiological SystemsVint PineNo ratings yet
- Acute Biologic CrisisDocument385 pagesAcute Biologic CrisisSheryl Ann Barit PedinesNo ratings yet
- Heart and Its External Features For Paramedical StudentsDocument26 pagesHeart and Its External Features For Paramedical Studentslakshmiraman1770No ratings yet
- CoronarografieDocument72 pagesCoronarografieLaurentiu AndreiNo ratings yet
- UNITISS: Competence Development in Catheter Design For Reduced Clinical ComplicationsDocument14 pagesUNITISS: Competence Development in Catheter Design For Reduced Clinical ComplicationsHafsaNo ratings yet
- CVS Qus. Banq 2023Document7 pagesCVS Qus. Banq 2023aniskoharNo ratings yet
- Coronary Artery DiseaseDocument26 pagesCoronary Artery Diseasesmart reyNo ratings yet
- Fetal CirculationDocument5 pagesFetal CirculationZam PamateNo ratings yet
- Farmakologi Antiagina TTMDocument83 pagesFarmakologi Antiagina TTMEpha Lumban GaolNo ratings yet
- Neuropharmacology: Raj N. KalariaDocument14 pagesNeuropharmacology: Raj N. KalariadeswitrigintaNo ratings yet
- Evolution of Aortic Arches in VertebratesDocument2 pagesEvolution of Aortic Arches in Vertebratesarbazkhan825lNo ratings yet
- Cardiac Risk Stratification - CardiologyDocument10 pagesCardiac Risk Stratification - CardiologyDaniel A. Velarde LópezNo ratings yet
- SirkulasiDocument17 pagesSirkulasiJessica VanyaNo ratings yet
- C1 Lab 4 - 55654Document23 pagesC1 Lab 4 - 55654anaNo ratings yet
- Types of ArrhythmiaDocument10 pagesTypes of ArrhythmiaRonilyn Mae AlvarezNo ratings yet
- Lesson Plan in BiologyDocument3 pagesLesson Plan in BiologyTherese Angeli MagallanesNo ratings yet
- The Circulatory System PDFDocument4 pagesThe Circulatory System PDFPerry SinNo ratings yet
- Section 5 of The European Resuscitation Council GuidelinesDocument28 pagesSection 5 of The European Resuscitation Council GuidelinesАнђела КостићNo ratings yet
- Heart FailureDocument8 pagesHeart FailureApple Mae AlmoniaNo ratings yet
- AtherosclerosisDocument7 pagesAtherosclerosisFaris Mufid Madyaputra100% (1)
- Pulmonary EmbolismDocument34 pagesPulmonary EmbolismSanjeev Harry BudhooramNo ratings yet
- Activity 7 The Cardiovascular SystemDocument4 pagesActivity 7 The Cardiovascular SystemEllen Mynelle MabulacNo ratings yet
- Curriculum Vitae2011Document2 pagesCurriculum Vitae2011Rafik MargaryanNo ratings yet
- Sinus TachycardiaDocument26 pagesSinus TachycardiaCalvin Martin LeeNo ratings yet
- Anatomy & PhysiologyDocument11 pagesAnatomy & PhysiologyArah Lyn ApiagNo ratings yet
- Renin-Angiotensin-Aldosterone System (RAAS) : Hyponatremia or Increased Sympathetic ToneDocument2 pagesRenin-Angiotensin-Aldosterone System (RAAS) : Hyponatremia or Increased Sympathetic ToneDrbee10No ratings yet
- Siemens Imaging AllDocument24 pagesSiemens Imaging AllVishnu0049No ratings yet