Professional Documents
Culture Documents
A Method of Teaching Clinical Problem Solving Skills To Primary Health Care Student Nurses
A Method of Teaching Clinical Problem Solving Skills To Primary Health Care Student Nurses
Uploaded by
Jugal HarkutCopyright:
Available Formats
You might also like
- Five Models of Staff DevelopmentDocument34 pagesFive Models of Staff DevelopmentZulaiha Abdul Rahman100% (3)
- Layers of The Earth Lesson PlanDocument6 pagesLayers of The Earth Lesson PlanRutchel Martinez33% (3)
- Annual Instructional Supervisory PlanDocument8 pagesAnnual Instructional Supervisory PlanVictoria Beltran SubaranNo ratings yet
- A Self Reflection On The Evolution & Historical Impact of The DNPDocument8 pagesA Self Reflection On The Evolution & Historical Impact of The DNPapi-577750864No ratings yet
- Analysis of The Concept Continuing Education in Nursing EducatioDocument11 pagesAnalysis of The Concept Continuing Education in Nursing EducatioTapodhan VishuNo ratings yet
- Evidence Based PracticeDocument18 pagesEvidence Based Practicemeghana100% (11)
- Differentiates Between Equations and InequalitiesDocument7 pagesDifferentiates Between Equations and InequalitiesMarc Galos100% (2)
- Clinical Field Experience B Peer Instructional Planning ReviewDocument3 pagesClinical Field Experience B Peer Instructional Planning Reviewapi-5189947450% (1)
- Korean Nursing Students' Experiences of Their First Clinical PracticeDocument11 pagesKorean Nursing Students' Experiences of Their First Clinical PracticeKruh Kwabena IsaacNo ratings yet
- Research BriefsDocument8 pagesResearch BriefsNur MiladiyahNo ratings yet
- International Journal of Nursing SciencesDocument5 pagesInternational Journal of Nursing SciencesWahyu Phaling FienterNo ratings yet
- Scholarly Paper CapstoneDocument6 pagesScholarly Paper Capstoneapi-662404021No ratings yet
- 1 PBDocument7 pages1 PBAngie MandeoyaNo ratings yet
- Role of ResearchDocument8 pagesRole of ResearchDipti Punjal100% (1)
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument4 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyWednesdayNo ratings yet
- Scholarly Article PaperDocument7 pagesScholarly Article Paperapi-545697687No ratings yet
- Nursing Attitudes and BeliefsDocument5 pagesNursing Attitudes and Beliefsyovanimanuel imanuelNo ratings yet
- Cabarrubias Jovelyn - Enrichment Activity For Module 1Document3 pagesCabarrubias Jovelyn - Enrichment Activity For Module 1cabarrubiasjovy40No ratings yet
- Clinical Nursing JudgmentDocument5 pagesClinical Nursing Judgmentapi-662884360No ratings yet
- Clinicalteachingmethods 180306040756Document31 pagesClinicalteachingmethods 180306040756abcqwe123No ratings yet
- Clinical Teaching MethodsDocument5 pagesClinical Teaching MethodsFlora AlfaxdNo ratings yet
- Nursing Research Challenges and OpportunitiesDocument27 pagesNursing Research Challenges and Opportunitiessara mohamedNo ratings yet
- 1.clinical Teaching Methods MokshithaDocument23 pages1.clinical Teaching Methods MokshithaVeena DalmeidaNo ratings yet
- Analysis of Midwifery Teachers' Approach To Identifying Student Midwives With Poor Clinical Reasoning SkillsDocument7 pagesAnalysis of Midwifery Teachers' Approach To Identifying Student Midwives With Poor Clinical Reasoning SkillsIntan Mustika SariNo ratings yet
- Womens PetDocument3 pagesWomens Petapi-307931906No ratings yet
- Goals and Objectives of Fellow and ResidentsDocument38 pagesGoals and Objectives of Fellow and ResidentsjustinemaeferrerpinedaNo ratings yet
- Stave Ski 2015Document8 pagesStave Ski 2015Dian Rachmah FaoziahNo ratings yet
- Nursing RoundDocument7 pagesNursing RoundBishwajitMazumder100% (5)
- FINAL Brochure Oudce EvidenceDocument16 pagesFINAL Brochure Oudce Evidencexbsd100% (2)
- Clinical Objectives PDFDocument4 pagesClinical Objectives PDFYhuhan James TejadaNo ratings yet
- Clinical Nursing JudgementDocument5 pagesClinical Nursing Judgementapi-449796082No ratings yet
- Seminar For Educators: Teaching at The BedsideDocument4 pagesSeminar For Educators: Teaching at The Bedsidestarskyhutch0000No ratings yet
- Scholarly PaperDocument5 pagesScholarly Paperapi-661467979No ratings yet
- Shadow ANurseDocument8 pagesShadow ANurseSculpting FutureNo ratings yet
- Peplau's Interpersonal Relations Theory Power PointDocument10 pagesPeplau's Interpersonal Relations Theory Power PointPerlie Loren Arreo Cabatingan100% (1)
- Residency Manual 2018Document85 pagesResidency Manual 2018shazia kaziNo ratings yet
- Nms 3540 Study GuideDocument16 pagesNms 3540 Study GuideSepo CaciousNo ratings yet
- Clinical Skills IIIDocument16 pagesClinical Skills III4t72vb9kkdNo ratings yet
- Peplau's Interpersonal Relations Theory Power PointDocument10 pagesPeplau's Interpersonal Relations Theory Power PointCharisse Nicole DiazNo ratings yet
- Diploma in Family MedicineDocument29 pagesDiploma in Family Medicineamira_hassan100% (1)
- PROGRAMA EDUCACIÓ CONTINUApirong1982Document3 pagesPROGRAMA EDUCACIÓ CONTINUApirong1982GladysNo ratings yet
- WEEK 10 CU 10 - Evidenced Base Practice in Health Education NewDocument5 pagesWEEK 10 CU 10 - Evidenced Base Practice in Health Education Newarmanuel1390antNo ratings yet
- ME - Ethical Decision Making On Truth Telling in Terminal Cancer - Medical Students' Choices Between Patient Autonomy and Family PaternalismDocument9 pagesME - Ethical Decision Making On Truth Telling in Terminal Cancer - Medical Students' Choices Between Patient Autonomy and Family PaternalismAya SalahNo ratings yet
- Faculty Development One MinuteDocument9 pagesFaculty Development One MinuteDaniel Alejandro Lozano MorenoNo ratings yet
- Effect of High Fidelity Simulation On Clinical Decision Making Among Nursing StudentsDocument10 pagesEffect of High Fidelity Simulation On Clinical Decision Making Among Nursing Studentsاحمد العايديNo ratings yet
- Nurs490 Safety Performance Improvement Paper Neuburg IntroDocument2 pagesNurs490 Safety Performance Improvement Paper Neuburg Introapi-452041818No ratings yet
- FINAL OB - PATHO - Case PresentationDocument75 pagesFINAL OB - PATHO - Case PresentationBEATRICE CAXANDRA NAMBATAC BACASNo ratings yet
- Calculous CholecystitisDocument137 pagesCalculous Cholecystitisrremonde100% (5)
- Evidence-Based Practice and Applied Nursing ResearchDocument6 pagesEvidence-Based Practice and Applied Nursing ResearchErickNo ratings yet
- Research in Continuing Education Programme: C. Meribha Christy, V. HemavathyDocument4 pagesResearch in Continuing Education Programme: C. Meribha Christy, V. HemavathyRubina MasihNo ratings yet
- Self Assessment - Midterm 2016Document11 pagesSelf Assessment - Midterm 2016api-341527743No ratings yet
- Evidence Based Nursing in Clinical PractDocument5 pagesEvidence Based Nursing in Clinical PractVivi DisNo ratings yet
- Tujuan Teori KeperawatanDocument15 pagesTujuan Teori KeperawatankintaniaNo ratings yet
- Course Plan: Obstetric & Gynaecological NursingDocument11 pagesCourse Plan: Obstetric & Gynaecological NursingPriya100% (3)
- Journal of Midwifery & Women-S HealthDocument11 pagesJournal of Midwifery & Women-S HealthJuniatiNo ratings yet
- Assignment of AnpDocument18 pagesAssignment of Anpcharanjit kaurNo ratings yet
- Clinical Teaching: S.M. Nazmul Al-Deen Subject: Principles and Methods of TeachingDocument9 pagesClinical Teaching: S.M. Nazmul Al-Deen Subject: Principles and Methods of TeachingNazmul Al-deenNo ratings yet
- Research PresentationDocument14 pagesResearch PresentationCeeNo ratings yet
- Nurse Educator Practicum - Reflective Journal 2Document4 pagesNurse Educator Practicum - Reflective Journal 2api-643881078No ratings yet
- Clinical Nursing JudgementDocument6 pagesClinical Nursing Judgementapi-507960658No ratings yet
- Bi, 2019Document6 pagesBi, 2019aminNo ratings yet
- Iebp PDFDocument5 pagesIebp PDFchuramarak23No ratings yet
- Bucknall 2016Document13 pagesBucknall 2016mnazri98No ratings yet
- CH 01 PDFDocument25 pagesCH 01 PDFkikiNo ratings yet
- Advanced Practice and Leadership in Radiology NursingFrom EverandAdvanced Practice and Leadership in Radiology NursingKathleen A. GrossNo ratings yet
- New SN of Polling Station Locality Building in Which It Will Be Polling Areas Wheather For All Voters or Men Only or Women OnlyDocument51 pagesNew SN of Polling Station Locality Building in Which It Will Be Polling Areas Wheather For All Voters or Men Only or Women OnlyJugal HarkutNo ratings yet
- List of Judicial OfficersDocument1 pageList of Judicial OfficersJugal HarkutNo ratings yet
- Clinical Signs and Symptoms at Diagnosis and Its Differential DiagnosisDocument9 pagesClinical Signs and Symptoms at Diagnosis and Its Differential DiagnosisJugal HarkutNo ratings yet
- Evidence Base of Clinical DiagnosisDocument4 pagesEvidence Base of Clinical DiagnosisJugal HarkutNo ratings yet
- Anti CD20 Monoclonal Antibodies Reviewing A RevolutionDocument23 pagesAnti CD20 Monoclonal Antibodies Reviewing A RevolutionJugal HarkutNo ratings yet
- The Design of Discrete Vocabulary TestsDocument19 pagesThe Design of Discrete Vocabulary TestsPiroska SzolnokiNo ratings yet
- Week 12 AssignmentDocument6 pagesWeek 12 AssignmentLinhNo ratings yet
- Uts Final ReviewerDocument14 pagesUts Final ReviewerCarla QuiñonesNo ratings yet
- KPS Bluebook 26 MarchDocument80 pagesKPS Bluebook 26 Marchvijeth3110No ratings yet
- Organisational Climate, Ethos and Learning in Organisation: Presented by Swetha K Kethireddy Sri CharanDocument28 pagesOrganisational Climate, Ethos and Learning in Organisation: Presented by Swetha K Kethireddy Sri CharanSri Charan ReddyNo ratings yet
- Cambridge ICT Starters Annual Plan 2nd-8th Grade ALL SCHOOLS 2022Document4 pagesCambridge ICT Starters Annual Plan 2nd-8th Grade ALL SCHOOLS 2022Allen Panamá GutzNo ratings yet
- Tutorial Week 1: Norfadzilah Sulaiman Anis Wardah Yusri Nur Amanina AzhariDocument8 pagesTutorial Week 1: Norfadzilah Sulaiman Anis Wardah Yusri Nur Amanina AzhariTeo Khim SiangNo ratings yet
- IM Evaluation Rubric Form - Ela 7213 PDFDocument3 pagesIM Evaluation Rubric Form - Ela 7213 PDFEmir UzairNo ratings yet
- NegOr Q3 English4 Module4 v2 PDFDocument19 pagesNegOr Q3 English4 Module4 v2 PDFBambi BandalNo ratings yet
- PSY 540 Milestone Three (3) .Docx65507df63786335675Document13 pagesPSY 540 Milestone Three (3) .Docx65507df63786335675master lamarNo ratings yet
- Long Quiz in Practical Research I Test 1. Multiple Choice Direction: Choose The Letter of The Correct Answer. Encircle The Letter of Your AnswerDocument2 pagesLong Quiz in Practical Research I Test 1. Multiple Choice Direction: Choose The Letter of The Correct Answer. Encircle The Letter of Your AnswerRobert Jay MejoradaNo ratings yet
- Personal InformationDocument8 pagesPersonal InformationashishNo ratings yet
- Types and Characteristics of Teaching MediaDocument10 pagesTypes and Characteristics of Teaching MediaLami Lee0% (1)
- LEARNING ENGLISH Kindergarten 1 - New Book Information (NBI)Document1 pageLEARNING ENGLISH Kindergarten 1 - New Book Information (NBI)Sam OeunNo ratings yet
- A Clil Guide 5 Activities For Every Clil Teacher PDFDocument10 pagesA Clil Guide 5 Activities For Every Clil Teacher PDFClaudine74No ratings yet
- Barrow Lions Club Scholarship Application FormDocument4 pagesBarrow Lions Club Scholarship Application FormBarrow Lions ClubNo ratings yet
- TKT Module 3Document11 pagesTKT Module 3Татьяна АндрющенкоNo ratings yet
- 19 - iPLANDocument3 pages19 - iPLANMarlyn CaballeroNo ratings yet
- Teaching English Through KangGuru English MagazineDocument8 pagesTeaching English Through KangGuru English Magazineyusuf hidayatNo ratings yet
- Visible Learning For Teachers MaximisingDocument5 pagesVisible Learning For Teachers MaximisingNatalia FaleroNo ratings yet
- Reading and Writing Write It Out: by The End of This Lesson Ss Will Be Able ToDocument2 pagesReading and Writing Write It Out: by The End of This Lesson Ss Will Be Able ToLarbi Nadia100% (1)
- Constructivism Approach in Teaching Higher Order Thinking SkillsDocument6 pagesConstructivism Approach in Teaching Higher Order Thinking SkillsIvan ChooNo ratings yet
- ct9 Ilm1Document13 pagesct9 Ilm1heart MUNOZNo ratings yet
- DLP MTB Co 1Document10 pagesDLP MTB Co 1kerl karen ferrerNo ratings yet
- Animal Legs LessonDocument7 pagesAnimal Legs Lessonapi-374359720100% (1)
A Method of Teaching Clinical Problem Solving Skills To Primary Health Care Student Nurses
A Method of Teaching Clinical Problem Solving Skills To Primary Health Care Student Nurses
Uploaded by
Jugal HarkutOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Method of Teaching Clinical Problem Solving Skills To Primary Health Care Student Nurses
A Method of Teaching Clinical Problem Solving Skills To Primary Health Care Student Nurses
Uploaded by
Jugal HarkutCopyright:
Available Formats
South African Family Practice
ISSN: 2078-6190 (Print) 2078-6204 (Online) Journal homepage: https://www.tandfonline.com/loi/ojfp20
A method of teaching clinical problem-solving
skills to primary health care student nurses
A Truscott
To cite this article: A Truscott (2010) A method of teaching clinical problem-solving skills
to primary health care student nurses, South African Family Practice, 52:1, 60-63, DOI:
10.1080/20786204.2010.10873937
To link to this article: https://doi.org/10.1080/20786204.2010.10873937
© 2010 SAAFP. Published by Medpharm.
Published online: 15 Aug 2014.
Submit your article to this journal
Article views: 1969
View related articles
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=ojfp20
Original Research: A method of teaching clinical problem-solving skills to primary health care student nurses
A method of teaching clinical problem-solving skills
to primary health care student nurses
Truscott A, MBBCh(Wits), MFGP(SA), HDipAdEd(Wits)
Division of Rural Health, Department of Family Medicine, University of the Witwatersrand, Johannesburg, South Africa
Correspondence to: Prof Ian Couper, e-mail: Ian.Couper@wits.ac.za
Keywords: clinical problem solving process; nurse clinicians; PHC nurse training; mind maps; self teaching
Abstract SA Fam Pract 2010;52(1):60-63
The article provides a description of a method of teaching a clinical problem-solving process to primary health care nurses/clinical nurse practitioners
(PHC nurses). The process was developed in the Soweto PHC Nurse Training Unit over the past 30 years as a result of the changing availability and
role of nurse and doctor teaching staff. Students doing the diploma for nurse clinicians (Diploma in Clinical Nursing Science, Health Assessment,
Treatment and Care) are guided in the use of mind maps, assisted by constant clinical practice and group discussions to develop their clinical
problem-solving process. This method has assisted in clinical training
Peer reviewed. (Submitted: 2009-03-14, Accepted: 2009-09-21). © SAAFP
Introduction • Generates appropriate working diagnoses
• Seeks relevant and discriminating physical signs to help confirm or
On 16 June 1976, Soweto erupted in protest against the apartheid
refute working diagnoses
government. Later that day, all government doctors were withdrawn
from the clinics. They only returned to the clinics several years later. • Correctly interprets and applies information obtained from all sources
The medical superintendent of the then Baragwanath Hospital, Dr PJ about a patient
Beukes, had for several years been motivating his head office to start • Applies knowledge of basic, behavioural and clinical sciences to the
training nurses to assist with the diagnosis and management of patients identification, management and solution of patients’ problems
in the Soweto clinics. He took the opportunity provided by the withdrawal • Recognises limits of competence and responds appropriately
of doctors to approach Professor Wagstaff from the Baragwanath
It has been an ongoing concern in the Soweto training unit as to how
Paediatric Department to start training nurses in clinical skills so that
much theory students need before they can start clinical practice.
they could manage patients at the clinics. Prof Wagstaff initially started
Initially, traditional lecturing methods were used to introduce theory, with
training nurses in paediatrics. She found that it took on average three
emphasis placed on patient-based clinical teaching. During a course to
months for the students to become clinically competent. Clinic doctors
develop clinical skills for midwives, it was found that these students, who
with good experience in managing adult clinic patients were seconded
had no previous experience of doing patient consultations, demonstrated
to start training other professional nurses in adult clinical care. This was
an unexpected level of competence when allowed to perform clinical
found to take longer – on average six months.
consultations on patients. It was realised that, as a result of their nursing
After four years the South African Nursing Council (SANC) agreed to education and experience of working with patients, nurses developed
accept the course as a one-year postgraduate diploma. The diploma quite an advanced process of clinical problem solving. This observation
was named the Diploma in Clinical Nursing Science, Health Assessment, made us realise that the main aim of training should be to promote this
Treatment and Care. The paediatric and adult training in Soweto was innate clinical problem-solving process.
combined into this one-year diploma. The training has proved to be
Practising PHC nurses who had demonstrated good clinical problem-
effective.1−4
solving skills and attitudes over several years in the working situation
were asked to become nurse tutors. They became aware of the
Development of a process of clinical problem solving
importance of promoting the clinical problem-solving process. It seemed
A clinical problem-solving process is defined by Fraser5 as one in which to be related to the degree to which students developed confidence in
a practitioner: their ability to use their own intrinsic problem-solving processes. Tutors
• Elicits relevant and specific information from patients to help began to develop ways to promote this process. From the beginning
distinguish between working diagnoses of the course, the tutors encouraged the students to present patients
SA Fam Pract 2010 60 Vol 52 No 1
Original Research: A method of teaching clinical problem-solving skills to primary health care student nurses
seen the previous day to the whole student group. They encouraged the This clinical problem-solving method has been tried out with nurses
students to challenge each other’s findings and to provide reasons for doing the diploma on a part-time basis, with teaching based at clinics.
their history, assessments, examination or final diagnosis. It was found The students alternate one week in the working situation and one week
that, in the safety of an environment of their own colleagues and nurse in the classroom for 18 months. This allows them to apply any new
tutors, and with positive dynamics in the student groups, the students knowledge immediately in a working situation. When they return for the
grew in the confidence that they had the ability to solve these clinical teaching week, their clinical experiences of the previous week are used
problems themselves. for reflection and discussion. During the teaching week in the training
The tutors were aware of the delicateness of the initial process of gaining section, students, under the supervision of nurse tutors, spend half of
confidence. A relaxed and accepting relationship was needed on the part each day seeing patients. In the afternoon the students work as a group,
of the teachers so that the students would feel safe in exploring new using the clinical problem-solving process to integrate and develop their
areas, acknowledging difficulties and being allowed to make mistakes. biopsychosocial theory and clinical knowledge.
The success of the course and the support for the weaker students were Once the students have become confident with the clinical problem-
fundamentally dependent on the ability of the group to work together. solving process, they begin to use reference books and to develop their
The tutors would actively remove a doctor from the teaching situation own theory knowledge. One group of students initially demanded copies
if they saw that his/her teaching was causing the students to regress
of the doctors’ lectures; later in the course, when they had become more
back to a rote learning mode as a result of the doctor’s more threatening
confident in their ability to learn theory themselves, they preferred to use
presence. This method of training seems to suit students from less
group self-study methods.
developed educational backgrounds. Students with further post-basic
education often had more difficulty learning the clinical problem-solving An important support for learning is the method used for assessing clinical
process. It is thought that this is because they have more trust in an skills and knowledge. The qualified PHC nurses say that the method of
artificial, learnt problem-solving method than in their own intrinsic assessment has helped prepare them for the working situation.
problem-solving ability.
The method entails written tests based on assessing the clinical
The courses started with the adult module first and others with the problem-solving process. Clinical assessment is done using five or six
paediatric module first. When comparing the results of the two methods stations with patients. Each station lasts for 10 or 20 minutes, depending
over several years and many courses, it was found that starting with on how much the students have to complete. All the students have to
the paediatric module promoted the clinical problem-solving process complete all the stations. Students are not observed and are marked on
better. An explanation may be that paediatric diseases tend to have what they have written. Patients are clerked by the examiners before
clearer disease patterns and are easier for decision making. Adult being hand-chosen from the available patients in the clinic. Mark
clinical decision making is complex and needs a more formal method guides are generated as far as possible in discussion amongst the
of decision making. History taking and physical examination are based examiners. Students have to complete a hypothetico-deductive history,
on the hypothetico-deductive method (encouraging the student to form demonstrating the likely causes and disease patterns and generating an
hypotheses based on the presenting symptoms and then testing them appropriate differential diagnosis. The students are given the specific
progressively on history and examination), similar to the Leicester body system that they should examine, including a general examination.
method.5 This is supported by Baye’s theorem that clinicians change their They must then complete the relevant examination and draw up final
diagnosis using the likelihood of a disease based on the initial evidence diagnoses. Using real patients from their working situation has been
of the disease, balanced against the strength of new information about found to encourage students to use the clinical problem-solving cycle.
another disease.6,7 The Leicester method has been found to result in
quicker and more natural development of the clinical problem-solving Results comparing students using different teaching
process.5 methods
Use of a learning structure In 2008, two types of teaching were used at the Soweto training centre.
One group of 20 students did a one-year full-time course. This group had
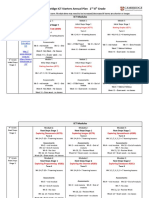
About 25 years ago, a visiting lecturer, whose first name was Bonny,
as their trainer a highly competent and experienced full-time doctor who
illustrated the use of mind maps for learning. These were adapted for
had been training PHC students for over 30 years. He gives extensive
clinical teaching by the author, and nicknamed “Bonny diagrams”. The
theory lectures and provides support and teaching when the students
students found the one-page mind map showing all important local
are seeing patients themselves throughout the course.
causes of a symptom combined with summary clinical features useful for
clinical problem solving. Causes are classified according to systems of Two other groups did an 18-month part-time course. The clinical problem-
the body. Common causes for each of the systems in Soweto are given, solving process was used as the basis of teaching. One group had doctor
as are the critical symptoms and signs for each disease. References to input on one or two days per month, mainly giving teaching regarding
the (Soweto) Primary Clinical Care Manual,8 which is the students’ main the patients. The other group had three to four hours of doctor input per
reference, are given to enable them to look up more details of the clinical month, mainly on the use of the clinical problem-solving cycle, for the
features and management of some of the diseases. An example of a first half of the course. Later in the course, the group had traditional-type
Bonny diagram for “Cough in an Adult” is given in Figure 1 below. lectures one day a week from the doctor teaching the full-time course.
SA Fam Pract 2010 61 Vol 52 No 1
Original Research: A method of teaching clinical problem-solving skills to primary health care student nurses
Figure 1. Bonny diagram for a cough in an adult9
Cough: Important causes
RESPIRATORY TRACT CARDIAC EAR, NOSE, THROAT
Symptoms of respiratory tract illness Symptoms of CVS illness Symptoms of ENT illness
• cough • shortness of breath on walking • runny/blocked nose
• chest pain • shortness of breath at night • sore throat
• +- dyspnoea • hypertension/elderly • cough dry or hawking
• left sided chest pain
Mild RTI • chest pain radiates to left arm Tonsillitis
• white sputum • palpitations • sore throat
• dry of mildly productive cough • previous heart disease • fever
• mild fever • severe swelling of feet • painful neck glands
• no distress • red/enlarged tonsils
• resp rate < 20
• pulse < 100 per min Sinusitis
• frontal headache worse on
Moderate RTI bending
• yellow/green/blood stained sputum • halitosis
• mild short of breath • tender sinuses
• resp rate 20 – 30
• pulse < 110 Viral Rhinitis (Cold)
• nasal discharge
Severe RTI • fever
• sharp localized chest pain • headache
• severe fever/rigors
• short of breath++ Allergy Rhinitis
• resp distress • related to allergies e.g. pets,
• resp rate >30 in adult pollens, smoke
• pulse < 110 • recurrent sneezing
• chronic itching nose
Allergy/Asthma • watery nasal discharge
• tight chest
• recurrent
COUGH
• other allergy symptoms
• precipitating and relieving factors
COAD
• chronic cough
• progressive dyspnoea + smoker
Lung abscess
• severe acute fever GIT
• severe Halitosis Oesophageal Reflux
• offensive sputum • worse at night
• localized chest pain • other symptoms of reflux
Carcinoma lung
• severe pain in ribs or spine
• haemoptisis
• sudden onset of dubbing P.C.P MENTAL
• smoker (pneumocystis caririi pneumonia) Stress and anxiety
• severe loss of weight • dry cough
TB • acute shortness of breath • increased with stress
• chronic progressive cough • severe dry cough • chronic
• chronic loss of weight > 5kg • oral thrush • no other symptoms or signs
• chronic severe night sweats • other symptoms or signs of HIV
The full-time and part-time students wrote the same two final summative Discussion
theory papers of three hours each. These were set by all the nurse tutors
Organising the knowledge helps both the teachers and learners. Elstein
involved with the course, and had an external examiner. The average
states the emphasis should be on helping students acquire a functional
theory mark for the full-time group of 20 students was 57.1. The average organisation of content by using clinically usable schemas.7 Mandin et
mark for the 26 students doing the part-time course was 65.8 (T test al comment that successful problem solvers have a way of organising
value of 0.0006). All student groups were selected randomly. Several their knowledge. Knowledge needs to be organised to understand and
of the examiners commented that the part-time group showed deeper to assist with clinical problem solving. These authors propose that
understanding of clinical problem solving. a scheme-driven strategy be used to help students develop a more
SA Fam Pract 2010 62 Vol 52 No 1
Original Research: A method of teaching clinical problem-solving skills to primary health care student nurses
organised and logical approach to problem solving.10 Doshi and Brown Conclusion
noted that there is increasing evidence of the effectiveness of more
A cyclical mind map can develop and enhance the ability of students to
structured approaches to patient-based teaching.11
use self-learning methods for integrating theory into a clinical problem-
In discussions, the nurse tutors emphasise the importance of patient- solving process. Our experience has been that primary-level nurse
based teaching to facilitate the clinical problem-solving process. The instructors and doctors find using the mind map makes teaching easier
advantages of patient-based teaching are that it is closer to real life for them. This method of teaching may be of value to family practitioners
and has more relevance for the students’ future work situations.12 This who are teaching nurse clinicians.
patient-based teaching is strengthened by our students going back into
the work situation every alternate week. Many of the students comment Acknowledgements
that it is easier to learn and remember if the teaching has been based on
The author would like to thank Ms Mahlo, Ms Mbelu, Ms Prinsloo and Dr
real patients. Patient-based teaching offers the important aspect of the
Kalain for their pioneering work in applying this method of teaching in
patient giving direct feedback to the student.13 We find that the patients
their PHC student courses, and Professor Couper, Professor Hammond
promote better behaviour patterns in our students because they challenge
and Ms Sondzaba for extensively reviewing and revising this article.
the students about impolite behaviour or incorrect approaches. As the
students begin to better understand the issues the patients are facing, Conflicts of interest
they become more tolerant in their behaviour. Patients often demonstrate
to the students how much they know and how well they have been There are no conflicts of interest.
dealing with their illnesses. This helps the students develop respect for
References
their patients’ knowledge and understanding of their diseases. It makes
1. Irwig LM, Porter B, Wilson TD, Saunders LD, Wagstaff LA, Liesch N, et al. Clinical competence of
consultations more interesting for the students and the practising nurse paediatric primary health care nurses in Soweto. S Afr Med J 1985;J19:67(3):92–5.
clinicians. It also makes health education more effective, as the clinician 2. Wagstaff LA, Shuenyane EN, Mkhasibe CM, Geefhuysen J, Platzky D. Comparisons in the therapeutic
management of black paediatric outpatients by primary health care nurses and doctors. S Afr Med
can concentrate on areas the patient does not know about. We find that J 1982;62(18):654–7.
teaching around a patient helps to show all the aspects of clinical problem 3. Wagstaff LA, Beukes PJ. The paediatric primary health care nurse project in Soweto. S Afr Med J
1977;52(27):1086–8.
solving in a practical and vivid way. Many different aspects of assessing
4. Wagstaff LA. The changing role of doctors in the Soweto clinics’ health care teams. S Afr Med J
and managing a patient holistically can be taught around a patient, such 1978;53(20):805–6.
as the social or family background or work-related issues.14 5. Fraser RC. Clinical method: a general practice approach. 3rd edition. Oxford: Butterworth Heinemann;
2003.
Interestingly, Doshi and Brown comment on the problem of a dwindling 6. Gill CJ, Sabin L, Schmid CH. Education and debate. Why clinicians are natural Bayesians.
BMJ 2005;330(7499):1080–3.
patient base in their environment.11 One of the privileges of teaching in the 7. Elstein AS, Schwarz A. Clinical problem solving and diagnostic decision making: selective review of
primary care situation in South Africa is the amazing variety of patients the cognitive literature. BMJ 2002;324(7339):729–32.
8. Pein L, Truscott A. Primary clinical care manual. 4th edition. Johannesburg: Jacana; 2005.
available at PHC clinics for teaching purposes. Patients sometimes
9. Truscott A. Clinical problem solving notes for nurse clinicians. Johannesburg: Bytes Solutions;
request to be seen at the teaching section, as this may ensure a more 2008.
comprehensive consultation. However, other patients avoid the teaching 10. Mandin H, Jones A, Woloschuk W, Harasym P. Helping students learn to think like experts when
solving clinical problems. Acad Med 1997;72(3):173–9.
section as the consultation takes too long!
11. Doshi M, Brown N. Whys and hows of patient based teaching. Advances in Psychiatric Treatment
2005;11:223–31.
12. Spencer J. ABC of learning and teaching in medicine: learning and teaching in the clinical
environment. BMJ 2003;326(7389):591–4.
13. Ferenchick G, Simpson D, Blackman J, et al. Strategies for efficient and effective teaching in the
ambulatory care setting. Academic Medicine 1997;72(4):277–80.
14. Ramani, S. Twelve tips to improve bedside teaching. Medical Teacher 2003;25(2):112–5.
SA Fam Pract 2010 63 Vol 52 No 1
You might also like
- Five Models of Staff DevelopmentDocument34 pagesFive Models of Staff DevelopmentZulaiha Abdul Rahman100% (3)
- Layers of The Earth Lesson PlanDocument6 pagesLayers of The Earth Lesson PlanRutchel Martinez33% (3)
- Annual Instructional Supervisory PlanDocument8 pagesAnnual Instructional Supervisory PlanVictoria Beltran SubaranNo ratings yet
- A Self Reflection On The Evolution & Historical Impact of The DNPDocument8 pagesA Self Reflection On The Evolution & Historical Impact of The DNPapi-577750864No ratings yet
- Analysis of The Concept Continuing Education in Nursing EducatioDocument11 pagesAnalysis of The Concept Continuing Education in Nursing EducatioTapodhan VishuNo ratings yet
- Evidence Based PracticeDocument18 pagesEvidence Based Practicemeghana100% (11)
- Differentiates Between Equations and InequalitiesDocument7 pagesDifferentiates Between Equations and InequalitiesMarc Galos100% (2)
- Clinical Field Experience B Peer Instructional Planning ReviewDocument3 pagesClinical Field Experience B Peer Instructional Planning Reviewapi-5189947450% (1)
- Korean Nursing Students' Experiences of Their First Clinical PracticeDocument11 pagesKorean Nursing Students' Experiences of Their First Clinical PracticeKruh Kwabena IsaacNo ratings yet
- Research BriefsDocument8 pagesResearch BriefsNur MiladiyahNo ratings yet
- International Journal of Nursing SciencesDocument5 pagesInternational Journal of Nursing SciencesWahyu Phaling FienterNo ratings yet
- Scholarly Paper CapstoneDocument6 pagesScholarly Paper Capstoneapi-662404021No ratings yet
- 1 PBDocument7 pages1 PBAngie MandeoyaNo ratings yet
- Role of ResearchDocument8 pagesRole of ResearchDipti Punjal100% (1)
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument4 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyWednesdayNo ratings yet
- Scholarly Article PaperDocument7 pagesScholarly Article Paperapi-545697687No ratings yet
- Nursing Attitudes and BeliefsDocument5 pagesNursing Attitudes and Beliefsyovanimanuel imanuelNo ratings yet
- Cabarrubias Jovelyn - Enrichment Activity For Module 1Document3 pagesCabarrubias Jovelyn - Enrichment Activity For Module 1cabarrubiasjovy40No ratings yet
- Clinical Nursing JudgmentDocument5 pagesClinical Nursing Judgmentapi-662884360No ratings yet
- Clinicalteachingmethods 180306040756Document31 pagesClinicalteachingmethods 180306040756abcqwe123No ratings yet
- Clinical Teaching MethodsDocument5 pagesClinical Teaching MethodsFlora AlfaxdNo ratings yet
- Nursing Research Challenges and OpportunitiesDocument27 pagesNursing Research Challenges and Opportunitiessara mohamedNo ratings yet
- 1.clinical Teaching Methods MokshithaDocument23 pages1.clinical Teaching Methods MokshithaVeena DalmeidaNo ratings yet
- Analysis of Midwifery Teachers' Approach To Identifying Student Midwives With Poor Clinical Reasoning SkillsDocument7 pagesAnalysis of Midwifery Teachers' Approach To Identifying Student Midwives With Poor Clinical Reasoning SkillsIntan Mustika SariNo ratings yet
- Womens PetDocument3 pagesWomens Petapi-307931906No ratings yet
- Goals and Objectives of Fellow and ResidentsDocument38 pagesGoals and Objectives of Fellow and ResidentsjustinemaeferrerpinedaNo ratings yet
- Stave Ski 2015Document8 pagesStave Ski 2015Dian Rachmah FaoziahNo ratings yet
- Nursing RoundDocument7 pagesNursing RoundBishwajitMazumder100% (5)
- FINAL Brochure Oudce EvidenceDocument16 pagesFINAL Brochure Oudce Evidencexbsd100% (2)
- Clinical Objectives PDFDocument4 pagesClinical Objectives PDFYhuhan James TejadaNo ratings yet
- Clinical Nursing JudgementDocument5 pagesClinical Nursing Judgementapi-449796082No ratings yet
- Seminar For Educators: Teaching at The BedsideDocument4 pagesSeminar For Educators: Teaching at The Bedsidestarskyhutch0000No ratings yet
- Scholarly PaperDocument5 pagesScholarly Paperapi-661467979No ratings yet
- Shadow ANurseDocument8 pagesShadow ANurseSculpting FutureNo ratings yet
- Peplau's Interpersonal Relations Theory Power PointDocument10 pagesPeplau's Interpersonal Relations Theory Power PointPerlie Loren Arreo Cabatingan100% (1)
- Residency Manual 2018Document85 pagesResidency Manual 2018shazia kaziNo ratings yet
- Nms 3540 Study GuideDocument16 pagesNms 3540 Study GuideSepo CaciousNo ratings yet
- Clinical Skills IIIDocument16 pagesClinical Skills III4t72vb9kkdNo ratings yet
- Peplau's Interpersonal Relations Theory Power PointDocument10 pagesPeplau's Interpersonal Relations Theory Power PointCharisse Nicole DiazNo ratings yet
- Diploma in Family MedicineDocument29 pagesDiploma in Family Medicineamira_hassan100% (1)
- PROGRAMA EDUCACIÓ CONTINUApirong1982Document3 pagesPROGRAMA EDUCACIÓ CONTINUApirong1982GladysNo ratings yet
- WEEK 10 CU 10 - Evidenced Base Practice in Health Education NewDocument5 pagesWEEK 10 CU 10 - Evidenced Base Practice in Health Education Newarmanuel1390antNo ratings yet
- ME - Ethical Decision Making On Truth Telling in Terminal Cancer - Medical Students' Choices Between Patient Autonomy and Family PaternalismDocument9 pagesME - Ethical Decision Making On Truth Telling in Terminal Cancer - Medical Students' Choices Between Patient Autonomy and Family PaternalismAya SalahNo ratings yet
- Faculty Development One MinuteDocument9 pagesFaculty Development One MinuteDaniel Alejandro Lozano MorenoNo ratings yet
- Effect of High Fidelity Simulation On Clinical Decision Making Among Nursing StudentsDocument10 pagesEffect of High Fidelity Simulation On Clinical Decision Making Among Nursing Studentsاحمد العايديNo ratings yet
- Nurs490 Safety Performance Improvement Paper Neuburg IntroDocument2 pagesNurs490 Safety Performance Improvement Paper Neuburg Introapi-452041818No ratings yet
- FINAL OB - PATHO - Case PresentationDocument75 pagesFINAL OB - PATHO - Case PresentationBEATRICE CAXANDRA NAMBATAC BACASNo ratings yet
- Calculous CholecystitisDocument137 pagesCalculous Cholecystitisrremonde100% (5)
- Evidence-Based Practice and Applied Nursing ResearchDocument6 pagesEvidence-Based Practice and Applied Nursing ResearchErickNo ratings yet
- Research in Continuing Education Programme: C. Meribha Christy, V. HemavathyDocument4 pagesResearch in Continuing Education Programme: C. Meribha Christy, V. HemavathyRubina MasihNo ratings yet
- Self Assessment - Midterm 2016Document11 pagesSelf Assessment - Midterm 2016api-341527743No ratings yet
- Evidence Based Nursing in Clinical PractDocument5 pagesEvidence Based Nursing in Clinical PractVivi DisNo ratings yet
- Tujuan Teori KeperawatanDocument15 pagesTujuan Teori KeperawatankintaniaNo ratings yet
- Course Plan: Obstetric & Gynaecological NursingDocument11 pagesCourse Plan: Obstetric & Gynaecological NursingPriya100% (3)
- Journal of Midwifery & Women-S HealthDocument11 pagesJournal of Midwifery & Women-S HealthJuniatiNo ratings yet
- Assignment of AnpDocument18 pagesAssignment of Anpcharanjit kaurNo ratings yet
- Clinical Teaching: S.M. Nazmul Al-Deen Subject: Principles and Methods of TeachingDocument9 pagesClinical Teaching: S.M. Nazmul Al-Deen Subject: Principles and Methods of TeachingNazmul Al-deenNo ratings yet
- Research PresentationDocument14 pagesResearch PresentationCeeNo ratings yet
- Nurse Educator Practicum - Reflective Journal 2Document4 pagesNurse Educator Practicum - Reflective Journal 2api-643881078No ratings yet
- Clinical Nursing JudgementDocument6 pagesClinical Nursing Judgementapi-507960658No ratings yet
- Bi, 2019Document6 pagesBi, 2019aminNo ratings yet
- Iebp PDFDocument5 pagesIebp PDFchuramarak23No ratings yet
- Bucknall 2016Document13 pagesBucknall 2016mnazri98No ratings yet
- CH 01 PDFDocument25 pagesCH 01 PDFkikiNo ratings yet
- Advanced Practice and Leadership in Radiology NursingFrom EverandAdvanced Practice and Leadership in Radiology NursingKathleen A. GrossNo ratings yet
- New SN of Polling Station Locality Building in Which It Will Be Polling Areas Wheather For All Voters or Men Only or Women OnlyDocument51 pagesNew SN of Polling Station Locality Building in Which It Will Be Polling Areas Wheather For All Voters or Men Only or Women OnlyJugal HarkutNo ratings yet
- List of Judicial OfficersDocument1 pageList of Judicial OfficersJugal HarkutNo ratings yet
- Clinical Signs and Symptoms at Diagnosis and Its Differential DiagnosisDocument9 pagesClinical Signs and Symptoms at Diagnosis and Its Differential DiagnosisJugal HarkutNo ratings yet
- Evidence Base of Clinical DiagnosisDocument4 pagesEvidence Base of Clinical DiagnosisJugal HarkutNo ratings yet
- Anti CD20 Monoclonal Antibodies Reviewing A RevolutionDocument23 pagesAnti CD20 Monoclonal Antibodies Reviewing A RevolutionJugal HarkutNo ratings yet
- The Design of Discrete Vocabulary TestsDocument19 pagesThe Design of Discrete Vocabulary TestsPiroska SzolnokiNo ratings yet
- Week 12 AssignmentDocument6 pagesWeek 12 AssignmentLinhNo ratings yet
- Uts Final ReviewerDocument14 pagesUts Final ReviewerCarla QuiñonesNo ratings yet
- KPS Bluebook 26 MarchDocument80 pagesKPS Bluebook 26 Marchvijeth3110No ratings yet
- Organisational Climate, Ethos and Learning in Organisation: Presented by Swetha K Kethireddy Sri CharanDocument28 pagesOrganisational Climate, Ethos and Learning in Organisation: Presented by Swetha K Kethireddy Sri CharanSri Charan ReddyNo ratings yet
- Cambridge ICT Starters Annual Plan 2nd-8th Grade ALL SCHOOLS 2022Document4 pagesCambridge ICT Starters Annual Plan 2nd-8th Grade ALL SCHOOLS 2022Allen Panamá GutzNo ratings yet
- Tutorial Week 1: Norfadzilah Sulaiman Anis Wardah Yusri Nur Amanina AzhariDocument8 pagesTutorial Week 1: Norfadzilah Sulaiman Anis Wardah Yusri Nur Amanina AzhariTeo Khim SiangNo ratings yet
- IM Evaluation Rubric Form - Ela 7213 PDFDocument3 pagesIM Evaluation Rubric Form - Ela 7213 PDFEmir UzairNo ratings yet
- NegOr Q3 English4 Module4 v2 PDFDocument19 pagesNegOr Q3 English4 Module4 v2 PDFBambi BandalNo ratings yet
- PSY 540 Milestone Three (3) .Docx65507df63786335675Document13 pagesPSY 540 Milestone Three (3) .Docx65507df63786335675master lamarNo ratings yet
- Long Quiz in Practical Research I Test 1. Multiple Choice Direction: Choose The Letter of The Correct Answer. Encircle The Letter of Your AnswerDocument2 pagesLong Quiz in Practical Research I Test 1. Multiple Choice Direction: Choose The Letter of The Correct Answer. Encircle The Letter of Your AnswerRobert Jay MejoradaNo ratings yet
- Personal InformationDocument8 pagesPersonal InformationashishNo ratings yet
- Types and Characteristics of Teaching MediaDocument10 pagesTypes and Characteristics of Teaching MediaLami Lee0% (1)
- LEARNING ENGLISH Kindergarten 1 - New Book Information (NBI)Document1 pageLEARNING ENGLISH Kindergarten 1 - New Book Information (NBI)Sam OeunNo ratings yet
- A Clil Guide 5 Activities For Every Clil Teacher PDFDocument10 pagesA Clil Guide 5 Activities For Every Clil Teacher PDFClaudine74No ratings yet
- Barrow Lions Club Scholarship Application FormDocument4 pagesBarrow Lions Club Scholarship Application FormBarrow Lions ClubNo ratings yet
- TKT Module 3Document11 pagesTKT Module 3Татьяна АндрющенкоNo ratings yet
- 19 - iPLANDocument3 pages19 - iPLANMarlyn CaballeroNo ratings yet
- Teaching English Through KangGuru English MagazineDocument8 pagesTeaching English Through KangGuru English Magazineyusuf hidayatNo ratings yet
- Visible Learning For Teachers MaximisingDocument5 pagesVisible Learning For Teachers MaximisingNatalia FaleroNo ratings yet
- Reading and Writing Write It Out: by The End of This Lesson Ss Will Be Able ToDocument2 pagesReading and Writing Write It Out: by The End of This Lesson Ss Will Be Able ToLarbi Nadia100% (1)
- Constructivism Approach in Teaching Higher Order Thinking SkillsDocument6 pagesConstructivism Approach in Teaching Higher Order Thinking SkillsIvan ChooNo ratings yet
- ct9 Ilm1Document13 pagesct9 Ilm1heart MUNOZNo ratings yet
- DLP MTB Co 1Document10 pagesDLP MTB Co 1kerl karen ferrerNo ratings yet
- Animal Legs LessonDocument7 pagesAnimal Legs Lessonapi-374359720100% (1)