Professional Documents
Culture Documents
AKI Case Discussion 2.0
AKI Case Discussion 2.0
Uploaded by
Mary Dominique RomoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AKI Case Discussion 2.0
AKI Case Discussion 2.0
Uploaded by
Mary Dominique RomoCopyright:
Available Formats
To discuss Acute Kidney Injury in terms of its
a. Epidemiology, Etiology, and Pathophysiology
b. Diagnostic evaluation
c. Treatment and Complications
DEFINITION
Harrison’s 20th Edition
AKI is defined by the impairment of kidney filtration and excretory function over days to weeks,
resulting in the retention of nitrogenous and other waste products normally cleared by the
kidneys. is not a single disease but, rather, a designation for a heterogeneous group of
conditions that share common diagnostic features: specifically, an increase in serum creatinine
(SCr) concentration often associated with a reduction in urine volume.
KDIGO 2012
AKI is defined as any of the following (Not Graded):
o Increase in SCr by ≥0.3 mg/dl (≥26.5 lmol/l) within 48 hours; or
o Increase in SCr to ≥1.5 times baseline, which is known or presumed to have occurred
within the prior 7 days; or
o Urine volume <0.5 ml/kg/h for 6 hours.
EPIDEMIOLOGY
AKI complicates 5–7% of acute care hospital admissions and up to 30% of admissions to the
intensive care unit. AKI is associated with a markedly increased risk of death in hospitalized
individuals, particularly in those admitted to the ICU where in-hospital mortality rates may
exceed 50%. AKI increases the risk for the development or worsening of chronic kidney disease
(CKD).
ETIOLOGY AND PATHOPHYSIOLOGY
The causes of AKI have traditionally been divided into three broad categories: prerenal azotemia,
intrinsic renal parenchymal disease, and postrenal obstruction.
DIAGNOSTIC EVALUATION
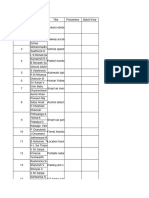
RIFLE Criteria
o The Acute Dialysis Quality Initiative (ADQI) group developed a system for diagnosis and
classification of a broad range of acute impairment of kidney function through a broad consensus
of experts.
o The acronym RIFLE stands for the increasing severity classes Risk, Injury, and Failure; and the
two outcome classes, Loss and End-Stage Renal Disease (ESRD). The three severity grades are
defined on the basis of the changes in SCr or urine output where the worst of each criterion is
used. The two outcome criteria, Loss and ESRD, are defined by the duration of loss of kidney
function.
TREATMENT
COMPLICATIONS
The kidney plays a central role in homeostatic control of volume status, blood pressure, plasma
electrolyte composition, and acid-base balance, and for excretion of nitrogenous and other waste
products. Complications associated with AKI are, therefore, protean, and depend on the severity of AKI
and other associated conditions. Mild to moderate AKI may be entirely asymptomatic, particularly early
in the course.
1. Uremia
2. Hypervolemia and Hypovolemia
3. Hyponatremia
4. Hyperkalemia
5. Acidosis
6. Hyperphosphatemia and Hypocalcemia
7. Bleeding
8. Infections
9. Cardiac complications
10. Malnutrition
You might also like
- History Taking Form in Gynecology & ObstetricsDocument8 pagesHistory Taking Form in Gynecology & ObstetricsAbdullah Matar86% (7)
- Baseline Discrimagon User ManualDocument2 pagesBaseline Discrimagon User ManualphcproductsNo ratings yet
- Understanding Chronic Kidney Disease: A guide for the non-specialistFrom EverandUnderstanding Chronic Kidney Disease: A guide for the non-specialistRating: 4 out of 5 stars4/5 (3)
- Ahmed Ali - CKDDocument20 pagesAhmed Ali - CKDAhmed AliNo ratings yet
- Global Epidemiology and Outcomes of Acute Kidney InjuryDocument19 pagesGlobal Epidemiology and Outcomes of Acute Kidney Injuryredouane bennaiNo ratings yet
- Chew, Dennis - Acute - Kidney - Disease - Cats - STYLEDDocument7 pagesChew, Dennis - Acute - Kidney - Disease - Cats - STYLEDPatricia QueroNo ratings yet
- Global EpidemiologyDocument19 pagesGlobal EpidemiologySoniamartilovaNo ratings yet
- Acute Renal FailureDocument12 pagesAcute Renal FailureRifa Aprillia CahyaniNo ratings yet
- Kidney Injury: AcuteDocument14 pagesKidney Injury: AcutealfredoibcNo ratings yet
- 1.1 AkiDocument89 pages1.1 Akilibentadesse57No ratings yet
- Integrated Therapeutics-Ii For 3 Year STS: Chapter-1Document69 pagesIntegrated Therapeutics-Ii For 3 Year STS: Chapter-1Geleta GalataaNo ratings yet
- Síndrome Hepatorrenal Cirrosis Eur Gast J 2021Document9 pagesSíndrome Hepatorrenal Cirrosis Eur Gast J 2021Anabel GonzalezNo ratings yet
- Aetiology: Save Time & Improve Your PDP On Patient - Co.ukDocument9 pagesAetiology: Save Time & Improve Your PDP On Patient - Co.ukBaihaqi SaharunNo ratings yet
- Integrated Therapeutics IiDocument165 pagesIntegrated Therapeutics IiSalahadinNo ratings yet
- Renal DisordersDocument164 pagesRenal Disorderspblinder1319No ratings yet
- Surgery in The Patient With Renal DysfunctionDocument11 pagesSurgery in The Patient With Renal DysfunctionAps CnjNo ratings yet
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocument5 pagesEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryyinyangdongNo ratings yet
- Acute Kidney Injury: Current Concepts and New Insights: Key WordsDocument5 pagesAcute Kidney Injury: Current Concepts and New Insights: Key WordsIHNo ratings yet
- Acute Kidney Injury An UpdateDocument9 pagesAcute Kidney Injury An Updatekarol fernandezNo ratings yet
- Inter'Medic CKDDocument31 pagesInter'Medic CKDMAHEJS HD100% (1)
- Coursematerial 136Document13 pagesCoursematerial 136Nyj QuiñoNo ratings yet
- Renal FailureDocument35 pagesRenal FailureJawad SaleemNo ratings yet
- Lecture 2. Acute Renal FailureDocument85 pagesLecture 2. Acute Renal FailurePharmswipe KenyaNo ratings yet
- Acute Kidney InjuryDocument15 pagesAcute Kidney Injurykuchaibaru90No ratings yet
- Acute Kidney Injury (AKI) : BackgroundDocument22 pagesAcute Kidney Injury (AKI) : BackgroundDeif TunggalNo ratings yet
- Chronic Kidney DiseaseDocument30 pagesChronic Kidney Diseasenathan asfahaNo ratings yet
- Acute Kidney InjuryDocument17 pagesAcute Kidney InjuryCha-cha UzumakiNo ratings yet
- 2016 AJKD Volume 67 Issue 2 February (33) HepatorenalDocument11 pages2016 AJKD Volume 67 Issue 2 February (33) HepatorenalAnonymous Yo0mStNo ratings yet
- CKD UnsoedDocument42 pagesCKD UnsoedSutan Malik IbrahimNo ratings yet
- WWW - Uwonephrology.ca Pdfs Academichalfday 20110308 AKIPart12011Document8 pagesWWW - Uwonephrology.ca Pdfs Academichalfday 20110308 AKIPart12011Ale Marques - TarólogoNo ratings yet
- Problem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureDocument48 pagesProblem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureAnishilNo ratings yet
- Novel Aspects of Pharmacological Therapies For Acute Renal FailureDocument16 pagesNovel Aspects of Pharmacological Therapies For Acute Renal FailureproluvieslacusNo ratings yet
- Acute Renal Failure in The ICU PulmCritDocument27 pagesAcute Renal Failure in The ICU PulmCritchadchimaNo ratings yet
- Chronic Kidney DiseaseDocument40 pagesChronic Kidney DiseaseEsayas KebedeNo ratings yet
- Renal DisorderDocument102 pagesRenal DisorderIbsaa UsmanNo ratings yet
- Acute Kidney InjuryDocument9 pagesAcute Kidney InjuryRobertNo ratings yet
- Renal Disease: Acute Kidney Injury (AKI)Document5 pagesRenal Disease: Acute Kidney Injury (AKI)api-142637023No ratings yet
- Chronic Kidney DiseaseDocument55 pagesChronic Kidney DiseaseBentoys Street100% (1)
- Acute Kidney Injury - Chronic Kidney DeseaseDocument71 pagesAcute Kidney Injury - Chronic Kidney DeseaseFina Ahmad Fitriana100% (1)
- Primer: Acute Kidney InjuryDocument17 pagesPrimer: Acute Kidney InjuryDiana AngelesNo ratings yet
- Gagal Ginjal Akut - Bhs InggrisDocument27 pagesGagal Ginjal Akut - Bhs InggrisAgustinusNo ratings yet
- AkiDocument20 pagesAkiEnvhy AmaliaNo ratings yet
- CKD - Case PresDocument29 pagesCKD - Case PresChristine Joy Ilao PasnoNo ratings yet
- Role of Kidney Injury in Sepsis: Review Open AccessDocument6 pagesRole of Kidney Injury in Sepsis: Review Open AccessnudhakoNo ratings yet
- Jurnal CKDDocument7 pagesJurnal CKDJuni ClaudiaNo ratings yet
- Canine Chronic Kidney Disease Current Diagnostics & Goals For Long-Term ManagementDocument7 pagesCanine Chronic Kidney Disease Current Diagnostics & Goals For Long-Term ManagementJuni ClaudiaNo ratings yet
- AKI PathogenesisDocument11 pagesAKI PathogenesisKaren RamNo ratings yet
- Acute Kidney Injury - by Kameron MandDocument9 pagesAcute Kidney Injury - by Kameron MandKacey MandNo ratings yet
- CKDDDocument11 pagesCKDDAnaNo ratings yet
- Insuficiencia Renal AgudaDocument10 pagesInsuficiencia Renal AgudaJordan NanoNo ratings yet
- Renal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030Document31 pagesRenal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030jsksNo ratings yet
- RetrieveDocument10 pagesRetrieveDavid Sebastian Boada PeñaNo ratings yet
- Pharmacotherapy of Renal DisordersDocument231 pagesPharmacotherapy of Renal DisordersTewodros GetahunNo ratings yet
- CaseStudy ChronicRenalFailureDocument29 pagesCaseStudy ChronicRenalFailureCarlcedrick ManlapusNo ratings yet
- Hypomagnesemia Associated With Chronic Renal Diseases: A Review ArticleDocument12 pagesHypomagnesemia Associated With Chronic Renal Diseases: A Review ArticleRandom PersonNo ratings yet
- Chronic Kidney DiseaseDocument2 pagesChronic Kidney DiseasechyNo ratings yet
- Acute Kidney Injury and Chronic Kidney DiseaseDocument44 pagesAcute Kidney Injury and Chronic Kidney DiseaseIda Bagus Putu Swabawa100% (1)
- Azotemia - StatPearls - NCBI BookshelfDocument1 pageAzotemia - StatPearls - NCBI Bookshelfmellinda anastasyaNo ratings yet
- Acute Kidney Injury and Chronic Kidney DiseaseDocument44 pagesAcute Kidney Injury and Chronic Kidney DiseaseshihochanNo ratings yet
- Restoring Chronic Kidney Disease : Restoring, Preserving, and Improving CKD to Avoid DialysisFrom EverandRestoring Chronic Kidney Disease : Restoring, Preserving, and Improving CKD to Avoid DialysisNo ratings yet
- Medical Infographics by SlidesgoDocument32 pagesMedical Infographics by SlidesgoMary Dominique RomoNo ratings yet
- Extracellular Fluid VolumeDocument4 pagesExtracellular Fluid VolumeMary Dominique RomoNo ratings yet
- Chapter 16 SummaryDocument3 pagesChapter 16 SummaryMary Dominique RomoNo ratings yet
- Community CensusDocument2 pagesCommunity CensusMary Dominique RomoNo ratings yet
- Bullous-2018 TPDocument136 pagesBullous-2018 TPMary Dominique RomoNo ratings yet
- Sciexpo - Old Project (2022-2023)Document37 pagesSciexpo - Old Project (2022-2023)SrikrishnaBellamNo ratings yet
- Module 3a - Steps in Health Assessment - Subjective DataDocument7 pagesModule 3a - Steps in Health Assessment - Subjective DataGhian Bataller GonzalesNo ratings yet
- First Year Final OSCE EXAM 2018 2019Document4 pagesFirst Year Final OSCE EXAM 2018 2019محمد المنصورNo ratings yet
- Journal in Medical WardDocument4 pagesJournal in Medical WardApol PenNo ratings yet
- 3i T3 Implant Surgical Manual - CATMT3 - ENDocument67 pages3i T3 Implant Surgical Manual - CATMT3 - ENSalem RawashdahNo ratings yet
- Home Care For EpilepsyDocument16 pagesHome Care For Epilepsysanish4uNo ratings yet
- Pregnant Women With UtiDocument9 pagesPregnant Women With UtiJULIANNE BAYHONNo ratings yet
- Nausea and Vomiting of PregnancyDocument8 pagesNausea and Vomiting of PregnancycintacitraNo ratings yet
- ElectrocardiographyDocument29 pagesElectrocardiographyJhevey ValdezNo ratings yet
- GENERIC NAME: FENOFIBRATE - ORAL (fen-oh-FYE-brate) BRAND NAME (S) : Tricor, TriglideDocument3 pagesGENERIC NAME: FENOFIBRATE - ORAL (fen-oh-FYE-brate) BRAND NAME (S) : Tricor, TriglideDevesh GaurNo ratings yet
- Reading 5 Blood and Body DefensesDocument18 pagesReading 5 Blood and Body Defenseslephuongvy1406No ratings yet
- TUBERCLUOSIS MCQS, ZSMU, UkraineDocument26 pagesTUBERCLUOSIS MCQS, ZSMU, UkraineDrRaghavender Reddy100% (1)
- Aminoglycoside AntibioticsDocument56 pagesAminoglycoside AntibioticsMaharani IndriatyNo ratings yet
- Practical Application of CPAP: Dr. Srinivas MurkiDocument8 pagesPractical Application of CPAP: Dr. Srinivas MurkiRaji MohanNo ratings yet
- Oncology Revision: Paul BaillieDocument299 pagesOncology Revision: Paul BaillieMourian AmanNo ratings yet
- GROUP F Compilation PsychiaFinalDocument20 pagesGROUP F Compilation PsychiaFinalFrancis Raphael PitogoNo ratings yet
- Product Datasheet: MCM7 Antibody NBP1-85721Document5 pagesProduct Datasheet: MCM7 Antibody NBP1-85721JoaoNo ratings yet
- Tyrosinemia Type 1Document8 pagesTyrosinemia Type 1Muhammad LawalNo ratings yet
- Esophagus QuesDocument8 pagesEsophagus QuesnehaNo ratings yet
- Effect of The Rho-Associated Kinase Inhibitor Eye Drop (Ripasudil) On Corneal Endothelial Wound HealingDocument9 pagesEffect of The Rho-Associated Kinase Inhibitor Eye Drop (Ripasudil) On Corneal Endothelial Wound HealingRaúl Plasencia SaliniNo ratings yet
- Cpm15th Dengue Fever (Doh)Document18 pagesCpm15th Dengue Fever (Doh)Marko ParungoNo ratings yet
- Statistical Diabetic ReportDocument10 pagesStatistical Diabetic ReportSunila AkramNo ratings yet
- Andi Muh. Octavian Pratama Et Anwar Lewa-1Document9 pagesAndi Muh. Octavian Pratama Et Anwar Lewa-1octavian pratamaNo ratings yet
- How To Use This MedicineDocument2 pagesHow To Use This MedicinelelaniaNo ratings yet
- Bachelor of Science in Nursing: Care of Mother and Child and AdolescentDocument12 pagesBachelor of Science in Nursing: Care of Mother and Child and AdolescentJaja ManezNo ratings yet
- Pharmacotherapy of TB - Handout (Final) 4-08Document3 pagesPharmacotherapy of TB - Handout (Final) 4-08Ahmedshaker21No ratings yet
- Eden University: Department of Clinical Medicine Diploma in Clinical MedicineDocument1 pageEden University: Department of Clinical Medicine Diploma in Clinical MedicineParker KapembwaNo ratings yet
- Effect of Intraoperative Dexmedetomidine On Post-Craniotomy PainDocument9 pagesEffect of Intraoperative Dexmedetomidine On Post-Craniotomy PainIva SantikaNo ratings yet