Professional Documents
Culture Documents
Microbiology Summaries 1-30 Microbiology Summaries 1-30
Microbiology Summaries 1-30 Microbiology Summaries 1-30
Uploaded by
yepOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Microbiology Summaries 1-30 Microbiology Summaries 1-30
Microbiology Summaries 1-30 Microbiology Summaries 1-30
Uploaded by
yepCopyright:
Available Formats
lOMoARcPSD|4886157
Microbiology Summaries 1-30
Microbiology (Medical University-Pleven)
StuDocu is not sponsored or endorsed by any college or university
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Microbiology Summaries 1-30
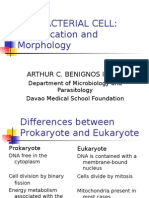
1. THE SCIENCE OF MICROBIOLOGY.CELLULAR AND NON-CELLULAR MICROORGANISMS. PROKARYOTES AND
EUKARYOTES. BACTERIA GENERAL CHARACTERISTICS
Microbiology is the study of microorganisms. Microorganisms are divided into cellular and non-cellular.
Cellular: Eukaryotes (protozoa, fungi)
Prokaryotes (bacteria)
Non-cellular: virus, viroid, prions
DIFFERENCES BETWEEN CELLULAR AND NON-CELLULAR M.O
CRITERIA CELLULAR NON-CELLULAR
STRUCTURE Nucleus Pores
Cytoplasm Protein coat (capsid)
METHOD OF REPLICATION Binary fission Not binary fission, but complex
reproduction
NATURE OF NUCLEIC ACID DNA &RNA Either of both
Cellular: cellular bacteria is divided into eukaryotes and prokaryotes
Eukaryotes: eukaryotes are organisms that have nucleus within their cell
Prokaryotes: are organisms that have no nucleus (like bacteria) but have DNA.
Eukaryotes Prokaryotes
Small cells Larger cells
Always unicellular Often multicellular
DNA is circular, without proteins DNA is linear and associated with
proteins to form chromatin
No nucleus or any membrane Always have nucleus and
bound organelles membrane bound organelles
Non-cellular: non cellular bacteria are bacteria lacking cells and they include viruses, prions and viroids
Virus: they are particles that consists of a nucleic acid molecule, either DNA or RNA, enclosed in a
protein coat or capsid, they are known to infect all cells. They only replicate within living cells and are
enclosed in a capsid envelope
Prions: they are infectious agents composed entirely of a protein material that can fold in multiple,
structurally abstract ways. Prions are composed of prion protein (Prp) which are believed to be the
cause of transmissible spongiform encephalopathies (TSEs) which is a form of neurodegenerative
diseases among other diseases .they have no nucleic acid
Viroids : they are the smallest infectious agents known, they have no protein and only small circular RNA
and they can cause plant diseases.
BACTERIA: GENERAL CHARACTERISTICS
Unicellular with independent metabolic existence
Reproduce by binary fission
Can grow on artificial media
Can survive only in infected hosts
Shapes:
Cocci (staphylococcus, streptococcus and diplococcus)
Bacilli
Spirals
The essential structures of bacteria are: cytoplasm, ribosome and cell envelope
Non-essential structures are Pilli, flagella, capsule
Cytoplasmic membrane: no sterols with phospholipid layer and protein, the cytoplasmic membrane
secretes hydrolytic enzymes and toxins
2. MORPHOLOGY OF BACTERIA. BACTERIAL STRUCTURE. RIBOSOMES. NUCLEOID. CYTOPLASMIC MEMBRANE.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Morphology of bacterial cells deals with study of:
Size of bacteria
Shape of bacteria
Arrangement of bacteria #
Size of bacteria
Size of bacteria cells is less than 3 micrometers
These bacteria may be spherical, cylindrical or spiral in shape
Shape of bacteria
Spherical or cocci shape
Cylindrical shape or rod-shape
Spiral shape: twisted two or more times along the axis
Arrangement of bacteria
Arrangement of cocci shaped bacteria
Cocci- o
Diplococci- oo
Streptococci- oooo
Staphylococci- clusters
Arrangement of rod shaped bacteria
Bacilli- one rod
Diplobacilli- two rods
Streptobacilli- in a chain of two or more rods
Bacterial structure
Bacteria are prokaryotes, lacking well defined nuclei and membrane bound organelles, and with chromosomes
composed of a single closed DNA circle. There are two ways of grouping bacteria. They can be divided into three
types based on their response to gaseous oxygen.
Aerobic bacteria: they require oxygen for their health and existence and will die without it
Anaerobic bacteria: they cant tolerate gaseous oxygen at all and die when exposed to it
Facultative anaerobes: they prefer oxygen but can live without it
The second way of grouping them is by how they obtain their energy.
Bacteria that have to consume and break down complex organic compounds are HETEROTROPHS
Bacteria that can create their own energy, fuelled by light or through chemical reactions are knows as
AUTOTROPHS.
Structure:
Capsule: some species of bacteria have a third protective layer which is a capsule the main function of the capsule
is to prevent it from phagocytosis. The capsule is a major virulence factor in the major-disease causing bacteria,
such as E.coli and streptococcus.pneumonia.
Cell wall: each bacterium is enclosed by a rigid cell wall composedof peptidoglycan, a protein-sugar
(polysaccharide) molecule. The cell wall gives the cell its shape and surrounds the cytoplasmic membrane,
protecting it from the environment. It also helps to anchor appendages like the pili and flagella, which originates in
the cytoplasm membrane and protrude through the wall is responsible for keeping the cell from bursting when
there are large differences in osmotic pressure between the cytoplasm and the environment.
Cytoplasmic membrane: a layer of phospholipids and proteins, called the cytoplasmic membrane encloses the
interior of the bacterium regulating the flow of materials in and out of the cell. This is a structural tract bacteria
share with all the other living cells; a barrier that allows them selectively interact with their environment.
Membranes are highly organized and asymmetric having two sides each side with a different function, membranes
are also dynamic, constantly adopting to different conditions
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Cytoplasm: the cytoplasm or protoplasm of bacterial cells is where the function fro cell growth, metabolism and
replication are carried out. It is a gel-like matrix composed of water, enzymes, nutrients, wastes and gases and
contains cell structures such as ribosomes, a chromosome and plasmids.
Flagella: flagella (singular flagellum) are hair-like structures that provide a means of locomotion for those bacteria
that have them. They can be found at either or both ends of the bacterium or all over its surface. The flagella move
in a propeller-like motion to help the bacterium move towards nutrients, away from toxic chemicals, or in the case
of the photosynthetic cyanobacterium towards light.
Nucleoid: the nucleoid is a region of cytoplasm where the chromosomal DNA is located. It is not a membrane
bound nucleus, but simply an area of the cytoplasm where the strands of DNA are found. Most bacteria have a
singular, circular chromosome that is responsible for replication. Plasmids are also found in the cytoplasm.
Pili: many species of bacteria have Pili, they are small hair-like projections emerging from the outside cell surface.
These outgrowths assist the bacteria in attaching in other cells and surfaces, such as teeth, intestines and rocks.
Without pili many disease causing bacteria lose their ability to infect because they’re unable to attach to the host’s
tissue.
Ribosomes: ribosomes are microscopic ‘factories’ found in all cells, including bacteria. They translate the genetic
code from the molecular language of nuclei acid to that of amino acids- the building blocks of proteins. Proteins are
the molecules that perform all the function of cells and living organisms.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
3. CELL WALL. PEPTIDOGLYCAN. TEICHOIC ACIDS.SPECIAL COMPONENTS OF GRAM-NEGATIVE CELL WALL.
The agents affecting cytoplasmic membrane include: detergents, antimicrobials, ionophores.
Cell wall
Outermost component Teichoic acids
Gives protection One of the special components of Gram+ve
Joins in cell division bacteria
Rigid-the skeleton On the outer layer of the cell wall
Peptidoglycan Functions as a surface antigen and mediates
Also called mucin or mucopeptide adherence
Only found in bacterial cell walls They are polymers of glycerol
Has 3 parts: glycan backbone, tetrapeptide side There are: wall teichoic acid and membrane
and peptide cross bridges. teichoic acid
BACTERIA ARE CLASSIFIED INTO TWO GROUPS
GRAM(+VE) GRAM(-VE)
Thicker, multilayer of peptidoglycan Thinner single layer
Teichoic acid layer in some bacteria Outer membrane with periplasmic
SPECIAL COMPONENTS OF GRAM(-VE) CELL WALL
Lipopolysaccharide is an integral part of cell wall. It has 3 layers
Lipid A (endotoxin)
Core oligosaccharide
Outer polysaccharide (O-antigen)
O-antigen:
it is a repetitive glycan polymer within the lipopolysaccharide
the O antigen is attached to the core oligosaccharide and is the outermost domain of the LPS
The presence or absence of O chains determines whether the LPS is considered rough or smooth
Full-length O-chains would render the LPS smooth.
Absence or reduction of O-chains would make the LPS rough
Bacteria with rough LPS usually have more penetrable cell membranes to hydrophobic antibiotics
Core oligosaccharide
It is attached directly to lipid A
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
They contain sugars such as heptose and 3-Deoxy-D-manno-oct-2-ulosonic acid (also known as KDO, keto-
deoxyoctulosonate)
They may also contain non-carbohydrate components, such as phosphate, amino acids, and ethanolamine
substituents.
Lipid A
They are hydrophobic fatty acids chains that anchor the LPS into the bacterial membrane, and the rest of the LPS
projects from the cell surface
The lipid A domain is responsible for much of the toxicity of the Gram-negative bacteria
When bacterial cells are lysed by the immune system, fragments of membrane containing lipid A are realised into the
circulation, causing fever, diarrhoea and possible fatal endotoxic shock (also called septic shock)
It is a conserved component of the LPS
Periplasmic space
Contains peptidoglycan layer
Has many enzymes (hydrolytic, lytic enzymes) and virulence factor
Gram stain
Based on the different between gram(+ve) and -ve bacteria .
+ve are purple stained while -ve are stained in red
This shows different in susceptibility of +ve and -ve bacteria to antimicrobials and
4. CAPSULE AND GLYCOCALYX. FLAGELLA. PILLI. ENDOSPORES
Specialized structures outside the cell wall are:
Capsule
Flagella
Pilli
Capsule: it is a well defined gelatinous layer composed of polysaccharides (except Bacillus anthracis)
1.capsular antigens (k antigens)
2.determine serologic types (84 serotypes in S.pneumoniae)
3.used as antigens in certain vaccines.
Determinant of virulence
1.antiphagocytic action
2.promote adherence
Glycocalyx (slime layer): it is a loose amorphous extracellular mass of polysaccharides. It promotes adherence of
bacteria of various structures.
-skin
-heart valves and catheters (S.epidermidis)
-tooth enamel (S.mutans)
Flagella: it is long (3-12µm) filamentous appendages (12-30nm in diameter) and it has three parts
Filamentous composed of flagellin
Hook structure
Basal body
It also has H.antigens and moves bacteria in response to attractants and repellants (chemotaxis)
Flagellated bacteria
Monotrichous e.g Vibrocholerae
Lophotrichous e.g Bartonella bacilliformis
Amphitrichous e.g Spirillum serpens
Peritrichous e.g Escherichia coli.
Pilli: Thin hair-like appendages composed of pilin (protein)
Shorter and straighter than flagella
Found mainly in gram-negative bacteria but in a small number of gram(+); There are 2 types:
COMMON PILI SEX PILI
-short - long
-abundant -small number (1-6)
-adhesions -participate in conjugation
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
-participate in colonization
Spores (Endospores)
Spore formation(sporulation) occurs when nutrients are depleted
Can survive in dormant state for many years
Sporulation is not a means of reproduction.
Only two medically important genera from endospores
-genus Bacillus and –genus Clostridium
Main components of endospores
Core
Spore wall
Cortex
Thick keratin-like coat
Sporulation Spore maturation
Formation of axial chromatin filament Liberation of endospores
Fore spore septum formation
Spore protoplast formation Medical importance of spores
Cortex formation Special sterilizing methods
Spore coat formation Heat resistant
5. Classification of bacteria. Taxonomy. Approaches to taxonomy. Nomenclature.
Taxonomy: the science of classification
Classification: the arrangement of organisms into taxonomic groups on the basis of similarities
Identification: process of determining which taxonomic group an organism belongs to
Nomenclature: naming an organism by international rules according to its characteristics
Formal taxonomic ranks:
1. Kingdom 5. Family 8. Acronym: King Phillip came
2. Division/ Phylum 6. Genus over for good spaghetti
3. Class 7. Species
4. Order
Bacterial species: a basic taxonomic group
They are a group of organisms with a high degree of similarities in their phenotypic and genotypic characteristics
Bacterial stain: a single isolate of one species from a specimen
The species can be sub divided into:
Biotypes: on the basis of biochemical properties
Serotypes: on the basis of antigenic features
Phage types: on the basis of susceptibility of bacteriophages
Bergey's Manual of Determinative Bacteriology involves: 1) Classification of known bacteria. 2) Key's for their
identification
Approaches to taxonomy:
Numerical Taxonomy
It is based on computerised numerical comparisons of many characteristics (50-200):
Morphological Biochemical
Cultural Susceptibility of antibiotics
Steps:
1. Coefficient of similarity (%) between the compared strains is calculated
2. Dendrogram (similarity matrix) is constructed. It jois individual strains into groups on the basis of their similarity %
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Phylogenic Taxonomy
It is based on the determination of DNA relatedness between a given strain and every known species using:
1. Genome size: in true bacteria it is from 1x10 9 to 8 x109 (Mr)
2. Guanine and cytosine content: in bacterial DNA G+C is 25-75% (specific for each species)
3. DNA relatedness under conditions optimal for DNA re-association: determined by re-association of ssDNA from 2
different strains to form dsDNA; these are specific temperature dependant reactions. The optimal re-association
temperature for DNA is ~25-30°C; below which denaturation occurs.
4. Thermal stability of related DNA sequences: each 1% of unpaired nucleotide bases in a dsDNA sequence causes a 1%
decrease in thermal stability.
5. DNA relatedness under supra-optimal conditions for DNA re-association: in such conditions only very closely related
DNA sequences ca re-associate.
Polyphasic Taxonomy
1. Phenotype grouping of strains by biochemical and antigenic reactions
2. Testing of phenotyping groups for DNA relatedness
3. Re-examination of biochemical characteristics of the "DNA relatedness" groups
Nomencalture:
Scientifically, the naming of bacteria species has two words:
Name of genus (capital letter)
Name of species (simple letter)
Characteristics Genus Representative Disease
b. Spore forming rods
1. Aerobic Bacillus Anthrax
2. Anaerobic Clostridium Tetanus, gas gangrenes, botulism
c. Non-Spore forming rods
1. Non-filamentous Corynebacterium Listeria Diptheria, Meningitis
2. Filamentous Actinomyces, Nocardia Actinomycosis, Nocardiosis
A. Free living (extracellular bacteria)
1. Gram (+) Streptococcus Pneumonia, pharyngitis, cellulitis, abscesses of skin &
u.cocci Staphylococcus other organs
2. Gram (-)
a. Cocci Neisseria Gonorrhea, meningitis
b. Rods
1) Facultative anaerobes
a) Straight
i) Respiratory organisms Haemophillus Meningitis
Bordatella Whopping cough
Legionella Pneumonia
ii) Zoonotic organisms Brucella Brucellosis
Francisella Tularemia
Yersinia Cellulitis, plague
iii) Enteric & related organisms Escheria UTIs, diarrhoea
Enterobacter UTIs
Serratia UTIs
Klebsiella Pneumonia
Salmonella Enterocolitis, typhoid feveer
Shigella Enterocolitis
Proteus UTIs
Campylobacter vibria Enterocolitis cholera
b) Curved
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
1) Aerobic Pseudomonas Pneumonia, UTIs
2) Anaerobic Bacteriodes Peritonitis
3) Acid-fast Mycobacterium Tuberculosis , leprosy
B. Non-free living (obligate intracellular Rickettsia Rochy mountains, spotted fever, typhus, Q fever.
parasites) Urethritis, trachonoma, psittacosis
Chlamydia
I. Flexible, thin wall cells (spirochetes) Treponoma Syphilis
Borellia Lyme disease
Leptospira Leptospirosis
II. Wall-less cells Mycoplasma Pneumonia
6. Classification of medically important bacteria
7. The growth of microorganisms.
One parent cell divides to form two progeny cells No. Of cells 1 2 4 8 16
0 1 2 3
Eukaryotic cells reproduce by mitosis, whereas bacteria Exponential 2 2 2 2 24
reproduce by binary fission.
Bacteria undergo exponential growth (logarithmic growth)
Example:
1. E.coli organism 1000 progeny cells in ~3 minutes 1x106 cells in ~7 hours
Generation time: time internal between 2 cell divisions
The growth cycle of bacteria has 4 major phases (if a small number of bacteria are inoculated into a liquid nutrient
medium and the bacteria are counted in frequent intervals, typical phases of the standard growth curve can be shown):
1. Lag Phase (a): vigorous metabolic activity occurs but cells do not divide. Lasts from a few minutes up to several hours
2. Log (logarithmic) phase/ exponential phase (b): when rapid cell division occurs. Β-Lactam drugs (e.g.: penicillin) act in
phase 2 because these drugs are effective when the cells are making peptidoglycan.
3. Stationary phase (c): occurs when nutrient depletion or toxic products
cause growth to slow until the number of cells produced balances
the number of cells that die, resulting in a steady state.
4. Death phase (d): marked in the decline in the number of viable
bacteria.
Aerobic & Anaerobic growth:
Obigate aerobes: they require oxygen to grow as their ATP
generating system is oxygen dependent, oxygen is the hydrogen acceptor
(e.g.: M.tuberculosis)
Facultative anaerobes: they utilize oxygen if it is available, to generate energy by respiration. However they can also use
the fermentation pathway to synthesise ATP in the absence of sufficient oxygen. (e.g.: E.coli)
Obligate anaerobes: cannot grow in the presence of oxygen as they lack either superoxide dismutase or catalase or both.
Their response in exposure to oxygen varies, some are killed slowly, some immediately. (e.g.: Clostridium tetani)
Fermentation of Sugars:
It is the breakdown of a sugar (e.g.: glucose/ maltose) to pyruvic acid and then, usually, to lactic acid.
Sugar (specifically a monosaccharide) Pyruvic acid lactic acid
If oxygen is present: pyruvate enters Krebs cycle and is eventually metabolised to CO 2 and H2O.
The Krebs Cycle generates a lot more ATP than the glycolitic cycle, hence why facultative bacteria grow faster in the
presence of oxygen.
Facultative and anaerobic bacteria ferment but aerobes do not.
Iron metabolism:
Iron, in the form of ferric ion (Fe3+) is required for the growth of bacteria as it is an essential component of cytochromes
and other enzymes.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
To obtain this iron, bacteria produce iron binding compounds called siderophores.
Siderophores, like enterobactin produced by E.coli, are secreted by bacteria capture iron by chelating it then
attach to specific receptors on the bacterial surface and are actively transported into the cell where the iron becomes
available for use.
8. BACTERIAL METABOLISM. HETEROTROPHIC BACTERIA. GLUCOSE DISSIMILATION PATHWAYS. RESPIRATION.
FERMENTATION.
Metabolism: all the biochemical reactions that occur in a cell organism. There are two types:
Dissimilation reactions: substrate molecules are broken down, energy is generated.
Assimilation: synthesis of cell components
Physiologic groups of bacteria
Heterotrophic
Autotrophic
Phototrophic
HETEROTROPHIC BACTERIA
Include all pathogenic bacteria
Obtain energy from oxidation compounds include:
Carbohydrates
Lipids
Proteins
Metabolism: biologic oxidation of organic compounds. Result of the biologic oxidation of organic
compounds. Result of the biologic oxidation.
Synthesis of ATP
Generation of precursor molecules or biosynthesis reactions.
GLUCOSE DISSIMILATION
Complete oxidation of glucose occurs by:
Glycolytic pathway
Krebs cycle
Series of membrane-bound electron transport oxidations coupled to oxidative phosphorylation. Unlike
eukaryotes, in bacteria glucose oxidation may occur by more than one pathway.
MAJOR GLUCOSE DISSIMILATION PATHWAYS IN BACTERIA.
Glycolytic pathway: obligate anaerobes, facultative anaerobes
Enter-Doudorrott pathway: obligate aerobes
Oxidative- pentose phosphate pathway
#pyruvate is the terminal product from glucose dissimilation in the glycolytic pathway.
KREB’S CYCLE
It functions similarly in bacteria and eukaryotic cells.
Major differences are found among different bacteria
The glyoxolate cycle is a modification of the kreb’s cycle
Acetyl-scoA is generated from the oxidation of fatty acids
Found in bacteria and plants but not in animal cells.
ELECTRON TRANSPORT AND OXIDATIVE PHOSPHORYLATION
Final stage of respiration
Series of oxidative-reduction transfer reactions.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
The enzymes involved in the processes reside on the cytoplasmic membrane.
ELECTRON TRANSPORT CHAINS
Show some differences compared to eukaryotic ones.
Include flavins, non-heme iron compounds and multiple cytochrome oxidases.
Finale e- transfer reaction occurs between a cytochrome oxidase and o 2.
RESPIRATION
Cellular respiration is a complex process in which nutrients such as glucose carbon dioxide are generated.to get
energy from molecules such as sugars, bacteria must use fermentation or cellular respiration.
There are three types of respiration:
Aerobic
Anaerobic
Facultative anaerobe
1.) Aerobic respiration: This is the respiration in the presence of oxygen. Sugars are broken down in the presence
of oxygen to produce carbon dioxide, water and energy. Without oxygen microorganisms are unable to produce
energy and quickly die. Most unicellular organisms and many microorganisms produce their energy using
aerobic respiration.
2.) Aerobic respiration: They do not need oxygen for their respiration, they perform anaerobic respiration
sometimes known as fermentation.
Unique model of respiration
Terminal e- acceptor is a specific component other than o 2
Specific compounds have to be added to the medium. No 3- (nitrate), No(nitrous oxide), So4- , H2. Nitrate
producing anaerobic bacteria use No3- ion as a terminal acceptor.
3.) Facultative anaerobes: They can perform both anaerobic and aerobic respiration depending in their oxygen
content. If they have sufficient oxygen levels then they will perform aerobic respiration however, in the absence
of oxygen they can switch over to anaerobic respiration.
FERMENTATION
Fermentation is a metabolic process that consumes energy or sugar in the absence of oxygen. The products are
organic compounds (acids), gases or alcohol. It occurs in yeast and bacteria.
The terminal electrons acceptors are simple organic components:
Incomplete biologic-oxidation process
Formed from anaerobic dissimilation of glucose
Production of organic end products
Secreted into the medium as alcoholic acid
Generation of energy.
Glucose dissimilation
↓
Glycolytic pathway
↓
Pyruvate, acetaldehyde, acetyl-coA
↓
Reduction by NAOH + H+
↓
Ethanol
↓
Excretion of cells.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
9. Aerobic & Anaerobic bacteria. Biosynthetic pathways. Synthesis of peptidoglycan.
There are 3 groups of bacteria on the basis of their tolerance to oxygen:
1. Obligate Aerobes
2. Facultative Anaerobes
3. Obligate Anaerobes
Obligate Aerobes – requires oxygen as a terminal acceptor of e - (eg mycobacterium tuberculosis)
Facultative Anaerobes :
Grows in presence or absence of O2 .
Generate energy by respiration in the presence of O2.
Use fermentation pathways in the absence of O 2.
The above 2 points are all enteric bacteria (bacteria of the intestines aka gut flora).
Obligate Anaerobes:
Cannot grow in the presence of O2 (lack of either superoxide dismutase or/& catalase).
They have variations in their response to O2:
Aerotolerant anaerobes – use fermentation to produce ATP. (eg Bacteroide fragilis)
Strict Anaerobes (eg clostridia tetani – tetanus)
Obligate anaerobes: members worth knowing ABC:
Actinomyces
Bacteroides
Clostridium
Microaerophilic organisms grow best at low O2 concentrations. Eg camylobacteria jejini.
They need O2 because they cannot ferment or respire anaerobically; however they are poisoned by high
concentrations of O2.
Most bacteria are facultative anaerobes ie grow in the presence/absence of O 2. (eg ALL enteric bacteria).
Biosynthetic pathways:
Biosynthesis is a multi-step, enzyme-catalyzed process where substrates are converted into more complex
products in living organisms.
Synthesis of peptidoglycan: peptidoglycan is a transfer for the action of many antimicrobials.
3 stages of peptidoglycan synthesis at different sites in the cell:
1st stage:
Occurs in the cytoplasm
UDP derivatives of N-acetylglucosamine & N-acetylmuramylpentapeptide are synthesised.
nd
2 stage:
Occurs on the inner surface of the cytoplasmic membrane
N-acetylmuramylpeptide is transferred from UDP to a carrier lipid
Formation of a complete nascent peptidoglycan subunit
Transfer of the subunit to the exterior surface of the cytoplasmic membrane
rd
3 stage:
Occurs on the outer surface of the cytoplasmic membrane
Polymerisation of the peptidoglycan subunits by transglycosylation
Restoration of the lipidcarrier
ranspeptidation & binding of peptidoglyycan subunits
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
10. Microbial genetics. Genetic material in bacteria. Bacterial chromosome and plasmids. Bacteriophages. Transposons.
Genetic material of bacteria: double stranded DNA.
Essential functions of genetic material:
Replication; it's semi-conservative
Expression of genetic determinants
Results in unidirectional flow o information. DNA RNA protein
Replicons: DNA molecules that replicate autonomously
Replicons of bacteria can be: Bacterial chromosomes / plasmids/ bacteriophages
Bacterial chromosomes:
Single, circular DNA molecule Transmissible Plasmids: conjugative
DNA is supercoiled Can transfer from cell to cell by conjugation
Has 5x106 base pairs Large plasmids
Codes for ~2000 proteins Contain genes for synthesis of sex pili
Length ~1.35mm Usually present in a few (1-3) copies per cell
Chromosomal replication: Distributed in equal numbers in daughter cells
Starts at a specific site called the site of origin
It proceeds bidirectionally and new replication begins before the previous is complete
Plasmids:
Extrachromosomal, circular, double stranded DNA molecules
Capable of replicating independently
They are integrated in the bacterial chromosome and exist autonomously out of the bacterial chromosome
Much smaller than bacterial chromosomes (5-100kB)
Variable number of plasmid copies per cell
Several types of plasmids can exist in one cell, they exist in both gram (+) & gram (-) bacteria
Medically important properties of pathologic bacteria encoded by plasmids:
Resistance to one or several antibiotics
Production of toxins
Synthesis of cell surface structures (pili or fimbria) Non-transmissible Plasmids: Nonconjugative
R-plasmids or R-factors: are used to determine Cannot transfer from cell to cell resistance
to antibiotics Small plasmids
Toxins encoded by plasmids: Don't have transfer genes
Heat labile and heat stable enterotoxins of E.coli Usually present in many copies (10-60) per cell
Exfoliative toxin of staphylococcus aureus Distributed randomly in daughter cells
Tetanus toxin of clostridium tetani
Bacteriophages: Infectious agents that replicate in bacteria
Structure:
Internal core: contains either DNA/ RNA (ds DNA, ssDNA, ssRNA)
Protective protein coat (capsid): Composed of protein subunits called capsomers
3 morphological types of phages:
Icosahedral phages: 20 walls, each wall is an equilateral triangle
Filamentous phages: Filamentous structure
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Complex phages: head structure, containing the phage nucleic acid; has a tail, that serves as a cell attachment organ and
as a tube via which phage nucleic acid can pass.
Large phage tail: has a hollow core, sheath structure that can contract; multiple tail fibers that recognise specific binding
sites
Bacteriophages on the basis of their propagation can be: Virulent or Temperate
Virulent:
Lytic phages
Always lyse their host
Temperate:
Lysogenic phages
Can exist in dormant state in the bacterial wall
Can undergo a lytic cycle:
1. Adsorption: of phage particle to specific receptors
2. Penetration: of a phage particle; capsid remains at cell surface and phage nucleic acid enters cell
3. Eclipse period: Phage DNA/RNA is replicated to produce many copies; phage proteins are produced
4. Assembly phage: progeny particles in the cytoplasm of bacterial cell; packing of phage nucleic acid into phage
capsid
5. Release : of phage progeny; lysis of infected bacterial cell and average number of phage particles produces by each
infected cell ranges between 50 and several 100
Infection with temperate phages: by lysogeny or the lytic cycle.
Lysogeny: Latent viral infections in which the phage genome exists as a prophage, 2 forms of prophages:
Integrated in bacterial chromosome and replicate as a part of the bacterial chromosome
Remains physically independent from the bacterial chromosome and replicates as extrachromosomal plasmid
Lysogenic bacteria: are bacteria carrying prophages
Genes needed for lytic phage cycle are NOT expressed
Lytic phage cycles occur: 1) spontaneously or 2) after treatment with agents that damage DNA
Phage conversion/ Lysogenic conversion:
Expression of phage genes encoding important bacterial characteristics
Bacterial virulence factor encoding:
By temperate phage genome:
Production of diptheria toxin by corynebacterium diptheriae
Production of erythrogenic toxin by streptococcus pyrogenes
Production of botulism toxin by clostridium botolinum
Production of shiga-like-toxins by E.coli
Phage typing:
Testing of strains of a particular bacterial species for susceptibility to specific bacteriophages
Pattern of susceptibility to the set of phages shows possible relatedness between different clinical isolates
Useful for epidemiologic purposes
Transposons (jumping genes): Small pieces of DNA with the unusual ability to move either:
From one site of one DNA molecule (chromosome/plasmid) to another site of the same molecule OR
Between DNAs of the chromosome, plasmids & bacteriophages
Transposons can encode the production of:
Drug resistant enzymes
Toxins
Metabolic enzymes
They can cause: mutation in the gene they insert into and change the expression of nearby genes
They're not capable of independent replication; they replicate as part of recipient's DNA
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
More than one transposon can be located in a DNA molecule
nsertion sequences: type transposons have fewer bases- encode only function of their transpostion
11. Bacterial mutations. Transfer of DNA between bacterial cells. Conjugations.
Mutation= the change in the base sequence of DNA. Mutations may be due to:
1. Base substitution
2. Insertion or deletion of one or more bases
3. Integration of transposons or insertion sequences
1. Base substitution :
- one base is inserted in the place of another
- Occurs at the same time of DNA replication
- May be due to error or DNA polymerase
- May be due to error of hydrogen bonding
Result of the base substitution:
- Generation of a codon for another
- Generation of a terminal codon; leads to protein synthesis stop (nonsense).
2. Insertion or deletion of one or more bases:
- Changes the reading frame
- Incorporation of the wrong amino acid
- Production of an inactive protein
3. Integration of Transposons/insertion sequences :
- Changes in the gene in which they insert
- Changes in the adjacent genes
Mutations can be spontaneous or induced.
Spontaneous – occur spontaneously with low rate (10 -2 – 10-10 ) for different genes
Induced - occurs under the action of mutagenic agents (chemical & physical agents that cause increase of
mutation rates).
Chemical mutagenic agents:
- Bind to the exiting DNA bases & change the reading frame (eg benzpyrene in tobacco
smoke)
- Base analogues that can insert in the place of a normal base (eg the antiviral drug
iodeoxyuridine)
- Alter an existing base so that it forms a H bond with a wrong base (eg nitrous oxide &
alkylating agents)
Physical mutagenic agents:
- X-rays
- UV lights
Conditional lethal mutations:
- Expresses only under certain conditions
- They may be used as vaccines
Temperature-sensitive mutant of influenza virus:
- Can’t grow at 37C therefore can’t infect the lungs
- Can grow at 32C in the nose therefore can induce immune response
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
- Experimental influenza vaccines (new vaccines are needed each year)
Transfer of DNA between bacterial cells
Transfer of DNA:
- Only relatively small fragments of DNA are transferred
- Transferred donor DNA; can be integrated into the recipient’s DNA &/or can be
established as independent replicon
The most important consequence of the transfer of DNA between bacteria is the spread of genes encoding
resistance to antibiotics.
Basic mechanisms for transfer or DNA between bacterial cells:
1. Conjugation
2. Transduction
3. Transformation
1. Conjugation – process of transfer of DNA from the donor to the recipient cell by direct contact between
both cells.
Donor (F+) cell – possess a specific F- plasmid (as fertility factor)
- Encodes the synthesis of proteins for forming the sex pilus
- Possesses sex pilli/conjugation tubes
- Function as a donor
Recipient (F- ) cell – does not possess F- plasmid
- Does not possess pili
- Functions as a recipient
Stages of conjugation:
(I) Attachment of the sex pilus of F+ donor cell to the specific receptor on the surface of F - receptor cell.
(II) Formation of cytoplasmic bridges between both cells
(III) Enzymatic cleavage of one strand of the F - factor DNA by endonuclease
(IV) Transfer of one strand of the F- factor DNA across the conjugate bridge into the recipient cell
(V) Synthesis of the complementary strands to form a double stranded F - factor in both donor &
recipient cells
Conversion of the F- recipient cell into F+ donor cell:
High frequency of recombination cells (HFr) = F – donors (HFr) in which F- factor (episomes) is integrated into the
bacterial chromosome.
HFr cells using the conjugation the F – plasmid & parts of the bacterial chromosome are transferred:
- A piece of the F-factor
- Bacterial chromosome
- The remainder of the F-factor
Around 100mins for complete transfer of the bacterial chromosome
ransferred DNA can recombine with the recipient’s DNA.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
12. TRANSDUCTION.TRANSFORMATION
TRANSDUCTION
Transfer of bacterial DNA from one bacterium to another by the bacteriophages.
Lytic phage cycle in lysogenic bacteria occurs under the action of chemicals, e.g UV-rays and other factors.
The lytic cycle in lysogenic bacteria.
Fragmentation of bacterial DNA
↓
A packing error during assembling of a phage particle.
↓
In cooperation of a segment of bacterial DNA into the phage capsid (rate ⅹ10-3 )
↓
Conversion of phage into a transducing particle
↓
Capable of injecting bacterial DNA into another bacterium.
There are two types of transduction
Generalized transduction
Specialized transduction
GENERALIZED TRANSDUCTION
Allows genes to be transferred from one bacterial cell to another. In this case a virus accidentally transfers the
genes. Just like there are viruses that infect animal cells, there are viruses that infect plant cells and also
bacteria. A bacterial virus is called a Bacteriophage (or just Phage). Understanding this process requires a bit of
background on how viruses work. Viruses cannot replicate on their own. They infect a host cell and take over the
replicating machinery of the cell to make baby viruses. Two things are produced, genetic information is
duplicated and protein parts needed for the shell of the virus are manufactured. Once the viral DNA replication
process is finished, the parts of the virus are assembled and the virus particles are released. They then go on to
infect other cells.
This may occur in two main ways
Recombination
Headful packaging- If the virus replicates using 'headful packaging', it attempts to fill the
nucleocapsid with genetic material. If the viral genome results in spare capacity, viral packaging
mechanisms may incorporate bacterial genetic material into the new virion.
SPECIALIZED TRANSDUCTON
Specialized transduction is the process by which a restricted set of bacterial genes is transferred to another
bacterium. When a phage genome is introduced in the bacterial cell, it becomes integrated with bacterial
chromosome as prophage
(A). Upon induction the DNA becomes free containing a small segment (about 5 to 10%) of bacterial
chromosome
(B). It multiplies and disintegrates the bacterial chromosome
(C). After assembly of phage DNA plus bacterial chromosome, the bacteriophage is released from the bacterial
host
(D) Usually this phage is defective and lacks some part of its attachment site. When this defective phage infects a
bacterium it introduces its DNA containing a piece of bacterial chromosome
(E). The defective phage cannot reproduce without the assistance of helper phage. The genes of the phage can
insert with homologous DNA of the infected bacterium
(F). Sometimes crossing over occurs between the homologous gene loci of the bacterial chromosome and the
donor DNA attached with phage genome
(G) resulting in integration of the donor DNA with the recipient DNA.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
TRANFORMMATION
Transfer of DNA pieces of DNA from one bacterium to another (only small DNA fragments are transferred). It can
occur by
Nature
In lab
Nature
Occurs in dying cells
↓
Fragmentation and release of DNA
↓
A small fragment of DNA may be taken up by live recipients
↓
It is a rate phenomenon and occurs only in certain gram(-) and gram(+) species.
LAB
Extraction of DNA from a given bacteria cell
↓
Introduction of DNA in recipient cells from the different species.
↓
Many bacterial species are not capable of natural transformation.
. This can be artificially induced to accept DNA (genetic engineering )
Competence: This is the ability of bacteria to take up extracellular DNA and to become transformed.
Gram(-): possess a competence factor (small protein) it induces the states of competence
Gram(+): don’t have a competence factor Ca 2+ and Mg2+ can artificially induce the state of
competence.
STAGES OF TRANSFORMATION
Binding of transforming DNA specific receptors of the recipient cell.
Entry of transforming DNA into the recipient cell
Gram(+): SS DNA fragment enters
Gram(-): ds DNA fragment enters
Incoorperation of transforming DNA into the recipients cell genome
Only one strand of transforming DNA is incoorperated
Formation of heterodiplex
The other strand of the transmitting DNA is destroyed.
FATE OF TRANSFERRED DNA (REGARDLESS OF THE MEANS BY WHICH IT IS TRANSFERRED)
In most cases the transferred DNA is recognised as foreign and is digested by the host’s endonucleases.
It may be incoorperated into the recipients cell’s genome by means of recombination
It may exist as autonomously within the recipient’s cell as a plasmid or a defective phage.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
13. Pathogenesis of bacterial infections. Virulence factors of bacteria; adherence and colonization factors; invasion factors;
factors for escaping host defenses; toxin production
A microorganism is a pathogen if it is capable of causing disease
Opportunistic pathogen: microorganisms that rarely, if ever, cause disease in immunocompetent people, but cause
serious infection in immunocompromised patients they are usually part of normal flora
Virulence is a quantitative measure of pathogenicity and is measured by the number of organisms required to cause
disease;
The infectious dose of an organism required to cause disease varies greatly among the pathogenic bacteria (e.g.: both
Shigella and Salmonella cause diarrohea by infecting GIt but infectious dose for Shigella is less than 100 organisms and for
Salmonella is ~10000 organisms)
The infectious dose depends primarily on the microorganisms virulence factor (whether the pili will allow them to
adhere well to mucus membranes, whether they produce exotoxins or endotoxins, whether they posses a capsule to protect
them from phagocytosis and whether they can survuve various non specific host defenses like gastric acid)
Virulence factors are molecules produced by microorganisms (bacteria, virus, fungi, protozoa) and help:
colonization of a niche in the host (this includes attachment to cells)
immunoevasion, evasion of the host's immune response
immunosuppression, inhibition of the host's immune response
entry into and exit out of cells (if the pathogen is an intracellular one)
obtain nutrition from the host
Stages of pathogenesis:
1. Transmission from an external source into the portal of entry
2. Evasion of primary host defences such as skin or gastric acid
3. Adherence to mucous membranes, usually by bacterial pili
4. Colonisation by growth of the bacteria at the site of adherence
5. Disease symptoms caused by toxin production or invasion accompanied by inflammation
6. Host responses, not specific and non specific, during steps 3, 4, and 5.
7. Progression or resolution of the disease.
Determinants of bacterial pathogenesis:
Transmission:
Interrupting the chain of transmission is an excellent way to prevent infectious diseases
Although some infections are caused by members of normal flora, most are acquired by transmission from external
sources
Pathogens exit infected patients mostly from the respiratory and gastrointestinal tracts; hence why transmission to the
new host usually occurs via airborne respiratory droplets or faecal contamination of food and water
Organisms can also be transmitted by sexual contact, urine, skin contact, blood transfusions, contaminated needles or
biting insects
Organisms can also be transmitted from mother to child by vertical transmission, there are 3 modes:
Across the placenta
Within the birth canal during birth
Via breastmilk
Adherence to cell surfaces
Certain bacteria have specialized structures (e.g.: pili) pr produce substances (e.g.: capsules) that allow them to adhere
to surfaces of human cells, which enhances their ability to cause disease
Organisms without the adherence mechanisms are usually non pathogenic
After the bacteria attach they often produce a protective matrix called a biofilm (made of various polysaccharides and
proteins)
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Invasion, Inflammation & Intracellular survival
The main mechanisms by which bacteria cause disease:
1. Invasion of tissue by inflammation
2. Toxin production
3. Immunopathogenesis
Several enzymes secreted by invasive bacteria play a role in pathogenesis, the prominent ones are:
Collagenase & Hyaluronidase: degrade collagen and hyaluronic acid; alllowing bacteria to spread through subcutaneous
tissue
Coagulase: accelerates formation of a fibrin clot from its precursor, fibrinogen. The clot may protect the bacteria from
phagocytosis by walling off the infected area and by area and by coating organisms with a fibrin layer.
Immunoglobulin A (IgA) protease: degrades IgA, letting the organisms adhere to the mucous membrane and is produced
chiefly by N.gonorrhoeae, H.influenzae and Str.pneumoniae
Leukocidins: destroy both neutrophilic leukocytes and macrophages
Antiphagocytic factors:
Capsule external to cell wall: (part of Str. Pneumoniae, N.meningitis) The polsaccharide capsule prevents phagocytes
from adhering to bacteria anticapsular antobodies allow more effective phagocytosis to occur, this is called
opsonisation, vaccine format.
Cell wall proteins of gram (+) cocci: (e.g.: protein A of S. Aureus) Protein binds to IgG and prevents activation of
complement.
Toxin production: another mechanism by which bacteria cause disease; main features: exotoxins and endotoxins
Immunop
athogenes
is
Sometime
s it it not
the
organism
itself that
causes the
symptoms
of the
disease
but rather
the
immune response.
E.g.: Rheumatic fever: antibodies are formed against M protein of S.pyrogenes, which cross react with joint, heart and
brain tissue. Inflammation occurs, resulting in arthiritis, carditis and chorea. These are the characteristic findings in
rheumatic fever.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
14. INFECTION. STAGES OF A TYPICAL ACUTE INFECTIOUS DISEASE. TYPES OF BACTERIAL INFECTIONS. KOCH’S
POSTULATES.
Infection: what is an infection?- an infection is the prescence of microorganisms causing damage to the body
tissues, usually in the presence of acute inflammation (pain, swelling, redness, heat and loss of function) e.g
S.aureus on intact skin does not cause an infection because it is the normal flora of the skin but if there is cut
then it can be infected by Staph.aureus.
STAGES OF TYPICAL ACUTE INFETIOUS DISEASE
Incubation period: This is the time between the entrance of the microorganism (or toxin) and
the beginning of clinical symptoms. It varies from hours to days, weeks to months
Prodrome period: Nonspecific symptoms occur (fever, malaise, loss of appetite)
Specific-illness period: Specific symptoms appear
Recovery period: Symptoms disappear and the patient returns to a healthy state
TYPES OF INFECTIONS
Exogenous: microbes from external sites
Endogenous: microbes from normal flora of the body
Localized: confined to a small area or an organ
Generalized: disseminated to many body regions
Monomicrobial: caused by one microbe
Polymicrobial(mixed): caused by two or more microbes
Primary: clinically apparent infection in body tissues
Secondary: subsequent to primary infections (bacterial pneumonia following a viral lung
infection)
Asymptomatic(inapparent): no clinical symptoms but laboratory tests are positive and
microorganisms are detected
Symptomatic: -typical : The clinical symptoms are detected and they
-atypical: -out patient are two: a.) specific
-Fuliminant b.)non-specific
-discreet symptoms
-occurs suddenly and intensely
Carrier state: presence of m.o without clinical and lab data of infection
Acute: rapid onset, brief duration (day or weeks)
Chronic: prolonged duration (months or years)
Latent: dormant
Reinfection: simultaneously infected with 2 microorganisms
Relapse: return of s disease after recovery caused by the same m.o persistent in the body
Superinfection: second infection with the same m.o superimposed or an earlier one
KOCH’S POSTULATES
Roberts Koch(1884) formulated conditions that confirm the confirm the casual role of m.o
The microbe must be present in every case of the disease
The microbe must be isolated from the diseased host and grown in pure culture
The disease must be reproduced when a pure culture is introduced into a healthy susceptible animal
The microbe must induce a specific immune response
KOCH’S POSTULATES NOW COULD BE REVISED
Some m.o could not always be grown in the lab
For some m.o there are no susceptible animal species
DNA for some viruses is integrated into the host’s genome
Some viruses can trigger the disease and then disappear.
15. Host defences. Nonspecific defences. Physical barriers. Phagocytic cells. Proteins: the complement system,
lysozyme & interferons.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Host defenses protect the body against infection and include:
Natural barriers (eg, skin, mucous membranes)
Nonspecific immune responses (eg, phagocytic cells [neutrophils, macrophages] and their products)
Specific immune responses (eg, antibodies, lymphocytes)
To defend against invaders—bacteria, viruses, and other pathogens—our bodies have these host defences in
place.
Nonspecific Defense Mechanisms
A kind of defense that is not specialized for a particular kind of invader.
It is a general defense against any kind of pathogen.
There are two levels of nonspecific defense:
1. First line of defense: physical barriers
2. Second line of defense: internal defenses
1. Physical Barriers
Skin
o A barrier on the outside of the body
o Sweat glands produce oily and acidic liquids that inhibit pathogens.
Mucous Membranes
o Barriers on the inside of the body: they line the digestive, respiratory, and genitourinary tracts.
o Secrete many kinds of fluids like: saliva, tears, nasal secretions, etc.
The secretions contain lysozyme, an enzyme that digests the cell walls of bacteria.
Mucus is a viscous fluid that can trap pathogens.
Cilia
o Small hairs lining the respiratory system that beat away from the lungs.
o Move mucus and trapped particles out of the body.
Gastric Juice
o Concentrated hydrochloric acid (HCl) and proteases that destroy pathogens in the stomach.
2. Internal Defenses
If the pathogens penetrate the skin or the mucus membranes, they have moved across the first line of
defense—the barrier.
When this happens, the body uses its second line of defense, composed of three parts:
1. Leukocytes
2. Antimicrobial proteins
3. The inflammatory response
2.1 Leukocytes
If the pathogens penetrate the skin or the mucous membranes, they have moved across the first line of
defense—the barrier.
When this happens, the body uses its second line of defense: leukocytes: white blood cells
There are many different kinds of leukocytes, which are classified into two broad categories:
o Phagocytes
o Lymphocytes
Most lymphocytes are part of specific defense mechanisms.
However, natural killer cells are part of the nonspecific internal defenses.
Phagocytes - “Cell eaters”
The most important part of the second line of defense
There are at least six different phagocytes (do not memorize):
o Basophils
o Eosinophils
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
o Neutrophils
o Mast cells
o Monocytes
o Macrophages:
“Big eaters”
The most famous phagocyte (although not the most abundant)
Moves around like an amoeba “eating” pathogens.
Natural Killer Cells (NK cells)
An example of a lymphocyte, a different kind of white blood cell from phagocytes
Can identify virus infected cells and some tumor cells (cancer cells).
Kills the cell by attacking the cell membrane, causing the cell to lyse (split open).
The photograph below shows a cancer cell surrounded by a number of natural killer cells.
2.2 Antimicrobial Proteins
Two different antimicrobial protein systems exist:
The complement system
o Composed of twenty different proteins that “complement” other defenses.
o Help activate the inflammatory response and attract phagocytes to the site of infection.
o Attach to microbes, helping phagocytes destroy them.
o Help lyse the cell membrane of microbes.
Interferons
o When cells are infected by a virus, they produce small amounts of proteins called interferons.
o These proteins increase the resistance of neighboring cells to infection by the same or other
viruses.
o They seem to do this by inhibiting viral reproduction.
16. Nonspecific defences. Skin and mucous
membranes. Inflammatory response and
phagocytosis.
Innate immunity is the nonspecific defence that exists
prior to exposure to the microbe/antigen; It includes:
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
host defences, like barriers to infectious agents (e.g.: skin, mucous membranes)
Certain cells (Natural killer cells [NK cells])
Certain proteins (complement cascade, interferons)
Processes like inflammation and phagocytosis
Skin:
It is the largest organ of the body and acts as a protective coat to ensure exogenous agents do not jeopardise the
function of vital internal organ systems. It is situates at the interface between external and internal environment of
the body.
Normal skin consists of multiple cell types – some that form the different layers and others that function as
sentinels of the immune system.
Epidermal surface: Keratinized cells and Langerhan cells
Sweat glands, sebaceous glands: low pH, washing action
The primary barrier to the entrance of microorganisms into the body is the skin.
It is covered with a layer of dead, keratinized epithelium that is too dry for bacteria in which to grow, but as these cells
are continuously sloughed off from the skin, they carry bacteria and other pathogens with them.
Additionally, sweat and other skin secretions may lower pH, contain toxic lipids, and physically wash microbes away.
Skin is colonised by a variety of microorganisms under homoeostatic conditions.
Mucous membranes: Mucous layers of GI tract, respiratory tract, reproductive tract, eyes, ears and nose:
Trap microbes and debris
Facilitate the removal of these trapped foreign bodies
In the upper respiratory tract: ciliated epithelial cells move potentially contaminated mucus up towards the mouth,
where it is swallowed into the GI tract
Ending up in the acidic environment of the stomach; most pathogens do not survive in such acidic conditions.
Inflammatory response:
The inflammatory reaction brings in phagocytic cells to the damaged area to clear cellular debris and to set the stage for
wound repair.
It brings in the cells of the innate immune system, allowing them to get rid of the sources of a possible infection and also
helps to isolate the site, limiting the spread of the pathogen.
Acute inflammation: short-term inflammatory response to an insult to the body. If the cause of the inflammation is not
resolved, however, it can lead to chronic inflammation.
Chronic inflammation: ongoing inflammation. It can be caused by foreign bodies, persistent pathogens, and
autoimmune diseases such as rheumatoid arthritis. (associated with major tissue destruction and fibrosis.)
There are 4 major parts of inflammation:
1. Tissue Injury: the released contents stimulate release of mast cell granules like histamine that encourage:
2. Vasodilation: allows increased access to blood at site
3. Increased vascular permeability: encourages entry of clotting factors first step to wound repair
4. Recruitment of phagocytes: encouraging phagocytosis
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Phagocytosis
:
Phagocytes
recognise the
pathogen
The cell
membrane of
the
phagocyte
fuses with
the
pathogen,
engulfing it;
the
phagocyte is
a phagosome
now
The phagosome fuses with a lysosome, which lysozymes; forming a phagolysosome
The lysozymes break the pathogen down and digest it; after it is digested the macrophage absorbs the antigens on the
pathogen and presents it on the surface. From there adaptive immune responses act.
17.SPECIFIC IMMUNITY. ACTIVE AND PASSIVE ACQUIRED IMMUNITY. IMMUNOGENS, ANTIGENS AND
EPITOPES. CELLULAR BASIS OF THE IMMUNE SYSTEM.
The immune system is the third line of defense against infection, it involves the production of antibodies and
generation of specialized lymphocytes against specific antigens.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
There are two major types of defense
↙ ↘
Innate or natural immunity Acquired or specific immunity
Innate or Natural or Non-specific immunity
Immunity an organism is born with
Genetically determined. Effective from birth
Present before exposure to pathogens
Nonspecific responses to pathogens
Acquired or Specific immunity
Immunity that an organism develops during lifetime
Not genetically determined
Develops after exposure to antigens (microbes, toxins or other foreign substances)
Very specific response to pathogens
May be acquired naturally or artificially
TYPES OF ACQUIRED IMMUNTIY
Naturally acquired
Active immunity
Passive immunity
Artificially acquired
Active immunity
Passive immunity
Acquired immunity: active immunity involves your bodies direct response to an unknown pathogen. This
response is the production of antibodies specific to the antigen of a particular pathogen. This type of immunity is
not immediate it takes time to have created enough antibodies to fight the pathogen, however the response
lasts for a long period of time and in some cases where antibodies remain in the body as memory cells, immunity
to the specific pathogen may be lifelong.
Passive immunity: this immune response involves antibodies obtained from outside the body, immunity to the
pathogens which these antibodies are specific to is therefore immediate, as no time is needed to create them,
however this immunity is not long term and may only last a few days.
Naturally acquired active immunity
Antigens or pathogens enter the body naturally
Person contracts disease and generates specific immune response to the antigen
Immunity may be lifelong (chickenpox) or temporary (influenza)
Naturally acquired passive immunity
Antibodies pass from mother to Fetus via placenta or breast feeding (IgG)
Develops immediately and is usually short-lived (weeks to months)
Affects all antigens to which the mother has immunity
Protection until child’s immune system develops
Artificially acquired active immunity
Involves production of antibody following exposure of specially prepared antigen
Antigens are introduced as vaccines (immunization)
Body generates an immune response slowly and is specific to the antigen for which the
immunization was given
Immunity can be lifelong (oral polio vaccine) or temporary (tetanus toxoid and Diphtheria toxoid
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Artificially acquired passive immunity
Transfer of immunity from immunised person to a non-immunized person by transferring
Abs(antibodies) or sensitised cells e.g snake antivenom injection from horses or rabbits
Immunity is immediate, but short lived (half life of 3 weeks)
Affects all antigens to which the donor has the immunity
Host immune system does not respond to antigens
Immunogens
Immunogens are substances that induce a specific immune response in other words, it is any antigen (but it is
not an antigen) that is capable of inducing humoral and or cell-mediated immune response rather than
immunological tolerance. This ability is called IMMUNOGENICITY.
Factors influencing immunogenicity
Foreignness: the immune system can discriminate between self and non-self, so foreign molecules are
immunogenic
Size: the larger the size the more immunogenic it is likely to be
Chemical composition: the more chemically complex the more immunogenic
Physical form: the more particulate the more immunogenic, than soluble ones
Degradability
ANTIGENS
Antigens are substances that react with the products of a specific immune response (antibodies are the
products). It is a molecule which can be specifically recognized and bound by an antibody. It cannot necessarily
induce an immune response on its won it has to be bound to the antigen-receptor site on an antibody to
produce a response.
Types of antigens
T-independent Antigens
The can directly stimulate the B cells to produce antibody without the requirement for T cell
help.
Polysaccharides are T-independent antigens
T-independent antigens are generally more resistant to degradation and thus they persist for
longer periods of time and continue to stimulate the immune system
T-dependent Antigens
They do not directly stimulate the production of antibodies without the help of T cells
Proteins are T-dependent antigens
EPITOPE (ANTIGENIC DTERMINANT)
This is the portion of an antigen that combines with the products of a specific immune response (antibodies).
The part of an antibody that binds to the epitope is called a PARATOPE.
Determinant recognized by B cells
Composition: antigenic determinants recognized by B cells and the antibodies secreted by B cells are
created by the
linear or sequence determinants which interact with the paratope based on their primary
structure (they are formed by a continuous sequence of amino acids of the antigen) or
conformational determinants which interact with the paratope based on the secondary, tertiary
or quaternary structure of the molecule (they are composed of discontinuous sections of the
antigen’s amino acids)
Size: the antigenic determinants are limited to approx. 4-8 sites on the antibody
Number: the antigenic determinants are limited to portions of the antigen that are accessible to
antibodies approx. 4-8
Determinants recognized by T cells
Composition: antigenic determinants recognized by T cells are created by the primary sequence of
amino acids in proteins. T cells do not recognize polysaccharide or nucleic acid antigens. This is why
polysaccharides are generally T-independent antigens are proteins are T-dependent. Free peptides
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
are not recognized by T cells, rather the peptides that are bound to molecules coded (antigen
presenting cells) for by the major histocompatibility complex(MHC)
Size: they are limited to approx. 8-15 amino acids
Number: the antigenic determinants are limited to those portions of the antigen that can bind to
MHC molecules
CELLULAR BASIS OF THE IMMUNE SYSTEM
Origin of immune cells
The lymphoid cells are the main cells responsible for immunologic stimuli
During embryonic development, blood cell precursors originate mainly in the fetal liver and yolk sac; in
postnatal life, the stem cells reside in the bone marrow
Stem cells differentiate into cells of the erythroid, myeloid, or lymphoid series
Myeloid series leads to formation of monocytes and macrophages, erythrocytes, neutrophils, basophils,
eosinophils, megakaryocytes, platelets and dendritic cells.
Lymphoid series evolve into two main lymphocyte cells: T cells and B cells
Stem cells in the bone marrow (or fetal liver) are the precursors of both T and B lymphocytes
Stem cells differentiate into T cells in the thymus, whereas they differentiate into B cells in the bone
marrow.
T CELLS
T cell development occurs in the thymus
Within the thymus, T cells become either CD4-positive (helper) cells or CD8-positive (cytotoxic) cells.
In the cortex of thymus within the cortical epithelium T-cells progenitors differentiate under the
influence of thymic hormones into T-cell sub population
All T-cells have CD-3 receptor on their surface (CD-3 is a complex of 5 trans-membranous proteins
which takes information from the outside to the inside of the cell
The process of T lymphocyte maturation begins with the migration of T-cell recursors from the bone-
marrow cortical regions of the thymus
The earliest recognizable thymocyte committed to the T cell lineage is the pro-T cell
As the thymocytes process from the cortex to medulla they become mature, characterized by the
expression of TcR and CD3
The most mature cells leave the thymus and enter the peripheral circulation, forming a repertoire of
T-cells able to respond to foreign antigens
B CELLS
B cells are generated from the common lymphoid progenitors, which are originated from the
differentiation of the haematopoietic stem cells in the bone marrow.
The yolk sac and fetal liver are the sites in the body where these cells are generated and developed
during early development
In the bone marrow in early stages, the B cell precursors (pre-pro B cells) must interact physically with
the stromal cells in order for proliferation and maturation to occur
Later stages late pro-B cells need the growth factors produced by stromal cells ‘interleukin-7’
The earliest identifiable stage of B cell differentiation is the pre-pro B cell. In this stage the process of Ig
gene rearrangement begins.
The first rearrangement entails the joining of the D segment to the J segment of the Ig heavy chain gene
(IgH)
Subsequent rearrangements bring the v region to the DJ portion. After this surrogate light chains can
combine with the µ heavy chain protein in pro- and pre-B cells forming a structure knows as the pre-B
cell receptor
The newly formed B cell displays IgM on the cell surface, these cells are still immature
The immature cells are removed by negative selection and those that are not removed by negative
selection leave the bone marrow and migrate to peripheral or secondary lymphoid tissues such as the
spleen and lymph nodes
Here further maturation takes place and the newly formed B cells express IgD in addition to IgM on the
cell surface
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
The mature cells are now fully responsive to antigens and interaction with T cells.
18. Antibodies. Humoral Immunity.
Antibody-Mediated (Humoral) Immunity (AMI)
On exposure to antigenic determinants in lymphatic organs, B-lymphocytes are activated and differentiated to form plasma
cells. Plasma cells are specialized, differentiated cells that synthesize and secrete antibodies specific for an antigen. Other
activated B-lymphocytes form memory cells. These cells can be activated later to differentiate to plasma cells for rapid
antibody production. This antibody production will occur on future re-entry of the antigen to the body and is the basis of long-
term immunity.
The products of plasma cells are antibodies (aka immunoglobulins)
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
An antibody is a specialized protein substance produced by the host cells in response to an antigen in the host's tissues.
Antibodies are capable of reacting specifically with the antigen that provoked their production. They circulate in the blood and
are associated with the gamma globulin fraction of the plasma.
Structure of antibodies.
Structurally, the antibodies (immunoglobulins) are composed of four protein chains arranged in a distinctive pattern. Each
molecule has two long chains of heavy molecular weight protein (H chains) and two short chains of light molecular weight
protein (L chains). The chains are linked by sulfur bonds.
At the outer end of each arm of the antibody molecule, a specific amino acid sequence exists. This is where the antibody
molecule reacts with the antigenic determinant that provoked its production. The combining site is known as the Fab
region. The most common antibody molecules have two Fab regions and are said to be bivalent (having two combining sites).
The remaining portion of the antibody molecule is called the Fc region because it can be crystallized. Its amino acid content is
relatively constant and characteristic for its class. This portion of the molecule activates the complement system and
encourages phagocytosis.
When the antibody molecule reacts with the antigen, the two surfaces fit together like the pieces of a jigsaw puzzle. This
“recognition” is exquisitely accurate and accounts for the extreme specificity of antibody molecules.
Classes of antibodies.
Five classes of antibodies (immunoglobulins) are produced by the plasma cells. The first class, called IgM, is the major
component of the primary antibody response in adult humans and is the first antibody to appear in the immune reaction. It is
composed of five units joined by a J (joining) chain. IgM cannot diffuse through cell
membranes and is found almost exclusively in the blood. Because of its many
binding sites, it is more reactive with antigens than are other kinds of antibodies. IgM is
also formed by the fetus during uterine development and is active against the A and B
factors of the red blood cells. Many antitoxins formed against bacterial toxins are
composed of JgM.
The principal antibody of the secondary immune response is IgG. This antibody is the
most common in the bloodstream and is found in many secretions, such as spinal,
synovial, lymph, and peritoneal fluids. IgG crosses the placenta and protects the fetus
and newborn. IgG therefore provides a natural type of passive immunity. IgG also forms
in the primary antibody reaction after a large amount of IgM has already formed. IgG has the “typical” antibody structure of
four protein chains.
The third class of antibody is IgA. This antibody is found in external secretions such as those at the mucosal surfaces of the
respiratory, gastrointestinal, and urogenital tracts. It is also present in the tears, saliva, bile, urine, and colostrum, and it is
transferred in the breast milk. IgA consists of two antibody units held together by a J chain and secretory component. IgA
resists infections at the body surface.
The fourth class of antibody, IgD, is found in extremely small quantities in the serum. IgD is found at the surface of B-
lymphocytes and is believed to be an antigen receptor at this location. IgM is also believed to be a receptor.
The final kind of antibody, IgE, occurs in minute concentrations in the serum and is important in hypersensitivity reactions,
especially the anaphylactic reaction. A localized reaction is called allergy.
The reaction of antibodies with antigens helps neutralize the antigen and restrict the spread of infection. Certain antibodies
react with the bacterial surface, while others react with the flagella, pili, or capsules. These reactions encourage phagocytosis.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
When antibodies react with a virus, viruses cannot attach to host cells and replicate. Antibody reaction with antigens also sets
off the complement system, which results in the formation of an attack complex along with increased phagocytosis. Antibody
reactions with toxin molecules neutralize the toxins and prevent further damage to body tissues.
Types of immunity.
Active immunity is acquired when the body produces antibodies. The immunity is usually long lasting because the immune
system has been stimulated into action. However, it takes several hours to develop. Active immunity can be natural or artificial.
Naturally acquired active immunity develops when a person produces antibodies during a bout of illness or on exposure to a
microorganism even though disease does not occur. The B-lymphocytes and plasma cells function, and this immunity occurs
during the “natural” scheme of events.
Active immunity can also occur by artificial means. Artificially acquired active immunity occurs when a person produces
antibodies after exposure to a vaccine. A vaccine consists of bacteria, viruses, or fragments of these. A vaccine may also
contain toxoids, which are chemically treated bacterial toxins. Toxoid vaccines are available against diphtheria and tetanus.
Viral vaccines are available against measles, mumps, rubella, polio, rabies, hepatitis A, hepatitis B, and yellow fever. Because
vaccine exposures do not happen in the natural scheme of events, the immunity is said to be artificial.
Passive immunity comes about when the body receives antibodies from an outside source. In passive immunity, the immune
system does not operate and the immunity is not long lasting. However, it protects instantaneously. Passive immunity can be
either natural or artificial.
Naturally aquired passive immunity develops when antibodies pass from mother to child across the placental lining. The
newborn is born with IgG, and it receives maternal IgA if it is breast-fed. These antibodies will remain for approximately six
months after birth before fading away.
For artificially acquired passive immunity, a person is given an injection of antibodies. Usually these antibodies are derived
from the blood of another individual who has produced antibodies when confronted with a certain disease. The antibody
injected is usually IgG. The antibodies will remain for a period of several days or weeks and then disappear. This type of
immunity is given to protect people who have been exposed to tetanus, diphtheria, or botulism. It is also used to protect
against certain serious viral diseases. Allergic reactions to the serum proteins (serum sickness) limit the use of the preparations.
19. Cell mediated immunity. Antibacterial responses. Innate response. Antigen-specific responses.
The constituents of the cell-mediated immune system include several cell types:
1. Macrophages, which present the antigen to T cells
2. Helper T cells, which participate in antigen recognition and in regulation (helper and suppressor) functions
3. Macrophages and helper T cells produce cytokines that activate helper and cytotoxic T cells, leading to the killing of
the pathogen or tumour cell.
4. Natural killer (NK) cells, which can inactivate pathogens
5. Cytotoxic T cells, which can kill virus-infected cells with or without antibody.
Antibacterial responses:
Innate response: is the nonspecific defence that exists prior to exposure to the microbe/antigen; It includes:
host defences, like barriers to infectious agents (e.g.: skin, mucous membranes)
Certain cells (Natural killer cells [NK cells])
Certain proteins (complement cascade, interferons)
Processes like inflammation and phagocytosis
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
The innate immune system is always general, or nonspecific, meaning anything that is identified as foreign or non-self is
a target for the innate immune response. The innate immune system is activated by the presence of antigens and their
chemical properties.
Antigen-specific response:
Antigens are anything that causes an immune response. Antigens can
be entire pathogens, like bacteria, viruses, fungi, and parasites, or smaller
proteins that pathogens express
An antigen specific response is triggered by adaptive immunity.
The adaptive immune system relies on:
B cells/ B lymphocytes:
They are made in the bone marrow and move to the lymphatic
system to circulate throughout the body
B cells have a variety of antigen specific receptors on their surface, they
are membrane bound antibodies
Each B cell has one type of antibody, specific to one type of antigen
When a b cell encounters an antigen that fits the membrane bound
antibody it rapidly divides to become a memory B cell (a.k.a: plasma cell)
T cells/ T lymphocytes:
They are made in the bone marrow and migrate to the Thymus o
mature.
The developing T cells start to express T cell receptors (TCRs) and other
receptors called CD4 & CD8 receptors
A T cell either presents CD4 receptors OR CD8 receptors
T cells can only recognise antigens that are bound to certain receptor molecules major histocompatibility complex
Class 1 (MHC I) or Class 2 (MHC II).
The MHC colecules are membrane bound surface receptors on antigen
presenting cells (e.g.: macrophages)
Once a T cell recognises an antigen it will activate other immune cells
(like B cells) to assist in the elimination of pathogens and infected host
cells.
20. HYPERSENSITIVITY. IMMEDIATE (ANAPHYLACTIC)
HYPERSENSITIVITY. CYTOTOXIC HYPERSENSITIVITY
Hypersensitivity a.k.a hypersensitivity reaction or intolerance is a set of undesirable reactions produced by the
normal immune systems, including allergies and autoimmunity. It is also when immune response results in an
exaggerated or in appropriate reactions harmful to the host.
-There are four types; based on the mechanisms involved and the time taken for the reaction:
Mediators
Type I- Immediate (allergy or anaphylactic) IgE
Type II- Cytotoxic IgG, complement, MAC
Type III- Immune complex Ag-Ab complexes, neutrophils
Type IV- Cell mediated T cells
IMMEDIATE(ANAPHYLACTIC) HYPERSENSITIVITY
It is commonly called allergy
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
It is mediated by IgE antibodies produced by plasma cells in response to stimulation of Th 2 cells by
antigens.
The antigens that stimulate it are called allergens (house dust, pollens, cosmetics, insects, clothing and
drugs)
Exposure may be ingested, by inhalation, injection or direct.
Type I hypersensitivity reactions can be systemic ( e.g systemic anaphylaxis) or localized to a specific
target tissue or organ (e.g allergic rhinitis, asthma).
Fast response which occurs in minutes, rather than multiple hours or days.
Anaphylaxis: This is a sever and rapid systemic allergic reaction to an allergic reaction to an allergen, causing a
constriction of the trachea, preventing breathing; anaphylactic shock, this affects many body systems due to the
release of inflammatory mediators and cytokines from mast cells and basophils.
Anaphylaxis produces different symptoms over minutes or hours
Symptoms include raised bumps on the skin(hives), itchiness, red face or skin(flushing), or swollen lips
and eyes.
Food are the most common trigger in children and young adults
Medications and insect bites and stings are more common triggers in older adults
Sequence of events I immediate hypersensitivity
First exposure to allergen
Antigen activation of TH2 cells and stimulation of IgE class switching in B cells
Production of IgE
Binding of IgE to FcԑRI receptors on mast cells
Repeat exposure to allergen
Activation of mast cell, release of mediators, these mediators are produced as a result of IgE
antibodies binding to mast cells and basophils. The mediators are histamines, prostaglandins
and leukotrienes, cytokines, a vasodilator and heparin
Clinical manifestations may be:
Local- rhinitis
Systemic- anaphylaxis e.g asthma is a form of anaphylaxis, as a combination of oedema and airway
constriction which prevents tissues from getting sufficient oxygen.
Examples of type I hypersensitivity include:
Allergic asthma
Allergic conjunctivitis
Allergic rhinitis (hay fever)
Anaphylaxis
Angio-oedema
Atopic dermatitis(eczema)
Eosinophilia
Urticaria (hives)
DIAGNOSIS AND TREATMENT OF ALLERGIES.
For assessing the presence of allergen-specific IgE antibodies, there are two different methods
Skin prick test
Allergy blood test
Other tests include
Challenge testing: when small amounts of suspected allergen are introduced to the body orally,
through inhalation, or via other routes, they are often utilized most often with medicines or
foods.
Patch testing is used to help ascertain the cause of skin contact allergy (contact dermatitis)
Treatment: treatment can be traditional (as in the avoidance of allergens) also desensitization or
hyposensitization is a treatment in which the patient is gradually vaccinated with progressively larger doses of
the allergen in question, this can either reduce the severity or eliminate hypersensitivity altogether.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
CYTOTOXIC HYPERSENSITIVITY
In this the antibodies produced by the immune response bind to antigens on the patient’s own cell surfaces, the
antigens recognized in this way may either be intrinsic(‘self’ antigen, innately part of the patient’s cells) or
extrinsic (adsorbed onto the cells during exposure to some foreign antigen, possibly as part of infection with a
pathogen). These cells are recognized by macrophages or dendritic cells, which act as antigen-presenting cells.
This causes a B cell response, wherein antibodies are produced against the foreign antigen
An example of type II hypersensitivity is the reaction to penicillin wherein the drug can bind to red blood
cells, causing them to be recognized as different; B cell proliferation will take place and antibodies to the
drug are produced. IgM and IgG antibodies bind to these antigens to form complexes that activate the
classical pathway of complement activation to eliminate cells presenting foreign antigens (which are
usually, but not in this case, pathogens)
The reaction takes hours to a day. The membrane attack complex (MAC); is typically formed on the
surface of pathogenic bacterial cells as a result of the activation of the alternative pathway and the
classical pathway of the complement system, and it is one of the effector proteins of the immune system
The membrane-attack complex (MAC) forms transmembrane channels. These channels disrupt the
phospholipid bilayer of target cells, leading to cell lysis and death.
Another form of type II hypersensitivity is called antibody-dependent cell-mediated cytotoxicity (ADCC).
Here cells exhibiting the foreign antigen are tagged with antibodies (IgM or IgG). These tagged cells are
then recognised by natural killer (NK) cells and macrophages (recognised via IgG bound via the Fc region)
to the effector cell surface receptor, CD16, which in turn kills these tagged cells.
Type II reactions can affect healthy cells, and this can cause autoimmune diseases e.g haemolytic anemia and myasthenia gravis
21. Immune- complex hypersensitivity. Delayed (cell-mediated) hypersensitivity.
CHECK OSMOSIS ON YOUTUBE FOR ALL THE HYPERSENSITIVITY VIDEOS; they are quite good.
HYPERSENSITIVITY REACTIONS
Hypersensitivity refers to excessive, undesirable (damaging, discomfort-producing and sometimes fatal) reactions produced by
the normal immune system. Hypersensitivity reactions require a pre-sensitized (immune) state of the host. Hypersensitivity
reactions can be divided into four types: type I, type II, type III and type IV, based on the mechanisms involved and time taken for
the reaction. Frequently, a particular clinical condition (disease) may involve more than one type of reaction.
TYPE III HYPERSENSITIVITY
Type III hypersensitivity occurs when there is an excess of antigen, leading to small immune complexes being formed that
fix complement and are not cleared from the circulation. It involves soluble antigens that are not bound to cell surfaces (as
opposed to those in type II hypersensitivity). When these antigens bind antibodies, immune complexes of different sizes form.
Large complexes can be cleared by macrophages but macrophages have difficulty in the disposal of small immune complexes.
These immune complexes insert themselves into small blood vessels, joints, and glomeruli, causing symptoms. Unlike the free
variant, a small immune complex bound to sites of deposition (like blood vessel walls) are far more capable of interacting with
complement; these medium-sized complexes, formed in the slight excess of antigen, are viewed as being highly pathogenic.
Such depositions in tissues often induce an inflammatory response which leads to the release of tissue-damaging substances,
such as enzymes that destroy tissues locally, and interleukin-1, which, among its other effects, induces fever. The cause of
damage is as a result of the action of cleaved complement anaphylotoxins C3a and C5a, which, respectively, mediate the
induction of granule release from mast cells (from which histamine can cause urticaria), and recruitment of inflammatory cells
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
into the tissue (mainly those with lysosomal action, leading to tissue damage through frustrated phagocytosis by PMNs and
macrophages).
The reaction may be general (e.g., serum sickness) or may involve individual organs including skin (e.g., systemic lupus
erythematosus, Arthus reaction), kidneys (e.g., lupus nephritis), lungs (e.g., aspergillosis), blood vessels (e.g., polyarteritis), joints
(e.g., rheumatoid arthritis) or other organs. This reaction may be the pathogenic mechanism of diseases caused by many
microorganisms.
The reaction may take 3 - 10 hours after exposure to the antigen (as in Arthus reaction). It is mediated by soluble immune
complexes. They are mostly of the IgG class, although IgM may also be involved. The antigen may be exogenous (chronic
bacterial, viral or parasitic infections), or endogenous (non-organ specific autoimmunity: e.g., systemic lupus erythematosus,
SLE). The antigen is soluble and not attached to the organ involved. Primary components are soluble immune complexes and
complement (C3a, 4a and 5a). The damage is caused by platelets and neutrophils. The lesion contains primarily neutrophils and
deposits of immune complexes and complement. Macrophages infiltrating in later stages may be involved in the healing process.
The affinity of antibody and size of immune complexes are important in production of disease and determining the tissue
involved. Diagnosis involves examination of tissue biopsies for deposits of Ig and complement by immunofluorescence. The
immunofluorescent staining in type III hypersensitivity is granular (as opposed to linear in type II such as seen in Goodpasture's
syndrome). The presence of immune complexes in serum and depletion in the level of complement are also diagnostic.
Polyethylene glycol-mediated turbidity (nephelometry), binding of C1q and Raji cell test are utilized to detect immune
complexes. Treatment includes anti-inflammatory agents.
TYPE IV HYPERSENSITIVITY
Type 4 hypersensitivity is often called delayed type hypersensitivity as the reaction takes several days to develop. Unlike the
other types, it is not antibody-mediated but rather is a type of cell-mediated response.
CD4+ Th1 helper T cells recognize antigen in a complex with
the MHC class II major histocompatibility complex on the surface
of antigen-presenting cells. These can be macrophages that
secrete IL-12, which stimulates the proliferation of further CD4+ Th1
cells. CD4+ T cells secrete IL-2 and interferon gamma, inducing the
further release of other Th1 cytokines, thus mediating the
immune response. Activated CD8+ T cells destroy target cells on
contact, whereas activated macrophages produce hydrolytic
enzymes and, on presentation with certain
intracellular pathogens, transform into multinucleated giant
cells.
The classical example of this hypersensitivity is tuberculin
(Montoux) reaction which peaks 48 hours after the injection of antigen (PPD or old tuberculin). The lesion is characterized by
induration and erythema.
Type IV hypersensitivity is involved in the pathogenesis of many autoimmune and infectious diseases (tuberculosis, leprosy,
blastomycosis, histoplasmosis, toxoplasmosis, leishmaniasis, etc.) and granulomas due to infections and foreign antigens.
Another form of delayed hypersensitivity is contact dermatitis (poison ivy (figure 6), chemicals, heavy metals, etc.) in which the
lesions are more papular. Type IV hypersensitivity can be classified into three categories depending on the time of onset and
clinical and histological presentation (Table 3).
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Mechanisms of damage in delayed hypersensitivity include T lymphocytes and monocytes and/or macrophages. Cytotoxic T cells
(Tc) cause direct damage whereas helper T (TH1) cells secrete cytokines which activate cytotoxic T cells and recruit and activate
monocytes and macrophages, which cause the bulk of the damage (figure 4). The delayed hypersensitivity lesions mainly contain
monocytes and a few T cells.
Major lymphokines involved in delayed hypersensitivity reaction include monocyte chemotactic factor, interleukin-2, interferon-
gamma, TNF alpha/beta, etc.
Diagnostic tests in vivo include delayed cutaneous reaction (e.g. Montoux test (figure 5)) and patch test (for contact dermatitis).
In vitro tests for delayed hypersensitivity include mitogenic
response, lympho-cytotoxicity and IL-2 production.
Corticosteroids and other immunosuppressive agents are
used in treatment.
22. IMMUNOPROPHYLAXIS AND IMMUNOTHERAPY OF INFECTIOUS DISEASES
Immunoprophylaxis
Immunoprophylaxis is the protection against infectious diseases by immunization and acquired by the individual
either passively or actively.
Passive acquired immunity
Active acquired immunity
Passive acquired immunity
Ready made Ab transferred to individual giving rapid protection and short lasting immunity. There are two types:
Naturally acquired passive immunity: occurs when antibody are transferred from mother fetus (igG) or
in colostrum (igA).
Artificially acquired passive immunity: short-term immunization by injection of antibodies, for example:
Injection of antibiotic serum for treatment of diphtheria or tetanus.
Injection of gamma globulin that are not produced by the recipient’s cells, to
hypogammaglobulin children.
Active acquired immunity
Individual actively produces his own Ab. The immunity develops slowly and is long lasting due to the
development of immunological memory.
Nature active acquired immunity: the person becomes immune as a result of previous exposure to a live
pathogen.
Artificially active acquired immunity: a vaccine stimulates a primary response against the antigen
without causing symptoms of the disease
Vaccination
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
This is immunity against pathogens( viruses and bacteria) by using:
Live attenuated
Killed
Altered pathogens that stimulate the body to produce antibodies.
Vaccines work with the immune systems’s ability to recognise and destroy foreign proteins’s (antigens)
Vaccination prevents and controls such diseases such as cholera, rabies, poliomyelitis, diphtheria,
tetanus, measles and typhoid fever.
Vaccines can be:
Prophylactic: prevent the effects of a future infection by any natural or wild pathogen.
Therapeutic.
Types of vaccines
Killed vaccines ( e.g TAB vaccine against enteric fever, Salk vaccine against poliomyelitis, Semples
vaccines against rabies, d-Pertussis vaccine against whopping cough)
They do not stimulate local immunity
Short lasting
Do not stimulate cytotoxic T cell response in contrast to live attenuated vaccines
Safe, can be given to pregnant woman and an immunocompromised host.
It is heat stable
Live attenuated vaccines
Stimulate both humoral and cell mediated immunity, local and systemic
Heat stable
Living microorganisms lost its virulence factor so they do not produce diseases but immunity.
Toxoids
It is prepared by detoxifying bacterial toxins.
Bacterial exotoxins are treated by formalin to destroy toxicity and retain antigenicity e.g
diphtheria and tetanus toxoid.
Microbial products
These vaccines are prepared from bacterial products or viral components e.g:
Capsular polysaccharide vaccines
Cellular purified proteins of pertussis
Purified surface Ag of hepatitis B virus
Influenza viruses
IMMUNOTHERAPY
Immunotherapy is the treatment of an already existing disease, it is the treatment of diseases by inducing,
enhancing or suppressing an immune response. There are two types of immunotherapy
Activation: designed to amplify an immune response towards the disease
Suppression: they reduce or suppress the immune response
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
23. Antimicrobial chemotherapy. Desired properties of antimicrobials. Mechanisms of actions of antibacterial
& antifungal drugs. Inhibitors of cell wall synthesis.
Antimicrobial chemotherapy: treatment of infections/diseases by antimicrobial drugs.
Selective toxicity of antimicrobial drugs:
- Selective inhibition or killing of microorganisms without damage to the host cells
- Based on the difference between microbial & human cells
Antimicrobial drugs:
- Antibacterial agents
- Antifungal agents
- Antiviral agents
- Antiparasitic drugs
Antimicrobial drugs can either be antibiotics or antimicrobial agents.
Antibiotics: chemical substances produced by microorganisms.
Antimicrobial agents: chemical substances derived from a biological source or produced by chemical synthesis.
Antibacterial agents:
- Natural antibiotics – produced by fungi, organisms develop resistance faster
- Semisynthetic agents – chemically altered natural compounds, lower toxicity + higher effectiveness
- Synthetic agents - chemically synthesised in the lab, greater effectiveness +less toxicity
Desired antimicrobial properties of antimicrobial drugs:
- Selective toxicity
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
- Broad spectrum of activity
- Bactericidal activity
Desired pharmalogicial properties of antimicrobial drugs:
- non toxic to host
- long plasma half life
- good tissue distribution incl. CSF
- low plasma protein binding
- oral +parenteral (forms for injection) dosing forms
- to not interfere with other drugs
Antibacterial spectrum: Range of activity of an antimicrobial against bacteria:
- broad spectrum drugs – inhibit many gram (+) & many gram (-) bactera
- narrow spectrum drugs – inhibit a limited variety of bacteria
Bacteriostatic & bacteriocidal activity:
- bactericidal antibacterial drugs KILL bacteria
- bacteriostatic drugs INHIBIT bacteria:
they prevent the increase of bacterial population
Host defense mechanisms can cope with static population
4 major target sites for antibacterial drugs:
1. Cell wall
2. Ribosomes
3. Nucleic acids
4. Cell membrane
Basic mechanisms of actions of antibacterial & antifungal drugs:
- Inhibition of cell wall synthesis
- Inhibition of protein synthesis
- Inhibition of nucleic acid synthesis
- Alteration of cell membrane function
Main group of antimicrobial drugs:
A. Inhibitors of cell wall synthesis
B. Inhibitors of protein synthesis
C. Inhibitors of nucleic acid synthesis
D. Inhibitors of cell membrane function
E. Inhibitors of folate synthesis
A. Inhibitors of cell wall synthesis:
(I) Inhibitors of transpeptidation of peptidoglycan synthesis
(II) Inhibitors of other steps in peptidoglycan synthesis
(III) Inhibitors of mycobacterial cell wall synthesis
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
1. Inhibitors of transpeptidation of peptidoglycan synthesis
B lactam antibiotics:
1. Penicillins
2. Cephalosporins + Cephamycins
3. Carbapenems
4. Monobactams
5. B-lactamase inhibitors
B-lactam antibiotics – bind enzymes called PBPs (penicillin binding proteins) – activation of autolytic enzymes –
degeneration of peptidoglycan – disruption of cell wall.
24. Βeta-Lactam antibiotics.
They are a class of broad spectrum antibiotics, consisting of all antibiotic agents that contain a β-lactam ring in their
molecular structure; this includes: penicillin derivatives, cephalosporins.
Most β-lactam antibiotics work by inhibiting cell wall biosynthesis in the bacterial organisms.
Bacteria often develop resistance to β-lactam antibiotics by synthesising β-lactamase, an enyme that attacks the β-
lactam ring. To overcome this resistance β-lactam antibiotics are given with β-lactamase inhibitors like clauvulanic acid.
Medical use of β-lactam antibiotics:
They are indicated for the prevention and treatment of bacterial infections caused by susceptible organisms
As they are broad spectrum antibiotics they can be used against various gram (+) and gram (-) bacteria
Adverse effects:
Diarrhoea
Nausea
Rash
Urticaria
Superinfection (includind candidiasis)
Pain and inflammation at injection site- for parenterally administered β-lactam antibiotics
Allergy/hypersensitivity:
Occurs in ~10% of patients
Anaphylaxis occurs in 0.01% (causes itchy rash, throat/tongue swelling, shortness of breath, vomit, death)
Mechanism:
β-lactam antibiotics are bacteriocidal (substance that kills bacteria)
They act by inhibiting the peptidoglycan layer of bacterial cell walls
The petidoglycan layer is important for cell wall structural integrity, especially in gram(+) organisms, being the
outermost, primary component of the wall.
The final transpeptidation step in the synthesis of the petidoglycan is fascilitated by DD-transpeptidases, they are
penicilin binding proteins (PBPs)
When they bind to penicillin, the β-lactam amide bond is ruptured to form a covalent bond with the catalytic serine
residue at the PBPs active site. This is an irreversible reaction and inactivates the enzyme.
This prevents synthesis of the peptidoglycan cell wall and eventually kills the organisms.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Modes of resistance:
Enzymatic hydrolysis of the β-lactam ring:
If the bacterium produces the enzyme β-lactamase or penicillinase, the enzyme will hydrolyse the β-lactam ring ; making
the antibiotic ineffective
The genes for these enzymes can be inherently present in bacterial chromosomes or acquired via plasmid transfer
To overcome this resistance: the β-lactam antibiotic is administered along with a β-lactamase inhibitor
Possession of altered penicillin-binding proteins:
As a response to the use of β-lactam to control bacterial infections some bacteria have evolved PBPs with new
structures.
β-lactam antibiotics cannot bind as effectively to the new, altered PBPs and this results in the antibiotic being less
effective in disrupting the cell wall synthesis.
E.g.: MRSA (methicillin-resistant Staphylococcus Aureus) and penicillin resistanat Streptococcus pneumoniae; the
alteration in PBPs doesn't rule out treatment options.
MRSA can be treated with vancomycin
25. Inhibitors of protein synthesis.
1. Action on 30s ribosomal subunit:
i. Aminoglycosides
ii. Tetracyclines and glycyclines
2. Action on 50s ribosomal subunit:
i. Chloramphenicol
ii. Macrolides
iii. Ketolides
iv. Lincosamides
v. Oxasolidinones
vi. Streptogranins
1. Inhibitors of 30s ribosomal subunits
i. Aminoglycosides:
- Bind irreversibly to the 30s ribosomal subunit blocking the function of initiation complex
+ cause misreading mRNA.
- Bactericidal broad spectrum
- Active against Gram (-) (incl. P. Aeruginosa) + Gram (+) cocci
Disadvantages of Aminoglycosides:
- High toxicity
Nephrotoxicity (hurt the kidneys)
Ototoxicity (hurt the ears; can cause deafness or affect hearing)– cochlear + vestibular toxicity
- Poorly absorbed from the GIT & can’t be given orally
- Inactive against anaerobes – their transport into bacterial cells require oxygen.
Mechanisms of resistance to aminoglycosides:
- Enzymatic modification of the antibiotic (most common)
- Alteration of the ribosome binding site
- Decreased permeability of the bacterium to the drug.
Clinically used aminoglycosides:
- Gentamycin
- Nethimicin
- Tobramycin
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
- Streptomycin
- Amikacin
- Neomycin
Antibiotic Clinical use Comments
Gentamycin + Tobramycin Many gram (-) rod infections Most widely used
incl. P. Aeruginosa aminoglycosides
Amikacin “ “ Effective against organisms
resistant to Gen+Tob
Nethimicin “ “ Less ototoxic than Gen+Tob but
less antibacterial activity
Streptomycin Tuberculosis, Plague, Ototoxic +nephrotoxic
Tularemia, brucellosis
Neomycin Preoperative bowel Toxic to be used systemically
preparation since not absorbed
ii. Tetracyclines:
- Block tRNA binding to the 30s ribosome
- Bacteriostatic, broad spectrum drugs
- Active against:
Several gram (+) bacteria
Several gram (-) bacteria
Chlamydia spp.
Mycoplasma spp.
Ricketssia spp.
- Low toxicity
Disadvantages of tetracyclines:
- Suppression of the normal intestinal flora: development of diarrhea,
overgrowth of drug resistant bacteria + fungi
- Brown staining of teeth: results of the drug deposition in developed teeth
Mechanisms of resistance to tetracyclines:
- Efflux of the antibiotic out of the cell
- Alteration of the target site
- Enzymatic modification
- Decreased penetration
Clinically used tetracyclines:
- Tetracyclin
- Doxycyclin (most used)
- Minocyclin
Indications for used tetracyclines:
- Treatment as infections caused by:
Chlamydia spp.
Mycoplasma spp.
Rickettsia spp.
iii. Glycylcyclines:
- Semi synthetic tetracycline derivatives - bacteriostatic
- Spectrum of activity:
More active against mycoplasma spp. & Chlamydia spp.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Gram + bacteria (incl. MRSA & URE)
Gram – bacteria
Anaerobic bacteria
- Similar adverse effects as tetracyclines
- Clinically used glyclycyclines – Tigecycline
- Clinical use:
Complicated skin infections
Intra abdominal infections
Nosocomial infections
2. Inhibitors of 50s ribosomal subunit
i. Chloramphenicol group
- Block the action of the peptidyl-transferase
- Bacteriostatic agent against
Certain gram – aerobic + anaerobic bacteria
Certain gram + aerobic + anaerobic bacteria
- Bactericidal against
Haemophilus influenza
Streptococcus pneumonia
Neisseria meningitides
Clinically used drugs:
- Chloramphenicol
- Thiumphenicol
Chloramphenicol:
- Toxic drug (in some extent inhibits mitochondrial protein synthesis)
- Toxic for bone marrow
- Dose dependent reversible suppression
- A plastic anemia – not reversible & not dose dependent
Mechanisms of resistance to chloramphenicol:
- Production of drug inactivating enzymes
Indications for use of chloramphenicol:
- Drug for poor countries
- As an alternative drug for:
Bacterial meningitis caused by susceptible organisms in a penicillin allergic patient
Salmonella typhi infections
Anaerobic infections
ii. Macrolides:
- Block polypeptide elongation by reversible binding to the 23s rRNA
- Broad spectrum of activity
- Bacteriostatic against:
Certain gram + bacteria (streptococcus spp. + cornyebacterium diphtheria)
Certain gram – bacteria (campylobacteria spp, bortadella pertussis, legionella
pneumopila)
Mycoplasma spp.
Chlamydia spp.
Spirochetes
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
- Non toxic drugs
- The newer macrolides have improved pharmacological properties (erythromycin causes
nausea + vomiting).
Mechanisms of resistance:
Alteration of the target site
Production of inactivating enzymes
Clinical use – pulmonary infections caused by:
Mycoplasma spp.
Chlamydia spp.
Legionella pneumopjilia
Infections caused by campylobacter spp.
Whooping cough
As an alternative to penicillin in penicillin-allergic patients
Clinically used macrolides:
- Erythromycin
- Azithromycin
- Clarithromycin
iii. Ketolides:
- Semi synthetic derivatives of erythromycin
- Spectrum of activity – more active than macrolides against respiratory pathogens (incl.
Mycoplasma pneumonia & Chlamydia pneumonia)
- Clinically used drugs – Telithromycin
- Clinical use – treatment of community acquired respiratory tract infections
iv. Lincosamides:
- Block polypeptide elongation by reversible inhibition of peptidyltransferase
- Bacteriostatic agains:
Gram + bacteria & cocci
Gram + & Gram – anaerobic bacteria
Mechanisms of resistance:
Alteration of the ribosomal binding site
Production of inactivating enzyme
Clinically used lincosamides:
- Clindamycin
- Lincamycin
Disadvantages of clindamycin:
The most important adverse effect is development of pseudomembranous colitis
Frequently during treatment with clindamycin
Rarely during treatments with ampicillin or cephalosporins
Development of Pseudomembranous Colitis:
1. Suppression of the bowel normal flora.
2. Overgrowth of drug resistant strain of Clostridium difficile.
3. The organism secretes an exotoxin.
4. Formation of pseudo membranes in the colon.
5. Diarrhea, abdominal pain, fever.
Clinical use of lincosamides:
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Anaerobic infections
As an alternative to penicillin-allergic patients
v. Oxazolidinones:
- Block synthesis of the initiation complex
- Bacteriostatic narrow spectrum drugs
- Active against Gram + cocci:
Staphylococcus spp. (incl. MRSA)
Streptococcus spp.
Enterococcus spp. (incl. Vancomycin Res)
Disadvantages: reversible myelosuppression after prolonged use (> 2 weeks)
Clinical use of oxazolidinones:
Infections due to methicillin resistant (MRSA)
Infections due to vancomycin – resistant enterococci (VRE)
Clinically used oxazolidinones : Linezoid
vi. Streptogramins:
- Unique class of antibiotics
- Each of them is a combination of at least 2 streptogramins acting synergistically
Clinically used: Quinupristin/Dalfopristin (Synercid)
Dalfopristin:
- Causes conformational change of the 50s ribosome (facilitates binding of Qinupristin)
- Prevent peptide chain elongation
Quinupristin:
- Initiates premature release of peptide chain
Quinupristin/Dalfopristin:
- Bactericidal narrow – spectrum antibiotic
- Active against Gram + cocci:
Staphylococcus spp. (inc. MRSA)
Streptococcus spp.
Enterococcus faecium (but not E.faecalis)
Disadvantages:
Phlebitis (inflammation of vein) at the site of infusion
Arthralgia (joint pains) + myalgia (muscle pain)
Skin reactions
Clinical uses: Treatment of vancomycin-resistant enterococcus faecium infections.
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Topic 26: Inhibitors of nucleic acid synthesis
I. Inhibitors of DNA synthesis
II. Inhibitors of RNA synthesis
I. Inhibitors of DNA synthesies
1. Quinolones
2. Metronidazole
1. Quinolones:
- Inhibit bacterial DNA gyrases
- Bactericidal drugs
- Mechanisms of resistance to quinolones:
Alteration of the target enzyme
Formation of permeability barrier
- Nalidixic acid is the first agent:
Narrow spectrum of activity
Poor pharmacological properties
- New quinolones (fluoroquinolones):
Extended spectrum of activity
Improved pharmacological properties
Antibacterial activity of fluoroquinolones:
Gram + & Gram – cocci
Enterobacteriaceae
Pseudomonas aeruginosa
Mycoplasma spp. (only some drugs)
Rickettsia spp. (only some drugs)
Disadvantages of Quinolones:
Gastrointestinal disturbances
CNS symptoms (headache, slight dizziness, mild sleep disturbances)
Skin allergic reactions
Possible toxic effects on growing cartilage developments.
* DO NOT USE FLUOROQUINOLONES IN: children, pregnant women, nursing mothers.
Clinical use of fluoroquinolones:
UTIs
Systemic Gram – infections
STDs: gonococcal infections, Chlamydia trachomatis infections
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Osteomyelitis & soft tissue infections
Respiratory tract infections (RTIs)
Bacterial gastroenteritis including shigellosis
Clinically used quinolones:
Nalidixic acid
Lomefloxacin
Ciprofloxacin (basic drug)
Trovafloxacin
Levofloxacin (important against respiration)
Enoxacin
Moxifloxacin (important against respiration)
Clinafloxacin
Temafloxacin
Sparfloxacin
2. Metronidazole:
- Breaks the bacterial DNA
- Active only against anaerobic organisms
Disadvantages of metronidazole:
- Gastrointestinal disturbances
- Peripheral neuropathy
Bactericidal drug against:
- Anaerobic bacteria
- Several parasites: entamoeba histolytica, Giardia lambia, Trichomonas vaginalis
Classical use of metronidazole:
- Pseudomembranous colitis
- Trichomoniasis
- Bacterial vaginosis
- Giardiasis
- Amebiasis
II. Inhibitors of RNA synthesis – Rifamycins (Ansamycins):
- Bind to RNA polymerase & block the synthesis at mRNA
- Bactericidal broad spectrum
- Active against:
Some gram + cocci & rods
Some gram – cocci & rods
Mycobacteria
Rifamycins:
Mechanisms of resistance – modification of the target enzyme
Disadvantages:
Allergic skin reactions
Drug fever
Hepatic toxicity
Clinically used rifamycins:
Rifamycin
Rifabutin
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Clinical use of rifamycin:
Treatment of tuberculosis & other mycobacterial infections
Always in combination with other antituberculosis drugs
Prophylaxis of close contacts of meningococcal & Haemophilus influenza type B meningitis
Excreted in high conc. In saliva
Clinical use of rifabutin:
Treatment of mycobacterium cilium-intracellular complex in patients with AIDs.
27. Cell membrane inhibitors. Drugs with antibacterial and antifungal activity.
(make sure you learn Polymixins and lipopeptides)
Drugs with antibacterial activity:
Polymixins: Clinically used: Polymixin B & Polymixin E
Disrupts phospholipid structure of cell membrane
Is only active against gram(-) bacteria (including pseudomonas aeruginosa)
Disadvantages: to some extent it is toxic to human cell membranes has high nephotoxicity
Lipopeptides: Clinically used drug: daptomycin
Primarily for topical treatment of external oitis, eye infections and skin infections
Disrupts cytoplasmic membrane permeability
Is a bactericidal drug
Do not penetrate outer membrane of gram (-) bacteria
Are active against gram (+) bacteria
Penicillins (and cephalosporins):
They act by inhibiting transpeptidases, the enzyme that catalyse the final cross-linking step in the synthesis of
peptidoglycan.
Penicillin binds to a variety of receptors in the bacterial cell membrane and cell wall (PBPs); some of these PBPs are
transpeptidases. (alterations in the PBPs causes resistance)
Autolytic enzymes calles peptidoglycan hydrolases are activated in penicillin treated cells, they degrade the peptdoglycan
Penicillin treated cells die by rupture due to influx of water into high osmotic pressure interior of bacterial cell
Penicillins and cephalosporins are called β-lactam drugs due to the β-lactam ring. The most important naturally occurring
compound is benzylpenicillin (penicillin G); it is available in 3 forms:
Aqueous penicillin G: metabolises most rapidly
Procaine penicillin G: metabolised more slowly
Benzathine penicillin G: metabolises very slowly
Penicillin G is the most widely used effective antibiotic; however its disadvantages are:
Limited effectiveness against many gram (-) rods; as it cannot penetrate the outer membrane (e.g.: pseudomonas
aeroginosa, Klebsiella pneumoniae)
Hydrolysis by gastric acids (hence cannot be taken orally)
Inactivation of β-lactamases
Hypersensitivity; particularly anaphylaxis in some recipients
Cephalosporins: 6-membered ring adjactent to β-lactam ring; whereas penicillin has a 5-membered ring
First generation cephalosporins are active primarily against gram(+) cocci
2nd, 3rd, 4th generations each have increased expanded coverage against certain gram(-) rods
4th and 5th generations have coverage against gram (+) rods as well
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Monobactams: are also β-lactam drugs but structurally different from penicillin and cephalosporin
Currently the most useul monobactam is Aztreonam; it has excellent activity against many gram (-) rods (like
enterobacteriaceae, pseudomonas)
However it is inactive against gram (+) and anaerobic bacteria
It is resistant to β-lactamases
Very useful for patients with hypersensitivity to penicillin as there is no cross reactivity
Vancomycin:
It is a glycopeptide that inhibits cell wall peptidoglycan synthesis by blocking transpeptidation; however the mechanism it
uses is different to that used by β-lactam drugs
It inhibits the enzymes: transpeptidase and transglycosylase; both function in peptidoglycan synthesis
It is effective against certain gram(+) bacteria. Mostly used to treat infections caused by S.aureus strains that are
resistant to penicillin (MRSA)
Drugs with antifungal activity:
Drugs used to treat bacterial diseases have no effect on fungal diseases. E.g.: penicillin and aminoglycosides inhibit the
growth of many bacteria but do not affect the growth of fungi.
The difference is due to the presence of peptidoglycan and 70S ribosomes in bacteria, they are absent in fungi
The most effective fungal drugs: Amphotericin B and various azoles
These antifungal drugs utilize the presence of ergosterol in fungal cell membranes that is not found in bacterial/human
cell membranes. (Human cell's have cholesterol)
Polyenes:
Inhibit membrane functions by binding to ergosterol molecules of fungal membrane; resulting in pores; this increases
permeability of the membrane and causes the loss of important metabolites; causing cell death
Broad spectrum fungicidals against: Candida, histoplasma, cryptococcus, sportonix, aspergilus, blastomyces, coccidiodes
(species)
Mechanisms of resistance:
Decrease in membrane ergosterol content
Decreased affinity of ergosterol content to polyenes
Disadvantages:
Bind to cholesterol in human cells
Very toxic drugs that cause: fever, chills, nausea, renal toxicity, anaemia
Clinically used: Amphotericin B; lipid based Ampho B products are less toxic and cheaper
Azoles:
They inhibit ergosterol synthesis, are fungistatic agents and are less toxic than polyenes
Disadvantage: heptaic toxicity Examples:
Imidazoles; for local treatment of cutaneous and vaginal candidasis
Triazoles:they are less toxic than imidazoles and used for oral and intravenous formulations
Fluconazole: low toxicity; used in systemic and mucutaneous candidasis, cryptococcal meningitis. Prophylaxis is a high
risk
Itraconazole: used to treat mucocutaneous candidasis, dermatophytic infections
Echinocandins:
Capsofungin (Cancidas): inhibits synthesis of β-glucan, which is found in fungal cell walls but not in bacterial cell walls
Clinical uses agains systemic candidasis and invasive aspergillosis
Antimetabolites:
Interfere with synthesis of DNA, RNA and proteins
E.g.: flucystosine: always in combination with Ampho B or fluconazole
Allylamines:
Inhibit fungal cell membrane and is a broad spectrum agent
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Active against: dermatophytes, candida species.
28. RESISTANCE TO ANTIMICROBIAL DRUGS. BASIC MECHANISMS OF BACTERIAL RESISTANT. GENETIC BASIS
OF RESISTANCE.
Resistant Organism: this is an organism that will not be inhibited or killed by an antibacterial drug at therapeutic
concentrations.
Therapeutic concentration: drug achievable concentration in the body after normal dosage.
TYPES OF RESISTANCE
Intrinsic: bacteria lack a susceptible target and they are impermeable to antimicrobial agent.
Acquired: due to genetic change subsequent selection process by antimicrobial targets
BASIC MECHANISMS OF BACTERIAL RESISTANCE
Production of enzymes that inactivate the drug
Synthesis of modified targets
Decreased permeability or increased efflux of a drug.
PRODUCTION OF ENZYMES THAT INACTIVATE THE DRUG
INACTIVATING ENZYMES DRUGS
Βeta-lactamases beta-lactams
Phosphorylating
Adenylating Aminoglycosides
Actylating
Acetyltransferase Chloramphenicol
SYNTHESIS OF MODIFIED TARGETS
PBP( penicillin binding proteins): beta-lactams
RNA polymerase →Rifampin
DNA gyrase →Quinolones
Methylated 23s RNA→ Erythromycin
Tetrahydropteroic acid synthase→ Sulfonamides
Dihydroflolate reductase→ Trimethoprim
Altered sterol → Amphotericin B
PREVENTION OF ACCESS OF THE TARGETS RESULTING FROM DECREASED PERMEABILITY OR INCREASED
EFFLUX OF THE DRUG.
Prevention of access to the target drugs
Altered prion channels beta-lactams
Decreased permeability aminoglycosides
Efflux of drug tetracyclines
GENETIC BASES OF RESISTANCE
Resistance: Chromosomal
Extrachromosomal: plasmids and transposons
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Chromosomal
Due to the spontaneous mutation in the gene encoding
-target site
-transport system
Antimicrobial drugs act as selecting agents
-suppress susceptible organisms
-flavour the growth of drug resistant mutants.
It may arise from
-single mutation e.g streptomycin resistant via acteratin in a single ribosomal protein
-series of mutation e.g changes in PBP’s in penicillin resistant S.pneumoniae
Low frequency of spontaneous mutations
-from 10-7 to 10-12
-lower than the frequency of acquisition of R-plasmids
‘chromosomal resistance is not as important as extrachromosomal resistance’
Extrachromosomal resistance( plasmid mediated resistance): this is due to the acquisition of
-plasmids
-transposons
Resistant plasmids( R-factors)
Carry genes for Res to one or more antimicrobials
Occur in many bacterial species (especially gram-negative rod)
They have a high rate of transfer by
-conjugation
-transduction(rarely) but typical for stap.aureus
It can be transferred to cells of the
-same species
-other species
-other genera
Transposons( jumping genes)
Integrated into chromosome or into plamids
They move:
-from chromosome to plasmids
-from plasmids to the chromosome
-between plasmids
-between chromosomes
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
29. Antibiotic use. Factors for selection of antimicrobial drugs for therapy in individual patients. Antimicrobial combinations.
Prophylaxis with antimicrobial agents.
Factors for selection of antimicrobial drugs for therapy of individual patients:
Does the patient have an infection? If yes, what is the likely source?
What are the likely causative microorganisms?
Does the patient need an antibiotic or is the infection self limiting? Is urgent treatment required?
What antibiotic is active against the microorganism?
Does that antibiotic enter the site on infection?
What route of administration should be used?
How much antibiotic should be prescribed?
Are there any contraindications or cautions for prescribing this antibiotic?
What are the side effects of the antibiotic?
When should the patient be reviewed?
Antimicrobial/Antibiotic combinations:
In most cases the single, best antimicrobial agent should be used, as this minimises side effects
However, more than one drug can be prescribed:
To treat serious infections before the identity of the organism is known
To achieve a synergistic inhibitory effect against certain organisms
To prevent the emergence of resistant organisms (i.e.: if organisms is resistant to 1 drug the 2nd drug will kill it)
Two drugs can interact with each other in different ways, they can have:
Synergistic interaction: effect of both drugs together is significantly greater than the two drugs acting alone
Antagonistic interaction (rare): results in significantly lower activity than sum of both drugs
Example of synergistic effect:
Penicillin + an aminoglycoside (like gentamicin) on Enterococci (Ent.faecalis) causes killing of the microorganism, as
penicillin damages the cell wall significantly to let the aminoglycoside enter the cell. If either drug is administered alone it
only has a minor effect
Prophylaxis: treatment given or action taken to
prevent disease
Antibiotic prophylaxis/chemoprophylaxis: is the
prevention of infection complications using microbial
therapy
Prophylactic antimicrobial agents are given in 3
circumstances;To prevent:
Surgical wound infections
Opportunistic infections in immunocompromised
patients
Infections in those known to be exposed to
pathogens that cause serious infectious diseases
For prophylaxis in surgery: only antibiotics with good
tolerability are used;
Downloaded by Kat Enriquez (katmacen@gmail.com)
lOMoARcPSD|4886157
Cephalosporins are preferred due to their low toxicity (3rd generation is more effective than 1st/2nd)
Parenteral systemic antibiotics are more appropriate than oral or topical antibiotics
Broad spectrum antibiotics are more likely to prevent gram (-) sepsis
Prophylaxis is used by surgeons against infective endocarditis prior to GI or genitourinary tract surgeries
30. Normal microbial flora of the human body.
Normal flora are various bacteria and fungi that are permanent residents of certain body sites; especially the skin,
oropharynx, colon and vagina (there are non-sterile sites, unlike CSF)
The viruses and parasites of other groups of microorganisms are not considered normal flora, but can be present in
asymptomatic individuals
Normal flora organisms ar often called comensals; these derive benefit from the host but do not harm the host
Members of normal flora vary in number and kind depending on the site they are in. The central nervous system, blood,
lower bronchi and alveoli, kidney, spleen and bladder are usually sterile.
Normal flora help maintain health and in causation of disease in 3 main ways:
They cause disease, especially in immunocompromised and injured individuals; even though they are non-pathogenic in
their site they can act as pathogens in other regions of the body
They constitute a protective host defence mechanism; their ability to limit growth of pathogens is called colonisation
resistance. If the normal flora is suppressed pathogens can grow and cause disease
They may serve a nutritional function; intestinal normal flora produce several B and K vitamins
Downloaded by Kat Enriquez (katmacen@gmail.com)
You might also like
- BMI1014: Chapter 2 - Bacteria-Morphology and ClassificationDocument6 pagesBMI1014: Chapter 2 - Bacteria-Morphology and ClassificationAkmal Adib FadzilNo ratings yet
- Morphology of BacteriaDocument44 pagesMorphology of BacteriaDr Harender SimarNo ratings yet
- Cell Structure and TaxonomyDocument50 pagesCell Structure and Taxonomyporkypig100% (11)
- Infectious Disease NotesDocument43 pagesInfectious Disease NotessaguNo ratings yet
- Kul II Characterization of Living System-Vr Cahyani-07092020Document15 pagesKul II Characterization of Living System-Vr Cahyani-07092020Ivan Avicenna ArisandyNo ratings yet
- SGL 2 (Structure of Bacterial Cell)Document32 pagesSGL 2 (Structure of Bacterial Cell)rekanshwan5No ratings yet
- Prokaryotes: NucleoidDocument3 pagesProkaryotes: NucleoidHubdar Ali KolachiNo ratings yet
- Cell Structure and TaxonomyDocument50 pagesCell Structure and TaxonomyCarl Elexer Cuyugan AnoNo ratings yet
- Microbiology Notes Final-2Document58 pagesMicrobiology Notes Final-2arvindk962706No ratings yet
- BNC MicroorganismsDocument11 pagesBNC Microorganismsashenafihailemariam43No ratings yet
- Cell and Cell OrganellesDocument53 pagesCell and Cell OrganellesShiffa SaheedNo ratings yet
- General Principles of Cell OrganisationDocument3 pagesGeneral Principles of Cell Organisation22194No ratings yet
- Procaryotic and Eukaryotic CellsDocument64 pagesProcaryotic and Eukaryotic CellsNaufal QaweimNo ratings yet
- Mod 2Document24 pagesMod 2The GreatNo ratings yet
- CellDocument22 pagesCellrapidalerthubNo ratings yet
- Microbiology Lec 1 PDFDocument7 pagesMicrobiology Lec 1 PDFAhmed AliNo ratings yet
- Prokaryotic and Eukaryotic Cells 3.1 CellDocument9 pagesProkaryotic and Eukaryotic Cells 3.1 CellJosebeth CairoNo ratings yet
- What Is A Prokaryotic Cell?: Genetic MaterialDocument7 pagesWhat Is A Prokaryotic Cell?: Genetic MaterialAnkan RoyNo ratings yet
- The Bacterial Cell: Classification and Morphology: Arthur C. Benignos Ii M.DDocument51 pagesThe Bacterial Cell: Classification and Morphology: Arthur C. Benignos Ii M.Dunno hiquianaNo ratings yet
- Microbiology: PROKARYOTIC & EUKARYOTIC CELLSDocument10 pagesMicrobiology: PROKARYOTIC & EUKARYOTIC CELLSEmily RaeNo ratings yet
- 9 Antibacterial ReviewDocument22 pages9 Antibacterial ReviewBrahmanand KuraneNo ratings yet
- 3A.4 Prokaryotic CellsDocument9 pages3A.4 Prokaryotic CellstasmiahNo ratings yet
- Unit 3 Medically Important MicroorganismsDocument9 pagesUnit 3 Medically Important Microorganisms2023800041No ratings yet
- 1 - Introduction To Medical MicrobiologyDocument63 pages1 - Introduction To Medical MicrobiologyAhmed MohamedNo ratings yet
- Structure & Functions of Prokaryotic Cell. Bacteriophages.: Lecturer: - Sergei V. RedkozubovDocument54 pagesStructure & Functions of Prokaryotic Cell. Bacteriophages.: Lecturer: - Sergei V. RedkozubovJustineNo ratings yet
- Prokaryotic and Eukaryotic CellsDocument122 pagesProkaryotic and Eukaryotic CellsAdithya NanuvalaNo ratings yet
- LESSON 3 - Prokaryotid Vs Eukaryotic CellsDocument41 pagesLESSON 3 - Prokaryotid Vs Eukaryotic CellsHyacinth RaeNo ratings yet
- StructureDocument15 pagesStructurefatimasanusimorikiNo ratings yet
- Act. 3 Cytology PeraltaDocument18 pagesAct. 3 Cytology PeraltaCogie PeraltaNo ratings yet
- Chapter 3 Micropara (Outline)Document5 pagesChapter 3 Micropara (Outline)Jezrylle BalaongNo ratings yet
- 1 2020 PHARM232 - Intro To Bacteriology - NarratedDocument59 pages1 2020 PHARM232 - Intro To Bacteriology - Narrateddanst123No ratings yet
- نسخة من 1-Medical Microbiology slides PDFDocument154 pagesنسخة من 1-Medical Microbiology slides PDFسيما مصطفىNo ratings yet
- L2 Bacterial StructureDocument46 pagesL2 Bacterial StructureNarmathaa ThevarNo ratings yet
- Chapter 4: Functional Anatomy of Prokaryotic and Eukaryotic CellsDocument94 pagesChapter 4: Functional Anatomy of Prokaryotic and Eukaryotic CellsTrevannie EdwardsNo ratings yet
- Bacterial Morphology and StructureDocument21 pagesBacterial Morphology and StructurevaidyamNo ratings yet
- Assigment 1 BiologyDocument8 pagesAssigment 1 BiologyshimaabdollahpourNo ratings yet
- Bacterial Notes 2022Document5 pagesBacterial Notes 2022Banji MaikaNo ratings yet
- Basics of Clinical Microbiology For Surgeons: 1. Classification and General Characteristics of BacteriaDocument27 pagesBasics of Clinical Microbiology For Surgeons: 1. Classification and General Characteristics of BacteriaDiary JafNo ratings yet
- Cell The Unit of Life: 16 June 2022 03:52Document19 pagesCell The Unit of Life: 16 June 2022 03:52Dhanalakshmi LakshmiNo ratings yet
- HDTD-B-4 - Cell OrganellesDocument43 pagesHDTD-B-4 - Cell OrganellesMariam Qais100% (1)
- Presentation 2Document54 pagesPresentation 2hunter zoneNo ratings yet
- in Micro para Lecture Chapter 2Document21 pagesin Micro para Lecture Chapter 2Mica-Ella CasasolaNo ratings yet
- Unit II Part IDocument37 pagesUnit II Part Imamiko26yamamotoNo ratings yet
- Microbiology Bacteria Virus FungiDocument54 pagesMicrobiology Bacteria Virus FungiMuhammad TaufiqurrachmanNo ratings yet
- Biol 1017-Cell Biology: Prokaryotes & MicrosDocument50 pagesBiol 1017-Cell Biology: Prokaryotes & MicrosJoshua HarveyNo ratings yet
- Robert Hooke (1665) - Who Named The Biological Unit Cell Cell Theory 1839 - byDocument11 pagesRobert Hooke (1665) - Who Named The Biological Unit Cell Cell Theory 1839 - byKamlesh RatnamNo ratings yet
- For Ntse CellDocument73 pagesFor Ntse CellPrakhar RajNo ratings yet
- Chapter II Bacterial StructureDocument45 pagesChapter II Bacterial StructureBROOKNo ratings yet
- Crizzel Ruth Padernal Castor GWAPADocument73 pagesCrizzel Ruth Padernal Castor GWAPACrizzel Ruth CastorNo ratings yet
- Unit I Module 2: Prokaryotic and Eukaryotic CellsDocument8 pagesUnit I Module 2: Prokaryotic and Eukaryotic CellsMirunalini GobinathNo ratings yet
- Botany Full PDF EMDocument72 pagesBotany Full PDF EMAbinaya PalaniNo ratings yet
- CellDocument16 pagesCellanantchouhdary1709No ratings yet
- MicroPara 03 - Prokaryotic CellsDocument23 pagesMicroPara 03 - Prokaryotic CellsJianne CaloNo ratings yet
- Bacterial Structure 1 1 2Document41 pagesBacterial Structure 1 1 2Nour MohammedNo ratings yet
- Module 1 Microorganisms in Food and SpoilageDocument24 pagesModule 1 Microorganisms in Food and SpoilageSiddNo ratings yet
- Prokaryotic CellDocument4 pagesProkaryotic Cellkrista mae logronoNo ratings yet
- BIOL107 - Different Cell TypesDocument4 pagesBIOL107 - Different Cell TypesJahsuah OrillanedaNo ratings yet
- Micro para 1Document4 pagesMicro para 1Reselle EspirituNo ratings yet
- Environmental Microbiology UNIT 1Document43 pagesEnvironmental Microbiology UNIT 1Esai Kanaga YadavNo ratings yet
- Microbiology: a QuickStudy Laminated 6-Page Reference GuideFrom EverandMicrobiology: a QuickStudy Laminated 6-Page Reference GuideNo ratings yet
- Basella Rubra Biological Stain: Health Benefits of Basella (Vine Spinach)Document3 pagesBasella Rubra Biological Stain: Health Benefits of Basella (Vine Spinach)yepNo ratings yet
- Characteristics of Blood Group Antibodies: Immunoglobulin Class Remarks Associated With Antigen Frequency (%)Document1 pageCharacteristics of Blood Group Antibodies: Immunoglobulin Class Remarks Associated With Antigen Frequency (%)yepNo ratings yet
- ChinilinDocument37 pagesChinilinyepNo ratings yet
- Summary of Coagulation FactorsDocument2 pagesSummary of Coagulation FactorsyepNo ratings yet
- Bachelor in Science of Medical Technology Central Luzon Doctors' Hospital Educational Institution S.Y. 2018 - 2019Document7 pagesBachelor in Science of Medical Technology Central Luzon Doctors' Hospital Educational Institution S.Y. 2018 - 2019yepNo ratings yet
- Sa Kabilang MedyasDocument31 pagesSa Kabilang MedyasyepNo ratings yet
- WaloDocument67 pagesWaloyepNo ratings yet
- Appendix C ComputationDocument2 pagesAppendix C ComputationyepNo ratings yet
- Citizens Charter 2018Document77 pagesCitizens Charter 2018yepNo ratings yet
- Instructions MPH Data: A. Process Workflow and AccountabilityDocument57 pagesInstructions MPH Data: A. Process Workflow and AccountabilityyepNo ratings yet
- Special Staining Cytochemistry: BY Zenaida Capistrano-Cajucom, RMT, Ma - Ed.Mgt, FpametDocument93 pagesSpecial Staining Cytochemistry: BY Zenaida Capistrano-Cajucom, RMT, Ma - Ed.Mgt, FpametyepNo ratings yet
- PA41 - R14001B - Clinical Chemistry SummaryDocument3 pagesPA41 - R14001B - Clinical Chemistry SummaryyepNo ratings yet
- Multiplication: Grade 3Document27 pagesMultiplication: Grade 3yepNo ratings yet
- WaloDocument67 pagesWaloyepNo ratings yet
- Science 2Document2 pagesScience 2yepNo ratings yet
- Penis: Male Genital System and Lower Urinary TractDocument21 pagesPenis: Male Genital System and Lower Urinary TractyepNo ratings yet
- Bring My Device (BMD) Policy (Philippine Employees)Document4 pagesBring My Device (BMD) Policy (Philippine Employees)yepNo ratings yet
- Gestational and Placental Disorders: Ovary Pregnancy Results From TheDocument4 pagesGestational and Placental Disorders: Ovary Pregnancy Results From TheyepNo ratings yet
- Alorica WAH Expectations Supplement RJBDocument3 pagesAlorica WAH Expectations Supplement RJByepNo ratings yet
- Observational Study of Safe Injection Practices in A Tertiary Care Teaching HospitalDocument5 pagesObservational Study of Safe Injection Practices in A Tertiary Care Teaching HospitalMuhammad HaezarNo ratings yet
- AbstractDocument8 pagesAbstractMa Ceres P SisonNo ratings yet
- STE8 - Q4 - Wk1 2 - Describe The Application of Biotechnology in Health QA GQA - LRQA1Document15 pagesSTE8 - Q4 - Wk1 2 - Describe The Application of Biotechnology in Health QA GQA - LRQA1Alyssa CuellarNo ratings yet
- Company Overview & ProductsDocument16 pagesCompany Overview & ProductsAbdalazeez AlsayedNo ratings yet
- Understanding Immuno-Oncology - The Interplay Between TheDocument9 pagesUnderstanding Immuno-Oncology - The Interplay Between Thenathalylara050590No ratings yet
- Epidemiological SurveillanceDocument22 pagesEpidemiological SurveillanceSyafiq HusniNo ratings yet
- Shifting Exams Reviewer For MEDTECH in ParasitologyDocument12 pagesShifting Exams Reviewer For MEDTECH in ParasitologyIwa RohasNo ratings yet
- Salivary GlandsDocument97 pagesSalivary GlandsSwati George100% (2)
- MCI FMGE 2009 Previous Year From Memory Question Paper PDFDocument6 pagesMCI FMGE 2009 Previous Year From Memory Question Paper PDFNandita TiwariNo ratings yet
- National Health Programs Final 150324130140 Conversion Gate01Document141 pagesNational Health Programs Final 150324130140 Conversion Gate01Manoj Garg100% (1)
- CHNDocument49 pagesCHNAlbert Remollo Jr100% (2)
- Sexually Transmitted Diseases: Nelia B. Perez RN, MSN Class 2015Document94 pagesSexually Transmitted Diseases: Nelia B. Perez RN, MSN Class 2015Mariana CreciunNo ratings yet
- C3iMagazine Pandemic Ebook RBMStudio2020Document6 pagesC3iMagazine Pandemic Ebook RBMStudio2020Wilson CrunchNo ratings yet
- Morphology of HookwormsDocument2 pagesMorphology of HookwormsZam PamateNo ratings yet
- Pedoman Pelayanan Bagian Rekam Medis - Daftar Singkatan EditDocument18 pagesPedoman Pelayanan Bagian Rekam Medis - Daftar Singkatan EditEki JalesvevaNo ratings yet
- Rheumatic Heart DiseaseDocument3 pagesRheumatic Heart DiseaseWay LeeNo ratings yet
- CMV Igm: Igm Antibodies To Cytomegalovirus 04784618 190 100 TestsDocument4 pagesCMV Igm: Igm Antibodies To Cytomegalovirus 04784618 190 100 TestsModestusNo ratings yet
- Mosquito Bite (Overview) Mosquito Bites Usually Are Not Very Visible On Skin Unless There IsDocument3 pagesMosquito Bite (Overview) Mosquito Bites Usually Are Not Very Visible On Skin Unless There IsArunKumarNo ratings yet
- Abyssinian Ground HornbillDocument4 pagesAbyssinian Ground HornbillEmilio Lecaros BustamanteNo ratings yet
- Niaid Strategic Plan For COVID-19 Research: FY2020 - FY2024Document12 pagesNiaid Strategic Plan For COVID-19 Research: FY2020 - FY2024s pNo ratings yet
- Differentiating Between The Common Cold and The Flu.: Lipsticks Contain Excessive Lead, Tests RevealDocument4 pagesDifferentiating Between The Common Cold and The Flu.: Lipsticks Contain Excessive Lead, Tests RevealDwayne HausNo ratings yet
- NKC Fast Facts - Poop Chart - 5 2017 PDFDocument1 pageNKC Fast Facts - Poop Chart - 5 2017 PDFFaniaNo ratings yet
- Exercise No Plant Path 1Document3 pagesExercise No Plant Path 1ROGNo ratings yet
- Chapter 12 - Congenital and Acquired ImmunodeficienciesDocument11 pagesChapter 12 - Congenital and Acquired ImmunodeficienciesFYMNo ratings yet
- Covid-19 Epidemic EditorialDocument2 pagesCovid-19 Epidemic EditorialAdam CayongcongNo ratings yet
- VINCENT P. Et Al. 2007 PDFDocument3 pagesVINCENT P. Et Al. 2007 PDFLiga Odontopediatria RondonienseNo ratings yet
- IPC Guideline - FINAL Updated Version 11july2018 - RevisedDocument279 pagesIPC Guideline - FINAL Updated Version 11july2018 - Revisedprisco linusiNo ratings yet
- TrypanosomiasisDocument39 pagesTrypanosomiasisNani HendrianiNo ratings yet
- Chapter 13: Microbe-Human Interactions: Infection, Disease, and EpidemiologyDocument11 pagesChapter 13: Microbe-Human Interactions: Infection, Disease, and EpidemiologyElloNo ratings yet
- Product-List PCR-AND-ELISA 2022 V1-EN Doc13347Document36 pagesProduct-List PCR-AND-ELISA 2022 V1-EN Doc13347Luis HidalgoNo ratings yet