Professional Documents
Culture Documents
Hipertonic Saline
Hipertonic Saline
Uploaded by
MARIA SALOMONOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hipertonic Saline
Hipertonic Saline
Uploaded by
MARIA SALOMONCopyright:
Available Formats
Journal of Neurosurgical Anesthesiology
Vol. 14, No. 3, pp. 187–193
© 2002 Lippincott Williams & Wilkins, Inc., Philadelphia
Hypertonic Saline Ameliorates Cerebral Edema Associated With
Experimental Brain Tumor
*Thomas J. K. Toung, †Betty Tyler, †Henry Brem, *Richard J. Traystman, *Patricia D. Hurn, and
*‡Anish Bhardwaj
Departments of *Anesthesiology/Critical Care Medicine, ‡Neurology, and †Neurological Surgery, Johns Hopkins University School
of Medicine, Baltimore, Maryland
Summary: Cerebral edema commonly accompanies brain tumors and frequently leads
to lethal intracranial compartmental shifts and elevated intracranial pressure. Therapeutic
modalities for tumor–associated cerebral edema include diuretics, osmotherapy, and
corticosteroids. Recently, hypertonic saline (HS) has received attention as an osmotic
agent in the treatment of cerebral edema from diverse causes. The effects of continuous
HS infusion in brain tumor–associated edema have not been previously reported. There-
fore, we tested the hypothesis that HS given as a continuous intravenous infusion ame-
liorates tumor-associated edema in a rat model of brain tumor. 9L gliosarcoma, propa-
gated as a solid flank tumor, was implanted intracranially over the left hemisphere in
adult female Fischer 344 rats (180–220 g). On day 11 after implantation, rats were
divided in a blinded, randomized fashion into groups that received no treatment or
continuous infusion of 0.9% saline (NS) (0.3 mL/h) and in a subsequent series that
included NS + intravenous furosemide 2.5 mg/kg every six hours, NS + intravenous
mannitol 2.5 g/kg every six hours, or continuous infusion 7.5% HS (chloride:acetate
50:50) (0.3 mL/h). Hemispheric water content ipsilateral (IH) and contralateral to tumor
implantation was determined at day 13 by wet-to-dry weight ratio after 48 hours of
therapy. Ipsilateral hemispheric water content (mean ± SEM) was significantly increased
in rats with intracranial tumor on day 11 (80.3 ± 0.5%) (n ⳱ 7) and day 13 (81.4 ± 0.3%)
(n ⳱ 10), as compared to naive weight-matched rats without tumor implant (79.3 ±
0.1%) (n ⳱ 13) (P < .05). After 48 hours of treatment, IH water content was attenuated
with continuous HS (n ⳱ 15) (79.3 ± 0.2%), mannitol (n ⳱ 14) (80.1 ± 0.2%), and
furosemide (n ⳱ 15) (79.9 ± 0.2%) as compared to NS (n ⳱ 7) (80.8 ± 0.5%).
Continuous HS infusion attenuated cerebral edema in the affected hemisphere as well as
the contralateral noninjured hemisphere to a larger extent than was observed with furo-
semide or mannitol. These findings suggest a potential new treatment strategy for tumor–
associated cerebral edema. Key Words: Furosemide—Hypertonic saline—Mannitol—
Edema—Tumor—Osmotic
Cerebral edema is a frequent cause of morbidity and with or without elevated intracranial pressure (ICP) in
mortality from lethal intracranial compartmental shifts patients with brain tumors (1–3). Therapeutic modalities
used for the treatment of tumor–associated cerebral edema
Address correspondence and reprint requests to Dr. Anish Bhardwaj, include systemic administration of diuretics, osmotherapy,
Neuroscience Critical Care Division, Meyer 8–140, Johns Hopkins Hos- and corticosteroids (2,3). Conventional therapies for cere-
pital, 600 North Wolfe Street, Baltimore, MD 21287. Accepted for pub- bral edema are aimed at improving intracranial compli-
lication on February 20, 2002.
Supported in part by U.S. Public Health Service National Institutes of ance by altering the three major compartments of the in-
Health grants NS20020, NS33668, NIH NCDDG U01 CA525857. tracranial vault: blood, cerebrospinal fluid (CSF), and
187 DOI: 10.1097/01.ANA.0000017173.39312.DD
188 T. J. K. TOUNG ET AL.
brain (3). This can be achieved by facilitating cerebral chloride (25 mg/mL), xylazine (2.5 mg/mL), and ethyl
venous outflow, maintaining adequate cerebral perfusion alcohol (14%) in normal saline. Skin was prepared in an
and oxygenation, controlled hyperventilation, external aseptic fashion with 70% ethyl alcohol and providone-
CSF drainage for hydrocephalus and cerebral osmotic “de- iodine solution. Using microsurgical technique, a midline
hydration” with osmotic agents and diuretics (3). Acute incision was made over the skull, and the periosteum was
administration of osmotic agents has a potent antiedema displaced. A 3-mm burr hole was drilled over the left
action, primarily on undamaged brain regions with an in- hemisphere with its center 5 to 6 mm behind the coronal
tact blood–brain barrier, theoretically drawing water from suture and 3 to 4 mm lateral to the sagittal suture. The dura
the interstitial and extracellular space into the intravascu- was opened sharply in a cruciate fashion, and the cortex
lar compartment, thereby at least transiently improving was aspirated to expose the highly vascular sulcus be-
intracranial compliance (3–5). In addition, osmotic agents tween the thalamus and the superior colliculus. Bleeding
may exert beneficial nonosmotic cerebral effects, includ- was allowed to subside spontaneously, and the tumor frag-
ing enhancing cerebral blood flow by reducing blood vis- ment was implanted into the brain defect. The surgical
cosity (4–6), free radical scavenging (7), enhancing oxy- wound was thoroughly irrigated, and the skin was closed
gen delivery, and affecting CSF dynamics (8). A variety of with surgical clips.
osmotic agents have been studied including mannitol,
glycerol, urea, sorbitol, and more recently, hypertonic sa-
Instrumentation
line (HS) (3–5).
All techniques are as previously described (15). In brief,
We have previously shown that continuous HS infusion
on day 11, tumor-implanted rats were anesthetized with
is efficacious in some forms of neuroinjury by ameliorat-
halothane (1.0–2.0%) in oxygen-enriched air and were
ing elevated ICP and midline shift in patients with edema
allowed to ventilate spontaneously. Using aseptic surgical
associated with resection of brain tumors postoperatively
technique, the right femoral artery was cannulated to
and in traumatic brain injury (6). However, there have
monitor arterial blood pressure and arterial blood gases,
been no direct comparisons between efficacy of continu-
and the femoral vein was cannulated for vascular access.
ous HS therapy and standard osmotic or diuretic agents,
After cannulation, both catheters were exteriorized in the
for example, mannitol and furosemide (2,5,8,9), respec-
posterior midthorax. Incision sites for intravascular cath-
tively, in reducing tumor–associated cerebral edema. Ac-
eters were injected locally with 0.25% bupivacaine. Rectal
cordingly, the present study was designed 1) to compare
temperature was maintained with a heating lamp (38.0–
the effects of furosemide, mannitol, and HS on brain water
39.0°C) throughout the surgical procedure. Rats were then
content, and 2) to test the hypothesis that maintenance of
allowed to emerge from anesthesia and were housed in
a constant osmotic gradient with continuous HS infusion
separate cages maintained at room temperature and al-
is more efficacious in ameliorating edema in a well-
lowed free access to food and water.
characterized model of intracranial tumor in the rat.
Experimental Groups
MATERIALS AND METHODS Brain was harvested from age- and weight-matched na-
ive (without tumor implants) Fisher 344 rats (n ⳱ 13) and
The experimental protocol was approved by the Insti- tumor-implanted rats on day 11 (n ⳱ 7) and day 13 (n ⳱
tutional Animal Care and Use Committee and conforms to 10) and analyzed for hemispheric water content. After
the National Institutes of Health guidelines for the care surgical interventions on day 11, tumor-implanted rats
and use of animals in research. were divided in a blinded, randomized fashion into ex-
perimental groups that received no treatment (n ⳱ 7) or
Tumor Implantation continuous infusion of 0.9% saline (NS) (0.3 mL/h) (n ⳱
All methods have been previously described (10–14). 7) and in a subsequent series that included NS + intrave-
9L gliosarcoma was propagated as a solid tumor in the nous furosemide 2.5 mg/kg every six hours (n ⳱ 15), NS
flanks of adult female Fischer 344 rats (180–200 g). For + intravenous mannitol 2.5 g/kg every six hours (n ⳱ 14)
intracranial implantation, tumor fragments were trimmed or continuous infusion 7.5% HS (chloride:acetate 50:50)
to pieces measuring approximately 2 × 2 × 1 mm. Rats (0.3 mL/h) (n ⳱ 15). Treatments were continued for 48
were anesthetized with an intraperitoneal injection of 3 to hours (day 13 of tumor implantation), and then tissue was
5 mL/kg of a stock solution containing ketamine hydro- harvested.
Journal of Neurosurgical Anesthesiology, Vol. 14, No. 3, 2002
BRAIN TUMOR–ASSOCIATED CEREBRAL EDEMA 189
Assessment of Brain Edema and Plasma Osmolality
Arterial blood was sampled for determination of hemat-
ocrit, serum sodium, and for plasma osmolality
(mOSm/L) as measured by freezing-point depression mi-
cro-osmometer (Advanced Instruments, Norwood, MA) at
baseline and the end of 48 hours of treatment. After 48
hours of treatment, brain edema was estimated by com-
paring wet to dry tissue weight ratios (15,16). Briefly, rats
were decapitated while under deep halothane anesthesia.
The brain was quickly removed, blotted to remove re-
sidual adsorbent moisture, and dissected through the in-
terhemispheric fissure into right and left hemispheres. Wet
weight was determined with a resolution of 0.1 mg. Dry
weight of whole ipsilateral and contralateral hemispheres
was determined after heating the tissue for 3 days at 100°C
in a drying oven. Tissue water content was then calculated
as % H2O ⳱ (1-dry wt/wet wt) × 100% (15,16).
Histopathology
On days 11 and 13 after implantation, additional co-
horts (n ⳱ 3 each) were deeply anesthetized, and the
brains were perfused-fixed with 10% neutral buffered for-
malin. Tissue was paraffin-embedded, sectioned (10 m),
and stained for standard hematoxylin and eosin histology.
Statistical Analysis
All values are expressed as mean ± SEM. Physiologic
parameters among groups were subjected to repeated-
measures analysis of variance. Differences in cerebral
edema among treatment groups were determined by two- FIG. 1. Representative photomicrograph of brain from a tumor-
way analysis of variance with post hoc Newman-Keuls implanted rat on day 13 demonstrating tumor in the right parietal region.
test. The criterion for statistical significance was P < .05.
RESULTS evated as compared to the NS-treated group (265 ± 1) (P
< .05). Serum osmolality in the furosemide-treated rats at
Untreated tumor-implanted rats demonstrated signifi- 48 hours (271 ± 3) was also significantly elevated as com-
cant infiltrative tumor growth between day 11 and day 13, pared to baseline (264 ± 2 mEq/L). No rats died in any of
causing a significant midline shift (Fig. 1 and 2). In rats the treatment groups before completion of the experimen-
randomized to various treatment groups, mean arterial tal protocol. Ipsilateral hemispheric water content on day
blood pressure, arterial carbon dioxide (PaCO2) and oxy- 11 (80.3 ± 0.5%, n ⳱ 7) and day 13 (81.4 ± 0.3%, n ⳱
gen (PaO2), and pH were within normal physiologic 10) was significantly increased in rats with intracranial
ranges in all groups immediately after placement of intra- tumor, as compared to naive rats with no tumor implants
vascular catheters (data not shown). Baseline serum os- (79.3 ± 0.1%, n ⳱ 13) (P < .05) (Fig. 3). Ipsilateral
molality, Na+, and hematocrit were similar in all treatment hemispheric water content was attenuated to a larger ex-
groups (Table 1). At 48 hours, serum Na+ was signifi- tent with continuous HS (79.3 ± 0.2%, n ⳱ 15), as com-
cantly higher in rats treated with HS (157 ± 2 mEq/L) and pared to 0.9% saline (80.8 ± 0.5%, n ⳱ 7), mannitol (80.1
furosemide (150 ± 1) (P < .05) as compared with rats ± 0.2%, n ⳱ 14), or furosemide treatment (79.9 ± 0.2%,
treated with NS (144 ± 1) and mannitol (141 ± 2). Serum n ⳱ 15). Furthermore, contralateral hemispheric water
osmolality was similar in rats treated with HS (311 ± 3 content was lower in HS-treated animals as compared to
mOsm/L) and mannitol (308 ± 4) but significantly el- untreated brain or the alternative treatments.
Journal of Neurosurgical Anesthesiology, Vol. 14, No. 3, 2002
190 T. J. K. TOUNG ET AL.
from lethal intracranial compartmental shifts (3,5,18,19).
Although some brain tumors are steroid responsive and
undergo reduction in size, the initial favorable response in
tumor–associated cerebral edema to steroid treatment is
often short-lived (20). Mannitol has long been designated
as the osmotic agent of choice (5,21). Hypertonic saline
solutions have recently received renewed attention as hy-
perosmolar agents and are used increasingly in a variety of
brain injury paradigms (3,6,21–26). A variety of experi-
mental evidence and clinical case series reports suggest
that HS may be superior to mannitol in some settings
(3,22). Sodium chloride (reflection coefficient ⳱ 1.0)
(3,22) is completely excluded from brain as long as the
blood–brain barrier is intact. Like mannitol (27), HS also
exerts nonosmotic cerebral effects including improved ce-
rebral perfusion and oxygen delivery (28) and decreases
CSF formation (29). Furthermore, HS may maintain a
desirably “euvolemic hyperosmolar” state in a variety of
brain injury paradigms (3). In our retrospective clinical
series (6), continuous 3% HS therapy attenuated ICP and
improved midline shifts in patients with traumatic brain
injury and in postoperative neurosurgical patients with in-
tracranial lesions. In contrast, patients with intracerebral
hemorrhage and cerebral infarction did not benefit from
FIG. 2. A. Representative photomicrograph of hematoxylin and eosin
(H&E) stain of coronal section of brain from a tumor-implanted rat on
HS therapy. The value of HS therapy remains unproven in
day 13 demonstrating midline and compartmental shift. B. Representa- clinical stroke.
tive photomicrograph (×20) of H&E stain of a section demonstrating the In the present study, wet-to-dry weight comparisons
tumor infiltrating into normal surrounding brain tissue.
were used as a simple and reproducible assessment of
hemispheric brain water, without subdissection to identify
DISCUSSION regional water content differences or differential treatment
effects in tumoral or peritumoral regions. We confirmed
This study demonstrates two important findings. First, infiltrative tumor growth in the window of 48 hours (be-
ipsilateral hemispheric brain water content accumulates tween days 11 and 13) in our experimental model with
over time after tumor implantation in this well- histopathologic studies. As expected, there were increases
characterized experimental model of brain tumor. Second, in brain water content in rats with brain tumor implants
this increase in water content is responsive to a conven- compared to naive controls, and this increase was time
tional osmotic agent, mannitol, as well as the diuretic fu- dependent. We tested the various treatments between days
rosemide. For the treatment doses used here, maintenance 11 and 13 because it was likely that maximal effects
of a constant osmotic gradient with continuous HS therapy would be observed, given that mortality in this animal
was more efficacious in ameliorating cerebral edema in model approaches 100% by day 16 after tumor implanta-
the injured hemisphere than these conventional therapies tion. The doses of mannitol and furosemide employed
were. here were chosen based on previous reports of efficacy
Cerebral edema invariably accompanies brain tumor in (30,31). Furosemide, a potent loop diuretic, has been less
patients, and its cause is thought to be largely vasogenic rigorously and extensively studied than mannitol for treat-
(3,5,17). The location and degree of edema are variable ment of vasogenic cerebral edema. The potent antiedema
and dependent on size, regional location, and tumor his- actions of both mannitol and furosemide are complex and
tology. Surgical tumor resection remains the definitive thought to be secondary to a combination of osmotic de-
management in most cases. Nevertheless, emergent medi- hydration (32), reduction of choroidal CSF formation (33)
cal therapies comprising steroids, osmotic agents, and/or and decreased cerebral blood volume secondary to reflex
diuretics are important adjuncts in “brain resuscitation” vasoconstriction (a response to decreased blood viscosity)
Journal of Neurosurgical Anesthesiology, Vol. 14, No. 3, 2002
BRAIN TUMOR–ASSOCIATED CEREBRAL EDEMA 191
TABLE 1. Summary of selected physiologic variables at baseline and after 48 hours of treatment in tumor-implanted rats
0.9% Saline Mannitol Furosemide HS
(n ⳱ 7) (n ⳱ 14) (n ⳱ 15) (n ⳱ 15)
Hematocrit (%) Baseline 40 ± 1 39 ± 1 39 ± 1 40 ± 1
48 h 37 ± 1* 34 ± 1*† 37 ± 1* 38 ± 1*
Osmolality (mOsm/L) Baseline 264 ± 2 265 ± 1 263 ± 1 267 ± 1
48 h 265 ± 1 309 ± 4*‡ 271 ± 3* 311 ± 3*‡
Serum Na+ (mEq/L) Baseline 141 ± 1 138 ± 1 139 ± 2 138 ± 1
48 h 144 ± 1 141 ± 2 151 ± 1*† 157 ± 2*†
Values are mean ± SEM.
*P < .05 compared to Baseline; †p < 0.05 compared to 0.9% saline and mannitol;
†P < .05 compared to 0.9% saline, furosemide, and HS.
‡P < .05 compared to 0.9% saline and furosemide.
HS ⳱ hypertonic saline; Na+ ⳱ serum sodium.
(32,34). Both furosemide and mannitol were comparable We have used HS safely as a continuous infusion rather
in attenuation of brain water increase in our experimental than intravenous bolus in brain-injured patients with the
paradigm. However, HS demonstrated the largest percent premise that a constant osmotic gradient between brain
decrease in brain water content both in regions of intact and cerebral vasculature is better achieved and maintained
blood–brain barrier integrity (contralateral hemisphere) with continuous infusion (6,42). Although there is consid-
and in the lesioned hemisphere. Although the present erable uncertainty about the absolute increase in plasma
study was not designed to delineate mechanisms for these osmolality that is required to significantly decrease brain
findings, several must be considered. The osmolar load of volume and therefore ICP, some investigators have sug-
7.5% HS (2310 mOsm/L) is slightly higher than 20% gested that increases of ≈ 30 mOsm/L are essential
mannitol (1098 mOsm/L), potentially making it the more (38,39). Others have shown that serum osmolality of 300
effective agent for brain “dehydration.” This characteristic to 320 mOsm/L (corresponding to serum Na+ of 145–155
may explain the present observation that HS decreased mEq/L) is optimal in patients with poor intracranial com-
brain water in the contralateral hemisphere to less than pliance (40). In many instances, the latter level is the
that of naive brain. Hypertonic saline solutions also modu- currently accepted goal for clinical osmotherapy in brain-
late the inflammatory response of the brain to injury (35) injured patients (3,40). We have recently shown that in-
by attenuating polymorphonuclear neutrophil cytotoxicity duced hypernatremia to these desired goals does not cause
(36) and augmenting immune responses (37). neuronal, glial, or myelin pathology in experimental
FIG. 3. Brain water content in the ipsilat-
eral and contralateral hemispheres from na-
ive controls and tumor-implanted rats and
after treatment with 0.9% saline (NS), 7.5%
hypertonic saline (HS), furosemide, and
mannitol. *P < .05 versus naive; †P < .05
versus day 11; #P < .05 versus furosemide
and mannitol of corresponding hemisphere;
‡P < .05 versus corresponding hemispheres
in naive and on day 11 and day 13 of tumor-
implanted rats; ¶P < .05 versus correspond-
ing hemisphere in naive, untreated, and NS-
treated tumor-implanted rats on day 11 and
day 13.
Journal of Neurosurgical Anesthesiology, Vol. 14, No. 3, 2002
192 T. J. K. TOUNG ET AL.
stroke (15). In the present study, we compared 20% man- rebral edema occurs in tissue ipsilateral to brain tumor and
nitol given as a bolus to continuous infusion of 7.5% HS progresses with a time course that simulates human dis-
because the targeted serum osmolality was achieved in ease. Although it is difficult to make comparisons between
both treatment groups. treatment regimens that are not iso-osmolar, our data in-
Our study has some clear limitations. First, the data dicate that maintenance of a constant osmotic gradient
cannot address the potential for “rebound” cerebral with continuous HS therapy appears to provide effective
edema. Although never definitively characterized, osmo- hyperosmolar “dehydration” of both lesioned and nonle-
therapy may be limited by secondary entry and accumu- sioned brain regions in our experimental model of brain
lation of nonmetabolized osmotic agent in damaged tissue tumor compared to that obtained with bolus mannitol and
with disrupted barrier integrity and/or secondary to in- furosemide. Further study is required to determine the
creases in idiogenic tissue osmoles (5). Second, we did not antiedema mechanisms and differential effect of HS in
measure ICP or behavioral outcomes. Therefore, it is not tumoral and peritumoral brain regions. Nevertheless, our
certain whether the large reduction of ipsilateral hemi- study may have therapeutic implications, in that it pro-
spheric brain water observed here is translated into func- vides further experimental evidence that HS may be an-
tional consequences for tumor-infiltrated brain. Mannitol other modality in the armamentarium of medical therapy
and furosemide are known to cause systemic dehydration. for tumor-associated cerebral edema.
To prevent intravascular volume depletion, a continuous
Acknowledgment: Dr. Bhardwaj is supported in part by the
intravenous infusion of normal saline was maintained in
Established Investigator Grant from the American Heart Asso-
all animals for the duration of the experiment. While we ciation.
attempted to create a “euvolemic hyperosmolar” state in
each treatment group, we did not assess fluid status vari-
REFERENCES
ables such as urinary output or central venous pressure in
rat. While correlations have been described between post- 1. Ropper AH. Lateral displacement of the brain and level of con-
ischemic brain water and body weight (41), body weight is sciousness in patients with acute hemispheral mass. N Engl J Med
1986;314:953–8.
greatly influenced in brain tumor–bearing rats that sustain 2. Fishman RA. Disorders of Intracranial Pressure: Hydrocephalus,
diminished oral intake and a markedly catabolic state. Brain Edema, Pseudotumor, Intracranial Hypertension, and Related
Third, we only measured arterial blood pressure, blood Disorders in Cerebrospinal Fluid Diseases of the Nervous System.
2nd ed. Philadelphia: WB Saunders, 1992.
gases, and rectal temperature after placement of intravas- 3. Bhardwaj A, Ulatowski JA. Cerebral edema: hypertonic saline so-
cular catheters and did not monitor these parameters dur- lutions. Curr Treat Options Neurol 1999;1:179–87.
ing the 48-hour treatment period in any of the treatment 4. Schell RM, Applegate II RL, Cole DJ. Salt, starch, and water on the
brain. J Neurosurg Anesth 1996;8;178–82.
groups in our study. However, we have previously shown 5. Paczynski RP. Osmotherapy. Basic concepts and controversies. Crit
that continuous infusion of HS or NS does not affect these Care Clin 1997;13:105–29.
physiologic parameters (15). It is conceivable that there 6. Qureshi AI, Suarez JI, Bhardwaj A, et al. Use of hypertonic (3%)
saline/acetate infusion in the treatment of cerebral edema: effect on
were alterations in blood pressure (possibly transient) in intracranial pressure and lateral displacement of the brain. Crit Care
rats treated with bolus mannitol and furosemide. Serum Med 1998;26:440–6.
osmolality, Na+, and hematocrit were measured after 7. Gaab M, Knoblich OE, Shupp J, et al. Effect of furosemide (Lasix)
on acute severe experimental cerebral edema. J Neurol 1979;220:
placement of intravascular catheters, before randomiza- 185–97.
tion to any treatment groups (baseline) and at the end of 48 8. Cascino T, Baglivo J, Conti J, et al. Quantitative CT assessment of
hours (day 13) in our study. More frequent measurements furosemide-and mannitol-induced changes in brain water content.
Neurology 1983;33:898–903.
are not feasible in a small rodent model with limited tol- 9. Cottrell JE, Robustelli A, Post K, et al. Furosemide- and mannitol-
erance of repeated blood loss for samples. Serum osmo- induced changes in intracranial pressure and serum osmolality and
lality may fluctuate with bolus or pulse therapy with man- electrolytes. Anesthesiology 1977;47:28–30.
10. DiMeco F, Rhines LD, Hanes J, et al. Paracrine delivery of IL-12
nitol and furosemide, and this remains an important issue against intracranial 9L gliosarcoma in rats. J Neurosurg 2000;92:
in clinical practice as well. Hematocrit was significantly 419–27.
elevated with HS and furosemide, as compared with man- 11. Tamargo RJ, Sills AK Jr, Reinhard CS, et al. Interstitial delivery of
dexamethasone in the brain for the reduction of peritumoral edema.
nitol treatment. Although the effects of mannitol on blood J Neurosurg 1991;74:956–61.
viscosity and red blood cell rheology have been well stud- 12. Tamargo RJ, Myseros JS, Epstein JI, et al. Interstitial chemotherapy
ied (43), similar studies have not yet been carried out with of the 9L gliosarcoma: controlled release polymers for drug delivery
in the brain. Can Res 1993;53:329–33.
HS and furosemide. 13. Weingart JD, Sipos EP, Brem H. The role of minocycline in the
In conclusion, our data demonstrate that significant ce- treatment of intracranial 9L glioma. J Neurosurg 1995;82:635–40.
Journal of Neurosurgical Anesthesiology, Vol. 14, No. 3, 2002
BRAIN TUMOR–ASSOCIATED CEREBRAL EDEMA 193
14. Weingart JD, Thompson RC, Tyler B, et al. Local delivery of the 29. Artru AA. Cerebrospinal fluid. In: Cotrell JE, Smith DS, eds. An-
topoisomerase I inhibitor camptothecin sodium prolongs survival in esthesia and Neurosurgery. St. Louis: CV Mosby, 2001:83–100.
the rat intracranial 9L gliosarcoma model. Int J Cancer 1995;62: 30. Cascino T, Baglivo J, Conti J, et al. Quantitative CT assessment of
605–9. furosemide and mannitol induced changes in brain water content.
15. Bhardwaj A, Harukuni I, Murphy S, et al. Hypertonic saline worsens Neurology 1983;33:898–903.
infarct volume after transient focal ischemia in rats. Stroke 2000;31: 31. Paczynski RP, He YY, Diringer MN, et al. Multiple-dose mannitol
1694–7001. reduces brain water content in a rat model of cortical infarction.
16. Lin TN, He YY, Wu G, et al. Effect of brain edema on infarct Stroke 1997;28:1437–44.
volume in a focal cerebral ischemia model in rats. Stroke 1993;24: 32. Milhorat TH, Pan J. The blood-brain barrier and cerebral edema. In:
117–21. Cotrell JE, Smith DS, eds. Anesthesia and Neurosurgery. St. Louis:
17. Bingaman WE, Frank JI. Malignant cerebral edema and intracranial CV Mosby, 2001:115–27.
hypertension. Neurol Clin 1995;13:479–509. 33. Vogh BP, Langham MR. The effect of furosemide and bumetanide
18. Miller JD, Leech P. Effects of mannitol and steroid therapy on on cerebrospinal function. Brain Res 1981;221:171–83.
intracranial pressure on intracranial-pressure relationships in pa- 34. Avellino AM, Lam AM, Winn HR. Management of acute head
tients. J Neurosurg 1975;42:274–81. injury. In: Albin MS, ed. Textbook of Neuroanesthesia. New York:
19. Skjoeth J, Bjerre PK. Effect of glucocorticoids on ICP in patients McGraw Hill, 1997:1137–1175.
with a cerebral tumor. Acta Neurol Scand 1997;96:167–70. 35. Hartl R, Medary MB, Ruge M, et al. Hypertonic/hyperoncotic saline
20. Shapiro WR, Posner JB. Corticosteroid hormones: effect in an ex- attenuates microcirculatory disturbances after traumatic brain injury.
perimental brain tumor. Arch Neurol 1974;30:217–21. J Trauma 1997;42:S41–47.
21. Zornow MH. Hypertonic saline as a safe and efficacious treatment of 36. Ciesla DJ, Moore EE, Zallen G, et al. Hypertonic saline attenuation
intracranial hypertension. J Neurosurg Anesth 1996;8:175–7. of polymorphonuclear neutrophil cytotoxicity: timing is everything.
22. Prough DS, Whitley J, Taylor CL, et al. Regional cerebral blood J Trauma 2000;48:388–395.
flow following resuscitation from hemorrhagic shock with hyper-
37. Junger WG, Coimbra R, Liu FC, et al. Hypertonic saline resuscita-
tonic saline. Influence of a subdural mass. Anesthesiology 1991;75:
tion: a tool to modulate immune function in trauma patients? Shock
319–27.
1997;8:235–241.
23. Fisher B, Thomas D, Peterson B. Hypertonic saline lowers raised
intracranial pressure in children after head trauma. J Neurosurg 38. Suarez AI, Qureshi AI, Parekh PD, et al. Administration of hyper-
Anesthesiol 1992;4:4–10. tonic (3%) sodium chloride/acetate in hyponatremic patients with
24. Shackford SR, Bourguignon PR, Wald SL, et al. Hypertonic saline symtomatic vasospasm following subarachnoid hemorrhage. J Neu-
resuscitation of patients with head injury: a prospective, randomized rosurg Anesthesiol 1999;11:178–84.
clinical trial. J Trauma 1998;44:50–8. 39. Guisado R, Arieff AI, Massary SG. Effects of glycerol infusion on
25. Simma B, Burger R, Falk M, et al. A prospective, randomized, and brain water and electrolytes. Am J Physiol 1974;227:865–72.
controlled study of fluid management in children with severe head 40. Di Mattio J, Hochwald GM, Malhan C, et al. Effects of changes in
injury: lactated Ringer’s solution versus hypertonic saline. Crit Care serum osmolality on bulk flow of fluid into cerebral ventricles and
Med 1998;26:1265–70. on brain water content. Pfluegers Arch 1975;359:253–64.
26. Gemma M, Cozzi S, Tommasino C, et al. 7.5% hypertonic saline 41. Ropper AH. Treatment of intracranial hypertension. In: Neurologi-
versus 20% mannitol during elective neurosurgical supratentorial cal and Neurosurgical Intensive Care. New York: Raven Press,
procedures. J Neurosurg Anesthesiol 1997;9:329–34. 1993:29-52.
27. Jaffar JJ, Johns LM. Mullan SF. The effect of mannitol on cerebral 42. Paczynski RP, Ventatesan R, Diringer MN, et al. Effects of fluid
blood flow. J Neurosurg 1986;64:754–9. management on edema volume and midline shift in a rat model of
28. Schmoker J, Zhuang J, Schackford S. Hypertonic fluid resuscitation ischemic stroke. Stroke 2000;31:1702–8.
improves cerebral oxygen delivery and reduces intracranial pressure 43. Burke AM, Quest DO, Chien S, et al: The effects of mannitol on
after hemorrhagic shock. J Trauma 1991;31:1607–13. blood viscosity. J Neurosurg 1981;55:550–553.
Journal of Neurosurgical Anesthesiology, Vol. 14, No. 3, 2002
You might also like
- Anger in Animus DevelopmentDocument2 pagesAnger in Animus DevelopmentAnca HatieganNo ratings yet
- Uterine LeiomyomaDocument57 pagesUterine LeiomyomaRomy Mansour100% (2)
- Cerebral Herniation Syndromes and Intracranial HypertensionFrom EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigNo ratings yet
- Austrilia Health CareDocument23 pagesAustrilia Health CarePandaman PandaNo ratings yet
- XareltoDocument2 pagesXareltoMichael Kuzbyt100% (1)
- Zheng 2013Document10 pagesZheng 2013Aldo ValenzuelaNo ratings yet
- Jurnal 12Document10 pagesJurnal 12Zella ZakyaNo ratings yet
- Disertasi Dr. TerawanDocument8 pagesDisertasi Dr. TerawanNurhaidah AchmadNo ratings yet
- Tranexamic Acid in NeurosurgeryDocument12 pagesTranexamic Acid in NeurosurgeryNells Jesús Olivos LozanoNo ratings yet
- Hypertonic Saline and Mannitol Therapy in Critical Care NeurologyDocument9 pagesHypertonic Saline and Mannitol Therapy in Critical Care NeurologyRonAlNo ratings yet
- Central Role For Aldose Reductase Pathway in Myocardial Ischemic InjuryDocument8 pagesCentral Role For Aldose Reductase Pathway in Myocardial Ischemic Injurysinta mahastutiNo ratings yet
- 1632 FullDocument4 pages1632 Fullyohanes0gadiNo ratings yet
- 2019 Journal of Surgical ResearchDocument8 pages2019 Journal of Surgical ResearchFernando ZanoniNo ratings yet
- Hyponatremic Encephalopathy To The Editor:: ReferencesDocument1 pageHyponatremic Encephalopathy To The Editor:: ReferencesAnonymous Us5v7C6QhNo ratings yet
- Endovascular and Neurosurgical MX of StrokeDocument18 pagesEndovascular and Neurosurgical MX of StrokeAndrei ChirtoacaNo ratings yet
- Seo2016 PDFDocument8 pagesSeo2016 PDFNovia AyuNo ratings yet
- Critical Care Management of Potential Donors Clin Transplant 2009Document8 pagesCritical Care Management of Potential Donors Clin Transplant 2009Marisol Gallego DuqueNo ratings yet
- Endovascular Management of Acute Epidural Hematomas: Clinical Experience With 80 CasesDocument7 pagesEndovascular Management of Acute Epidural Hematomas: Clinical Experience With 80 CasesDeby AnditaNo ratings yet
- Hypertonic Saline Attenuates Cord Swelling and Edema in Experimental Cord Injury - Experimental (2009) PDFDocument7 pagesHypertonic Saline Attenuates Cord Swelling and Edema in Experimental Cord Injury - Experimental (2009) PDFCoal CoalyNo ratings yet
- Evaluation of Morphological Changes in Experimental Models of Myocardial Infarction: Electron and Light Microscopical EvidenceDocument11 pagesEvaluation of Morphological Changes in Experimental Models of Myocardial Infarction: Electron and Light Microscopical EvidenceRania QhalisyaNo ratings yet
- Saline TherapyDocument3 pagesSaline Therapysatyagraha84No ratings yet
- Temporal Bone Encephalocele and Cerebrospinal Fluid FistulaDocument9 pagesTemporal Bone Encephalocele and Cerebrospinal Fluid FistulaSa'Deu FondjoNo ratings yet
- 2020 Sanjeev Physiology International 2020Document15 pages2020 Sanjeev Physiology International 2020maloymandalNo ratings yet
- Desferrioxamine Induces Delayed Tolerance Against Cerebral Ischemia in Vivo and in VitroDocument6 pagesDesferrioxamine Induces Delayed Tolerance Against Cerebral Ischemia in Vivo and in VitroJephte LaputNo ratings yet
- Finding The Right Osmotic Agent: Why Mannitol PrevailedDocument4 pagesFinding The Right Osmotic Agent: Why Mannitol PrevailedArturo FuentesNo ratings yet
- Stroke Protection by 3-Hydroxy-3-Methylglutaryl (HMG) - Coa Reductase Inhibitors Mediated by Endothelial Nitric Oxide SynthaseDocument6 pagesStroke Protection by 3-Hydroxy-3-Methylglutaryl (HMG) - Coa Reductase Inhibitors Mediated by Endothelial Nitric Oxide SynthaseVasco ClaroNo ratings yet
- Histamine Induces Endothelium-Dependenf Relaxation of Bovine Retinal ArteriesDocument7 pagesHistamine Induces Endothelium-Dependenf Relaxation of Bovine Retinal ArteriesAna IonNo ratings yet
- Anesthesiology Pain Medicine: Effect of Clonidine Premedication On Blood Loss in Spine SurgeryDocument5 pagesAnesthesiology Pain Medicine: Effect of Clonidine Premedication On Blood Loss in Spine SurgeryRizkyRNo ratings yet
- 1-S2.0-S0003999315014240-Neuromuskular Electrical SimulationDocument8 pages1-S2.0-S0003999315014240-Neuromuskular Electrical SimulationMarina UlfaNo ratings yet
- 402 FullDocument7 pages402 Fullyohanes0gadiNo ratings yet
- Effects of A Single Mannitol Bolus On CerebralDocument8 pagesEffects of A Single Mannitol Bolus On CerebralIndri WidyantiNo ratings yet
- Effects of Continuous Hypertonic Saline Infusion On Perihemorrhagic Edema EvolutionDocument8 pagesEffects of Continuous Hypertonic Saline Infusion On Perihemorrhagic Edema Evolutionwe sagara dewiNo ratings yet
- Isovolume Hypertonic Solutes Sodium ChloDocument5 pagesIsovolume Hypertonic Solutes Sodium Chlodai leNo ratings yet
- Review Article: Hydrocephalus After Subarachnoid Hemorrhage: Pathophysiology, Diagnosis, and TreatmentDocument9 pagesReview Article: Hydrocephalus After Subarachnoid Hemorrhage: Pathophysiology, Diagnosis, and TreatmentDewi DewiNo ratings yet
- Vol55 No4 Article 4Document6 pagesVol55 No4 Article 4Rizal AhmadNo ratings yet
- EFNS Congress Vienna Semax AbstractDocument60 pagesEFNS Congress Vienna Semax AbstractnontjeNo ratings yet
- Vasospasm Metaanalysis 2011Document9 pagesVasospasm Metaanalysis 2011mlannesNo ratings yet
- Jaha 119 011960Document22 pagesJaha 119 011960Rodrigo GoedertNo ratings yet
- Thrombolytic Therapy For Ischemic StrokeDocument7 pagesThrombolytic Therapy For Ischemic StrokechandradwtrNo ratings yet
- "Triple H" Therapy For Aneurysmal Subarachnoid Haemorrhage: Real Therapy or Chasing Numbers?Document0 pages"Triple H" Therapy For Aneurysmal Subarachnoid Haemorrhage: Real Therapy or Chasing Numbers?ganpur01No ratings yet
- B5W2 - Brainstem Herniation TreatmentDocument2 pagesB5W2 - Brainstem Herniation TreatmentCatherine MernaNo ratings yet
- Dipyridamole Plus Tri Usal Versus Tri Usal Alone in Infarct Reduction After Middle Cerebral Artery OcclusionDocument5 pagesDipyridamole Plus Tri Usal Versus Tri Usal Alone in Infarct Reduction After Middle Cerebral Artery OcclusionAhmad Husnul HuluqNo ratings yet
- Tsona 2010Document3 pagesTsona 2010harold.atmajaNo ratings yet
- Bruce C V Campbell Ischaemic Stroke 2019Document22 pagesBruce C V Campbell Ischaemic Stroke 2019yiyecNo ratings yet
- Hyponatremia Sah 1Document13 pagesHyponatremia Sah 1RA Tri Retno WulanNo ratings yet
- Documento PDFDocument5 pagesDocumento PDFJose Miguel CastellonNo ratings yet
- 10 1001@jamaneurol 2017 5162Document9 pages10 1001@jamaneurol 2017 5162Walter Espinoza CiertoNo ratings yet
- Joung2007-BM Mononuclear Cells - MIDocument11 pagesJoung2007-BM Mononuclear Cells - MIiulia andreeaNo ratings yet
- ICA'sDocument37 pagesICA'sVeronica TanNo ratings yet
- 12 JMSCRDocument6 pages12 JMSCRArdianNo ratings yet
- Hyperintense Vessels On FLAIR: Hemodynamic Correlates and Response To ThrombolysisDocument5 pagesHyperintense Vessels On FLAIR: Hemodynamic Correlates and Response To ThrombolysisKumail KhandwalaNo ratings yet
- PTJ 1563Document12 pagesPTJ 1563vanNo ratings yet
- Jurnal Reading DavidDocument14 pagesJurnal Reading DavidAbraham WilliamNo ratings yet
- Cardiovascular Risk: The Safety of Local Anesthesia, Vasoconstrictors, and Sedation in Heart DiseaseDocument7 pagesCardiovascular Risk: The Safety of Local Anesthesia, Vasoconstrictors, and Sedation in Heart DiseaseMARIA KARINA HERNANDEZ PEREZNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofNatalia ArizaNo ratings yet
- Dynamic Changes of - Melanocyte-Stimulating Hormone Levels in The Serum of Patients With Craniocerebral TraumaDocument6 pagesDynamic Changes of - Melanocyte-Stimulating Hormone Levels in The Serum of Patients With Craniocerebral TraumaAwilia Eka PutriNo ratings yet
- ESTUDIO - El Vendaje Neuromuscular Reduce La Presion Arterial en La Hipertension Arterial SistemicaDocument3 pagesESTUDIO - El Vendaje Neuromuscular Reduce La Presion Arterial en La Hipertension Arterial SistemicainfodhNo ratings yet
- Efficacy and Safety of Thrombolytic Therapy in ProDocument5 pagesEfficacy and Safety of Thrombolytic Therapy in ProgalalNo ratings yet
- NeuralRegenRes9184-8563115 234711Document8 pagesNeuralRegenRes9184-8563115 234711JouleAlSBNo ratings yet
- Mechanism of Dexamethasone Suppression of Brain Tumor-Associated Vascular Permeability in RatsDocument9 pagesMechanism of Dexamethasone Suppression of Brain Tumor-Associated Vascular Permeability in Ratszefri suhendarNo ratings yet
- Alteplase Data 4Document9 pagesAlteplase Data 4Muhammad FirmansyahNo ratings yet
- Abnormal Regional Cerebral Blood Flow in Cognitively Normal Elderly Subjects With HypertensionDocument7 pagesAbnormal Regional Cerebral Blood Flow in Cognitively Normal Elderly Subjects With HypertensionAminarsihNo ratings yet
- Effects of Ultrasound and Ultrasound Contrast AgenDocument10 pagesEffects of Ultrasound and Ultrasound Contrast AgenWaleed sattarNo ratings yet
- Aneurysm BJADocument17 pagesAneurysm BJAParvathy R NairNo ratings yet
- Chapter 1 Introduction - Convergence and Divergence of Opinion On Spinal ControlDocument4 pagesChapter 1 Introduction - Convergence and Divergence of Opinion On Spinal ControlChristian Donoso AguilarNo ratings yet
- Water 09 00013Document17 pagesWater 09 00013muratout3447No ratings yet
- AlcoholDocument12 pagesAlcoholLauraLoaizaNo ratings yet
- Subang Jaya BranchDocument14 pagesSubang Jaya Branchshanmuganathan maliniNo ratings yet
- MCQs 2Document2 pagesMCQs 2Yahya AlbornoNo ratings yet
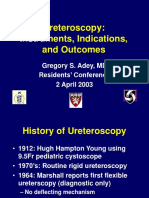
- Ureteroscopy G AdeyDocument66 pagesUreteroscopy G AdeyCentanarianNo ratings yet
- Long Term ABA Is AbusiveDocument9 pagesLong Term ABA Is AbusiveLorena MatosNo ratings yet
- Int Endodontic J - January 1995 - RAY - Periapical Status of Endodontically Treated Teeth in Relation To The TechnicalDocument8 pagesInt Endodontic J - January 1995 - RAY - Periapical Status of Endodontically Treated Teeth in Relation To The Technicalj sNo ratings yet
- Janice L. Kazmier Health Care LawDocument305 pagesJanice L. Kazmier Health Care LawDesti SetyaningrumNo ratings yet
- What Is Child Abuse?: Child Abuse or Child Maltreatment Is Physical, Sexual, or Psychological Maltreatment orDocument3 pagesWhat Is Child Abuse?: Child Abuse or Child Maltreatment Is Physical, Sexual, or Psychological Maltreatment orprincessNo ratings yet
- Clinical Practice Guidelines PDFDocument315 pagesClinical Practice Guidelines PDFDian Sulistya EkaputriNo ratings yet
- Tower WaterDocument6 pagesTower WaterberanoshNo ratings yet
- Hamp Son 2016Document18 pagesHamp Son 2016Zen Ary PrasetyoNo ratings yet
- Posibile Scaderi PretDocument18 pagesPosibile Scaderi PretDany DidiNo ratings yet
- 302333KW PDFDocument19 pages302333KW PDFdhineshNo ratings yet
- Anaphylaxis Diagnosis and ManagementDocument10 pagesAnaphylaxis Diagnosis and Managementd dNo ratings yet
- OlanzapineDocument1 pageOlanzapineKallie ChartrandNo ratings yet
- Blood Flow Restriction Rehabilitation For Extremity Weakness - A Case SeriesDocument7 pagesBlood Flow Restriction Rehabilitation For Extremity Weakness - A Case SeriesTamas KalmarNo ratings yet
- Anterior Cruciate LigamentDocument10 pagesAnterior Cruciate LigamentLaura LauraaNo ratings yet
- Chapter 4 Health and IllnessDocument31 pagesChapter 4 Health and IllnessKrishnaveni MurugeshNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaEdwin Batara SaragihNo ratings yet
- Non-Nutritive Sucking Habits: Project OverviewDocument42 pagesNon-Nutritive Sucking Habits: Project OverviewvelangniNo ratings yet
- Latent TB Infection Provider GuideDocument17 pagesLatent TB Infection Provider GuideRivani KurniawanNo ratings yet
- Drug StudyDocument12 pagesDrug Studychelsea anne80% (5)
- Seven Stages of Crisis Intervention Model PDFDocument27 pagesSeven Stages of Crisis Intervention Model PDFAngeila TolosaNo ratings yet
- Adrenal Fatigue and How To Overcome ItDocument11 pagesAdrenal Fatigue and How To Overcome ItKika Spacey Ratm0% (1)