Professional Documents
Culture Documents
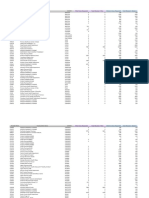
Bloodbook 2017 660 PDF
Bloodbook 2017 660 PDF
Uploaded by
Sambit DashCopyright:
Available Formats
You might also like
- Lyme Disease, Mycoplasma, and Bioweapons Development TimelineDocument71 pagesLyme Disease, Mycoplasma, and Bioweapons Development TimelineAdam F.100% (5)
- How Long Do The Vaccinated Have To Live, Stephen Fishman - James FetzerDocument2 pagesHow Long Do The Vaccinated Have To Live, Stephen Fishman - James FetzerAlan N100% (1)
- American HolocaustDocument134 pagesAmerican HolocaustEditor 1100% (2)
- Peptic Ulcer Disease-DoneDocument5 pagesPeptic Ulcer Disease-Donecory kurdapyaNo ratings yet
- The Injection Fraud - It's Not A Vaccine - Solari ReportDocument7 pagesThe Injection Fraud - It's Not A Vaccine - Solari ReportisBubba100% (1)
- Aflds White Paper: Covid-19: Experimental Vaccine CandidatesDocument35 pagesAflds White Paper: Covid-19: Experimental Vaccine CandidatesfabioNo ratings yet
- 5 Most Powerful Families That Secretly Control The WorldDocument16 pages5 Most Powerful Families That Secretly Control The WorldGino ToralbaNo ratings yet
- Danielle Charlie Ward and Simon ParkesDocument13 pagesDanielle Charlie Ward and Simon ParkesAurel100% (1)
- Transfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaDocument41 pagesTransfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaAETCM Emergency medicineNo ratings yet
- Coronabook - Full - Book - 13-5 - Web PDFDocument1,194 pagesCoronabook - Full - Book - 13-5 - Web PDFsushilNo ratings yet
- America Civil Defense 1945-1984 - FEMA (1986)Document32 pagesAmerica Civil Defense 1945-1984 - FEMA (1986)staedtlermarsNo ratings yet
- Unanswered Questions From The Vaccine Injury Compensation ProgramDocument65 pagesUnanswered Questions From The Vaccine Injury Compensation ProgramHeather X Rhodes100% (1)
- Terra PapersDocument56 pagesTerra PapersrkkriveraNo ratings yet
- The PREP Act and COVID-19: Limiting Liability For Medical CountermeasuresDocument7 pagesThe PREP Act and COVID-19: Limiting Liability For Medical CountermeasuresSkyapakaNo ratings yet
- Adrenochrome - C9H9NO3 - PubChemDocument22 pagesAdrenochrome - C9H9NO3 - PubChemMatías PierottiNo ratings yet
- The Sayings Gospel Q The Text of QDocument17 pagesThe Sayings Gospel Q The Text of QtraperchaperNo ratings yet
- White Star LineDocument9 pagesWhite Star Lineelenaanalia88No ratings yet
- Luciferase Tatoo VaxxinationDocument10 pagesLuciferase Tatoo VaxxinationHelenaNo ratings yet
- Rush To Trash HydroxychloroquineDocument34 pagesRush To Trash HydroxychloroquinesylodhiNo ratings yet
- The 'X' Chronicles Newspaper - 2018-01-02Document92 pagesThe 'X' Chronicles Newspaper - 2018-01-02Rob McConnellNo ratings yet
- Swine Flu Vac BioweaponDocument2 pagesSwine Flu Vac BioweaponThorsteinn Thorsteinsson100% (1)
- Prepared For The Coronavirus - 9 Simulations, Drills & Laws Planned For It - 28-04-2020 - Makia Freeman - Thefreedomarticles PDFDocument29 pagesPrepared For The Coronavirus - 9 Simulations, Drills & Laws Planned For It - 28-04-2020 - Makia Freeman - Thefreedomarticles PDFWolf GantNo ratings yet
- Antimatter CERN Apr 2011 NORDocument49 pagesAntimatter CERN Apr 2011 NORRekha BhasinNo ratings yet
- Crimes Against HumanityDocument13 pagesCrimes Against HumanityjayjonbeachNo ratings yet
- Viral! World Lockdown Plan Leaked: Latest NewsDocument14 pagesViral! World Lockdown Plan Leaked: Latest NewsKaroline Marx100% (1)
- Covid-19 Vaccine OrdersDocument21 pagesCovid-19 Vaccine Orders13WMAZ100% (1)
- MRNA Vaccines - Day - 04.14.20 PDFDocument259 pagesMRNA Vaccines - Day - 04.14.20 PDFTammy G100% (1)
- Gods Fury and Wrath Upon The Children of Disobedience!Document10 pagesGods Fury and Wrath Upon The Children of Disobedience!Ernie King GiroNo ratings yet
- Fetal-Free: New Product Warning Label NeededDocument11 pagesFetal-Free: New Product Warning Label Neededbethanyhengst100% (1)
- Atlanta Executive OrderDocument6 pagesAtlanta Executive OrderNewsChannel 9 StaffNo ratings yet
- How The Christian Church and U.S. Government Work Together To Traffick Children Worldwide Through The Lucrative Adoption BusinessDocument13 pagesHow The Christian Church and U.S. Government Work Together To Traffick Children Worldwide Through The Lucrative Adoption Businesspastorrlc8852100% (1)
- Who Was Bill Gates Before Microsoft?Document7 pagesWho Was Bill Gates Before Microsoft?Marvin MartinsNo ratings yet
- Remdesivir LetterDocument9 pagesRemdesivir LetterJennifer Weaver100% (2)
- History of Human CloningDocument19 pagesHistory of Human CloningAnanda IffahNo ratings yet
- The COVID-19 Lockdown EconomDocument11 pagesThe COVID-19 Lockdown EconomahlekhudaNo ratings yet
- Prev Injuries 052407Document124 pagesPrev Injuries 052407Anonymous 1sd8foGfGNo ratings yet
- The Nag Hammadi Library: The Thought of NoreaDocument2 pagesThe Nag Hammadi Library: The Thought of Noreacarmen.nitu7No ratings yet
- The Nuremburg Code (Wiki)Document4 pagesThe Nuremburg Code (Wiki)Tara AlvaradoNo ratings yet
- Fetuses in Food: Which Are Often Deceptively Labeled As "Natural Flavors"Document4 pagesFetuses in Food: Which Are Often Deceptively Labeled As "Natural Flavors"mariano martinez100% (1)
- "We're All in This Together".: Karen HudesDocument30 pages"We're All in This Together".: Karen HudesFranz Dip100% (1)
- Arrest Bill Gates HashtagDocument231 pagesArrest Bill Gates HashtagCOVID 19 CORONA VIRUS100% (1)
- Why Explosive Nuclear Devices May Not ExistDocument20 pagesWhy Explosive Nuclear Devices May Not ExistJeremy James100% (3)
- About Camp David Raven Rock Mountain ComplexDocument24 pagesAbout Camp David Raven Rock Mountain ComplexgenedandreaNo ratings yet
- Vaccines and AutismDocument9 pagesVaccines and AutismDr. Heath MotleyNo ratings yet
- Killtown 9 11 2003Document30 pagesKilltown 9 11 2003Aidan MonaghanNo ratings yet
- Text of The Antarctic Treaty, 1959Document5 pagesText of The Antarctic Treaty, 1959TURKELNo ratings yet
- Silent Revolution of Truth - Vol3 - v1-2022 - FREE EDITION - Billy Meier, Plejarens - Humanity at The CrossroadsDocument139 pagesSilent Revolution of Truth - Vol3 - v1-2022 - FREE EDITION - Billy Meier, Plejarens - Humanity at The CrossroadsSumaya WebsterNo ratings yet
- Bombshell - PCR Tests Can't Identify Delta Variant It's All FictionDocument15 pagesBombshell - PCR Tests Can't Identify Delta Variant It's All FictionNuerteNo ratings yet
- United States Patent Application - 0060257852 PDFDocument297 pagesUnited States Patent Application - 0060257852 PDFMatt OusleyNo ratings yet
- ID2020 Alliance OverviewDocument5 pagesID2020 Alliance OverviewTravis100% (1)
- Z - 2.a Hydra (1) 2021Document10 pagesZ - 2.a Hydra (1) 2021Ishrak ZamanNo ratings yet
- Defluoridation TechniquesDocument7 pagesDefluoridation TechniquesS Bharadwaj Reddy100% (1)
- The Australian Fluoridation NewsDocument12 pagesThe Australian Fluoridation Newshampshire Against100% (3)
- From Q Clearance Patriot + To All Fellow Patriots + For God and Country + The Storm Is Upon UsDocument332 pagesFrom Q Clearance Patriot + To All Fellow Patriots + For God and Country + The Storm Is Upon Ustbh100% (5)
- Why Popes Banned The BibleDocument4 pagesWhy Popes Banned The BibleLuis D. Mendoza PérezNo ratings yet
- Mebendazole Anti CancerDocument16 pagesMebendazole Anti CancerSpore FluxNo ratings yet
- Dave HodgesDocument30 pagesDave HodgesBob100% (2)
- The Great Poisoning of America Begins October 2009Document4 pagesThe Great Poisoning of America Begins October 2009wisemen2No ratings yet
- Summary of Judy Mikovits & Kent Heckenlively's Plague of CorruptionFrom EverandSummary of Judy Mikovits & Kent Heckenlively's Plague of CorruptionNo ratings yet
- Summary: : Red -Handed by Peter Schweizer: How American Elites Get Rich Helping China WinFrom EverandSummary: : Red -Handed by Peter Schweizer: How American Elites Get Rich Helping China WinNo ratings yet
- The Tribulation Hand-Book: For Those Left Behind When Jesus Christ Comes for His Church of BelieversFrom EverandThe Tribulation Hand-Book: For Those Left Behind When Jesus Christ Comes for His Church of BelieversNo ratings yet
- FigureDocument1 pageFigureSambit DashNo ratings yet
- 1471 2377 12 13 PDFDocument6 pages1471 2377 12 13 PDFSambit DashNo ratings yet
- FigureDocument1 pageFigureSambit DashNo ratings yet
- Frontiers in Neuroendocrinology: Jennifer C. Felger, Andrew H. MillerDocument13 pagesFrontiers in Neuroendocrinology: Jennifer C. Felger, Andrew H. MillerSambit DashNo ratings yet
- Emergencies and Critical Issues in Parkinson's DiseaseDocument12 pagesEmergencies and Critical Issues in Parkinson's DiseaseSambit DashNo ratings yet
- Etiology and Significance of Thrombocytopenia in Critically Ill PatientsDocument13 pagesEtiology and Significance of Thrombocytopenia in Critically Ill PatientsSambit DashNo ratings yet
- Thrombocytopenia in The Intensive Care Unit - Diagnostic Approach and ManagementDocument12 pagesThrombocytopenia in The Intensive Care Unit - Diagnostic Approach and ManagementSambit DashNo ratings yet
- 1471 2377 12 13 PDFDocument6 pages1471 2377 12 13 PDFSambit DashNo ratings yet
- Ijccm 23 S185 PDFDocument4 pagesIjccm 23 S185 PDFSambit DashNo ratings yet
- Abdul Aziz2015 PDFDocument18 pagesAbdul Aziz2015 PDFSambit DashNo ratings yet
- Pharmacokineticsand Pharmacodynamics: Optimalantimicrobial Therapyinthe IntensivecareunitDocument18 pagesPharmacokineticsand Pharmacodynamics: Optimalantimicrobial Therapyinthe IntensivecareunitSambit DashNo ratings yet
- Relevance of Routine Use of The Anaerobic Blood Culture BottleDocument5 pagesRelevance of Routine Use of The Anaerobic Blood Culture BottleSambit DashNo ratings yet
- Antibiotic Resistance, Part 2: Gram-Negative Pathogens: Catherine M. Oliphant, Pharmd, and Kathryn Eroschenko, PharmdDocument8 pagesAntibiotic Resistance, Part 2: Gram-Negative Pathogens: Catherine M. Oliphant, Pharmd, and Kathryn Eroschenko, PharmdSambit DashNo ratings yet
- 134 2018 Article 5147Document9 pages134 2018 Article 5147Sambit DashNo ratings yet
- 1.3 Soft Tissue InjuryDocument44 pages1.3 Soft Tissue InjurySylvinho46100% (1)
- Anaphy Reviewer Tissue and Integumentary SystemDocument7 pagesAnaphy Reviewer Tissue and Integumentary System10. Briol AlvinNo ratings yet
- Histology Notes: Epithelial TissueDocument4 pagesHistology Notes: Epithelial TissueSteph AsideNo ratings yet
- Concept Map - HISTOLOGYDocument1 pageConcept Map - HISTOLOGYDhon Edriel ManciaNo ratings yet
- Hemolisis (Intravaskular Dan Ekstravaskular) : Tugas PendahuluanDocument10 pagesHemolisis (Intravaskular Dan Ekstravaskular) : Tugas PendahuluanRiskullah MakmurNo ratings yet
- (Prothrombin Time) : Intended UseDocument2 pages(Prothrombin Time) : Intended UseDharmesh PatelNo ratings yet
- CBC Diagnostic ExamDocument2 pagesCBC Diagnostic ExamHoseña, Kathea Khyll BSN3No ratings yet
- Form 5 Biology Chapter 1 TransportDocument12 pagesForm 5 Biology Chapter 1 TransportMohdAmerAhmadNo ratings yet
- (S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 249Document1 page(S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 249Indah Rizka AprilianiNo ratings yet
- Minor Blood Group McqsDocument4 pagesMinor Blood Group Mcqsjehangir khanNo ratings yet
- Blood Banking ReviewDocument442 pagesBlood Banking ReviewMayra Flor100% (2)
- 3 s2.0 B9780702066962000230 MainDocument14 pages3 s2.0 B9780702066962000230 MainKate ClarksonNo ratings yet
- Red and White Blood Cell DisordersDocument11 pagesRed and White Blood Cell DisordersVittorio Di PaoloNo ratings yet
- TransesDocument2 pagesTransesGelaaaNo ratings yet
- ANA PHY Lab Activity 6 Physiology of BonesDocument5 pagesANA PHY Lab Activity 6 Physiology of Bonesriya haryaniNo ratings yet
- Connective TissueDocument4 pagesConnective TissueMahmoud AbdAllahNo ratings yet
- ABO - RH - Blood - Grouping Guidance - Manucal - 26 - 03 - 2013 PDFDocument31 pagesABO - RH - Blood - Grouping Guidance - Manucal - 26 - 03 - 2013 PDFLalrinchhanaNo ratings yet
- Anatomy & PhysiologyDocument12 pagesAnatomy & PhysiologyTyrNo ratings yet
- National Haematology Update 2022 - Flyer (13052022e)Document4 pagesNational Haematology Update 2022 - Flyer (13052022e)Alice HuiiNo ratings yet
- Idiopathic Thrombocytopenic Purpura (ITP)Document20 pagesIdiopathic Thrombocytopenic Purpura (ITP)saiibelieves0% (1)
- LAPORAN ILMIAH KEHAMILAN PATOLOGIS ANEMIA - NadiaDocument23 pagesLAPORAN ILMIAH KEHAMILAN PATOLOGIS ANEMIA - NadiaNadia Nur SalsabilaNo ratings yet
- 37 - Shock in ObstetricsDocument22 pages37 - Shock in Obstetricsdr_asaleh90% (10)
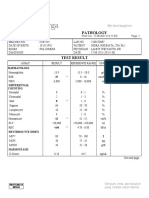
- Pathology: HaematologiDocument2 pagesPathology: HaematologiFerry SukinataNo ratings yet
- Complete Blood Count: Abdellatif Aly MohamedDocument81 pagesComplete Blood Count: Abdellatif Aly MohamedGroup 11No ratings yet
- Animal Structure and FunctionDocument49 pagesAnimal Structure and FunctionJohn Steven AalaNo ratings yet
- Cell Body Perikaryon Soma: Neural PlasticityDocument29 pagesCell Body Perikaryon Soma: Neural PlasticitymaNo ratings yet
- The Importance of Trephine Biopsy and Aspirate in Bone Marrow AnalysisDocument5 pagesThe Importance of Trephine Biopsy and Aspirate in Bone Marrow Analysisoki harisandiNo ratings yet
- ANAPHY Lec Session #14 - SAS (Agdana, Nicole Ken)Document8 pagesANAPHY Lec Session #14 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet
Bloodbook 2017 660 PDF
Bloodbook 2017 660 PDF
Uploaded by
Sambit DashOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bloodbook 2017 660 PDF
Bloodbook 2017 660 PDF
Uploaded by
Sambit DashCopyright:
Available Formats
| THROMBOCYTOPENIA IN HOSPITALIZED PATIENTS |
Assessing thrombocytopenia in the intensive care unit:
the past, present, and future
Ryan Zarychanski1,2,3 and Donald S. Houston2,3
1
Division of Hematology/Medical Oncology and 2Division of Critical Care, Department of Internal Medicine,
University of Manitoba, Winnipeg, MB, Canada; and 3Department of Medical Oncology & Hematology,
Cancercare Manitoba, Winnipeg, MB, Canada
Thrombocytopenia is common among patients admitted to the intensive care unit (ICU). Multiple pathophysiological
mechanisms may contribute, including thrombin-mediated platelet activation, dilution, hemophagocytosis, extracellular
histones, ADAMTS13 deficiency, and complement activation. From the clinical perspective, the development of
thrombocytopenia in the ICU usually indicates serious organ system derangement and physiologic decompensation
rather than a primary hematologic disorder. Thrombocytopenia is associated with bleeding, transfusion, and adverse
clinical outcomes including death, though few deaths are directly attributable to bleeding. The assessment of
thrombocytopenia begins by looking back to the patient’s medical history and presenting illness. This past information,
combined with careful observation of the platelet trajectory in the context of the patient’s clinical course, offers clues
to the diagnosis and prognosis. Management is primarily directed at the underlying disorder and transfusion of
platelets to prevent or treat clinical bleeding. Optimal platelet transfusion strategies are not defined, and a conser-
vative approach is recommended.
severity of illness, organ dysfunction, sepsis, vasopressor use, and
Learning Objectives renal failure.1,3
• Characterize the multiple mechanisms that can contribute to
thrombocytopenia in the ICU In comparison with patients who had a platelet count of .150 3 109/L,
• Evaluate the trajectory of the patient’s platelet count and apply the development of thrombocytopenia in critically ill patients is
this information to establish a diagnosis and inform prognosis associated with increased bleeding and transfusion risk.1,3,4 In the
• Transfuse platelets appropriately to prevent and manage bleed- PROTECT trial, thrombocytopenia of any severity increased the risk
ing in thrombocytopenic patients admitted to the ICU of major bleeding and was associated with increased risk of trans-
fusion with red cells, platelets, plasma, or cryoprecipitate.5 In a large
observational study, rates of major hemorrhage in patients with
Definition, incidence, and outcomes of thrombocytopenia present at ICU admission (prevalent) or with new-
onset thrombocytopenia after ICU admission (incident) were 20%
thrombocytopenia in the ICU
Thrombocytopenia is a common hematologic abnormality among and 19%, respectively, in comparison with 13% in patients without
patients admitted to the intensive care unit (ICU). In adults, the thrombocytopenia.2 Similar to the PROTECT trial, most observa-
prevalence of thrombocytopenia at the time of ICU admission tional studies have reported thrombocytopenia to be associated with
ranges from 8.3% to 67.6%. The incidence of thrombocytopenia red cell transfusion.1
developing during ICU admission ranges from 14% to 44%.1,2
Variability in these estimates reflects differences in patient pop- Among 8 observational studies that used multivariate analysis to
ulations (eg, age, severity of illness, diagnoses), ICU characteristics determine the association between thrombocytopenia and death,
(eg, medical, surgical, cardiac), and the definition of thrombocy- 6 found thrombocytopenia to be an independent predictor of
topenia across published observational studies (eg, platelet count mortality.1 Both the presence and severity of thrombocytopenia
of ,150 3 109/L, ,100 3 109/L, and sometimes ,50 3 109/L).1 have been shown to predict mortality.2,6 In the PROTECT trial,
In the PROTECT trial, a large randomized trial of thrombopro- after adjustment for age, severity of illness, baseline use of me-
phylaxis in patients admitted to medical-surgical ICUs, the in- chanical ventilation, and inotrope or vasopressor use, both mod-
cidence of new mild (100-149 3 109/L), moderate (59-99 3 109/L), erate and severe thrombocytopenia were associated with increased
and severe (,50 3 109/L) thrombocytopenia was 15.3%, ICU and hospital mortality.5 Thrombocytopenia has also been
5.1%, and 1.6%, respectively.3 Although thrombocytopenia has associated with increased ICU and hospital length of stay and need
many possible causes, risk factors commonly associated with for organ support.2 A blunted platelet recovery appears to further
ICU-acquired thrombocytopenia, in multivariate analyses, include predict increased mortality,7 whereas recovery of platelet count
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Off-label drug use: None disclosed.
660 American Society of Hematology
uncontrolled, as in disseminated intravascular coagulation (DIC). In
Box 1. Causes of thrombocytopenia in the ICU either case, platelets may be activated and consumed. In thrombo-
Common causes of thrombocytopenia in ICU patients: cytopenic patients, serial measurement of international normalized
• Sepsis ratio and fibrinogen may allow recognition of nonovert DIC.9 Re-
• Disseminated intravascular coagulation grettably, high-quality evidence to inform optimal management of
• Consumption (eg, major trauma, cardiopulmonary bypass) DIC (apart from identification and correction of the underlying cause)
• Dilution (with massive transfusion) is lacking.9
• Myelosuppressive chemotherapy
• Mechanical circulatory support devices (eg, intra-aortic bal- Antibodies. The antibodies that most often lead to thrombocyto-
loon pump) penia in ICU patients are those against the heparin-PF4 complex
Less common but important causes of thrombocytopenia that mediating heparin-induced thrombocytopenia (HIT). Even so, as was
should not be missed: discussed by L. Rice in the 2017 American Society of Hematology
• Heparin-induced thrombocytopenia Education Program, HIT is confirmed in fewer than 5% of throm-
• Hemophagocytic syndrome bocytopenic ICU patients.10 Screening tests for HIT should be
Uncommon causes of thrombocytopenia that develop during performed in any patient who has a rapid drop in platelet count
ICU admission: occurring between 5 and 10 days after first heparin exposure re-
• Drug-induced thrombocytopenia (other than heparin or cy- gardless of baseline count.10,11 Other drug-immune thrombocyto-
totoxic chemotherapy) penias involving agents such as ranitidine, b-lactam antibiotics,
• Leukemia, myelodysplasia, aplastic anemia, etc, unless ab- vancomycin, and linezolid can occur but are infrequent. For example,
normalities were already present before ICU admission although vancomycin is a recognized cause of thrombocytopenia, in
• Thrombotic thrombocytopenic purpura a major American referral laboratory, only 34 cases of vancomycin
• Immune/idiopathic thrombocytopenia antibody-dependent thrombocytopenia were confirmed over a 5-year
• Posttransfusion purpura period.12 Comprehensive and unbiased estimates of the incidence of
drug-immune thrombocytopenia are lacking. Glycoprotein IIb/IIIa
receptor antagonists are known to cause thrombocytopenia; how-
strongly predicts survival.8 As such, thrombocytopenia is a readily ever, use of these agents has declined considerably. Autoantibodies
accessible marker of clinical status among patients admitted to the (ie, immune thrombocytopenia [ITP]) are unlikely to be the cause of
ICU. thrombocytopenia in an ICU patient unless there is a previous history
of the disorder. Alloantibodies (posttransfusion purpura) are even
Mechanisms of thrombocytopenia in the ICU less common.
The mechanisms contributing to thrombocytopenia in critically
ill patients remain poorly understood. Moreover, thrombocytopenia Hemophagocytosis. Hemophagocytic syndrome (HPS) in adults
arising in an individual patient may have multiple possible causes, (also known as hemophagocytic lymphohistiocytosis or macrophage
and our tools to distinguish between them are limited. In the dis- activation syndrome) is a poorly understood process of uncontrolled
cussion that follows, we focus on the causes that are most pertinent to cytokine production and unregulated macrophage activation trig-
critically ill patients (Box 1). gered by a variety of infections, malignancies, or autoimmune
processes. It is characterized by cytopenias, fevers, splenomegaly,
Decreased production extreme hyperferritinemia, and usually (but not always) hemopha-
The extent to which decreased platelet production contributes gocytosis on bone marrow biopsy.13 Although uncommon, it is an
to thrombocytopenia in multiorgan failure is unknown and has increasingly recognized clinical entity with evolving diagnostic
never been critically assessed. Whereas inflammatory cytokines criteria.14 Bone marrow findings of hemophagocytic activity are neither
(eg, interleukin-6 [IL-6]) are known to blunt erythropoiesis, they highly sensitive nor specific. Histological evidence of hemophagocytic
stimulate thrombopoiesis. As such, decreased production is un- activity has been reported to be common in patients with thrombo-
likely to be the dominant factor unless there was preexisting marrow cytopenia and sepsis.15 However, it is unknown whether similar
disease or the patient has undergone cytotoxic chemotherapy. findings would be present in nonthrombocytopenic critically ill pa-
Thrombocytopenia associated with acute alcohol toxicity is a notable tients, and thus the contribution of hemophagocytosis to the peripheral
exception. cytopenias is uncertain.
Sequestration Histones. Extracellular histones are released during cellular injury
Splenic sequestration is usually a factor only if it was a preexisting and as part of neutrophil extracellular traps. Histones induce platelet
problem (most often in liver disease with portal hypertension), but aggregation, and infusion of histones in animal models causes a rapid
it may contribute to the severity of thrombocytopenia and reduce drop in platelet count and accompanying tissue toxicity.16 In ICU
posttransfusion platelet increments. An exception is the acute splenic patients, plasma histone levels have been shown to correlate with
sequestration crisis that can occur in infants with hemoglobin (Hb) thrombocytopenia,17 but whether the association is causal or reflects
SS and adults with sickle variants such as Hb SC. illness severity needs to be further explored.
Destruction, consumption, or both ADAMTS13 depletion. Nguyen et al have shown that ADAMTS13
The destruction or consumption of platelets likely explains the bulk of levels are reduced in sepsis, although not typically as severely as is
thrombocytopenia in the ICU. Mechanisms may include the following. seen in thrombotic thrombocytopenic purpura (TTP).18 It is un-
known whether this degree of deficiency contributes to micro-
Thrombin. Thrombin-mediated platelet activation may be physio- vascular occlusion, thrombocytopenia, or multiorgan failure in
logically appropriate but extensive, as in major surgery or trauma, or septic patients.
Hematology 2017 661
sepsis, the HALO (Heparin AnticoaguLation to improve Outcomes in
septic shock) research program investigators have recently completed
a feasibility pilot randomized trial of unfractionated heparin in septic
shock and are preparing to commence an international trial of heparin in
septic shock.25
Hemophagocytosis
Unfortunately, high-quality evidence to inform the optimal treatment
of sepsis-associated HPS in adult patients is lacking. Recommended
therapies target T cells (steroids, cyclosporine) and macrophages
(etoposide).26 Intravenous immunoglobulin (IVIG) to support de-
fective humoral immunity and reduce systematic inflammation has
also been suggested.26 Data from randomized trials suggest a po-
tential survival benefit of IVIG in patients with sepsis.27 Whether the
potential beneficial effects of IVIG correlate with the presence of
HPS is unknown.
ADAMTS13 deficiency
The possible contribution of ADAMTS13 deficiency to thrombo-
cytopenia and microvascular injury in sepsis should lead to con-
sideration of future trials evaluating plasma exchange28 or infusion
of recombinant ADAMTS13.
Figure 1. Mechanisms of thrombocytopenia in sepsis. Multiple
mechanisms have been proposed to contribute to the thrombocytopenia of
Complement
sepsis. The relative contribution of each potential mechanism may vary
A coming wave of targeted complement inhibitors, of which ecu-
among patients and within a given patient over time. DIC, disseminated
lizumab is a prototype, should permit elucidation of the comple-
intravascular coagulation.
ment’s contribution to the thrombocytopenia and other pathologies
of sepsis.
Complement activation. Immune complexes may activate the
classical pathway, and bacterial cell walls may activate the alter- How we approach thrombocytopenia in the critically
native pathway of the complement cascade. Complement can bind ill patient
and activate platelets, contributing to platelet destruction in sepsis.19 In assessing a critically ill patient with thrombocytopenia, there are
Complement activation and completion of the membrane attack 3 time frames to consider. First, the past: what is the context of the ICU
complex is a powerful platelet activator and contributor of platelet admission, and what was the platelet count profile prior to the current
destruction.6 illness? Second, the present: what is the trajectory of the platelet count,
and how does it relate to the patient’s clinical course; how severe is the
Thrombocytopenia in sepsis thrombocytopenia; and is there evidence of thrombosis? Third, the
Sepsis is a common clinical problem, accounting for 10% of ICU
admissions and roughly 50% of all thrombocytopenias in critically ill
patients, yet the mechanisms underlying thrombocytopenia in sepsis Box 2. Questions to ask when evaluating
are poorly understood.20,21 Several pathological processes likely thrombocytopenia in the ICU patient
contribute to thrombocytopenia in sepsis (Figure 1). Thrombocyto- Past:
penia may also independently modify the host immune response to • What is the context of the patient’s ICU admission?
infection.22 Consideration of the contributing mechanisms suggests • Is there evidence of a preexisting illness or the use of a drug
directions for possible therapeutic trials. known to cause thrombocytopenia?
• Could the ICU admission have been precipitated by a cata-
Thrombin strophic illness associated with thrombocytopenia, such as
Sepsis is a well-recognized trigger of DIC, largely driven by the thrombotic thrombocytopenic purpura, hemophagocytic syn-
upregulation of tissue factor expression on monocytes and other cells in drome, or acute leukemia?
response to inflammatory mediators such as endotoxin. Even in the • Was there major trauma or surgery that would consume
absence of overt DIC, markers of coagulation activation (eg, thrombin- platelets, or transfusion and fluid resuscitation that would
antithrombin complexes, prothrombin fragment 1.2) are increased. cause dilution?
Several anticoagulants, including tissue factor pathway inhibitor, anti- Present:
thrombin, and activated protein C have been evaluated in the treatment • What is the trajectory of the platelet count, and how does it
of sepsis, with negative or mixed results.23 Compared with prophylactic- relate to the patient’s clinical course?
dose unfractionated heparin or no thromboprophylaxis, the use of • How low is the platelet count?
low-molecular- weight heparin for venous thromboprophylaxis has been • Is there thrombosis?
shown to be associated with lower risk of moderate thrombocytopenia Future:
(hazard ratio, 0.62; 95% confidence interval, 0.47-0.84).3 Data from • Is the platelet count following the expected trajectory, given
published randomized trials indicate the potential for heparin to improve your analysis of the cause?
clinical outcomes in sepsis.24 To better define the role of heparin in
662 American Society of Hematology
future: what trajectory or changes in the platelet count should we • Platelets fall within the first few days and recover after the critical
expect on the basis of what we have deduced to be the cause of the illness improves: This pattern is typical of sepsis and similar non-
thrombocytopenia? (Box 2 provides questions for evaluating throm- infection-related multisystem inflammatory illness (eg, pancrea-
bocytopenia in the ICU patient.) titis, burns). In septic shock, the median time from ICU admission
to the development of thrombocytopenia (,100 3 109/L) is 2 days
(interquartile range [IQR], 1-3). The median duration of throm-
Past bocytopenia in survivors is 6 days (IQR, 4-8).29
To understand the likely causes of a patient’s thrombocytopenia, it • Platelets fall and stay low in a patient whose clinical course is
is essential to have a full picture of the prior medical history, comor- otherwise recovering: In these patients, an iatrogenic cause of
bidities, and medications (eg, cytotoxic chemotherapy, antiproliferative thrombocytopenia should be considered. In HIT, the signature
agents, and relevant antibiotics), as well as a clear framing of the illness drop in platelet count evolves over a day or 2 and occurs between
that precipitated the ICU admission. It is especially important to obtain 5 and 10 days after initial heparin exposure. Testing for HIT
previous complete blood counts, because they may show whether the antibodies, cessation of all heparin exposure, and the use of al-
patient has a preexisting disorder causing the thrombocytopenia. Pre- ternative anticoagulants are recommended.11 Posttransfusion
existing thrombocytopenia may signify an unrecognized marrow dis- purpura and other drug-related immune thrombocytopenias would
order, such as myelodysplasia or a lymphoproliferative disorder, in also follow this pattern but are far less common.
which case concomitant anemia would be likely. Thrombocytopenia • Platelets fall within the first few days and stay low in a patient with
may represent splenic sequestration due to portal hypertension, usually persistent multiorgan failure: This is the pattern observed in the
in the setting of cirrhosis, in which case mild leukopenia may also be sickest of patients who have the worst prognosis. Sepsis, DIC,
present. Alternatively, the patient may have chronic ITP, in which case HPS, and shock are possible. It is not clear to what extent the
the other counts should be normal. These conditions will persist during thrombocytopenia contributes to their poor outcomes, and in such
the critical illness, although transient pseudocorrection of the platelet patients the thrombocytopenia is probably significant mainly as an
count may occur later with the reactive rise in platelet count when the indicator of the severity of their illness.1
acute phase response sets in.
Apart from the temporal pattern of platelet counts, the severity of
The illness that precipitated ICU admission must also be fully
thrombocytopenia and the presence or absence of thrombosis are
characterized. Although the critical illness is usually obvious, pa-
readily available clues that may help to determine the mechanism of
tients may become acutely ill and require transfer to the ICU before
thrombocytopenia and the outlook for the patient. Severe throm-
a diagnosis has been established. One must consider whether the
bocytopenia (,20 3 109/L) has a much more limited differential
critical illness is one of those catastrophic multisystem disorders in
diagnosis than do milder degrees of thrombocytopenia. In the critical
which platelets are directly involved, such as an aggressive myeloid
care patient, severe thrombocytopenia is most likely to reflect one of
or lymphoid neoplasm, HPS, or TTP. Significant platelet con-
the following:
sumption may be expected when the admission was precipitated by
• Profound bone marrow failure, due to either cytotoxic chemotherapy
polytrauma or major surgery. Massive transfusion or large-volume
or an aggressive hematologic neoplasm. The absolute neutrophil and
fluid resuscitation resulting in hemodilution may also contribute to
reticulocyte counts should also be severely depressed.
a transient fall in platelet count. An underlying preexisting condition
• Overt DIC. Fibrinogen and other coagulation factors should be
such as cancer or a complicated pregnancy may predispose to DIC
consumed and tests for D-dimer and fibrin degradation products
and consequent thrombocytopenia.
should be strongly positive.
• Antibody mediated, whether autoimmune (ITP), alloimmune
(posttransfusion purpura), or drug-related immune. HIT is a notable
Present exception, in which the typical platelet nadir is .20 3 109/L.11
The trajectory of a patient’s platelet count during the ICU stay (and • Hemophagocytic syndrome.
pre-ICU hospitalization) allows inferences about likely causes and
may inform prognosis. The platelet trajectory can only be interpreted,
however, with reference to the course of the patient’s critical illness. The occurrence of thrombosis in the thrombocytopenic patient
The earliest blood test results (eg, from the emergency room or is a paradox, which should trigger consideration of HIT, anti-
hospital from which the patient was transferred) should be obtained phospholipid syndrome, and prothrombotic DIC (usually associated
to capture the complete platelet profile. with cancer, and occasionally with sepsis) as possible diagnoses.
Coagulation activation in the setting of depleted natural anticoag-
Though neither rigid nor comprehensive, we believe several distinct ulants (eg, warfarin initiation, which depletes protein C faster than
trajectories may be recognized: procoagulant factors, or after ischemic liver injury) may trigger
• Platelets are low at presentation and stay low, without apparent a process of peripheral small-vessel thrombosis and gangrene despite
relation to the course of critical illness: This pattern suggests an thrombocytopenia and despite adequate arterial inflow.30
independent cause of thrombocytopenia, such as marrow failure or
hypersplenism. Investigation directed at those possibilities could
include assessment of spleen size, review of the peripheral blood Future
film, and bone marrow examination. By scrutinizing the clinical and laboratory features of the case, in-
• Platelets fall immediately and recover quickly: In the absence cluding the trajectory of the platelet count, one aims to arrive at
of a major operative complication, this pattern is expected after a working diagnosis of the cause of thrombocytopenia. In most
major surgery, especially those procedures using cardiopulmonary instances, treatment of the thrombocytopenia is not required, but
bypass, and can be observed in patients requiring a massive establishing a diagnosis permits one to predict the future trajectory of
transfusion. the platelet count. If the count follows the projected course of
Hematology 2017 663
Figure 2. Time course of thrombocytopenia in septic shock. Mean platelet count (695% confidence interval) in patients with septic shock who developed
thrombocytopenia after ICU admission. Time axis is anchored to the day that vasopressors were discontinued (day 0). Only data for survivors are
included.29
recovery, unnecessary investigation can be avoided; conversely, thrombocytopenia is due to sepsis, prompt and appropriate anti-
timely investigation can be pursued if the platelet count deviates from microbial therapy, source control, and organ support are required.33
the anticipated course. If the thrombocytopenia is due to severe bleeding (eg, trauma),
• Surgery or trauma: with major surgery, there is typically a modest, hemostatic control is the priority. In the presence of mechanical
immediate drop in the platelet count due to consumption, he- circulatory support devices, such as intra-aortic balloon pumps,
modilution, or both. The count normally begins to rise 3 to 4 days device-related thrombocytopenia may persist and may be further
after surgery and should continue to rise over the next 10 days to influenced by underlying cardiogenic shock and multiorgan failure.
levels above baseline because of the thrombopoietic activities of Although uncertainty exists whether extracorporeal membrane ox-
IL-6 and other acute-phase cytokines; the same pattern is expected ygenation (ECMO) is independently associated with thrombocyto-
with polytrauma.31 penia, the conditions associated with the need for ECMO certainly
• Cytotoxic chemotherapy: with most cyclic chemotherapy regi- are.34 Until these underlying conditions improve, resolution of
mens, the nadir platelet count typically occurs on days 12 to 18, or platelet counts is not anticipated.
a few days longer with platinum drugs, with recovery proceeding
briskly thereafter.32 Thrombocytopenia is consistently associated with increased risks
• Septic shock: in patients with septic shock who develop throm- of bleeding, transfusion, and death; however, the effectiveness of
bocytopenia, despite signs of clinical improvement, on average, platelet transfusion to stop bleeding, reduce transfusion of other blood
platelet recovery is not anticipated until several days after vaso- components, or improve clinical outcomes is uncertain.1,3,35 The need
pressor independence. The median time from discontinuation of for evidence addressing this uncertainty is especially relevant in the
vasopressors to recovery of platelet counts above 100 3 109 per ICU. Past practices of liberally correcting abnormal laboratory values
liter is 2 days (IQR, 0-4) (Figure 2).29 (eg, hemoglobin, albumin) or aggressively supporting deranged
physiologic parameters that are recognized to be associated with poor
Management of thrombocytopenia in critical illness prognosis (eg, supranormal oxygen therapy or high tidal volume
Given that incident (new) thrombocytopenia in the ICU is generally mechanical ventilation) have either failed to benefit or harmed pa-
due to physiologic perturbation associated with increased severity tients when evaluated in randomized trials. Platelet transfusion may
of illness, treating the underlying cause of the critical illness is be associated with harm, including increased incidence of nosoco-
paramount and likely to result in improved platelet counts. If mial infection and transfusion-associated acute lung injury.36-38
664 American Society of Hematology
Table 1. Thresholds for platelet transfusion in critical illness21,38,42
Indication Platelet threshold* Strength of recommendation Quality of evidence
Severe bleeding Maintain PLT . 50 3 10 /L; 9
Strong Low
consider using an MTP
Prophylaxis in adults 10 3 109/L Moderate Low
Prior to elective central venous catheter 20 3 109/L† Weak Low
Prior to chest tube insertion or thoracentesis 50 3 109/L Weak Low
Prior to bronchoscopy with lavage 20 3 109/L Weak Low
Prior to paracentesis Not routinely required Weak Low
Prior to bone marrow biopsy Not routinely required Weak Low
Prior to elective diagnostic lumbar puncture 50 3 109/L Weak Very low
Prior to urgent diagnostic lumbar puncture 20 3 109/L Weak Very low
Prior to major elective surgery (excluding neurosurgery) 50 3 109/L Weak Very low
Prior to neurosurgery 100 3 109/L Weak Very low
Traumatic brain injury, intracranial hemorrhage 100 3 109/L Weak Low
Prior to insertion of an intraventricular drain 100 3 109/L Weak Very low
MTP, massive transfusion protocol; PLT, platelet count.
*May be modified by several factors including platelet dysfunction or other risk factors for bleeding, indication for the procedure, urgency, and medical comorbidities.
†Inserted with bedside ultrasound and by experienced personnel. Avoid noncompressible vessels if platelets are ,50 3 109 per liter. Choosing a compressible site is preferable
to platelet transfusion.
Randomized trials of transfusion strategies to treat or prevent bleeding hemorrhage is a recognized consequence of critical illness with
in thrombocytopenic ICU patients have not been conducted, and a multiple organ failure and can occur at any platelet count.
conservative approach seems warranted.
Periprocedural platelet transfusion
Therapeutic platelet transfusion Platelet transfusion is recommended to minimize bleeding during
In the context of massive transfusion, treatment of bleeding with a placement of an elective central venous catheter if the platelet
1:1:1 or a 1:2:1 ratio of red cells, plasma, and platelets is supported is ,20 3 10/L38,42 (Table 1). Data to support this recommendation
by clinical studies and widely recommended in clinical guidelines come from observational studies, of which a subset of patients were
to prevent severe thrombocytopenia or hemodilution of coagulation admitted to an ICU. In 2 large observational studies, only patients
factors. The optimal ratio of platelet concentrates in this setting with a preprocedural platelet count of ,20 or 25 3 109/L were at risk
remains unknown.39 Caring for patients requiring massive trans- for bleeding.43,44 Central venous catheters should ideally be placed
fusion is complex; comprehensive transfusion protocols can help under ultrasound guidance and by expert operators to reduce the risk
achieve transfusion goals and improve outcomes.40 In general medical- of bleeding. With the use of bedside ultrasound and clear vascular
surgical ICU patients with severe bleeding and, in the absence of windows, the incremental benefit of platelet transfusion is uncertain.
informative clinical trials, current guidelines recommend that platelet In absence of informative trials, practice variability exists. Rec-
transfusion be considered if the platelet count is ,50 3 109/L or if ommended platelet thresholds for lumbar puncture and surgical
significant platelet dysfunction is suspected or confirmed (Table 1).38 procedures are itemized in Table 1.
Platelet dysfunction is relatively common in the ICU and may be
aggravated by factors including uremia, liver failure, antiplatelet agents,
and extracorporeal circuits. The extent to which platelet transfusion can
Conclusion
Thrombocytopenia in the ICU is common, especially among those
overcome these effects is unclear.
with septic shock, and correlates with an adverse prognosis. Multiple
mechanisms may contribute to thrombocytopenia, and differentiating
Prophylactic platelet transfusion the pertinent cause (or causes) in individual patients is challenging.
Most platelet units in an ICU are transfused to prevent clinical Looking back at the patient’s medical history and presenting illness,
bleeding. Clinical trials to guide best practice are needed, and con- while observing the platelet trajectory and the clinical course, offers
siderable practice variability exists. Extrapolating from randomized clues to the diagnosis and prognosis. Pragmatic guidelines are pre-
trials evaluating prophylactic platelet transfusion in hospitalized adult sented; however, optimal platelet transfusion strategies to prevent or
patients with chemotherapy-induced hypoproliferative thrombocyto- treat bleeding in thrombocytopenic ICU patients remain to be defined.
penia, the American Association of Blood Banks (AABB) and
the Society for Critical Care Medicine (SCCM) 2016 Surviving
Sepsis Guideline recommends prophylactic platelet transfusion below Correspondence
Ryan Zarychanski, Department of Medical Oncology and Haematology,
a threshold of 10 3 109/L.33,38 This extrapolation, however, may not
Cancercare Manitoba, ON2051, 675 McDermot Ave, Winnipeg, MB
be valid; in patients admitted to medical-surgical ICUs, thrombocy-
topenia is frequently multifactorial and may be accompanied by ac- R3E 0V9, Canada; e-mail: rzarychanski@cancercare.mb.ca.
quired platelet dysfunction but also increased platelet turnover.
Furthermore, posttransfusion platelet increments and the durability References
of platelet increases are known to be attenuated in ICU patients. In 1. Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and
observational studies, the median increase in platelet count per platelet clinical significance of thrombocytopenia complicating critical illness:
transfusion was 15 3 109/L.41 It should also be recognized that major a systematic review. Chest. 2011;139(2):271-278.
Hematology 2017 665
2. Williamson DR, Lesur O, Tétrault JP, Nault V, Pilon D. Thrombocy- 24. Zarychanski R, Abou-Setta AM, Kanji S, et al; Canadian Critical Care Trials
topenia in the critically ill: prevalence, incidence, risk factors, and clinical Group. The efficacy and safety of heparin in patients with sepsis: a sys-
outcomes. Can J Anaesth. 2013;60(7):641-651. tematic review and metaanalysis. Crit Care Med. 2015;43(3):511-518.
3. Williamson DR, Albert M, Heels-Ansdell D, et al; PROTECT collab- 25. Clinicaltrials.gov. Heparin Anticoagulation to Improve Outcomes in
orators, the Canadian Critical Care Trials Group, and the Australian and Septic Shock. Available at: https://clinicaltrials.gov/ct2/show/NCT01648036.
New Zealand Intensive Care Society Clinical Trials Group. Thrombo- Accessed 4 August 2017. 2017.
cytopenia in critically ill patients receiving thromboprophylaxis: fre- 26. La Rosee P. Treatment of hemophagocytic lymphohistiocytosis in adults.
quency, risk factors, and outcomes. Chest. 2013;144(4):1207-1215. Hematology Am Soc Hematol Educ Program. 2015;2015:190-196.
4. Lauzier F, Arnold DM, Rabbat C, et al. Risk factors and impact of major 27. Alejandria MM, Lansang MA, Dans LF, Mantaring JB III. Intravenous
bleeding in critically ill patients receiving heparin thromboprophylaxis. immunoglobulin for treating sepsis, severe sepsis and septic shock.
Intensive Care Med. 2013;39(12):2135-2143. Cochrane Database Syst Rev. 2013; (9):CD001090.
5. Cook D, Meade M, Guyatt G, et al; PROTECT Investigators for the 28. Rimmer E, Houston BL, Kumar A, et al. The efficacy and safety of
Canadian Critical Care Trials Group and the Australian and New Zealand plasma exchange in patients with sepsis and septic shock: a systematic
Intensive Care Society Clinical Trials Group. Dalteparin versus un- review and meta-analysis. Crit Care. 2014;18(6):699.
fractionated heparin in critically ill patients. N Engl J Med. 2011;364(14): 29. Menard CE, Kumar A, Rimmer E, et al. Evolution & impact of
1305-1314. thrombocytopenia in septic shock. Intensive Care Med Exp. 2016;
6. Thachil J, Warkentin TE. How do we approach thrombocytopenia in 4(Suppl 1):A586.
critically ill patients? Br J Haematol. 2017;177(1):27-38. 30. Warkentin TE. Ischemic limb gangrene with pulses. N Engl J Med. 2015;
7. Nijsten MW, ten Duis HJ, Zijlstra JG, et al. Blunted rise in platelet count 373(7):642-655.
in critically ill patients is associated with worse outcome. Crit Care Med. 31. Warkentin TE, Levine MN, Hirsh J, et al. Heparin-induced thrombo-
2000;28(12):3843-3846. cytopenia in patients treated with low-molecular-weight heparin or
8. Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG. unfractionated heparin. N Engl J Med. 1995;332(20):1330-1336.
Thrombocytopenia in patients in the medical intensive care unit: bleeding 32. Basser RL, Rasko JE, Clarke K, et al. Randomized, blinded, placebo-
prevalence, transfusion requirements, and outcome. Crit Care Med. 2002;
controlled phase I trial of pegylated recombinant human megakaryocyte
30(8):1765-1771. growth and development factor with filgrastim after dose-intensive che-
9. Thachil J. Disseminated intravascular coagulation: a practical approach. motherapy in patients with advanced cancer. Blood. 1997;89(9):3118-3128.
Anesthesiology. 2016;125(1):230-236.
33. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign:
10. Rice L. HITs and misses of 100 years of heparin. Hematology Am Soc
international guidelines for management of sepsis and septic shock: 2016.
Hematol Educ Program. 2017;2017:667-673.
Crit Care Med. 2017;45(3):486-552.
11. Warkentin TE. Heparin-induced thrombocytopenia in critically ill pa-
34. Abrams D, Baldwin MR, Champion M, et al. Thrombocytopenia and
tients. Semin Thromb Hemost. 2015;41(1):49-60.
extracorporeal membrane oxygenation in adults with acute respiratory
12. Von Drygalski A, Curtis BR, Bougie DW, et al. Vancomycin-induced
failure: a cohort study. Intensive Care Med. 2016;42(5):844-852.
immune thrombocytopenia. N Engl J Med. 2007;356(9):904-910.
35. Ning S, Barty R, Liu Y, Heddle NM, Rochwerg B, Arnold DM. Platelet
13. Allen CE, McClain KL. Pathophysiology and epidemiology of hemo-
transfusion practices in the ICU: data from a large transfusion registry.
phagocytic lymphohistiocytosis. Hematology Am Soc Hematol Educ
Chest. 2016;150(3):516-523.
Program. 2015;2015:177-182.
14. Nikiforow S, Berliner N. The unique aspects of presentation and di- 36. Aubron C, Flint AW, Bailey M, et al. Is platelet transfusion associated
with hospital-acquired infections in critically ill patients? Crit Care.
agnosis of hemophagocytic lymphohistiocytosis in adults. Hematology
Am Soc Hematol Educ Program. 2015;2015:183-189. 2017;21(1):2.
15. François B, Trimoreau F, Vignon P, Fixe P, Praloran V, Gastinne H. 37. Tariket S, Sut C, Hamzeh-Cognasse H, et al. Transfusion-related acute
Thrombocytopenia in the sepsis syndrome: role of hemophagocytosis lung injury: transfusion, platelets and biological response modifiers.
and macrophage colony-stimulating factor. Am J Med. 1997;103(2): Expert Rev Hematol. 2016;9(5):497-508.
114-120. 38. Kaufman RM, Djulbegovic B, Gernsheimer T, et al; AABB. Platelet
16. Fuchs TA, Bhandari AA, Wagner DD. Histones induce rapid and pro- transfusion: a clinical practice guideline from the AABB. Ann Intern
found thrombocytopenia in mice. Blood. 2011;118(13):3708-3714. Med. 2015;162(3):205-213.
17. Alhamdi Y, Abrams ST, Lane S, Wang G, Toh CH. Histone-associated 39. Hallet J, Lauzier F, Mailloux O, et al. The use of higher platelet: RBC
thrombocytopenia in patients who are critically ill. JAMA. 2016;315(8): transfusion ratio in the acute phase of trauma resuscitation: a systematic
817-819. review. Crit Care Med. 2013;41(12):2800-2811.
18. Nguyen TC, Cruz MA, Carcillo JA. Thrombocytopenia-associated 40. Bawazeer M, Ahmed N, Izadi H, McFarlan A, Nathens A, Pavenski K.
multiple organ failure and acute kidney injury. Crit Care Clin. 2015; Compliance with a massive transfusion protocol (MTP) impacts patient
31(4):661-674. outcome. Injury. 2015;46(1):21-28.
19. Ojha A, Nandi D, Batra H, et al. Platelet activation determines the se- 41. Lieberman L, Bercovitz RS, Sholapur NS, Heddle NM, Stanworth SJ,
verity of thrombocytopenia in dengue infection. Sci Rep. 2017;7:41697. Arnold DM. Platelet transfusions for critically ill patients with throm-
20. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. bocytopenia. Blood. 2014;123(8):1146-1151, quiz 1280.
2013;369(21):2063. 42. Estcourt LJ, Birchall J, Allard S, et al; British Committee for Standards
21. Greinacher A, Selleng S. How I evaluate and treat thrombocytopenia in in Haematology. Guidelines for the use of platelet transfusions. Br J
the intensive care unit patient. Blood. 2016;128(26):3032-3042. Haematol. 2017;176(3):365-394.
22. Claushuis TA, van Vught LA, Scicluna BP, et al; Molecular Diagnosis 43. Haas B, Chittams JL, Trerotola SO. Large-bore tunneled central venous
and Risk Stratification of Sepsis Consortium. Thrombocytopenia is as- catheter insertion in patients with coagulopathy. J Vasc Interv Radiol.
sociated with a dysregulated host response in critically ill sepsis patients. 2010;21(2):212-217.
Blood. 2016;127(24):3062-3072. 44. Zeidler K, Arn K, Senn O, Schanz U, Stussi G. Optimal preprocedural
23. Levi M, van der Poll T. Coagulation and sepsis. Thromb Res. 2017;149: platelet transfusion threshold for central venous catheter insertions in
38-44. patients with thrombocytopenia. Transfusion. 2011;51(11):2269-2276.
666 American Society of Hematology
You might also like
- Lyme Disease, Mycoplasma, and Bioweapons Development TimelineDocument71 pagesLyme Disease, Mycoplasma, and Bioweapons Development TimelineAdam F.100% (5)
- How Long Do The Vaccinated Have To Live, Stephen Fishman - James FetzerDocument2 pagesHow Long Do The Vaccinated Have To Live, Stephen Fishman - James FetzerAlan N100% (1)
- American HolocaustDocument134 pagesAmerican HolocaustEditor 1100% (2)
- Peptic Ulcer Disease-DoneDocument5 pagesPeptic Ulcer Disease-Donecory kurdapyaNo ratings yet
- The Injection Fraud - It's Not A Vaccine - Solari ReportDocument7 pagesThe Injection Fraud - It's Not A Vaccine - Solari ReportisBubba100% (1)
- Aflds White Paper: Covid-19: Experimental Vaccine CandidatesDocument35 pagesAflds White Paper: Covid-19: Experimental Vaccine CandidatesfabioNo ratings yet
- 5 Most Powerful Families That Secretly Control The WorldDocument16 pages5 Most Powerful Families That Secretly Control The WorldGino ToralbaNo ratings yet
- Danielle Charlie Ward and Simon ParkesDocument13 pagesDanielle Charlie Ward and Simon ParkesAurel100% (1)
- Transfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaDocument41 pagesTransfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaAETCM Emergency medicineNo ratings yet
- Coronabook - Full - Book - 13-5 - Web PDFDocument1,194 pagesCoronabook - Full - Book - 13-5 - Web PDFsushilNo ratings yet
- America Civil Defense 1945-1984 - FEMA (1986)Document32 pagesAmerica Civil Defense 1945-1984 - FEMA (1986)staedtlermarsNo ratings yet
- Unanswered Questions From The Vaccine Injury Compensation ProgramDocument65 pagesUnanswered Questions From The Vaccine Injury Compensation ProgramHeather X Rhodes100% (1)
- Terra PapersDocument56 pagesTerra PapersrkkriveraNo ratings yet
- The PREP Act and COVID-19: Limiting Liability For Medical CountermeasuresDocument7 pagesThe PREP Act and COVID-19: Limiting Liability For Medical CountermeasuresSkyapakaNo ratings yet
- Adrenochrome - C9H9NO3 - PubChemDocument22 pagesAdrenochrome - C9H9NO3 - PubChemMatías PierottiNo ratings yet
- The Sayings Gospel Q The Text of QDocument17 pagesThe Sayings Gospel Q The Text of QtraperchaperNo ratings yet
- White Star LineDocument9 pagesWhite Star Lineelenaanalia88No ratings yet
- Luciferase Tatoo VaxxinationDocument10 pagesLuciferase Tatoo VaxxinationHelenaNo ratings yet
- Rush To Trash HydroxychloroquineDocument34 pagesRush To Trash HydroxychloroquinesylodhiNo ratings yet
- The 'X' Chronicles Newspaper - 2018-01-02Document92 pagesThe 'X' Chronicles Newspaper - 2018-01-02Rob McConnellNo ratings yet
- Swine Flu Vac BioweaponDocument2 pagesSwine Flu Vac BioweaponThorsteinn Thorsteinsson100% (1)
- Prepared For The Coronavirus - 9 Simulations, Drills & Laws Planned For It - 28-04-2020 - Makia Freeman - Thefreedomarticles PDFDocument29 pagesPrepared For The Coronavirus - 9 Simulations, Drills & Laws Planned For It - 28-04-2020 - Makia Freeman - Thefreedomarticles PDFWolf GantNo ratings yet
- Antimatter CERN Apr 2011 NORDocument49 pagesAntimatter CERN Apr 2011 NORRekha BhasinNo ratings yet
- Crimes Against HumanityDocument13 pagesCrimes Against HumanityjayjonbeachNo ratings yet
- Viral! World Lockdown Plan Leaked: Latest NewsDocument14 pagesViral! World Lockdown Plan Leaked: Latest NewsKaroline Marx100% (1)
- Covid-19 Vaccine OrdersDocument21 pagesCovid-19 Vaccine Orders13WMAZ100% (1)
- MRNA Vaccines - Day - 04.14.20 PDFDocument259 pagesMRNA Vaccines - Day - 04.14.20 PDFTammy G100% (1)
- Gods Fury and Wrath Upon The Children of Disobedience!Document10 pagesGods Fury and Wrath Upon The Children of Disobedience!Ernie King GiroNo ratings yet
- Fetal-Free: New Product Warning Label NeededDocument11 pagesFetal-Free: New Product Warning Label Neededbethanyhengst100% (1)
- Atlanta Executive OrderDocument6 pagesAtlanta Executive OrderNewsChannel 9 StaffNo ratings yet
- How The Christian Church and U.S. Government Work Together To Traffick Children Worldwide Through The Lucrative Adoption BusinessDocument13 pagesHow The Christian Church and U.S. Government Work Together To Traffick Children Worldwide Through The Lucrative Adoption Businesspastorrlc8852100% (1)
- Who Was Bill Gates Before Microsoft?Document7 pagesWho Was Bill Gates Before Microsoft?Marvin MartinsNo ratings yet
- Remdesivir LetterDocument9 pagesRemdesivir LetterJennifer Weaver100% (2)
- History of Human CloningDocument19 pagesHistory of Human CloningAnanda IffahNo ratings yet
- The COVID-19 Lockdown EconomDocument11 pagesThe COVID-19 Lockdown EconomahlekhudaNo ratings yet
- Prev Injuries 052407Document124 pagesPrev Injuries 052407Anonymous 1sd8foGfGNo ratings yet
- The Nag Hammadi Library: The Thought of NoreaDocument2 pagesThe Nag Hammadi Library: The Thought of Noreacarmen.nitu7No ratings yet
- The Nuremburg Code (Wiki)Document4 pagesThe Nuremburg Code (Wiki)Tara AlvaradoNo ratings yet
- Fetuses in Food: Which Are Often Deceptively Labeled As "Natural Flavors"Document4 pagesFetuses in Food: Which Are Often Deceptively Labeled As "Natural Flavors"mariano martinez100% (1)
- "We're All in This Together".: Karen HudesDocument30 pages"We're All in This Together".: Karen HudesFranz Dip100% (1)
- Arrest Bill Gates HashtagDocument231 pagesArrest Bill Gates HashtagCOVID 19 CORONA VIRUS100% (1)
- Why Explosive Nuclear Devices May Not ExistDocument20 pagesWhy Explosive Nuclear Devices May Not ExistJeremy James100% (3)
- About Camp David Raven Rock Mountain ComplexDocument24 pagesAbout Camp David Raven Rock Mountain ComplexgenedandreaNo ratings yet
- Vaccines and AutismDocument9 pagesVaccines and AutismDr. Heath MotleyNo ratings yet
- Killtown 9 11 2003Document30 pagesKilltown 9 11 2003Aidan MonaghanNo ratings yet
- Text of The Antarctic Treaty, 1959Document5 pagesText of The Antarctic Treaty, 1959TURKELNo ratings yet
- Silent Revolution of Truth - Vol3 - v1-2022 - FREE EDITION - Billy Meier, Plejarens - Humanity at The CrossroadsDocument139 pagesSilent Revolution of Truth - Vol3 - v1-2022 - FREE EDITION - Billy Meier, Plejarens - Humanity at The CrossroadsSumaya WebsterNo ratings yet
- Bombshell - PCR Tests Can't Identify Delta Variant It's All FictionDocument15 pagesBombshell - PCR Tests Can't Identify Delta Variant It's All FictionNuerteNo ratings yet
- United States Patent Application - 0060257852 PDFDocument297 pagesUnited States Patent Application - 0060257852 PDFMatt OusleyNo ratings yet
- ID2020 Alliance OverviewDocument5 pagesID2020 Alliance OverviewTravis100% (1)
- Z - 2.a Hydra (1) 2021Document10 pagesZ - 2.a Hydra (1) 2021Ishrak ZamanNo ratings yet
- Defluoridation TechniquesDocument7 pagesDefluoridation TechniquesS Bharadwaj Reddy100% (1)
- The Australian Fluoridation NewsDocument12 pagesThe Australian Fluoridation Newshampshire Against100% (3)
- From Q Clearance Patriot + To All Fellow Patriots + For God and Country + The Storm Is Upon UsDocument332 pagesFrom Q Clearance Patriot + To All Fellow Patriots + For God and Country + The Storm Is Upon Ustbh100% (5)
- Why Popes Banned The BibleDocument4 pagesWhy Popes Banned The BibleLuis D. Mendoza PérezNo ratings yet
- Mebendazole Anti CancerDocument16 pagesMebendazole Anti CancerSpore FluxNo ratings yet
- Dave HodgesDocument30 pagesDave HodgesBob100% (2)
- The Great Poisoning of America Begins October 2009Document4 pagesThe Great Poisoning of America Begins October 2009wisemen2No ratings yet
- Summary of Judy Mikovits & Kent Heckenlively's Plague of CorruptionFrom EverandSummary of Judy Mikovits & Kent Heckenlively's Plague of CorruptionNo ratings yet
- Summary: : Red -Handed by Peter Schweizer: How American Elites Get Rich Helping China WinFrom EverandSummary: : Red -Handed by Peter Schweizer: How American Elites Get Rich Helping China WinNo ratings yet
- The Tribulation Hand-Book: For Those Left Behind When Jesus Christ Comes for His Church of BelieversFrom EverandThe Tribulation Hand-Book: For Those Left Behind When Jesus Christ Comes for His Church of BelieversNo ratings yet
- FigureDocument1 pageFigureSambit DashNo ratings yet
- 1471 2377 12 13 PDFDocument6 pages1471 2377 12 13 PDFSambit DashNo ratings yet
- FigureDocument1 pageFigureSambit DashNo ratings yet
- Frontiers in Neuroendocrinology: Jennifer C. Felger, Andrew H. MillerDocument13 pagesFrontiers in Neuroendocrinology: Jennifer C. Felger, Andrew H. MillerSambit DashNo ratings yet
- Emergencies and Critical Issues in Parkinson's DiseaseDocument12 pagesEmergencies and Critical Issues in Parkinson's DiseaseSambit DashNo ratings yet
- Etiology and Significance of Thrombocytopenia in Critically Ill PatientsDocument13 pagesEtiology and Significance of Thrombocytopenia in Critically Ill PatientsSambit DashNo ratings yet
- Thrombocytopenia in The Intensive Care Unit - Diagnostic Approach and ManagementDocument12 pagesThrombocytopenia in The Intensive Care Unit - Diagnostic Approach and ManagementSambit DashNo ratings yet
- 1471 2377 12 13 PDFDocument6 pages1471 2377 12 13 PDFSambit DashNo ratings yet
- Ijccm 23 S185 PDFDocument4 pagesIjccm 23 S185 PDFSambit DashNo ratings yet
- Abdul Aziz2015 PDFDocument18 pagesAbdul Aziz2015 PDFSambit DashNo ratings yet
- Pharmacokineticsand Pharmacodynamics: Optimalantimicrobial Therapyinthe IntensivecareunitDocument18 pagesPharmacokineticsand Pharmacodynamics: Optimalantimicrobial Therapyinthe IntensivecareunitSambit DashNo ratings yet
- Relevance of Routine Use of The Anaerobic Blood Culture BottleDocument5 pagesRelevance of Routine Use of The Anaerobic Blood Culture BottleSambit DashNo ratings yet
- Antibiotic Resistance, Part 2: Gram-Negative Pathogens: Catherine M. Oliphant, Pharmd, and Kathryn Eroschenko, PharmdDocument8 pagesAntibiotic Resistance, Part 2: Gram-Negative Pathogens: Catherine M. Oliphant, Pharmd, and Kathryn Eroschenko, PharmdSambit DashNo ratings yet
- 134 2018 Article 5147Document9 pages134 2018 Article 5147Sambit DashNo ratings yet
- 1.3 Soft Tissue InjuryDocument44 pages1.3 Soft Tissue InjurySylvinho46100% (1)
- Anaphy Reviewer Tissue and Integumentary SystemDocument7 pagesAnaphy Reviewer Tissue and Integumentary System10. Briol AlvinNo ratings yet
- Histology Notes: Epithelial TissueDocument4 pagesHistology Notes: Epithelial TissueSteph AsideNo ratings yet
- Concept Map - HISTOLOGYDocument1 pageConcept Map - HISTOLOGYDhon Edriel ManciaNo ratings yet
- Hemolisis (Intravaskular Dan Ekstravaskular) : Tugas PendahuluanDocument10 pagesHemolisis (Intravaskular Dan Ekstravaskular) : Tugas PendahuluanRiskullah MakmurNo ratings yet
- (Prothrombin Time) : Intended UseDocument2 pages(Prothrombin Time) : Intended UseDharmesh PatelNo ratings yet
- CBC Diagnostic ExamDocument2 pagesCBC Diagnostic ExamHoseña, Kathea Khyll BSN3No ratings yet
- Form 5 Biology Chapter 1 TransportDocument12 pagesForm 5 Biology Chapter 1 TransportMohdAmerAhmadNo ratings yet
- (S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 249Document1 page(S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 249Indah Rizka AprilianiNo ratings yet
- Minor Blood Group McqsDocument4 pagesMinor Blood Group Mcqsjehangir khanNo ratings yet
- Blood Banking ReviewDocument442 pagesBlood Banking ReviewMayra Flor100% (2)
- 3 s2.0 B9780702066962000230 MainDocument14 pages3 s2.0 B9780702066962000230 MainKate ClarksonNo ratings yet
- Red and White Blood Cell DisordersDocument11 pagesRed and White Blood Cell DisordersVittorio Di PaoloNo ratings yet
- TransesDocument2 pagesTransesGelaaaNo ratings yet
- ANA PHY Lab Activity 6 Physiology of BonesDocument5 pagesANA PHY Lab Activity 6 Physiology of Bonesriya haryaniNo ratings yet
- Connective TissueDocument4 pagesConnective TissueMahmoud AbdAllahNo ratings yet
- ABO - RH - Blood - Grouping Guidance - Manucal - 26 - 03 - 2013 PDFDocument31 pagesABO - RH - Blood - Grouping Guidance - Manucal - 26 - 03 - 2013 PDFLalrinchhanaNo ratings yet
- Anatomy & PhysiologyDocument12 pagesAnatomy & PhysiologyTyrNo ratings yet
- National Haematology Update 2022 - Flyer (13052022e)Document4 pagesNational Haematology Update 2022 - Flyer (13052022e)Alice HuiiNo ratings yet
- Idiopathic Thrombocytopenic Purpura (ITP)Document20 pagesIdiopathic Thrombocytopenic Purpura (ITP)saiibelieves0% (1)
- LAPORAN ILMIAH KEHAMILAN PATOLOGIS ANEMIA - NadiaDocument23 pagesLAPORAN ILMIAH KEHAMILAN PATOLOGIS ANEMIA - NadiaNadia Nur SalsabilaNo ratings yet
- 37 - Shock in ObstetricsDocument22 pages37 - Shock in Obstetricsdr_asaleh90% (10)
- Pathology: HaematologiDocument2 pagesPathology: HaematologiFerry SukinataNo ratings yet
- Complete Blood Count: Abdellatif Aly MohamedDocument81 pagesComplete Blood Count: Abdellatif Aly MohamedGroup 11No ratings yet
- Animal Structure and FunctionDocument49 pagesAnimal Structure and FunctionJohn Steven AalaNo ratings yet
- Cell Body Perikaryon Soma: Neural PlasticityDocument29 pagesCell Body Perikaryon Soma: Neural PlasticitymaNo ratings yet
- The Importance of Trephine Biopsy and Aspirate in Bone Marrow AnalysisDocument5 pagesThe Importance of Trephine Biopsy and Aspirate in Bone Marrow Analysisoki harisandiNo ratings yet
- ANAPHY Lec Session #14 - SAS (Agdana, Nicole Ken)Document8 pagesANAPHY Lec Session #14 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet