Professional Documents
Culture Documents
Actividad Fisica y Salud Osea 2019 PDF
Actividad Fisica y Salud Osea 2019 PDF
Uploaded by
Lalito Manuel Cabellos AcuñaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Actividad Fisica y Salud Osea 2019 PDF
Actividad Fisica y Salud Osea 2019 PDF
Uploaded by
Lalito Manuel Cabellos AcuñaCopyright:
Available Formats
Review
Physical activity and skeletal health in adults
Jane A Cauley*, Lora Giangregorio*
The purpose of this Review is to examine the associations between physical activity and skeletal health, with an Lancet Diabetes Endocrinol 2019
emphasis on observational studies with fracture outcomes and randomised controlled trials (RCTs) of physical activity Published Online
interventions in adults older than 40 years. In general, increased physical activity—primarily leisure time activity or November 20, 2019
https://doi.org/10.1016/
moderate or vigorous physical activity—is associated with a 1–40% lower risk of hip and all fractures. The primary
S2213-8587(19)30351-1
limitation of these studies relates to health status; healthy people are more likely to exercise and less likely to fracture.
*Contributed equally
Although there is no sufficiently powered RCT of exercise with a fracture outcome, there is evidence that some types
Graduate School of Public
of exercise prevent falls and bone loss, and meta-analyses support the anti-fracture effectiveness of exercise. RCTs and Health, Department of
meta-analyses suggest that programmes combining impact exercise with moderate or high-intensity progressive Epidemiology, University of
resistance exercise might maintain or improve bone mass and prevent fractures, and that functional strength and Pittsburgh, Pittsburgh, PA,
USA (J A Cauley PhD); and
balance training prevents falls.
BC Matthews Hall and
Lyle S Hallman Institute,
Introduction one on vertebral fractures.26 We graded all of the studies Department of Kinesiology,
Osteoporosis is a major public health problem.1 according to our search strategy criteria. Physical activity University of Waterloo,
Waterloo, ON, Canada
Worldwide, one in two women aged 50 years or older and was typically measured once at baseline, except in one
(L Giangregorio PhD)
one in five men aged 50 years or older will have an study that measured it four times across 15 years.25 The
Correspondence to:
osteoporotic fracture in their lifetime.1–3 In 2005, more studies defined physical activity as work activity,9,10,12,16 Dr Jane A Cauley, Graduate
than 2 million fractures were reported in the USA alone, “leisure time” activity,9,10,12–16,18,23,25 “exercise”, 12,16,19,20 “home School of Public Health,
with a total cost of US$19 billion. The number of activities”,10,13 “commuting activities” (eg, driving a car, Department of Epidemiology,
fractures is expected to increase by 48% to more than biking, or walking),12 “sports”, and overall activity.13,17 One University of Pittsburgh,
Pittsburgh, PA 15261, USA
3 million in the USA by 2025, costing $25·3 billion.4 prospective study measured physical activity objectively jcauley@pitt.edu
Osteoporosis-related fractures impose substantial using wearable devices,22 and the follow-up duration
burden of disability, costs, morbidity, and mortality.1,5 ranged from 2·3 years16 to more than 30 years.9 Six papers
Physical activity, defined as “any bodily movement studied men only,9,13,17,19,22,23 seven studied women
produced by skeletal muscle that requires energy only,11,12,14,18,22,25,26 and five studied both.10,15,16,20,21 Participants’
expenditure”,6 might be a modifiable risk factor for ages ranged from 40 years to 97 years.
osteoporotic fractures. However, the prevalence of physical
inactivity is high; only 16% of US adults aged 65 years or Hip fracture
older met both aerobic and muscle strengthening Trimpou and colleagues9 studied 7495 randomly selected
guidelines.7 Within the EU, less than a third of adults men in Gothenburg, Sweden, who were followed up for
declared that they spend at least 150 min/week being more than 30 years. High physical activity during leisure
physically active.8 time was associated with reduced risk of hip fracture, but
In this Review, we aim to provide a broad perspective high physical activity at work was associated with
on the association between physical activity and fracture increased risk. However, once occupational class was
risk from prospective observational studies and RCTs. added to the multivariable model, the association between
We chose a narrative review rather than a systematic work activity and hip fracture was no longer significant,
review to incorporate different study designs and suggesting confounding by socioeconomic status. The
research questions, to address evolving areas in which strengths of the study include its generalisability, length
there is insufficient evidence to do a systematic review, of follow-up, and adjustment for confounding, and its
and to connect ideas across various content (eg, fall limitations include the non-specific assessment of
prevention, physical activity and fracture epidemiology, physical activity. In the UK, Moayyeri and colleagues10
and clinical trials on the effect of exercise interventions studied about 15 000 men and women enrolled in the
on bone strength). We discuss the types of activity that European Prospective Investigation into Cancer (EPIC)
might prevent osteoporotic fractures, and we highlight Norfolk study. Stair climbing increased the risk of hip
knowledge gaps. fracture in men by a factor of three, perhaps because of
an increased exposure to falls, but there was no association
Prospective observational studies of physical in women. Walking for leisure or transport was suggestive
activity and fractures of reduced risk of hip fracture in women (ptrend=0·049)
We identified 18 prospective observational studies and men (ptrend=0·078). There was no association between
published between 2009 and 2019 that examine the housework activity, cycling, swimming, or television
association between physical activity and incident fractures viewing and hip fracture. This study has many strengths,
in individuals aged 40 years or older (table). These studies including its generalisability, inclusion of both men and
include ten on hip fractures,9–18 eight on low trauma or women, assessment of multiple activity domains, and
non-spinal fractures,10,15,19–24 two on wrist fractures,14,25 and documentation of fractures.
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 1
Review
A study by Jokinen and collegaues11 involved the risk of hip fracture. There was no association with
1681 women aged 70–73 years for 10 years. There was no commuting, occupation, training activities, or cycling.
association between leisure activity and hip fractures in This study involved a younger cohort (40–60 years) than
general, but low physical activity was associated with is often studied, and hip fractures are rare in this age
three times the risk of cervical hip fractures. This study group. Nevertheless, the study has various strengths,
was limited by only assessing 53 hip fractures but was including its population-based design, confirmation
unique in its examination by type of hip fracture. The of fracture, and multivariable adjustments for key
Umea Fracture and Osteoporosis study12 used a nested covariates.
case-control design and identified 81 women with an Mackey and colleagues13 studied 5682 men enrolled in
incident hip fracture, matching them with two controls the US population-based Osteoporotic Fractures in Men
by age and assessment date. Walking above and beyond (MrOS) study. In unadjusted analyses, men with the
commuting activity at least once a week was associated highest physical activity (quartile 4) had a 50% reduced
with an 84% reduction in hip fracture. Moderate to high risk of hip fracture. However, in analyses that controlled
spare-time activities were also associated with reducing for confounding, this association was no longer
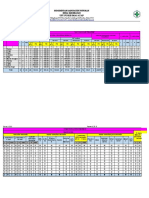
Participant Participant Follow-up Exposure Outcome Results Comments Quality
number and sex age range (years) (fractures) rating
(mean,
years)
Hip fractures
Trimpou et al9 7495 men 46–56 >30 PA at work and leisure; 451 hip fractures Leisure PA: HR 0·79 (95% CI 0·68–0·92); Work PA not associated with Good
(2010); (mean age scored 1–4 for PA: from EMR; uses work PA: HR 1·12 (1·01–1·24) fractures after adjustment
Sweden NA) 1=inactive or sedentary; International for social class; adjusted for
2=moderate Classification of age, lifestyle, BMI, and
(≤4 h/week; general Disease codes history of stroke and
office work); 3=more dementia; no BMD given
strenuous (walking or
lifting); 4=regular hard
competitive (training
or heavy manual work)
Moayyeri 6514 women; 40–79 (62) 7·5 PA questionnaire about 504 fractures Low PA: HR 1·00 for both men and Population-based therefore Good
et al10 (2010); 8389 men the past year; measured (164 hip fractures) women; moderate housework PA: HR highly generalisable;
UK, EPIC PA in and around from EMR for any fracture 1·76 (95% CI 1·18–2·60) adjusted for age, height,
Norfolk study home, at work, in for men, 0·58 (0·40–0·85) for women; BMI, lifestyle, and QUS; no
transportation to work, HR for hip fracture 0·85 (0·40–1·80) for association apparent with
and recreational PA men, 0·34 (0·19–0·61) for women; high cycling, swimming, or TV
housework PA: HR for any fracture 2·63 viewing; walking for leisure
(1·55–4·45) for men, 0·60 (0·42–0·86) associated with decreased
for women; HR for hip fracture 1·51 risk of hip fracture in women
(0·60–0·38) for men, 0·43 (0·25–0·74)
for women
Jokinen et al11 1681 women 70–73 10 Paffenbarger leisure 53 confirmed hip No association of PA with all hip Study includes small number Poor
(2010), time PA questionnaire; fractures, including fractures, but association with cervical of hip fractures and has low
Finland measured participation 32 cervical fractures hip fracture; moderate or more PA: power; adjusted for age,
in PA at age 15 years, and 21 trochanter HR 1·00; low PA: HR 3·86 (95% CI BMI, physical performance,
30 years, 50 years, and fractures 1·37–7·74) low mobility, and QUS
currently
Englund et al12 100 000 women 40–60 8·4 Measured commuting 81 confirmed hip Never walking: OR 1·00; walking once Nested case-control, Good
(2011); (57·2) PA, occupational PA, fractures; per week: OR 0·14 (95% CI 0·04–0·53); adjusted for height, weight,
Sweden, leisure PA, and training 237 controls walking two or more times per week: smoking, and menopausal
Umea Fracture PA matched on age OR 0·33 (0·10–1·01); low leisure PA: status; no BMD; no
and OR 1·00; moderate leisure PA: OR 0·19 association of fractures with
Osteoporosis (0·08–0·46); high leisure PA: OR 0·17 commuting PA, occupational
Study (0·05–0·64) PA, training PA, or cycling;
younger cohort and hip
fractures are rare
Mackey et al13 5682 men ≥65 (≈72) 6·3 Used Physical Activity 95 hip fractures Low PA: HR 1·00; moderate PA: HR 0·85 Adjusted for lifestyle, Good
(2011); USA, Scale for Elderly (95% CI 0·52–1·28); high PA: HR 0·79 demographics, physical
MrOS (includes overall (0·40–1·76) performance, and BMD; HR
household and leisure calculated from inverse
time activities); Q1=low probability of treatment
PA; Q2–3=moderate PA; weighting; also gives other
Q4=high PA statistical approaches with
similar results
(Table continues on next page)
2 www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1
Review
Participant Participant Follow-up Exposure Outcome Results Comments Quality
number and sex age range (years) (fractures) rating
(mean,
years)
(Continued from previous page)
Armstrong 1 155 304 women 50–84 (56) 8·3 Frequency of strenuous Self-reported Strenuous PA: rarely or never: RR 1·00 No association of PA with Good
et al14 (2012), activity and any fractures: for both ankle and hip fractures; PA wrist fracture; adjusted for
UK, Million exercise 6807 ankle once per week: RR 1·03 (95% CI age, region, socioeconomic
Women Study fractures, 0·99–1·08) for ankle fractures, 0·74 status, lifestyle, hormone
9733 wrist (0·70–0·79) for hip fractures; PA more therapy, and comorbidities;
fractures, and than once per week: RR 1·06 (1·01–1·17) no BMD given
5267 hip fractures for ankle fractures, 0·63 (0·59–0·67)
for hip fractures; ptrend= 0·05 for ankle
fractures, 0·001 for hip fractures.
Any exercise: rarely or never doing any:
RR 1·00 for both ankle and hip
fractures; once per week: RR 1·01
(0·96–1·07) for ankle fractures, 0·78
(0·74–0·84) for hip fractures; two or
three times per week: RR 1·00
(0·95–1·06) for ankle fractures,
0·67 (0·63–0·72) for hip fractures;
four or more times per week: RR 1·11
(1·06–1·16) for ankle fractures,
0·72 (0·68–0·76) for hip fractures;
ptrend=0·004 for ankle fractures, <0·001
for hip fractures
Morseth et al15 3450 men; 55–97 11·6 Measured leisure time 1693 confirmed Sedentary: HR 1·00 for any Adjusted for age, smoking, Good
(2012); 4072 women (66·7) PA (h/week) for low non-vertebral non-vertebral, weight-bearing, or hip BMI, height, and previous
Norway activity (no sweat) and fractures; 194 hip fracture. Non-vertebral fractures: low fractures; no BMD given;
hard activity (sweat, fractures; PA: HR 0·86 (95% CI 0·64–1·17) for no association of PA and
out of breath); PA 274 weight-bearing men, 0·90 (0·77–1·04) for women; non-weight bearing bone
variable in analysis: fractures moderate to high PA: HR 0·71 fracture or distal forearm
sedentary=<3 h/week, (0·53–0·95) for men, 0·90 (0·77–1·05) fracture
moderate=3–6 h/week, for women; ptrend=0·006 for men and
high=≥6 h/week 0·150 for women. Weight-bearing
fractures: low PA: HR 0·72 (0·51–1·03)
for men, 0·82 (0·66–1·01) for women;
moderate to high PA: HR 0·63
(0·45–0·88) for men, 0·77 (0·62–0·95)
for women; ptrend=0·003 for men, 0·013
for women. Hip fractures: low PA:
HR 0·71 (0·47–1·07) for men, 0·86
(0·69–1·08) for women; moderate to
high PA: HR 0·60 (0·41–0·90) for men,
0·74 (0·58–0·94) for women;
ptrend=0·005 for men, 0·016 for women
Lai et al16 84 532 women; ≥45 (≈60) 2·3 Measured number of 293 confirmed hip PA ≤5 METs: RR 1·00; 5–9 METs: RR 0·57 Adjusted for age, sex, Good
(2013); 73 525 men times in past week of fractures (95% CI 0·41–0·79); 9–14 METs: RR 0·60 lifestyle, hormone therapy,
Australia, walking continually (0·44–0·83); PA ≥14 METs: RR 0·49 socioeconomic status, BMI,
45 and Up (≥10 min), vigorous (0·34–0·70); ptrend<0·01 height, previous fractures,
Study activity, or moderate and QUS; PA not significant
activity; PA converted after adjusting for physical
into METs units functioning;
population-based study
Cauley et al17 5994 men ≥65 (≈73) 8·6 Used Physical Activity 178 confirmed hip 1 SD increase in PA; adjusted for age, Adding BMD to the model Good
(2016); USA, Scale for Elderly fractures race, and clinic: HR 0·84 (95% CI attenuated the association
MrOS 0·71–0·99); adjusted for age, race, clinic,
and BMD: HR 0·89 (0·75–1·05)
Gregson et al18 4286 women 59–80 6·7 Composite PA score 140 self-reported No association of fractures with PA; Included women with Poor
(2010); UK, (69·1) developed from usual wrist or hip p=0·30 previous hip or wrist
British duration of walking, fractures fractures; adjusted for age,
Women’s cycling, fitness class, leg length, marital status,
Heart and aerobics, swimming, lifestyle, socioeconomic
Health s tudy jogging, tennis, golf, status, and chronic disease
running, squash,
bowling, or gardening
(Table continues on next page)
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 3
Review
Participant Participant Follow-up Exposure Outcome Results Comments Quality
number and sex age range (years) (fractures) rating
(mean,
years)
(Continued from previous page)
All clinical fractures
Thomas-John 257 men ≥70 (72) 3 Recorded history of 41 low-trauma No association between PA and fracture Selection bias (all individuals Fair
et al19 (2009); exercise fractures from EMR were veterans from a single
USA site); low power; no BMD
given; PA not included in
final multivariable model
Lee et al20 4732 men; 40–69 3·8 Measured regular 195 self-reported, Women: RR 0·58 (95% CI 0·34–0·98); Adjusted for age, BMI, Fair
(2010); Korea 4619 women (≈53) exercise (any exercise low-trauma men: RR 1·26 (0·75–2·13) menopausal status, previous
done for <30 min/day) fractures fracture, hip circumference,
dairy intake, alcohol,
osteoarthritis, rheumatoid
arthritis, and QUS; lower
study power in men (men:
61 fractures; women:
124 fractures)
Rouzi et al21 707 women ≥50 (61) 5·2 Used 7-day PA scale 138 confirmed, low Low PA (Q1) vs Q2, Q3, and Q4: RR 2·87 Adjusted for age, grip Fair
(2012); (0–27); Q1 vs Q2, Q3, trauma, (95% CI 1·88–4·38) strength, BMI, serum
Saudi Arabia and Q4 non-vertebral 25-hydroxyvitamin D-1
fractures alpha hydroxylase, calcium
intake, and BMD; PA
population attributable
risk=49·5% similar to age;
18% lost to follow-up
Cauley et al22 2731 men 72–100 3·5 Objective measures of 1861 confirmed Sedentary activity: Q1 (low PA): HR 0·72 Adjusted for age, race, clinic, Good
(2013); USA, PA; SenseWear Pro non-vertebral (95% CI 0·43–1·20); Q2 PA: HR 0·65 season, health status,
MrOS Armband for 7 days; fractures (0·39–1·08); Q3 PA: HR 0·83 (0·53–1·30); height, weight, smoking,
measured TEE Q4 PA: HR 0·93 (0·60–1·42); ptrend=0·09. diabetes, fracture history,
(kcal/day), active EE, TEE: Q1 (low PA): HR 1·71 (0·94–3·11); Q2 and BMD
and sedentary activity PA: HR 1·70 (1·01–2·85); Q3 PA: HR 0·90
(kcal/day) (0·52–1·56); Q4 PA: HR 1·00 (0·59–1·68);
ptrend=0·020
Nikander 2780 women; ≥50 (≈60) 5 Self-reported leisure 258 self-reported, Walking (for women): never: OR 1·00; No association of fracture Poor
et al23 (2011); 2129 men time PA; measured low-trauma one or two times per week: OR 1·28 and total PA, categories of
Australia, total sedentary time fractures in (95% CI 0·92–1·80); three to five times PA, or sedentary time;
Diabetes, and total PA: total time women; 49 in men per week: OR 1·19 (0·85–1·66); six or adjusted for age, BMI,
Obesity, and spent and frequency of more times per week: OR 1·46 physical functioning, history
Lifestyle Study walking (h/week) or (1·05–2·03); ptrend=0·05 of fracture, cardiovascular
doing other moderate disease, smoking, calcium
to vigorous activities intake, and serum
25-hydroxyvitamin D-1
alpha hydroxylase; no BMD
given
Holloway-Kew 656 men 67–81 (74) 6·3 Recorded sports score: Any fracture (82), Household activity: OR 0·85 (0·51–1·41) Adjusted for age, smoking, Good
et al24 (2018); time in sports MOF (58); for any fracture, 0·84 (0·47–1·50) for falls, comorbidity, calcium
Australia, (accounting for confirmed by MOF; leisure activity: OR 0·98 intake, mobility, and BMD
Geelong Study intensity and duration), radiology records (0·95–1·01) for any fracture, 0·98
household activity, and (0·95–1·02) for MOF; sports
leisure activity participation: OR 0·52 (0·29–0·91) for
any fracture, 0·48 (0·24–0·95) for MOF
Wrist fractures
Rikkonen 8560 women 47–56 15 Measured PA in winter 830 wrist fractures Q1 (low PA): HR 1·00; Q2 PA: HR 1·24 Adjusted for age, BMI, Poor
et al25 (2010); (52·2) and summer in h/week confirmed by (95% CI 1·02–1·52); Q3 PA: HR 1·14 menopausal status, calcium
Finland at baseline, with 5 year, medical record. (0·93–1·40); Q4 PA: HR 1·24 (1·02–1·52) intake, hormone use, and
10 year, and 15 year fracture history; no BMD
follow-up, summed given; population based; PA
and divided into unrelated to overall fracture
quartiles; mostly leisure risk; increased PA associated
activities with decreased femoral neck
bone loss
(Table continues on next page)
4 www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1
Review
Participant Participant Follow-up Exposure Outcome Results Comments Quality
number and sex age range (years) (fractures) rating
(mean,
years)
(Continued from previous page)
Vertebral fractures
Nakamura 23 757 women 40–69 10 Measured PA as average Vertebral fracture, Sedentary activities: <3 h/day: No association with walking Good
et al26 (2014); (53·7) time per day of heavy or self-reported. RR 1·00; 3–8 h/day: RR 0·60 (95% CI or standing (h/day or
Japan strenuous work or 0·4–0·83); ≥8 h/day: RR 0·22 METs/day); borderline trend
exercise, being (0·05–0·85); ptrend=0·0002 (p=0·070) for increasing
sedentary, walking, and frequency of sports activities
standing; converted and lower vertebral fractures;
into METs; sports adjusted for age,
activity: less than once bodyweight, calcium intake,
per month; once to lifestyle; no BMD given
three times per month;
once or twice per week;
three or more times per
week
PA=physical activity. EMR=electronic medical record. HR=hazard ratio. BMD=bone mineral density. EPIC=European Prospective Investigation in Cancer. Lifestyle=alcohol consumption and smoking.
QUS=quantitative ultrasound. MET=metabolic equivalent. NA=not available. OR=odds ratio. MrOS=Osteoporotic Fracture in Men Study. Q=quintile. RR=relative risk. MOF=major osteoporotic fracture (wrist,
spine, proximal humerus, hip). TEE=total energy expenditure. EE=energy expenditure.
Table: Prospective observational studies of physical activity and fractures
significant. This study was underpowered (<100 hip of activity on BMD could account for at least part of the
fractures) but well designed. observed reduction in fractures.
The Million Women Study14 is a large, well designed
prospective study of almost 1·2 million UK women All clinical fractures
recruited for breast cancer screening, which showed that Thomas-John and colleagues19 studied 257 men from a
increased frequency of strenuous activity and any exercise Veterans Administration Medical Center, but their
was associated with a 37% lower risk of self-reported information on physical activity was limited to “a history
hip fracture. Morseth and colleagues15 considered of exercise”. There was no association of activity with
7522 individuals enrolled in the population-based study fracture, and this study of highly selected men was poor
in Tromsø, Norway, including 3450 men and 4072 women. with little information on physical activity and low power.
Moderate to high leisure activity was associated with a Lee and colleagues20 studied 4732 men and 4619 women
40% reduction in hip fracture in men and a 26% reduction enrolled in the Korean Health and Genome Study, a
in women. Lai and colleagues16 analysed individuals prospective population-based study from one rural and
enrolled in the 45 and Up Study, in which increasing one urban community. Women who reported regular
physical activity was associated with a significantly exercise, meaning more than 30 min/day, had a
reduced risk of hip fracture. However, when physical 42% reduced risk of any fracture. There was no association
activity models were adjusted for physical functioning, between physical activity and fractures in men, which
the association was no longer significant, suggesting that perhaps reflects lower power, because the number of
effects of activity on functioning account for the fracture fractures in men was half that in women.
benefit. There was a statistically significant interaction In the EPIC Norfolk study,10 men who reported
between physical activity and physical functioning. In moderate or high housework activity had a significantly
people with high physical functioning, there was no increased risk of any fractures, whereas women who
association with hip fracture, but in people with low reported moderate household activity had a reduced risk.
physical functioning, individuals with the lowest physical The nature of the household activity could have differed
activity had an increased risk of hip fracture (RR 3·67, in men and women; men might have participated in
95% CI 2·33–5·79) compared with those with both high activities with greater risk of falling than did women.
physical functioning and high activity. These studies had Nikander23 studied 2780 women and 2129 men, finding
various strengths and were rated as good.14–16 that increased frequency of walking was associated with
A second population-based MrOS study, by Cauley and an increased risk of fractures in women, perhaps due to
colleagues,17 followed up on risk factors for hip fracture greater exposure to falls. Neither men nor women who
among 5994 men. One standard deviation increase in met the current physical activity guidelines were
physical activity was associated with a 16% reduction in protected against fractures. There was no association of
risk of hip fracture in minimally adjusted models. The fractures with sedentary time. Although this study was
association was attenuated, however, after adjusting for unique in its inclusion of sedentary time, fractures were
hip bone mineral density (BMD), suggesting that effects self-reported and there were few fractures in men.
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 5
Review
In their Tromsø study, Morseth and colleagues15 outdoor activities, such as cross-country skiing. These
collected information on leisure time activity per week, results are consistent with an earlier study that suggested
ranked as low activity (no sweat) and hard activity (sweat, that wrist fractures tend to occur in healthier, more
out of breath). Men with greater leisure time activity had active, younger postmenopausal women than in less
a reduced risk of any non-vertebral fracture, but this healthy, less active, older postmenopausal women.27
association was not significant in women. Increasing
leisure activity was associated with a reduced risk of Vertebral fractures
fracture at weight-bearing sites but not at non-weight- Finally, a Japanese study examined the association between
bearing sites. Rouzi and colleagues21 studied 707 randomly physical activity and self-reported vertebral fracture in a
selected women from Saudi Arabia, finding low physical large cohort of 23 757 women aged 40–69 years.26 Women
activity to be associated with almost three times the risk who engaged in strenuous activity (<1 h/day) had a lower
of low-trauma fracture. This study was unique in risk of vertebral fracture than did those who did not engage
adjusting for a comprehensive set of physiological and in strenuous activity (RR 0·52, 95% CI 0·28–0·97). A long
physical function variables. duration of sedentary activity was associated with a reduced
A third MrOS study, by Cauley and colleagues,22 risk of vertebral fractures, and there was no association
involved 2731 men and measured physical activity between fractures and walking or standing. We rated this
objectively by using accelerometry. There was an study as poor because of its reliance on self-reported
increased risk of non-vertebral fracture in men with vertebral fractures. The agreement between self-reported
low (quintile 1) total energy expenditure (ptrend=0·020) and confirmed vertebral fractures is low (51%),28 and only a
and active energy expenditure (ptrend=0·040), whereas quarter to a third of vertebral fractures are clinically
there was no statistically significant association recognised.29,30
between low sedentary activity and risk of fracture in
men (ptrend=0·09). The results suggested that 30 min Discussion of observational studies and future research
moderate activity per day was associated with reduced Of the 18 prospective studies, we rated 11 as good, four as
fracture risk. fair, and three as poor (table; and according to the criteria
The Geelong Osteoporosis Study24 is a population- in the search strategy and selection criteria panel). The
based study of men in southeast Australia. Information high-quality prospective studies mostly suggested that
on physical activity was categorised into sports, increasing physical activity—primarily via leisure time
household, and leisure activities, each with separate activities or moderate or vigorous activity—was
scores. Men who reported doing sports had a reduced associated with a reduced risk of hip fractures and all
risk of any fracture and major osteoporotic fractures fractures.9,10,12,14,15,21,24 Two studies associated higher physical
(wrist, spine, proximal humerus, hip), but there was no activity at work with an increased risk of fracture in
association with household activity or leisure activity. men.9,10 A single study used objective measures of
physical activity and showed a decreased risk of any non-
Wrist fractures vertebral fracture with increasing activity.22 Wrist
In the Million Women Study,14 physical activity had no fractures could be the exception; increasing physical
effect on ankle and wrist fracture. Gregson and activity was associated with an increased risk of fracture
colleagues18 studied women enrolled in the British in one study,25 but there was no association in another.18 A
Women’s Heart and Health study, a cohort study of single study, graded as poor, examined vertebral fractures
women randomly selected from general practitioner and found no association.26
lists, which had a 60% response rate. There was no Reliance on self-reported physical activity and its vague
association between leisure activity and self-reported definitions prevent researchers from making conclusive
combined hip and wrist fracture. The association inferences or deriving useful recommendations for
between physical activity and hip fracture9,10,12,15,16 and wrist frequency, intensity, time, and type of activity. Lower
fracture25 has been shown to vary, whereby it might be intensity activities and unstructured activities, which
protective against hip fracture but might increase the account for most total energy expenditure, are more
risk of wrist fracture. Hence, combining these two difficult to quantify using self-report than is time spent
fracture sites may have cancelled out the effects of in sports activities. Self-report is subject to recall bias and
physical activity. overestimated physical activity; current recommendations
Rikkonen and colleagues25 studied 8560 women with a are to include objective measurements.31 Higher intensity
mean age of 52 years, in a population-based study in activities are easier to recall, yet few older individuals,
Finland. A long-term activity variable was created by especially those at high risk of hip fractures, engage in
summing up the average weekly hours spent at baseline moderate to vigorous activity.22 Assignment of metabolic
and at each of three follow-up visits. Physical activity was equivalent values to activities does not take into
unrelated to overall fracture risk, but increased activity consideration the effects of age on energy expenditure.
was associated with increased risk of wrist fracture. Wrist Future research should consider measuring impact or
fractures followed a seasonal pattern and were related to intensity with wearable devices. Most of the studies
6 www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1
Review
assessed physical activity only once and could not account the anti-fracture efficacy of exercise in adults older than
for changes in it through follow-up. Most studies 60 years.34,37–40
adjusted for important covariates, such as BMI, which is
important because increased BMI is associated with RCTs of exercise and effects on bone health outcomes
reduced physical activity but lower risk of fracture.32 Only When pooled together, RCTs of exercise in older adults
six studies adjusted for a measure of skeletal strength to older than 60 years reveal a modest but consistent effect
test whether the association with physical activity was of exercise on bone strength outcomes. A systematic
independent of bone strength. Early-life exposure to review reported that exercise in postmenopausal women
physical activity is important but was not considered. might have modest effects on volumetric BMD (distal
As with any observational study, residual confounding tibia) and cortical volumetric BMD (tibial shaft).41 A
by unmeasured factors is a limitation. The most subsequent RCT reported no effect of training on tibial
important confounding variable in studies of physical volumetric BMD with external resistance (more than
activity in older adults is health status and comorbidity; twice per week), compared with exercises using only
only five studies adjusted for comorbidity or health bodyweight as resistance.42 However, 16–20% of
status. Healthy people exercise, and it is highly likely that participants were using bisphosphonates, which could
individuals with poor health were under-represented in limit bone cell responses to exercise.
these studies. Moreover, exercise and physical activity are Meta-analyses have reported BMD response to
broad terms; teasing out the effects of different activities exercise,43–46 resistance training,47 walking,48 water-based
or exercise types is difficult in cohort studies that use exercise,49 and tai chi.50,51 Water-based exercise might be
self-report or accelerometers. less effective than land-based exercise,49 and tai chi had
little effect on bone health.50,51 A 2011 meta-analysis of the
RCTs of exercise and fracture risk effects of exercise on BMD in postmenopausal women
A common approach of RCTs examining the effects of pooled RCTs of all exercise types together, reporting a
exercise on bones is to align exercise mode or intensity between-group difference in favour of the effects of
with osteogenic mechanical loading characteristics,33,34 exercise on BMD at the lumbar spine but no significant
such that exercise interventions include high magnitude difference at the hip.34 Heterogeneity in the effect was
forces from impact (ground reaction forces) or muscle explained in part by exercise mode or intensity. For
pull on bones. Examples include progressive impact, example, walking or weight-bearing exercise is often
progressive resistance training (muscle pull), or their touted as good for bones, but lower impact activities,
combination. Impact activities are those in which one or such as walking or tai chi, had no effect on hip BMD and
both feet leave and return to the ground, applying a a modest effect on spinal BMD. Similarly, low-intensity
ground reaction force. Running, plyometric exercises resistance or balance exercise had no effect on hip or
(involving rapid stretch followed by muscle contraction), spinal BMD.34,52 Factors such as training intensity, change
jumping, and drop jumps are moderate or high impact in lean mass, age, and compliance could be associated
activities (depending on the height and ground reaction with the magnitude of the effect on BMD.51–53
forces). Alternatively, it could be advantageous to design Other research suggests that progressive resistance
exercise to reduce the risk of falls, because the majority training (PRT) combined with impact activities could
of non-vertebral fractures occur from a fall. Examples best benefit bone strength.34,54 A meta-analysis of
include balance training and functional training.35 24 studies (1769 postmenopausal women) reported that
Individual tailoring of exercise and progression are PRT combined with high-impact or weight-bearing
important to ensure sufficient training stimulus. exercise significantly increased BMD at the femoral neck
(standardised mean difference [SMD] 0·41, 95% CI
Do RCTs show that exercise can reduce fracture risk? 0·18–0·65; p=0·001) and lumbar spine (SMD 0·43,
There is strong evidence that exercise can reduce falls, 0·16–0·70; p=0·002).47 A 2012 meta-analysis reported
particularly exercise that includes functional strength that the effect of resistance or impact exercise was more
and balance training.36 In meta-analyses examining the favourable than controls for the femoral neck (n=1632;
effects of exercise on falls or fall-related injuries, few standardised effect size of g=0·288; 95% CI 0·10 to 0·47;
studies report fracture outcomes. A network meta- p=0·002) and lumbar spine (g=0·179; −0·003 to 0·361;
analysis revealed that exercise was the only single p=0·05).53 These results suggest that only six patients
intervention that was effective for preventing fall-related would need to be treated with exercise for one
injuries (OR 0·51, 95% CI 0·33–0·79; absolute risk postmenopausal woman to maintain or increase lumbar
difference –0·67, 95% CI –1·10 to –0·24).37 A Cochrane spine or hip BMD, translating to a 20-year relative
meta-analysis of ten studies (n=4047) reported that reduction in fracture risk of 10–11%.53 Whether this
exercise might reduce the number of people having one estimate would be true in people with low BMD is not
or more fall-related fractures (RR 0·73, 95% CI known.
0·56–0·95), but the evidence was judged to be of low Another exercise variable is the speed of movement
certainty.36 However, RCTs and meta-analyses support during exercise. High-velocity PRT trains muscular
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 7
Review
Panel 1: Exercise guidelines or recommendations published in the past 5 years in partnership with one or more osteoporosis
societies
Osteoporosis Canada: Too Fit To Fracture82 Balance exercises
Multicomponent exercise programme, including resistance • Two or three times per week at a challenging intensity
training, balance exercise, and aerobic physical activity; Spine-caring exercises
recommends against aerobic physical activity to the exclusion • For example, safe movements and back extensor exercises
of resistance and balance training • Two or three times per week (might need daily for back pain),
Progressive resistance training with a focus on endurance: ten repetitions held for 3–5 s
• 2 or more days per week; 8–12 repetitions maximum
Exercise and Sports Science Australia and Osteoporosis
Balance exercises Australia86
• Daily; sufficient intensity to challenge balance Moderate to high impact loading
Aerobic physical activity • 4–7 days per week, 50 jumps per session
• 150 min per week or more of moderate to vigorous physical • For individuals at moderate risk, more than four times
activity that involves weight-bearing or impact activity bodyweight; for individuals at high risk, two to three times
(moderate if individuals are at high risk) bodyweight
Posture awareness training Progressive resistance training
• Attention to posture, spine-sparing strategies, exercises for • Twice per week, at high to very high intensity
back extensor muscles; daily, with emphasis on endurance Balance training
UK Royal Osteoporosis Society: Strong, Steady, and • Four sessions per week at a challenging intensity
Straight83–85 European Society for Clinical and Economic Aspects of
Weight-bearing or impact exercise Osteoporosis and Osteoarthritis, and the Committees of
• For example, low jumps, skipping, hopping, jogging, stairs, Scientific Advisors and National Societies of the
marching or brisk walking, and walking International Osteoporosis Foundation (IOF)87
• Most days of the week, at moderate intensity for 50 min • Regular weight-bearing exercise should be advised, tailored
(but at low intensity and for 20 min if individual is frail, less to the needs and abilities of the individual patient
mobile, or has vertebral or multiple other fractures) • This advice was a guideline for the management of
Muscle strengthening osteoporosis, rather than a guideline focused on exercise;
• Two or three times per week, involving 2–3 sets of around the patient resources listed are those from the IOF website,
8–12 repetitions maximum which might not be associated with the guideline
power rather than strength; the emphasis is on moving ability to make inferences about exercise in people with
against resistance in the shortest amount of time to osteoporosis. Bone adaptations to loading are more
improve explosive power (ie, the concentric phase of the impaired in older than younger bone, and the threshold
movement is performed rapidly). An RCT of high-velocity for stimulating bone formation with mechanical loading
PRT with diverse, moderate impact exercises and balance could be higher in older bone.33,59–61 Moderate-intensity or
training reported statistically significant gains in BMD at high-intensity PRT can increase muscle strength.62
the femoral neck and lumbar spine (1·0–1·1%; p<0·05) Emerging research is examining whether combined
in older men and women without osteoporosis or fracture impact exercise and PRT can increase BMD in people
history.55 Only four studies have reported on the effects of with low bone mass. A small trial of impact, strength, and
exercise on BMD in men older than 45 years, and none balance exercises in women with osteopenia reported a
have studied men with osteoporosis.38,56–58 modest between-group difference in total hip BMD in
Impact exercise has a modest effect on the BMD of the favour of exercise.63 A study of 8 months of high-intensity,
femoral neck but not that of the spine, and PRT alone or progressive impact exercise and high-intensity PRT
in combination with impact exercise could give the most compared with unsupervised, low-intensity home exercise
benefit.56 Objectively measured moderate to vigorous reported significant between-group differences in change
physical activity was positively associated with peripheral scores for lumbar spine BMD (+2·9% [SD 2·8] for exercise
quantitative CT bone indices at the tibia but not the group vs –1·2% [2·8] for control; p<0·001) and femoral
radius in 1228 men and women aged 70 years.58 neck BMD (+0·3% [2·6] vs –1·9% [2·6]; p=0·004).54
Associations were stronger for peak vertical accelerations Studies like these should be replicated in individuals at
than for other directions. moderate or high risk of fracture. Exercise RCTs in
Many exercise RCTs in men or postmenopausal women individuals at high risk of fracture are sparse with small
have targeted individuals with normal BMD, or were sample sizes, and often have moderate or high risk of
heterogeneous with respect to BMD, limiting researchers’ bias.64
8 www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1
Review
Intermittently supervised home-based exercises Assessing what to recommend
(eg, stretching, training with resistance bands or Exercise recommendations to optimise bone health
bodyweight, or aerobic physical activity) in individuals might need to vary between children and adults, and with
with vertebral fracture had no significant effect on baseline fracture risk. In general, national physical
BMD.65 Another study reported that after kyphoplasty, activity guidelines are appropriate, recommending a
comprehensive treatment (ie, calcium, vitamin D, minimum of 150 min of moderate to vigorous aerobic
calcitonin, and back extensor strengthening) increased activity per week and strength training twice per week.
lumbar BMD compared with calcium and vitamin D Osteoporosis-specific guidelines, summarised in panel 1,
alone, but the risk of bias was high.66 There is less are not that different, but they emphasise moderate-
certainty regarding the balance between benefits and intensity or high-intensity PRT, and impact and balance
harms of exercise in people with osteoporosis, because training.88–90 To tailor general physical activity guidelines
most studies are not long enough or do not have adequate to optimise bone health, the recommendation is to choose
sample sizes to assess harms. daily moderate-impact or high-impact exercises and
Fear of falling, fracture, or injury could present a ensure that patients do not do aerobic activity to the
barrier to exercise participation in people with low exclusion of PRT. Many older adults walk for exercise, but
BMD. People with osteoporosis want to know what type few participate in strength training or balance training,91,92
of exercise programme is safe and effective,67,68 but as recommended by guidelines.88 The benefits observed
qualitative enquiry with clinicians reveals that they are in trials of physical activity or exercise might not be
fearful of recommending exercises to their patients achieved or sustained if the activities are discontinued or
with osteoporosis that might increase fracture risk.69 if adherence is suboptimal, and therefore strategies to
They are fearful of providing guidance on lifting, so maintain participation should be considered in terms of
they tell patients to avoid lifting more than 10 lbs their real-world application. Indeed, implementation
(4–5 kg).69 Patients can be referred to community-based, science related to physical activity participation for fall
gentle exercise programmes, but these programmes and fracture prevention is an important research priority.88
often deliver low-intensity exercise with little pro All adults, including those with osteoporosis, should
gression and are unlikely to increase BMD or muscle participate in a PRT programme targeting major muscle
strength.34,62 groups, at moderate or high intensity. A basic PRT
The benefits of exercise probably outweigh the risks, programme (appendix) might include a pull exercise See Online for appendix
and reports of fractures due to exercise have been (eg, lateral pull down, and seated, kneeling, or standing
infrequent.70 A meta-analysis suggests that exercise does row), a push exercise (eg, wall, counter, or floor pushup,
not increase the risk of hospitalisation or premature and bench press), lower extremity exercises (eg, squat,
death.71 In fact, sensitivity analyses reveal that in clinical step-ups, and lunges), and a shoulder raise or press.
populations (eg, cardiac disease, cognitive impairment), Exercises for back extensors and abdominals are
exercise participation reduced mortality. Joint pain or recommended to support the spine (eg, modified curl up,
muscle strain are the most commonly reported exercise- bird-dog, and side plank), and the intensity is prescribed
related adverse events.70,72 In trials of moderate-intensity to promote endurance (eg, repeated or prolonged holds).
PRT for 5–24 months in people older than 50 years (total Exercise professionals can guide individuals on how to
n=737), in which 43 had osteoporosis based on BMD and regress exercises to make them easier (eg, unweighted or
320 were osteopenic, there were no fractures or serious seated), but the exercises need to be progressed to more
adverse events that were deemed to be related to challenging versions once the form is learned. Daily
exercise.73–76 In a trial of home exercise in women with bouts of impact exercise can be introduced, progressively
vertebral fractures, there was one fall but no serious increasing the magnitude of impact.89 Individuals
adverse events.77 Although activity-related fractures have unaccustomed to impact exercise might need to start
been reported,65,72,78–80 a systematic review suggests that with PRT to build strength before initiating impact
positive effects probably outweigh the potential harms.70 exercise. Individuals at moderate or high risk of fracture
In a Cochrane review of exercise after osteoporotic might consider a progression from lower impact
vertebral fracture, there were two exercise-related challenges (eg, heel drops) to moderate impact (eg, hops
fractures in nine trials.64 The LIFTMOR trial81 in high- and jumps) or high impact (eg, drop jumps) activities.
intensity PRT reported one muscle strain. In a Although walking is technically a weight-bearing
subanalysis of half of the sample (n=50), there was no exercise, the impact is not very high, but if walking is a
difference in vertebral fractures on the basis of vertebral preferred activity, it can still be encouraged for other
fracture assessment.81 Therefore, in individuals who are health benefits. An exercise professional might need to
at high risk, it is crucial to coach safe movement both guide individuals on impact exercise selection and on
during exercise and during transitions. Home exercise progression for both PRT and impact exercises. Initiating
might seem practical or cost-effective, but it is difficult to exercise if nutrition is inadequate can cause weight loss
ensure adequate dosing, progression, or adherence with or limit strength gains. For example, the PROT-AGE
limited supervision. group recommends 1·0–1·2 g protein per kg bodyweight
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 9
Review
Panel 2: Opportunities and challenges for future research related to physical activity and bone health
Objective measurement of physical activity in cohort greater complexity in design and analyses and larger sample
studies with fracture outcomes sizes; clustered individuals are not independent and their
Opportunities characteristics are more likely to be similar within a cluster
• Assess sedentary activity and bouts of activity and breaks • Pragmatic trials risk non-adherence and high rates of loss to
for sedentary, mild, moderate, and vigorous activity follow-up, require large sample sizes, are unblinded, and
• Consider whether wearable accelerometers can capture lose internal validity to increase generalisability93
ground reaction forces or physical activity intensity • Cost-effectiveness studies need to evaluate long-term
Considerations and challenges effects on the clinical outcome of fracture
• Accelerometry currently does not distinguish between types • Health plans might not want to pay for exercise or strength
of activity training
• Difficult to quantify participation in resistance training or • Interventions that combine behaviour change strategies
balance exercises with exercise and physical activity prescription risk poor
adherence because of the increased complexity
Effects of different types of exercise on individuals at • Adaption of interventions to individual preferences or goals
moderate or high risk of fracture brings increased complexity and costs
Opportunities
• Investigate whether exercise increases bone strength Randomised controlled trials (RCTs) of exercise with fracture
• Evaluate dose duration, frequency, and type of activity as a primary outcome
Opportunity
Considerations and challenges • Develop surrogate outcomes for fracture
• Participants could be taking medications that affect bone
health, therefore research should stratify by medication use Considerations and challenges
and study effects of physical activity in combination with • Emerging meta-analyses and pooling studies would help but
medication challenges include harmonisation of eligibility, interventions,
• Individuals might not be willing to enrol if there is the and outcomes, and differences in study durations
potential to be randomly allocated to a control group, • Large, simple trials with multi-country collaboration might
therefore researchers should consider a waiting-list control not include the intensity of exercise and strength training
and active attention control needed to affect skeletal health
• Masking of participants is not possible and the control • RCTs of exercise in people with low bone mass or moderate
group could be contaminated, so researchers should to high fracture risk need to balance delivery of sufficient
consider active attention control exercise stimulus with risks of falls and fractures
• RCTs need to use appropriate dose and methods to ensure
Interventions that are practical or cost-effective in the real adequate adherence to establish efficacy
world and can achieve good adherence • RCTs directed by rehabilitation or exercise specialists could
Opportunity be too expensive to implement on a wide scale
• Develop science of implementation
Considerations and challenges
• Cluster trials of group-exercise interventions in individuals
at high risk aged 75 years or older in senior apartments have
per day for older adults, and more (>1·5–1·8 g/kg functional strength and balance training, such as step-
bodyweight per day) for active or frail individuals.94 ups, lunges, or shifting forward and backward to the
Exercise guidelines for older adults recommend balance limits of stability with both feet together or on one foot.
exercises.88,89 There is strong evidence that exercise can However, most vertebral fractures do not occur as a result
reduce falls and fall-related injuries36,37 and that the most of a fall,95 and thus exercises to maintain BMD and spine-
effective interventions include functional strength and sparing strategies should also be encouraged.
balance exercises, either alone or combined with
resistance exercises.36 Tai chi could reduce the rate of falls Future research related to bone health
by 19% (low certainty evidence) and reduce the risk of We have summarised the opportunities and challenges
being a faller by 20% (high certainty evidence).36 However, for future research related to physical activity and bone
the effects of walking, dance, or resistance exercise alone health in panel 2. To our knowledge, there is a single
on fall rate or fall risk are uncertain.36 Because most non- prospective study of objective physical activity and fracture
vertebral fractures result from a fall, exercise recom outcomes, which is confined to primarily white men older
mendations for fracture prevention should encourage than 72 years. Information on objective physical activity,
10 www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1
Review
including assessment of sedentary activities and bouts of evidence is related to clinical practice, the effects of
activity, could advance the field. RCTs are needed of exercise on fractures, falls, or BMD in older adults could
exercise in individuals at moderate or high risk of fracture be both site-specific and exercise mode-specific.
with a focus on intermediate markers of bone strength. Multicomponent programmes that combine impact
Developing interventions that are practical and cost- exercise with sufficiently dosed, moderate-intensity or
effective and translatable to the real world are also high-intensity PRT and that are progressive in nature
needed.34 Future research might explore which training will be most effective.
variables are necessary to observe a benefit to bone health, Contributors
to show whether what matters is exercise intensity or Both authors contributed equally to the manuscript.
variables such as training volume, speed of movement, or Declaration of interests
effort (ie, whether exercise is continued to fatigue). We declare no competing interests.
RCTs with fracture endpoints would be costly, long- References
lasting, and perhaps impractical. However, data from 1 Cauley JA. Public health impact of osteoporosis.
J Gerontol A Biol Sci Med Sci 2013; 68: 1243–51.
RCTs and meta-analyses exploring the effects of exercise
2 Bouxsein M, Genant H. The breaking spine. International
on fracture risk or on indirect measures, such as BMD or Osteoporosis Foundation, 2010. https://www.iofbonehealth.org/
falls, could provide insights into the dose and type of sites/default/files/PDFs/WOD%20Reports/2010_the_breaking_
spine_en.pdf (accessed Nov 12, 2019).
exercise. Recently, the Foundation for the National
3 Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA,
Institute of Health Bone Quality Project collected patient- Cooper C. A systematic review of hip fracture incidence and
level data from all randomised trials of osteoporosis drugs probability of fracture worldwide. Osteoporos Int 2012; 23: 2239–56.
to investigate surrogate endpoints for enhancing drug 4 Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A,
Tosteson A. Incidence and economic burden of osteoporosis-related
development in osteoporosis.96 A meta-regression of fractures in the United States, 2005–2025. J Bone Miner Res 2007;
38 placebo-controlled trials of 19 therapeutic agents 22: 465–75.
showed that for a 2% improvement in total hip BMD, 5 Dyer SM, Crotty M, Fairhall N, et al. A critical review of the
long-term disability outcomes following hip fracture. BMC Geriatr
a 28% reduction in vertebral fracture and 16% reduction 2016; 16: 158.
in hip fracture can be expected (and for a 6% improvement 6 Caspersen CJ, Powell KE, Christenson GM. Physical activity,
in total hip BMD, a 66% reduction in vertebral fracture exercise, and physical fitness: definitions and distinctions for
health-related research. Public Health Rep 1985; 100: 126–31.
and 40% reduction in hip fracture can be expected).96
7 Centers for Disease Control and Prevention. Adult participation
Although this meta-regression focused on drug trials, the in aerobic and muscle-strengthening physical activities—
use of surrogate endpoints such as BMD could be applied United States, 2011. MMWR Morb Mortal Wkly 2013; 62: 326.
to exercise interventions. 8 Directorate-General for Communication. Special Eurobarometer
472: sport and physical activity. March 22, 2018. http://data.europa.
eu/euodp/en/data/dataset/S2164_88_4_472_ENG (accessed
Summary June 19, 2019).
Observational studies suggest an 11–40% decline in 9 Trimpou P, Landin-Wilhelmsen K, Odén A, Rosengren A,
Wilhelmsen L. Male risk factors for hip fracture: a 30-year follow-up
fracture risk with increasing physical activity. When this study in 7,495 men. Osteoporos Int 2010; 21: 409–16.
10 Moayyeri A, Besson H, Luben RN, Wareham NJ, Khaw KT.
The association between physical activity in different domains of
Search strategy and selection criteria life and risk of osteoporotic fractures. Bone 2010; 47: 693–700.
11 Jokinen H, Pulkkinen P, Korpelainen J, et al. Risk factors for cervical
We identified references through searches of PubMed for and trochanteric hip fractures in elderly women: a population-based
10-year follow-up study. Calcif Tissue Int 2010; 87: 44–51.
articles published from Jan 1, 2009, to March 31, 2019,
12 Englund U, Nordström P, Nilsson J, et al. Physical activity in
using the terms “physical activity”, “exercise”, “fractures”, middle-aged women and hip fracture risk: the UFO study.
“bone strength”, and “osteoporosis”. Relevant articles were Osteoporos Int 2011; 22: 499–505.
also found in the references of these papers. We limited 13 Mackey DC, Hubbard AE, Cawthon PM, Cauley JA, Cummings SR,
Tager IB. Usual physical activity and hip fracture in older men:
articles to those published in English, and to those concerning an application of semiparametric methods to observational data.
adults aged 40 years and older. We excluded articles that were Am J Epidemiol 2011; 173: 578–86.
not prospective and that did not have a fracture outcome. 14 Armstrong ME, Cairns BJ, Banks E, Green J, Reeves GK, Beral V.
Different effects of age, adiposity and physical activity on the risk
The lists of articles were reviewed by a single author (JAC). of ankle, wrist and hip fractures in postmenopausal women. Bone
Incidence studies were graded according to criteria originally 2012; 50: 1394–400.
developed for the Fracture Risk Assessment Tool (FRAX) 15 Morseth B, Ahmed LA, Bjørnerem Å, et al. Leisure time physical
activity and risk of non-vertebral fracture in men and women aged
International Task Force statement to rate studies on fracture 55 years and older: the Tromsø Study. Eur J Epidemiol 2012;
incidence97 as follows: “good” if at least four criteria were met 27: 463–71.
of prospective study, study population representative of the 16 Lai JK, Lucas RM, Armstrong M, Banks E. Prospective observational
study of physical functioning, physical activity, and time outdoors
entire population, study duration more than 1 year, or and the risk of hip fracture: a population-based cohort study of
adequate definition of fracture or ICD codes used; and “poor” 158,057 older adults in the 45 and up study. J Bone Miner Res 2013;
if at least four criteria were met of retrospective study, study 28: 2222–31.
17 Cauley JA, Cawthon PM, Peters KE, et al. Risk factors for hip
duration of 1 year or less, non-population based, inadequate
fracture in older men: the Osteoporotic Fractures in Men Study
definition of fracture, or only abstract available. (MrOS). J Bone Miner Res 2016; 31: 1810–19.
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 11
Review
18 Gregson CL, Carson C, Amuzu A, Ebrahim S. The association 40 Sherrington C, Tiedemann A, Fairhall N, Close JC, Lord SR.
between graded physical activity in postmenopausal British women, Exercise to prevent falls in older adults: an updated meta-analysis
and the prevalence and incidence of hip and wrist fractures. and best practice recommendations. NSW Public Health Bull 2011;
Age Ageing 2010; 39: 565–74. 22: 78–83.
19 Thomas-John M, Codd MB, Manne S, Watts NB, Mongey AB. 41 Polidoulis I, Beyene J, Cheung AM. The effect of exercise on pQCT
Risk factors for the development of osteoporosis and osteoporotic parameters of bone structure and strength in postmenopausal
fractures among older men. J Rheumatol 2009; 36: 1947–52. women—a systematic review and meta-analysis of randomized
20 Lee SH, Khang YH, Lim KH, et al. Clinical risk factors for controlled trials. Osteoporos Int 2012; 23: 39–51.
osteoporotic fracture: a population-based prospective cohort study 42 Ashe MC, Gorman E, Khan KM, et al. Does frequency of resistance
in Korea. J Bone Miner Res 2010; 25: 369–78. training affect tibial cortical bone density in older women?
21 Rouzi AA, Al-Sibiani SA, Al-Senani NS, Radaddi RM, Ardawi MS. A randomized controlled trial. Osteoporos Int 2013; 24: 623–32.
Independent predictors of all osteoporosis-related fractures among 43 Gómez-Cabello A, Ara I, González-Agüero A, Casajús JA,
healthy Saudi postmenopausal women: the CEOR Study. Bone 2012; Vicente-Rodríguez G. Effects of training on bone mass in older
50: 713–22. adults: a systematic review. Sports Med 2012; 42: 301–25.
22 Cauley JA, Harrison SL, Cawthon PM, et al. Objective measures of 44 Bolam KA, van Uffelen JG, Taaffe DR. The effect of physical
physical activity, fractures and falls: the osteoporotic fractures in exercise on bone density in middle-aged and older men:
men study. J Am Geriatr Soc 2013; 61: 1080–88. a systematic review. Osteoporos Int 2013; 24: 2749–62.
23 Nikander R, Gagnon C, Dunstan DW, et al. Frequent walking, 45 Kemmler W, Shojaa M, Kohl M, von Stengel S. Exercise effects on
but not total physical activity, is associated with increased fracture bone mineral density in older men: a systematic review with
incidence: a 5-year follow-up of an Australian population-based special emphasis on study interventions. Osteoporos Int 2018;
prospective study (AusDiab). J Bone Miner Res 2011; 26: 1638–47. 29: 1493–504.
24 Holloway-Kew KL, Moloney DJ, Bucki-Smith G, et al. Sports 46 Sañudo B, de Hoyo M, Del Pozo-Cruz J, et al. A systematic review
participation and fracture in older Australian men. Arch Osteoporos of the exercise effect on bone health: the importance of assessing
2018; 13: 43. mechanical loading in perimenopausal and postmenopausal
25 Rikkonen T, Salovaara K, Sirola J, et al. Physical activity slows women. Menopause 2017; 24: 1208–16.
femoral bone loss but promotes wrist fractures in postmenopausal 47 Zhao R, Zhao M, Xu Z. The effects of differing resistance training
women: a 15-year follow-up of the OSTPRE study. J Bone Miner Res modes on the preservation of bone mineral density in
2010; 25: 2332–40. postmenopausal women: a meta-analysis. Osteoporos Int 2015;
26 Nakamura K, Kitamura K, Inoue M, Sawada N, Tsugane S. Physical 26: 1605–18.
activity and 10-year incidence of self-reported vertebral fractures in 48 Ma D, Wu L, He Z. Effects of walking on the preservation of bone
Japanese women: the Japan Public Health Center-based Prospective mineral density in perimenopausal and postmenopausal women:
Study. Osteoporos Int 2014; 25: 2565–71. a systematic review and meta-analysis. Menopause 2013; 20: 1216–26.
27 Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, 49 Simas V, Hing W, Pope R, Climstein M. Effects of water-based
Herndon JH. Distal radius fractures in older women: a 10-year exercise on bone health of middle-aged and older adults: a systematic
follow-up study of descriptive characteristics and risk factors: the review and meta-analysis. Open Access J Sports Med 2017; 8: 39–60.
study of osteoporotic fractures. J Am Geriatr Soc 2002; 50: 97–103. 50 Sun Z, Chen H, Berger MR, Zhang L, Guo H, Huang Y. Effects
28 Chen Z, Kooperberg C, Pettinger MB, et al. Validity of self-report of tai chi exercise on bone health in perimenopausal and
for fractures among a multiethnic cohort of postmenopausal postmenopausal women: a systematic review and meta-analysis.
women: results from the Women’s Health Initiative observational Osteoporos Int 2016; 27: 2901–11.
study and clinical trials. Menopause 2004; 11: 264–74. 51 Liu F, Wang S. Effect of tai chi on bone mineral density in
29 Fink HA, Milavetz DL, Palermo L, et al. What proportion of incident postmenopausal women: a systematic review and meta-analysis
radiographic vertebral deformities is clinically diagnosed and vice of randomized control trials. J Chin Med Assoc 2017; 80: 790–95.
versa? J Bone Miner Res 2005; 20: 1216–22. 52 Duckham RL, Masud T, Taylor R, et al. Randomised controlled trial
30 Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ 3rd. Incidence of of the effectiveness of community group and home-based falls
clinically diagnosed vertebral fractures: a population-based study in prevention exercise programmes on bone health in older people:
Rochester, Minnesota, 1985–1989. J Bone Miner Res 1992; 7: 221–27. the ProAct65+ bone study. Age Ageing 2015; 44: 573–79.
31 Dowd KP, Szeklicki R, Minetto MA, et al. A systematic literature 53 Kelley GA, Kelley KS, Kohrt WM. Effects of ground and joint
review of reviews on techniques for physical activity measurement reaction force exercise on lumbar spine and femoral neck bone
in adults: a DEDIPAC study. Int J Behav Nutr Phys Act 2018; 15: 15. mineral density in postmenopausal women: a meta-analysis of
32 Johansson H, Kanis JA, Odén A, et al. A meta-analysis of the randomized controlled trials. BMC Musculoskelet Disord 2012; 13: 177.
association of fracture risk and body mass index in women. 54 Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR.
J Bone Miner Res 2014; 29: 223–33. High-intensity resistance and impact training improves bone
33 Forwood MR, Turner CH. Skeletal adaptations to mechanical usage: mineral density and physical function in postmenopausal women
results from tibial loading studies in rats. Bone 1995; with osteopenia and osteoporosis: the LIFTMOR randomized
17 (suppl): S197–205. controlled trial. J Bone Miner Res 2018; 33: 211–20.
34 Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and 55 Gianoudis J, Bailey CA, Ebeling PR, et al. Effects of a targeted
treating osteoporosis in postmenopausal women. multimodal exercise program incorporating high-speed power
Cochrane Database Syst Rev 2011; 7: CD000333. training on falls and fracture risk factors in older adults:
35 Prevention of Falls Network Earth. Manual for the fall prevention a community-based randomized controlled trial. J Bone Miner Res
classification system, version 1. April 4, 2007. http://www.profane. 2014; 29: 182–91.
eu.org/documents/Falls_Taxonomy.pdf (accessed June 25, 2019). 56 Kelley GA, Kelley KS, Kohrt WM. Exercise and bone mineral
36 Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for density in men: a meta-analysis of randomized controlled trials.
preventing falls in older people living in the community. Bone 2013; 53: 103–11.
Cochrane Database Syst Rev 2019; 1: CD012424. 57 Allison SJ, Folland JP, Rennie WJ, Summers GD, Brooke-Wavell K.
37 Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of High impact exercise increased femoral neck bone mineral density
interventions for preventing falls in older adults: a systematic in older men: a randomised unilateral intervention. Bone 2013;
review and meta-analysis. JAMA 2017; 318: 1687–99. 53: 321–28.
38 El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect 58 Johansson J, Nordström A, Nordström P. Objectively measured
of fall prevention exercise programmes on fall induced injuries in physical activity is associated with parameters of bone in 70-year-old
community dwelling older adults: systematic review and men and women. Bone 2015; 81: 72–79.
meta-analysis of randomised controlled trials. BMJ 2013; 347: f6234. 59 Meakin LB, Galea GL, Sugiyama T, Lanyon LE, Price JS. Age-related
39 Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for impairment of bones’ adaptive response to loading in mice is
preventing falls in older people living in the community. associated with sex-related deficiencies in osteoblasts but no change
Cochrane Database Syst Rev 2012; 9: CD007146. in osteocytes. J Bone Miner Res 2014; 29: 1859–71.
12 www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1
Review
60 Holguin N, Brodt MD, Silva MJ. Activation of Wnt signaling by 79 Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW.
mechanical loading is impaired in the bone of old mice. Group treatment improves trunk strength and psychological status
J Bone Miner Res 2016; 31: 2215–26. in older women with vertebral fractures: results of a randomized,
61 Birkhold AI, Razi H, Duda GN, Weinkamer R, Checa S, Willie BM. clinical trial. J Am Geriatr Soc 2004; 52: 1471–78.
The influence of age on adaptive bone formation and bone 80 Hongo M, Adachi M. Therapeutic approaches to non-erosive
resorption. Biomaterials 2014; 35: 9290–301. GERD—comparison between the Western countries and Japan.
62 Borde R, Hortobágyi T, Granacher U. Dose-response relationships Nihon Rinsho 2005; 63: 1299–303.
of resistance training in healthy old adults: a systematic review and 81 Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR.
meta-analysis. Sports Med 2015; 45: 1693–720. High-intensity exercise did not cause vertebral fractures and improves
63 Bolton KL, Egerton T, Wark J, et al. Effects of exercise on bone thoracic kyphosis in postmenopausal women with low to very low
density and falls risk factors in post-menopausal women with bone mass: the LIFTMOR trial. Osteoporos Int 2019; 30: 957–64.
osteopenia: a randomised controlled trial. J Sci Med Sport 2012; 82 Guidelines. Osteoporosis Canada. https://osteoporosis.ca/health-
15: 102–09. care-professionals/clinical-practice-guidelines/exercise-
64 Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, recommendations/ (accessed Nov 6, 2019).
Papaioannou A. Exercise for improving outcomes after osteoporotic 83 Royal Osteoporosis Society. Strong, steady, and straight (quick
vertebral fracture. Cochrane Database Syst Rev 2013; 1: CD008618. guide). https://theros.org.uk/media/100224/royal-osteoporosis-
65 Papaioannou A, Adachi JD, Winegard K, et al. Efficacy of society-strong-steady-straight-quick-guide.pdf (accessed Nov 6, 2019).
home-based exercise for improving quality of life among elderly 84 Royal Osteoporosis Society. Information about exercise.
women with symptomatic osteoporosis-related vertebral fractures. https://theros.org.uk/media/100541/ros-about-exercise.pdf
Osteoporos Int 2003; 14: 677–82. (accessed Nov 6, 2019).
66 Wang XF, Xu B, Ye XY, Yang YY, Wang GH. Effects of different 85 Royal Osteoporosis Society. Exercise and physical activity with
treatments on patients with osteoporotic fracture after percutaneous osteoporosis videos. https://theros.org.uk/information-and-
kyphoplasty. Zhongguo Gu Shang 2015; 28: 512–16. support/living-with-osteoporosis/exercise-and-physical-activity-with-
67 Funnel L, Djekic-Ivankovic M, Chepesiuk R, Giangregorio L. osteoporosis/ (accessed Nov 6, 2019).
Patient engagement in clinical guidelines development: input 86 Osteoporosis Australia. Education and Onero exercise program
from >1000 members of the canadian osteoporosis patient information. https://www.osteoporosis.org.au/exercise (accessed
network. J Bone Miner Res 2018; 32 (suppl 1): https://www.asbmr. Nov 6, 2019).
org/education/AbstractDetail?aid=761a1f2c-0fb5-4c96-adab- 87 International Osteoporosis Foundation. Exercise recommendations.
0874f4173088 (accessed May 20, 2019). https://www.iofbonehealth.org/exercise-recommendations
68 Ziebart C, McArthur C, Papaioannou A. Using behaviour change (accessed Nov 6, 2019).
theory and user perspectives to design patient education materials 88 Giangregorio LM, Papaioannou A, Macintyre NJ, et al. Too Fit To
to enhance uptake of Too Fit To Fracture recommendations. Fracture: exercise recommendations for individuals with osteoporosis
J Bone Miner Res 2017; 31 (suppl 1): https://www.asbmr.org/ or osteoporotic vertebral fracture. Osteoporos Int 2014; 25: 821–35.
education/AbstractDetail?aid=c12d8733-de57-4038-ac5e- 89 Beck BR, Daly RM, Singh MA, Taaffe DR. Exercise and Sports
62d1a166455e (accessed May 20, 2019). Science Australia (ESSA) position statement on exercise
69 Clark RE, McArthur C, Papaioannou A, et al. “I do not have time. prescription for the prevention and management of osteoporosis.
Is there a handout I can use?”: combining physicians’ needs and J Sci Med Sport 2017; 20: 438–45.
behavior change theory to put physical activity evidence into 90 Giangregorio LM, McGill S, Wark JD, et al. Too Fit To Fracture:
practice. Osteoporos Int 2017; 28: 1953–63. outcomes of a Delphi consensus process on physical activity and
70 Liu CJ, Latham N. Adverse events reported in progressive resistance exercise recommendations for adults with osteoporosis with or
strength training trials in older adults: 2 sides of a coin. without vertebral fractures. Osteoporos Int 2015; 26: 891–910.
Arch Phys Med Rehabil 2010; 91: 1471–73. 91 Merom D, Pye V, Macniven R, et al. Prevalence and correlates of
71 de Souto Barreto P, Rolland Y, Vellas B, Maltais M. Association participation in fall prevention exercise/physical activity by older
of Long-term exercise training with risk of falls, fractures, adults. Prev Med 2012; 55: 613–17.
hospitalizations, and mortality in older adults: a systematic review 92 Saccone M, Mittmann N. Physical activity patterns and preferences
and meta-analysis. JAMA Intern Med 2019; 179: 394–405. in women with low bone mass. J Bone Miner Res 2011; 26 (suppl 1):
72 Chilibeck PD, Vatanparast H, Cornish SM, Abeysekara S, https://www.asbmr.org/education/AbstractDetail?aid=1eb435c5-
Charlesworth S. Evidence-based risk assessment and b887-4e20-8b26-bb48ba5840e2 (accessed Nov 6, 2019).
recommendations for physical activity: arthritis, osteoporosis, and 93 Ware JH, Hamel MB. Pragmatic trials—guides to better patient
low back pain. Appl Physiol Nutr Metab 2011; 36 (suppl 1): S49–79. care? N Engl J Med 2011; 364: 1685–7.
73 Abeysekara S, Chilibeck PD, Vatanparast H, Zello GA. 94 Bauer J, Biolo G, Cederholm T, et al. Evidence-based
A pulse-based diet is effective for reducing total and LDL-cholesterol recommendations for optimal dietary protein intake in older
in older adults. Br J Nutr 2012; 108 (suppl 1): S103–10. people: a position paper from the PROT-AGE Study Group.
74 Chilibeck PD, Vatanparast H, Pierson R, et al. Effect of exercise J Am Med Dir Assoc 2013; 14: 542–59.
training combined with isoflavone supplementation on bone and 95 Costa AG, Wyman A, Siris ES, et al. When, where and how
lipids in postmenopausal women: a randomized clinical trial. osteoporosis-associated fractures occur: an analysis from the Global
J Bone Miner Res 2013; 28: 780–93. Longitudinal Study of Osteoporosis in Women (GLOW). PLoS One
75 Chilibeck PD, Candow DG, Landeryou T, Kaviani M, 2013; 8: e83306.
Paus-Jenssen L. Effects of creatine and resistance training on bone 96 Bouxsein ML, Eastell R, Lui LY, et al. Change in bone density and
health in postmenopausal women. Med Sci Sports Exerc 2015; reduction in fracture risk: a meta-regression of published trials.
47: 1587–95. J Bone Miner Res 2019; 34: 632–42.
76 Duff WR, Kontulainen SA, Candow DG, et al. Effects of low-dose 97 Cauley JA, El-Hajj Fuleihan G, Arabi A, et al. Official positions for
ibuprofen supplementation and resistance training on bone and FRAX(R) clinical regarding international differences from Joint
muscle in postmenopausal women: a randomized controlled trial. Official Positions Development Conference of the International
Bone Rep 2016; 5: 96–103. Society for Clinical Densitometry and International Osteoporosis
77 Giangregorio LM, Gibbs JC, Templeton JA, et al. Build better bones Foundation on FRAX(R). J Clin Densitom 2011; 14: 240–62.
with exercise (B3E pilot trial): results of a feasibility study of
a multicenter randomized controlled trial of 12 months of home © 2019 Elsevier Ltd. All rights reserved.
exercise in older women with vertebral fracture. Osteoporos Int 2018;
29: 2545–56.
78 Binder EF, Brown M, Sinacore DR, Steger-May K, Yarasheski KE,
Schechtman KB. Effects of extended outpatient rehabilitation after
hip fracture: a randomized controlled trial. JAMA 2004;
292: 837–46.
www.thelancet.com/diabetes-endocrinology Published online November 20, 2019 https://doi.org/10.1016/S2213-8587(19)30351-1 13
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Nursing Care Plan - PreopDocument2 pagesNursing Care Plan - PreopXyprexia Dependent88% (16)
- Cribado de Deterioro Cognitivo 2018Document22 pagesCribado de Deterioro Cognitivo 2018Lalito Manuel Cabellos AcuñaNo ratings yet
- Deterioro Cognitivo Vascular y Demencia 2016Document9 pagesDeterioro Cognitivo Vascular y Demencia 2016Lalito Manuel Cabellos AcuñaNo ratings yet
- Tratamiento Farmacologico Alzheimer 2016Document7 pagesTratamiento Farmacologico Alzheimer 2016Lalito Manuel Cabellos AcuñaNo ratings yet
- Escala de Fragilidad de Edmonton-ValidacionDocument4 pagesEscala de Fragilidad de Edmonton-ValidacionLalito Manuel Cabellos AcuñaNo ratings yet
- Constipacion Refractaria en Ancianos - 2017Document19 pagesConstipacion Refractaria en Ancianos - 2017Lalito Manuel Cabellos AcuñaNo ratings yet
- Movilidad en El Anciano Hospitalizado 2018Document6 pagesMovilidad en El Anciano Hospitalizado 2018Lalito Manuel Cabellos AcuñaNo ratings yet
- Identificacion y Manejo de Fragilidad en Atencion Primaria 2018Document7 pagesIdentificacion y Manejo de Fragilidad en Atencion Primaria 2018Lalito Manuel Cabellos AcuñaNo ratings yet
- Cribado de Fragilidad de Paises Pobres 2016Document18 pagesCribado de Fragilidad de Paises Pobres 2016Lalito Manuel Cabellos AcuñaNo ratings yet
- STEADI Algorithm 2019Document2 pagesSTEADI Algorithm 2019Lalito Manuel Cabellos AcuñaNo ratings yet
- The Behavioral Neuroscience of TinnitudsDocument480 pagesThe Behavioral Neuroscience of TinnitudsBreiner Peñaranda100% (1)
- Mcom Project Sem 3Document26 pagesMcom Project Sem 3prathamesh gadgilNo ratings yet
- SYMPTOMATOLOGYDocument22 pagesSYMPTOMATOLOGYMntdher EadanNo ratings yet
- Flystrike Among Domestic Animals: An OverviewDocument3 pagesFlystrike Among Domestic Animals: An OverviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Countrywide NPIs - 19 Jan 22Document2 pagesCountrywide NPIs - 19 Jan 22Muhammad AsifNo ratings yet
- IntroductionDocument4 pagesIntroductionAries BernardinoNo ratings yet
- Pathology & Clinical Laboratory (M) SDN - BHD: HaematologyDocument2 pagesPathology & Clinical Laboratory (M) SDN - BHD: HaematologyHANIFNo ratings yet
- COVID FFS-Inclusive FAQs-updated 8.26.2020-Final 1 PDFDocument142 pagesCOVID FFS-Inclusive FAQs-updated 8.26.2020-Final 1 PDFVivi Agustini SampelanNo ratings yet
- The Global Funds Audit ReportDocument29 pagesThe Global Funds Audit ReportRahul BhanNo ratings yet
- Computer ScreenDocument15 pagesComputer ScreenShahmeer KhanNo ratings yet
- Eight Principles For Patient-Centred and Family-Centred Care For Newborns in The Neonatal Intensive Care UnitDocument5 pagesEight Principles For Patient-Centred and Family-Centred Care For Newborns in The Neonatal Intensive Care UnitPaola RoigNo ratings yet
- Part 1 of Cvs Anatomy and PhysiologyDocument11 pagesPart 1 of Cvs Anatomy and PhysiologyZacharia muraciaNo ratings yet
- Elisabeth Kübler-Ross - Five Stages of GriefDocument8 pagesElisabeth Kübler-Ross - Five Stages of Griefaastha jainNo ratings yet
- Slate Burris: HuainanziDocument13 pagesSlate Burris: HuainanzizhikNo ratings yet
- Homeopathic Medicine For Knee3Document1 pageHomeopathic Medicine For Knee3Pranav VermaNo ratings yet
- Benefits For Children With Disabilities: Socialsecurity - GovDocument20 pagesBenefits For Children With Disabilities: Socialsecurity - GovIrappa HosamaniNo ratings yet
- 1-Panadol Advance 6-Panadol Sinus 2-Panadol Extra 7-Panadol Night 3-Panadol Actifast 4-Panadol Joint 5-Panadol Cold and Flu and Their TypesDocument12 pages1-Panadol Advance 6-Panadol Sinus 2-Panadol Extra 7-Panadol Night 3-Panadol Actifast 4-Panadol Joint 5-Panadol Cold and Flu and Their TypesSulaiman AlqatfNo ratings yet
- Tugas Dokter Yulia Kelompok 2 EditDocument10 pagesTugas Dokter Yulia Kelompok 2 Editfk unpadNo ratings yet
- LSHTM Guidelines For LMIC To Report To GLASSDocument21 pagesLSHTM Guidelines For LMIC To Report To GLASSMuhammadAtharAbbasNo ratings yet
- Skillsfirst DIploma in Adult Care HandbookDocument119 pagesSkillsfirst DIploma in Adult Care HandbookLiza Gomez100% (1)
- Concepts of Occlusion JipsDocument7 pagesConcepts of Occlusion JipsDRPRIYA007No ratings yet
- Measuring Pulse OximeterDocument94 pagesMeasuring Pulse OximeterMuhammed HammadNo ratings yet
- Project Proposal MedalloDocument6 pagesProject Proposal MedalloSaturn NetunaeNo ratings yet
- Laboratory Report: Thyroid Function TestDocument2 pagesLaboratory Report: Thyroid Function Testtafiki4253No ratings yet
- Occupational Stress Level Among Personnel of Bureau of Fire ProtectionDocument11 pagesOccupational Stress Level Among Personnel of Bureau of Fire ProtectionAlaine Danica Dimaandal0% (1)
- Menopause and Cardiovascular Disease: Louise NewsonDocument6 pagesMenopause and Cardiovascular Disease: Louise NewsonMicaela CalvopiñaNo ratings yet
- DRRM-H Plan 2023Document12 pagesDRRM-H Plan 2023City Health Office Bais CityNo ratings yet
- OSCE Pediatric Dentistry Lecture-AnswersDocument40 pagesOSCE Pediatric Dentistry Lecture-AnswersR MNo ratings yet
- Upt Puskesmas Atap: Pemerintah Kabupaten Nunukan Dinas KesehatanDocument19 pagesUpt Puskesmas Atap: Pemerintah Kabupaten Nunukan Dinas KesehatanIin SulmawatiNo ratings yet