Professional Documents
Culture Documents
Physiology of Growth: Arlan L. Rosenbloom
Physiology of Growth: Arlan L. Rosenbloom
Uploaded by
انجمن بدنسازی ایرانOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Physiology of Growth: Arlan L. Rosenbloom
Physiology of Growth: Arlan L. Rosenbloom
Uploaded by
انجمن بدنسازی ایرانCopyright:
Available Formats
Ann Nestlé [Engl] 2007;65:97–108
DOI: 10.1159/000112232
Physiology of Growth
Arlan L. Rosenbloom
Division of Endocrinology, Department of Pediatrics, University of Florida College of Medicine, Gainesville, Fla., USA
Key Words sex hormone production marks the onset of adolescence
Human growth ⴢ Fetus ⴢ Infancy ⴢ Adolescence ⴢ Nutrition ⴢ which is associated with a growth spurt resulting from in-
Insulin-like growth factor-I ⴢ Growth hormone ⴢ creased insulin, GH, and IGF-I production, in addition to the
Pituitary differentiation ⴢ Growth hormone insensitivity sex hormone surge. Environmental influences on growth are
reflected in secular trends over the past 150 years. A myriad
of gene products acting on the growth plate have been de-
Abstract scribed. In addition, delineation of pituitary differentiation
Human growth is a dynamic and complex process that be- factors and their genetic control, as well as identification of
gins with fertilization of the ovum and is completed with the genes controlling multiple steps in key hormonal actions are
fusion of epiphyses and metastases of the long bones mark- increasing the understanding of the complex interplay of
ing the completion of adolescence. Growth occurs in phases genetics, environment, and hormonal milieu in the growth
with distinctive characteristics in terms of dominant influ- process. Copyright © 2008 Nestec Ltd., Vevey/S. Karger AG, Basel
ences from among genetic, environmental/nutritional, and
hormonal factors and patterns. Prenatal growth is the most
dramatic phase, achieving a velocity that is never again
matched. It is predominantly under the influence of mater- Definition and Natural History of Human Growth
nal size and nutritional status with little influence of parental
genetic endowment. Insulin-like growth factors (IGFs) and Human growth physiology encompasses the dynamic
insulin are critical, but thyroid hormone and growth hor- period beginning with cleavage of the zygote and ending
mone (GH) are not. Infancy is a period of rapidly changing with completion of adolescence which is marked by the
growth rate, from 20 cm/year during the first few months to end of long bone growth. Linear growth is built upon the
10–12 cm/year by 1 year of age. This phase is greatly depen- skeletal infrastructure; chondrocytes in the cartilage
dent on genetic endowment, with frequent adjustment to growth plate proliferate, enlarge, and ossify, with ulti-
an appropriate percentile; it is also dependent on normal mate fusion of the distal epiphyseal and central metaphy-
thyroid hormone and GH secretion and action (i.e. stimula- seal regions. This complex process is influenced by ge-
tion of IGF-I synthesis from the liver and promotion of chon- netic, nutritional/environmental, and hormonal factors
drocyte differentiation and local secretion of IGF-I). Growth that vary with the growth phases. These phases of growth
in the second year averages 10–13 cm/year, in the third year are prenatal, infancy, childhood, and adolescence.
7.5–10 cm/year and thereafter is stable at 5–6 cm/year, with
continued dependency on normal secretion and action of Prenatal Growth
thyroid hormone and GH. Relaxation of the suppression of Development of the microscopic zygote into the 51-cm
the hypothalamic-gonadotropin axis with a slow increase in newborn is the most dramatic period of growth. From
© 2008 Nestec Ltd., Vevey/S. Karger AG, Basel Arlan L. Rosenbloom, MD
0517–8606/07/0653–0097$23.50/0 Children’s Medical Services Center
Fax +41 61 306 12 34 1701 Southwest 16th Avenue
E-Mail karger@karger.ch Accessible online at: Gainesville, FL 32608 (USA)
www.karger.com www.karger.com/ane Tel. +1 352 334 1393, E-Mail Rosenal@peds.ufl.edu
completion of organogenesis in the first trimester, there grow more rapidly than females. While it was earlier
is rapid acceleration in the second trimester to a peak ve- thought that growth in the first 6 months of life was in-
locity of 2.5 cm/week. The most important influence on dependent of GH, it is now recognized that GH deficien-
fetal growth is maternal size and nutritional status. Ge- cy (GHD) and GH receptor deficiency, resulting in severe
netic factors have little influence on fetal growth, with the IGF-I deficiency, affect postnatal growth from the outset
exception of transmitted or new mutations affecting skel- [6].
etal growth, such as achondroplasia, or affecting key hor-
monal mechanisms [1, 2]. The intrauterine endocrine mi- Growth in Childhood
lieu is a complex interaction of fetal, placental, and ma- In the 2nd year, growth velocity averages 10–13 cm/
ternal substrates, precursors, and hormones affecting year and in the 3rd year, 7.5–10 cm/year. Thereafter, from
growth including, in addition to the insulin-like growth age 3 years to puberty, growth is stable at 5–6 cm/year,
factors (IGFs), fetal insulin production in response to ma- although there may be a slowing to as little as 2 cm/year
ternal glycemia, human placental lactogen, and sex ste- for a time preceding the adolescent growth spurt. This is
roids. Both IGF-I and IGF-II are essential for fetal growth, especially noticeable in children with constitutional de-
and their production in utero is independent of growth lay in growth and maturation, and is frequently accom-
hormone (GH). While thyroid hormone is absolutely es- panied by reduced GH responses to stimulatory testing,
sential for postnatal growth, its absence, as with inborn misdiagnosis of GHD, and inappropriate treatment with
errors of thyroidogenesis or thyroid aplasia, does not af- recombinant human GH. Childhood growth is also char-
fect fetal growth. Production of testosterone by the male acterized by a rapid change in body proportions, when
fetus, beginning at approximately 10 weeks gestation, is the legs grow faster than the trunk, and both grow much
essential to male genital differentiation. The ‘mini-ado- faster than the head in proportion to overall body length.
lescence’ characterized by elevated testosterone levels The ratio of upper body to lower segment (measured as
near term promotes penile growth and accounts for the the distance from the top of the symphysis pubis to the
observation that newborn males have slightly greater floor or measuring board with the legs straight) goes
lean mass and less fat mass than females and are on aver- from 1.7 at birth, to 1.4 at 2 years, to unity by age 10 [3].
age 0.9 cm longer and 150 g heavier [3].
Growth in Adolescence
Growth in Infancy At the appropriate biologic age, as reflected in osseous
Infancy can be considered a period of rapidly chang- maturation, suppression of the hypothalamic-gonado-
ing growth rate. Following birth, the infant shifts from a tropin axis of childhood begins to be lifted and results in
growth velocity primarily determined by maternal fac- a slow increase in the levels of sex hormones that result
tors to one adjusted for genetic endowment. While the in adolescence. Although girls start their adolescence,
mid-parental standard deviation score or percentile for signaled by breast budding, at an average 6 months ear-
height may estimate what this endowment consists of, lier than boys, whose signal is testicular enlargement, the
this is only reliable if the parental heights are actually adolescent growth spurt is 2 years earlier in girls. Thus,
measured and their own childhoods were devoid of fac- the adolescent growth spurt is early in female maturation
tors which might have impaired growth. Linear growth and late in male maturation. This timing, giving boys a
is a stepwise process rather than being continuous, as im- longer period of slow growth, accounts for some of the
plied by the smoothed growth charts derived from cross- greater adult height of males, along with the growth ef-
sectional data, and this is especially striking in infancy fects of testosterone. The pubertal growth spurt accounts
[4]. Growth velocity in the first year of life declines from for more than 20% of adult stature and 50% of adult bone
20 cm/year in the first few months to 10–12 cm/year by 1 mass accrual. Growth is completed when, under the in-
year of age, by which time length has increased 50% and fluence of estrogen, either secreted by the ovary or con-
weight threefold. The influence of parental genetic en- verted by aromatization from testosterone in males, fu-
dowment on infant growth is reflected in the shift of sion of the epiphyses occurs. In addition to sex hormones,
growth channels that occurs for about two thirds of nor- there are large increases in insulin, GH, and IGF-I that
mal infants during the first 6–18 months of life, with contribute to adolescent growth which, along with nor-
equal numbers shifting upward and downward [5]. mal thyroid function, are essential to the adolescent
The effect of the ‘mini-adolescence’ of the male fetus growth spurt [7].
continues for the first 3–6 months after birth, when males
98 Ann Nestlé [Engl] 2007;65:97–108 Rosenbloom
Environmental Factors in Growth opment, SOX9. FGFR3 stimulates the proliferation of
immature cells and limits division of proliferating chon-
During the 150 years preceding the mid-20th century, drocytes. Gain of function mutation of FGFR3 is associ-
there was a secular trend in the pace of maturation and ated with achondroplasia [7]. Prehypertrophic chondro-
adult size of individuals in the Western countries for cytes produce a protein referred to as Indian hedgehog
which such data are available. A century and a half ago, that coordinates the proliferation and differentiation of
average males did not reach adult height until 23 years of chondrocytes and osteoblasts, and the process of bone
age as opposed to the current 17 years and the age of men- formation; this protein is self-regulated by its control of
arche has declined from 17 to 12.5 years. The most appar- parathyroid hormone-related protein, gain of function or
ent explanation for this phenomenon is the improvement loss of function mutations of which result in specific
in nutrition and reduction in childhood disease frequen- chondrodysplasias with stunting.
cy and duration with attendant salutary effects on the The SHOX gene is found on the pseudo-autosomal re-
GH–IGF-I axis. This secular trend appears to have lev- gion of the short arms of the X and Y chromosomes and
eled off in the last 50 years [3]. For much of the world, does not undergo inactivation in normal females; short
undernutrition remains the most common cause of short stature in those with an absence of the pseudo-autosomal
stature. Overnutrition with obesity increases the rate of region of one X chromosome, i.e. Turner syndrome, is at-
growth, accelerates skeletal maturation, and may advance tributed to the need for both alleles. Loss of function mu-
pubertal onset in girls, but in contrast to the permanent tations in one SHOX allele or its isolated deletion has
effects of long-term childhood malnutrition or chronic been described in children with otherwise unexplained
disease, is not typically associated with an effect on adult short stature and in Leri-Weill dyschondrosteosis; loss of
height [7]. both alleles results in another form of osseous malforma-
It is noteworthy that growth differences in preschool tion, Langer mesomelic dysplasia. In contrast, overdos-
children are more influenced by socioeconomic factors age of SHOX alleles in girls with triple X syndrome results
than by racial or genetic factors [8]. That size differences in very tall stature and may explain the tall stature of
between ethnic or geographic groups result from envi- other multiple X and Y syndromes. Increased stature has
ronmental factors, rather than genetics, was demonstrat- also been associated with variants in the melanocortin-4
ed by the finding that 7-year-old boys in families in the receptor, and catecholamine o-methyltransferase affect-
upper socioeconomic classes from eight different coun- ing estrogen metabolism. The suppressor of cytokine sig-
tries had very similar heights corresponding to the 50th naling (SOCS2) inhibits GH signaling by competitive
percentile in the US [9]. binding to the GH receptor and in mice that have had this
gene knocked out, overgrowth occurs. Overexpression
can also lead to overgrowth, suggesting the kind of dual
Genetic Control of Growth effect that is emerging for a variety of gene products [7].
A recently recognized regulator of skeletal growth is
It is estimated that 70–90% of adult stature is geneti- C-type naturetic peptide (CNP). Homozygosity for muta-
cally determined, nutritional and socioeconomic factors tion of the CNP receptor-B resulting in loss of function
being equal. In addition to the genetic factors affecting causes the skeletal dysplasia referred to as Maroteaux-
the production of and response to insulin, thyroid hor- Lamy type (acromesomelic dysplasia). Heterozygous car-
mone, sex steroids, and the GH–IGF-I axis (discussed riers of the mutation were found to be significantly short-
below under Hormonal Control of Growth), extensive er than noncarriers, and it was estimated that ⬃3% of
genetic control of growth through the expression of nu- children with idiopathic short stature might be heterozy-
merous genes acting on the growth plate is being increas- gous for this mutation [10].
ingly recognized.
Fibroblast growth factors (FGFs) interact with various
FGF receptors to regulate the growth and development of Hormonal Control of Growth
enchondral bone and longitudinal growth and fusion of
long bones. The gene for FGF receptor 2 (FGFR2) is ex- As noted above, insulin, thyroid hormone, and sex ste-
pressed by the earliest chondrocytes and induces the ex- roids are important components at various stages of
pression of a transcription factor needed for the differen- growth. The absence of insulin in utero results in severe
tiation of the chondrocytes, as well as male genital devel- growth failure in leprechaunism. Thyroid hormone, as
Physiology of Growth Ann Nestlé [Engl] 2007;65:97–108 99
noted, does not affect intrauterine growth, but is essential initiate anterior pituitary gland development from the
subsequently for the differentiation and proliferation of oral ectoderm, and transcription factors that control pi-
chondrocytes and their ability to respond to growth fac- tuitary cell differentiation and specification. Several ho-
tors. There are several congenital or genetic defects affect- meodomain transcription factors directing embryologic
ing embryogenesis and migration of the thyroid gland, development of the anterior pituitary have been found to
thyroid-stimulating hormone (TSH) production, the TSH have mutations that result in congenital defects affecting
receptor, thyroid hormone production and conversion to the synthesis of GH and additional pituitary hormones
active triiodothyronine. In addition, acquired hypothy- [13]. The human mutations that cause isolated GHD or
roidism due to autoimmune thyroiditis can completely multiple pituitary hormone deficiency and associated
stop a child’s growth. Sex steroid effects on bone matura- features are summarized in table 1.
tion are via the estrogen receptor; mutations of this recep- The HESX1 (Homeobox gene Expressed in embryon-
tor or of the aromatase that controls the conversion of tes- ic Stem cells) gene is important in the development of the
tosterone to estrogen results in prolonged bone growth. optic nerve as well as the anterior pituitary. HESX1 in-
The remainder of this section will focus on the embry- hibits PROP1-mediated gene effects and mediates fore-
ology, functional anatomy, genetics, and biochemistry of brain development [14]. HESX1 has also been referred to
the GH–IGF-I pathway. Disorders anywhere along the as the Rpx or Rathke’s pouch homeobox gene. Some mu-
GH–IGF-I pathway preceding the IGF-I receptor result in tations that have been described account for a small sub-
IGF-I deficiency and may be congenital or acquired. Con- set of the cases of septo-optic dysplasia with variable GH
genital GHD is associated with structural malformations and other pituitary deficiencies [15].
of the central nervous system, hypothalamus, or pitu- PITX2 is a paired-like homeobox gene expressed in
itary. IGF-I deficiency/resistance may result from genetic the fetal pituitary and adult gland, thought to be required
defects involving critical factors in the embryologic de- for pituitary development shortly after formation of the
velopment of the pituitary or in the cascade from hypo- committed Rathke’s pouch. There have been at least eight
thalamic stimulation of GH release to completion of IGF mutations in PITX2 resulting in Rieger syndrome which
effects on growth. Acquired abnormalities affecting the includes anomalies of the anterior chamber of the eye,
GH/IGF axis range from damage to the hypothalamic dental hypoplasia, protuberant umbilicus, and mental re-
pituitary region from trauma, tumors, infection, autoim- tardation, but it is uncertain whether pituitary hormone
mune disease, or radiation, to a broad spectrum of chron- deficiencies are associated [16].
ic conditions characterized by catabolism. LHX3 accumulates in Rathke’s pouch and the primor-
dium of the pituitary, and is thought to be involved in the
Embryology of the Pituitary Gland establishment and maintenance of the differentiated cell
Pituitary differentiation in the embryo is in response types [17]. Mutations of this transcription factor result in
to an orchestration of transcription factors appearing deficiencies of all pituitary hormones except adrenocor-
and disappearing in precise sequence. At 3 weeks gesta- ticotropin, and cervical spine rigidity indicating extrapi-
tion, the ectodermal stomodeum of the embryo develops tuitary function for this factor in some families [18].
an outpouching anterior to the buccopharyngeal mem- LHX3 and LHX4 belong to the LIM family of homeobox
brane. This outpocketing is Rathke’s pouch, which usu- genes expressed early in Rathke’s pouch, with expression
ally separates from the oral cavity and will give rise to the persisting into adulthood. This has suggested a mainte-
adenohypophysis (anterior lobe) of the pituitary gland. nance function for anterior pituitary cells. Four patients
An evagination of the diencephalon then gives rise to the in two unrelated families have been identified with LHX3
neurohypophysis of the pituitary gland. Rarely, the prim- mutations with a hormonal phenotype similar to PROP1
itive oral cavity origin of the pituitary results in a func- deficiency, including marked pituitary enlargement in
tional pharyngeal adenohypophysis [11]. Secretion of pi- one patient (see below) [18]. There has been only one re-
tuitary hormones can be detected as early as week 12 in port of a mutation within LHX4 [19].
the fetus, and some of these hormones are found within The sonic hedgehog signaling pathway, mediated by
the pituitary by 8 weeks gestation [12]. three GLI genes, has been identified in a variety of tissues
Differentiation of the primordial pituitary gland re- and has been implicated in complex disorders of pituitary
quires a cascade of factors to be expressed in critical tem- development. Mutations of GLI2 are associated with ho-
poral and spatial relationships. These include extracellu- loprosencephaly [20]. Penetrance is variable, with all af-
lar signaling factors from the adjacent diencephalon that fected patients having pituitary gland dysfunction.
100 Ann Nestlé [Engl] 2007;65:97–108 Rosenbloom
Table 1. Mutations resulting in isolated growth hormone deficiency (IGHD) or multiple pituitary hormone deficiencies (MPHD)
Gene Hormone deficiency Pituitary anatomy Other abnormalities Inheritance
HESX1 IGHD to MPHD AP hypoplasia, ectopic PP, Septo-optic dysplasia; absent corpus Recessive,
absent infundibulum callosum dominant
LHX3 GH, TSH, LH, FSH, Small, normal, or enlarged AP Short neck and cervical spine with Recessive
PRL limited rotation in some families
LHX4 GH, TSH, ACTH Small AP, ectopic PP Cerebellar abnormalities Dominant
SOX3 IGHD to MPHD AP hypoplasia, ectopic PP, Mental retardation X-linked
absent infundibulum
GLI2 MPHD AP hypoplasia Holoprosencephaly; multiple midline Dominant
defects
PITX2 Unknown in human (Hypoplasia and MPHD in mice) Rieger syndrome (see text) Dominant
PROP1 GH, PRL, TSH, LH, Small, normal, or enlarged AP – Recessive
FSH, 8ACTH
PIT1 (POU1F1) GH, PRL, TSH Normal or hypoplastic AP – Recessive,
dominant
GHRH receptor IGHD Hypoplastic AP Small head size in one population Recessive
GH1 IGHD; some muta- Hypoplastic or normal AP Most IGHD-IA develop antibodies Recessive,
tions with MPHD with GH treatment; agammaglobulin- dominant,
emia in some IGHD III X-linked
AP = Anterior pituitary; PP = posterior pituitary.
X-linked hypopituitarism results from duplications of Somatotroph development is also dependent on hypo-
Xq26–27, a region that includes the SOX3 gene, for which thalamic GH-releasing hormone (GHRH). A mutation in
a polyalanine expansion has been described in a pedigree the gene encoding the GHRH receptor results in severe
with X-linked mental retardation and GHD [21–23]. Mu- GHD [30–32].
tations that result in either overdosage or underdosage of
SOX3 are associated with infundibular hypoplasia and Functional Anatomy of the Anterior Pituitary Gland
variable hypopituitarism [24]. (Adenohypophysis)
PROP1 (PROphet of Pit1) represses HESX1 expression The adenohypophysis receives hormonal modulating
and is required for initial determination of pituitary cell signals from the hypothalamus, transmitted from ven-
lineages, including gonadotropes and those of Pit1. At tromedial and infundibular nuclei axons which termi-
least 10 recessive mutations have been described in PROP1 nate in the hypophyseal portal system. These signals re-
that result in GH, prolactin (PRL), thyroid-stimulating sult in production of corticotropin (ACTH) by 8 weeks
hormone (TSH), gonadotropin and, in some families or gestation, thyrotropin (TSH) by 15 weeks gestation, so-
as the patients age, adrenocorticotropic hormone (ACTH) matotropin (GH) by 10–11 weeks gestation, PRL by 12
deficiency [25, 26]. Patients with PROP1 gene mutations weeks, and the gonadotropes luteinizing hormone (LH)
may have pituitary gland enlargement originating from and follicle-stimulating hormone (FSH) by 11 weeks.
the intermediate lobe [27, 28]. Eleven recessive and four There are at least three distinct hormone-producing cell
dominant mutations have been reported affecting the populations classified by staining characteristics [12].
Pit1 gene (currently referred to as POU1F1), with resul- Fifty percent of the cells are chromophobes, 40% are
tant GH, PRL, and TSH deficiency [13, 25]. POU1F1 gene characterized as acidophils, and the remainder as baso-
defects are associated with variable pituitary hypoplasia phils. Acidophils secrete GH or PRL. Basophils secrete
[29]. TSH, LH, FSH, or ACTH. Some basophils have a positive
Physiology of Growth Ann Nestlé [Engl] 2007;65:97–108 101
periodic acid-Schiff (PAS) base reaction: these are the dition to the GHRH receptor defects noted earlier, four
cells which secrete the glycoproteins LH, FSH, or TSH. autosomal recessive disorders, an autosomal dominant
While chromophobe cells are known to produce ACTH mutation, and an X-linked form of isolated GHD have
in the rat pituitary, the role of these cells in the human been described. Most children with a mutation of the
pituitary remains unclear. GH1 gene, resulting in the total absence of GH, treat in-
Anterior pituitary hormones enter the portal venous jected recombinant human GH as a foreign protein and
system to drain into the cavernous sinus, enter the gen- develop resistance after a few months of treatment due to
eral circulation, and ultimately exert long-distance influ- the inactivating antibodies they develop.
ence over their respective target organs. TSH promotes A number of synthetic hexapeptides, referred to as
growth of the thyroid and production of thyroxine. LH GH-releasing peptides (GHRPs), have been developed
and FSH stimulate gonadal maturation and hormonal cy- that act on other receptors to stimulate GH release [36,
cling. GH exerts indirect growth effects through the elab- 37]. The naturally occurring ligand for the GHRP recep-
oration of IGF-I in the liver and epiphyses, direct growth tor, ghrelin, has been isolated and cloned [38]. Ghrelin is
effects on chondrocyte proliferation, and direct metabol- unique among mammalian peptides in its requirement of
ic effects primarily in adipose tissue. a posttranslational modification for activation. This in-
The rich blood supply of the pituitary gland is subject volves addition of a straight chain octanyl group confer-
to interruption during periods of severe hypotensive ring a hydrophobic property to the N terminus which
stress and hypoxia, resulting in the Sheehan syndrome of may permit entry of the molecule into the brain. Similar
hypopituitarism, classically described after intrapartum to synthetic GHRPs, ghrelin binds with high affinity and
hypotension, but possible in any hypovolemic crisis or specificity to a distinct G protein-coupled receptor [39].
increased intracranial pressure episode, as in hypopitu- Unlike GHRH, ghrelin is synthesized primarily in the
itarism following recovery from cerebral edema compli- fundus of the stomach [38], as well as in the hypothala-
cating diabetic ketoacidosis [33]. The internal carotid ar- mus, heart, lung and adipose tissue, and its receptor is
teries supply the vascular branches which bathe the pitu- more widely distributed than that of GHRH [40]. Ghrelin
itary. The hypophyseal portal vessels, which originate has widespread metabolic effects in addition to inducing
from capillary beds in the median eminence and infun- GHRH release and being synergistic with GHRH in the
dibular stem, supply the adenohypophysis [34]. stimulation of GH release through the serine 3 residue of
ghrelin. Ghrelin increases prolactin, ACTH, cortisol and
Biochemistry and Physiology of the GH/IGF-I/IGF aldosterone release, and increases food intake and weight
Binding Protein Axis gain [41].
Growth Hormone Some 75% of the circulating GH is in the 22-kDa form.
Human GH is a single-chain, 191-amino acid, 22-kDa Alternative splicing of codon 2 results in a deletion of 11
protein, containing two intramolecular disulfide bonds amino acids and formation of a 20-kDa fragment ac-
[35]. Release of GH from the anterior pituitary somato- counting for 5–10% of secreted GH. Other circulating
trophs is controlled by the balance between stimulatory forms include deaminated, N-acetylated, and oligomeric
GH-releasing hormone (GHRH) and inhibitory soma- GH. About 50% of GH circulates in the free state, the rest
tostatin from the hypothalamus. This balance is regu- bound principally to GH-binding protein (GHBP). Be-
lated by neurologic, metabolic, and hormonal influences; cause the binding sites for the radioimmunoassay of GH
numerous neurotransmitters and neuropeptides are in- are not affected by the GHBP, both bound and unbound
volved. These include vasopressin, corticotropin-releas- GH are measured [42].
ing hormone, thyrotropin-releasing hormone, neuropep-
tide Y, dopamine, serotonin, histamine, norepinephrine, GHBP and the GH Receptor
and acetylcholine, which respond to various circum- A high-affinity GHBP was identified in rabbit and hu-
stances that affect GH secretion such as sleep, nutritional man serum in the mid-1980s [43], and separate reports in
state, stress, and exercise. Other hormones including glu- 1987 found this binding protein to be absent in the sera
cocorticoids, sex steroids, and thyroxin also influence se- of patients with GH resistance [44, 45], who were identi-
cretion of GH. These various influences are important in fied by a high circulating GH concentration with a phe-
the evaluation of GH secretion, which may be abnormal notype of severe GHD. The recognition that circulating
despite normal somatotroph function. Stimulation of GH GHBP in rabbit serum corresponded to liver cytosolic
release by GHRH is via specific GHRH receptors. In ad- GHBP was followed by the purification, cloning, and se-
102 Ann Nestlé [Engl] 2007;65:97–108 Rosenbloom
quencing of human GHBP [46]. The human GHBP was gene included the first description of a genetic defect of
found to be structurally identical to the extracellular hor- the GHR, a deletion of exons 3, 5, and 6 [47]; recognition
mone-binding domain of the membrane-bound GH re- that the exon-3 deletion represented an alternatively
ceptor (GHR). The entire human GHR gene on chromo- spliced variant without functional significance resolved
some 5 was subsequently characterized [47]. The GHR the dilemma of explaining the deletion of nonconsecu-
was the first to be cloned of a family of receptors that in- tive exons. In contrast to the alternatively spliced variant
cludes the receptor for PRL and numerous cytokine re- lacking exon 3, the first mutation of this exon has been
ceptors. Members of this family share ligand and receptor described in a typical GHR-deficient patient with hetero-
structure similarities, in particular the requirement that zygosity for a nonsense mutation in exon 4, and family
the ligand bind to two or more receptors or receptor sub- studies indicate that heterozygosity for the exon 3 mutant
units and interact with signal transducer proteins to ac- has no effect. This study also raises questions regarding
tivate tyrosine kinases [48]. the origin and function of the exon 3 deleted variant.
In humans, GHBP is the proteolytic product of the ex- More recently this isoform, present in either the homozy-
tracellular domain of the GHR. This characteristic per- gous or heterozygous state, was found to be associated
mits assaying circulating GHBP as a measure of cellular with 1.7–2 times more growth acceleration from GH ad-
bound GHR, which usually correlates with GHR func- ministration during 2 years of treatment of children with
tion. The GH molecule binds to cell surface GHR, which short stature who had been small for gestational age or
dimerizes with another GHR so that a single GH mole- had idiopathic short stature. In addition to the original
cule is enveloped by two GHR molecules [49]. The intact exon 5, 6 deletion, another deletion of exon 5 has been
receptor lacks tyrosine kinase activity, but is closely as- described, along with numerous nonsense mutations,
sociated with JAK2, a member of the Janus kinase family. missense mutations, frame shift mutations, splice muta-
JAK2 is activated by binding of GH with the GHR dimer, tions, and a unique intronic mutation resulting in inser-
which results in self-phosphorylation of the JAK2 and a tion of a pseudo-exon. A number of other mutations have
cascade of phosphorylation of cellular proteins. Included been described which are either polymorphisms or have
in this cascade are signal transducers and activators of not occurred in the homozygous or compound heterozy-
transcription (STATs), which couple ligand binding to gous state [54].
the activation of gene expression, and mitogen-activated The point mutations, which result in severe GH insen-
protein kinases. Other effector proteins have also been sitivity when present in the homozygous state or as a
examined in various systems. This is a mechanism typi- compound heterozygote, are all associated with the typi-
cal of the GH/PRL/cytokine receptor family [48, 50]. In cal phenotype of severe GHD. All but a few of the defects
human GH-GHR transduction, STAT5b appears to be result in absent or extremely low levels of GHBP. Note-
the most important cellular protein activated. Five dis- worthy is the D152H missense mutation which affects the
tinct homozygous mutations have been described in six dimerization site, thus permitting the production of the
patients from five families, resulting in severe growth extracellular domain in normal quantities but failure of
failure and variable immune incompetence, indicating dimerization at the cell surface, which is necessary for
the importance of STAT5b in cytokine function, as well signal transduction and IGF-I production. Two defects
as its primary role in GH-GHR transduction [51]. that are close to [G223G] or within [R274T], the trans-
The GHR in humans is also synthesized in a truncated membrane domain, result in extremely high levels of
form (GHRtr) lacking most of the intracellular domain. GHBP. These defects interfere with the normal splicing
Although the quantity of this GHRtr is small relative to of exon 8 which encodes the transmembrane domain,
the full-length GHR, release of GHBP from this isoform with the mature GHR transcript being translated into a
is increased [52]. Some of the changes in body composi- truncated protein that retains GH-binding activity but
tion that occur with GH treatment in GHD may be re- cannot be anchored to the cell surface.
lated to changes in the relative expression of GHR and As noted, all these homozygous defects and the com-
GHRtr [53]. pound heterozygotes, whether involving the extracellu-
Over 50 mutations in the GHR have been described in lar domain or the transmembrane domain and whether
the approximately 250 known patients with GH insensi- associated with very low or unmeasurable GHBP, result
tivity, which result in a clinical picture identical to that of in a typical phenotype of severe GHD. In contrast, the
severe GHD but with elevated serum GH concentrations intronic mutation present in the heterozygous state in a
[2, 51]. The report of the characterization of the GHR mother and daughter with relatively mild growth failure
Physiology of Growth Ann Nestlé [Engl] 2007;65:97–108 103
(both standard deviation score, SDS, for height –3.6), and Insulin-Like Growth Factor-I
resulting in a dominant negative effect on GHR forma- Most of the growth effect that gives GH its name is
tion, is not associated with other phenotypic features of actually an effect of IGF-I production [56, 57]. IGF-I is a
GHD. This splice mutation preceding exon 9 results in an 70-residue single-chain basic peptide, and IGF-II a slight-
extensively attenuated, virtually absent intracellular do- ly acidic 67-residue peptide. Their structure is similar to
main. Japanese siblings and their mother have a similar proinsulin, A and B chains connected by disulfide bonds
heterozygous point mutation of the donor splice site in and a connecting C-peptide, but unlike the posttransla-
intron 9, also resulting in mild growth failure compared tional processing of insulin, there is no cleavage of C-pep-
to GH receptor deficiency (GHRD), but with definite, al- tide. The two IGFs share approximately two thirds of
though mild, phenotypic features of GHD. GHBP levels their possible amino acid positions and are 50% homolo-
in the Caucasian patients were at the upper limit of nor- gous to insulin [58, 59]. The connecting C-peptide is 12
mal with a radiolabeled GH-binding assay, and in the amino acids long in the IGF-I molecule and 8 amino ac-
Japanese patients twice the upper limit of normal, using ids long in IGF-II, and has no homology with the compa-
a ligand immunofunction assay. These heterozygous rable region in the proinsulin molecule. The IGFs also
GHR mutants transfected into permanent cell lines have differ from proinsulin in having carboxy terminal exten-
demonstrated increased affinity for GH compared to the sions. These similarities and differences from insulin ex-
wild-type full-length GHR, with markedly increased plain the ability of IGFs to bind to the insulin receptor
production of GHBP. When co-transfected with full- and insulin’s ability to bind to the type-1 IGF receptor,
length GHR a dominant negative effect results from over- as well as the specificity of IGF binding to the IGF-bind-
expression of the mutant GHR and inhibition of GH-in- ing proteins (IGFBPs).
duced tyrosine phosphorylation and transcription acti-
vation. Naturally occurring truncated isoforms have also IGF-Binding Proteins
shown this dominant negative effect in vitro [54]. Hepatic IGF-I circulates almost entirely bound to
A novel intronic point mutation was discovered in a IGFBPs, with !1% being free. The IGFBPs are a family of
highly consanguineous family with two pairs of affected 6 structurally related proteins with a high affinity for
cousins with GHBP-positive GH insensitivity, severe binding IGF. At least 4 other related proteins with lower
short stature, but without the facial features of severe affinity for IGF peptides have been identified and are re-
GHD or GH insensitivity. This mutation resulted in a ferred to as IGFBP-related proteins [60]. The principal
108-bp insertion of a pseudo-exon between exons 6 and binding protein, IGFBP-3, binds about 90% of circulating
7, predicting an in-frame, 36-residue amino acid se- IGF-I in a large (150–200 kDa) ternary complex consist-
quence. This is a region critically involved in receptor ing of IGFBP-3, an acid labile subunit (ALS), and the IGF
dimerization. molecule. ALS and IGFBP-3 are produced in the liver as
Of approximately 250 reported cases of typical GHR a direct effect of GH. The ALS stabilizes the IGF–IGFBP3
deficiency, ethnic origin is predominantly Middle East- complex, reduces the passage of IGF-I to the extravascu-
ern, Mediterranean, and South Asian. Nearly 50% are lar compartment, and extends its half-life [61]. The re-
Oriental Jews as described in the original report, or mainder of bound IGF is in a 50-kDa complex with most-
known descendants of Iberian Jews who converted to Ca- ly IGFBP-1 and IGFBP-2. IGFBP-1 concentrations are
tholicism during the Spanish Inquisition. The latter com- controlled by nutritional status as reflected in insulin lev-
prise the largest cohort (n 170) and the only genetically els, with the highest IGFBP-1 concentrations found in the
homogenous group, all but one subject having the E180 fasting, hypoinsulinemic state. The circulating concen-
splice site mutation which was also found in one Israeli tration of IGFBP-2 is less fluctuant and is partly under the
patient of Moroccan heritage, and recently in several af- control of IGF-I; levels are increased in IGF-I deficiency
fected children from four families not previously known due to GH insensitivity, but increase further with IGF-I
to be related from northeast Brazil [55]. Most of the other therapy of such patients [62].
defects appear to be highly family specific, with the R43X The IGFBPs modulate IGF action by controlling stor-
mutation that is seen in a single Ecuadorian patient, two age and release of IGF-I in the circulation and influencing
other nonsense mutations (C38X, R217X), and the intron its binding to its receptor, facilitate storage of IGFs in
4 splice mutation being the only ones thus far described extracellular matrices, and exert independent actions.
which appear in disparate populations, on different ge- IGFBPs 1, 2, 4, and 6 inhibit IGF action by preventing
netic backgrounds, indicating mutational hotspots [54]. binding of IGF-I with its specific receptor. The binding of
104 Ann Nestlé [Engl] 2007;65:97–108 Rosenbloom
IGFBP-3 to cell surfaces is thought to decrease its affinity, tinuing investigation. The most familiar of these compo-
effectively delivering the IGF-I to the type-1 IGF receptor. nents are IGF-I, IGFBP-3, and ALS, because they are syn-
IGFBP-5 potentiates the effects of IGF-I in a variety of thesized by the liver and secreted into the circulation,
cells. Its binding to extracellular matrix proteins allows allowing them to be measured as circulating concentra-
fixation of IGFs and enhances binding to hydroxyapatite. tions. The other GH effects are not directly measurable
IGFs stored in such a manner in soft tissue may enhance but inferred from much animal and some human data;
wound healing. IGF independent mechanisms for IGFBP- they are epiphyseal prechondrocyte differentiation and
1 and IGFBP-3 proliferative effects have been demonstrat- enhancement of local (autocrine/paracrine) production
ed in vitro and nuclear localization of IGFBP-3 has been of IGF-I, thereby stimulating clonal expansion of the dif-
reported. In addition to IGFBP phosphorylation and cell ferentiating chondrocytes [2, 56, 57].
surface association determining the influence of IGFBPs, The importance of IGF-I in normal intrauterine
specific protease activity, particularly affecting IGFBP-3, growth in humans has been demonstrated in a single pa-
is also important in the modulation of IGF action in target tient with a homozygous partial deletion of the IGF-I
tissues. The proteolytic activity may alter the affinity of gene, a patient with mutation of the IGF-I gene resulting
the binding protein for IGF-I, resulting in the release of in high circulating levels of an ineffective IGF-I, and in
free IGF-I for binding to the IGF-I receptor [63]. two patients with mutations of the IGF-I receptor, all hav-
ing severe intrauterine growth retardation [2]. Cord se-
IGF Receptors rum IGF-I and IGF-II concentrations correlate with birth
IGF binding involves 3 types of receptors, the struc- weight and are significantly increased in large for gesta-
turally homologous insulin receptor, the type-1 IGF re- tional age infants compared with appropriate for gesta-
ceptor, and the distinctive type-2 IGF-II/mannose-6- tional age newborns [64]. Intrauterine IGF-I synthesis,
phosphate receptor. Splice variants and atypical forms however, does not appear to be GH-dependent, because
occur but have not been found to have physiologic sig- most patients with genetically determined severe IGF-I
nificance, insulin/IGF-I hybrid receptors, however, are deficiency, due to GHRH defects, GHRD, or GH gene
ubiquitous and may be the most important receptors for mutations, have normal or only minimally reduced intra-
IGF-I in some tissues [63]. uterine growth. SDS for length declines rapidly after
The type-1 IGF-I receptor and insulin receptor are het- birth, however, in these conditions, demonstrating the
erotetramers consisting of two ␣ subunits which contain immediate need for GH-stimulated IGF-I synthesis for
the binding sites and two  subunits containing a trans- postnatal growth [2]. Growth velocity in the absence of
membrane domain, an adenosine triphosphate-binding GH is approximately half normal, but has sometimes
site, and a tyrosine kinase domain comprising the signal been reported to be normal or supranormal [65]. This ap-
transduction system [63]. The IGF-I receptor is able to parent growth without GH has been described in patients
bind IGF-I and IGF-II with high affinity but the affinity after craniopharyngioma resection, in septo-optic dys-
for insulin is approximately 100-fold less. Although the plasia, in obese children with GHD, in GH-deficient in-
insulin receptor has a low affinity for IGF-I, IGF-I is pres- fants, and in patients who had undergone resection of a
ent in the circulation at molar concentrations that are variety of central nervous system tumors [66]. Normal or
1,000 times those of insulin. Thus, even a small insulin- supranormal growth velocity has been attributed to hy-
like effect of IGF-I could be more important than that of perinsulinemia, increased leptin levels, or hyperprolac-
insulin itself, were it not for the IGFBPs that control the tinemia. PRL levels are not consistently increased, how-
availability and activity of IGF-I. In fact, intravenous in- ever. Obesity or rapid weight gain is a frequent common
fusion of recombinant human IGF-I can induce hypogly- denominator among these patients who demonstrate low
cemia, especially in the IGFBP-3-deficient state [62]. It is GH levels to provocative stimuli, low IGF-I and IGFBP-1,
not known why IGF-II and mannose-6-phosphate share a and low IGFBP-3 levels.
receptor. This receptor differs from the type-1 receptor in The metabolic and growth effects of GH and IGF-I are
binding only IGF-II with high affinity, IGF-I with low af- compared in table 2. In addition to direct protein-sparing
finity, and insulin not at all [63]. effects and synthesis and release of IGF-I from the liver,
GH stimulates autocrine and paracrine production of
Role of the GH/IGF-I Axis in Growth IGF-I in other tissues, primarily bone and muscle. GH
The growth effect of GH has at least three compo- has a direct effect on differentiation of prechondrocytes
nents, their relative contributions being a subject of con- into early chondrocytes, which in turn secrete IGF-I. This
Physiology of Growth Ann Nestlé [Engl] 2007;65:97–108 105
Table 2. Metabolic effects of GH and IGF-I and the stimulation of local production of IGF-I led to
the hypothesis that autocrine/paracrine IGF-I was the
GH IGF-I main determinant of GH-dependent postnatal body
GH secretion – Decreased growth, and that hepatic or endocrine IGF-I served pre-
IGF-I production Increases – dominantly as a negative feedback regulator of GH secre-
IGFBP-1 Decreases Decreases tion [57]. Subsequent studies of mice with selective dele-
IGFBP-2 Decreases Increases tion of the hepatic IGF-I gene described unaffected
IGFBP-3 Increases No effect growth [2]. Deletion of the ALS gene in mice and its mu-
Insulin
Secretion Increases Decreases tation in man results in very low circulating IGF-I and
Sensitivity Decreases Increases IGFBP-3 concentrations, but only a 15% reduction in
Hepatic glucose output Increases Decreases postnatal growth in the mice [61]. It is uncertain if there
Muscle glucose uptake Decreases Increases was any growth effect in the two patients with ALS mu-
Lipolysis Increases No effect1 tations, one of whom reached a stature of –0.9 SDS and
Nitrogen balance Increases Increases
Protein synthesis Increases Increases the other a height that was 0.4 SDS greater than mean
parental height [2].
1 Decreases with high doses.
Conclusion
local IGF-I stimulates clonal expansion and maturation The study of the physiology of growth has gone from
of the chondrocytes, resulting in growth [57]. It is esti- auxological observations, description of dysmorphic syn-
mated that 20% of normal growth (i.e. 40% of GH-stimu- dromes and inferred hormonal dysfunction with growth
lated growth) is the result of the direct effect of GH failure or, far less commonly, excessive growth, to reason-
on maturing bone and the autocrine/paracrine produc- ably accurate measurement of hormones influencing
tion of IGF-I in this tissue. Treatment studies of children growth, identification of many more growth factors, un-
with GHRD compared to GHD patients support this hy- derstanding of the control of bone growth, and definition
pothesis [2]. IGF-II is considered an important growth of the molecular basis for normal and abnormal growth
factor in utero, but its role in extrauterine life is unclear; states. These developments span only a half century. With
concentrations of IGF-II in serum parallel those of the rapidly accelerating capabilities for hormonal and
IGF-I. molecular study, the complexity of the genetic, hormon-
The direct stimulation by GH of mitosis in cartilage al, and environmental factors and their interaction in the
precursor cells of the growth plate, which have GHRs, growth process will continue to be unraveled.
References
1 Jones KL: Smith’s Recognizable Patterns of 6 Rosenbloom AL, Guevara-Aguirre J, Rosen- 10 Olney RC, Bukulmez H, Bartels CF, et al:
Human Malformation, ed 6. Philadelphia, feld RG, Pollock BH: Growth in growth hor- Heterozygous mutations in natriuretic pep-
Saunders, 2005. mone insensitivity. Trends Endocrinol tide receptor-B (NPR2) are associated with
2 Rosenbloom AL: Recombinant human in- Metab 1994;5:296–303. short stature. J. Clin Endocrinol Metab 2006;
sulin-like growth factor-I (rhIGF-I) and 7 Root AW, Diamond FB Jr: Overgrowth syn- 91:1229–1232.
rhIGF-I/rhIGF-binding-protein-3:new dromes: evaluation and management of the 11 Weber FT, Donnelley WH, Behar RL: Hypo-
growth treatment options? J Pediatr 2007; child with excessive linear growth; in Lif- pituitarism following extirpation of a pha-
150:7–11. shitz F (ed): Pediatric Endocrinology, ed 5. ryngeal pituitary. Am J Dis Child 1977; 131:
3 Smith DW: Growth and Its Disorders. Phila- New York, Informa Health Care, 2007, vol 2, 525–528.
delphia, Saunders, 1977. pp 163–194. 12 Junqueira LC, Carneiro J: Basic Histology, ed
4 Lampl M, Veldhuis JD, Johnson ML: Salta- 8 Habicht J-P, Martorelli R, Yarborough C, et 3. Los Altos, Lange Medical, 1980, pp 410–
tion and stasis: a model of human growth. al: Height and weight standards for pre- 420.
Science 1992;258:801–803. school children. Lancet 1974;i:1051–1052. 13 Cohen LE: Genetic regulation of the embry-
5 Smith DW, Truog W, Rogers JE, et al: Shift- 9 Martorelli R: Genetics, environment and ology of the pituitary gland and somato-
ing linear growth during infancy: illustra- growth: Issues in the assessment of nutri- trophs. Endocrine 2000;12:99–106.
tion of genetic factors in growth from fetal tional status; in Velazquez A, Bourges H
life through infancy. J Pediatr 1976; 89: 225– (eds): Genetic Factors in Nutrition. New
230. York, Academic Press, 1985.
106 Ann Nestlé [Engl] 2007;65:97–108 Rosenbloom
14 Dattani M, Martinez-Barbera J-P, Thomas 28 Rosenbloom AL, Selman-Almonte A, Brown 41 Konturek PC, Konturek JW, Czesnikiewicz-
PQ: Mutations in the homeobox gene MR, et al: Clinical and biochemical pheno- Guzik M, et al: Neuro-hormonal control of
HESX1/HESX1 associated with septo optic type of familial anterior hypopituitarism food intake; basic mechanisms and clinical
dysplasia in human and in mouse. Nat Genet from mutation of PROP-1 gene. J Clin Endo- implications. J Physiol Pharmacol 2005;
1998;19:125–133. crinol Metab 1999;84:50–57. 56(suppl 6):5–25.
15 Cohen RN, Cohen LE, Botero D, et al: En- 29 Turton JP, Reynaud R, Mehta A, et al: Novel 42 Postel-Vinay MC, Kelly PA: Growth hor-
hanced repression by HESX1 as a cause of mutations within the POU1F1 gene associ- mone receptor signalling. Baillieres Clin En-
hypopituitarism and septooptic dysplasia. J ated with variable combined pituitary hor- docrinol Metab 1996;10:323–326.
Clin Endocrinol Metab 2003;88:4832–4839. mone deficiency. J Clin Endocrinol Metab 43 Ymer SI, Herrington AC: Evidence for the
16 Cohen LE, Radovick S: Molecular basis of 2005;90:4762–4770. specific binding of growth hormone to a re-
combined pituitary hormone deficiencies. 30 Maheshwari HG, Silverman BL, Dupuis J, ceptor like protein in rabbit serum. Mol Cell
Endocr Rev 2002;23:431–442. Baumann G: Phenotypic and genetic analy- Endocrinol 1985;41:153–161.
17 Zhadanov AB, Bertuzzi S, Taira M, et al: Ex- sis of a syndrome caused by an inactivating 44 Daughaday WH, Trivedi B: Absence of se-
pression pattern of the murine LIM class ho- mutation in the GH releasing hormone re- rum growth hormone binding protein in pa-
meobox gene Lhx3 in subsets of neural and ceptor: dwarfism of Sindh. J Clin Endocrinol tients with growth hormone receptor defi-
neuroendocrine tissues. Dev Dyn 1995; 202: Metab 1998;83:4065–4074. ciency (Laron dwarfism). Proc Natl Acad Sci
354–364. 31 Murray RA, Maheshwari HG, Russell EJ, USA 1987;84:4636–4640.
18 Netchine I, Sobrier M-L, Krude H, et al: Mu- Baumann G: Pituitary hypoplasia in patients 45 Baumann G, Shaw MA, Winter RJ: Absence
tations in LHX3 result in a new syndrome with a mutation in the growth hormone-re- of plasma growth hormone-binding protein
revealed by combined pituitary hormone de- leasing hormone receptor gene. Am J Neuro- in Laron-type dwarfism. J Clin Endocrinol
ficiency. Nat Genet 2000;25:182–186. radiol 2000;21:685–689. Metab 1987;65: 814–816.
19 Machinis K, Pantel J, Netchine I, et al: Syn- 32 Salvatori R, Fan X, Phillips JA 3rd, et al: 46 Leung DW, Spencer SA, Cachianes G, et al:
dromic short stature in patients with a germ- Three new mutations in the gene for the Growth hormone receptor and serum bind-
line mutation in the LIM homeobox LHX4. growth hormone (GH)-releasing hormone ing protein: purification, cloning and ex-
Am J Hum Genet 2001;69:961–968. receptor in familial isolated GH deficiency pression. Nature 1987;330:537–543.
20 Roessler EYZ, Mullor JL, Casas E, et al: Loss- type Ib. J Clin Endocrinol Metab 2001; 86: 47 Godowski PJ, Leung DW, Meacham LR, et al:
of-function mutations in the human GLI2 273–279. Characterization of the human growth hor-
gene are associated with pituitary anomalies 33 Keller RJ, Wolfsdorf JI: Isolated growth hor- mone receptor gene and demonstration of a
and holoprosencephaly-like features. Proc mone deficiency after cerebral edema com- partial gene deletion in two patients with
Natl Acad Sci USA 2003;100:13424–13429. plicating diabetic ketoacidosis. N Engl J Med Laron-type dwarfism. Proc Natl Acad Sci
21 Solomon NM, Nouri S, Warne GL, et al: In- 1987;316:857–859. USA 1989;86:8083–8087.
creased gene dosage at Xq26–q27 is associ- 34 Netter FH: The CIBA Collection of Medical 48 Kelly PA, Nagano M, Sotiropoulos A, et al:
ated with X-linked hypopituitarism. Ge- Illustrations. Vol 4: Endocrine System and Growth hormone-prolactin receptor gene
nomics 2002;79:553–559. Selected Metabolic Diseases. Chicago, Don- family; in Shiverick KT, Rosenbloom AL
22 Solomon NM, Ross SA, Morgan T, et al: Ar- nelley & Sons, 1964, section 1, plate 2.1. (eds): Human Growth Hormone Pharmacol-
ray comparative genomic hybridisation 35 Lewis UJ, Singh RNP, Tutwiler GH, et al: Hu- ogy: Basic and Clinical Aspects. Boca Raton,
analysis of boys with X linked hypopituita- man growth hormone: a complex of pro- CRC Press, 1995, pp 13–28.
rism identifies a 3.9 Mb duplicated critical teins. Recent Prog Horm Res 1980; 36: 477– 49 de Vos AM, Ultsch M, Kossiakoff AA: Hu-
region at Xq27 containing SOX3. J Med Gen- 508. man growth hormone and extracellular do-
et 2004;41:669–678. 36 Bowers CY, Momany F, Reynolds GA, Hong main of its receptor: crystal structure of the
23 Laumonnier F, Ronce N, Hamel BC, et al: A: On the in vitro and in vivo activity of a complex. Science 1992;255:306–312.
Transcription factor SOX3 is involved in X- new synthetic hexapeptide that acts on the 50 Campbell GS: Growth-hormone signal
linked mental retardation with growth hor- pituitary to specifically release growth hor- transduction. J Pediatr 1997;131:S42–S44.
mone deficiency. Am J Hum Genet 2002; 71: mone. Endocrinology 1984;114:1531–1536. 51 Rosenfeld RG, Belgorosky A, Camacho-
1450–1455. 37 Goth MI, Lyons CE, Canny BJ, Thorner MO: Hubner C, et al: Defects in growth hormone
24 Woods KS, Cundall M, Turton J, et al: Over- Pituitary adenylate cyclase activating poly- receptor signaling. Trends Endocrinol Metab
and underdosage of SOX3 is associated with peptides, growth hormone (GH) releasing 2007;18:134–141.
infundibular hypoplasia and hypopituita- peptide and GH releasing hormone stimu- 52 Dastot F, Sobrier ML, Duquesnoy P, et al: Al-
rism. Am J Hum Genet 2005;76:833–849. late GH release through distinct pituitary re- ternative spliced forms in the cytoplasmic
25 Bottner A, Keller E, Kratzsch J, et al: PROP1 ceptors. Endocrinology 1992; 130:939–944. domain of the human growth hormone (GH)
mutations cause progressive deterioration of 38 Kojima M, Hosada H, Date Y, et al: Ghrelin receptor regulate its ability to generate a sol-
anterior function including adrenal insuffi- is a growth hormone releasing acetylated uble GH binding protein. Proc Natl Acad Sci
ciency: a longitudinal analysis. J Clin Endo- peptide from stomach. Nature 1999; 402: USA 1996;93:10723–10728.
crinol Metab 2004;89:5256–5265. 656–660. 53 Fisker S, Kristensen K, Rosenfalck AM, et al:
26 Reynaud R, Chadli-Chaieb M, Vallette-Ka- 39 Bowers CY: Unnatural growth hormone-re- Gene expression of a truncated and the full-
sic S, et al: A familial form of congenital hy- leasing peptide begets natural ghrelin. J Clin length growth hormone (GH) receptor in
popituitarism due to a PROP1 mutation in a Endocrinol Metab 2001;86:1464–1469. subcutaneous fat and skeletal muscle in GH-
large kindred: phenotypic and in vitro func- 40 Korbonits M, Bustin SA, Kojima M, et al: The deficient adults: impact of GH treatment. J
tional studies. J Clin Endocrinol Metab 2004; expression of the growth hormone secreta- Clin Endocrinol Metab 2001;86:792–796.
89:5779–5786. gogue receptor ligand ghrelin in normal and 54 Rosenbloom AL, Connor EL: Hypopituita-
27 Voutetakis A, Argyropoulou M, Sertedaki A, abnormal human pituitary and other neuro- rism and other disorders of the growth hor-
et al: Pituitary magnetic resonance imaging endocrine tumors. J Clin Endocrinol Metab mone-insulin-like growth factor-I axis; in
in fifteen patients with PROP1 gene muta- 2001;86:881–887. Lifshitz F (ed): Pediatric Endocrinology, ed
tions: pituitary enlargement may originate 5. New York, Informa Health Care, 2007, vol
from the intermediate lobe. J Clin Endocri- 2, pp 65–99.
nol Metab 2004;89:2200–2206.
Physiology of Growth Ann Nestlé [Engl] 2007;65:97–108 107
55 de Lima Jorge AA, de Menezes Filho HC, 59 Rinderknecht E, Humbel RE: Primary struc- 63 Collett-Solberg PF, Cohen P: Genetics,
Soares Lins TS, et al: Founder effect of E180- ture of human insulin like growth factor II. chemistry, and function of the IGF/IGFBP
splice mutation in growth hormone receptor FEBS Lett 1978;89:283–287. system. Endocrine 2000;12:121–136.
gene (GHR) identified in Brazilian patients 60 Baxter RG, Binoux MA, Clemmons DR, et al: 64 Giudice LC, de Zegher F, Gargosky SE, et al:
with GH insensitivity. Arq Bras Endocrinol Recommendations for nomenclature of the Insulin like growth factors and their binding
Metabol 2005;49:384–389. insulin-like growth factor binding proteins proteins in the term and preterm human fe-
56 van der Eerden BC , Karperien M, Wit JM: superfamily. J Clin Endocrinol Metab 1998; tus and neonate with normal and extremes
Systemic and local regulation of the growth 83:3213. of intrauterine growth. J Clin Endocrinol
plate. Endocr Rev 2003;24:782–801. 61 Domene HM, Bengolea SV, Jasper HG, Bois- Metab 1995;80:1548–1555.
57 Isaksson OG, Lindahl A, Nilsson A, Isgaard clair YR: Acid-labile subunit deficiency: 65 Geffner ME: The growth without growth
J: Mechanism of the stimulatory effect of phenotypic similarities and differences be- hormone syndrome. Endocrinol Metab Clin
growth hormone on longitudinal bone tween human and mouse. J Endocrinol In- North Am 1996;25:649–663.
growth. Endocr Rev 1987;8:426–438. vest 2005;28(suppl):43–46. 66 Phillip M, Moran O, Lazar L: Growth with-
58 Rinderknecht E, Humbel RE: The amino 62 Vaccarello MA, Diamond FB Jr, Guevara- out growth hormone. J Pediatr Endocrinol
acid sequence of human insulin like growth Aguirre J, et al: Hormonal and metabolic ef- Metab 2002;15(suppl 5):1267–1272.
factor I and its structural homology with fects and pharmacokinetics of recombinant
proinsulin. J Biol Chem 1978;253: 2769– human insulin-like growth factor-I in GH
2776. receptor deficiency/Laron syndrome. J Clin
Endocrinol Metab 1993;77:273–280.
108 Ann Nestlé [Engl] 2007;65:97–108 Rosenbloom
You might also like
- Seller Code of Conduct AppealDocument4 pagesSeller Code of Conduct AppealMAHER FAHADNo ratings yet
- Colorado Insurance HandbookDocument36 pagesColorado Insurance Handbookbomama01No ratings yet
- 10.feeder Analysis & ModelingDocument117 pages10.feeder Analysis & ModelingNamiraNo ratings yet
- Factors Affecting Growth and DevelopmentDocument18 pagesFactors Affecting Growth and DevelopmentAjay Pal NattNo ratings yet
- Puberty: Normal Physiology (Brief Overview)Document35 pagesPuberty: Normal Physiology (Brief Overview)aisyafikritamaNo ratings yet
- 02 Kuliah Semester VI - 2011 - 1Document40 pages02 Kuliah Semester VI - 2011 - 1almahdy25051976No ratings yet
- Human Growth and DevelopmentDocument25 pagesHuman Growth and DevelopmentMac Paul Alariao100% (1)
- Growth at Puberty: Supplement ArticleDocument9 pagesGrowth at Puberty: Supplement ArticleJefri SandikaNo ratings yet
- Puberty - Dr. AntonioDocument74 pagesPuberty - Dr. AntonioMonique BorresNo ratings yet
- Bahan 4Document7 pagesBahan 4Bayu SetiawanNo ratings yet
- Module 3. Factors - Effecting - Growth of A ChildDocument4 pagesModule 3. Factors - Effecting - Growth of A ChildArpit GoelNo ratings yet
- Peran Faktor Sosial-Ekonomi Dan Gizi Pada Tumbuh Kembang AnakDocument20 pagesPeran Faktor Sosial-Ekonomi Dan Gizi Pada Tumbuh Kembang AnakvaughnsischaNo ratings yet
- Medical Rogress: Stature Physiology andDocument12 pagesMedical Rogress: Stature Physiology andramadhanuNo ratings yet
- First Page PDFDocument1 pageFirst Page PDFAndrian SirghiNo ratings yet
- Child Ado L3Document24 pagesChild Ado L3Michael Layo TacleNo ratings yet
- Factors Affecting Human HeightDocument9 pagesFactors Affecting Human HeightStudies AccountNo ratings yet
- A Study On Various Factors Affecting Growth During The First Two Years of LifeDocument22 pagesA Study On Various Factors Affecting Growth During The First Two Years of LifeesycosminNo ratings yet
- 10 Constitutional Delay of Growth and PubertyDocument19 pages10 Constitutional Delay of Growth and PubertyPratita Jati PermatasariNo ratings yet
- Handout On Adolescent MedicineDocument50 pagesHandout On Adolescent MedicineReymart FernandezNo ratings yet
- Growth (I)Document10 pagesGrowth (I)api-3858544No ratings yet
- Lecture 5Document29 pagesLecture 5Jack HirschbergNo ratings yet
- The Endocrinology of GrowthDocument3 pagesThe Endocrinology of GrowthMoana KayeNo ratings yet
- k.3b Hormone Control of GrowthDocument22 pagesk.3b Hormone Control of GrowthWinson ChitraNo ratings yet
- Failure To ThriveDocument68 pagesFailure To ThriveRachel SepthyNo ratings yet
- FACTORS AFFECTING GROWTH AND DEVELOPMENT by NavarroDocument5 pagesFACTORS AFFECTING GROWTH AND DEVELOPMENT by NavarroShereen AlobinayNo ratings yet
- Final Growth and DevelopmentDocument61 pagesFinal Growth and Developmentdeepika kushwah100% (1)
- Physiology and PubertyDocument8 pagesPhysiology and PubertynofiajahNo ratings yet
- Growth Hormone DeficiencyDocument11 pagesGrowth Hormone DeficiencyIgor VasićNo ratings yet
- Growth and DevelopmentDocument3 pagesGrowth and DevelopmentVikas NehraNo ratings yet
- Human Development and LearningDocument15 pagesHuman Development and Learningmirwais khanNo ratings yet
- Korelasi Life Expectancy Dan StuntingfDocument10 pagesKorelasi Life Expectancy Dan StuntingfHaqqul AminNo ratings yet
- GADDocument18 pagesGADRubina MasihNo ratings yet
- Growth SpurtDocument35 pagesGrowth SpurtNeeraj AroraNo ratings yet
- Theories Factors Affecting Growth and DevelopmentDocument73 pagesTheories Factors Affecting Growth and DevelopmentYasmeen Jaffer100% (1)
- Intrauterine Growth RestrictionDocument7 pagesIntrauterine Growth RestrictionNurfazlinaNo ratings yet
- 8610 NewwDocument22 pages8610 NewwMuhammad AhmadNo ratings yet
- Diagnostic Approach To Children and Adolescents With Short Stature - UpToDateDocument25 pagesDiagnostic Approach To Children and Adolescents With Short Stature - UpToDatePreetyFaceNo ratings yet
- 1 2 Growth & Dev. General PrinciplesDocument69 pages1 2 Growth & Dev. General PrinciplesPoonam K JayaprakashNo ratings yet
- Disorder of Puberty RevisiDocument29 pagesDisorder of Puberty RevisiRamaNo ratings yet
- Physical GrowthDocument5 pagesPhysical GrowthrevgandaNo ratings yet
- 410 FullDocument13 pages410 FullrayalarasatitiNo ratings yet
- Management of Children With Short Stature: Pediatric Oncall April 2019Document9 pagesManagement of Children With Short Stature: Pediatric Oncall April 2019Rahmadi SartivanNo ratings yet
- Growth & DevelopmentDocument74 pagesGrowth & DevelopmentSubhashini RajshekarNo ratings yet
- Child Health Nursing NotesDocument9 pagesChild Health Nursing NotesBindhu RaniNo ratings yet
- Envhper00379 0045Document6 pagesEnvhper00379 0045ambersNo ratings yet
- k.3b Hormone Control of GrowthDocument22 pagesk.3b Hormone Control of GrowthJane Andrea Christiano DjianzonieNo ratings yet
- Growth Hormone Deficiency - A Case ReportDocument3 pagesGrowth Hormone Deficiency - A Case ReportAyiek WicaksonoNo ratings yet
- K9, FL, Hormone Control of Growth GDS-K9-2Document23 pagesK9, FL, Hormone Control of Growth GDS-K9-2Mari BelajarNo ratings yet
- Factors Affecting Growth and DevelopmentDocument13 pagesFactors Affecting Growth and DevelopmentSumayya MuhamedNo ratings yet
- Final Factors That Affecting Growth and DevlopmentDocument72 pagesFinal Factors That Affecting Growth and DevlopmentRenuga SureshNo ratings yet
- 03 GrowthHormoneDeficiency PDFDocument12 pages03 GrowthHormoneDeficiency PDFmihaiacNo ratings yet
- Hormone Control of GrowthDocument23 pagesHormone Control of GrowthFira TasyaNo ratings yet
- Hormone Control of Growth: Dedi Ardinata Yetty MachrinaDocument23 pagesHormone Control of Growth: Dedi Ardinata Yetty MachrinaAgus Salim BhrNo ratings yet
- Factors Influencing Fetal GrowthDocument54 pagesFactors Influencing Fetal GrowthBernardus Mario VitoNo ratings yet
- AgingDocument27 pagesAgingapi-3805717No ratings yet
- Growth and DevelopmentDocument4 pagesGrowth and DevelopmentqueenilynNo ratings yet
- Normal and Abnormal PubertyDocument37 pagesNormal and Abnormal Pubertyhazab1968100% (1)
- Pathophysiology of Short Stature (Specifically in Children)Document16 pagesPathophysiology of Short Stature (Specifically in Children)Dennis SukadanaNo ratings yet
- Growth and Development of The ChildDocument18 pagesGrowth and Development of The ChildObremponba Kwadwo MensahNo ratings yet
- Alice Yu B1 Growth Pattern EssayDocument6 pagesAlice Yu B1 Growth Pattern EssayAlice YuNo ratings yet
- Growth: DR Omar Ali Nafi MRCP Mutah UniversityDocument66 pagesGrowth: DR Omar Ali Nafi MRCP Mutah UniversityDr-Sulaiman Bani Abdel-rahmanNo ratings yet
- Nutritional Anthropological Physical Development Clinical Characteristics and Biochemical Parameters Among ChildrenFrom EverandNutritional Anthropological Physical Development Clinical Characteristics and Biochemical Parameters Among ChildrenNo ratings yet
- CT T SpssDocument11 pagesCT T Spssانجمن بدنسازی ایرانNo ratings yet
- Periodization For Youth SoccerDocument2 pagesPeriodization For Youth Soccerانجمن بدنسازی ایرانNo ratings yet
- Effects of Creatine Supplementation and Resistance Training On Muscle Strength and Weightlifting PerformanceDocument10 pagesEffects of Creatine Supplementation and Resistance Training On Muscle Strength and Weightlifting Performanceانجمن بدنسازی ایرانNo ratings yet
- Functional Strength Training Versus Movement Performance Therapy For Upper Limb Motor Recovery Early After Stroke: A RCTDocument8 pagesFunctional Strength Training Versus Movement Performance Therapy For Upper Limb Motor Recovery Early After Stroke: A RCTانجمن بدنسازی ایرانNo ratings yet
- American Association For The Advancement of Science ScienceDocument2 pagesAmerican Association For The Advancement of Science Scienceانجمن بدنسازی ایرانNo ratings yet
- American Association For The Advancement of Science ScienceDocument3 pagesAmerican Association For The Advancement of Science Scienceانجمن بدنسازی ایرانNo ratings yet
- Warehouse & Storage Techniques - Lecture 3Document29 pagesWarehouse & Storage Techniques - Lecture 3Muhammad AhsanNo ratings yet
- Huizhe Wu, MD Mingyan Liu, MD Shuang Wang, MD Wanyu Feng, MD, PHD Weifan Yao, Bs Haishan Zhao, Bs and Minjie Wei, MD, PHDDocument10 pagesHuizhe Wu, MD Mingyan Liu, MD Shuang Wang, MD Wanyu Feng, MD, PHD Weifan Yao, Bs Haishan Zhao, Bs and Minjie Wei, MD, PHDDyva VanillaNo ratings yet
- BacktoBasics-Fundamental Resolution Equation V2Document7 pagesBacktoBasics-Fundamental Resolution Equation V2Yeoh XWNo ratings yet
- Vegetarian Moussaka Recipe With Mushroom SauceDocument1 pageVegetarian Moussaka Recipe With Mushroom SauceMarija JesicNo ratings yet
- Long Term LiabilitiesDocument21 pagesLong Term Liabilitiesnioriatti8924No ratings yet
- The Prohibition of Alcohol in IslamDocument9 pagesThe Prohibition of Alcohol in IslamAsim Raheel KhanNo ratings yet
- 2007 06 08 OA FEA Kalaeloa Asphalt TerminalDocument255 pages2007 06 08 OA FEA Kalaeloa Asphalt TerminalEsteban Lopez ArboledaNo ratings yet
- SOALDocument4 pagesSOALFitri ShanumNo ratings yet
- The Influence of Organic Fertilizers On The Yield and Quality of WatermelonsDocument3 pagesThe Influence of Organic Fertilizers On The Yield and Quality of WatermelonsresearchparksNo ratings yet
- Insurance Bar Questions and Suggested Answers 1. Question A. 6 (2019 Bar)Document7 pagesInsurance Bar Questions and Suggested Answers 1. Question A. 6 (2019 Bar)Brandon CrisostomoNo ratings yet
- Climate Action Incentive Payment Notice 2022 06 25 09 46 45 07823 PDFDocument3 pagesClimate Action Incentive Payment Notice 2022 06 25 09 46 45 07823 PDFalex mac dougallNo ratings yet
- Effects of Experimental Parameters On NF3 Decomposition Fraction in An Oxygen-Based 2004Document7 pagesEffects of Experimental Parameters On NF3 Decomposition Fraction in An Oxygen-Based 2004Регина ШаяхметоваNo ratings yet
- Skripsi Alvi AkmaliaDocument94 pagesSkripsi Alvi Akmaliakhoiriah nasutionNo ratings yet
- Crankcase Blowby, Measure PDF FORMATDocument51 pagesCrankcase Blowby, Measure PDF FORMATDARISON VINCENT100% (2)
- Drying Bed Design PDFDocument29 pagesDrying Bed Design PDFAshokNo ratings yet
- Plant Tissue Culture MediaDocument34 pagesPlant Tissue Culture MediavijendNo ratings yet
- 1 - Ne - b2 Sety Leksykalne U7iDocument1 page1 - Ne - b2 Sety Leksykalne U7iAneta WalejewskaNo ratings yet
- H. P. Lovecraft - PolarisDocument3 pagesH. P. Lovecraft - PolarisBárbara AlvesNo ratings yet
- QUARTER 1 MELC 1 Volcanoes, Earthquakes and Mountain RangesDocument15 pagesQUARTER 1 MELC 1 Volcanoes, Earthquakes and Mountain RangesHikøriNo ratings yet
- Env LawDocument16 pagesEnv LawHeena ShaikhNo ratings yet
- Technical Specification 1 No: Unit QtyDocument3 pagesTechnical Specification 1 No: Unit QtySuraj KhopeNo ratings yet
- Product Risk Assessment Practices Regulatory AgenciesDocument19 pagesProduct Risk Assessment Practices Regulatory AgenciesAllyssa FernandezNo ratings yet
- Unit 18.7 Identifying Dental InstrumentsDocument69 pagesUnit 18.7 Identifying Dental InstrumentsIndrani Das100% (2)
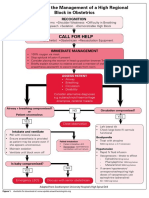
- Algorithm For The Management of A High Regional Block in ObstetricsDocument5 pagesAlgorithm For The Management of A High Regional Block in ObstetricsRaditya DidotNo ratings yet
- Olive Booklet PDFDocument83 pagesOlive Booklet PDFkareem3456No ratings yet
- Updated Manual02Document254 pagesUpdated Manual02claytoncash100% (2)
- 57-Online Rejection Note, Material ReturnDocument3 pages57-Online Rejection Note, Material Returnananth100% (1)