Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
37 viewsB12 Deficiency
B12 Deficiency
Uploaded by
Karrar A. AlShammaryThis patient presented with paresthesia, weight loss, jaundice, and anemia. On examination, he appeared pale and jaundiced with decreased sensation in his hands and feet. Differential diagnoses included conditions affecting the dorsal columns like vitamin deficiencies. Glossitis on exam suggested profound vitamin B12 deficiency, which can cause subacute combined degeneration of the spinal cord and anemia. Laboratory results confirmed vitamin B12 deficiency with macrocytic anemia and markers of hemolysis.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- TCAR ManualDocument193 pagesTCAR ManualJoe Reed (Game Master)No ratings yet
- ESRDDocument37 pagesESRDVecky TolentinoNo ratings yet
- EndocarditisDocument6 pagesEndocarditisMerry Joy DeliñaNo ratings yet
- Choose 2 From The Disease Below That Are Emerging in The PhilippinesDocument4 pagesChoose 2 From The Disease Below That Are Emerging in The PhilippinesMICHELLE BIANCA PATRICE CRUZNo ratings yet
- Severe AnemiaDocument62 pagesSevere AnemiaTracy Khate MNo ratings yet
- PracticeExam 3 AnsDocument52 pagesPracticeExam 3 AnsBehrouz YariNo ratings yet
- Ugib Case StudyDocument33 pagesUgib Case StudyRosemarie Cunanan Grifoni100% (1)
- Case Report - Complete Denture - 2Document4 pagesCase Report - Complete Denture - 2Astri Ggamjong Xiao LuNo ratings yet
- Prepared By: Dr. Abhishek Garg M.D Resident 3 Year Edited By: Dr. Arun Kumar SharmaDocument43 pagesPrepared By: Dr. Abhishek Garg M.D Resident 3 Year Edited By: Dr. Arun Kumar SharmaVijitha LenkalaNo ratings yet
- Case Histories 2019 - 113438Document12 pagesCase Histories 2019 - 113438mshuraifa1305No ratings yet
- All of Metabolism!!Document49 pagesAll of Metabolism!!KiaanNo ratings yet
- CasesDocument37 pagesCasesZakaria FarahNo ratings yet
- Hepatic Encephalopathy and ComaDocument4 pagesHepatic Encephalopathy and ComaAriana ValenciaNo ratings yet
- A) Importance of The Case StudyDocument73 pagesA) Importance of The Case StudyRaidis PangilinanNo ratings yet
- Week 4 Case 4 Internal MedicineDocument2 pagesWeek 4 Case 4 Internal MedicineINFO MANTICORE DUMMYNo ratings yet
- CA Pancreas BasirDocument9 pagesCA Pancreas BasirwhosenahNo ratings yet
- Acute Liver FailureDocument69 pagesAcute Liver FailureAsif.N.IqbalNo ratings yet
- Case Liver CirrhosisDocument73 pagesCase Liver CirrhosisJesus Orita-Delima100% (1)
- The Patient With Rhabdomyolysis: Have You Considered Quail Poisoning?Document2 pagesThe Patient With Rhabdomyolysis: Have You Considered Quail Poisoning?andriopaNo ratings yet
- Hyperthyroidism in Sickle Cell AnaemiaDocument6 pagesHyperthyroidism in Sickle Cell AnaemiaKIU PUBLICATION AND EXTENSIONNo ratings yet
- New ChartsDocument28 pagesNew Chartsgaxet79239No ratings yet
- C. Liver Function Test (Child Pugh Criteria-To See Albumin and Bilirubin)Document26 pagesC. Liver Function Test (Child Pugh Criteria-To See Albumin and Bilirubin)Nadhirah ZulkifliNo ratings yet
- Acute Renal FailureDocument76 pagesAcute Renal Failureikemas100% (7)
- Islamic University in Uganda: Name: Abdiqani Omar NoorDocument11 pagesIslamic University in Uganda: Name: Abdiqani Omar NoorUsaid SulaimanNo ratings yet
- Hepatic Encephalopathy and ComaDocument19 pagesHepatic Encephalopathy and ComaJas Castro JoveroNo ratings yet
- Spring 2004-05 Final MB Part IIDocument14 pagesSpring 2004-05 Final MB Part IIBen JonesNo ratings yet
- AnasarcaDocument54 pagesAnasarcaSulaiman TahsinNo ratings yet
- Medical Surgical Nursing - NeuroDocument19 pagesMedical Surgical Nursing - NeuroChristian EstevesNo ratings yet
- Hyper Kale Mia Case ReviewDocument4 pagesHyper Kale Mia Case ReviewSamina AhmadNo ratings yet
- Emergency CasesDocument11 pagesEmergency CaseszanoahzaveennaNo ratings yet
- A Case Study Presentation On: Chronic Kidney DiseaseDocument63 pagesA Case Study Presentation On: Chronic Kidney DiseaseFayeann Vedor LoriegaNo ratings yet
- Acute Renal FailureDocument5 pagesAcute Renal FailureJean De Vera MelendezNo ratings yet
- Nephrology QuestionsDocument8 pagesNephrology QuestionskaNo ratings yet
- Speciality: General Medicine Case: Nephrotic Syndrome HistoryDocument49 pagesSpeciality: General Medicine Case: Nephrotic Syndrome Historydrtpk100% (2)
- Acute Renal FailureDocument76 pagesAcute Renal FailureriyaNo ratings yet
- Nursing Care Plan Renal FailureDocument11 pagesNursing Care Plan Renal Failurenosevad88850% (2)
- 6 - Inborn Errors of Metabolism - Spring 23Document42 pages6 - Inborn Errors of Metabolism - Spring 23Abdo HaiderNo ratings yet
- CABRAL Diabetes Mellitus Case Presentation and DiscussionDocument9 pagesCABRAL Diabetes Mellitus Case Presentation and DiscussionCalingalan Hussin CaluangNo ratings yet
- Acute Quadriplegia: An Exercise in Differential Diagnosis: DR - RamDocument10 pagesAcute Quadriplegia: An Exercise in Differential Diagnosis: DR - Ramram49No ratings yet
- Neuropathy After Malnutrition Is Copper Deficiency The Missed Diagnosis E. Dowling 9.16.2014Document3 pagesNeuropathy After Malnutrition Is Copper Deficiency The Missed Diagnosis E. Dowling 9.16.2014xzx xNo ratings yet
- Lascano, Joanne Alyssa - RheumatologyDocument13 pagesLascano, Joanne Alyssa - RheumatologyJoanne Alyssa Hernandez LascanoNo ratings yet
- Topic 9 Ankit Int MedDocument4 pagesTopic 9 Ankit Int MedAnkit Kumar PatelNo ratings yet
- Diabetes Mellitus Complte LONG 2Document56 pagesDiabetes Mellitus Complte LONG 2John Vincent Dy OcampoNo ratings yet
- Case PresentationDocument41 pagesCase PresentationAhmad NawazNo ratings yet
- Anemia JournalDocument8 pagesAnemia JournalAmreen KausarNo ratings yet
- CAD - Tania Guzmán - 5toa URSEDocument14 pagesCAD - Tania Guzmán - 5toa URSEGuzZantyNo ratings yet
- Infectious Disease ReviewDocument12 pagesInfectious Disease ReviewjyothiNo ratings yet
- Acute GlumerulonephritisDocument77 pagesAcute GlumerulonephritisNicoleNo ratings yet
- Practice Exam 3Document93 pagesPractice Exam 3Arash SamieiNo ratings yet
- Coma-Causes, Diagnosis, Treatment and ManagementDocument19 pagesComa-Causes, Diagnosis, Treatment and ManagementHabtamu AdimasuNo ratings yet
- Emergency Medicine Block Seventh Problem: Group 15 Friday, November 3 2017Document94 pagesEmergency Medicine Block Seventh Problem: Group 15 Friday, November 3 2017Stefanie BlueNo ratings yet
- Nephrology by Prof NegoDocument9 pagesNephrology by Prof NegoAbedinego MalukaNo ratings yet
- PBL6Document111 pagesPBL6Sofea IzyanNo ratings yet
- Lopez, Lovelle Nmd-ClerkDocument11 pagesLopez, Lovelle Nmd-ClerkLovelle LopezNo ratings yet
- Chronic Splenic Torsion AdhesionsDocument5 pagesChronic Splenic Torsion AdhesionsDaniel CapuchoNo ratings yet
- Static OmarDocument61 pagesStatic OmarDh CndnNo ratings yet
- Asculitis Syndromes: Emily B. Martin, MD Rheumatology Board Review April 9, 2008Document54 pagesAsculitis Syndromes: Emily B. Martin, MD Rheumatology Board Review April 9, 2008Miguel M. Melchor RodríguezNo ratings yet
- Case Study PaperDocument14 pagesCase Study PaperClarisse AcacioNo ratings yet
- Guillain Barre Syndrome A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandGuillain Barre Syndrome A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The Slim Book of Health Pearls: Symptoms Never to IgnoreFrom EverandThe Slim Book of Health Pearls: Symptoms Never to IgnoreNo ratings yet
- The Reye Syndrome Sourcebook: A Concise Guide for Parents and PatientsFrom EverandThe Reye Syndrome Sourcebook: A Concise Guide for Parents and PatientsNo ratings yet
- Hepatic Encephalopathy: Causes, Tests, and Treatment OptionsFrom EverandHepatic Encephalopathy: Causes, Tests, and Treatment OptionsRating: 3.5 out of 5 stars3.5/5 (2)
- Ahmed Et Al IAA Journal of Biological Sciences 8 (1) :228-238,2022. ISSN: 2636-7254 ©iaajournalsDocument11 pagesAhmed Et Al IAA Journal of Biological Sciences 8 (1) :228-238,2022. ISSN: 2636-7254 ©iaajournalsKIU PUBLICATION AND EXTENSIONNo ratings yet
- KF - 07 - Blood Grouping 2019 - 03 - enDocument4 pagesKF - 07 - Blood Grouping 2019 - 03 - enSurta DevianaNo ratings yet
- Caffeine Literature Review-2Document6 pagesCaffeine Literature Review-2api-609577576100% (1)
- Newborn ScreeningDocument12 pagesNewborn ScreeningalreeveNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaPutri Ayu Helni LestariNo ratings yet
- Article Review ContohDocument15 pagesArticle Review ContohRadhi ShukriNo ratings yet
- Lamotrigine and Other Antiepileptics On Sleep Architecture - No Effect PDFDocument5 pagesLamotrigine and Other Antiepileptics On Sleep Architecture - No Effect PDFNones NoneachNo ratings yet
- Sdo PM QF Sgod SHN 001 Students Health Card ElementaryDocument3 pagesSdo PM QF Sgod SHN 001 Students Health Card ElementaryShiela E. EladNo ratings yet
- Clinical Utility of Multiphasic Questionnaire MPQ - 39 42Document5 pagesClinical Utility of Multiphasic Questionnaire MPQ - 39 42DN100% (1)
- Diseases of The Thyroid Gland PDFDocument72 pagesDiseases of The Thyroid Gland PDFKay BristolNo ratings yet
- Git BleedingDocument28 pagesGit Bleedingsembakarani thevagumaranNo ratings yet
- Benzodiazepines and Hypnotics: Key PointsDocument4 pagesBenzodiazepines and Hypnotics: Key Pointssaman mousaviNo ratings yet
- Invention of Insulin: Andreea 2016130148Document1 pageInvention of Insulin: Andreea 2016130148Eny KimNo ratings yet
- Cell BlockDocument25 pagesCell BlockD BNo ratings yet
- Cho Weekly Work PlanDocument1 pageCho Weekly Work PlanDayaram SikarwarNo ratings yet
- Science 9 - Q1 - Mod2 - Effects of Lifestyle in The Function of Respiratory and Circulatory System - VerFinalDocument34 pagesScience 9 - Q1 - Mod2 - Effects of Lifestyle in The Function of Respiratory and Circulatory System - VerFinalJames Dharell Trinidad100% (2)
- Resume Esmaeil ImaniDocument2 pagesResume Esmaeil ImaniSepideh MirzaeiNo ratings yet
- Personal Fitness Webquest Update 10-12-07Document16 pagesPersonal Fitness Webquest Update 10-12-07Information Point KapurthalaNo ratings yet
- Science of HeartbreakDocument6 pagesScience of HeartbreakPrashanth JanakiramNo ratings yet
- Koding DR IndraDocument196 pagesKoding DR Indrasuciayu33No ratings yet
- Sam BongDocument4 pagesSam BongAngelique GANo ratings yet
- Chapter 40: Gastrointestinal Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument6 pagesChapter 40: Gastrointestinal Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Ebola Virus Disease: Key FactsDocument5 pagesEbola Virus Disease: Key Facts黄銮添No ratings yet
- Knowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhanaDocument10 pagesKnowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhananicloverNo ratings yet
- Systemic Lupus ErythematosusDocument40 pagesSystemic Lupus ErythematosusAkshan SentinelNo ratings yet
- Normal Ranges Vital Signs 2017Document2 pagesNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- Tetracycline Sand Chlo Ramp He NicolDocument29 pagesTetracycline Sand Chlo Ramp He NicolArun DavesarNo ratings yet
B12 Deficiency
B12 Deficiency
Uploaded by
Karrar A. AlShammary0 ratings0% found this document useful (0 votes)
37 views33 pagesThis patient presented with paresthesia, weight loss, jaundice, and anemia. On examination, he appeared pale and jaundiced with decreased sensation in his hands and feet. Differential diagnoses included conditions affecting the dorsal columns like vitamin deficiencies. Glossitis on exam suggested profound vitamin B12 deficiency, which can cause subacute combined degeneration of the spinal cord and anemia. Laboratory results confirmed vitamin B12 deficiency with macrocytic anemia and markers of hemolysis.
Original Description:
Original Title
B12 Deficiency(1)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis patient presented with paresthesia, weight loss, jaundice, and anemia. On examination, he appeared pale and jaundiced with decreased sensation in his hands and feet. Differential diagnoses included conditions affecting the dorsal columns like vitamin deficiencies. Glossitis on exam suggested profound vitamin B12 deficiency, which can cause subacute combined degeneration of the spinal cord and anemia. Laboratory results confirmed vitamin B12 deficiency with macrocytic anemia and markers of hemolysis.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
37 views33 pagesB12 Deficiency
B12 Deficiency
Uploaded by
Karrar A. AlShammaryThis patient presented with paresthesia, weight loss, jaundice, and anemia. On examination, he appeared pale and jaundiced with decreased sensation in his hands and feet. Differential diagnoses included conditions affecting the dorsal columns like vitamin deficiencies. Glossitis on exam suggested profound vitamin B12 deficiency, which can cause subacute combined degeneration of the spinal cord and anemia. Laboratory results confirmed vitamin B12 deficiency with macrocytic anemia and markers of hemolysis.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 33
CASE RECORDS OF THE MASSACHUSETTS GENERAL
HOSPITAL
A 62-Year-Old Man with
Paresthesia, Weight Loss,
Jaundice, and Anemia
Presentation of Case
• 2 months before admission, when numbness, tingling, and
burning in his hands developed;
• symptoms intermittently radiated proximally to the mid-forearm.
• Pain, stiffness, and weakness of the hands occurred; he noted
decreased dexterity of his hands, without swelling, and he began
to drop objects.
• He took ibuprofen, with minimal symptomatic improvement. His
appetite decreased, and an unintentional weight loss of more than
6.5 kg occurred.
• 6 weeks before admission, the family noted that his eyes and skin (most
noticeably his palms) gradually became pale and yellowed.
• 2 weeks before admission, extreme fatigue, shortness of breath, and
weakness with exertion developed, and episodes of abdominal pain occurred
in the lower quadrants.
• Stiffness in his axillae developed, and it migrated to his shoulders and
abdomen.
• One week before admission, his wife noted a change in his gait, and he
appeared unsteady. He was unable to climb four stairs without resting and
was unsteady on standing, with resolution after ambulating.
• 2 nights before admission, dyspnea, weakness, and diaphoresis developed.
During the day, pressure radiated up his arms; this was associated with
diffuse abdominal pain that intermittently radiated to the axillae, and dark
urine developed.
• On the day of admission, he rated the pain in his joints at 7 on a scale
of 0 to 10. At that time, he came to the emergency department at this
hospital.
• The patient reported increased respiratory secretions, with a cough of 2
weeks' duration that was productive of white or yellow sputum, without
hemoptysis, fever, headache, nausea, vomiting, hematochezia, melena,
diarrhea, other changes in bowel function, or symptoms in his legs or
feet. He had hypertension and benign prostatic hypertrophy.
• The patient had been well on routine examination 4 months before admission.
• Medications included lisinopril (daily), ibuprofen and acetaminophen as needed for
discomfort; he had no known allergies.
• He lived with his wife and was retired, after working in the food industry and in
manufacturing, and he was previously very physically active.
• He ate chicken, fish, and vegetables regularly and ate red meat rarely.
• He stopped smoking (after 40 pack-years) and drinking alcohol 26 years before
admission, and he had not used illicit drugs.
• Four years before admission, he had visited his family in Greece. He also had gone
fishing and deer hunting in New England.
• His father was well, and his mother was bedridden; both were in their 90s. A sister
had died of breast cancer, and two brothers had died of lung cancer; his children
were healthy.
On examination..
• the patient appeared pale. Temp. 37.5°C, BP 136/63, pulse 113 /min, RR 20
/minute, O₂ saturation 99% while he was breathing ambient air.
• The tongue was swollen and smooth, the conjunctivae were pale and icteric,
and the palate, subglossal mucosa, and skin were jaundiced.
• The abdomen was soft, with mild-to-moderate tenderness in the
epigastrium, without rebound, guarding, organomegaly, or masses.
• On neurologic examination, there was pronator drift bilaterally. Sensation
to light touch was decreased in the hands and feet; sensation to vibration and
temperature was decreased in both legs in a “stocking” pattern and was
normal in both arms.
• A Romberg test was positive; toe, heel, and heel-to-toe gaits were normal.
• Muscle strength, reflexes, and the remainder of the examination were
normal.
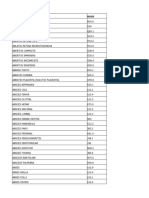
• The blood level of K⁺ was 3.2 mmol/l and globulin 2.1 g per deciliter
(reference range, 2.3 to 4.1).
• Blood levels of the other electrolytes, glucose, calcium, phosphorus,
magnesium, alkaline phosphatase, alanine aminotransferase, aspartate
aminotransferase, amylase, lipase, total protein, and albumin were normal,
as were tests of renal function; tests for creatine kinase isoenzymes and
troponin I were negative, and other test results are shown in Table 1. An
electrocardiogram was normal.
• A chest radiograph showed degenerative changes of the thoracic spine and
was otherwise normal. A stool specimen was negative for occult blood.
• One liter of crystalloid solution was administered intravenously, with
improvement in the tachycardia. Three hours after presentation, the patient
was admitted to this hospital; 2 units of red cells were transfused.
• Diagnostic test results were received.
Differential Diagnosis:
Paresthesia
• involve a sensation of tingling, numbness, crawling, or deadness,
and they are felt mainly in distal parts of the extremities.
• Although on rare occasions they can involve the thalamus,
paresthesia are mostly considered to originate from a spinal cord
disorder that probably results from ectopic discharge in damaged
dorsal-column axons and may be present before any other
abnormalities are detectable on neurologic examination.
Although there are many possible causes of paresthesias (Table 2),
most are not considerations in this case.
Ataxia
• A second salient neurologic feature in this case is the unsteady,
ataxic gait that developed insidiously over the course of this
patient's illness. Our patient felt unsteady on standing, had
difficulty climbing stairs, and seemed to improve with
ambulation.
• The differential diagnosis of ataxic gait is more concrete and
includes cerebellar, vestibular, and sensory causes. In this case,
there is no evidence of cerebellar dysfunction such as truncal
ataxia, wide gait, word scanning, apraxia, lack of coordination, or
dysmetria. There is also no evidence of vestibular dysfunction
such as dizziness, vertigo, nausea, or falls to one side.
• Sensory ataxia, which is characterized by decreased proprioception, is
often caused by a pathologic process affecting the dorsal columns or a
large-fiber polyneuropathy that may result in ataxic gait.
• In this patient, sensory ataxia affecting the dorsal columns was
manifested by a Romberg sign, decreased proprioception, and pronator
drift on examination.
• The patient feels unsteady because the brain is deprived of information
about the position of the feet and must rely on visual input and light to
see ground. This is why patients often have difficulty climbing stairs or
walking in the dark. Vision is able to compensate for the loss of
position sense to a great degree and thus minimizes sensory ataxia. If
the lesion affects the cervical cord, there is also upper-extremity ataxia.
• The list of possible causes of sensory ataxia is limited (Table 3). If
we combine the two features that we have selected — paresthesia
and sensory ataxic gait —
• The differential diagnosis would further narrow to those disorders
caused by dysfunction of the dorsal columns, including syphilis,
tickborne illnesses, human immunodeficiency virus (HIV)
infection, vitamin deficiencies (e.g., deficiencies of vitamin B12,
folate, and vitamin E), and systemic inflammatory conditions
(e.g., neoplasia, paraneoplastic syndromes, and autoimmune
diseases). Although they are less likely, multiple sclerosis and
amyloidosis should also be considered.
Anemia
• This patient presented with a hematocrit of 18.7%, which probably
explains his fatigue, shortness of breath, and pallor.
• His wife commented that he appeared pale and yellow, and these
findings were corroborated by the admitting physician's examination,
which confirmed that he was pale and jaundiced.
• Hemolysis is the likely mechanism to explain his anemia and jaundice.
If we consider causes of paresthesias, ataxia, and anemia—
• Our differential diagnosis narrows considerably to include infections
(tickborne disease and HIV), vitamin deficiencies (of vitamin B12 or
folate), and autoimmune, neoplastic, and paraneoplastic causes.
• We are not given a history of a recent tick exposure, making a tickborne illness
unlikely.
• Although we cannot rule out autoimmune or paraneoplastic phenomena with the
information we are given, one feature that perhaps makes our clinical approach
more discerning is the description of glossitis (swollen and smooth appearance of
the tongue) on physical examination.
• In addition to the other clinical features cited above, the presence of glossitis makes
it likely that this patient has a profound deficiency of vitamin B12 that is responsible
for the subacute degeneration of the dorsal columns of the spinal cord and
hemolysis. Indeed, we could easily make the diagnosis of vitamin B12 deficiency on
the basis of clinical information alone, since this patient presented with weakness
and fatigue, glossitis, and paresthesias — the classic triad of clinical findings
associated with vitamin B12 deficiency. In addition, other clinical findings were also
present, including anemia, clumsiness and unsteady gait, nonspecific
gastrointestinal symptoms, and weight loss, making the likelihood of this diagnosis
more certain.
• Although the clinical findings in this case strongly suggest a
profound vitamin B12 deficiency, the diagnosis needs to be
confirmed with an appropriate laboratory evaluation.
• The hemogram reveals profound anemia with a hemoglobin level
of 6.3 g per deciliter and a markedly elevated mean corpuscular
volume of 124 fl. In addition, we found that the patient also had
elevated levels of total bilirubin, most of which was unconjugated,
almost nonexistent serum haptoglobin levels, and a markedly
elevated serum level of lactate dehydrogenase; all these findings
strongly suggest the presence of a hemolytic process as the
probable cause of the severe anemia.
• When evaluating a patient with anemia, a quick look at three
basic hematologic studies — the red-cell indexes (mean
corpuscular volume, mean corpuscular hemoglobin, mean
corpuscular hemoglobin concentration, and red-cell distribution
width), the reticulocyte count, and the peripheral smear — is
likely to yield a manageable list of potential causes. Although we
are not shown the peripheral-blood smear, it was certainly done in
this case and should be considered a “biopsy” of the blood. It
allows us to visually analyze the hemogram in its entirety for
count, shape, and size of cells. Although far from perfect, when
analyzed together, the combination of these three studies has a
rather high initial diagnostic accuracy for anemia.
Red cell indexes
• Perhaps the most salient and discernible abnormality in this patient's red-cell
indexes is the markedly elevated mean corpuscular volume of 124 fl (normal
range, 80 to 100) in contrast to the reticulocyte count (0.8%), which is low for
the degree of anemia.
• The mean corpuscular volume gives the approximate size (volume) of a
population of red cells in a patient's blood. We can quickly ascertain by the
mean corpuscular volume of 124 fl that our patient has macrocytic anemia.
• On the basis of the pathogenesis, the different causes of macrocytic anemia
can be classified as arising from immature or stress cells (e.g., reticulocytosis,
aplasias, and Fanconi's anemia), abnormal DNA metabolism (e.g., vitamin
B12 and folate deficiency and drugs or toxins), abnormal lipid metabolism
(e.g., liver disease and hypothyroidism), a bone marrow disorder (e.g.,
myelodysplastic syndromes, leukemia, and congenital abnormalities), and an
unknown mechanism (e.g., alcoholism and plasma-cell dyscrasias).
• Although relatively short, this list is still too long to be of much help.
• Examination of the mean corpuscular hemoglobin, the mean corpuscular
hemoglobin concentration, and the red-cell distribution width can help us further
characterize our patient's anemia.
• The mean corpuscular hemoglobin describes the amount of hemoglobin per red
cell in a population of cells. This patient's mean corpuscular hemoglobin is 41.7 pg
(reference range, 26.0 to 34.0) and tells us that the patient, although anemic, has red
cells that contain more hemoglobin than expected; this argues against a
hemoglobinopathy as the cause of anemia.
• However, the mean corpuscular hemoglobin concentration is normal at 33.7 g
per deciliter (reference range, 31.0 to 37.0), indicating that the patient's erythrocytes,
although large and plentiful in hemoglobin content, are indeed normochromic.
• Furthermore, red cells can be described according to the relative frequency with
which varied shapes occur in a population of cells. The relative red-cell
distribution width, which in this patient is elevated at 21.8% (reference range, 11.5
to 14.5), suggests that a large proportion of the cells are of widely varied shapes and
sizes
• . On the basis of the red-cell indexes, we can conclude that this patient's
anemia is macrocytic and normochromic, with an elevated hemoglobin
content per red cell and a wide variety of shapes and sizes in the overall red-
cell population.
• How may these findings help us to further distinguish our patient's anemia
among the causes of macrocytosis?
• Returning to our list for mechanisms of macrocytosis, we can exclude the
presence of immature cells as a likely culprit, given that the reticulocyte
count in this patient's serum was normal. We can also discard disorders of
the bone marrow, heavy alcohol use, and plasma-cell dyscrasias as likely
causes, given that other cell lines, white cells, and platelets are intact. We are
left with abnormal DNA metabolism causing megaloblastic anemia or
abnormal lipid metabolism of the cell wall due to liver disease or
hypothyroidism as the possible etiologic mechanisms for macrocytosis in this
patient.
• The markedly elevated lactate dehydrogenase level, low haptoglobin level, and
unconjugated hyperbilirubinemia all point to a hemolytic process as a contributing
cause of anemia. Condensing all these variables into a unifying explanation for this
patient's anemia, we are left with megaloblastic anemia caused by vitamin B12 or
folate deficiency as the likely diagnosis.
• A hallmark of megaloblastic anemia is ineffective erythropoiesis due to defective
DNA and nuclear maturation and the consequent intramedullary destruction or
hemolysis of fragile and abnormal megaloblastic erythroid precursors. Such
ineffective erythropoiesis, if persistent and severe, may deplete iron stores, leading
to the coexistence of iron-deficiency anemia. This explains the absence of high
peripheral reticulocytosis in patients with profound vitamin B12 deficiency despite
avid red-cell destruction. In addition, overwhelming, ineffective erythropoiesis with
severe hemolysis may also result in depleted levels of serum potassium, which is
probably the case in this patient. The elevated red-cell distribution width is further
evidence of mixed anemic cell populations and may be explained by the coexistence
of vitamin B12 deficiency and iron-deficiency anemia.
Vitamin B12 deficiency
• In this case, the clinical signs and laboratory evaluation lead us to
the diagnosis of profound vitamin B12 deficiency. Given this
patient's age at the onset of illness, clinical presentation,
laboratory evaluation, and history of maintaining a normal diet,
the most likely cause of his vitamin B12 deficiency is pernicious
anemia. In the classic sense, pernicious anemia is caused by
inadequate production of intrinsic factor by parietal cells, thus
impeding the proper absorption of vitamin B12 in the ileum. It is
believed to be an autoimmune disease, with a high proportion of
patients having antibodies against parietal cells as well antibodies
against intrinsic factor as compared with healthy persons
• To make a firm diagnosis of pernicious anemia in this patient, I would
carefully examine the peripheral-blood smear and obtain vitamin B12 and red-
cell folate levels.
• To differentiate between vitamin B12 deficiency and folate deficiency, I would
obtain methylmalonic acid and homocysteine levels.
• The homocysteine level is elevated in both anemia due to vitamin
B12 deficiency and anemia due to folate deficiency.
• In contrast, the methylmalonic acid level is elevated only in vitamin
B12 deficiency and is normal in folate deficiency. Although it has fallen out of
favor, the Schilling test would reveal the cause of vitamin B12 deficiency, and
serologic testing for antibodies to intrinsic factor would point to pernicious
anemia as a cause. To complete the workup, it would be prudent to obtain
serum iron studies, given the high suspicion of concomitant iron deficiency.
• Finally, severe alcoholism can lead to a macrocytic anemia.
However, with alcoholism, one generally observes a mean
corpuscular volume between 100 and 110 fl.
• It would be extremely rare for alcoholism alone to cause a mean
corpuscular volume of 124 fl independent of any other symptoms.
Clinical diagnosis
• Vitamin B12 deficiency (pernicious anemia).
Pathological diagnosis
• Figure 1. Peripheral-Blood
Smear.A peripheral-blood
smear showed anisocytosis
with oval macrocytes
(arrowheads) and abundant
neutrophil hypersegmentation
(≥6 lobes; arrow). No
schistocytes or spherocytes
were present.
• Anemia studies were obtained.
• The level of vitamin B12 was very low at 61 pg per milliliter (45 pmol per liter) (>250 pg per
milliliter [>185 pmol per liter])
• the level of folate was normal at 17.2 ng per milliliter (38.9 nmol per liter) (3.1 to 17.5 ng per
milliliter [70.5 to 39.7 nmol per liter]).
• Iron studies revealed..
• a low serum iron level of 19 μg per deciliter (3 μmol per liter) (45 to 160 μg per deciliter [8 to
29 μmol per liter]),
• a slightly low total iron-binding capacity of 221 μg per deciliter (40 μmol per liter) (230 to
404 μg per deciliter [41 to 72 μmol per liter]),
• and an elevated ferritin level of 340 ng per milliliter (for men, 30 to 300).
• The calculated transferrin saturation (calculated as the level of iron divided by the total iron-
binding capacity) was 8.6%, suggestive of iron deficiency.
• It is well described that iron deficiency and elevated ferritin levels may develop in patients
with pernicious anemia.
• Since the initial laboratory evaluation was suggestive of pernicious anemia,
additional laboratory evidence for the diagnosis was sought. The presence of cellular
vitamin B12 deficiency was assessed by measurement of methylmalonic acid, the
metabolism of which requires vitamin B12 as a cofactor. The level of serum
methylmalonic acid was highly elevated at 19.78 nmol per liter (reference range,
<0.40), confirming the presence of cellular vitamin B12 deficiency.
• Classic findings associated with pernicious anemia include atrophic gastritis of the
body of the stomach (atrophic body gastritis) and intrinsic factor deficiency. A
highly elevated fasting gastrin level (504 pg per milliliter; reference range, <100) and
a reduced level of pepsinogen I (<24.6 ng per milliliter; reference range, 28 to 100)
were consistent with atrophic body gastritis. Since the Schilling test is now
unavailable at most centers, the detection of antibodies to intrinsic factor may be
used to support the diagnosis of pernicious anemia. In approximately 40 to 60% of
patients with pernicious anemia, positivity for anti–intrinsic factor antibodies is
present and provides evidence to support the diagnosis of pernicious anemia, with a
specificity approaching 100%. 12 Anti–intrinsic factor blocking antibodies were
measured, and the patient was found to be positive.
• Patients with pernicious anemia have an increased risk of gastric
carcinoma and carcinoid tumors.13 The patient underwent
endoscopy to evaluate the upper and lower gastrointestinal tract
to assess for a neoplastic condition and to rule out gastrointestinal
bleeding as a possible contributor to the patient's iron deficiency.
No evidence of gastric carcinoma or carcinoid was present (Figure
2A and 2B). The remainder of the endoscopic evaluation was
unremarkable.
• The role of H. pylori in the pathogenesis of pernicious anemia is
an area of active investigation.14 The patient was assessed for the
presence of H. pylori; both H. pylori IgG serologic tests and stool
antigen tests were negative.
• Figure 2. Endoscopic Evaluation and
Biopsy Specimen.Endoscopic
examination of the stomach revealed
diffuse atrophy of the gastric mucosa
(Panel A). A biopsy specimen from the
gastric body shows patchy foci of intestinal
metaplasia (arrows) and pseudopyloric
metaplasia (arrowheads) in the background
of chronic inactive gastritis, findings
consistent with autoimmune gastritis
(Panel B, hematoxylin and eosin). There is
no evidence of neuroendocrine
hyperplasia, carcinoid, or adenocarcinoma.
(Endoscopic image courtesy of Dr. Ashwin
Ananthakrishnan, Division of
Gastroenterology, Massachusetts General
Hospital.)
• In the emergency department, the patient received 2 units of
packed red cells. We consulted with the hematology service, and
an intramuscular vitamin B12 regimen as well as the
administration of intravenous iron were initiated. He had
improvement in his peripheral neuropathy, and the hematocrit on
discharge was 23%. Since discharge, he has received monthly
vitamin B12 injections. One year after discharge, the hematocrit is
44%, the vitamin B12 level 581 pg per milliliter, and the iron level
normal. He continues to have numbness and tingling in his hands
bilaterally, as well as some numbness in the distal part of his toes.
You might also like
- TCAR ManualDocument193 pagesTCAR ManualJoe Reed (Game Master)No ratings yet
- ESRDDocument37 pagesESRDVecky TolentinoNo ratings yet
- EndocarditisDocument6 pagesEndocarditisMerry Joy DeliñaNo ratings yet
- Choose 2 From The Disease Below That Are Emerging in The PhilippinesDocument4 pagesChoose 2 From The Disease Below That Are Emerging in The PhilippinesMICHELLE BIANCA PATRICE CRUZNo ratings yet
- Severe AnemiaDocument62 pagesSevere AnemiaTracy Khate MNo ratings yet
- PracticeExam 3 AnsDocument52 pagesPracticeExam 3 AnsBehrouz YariNo ratings yet
- Ugib Case StudyDocument33 pagesUgib Case StudyRosemarie Cunanan Grifoni100% (1)
- Case Report - Complete Denture - 2Document4 pagesCase Report - Complete Denture - 2Astri Ggamjong Xiao LuNo ratings yet
- Prepared By: Dr. Abhishek Garg M.D Resident 3 Year Edited By: Dr. Arun Kumar SharmaDocument43 pagesPrepared By: Dr. Abhishek Garg M.D Resident 3 Year Edited By: Dr. Arun Kumar SharmaVijitha LenkalaNo ratings yet
- Case Histories 2019 - 113438Document12 pagesCase Histories 2019 - 113438mshuraifa1305No ratings yet
- All of Metabolism!!Document49 pagesAll of Metabolism!!KiaanNo ratings yet
- CasesDocument37 pagesCasesZakaria FarahNo ratings yet
- Hepatic Encephalopathy and ComaDocument4 pagesHepatic Encephalopathy and ComaAriana ValenciaNo ratings yet
- A) Importance of The Case StudyDocument73 pagesA) Importance of The Case StudyRaidis PangilinanNo ratings yet
- Week 4 Case 4 Internal MedicineDocument2 pagesWeek 4 Case 4 Internal MedicineINFO MANTICORE DUMMYNo ratings yet
- CA Pancreas BasirDocument9 pagesCA Pancreas BasirwhosenahNo ratings yet
- Acute Liver FailureDocument69 pagesAcute Liver FailureAsif.N.IqbalNo ratings yet
- Case Liver CirrhosisDocument73 pagesCase Liver CirrhosisJesus Orita-Delima100% (1)
- The Patient With Rhabdomyolysis: Have You Considered Quail Poisoning?Document2 pagesThe Patient With Rhabdomyolysis: Have You Considered Quail Poisoning?andriopaNo ratings yet
- Hyperthyroidism in Sickle Cell AnaemiaDocument6 pagesHyperthyroidism in Sickle Cell AnaemiaKIU PUBLICATION AND EXTENSIONNo ratings yet
- New ChartsDocument28 pagesNew Chartsgaxet79239No ratings yet
- C. Liver Function Test (Child Pugh Criteria-To See Albumin and Bilirubin)Document26 pagesC. Liver Function Test (Child Pugh Criteria-To See Albumin and Bilirubin)Nadhirah ZulkifliNo ratings yet
- Acute Renal FailureDocument76 pagesAcute Renal Failureikemas100% (7)
- Islamic University in Uganda: Name: Abdiqani Omar NoorDocument11 pagesIslamic University in Uganda: Name: Abdiqani Omar NoorUsaid SulaimanNo ratings yet
- Hepatic Encephalopathy and ComaDocument19 pagesHepatic Encephalopathy and ComaJas Castro JoveroNo ratings yet
- Spring 2004-05 Final MB Part IIDocument14 pagesSpring 2004-05 Final MB Part IIBen JonesNo ratings yet
- AnasarcaDocument54 pagesAnasarcaSulaiman TahsinNo ratings yet
- Medical Surgical Nursing - NeuroDocument19 pagesMedical Surgical Nursing - NeuroChristian EstevesNo ratings yet
- Hyper Kale Mia Case ReviewDocument4 pagesHyper Kale Mia Case ReviewSamina AhmadNo ratings yet
- Emergency CasesDocument11 pagesEmergency CaseszanoahzaveennaNo ratings yet
- A Case Study Presentation On: Chronic Kidney DiseaseDocument63 pagesA Case Study Presentation On: Chronic Kidney DiseaseFayeann Vedor LoriegaNo ratings yet
- Acute Renal FailureDocument5 pagesAcute Renal FailureJean De Vera MelendezNo ratings yet
- Nephrology QuestionsDocument8 pagesNephrology QuestionskaNo ratings yet
- Speciality: General Medicine Case: Nephrotic Syndrome HistoryDocument49 pagesSpeciality: General Medicine Case: Nephrotic Syndrome Historydrtpk100% (2)
- Acute Renal FailureDocument76 pagesAcute Renal FailureriyaNo ratings yet
- Nursing Care Plan Renal FailureDocument11 pagesNursing Care Plan Renal Failurenosevad88850% (2)
- 6 - Inborn Errors of Metabolism - Spring 23Document42 pages6 - Inborn Errors of Metabolism - Spring 23Abdo HaiderNo ratings yet
- CABRAL Diabetes Mellitus Case Presentation and DiscussionDocument9 pagesCABRAL Diabetes Mellitus Case Presentation and DiscussionCalingalan Hussin CaluangNo ratings yet
- Acute Quadriplegia: An Exercise in Differential Diagnosis: DR - RamDocument10 pagesAcute Quadriplegia: An Exercise in Differential Diagnosis: DR - Ramram49No ratings yet
- Neuropathy After Malnutrition Is Copper Deficiency The Missed Diagnosis E. Dowling 9.16.2014Document3 pagesNeuropathy After Malnutrition Is Copper Deficiency The Missed Diagnosis E. Dowling 9.16.2014xzx xNo ratings yet
- Lascano, Joanne Alyssa - RheumatologyDocument13 pagesLascano, Joanne Alyssa - RheumatologyJoanne Alyssa Hernandez LascanoNo ratings yet
- Topic 9 Ankit Int MedDocument4 pagesTopic 9 Ankit Int MedAnkit Kumar PatelNo ratings yet
- Diabetes Mellitus Complte LONG 2Document56 pagesDiabetes Mellitus Complte LONG 2John Vincent Dy OcampoNo ratings yet
- Case PresentationDocument41 pagesCase PresentationAhmad NawazNo ratings yet
- Anemia JournalDocument8 pagesAnemia JournalAmreen KausarNo ratings yet
- CAD - Tania Guzmán - 5toa URSEDocument14 pagesCAD - Tania Guzmán - 5toa URSEGuzZantyNo ratings yet
- Infectious Disease ReviewDocument12 pagesInfectious Disease ReviewjyothiNo ratings yet
- Acute GlumerulonephritisDocument77 pagesAcute GlumerulonephritisNicoleNo ratings yet
- Practice Exam 3Document93 pagesPractice Exam 3Arash SamieiNo ratings yet
- Coma-Causes, Diagnosis, Treatment and ManagementDocument19 pagesComa-Causes, Diagnosis, Treatment and ManagementHabtamu AdimasuNo ratings yet
- Emergency Medicine Block Seventh Problem: Group 15 Friday, November 3 2017Document94 pagesEmergency Medicine Block Seventh Problem: Group 15 Friday, November 3 2017Stefanie BlueNo ratings yet
- Nephrology by Prof NegoDocument9 pagesNephrology by Prof NegoAbedinego MalukaNo ratings yet
- PBL6Document111 pagesPBL6Sofea IzyanNo ratings yet
- Lopez, Lovelle Nmd-ClerkDocument11 pagesLopez, Lovelle Nmd-ClerkLovelle LopezNo ratings yet
- Chronic Splenic Torsion AdhesionsDocument5 pagesChronic Splenic Torsion AdhesionsDaniel CapuchoNo ratings yet
- Static OmarDocument61 pagesStatic OmarDh CndnNo ratings yet
- Asculitis Syndromes: Emily B. Martin, MD Rheumatology Board Review April 9, 2008Document54 pagesAsculitis Syndromes: Emily B. Martin, MD Rheumatology Board Review April 9, 2008Miguel M. Melchor RodríguezNo ratings yet
- Case Study PaperDocument14 pagesCase Study PaperClarisse AcacioNo ratings yet
- Guillain Barre Syndrome A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandGuillain Barre Syndrome A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The Slim Book of Health Pearls: Symptoms Never to IgnoreFrom EverandThe Slim Book of Health Pearls: Symptoms Never to IgnoreNo ratings yet
- The Reye Syndrome Sourcebook: A Concise Guide for Parents and PatientsFrom EverandThe Reye Syndrome Sourcebook: A Concise Guide for Parents and PatientsNo ratings yet
- Hepatic Encephalopathy: Causes, Tests, and Treatment OptionsFrom EverandHepatic Encephalopathy: Causes, Tests, and Treatment OptionsRating: 3.5 out of 5 stars3.5/5 (2)
- Ahmed Et Al IAA Journal of Biological Sciences 8 (1) :228-238,2022. ISSN: 2636-7254 ©iaajournalsDocument11 pagesAhmed Et Al IAA Journal of Biological Sciences 8 (1) :228-238,2022. ISSN: 2636-7254 ©iaajournalsKIU PUBLICATION AND EXTENSIONNo ratings yet
- KF - 07 - Blood Grouping 2019 - 03 - enDocument4 pagesKF - 07 - Blood Grouping 2019 - 03 - enSurta DevianaNo ratings yet
- Caffeine Literature Review-2Document6 pagesCaffeine Literature Review-2api-609577576100% (1)
- Newborn ScreeningDocument12 pagesNewborn ScreeningalreeveNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaPutri Ayu Helni LestariNo ratings yet
- Article Review ContohDocument15 pagesArticle Review ContohRadhi ShukriNo ratings yet
- Lamotrigine and Other Antiepileptics On Sleep Architecture - No Effect PDFDocument5 pagesLamotrigine and Other Antiepileptics On Sleep Architecture - No Effect PDFNones NoneachNo ratings yet
- Sdo PM QF Sgod SHN 001 Students Health Card ElementaryDocument3 pagesSdo PM QF Sgod SHN 001 Students Health Card ElementaryShiela E. EladNo ratings yet
- Clinical Utility of Multiphasic Questionnaire MPQ - 39 42Document5 pagesClinical Utility of Multiphasic Questionnaire MPQ - 39 42DN100% (1)
- Diseases of The Thyroid Gland PDFDocument72 pagesDiseases of The Thyroid Gland PDFKay BristolNo ratings yet
- Git BleedingDocument28 pagesGit Bleedingsembakarani thevagumaranNo ratings yet
- Benzodiazepines and Hypnotics: Key PointsDocument4 pagesBenzodiazepines and Hypnotics: Key Pointssaman mousaviNo ratings yet
- Invention of Insulin: Andreea 2016130148Document1 pageInvention of Insulin: Andreea 2016130148Eny KimNo ratings yet
- Cell BlockDocument25 pagesCell BlockD BNo ratings yet
- Cho Weekly Work PlanDocument1 pageCho Weekly Work PlanDayaram SikarwarNo ratings yet
- Science 9 - Q1 - Mod2 - Effects of Lifestyle in The Function of Respiratory and Circulatory System - VerFinalDocument34 pagesScience 9 - Q1 - Mod2 - Effects of Lifestyle in The Function of Respiratory and Circulatory System - VerFinalJames Dharell Trinidad100% (2)
- Resume Esmaeil ImaniDocument2 pagesResume Esmaeil ImaniSepideh MirzaeiNo ratings yet
- Personal Fitness Webquest Update 10-12-07Document16 pagesPersonal Fitness Webquest Update 10-12-07Information Point KapurthalaNo ratings yet
- Science of HeartbreakDocument6 pagesScience of HeartbreakPrashanth JanakiramNo ratings yet
- Koding DR IndraDocument196 pagesKoding DR Indrasuciayu33No ratings yet
- Sam BongDocument4 pagesSam BongAngelique GANo ratings yet
- Chapter 40: Gastrointestinal Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument6 pagesChapter 40: Gastrointestinal Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Ebola Virus Disease: Key FactsDocument5 pagesEbola Virus Disease: Key Facts黄銮添No ratings yet
- Knowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhanaDocument10 pagesKnowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhananicloverNo ratings yet
- Systemic Lupus ErythematosusDocument40 pagesSystemic Lupus ErythematosusAkshan SentinelNo ratings yet
- Normal Ranges Vital Signs 2017Document2 pagesNormal Ranges Vital Signs 2017Elvis Nguyen100% (1)
- Tetracycline Sand Chlo Ramp He NicolDocument29 pagesTetracycline Sand Chlo Ramp He NicolArun DavesarNo ratings yet