Professional Documents
Culture Documents
Citrate Workbook V7.0 Aug 18 PDF
Citrate Workbook V7.0 Aug 18 PDF
Uploaded by
alexOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Citrate Workbook V7.0 Aug 18 PDF
Citrate Workbook V7.0 Aug 18 PDF
Uploaded by
alexCopyright:
Available Formats
Education Pack and Workbook for Citrate
Anticoagulation via Prismaflex
Name
Completion Date
Assessed by (Superuser)
Signature of Assessor
Citrate Workbook V7.0 Aug 2018 1
Contents
Introduction 3
CSIG Members 3
Part 1
Continuous Renal Replacement Therapy - Overview 4
Anticoagulation of the Circuit 5
Citrate Anticoagulation - Overview 5
Citrate Advantages vs Disadvantages 6
Setting up and priming circuit 7
Assessment – Part 1 9
Part 2
Starting CVVHDF using Citrate Anticoagulation 11
Treatment Monitoring 12
General Care of the RRT Patient 14
Troubleshooting Acid/Base disturbances 15
Assessment – Part 2 16
Frequently asked questions 18
Reading List & Useful Websites 20
Certificate 22
Citrate Workbook V7.0 Aug 2018 2
Introduction
This booklet is designed to enable you to update your knowledge regarding the care of patients
requiring Renal Replacement Therapy (RRT). It will help you gain the knowledge and skills to help you
achieve competency in Citrate anticoagulation therapy using the Prismaflex. It is yours to keep as a
resource and as a record of your learning.
The experience of staff using Citrate in other hospitals is overwhelmingly positive. It is best for patients
as they have fewer bleeding events and get more reliable RRT. Staff find that circuits last much longer
and there are fewer problems to troubleshoot.
You can work through the booklet at your own pace, using various resources. These include the Citrate
Special Interest Group (CSIG): this is a group of medical and nursing superusers in BCU who are happy to
be approached. The library contains useful reference books (see Further Reading), and the internet
contains a number of useful sites (See Useful Websites). The Gambro Prismaflex Manual is a good
resource, as is the Citrate Setup Guidelines attached to every machine.
In order to gain the necessary experience and skills to become competent in Citrate therapy using the
Prismaflex machine you are required to complete this workbook and have it assessed by a CSIG
Superuser.
CORE CSIG members:
Wrexham Maelor Hospital Glan Clwyd Hospital (YGC) Bangor Hospital (YG)
(WM)
1. Campbell Edmondson 1. John Glen 1. Alison Ingham
2. Graham Mayers 2. Richard Pugh 2. Janice Cadywould
4. Jennifer Smyth 3. Mark Williams-Jones 3. Pierre Peyrasse
5. Stewart Tasker 4. Phillip Rathbone 4. Sharon Evans
5. Uttam Chouhan
CSIG Superusers:
Wrexham Maelor Hospital (WM) Glan Clwyd Hospital (YGC) Bangor Hospital (YG)
Stewart Tasker Boyet Potunova Janice Cadywould
Louisa Erica Jon Pico Glenn Sanderson
Melissa Price Sion Thomas Louise Lloyd
Rachael Evans Jo White Ceri Twigge
Karen Austin Kerry Angus Nerys Elias
Kate Coleman Sharon Lynch Jaydee Castillo
Anwen Willams Shona Hollins-Davies Ferdinand Vitug
Clare Jones Garcia Marites
Linda Leech
Acknowledgements
We are grateful to the Intensive Care Staff at the Royal Marsden Hospital for allowing us to adapt their Citrate guidelines
and learning materials.
Citrate Workbook V7.0 Aug 2018 3
CITRATE - PART 1
Continuous Renal Replacement Therapy (CRRT) - Overview
This is a supportive therapy used in Critical Care patients who have developed an acute kidney injury (AKI). AKI is
characterized by a rapid deterioration in kidney function resulting in a failure to maintain fluid, electrolyte and acid-base
homoeostasis. There are a number of systems used to define and stage AKI, including RIFLE and KDIGO – for more
information on these visit the websites listed in the reading list. The end result, irrespective of which definition you use,
is a patient with gross biochemical abnormalities and (often) fluid overload. The aim of therapy is to normalize this
abnormal biochemistry as far as the technology will allow. This means:
• Relieving hypervolaemia and maintaining fluid balance.
• Removing excess urea and creatinine.
• Correcting and maintaining metabolic and electrolyte balance
This continuous technique was developed for critically ill patients with AKI who had previously been treated with
conventional dialysis. Those patients frequently became unstable during dialysis due to its short, intense nature. CRRT
by contrast allows fluid and waste products to be removed more gradually over a 24 hour period, which may give
greater cardiovascular stability. Of course this has been questioned, and many units run dialysis without a problem.
Technique
Using a double lumen Vascath and an extracorporeal circuit, blood is continuously removed from, and returned to, the
patient.
The circuit incorporates a blood pump and a filter containing a semi-permeable membrane. A pressure gradient within
the circuit forces fluid and solutes across the membrane to form filtrate (or effluent). In addition, dialysis fluid on the
other side of the membrane causes molecules to move across with their concentration gradient. The processes involved
here are termed:
• Ultrafiltration: Water forced across a semipermeable membrane by pressure.
• Convection: Also called ‘solvent drag’ – solutes moving along with the water because they are dissolved in it.
• Osmosis: Water moving across a semipermeable membrane with its concentration gradient.
• Diffusion. Solute moving across the membrane with its concentration gradient.
Fluid removed by ultrafiltration is replaced using replacement fluid – we use Prismasol 4, which has a similar electrolyte
composition to normal blood. Of course not all the fluid removed is replaced in this way: some of the patient’s fluid will
come from other sources like nutrition and drugs, and it may be desirable to remove fluid from the patient without
replacing it at all. The net fluid removal aim is set by medical staff on the morning/ evening ward round.
Citrate Workbook V7.0 Aug 2018 4
Anticoagulation of the circuit
Blood passes through the extracorporeal circuit, which has a colossal surface area. The large surface area leads to a
reduction in blood velocity which leads to platelets beginning to stick to the sides of the circuit. This in turn activates the
clotting cascade. Extra anticoagulation is therefore usually required to maintain the circuit and stop it from clotting off
altogether. The aim of any anticoagulation medication is to anticoagulate the circuit, not the patient.
There are three ways to anticoagulate CRRT circuits in BCU. The main method is (about to be!) regional Citrate, on which
this booklet concentrates. The other two methods are to use heparin (for example, when Citrate is contraindicated), and
to use Epoprostenol (when both citrate and heparin are contraindicated).
The anticoagulant being used will determine which Pre Blood Pump (PBP), Dialysis and Replacement Fluids to use. For
Heparin and Epoprostenol (Flolan) anticoagulation we can simply use Prismasol 4 on all three scales. Citrate is a bit more
complicated, and requires 3 different fluids, as well as a Calcium replacement syringe (see below).
Citrate Anticoagulation - Overview
Citrate binds ionized calcium in the extracorporeal circuit, which prevents the formation of blood clots.
This has no effect on the patient’s systemic coagulation, which means that it is safe to use on patients with bleeding
risks, (such as recent surgery or traumatic brain injury) and it is also safe to use in patients with Heparin-Induced
Thrombocytopenia (HIT).
The majority of citrate is cleared by dialysis as complexed calcium citrate. This means that the patient loses some of their
calcium. Calcium must therefore be given back to the patient at the end of the circuit, or they will become
hypocalcaemic. This is done via a 50mLs syringe attached to the Prismaflex machine. The rate of calcium given to the
patient is calculated by the Prismaflex machine, based on the rate of citrate administration and the flow of effluent.
The remaining citrate which returns to the patient is metabolised by the liver, skeletal muscle and kidney into
bicarbonate.
Because we don’t want the calcium to be present in the circuit, we have to use Calcium-free Dialysate (Prism0cal B22).
The Citrate itself is given in the Pre-Blood Pump (Prismocitrate 18/0).
We can give the usual Replacement (Prismasol 4).
Citrate Workbook V7.0 Aug 2018 5
Citrate – Advantages/Disadvantages
Advantages
• Safe to use on patients with active bleeding, recent bleeding or who are at risk of bleeding, e.g. recent surgery.
• Safe to use with patients at risk of Heparin Induced Thrombocytopenia (HIT).
• Citrate acts as a buffer, being metabolized into 3 molecules of bicarbonate. This may be beneficial in cases of
severe metabolic acidosis.
Disadvantages
• In patients with SEVERE liver disease, citrate metabolism may be inadequate, resulting in citrate accumulation,
metabolic acidosis and hypocalcaemia.
• Close monitoring of Calcium, pH, HCO3 and electrolytes is required.
• Citrate intolerance in a small number of patients.
Equipment needed
• 1 Prismaflex Filter ST150.
• 1 bag of 5L PrismoCitrate 18/0 (Citrate used as pre-dilution).
• 1 bag of 5L Prism0cal B22 (Dialysate, calcium-free).
• 1 bag or 5L Prismasol 4 (post-dilution replacement fluid).
• 2 bags of 0.9% 1000mLs Sodium Chloride (priming solution - No Heparin required).
• 1 CA250 calcium line.
• 1 50mL Luer lock syringe.
• 30mmol calcium (as calcium chloride) made up to 50ml with 0.9% Saline
Citrate Workbook V7.0 Aug 2018 6
Setting up and priming circuit
1. Select New Patient.
2. Input actual body weight.
3. Input haematocrit. This is found on the full blood count. Unlike in treatment with heparin, haematocrit is important.
Update the haematocrit every morning.
4. Choose CVVHDF.
5. Choose Citrate Anticoagulation via Prismaflex Pump.
6. Follow the installation steps on the screen:
• Install PrismoCitrate 18/0 on the white scale (PBP = pre blood pump).
• Install Prism0cal B22 on the green scale. (Dialysate).
• Install Prismasol 4 on the purple scale (Replacement).
7. Install the calcium chloride in the Prismaflex integral syringe pump.
8. Prime the circuit with 2 X 1L of 0.9% Sodium Chloride. Each 1L has 5000units heparin. (as per on screen instructions)
Notes on the above:
a. Circuit Installation
Throughout this process a series of Bullet Points appear on the left hand side of the screen; these are useful to press as
they highlight exactly which parts of the machine or circuit need to be looked at next. They will help you to correctly
install both the circuit and the syringe.
Citrate Workbook V7.0 Aug 2018 7
Setting up and priming circuit - continued
b. Priming the circuit
Circuits must be primed with 2 litres 0.9% Sodium Chloride to flush out the ethylene oxide used in the sterilizing process.
Once primed the circuit must be used within 30 minutes otherwise you need to do it again.
Each litre of Sodium Chloride should have 5000units Heparin if there are no contraindications to this drug.
c. Calcium Replacement
A 50mLs BD Plastipak syringe with 30mmol calcium (as calcium chloride) made up to 50mLs with 0.9% sodium chloride
(final concentration 0.6mmol/L) is inserted into the Prismaflex syringe driver before you start the prime (see Install
Calcium Syringe screen).
The Calcium syringe is connected to Calcium line and a Y connector in order to administer Calcium to the patient via the
return port of the Vascath. You need to attach these before the prime begins. The shorter line in the filter set (used for
other methods of anticoagulant) should be clamped.
d. Getting ready to start
Once the set has been primed it will ask you to check the circuit and then Prime Test. Once the prime test has been
completed, go no further. Now is the time to check the adequacy of the Access and Return ports of the Vascath.
▪ Withdraw 5mLs blood from each port and discard.
▪ Connect a 10mLs syringe to the Access port, draw back until full over 3 seconds: this will confirm patency of the
port.
▪ Repeat on the Return line.
If resistance is felt, line reposition may be required. The 10mLs of blood can be immediately returned before finally
flushing both ports with 5mLs Saline. Do not proceed with therapy in presence of poor access pressures, it is sure to
fail.
NB: avoid swapping lines unless absolutely necessary. If lines are swapped, ensure the lines are clearly labelled, and
the reason for the change is documented.
Citrate Workbook V7.0 Aug 2018 8
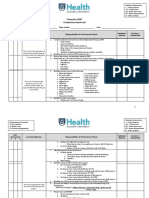
Part 1 Assessment
Using this booklet and any other resource you choose, complete the following questions.
Assessment Question 1
On the setup screen, what would you select for Regional Citrate?
Heparin via the Prismaflex syringe driver.
Anticoagulation via external syringe driver.
Citrate via Prismaflex pump.
Citrate via external syringe.
Assessment Question 2
List the disposable equipment required to administer CVVHDF using Citrate. (not including fluids or calcium) (3 items)
……………………………………………………………………………………………………………………….…………………………………………
Assessment Question 3
What must the bedside nurse regularly monitor in order to ensure appropriate citrate dosing (2 items)?
…………………………………………………………………………………………………………………………………………………………………
Assessment Question 4
What do you do if, during setup, you encounter resistance in the flow of the Vascath?
…………………………………………………………………………………………………………………………………………………………………
Assessment Question 5: tick the correct answer from below.
In Citrate anticoagulation, Calcium Chloride is adminstered: (1 point)
Directly to the patient?
Directly into the filter?
Via the PBP scale?
Assessment Question 6: tick the correct answer from below.
Citrate is Administered:
As a Dialysate?
Directly to the patient?
Via the PBP scale?
Assessment Question 7: tick the correct answer from below.
What is a potential side effect of citrate anticoagulation?
Hyperphosphataemia
Hypocalcaemia
Hypercoagulability
Citrate Workbook V7.0 Aug 2018 9
Assessment Question 8:
Haemodialysis, haemofiltration and haemodiafiltration are terms used to describe the removal of waste products and
water from the blood through a semipermeable membrane or filter. This is achieved through certain physiological
principles.
Briefly describe each of the physiological principles listed.
Osmosis
Diffusion
Ultrafiltration
Convection
Assessment Question 9:
Fill in the blanks below:
Mechanism Advantages Disadvantages
Citrate Binds Calcium
Heparin
Epoprostenol
Assessment Question 10: tick the correct answer from below.
Citrate PBP Fluid (Prismocitrate 18/0) Contains:
Citrate, Calcium, and Potassium.
Citrate, Sodium and Potassium.
Citrate and Sodium only.
Assessment Question 11: tick the correct answer from below.
Dialysis Fluid (Prism0Cal B22) Contains:
Calcium, Glucose and HCO₃ (22mmol/L)
Potassium 4mmol/L, Glucose and HCO₃ (22mmol/L)
Glucose, HCO₃ (22mmol/L), and Phosphate
Assessment Question 12: tick the correct answer from below.
Replacement Fluid (Prismasol 4) Contains:
Potassium, Calcium, HCO₃ (32mmol/L)
Potassium 4mmol/L, Phosphate 1.2mmol/L and HCO₃ 30mmol/L
No Potassium, no HCO₃, no Lactate
Citrate Workbook V7.0 Aug 2018 10
CITRATE - PART 2
Starting CVVHDF Using Citrate Anticoagulation.
Citrate (Prismocitrate 18/0) is administered pre-filter (White scale - PBP) so that the chelating process begins before the
blood has a chance to clot. The initial Citrate dose is always 3mmol/L. (If this is not the first circuit for this patient, then
restart with the previous Citrate dose and Calcium Replacement rates from when the treatment last finished.)
Setting the Flow rates:
For Citrate a slower blood pump speed is usually adequate (between 100 to 180mLs/hr). This is much slower than you
will be used to with heparin or epoprostenol. Follow the instructions below.
MODE: CVVHDF
FLUID REMOVAL: as advised by doctor
CITRATE DOSE: 3 mmol/L.
CALCIUM COMPENSATION: Depends on initial PATIENT IONISED CALCIUM level – see table 1 below.
Patient Ionised Calcium Starting Calcium Compensation (%)
Less than 1mmol/L 110%
AND
give 10mls calcium chloride 10% over 30 mins before starting
1 - 1.11 mmol/L 110%
1.12 – 1.3 mmol/L 100%
Greater than 1.3mmol/L 90%
Table 1: Initial Calcium Compensation
INITIAL FLOW SETTINGS: Based on Weight. See table 2 below.
INITIAL SETTINGS WITH CITRATE DOSE of 3 mmols/L blood
Weight
Replacement Actual Renal
(Actual in Kg) Blood Flow Dialysis rate
(post filter) rate Replacement
(Round up to mLs/min mLs/hr
mLs/hr Dose
nearest whole kg)
Up to 50 100 1000 200 37 mLs/kg/hr
51 to 60 110 1100 400 37 mLs/kg/hr
61 to 70 120 1200 500 35 mLs/kg/hr
71 to 80 130 1300 500 33 mLs/kg/hr
81 to 90 140 1400 500 31 mLs/kg/hr
91 to 100 150 1500 600 31 mLs/kg/hr
101 to 110 160 1600 700 30 mLs/kg/hr
111 to 120 170 1700 800 30 mLs/kg/hr
121 and up 180 1800 1000 30 mLs/kg/hr
Table 2: Initial Flow Settings
Citrate Workbook V7.0 Aug 2018 11
Treatment Monitoring
Low PATIENT IONISED CALCIUM values should ALWAYS be attended to as a priority as it will
have the biggest impact on patient physiology and stability.
If at any time during treatment the patient’s ionised calcium is less than 0.7 mmol/L,
administer 10mL calcium chloride 10% through peripheral or central line.
The PATIENT IONISED CALCIUM from the patient’s arterial line* is used to ensure that enough calcium chloride is being
given to the patient to replace the calcium used up in the reaction with the citrate.
A PATIENT IONISED CALCIUM of >1 is required TO KEEP THE PATIENT SAFE from the effects of hypocalcaemia.
The calcium replacement, initially estimated by the Prismaflex machine, may need to be changed based on these results.
The FILTER IONISED CALCIUM (from the blue port on the Prismaflex [i.e. post filter]) is checked on the blood gas
machine to ensure that enough calcium is being removed by the citrate infusion via the pre-blood pump.
A FILTER IONISED CALCIUM concentration of 0.25-0.5 mmol/L is required TO PREVENT FILTER CLOTTING.
The citrate dose, initially based on patient weight, may need to be changed based on these results.
So, once treatment is initiated and blood flow established, wait 60 minutes then check the:
PATIENT IONISED CALCIUM from the patient’s arterial line*.
FILTER IONISED CALCIUM (from blue port on Prismaflex).
The table below gives the timings of the FILTER IONISED CALCIUM and PATIENT IONISED CALCIUM checks
(as well as other blood tests which will be needed).
Parameter Initial check And then
FILTER IONISED CALCIUM – ABG from blue port on circuit Hourly until
Target 0.25 to 0.50 mmol/L 6 Hourly
stable**
PATIENT IONISED CALCIUM – ABG from arterial line*
Hourly until
Target 1.00 to 1.30 mmol/L 6 Hourly
stable**
TOTAL CALCIUM (corrected) – yellow tube sent to lab
Target 2.20 to 2.50 mmol/L After 6 hours Daily
TOTAL CALCIUM (corrected) to PATIENT IONISED CALCIUM ratio
Target ratio <2.5 After 6 hours Daily
U&E 6 hourly 12 hourly when stable
FBC/haematocrit Daily Daily
Magnesium/phosphate Daily Daily
Glucose As per protocol As per protocol
Table 3: Frequency of blood tests.
*Or central line, or peripheral venesection: the point is that it comes from the patient, not the machine.
** Stable = No changes required for 2 consecutive hours
Citrate Workbook V7.0 Aug 2018 12
Treatment Monitoring – continued
Adjust the Calcium Compensation and Citrate Dose based on the table below. Adjustments are made through the
Anticoag screen.
Filter Ionised Calcium Filter Ionised Calcium Filter Ionised Calcium
>0.50 0.25 – 0.5 <0.25
Patient Ionised Citrate dose increased by
Calcium 0.5mmols/L blood
AND Calcium compensation Citrate dose decreased by
< 1.0 Calcium compensation increased increased by 10% 0.5mmols/L blood
by 10%
Patient Ionised
Citrate dose increased by ‘Normal’ Citrate dose decreased by
Calcium 0.5mmols/L blood Ideal Values 0.5mmols/L blood
1.0 – 1.3
Patient Ionised Calcium compensation decreased by
Calcium 10%
Calcium compensation decreased
Calcium compensation AND
> 1.3 by 10%
decreased by 10% Citrate dose decreased by
0.5mmols/L blood
RECHECK ONE HOUR AFTER ANY CHANGE
Table 4: Adjusting Calcium and Citrate Dose
With the exceptions given in the table above, aim to make only one adjustment at a time. Then recheck for desired
effect in one hour. Making multiple changes to citrate dose, calcium compensation, blood flow or dialysis flow
simultaneously will make the interpretation of actions and subsequent troubleshooting difficult.
Total calcium to ionized calcium ratio monitoring
A high “total calcium to ionized calcium ratio” is a surrogate marker of citrate toxicity. To obtain the value, perform the
following calculation manually – TOTAL (corrected) CALCIUM ÷ PATIENT IONISED CALCIUM. Note that it is the total
corrected calcium that is used in the equation.
After 6 hours of treatment commencing, request a total corrected calcium from the lab (yellow tube, best sent with
U&Es). However, increasing calcium compensation in the preceding hours could indicate citrate accumulation. In these
circumstances, a total (corrected) calcium level may be checked before the 6 hour mark.
Ratio Action
<2.5 Check ratio daily
Consult medical staff.
Stop the PrismoCitrate for 20 minutes and restart afterwards with 70% of prior citrate dose.
Leave the calcium unchanged. This should result in a slightly higher filter ionised calcium. (0.4 to
>2.5 0.5 acceptable)
If ratio remains above 2.5 despite filter Ionised calcium of 0.4 – 0.5mmol/L then consider:
1. Doubling baseline dialysate flow (will increase citrate clearance)
2. Reducing blood pump speed (will reduce total administered citrate dose).
3. Stopping citrate and using an alternative anticoagulant (or no anticoagulant)
Table 5: Citrate Accumulation.
Citrate Workbook V7.0 Aug 2018 13
General care of patient undergoing Citrate CRRT
• Remember that it is the PATIENT IONISED CALCIUM which will affect your patient first. This is the priority for action if
you have abnormal blood tests.
• If calcium compensation is increasing and patient ionised calcium continues to decrease (by >50% of starting value)
then consider citrate accumulation. Seek help.
• Immediately after connecting and commencing therapy, check the fluid level in the deaeration chamber and adjust
appropriately. This will need to be monitored each hour and documented.
• Throughout the therapy monitor patient’s general condition for changes in hemodynamic stability. On
commencement of therapy it is not unusual for a patient’s blood pressure to fall. Sometimes a fluid bolus is
required.
• Once therapy has been commenced, it is important to calculate appropriate fluid removal. The target fluid balance
should be indicated on the medical prescription. It is important to take into consideration any fluids being
administered in the form of feed, drug volumes and drinks etc. and any fluids that are being passed or removed by
other means.
• Patient’s temperature will need to be monitored throughout treatment and the blood warmer attached to the
return line if required. Most patients will require a Bair Hugger to maintain normothermia (>36OC).
• The Prismaflex operates within fixed pressure ranges, and will stop if pressures are outside certain parameters.
These can be found on the side of the machine. Because lower blood flow rates are required with citrate, pressure-
related issues are unlikely unless you have a Vascath problem.
Citrate Workbook V7.0 Aug 2018 14
Troubleshooting Acid/Base Disturbances
BLOOD GASES POSSIBLE REASON POTENTIAL SOLUTIONS TO CONSIDER
Boost citrate removal in dialysis by increasing
dialysis flow by 500mLs/hr. Maximum dialysis
dose of 3000mLs/hr.
Too much citrate
Or:
(metabolised by the liver to
pH > 7.45 and BE > +5 Consider reducing citrate dose to patient by
bicarbonate).
reducing blood flow rate in 20mLs/min
increments.
Or:
Consider accepting higher post filter ionised
calcium by reducing citrate dose by 0.5mmol/L
pH < 7.35 and BE < -5 Reduce dialysis dose to reduce clearance of
Metabolic acidaemia – citrate, thus increasing citrate buffer load to
Total (corrected) calcium and more citrate may help patient.
patient ionised calcium Or:
normal Consider increasing blood flow rate, which will
increase citrate dose.
NB: NORMAL LIVER Or:
FUNCTION Consider systemic sodium bicarbonate infusion.
pH < 7.35 and BE < -5
Acidaemic - See Section on total (corrected) calcium to
too much citrate (and the ionised calcium ratio
Total (corrected) calcium
liver can’t handle it)
increased; patient ionised
Only generally seen in liver
calcium normal or decreased
dysfunction
CONSULTANT DISCUSSION
Ratio of total (corrected)
REQUIRED
Ca/ionised Ca > 2.5
RECHECK BLOODS ONE HOUR AFTER ANY CHANGE
ALWAYS REVIEW UNDERLYING PATHOLOGY
Table 6: Acid/Base
Citrate Workbook V7.0 Aug 2018 15
Part 2 Assessment
Using the booklet and any other resource you choose, complete the following questions.
Assessment Question 13:
The normal pressure ranges for the Prismaflex machine are:
Pressure Normal Range Limit
Access
Return
Filter
Effluent
Assessment Question 14:
a) What does a rising Transmembrane Pressure indicate?
………………………………………………………………………………………………………………………………………………………………….
b) What does a rising Pressure Drop indicate?
........................................................................................................................................................................
Assessment Question 15:
What parameters are monitored to check adequacy of anticoagulation? What else needs to be monitored for safety?
Blood Test for Adequacy Blood Test for Safety
Citrate
Assessment Question 16:
Name the site the bedside nurse should take blood from to check:
a) Circuit Ionised Calcium?
...........................................................................................................................................................
b) Patient Ionised Calcium?
...........................................................................................................................................................
Assessment Question 17:
What Blood Flow Rate will you start with for a 76kg male patient? (please tick)
100mLs/h
130mLs/h
The maximum the vascath will allow
Assessment Question 18:
What settings would you use for a 97kg woman? (please tick)
150mLs PBP, 1500mLs dialysate, 600mLs replacement
111mLs PBP, 1000mLs dialysate, 500mLs replacement
100mLs PBP, 2000mLs dialysate, 500mLs replacement
Citrate Workbook V7.0 Aug 2018 16
Assessment Question 19:
a) How often (if no changes to Citrate and Calcium compensation have been made) should you take blood?
.......................................................................................................................................................................
b) If you have to adjust your citrate dose at the first check, when must you next check?
........................................................................................................................................................................
c) You have to adjust your calcium compensation at the first check, when must you next check?
.......................................................................................................................................................................
d) You have just started CVVHDF using Citrate anticoagulation on your patient and find that on the first check the
post filter ionised calcium is 0.6mmol/L. What should you do?
........................................................................................................................................................................
e) On the next check, the post filter Ca++ is stable and the citrate dose is within the ideal range.
i. What is the ideal range? ......................................................................................................
ii. When would you next check Ca++? ......................................................................................
f) At the next check, you find that the patients Ionise Calcium is 1.45mmol/L. What do you do?
.............................................................................................................................................................
g) As you have just started Citrate therapy, when should we check the patient’s Total (corrected) Calcium?
........................................................................................................................................................................
Assessment Question 20:
a) Your patient’s ABG shows a worsening metabolic alkalosis with a high Sodium with no obvious pathology to
explain. What do you think may be the cause?
...........................................................................................................................................................
b) How might you resolve this?
..............................................................................................................................................................
c) The patient has a rise in Total (corrected) Calcium. Their bilirubin is also elevated. What might be the reason?
..............................................................................................................................................................
d) How might you resolve this?
........................................................................................................................................................................
Citrate Workbook V7.0 Aug 2018 17
Frequently Asked Questions
Q. Is heparin used to prime the circuit?
No. However patient’s lines should be “hep-locked” at the end of treatment.
Q. My patient is septic, and I want to increase my dose of RRT. How can I do this?
Increase the replacement by 10ml/kg/hr. For example, if you have a 70kg patient receiving a total RRT dose of
35ml/kg/hr, and you want to up it to 45, then increase their replacement by 700ml/hr.
Q. What do I do if I want to increase clearance?
Depending on solute to be removed, either increase replacement flow or dialysate flow or alternatively move patient up
to the next weight bracket.
• Changes to blood flow and dialysate flow rates will affect the citrate and calcium doses delivered. So change
flow rates with caution.
• Increases to post filter replacement flow should not have a demonstrable effect on patient ionised calcium or
citrate requirements. Increasing replacement rates to increase effluent dose does NOT require a change in
dialysis flow UNLESS the blood flow rate is changed also.
Q. How quickly does a change in citrate dose have its effect?
Changes to citrate dose will have a rapid effect on post filter calcium concentration, usually within 5 to 10 mins.
Q. The protocol says to reduce the citrate dose, and now the overall effluent dose has dropped. What should I do?
Should the protocol stipulate that the citrate dose be reduced, pre-blood pump flow and hence total effluent dose will
also fall. If the total effluent dose falls below 30mls/kg/hr as a result, increase the replacement flow until a dose of
30mls/kg/hr is achieved.
Q. My calcium compensation is very high. Is that normal?
There are lots of reasons why a patient’s calcium needs can increase, but if calcium compensation is above 150% this
could indicate citrate accumulation (citrate is not being metabolised and calcium is not being released). Check patient
total (corrected) calcium/patient ionised calcium ratio – if >2.5 follow protocol guideline above.
Q. What do I do if my bicarbonate is consistently low?
This could be a sign of citrate accumulation. Check calcium ratio. If within normal levels, consider giving bicarbonate.
Q. My calcium levels remain high, or are suddenly very low. What’s going on?
If post filter ionised calcium remains high with increasing citrate doses then check that the correct arrangment and type
of fluid has been installed on the replacement and dialysis lines.
A sudden and unexplained drop in the patient ionised calcium value and high post filter calcium should signal to check
the PrismoCitrate bag has been installed correctly on the pre blood pump and not the replacement line!
Q. Should I recheck bloods if the calcium chloride (CaCl) infusion adjusts by a very small amount?
Sometimes the calcium chloride infusion will adjust by 0.1 – 0.2mls when the Prismaflex attempts to compensate for
downtime when pumps have been stopped. No checks are required at very small levels if you are happy that there have
been recent reasons for pumps being stopped (e.g. for bag changes).
Q. How should citrate be re-started following a circuit change?
Citrate Workbook V7.0 Aug 2018 18
If a new circuit is started in less than an hour after stopping, then start at the previous levels of citrate and calcium
compensation. If more than an hour, then start all over again as if with a new patient.
Q. Why do I keep getting ‘calcium line clamped’ alarm??
Before filling syringe, pump the plunger up and down in the barrel of the syringe to improve movement. After making up
your syringe, discard some of the volume so that syringe volume is below 50mls. If alarm still persists – consider moving
calcium line to patient’s central line.
Q. How can I avoid machine interruptions?
Ensuring machine interruptions are kept to a minimum will maintain continuous blood circulation and therefore
seamless therapy. The following will help:
• Do not persist with therapy if –ve access pressure (>200mmHg) unresolved within 5- 10 minutes (contact
Superuser/Consultant for advice immediately)
• Recirculate blood in set ASAP in order to give time (60 mins) for Vascath manipulation (as required) or other
lengthy procedures that reduce Vascath patency.
• Ensure movement of fluid bags is kept to a minimum.
Q. The filter has clotted early despite following the protocol. What should I do?
If the patient demonstrates early filter clotting (less than 72 hours) then consider a lower target of FILTER IONISED
CALCIUM of 0.2 - 0.25mmol/L by increasing the citrate dose by 0.2mmols/L from the previous dose. Be aware of risks of
citrate accumulation and metabolic alkalosis.
Q. Does citrate affect drug pharmacokinetics or clearance ?
Not appreciably.
Citrate Workbook V7.0 Aug 2018 19
Reading List:
Ahmad, S (2009) Manual of Clinical Dialysis, 2nd edition, New York: Springer Science and Media Inc.
Davenport, A. And Tolwani, A. (2009) Citrate anticoagulation for continuous renal replacmeent therpay (CRRT) in patient
with acute kidney injuty to the intensive care unit, Nephrology Dialysis Transplantation Plus, 2, p439-447.
Hetzel GR et al (2011),Regional Citrate versus systemic heparin for anticoagulation in critically ill patients on continuous
venovenous haemfiltration: a prospective randomized mutlicentre trial, Journal of Nephrology Dialysis Transplant, 26,
(p232-239).
Kellum, J.A., Bellomo, R. And Ronco, C. (2010) Continuous Renal Replacement Therapy, New York: Oxford University
Press.
Kutsogiannis, D.J., Gibney, N., Stollery, D. and Gao, J. (2005). Regional citrate versus systemic heparin anticoagulation for
continuous renal replacement in critically ill patients. Kidney international, 67(6), p 2361-2367.
Useful Websites
http://www.gambro.com/en/uk
http://www.renal.org/Clinical/Guidelines
http://www.kdigo.org/clinical_practice_guidelines/pdf/KDIGO%20AKI%20Guideline.pdf
www.uptodate.com
Uptodate is a fantastic resource to which BCU subscribes. It is a continuous rolling review of the literature, written
and kept current by eminent physicians at prestigious American institutions. It covers just about everything. You can
get access to it via the library.
Citrate Workbook V7.0 Aug 2018 20
Page left blank intentionally – reverse of Certificate.
Citrate Workbook V7.0 Aug 2018 21
Citrate Workbook V7.0 Aug 2018 22
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Continuous Renal Replacement Therapy (CRRT) Initial Competency Assessment and ValidationDocument2 pagesContinuous Renal Replacement Therapy (CRRT) Initial Competency Assessment and Validationalex100% (1)
- HMC Unit Orientation Guideline For ICU Consortium: Clinical Day Expectations ExperiencesDocument2 pagesHMC Unit Orientation Guideline For ICU Consortium: Clinical Day Expectations ExperiencesalexNo ratings yet
- ,DanaInfo HMC Uwmedicine Org, SSL+PCC-ECG-ScheduleDocument1 page,DanaInfo HMC Uwmedicine Org, SSL+PCC-ECG-SchedulealexNo ratings yet
- Equations: Na K CLDocument2 pagesEquations: Na K CLalexNo ratings yet
- Fellows Forum: Pediatrics, Texas Children's Hospital/Baylor College of Medicine, Houston, Tex, USADocument8 pagesFellows Forum: Pediatrics, Texas Children's Hospital/Baylor College of Medicine, Houston, Tex, USAalexNo ratings yet
- Post Arrest Neuro AssessmentDocument11 pagesPost Arrest Neuro AssessmentalexNo ratings yet
- Hemodynamic Assessment ParametersDocument2 pagesHemodynamic Assessment ParametersalexNo ratings yet
- Hypothermia in Patients Resuscit A Nontraumatic Cardiac ArrestDocument3 pagesHypothermia in Patients Resuscit A Nontraumatic Cardiac ArrestalexNo ratings yet
- Consortium Schedule Summer 2014 Swedish Cherry Hill, SeattleDocument4 pagesConsortium Schedule Summer 2014 Swedish Cherry Hill, SeattlealexNo ratings yet
- Heart Failure Express Card HMCDocument2 pagesHeart Failure Express Card HMCalexNo ratings yet
- Prismaflex CRRT Competency Based Tool PDFDocument5 pagesPrismaflex CRRT Competency Based Tool PDFalex100% (1)
- PrismaFlex Flowpath PDFDocument1 pagePrismaFlex Flowpath PDFalexNo ratings yet
- Prismaflex CRRT Competency Based Tool PDFDocument5 pagesPrismaflex CRRT Competency Based Tool PDFalex100% (1)
- 1625 CRRT For OP3 PDFDocument21 pages1625 CRRT For OP3 PDFalexNo ratings yet
- A Institutional Guideline-Procedure The Management of An IABP From The University of Maryland. Uploaded 2015Document3 pagesA Institutional Guideline-Procedure The Management of An IABP From The University of Maryland. Uploaded 2015alexNo ratings yet
- CNEA - CCRN Review - Behavioral-PsychosocialDocument12 pagesCNEA - CCRN Review - Behavioral-PsychosocialalexNo ratings yet
- 00.00 Continuous Renal Replacement Therapy Handover Checklist and ReportDocument1 page00.00 Continuous Renal Replacement Therapy Handover Checklist and ReportalexNo ratings yet
- IABP - QuickReference - Systematic Approach To Evaluating IABP TimingDocument2 pagesIABP - QuickReference - Systematic Approach To Evaluating IABP Timingalex100% (1)
- 19 10th Science Question Bank English MediumDocument12 pages19 10th Science Question Bank English Mediumvadivel.km1527No ratings yet
- Role of Coupling Spin-Orbit On Damping EffectiveDocument4 pagesRole of Coupling Spin-Orbit On Damping EffectiveEdycleyson SouzaNo ratings yet
- Sans 5840Document7 pagesSans 5840Sergio Viana100% (1)
- Ventós: 1. Identification of The Substance/Mixture and The Company/UndertakingDocument5 pagesVentós: 1. Identification of The Substance/Mixture and The Company/UndertakingOctavian CoifanNo ratings yet
- IMO Coating KR PSPCDocument17 pagesIMO Coating KR PSPCJintaek Hong100% (1)
- RFCCDocument6 pagesRFCCMejdi Sylas Toudji100% (1)
- C2 Cussler PDFDocument37 pagesC2 Cussler PDFGil PinheiroNo ratings yet
- SPOTTING FinalDocument6 pagesSPOTTING FinalApurv SinhaNo ratings yet
- 11Document12 pages11Mario GonzalezNo ratings yet
- Penthouse Winter 1986Document2 pagesPenthouse Winter 1986John M. CavoteNo ratings yet
- Marine Technic Test EquipmentDocument91 pagesMarine Technic Test EquipmentBourbon EngineNo ratings yet
- Dual Fuel Waste Vegetable Oil Burner BrochureDocument2 pagesDual Fuel Waste Vegetable Oil Burner BrochureaaposxtoloNo ratings yet
- Marlex HGX 030spDocument1 pageMarlex HGX 030spErnesto CheguavaraNo ratings yet
- neodisher-IP-Spray MB en PN4304 2015-08-01 240205 152138Document1 pageneodisher-IP-Spray MB en PN4304 2015-08-01 240205 152138Lukas WijayantoNo ratings yet
- Lesson 05 - Main Steam CycleDocument20 pagesLesson 05 - Main Steam CycleAlvaro ObispoNo ratings yet
- Expression of Biological InformationDocument7 pagesExpression of Biological InformationNur Amalina KhozariNo ratings yet
- NNSA Mechanical Systems WordDocument264 pagesNNSA Mechanical Systems WordM J RhoadesNo ratings yet
- Standar Elektroda PDFDocument182 pagesStandar Elektroda PDFFakhar WindratamaNo ratings yet
- Effective Temperature ProcedureDocument4 pagesEffective Temperature ProcedurerakeshNo ratings yet
- Flexitallic SWG PDFDocument50 pagesFlexitallic SWG PDFQuang NhậtNo ratings yet
- Shs Daily Lesson Log Physical ScienceDocument33 pagesShs Daily Lesson Log Physical ScienceJaenicaPaulineCristobalNo ratings yet
- Dental RadiographsDocument96 pagesDental RadiographsAnonymous zmu21HP100% (1)
- Buehler Summet, Sample Prep and AnalysisDocument136 pagesBuehler Summet, Sample Prep and AnalysisSebastian RiañoNo ratings yet
- Lecture 4 Nozzle Theory and DesignDocument26 pagesLecture 4 Nozzle Theory and Design8기이규원No ratings yet
- Module 2Document7 pagesModule 2Fiona Belle DaganteNo ratings yet
- Vasitesa Sygef PVDFDocument380 pagesVasitesa Sygef PVDFIsrael AristaNo ratings yet
- What's The Difference Between Micro, Ultra & Nano Filtration - MembraconDocument6 pagesWhat's The Difference Between Micro, Ultra & Nano Filtration - MembraconJimmy Hend KhratNo ratings yet
- Symposium 2009 BookDocument30 pagesSymposium 2009 BookWolfram Dogman BureshNo ratings yet
- Cojinetes Lisos 4413Document56 pagesCojinetes Lisos 4413Roberto OrtegaNo ratings yet
- RamanSpectrumofGraphite 2Document6 pagesRamanSpectrumofGraphite 2Ibrahim SouleimanNo ratings yet