Professional Documents
Culture Documents
Articulo Evaluacion Final Antimicrobianos 1 2020
Articulo Evaluacion Final Antimicrobianos 1 2020
Uploaded by
Juan BojacaCopyright:
Available Formats
You might also like
- A Model of The Effects of Colonialism - DR Michael Yellow BirdDocument2 pagesA Model of The Effects of Colonialism - DR Michael Yellow Birdhuehue2100% (1)
- Fingerprint Mock Crime Scene Birch2015Document10 pagesFingerprint Mock Crime Scene Birch2015api-281965445No ratings yet
- 5.4 Risk Factors For MRSA ColonizationDocument8 pages5.4 Risk Factors For MRSA ColonizationQworldNo ratings yet
- 10Document10 pages10duarte.pheNo ratings yet
- Methicillin-Resistant Staphylococcus Aureus in NepDocument5 pagesMethicillin-Resistant Staphylococcus Aureus in NepHafiza AyeshaNo ratings yet
- Effectiveness of Contact Isolation During A Hospital Outbreak of Methicillin-Resistant Staphylococcus AureusDocument9 pagesEffectiveness of Contact Isolation During A Hospital Outbreak of Methicillin-Resistant Staphylococcus Aureusmoniart2587No ratings yet
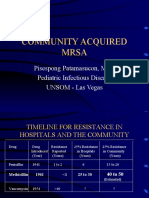
- Community Acquired Mrsa: Pisespong Patamasucon, M.D. Pediatric Infectious Disease UNSOM - Las VegasDocument48 pagesCommunity Acquired Mrsa: Pisespong Patamasucon, M.D. Pediatric Infectious Disease UNSOM - Las VegasRashed NazzalNo ratings yet
- Risk Factor For MRSA in Skin, Soft Tissue and Bone Infection in The Foot and Leg in California Community HospitalDocument11 pagesRisk Factor For MRSA in Skin, Soft Tissue and Bone Infection in The Foot and Leg in California Community HospitalReza Suryapandu NugrohoNo ratings yet
- Mssa 2011 PDFDocument8 pagesMssa 2011 PDFBebenzzzNo ratings yet
- MRSA Nosocomial Infection BacteryDocument6 pagesMRSA Nosocomial Infection BacteryZUKHRUFIA ISNA PRAMADEWINo ratings yet
- HTTPSWWW - Ncbi.nlm - nih.GovpmcarticlesPMC9024581pdfjcdd 09 00103 PDFDocument13 pagesHTTPSWWW - Ncbi.nlm - nih.GovpmcarticlesPMC9024581pdfjcdd 09 00103 PDFreza fahleviNo ratings yet
- MrsaDocument10 pagesMrsazia ul RahmanNo ratings yet
- Skin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusDocument11 pagesSkin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusFerdy RamadhanNo ratings yet
- Update On Antifungal Resistance - TimiDocument4 pagesUpdate On Antifungal Resistance - Timix994thng65No ratings yet
- Journal of Clinical Immunology and MicrobiologyDocument10 pagesJournal of Clinical Immunology and MicrobiologyAthenaeum Scientific PublishersNo ratings yet
- A Hospital Based Prospective Study of Prevalence of Methicillin Resistant Staphylococcus Aureus in Dermatology Indoor Patients by Phenotypic MethodDocument9 pagesA Hospital Based Prospective Study of Prevalence of Methicillin Resistant Staphylococcus Aureus in Dermatology Indoor Patients by Phenotypic MethodIJAR JOURNALNo ratings yet
- MRSA Skin and Soft Tissue InfectionsDocument5 pagesMRSA Skin and Soft Tissue Infectionsapi-3801331No ratings yet
- 1 s2.0 S1201971209000435 MainDocument7 pages1 s2.0 S1201971209000435 MainGopalaKrishnanNo ratings yet
- Life 13 01126Document14 pagesLife 13 01126s4cdbv4xjrNo ratings yet
- Surgical Site Infection in A Teaching Hospital: A Prospective StudyDocument7 pagesSurgical Site Infection in A Teaching Hospital: A Prospective StudymajedNo ratings yet
- 05 N312 18329Document9 pages05 N312 18329GinshaNo ratings yet
- JCDR 7 1339Document4 pagesJCDR 7 1339RahayuNo ratings yet
- Due To Two Methicillin-Resistant Widespread Skin and Soft-Tissue InfectionsDocument7 pagesDue To Two Methicillin-Resistant Widespread Skin and Soft-Tissue Infectionschilvys04No ratings yet
- Bacterial Skin and Soft Tissue Infections: Clinical Review ArticleDocument9 pagesBacterial Skin and Soft Tissue Infections: Clinical Review ArticleRini MayaSariNo ratings yet
- Antibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHDocument5 pagesAntibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHzia ul RahmanNo ratings yet
- Prevalence of CA MRSA Nasal Carriage Among Children of ConsultationDocument6 pagesPrevalence of CA MRSA Nasal Carriage Among Children of ConsultationGoGoPenguinVALNo ratings yet
- MRSADocument6 pagesMRSAIgnacio Velasquez MiñoNo ratings yet
- Staphylococcus Aureus in Neonatal: Methicillin-Resistant Intensive Care UnitDocument4 pagesStaphylococcus Aureus in Neonatal: Methicillin-Resistant Intensive Care UnitAulina Refri RahmiNo ratings yet
- Rab 9Document12 pagesRab 9Belia DestamaNo ratings yet
- Molecular EpidemiologyDocument11 pagesMolecular EpidemiologymotibaNo ratings yet
- Methicillin Resistant Staphylococcus Aureus (MRSA) in The Intensive Care UnitDocument8 pagesMethicillin Resistant Staphylococcus Aureus (MRSA) in The Intensive Care UnitMuhammad AliNo ratings yet
- Epidemiology and Clinical Manifestations of Mucormycosis CMIDocument9 pagesEpidemiology and Clinical Manifestations of Mucormycosis CMIDINESH VENKATESANNo ratings yet
- Methicillinresistant Staphylococcus Aureus A Mini ReviewDocument6 pagesMethicillinresistant Staphylococcus Aureus A Mini ReviewSandhi WiryaNo ratings yet
- Mrsa101 508Document45 pagesMrsa101 508Sam TullyNo ratings yet
- 1 - Name of The Candidate and AddressDocument19 pages1 - Name of The Candidate and AddressRini ThomasNo ratings yet
- Sphingomonas KoreensisDocument11 pagesSphingomonas KoreensisSMIBA MedicinaNo ratings yet
- Transferable Vancomycin Resistance in A Community-Associated MRSA LineageDocument8 pagesTransferable Vancomycin Resistance in A Community-Associated MRSA LineageMabel StracciaNo ratings yet
- Epidemiology Roun1Document10 pagesEpidemiology Roun1FebniNo ratings yet
- Methicillin-Resistant Staphylococcus Tuberculosis: Part 1: Aureus and Multidrug ResistantDocument3 pagesMethicillin-Resistant Staphylococcus Tuberculosis: Part 1: Aureus and Multidrug ResistantSukma EffendyNo ratings yet
- Research Paper On MrsaDocument4 pagesResearch Paper On Mrsam0d1p1fuwub2100% (1)
- IJMLR231704Document7 pagesIJMLR231704sandeep raiNo ratings yet
- PMID 36974854 OpportunisticDocument8 pagesPMID 36974854 Opportunisticajaya basnetNo ratings yet
- Free Research Papers On MrsaDocument8 pagesFree Research Papers On Mrsaafnhbijlzdufjj100% (1)
- Miller 2016Document4 pagesMiller 2016Lidia JimenezNo ratings yet
- Current Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusDocument15 pagesCurrent Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusSeptiani HasibuanNo ratings yet
- Jamainternal Jones 2020 Oi 190118-4Document9 pagesJamainternal Jones 2020 Oi 190118-4LuthfiNo ratings yet
- 1 s2.0 S0002934322007227 MainDocument8 pages1 s2.0 S0002934322007227 MainMaryatiNo ratings yet
- Measles Outbreak NejmoaDocument12 pagesMeasles Outbreak NejmoaVlad ManoleNo ratings yet
- Gill Et Al 2005 Insights On Evolution of Virulence and Resistance From The Complete Genome Analysis of An EarlyDocument13 pagesGill Et Al 2005 Insights On Evolution of Virulence and Resistance From The Complete Genome Analysis of An EarlyNora LeeNo ratings yet
- Artigo C Neoformans PDFDocument29 pagesArtigo C Neoformans PDFJorge Luis CarmoNo ratings yet
- Children and MRSADocument6 pagesChildren and MRSAcharanmann9165No ratings yet
- Lander 2016Document2 pagesLander 2016Jocilene Dantas Torres NascimentoNo ratings yet
- A Measles Outbreak in An Underimmunized Amish Community in OhioDocument12 pagesA Measles Outbreak in An Underimmunized Amish Community in Ohiomuhammad maadaNo ratings yet
- Clinical Microbiology and InfectionDocument9 pagesClinical Microbiology and InfectionAguilarKrystell'No ratings yet
- The Foot: Original ArticleDocument5 pagesThe Foot: Original ArticleKarinaayu SerinNo ratings yet
- A 10-Year Review of Ocular Methicillin-Resistant Staphylococcus Aureus InfectionsDocument6 pagesA 10-Year Review of Ocular Methicillin-Resistant Staphylococcus Aureus InfectionsBima RizkiNo ratings yet
- Meticillin Resistant - Staphylococcus - Aure20160520 7685 19p6anl With Cover Page v2Document11 pagesMeticillin Resistant - Staphylococcus - Aure20160520 7685 19p6anl With Cover Page v2Delvita ElyasNo ratings yet
- 1000 Genomas RusiaDocument9 pages1000 Genomas RusiaDamarisNo ratings yet
- Journal of Clinical Immunology & MicrobiologyDocument9 pagesJournal of Clinical Immunology & MicrobiologyAthenaeum Scientific PublishersNo ratings yet
- Species Identification and Antifungal Susceptibility of Uncommon Blood Yeast IsolatesDocument8 pagesSpecies Identification and Antifungal Susceptibility of Uncommon Blood Yeast Isolatesa.rahadianNo ratings yet
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementFrom EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouNo ratings yet
- Roadmap For Bible StudyDocument1 pageRoadmap For Bible Study4gen_3No ratings yet
- Cobb 500Document16 pagesCobb 500scribeascrapNo ratings yet
- Geographical Indication (DARJEELING TEA REPORT)Document8 pagesGeographical Indication (DARJEELING TEA REPORT)srksamNo ratings yet
- MS Access - Working With QueriesDocument69 pagesMS Access - Working With QueriesbogsbestNo ratings yet
- Chapter 1 TVTDocument14 pagesChapter 1 TVTtemedebereNo ratings yet
- The A To Z List of Reflexology Research3Document110 pagesThe A To Z List of Reflexology Research3Ahmad Saiful Ridzwan JaharuddinNo ratings yet
- Nolasco Labor I CompilationDocument115 pagesNolasco Labor I CompilationNico QuebalNo ratings yet
- Low Sperm Count and Its Homeopathic Cure - DR Bashir Mahmud ElliasDocument9 pagesLow Sperm Count and Its Homeopathic Cure - DR Bashir Mahmud ElliasBashir Mahmud ElliasNo ratings yet
- Intermediate Accounting - Kieso - Chapter 1Document46 pagesIntermediate Accounting - Kieso - Chapter 1Steffy AmoryNo ratings yet
- Lecture 01 - Construction EngineeringDocument18 pagesLecture 01 - Construction EngineeringKw TseNo ratings yet
- Towards A Radical RizalDocument34 pagesTowards A Radical RizalBryle CamaroteNo ratings yet
- The Swadeshi MovementDocument17 pagesThe Swadeshi Movementbharathkarna97No ratings yet
- Pedal Operated Washing Machine ReportDocument35 pagesPedal Operated Washing Machine ReportJack Johnson100% (1)
- Fluid Machines Lecture Notes CH-4-Centrifugal CompressorDocument21 pagesFluid Machines Lecture Notes CH-4-Centrifugal CompressorBINNo ratings yet
- "You Shall Not Take The Name of The Lord Your God in Vain": Anger Coarse Vulgar Speech, ProfanityDocument10 pages"You Shall Not Take The Name of The Lord Your God in Vain": Anger Coarse Vulgar Speech, ProfanityMarvin MonterosoNo ratings yet
- First Class Dhanbad 2012Document4 pagesFirst Class Dhanbad 2012ihateu1No ratings yet
- Manila Standard Today - Friday (November 23, 2012) IssueDocument28 pagesManila Standard Today - Friday (November 23, 2012) IssueManila Standard TodayNo ratings yet
- Upload 9Document3 pagesUpload 9Meghna CmNo ratings yet
- Basic Labor and Employment Education CourseDocument9 pagesBasic Labor and Employment Education CourseJennifer Tan Marcial100% (2)
- 2008olbrycht Alex OpisDocument23 pages2008olbrycht Alex OpisHamid Reza SorouriNo ratings yet
- Rundown Acara WorkshopDocument6 pagesRundown Acara WorkshopAnnas Nuraini br gintingNo ratings yet
- BIG-IP CGNAT ImplementationsDocument208 pagesBIG-IP CGNAT ImplementationsThiago CabralNo ratings yet
- The Gorgon's HeadDocument3 pagesThe Gorgon's HeadReden Macaraeg Juego100% (1)
- Thesis in Teaching English As Foreign LanguageDocument8 pagesThesis in Teaching English As Foreign Languagereneedelgadoalbuquerque100% (2)
- AWHERO - Military Applications Brochure - Gen2020Document4 pagesAWHERO - Military Applications Brochure - Gen2020زين الدين مروانيNo ratings yet
- Physics (From: Physik (Epist Mē)Document1 pagePhysics (From: Physik (Epist Mē)annmarieNo ratings yet
- United States v. Castillo Moronta, 27 F.3d 554, 1st Cir. (1994)Document3 pagesUnited States v. Castillo Moronta, 27 F.3d 554, 1st Cir. (1994)Scribd Government DocsNo ratings yet
- Sop QubDocument2 pagesSop QubAMRUD GAMINGNo ratings yet
Articulo Evaluacion Final Antimicrobianos 1 2020
Articulo Evaluacion Final Antimicrobianos 1 2020
Uploaded by
Juan BojacaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articulo Evaluacion Final Antimicrobianos 1 2020
Articulo Evaluacion Final Antimicrobianos 1 2020
Uploaded by
Juan BojacaCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Methicillin-Resistant S. aureus Infections
among Patients in the Emergency Department
Gregory J. Moran, M.D., Anusha Krishnadasan, Ph.D.,
Rachel J. Gorwitz, M.D., M.P.H., Gregory E. Fosheim, M.P.H.,
Linda K. McDougal, M.S., Roberta B. Carey, Ph.D., and David A. Talan, M.D.,
for the EMERGEncy ID Net Study Group*
A bs t r ac t
Background
From the Department of Emergency Med- Methicillin-resistant Staphylococcus aureus (MRSA) is increasingly recognized in infec-
icine (G.J.M., A.K., D.A.T.) and the Division tions among persons in the community without established risk factors for MRSA.
of Infectious Diseases (G.J.M., D.A.T.),
Olive View–UCLA Medical Center, Sylmar,
Calif.; and the Division of Healthcare Methods
Quality Promotion, National Center for We enrolled adult patients with acute, purulent skin and soft-tissue infections pre-
Infectious Diseases, Centers for Disease
Control and Prevention, Atlanta (R.J.G., senting to 11 university-affiliated emergency departments during the month of
G.E.F., L.K.M., R.B.C.). Address reprint re- August 2004. Cultures were obtained, and clinical information was collected. Available
quests to Dr. Moran at the Department of S. aureus isolates were characterized by antimicrobial-susceptibility testing, pulsed-field
Emergency Medicine, Olive View–UCLA
Medical Center, 14445 Olive View Dr., gel electrophoresis, and detection of toxin genes. On MRSA isolates, we performed
North Annex, Sylmar, CA 91342, or at typing of the staphylococcal cassette chromosome mec (SCCmec), the genetic element
idnet@ucla.edu. that carries the mecA gene encoding methicillin resistance.
*Members of the EMERGEncy ID Net Study
Group are listed in the Appendix. Results
S. aureus was isolated from 320 of 422 patients with skin and soft-tissue infections
N Engl J Med 2006;355:666-74.
Copyright © 2006 Massachusetts Medical Society. (76 percent). The prevalence of MRSA was 59 percent overall and ranged from 15 to
74 percent. Pulsed-field type USA300 isolates accounted for 97 percent of MRSA iso-
lates; 74 percent of these were a single strain (USA300-0114). SCCmec type IV and
the Panton–Valentine leukocidin toxin gene were detected in 98 percent of MRSA
isolates. Other toxin genes were detected rarely. Among the MRSA isolates, 95 per-
cent were susceptible to clindamycin, 6 percent to erythromycin, 60 percent to fluo-
roquinolones, 100 percent to rifampin and trimethoprim–sulfamethoxazole, and 92
percent to tetracycline. Antibiotic therapy was not concordant with the results of
susceptibility testing in 100 of 175 patients with MRSA infection who received anti-
biotics (57 percent). Among methicillin-susceptible S. aureus isolates, 31 percent were
USA300 and 42 percent contained pvl genes.
Conclusions
MRSA is the most common identifiable cause of skin and soft-tissue infections among
patients presenting to emergency departments in 11 U.S. cities. When antimicrobial
therapy is indicated for the treatment of skin and soft-tissue infections, clinicians
should consider obtaining cultures and modifying empirical therapy to provide MRSA
coverage.
666 n engl j med 355;7 www.nejm.org august 17, 2006
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
mrsa infections among patients in the emergency department
M
ethicillin-resistant staphylococ- geles; Minneapolis; New Orleans; New York; Phila-
cus aureus (MRSA) emerged in the 1960s delphia; Phoenix, Ariz.; and Portland, Oreg. These
as a cause of infection among patients departments had a combined approximate total of
exposed to the bacteria in health care settings.1 900,000 visits per year.14 The study was approved by
More recently, MRSA infections have been report- the institutional review board at each site.
ed among persons without such exposure (com- Patients 18 years of age or older presenting in
munity-associated MRSA).2,3 Community-associ- August 2004 with purulent skin and soft-tissue
ated outbreaks of MRSA infection have occurred infections of less than one week’s duration (ex-
among prisoners, intravenous-drug users, athletes, cluding perirectal abscesses) were enrolled in the
military trainees, and men who have sex with study. Consent was obtained in writing at eight
men.4-6 Community-associated MRSA has primar- sites and orally with provision of an information
ily been described as a cause of skin and soft-tissue sheet at three sites. Information on demographic
infections, but it has also been associated with sep- characteristics, clinical presentation, potential risk
sis and necrotizing pneumonia.7-9 As compared factors for MRSA infection, and treatments pro-
with health care–associated MRSA isolates, com- vided was collected by emergency department
munity-associated MRSA isolates tend to be re- physicians using standardized forms. Manage-
sistant to fewer antibiotics, to produce different ment decisions were made on an individual basis
toxins,10 and to have different types of the gene by physicians in the emergency department. Fol-
complex known as staphylococcal cassette chro- low-up data were obtained by telephone approxi-
mosome mec (SCCmec); this complex contains the mately two to three weeks after enrollment.
mecA gene that confers methicillin resistance.10 Specimens were obtained from the single larg-
Pulsed-field gel electrophoresis (PFGE) and other est area of infection with the use of sterile Dacron
methods have identified a small number of molec- swabs and were processed and cultured at hospital
ular types that have accounted for most commu- laboratories according to standard techniques.15
nity-associated MRSA isolates characterized in the Each laboratory determined the antimicrobial sus-
United States.11 ceptibility of S. aureus isolates to the panel of
Some institutions have a high prevalence of agents routinely tested at that laboratory.16 Avail-
MRSA isolated from patients with sporadic skin able S. aureus isolates were forwarded to the Cen-
and soft-tissue infections that are not associated ters for Disease Control and Prevention (CDC) for
with an outbreak.12,13 However, data are limited further characterization. The inducibility of clinda-
regarding the prevalence of MRSA as a cause of mycin resistance was determined by the D-zone
skin and soft-tissue infections among patients in disk-diffusion test.17 The presence of genes for
several communities throughout the United States staphylococcal enterotoxins A through E and H,
and the S. aureus isolates associated with these in- toxic shock syndrome toxin 1 (TSST-1), and Pan-
fections. Therefore, we determined the prevalence ton–Valentine leukocidin (pvl) and the type of
of MRSA as a cause of skin infections among adult SCCmec were determined by the polymerase chain
patients presenting to emergency departments in reaction. All isolates were typed by PFGE with
several geographically diverse, metropolitan areas the use of SmaI restriction endonuclease. Addi-
in the United States. We also determined the bac- tional methods are described in detail in the Sup-
teriologic characteristics of S. aureus isolated from plementary Appendix (available with the full text
skin and soft-tissue infections and evaluated fac- of this article at www.nejm.org).
tors potentially associated with MRSA infections of Descriptive statistics were used to summarize
skin and soft tissue. the characteristics of the patients and the preva-
lence of MRSA. To identify potential risk factors
Me thods for MRSA infection among patients with skin and
soft-tissue infections, we calculated adjusted odds
We conducted a prospective prevalence study in- ratios and 95 percent confidence intervals. Vari-
volving adult patients with skin and soft-tissue infec- ables associated with MRSA infection in bivariate
tions who presented to hospitals in the EMERGEncy analyses were explored further with the use of
ID Net, a network of university-affiliated emer- multivariate logistic regression.
gency departments in 11 U.S. cities: Albuquerque; Audits of emergency department and laboratory
Atlanta; Charlotte, N.C.; Kansas City, Mo.; Los An- logs for patients with a discharge diagnosis of ab-
n engl j med 355;7 www.nejm.org august 17, 2006 667
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
scess, cellulitis, or wound infection were conduct- The prevalence of MRSA ranged from 15 to 74
ed at all study sites (except Atlanta) to determine percent, and MRSA was the most common identi-
the proportion of patients meeting eligibility cri- fiable cause of skin and soft-tissue infections in
teria who were enrolled in the study. Demograph- 10 of 11 emergency departments. MRSA was iso-
ic and clinical characteristics of enrolled patients lated from 61 percent of abscesses, 53 percent of
were compared with those of unenrolled patients. purulent wounds, and 47 percent of cases of cel-
lulitis with purulent exudate. Other organisms
R e sult s isolated from 1 percent or more of infections
included 71 isolates of methicillin-susceptible
A total of 422 patients with skin and soft-tissue S. aureus (MSSA) (17 percent); 30 isolates of strep-
infections were enrolled. The median age was 39 tococcus species (7 percent) including 6 group B
years (range, 18 to 79; interquartile range, 28 to streptococcus, 2 group A streptococcus, 3 non–
47), and 62 percent were men. Race or ethnic group group A and non–group B β-hemolytic streptococ-
was determined by the clinicians: 49 percent of pa- cus, 4 anaerobic or microaerophilic streptococcus,
tients were non-Hispanic blacks, 25 percent were and 15 viridans group streptococcus; 12 isolates
non-Hispanic whites, 22 percent were Hispanic, of coagulase-negative staphylococci (3 percent);
and 4 percent belonged to other groups. Infections and 6 isolates of Proteus mirabilis (1 percent). Cul-
were located on the upper extremities in 29 percent tures from 31 patients were polymicrobial; 10 of
of patients, lower extremities in 27 percent, torso these patients had MRSA. No microorganism was
in 17 percent, perineum in 14 percent, and head isolated from 38 patients (9 percent).
and neck in 13 percent. Infections were classified A total of 218 MRSA isolates (88 percent) and
as an abscess in 81 percent of patients, an infected 55 MSSA isolates (77 percent) from 10 emergency
wound in 11 percent, and as cellulitis with purulent departments were sent to the CDC for genetic and
exudate in 8 percent. phenotypic characterization. The pulsed-field types
S. aureus was isolated from skin and soft-tissue of 216 of the MRSA isolates (99 percent) tested
infections in 320 patients (76 percent); 249 of the were characteristic of community-associated MRSA:
S. aureus isolates (78 percent) were MRSA. MRSA 212 were type USA300, 2 were type USA400, and
was isolated from 59 percent of patients (Table 1). 2 were type USA1000.11,18 Of 212 MRSA isolates
Table 1. Bacterial Isolates from Purulent Skin and Soft-Tissue Infections in 11 U.S. Emergency Departments.*
No. of Patients Enrolled MRSA MSSA Other Bacteria No Bacterial Growth
Site (N = 422) (N = 249)† (N = 71) (N = 64)‡ (N = 38)
number (percent)
Albuquerque 42 25 (60) 10 (24) 3 (7) 4 (10)
Atlanta 32 23 (72) 4 (12) 3 (9) 2 (6)
Charlotte, N.C. 25 17 (68) 0 4 (16) 4 (16)
Kansas City, Mo. 58 43 (74) 6 (10) 4 (7) 5 (9)
Los Angeles 47 24 (51) 6 (13) 8 (17) 9 (19)
Minneapolis 28 11 (39) 4 (14) 9 (32) 4 (14)
New Orleans 69 46 (67) 11 (16) 9 (13) 3 (4)
New York 20 3 (15) 8 (40) 5 (25) 4 (20)
Philadelphia 58 32 (55) 12 (21) 12 (21) 2 (3)
Phoenix, Ariz. 30 18 (60) 8 (27) 4 (13) 0
Portland, Oreg. 13 7 (54) 2 (15) 3 (23) 1 (8)
* A total of 31 cultures, including 10 cultures from which MRSA was isolated, were polymicrobial. Because of rounding,
percentages may not total 100. MSSA denotes methicillin-resistant Staphylococcus aureus.
† P<0.001 for the test for homogeneity of MRSA prevalence across sites.
‡ Other bacteria isolated were as follows: MSSA (17 percent), streptococcus species (7 percent), coagulase-negative
staphylococci (3 percent), and Proteus mirabilis (1 percent).
668 n engl j med 355;7 www.nejm.org august 17, 2006
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
mrsa infections among patients in the emergency department
characterized as type USA300, 156 (74 percent) teria (Table 2) included antibiotic use in the month
had a single pulsed-field pattern (strain USA300- before enrollment, the presence of an abscess or
0114). SCCmec type IV, characteristic of commu- a lesion attributed to a spider bite at enrollment,
nity-associated MRSA,19 was found in 214 (98 history of MRSA infection, and a recent history of
percent) of the MRSA isolates, and pvl toxin genes close contact with someone with a similar skin
were present in 213 (98 percent). Genes for staph- infection. The presence of an underlying illness
ylococcal enterotoxins A, B, C, D, E, and H and and characterization as belonging to the “other”
TSST-1 were identified in five or fewer MRSA iso- category of race or ethnic background were nega-
lates. Eight S. aureus isolates collected at the At- tively associated with the isolation of MRSA. In
lanta site in April 2005 were similar to other study multivariate logistic-regression analyses, all these
isolates with regard to PFGE and toxin character- factors were associated with MRSA infection, with
istics. the exception of the presence of an abscess (Table
USA300 was also the most common pulsed- 3). Black race was independently associated with
field type among MSSA isolates, accounting for 17 MRSA infection. Controlling for study site did not
of 55 MSSA isolates (31 percent) sent to the CDC. affect the association between any of these factors
Among these type USA300 isolates, 8 (47 percent) and MRSA infection. Among 64 patients with
had a pulsed-field pattern closely related to that of none of these factors, 31 (48 percent) were infected
the MRSA strain USA300-0114. In addition, pvl with MRSA. The only factor that was significantly
genes were detected in 23 MSSA isolates (42 per- associated with isolation of MRSA, as compared
cent), including 17 (100 percent) of the isolates with MSSA, was the presence of abscess at enroll-
characterized as USA300. ment (odds ratio, 2.3; 95 percent confidence inter-
MRSA susceptibilities were as follows: 100 val, 1.2 to 4.4).
percent were susceptible to trimethoprim–sulfa- Complete information about treatment was
methoxazole (217 of 217) and to rifampin (186 of available for 406 of the 422 patients (96 percent).
186); 95 percent were susceptible to clindamycin Of these, 79 (19 percent) were treated with incision
(215 of 226), 92 percent to tetracycline (207 of and drainage alone, 39 (10 percent) received anti-
226), 60 percent to fluoroquinolones (106 of 176), biotics alone, 267 (66 percent) were treated with
and 6 percent to erythromycin (13 of 226). Al- both incision and drainage and antibiotics, and 21
though the proportion of all S. aureus isolates (5 percent) neither underwent incision and drain-
(MRSA and MSSA) that were resistant to clindamy- age nor received antibiotics. Of 400 patients for
cin was less than 15 percent at 10 of the study whom information about the outcome was avail-
sites, 6 of 10 S. aureus isolates from New York City able, 59 (15 percent) were admitted to the hospital.
(60 percent) were resistant to clindamycin. Among An antistaphylococcal penicillin or cephalospo-
the isolates that were sent to the CDC, 11 of 218 rin was given to 198 of 311 patients who received
MRSA isolates (5 percent) and 7 of 55 MSSA iso- antibiotics (64 percent). In 100 of 175 MRSA in-
lates (13 percent) were not susceptible to clinda- fections for which antibiotic treatment was pro-
mycin, including 4 (2 percent) MRSA isolates and vided (57 percent), antibiotic therapy was not con-
5 (9 percent) MSSA isolates with inducible clinda- cordant with the results of susceptibility testing.
mycin resistance detected by an antimicrobial- Of the 422 patients, 248 (59 percent) were con-
susceptibility D-zone disk-diffusion test. Sixty-six tacted for follow-up 15 to 21 days (median, 17)
patients with MRSA infections (27 percent) had after their visit to the emergency department, and
one or more established risk factors for health 238 (96 percent) of those patients who were con-
care–associated MRSA; these included 43 pa- tacted for follow-up reported that their infection
tients who had been hospitalized within the past had resolved or improved. There were no signifi-
year, 28 with a history of MRSA infection, 2 who cant differences in the outcome between patients
resided in a long-term care facility, and 1 who infected with MRSA and those infected with other
was undergoing dialysis. Isolates from 55 of these bacteria or between patients in whom the infect-
patients were evaluated at the CDC, and 54 (98 ing MRSA isolate was resistant and those in whom
percent) had pulsed-field types characteristic of the isolate was susceptible to the prescribed anti-
community-associated MRSA. biotic. Baseline characteristics were similar for
Features associated with the isolation of MRSA patients with and those without follow-up infor-
as compared with the isolation of any other bac- mation.
n engl j med 355;7 www.nejm.org august 17, 2006 669
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 2. Potential Risk Factors for Infection with MRSA, as Compared with Other Bacteria, in Patients with Purulent Skin
and Soft-Tissue Infections in 11 U.S. Emergency Departments.*
MRSA Other Bacteria Odds Ratio
Risk Factor (N = 249) (N = 135) (95% CI)†
no./total no. (%)
Race or ethnic group
Non-Hispanic white 61/247 (25) 37/135 (27) 1.0‡
Non-Hispanic black 134/247 (54) 53/135 (39) 1.6 (0.9–2.6)
Hispanic 48/247 (19) 36/135 (27) 0.8 (0.4–1.5)
Other 4/247 (2) 9/135 (7) 0.3 (0.1–0.9)§
Intravenous-drug user 26/244 (11) 11/135 (8) 1.3 (0.6–3.0)
Taken any antibiotic in past mo 84/245 (34) 24/134 (18) 2.4 (1.4–4.1)§
Taking antibiotic for the infection 61/244 (25) 24/134 (18) 1.5 (0.9–2.7)
Prison or jail in past yr 53/244 (22) 19/135 (14) 1.7 (0.9–3.1)
Competitive sports involving contact in past mo 21/246 (9) 8/135 (6) 1.5 (0.6–3.8)
Homeless in past yr 40/246 (16) 17/135 (13) 1.3 (0.7–2.6)
Abscess 203/243 (84) 97/131 (74) 1.8 (1.0–3.1)§
Spontaneous infection (no apparent precipitating factor) 100/248 (40) 49/135 (36) 1.2 (0.8–1.9)
Reported spider bite 71/248 (29) 17/135 (13) 2.8 (1.5–5.3)§
Underlying illness 25/249 (10) 34/135 (25) 0.3 (0.2–0.6)§
HIV infection 11/249 (4) 4/135 (3) 1.5 (0.5–4.9)
History of MRSA infection 28/242 (12) 5/132 (4) 3.3 (1.2–10.1)§
Hospitalized in past yr 43/247 (17) 32/135 (24) 0.7 (0.4–1.2)
Resident in long-term care facility 2/244 (1) 2/134 (1) 0.6 (0.0–7.6)
Health care worker 17/244 (7) 5/135 (4) 1.9 (0.7–6.9)
Homosexual male contact 7/132 (5) 5/79 (6) 0.8 (0.2–3.4)
Close contact with person with similar infection 43/245 (18) 8/135 (6) 3.4 (1.5–8.1)§
Household contact with MRSA infection 15/245 (6) 3/131 (2) 2.8 (0.8–15.2)
Household contact with health care exposure¶ 46/249 (18) 30/135 (22) 0.8 (0.5–1.4)
Household contact with jail exposure 42/243 (17) 15/131 (11) 1.6 (0.8–3.2)
Household contact with intravenous-drug use 27/245 (11) 11/133 (8) 1.4 (0.6–3.1)
* CI denotes confidence interval, and HIV human immunodeficiency virus.
† Missing data were excluded in these calculations. Information regarding race was missing for two patients.
‡ This group served as the reference group for other race variables.
§ P<0.05.
¶ This category includes hospitalization or residence in a long-term care facility in past year, employment as a health care
worker, receipt of dialysis, or presence of an indwelling catheter or tube.
Case-finding audits revealed that approximate- from whom wound cultures were obtained (57
ly 42 percent of eligible patients were enrolled. As percent).
compared with enrolled patients, unenrolled pa-
tients were similar in terms of age (mean, 38 years; Dis cus sion
range, 18 to 82), sex (63 percent were male), and
race or ethnic group (57 percent were white non- MRSA has emerged as the most common identi-
Hispanic or Hispanic, 39 percent were black, and fiable cause of skin and soft-tissue infections in
4 percent were in other groups). MRSA was iso- several metropolitan areas across the United States.
lated in 135 of 236 eligible but unenrolled patients Although more than 80 percent of patients with
670 n engl j med 355;7 www.nejm.org august 17, 2006
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
mrsa infections among patients in the emergency department
skin and soft-tissue infections associated with
Table 3. Results of Multivariate Logistic-Regression Analyses to Identify Potential
MRSA in this study received empirical antimicro- Risk Factors for MRSA Infection.*
bial therapy for their infection, the infecting iso-
late was resistant to the agent prescribed for 57 Adjusted Odds Ratio
Characteristic (95% CI)*
percent of these patients. This finding suggests a
Race
need to reconsider empirical antimicrobial choic-
es for skin and soft-tissue infections in areas where Non-Hispanic white 1.0†
MRSA is prevalent in the community. Non-Hispanic black 1.9 (1.1–3.4)
Our findings are consistent with the dramatic Other 0.3 (0.1–1.0)
trend of increasing reports of outbreaks and in- Use of any antibiotic in past mo (vs. no use) 2.4 (1.3–4.3)
creased prevalence of community-associated MRSA Reported spider bite (vs. other cause of infection) 3.0 (1.6–5.7)
during the past few years. MRSA was uncommon
Underlying illness (vs. no underlying infection) 0.3 (0.2–0.6)
in community-acquired skin and soft-tissue infec-
tions before 2000 and accounted for only 3 percent History of MRSA infection (vs. absence of such history) 3.4 (1.1–10)
of staphylococcal isolates submitted to Minnesota Close contact with person with similar infection 3.8 (1.6–9.3)
(vs. no close contact)
laboratories in 2000.20 Between 2001 and 2004,
the prevalence of MRSA among patients with * Estimates were adjusted for all other variables in the table. CI denotes confi-
skin and soft-tissue infections at our Los Ange- dence interval.
les institution increased from 29 percent to 64 † This group served as the reference group for other race variables.
percent.13
Virtually all (99 percent) MRSA strains isolated consistent with other recent reports.24,25 S. aureus
from skin and soft-tissue infections in this study strains containing pvl genes have been associated
had pulsed-field types characteristic of commu- with spontaneous skin and soft-tissue infections
nity-associated MRSA, even though more than and necrotizing pneumonia; however, the role of
25 percent of patients had established risk fac- pvl toxin in the pathogenesis of S. aureus skin and
tors for health care–associated MRSA. A single soft-tissue infections has not been fully eluci-
pulsed-field type (USA300) accounted for 97 per- dated.26
cent of MRSA isolates and 31 percent of MSSA Most patients in our study were treated with
isolates. A single strain (USA300-0114) associated β-lactam agents such as cephalexin and dicloxa-
with previously reported community outbreaks5 cillin, to which MRSA isolates are not suscepti-
accounted for 72 percent of MRSA isolates, and ble. Although we had limited follow-up informa-
a closely related strain was the single most com- tion, we found no association between patients’
mon MSSA strain identified. Pulsed-field type outcomes and the susceptibility of the pathogen
USA300 has been linked to community-associ- to the prescribed antimicrobial agents. This ab-
ated MRSA outbreaks throughout the country5,11 sence of an association, which is consistent with
and represents the leading cause of community- previous reports,3,27 suggests that most simple
associated MRSA in single-center prevalence stud- skin abscesses, even when caused by MRSA, can
ies.12,21 USA300 has rapidly replaced other pulsed- be cured with adequate drainage alone. Nonethe-
field types to become predominant among centers less, when antibiotics are clinically indicated and
that have conducted longitudinal studies.22 Our MRSA is prevalent in the community, it is diffi-
finding of the genetic similarity of MRSA and MSSA cult to justify empirical use of agents known to
isolates from community-associated infections be inactive against MRSA. The susceptibility of a
is consistent with previous reports.7,8,21,23 This given pathogen to prescribed antimicrobial agents
similarity suggests the acquisition of SCCmec by may be more likely to affect the outcome among
S. aureus strains established in the community or patients with cellulitis or purulent wounds. Un-
the loss of SCCmec by community-associated MRSA fortunately, there were insufficient numbers of
strains. The predominance of isolates from one these patients with follow-up information in our
genetic background may be related to virulence or study to assess this relationship. Although we
transmissibility factors that confer unusual fitness. identified several clinical and epidemiologic fac-
Ninety-eight percent of MRSA isolates and tors associated with MRSA infection, it does not
more than 40 percent of MSSA isolates in our appear that the presence or absence of these fac-
study contained pvl genes; these findings are tors would be useful to guide decisions about the
n engl j med 355;7 www.nejm.org august 17, 2006 671
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
use of empirical antibiotics. Most patients with- agent such as vancomycin for MRSA coverage re-
out MRSA had at least one of these factors, and mains appropriate. One study reported that clinda-
almost half of those without any of these factors mycin therapy was successful in children with in-
were found to have MRSA. vasive community-associated MRSA infections.29
Various antimicrobial agents, such as clindamy- In recent randomized clinical trials, newer agents
cin, trimethoprim–sulfamethoxazole, and doxycy- with MRSA activity had efficacy similar (dapto-
cline, have been recommended for outpatient em- mycin and tigecycline) or superior (linezolid) to
pirical treatment of community-associated skin that of vancomycin for the treatment of compli-
and soft-tissue infections that may be attributable cated skin and soft-tissue infections or skin and
to MRSA.28-30 More than 90 percent of MRSA iso- soft-tissue infections associated with MRSA.35-37
lates in our study were susceptible to each of these As compared with patients with other bacte-
agents. Likewise, 100 percent of the MRSA isolates rial infections of the skin, patients with MRSA
were susceptible to rifampin. Although resistance infection were more likely to report a spider bite
to rifampin monotherapy has occurred rapidly, the as the reason for their skin lesion, perhaps be-
combination of rifampin plus trimethoprim–sul- cause of the propensity for MRSA strains circu-
famethoxazole has been shown to eradicate MRSA lating in the community to cause painful lesions
colonization and has been suggested for the treat- in the absence of previous skin trauma. Thus, cli-
ment of MRSA infection in the community.31 Re- nicians should consider the possibility of MRSA
sistance to macrolides and fluoroquinolones was infection in patients who report spider bites. Eigh-
prevalent among MRSA isolates in this and other teen percent of patients with skin and soft-tissue
studies.3,12,13 infections associated with MRSA reported close
Although the prevalence of clindamycin resis- contact with a person who had a similar infection.
tance, including inducible resistance, was low This finding highlights the importance of educat-
overall, it varied geographically. Clindamycin has ing patients about methods to prevent further
been used successfully in the treatment of infec- transmission of infection, including keeping le-
tions with MRSA isolates possessing inducible sions covered with clean, dry bandages; practicing
resistance.29,32 However, clinical treatment failures good hand hygiene; and avoiding the sharing of
have also been reported.33 Therefore, if clindamy- contaminated items.
cin therapy is being considered, S. aureus isolates The high prevalence of MRSA among patients
with the potential for inducible clindamycin re- with community-associated skin and soft-tissue
sistance (i.e., isolates resistant to erythromycin infections has implications for hospital policies
but susceptible to clindamycin on initial testing) regarding infection control. Standard precautions
should be evaluated for inducible resistance by (including the use of gowns and gloves by health
D-zone disk-diffusion testing.17 care workers for contact with wound drainage)
Patients with nonpurulent cellulitis were not should be used for all patients. Contact precau-
included in our study. Previous studies have shown tions, which include the use of gowns and gloves
that a large proportion of cellulitis may be attrib- for all contact with patients or their environment,
utable to group A streptococcus.34 In contrast, have been recommended for patients in acute care
among infections characterized as cellulitis with inpatient facilities who are known to be infected
purulent drainage in our study, MRSA was isolated or colonized with MRSA.38 Our results suggest
from 47 percent and group A streptococcus was that strategies used for patients with confirmed
rarely isolated. Although generally susceptible in MRSA infections should be considered for all pa-
vitro to clindamycin, most group A streptococci tients with purulent skin and soft-tissue infections
are resistant to trimethoprim–sulfamethoxazole. in areas with a high prevalence of MRSA.
To provide coverage for streptococcal infection, the In many U.S. cities, MRSA is now the most
use of clindamycin or a combination of a β-lac- common pathogen isolated in the emergency
tam plus trimethoprim–sulfamethoxazole may be department from patients with skin and soft-tis-
preferable for nonpurulent cellulitis. sue infections. Clinicians should consider obtain-
Optimal empirical therapy for severely ill hos- ing cultures from patients with skin and soft-tis-
pitalized patients with complicated skin and soft- sue infections and modifying standard empirical
tissue infections has not been established; however, therapy to provide MRSA coverage when antibiot-
broad-spectrum intravenous therapy including an ics are indicated. Further studies are needed to
672 n engl j med 355;7 www.nejm.org august 17, 2006
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
mrsa infections among patients in the emergency department
determine the extent of this infection in other lo- ports having received consulting fees from or having served on
advisory boards for Pfizer and Ortho-McNeil; lecture fees from
cations, follow trends in antimicrobial suscepti- Schering-Plough; and research support from Pfizer and Aventis.
bility, and identify optimal therapy. No other potential conflict of interest relevant to this article was
Supported by a cooperative agreement (U50/CCU912342) with reported.
the CDC. We are indebted to Daniel Jernigan, Sigrid McAllister, Jean Pa-
The findings and conclusions of this report are those of the tel, David Lonsway, George Killgore, Brandi Limbago, and Laura
authors and do not necessarily represent the views of the fund- Jevitt at the CDC for providing technical and laboratory assistance;
ing agency. to the following site research coordinators: Ricky Amii, Cynthia
Dr. Moran reports having received consulting fees from or Nguyen, Deborah Sibley, Mehr Merabodi, Carolyn Oakes, Marlena
having served on advisory boards for Schering-Plough and Pfiz- Wald, Tove Ryman, Yvonne Sanchez, Joni Kopitzke, Karen Pfaff,
er; lecture fees from Schering-Plough, Pfizer, Aventis, and Cub- Sara Newton, Mary Mulrow, and Carol Von Hofen; and to the
ist; and research support from Pfizer and Aventis. Dr. Talan re- physicians at our study sites who assisted with data collection.
appendix
The following investigators participated in the EMERGEncy ID Net Study Group: Olive View–University of California at Los Angeles Medical
Center, Sylmar: F.M. Abrahamian; Hennepin County Medical Center, Minneapolis: M. Biros; University of New Mexico Health Sciences Center, Albuquer-
que: P.R. Cheney; Bellevue Hospital Center, New York: W.K. Chiang; Louisiana State University Health Science Center, New Orleans: L.M. Dunbar;
Maricopa Medical Center, Phoenix, Ariz.: E. Gross; Emory University School of Medicine, Atlanta: K.L. Heilpern; Oregon Health Sciences University,
Portland: J. Jui; Temple University School of Medicine, Philadelphia: D.J. Karras; University of Missouri–Kansas City, Kansas City: M.T. Steele; Carolinas
Medical Center, Charlotte, N.C.: M. Sullivan.
References
1. Barrett FF, McGehee RF Jr, Finland M. resistant Staphylococcus aureus carrying the tional supplement. M100-S16. Wayne, Pa.:
Methicillin-resistant Staphylococcus aureus at Panton-Valentine leukocidin genes. Clin Clinical and Laboratory Standards Insti-
Boston City Hospital: bacteriologic and epi- Infect Dis 2005;40:100-7. tute, 2006.
demiologic observations. N Engl J Med 10. Naimi TS, LeDell KH, Como-Sabetti K, 18. Pan ES, Diep BA, Charlebois ED, et al.
1968;279:441-8. et al. Comparison of community- and Population dynamics of nasal strains of
2. Herold BC, Immergluck LC, Maranan health care-associated methicillin-resis- methicillin-resistant Staphylococcus aureus
MC, et al. Community-acquired methicil- tant Staphylococcus aureus infection. JAMA — and their relation to community-asso-
lin-resistant Staphylococcus aureus in children 2003;290:2976-84. ciated disease activity. J Infect Dis 2005;
with no identified predisposing risk. JAMA 11. McDougal LK, Steward CD, Killgore 192:811-8.
1998;279:593-8. GE, Chaitram JM, McAllister SK, Tenover 19. Daum RS, Ito T, Hiramatsu K, et al.
3. Fridkin SK, Hageman JC, Morrison M, FC. Pulsed-field gel electrophoresis typ- A novel methicillin-resistance cassette in
et al. Methicillin-resistant Staphylococcus au- ing of oxacillin-resistant Staphylococcus au- community-acquired methicillin-resistant
reus disease in three communities. N Engl reus isolates from the United States: estab- Staphylococcus aureus isolates of diverse ge-
J Med 2005;352:1436-44. [Erratum, N Engl lishing a national database. J Clin Microbiol netic backgrounds. J Infect Dis 2002;186:
J Med 2005;352:2362.] 2003;41:5113-20. 1344-7.
4. Outbreaks of community-associated 12. Frazee BW, Lynn J, Charlebois ED, 20. Naimi TS, LeDell KH, Boxrud DJ, et
methicillin-resistant Staphylococcus aureus Lambert L, Lowery D, Perdreau-Reming- al. Epidemiology and clonality of commu-
skin infections — Los Angeles County, ton F. High prevalence of methicillin- nity-acquired methicillin-resistant Staphy-
California, 2002–2003. MMWR Morb Mor- resistant Staphylococcus aureus in emergency lococcus aureus in Minnesota, 1996-1998. Clin
tal Wkly Rep 2003;52:88. department skin and soft tissue infec- Infect Dis 2001;33:990-6.
5. Kazakova SV, Hageman JC, Matava M, tions. Ann Emerg Med 2005;45:311-20. 21. Mishaan AM, Mason EO Jr, Martinez-
et al. A clone of methicillin-resistant Staph- 13. Moran GJ, Amii RN, Abrahamian FM, Aguilar G, et al. Emergence of a predomi-
ylococcus aureus among professional foot- Talan DA. Methicillin-resistant Staphylo- nant clone of community-acquired Staphy-
ball players. N Engl J Med 2005;352:468- coccus aureus in community-acquired skin lococcus aureus among children in Houston,
75. infections. Emerg Infect Dis 2005;11:928- Texas. Pediatr Infect Dis J 2005;24:201-6.
6. Zinderman CE, Conner B, Malakooti 30. 22. Chavez-Bueno S, Bozdogan B, Katz K,
MA, LaMar JE, Armstrong A, Bohnker BK. 14. Talan DA, Moran GJ, Mower W, et al. et al. Inducible clindamycin resistance and
Community-acquired methicillin-resistant EMERGEncy ID NET: an emergency de- molecular epidemiologic trends of pedi-
Staphylococcus aureus among military re- partment-based emerging infections sen- atric community-acquired methicillin-
cruits. Emerg Infect Dis 2004;10:941-4. tinel network. Ann Emerg Med 1998;32: resistant Staphylococcus aureus in Dallas, Tex-
7. Gonzalez BE, Martinez-Aguilar G, 703-11. as. Antimicrob Agents Chemother 2005;
Hulten KG, et al. Severe staphylococcal sep- 15. Bannerman TL. Staphylococci and 49:2283-8.
sis in adolescents in the era of community- other catalase positive cocci that grow 23. Adem PV, Montgomery CP, Husain
acquired methicillin-resistant Staphylococcus aerobically. In: Murray PR, Baron EJ, Jo- AN, et al. Staphylococcus aureus sepsis and
aureus. Pediatrics 2005;115:642-8. gensen JH, eds. Manual of clinical micro- the Waterhouse–Friderichsen syndrome in
8. Mongkolrattanothai K, Boyle S, Kahana biology. 8th ed. Washington, D.C.: ASM children. N Engl J Med 2005;353:1245-51.
MD, Daum RS. Severe Staphylococcus aureus Press, 2003:384-404. 24. Yamasaki O, Kaneko J, Morizane S, et
infections caused by clonally related com- 16. Performance standards for antimicro- al. The association between Staphylococcus
munity-acquired methicillin-susceptible bial susceptibility testing: 14th informa- aureus strains carrying Panton-Valentine
and methicillin-resistant isolates. Clin In- tional supplement. M1000-S14. Wayne, leukocidin genes and the development of
fect Dis 2003;37:1050-8. Pa.: National Committee for Clinical Lab- deep-seated follicular infection. Clin In-
9. Francis JS, Doherty MC, Lopatin U, et oratory Standards, 2004. fect Dis 2005;40:381-5.
al. Severe community-onset pneumonia 17. Performance standards for antimicro- 25. Issartel B, Tristan A, Lechevallier S, et
in healthy adults caused by methicillin- bial susceptibility testing: 16th informa- al. Frequent carriage of Panton-Valentine
n engl j med 355;7 www.nejm.org august 17, 2006 673
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
mrsa infections among patients in the emergency department
leucocidin genes by Staphylococcus aureus coccus aureus in children. Pediatr Infect Dis lulitis in adults: a microbiologic study us-
isolates from surgically drained abscess- J 2003;22:593-8. ing a direct immunofluorescence tech-
es. J Clin Microbiol 2005;43:3203-7. 30. Rybak MJ, LaPlante KL. Community- nique. Arch Dermatol 1989;125:779-82.
26. Lina G, Piemont Y, Godail-Gamot F, associated methicillin-resistant Staphylococ- 35. Weigelt J, Itani K, Stevens D, et al. Li-
et al. Involvement of Panton-Valentine cus aureus: a review. Pharmacotherapy 2005; nezolid versus vancomycin in treatment
leukocidin-producing Staphylococcus aureus 25:74-85. of complicated skin and soft tissue infec-
in primary skin infections and pneumo- 31. Chambers HF. Treatment of infection tions. Antimicrob Agents Chemother 2005;
nia. Clin Infect Dis 1999;29:1128-32. and colonization caused by methicillin- 49:2260-6.
27. Lee MC, Rios AM, Aten MF, et al. resistant Staphylococcus aureus. Infect Con- 36. Carpenter CF, Chambers HF. Dapto-
Management and outcome of children trol Hosp Epidemiol 1991;12:29-35. mycin: another novel agent for treating
with skin and soft tissue abscesses caused 32. Drinkovic D, Fuller ER, Shore KP, infections due to drug-resistant gram-pos-
by community-acquired methicillin-resis- Holland DJ, Ellis-Pegler R. Clindamycin itive pathogens. Clin Infect Dis 2004;38:
tant Staphylococcus aureus. Pediatr Infect treatment of Staphylococcus aureus express- 994-1000.
Dis J 2004;23:123-7. ing inducible clindamycin resistance. J An- 37. Nathwani D. Tigecycline: clinical evi-
28. Kaplan SL. Treatment of community- timicrob Chemother 2001;48:315-6. dence and formulary positioning. Int J An-
associated methicillin-resistant Staphylo- 33. Siberry GK, Tekle T, Carroll K, Dick J. timicrob Agents 2005;25:185-92.
coccus aureus infections. Pediatr Infect Dis J Failure of clindamycin treatment of meth- 38. Garner JS. Guidelines for isolation pre-
2005;24:457-8. icillin-resistant Staphylococcus aureus ex- cautions in hospitals. Part I. Evolution of
29. Martinez-Aguilar G, Hammerman pressing inducible clindamycin resistance isolation practices. Am J Infect Control
WA, Mason EO Jr, Kaplan SL. Clindamy- in vitro. Clin Infect Dis 2003;37:1257-60. 1996;24:24-31.
cin treatment of invasive infections caused 34. Bernard P, Bedane C, Mounier M, De- Copyright © 2006 Massachusetts Medical Society.
by community-acquired, methicillin-resis- nis F, Catanzano G, Bonnetblanc JM.
tant and methicillin-susceptible Staphylo- Streptococcal cause of erysipelas and cel-
PERSONAL ARCHIVES IN THE JOURNAL ONLINE
Individual subscribers can store articles and searches using a feature
on the Journal’s Web site (www.nejm.org) called “Personal Archive.”
Each article and search result links to this feature. Users can create
personal folders and move articles into them for convenient retrieval later.
674 n engl j med 355;7 www.nejm.org august 17, 2006
The New England Journal of Medicine
Downloaded from nejm.org on May 18, 2020. For personal use only. No other uses without permission.
Copyright © 2006 Massachusetts Medical Society. All rights reserved.
You might also like
- A Model of The Effects of Colonialism - DR Michael Yellow BirdDocument2 pagesA Model of The Effects of Colonialism - DR Michael Yellow Birdhuehue2100% (1)
- Fingerprint Mock Crime Scene Birch2015Document10 pagesFingerprint Mock Crime Scene Birch2015api-281965445No ratings yet
- 5.4 Risk Factors For MRSA ColonizationDocument8 pages5.4 Risk Factors For MRSA ColonizationQworldNo ratings yet
- 10Document10 pages10duarte.pheNo ratings yet
- Methicillin-Resistant Staphylococcus Aureus in NepDocument5 pagesMethicillin-Resistant Staphylococcus Aureus in NepHafiza AyeshaNo ratings yet
- Effectiveness of Contact Isolation During A Hospital Outbreak of Methicillin-Resistant Staphylococcus AureusDocument9 pagesEffectiveness of Contact Isolation During A Hospital Outbreak of Methicillin-Resistant Staphylococcus Aureusmoniart2587No ratings yet
- Community Acquired Mrsa: Pisespong Patamasucon, M.D. Pediatric Infectious Disease UNSOM - Las VegasDocument48 pagesCommunity Acquired Mrsa: Pisespong Patamasucon, M.D. Pediatric Infectious Disease UNSOM - Las VegasRashed NazzalNo ratings yet
- Risk Factor For MRSA in Skin, Soft Tissue and Bone Infection in The Foot and Leg in California Community HospitalDocument11 pagesRisk Factor For MRSA in Skin, Soft Tissue and Bone Infection in The Foot and Leg in California Community HospitalReza Suryapandu NugrohoNo ratings yet
- Mssa 2011 PDFDocument8 pagesMssa 2011 PDFBebenzzzNo ratings yet
- MRSA Nosocomial Infection BacteryDocument6 pagesMRSA Nosocomial Infection BacteryZUKHRUFIA ISNA PRAMADEWINo ratings yet
- HTTPSWWW - Ncbi.nlm - nih.GovpmcarticlesPMC9024581pdfjcdd 09 00103 PDFDocument13 pagesHTTPSWWW - Ncbi.nlm - nih.GovpmcarticlesPMC9024581pdfjcdd 09 00103 PDFreza fahleviNo ratings yet
- MrsaDocument10 pagesMrsazia ul RahmanNo ratings yet
- Skin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusDocument11 pagesSkin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusFerdy RamadhanNo ratings yet
- Update On Antifungal Resistance - TimiDocument4 pagesUpdate On Antifungal Resistance - Timix994thng65No ratings yet
- Journal of Clinical Immunology and MicrobiologyDocument10 pagesJournal of Clinical Immunology and MicrobiologyAthenaeum Scientific PublishersNo ratings yet
- A Hospital Based Prospective Study of Prevalence of Methicillin Resistant Staphylococcus Aureus in Dermatology Indoor Patients by Phenotypic MethodDocument9 pagesA Hospital Based Prospective Study of Prevalence of Methicillin Resistant Staphylococcus Aureus in Dermatology Indoor Patients by Phenotypic MethodIJAR JOURNALNo ratings yet
- MRSA Skin and Soft Tissue InfectionsDocument5 pagesMRSA Skin and Soft Tissue Infectionsapi-3801331No ratings yet
- 1 s2.0 S1201971209000435 MainDocument7 pages1 s2.0 S1201971209000435 MainGopalaKrishnanNo ratings yet
- Life 13 01126Document14 pagesLife 13 01126s4cdbv4xjrNo ratings yet
- Surgical Site Infection in A Teaching Hospital: A Prospective StudyDocument7 pagesSurgical Site Infection in A Teaching Hospital: A Prospective StudymajedNo ratings yet
- 05 N312 18329Document9 pages05 N312 18329GinshaNo ratings yet
- JCDR 7 1339Document4 pagesJCDR 7 1339RahayuNo ratings yet
- Due To Two Methicillin-Resistant Widespread Skin and Soft-Tissue InfectionsDocument7 pagesDue To Two Methicillin-Resistant Widespread Skin and Soft-Tissue Infectionschilvys04No ratings yet
- Bacterial Skin and Soft Tissue Infections: Clinical Review ArticleDocument9 pagesBacterial Skin and Soft Tissue Infections: Clinical Review ArticleRini MayaSariNo ratings yet
- Antibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHDocument5 pagesAntibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHzia ul RahmanNo ratings yet
- Prevalence of CA MRSA Nasal Carriage Among Children of ConsultationDocument6 pagesPrevalence of CA MRSA Nasal Carriage Among Children of ConsultationGoGoPenguinVALNo ratings yet
- MRSADocument6 pagesMRSAIgnacio Velasquez MiñoNo ratings yet
- Staphylococcus Aureus in Neonatal: Methicillin-Resistant Intensive Care UnitDocument4 pagesStaphylococcus Aureus in Neonatal: Methicillin-Resistant Intensive Care UnitAulina Refri RahmiNo ratings yet
- Rab 9Document12 pagesRab 9Belia DestamaNo ratings yet
- Molecular EpidemiologyDocument11 pagesMolecular EpidemiologymotibaNo ratings yet
- Methicillin Resistant Staphylococcus Aureus (MRSA) in The Intensive Care UnitDocument8 pagesMethicillin Resistant Staphylococcus Aureus (MRSA) in The Intensive Care UnitMuhammad AliNo ratings yet
- Epidemiology and Clinical Manifestations of Mucormycosis CMIDocument9 pagesEpidemiology and Clinical Manifestations of Mucormycosis CMIDINESH VENKATESANNo ratings yet
- Methicillinresistant Staphylococcus Aureus A Mini ReviewDocument6 pagesMethicillinresistant Staphylococcus Aureus A Mini ReviewSandhi WiryaNo ratings yet
- Mrsa101 508Document45 pagesMrsa101 508Sam TullyNo ratings yet
- 1 - Name of The Candidate and AddressDocument19 pages1 - Name of The Candidate and AddressRini ThomasNo ratings yet
- Sphingomonas KoreensisDocument11 pagesSphingomonas KoreensisSMIBA MedicinaNo ratings yet
- Transferable Vancomycin Resistance in A Community-Associated MRSA LineageDocument8 pagesTransferable Vancomycin Resistance in A Community-Associated MRSA LineageMabel StracciaNo ratings yet
- Epidemiology Roun1Document10 pagesEpidemiology Roun1FebniNo ratings yet
- Methicillin-Resistant Staphylococcus Tuberculosis: Part 1: Aureus and Multidrug ResistantDocument3 pagesMethicillin-Resistant Staphylococcus Tuberculosis: Part 1: Aureus and Multidrug ResistantSukma EffendyNo ratings yet
- Research Paper On MrsaDocument4 pagesResearch Paper On Mrsam0d1p1fuwub2100% (1)
- IJMLR231704Document7 pagesIJMLR231704sandeep raiNo ratings yet
- PMID 36974854 OpportunisticDocument8 pagesPMID 36974854 Opportunisticajaya basnetNo ratings yet
- Free Research Papers On MrsaDocument8 pagesFree Research Papers On Mrsaafnhbijlzdufjj100% (1)
- Miller 2016Document4 pagesMiller 2016Lidia JimenezNo ratings yet
- Current Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusDocument15 pagesCurrent Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusSeptiani HasibuanNo ratings yet
- Jamainternal Jones 2020 Oi 190118-4Document9 pagesJamainternal Jones 2020 Oi 190118-4LuthfiNo ratings yet
- 1 s2.0 S0002934322007227 MainDocument8 pages1 s2.0 S0002934322007227 MainMaryatiNo ratings yet
- Measles Outbreak NejmoaDocument12 pagesMeasles Outbreak NejmoaVlad ManoleNo ratings yet
- Gill Et Al 2005 Insights On Evolution of Virulence and Resistance From The Complete Genome Analysis of An EarlyDocument13 pagesGill Et Al 2005 Insights On Evolution of Virulence and Resistance From The Complete Genome Analysis of An EarlyNora LeeNo ratings yet
- Artigo C Neoformans PDFDocument29 pagesArtigo C Neoformans PDFJorge Luis CarmoNo ratings yet
- Children and MRSADocument6 pagesChildren and MRSAcharanmann9165No ratings yet
- Lander 2016Document2 pagesLander 2016Jocilene Dantas Torres NascimentoNo ratings yet
- A Measles Outbreak in An Underimmunized Amish Community in OhioDocument12 pagesA Measles Outbreak in An Underimmunized Amish Community in Ohiomuhammad maadaNo ratings yet
- Clinical Microbiology and InfectionDocument9 pagesClinical Microbiology and InfectionAguilarKrystell'No ratings yet
- The Foot: Original ArticleDocument5 pagesThe Foot: Original ArticleKarinaayu SerinNo ratings yet
- A 10-Year Review of Ocular Methicillin-Resistant Staphylococcus Aureus InfectionsDocument6 pagesA 10-Year Review of Ocular Methicillin-Resistant Staphylococcus Aureus InfectionsBima RizkiNo ratings yet
- Meticillin Resistant - Staphylococcus - Aure20160520 7685 19p6anl With Cover Page v2Document11 pagesMeticillin Resistant - Staphylococcus - Aure20160520 7685 19p6anl With Cover Page v2Delvita ElyasNo ratings yet
- 1000 Genomas RusiaDocument9 pages1000 Genomas RusiaDamarisNo ratings yet
- Journal of Clinical Immunology & MicrobiologyDocument9 pagesJournal of Clinical Immunology & MicrobiologyAthenaeum Scientific PublishersNo ratings yet
- Species Identification and Antifungal Susceptibility of Uncommon Blood Yeast IsolatesDocument8 pagesSpecies Identification and Antifungal Susceptibility of Uncommon Blood Yeast Isolatesa.rahadianNo ratings yet
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementFrom EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouNo ratings yet
- Roadmap For Bible StudyDocument1 pageRoadmap For Bible Study4gen_3No ratings yet
- Cobb 500Document16 pagesCobb 500scribeascrapNo ratings yet
- Geographical Indication (DARJEELING TEA REPORT)Document8 pagesGeographical Indication (DARJEELING TEA REPORT)srksamNo ratings yet
- MS Access - Working With QueriesDocument69 pagesMS Access - Working With QueriesbogsbestNo ratings yet
- Chapter 1 TVTDocument14 pagesChapter 1 TVTtemedebereNo ratings yet
- The A To Z List of Reflexology Research3Document110 pagesThe A To Z List of Reflexology Research3Ahmad Saiful Ridzwan JaharuddinNo ratings yet
- Nolasco Labor I CompilationDocument115 pagesNolasco Labor I CompilationNico QuebalNo ratings yet
- Low Sperm Count and Its Homeopathic Cure - DR Bashir Mahmud ElliasDocument9 pagesLow Sperm Count and Its Homeopathic Cure - DR Bashir Mahmud ElliasBashir Mahmud ElliasNo ratings yet
- Intermediate Accounting - Kieso - Chapter 1Document46 pagesIntermediate Accounting - Kieso - Chapter 1Steffy AmoryNo ratings yet
- Lecture 01 - Construction EngineeringDocument18 pagesLecture 01 - Construction EngineeringKw TseNo ratings yet
- Towards A Radical RizalDocument34 pagesTowards A Radical RizalBryle CamaroteNo ratings yet
- The Swadeshi MovementDocument17 pagesThe Swadeshi Movementbharathkarna97No ratings yet
- Pedal Operated Washing Machine ReportDocument35 pagesPedal Operated Washing Machine ReportJack Johnson100% (1)
- Fluid Machines Lecture Notes CH-4-Centrifugal CompressorDocument21 pagesFluid Machines Lecture Notes CH-4-Centrifugal CompressorBINNo ratings yet
- "You Shall Not Take The Name of The Lord Your God in Vain": Anger Coarse Vulgar Speech, ProfanityDocument10 pages"You Shall Not Take The Name of The Lord Your God in Vain": Anger Coarse Vulgar Speech, ProfanityMarvin MonterosoNo ratings yet
- First Class Dhanbad 2012Document4 pagesFirst Class Dhanbad 2012ihateu1No ratings yet
- Manila Standard Today - Friday (November 23, 2012) IssueDocument28 pagesManila Standard Today - Friday (November 23, 2012) IssueManila Standard TodayNo ratings yet
- Upload 9Document3 pagesUpload 9Meghna CmNo ratings yet
- Basic Labor and Employment Education CourseDocument9 pagesBasic Labor and Employment Education CourseJennifer Tan Marcial100% (2)
- 2008olbrycht Alex OpisDocument23 pages2008olbrycht Alex OpisHamid Reza SorouriNo ratings yet
- Rundown Acara WorkshopDocument6 pagesRundown Acara WorkshopAnnas Nuraini br gintingNo ratings yet
- BIG-IP CGNAT ImplementationsDocument208 pagesBIG-IP CGNAT ImplementationsThiago CabralNo ratings yet
- The Gorgon's HeadDocument3 pagesThe Gorgon's HeadReden Macaraeg Juego100% (1)
- Thesis in Teaching English As Foreign LanguageDocument8 pagesThesis in Teaching English As Foreign Languagereneedelgadoalbuquerque100% (2)
- AWHERO - Military Applications Brochure - Gen2020Document4 pagesAWHERO - Military Applications Brochure - Gen2020زين الدين مروانيNo ratings yet
- Physics (From: Physik (Epist Mē)Document1 pagePhysics (From: Physik (Epist Mē)annmarieNo ratings yet
- United States v. Castillo Moronta, 27 F.3d 554, 1st Cir. (1994)Document3 pagesUnited States v. Castillo Moronta, 27 F.3d 554, 1st Cir. (1994)Scribd Government DocsNo ratings yet
- Sop QubDocument2 pagesSop QubAMRUD GAMINGNo ratings yet