Professional Documents
Culture Documents
Risk Factors of Acute Otitis Externa Seen in Patie
Risk Factors of Acute Otitis Externa Seen in Patie
Uploaded by
Suwandi WandiCopyright:
Available Formats
You might also like
- CPG On CsomDocument8 pagesCPG On CsomRobert Ross DulayNo ratings yet
- Chronic Suppurative Otitis Media in AdultsDocument10 pagesChronic Suppurative Otitis Media in AdultsRstadam TagalogNo ratings yet
- Case Study BlepharitisDocument12 pagesCase Study BlepharitisNorshahidah IedaNo ratings yet
- The Most Common Causes of Bacterial Ear InfectionsDocument6 pagesThe Most Common Causes of Bacterial Ear InfectionsCentral Asian StudiesNo ratings yet
- Head and Neck AbsesDocument8 pagesHead and Neck AbsesNandaNo ratings yet
- Aerobic Bacteria Associated With Chronic Suppurative Otitis Media in AngolaDocument10 pagesAerobic Bacteria Associated With Chronic Suppurative Otitis Media in AngolaRawcath DOOMNo ratings yet
- Research: Pattern of Otitis Externa in Kaduna NigeriaDocument4 pagesResearch: Pattern of Otitis Externa in Kaduna NigeriaRicky AmeNo ratings yet
- A Prospective Study of Seven Patients With Chronic MastoiditisDocument5 pagesA Prospective Study of Seven Patients With Chronic MastoiditisarioNo ratings yet
- To Determine The Symptoms, Predisposing Factors and Causative Organisms of OtomycosisDocument3 pagesTo Determine The Symptoms, Predisposing Factors and Causative Organisms of OtomycosisAnonymous lAfk9gNPNo ratings yet
- d098 PDFDocument7 pagesd098 PDFMayiz Renata LimerseNo ratings yet
- Tonsillitis and Their Complications: Epidemiological, Clinical and Therapeutic ProfilesDocument8 pagesTonsillitis and Their Complications: Epidemiological, Clinical and Therapeutic ProfilesMarsya Yulinesia LoppiesNo ratings yet
- 6-7 Omsk MalignaDocument2 pages6-7 Omsk MalignaAlvina Ulfah RusmayuniNo ratings yet
- Recent Advancements in Management of Alveolar Osteitis (Dry Socket)Document5 pagesRecent Advancements in Management of Alveolar Osteitis (Dry Socket)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Otitis Externa: Investigation and Evidence-Based TreatmentDocument45 pagesOtitis Externa: Investigation and Evidence-Based TreatmentSonya HyekyoNo ratings yet
- EtiologiDocument8 pagesEtiologiRizka AmeliaNo ratings yet
- Acute Otitis Externa:Pathophysiology, Clinicalpresentation, and TreatmentDocument6 pagesAcute Otitis Externa:Pathophysiology, Clinicalpresentation, and TreatmentIOSRjournalNo ratings yet
- Murray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryDocument17 pagesMurray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryAndi Karwana CiptaNo ratings yet
- Odontogenic Infections: Etiology and Management: Ahmed J. Al-Naqeeb and Hala J. M. Al-Naqeeb ANB. MED. J. 15 (1), 2019Document4 pagesOdontogenic Infections: Etiology and Management: Ahmed J. Al-Naqeeb and Hala J. M. Al-Naqeeb ANB. MED. J. 15 (1), 2019lee zaraNo ratings yet
- SJAMS 66 2563 2566 C PDFDocument4 pagesSJAMS 66 2563 2566 C PDFVitta Kusma WijayaNo ratings yet
- 443 1871 1 PBDocument6 pages443 1871 1 PBRetno arunNo ratings yet
- Entamoeba Gingivalis and Trichomonas Tenax In: Periodontal DiseaseDocument12 pagesEntamoeba Gingivalis and Trichomonas Tenax In: Periodontal Diseasefadhilah RizkiyahNo ratings yet
- Effectiveness of Ciprofloxacin in The Treatment of Acute Otitis Media (#978213) - 1906643Document4 pagesEffectiveness of Ciprofloxacin in The Treatment of Acute Otitis Media (#978213) - 1906643Dinda NovitaNo ratings yet
- Pediatric ENT EmergenciesDocument20 pagesPediatric ENT EmergenciesAiri FirdausiaNo ratings yet
- Jurnal OtomikosissDocument7 pagesJurnal Otomikosissrahmy kubangunNo ratings yet
- Am J Otolaryngol: COVID-19 and Hearing DifficultiesDocument2 pagesAm J Otolaryngol: COVID-19 and Hearing DifficultiesDhyo Asy-shidiq HasNo ratings yet
- Current Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaDocument10 pagesCurrent Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaFrancis RomanosNo ratings yet
- COVID 19 and Dentistry A PerspectiveDocument12 pagesCOVID 19 and Dentistry A PerspectiveAthenaeum Scientific PublishersNo ratings yet
- Cervicofacial InfectionsDocument6 pagesCervicofacial InfectionsAngélica Valenzuela AndrighiNo ratings yet
- 3612 6812 1 SMDocument9 pages3612 6812 1 SMRizky Agustian HadiNo ratings yet
- A Study On Deep Neck Space InfectionsDocument6 pagesA Study On Deep Neck Space InfectionsbebetteryesyoucanNo ratings yet
- Microbial Profile and Patients of Chronic Suppurative Otitis Media in Latur, Maharashtra, IndiaDocument4 pagesMicrobial Profile and Patients of Chronic Suppurative Otitis Media in Latur, Maharashtra, IndiaiisisiisNo ratings yet
- Otomycosis in Relation To Csom: Gujarat Journal of Otorhinolaryngology and Head and Neck Surgery January 2011Document4 pagesOtomycosis in Relation To Csom: Gujarat Journal of Otorhinolaryngology and Head and Neck Surgery January 2011Shovie Thalia MirandaNo ratings yet
- OMSKDocument4 pagesOMSKYusnida RahmawatiNo ratings yet
- Jurnal Otitis Eksterna WordDocument14 pagesJurnal Otitis Eksterna WordmedyaanaNo ratings yet
- Mastoiditis in Childhood: Review of The LiteratureDocument6 pagesMastoiditis in Childhood: Review of The LiteratureElysabeth MargarethaNo ratings yet
- Severe Intracranial and Extracranial Complications of The Middle Ear Cholesteatoma A Report CaseDocument5 pagesSevere Intracranial and Extracranial Complications of The Middle Ear Cholesteatoma A Report CaseChoirul UmamNo ratings yet
- Otitis ExternaDocument4 pagesOtitis ExternaCesar Mauricio Daza CajasNo ratings yet
- Xu 2020Document6 pagesXu 2020Cintya RambuNo ratings yet
- Laura A Goguen, MD Daniel G Deschler, MD, FACS Morven S Edwards, MD Howard Libman, MD Contributor Disclosures Peer Review ProcessDocument4 pagesLaura A Goguen, MD Daniel G Deschler, MD, FACS Morven S Edwards, MD Howard Libman, MD Contributor Disclosures Peer Review ProcessDaniela Chavez DiazNo ratings yet
- Jurnal 1Document5 pagesJurnal 1Lian Tolombot LambeyNo ratings yet
- Jurnal 2Document11 pagesJurnal 2Ainun Jariah FahayNo ratings yet
- ADJ-odontogenic InfectionDocument9 pagesADJ-odontogenic Infectiondr.chidambra.kapoorNo ratings yet
- Presentation of Thesis JEWELDocument165 pagesPresentation of Thesis JEWELMuhammad AbdulWahidKarim MusafirNo ratings yet
- Ns. Heni Kusumawati M.Kep - EFFECT OF DEBRIDEMENT ON MANDIBULA ABSCESS PATIENTS CASE STUDYDocument8 pagesNs. Heni Kusumawati M.Kep - EFFECT OF DEBRIDEMENT ON MANDIBULA ABSCESS PATIENTS CASE STUDYcandra kusumaNo ratings yet
- Management of Odontogenic Infection of Primary Teeth in Child That Extends To The Submandibular and Submental Space Case ReportDocument5 pagesManagement of Odontogenic Infection of Primary Teeth in Child That Extends To The Submandibular and Submental Space Case ReportMel FANo ratings yet
- Incidence of Bacterial Flora Associated With Earphones Used Among Students of Saveetha Medical College and Hospital, Chennai, TamilnaduDocument5 pagesIncidence of Bacterial Flora Associated With Earphones Used Among Students of Saveetha Medical College and Hospital, Chennai, TamilnaduAnonymous lAfk9gNPNo ratings yet
- Odontogenic Infections PDFDocument50 pagesOdontogenic Infections PDFGiannisa Fathina FairuzNo ratings yet
- Microbial Etiology of Acute Otitis Externa - A One Year StudyDocument5 pagesMicrobial Etiology of Acute Otitis Externa - A One Year StudyGading AuroraNo ratings yet
- Access From The University of Nottingham Repository:: For More Information, Please ContactDocument11 pagesAccess From The University of Nottingham Repository:: For More Information, Please ContactsolidtapeNo ratings yet
- 2008-0510 - Otitis Eksterna (Diffusa) PDFDocument14 pages2008-0510 - Otitis Eksterna (Diffusa) PDFEka 'Percival' AnggrainiNo ratings yet
- Epidemiology and Pathogenesis of Chronic Suppurative Otitis Media: Implications For Prevention and TreatmentDocument17 pagesEpidemiology and Pathogenesis of Chronic Suppurative Otitis Media: Implications For Prevention and TreatmentAngge TumimomorNo ratings yet
- Current Concepts in The Pathogenesis and Treatment of Chronic Suppurative Otitis Media - PMCDocument26 pagesCurrent Concepts in The Pathogenesis and Treatment of Chronic Suppurative Otitis Media - PMCDanny. JayNo ratings yet
- IFEA IES Endodontic and Dental Practice During COVID-19Document24 pagesIFEA IES Endodontic and Dental Practice During COVID-19Mohammed TarekNo ratings yet
- Jurnal Ulkus KorneaDocument10 pagesJurnal Ulkus KorneaPutri Dery CahyaniNo ratings yet
- 1 PBDocument11 pages1 PBDesy FatmawatiNo ratings yet
- Researcharticle Open Access: BackgroundDocument4 pagesResearcharticle Open Access: BackgroundMagfira Al HabsyiNo ratings yet
- A Clinical Study of Otomycosis: H.S. Satish, Viswanatha.B, Manjuladevi.MDocument6 pagesA Clinical Study of Otomycosis: H.S. Satish, Viswanatha.B, Manjuladevi.MKepompong KupukupuNo ratings yet
- Microbial Pattern and Sensitivity Analysis of OtitDocument9 pagesMicrobial Pattern and Sensitivity Analysis of Otitmax terowNo ratings yet
- Karakteristik Kasus Otitis Eksterna Di RSUP Sanglah Denpasar Periode April 2015-April 2016Document4 pagesKarakteristik Kasus Otitis Eksterna Di RSUP Sanglah Denpasar Periode April 2015-April 2016xzcvvvvNo ratings yet
- Noma Cancrum OrisDocument4 pagesNoma Cancrum OrisAnonymous Syjpyt4MoNo ratings yet
- Birth StoryDocument7 pagesBirth StoryKaty Whipple100% (1)
- TM Housekeeping NciiDocument140 pagesTM Housekeeping NciiJane DagpinNo ratings yet
- VentolinDocument13 pagesVentolinFitrah NstNo ratings yet
- PCPDocument19 pagesPCPJafer DetamoNo ratings yet
- People Should Avoid Junk FoodsDocument4 pagesPeople Should Avoid Junk FoodsShireen BatoolNo ratings yet
- SuboxonecenterbriefDocument5 pagesSuboxonecenterbriefapi-314460549No ratings yet
- Employee Health and Safety of BPCLDocument4 pagesEmployee Health and Safety of BPCLpooji25No ratings yet
- Code Blue Policy - Adult Care Sites - Calgary ZoneDocument9 pagesCode Blue Policy - Adult Care Sites - Calgary ZoneLLyreONo ratings yet
- Janitorial ProductivityDocument7 pagesJanitorial ProductivityThe Cleaning LibraryNo ratings yet
- Adriene Vialpando: ExperienceDocument3 pagesAdriene Vialpando: ExperienceKritika NigamNo ratings yet
- Macro Analysis PhilippinesDocument9 pagesMacro Analysis PhilippinesAnthony AlferesNo ratings yet
- 01 Manajemen Risiko Klinik (MRK)Document32 pages01 Manajemen Risiko Klinik (MRK)irmaNo ratings yet
- KasaiDocument7 pagesKasaishalukiriNo ratings yet
- Critical Appraisal Checklist For An Article OnDocument4 pagesCritical Appraisal Checklist For An Article OnTiaz DiniutamiNo ratings yet
- Exercise Prescription - OCT 17 ABATONDocument92 pagesExercise Prescription - OCT 17 ABATONReignerPaulVillacortaDavidNo ratings yet
- An Exploratory Study To Assess The Academic Stress, Stress Reactions and Coping Strategies Among The B.Sc. Nursing 1st Year Students in Selected Colleges of Moga, PunjabDocument4 pagesAn Exploratory Study To Assess The Academic Stress, Stress Reactions and Coping Strategies Among The B.Sc. Nursing 1st Year Students in Selected Colleges of Moga, PunjabEditor IJTSRDNo ratings yet
- Chapter-Ii Review of LiteratureDocument8 pagesChapter-Ii Review of LiteratureANU GRAPHICSNo ratings yet
- Chronic MeningitisDocument7 pagesChronic Meningitisneurojuancarfab100% (1)
- Factors That Affect Physical DevelopmentDocument4 pagesFactors That Affect Physical DevelopmentmomuNo ratings yet
- SCIDDocument10 pagesSCIDIbrahimNo ratings yet
- SPC HIRADC - 022 - Road WorksDocument5 pagesSPC HIRADC - 022 - Road WorksKalai ArasanNo ratings yet
- 2021 DPharm - Clinical InkDocument8 pages2021 DPharm - Clinical InkEd SeguineNo ratings yet
- This Is A Awarreness Poster Made by Harsh Vagal About The Eating Disorders Namely Bulimia/anorexia Nervosa and ObesityDocument2 pagesThis Is A Awarreness Poster Made by Harsh Vagal About The Eating Disorders Namely Bulimia/anorexia Nervosa and ObesityHarsh VagalNo ratings yet
- How Can You Help Your Patients With An Uncomplicated UTI?: Know?Document1 pageHow Can You Help Your Patients With An Uncomplicated UTI?: Know?gegeNo ratings yet
- Poverty and Health Teacher's Guide: TopicsDocument42 pagesPoverty and Health Teacher's Guide: TopicsxzqpxzNo ratings yet
- Asian Pacific ScientistsDocument28 pagesAsian Pacific ScientistsMahmood SanglayNo ratings yet
- Pedia ReviewDocument22 pagesPedia ReviewDebbie LanceroNo ratings yet
- PIIS019096222032288XDocument39 pagesPIIS019096222032288XMarlina watiNo ratings yet
- Park Design Guidelines PDFDocument84 pagesPark Design Guidelines PDFmaisarahwderamanNo ratings yet
Risk Factors of Acute Otitis Externa Seen in Patie
Risk Factors of Acute Otitis Externa Seen in Patie
Uploaded by
Suwandi WandiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Risk Factors of Acute Otitis Externa Seen in Patie
Risk Factors of Acute Otitis Externa Seen in Patie
Uploaded by
Suwandi WandiCopyright:
Available Formats
[Downloaded free from http://www.smjonline.org on Thursday, October 20, 2016, IP: 90.206.78.
193]
Original Article
Risk factors of acute otitis externa seen in
patients in a Nigerian tertiary institution
Mohammed Abdullahi, D. Aliyu
Department of Otorhinolaryngology, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
A B S T R A C T
Background: Acute otitis externa is a common clinical problem which is associated with preventable risk factors. Objective: The
aim of this study is to determine the practices that are risk factors in patients with acute otitis externa in a Nigerian tertiary institution.
Patients and Methods: This was a 6‑month cross‑sectional study of patients with acute otitis externa carried out between April
and September 2013 at the Ear, Nose, and Throat Clinic of the Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria.
Results: A total of 2350 patients were seen during the study period, of which 88 (3.7%) were diagnosed with acute otitis externa. The
males and females were 32 (36.4%) and 56 (63.6%), respectively, with a ratio of 1:1.8 The age range was 3 months to 70 years, with the
mean age of 18.9 years. Self‑ear cleaning with cotton bud 65 (73.9%) constituted the majority of object introduced into the ear canal(s)
and the reasons for self‑ear cleaning were because of itching of the ear(s) in 47 (53.4%), habitual 9 (10.2%), and perceiving that the
ears were dirty 32 (36.4%). The introduction of extraneous moisture into the ears was seen in 46 (52.3%) including self‑medication
with topical antibiotic, instilling plain and soapy water in the ear canal(s), and swimming. The comorbid conditions which are known
risk factors for otitis externa were seen in 35 (39.8%) patients, of which allergy was the most frequent with 22 (25%), followed by
diabetic mellitus 7 (8%) and AIDS 6 (6.8%). Only 14 (16%) of these patients had their comorbid conditions diagnosed at their first
presentation. Conclusion: Self‑ear cleaning with cotton bud was the major risk factor seen in our patients with otitis externa, followed
by the introduction of extraneous moisture into the ear canals and untreated comorbid risk factors for acute otitis externa. These risk
factors are preventable through creation of awareness and prompt treatment of other associated disease conditions.
Keywords: Acute otitis externa, prevention, risk factors
INTRODUCTION Otitis externa usually represents an acute bacterial
infection of the skin of the ear canal which is
Otitis externa is an inflammation or infection of the commonly attributable to Pseudomonas aeruginosa or
external auditory canal.[1] This condition can be acute Staphylococcus aureus.[5] The infections can also be due
or chronic, with the acute form affecting 4 in 1000 to other bacteria, viruses, or fungal agents.
persons annually.[2] Acute otitis externa is unilateral in
90% of patients, and it is uncommon below the age of Several factors can contribute to external auditory
2 years. The peak age incidence is from 7 to 12 years canal infection and the development of otitis externa:
and declines after 50 years of age.[3,4] Absence of cerumen, high humidity, retained water
in the ear canal, increased temperature, local
Corresponding Author: Dr. Mohammed Abdullahi, trauma (e.g., use of cotton swabs), anatomical
Department of Otorhinolaryngology, Usmanu Danfodiyo anomaly of the external auditory canal, dermatological
University Teaching Hospital, Sokoto, Nigeria. conditions, etc.[6,7]
E‑mail: mabdullahi7174@gmail.com
Access this article online This is an open access article distributed under the terms of the Creative
Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows
Quick Response Code: others to remix, tweak, and build upon the work non‑commercially, as long as the
Website: author is credited and the new creations are licensed under the identical terms.
www.smjonline.org
For reprints contact: reprints@medknow.com
DOI:
10.4103/1118-8561.192395 Cite this article as: Abdullahi M, Aliyu D. Risk factors of acute otitis externa
seen in patients in a Nigerian tertiary institution. Sahel Med J 2016;19:146-9.
146 © 2016 Sahel Medical Journal | Published by Wolters Kluwer - Medknow
[Downloaded free from http://www.smjonline.org on Thursday, October 20, 2016, IP: 90.206.78.193]
Abdullahi and Aliyu: Risk factors of acute otitis externa
Otitis externa is a clinical diagnosis based on the Data were analyzed using Statistic Package for Social
symptoms and signs such as pain, itching, edema, and Science (SPSS) Version 18 (Chicago: SPSS Inc.) for
erythema of the external auditory canal with purulent mean, standard deviation, and frequency distributions.
otorrhea and debris in the meatus.[7]
RESULTS
Risk factors for otitis externa are well documented in the
literature;[6‑8] there is dearth of information on the risk A total of 2350 outpatients were seen during the study
factors practiced by patients with acute otitis externa period, of which 88 (3.7%) were diagnosed with acute
in our environment. otitis externa. The males and females were 32 (36.4%) and
56 (63.6%), respectively, with male to female ratio of 1:1.8.
The aim of this study is to determine the practices that The age range was 3 months to 70 years, with the mean
are risk factors for acute otitis externa and the influence age of 18.9 years. Majority of these patients were below
of the known comorbid conditions usually associated the age of 10 years, with 30 (34.1%) patients [Figure 1].
with it in patients seen in the Ear, Nose, and Throat (ENT) Self‑ear cleaning with the use of various objects were seen
Clinic, of the Usmanu Danfodiyo University Teaching in all patients with acute otitis externa for which the use
Hospital (UDUTH), Sokoto, and to create awareness on of cotton bud 65 (73.9%) constituted the majority of object
prevention of the disease in our environment. introduced into the ear canals, and the other objects used
for self‑ear cleaning include use of both fingertip and cotton
PATIENTS AND METHODS bud 8 (9.1%), broomstick 6 (6.8%), fingertips 4 (4.5%), pen
covers 4 (4.5%), and matchstick 1 (1.1%) [Table 1]. The
This was a 6‑month cross‑sectional study using self‑ and reasons for self‑ear cleaning were because of itching of the
interviewer‑administered questionnaires (for patients ear canals 47 (53.4%), habitual 9 (10.2%), and perceiving
with no educational background). The study population
was all consecutive patients who presented for treatment
at the ENT Clinic of the UDUTH, Sokoto, Nigeria (a
tertiary institution with a referral from other centers
in the neighboring states of Northern Nigeria: Kebbi,
Niger, and Zamfara), from August 2013 to January 2014.
This study was carried out after the approval from the
Ethical Committee of the reference institution.
The clinical diagnosis of acute otitis externa was based
on the major presentations such as rapid onset (usually
within 48 h) in the past 3 weeks of otalgia, itching of the
ear canal or fullness in the ear canal, and the signs of ear
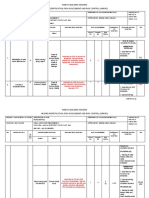
Figure 1: Age distribution in percentages
canal inflammation: Tenderness of the tragus/pinna or
both with or without otorrhea, regional lymphadenitis.[9]
Table 1: Risk factors for acute otitis externa and the
associated comorbid conditions
The questionnaires completed consist of biodata and
Practiced risk factors ad comorbid conditions Numbers (%)
risk factors for otitis externa which includes use of
Objects introduced into ear canal(s)
cotton bud and other objects for self‑ear cleaning, Cotton bud 65 (73.9)
introduction of extraneous moisture into the ear canals: Fingertip and cotton bud 8 (9.1)
Broomstick 6 (6.8)
Use of topical ear drops, swimming, instilling of plain
Fingertip 4 (4.5)
and soapy water, and the reasons for that history of Pen covers 4 (4.5)
comorbid conditions associated with acute otitis externa Matchstick 1 (1.1)
Extraneous moisture
such as allergy, diabetic, AIDS, and others.
Prolonged use of topical ear drops 21 (23.9)
Instilling water into the ear canal(s) 15 (17)
Inclusion criteria were patients with acute otitis externa Instilling soapy water in the ear canal(s) 6 (6.8)
who were first seen at the ENT Clinic and the exclusion Swimming 4 (4.5)
Comorbid conditions
criteria were patients with discharging ears from otitis Allergy 22 (25)
media, chronic otitis externa, and referred otalgia from Diabetic mellitus 7 (8)
other causes. AIDS 6 (6.8)
Sahel Medical Journal / July-September 2016 / Vol 19 | Issue 3 147
[Downloaded free from http://www.smjonline.org on Thursday, October 20, 2016, IP: 90.206.78.193]
Abdullahi and Aliyu: Risk factors of acute otitis externa
that the ears were dirty 32 (36.4%) [Figure 2]. Other risk introduced extraneous moisture into the ear canal(s);
factors practiced by the patients with acute otitis externa this can cause maceration of the canal skin and
include deliberate introduction of extraneous moisture encourages destruction of the protective barrier and
into the ear canals such as self‑medication with topical hence a favorable condition for bacterial growth
antibiotic ear drops 21 (23.9%), instilling plain water into and forming good environment for otomycosis.[12‑14]
the ear canal(s) 15 (17%), instilling soapy water into the Cerumen plays an important role in the protection of
ear canal(s) 6 (6.8%), and swimming 4 (4.5%) [Table 1]. the external auditory canal by creating an acidic pH
The comorbid conditions which are risk factors for acute which is hostile to infection;[3,15] this can be altered
otitis externa are allergy 22 (25%), diabetic mellitus 7 (8%), by extraneous moisture exposure, soapy deposit, and
and AIDS 6 (6.8%). Out of these 35 (39.8%) patients with aggressive cleaning,[3] especially in the form of self‑ear
comorbid conditions, 14 (40%) patients were not aware cleaning.
of their comorbid conditions. Forty (45.5%), 38 (43.2%),
and 10 (11.4%) had right, left, and bilateral acute otitis Although the study showed respondent practices that
externa, respectively. predispose them to acute otitis externa, prospective
studies are needed to determine if these practiced
DISCUSSION risk factors are actually responsible for this disease
condition.
Acute otitis externa is a common clinical condition.[10]
This study showed that this condition is more common Acute otitis externa can progress to a chronic form either
in females, which agrees with the studies by Amutta when the risk factors persist or when it is inadequately
et al. and Rowlands et al.[10,11] Probably, the female treated, especially the risk can be very significant
preponderance may be explained by the early when malignant otitis externa develops in patients
presentation and frequent habits of engaging in self‑ear with immunosuppressive conditions such as HIV and
cleaning that predisposes to acute otitis externa. diabetes mellitus.[16] Therefore, we recommend public
enlightenment programs, especially for mothers who
The accessible location of the external ear will explain frequently engaged in self‑ear cleaning and introduction
its susceptibility to various risk factors. These various of extraneous moisture into the external auditory canal
risk factors are well enumerated in the previous studies for the purpose of removing wax and early diagnosis and
on otitis externa.[1,6‑8,12] This study showed that all prompt treatment of patients with immunosuppression.
patients with acute otitis externa practiced self‑ear
cleaning with cotton‑tip application as the leading CONCLUSION
object introduced into the ear canal(s), which agrees
with other previous studies.[1,11] Self‑ear cleaning with various objects, especially with
cotton bud, introduction of extraneous moisture into
Apart from the use of cotton‑tip applicator and other the ear canal(s), and untreated comorbid conditions
objects for self‑ear cleaning, 52.3% of the respondents are the risk factors practiced by our patients with acute
otitis externa; they are preventable through creation of
awareness, especially to mothers who frequently engage
in self‑ear cleaning for their children, and to promote
routine medical checkup for early diagnosis and prompt
treatment of associated comorbid condition(s).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
1. Nussinovitch M, Rimon A, Volovitz B, Raveh E, Prais D, Amir J.
Cotton‑tip applicators as a leading cause of otitis externa. Int J Pediatr
Figure 2: Reasons for self-ear cleaning in percentages Otorhinolaryngol 2004;68:433‑5.
148 Sahel Medical Journal / July-September 2016 / Vol 19 | Issue 3
[Downloaded free from http://www.smjonline.org on Thursday, October 20, 2016, IP: 90.206.78.193]
Abdullahi and Aliyu: Risk factors of acute otitis externa
2. Osguthorpe JD, Nielsen DR. Otitis externa: Review and clinical 10. Rowlands S, Devalia H, Smith C, Hubbard R, Dean A. Otitis externa
update. Am Fam Physician 2006;74:1510‑6. in UK general practice: A survey using the UK General Practice
3. Rosenfeld RM, Schwartz SR, Cannon CR, Roland PS, Simon GR, Research Database. Br J Gen Pract 2001;51:533‑8.
Kumar KA, et al. Clinical practice guideline: Acute otitis externa. 11. Amutta SB, Mufutau AY, Iseh KR, Obembe A, Egili E, Aliyu D, et al.
Otolaryngol Head Neck Surg 2014;150 1 Suppl: S1‑24. Sociodemographic characteristics and prevalence of self ear cleaning
4. Beers SL, Abramo TJ. Otitis externa review. Pediatr Emerg Care in Sokoto Metropolis. Int J Otolaryngol Head Neck Surg 2013;2:276‑9.
2004;20:250‑6. 12. Wang MC, Liu CY, Shiao AS, Wang T. Ear problems in swimmers.
5. Clark WB, Brook I, Bianki D, Thompson DH. Microbiology of otitis J Chin Med Assoc 2005;68:347‑52.
externa. Otolaryngol Head Neck Surg 1997;116:23‑5. 13. Jackman A, Ward R, April M, Bent J. Topical antibiotic induced
6. Hughes E, Lee JH. Otitis externa. Pediatr Rev 2001;22:191‑7. otomycosis. Int J Pediatr Otorhinolaryngol 2005;69:857‑60.
7. Carney SA. Otitis externa and otomycosis. In: Gleeson M, 14. van Asperen IA, de Rover CM, Schijven JF, Oetomo SB,
Browning GG, Burton MJ, Clark R, Hibbert J, Jones NS, et al., Schellekens JF, van Leeuwen NJ, et al. Risk of otitis externa after
editors. Scott‑Brown Otorhinolaryngology, Head and Neck Surgery. swimming in recreational fresh water lakes containing Pseudomonas
7th ed., Vol 3. London: Hodder Arnold; 2008. p. 3351-6. aeruginosa. BMJ 1995;311:1407‑10.
8. Sander R. Otitis externa: A practical guide to treatment and 15. Sirigu P, Perra MT, Ferreli C, Maxia C, Turno F. Local immune response
prevention. Am Fam Physician 2001;63:927‑36, 941‑2. in the skin of the external auditory meatus: An immunohistochemical
9. Hui CP; Canadian Paediatric Society, Infectious Diseases and study. Microsc Res Tech 1997;38:329‑34.
Immunization Committee. Acute otitis externa. Paediatr Child Health 16. Karaman E, Yilmaz M, Ibrahimov M, Haciyev Y, Enver O. Malignant
2013;18:96‑101. otitis externa. J Craniofac Surg 2012;23:1748‑51.
Sahel Medical Journal / July-September 2016 / Vol 19 | Issue 3 149
You might also like
- CPG On CsomDocument8 pagesCPG On CsomRobert Ross DulayNo ratings yet
- Chronic Suppurative Otitis Media in AdultsDocument10 pagesChronic Suppurative Otitis Media in AdultsRstadam TagalogNo ratings yet
- Case Study BlepharitisDocument12 pagesCase Study BlepharitisNorshahidah IedaNo ratings yet
- The Most Common Causes of Bacterial Ear InfectionsDocument6 pagesThe Most Common Causes of Bacterial Ear InfectionsCentral Asian StudiesNo ratings yet
- Head and Neck AbsesDocument8 pagesHead and Neck AbsesNandaNo ratings yet
- Aerobic Bacteria Associated With Chronic Suppurative Otitis Media in AngolaDocument10 pagesAerobic Bacteria Associated With Chronic Suppurative Otitis Media in AngolaRawcath DOOMNo ratings yet
- Research: Pattern of Otitis Externa in Kaduna NigeriaDocument4 pagesResearch: Pattern of Otitis Externa in Kaduna NigeriaRicky AmeNo ratings yet
- A Prospective Study of Seven Patients With Chronic MastoiditisDocument5 pagesA Prospective Study of Seven Patients With Chronic MastoiditisarioNo ratings yet
- To Determine The Symptoms, Predisposing Factors and Causative Organisms of OtomycosisDocument3 pagesTo Determine The Symptoms, Predisposing Factors and Causative Organisms of OtomycosisAnonymous lAfk9gNPNo ratings yet
- d098 PDFDocument7 pagesd098 PDFMayiz Renata LimerseNo ratings yet
- Tonsillitis and Their Complications: Epidemiological, Clinical and Therapeutic ProfilesDocument8 pagesTonsillitis and Their Complications: Epidemiological, Clinical and Therapeutic ProfilesMarsya Yulinesia LoppiesNo ratings yet
- 6-7 Omsk MalignaDocument2 pages6-7 Omsk MalignaAlvina Ulfah RusmayuniNo ratings yet
- Recent Advancements in Management of Alveolar Osteitis (Dry Socket)Document5 pagesRecent Advancements in Management of Alveolar Osteitis (Dry Socket)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Otitis Externa: Investigation and Evidence-Based TreatmentDocument45 pagesOtitis Externa: Investigation and Evidence-Based TreatmentSonya HyekyoNo ratings yet
- EtiologiDocument8 pagesEtiologiRizka AmeliaNo ratings yet
- Acute Otitis Externa:Pathophysiology, Clinicalpresentation, and TreatmentDocument6 pagesAcute Otitis Externa:Pathophysiology, Clinicalpresentation, and TreatmentIOSRjournalNo ratings yet
- Murray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryDocument17 pagesMurray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryAndi Karwana CiptaNo ratings yet
- Odontogenic Infections: Etiology and Management: Ahmed J. Al-Naqeeb and Hala J. M. Al-Naqeeb ANB. MED. J. 15 (1), 2019Document4 pagesOdontogenic Infections: Etiology and Management: Ahmed J. Al-Naqeeb and Hala J. M. Al-Naqeeb ANB. MED. J. 15 (1), 2019lee zaraNo ratings yet
- SJAMS 66 2563 2566 C PDFDocument4 pagesSJAMS 66 2563 2566 C PDFVitta Kusma WijayaNo ratings yet
- 443 1871 1 PBDocument6 pages443 1871 1 PBRetno arunNo ratings yet
- Entamoeba Gingivalis and Trichomonas Tenax In: Periodontal DiseaseDocument12 pagesEntamoeba Gingivalis and Trichomonas Tenax In: Periodontal Diseasefadhilah RizkiyahNo ratings yet
- Effectiveness of Ciprofloxacin in The Treatment of Acute Otitis Media (#978213) - 1906643Document4 pagesEffectiveness of Ciprofloxacin in The Treatment of Acute Otitis Media (#978213) - 1906643Dinda NovitaNo ratings yet
- Pediatric ENT EmergenciesDocument20 pagesPediatric ENT EmergenciesAiri FirdausiaNo ratings yet
- Jurnal OtomikosissDocument7 pagesJurnal Otomikosissrahmy kubangunNo ratings yet
- Am J Otolaryngol: COVID-19 and Hearing DifficultiesDocument2 pagesAm J Otolaryngol: COVID-19 and Hearing DifficultiesDhyo Asy-shidiq HasNo ratings yet
- Current Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaDocument10 pagesCurrent Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaFrancis RomanosNo ratings yet
- COVID 19 and Dentistry A PerspectiveDocument12 pagesCOVID 19 and Dentistry A PerspectiveAthenaeum Scientific PublishersNo ratings yet
- Cervicofacial InfectionsDocument6 pagesCervicofacial InfectionsAngélica Valenzuela AndrighiNo ratings yet
- 3612 6812 1 SMDocument9 pages3612 6812 1 SMRizky Agustian HadiNo ratings yet
- A Study On Deep Neck Space InfectionsDocument6 pagesA Study On Deep Neck Space InfectionsbebetteryesyoucanNo ratings yet
- Microbial Profile and Patients of Chronic Suppurative Otitis Media in Latur, Maharashtra, IndiaDocument4 pagesMicrobial Profile and Patients of Chronic Suppurative Otitis Media in Latur, Maharashtra, IndiaiisisiisNo ratings yet
- Otomycosis in Relation To Csom: Gujarat Journal of Otorhinolaryngology and Head and Neck Surgery January 2011Document4 pagesOtomycosis in Relation To Csom: Gujarat Journal of Otorhinolaryngology and Head and Neck Surgery January 2011Shovie Thalia MirandaNo ratings yet
- OMSKDocument4 pagesOMSKYusnida RahmawatiNo ratings yet
- Jurnal Otitis Eksterna WordDocument14 pagesJurnal Otitis Eksterna WordmedyaanaNo ratings yet
- Mastoiditis in Childhood: Review of The LiteratureDocument6 pagesMastoiditis in Childhood: Review of The LiteratureElysabeth MargarethaNo ratings yet
- Severe Intracranial and Extracranial Complications of The Middle Ear Cholesteatoma A Report CaseDocument5 pagesSevere Intracranial and Extracranial Complications of The Middle Ear Cholesteatoma A Report CaseChoirul UmamNo ratings yet
- Otitis ExternaDocument4 pagesOtitis ExternaCesar Mauricio Daza CajasNo ratings yet
- Xu 2020Document6 pagesXu 2020Cintya RambuNo ratings yet
- Laura A Goguen, MD Daniel G Deschler, MD, FACS Morven S Edwards, MD Howard Libman, MD Contributor Disclosures Peer Review ProcessDocument4 pagesLaura A Goguen, MD Daniel G Deschler, MD, FACS Morven S Edwards, MD Howard Libman, MD Contributor Disclosures Peer Review ProcessDaniela Chavez DiazNo ratings yet
- Jurnal 1Document5 pagesJurnal 1Lian Tolombot LambeyNo ratings yet
- Jurnal 2Document11 pagesJurnal 2Ainun Jariah FahayNo ratings yet
- ADJ-odontogenic InfectionDocument9 pagesADJ-odontogenic Infectiondr.chidambra.kapoorNo ratings yet
- Presentation of Thesis JEWELDocument165 pagesPresentation of Thesis JEWELMuhammad AbdulWahidKarim MusafirNo ratings yet
- Ns. Heni Kusumawati M.Kep - EFFECT OF DEBRIDEMENT ON MANDIBULA ABSCESS PATIENTS CASE STUDYDocument8 pagesNs. Heni Kusumawati M.Kep - EFFECT OF DEBRIDEMENT ON MANDIBULA ABSCESS PATIENTS CASE STUDYcandra kusumaNo ratings yet
- Management of Odontogenic Infection of Primary Teeth in Child That Extends To The Submandibular and Submental Space Case ReportDocument5 pagesManagement of Odontogenic Infection of Primary Teeth in Child That Extends To The Submandibular and Submental Space Case ReportMel FANo ratings yet
- Incidence of Bacterial Flora Associated With Earphones Used Among Students of Saveetha Medical College and Hospital, Chennai, TamilnaduDocument5 pagesIncidence of Bacterial Flora Associated With Earphones Used Among Students of Saveetha Medical College and Hospital, Chennai, TamilnaduAnonymous lAfk9gNPNo ratings yet
- Odontogenic Infections PDFDocument50 pagesOdontogenic Infections PDFGiannisa Fathina FairuzNo ratings yet
- Microbial Etiology of Acute Otitis Externa - A One Year StudyDocument5 pagesMicrobial Etiology of Acute Otitis Externa - A One Year StudyGading AuroraNo ratings yet
- Access From The University of Nottingham Repository:: For More Information, Please ContactDocument11 pagesAccess From The University of Nottingham Repository:: For More Information, Please ContactsolidtapeNo ratings yet
- 2008-0510 - Otitis Eksterna (Diffusa) PDFDocument14 pages2008-0510 - Otitis Eksterna (Diffusa) PDFEka 'Percival' AnggrainiNo ratings yet
- Epidemiology and Pathogenesis of Chronic Suppurative Otitis Media: Implications For Prevention and TreatmentDocument17 pagesEpidemiology and Pathogenesis of Chronic Suppurative Otitis Media: Implications For Prevention and TreatmentAngge TumimomorNo ratings yet
- Current Concepts in The Pathogenesis and Treatment of Chronic Suppurative Otitis Media - PMCDocument26 pagesCurrent Concepts in The Pathogenesis and Treatment of Chronic Suppurative Otitis Media - PMCDanny. JayNo ratings yet
- IFEA IES Endodontic and Dental Practice During COVID-19Document24 pagesIFEA IES Endodontic and Dental Practice During COVID-19Mohammed TarekNo ratings yet
- Jurnal Ulkus KorneaDocument10 pagesJurnal Ulkus KorneaPutri Dery CahyaniNo ratings yet
- 1 PBDocument11 pages1 PBDesy FatmawatiNo ratings yet
- Researcharticle Open Access: BackgroundDocument4 pagesResearcharticle Open Access: BackgroundMagfira Al HabsyiNo ratings yet
- A Clinical Study of Otomycosis: H.S. Satish, Viswanatha.B, Manjuladevi.MDocument6 pagesA Clinical Study of Otomycosis: H.S. Satish, Viswanatha.B, Manjuladevi.MKepompong KupukupuNo ratings yet
- Microbial Pattern and Sensitivity Analysis of OtitDocument9 pagesMicrobial Pattern and Sensitivity Analysis of Otitmax terowNo ratings yet
- Karakteristik Kasus Otitis Eksterna Di RSUP Sanglah Denpasar Periode April 2015-April 2016Document4 pagesKarakteristik Kasus Otitis Eksterna Di RSUP Sanglah Denpasar Periode April 2015-April 2016xzcvvvvNo ratings yet
- Noma Cancrum OrisDocument4 pagesNoma Cancrum OrisAnonymous Syjpyt4MoNo ratings yet
- Birth StoryDocument7 pagesBirth StoryKaty Whipple100% (1)
- TM Housekeeping NciiDocument140 pagesTM Housekeeping NciiJane DagpinNo ratings yet
- VentolinDocument13 pagesVentolinFitrah NstNo ratings yet
- PCPDocument19 pagesPCPJafer DetamoNo ratings yet
- People Should Avoid Junk FoodsDocument4 pagesPeople Should Avoid Junk FoodsShireen BatoolNo ratings yet
- SuboxonecenterbriefDocument5 pagesSuboxonecenterbriefapi-314460549No ratings yet
- Employee Health and Safety of BPCLDocument4 pagesEmployee Health and Safety of BPCLpooji25No ratings yet
- Code Blue Policy - Adult Care Sites - Calgary ZoneDocument9 pagesCode Blue Policy - Adult Care Sites - Calgary ZoneLLyreONo ratings yet
- Janitorial ProductivityDocument7 pagesJanitorial ProductivityThe Cleaning LibraryNo ratings yet
- Adriene Vialpando: ExperienceDocument3 pagesAdriene Vialpando: ExperienceKritika NigamNo ratings yet
- Macro Analysis PhilippinesDocument9 pagesMacro Analysis PhilippinesAnthony AlferesNo ratings yet
- 01 Manajemen Risiko Klinik (MRK)Document32 pages01 Manajemen Risiko Klinik (MRK)irmaNo ratings yet
- KasaiDocument7 pagesKasaishalukiriNo ratings yet
- Critical Appraisal Checklist For An Article OnDocument4 pagesCritical Appraisal Checklist For An Article OnTiaz DiniutamiNo ratings yet
- Exercise Prescription - OCT 17 ABATONDocument92 pagesExercise Prescription - OCT 17 ABATONReignerPaulVillacortaDavidNo ratings yet
- An Exploratory Study To Assess The Academic Stress, Stress Reactions and Coping Strategies Among The B.Sc. Nursing 1st Year Students in Selected Colleges of Moga, PunjabDocument4 pagesAn Exploratory Study To Assess The Academic Stress, Stress Reactions and Coping Strategies Among The B.Sc. Nursing 1st Year Students in Selected Colleges of Moga, PunjabEditor IJTSRDNo ratings yet
- Chapter-Ii Review of LiteratureDocument8 pagesChapter-Ii Review of LiteratureANU GRAPHICSNo ratings yet
- Chronic MeningitisDocument7 pagesChronic Meningitisneurojuancarfab100% (1)
- Factors That Affect Physical DevelopmentDocument4 pagesFactors That Affect Physical DevelopmentmomuNo ratings yet
- SCIDDocument10 pagesSCIDIbrahimNo ratings yet
- SPC HIRADC - 022 - Road WorksDocument5 pagesSPC HIRADC - 022 - Road WorksKalai ArasanNo ratings yet
- 2021 DPharm - Clinical InkDocument8 pages2021 DPharm - Clinical InkEd SeguineNo ratings yet
- This Is A Awarreness Poster Made by Harsh Vagal About The Eating Disorders Namely Bulimia/anorexia Nervosa and ObesityDocument2 pagesThis Is A Awarreness Poster Made by Harsh Vagal About The Eating Disorders Namely Bulimia/anorexia Nervosa and ObesityHarsh VagalNo ratings yet
- How Can You Help Your Patients With An Uncomplicated UTI?: Know?Document1 pageHow Can You Help Your Patients With An Uncomplicated UTI?: Know?gegeNo ratings yet
- Poverty and Health Teacher's Guide: TopicsDocument42 pagesPoverty and Health Teacher's Guide: TopicsxzqpxzNo ratings yet
- Asian Pacific ScientistsDocument28 pagesAsian Pacific ScientistsMahmood SanglayNo ratings yet
- Pedia ReviewDocument22 pagesPedia ReviewDebbie LanceroNo ratings yet
- PIIS019096222032288XDocument39 pagesPIIS019096222032288XMarlina watiNo ratings yet
- Park Design Guidelines PDFDocument84 pagesPark Design Guidelines PDFmaisarahwderamanNo ratings yet