Professional Documents
Culture Documents
Mod 6 - Micro To para
Mod 6 - Micro To para
Uploaded by
Donzzkie DonCopyright:
Available Formats
You might also like
- R.A. 6675Document91 pagesR.A. 6675Donzzkie Don50% (2)
- Phle Reviewer Module 6 Qa QCDocument66 pagesPhle Reviewer Module 6 Qa QCMARIA FREDIJEAN CARIÑONo ratings yet
- Pattaguan, Donesthel M PDFDocument2 pagesPattaguan, Donesthel M PDFDonzzkie DonNo ratings yet
- Module 4 - PharmacologyDocument53 pagesModule 4 - PharmacologyDonzzkie Don100% (3)
- R.A. 8344Document16 pagesR.A. 8344Donzzkie DonNo ratings yet
- Part 10 ProkaryoticDocument54 pagesPart 10 ProkaryoticLê Thanh HằngNo ratings yet
- Kingdoms WorksheetsDocument5 pagesKingdoms WorksheetsTessNo ratings yet
- OkieDocument3 pagesOkieFebeval CastilloNo ratings yet
- Chapter 1Document20 pagesChapter 1Guy SebNo ratings yet
- Nmat Biology Cell Biology 1.1 Eukaryotic & Prokaryotic CellsDocument12 pagesNmat Biology Cell Biology 1.1 Eukaryotic & Prokaryotic Cellssavina100% (1)
- Leson 6Document2 pagesLeson 6Idk UlitNo ratings yet
- SDL - Cell Structure and Function in BacteriaDocument3 pagesSDL - Cell Structure and Function in Bacteriagovicky565No ratings yet
- Prokaryotic and Eukaryotic Cells ReviewerDocument5 pagesProkaryotic and Eukaryotic Cells ReviewerAnna Kathleen LimNo ratings yet
- Cabucana, Paul Lester Finals BacteDocument91 pagesCabucana, Paul Lester Finals BactePaul LesterNo ratings yet
- Endosymbiotic TheoryDocument9 pagesEndosymbiotic TheoryFrancisco CañonNo ratings yet
- Bacterial Cell Structure: BacteriaDocument5 pagesBacterial Cell Structure: BacteriaHassan AljaberiNo ratings yet
- MicroPara Lesson 3 - ReviewerDocument5 pagesMicroPara Lesson 3 - Reviewerrobelynjoy.alparo.cvtNo ratings yet
- 3-Prokaryotic - Eukaryotic MicroorganismsDocument16 pages3-Prokaryotic - Eukaryotic Microorganismsguestiam29No ratings yet
- Reviewer On EukaryotesDocument6 pagesReviewer On EukaryotesAlaica Joice B. JaboneteNo ratings yet
- Domain Bacteria Domain Archaea Domain Eukarya Structure and Organization of Genetic MaterialDocument2 pagesDomain Bacteria Domain Archaea Domain Eukarya Structure and Organization of Genetic MaterialAaron AsneNo ratings yet
- Zoology Lec Module 3Document6 pagesZoology Lec Module 3Camille AlzolaNo ratings yet
- Chapter 1 Basic Biology For Engineer: Microbial Diversity Taxonomy Cell Naming Gram StainDocument42 pagesChapter 1 Basic Biology For Engineer: Microbial Diversity Taxonomy Cell Naming Gram StainDivyashini MohanNo ratings yet
- Biology QuicksheetsDocument11 pagesBiology QuicksheetsMaria Renee Lian Noble100% (1)
- Chapter-2-Prokaryotes-and-Eukaryotes-MICROBIOLOGY AND PARAASITOLOGYDocument2 pagesChapter-2-Prokaryotes-and-Eukaryotes-MICROBIOLOGY AND PARAASITOLOGYIsaiah PascuaNo ratings yet
- Cell UltrastructureDocument5 pagesCell UltrastructureIrish Mae LunaNo ratings yet
- Session 1: Transmission Electron MicroscopesDocument13 pagesSession 1: Transmission Electron MicroscopesFerell GerryNo ratings yet
- (Zoolone) Animal CellDocument5 pages(Zoolone) Animal CellRenee Margarette GrapilonNo ratings yet
- Micro Chapter 2Document34 pagesMicro Chapter 2Farrah GwynethNo ratings yet
- BIO104E-Laboratory Activity. (The Cell)Document5 pagesBIO104E-Laboratory Activity. (The Cell)Stephen AzaresNo ratings yet
- P1 General Properties of VirusesDocument40 pagesP1 General Properties of VirusesLoren EscotoNo ratings yet
- Morphology of BacteriaDocument44 pagesMorphology of BacteriaDr Harender SimarNo ratings yet
- CH 16Document24 pagesCH 16Zachary0HendrixNo ratings yet
- MICROBIOLOGYDocument5 pagesMICROBIOLOGYCia RraNo ratings yet
- Cheatt Sheet #2Document2 pagesCheatt Sheet #2layanhaliloNo ratings yet
- Cell Unit of Life - 011321Document73 pagesCell Unit of Life - 011321abhishek KumarNo ratings yet
- Genbio NotesDocument10 pagesGenbio NotesD-B02 Ancheta IanNo ratings yet
- Lesson 4Document3 pagesLesson 4Samantha VeraNo ratings yet
- BahanKuliah BiologiMolekuler JasadHidupSelulerDocument43 pagesBahanKuliah BiologiMolekuler JasadHidupSelulerMochamad Untung Kurnia AgungNo ratings yet
- 01-02 Microbiology - The Science of Microbiology and Cell StructureDocument6 pages01-02 Microbiology - The Science of Microbiology and Cell StructureJanet SantosNo ratings yet
- Cell Structure 3Document3 pagesCell Structure 3Lisa LuNo ratings yet
- Plant Cell LabelDocument1 pagePlant Cell LabelAllen TagatacNo ratings yet
- Biology and Biochemistry ReviewerDocument45 pagesBiology and Biochemistry ReviewerArviNo ratings yet
- The Cell: Exercise 2Document5 pagesThe Cell: Exercise 2Jasmine Nicole EnriquezNo ratings yet
- (PARA) 1.5 - Blood and Tissue FlagellatesDocument6 pages(PARA) 1.5 - Blood and Tissue FlagellatesGuia De GuzmanNo ratings yet
- Ruling The World: Microbial DiversityDocument47 pagesRuling The World: Microbial Diversityss2945No ratings yet
- Cell Structures and FunctionsDocument3 pagesCell Structures and FunctionsLea IoaNo ratings yet
- Bacteria: Prokaryotes EukaryotesDocument4 pagesBacteria: Prokaryotes EukaryotesJerson Aizpuro SuplementoNo ratings yet
- Lecture 1 Bacterial StructureDocument38 pagesLecture 1 Bacterial StructureAyat MostafaNo ratings yet
- NMAT Part II Reviewer - PersonalDocument38 pagesNMAT Part II Reviewer - PersonalReycel MayNo ratings yet
- Cloroplastos y Peroxisomas: Sitios WEB para EstudiarDocument20 pagesCloroplastos y Peroxisomas: Sitios WEB para EstudiarNicolas Ignacio Aliaga MachucaNo ratings yet
- The Cell and Its BeginningDocument6 pagesThe Cell and Its BeginningZarc VenturaNo ratings yet
- BIO104E - Laboratory Activity (The Cell)Document5 pagesBIO104E - Laboratory Activity (The Cell)Stephen AzaresNo ratings yet
- Bacillus SPP Dormant: Clinical Bacteriology LecDocument5 pagesBacillus SPP Dormant: Clinical Bacteriology LecJamie BartolomeNo ratings yet
- Cell: The Unit of Life: Chapter - 00Document32 pagesCell: The Unit of Life: Chapter - 00athuNo ratings yet
- As-Level Biology Notes: By: Bianca HimawanDocument65 pagesAs-Level Biology Notes: By: Bianca HimawanLauren ChikwehwaNo ratings yet
- Viruses: Key Characteristics!Document7 pagesViruses: Key Characteristics!Melody Jane PardilloNo ratings yet
- Phagocyte System.: Innate/non-Specific Immune SystemDocument6 pagesPhagocyte System.: Innate/non-Specific Immune SystemAngela ReyesNo ratings yet
- Assignment 7thDocument20 pagesAssignment 7thMuhammad kamran khanNo ratings yet
- 2 - CellDocument44 pages2 - CellNorie palmesNo ratings yet
- Biology Prelim Notes Module 1-4Document54 pagesBiology Prelim Notes Module 1-4kkanaksingh124No ratings yet
- Cellular PhysiologyDocument32 pagesCellular Physiologyانس ابوهيبة0% (1)
- Isolating, Cloning and Sequencing Dna: B. Applications SyllabusDocument7 pagesIsolating, Cloning and Sequencing Dna: B. Applications SyllabusNicholas OwNo ratings yet
- Microbiology: a QuickStudy Laminated 6-Page Reference GuideFrom EverandMicrobiology: a QuickStudy Laminated 6-Page Reference GuideNo ratings yet
- Transfer Factors: Properties, Mechanism of Action and Its Clinical ApplicationsFrom EverandTransfer Factors: Properties, Mechanism of Action and Its Clinical ApplicationsNo ratings yet
- DiarrheaDocument22 pagesDiarrheaDonzzkie DonNo ratings yet
- VirologyDocument31 pagesVirologyDonzzkie DonNo ratings yet
- Department of BiochemistryDocument16 pagesDepartment of BiochemistryDonzzkie DonNo ratings yet
- Aspects of DeathDocument45 pagesAspects of DeathDonzzkie DonNo ratings yet
- Understand The ProblemDocument1 pageUnderstand The ProblemDonzzkie DonNo ratings yet
- Schwartz's Principles of Surgery ABSITE and Board Review, Ninth Edition (PDFDrive)Document517 pagesSchwartz's Principles of Surgery ABSITE and Board Review, Ninth Edition (PDFDrive)Donzzkie Don100% (1)
- Pico Format Population Exposure OutcomeDocument4 pagesPico Format Population Exposure OutcomeDonzzkie DonNo ratings yet
- Third Paragraph On PHYSICAL ACTIVITYDocument1 pageThird Paragraph On PHYSICAL ACTIVITYDonzzkie DonNo ratings yet
- Chapter 6: Microbial GrowthDocument9 pagesChapter 6: Microbial GrowthDonzzkie DonNo ratings yet
- Module 6 - Microbiology and ParasitologyDocument35 pagesModule 6 - Microbiology and ParasitologyDonzzkie DonNo ratings yet
- A Case On Typhoid Fever: Group 4Document27 pagesA Case On Typhoid Fever: Group 4Donzzkie DonNo ratings yet
- Density, Specific Gravity, and Specific Volume PDFDocument22 pagesDensity, Specific Gravity, and Specific Volume PDFDonzzkie Don100% (1)
- R.A. 10354Document36 pagesR.A. 10354Donzzkie Don100% (5)
- Group 3 Drug LitDocument79 pagesGroup 3 Drug LitDonzzkie DonNo ratings yet
- Mod 5 - Phardose PDFDocument7 pagesMod 5 - Phardose PDFDonzzkie DonNo ratings yet
- February 7,1992: " Senior Citizens Act"Document98 pagesFebruary 7,1992: " Senior Citizens Act"Donzzkie DonNo ratings yet
- R.A. 7581Document34 pagesR.A. 7581Donzzkie DonNo ratings yet
- R.A. 7394Document62 pagesR.A. 7394Donzzkie DonNo ratings yet
- June 6, 2008: Gloria Macapagal - ArroyoDocument39 pagesJune 6, 2008: Gloria Macapagal - ArroyoDonzzkie DonNo ratings yet
- R.A. 9502Document39 pagesR.A. 9502Donzzkie DonNo ratings yet
- Counseling Chronically Ill Adults in The HealthcarDocument19 pagesCounseling Chronically Ill Adults in The HealthcarDonzzkie DonNo ratings yet
- R.A. 10354Document36 pagesR.A. 10354Donzzkie DonNo ratings yet
- 1 Prescription FinalDocument62 pages1 Prescription FinalDonzzkie DonNo ratings yet
- Rational Drug Design PDFDocument7 pagesRational Drug Design PDFDonzzkie DonNo ratings yet
- Aseptic TechniquesDocument26 pagesAseptic TechniquesDonzzkie DonNo ratings yet
- The Effect of Antioxidants On Micropropagation of Avocado by Nodal SegmentsDocument6 pagesThe Effect of Antioxidants On Micropropagation of Avocado by Nodal SegmentsbryanNo ratings yet
- BioboxDocument1 pageBioboxJesúsNo ratings yet
- 2021 Molecular Basis of Prostate Cancer. FixDocument40 pages2021 Molecular Basis of Prostate Cancer. FixIrfandi AmiruddinNo ratings yet
- Harvesting Stage & Grades of Gerbera & Tube RoseDocument21 pagesHarvesting Stage & Grades of Gerbera & Tube RoseSantagriNo ratings yet
- Notice: Endangered and Threatened Species: Columbia River Salmon and Steelhead Recovery PlanDocument6 pagesNotice: Endangered and Threatened Species: Columbia River Salmon and Steelhead Recovery PlanJustia.comNo ratings yet
- Module 25 Edited Pages DeletedDocument12 pagesModule 25 Edited Pages DeletedDos DosNo ratings yet
- New Plant Breeding Techniques. State-Of-The-Art and Prospects For Commercial DevelopmentDocument220 pagesNew Plant Breeding Techniques. State-Of-The-Art and Prospects For Commercial DevelopmentJulian Andres Tovar MedinaNo ratings yet
- Buffer System For NursingDocument2 pagesBuffer System For NursingjasonNo ratings yet
- Georges Cuvier's Theory of Correlation of PartsDocument5 pagesGeorges Cuvier's Theory of Correlation of PartsSoc SaballaNo ratings yet
- Miniaturization of Rectangular Microstrip Patches Using Genetic AlgorithmsDocument4 pagesMiniaturization of Rectangular Microstrip Patches Using Genetic AlgorithmsSubba Rao ChalasaniNo ratings yet
- Prevention and Treatment of Moderate and Severe Ovarian Hyperstimulation Syndrome NoprintDocument14 pagesPrevention and Treatment of Moderate and Severe Ovarian Hyperstimulation Syndrome NoprintDo le QuangNo ratings yet
- SGBAU B.Pharm 1 SEM Human-Anatomy-n-Physiology-I 2018Document2 pagesSGBAU B.Pharm 1 SEM Human-Anatomy-n-Physiology-I 2018Abhay DeulkarNo ratings yet
- Amniotic Fluid Index (AFI) - StatPearls - NCBI BookshelfDocument2 pagesAmniotic Fluid Index (AFI) - StatPearls - NCBI BookshelfTarzan SmithNo ratings yet
- EL 108 Midterm Module 1Document22 pagesEL 108 Midterm Module 1Ella Marie Gamayon PoloNo ratings yet
- Okavango Delta Valuation Study FINAL REPORTDocument139 pagesOkavango Delta Valuation Study FINAL REPORTAse JohannessenNo ratings yet
- Genetically Engineered CropsDocument3 pagesGenetically Engineered Cropsapi-273084430No ratings yet
- Jerry Sudarsky, Wasco Inventor and HumanitarianDocument24 pagesJerry Sudarsky, Wasco Inventor and HumanitarianGilbert GiaNo ratings yet
- The Novice Nurse's Guide To Calling "Code Blue": Wayne Thomas Brice, MA, RN-BCDocument5 pagesThe Novice Nurse's Guide To Calling "Code Blue": Wayne Thomas Brice, MA, RN-BCniraNo ratings yet
- Periodontal LigamentDocument3 pagesPeriodontal LigamentCzarina DavidNo ratings yet
- Penile Cancer 2010Document28 pagesPenile Cancer 2010raghavagummadiNo ratings yet
- Module 2. Content Module Topic: Cell Cycle and Cell DivisionDocument5 pagesModule 2. Content Module Topic: Cell Cycle and Cell DivisionErolin PobleteNo ratings yet
- Bacteria ClassificationDocument395 pagesBacteria ClassificationJitendra MishraNo ratings yet
- MamosaceaeDocument12 pagesMamosaceaeBashir KhanNo ratings yet
- PAT BAHASA INGGRIS KELAS 6 SMT 2Document2 pagesPAT BAHASA INGGRIS KELAS 6 SMT 2mira ardeatikaNo ratings yet
- Franchinietal - Physiological Characteristics of Karate AthletesDocument9 pagesFranchinietal - Physiological Characteristics of Karate AthletesMiodragNo ratings yet
- Breeding ProgramDocument13 pagesBreeding ProgramgabNo ratings yet
- Fischer-Mamblona 2000Document14 pagesFischer-Mamblona 2000Gizem KaymakçıNo ratings yet
- Chapter 25: The Urinary System: Page 19 of 25Document1 pageChapter 25: The Urinary System: Page 19 of 25JAGDEV PANESARNo ratings yet
- Blood Storage Centre Standards Edition 1Document55 pagesBlood Storage Centre Standards Edition 1bloodstoragecentersuryaNo ratings yet
- Dairy Whole Dairy Packet 1 WorksheetsDocument14 pagesDairy Whole Dairy Packet 1 WorksheetsMoonkhan BlessedNo ratings yet
Mod 6 - Micro To para
Mod 6 - Micro To para
Uploaded by
Donzzkie DonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mod 6 - Micro To para
Mod 6 - Micro To para
Uploaded by
Donzzkie DonCopyright:
Available Formats
MICROBIOLOGY, IMMUNOLOGY, MYCOLOGY,
VIROLOGY, BACTERIOLOGY AND PARASITOLOGY
------------------------------------------------------------------------
I. MICROBIOLOGY Halophiles – live in high salt concentration environments
Basophiles – live in high pressure environment
study of microorganisms which are large and diverse group of
Methanogens – live in high methane concentration
microscopic organisms that can occur as either single cell or in
environment
cluster arrangement including viruses which are microscopic
o PROKARYOTIC CELL STRUCTURE
but acellular
Plasma Membrane – phospholipid bilayer
Cytoplasm
I. CELLULAR STRUCTURES
Inclusion Bodies – storage of energy; (ex. glycogen
Eukaryotes – presence of true nucleus; nucleus enclosed by
granules; sulfur granules; polyhydroxybutyric acid
nuclear membrane
granules; magnetosomes; metachromatic granules)
o Fungi – multicellular
Nucleoid – composed of genetic material
Yeast – unicellular fungi; filamentas; saprophytic; process
TRANSFER OF DNA
a cell wall (chitin)
o Conjugation – transfer of genetic material using
o Animals
plasmids
Endoparasites – helminthes
o Transduction – bacteriophage – mediated transfer
Ectoparasites – insects, arachnids
of genetic material
o Protozoans – considered as endoparasites; unicellular; free
o Transformation – direct transfer of genetic material
living
from donor to recipient cell
o Plants (e.g. algae) – multicellular; photosynthetic (cellulose);
Specialized Structures
possess a cell wall
GRAM POSITIVE GRAM NEGATIVE
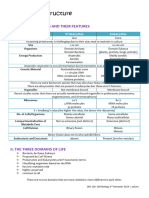
o EUKARYOTIC CELL STRUCTURE Peptidoglycan (7-8 layers) – Outer membrane
Plasma Membrane – phospholipid bilayer crystal violet
Cytoplasm – composed of fluid and organelles Plasma Membrane Peptidoglycan (1-2 layers)
Organelles Teichoic Acid (cell wall; Periplasmic space
Golgi Apparatus – packaging center; post-translational plasma membrane)
Plasma Membrane
modification; removes unnecessary peptides
Endospores
Mitochondria – “powerhouse of the cell”; oxidative
o Genus: Bacillus – aerobe; Clostridium – anaerobe
phosphorylation; 1% of DNA
o Dormant Stage: depleted with required nutrients
Endoplasmic Reticulum
o Rough ER – ribosomal attachment sporulation
active cell
o Smooth ER – lipid attachment (vegetative) SPORES
Ribosomes – site of protein synthesis; primary germination
ribosomal subunit (RSU); (80S 40S; 60S)
o heat resistant; desiccation resistant (Ca2+
Nucleus – composed of genetic materials; biochemical
dipicolinate heat resistant spore)
processes: DNA Replication (synthesis); Transcription
o Spore staining: malachite green; VR green
(synthesis of RNA – mRNA, tRNA, rRNA)
o Microscopy: Bacillus – non-swollen spore;
Prokaryotes – pathogenic + non-pathogenic; absence of true
Clostridium - swollen spore
nucleus + organelles; with ribosomes, Golgi bodies,
Plasmids – extrachromasomal genetic material (ex. R
endoplasmic reticulum; relatively small in size (diameter:
factor/ R plasmid – antimicrobial resistance)
<1µm)
Teichoic Acid –primary surface antigen gram positive;
o Eubacteria – simple bacteria; pathogenic; cell wall – 1o
functions: (1) provides negative charged surface for
component: peptidoglycan (aka murein/mucopeptide)
gram positive; (2) surface antigen of gram positive
o Arachaebacteria – non-pathogenic; no cell wall; lives in
organisms stimulates antibody production
extreme environmental conditions
Outer Membrane – exclusively found in gram negative
Thermophiles – (>85oC); lives in high temperature
organisms; composed of: lipopolysaccharides (LPS) &
environments
lipid A
PAGE 1 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Periplasmic Space – gram negative only; contains α Monotrichous – single polar flagella at 1 end
hydrolytic enymes (ex. beta lactamases)
Cell Wall – rigid structure that protects organism
against difference in osmotic pressure
o 1O component – peptidoglycan
o interlinking of peptidoglycan layer: N- α Peritrichous – flagella all over the cell
acetylmuramic acid (N-AM); N-acetylglucosamide
(N-AG)
o Pili – small rigid structure
Function: special type of movement or
locomotion; twitching motion
Forms:
α Ordinary Pili/Fimbriae
Function: bacterial attachment
PENICILLIN BINDING PROTEINS (PBP)
α Sex Pili
NAG Function: bacterial conjugation
N-AM
o Axial Fillament – (ex. spirochetes Leptospira
Glycocalyx – polysaccharide materials found outside enterogans; Treponema palidum; Borrelia
cell wall burgdorferi; Borelia recurrentis)
o Capsule – firmly attached to cell, does exclude Function: spiral locomotion
particle
Function: contribute to bacterial virulence II. OPTICAL METHODS/STAINING METHODS
escape phagocytosis Optical Methods
General Rule: o Light Microscope
α ALL cocci are non-encapsulated except: Bright Field Light Microscope – difference in contrast
streptococci black and white the specimen and surrounding medium;
α ALL bacilli are non-encapsulated except: killed and stained specimen
Bacillus, Haemophilus, Klebsiella Magnification: 1000x
o Slime Layer – loosely attached to cell, does not Ocular Lens: 10x
exclude particle
Objective Lens: 100x
Function: contribute to bacterial attachment to
Phase Contrast Light Microscope – provides
mucosal membrane
magnification of living cells which are unstained
Cell Appendages Dark Field Light Microscope – lighting system is just able
o Flagella – (ex. Vibrionaceae) to reach sides of specimen; (ex. Treponema pallidum)
Function: locomotion/movement Fluorescent Microscope – substances or specimen that
Highly Antigenic: H-antigen fluoresces – able to short wavelengths of light and emits
Primary Protein: flagellin long wavelength of light; used in clinical diagnostic
Forms: microbiology; (ex. Auramin O – used for staining M.
α Lophotrichous – tuft of flagella at 1 end tuberculosis)
Differential Interference Contrast Microscope –
polarizer; provides 3D structure of spores, vacuoles and
granules
o Electron Microscope
α Amphitrichous – single polar flagella at both Transmission Electron Microscope – uses electron beam
ends coming from an electron gun focused by an electron
condenser into a thin specimen
Scanning Electron Microscope – provides 3D structure of
microscopic surfaces of microorganism
PAGE 2 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Staining Methods Stages of Infectious Disease – imbalance of 3 agents of disease
o Gram Staining
FUNCTION GRAM + GRAM -
CONVALESCENCE PERIOD
crystal violet primary stain blue violet blue violet
INCUBATION PERIOD
PRODROMAL PERIOD
DECLINE PERIOD
iodine mordant blue violet blue violet
ACME PERIOD
ethanol decolorizer blue violet colorless
saffranin counterstain blue vioet pink red
o Acid-Fast Staining – Ziehl-Neelsen Staining; hot method and
cold method
FUNCTION
carbol fuschin primary stain
heat mordant
TIME
ethanol decolorizer
methylene blue counterstain a. Incubation Period – pre-pathogenesis period; absence of
o Negative Staining – cell/specimen appears colorless; signs and symptoms; varies on characteristic of organism;
primary stain: nigrosin (ex. Rabies the nearer the site of the bite to the brain, the
o Flagella Staining – stain: unstable colloidal suspension of shorter the incubation period)
tannic acid which forms a precipitate b. Prodromal Period – presence of prodromes or mild signs
o Capsule Staining – stain: (1) hot solution of crystal violet and symptoms (non-pathognomonic) of infection; (ex.
then rinsing with copper sulfate; (2) india ink – use for measles 3Cs: cough, corysa, conjunctivitis)
Cryptococcus neoformans (pigeon fluconazole) c. ACME Period – period of illness; presence of major signs and
o Nucleoid Staining – stain: Feulgen stain – sensitive for DNA symptoms (pathognomonic); (ex. measles rashes, Koplik
o Spore Staining – stain: malachite green; carbol fucshin spots)
d. Decline Period – signs and symptoms subsides
III. GROWTH, CULTIVATION, AND REPRODUCTION e. Convalescence Period – body is restored to its healthy
Primary Method of Reproduction – bacteria: binary fission condition
(asexual reproduction) Epidemiologic Triangle
Stages of Microbial Growth
LAG PHASE
LOG PHASE
STATIONARY PHASE
DEATH PHASE
TIME
o Lag Phase – phase of adjustment; synthesis of important
Koch’s Postulates
macromolecules/nutrients; susceptible to effects of
o Causative Agent – suspected microorganism must be
antimicrobials
present in all stages of disease
o Log Phase – exponential growth rate; rapid increase in
o Environment/Pure Culture Media – suspected
number of microorganisms at a constant maximum rate;
microorganism must be grown in pure culture media
accumulation of toxic waste
o Healthy Host – suspected microorganism when inoculated
o Stationary Phase – phase of equilibrium; cell division = cell
or introduced to a healthy host, must cause same disease
death
o Disease Host – suspected microorganism when isolated
o Death Phase – cell death > cell division
from disease host, must be same organism
Occurrence of Disease
o Endemic Disease – presence of clinical cases all year round;
January to December; (ex. schistosomiasis – Samar, Leyte;
malaria – Palawan, Mindoro; filariasis – Bicol)
PAGE 3 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
o Epidemic Disease – outbreak; sudden increase in number of o Enterobacteriaceae
clinical case at a certain place and time period Rapid Lactose Fermenters (EKE) – E. coli; Klebsiella;
o Sporadic Disease – scattered or isolated number of clinical Enterobacter
cases at a certain place or time period Slow Lactose Fermenters (SCAPE Edward Haf) – Serratia;
o Pandemic Disease – affects more than one continent; Citrobacter; Arizona; Providencia; Erwinia; Edwardsiella;
highest level: level 6; (ex. 2009 – influenza AH1N1; 2014 – Hafnia
Ebola virus = level 4) Non-Lactose Fermenters (SPPS) – Shigella; Proteus;
Culture Media Pseudonomas; Salmonella
TYPE OF CULTURE CULTURE MEDIA o Hemolytic Reaction
MEDIA α-Hemolytic Reaction – partial hemolysis green (ex.
Simple Media – 1. Nutrient Agar Streptococcus pneumoniae; Viridans streptococci;
used for non- 2. Nutrient Broth
fastidious
Streptococcus mutans)
microorganisms β-Hemolytic Reaction – complete hemolysis colorless;
Enriched Media – 1. Milk Agar high protein nutrition further subclassified into Lancefield Classification (A-G)
used for fastidious 2. Chocolate Agar sheep’s blood (1%); Group A – Streptococcus pyogenes
microorganisms; high hemoglobin nutrition
Group B – Streptococcus agalactiae
contains special
nutrients, vitamins, Gamma-Hemolytic Reaction – no visible reaction
minerals needed for
development IV. CONTROL OF MICROORGANISMS
Differential Media 1. Eosin Methylene Blue (EMB) Chemotherapy – Paul Ehrlich (1) atineoplastics; (2)
– subclassifies large & MacConkey Agar (MCA) – subclassify antimicrobials
group of group of enterobacteriaceae into lactose
microorganisms and non-lactose fermenters Antibiotics – compounds sourced from microorganisms that
into categories; VR LF NLF can inhibit growth of other microorganisms
EMB metallic green colorless
presence of visible o Classifications
MCA pink colorless
reaction a. Based on their Source – (ex. bacteria, fungi)
2. Blood Agar Plate (BAP) – both enriched
and differential media; identification of ANTIBIOTIC SOURCE
streptococci based on hemolytic Bacitracin Bacillus subtilis
reactions Polymyxin Bacillus polymyxa
Penicillin Penicillum notatum
3. Mannitol Salt Agar (MSA) –
Griseofulvin Penicillum griseofulvum
subclassifies group of staphylococci
Gentamicin MIcromonospora purpurea
- s. aureus golden yellow Streptomycin Streptomyces griseus
- s. epidermidis porcelain white Vancomycin Streptomyces orientalis
- s. saprophyticus no visible reaction Chloramphenicol Streptomyces venezuelae
Selective Media – 1. EMB & TCA – both differential and Clindamycin Streptomyces lincolnensis
allows growth of selective media Nystatin Streptomyces noursei
one group of 2. Saboraud Dextrose Agar (SDA) – Amphotericin B Streptomyces nodosus
microorganism and selective only for fungal growth; Erythromycin Streptomyces erythreus
inhibits other provides an acidic pH (pH = 5.6) Cycloserine Streptomyces orchidaceus
groups 3. Colistin-Nalidixic Acid (CNA) – selective b. Based on Spectrum of Activity
only for gram positive organisms Narrow Spectrum – (ex. Aztreonam)
4. Theyer-Martin – selective for gram-
Broad Spectrum – (ex. Carbopenems; Tetracylines)
negative diplococcic, Neisseriae;
modified chocolate agar c. Based on Antimicrobial Activity
5. Lowenstein-Jenssen Media – very Bacteriostatic Agents – inhibits growth and
selective only for Mycobacterium reproduction of microorganisms; general rule ALL
tuberculosis; very expensive protein synthesis inhibitors and antimetabolites are
extrapulmonary TB
bacteriostatic except aminoglycosides
6. Thiosulfate Citrate Bile Sucrose (TCBS)
– selective only for Vibrionaceae Bactericidal Agents – kills pathogens; general rule
7. Leoffler’s Serum Media & Tellurite ALL cell wall synthesis inhibitors are bactericidal
Media – selective only for d. Based on Mechanism of Action
Corynebacterium diphtheriae MECHANISM OF ACTION ANTIBIOTICS
8. Skirrow’s Agar & Campy BAP – Inhibitor of Cell Wall Synthesis Beta Lactams – Penicillins;
selective only for Campylobacter jejuni Cephalosporins; Carbapenems;
9. Bordet-Gengou Agar – selective only Monobactams
for Bordetella pertussis Glycopeptides – Vancomycin;
Anaerobic Media 1. Candle Jar Method Teicoplanin; Telavancin
2. Thioglycollate Agar Cycloserine
Polypeptide
3. GasPak®
PAGE 4 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Inhibitor of Protein Synthesis 30s Inhibitors – Tetracyclines; 2.) Cephalosporins
Aminoglycosides RANGE OF EFFECTIVENESS NOMENCLATURE
50s Inhibitors – Macrolides; G+ G-
Chloramphenicol; 1st +++ + ALL starts with CEPH except
Lincosamides; Oxazolidinones; Cefazolin, Cefadroxil
Streptogramins
2nd ++ ++ ALL starts with CEPH; nothing
Inhibitor of Nucleic Acid Rifamycins ends in –ONE or –IME except
Synthesis Quinolones/Fluoroquinolones Cefuroxime, Lovacarbef
Antitubercular Agents First Line Agents (RIPE) – 3rd + +++ ALL starts with CEF; ALL ends
Rifampicin; Isoniazid; with –ONE or –IME except
Pyrazinamide; Ethambutol Cefdinir, Ceftibulen,
Second Line Agent – Cefditoren, Moxalactam
Aminoglycosides; 4th +++ ++ Cefepime, Cefipirome
Fluoroquinolones; 5th Ceftaroline fosamil
Ethonamides; p-aminosalycilic
acid
COMMONLY USED CEPHALOSPORINS:
Antimetabolites Sulfonamides Cefazolin – only 1st generation ceph in parenteral form;
Pyrimethamine/Trimethoprim clinical use surgical prophylaxis
Miscellaneous Agents Nitroimidazole
Cefuroxime – extensively used for treatment of
Mupirocin
Polymyxin community-acquired pneumonia
Urinary Antiseptics – Cephamycins – 2nd generation cephs with activity for
Nitrofurantoin; Methenamine
anaerobic infection (Cefoxitin, Cefotetan, Cefmetazole)
A. Inhibitors of Cell Wall Synthesis
Ceftaroline Fosamil – only ceph active against MRSA and
Beta Lactam
MRSE
o MOA: inhibits cell wall synthesis by binding to penicillin-
Ceftriaxone & Cefotaxime – used for treatment of
binding proteins (PBP)
meningitis (except: Listeria monocytogens)
o Clinical Use:
Cefexime – used for treatment of gonococcal or non-
effective for gram positive and gram negative
gonoccocal urethritis and cervicitis
ineffective for:
Cefoperazone & Ceftazidime – has activity for
(1) wall-less microorganisms (ex. mycoplasma)
Pseudomonas infection
(2) microorganisms with atypical cell wall component (ex.
3.) Carbapenems – widest spectrum among beta-lactam
mycobacterium)
antibiotics
(3) intracellular parasites (ex. legionella; brucella;
Imipenem + Cilastatin dihydropeptidase enzyme
chlamydia; rickettsia)
inhibitor
(4) resistant microorganisms (ex. MRSA; MRSE)
Meropenem
o Adverse Effects: allergic reaction; anaphylactic reaction;
cross-sensitivity reaction PENs & CEPHs; Jarisch- Ertapenem
Herxheimer Reaction – idiosyncratic reaction 4.) Monobactam – (ex. Aztreonam) – only effective for aerobic
1.) Penicillins and gram negative organisms
a. Natural Penicillins Glycopeptides
Pen G – benzyl penicillin; poor oral bioavailability; o Vancomycin
parenteral (IV/IM) MOA: inhibits cell wall synthesis by binding to terminal
peptide D-ala-D-ala terminus of nascent peptide chain
Pen V – phenoxymethyl penicillin; good oral
Clinical Use: formerly DOC for Pseudomembranous colitis;
bioavailability; oral
DOC for treatment infection caused by MRSA and MRSE
b. Isoxazolyl Penicillins – antistaphylococcal penicillins;
Adverse Effect: Red Man Syndrome – form of phlebitis or
resistant to action of beta lactamases; prototype:
allergic reaction; management: prophylaxis N-
methicillin – withdrawn due to nephrotoxicity; (ex.
diphenhydramine (via slow IV infusion)
cloxacillin; oxacillin; dicloxacillin; nafcillin)
o Teicoplanin – same MOA, same spectrum; IV and IM
c. Extended Spectrum Penicillins – increases gram
o Telavancin
negative coverage; increases gram negative membrane
Chemical Structure: semisynthetic lipoglycopeptide
penetration
derived from Vancomycin
Aminopenicillins – (ex. amoxicillin; ampicillin;
MOA: same with Vancomycin; alters membrane potential
bacampicillin)
and membrane permeability
Carboxypenicillins – has activity for Pseudomonas
o Dalbavacin
infection – (ex. carbenicillin; ticarcillin)
Chemical Structure: semisynthetic lipoglycopeptide
Ureidopenicillins – (ex. piperacillin; azlocillin;
derived from Teicoplanin
mezlocillin)
PAGE 5 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Cycloserine Clinical Use: treatment for infection caused by
o MOA: inhibits cell wall synthesis by inhibiting activity of: (1) staphylococci and streptococci; treatment for peptic
alanine racemase, (2) D-ala-D-alanyl ligase ulcer disease caused by H. plyori
o Clinical Use: 2nd line of agent for Mycobacterium o Azitrhromycin
tuberculosis resistant to the first line agents Pharmacokinetics: (1) excellent distribution to body
Polypeptide (ex. Bacitracin) – poor oral bioavailability tissues; (2) longer t ½
topical Dosing: once a day for 3-5 days
o Chemical Structure: mixed cyclic polypeptide Adverse Effect: arrhythmia
2.) Chloramphenicol
B. INHIBITORS OF PROTEIN SYNTHESIS o MOA: inhibition of peptidyl transferase; (RLE: peptide
Inhibitors of 30s Ribosomal Subunit elongation)
1.) Tetracyclines – (ex. Tetracyclines; Doxycycline; o Adverse Events: nitro group
Minocycline; Demedocyline) aplastic anemia – low RBC, WBC, platelets
o widest/broadest spectrum among antibiotics (gram Grey Baby Syndrome – lacking for enzyme for
positive, gram negative, wall less organisms, intracellular glucoronidation
parasites; spirochetes, plasmodium) o Toxic Dose: > 50mg/kg/day
o Chemical Structure: naphthacene ring o Clinical Use: alternative for treatment of typhoid fever
o MOA: inhibition of binding of aminoocyl tRNA to mRNA (enteric fever)
prevents peptide elongation 3.) Lincosamides – MOA: same as macrolides
o Adverse Effects: (contraindicated in patients < 8 yrs old) o Lincomycin
Permanent yellow staining of teeth Chemical Structure: sulfur containing antibiotic
Hypoplasia of teeth o Clindamycin – DOC for anaerobic infections above
Use of expired tetracyclines Fanconi-like diaphragm; alternative treatment for toxoplasmosis (+
Syndrome pyrimethamine); treatment of skin and soft tissue
Ototoxicity Minocycline infection caused by staphylococci and streptococci
Phototoxicity Demeclocycline 4.) Oxazolidinones – (ex. Linezolid – treatment of VRSA, VRSE)
2.) Aminoglycosides o MOA: inhibits 23s subunit of the 50s subunit
o Source: Micromonaspora (-micins); Streptomyces (- 5.) Streptogramins
mycins) o Ratio: 70 (A) : 30 (B)
o MOA: inhibit protein synthesis: (1) prevention of Streptogramin A – Dalfopristin
formation of initiation complex, (2) misreading of mRNA Streptogramin B – Quinupristin
complex, (3) formation of nonfunctional polysomes o Clinical Use: treatment of VRSA, VRSE
o Pharmacodynamic Properties: concentration dependent
killing; postantibiotic effect; synergistic effect C. INHIBITORS OF NUCLEIC ACID SYNTHESIS
o Adverse Effects: Rifamycin – (ex. Rifampicin; Rifabutin)
Ototoxicity – Kanamycin; Amikacin; Neomycin o MOA: Inhibition of RNA polymerase (RLE: transcription)
Vestibulotoxicity – Streptomycin; Gentamicin o Clinical Use: treatment of pulmonary and extrapulmonary
Nephrotoxicity – Neomycin; Gentamicin; Tobramycin tuberculosis; treatment of cutaneous tuberculosis (leprosy)
Inhibitors of 50s Ribosomal Subunit o Adverse Effect: Red-orange discoloration of body fluids (ex.
1.) Macrolides sweat, urine, saliva)
o Chemical Structure: large lactone ring Quinolones/ Fluoroquinolones
o MOA: blocks peptide exit tunnel dissociation of o MOA: inhibitor of:
peptidyl tRNA from ribosome Topoisomerase II (DNA Gyrase) – relaxation of
o Erythromycin supercoiled DNA
Clinical Use: alternative for patients allergic to B- Topoisomerase IV – separates DNA strand
lactam antibiotics o Addition of fluorine:
Adverse Effect: abdominal discomfort; stimulates Increase gram negative coverage
motillin receptors (increases peristalsis); jaundice – Improved penetration to gram negative membrane
associated with use of erythromycin estolate salt
o Clarithromycin – least associated with adverse effects
Chemical Structure: methylated erythromycin
PAGE 6 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
First Nalidixic acid and Cinaxacin E. ANTIMETABOLITES
Generation Moderate gram (-) activity SULFONAMIDES
Limited use for uncomplicated UTI PABA
Second Ciprofloxacin, Ofloxacin, Norfloxacin, Eroxacin, X
X dihydropteroate synthetase
Generation Lomefloxacin PYRIMETHAMINE/TRIMETHOPRIM
Improved gram (-) activity Dihydrofolate
Has activity for gram (+) and atypical microorganisms dihydrofolate reductase X X
Third Levofloxacin, Sparfloxacin, Gemifloxacin, Gatifloxacin,
Tetrahydrofolate
Generation Moxifloxacin
Retained gram (-) activity
Improved activity for gram (+) and atypical Purine Bases
microorganisms
Fourth Trovafloxacin
Generation Retained activity for gram (-), gram (+), and atypical Nucleic Acid Synthesis
microorganisms
Sulfonamides
Has activity for anaerobic microorganisms
o Chemical Structure: PABA-like
o COMMONLY USED FLUOROQUINOLONES
o MOA: inhibition of dihydropteroate synthetase
Ciprofloxacin – used as treatment and prophylaxis for
o Adverse Effects:
anthrax
Respiratory Fluoroquinolones – used for treatment of lower Steven-Johnson Sydrome
Counterindicated: G6PD Deficient
respiratory tract infections and upper respiratory tract
G6PD↓ NADPH↓ oxidized glutathione –(glutathione
infection; (Levofloxacin; Gatifloxacin; Gemifloxacin;
reductase)-> reduced glutathione (master antioxidant)
Moxifloxacin)
Jaundice
Ciprofloxacin and Levofloxacin – treatment of
uncomplicated UTI Pyrimethamine/Trimethoprim
o MOA: inhibition of enzyme dihydrofolate reductase
Adverse Effects: bone/cartilage toxicity; (ex. tendinitis;
o Adverse Effects: megaloblastic anemia management:
phototoxicity)
leucovorin
D. ANTITUBERCULAR AGENTS Combinations:
o Sulfamethoxazole + Trimethoprim (Co-Trimoxazole) – DOC
First Line Agents – (HRZE or RIPE)
for Pneumocystis jiroveci pneumonia
o Isoniazid
o Sulfadiazine + Pyrimethamine (Daraprim®) – DOC for
Chemical Structure: isonicotinic hydrazine
toxoplasmosis
MOA: inhibits mycolic acid synthesis
o Sulfadoxime + Pyrimethamine (Fansidar®) – treatment of
Pharmacokinetics: acetylation
malaria
Enzyme: N-acetyltransferase; fast acetylators rapid
development of resistance
F. MISCALLANEOUS AGENTS
Management: ethambutol
Adverse Effects: peripheral neuritis management: Vit Nitroimidazoles – (ex. Metronidazole; Tinidazole)
B6 (Pyridoxine) o Clinical Use: DOC for trichomoniasis, amobiasis, giardiasis
o Rifampicin (TAG); DOC for anaerobic infection below diaphragm; DOC
o Pyrazinamide – short term therapy; Adverse Effect: for Pseudomembranous colitis
hepatotoxicity o Adverse Effect: metallic aftertaste + etOH disulferam-like
o Ethambutol effect
MOA: inhibits arabinosyl transferase ↓arabinoglucan Mupirocin – pseudomonic acid; topical
Adverse Effects: red-green visual disturbance (optic o MOA: inhibits staphylococcal isoleucyl tRNA synthetase
neuritis) o Clinical Use: treatment of skin infection caused by
staphylococcus (Impetigo)
Second Line Agents
o Aminoglycosides – Streptomycin IM Polymyxin – (ex. Polymixin B; Polymixin E – Colistin); topical
o Fluoroquinolones – Levofloxacin or Moxifloxacin o MOA: acts like cationic detergents disruption of cell
o Ethionamides membrane
o Cycloserine
o p-Aminosalicylic Acid G. URINARY ANTISEPTICS
Nitrofurantoin – active at an acidic pH; for uncomplicated UTI
Methanamine – prodrug formaldehyde (urinary
antiseptic); active at an acidic pH; for uncomplicated UTI
PAGE 7 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
H. DRUG-DRUG RELATIONSHIPS Natural Killer Cells (NK cells) – Antibody Dependent
Addition (1+1 = 2) – bacteriocidal + bacteriocidal; except: Cellular Cytotoxicity (ADCC); indirectly attacks viruses and
penicillins + aminoglycosides tumor/cancer cells
Synergistic (1+1 = 3) – bacteriostatic + bacteriostatic
Antagonism (1+1 = 0) – bacteriocidal + bacteriostatic III. NON-SPECIFIC IMMUNITY – Innate Immunity
Potentiation (1+0 = 2) – penicillins + β lactamase inhibitors; Inflammation
(ex. amoxicillin + clavulanic acid; ampicillin + sulbactam; o 5 Cardinal Steps:
piperacillin + tazobactam; imipenem + cilastatin) Rubor – redness
Calor – heat
II. IMMUNOLOGY Tumor – swelling/edema
Dolor - pain
physiological process in which body (self) recognizes itself
Functio Laesa – loss of function
from foreign (non-self)
Chemotaxis – movement of neutrophils to site of infection
Types of Immunity:
o Margination
NON-SPECIFIC (INNATE) SPECIFIC (ADAPTIVE)
does not require antigen requires antigen recognition o Diapedesis
recognition antigen specific Phagocytosis
not antigen specific lagtime before response
Complement System
response is immediate result to antibody production
does not result to antibody results to immunologic memory o Primary Goal – to create membrane attack complex (C5b, C6,
production C7, C8, C9)
does not result to immunologic o MAC:
memory
Classical Pathway
I. CELLS INVOLVED IN IMMUNITY Alternative Pathway
Mannose-Binding Lectin
Granulocytes (BEN)
o Basophils – for histamine release; present during acute
allergic reaction; found in peripheral circulation
Mast Cells – for histamine release; found near
organs/tissues Bacteria MAC
o Eosinophils – present during type I HS reaction and
N
helminthic infestation
o Neutrophils – for phagocytosis; present in bacterial
IV. SPECIFIC IMMUNITY – Adaptive Immunity
infection and acute inflammation
Branches:
Agranulocytes
o Humoral Immunity – B-cells
o Monocytes + Macrophages
o Cellular-Mediated Immunity – T-cells
Monocytes – young macrophages; no phagocytic
Lymphoid Organs
effect
o Primary Lymphoid Organs – site of maturity; (ex. bone
o Macrophages – for phagocytosis and antigen presentation;
marrow; thymus)
(>2 weeks) – present during chronic inflammation
o Secondary Lymphoid Organs – site of activation; (ex. tonsils;
Lymphocytes – mature/activated in lymphoid organs lymph nodes; spleen; Peyer’s Patches)
o B Lymphocytes/B Cells – for antigen presentation; matures
Immunoglobulins
into 2 types of cells: (1) Plasma Cells – antibody production;
(2) – Memory Cells – immunologic memory
Example: Vaccination:
Measles – 1 strain; 9 months
Dengue Virus – 1, 2 (memory cells), 3, 4
o T Lymphocytes/T Cells
Helper T Cells – aka CD4 + cells; attacked by HIV;
stimulates B cells and cytotoxic T cells
Cytotoxic T Cells – aka CD8 + cells; for directly attacks;
viruses and tumor/cancer cells o Immunoglobulin A – aka secretory immunoglobulin; found
B CELLS HELPER T CELLS CYTOTOXIC T CELL in body secretions/fluids (saliva; sweat; tears; colostrum)
o Immunoglobulin E – responsible for type I hypersensitivity
PLASMA CELLS MEMORY CELLS CT CT CT
CT (allergy)
PAGE 8 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
o Immunoglobulin M – largest immunoglobulin Mycoses
(macroglobulin); first to respond during infection o Hypersensitivity Reaction
o Immunoglobulin G – most dominant immunoglobulin; o Mycotoxicosis – ingestion of preformed fungal toxin; (ex.
crosses placental barrier Aflatoxin – stale peanuts acted upon Aspergillus, carcinogen
o Immunoglobulin D – has no known function; found in B cell hepatocellular carcinoma; Ergotoxin – wheat acted upon
receptor by Claviceps purpurea)
Hypersensitivity Reaction o Mycetisma – ingestion of a poisonous fungi; (ex. Amanita
o Antibody Mediated Hypersensitivity Reaction – Type I, II, III phalloides)
Type I Hypersensitivity Reaction – aka Intermediate o Fungal Infections
Hypersensitivity Reaction; (ex. allergy; atropy; Superficial Mycoses
anaphylaxis); mediated by IgE MYCOSES CAUSATIVE AGENT CLINICAL
MANIFESTATIONS
Type II Hypersensitivity Reaction – aka Cytotoxic
Black Piedra – Piedraia hortae Black nodules found on
Hypersensitivity Reaction; (ex. blood transfusion reaction aka Tinea nodosa hairshaft
– ABO incompatibility, Rh incompatibility; erythroblastosis White Piedra Trichosporon beigelii Beige nodules found on
hairshaft
fetalis; grave’s disease)
Pityriasis – aka Malasssezia furfur Hypo/hyperpigmented
Type III Hypersensitivity Reaction – aka Antigen-Antibody Tinea vesicolor serpentine skin lesions
Complex Formation; mediated by IgG; (ex. rheumatic Tinea Nigra Exophiala werneckii Brown to black lesions
heart disease; acute glomerulonephritis; arthus reaction; found on palms and
soles
vasculitis; serum sickness; SLE)
Cutaneous Mycoses
o Cellular Mediated Hypersensitivity
Causative Agent: Dermatophytes
Type IV Hypersensitivity Reaction – aka Delayed
o Epidermophyton – affects skin and nails
Hypersensitivity Reaction; (ex. tuberculin skin test/PDD;
o Microsporon – affects skin and hair
contact dermatitis)
o Trichophyton – affects skin, nails, and hair
Clinical Manifestation: Tinea/Ringworms
III. MYCOLOGY TINEA PART OF BODY DERMATOPHYTES
Forms Tinea Pedis feet T. rubrum;
E. mentagrophytes;
o Molds – multicellular; filamentous; lives at room E. Acossum
temperature (20-25oC) Tinea Cruris – jock groin area T. rubrum;
o Yeasts – unicellular; non-filamentous; lives at body itch E. mentagrophytes;
E. Acossum
temperature (37oC) Tinea Unguium – nail/hands T. rubrum;
Characteristics – multicellular and filamentous (except yeasts); onchomycosis E. mentagrophytes;
E. Acossum
saphrophytic; parasitic/pathogenic; plant-like
Tinea Corporis trunk/body T. rubrum;
Morphology E. flocossum
o Hyphae – filamentous; microtubular structures found in Tinea Barbae beard area E. mentagophytes
molds Tinea Capitis scalp area E. mentagophytes;
M. canis
o Septum – cross-walled structures; found inside a hyphae Subcutaneous Mycoses – introduced into SQ/hypodermis
o Conidia & Spores – primary method of asexual reproduction area via a skin incision/trauma
Phyla MYCOSES CAUSATIVE AGENT CLINICAL
PHYLA SEXUAL ASEXUAL MANIFESTATIONS
REPRODUCTION REPRODUCTION Chromoblastomycosis Phialophora verrucosa; warty-
Fonsaccrea pedrosoi; like/verracous skin
Phylum zygospores sprorangium/spores
Fonsacaea compacta; lesions found along
Glomerulomycota, Rhinocladiella aquaspersa; draining of
Order Mucorales – Chladophialophora carrionii lymphatics
formerly known as Mycetoma – aka Pseudallescheria boydii; suppuration;
Phylum Madura Foot; Modurella mycetomatis; abcess formation;
Zygomycota associated with Modurella grisea; granuloma
Phylum ascospores conidia barefoot individuals Exophiala jeanselmei; formation
Acremonium falciforme
Ascomycota –
Sporotrichosis – aka nodules found
largest phylum;
Occupational Disease along draining of
aka “sac” fungi of Gardeners; lymphatics
Phylum basidiospores conidia/spores MOT: rose thorns; tree
Basidiomycota – barks; and soil
aka “club” fungi Phaeohyphomycosis Phialophora richardsiae; solitary
Wangiella dermatitidis; encapsulated cyst
Bipolaris spicifira; found on skin
I. MEDICAL MYCOLOGY Exophiala jeanselmei;
Alternaria (sp. of molds);
study of fungal diseases (mycoses) and associated treatment curvuloria; Exorhilum
rostratum
PAGE 9 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Systemic/Endemic Mycoses III. ANTIFUNGAL
Causative Agent: Thermally Dimorphic Fungi Superficial Mycoses – oral; topical
Mode of Transmission: respiratory (initial site of lungs) o Griseofulvin – fungistatic
Mode of Treatment: no known MOA; PROPOSED MOA: protects early formed
o Mild to Moderate – Itoconazole (DOC) skin against dermatophytic infection
o Moderate to Severe – Amphotericin B (DOC) Pharmacokinetics: ↑absorption: high lipid/fatty meal
MYCOSES CAUSATIVE CLINICAL TISSUE FORM/ Clinical Use: treatment of skin infection caused by
AGENT MANIFESTATION MICROSCOPIC
FORM dermatophytes
Coccidiomycosis Coccidioides Valley spherules o Terbenafine – fungicidal
– First Outbreak: immitis; Fever/Desert containing
San Joaquin Coccidioides Rheumatism endospores MOA: inhibition of squalene epoxidase ↑↑↑
Valley, California posadasii squalene epoxide
Histoplasmosis Histoplasma mimics signs and oral yeasts
– Spelunker’s capsulatum symptoms of PTB inside o Nystatin – topical; poorly absorbed
Disease; (cough hemolysis) macrophages Chemical Structure: polyene antifungal
MOT: inhalation
of spores from MOA: inhibition of ergosterol synthesis
bat droppings Clinical Use: effective for skin infection caused by yeasts
South American Paracoccidioides painful mouth and large, multiple
Blastomycosis brasiliensis pharyngeal ulcers budding yeast o Azoles
North American Blastomyces pulmonary/lung thick walled MOA: inhibition of fungal CYP450
Blastomycosis dermatitidis infiltrates lesions yeast with
or ulcerations broad based Chemical Structures:
found
genitalia, bones
on single bud
Imidazoles – less selective in inhibiting human CYP450;
and CNS-brain (ex. Ketoconazole; Topical Azoles – Clotrimazole,
Opportunistic Mycoses Ticonazole, Miconazole)
MYCOSES CAUSATIVE
AGENT
CLINICAL
MANIFESTATION
TREATMENT
Triazoles – more selective in inhibiting fungal CYP450;
Candidiasis Candida cutaneous/mucosal – Nystatin (ex. Fluconazole; Voriconazole; Itraconazole;
albicans – oral thrush, diaper (DOC);
formation of rash, vaginosis, Ketoconazole
Posaconazole)
germ tube; intertriginous Adverse Effects: antiadrogenic effects (Males:
C. glabrata; infections,
C. tropicalis; onychomycosis;
gynecomastia; Females: galactorrhea); enzyme inhibition
C. krusei; systemic – associated o Topical Agents
C. lusetanei with prosthetic
devices;
Standard Salicylic Acid – APAP solution
Treatment –
chronic
Amphotericin Salicylic Acid + Benzoic Acid – Whitfield’s ointment
mucocutaneous –
associated with
B+ Selenium Sulfide – Selsun Blue Shampoo
Flucytosine;
immunocompromised
Alternative - Potassium Iodide Solution – DOC for sporotrichosis
state and
endocrinopathies (ex.
Fluconazole Less Serious Mycoses
diabetes mellitus) o Ketoconazole – 1st azole available for clinical use
Cryptococcosis Cryptococcus cryptococcus Meningitis –
–MOT: spores neoformans meningitis Fluconazole o Fluconazole – (1) excellent penetration into BBB; (2) good
inhaled from (DOC); water solubility; least associated with adverse effects
pigeon Systemic:
droppings; Amphotericin o Itraconazole – 2nd line treatment for systemic/endemic
Capsule B + mycoses
Staining: india Flucytosine
ink Life Threatening Mycoses
Pneumocystis Pneumocystis pneumonia Cotrimoxazole
Jiroveci jiroveci – (DOC)
o Amphotericin B – grandfather of antifungals; + flucytosine =
Pneumonia Humans synergistic effect
(former
protozoan)
MOA: binds to ergosterol in fungal membrane and create
Aspergillosis Aspergillus bronchopulmonary Variconazole holes (cytoplasmic leakage)
fumigatus; aspergillus; invasive (DOC)
Aspergillus aspergillosis;
Clinical Use: initially use to decease fungal burden
flavus aspergilloma – fungal Adverse Effects: nephrotoxicity – acute renal failure with
ball
Mycomycosis Zygomucor rhinocerebellar Posaconazole wasting K+ and Mg2+
infection (DOC) o Flucytosine
Chemical Structure: pyrimidine analogue
Prodrug 5-fluorouracil (antifungal)
MOA: (1) taken up cytosine permease; (2) converted to 6-
fluorouracil; (3) 5-fluorouracil is converted to:
fluorodoxyuridine monophosphate (FDUMP),
fluorouridine triphosphate (FUTP)
PAGE 10 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Clinical Use: treatment for systemic yeast infection; + Prion Diseases
amphotericin B Bovine Spongiform Encephalopathy – Mad Cow’s
o Echinocandins Disease
MOA: inhibition of β-1,3-D-glucan synthesis
Examples: caspofungin; anidulafungin; micafungin
o Voriconazole
o Posaconazole – broadest spectrum among azoles; Scrapie – prion disease in sheeps
zygomucor, aspergillus, candida (ZAC) Kuru – association with human cannibalism; tribe in
Papua New Guinea
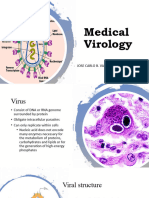
IV. VIROLOGY Creutzfeld-Jakob Disease – associated with use of
Characteristics – obligate intracellular parasites; acellular human growth hormone from corpse
(nucleic acids + proteins); does not replicate (replication
happens inside cell) II. GENERAL PROPERTIES OF DNA & RNA VIRUSES
DNA VIRUSES EXCEPTION:
Morphology Double Stranded Parvoviridae (ss)
o Nucleic Acid Core – either DNA or RNA Icosahedral Poxviridae
o Viral Capsid – protein part; for protection and basis for viral Nucleus Poxviridae (cytoplasm)
(replication)
symmetry
NAKED DNA ENVELOPED DNA
o Viral Envelope – enveloped virus – more vulnerable to Adenoviridae Hepadnaviridae
effects of surfactants; naked virus Parvoviridae Poxviridae
Papilloviridae Herpesviridae
Viral Symmetry
Polyomaviridae
o Cubic/Icosahedral – spherical RNA VIRUSES EXCEPTION:
General Rule: (1) all DNA viruses except POXVIRIDAE; (2) Single Stranded Reoviridae (ds)
all RNA (+) sense viruses except FLAVIVIRIDAE, Enveloped Picornaviridae; Reoviridae; Caliciviridae (PRC)
Cytoplasm Retroviridae; Orthomyxoviridae; Influenza
CORONAVIRIDAE, RETROVIRIDAE Spherical – (nucleus)
o Helical Helical Rabies Virus (helical-bullet shape)
General Rule: all RNA (-) sense viruses except
AENAVIRIDAE III. DNA VIRUSES
o Complex – neither cube nor helical; Poxviridae, Flaviviridae, Adenoviridae
Aenaviridae, Coronaviridae, Retroviridae (PoFACoR) o Sites of Infection: conjunctiva; pharynx; small intestine;
Viral Genome urinary bladder
o Double Stranded (DS) o Clinical Manifestation: pink conjunctivitis (sore eyes);
General Rule: all DNA viruses except PARVOVIRIDAE pharyngitis (sore throat); gastroenteritis; hemorrhagic cystis
o Single Stranded (SS) Parvoviridae – simplest DNA virus (single stranded);
General Rule: all RNA viruses except REOVIRIDAE Parvovirus B19 (humans); red blood cell (tropism)
o Segmented Viruses – Bunyaviridae, Arenaviridae, o Clinical Manifestation:
Reoviridae, Orthomyxoviridae (BARO) Erythema Infectiosum – aka “5th disease”; slapped cheek
Viral Life Cycle appearance (children); severe arthralgia (adults)
o Lysogenic Stage – no signs and symptoms (avirulent stage); Glove and Socking Syndrome – rashes found on hands
synthesis and packaging of virions (mature viral particles) and lower extremeties
o Lytic Stage – presence of signs and symptoms; release of Transient Aplastic Anemia
virions Pure Red Cell Aplasia
Steps in Viral Infection – ASPERSP Hydrops Fetalis
1. Attachment of virus to host cell Papillomaviridae – human papilloma virus
2. Penetration of virus into host cell HPV STRAINS DISEASES
1 Plantar Warts
3. Expression of viral genome
2 Common Skin Warts
4. Replication of virus 3 Cutaneous Warts
5. Synthesis of virions 7 Butcher’s Hand Warts
6. Packaging and release of virions 6, 11 Anogengenital Warts, Laryngeal Carcinoma
16, 18 Cervical Carcinoma
Unconventional Virus
o Prevention:
o Viroid – single stranded; smallest pathogen that can infect
Papanicolau Smear (Pap Smear) – early detection; start at
plants
age 21 years old
o Prions – only composed of proteins; heat resistant;
desiccation resistant
PAGE 11 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Vaccination Hepadnaviridae – Hepatitis B
Gardasil (Quadrivalent) – HPV 6, 11, 16, 18
Cervarix (Bivalent) – HPV 16, 18
Polymaviridae – BK virus; JC virus; Ki and Wu virus; Merkett
cell virus; SVAD virus
Poxviridae – brick shape virus
o Orthopox
Monkey Pox – 1o member; clinical manifestation: cervical
and inguinal lymphadenopathy IV. RNA VIRUSES
Small Pox – variola; eradicated (last case was 1978 – RNA (+) SENSE – immediately translated into proteins;
Somalia); clinical manifestation: skin lesions (starts at (PiCoTCaFlaRe2)
head/facial area; skin lesions are of same stages) o Picornaviridae – smallest RNA virus
Vaccinia – 1o component of small pox vaccine; model Enterovirus
virus in terms of structure and replication a. Polio Virus
Cow Pox – ancestor of vaccinia; rodents (host); clinical Clinical Manifestation: paralytic poliomyelitis
manifestation: hemorrhagic/red-based skin lesions Prevention: vaccination
o Parapox Sabin – live attenuated virus; oral (OPV)
ORF Virus – found in sheeps; clinical manifestation: Salk – killed virus; IM (IPV)
benign pustular dermatitis; aka occupational disease b. Rhino Virus – most common cause of common colds
among sheep handlers c. Coxsakie Virus
o Mollusca Pox Coxsackie A – herpangian (vesicular pharyngitis);
Mollusca Contagiosum Virus – clinical manifestation: hand-foot-mouth disease; hemorrhagic
small, pink warty-like skin lesions found at back, buttocks, conjunctivitis
and genitalia Coxsackie B – pleurodynia; pericardis; myocarditis
o Yatapox – Yaba Pox; Tana Pox Aphtho Virus – foot and mouth disease
Herpesviridae – latency period – asymptomatic; cytopathic Kobu Virus
effects – formation of “giant” cells Cardio Virus
FAMILY STRAIN COMMON NAME CLINICAL MANIFESTATIONS Hepato Virus – Hepatitis A
Alpha 1 Herpes Simplex Virus 1 – gingivastomatitis; cold sores;
Herpes non-sexually fever blisters; hepatic o Coronaviridae – solar/petal shape; clinical manifestations:
transmitted encephalitis SARS; MERS; gastroenteritis; common colds
2 Herpes Simplex Virus 2 – genital herpes; neonatal
sexually tranmitted sepsis; hepatic meningitis o Togaviridae – arbovirus (arthropod borne)
3 Varicella-Zoster Virus skin lesions (starts at trunk); Alpha Virus – Chinkungunya Virus – crippling arthritis
Varicella (chicken pox); skin lesions are of different
stages (most are vesicular) Rubi Virus – Rubella (german measles) – clinical
Zoster (shingles) skin lesions are dermatomal manifestations: 3-day maculopapular rash; congenital
reactivation of varicella (dermatomes); more painful
defects: cataract formation (blindness), deafness, valvular
Beta 5 Cytomegalovirus (CMV) 90-95% asymptomatic
Herpes – most common 5-10% symptomatic:
defects; forchheimer spots – petechiae seen at soft palate
congenital infection* stillbirth; intrauterine; o Calciviridae
growth retardation;
blindness; deafness; mental Callci Virus/Norwalk Virus – Norwalk Ohio Elementary
retardation School (first outbreak); clinical manifestations: viral
6 Human Herpes Virus 6 roseola – aka infanten
7 Human Herpes Virus 7 subitum; 6th disease gastroenteritis
Gamma 4 Epstein-Barr Virus (EBV) infectious mononucleosis o Flaviviridae – arbovirus
Herpes (IM) – aka kissing disease,
monospot test (diagnosis); Dengue Virus
burkitt’s lymphoma; Vector: aedes aegypti; aedes albopictus
hodgkin’s and nonhodgkin’s
lymphoma; gastric carcinoma Clinical Manifestations: dengue hemorrhagic fever
8 Human Herpes Virus 8 kaposi sarcoma 3 Clinical Phases:
*Organisms that can cross placenta: toxoplasma gondii; rubella; cytomegalovirus;
herpes/HIV/Hepa B; syphilis (TrOCHeS – Toxoplasmosis, Other agents, Rubella, (1) Febrile Phase – occurs below D2 – D7 of illness
Cytomegalovirus, Herpes Simplex) (2) Critical Phase – occurs at D5 – D6 of illness; signs and
symptoms include: plasma leakage; bleeding;
severe organ involvement; can last for 24 – 48
hours
(3) Convalescence Period – recovery phase
PAGE 12 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Classification: Clinical Manifestations: morbilliform rashes all over
o Probable Dengue – recent travel/residency in a body; Koplik spots; opposite lower molar
place with dengue epidemic; fever + 2 of the Complications: otitis media – most common;
following: nausea/vomiting, rashes, muscle pneumonia – most fatal; sub sclerosing
aches/joint pains, mucosal bleeding, positive panencephalitis (SSPE) – chronic complication
tourniquet test – > 20 petechiae/sq. inch, CBCPC – Prevention: MMR vaccine – given at 9 months
leukopenia Pneumovirus – Respiratory Syncytial Virus (RSV) – clinical
o Dengue with Warning Signs – abdominal pain; manifestations: acute bronchiolitis (< 1 year old)
persistent vomiting; mucosal bleeding; clinical sign Filoviridae – thread-like virus
of plasma leakage (low BP); lethargy/restlessness; o Ebola Virus
liver enlagement (> 2 cm); laboratory confirmation MOT: direct contact to body fluids (ex. blood)
(↓platelets; ↑hematocrit) 5 Strains:
o Severe Dengue – severe hemorrhage/bleeding; a. Zaire & Sudan – most virulent; 2014 West Africa
severe plasma leakage; severe organ involvement Outbreak
(liver + kidneys) b. Tail Forest
Yellow Fever Virus c. Bundibugyo
Japanese Encephalitis Virus – most common cause of viral d. Reston – found in Philippines and China; sourced from
encephalitis in Asia; vector: culex mosquito Philippine Macaque Monkey; does not cause disease in
St. Louis Encephalitis Virus humans; disease in swines/pigs
Zika Virus Clinical Manifestations: severe bleeding in all outlets of
West Nile Fever Virus body
Hepacivirus – Hepatitis C o Marburg Virus – came from African Green Monkey
o Retroviridae – presence of reverse transcriptase (RNA Arenaviridae
DNA); promote effect of oncogenes o Lassa Virus – house rat
Human T Lymphocyte Virus (HTLV) – clinical o Tacaribe Complex – South American Hemorrhagic Fever
manifestations: leukemia Junin Virus – Argentine Hemorrhagic Fever
Human Immunodeficiency Virus (HIV) – tropism: helper T Machupo Virus – Bolivian Hemorrhagic Fever
cells; strains: (1) HIV 1 – Philippines; (2) HIV 2 – Africa Guanarito Virus – Venezuelan Hemorrhagic Fever
o Reoviridae – double stranded Sambia Virus – Brazilian Hemorrhagic Fever
Coltivirus – vector: dermacentor andersoni (tick); clinical Lymphocytic Choriomeningits (LCM) – house mouse
manifestations: Colorado tick fever/mountain fever Bunyaviridae – arbovirus
Rotavirus – most common cause of diarrheal illness in o Encephalitis – arbovirus; phlebo virus; la crosse virus
infants o Hemorrhagic Fever – Harta Virus; Dobrava Virus; Sin
Orbivirus Nombre Virus; Puumala Virus
RNA (-) SENSE – (ParFABOR) Orthomyxoviridae – influenza virus
o Paramyxoviridae o Influenza A – most antigenically unstable genetic
Respiro Virus rearrangement; cause of major epidemics; antigens:
a. Para Influenza Virus – aka laryngotracheobronchiolitis Haemaggglutinin (H); Neuraminidase (N)
(LTB); signs and symptoms: barking cough o Influenza B – may cause epidemics
Viral Group: 1, 2, 3 o Influenza C – most antigenically stable; does not cause
Mild URTI: 4 epidemics
Rubula Virus Rhabdoviridae
a. Mumps Virus o Rabies Virus – helical-bullet shape
Host: humans Incubation Period: 1 – 3 months (usual)
MOT: respiratory droplets Clinical Manifestations: rabies encephalitis – 100% fatal
Clinical Manifestations: infectious parotitis General Rule:
Complication: orchitis – inflammation of prostate a. Observation Period: 10 days
glands b. All suspected rabid animals should be sacrificed for
Mobili Virus autopsy
a. Measles – Rubeola c. Check for negri bodies for confirmation in autopsy
Host: humans Levels of Exposure
MOT: respiratory droplets a. Casual Contact – wash area with soap and water; do not
Prodromes: 3 C’s – cough, coryza, conjunctivitis give vaccine; do not give rabies immune globulin (RIG)
PAGE 13 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
b. Minor Scratches/Abrasions – wash area with soap and associated with infections of implants, prosthetic devices;
water; give vaccine; do not admin RIG catalase (+); coagulase (-)
c. Transdermal Wound – wash area with soap and water; o Staphylococcus saprophyticus – most common cause of
administer vaccine and RIG UTI in sexually active women
Streptococci
V. ANTIVIRALS o Streptococcus pneumonia – lancet shaped; capsulated
Treatment for Respiratory Viral Infection Quellung reaction
o Neuraminidase Inhibitors – (ex. Oseltamivir; Zanamivir); for Clinical Manifestations: bacterial pneumonia adults
influenza A, B Treatments: penicillins (amoxicillin); cephalosporins
o Inhibitors of Viral Uncoating – (ex. Amantadine; (cefuroxime)
Rimantadine); for influenza A o Streptococcus mutans – α-hemolysis; clinical
o Ribavirin – DOC for treatment of respiratory syncytial virus manifestations: dental carries
infection (RSV) in children; combine with interferon alpha sucrose -(fermentation)-> lactic acid -> destroys
for treatment for Hepatitis C enamel -> dental cones
Treatment for Hepatic Viral Infection – Interferon Alpha; o Viridans – α-hemolytic; causing subacute infective
Lamivudine – hepatitis B, HIV; Adefovir; Entecavir; Telbivudine endocarditis; treatment: pen G (DOC)
Treatment for Herpetic Viral Infection – Acyclovir; Cidofovir; o Streptococcus pyogenes – only group A, β-hemolytic
Ganciclovir – herpes resistant to Acyclovir; Foscarnet; Clinical Manifestations: most common cause of
Fumivirsen; Penaclovir; Famciclovir; Trifluridine bacterial pharyngitis, sore throat/strep throat
Treatment for Retroviral Infections Complications: peritonsilar abcess formation;
o Mode of Treatment functional otitis media; scarlet fever (2nd disease);
2 NRTI’s + 1 NNRTI’s rheumatic heart disease; acute glomerulonephritis
Lamivudine + Tenofovir + Efavirenz Treatments: penicillins (amoxicillin)
Lamivudine + Zidovudine + Efavirenz o Streptococcus agalactiae – group B, β-hemolytic; clinical
o Nucleoside Reverse Transcriptase Inhibitors (NRTI’s) – end manifestations: neonatal sepsis meningitis; normal flora
in –ine; (DAZZLE ST) in vagina
Didanosine; Abacavir; Zidovudine; Zalcitabine; Non-Spore Forming Aerobic Bacilli
Lamivudine; Emtricitabine; Stavudine; Tenofovir o Corynebacterium diptheriae – Chinese letter appearance
o Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTI’s) in microscope metachromatic granules (Babes-Ernest
– (NEED) Bodies); clinical manifestations: diphtheria – formation of
Nevirapine; Efavirenz; Etravirine; Delaviridine necrotic membrane, found in tonsil area, bull-neck
o Protease Inhibitors – end in –vir; (Trip sa SRI LANFA) appearance; Dacron Swab; DOC macrolides
Tripranavir; Saquinavir; Ritonavir; Indinavir; Lopenavir; (Erythromycin, Azithromycin); prevention: Diptheria
Ampenavir; Nelfinavir; Fosamprenavir; Alazanivir vaccine, Pentavax (1) D; (2) P (3) T; (4) Hep B; (5) Hib
o Entry Inhibitors – Enfaviritide; Maraviroc (Haemophilus Influenzae Type B)
o Integrase Inhibitors – Raltegravir o Listeria monocytogenes – clinical manifestations:
meningitis, granulomatosis infantiseptica; treatment:
V. BACTERIOLOGY penicillin (ampicillin)
I. GRAM POSITIVE Spore Forming Bacteria
Staphylococci o Bacillus (Aerobes)
o Staphylococcus aureus – acute infevtive endocarditis; Bacillus cereus
catalase (+); coagulase (+); most abundant: anterior nares; Clinical Manifestations: food poisoning
Clinical Types:
Manifestations: abcess formation – stye, furuncle, o Emetic Type – associated with contaminated fried
carbuncle; food poisoning – toxic producer rice
(enterotoxin), projective vomiting; toxic shock syndrome o Diarrheal Type – associated with saucy/meaty
– sepsis, toxic shock syndrome TTST-1 (toxin food
responsible), associated with child-bearing age women Bacillus anthracis – discovered by Robert Cobb; anthrax
that uses tampons; acute infective endocarditis; Forms:
osteomyelitis o Cutaneous Anthrax – most common form;
Treatment: penicillins necrotic tissue, black eschar
o Staphylococcus epidermis - most common microorganism o Pulmonary Anthrax – Woolsorter’s Disease;
on skin; most contaminant of laboratory samples; zoonotic disease; most fatal form of anthrax;
PAGE 14 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
widening of mediastinum (compartment of o PPD Skin Test/Tuberculin Skin Test – used to
thoracic cavity), death due to inability to breathe determine TB exposure; reading: after 48-72 hours
o Gastrointestinal Anthrax – rarest form; positive result = > 15 mm
treatment: antibiotic (ciprofloxacin) Culture: Lowenstein-Jenssen Media – used to determine
o Clostridium (Anaerobes) extrapulmonary TB
Clostridium botulinum – botolinum toxin (botox) Prevention: TB-DOTS
MOT: inhibition of 1o excitatory transfer neuron o 5 Pillars: (1) tool for diagnosis; (2) adequate drug supply;
(acetylcholine) (3) treatment partner; (4) LGU support; (5) proper
Clinical Manifestations: flaccid paralysis; floppy reading and monitoring
baby syndrome – associated with ingestion of o Follow Up: 2nd, 5th, 6th month of treatment
contaminated honey o Failure of Treatment: non-compliance for more than 2
Treatment: give antitoxin months
Clostridium tetani – tennis-racket shape;
tetanospasmin (toxin) III. GRAM NEGATIVE
MOT: inhibition of GABA and glycine = ↑Ach Spirochetes
Clinical Manifestations: spastic paralysis trismus o Treponema pallidum – MOT: sexual contact, child birth;
(lock jaw), sardonic smile, dysphagia/dyspnea, incubation period: 3 weeks; clinical manifestations: syphilis,
muscle stiffness, opisthotonus congenital syphilis
Treatment: antibiotic (metronidazole) – DOC Syphilis
Prevention: tetanus toxoid; antitetanus serum Stages:
Clostridium perfringens – alpha toxin (toxin); clinical o Primary – appearance of hard chancre (painless
manifestations: gas gangrene genital lesion/ulcer); inflammation of groin area;
Clostridium difficile – clinical manifestations: resolves after 1 week
pseudomembranous colitis; treatment: metronidazole o Secondary – latency period: asymptomatic;
(DOC) reactivation: rashes all over body
o Tertiary – multiorgan involvement; gumma
II. ACID-FAST formation
Mycobacterium – 1o component mycolic acid (waxy) Congenital Syphilis – ToRCHes; transmitted during 2nd
o Mycobacterium leprae trimester of pregnancy
Clinical Manifestations: leprosy; Hansen’s disease; STI Work Up: - Venereal Disease Research Laboratory
cutaneous tuberculosis (VDRL); Rapid Plasma Reagin (RPR); HIV test; Hepatitis
Forms: B Surface antigen (HBsAg)
TUBERCULOUS LEPROMATOUS Clinical Manifestations: still birth; intrauterine growth
Description small number of depressed cutaneous restriction (IUGR); congenital defects (saddle nose;
microorganisms sensation; large number of
microorganisms; Treatment:
hutchinson teeth; mulberry molars; scaphoid scapula;
dapsone (DOC); rifampicin; saber skin)
clofazimine Diagnosis: Serological Methods
Skin Lesion erythematous; flat nodular skin lesions found in
skin lesions well-ventilated parts of body o Non-Treponemal – screening: Veneral Disease
(ex. nose) Research Lab Method (VDRL); Rapid Plasma Reagin
Lepromin Test positive negative (RPR)
o Mycobacterium tuberculosis o Treponemal – confirmation: Treponema Pallidum
Clinical Manifestations: pulmonary TB; extrapulmonary TB Hemagglutination Assay (TPHA); Fluorescenth
Diagnosis: Treponemal Antibody Absorption (FTA-Abs)
Clinical Diagnosis – based on signs and symptoms Treatment: penicillin (DOC)
cough (> 2 weeks); unexplainable weight loss; low o Leptospira interoggans – MOT: direct contact with
grade fever; night sweats; chest pain/back pain; leptospire infected urine; clinical manifestation:
hemoptysis leptospirosis
Laboratory Diagnosis Classifications:
o Direct Sputum Smear Microscopy (DSSM) – gold Suspected Leptospirosis
standard; submit 2 samples (consecutive days); Anicteric Leptospirosis – mild
positive result = at least 1 sample has acid-fast Icteric Leptospirosis – severe; aka Weil’s Disease;
bacillus triad: jaundice, hemorrhage, proteinuria
o Chest X-Ray (PAIL)
PAGE 15 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Treatment: doxycycline (DOC prophylaxis and mild); trachoma; lymphogranuloma vencreum (LGV); STI:
pen G (severe) urethritis, cervicitis, precititis, epidydimitis
o Borrelia Treatment: tetracycline (ex. doxycycline)
Borrelia burgodoferi – vector: tick; clinical manifestations: o Chalmydophila
Lyme Disease – bull’s eye appearance (tick bite) Chlamydia psittaci – clinical manifestations: psittacosis
Borrelia recurrentis – clinical manifestations: relapsing Chlamydia pneumoniae
fever Mycoplasma and Ureaplasma
Forms: o Mycoplasma pneumoniae – wall-less; pleomorphic
o Epidemic – body louse (vector); humans (host) 1o component – sterols
o Endemic – ticks (vector); rodents (host) Staining Method: Diene’s Staining; colony: fried egg
Neisseriae colony
o Neisseriae gonorrhea – gram (-); intracellular; diplococcic Clinical Manifestations: walking pneumonia
MOT: sexual contact (1o); child birth Treatment: tetracycline (DOC)
Risk of Infection: o Ureaplama urealyticum – clinical manifestation: non-
Men – 20%; asymptomatic gonococcal urethritis in men
Women – 50%; symptomatic Enterobacteriaceae
Clinical Manifestations: Pelvic Inflammatory Disease o Shigella
(PID); opthalmia neonatorum – blindness: < 24 hours; STI Causative Agent: shigella dysenteriae; s. flexneri; s. sonnei;
– urethritis, epidydimitis, cervicitis s. boydii
Treatment: ceftriaxone; cefixime; azithromycin MOT: fecal-oral (associated with improper hand washing)
o Neisseria meningitides – gram (+); diplococci; coffee Clinical Manifestation: bloody dysentery – scanty stool
bean/kidney shape; clinical manifestations: meningitis; with blood and mucus
meningococcemia – fulminant stage (purpura fulminans – Treatment: ampicillin (DOC)
large ecchymoses bullae) o Salmonella typhii
Bordetella Pertussis – strict aerobe MOT: ingestion of contaminated poultry products (ex.
o Selective Media: Bordet-Gengou Media; colony: mercury chicken; eggs)
drop colony Clinical Manifestations: bacterial gastroenteritis ot
o Clinical Manifestations: pertussis – whooping cough salmonellosis; typhoid fever – enteric fever rose spots
Stages: (1) paroxysmal; (2) catarrhal – infectious; toxin – samon colored; blanching maculopapular rashes
production Treatment: empirical therapy – ceftriaxone;
o Treatment: macrolides (ex. azithromycin) azithromycin; severe typhoid fever – ciprofloxacin (1st
o Prevention: DPT vaccine line)
Haemophilus o Escherichia coli – most common cause of UTI
o Haemophilus infuenzae Strains:
Humans: Type B (Hib) ETEC – enterotoxigenic; associated with Traveller’s
Clinical Manifestations: pneumonia (infants); meningitis; Diarrhea
sepsis; osteomyelitis EPEC – enteropathogenic; associated with infantile
Prevention: H influenza b conjugate vaccine diarrhea in 3rd world countries
Treatment: vaccination EIEC – enteroinvasive; associated with shigella-like
Complete – penicillin (pen G) diarrhea
Incomplete – penicillin (ampicillin) EAEC – enteroaggregative; associated with diarrhea in
o Haemophilus ducreyi – appears like a school of red fish; immunocompromised individuals
MOT: sexual contact; clinical manifestations: soft EHEC – enterohemorrhagic; aka O157:H7 strain;
chancre/chancroid – painful genital ulcer/lesion; treatment: hemolytic uremic syndrome (HUS)
ceftriaxone (DOC), cefixime Pseudomonas aeruginosa – obligate aerobe; oxidase (+)
Chlamydia o Clinical Manifestations: wound infection/burn wound
o Chlamydiae infection (pigment: pyocyanin, pyoverdin; odor: grape-
Chlamydia trachomatis like/sweet-taco-corn like); sepsis – skin lesion: ecthyma
MOT: sexual contact (1o); child birth gangeonosum; pneumonia atypical
Risks of Infection: men symptomatic; women o Treatment: penicillin (ex. carbenicillin; ticarcillin;
asymptomatic piperacillin); cephs (ex. ceftazidine; cefoperazone)
Clinical Manifestations: pelvic inflammatory disease;
ophthalmia neonatorum; blindness: > 72 hours;
PAGE 16 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Campylobacter and Helicobacter CAUSATIVE
AGENT
MOT CLINICAL
MANIFESTATION
TREATMENT
o Campylobacter jejuni – j-shape/gull-wing shape; MOT: Amebiasis Entamoeba fecal-oral amebic dysentery; Metronidazole
histolytica amebic liver abcess (DOC);
fecal-oral; clinical manifestation: bloody diarrhea; Entamoeba Tinidazole;
dispar Iodoquinol
treatment: macrolides (ex. azithromycin) Fresh Water Naegleria fowleri Primary amebic meningoencepalopathy
Amoeba (PAM)
o Helicobacter pylori – urease (+) Acanthamoeba castellani Granulomatous amebic encephalopathy
Clinical Manifestations: gastric carcinoma; peptic ulcer (GAE)
Giardiasis Giardia fecal-oral traveller’s diarrhea; Metronidazole
disease (gastric – 70%, nocturnal pain; duodenal – 90%, lamblia gay bowel syndrome (DOC)
abdominal pain; foul
pain is relieved by food obese patients) –smelling diarrhea;
malabsorption of
Diagnosis: endoscopy – gold standard; urea breathe test adek (steatorrhea)
Cyclosporidiasis Cylcospora ingestion of abdominal pain; Co-Trimoxazole
– urea –(urease)-> ammonia cayetanensis cyst- nausea and vomiting; (DOC)
Treatment: contaminated diarrhea
fruits and
Monotherapy vegetables
Trichomoniasis Trichomonas sexual contact dysuria; burning Metronidazole
Double Therapy vaginalis sensation during (DOC)
urination; severe
Triple Therapy – PPI + 2 ABX (clarithromycin; vaginal pruritis;
yellow-green/yellow
amoxicillin; metronidazole) curdy vaginal
Quadriple Therapy – PPI + 2 ABX + surface coating discharge with fishy
odor
agent (sucralfate; rebamipide) Toxoplasmosis Toxoplamsa inhalation of cervical Sulfadiazine +
gondii cyst from cat’s lymphadenopathy; Pyrimethamine
Vibrionaceae feces; ingestion retinitis (DOC);
of raw pork Clindamycin
o Vibrio cholerae (Alternative)
MOT: fecal-oral Malaria Vector: anopheles mosquito (female)
Causative Agent: Plasmodium spp.
Clinical Manifestations: cholera – osmotic type diarrhea Plasmodium falciparum – 50%; most virulent; malignant tertian malaria
Plasmodium vivax – 40%; benign tertian malaria
rice watery stool Plasmodium malaria – 10%; quartan malaria
Plasmodium ovale – rarest form; benign tertian malaria
Diagnosis: selective media TCBS – colony: yellow Life Cycle:
sporozoites merozoites (liver) ↔ trophozoites (erythrocytes) gametocytes
colony Treatment:
Treatment: fluoroquinolones (ex. ciprofloxacin) chloroquine + Fansidar® (sulfadoxine + pyrimethamine) – DOC as first line
agent for P. falciparum non-resistant and severe
o Vibrio parahemolyticus – MOT: ingestion of raw shell fish; arthemeter + lumenfantrine – DOC as second line treatment for plasmodium
resistant to first line
clinical manifestations: cholera-like diarrhea; TCBS: green quinine + doxycycline – DOC as third line agent for SEVERE malaria
primaquine – radical cure; DOC to prevent transmission and relapse
colony chloroquine – DOC for erythrocytic stage of malaria; DOC for P. vivax
o Vibrio vulnificus – clinical manifestations: mild URTI, wound Leishmaniasis Vector: sand fly
Causative Agent: Leishmania spp.
infection; TCBS: blue-green colony Leishmania tropica, L. Mexicana – cutaneous leishmaniasis
Leishmania brasiliensis – mucocutaneous leishmaniasis (espundia)
Leishmania donovani, L. chagasi – visceral leishmaniasis (Kala-azar)
Treatment: Stibogluconate
VI. PARASITOLOGY Trypanosiomasis
African Trypanosoma tse-tse fly West African Non-Nervous:
Branches protozoology & helminthology Trypanosomiasis brucei Suramin,
gambiense Pentamidine
Trypanosoma East African Nervous:
brucei Melarsprol
I. PROTOZOAN – unicellular; free-living rhodesiens
Phyla: American
Trypanosomiasis
Typanosoma
cruzi
kissing bug Chaga’s disease Nifurtimox;
Benznidazole
o Sarcomastigophora
Sarcodina > Pseudopods II. HELMINTHOLOGY
Mastigophola > Flagella Platyhelminthes – flatworms; trematodes (flukes); cestodes
o Cillophora – cilia; (ex. Balantidium coli – spherical shape (tapeworm)
ulcer) Roundworms – nematodes
o Apicomplexa
o Microspora I. NEMATODES
CAUSATIVE MOT CLINICAL TREATMENT
AGENT MANIFESTATION
Ascariasis – aka Ascaris ingestion of eggs Albendazole;
giant intestinal lumbricoides Mebendazole
roundworm
Strongloidiasis Stronglyoides direct massive Ivermectin
– aka thread stercoralis penetration into autoinfection
worm skin of larvae
Hookworm Necator direct iron deficiency Albendazole;
americanus penetration of anemia Mebendasone
(New World); larvae into skin
Ancylostoma
duodenale
(Old World)
Trichinellosis Trichinella ingestion of eggs muscle aches Albendazole;
spiralis encysted in raw Mebendazole
pork
PAGE 17 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
Whip Worm Trichuris ingestion of eggs rectal prolapse Albendazole;
trichiuria Mebendazole
Enterobiasis Enterobius ingestion of eggs severe nocturnal Pyrantel pamoate;
vermicularis perianal itching Albendazole;
(Human Diagnosis: scotch
Pinworm) tape swab test
Onchocerca Onchocerca black fly (vector) river blindness Ivermectin
Volvus Volvus
Filiriasis Wuchereria mosquito bites elephantiasis; Diethylcarbamazine
bancrofti; tropical
Brugia eosinophilia
malayi
II. TREMATODES
Schisotomiasis
o Causative Agent: Schistosoma japonicum; S. mansoni (liver);
S. haematobium (urinary bladder)
o MOT: direct penetration of cercariae into skin
o Clinical Manifestations: swimmer’s itch; katayama fever;
liver cirrhosis; portal HTN ascites
o Treatment: praziquantel
III. CESTODES
COMMON MOT CLINICAL TREATMENT
NAME MANIFESTATION
Taenia solium pork Ingestion of raw neurocystecercosis Niclosamide;
tapeworm pork Praziquantel
Taenia saginata beef Ingestion of raw GI disturbances Praziquantel
tapeworm beef
Diphyllobothrium fish ingestions of eggs Vitamin B12 Praziquantel
latum tapeworm raw fish deficiency
Hymenolepis dwarf ingestion of eggs Praziquantel
nana tapeworm
PAGE 18 OF 18 © MANOR REVIEW CENTER NOTES (K.L)
You might also like
- R.A. 6675Document91 pagesR.A. 6675Donzzkie Don50% (2)
- Phle Reviewer Module 6 Qa QCDocument66 pagesPhle Reviewer Module 6 Qa QCMARIA FREDIJEAN CARIÑONo ratings yet
- Pattaguan, Donesthel M PDFDocument2 pagesPattaguan, Donesthel M PDFDonzzkie DonNo ratings yet
- Module 4 - PharmacologyDocument53 pagesModule 4 - PharmacologyDonzzkie Don100% (3)
- R.A. 8344Document16 pagesR.A. 8344Donzzkie DonNo ratings yet
- Part 10 ProkaryoticDocument54 pagesPart 10 ProkaryoticLê Thanh HằngNo ratings yet
- Kingdoms WorksheetsDocument5 pagesKingdoms WorksheetsTessNo ratings yet
- OkieDocument3 pagesOkieFebeval CastilloNo ratings yet
- Chapter 1Document20 pagesChapter 1Guy SebNo ratings yet
- Nmat Biology Cell Biology 1.1 Eukaryotic & Prokaryotic CellsDocument12 pagesNmat Biology Cell Biology 1.1 Eukaryotic & Prokaryotic Cellssavina100% (1)
- Leson 6Document2 pagesLeson 6Idk UlitNo ratings yet
- SDL - Cell Structure and Function in BacteriaDocument3 pagesSDL - Cell Structure and Function in Bacteriagovicky565No ratings yet
- Prokaryotic and Eukaryotic Cells ReviewerDocument5 pagesProkaryotic and Eukaryotic Cells ReviewerAnna Kathleen LimNo ratings yet
- Cabucana, Paul Lester Finals BacteDocument91 pagesCabucana, Paul Lester Finals BactePaul LesterNo ratings yet
- Endosymbiotic TheoryDocument9 pagesEndosymbiotic TheoryFrancisco CañonNo ratings yet
- Bacterial Cell Structure: BacteriaDocument5 pagesBacterial Cell Structure: BacteriaHassan AljaberiNo ratings yet
- MicroPara Lesson 3 - ReviewerDocument5 pagesMicroPara Lesson 3 - Reviewerrobelynjoy.alparo.cvtNo ratings yet
- 3-Prokaryotic - Eukaryotic MicroorganismsDocument16 pages3-Prokaryotic - Eukaryotic Microorganismsguestiam29No ratings yet
- Reviewer On EukaryotesDocument6 pagesReviewer On EukaryotesAlaica Joice B. JaboneteNo ratings yet
- Domain Bacteria Domain Archaea Domain Eukarya Structure and Organization of Genetic MaterialDocument2 pagesDomain Bacteria Domain Archaea Domain Eukarya Structure and Organization of Genetic MaterialAaron AsneNo ratings yet
- Zoology Lec Module 3Document6 pagesZoology Lec Module 3Camille AlzolaNo ratings yet
- Chapter 1 Basic Biology For Engineer: Microbial Diversity Taxonomy Cell Naming Gram StainDocument42 pagesChapter 1 Basic Biology For Engineer: Microbial Diversity Taxonomy Cell Naming Gram StainDivyashini MohanNo ratings yet
- Biology QuicksheetsDocument11 pagesBiology QuicksheetsMaria Renee Lian Noble100% (1)
- Chapter-2-Prokaryotes-and-Eukaryotes-MICROBIOLOGY AND PARAASITOLOGYDocument2 pagesChapter-2-Prokaryotes-and-Eukaryotes-MICROBIOLOGY AND PARAASITOLOGYIsaiah PascuaNo ratings yet
- Cell UltrastructureDocument5 pagesCell UltrastructureIrish Mae LunaNo ratings yet
- Session 1: Transmission Electron MicroscopesDocument13 pagesSession 1: Transmission Electron MicroscopesFerell GerryNo ratings yet
- (Zoolone) Animal CellDocument5 pages(Zoolone) Animal CellRenee Margarette GrapilonNo ratings yet
- Micro Chapter 2Document34 pagesMicro Chapter 2Farrah GwynethNo ratings yet
- BIO104E-Laboratory Activity. (The Cell)Document5 pagesBIO104E-Laboratory Activity. (The Cell)Stephen AzaresNo ratings yet
- P1 General Properties of VirusesDocument40 pagesP1 General Properties of VirusesLoren EscotoNo ratings yet
- Morphology of BacteriaDocument44 pagesMorphology of BacteriaDr Harender SimarNo ratings yet
- CH 16Document24 pagesCH 16Zachary0HendrixNo ratings yet
- MICROBIOLOGYDocument5 pagesMICROBIOLOGYCia RraNo ratings yet
- Cheatt Sheet #2Document2 pagesCheatt Sheet #2layanhaliloNo ratings yet
- Cell Unit of Life - 011321Document73 pagesCell Unit of Life - 011321abhishek KumarNo ratings yet
- Genbio NotesDocument10 pagesGenbio NotesD-B02 Ancheta IanNo ratings yet
- Lesson 4Document3 pagesLesson 4Samantha VeraNo ratings yet
- BahanKuliah BiologiMolekuler JasadHidupSelulerDocument43 pagesBahanKuliah BiologiMolekuler JasadHidupSelulerMochamad Untung Kurnia AgungNo ratings yet
- 01-02 Microbiology - The Science of Microbiology and Cell StructureDocument6 pages01-02 Microbiology - The Science of Microbiology and Cell StructureJanet SantosNo ratings yet
- Cell Structure 3Document3 pagesCell Structure 3Lisa LuNo ratings yet
- Plant Cell LabelDocument1 pagePlant Cell LabelAllen TagatacNo ratings yet
- Biology and Biochemistry ReviewerDocument45 pagesBiology and Biochemistry ReviewerArviNo ratings yet
- The Cell: Exercise 2Document5 pagesThe Cell: Exercise 2Jasmine Nicole EnriquezNo ratings yet
- (PARA) 1.5 - Blood and Tissue FlagellatesDocument6 pages(PARA) 1.5 - Blood and Tissue FlagellatesGuia De GuzmanNo ratings yet
- Ruling The World: Microbial DiversityDocument47 pagesRuling The World: Microbial Diversityss2945No ratings yet
- Cell Structures and FunctionsDocument3 pagesCell Structures and FunctionsLea IoaNo ratings yet
- Bacteria: Prokaryotes EukaryotesDocument4 pagesBacteria: Prokaryotes EukaryotesJerson Aizpuro SuplementoNo ratings yet
- Lecture 1 Bacterial StructureDocument38 pagesLecture 1 Bacterial StructureAyat MostafaNo ratings yet
- NMAT Part II Reviewer - PersonalDocument38 pagesNMAT Part II Reviewer - PersonalReycel MayNo ratings yet
- Cloroplastos y Peroxisomas: Sitios WEB para EstudiarDocument20 pagesCloroplastos y Peroxisomas: Sitios WEB para EstudiarNicolas Ignacio Aliaga MachucaNo ratings yet
- The Cell and Its BeginningDocument6 pagesThe Cell and Its BeginningZarc VenturaNo ratings yet
- BIO104E - Laboratory Activity (The Cell)Document5 pagesBIO104E - Laboratory Activity (The Cell)Stephen AzaresNo ratings yet
- Bacillus SPP Dormant: Clinical Bacteriology LecDocument5 pagesBacillus SPP Dormant: Clinical Bacteriology LecJamie BartolomeNo ratings yet
- Cell: The Unit of Life: Chapter - 00Document32 pagesCell: The Unit of Life: Chapter - 00athuNo ratings yet
- As-Level Biology Notes: By: Bianca HimawanDocument65 pagesAs-Level Biology Notes: By: Bianca HimawanLauren ChikwehwaNo ratings yet
- Viruses: Key Characteristics!Document7 pagesViruses: Key Characteristics!Melody Jane PardilloNo ratings yet
- Phagocyte System.: Innate/non-Specific Immune SystemDocument6 pagesPhagocyte System.: Innate/non-Specific Immune SystemAngela ReyesNo ratings yet
- Assignment 7thDocument20 pagesAssignment 7thMuhammad kamran khanNo ratings yet
- 2 - CellDocument44 pages2 - CellNorie palmesNo ratings yet
- Biology Prelim Notes Module 1-4Document54 pagesBiology Prelim Notes Module 1-4kkanaksingh124No ratings yet
- Cellular PhysiologyDocument32 pagesCellular Physiologyانس ابوهيبة0% (1)
- Isolating, Cloning and Sequencing Dna: B. Applications SyllabusDocument7 pagesIsolating, Cloning and Sequencing Dna: B. Applications SyllabusNicholas OwNo ratings yet
- Microbiology: a QuickStudy Laminated 6-Page Reference GuideFrom EverandMicrobiology: a QuickStudy Laminated 6-Page Reference GuideNo ratings yet
- Transfer Factors: Properties, Mechanism of Action and Its Clinical ApplicationsFrom EverandTransfer Factors: Properties, Mechanism of Action and Its Clinical ApplicationsNo ratings yet
- DiarrheaDocument22 pagesDiarrheaDonzzkie DonNo ratings yet
- VirologyDocument31 pagesVirologyDonzzkie DonNo ratings yet
- Department of BiochemistryDocument16 pagesDepartment of BiochemistryDonzzkie DonNo ratings yet
- Aspects of DeathDocument45 pagesAspects of DeathDonzzkie DonNo ratings yet
- Understand The ProblemDocument1 pageUnderstand The ProblemDonzzkie DonNo ratings yet
- Schwartz's Principles of Surgery ABSITE and Board Review, Ninth Edition (PDFDrive)Document517 pagesSchwartz's Principles of Surgery ABSITE and Board Review, Ninth Edition (PDFDrive)Donzzkie Don100% (1)
- Pico Format Population Exposure OutcomeDocument4 pagesPico Format Population Exposure OutcomeDonzzkie DonNo ratings yet
- Third Paragraph On PHYSICAL ACTIVITYDocument1 pageThird Paragraph On PHYSICAL ACTIVITYDonzzkie DonNo ratings yet
- Chapter 6: Microbial GrowthDocument9 pagesChapter 6: Microbial GrowthDonzzkie DonNo ratings yet
- Module 6 - Microbiology and ParasitologyDocument35 pagesModule 6 - Microbiology and ParasitologyDonzzkie DonNo ratings yet
- A Case On Typhoid Fever: Group 4Document27 pagesA Case On Typhoid Fever: Group 4Donzzkie DonNo ratings yet
- Density, Specific Gravity, and Specific Volume PDFDocument22 pagesDensity, Specific Gravity, and Specific Volume PDFDonzzkie Don100% (1)
- R.A. 10354Document36 pagesR.A. 10354Donzzkie Don100% (5)
- Group 3 Drug LitDocument79 pagesGroup 3 Drug LitDonzzkie DonNo ratings yet
- Mod 5 - Phardose PDFDocument7 pagesMod 5 - Phardose PDFDonzzkie DonNo ratings yet
- February 7,1992: " Senior Citizens Act"Document98 pagesFebruary 7,1992: " Senior Citizens Act"Donzzkie DonNo ratings yet
- R.A. 7581Document34 pagesR.A. 7581Donzzkie DonNo ratings yet
- R.A. 7394Document62 pagesR.A. 7394Donzzkie DonNo ratings yet
- June 6, 2008: Gloria Macapagal - ArroyoDocument39 pagesJune 6, 2008: Gloria Macapagal - ArroyoDonzzkie DonNo ratings yet
- R.A. 9502Document39 pagesR.A. 9502Donzzkie DonNo ratings yet
- Counseling Chronically Ill Adults in The HealthcarDocument19 pagesCounseling Chronically Ill Adults in The HealthcarDonzzkie DonNo ratings yet
- R.A. 10354Document36 pagesR.A. 10354Donzzkie DonNo ratings yet
- 1 Prescription FinalDocument62 pages1 Prescription FinalDonzzkie DonNo ratings yet
- Rational Drug Design PDFDocument7 pagesRational Drug Design PDFDonzzkie DonNo ratings yet
- Aseptic TechniquesDocument26 pagesAseptic TechniquesDonzzkie DonNo ratings yet
- The Effect of Antioxidants On Micropropagation of Avocado by Nodal SegmentsDocument6 pagesThe Effect of Antioxidants On Micropropagation of Avocado by Nodal SegmentsbryanNo ratings yet
- BioboxDocument1 pageBioboxJesúsNo ratings yet
- 2021 Molecular Basis of Prostate Cancer. FixDocument40 pages2021 Molecular Basis of Prostate Cancer. FixIrfandi AmiruddinNo ratings yet
- Harvesting Stage & Grades of Gerbera & Tube RoseDocument21 pagesHarvesting Stage & Grades of Gerbera & Tube RoseSantagriNo ratings yet
- Notice: Endangered and Threatened Species: Columbia River Salmon and Steelhead Recovery PlanDocument6 pagesNotice: Endangered and Threatened Species: Columbia River Salmon and Steelhead Recovery PlanJustia.comNo ratings yet
- Module 25 Edited Pages DeletedDocument12 pagesModule 25 Edited Pages DeletedDos DosNo ratings yet
- New Plant Breeding Techniques. State-Of-The-Art and Prospects For Commercial DevelopmentDocument220 pagesNew Plant Breeding Techniques. State-Of-The-Art and Prospects For Commercial DevelopmentJulian Andres Tovar MedinaNo ratings yet
- Buffer System For NursingDocument2 pagesBuffer System For NursingjasonNo ratings yet
- Georges Cuvier's Theory of Correlation of PartsDocument5 pagesGeorges Cuvier's Theory of Correlation of PartsSoc SaballaNo ratings yet
- Miniaturization of Rectangular Microstrip Patches Using Genetic AlgorithmsDocument4 pagesMiniaturization of Rectangular Microstrip Patches Using Genetic AlgorithmsSubba Rao ChalasaniNo ratings yet
- Prevention and Treatment of Moderate and Severe Ovarian Hyperstimulation Syndrome NoprintDocument14 pagesPrevention and Treatment of Moderate and Severe Ovarian Hyperstimulation Syndrome NoprintDo le QuangNo ratings yet
- SGBAU B.Pharm 1 SEM Human-Anatomy-n-Physiology-I 2018Document2 pagesSGBAU B.Pharm 1 SEM Human-Anatomy-n-Physiology-I 2018Abhay DeulkarNo ratings yet
- Amniotic Fluid Index (AFI) - StatPearls - NCBI BookshelfDocument2 pagesAmniotic Fluid Index (AFI) - StatPearls - NCBI BookshelfTarzan SmithNo ratings yet
- EL 108 Midterm Module 1Document22 pagesEL 108 Midterm Module 1Ella Marie Gamayon PoloNo ratings yet
- Okavango Delta Valuation Study FINAL REPORTDocument139 pagesOkavango Delta Valuation Study FINAL REPORTAse JohannessenNo ratings yet
- Genetically Engineered CropsDocument3 pagesGenetically Engineered Cropsapi-273084430No ratings yet
- Jerry Sudarsky, Wasco Inventor and HumanitarianDocument24 pagesJerry Sudarsky, Wasco Inventor and HumanitarianGilbert GiaNo ratings yet
- The Novice Nurse's Guide To Calling "Code Blue": Wayne Thomas Brice, MA, RN-BCDocument5 pagesThe Novice Nurse's Guide To Calling "Code Blue": Wayne Thomas Brice, MA, RN-BCniraNo ratings yet
- Periodontal LigamentDocument3 pagesPeriodontal LigamentCzarina DavidNo ratings yet
- Penile Cancer 2010Document28 pagesPenile Cancer 2010raghavagummadiNo ratings yet
- Module 2. Content Module Topic: Cell Cycle and Cell DivisionDocument5 pagesModule 2. Content Module Topic: Cell Cycle and Cell DivisionErolin PobleteNo ratings yet
- Bacteria ClassificationDocument395 pagesBacteria ClassificationJitendra MishraNo ratings yet
- MamosaceaeDocument12 pagesMamosaceaeBashir KhanNo ratings yet
- PAT BAHASA INGGRIS KELAS 6 SMT 2Document2 pagesPAT BAHASA INGGRIS KELAS 6 SMT 2mira ardeatikaNo ratings yet
- Franchinietal - Physiological Characteristics of Karate AthletesDocument9 pagesFranchinietal - Physiological Characteristics of Karate AthletesMiodragNo ratings yet
- Breeding ProgramDocument13 pagesBreeding ProgramgabNo ratings yet
- Fischer-Mamblona 2000Document14 pagesFischer-Mamblona 2000Gizem KaymakçıNo ratings yet
- Chapter 25: The Urinary System: Page 19 of 25Document1 pageChapter 25: The Urinary System: Page 19 of 25JAGDEV PANESARNo ratings yet
- Blood Storage Centre Standards Edition 1Document55 pagesBlood Storage Centre Standards Edition 1bloodstoragecentersuryaNo ratings yet
- Dairy Whole Dairy Packet 1 WorksheetsDocument14 pagesDairy Whole Dairy Packet 1 WorksheetsMoonkhan BlessedNo ratings yet