Professional Documents
Culture Documents
BreastCare - 2015 10320 324
BreastCare - 2015 10320 324
Uploaded by
Rohit MaldeCopyright:
Available Formats
You might also like
- 4 Types of Symmetry in The PlaneDocument5 pages4 Types of Symmetry in The PlaneRohit MaldeNo ratings yet
- NSAIDDocument1 pageNSAIDShubhangiNo ratings yet
- Bioavailability PK Practice Problems 2013Document2 pagesBioavailability PK Practice Problems 2013Linh PhamNo ratings yet
- The Role of Hypofractionated Radiotherapy in ProstDocument10 pagesThe Role of Hypofractionated Radiotherapy in ProstАнастасия АнохинаNo ratings yet
- Uganda - CervixDocument9 pagesUganda - CervixDaniel PalmeraNo ratings yet
- 5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021Document10 pages5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021hugo francisco romero anduagaNo ratings yet
- Radiation Treatment For Breast CancerDocument13 pagesRadiation Treatment For Breast CancerZuriNo ratings yet
- PublicacionDocument5 pagesPublicacionNoelia Peirats AymerichNo ratings yet
- Breast RTH 2020Document10 pagesBreast RTH 2020Sara HossamNo ratings yet
- Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer – A study based on the EORTC trial 22881–10882 ‘boost versus no boost’ / European Journal of Cancer Collette, 2008Document13 pagesPredictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer – A study based on the EORTC trial 22881–10882 ‘boost versus no boost’ / European Journal of Cancer Collette, 2008saipraveen03No ratings yet
- Clinical and Translational Radiation Oncology: Original Research ArticleDocument6 pagesClinical and Translational Radiation Oncology: Original Research ArticleGörkem TürkkanNo ratings yet
- Aoki 2002Document10 pagesAoki 2002Drsaumyta MishraNo ratings yet
- Prophylactic Irradiation To The Contralateral BreaDocument6 pagesProphylactic Irradiation To The Contralateral Breaashnamuni07No ratings yet
- Pi Is 0360301611018256Document1 pagePi Is 0360301611018256Olyndo IwanNo ratings yet
- Hypofractionation in The Real World Rodin 2021Document8 pagesHypofractionation in The Real World Rodin 2021Gloribel BolívarNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyTit fuckerNo ratings yet
- Head NeckDocument8 pagesHead NeckerandolphsavageNo ratings yet
- Update On Radiotherapy in Gynaecological Malignancies: ReviewDocument8 pagesUpdate On Radiotherapy in Gynaecological Malignancies: ReviewDesrha TangdiseruNo ratings yet
- Hypofractionated Postmastectomy RadiationDocument8 pagesHypofractionated Postmastectomy RadiationEmin PehlivanogluNo ratings yet
- 2019 Article 5894 PDFDocument8 pages2019 Article 5894 PDFGalgalo GarbichaNo ratings yet
- Vaginal Dose Is Associated With Toxicity in Image Guided Tandem Ring or Ovoid-Based BrachytherapyDocument7 pagesVaginal Dose Is Associated With Toxicity in Image Guided Tandem Ring or Ovoid-Based BrachytherapyFlor ZalazarNo ratings yet
- Clinical Oncology: EditorialDocument3 pagesClinical Oncology: EditorialSyed HossainNo ratings yet
- Radiotherapy and Oncology: Brachytherapy of Cervical CancerDocument8 pagesRadiotherapy and Oncology: Brachytherapy of Cervical CancerodivarNo ratings yet
- Brachytherapy in The Treatment of Cervical CancerDocument10 pagesBrachytherapy in The Treatment of Cervical CancervchendilNo ratings yet
- Din 2013Document5 pagesDin 2013Med MedNo ratings yet
- 15 20a BartelinkDocument10 pages15 20a Bartelink980Denis FernandezNo ratings yet
- Radiotherapy and OncologyDocument5 pagesRadiotherapy and Oncologyhugo francisco romero anduagaNo ratings yet
- Endometrial Cancer - Reduce To The Minimum. Anew Paradigm For Adjuvant Treatments?Document6 pagesEndometrial Cancer - Reduce To The Minimum. Anew Paradigm For Adjuvant Treatments?najmulNo ratings yet
- Radiotherapy and Oncology: Original ArticleDocument8 pagesRadiotherapy and Oncology: Original ArticleJuancarlos Pari SalasNo ratings yet
- Special ArticleDocument21 pagesSpecial ArticleAhana MukherjeeNo ratings yet
- Systemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewDocument11 pagesSystemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewLorena Sánchez PérezNo ratings yet
- s13014 015 0495 4Document6 pagess13014 015 0495 4produxing 101No ratings yet
- Final CapstoneDocument11 pagesFinal Capstoneapi-603721790No ratings yet
- Brachytherapy in The Treatment of Breast CancerDocument10 pagesBrachytherapy in The Treatment of Breast CancerwahidNo ratings yet
- 10 1016@j Ejca 2019 10 025Document8 pages10 1016@j Ejca 2019 10 025habib diopNo ratings yet
- 10.1007@s00066 021 01782 5Document8 pages10.1007@s00066 021 01782 5Alberto GonzalesNo ratings yet
- Analysis of Compliance, Toxicity and Survival WeeklyDocument11 pagesAnalysis of Compliance, Toxicity and Survival Weeklydanu20No ratings yet
- Eport Res PaperDocument13 pagesEport Res Paperapi-309296181No ratings yet
- BCTT 15 721Document10 pagesBCTT 15 721Annisya MaharaniNo ratings yet
- 10 14338 - Ijpt-22-00041 1Document12 pages10 14338 - Ijpt-22-00041 1Raul Matute MartinNo ratings yet
- Theraphy RadDocument4 pagesTheraphy RadMega PuspitaNo ratings yet
- F - 3602 BCBCR Dose Distribution in The Heart and Cardiac Chambers Following 4 Field .PDF - 4865Document9 pagesF - 3602 BCBCR Dose Distribution in The Heart and Cardiac Chambers Following 4 Field .PDF - 4865Windy HardiyantyNo ratings yet
- Jco 2007 11 4991Document7 pagesJco 2007 11 4991brasilianaraNo ratings yet
- Principles of Chemotherapy and Radiotherapy PDFDocument7 pagesPrinciples of Chemotherapy and Radiotherapy PDFNora100% (3)
- Intensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningDocument8 pagesIntensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningAlberto GonzalesNo ratings yet
- Final CompleteDocument11 pagesFinal Completeapi-575843507No ratings yet
- Healthcare 07 00120Document9 pagesHealthcare 07 00120Ryantino IrdanNo ratings yet
- September 2013 - Radiotherapy For Localised Prostate Cancer - DR V KhooDocument4 pagesSeptember 2013 - Radiotherapy For Localised Prostate Cancer - DR V KhooHyago FrançaNo ratings yet
- Pub Paediatric Imaging Manual Notes in RadiologyDocument167 pagesPub Paediatric Imaging Manual Notes in RadiologydrAlbertoVV100% (1)
- Breast Cancer Notes Part 2Document60 pagesBreast Cancer Notes Part 2Tony YongNo ratings yet
- Vestibular Schwannoma Results of HypofractionatedDocument14 pagesVestibular Schwannoma Results of HypofractionatedTimothy CaldwellNo ratings yet
- RT en Pancreas Horowitz 2021Document2 pagesRT en Pancreas Horowitz 2021Carlos N. Rojas PuyolNo ratings yet
- Radiation Therapy and Esophageal CancerDocument14 pagesRadiation Therapy and Esophageal Cancerkrsna2studyNo ratings yet
- Rinky 712024 AORJ113575Document7 pagesRinky 712024 AORJ113575sazzad suvroNo ratings yet
- Wa0024 PDFDocument5 pagesWa0024 PDFmr copy xeroxNo ratings yet
- 1 s2.0 S2405632423000197 MainDocument11 pages1 s2.0 S2405632423000197 Mainsaros22568No ratings yet
- Comparison of Carbon Ion and Photon Reirradiation For Recurrent GlioblastomaDocument9 pagesComparison of Carbon Ion and Photon Reirradiation For Recurrent Glioblastomachanmaulana30No ratings yet
- Q 3 WedefDocument6 pagesQ 3 Wedefsupaidi97No ratings yet
- Post Treatment ADC Changes in The Periresectional Area in Patients With GBMDocument7 pagesPost Treatment ADC Changes in The Periresectional Area in Patients With GBMafdhal.888980No ratings yet
- The Evolving Role of Hypofractionated Radiotherapy in Older Adults With Gastrointestinal CancersDocument9 pagesThe Evolving Role of Hypofractionated Radiotherapy in Older Adults With Gastrointestinal CancersRaul Matute MartinNo ratings yet
- Ji-Hye Park2019Document9 pagesJi-Hye Park2019Naiadja Santana CerqueiraNo ratings yet
- Genot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaDocument8 pagesGenot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaLarisssaa FerreiraNo ratings yet
- Radiotherapy of Liver CancerFrom EverandRadiotherapy of Liver CancerJinsil SeongNo ratings yet
- ASTRO17 Abdel-WahabDocument5 pagesASTRO17 Abdel-WahabRohit MaldeNo ratings yet
- Eligibility Guide - V29 - Non NeoadjuvantDocument1 pageEligibility Guide - V29 - Non NeoadjuvantRohit MaldeNo ratings yet
- Famous Indian Classical Musicians & Vocalists: OliveDocument8 pagesFamous Indian Classical Musicians & Vocalists: OliveRohit MaldeNo ratings yet
- STD 5 Civics Worksheet Indian CitizenshipDocument2 pagesSTD 5 Civics Worksheet Indian CitizenshipRohit MaldeNo ratings yet
- Instruction: Do Not Copy The Questions. Number The Questions Properly. Start The New Session On A New Page. Present Your Work NeatlyDocument3 pagesInstruction: Do Not Copy The Questions. Number The Questions Properly. Start The New Session On A New Page. Present Your Work NeatlyRohit MaldeNo ratings yet
- STD 5 TERM II Exam Time TableDocument1 pageSTD 5 TERM II Exam Time TableRohit MaldeNo ratings yet
- Smt. Sulochanadevi Singhania School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 ElectricityDocument2 pagesSmt. Sulochanadevi Singhania School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 ElectricityRohit MaldeNo ratings yet
- Smt. Sulochanadevi Singhanai School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 Human Body: Skeletal and Muscular SystemDocument2 pagesSmt. Sulochanadevi Singhanai School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 Human Body: Skeletal and Muscular SystemRohit MaldeNo ratings yet
- MeiosisDocument8 pagesMeiosisRohit MaldeNo ratings yet
- Gracia Arredondo - Symmetry-Gracia Arredondo (2019)Document230 pagesGracia Arredondo - Symmetry-Gracia Arredondo (2019)Rohit MaldeNo ratings yet
- 29-Article Text-180-1-10-20200430Document7 pages29-Article Text-180-1-10-20200430Drizella anatasyaNo ratings yet
- Stockleys 12e - 9780857113474 PDFDocument1 pageStockleys 12e - 9780857113474 PDFPark arimaNo ratings yet
- SPC - Ma130 00201Document6 pagesSPC - Ma130 00201Cassia FistulaNo ratings yet
- Kelompok 7 - 4b - Buku Saku Antibiotik Dan AntivirusDocument62 pagesKelompok 7 - 4b - Buku Saku Antibiotik Dan AntivirusWidya PratiwiNo ratings yet
- Web Non Subsidized Fully Manufactured LocallyDocument16 pagesWeb Non Subsidized Fully Manufactured LocallyA GhNo ratings yet
- MGH Bupe Home Induction Patient Final PDFDocument2 pagesMGH Bupe Home Induction Patient Final PDFben swaseyNo ratings yet
- Approved Price List of Medicine2007-08 (1) 07!09!07Document10 pagesApproved Price List of Medicine2007-08 (1) 07!09!07Anonymous m65TTcfOTNo ratings yet
- Principles of Practice For Pharmaceutical CareDocument29 pagesPrinciples of Practice For Pharmaceutical CareNgetwa TzDe TheWirymanNo ratings yet
- Umesh Pharma 669708399 - 9075Document24 pagesUmesh Pharma 669708399 - 9075Training and PlacementNo ratings yet
- Brochure - MagicTouch, Concept MedicalDocument6 pagesBrochure - MagicTouch, Concept MedicalBUSHRA ILYASNo ratings yet
- No Expired Dekat Exp Stok Menumpuk: Soal KadaluarsaDocument4 pagesNo Expired Dekat Exp Stok Menumpuk: Soal KadaluarsaAnnisa FitrianaNo ratings yet
- Laporan Pemakaian Dan Lembar Permintaan Obat Puskesmas: (Harus Diisi)Document12 pagesLaporan Pemakaian Dan Lembar Permintaan Obat Puskesmas: (Harus Diisi)Winda RosiNo ratings yet
- Fake Medicine Test 3asDocument2 pagesFake Medicine Test 3asSara EnglishNo ratings yet
- Calcium CarbonateDocument1 pageCalcium Carbonatecop_per0% (1)
- Lippincott Illustrated Reviews (PDFDrive) - Pages-396Document1 pageLippincott Illustrated Reviews (PDFDrive) - Pages-396Eman ShalabyNo ratings yet
- INJartesunate 60mg Booklet ENGDocument6 pagesINJartesunate 60mg Booklet ENGElly PetroNo ratings yet
- BLS Guidelines 2015Document9 pagesBLS Guidelines 2015Avicenna Zahara BungaNo ratings yet
- Introduction, Therapeutic Drug Monitoring & Patient CouncellingDocument22 pagesIntroduction, Therapeutic Drug Monitoring & Patient CouncellingSham Sakhare100% (1)
- 15 Mixing Medications Using One SyringeDocument2 pages15 Mixing Medications Using One SyringeMarky RoqueNo ratings yet
- 478 PeriodizationDocument13 pages478 Periodizationomarou1867% (3)
- Fact Sheets Graseby 1200Document10 pagesFact Sheets Graseby 1200Cherry EstradaNo ratings yet
- Coordinated Spontaneous Awakening and Breathing Trials ProtocolDocument6 pagesCoordinated Spontaneous Awakening and Breathing Trials ProtocolRidski D. MiruNo ratings yet
- Humalog Novolog Apidra: Type of Insulin & Brand Names Onset Peak Duration Role in Blood Sugar Management Rapid-ActingDocument2 pagesHumalog Novolog Apidra: Type of Insulin & Brand Names Onset Peak Duration Role in Blood Sugar Management Rapid-ActingkatrinasdNo ratings yet
- Module 2: Drug Classes and Schedules: Learning OutcomesDocument5 pagesModule 2: Drug Classes and Schedules: Learning OutcomesShaina JavierNo ratings yet
- 2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumDocument8 pages2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumJad DegheiliNo ratings yet
- CJR Isu OlahragaDocument15 pagesCJR Isu OlahragaDanang Dwi NopriandaNo ratings yet
- ATC Guidelines 2010Document139 pagesATC Guidelines 2010Chirag ChavdaNo ratings yet
- 10 MG 5 MG: Antasida Doen Chew-TabDocument9 pages10 MG 5 MG: Antasida Doen Chew-TabUlfa ErviliaNo ratings yet
BreastCare - 2015 10320 324
BreastCare - 2015 10320 324
Uploaded by
Rohit MaldeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BreastCare - 2015 10320 324
BreastCare - 2015 10320 324
Uploaded by
Rohit MaldeCopyright:
Available Formats
Review Article
Breast Care 2015;10:320–324 Published online: July 10, 2015
DOI: 10.1159/000436951
Emerging Role of Hypofractionated Radiotherapy with
Simultaneous Integrated Boost in Modern Radiotherapy
of Breast Cancer
Mirko Nitsche a, b Juergen Dunst b Ulrich M. Carl a Robert M. Hermann a, c
a
Zentrum für Strahlentherapie und Radioonkologie, Bremen/Westerstede, Germany;
b
Klinik für Strahlentherapie, Karl-Lennert-Krebscentrum, Universität Kiel, Germany;
c Abteilung Strahlentherapie und Spezielle Onkologie, Medizinische Hochschule Hannover, Germany
Keywords Is There a Rationale for Changing the Established
Breast cancer · Hypofractionation · Radiotherapy Fractionation Regimens in the Near Future?
Summary Malignant tumor cells and the surrounding healthy tissues dif-
Hypofractionated radiotherapy for breast cancer is be- fer with regard to their radiation sensitivity. The cells of normal
coming increasingly important. The scientific back- healthy tissues are able to recover from sublethal radiation damage,
ground of this development as well as the introduction whereas tumor cells show limited repair. These differences have
of the simultaneous integrated boost to the primary been investigated intensively and have resulted in distinctive radio-
tumor region in this context are discussed here. therapeutic treatment regimens in which the daily fraction dose,
© 2015 S. Karger GmbH, Freiburg TD, and adherent treatment schedules have been established [6].
Dose effectiveness in modern radiotherapy is described with the
linear-quadratic model (α/β model), predicting radiobiologically
equivalent (isoeffective) doses. The α/β value of the linear-quad-
ratic model describes the sensitivity of healthy tissue and tumor
cells depending on fractionation and TD. The fractionation sensi-
Introduction tivity of any tissue is characterized by its α/β value; the α/β value is
a mathematically calculated term derived from the dose-effect
Current standard whole breast irradiation (WBI) in breast-con- curve of the tissue, given in units of Gray (Gy). Generally, the α/β
serving concepts consists of a total dose (TD) of 50 Gy delivered in values of healthy tissues for late reactions are low (in the range of
25 daily fractions over a period of approximately 35 days. Alterna- 2–3 Gy). In contrast, tumors and early reacting tissues have much
tively, 50.4 Gy are applied using a daily dose of 1.8 Gy. An addi- higher α/β values in the range of 10 Gy or more [7]. In order to
tional boost to the primary tumor region at a TD of 12–16 Gy is protect the healthy tissue from late radiation effects, irradiation
indicated in the majority of patients, resulting in an overall treat- should therefore be administered at low single doses of 1.2–2 Gy.
ment period of up to 47 days [1–4]. Impressive data of more than The linear-quadratic model has been confirmed in a variety of
10,000 women in 17 randomized trials with a 15-year follow-up randomized studies, and it is a proven radiobiological fact that the
confirm a risk reduction of ipsilateral breast recurrences by a factor greatest therapeutic window with regard to both local tumor con-
of at least 3–4 [5]. This translates into a risk reduction of about 3% trol and late tissue effects is achieved if low doses per fraction are
for breast cancer deaths in node-negative patients and about 8% in administered. However, the dogma that all tumors have high α/β
node-positive patients. Moreover, there is plenty of experience values has been challenged over the past years. Over the past dec-
concerning treatment-related acute and late toxicity accompanied ade, growing evidence has accumulated that at least some cancers
by excellent cosmetic results [1]. may have exceptionally low α/β values. This has so far been proven
149.126.75.33 - 11/10/2015 10:34:32 AM
Universitätsbibliothek Kiel
© 2015 S. Karger GmbH, Freiburg Dr. med. Mirko Nitsche
1661–3791/15/0105–0320$39.50/0 Zentrum für Strahlentherapie und Radioonkologie
Downloaded by:
Fax +49 761 4 52 07 14 Gröpelinger Heerstr. 406–408, 28239 Bremen, Germany
Information@Karger.com Accessible online at: nitsche@strahlentherapie-bremen.com
www.karger.com www.karger.com/brc
for prostate cancer with an α/β value of about 1.5 Gy. If the α/β START trials 61% of all patients finally received a sequential boost
value of the tumor is below the α/β value of late-reacting surround- with 10 Gy (2 Gy/fraction). The boost was always administered
ing tissue, treatment with higher doses per fraction is, from a theo- after hypofractionated breast irradiation.
retical point of view, advantageous. Therefore, hypofractionation After 10-years, all treatment concepts showed equivalent out-
has a well-defined theoretical basis in prostate cancer, and the re- comes for hypofractionated radiotherapy compared to the tradi-
sults of completed and ongoing randomized studies support the tional schedule, favoring the use of 40 Gy in 15 fractions with a low
notion that at least moderate hypofractionation is feasible in pros- local recurrence rate of 5.6% [9]. All 3 trials included women with
tate cancer. Moreover, recent data suggest that prostate cancer is operable T1–3 N0–1 M0 invasive breast cancer and mostly small or
probably not the only exception and that some form of hypofrac- medium breast size.
tionation may be feasible in certain other cancer entities [8]. Another trial reproduced these results independently: The On-
tario Clinical Oncology Group randomly assigned 1,234 patients to
standard WBI or to 42.5 Gy in 16 fractions within 22 days [15].
Why Was Hypofractionation Introduced in Breast 1,234 women with invasive breast cancer (< 5 cm, no T3–4, nega-
Cancer? tive margins, node-negative) and without multicentric disease,
large breast size, and bilateral breast cancer were included. After 10
The hypofractionation studies in breast cancer were started at a years, the risk of recurrence was 6.7% in the standard group and
time when the data on low α/β values in tumors were not yet avail- 6.2% in the hypofractionated group. Cosmetic outcome was re-
able. The aim of these breast cancer studies was a more pragmatic ported as good or excellent with 71.3% in the standard group and
one, mainly to decrease the number of visits to the radiotherapy 69.8% in the hypofractionated group. These studies built the clini-
department and to shorten overall treatment time, thereby making cal basis for an α/β value of breast cancer in the range of 3–3.5 Gy,
adjuvant radiotherapy more convenient for patients. These studies similar to that of the surrounding healthy tissues (table 1).
were conducted in countries with centralized radiotherapy struc-
tures and long travel distances. It was assumed that a relevant sub-
group of patients who were candidates for breast-conserving treat- Ongoing Controversies Concerning the
ment did in fact choose mastectomy as primary treatment due to Hypofractionated Treatment of Breast Cancer
the inability to withstand a 6–8-week course of radiotherapy.
Therefore, studies were started in the 1990s evaluating an overall
shortened treatment time to increase acceptance of adjuvant radio- High-Risk Features
therapy and reduce costs. The majority of patients in the above mentioned trials had es-
Surprisingly, the latest data from these studies assume an α/β trogen receptor-positive and HER2-negative tumors. It is well
value for breast cancer of 3–3.5 Gy which is similar to that of the known that patients with high-grade tumors have a higher risk of
surrounding normal healthy tissue [9, 10]. This would mean that local recurrence after radiation. It is therefore questionable
fraction size can be changed within a relatively broad range with- whether hypofractionated WBI is suitable for all patients [1]. The
out negative impact on tumor control and late radiation sequelae. 10-year update of the START trials including 1,272 women with
Although not expected at the beginning of these trials, the data grade 3 breast cancer showed no difference between hypo- and
form a stable theoretical basis for the use of moderate hypofrac- normofractionation in terms of local recurrence in this group [9],
tionation in breast cancer. whereas the Ontario trial documented a significantly higher local
failure rate in the hypofractionation arm [15], which was somehow
considered a statistical fluke. In contrast to the Ontario trial, a se-
Which Studies Support the Effectiveness and quential boost to the primary tumor site was allowed in the START
Safety of Hypofractionation in Breast Cancer? trials, which may also be a possible explanation for the different
treatment results in the high-risk group. Recently, the Ontario
So far, 4 randomized trials have examined a hypofractionated group published the results of their analysis of tumor factors pre-
schedule as compared to the standard 5-week fractionation sched- dictive for response to hypofractionated versus normofractionated
ule for adjuvant WBI. radiotherapy. They stated that tumor grade, histological subtype,
The UK START pilot trial assessed dose schedules using either 3 and hypoxia did not predict for hypofractionation response, proof-
Gy/fraction up to a TD of 39 Gy, or 3.3 Gy/fraction with a TD of ing that hypofractionation can be safely administered in all breast
42.9 Gy (13 fractions) compared to the standard regimen of 2 Gy/ cancer patients [16].
fraction and a TD of 50 Gy [11, 12]. The following START-A ran-
domized 2,236 patients to 1 of 3 treatment arms: 3 Gy/fraction Young Age
(every second day) to a TD of 39 Gy, 3.2 Gy to a TD of 41.6 Gy, and The 2011 ASTRO consensus did not recommend hypofraction-
standard normofractionation [13]. START-B compared the stan- ation in women < 50 years of age [17] as younger women have a
dard schedule with a daily hypofractionated schedule using 40 Gy higher risk of local recurrence compared with older patients, and
with a fraction size of 2.66 Gy [14]. It should be noted that in both only few younger patients were randomized in those studies at this
149.126.75.33 - 11/10/2015 10:34:32 AM
Universitätsbibliothek Kiel
Hypofractionated RT in Breast Cancer Breast Care 2015;10:320–324 321
Downloaded by:
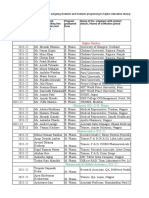
Table 1. Study data on hypofractionation in breast cancer treatment [25]
10-year event RMH/GOC START A START B Canadian
Arm, Gy Result, % p Arm, Gy Result, % p Arm, Gy Result, % p Arm, Gy Result, % p
Ipsilateral 50 12.1 0.027 50 6.7 NS 50 3.8 NS 50 7.4 NS
breast tumor
relapse
42.9 9.6 41.6 5.6 50 5.2 42.5 7.5
39 14.8 39 8.1
Distant NR 50 14.7 NS 50 16.0 0.014 NR
relapse
41.6 16.8 40 12.3
39 18.0
All-cause NR 50 19.8 NS 50 19.2 0.042 50 15.6 NS
mortality
41.6 18.4 40 15.9 42.5 15.4
39 20.3
Cosmesis, telangiectasia excellent–
selected end good
points
50 18.1 0.065 50 7.2 – 50 5.8 0.032 42.5 69.8 NS
42.9 18.0 41.6 7.1 0.99 40 4.2 50 71.3
39 12.0 39 3.0 0.003
breast edema
50 13.8 0.004 50 13.5 – 50 9.0 0.001
42.9 21.5 41.6 11.8 0.24 40 5.1
39 11.5 39 7.3 0.001
Toxicity, ischemic heart grade 3 skin
selected end disease
points
50 1.9 50 2.1 42.5 2.7 NS
41.6 1.5 40 1.5 50 2.5
39 1.1
symptomatic grade 3
lung fibrosis subcutaneous
tissue
50 1.2 50 1.7 42.5 3.6 NS
41.6 1.1 40 1.7 50 2.5
39 1.0
NR = Not reported; NS = not significant; RMH/GOC = Royal Marsden Hospital/Gloucester Oncology Center; START A/B = Standardization of Breast Radiotherapy
Trial A/B.
time. However, of the 4 major trials, only the Ontario study strati- under investigation. In the START trials, the only reported plex-
fied by age and detected no significant differences in ipsilateral opathy occurred with the 41.6 Gy fractionation schedule [9].
tumor recurrence, although no boost was applied [15]. The 10-year
update of the START trials included 1,398 women < 50 years of age Cardiotoxicity
and demonstrated the effectiveness of hypofractionation in Late cardiac side effects of hypofractionated radiotherapy have
younger patients, even showing a trend towards an improved effect only been evaluated to a maximum follow-up of 10 years. Since
of hypofractionation in this cohort [9]. most radiotherapy-associated cardiac side effects occur after 15
years or more, currently available results must be assessed with
Regional Nodal Irradiation caution, especially in women with a long life expectancy and an
There is only limited experience with hypofractionated regional unhealthy lifestyle. However, no significant cardiotoxicity has been
irradiation due to the small number of women with regional radio- observed in modern normofractionated radiotherapy for breast
therapy recruited in the reported studies. The safety of the investi- cancer with current radiotherapy techniques making it now safer
gated fractionation schemes in view of brachial plexopathy is still than in the past [18]. Recently, Chan et al. [19] reported a 15-year
149.126.75.33 - 11/10/2015 10:34:32 AM
Universitätsbibliothek Kiel
322 Breast Care 2015;10:320–324 Nitsche/Dunst/Carl/Hermann
Downloaded by:
follow-up of cardiac injury, comparing hypofractionation versus up is still missing. The new prospective multicenter 2-arm phase
normofractionation in left-sided early-stage breast cancer patients. III German HYPOSIB trial will provide data on hypofractionated
In 5,334 patients receiving breast or chest wall irradiation, no sta- irradiation with SIB with an overall very much shortened treat-
tistically significant difference in cardiac mortality was detected. ment time compared to standard radiotherapy. This non-inferior-
ity trial is designed to recruit 1,162 patients in each arm. The study
will randomize all patients with histologically confirmed unilateral
Implementation of a Simultaneous Integrated Boost invasive breast cancer after breast-conserving surgery with an indi-
in Hypofractionated Radiotherapy of Breast Cancer cation for a boost.
A boost to the primary tumor site improves local control in all
age groups. In R0-resected patients, the local recurrence rate is re- Conclusion
duced by 4–6.2% within 10 years [20]. To maintain this important
treatment effect in hypofractionated WBI without altering the Current clinical results of hypofractionated WBI support its in-
overall shortened treatment time, 4 studies have been conducted so troduction into clinical routine in the near future. Hypofractiona-
far in which a simultaneous integrated boost (SIB) was introduced. tion offers an alternative to standard fractionation regimens at least
Scorsetti et al. [21] enrolled 50 women to be treated with an SIB- in a subset of patients. There is now a clear radiobiological basis for
VMAT (volumetric-modulated arc therapy) approach, applying the use of moderate hypofractionation with a decrease in the num-
doses of 40.5 Gy to the whole breast and 48 Gy to the primary ber of fractions by about 50%; extreme hypofractionation (e.g. less
tumor bed in 15 fractions. They observed 1 grade 3 and 32 grade 1 than 10 fractions) or extremely reduced treatment times (e.g. less
skin toxicities, with the latter resolving within 3 weeks of treatment than 3 weeks) should, however, be restricted to clinical trials.
completion. No significant changes in cosmetic outcome were ob- Moreover, there is limited data on potentially different effects of
served 3 and 6 months after radiotherapy. Another protocol deliv- hypofractionation in subgroups, and it is unclear whether the ef-
ering 40.5 Gy to the breast and 45 Gy as an SIB in 15 fractions over fects of standard fractionation and hypofractionation are really
19 days was investigated by Chada et al. [22]. The 5-year disease- identical in all tumor subtypes. Delivery of a tumor bed boost in
free survival was 97%, based on a median follow-up of 3.5 years. the form of an SIB seems to be safe, feasible, and effective while
Acute and late toxicity were low without any grade 3 or 4 skin tox- further reducing the overall treatment time without compromising
icity after 2 years. A randomized trial by van Parijs et al. [23] com- established excellent overall results. The new HYPOSIB trial will
pared conventional radiotherapy to hypofractionated tomotherapy clarify the question of simultaneous boost application and hypof-
with 2.8 Gy/fraction to the whole breast and an SIB of 0.6 Gy/frac- ractionation in breast cancer on the basis of a high number of pa-
tion in 15 fractions. The primary purpose of this study was to eval- tients. All German radiotherapy facilities are encouraged to partici-
uate whether tomotherapy reduces heart and lung toxicity in this pate in the HYPOSIB trial as the study subject is a highly relevant
setting. They demonstrated a slight trend in favor of tomotherapy, key issue in the development of modern radiotherapy of breast
stating that short-course treatment with SIB is feasible with no se- cancer in Germany.
vere toxicity. The largest prospective investigation so far, a German
multicenter phase II study, treated 141 patients with 40 Gy to the
whole breast and an SIB of 48 Gy in 16 fractions. The regimen was Disclosure Statement
well tolerated with no grade 3 or 4 adverse events [24]. According
All authors declare no conflict of interests.
to this trial, hypofractionation with SIB seems to be safe and feasi-
ble with unchanged quality of life, even though long-term follow-
References
1 Sedlmayer F, Sautter-Bihl ML, Budach W, et al.; Breast 4 Scottish Intercollegiate Guidelines Network (SIGN): 7 Thames HD Jr, Withers HR, Peters LJ, Fletcher GH:
Cancer Expert Panel of the German Society of Radia- Treatment of primary breast cancer. Edinburgh: SIGN; Changes in early and late radiation responses with al-
tion Oncology (DEGRO): DEGRO practical guide- 2013. (SIGN publication no. 134). September 2013. tered dose fractionation: implications for dose-survival
lines: radiotherapy of breast cancer I: radiotherapy fol- www.sign.ac.uk Accessed on 23/04/2014. relationships. Int J Radiat Oncol Biol Phys 1982; 8:
lowing breast conserving therapy for invasive breast 5 Darby S, McGale P, Correa C et al.; Early Breast Can- 219–226.
cancer. Strahlenther Onkol 2013; 189: 825–833. cer Trialists’ Collaborative Group (EBCTCG): Effect of 8 Koontz BF, Bossi A, Cozzarini C, et al.: A systematic
2 Interdisziplinäre S3-Leitlinie für die Diagnostik, The- radiotherapy after breast-conserving surgery on 10- review of hypofractionation for primary management
rapie und Nachsorge des Mammakarzinoms, Langver- year recurrence and 15-year breast cancer death: meta- of prostate cancer. Eur Urol 2014;Epub ahead of print.
sion 3.0, Aktualisierung 2012, AWMF-Register-Num- analysis of individual patient data for 10,801 women in 9 Haviland JS, Owen JR, Dewar JA, et al.; START Trial-
mer: 032–045OL. 17 randomised trials. Lancet 2011; 378: 1707–1716. ists’ Group: The UK Standardisation of Breast Radio-
3 NCCN (National Comprehensive Cancer Network®), 6 Thames HD, Bentzen SM, Turesson I, et al.: Time-dose therapy (START) trials of radiotherapy hypofractiona-
NCCN Guidelines Version 2.2013 Invasive Breast can- factors in radiotherapy: a review of the human data. tion for treatment of early breast cancer: 10-year fol-
cer NCCN (National Comprehensive Cancer Net- Radiother Oncol 1990; 19: 219–235. low-up results of two randomised controlled trials.
work®), Practice Guidelines in Oncology (NCCN Lancet Oncol 2013; 14: 1086–1094.
Guidelines®), Breast Cancer Version 3.2013.
149.126.75.33 - 11/10/2015 10:34:32 AM
Universitätsbibliothek Kiel
Hypofractionated RT in Breast Cancer Breast Care 2015;10:320–324 323
Downloaded by:
10 Hennequin C, Dubray B: (Alpha/beta ratio revisited in 16 Bane AL, Whelan TJ, Pond GR, et al.: Tumor factors 22 Chadha M, Woode R, Sillanpaa J, et al.: Early-stage
the era of hypofractionation). Cancer Radiother 2013; predictive of response to hypofractionated radiother- breast cancer treated with 3-week accelerated whole-
17: 344–348. apy in a randomized trial following breast conserving breast radiation therapy and concomitant boost. Int J
11 Yarnold J, Ashton A, Bliss J, et al.: Fractionation sensi- therapy. Ann Oncol 2014; 25: 992–998. Radiat Oncol Biol Phys 2013; 86: 40–44.
tivity and dose response of late adverse effects in the 17 Smith BD, Bentzen SM, Correa CR, et al.: Fractiona- 23 Van Parijs H, Miedema G, Vinh-Hung V, Verbanck S,
breast after radiotherapy for early breast cancer: long- tion for whole breast irradiation: an American Society Adriaenssens N, Kerkhove D, Reynders T, Schuermans
term results of a randomised trial. Radiother Oncol for Radiation Oncology (ASTRO) evidence-based D, Leysen K, Hanon S, Van Camp G, Vincken W,
2005; 75: 9–17. guideline. Int J Radiat Oncol Biol Phys 2011; 81: 59–68. Storme G, Verellen D, De Ridder M: Short course
12 Owen JR, Ashton A, Bliss JM, et al.: Effect of radio- 18 Nitsche M, Pahl R, Huber K, et al.: Cardiac toxicity radiotherapy with simultaneous integrated boost for
therapy fraction size on tumour control in patients after radiotherapy for breast cancer: myths and facts. stage I–II breast cancer, early toxicities of a ran-
with early-stage breast cancer after local tumour exci- Breast Care, accepted for publication. domized clinical trial. Radiat Oncol 2012; 7: 80.
sion: long-term results of a randomised trial. Lancet 19 Chan EK, Woods R, Virani S, et al.: Long-term mortal- 24 Dellas K, Vonthein R, Zimmer J, et al.; ARO Study
Oncol 2006; 7: 467–471. ity from cardiac causes after adjuvant hypofractionated Group: Hypofractionation with simultaneous inte-
13 Bentzen SM, Agrawal RK, Aird EG, et al.; START Tri- vs. conventional radiotherapy for localized left-sided grated boost for early breast cancer: results of the
alists’ Group: The UK Standardisation of Breast Radio- breast cancer. Radiother Oncol 2015; 114: 73–78. German multicenter phase II trial (ARO-2010—01).
therapy (START) Trial A of radiotherapy hypofrac- 20 Poortmans PM, Collette L, Bartelink H, et al.: The ad- Strahlenther Onkol 2014; 190: 646–653.
tionation for treatment of early breast cancer: a ran- dition of a boost dose on the primary tumour bed after 25 Fisher CM, Rabinovitch R: Frontiers in radiotherapy
domised trial. Lancet Oncol 2008; 9: 331–341. lumpectomy in breast conserving treatment for breast for early-stage invasive breast cancer. J Clin Oncol
14 Bentzen SM, Agrawal RK, Aird EG, et al.; START cancer. A summary of the results of EORTC 22881– 2014; 32: 2894–2901.
Trialists’ Group: The UK Standardisation of Breast 10882 ‘boost versus no boost’ trial. Cancer Radiother
Radiotherapy (START) Trial B of radiotherapy hypo- 2008; 12: 565–570.
fractionation for treatment of early breast cancer: a 21 Scorsetti M, Alongi F, Fogliata A, et al.: Phase I–II
randomised trial. Lancet 2008; 371: 1098–1107. study of hypofractionated simultaneous integrated
15 Whelan T, Pignol J-P, Levine M, et al.: Long-term re- boost using volumetric modulated arc therapy for ad-
sults of hypofractionated radiation therapy for breast juvant radiation therapy in breast cancer patients: a
cancer. N Engl J Med 2010; 362: 513–520. report of feasibility and early toxicity results in the first
50 treatments. Radiat Oncol 2012; 7: 145.
149.126.75.33 - 11/10/2015 10:34:32 AM
Universitätsbibliothek Kiel
Downloaded by:
You might also like
- 4 Types of Symmetry in The PlaneDocument5 pages4 Types of Symmetry in The PlaneRohit MaldeNo ratings yet
- NSAIDDocument1 pageNSAIDShubhangiNo ratings yet
- Bioavailability PK Practice Problems 2013Document2 pagesBioavailability PK Practice Problems 2013Linh PhamNo ratings yet
- The Role of Hypofractionated Radiotherapy in ProstDocument10 pagesThe Role of Hypofractionated Radiotherapy in ProstАнастасия АнохинаNo ratings yet
- Uganda - CervixDocument9 pagesUganda - CervixDaniel PalmeraNo ratings yet
- 5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021Document10 pages5 Fracciones RT CA MAMA - FAST-Forward To IMPLEMENTACION 2021hugo francisco romero anduagaNo ratings yet
- Radiation Treatment For Breast CancerDocument13 pagesRadiation Treatment For Breast CancerZuriNo ratings yet
- PublicacionDocument5 pagesPublicacionNoelia Peirats AymerichNo ratings yet
- Breast RTH 2020Document10 pagesBreast RTH 2020Sara HossamNo ratings yet
- Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer – A study based on the EORTC trial 22881–10882 ‘boost versus no boost’ / European Journal of Cancer Collette, 2008Document13 pagesPredictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer – A study based on the EORTC trial 22881–10882 ‘boost versus no boost’ / European Journal of Cancer Collette, 2008saipraveen03No ratings yet
- Clinical and Translational Radiation Oncology: Original Research ArticleDocument6 pagesClinical and Translational Radiation Oncology: Original Research ArticleGörkem TürkkanNo ratings yet
- Aoki 2002Document10 pagesAoki 2002Drsaumyta MishraNo ratings yet
- Prophylactic Irradiation To The Contralateral BreaDocument6 pagesProphylactic Irradiation To The Contralateral Breaashnamuni07No ratings yet
- Pi Is 0360301611018256Document1 pagePi Is 0360301611018256Olyndo IwanNo ratings yet
- Hypofractionation in The Real World Rodin 2021Document8 pagesHypofractionation in The Real World Rodin 2021Gloribel BolívarNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyTit fuckerNo ratings yet
- Head NeckDocument8 pagesHead NeckerandolphsavageNo ratings yet
- Update On Radiotherapy in Gynaecological Malignancies: ReviewDocument8 pagesUpdate On Radiotherapy in Gynaecological Malignancies: ReviewDesrha TangdiseruNo ratings yet
- Hypofractionated Postmastectomy RadiationDocument8 pagesHypofractionated Postmastectomy RadiationEmin PehlivanogluNo ratings yet
- 2019 Article 5894 PDFDocument8 pages2019 Article 5894 PDFGalgalo GarbichaNo ratings yet
- Vaginal Dose Is Associated With Toxicity in Image Guided Tandem Ring or Ovoid-Based BrachytherapyDocument7 pagesVaginal Dose Is Associated With Toxicity in Image Guided Tandem Ring or Ovoid-Based BrachytherapyFlor ZalazarNo ratings yet
- Clinical Oncology: EditorialDocument3 pagesClinical Oncology: EditorialSyed HossainNo ratings yet
- Radiotherapy and Oncology: Brachytherapy of Cervical CancerDocument8 pagesRadiotherapy and Oncology: Brachytherapy of Cervical CancerodivarNo ratings yet
- Brachytherapy in The Treatment of Cervical CancerDocument10 pagesBrachytherapy in The Treatment of Cervical CancervchendilNo ratings yet
- Din 2013Document5 pagesDin 2013Med MedNo ratings yet
- 15 20a BartelinkDocument10 pages15 20a Bartelink980Denis FernandezNo ratings yet
- Radiotherapy and OncologyDocument5 pagesRadiotherapy and Oncologyhugo francisco romero anduagaNo ratings yet
- Endometrial Cancer - Reduce To The Minimum. Anew Paradigm For Adjuvant Treatments?Document6 pagesEndometrial Cancer - Reduce To The Minimum. Anew Paradigm For Adjuvant Treatments?najmulNo ratings yet
- Radiotherapy and Oncology: Original ArticleDocument8 pagesRadiotherapy and Oncology: Original ArticleJuancarlos Pari SalasNo ratings yet
- Special ArticleDocument21 pagesSpecial ArticleAhana MukherjeeNo ratings yet
- Systemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewDocument11 pagesSystemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewLorena Sánchez PérezNo ratings yet
- s13014 015 0495 4Document6 pagess13014 015 0495 4produxing 101No ratings yet
- Final CapstoneDocument11 pagesFinal Capstoneapi-603721790No ratings yet
- Brachytherapy in The Treatment of Breast CancerDocument10 pagesBrachytherapy in The Treatment of Breast CancerwahidNo ratings yet
- 10 1016@j Ejca 2019 10 025Document8 pages10 1016@j Ejca 2019 10 025habib diopNo ratings yet
- 10.1007@s00066 021 01782 5Document8 pages10.1007@s00066 021 01782 5Alberto GonzalesNo ratings yet
- Analysis of Compliance, Toxicity and Survival WeeklyDocument11 pagesAnalysis of Compliance, Toxicity and Survival Weeklydanu20No ratings yet
- Eport Res PaperDocument13 pagesEport Res Paperapi-309296181No ratings yet
- BCTT 15 721Document10 pagesBCTT 15 721Annisya MaharaniNo ratings yet
- 10 14338 - Ijpt-22-00041 1Document12 pages10 14338 - Ijpt-22-00041 1Raul Matute MartinNo ratings yet
- Theraphy RadDocument4 pagesTheraphy RadMega PuspitaNo ratings yet
- F - 3602 BCBCR Dose Distribution in The Heart and Cardiac Chambers Following 4 Field .PDF - 4865Document9 pagesF - 3602 BCBCR Dose Distribution in The Heart and Cardiac Chambers Following 4 Field .PDF - 4865Windy HardiyantyNo ratings yet
- Jco 2007 11 4991Document7 pagesJco 2007 11 4991brasilianaraNo ratings yet
- Principles of Chemotherapy and Radiotherapy PDFDocument7 pagesPrinciples of Chemotherapy and Radiotherapy PDFNora100% (3)
- Intensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningDocument8 pagesIntensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningAlberto GonzalesNo ratings yet
- Final CompleteDocument11 pagesFinal Completeapi-575843507No ratings yet
- Healthcare 07 00120Document9 pagesHealthcare 07 00120Ryantino IrdanNo ratings yet
- September 2013 - Radiotherapy For Localised Prostate Cancer - DR V KhooDocument4 pagesSeptember 2013 - Radiotherapy For Localised Prostate Cancer - DR V KhooHyago FrançaNo ratings yet
- Pub Paediatric Imaging Manual Notes in RadiologyDocument167 pagesPub Paediatric Imaging Manual Notes in RadiologydrAlbertoVV100% (1)
- Breast Cancer Notes Part 2Document60 pagesBreast Cancer Notes Part 2Tony YongNo ratings yet
- Vestibular Schwannoma Results of HypofractionatedDocument14 pagesVestibular Schwannoma Results of HypofractionatedTimothy CaldwellNo ratings yet
- RT en Pancreas Horowitz 2021Document2 pagesRT en Pancreas Horowitz 2021Carlos N. Rojas PuyolNo ratings yet
- Radiation Therapy and Esophageal CancerDocument14 pagesRadiation Therapy and Esophageal Cancerkrsna2studyNo ratings yet
- Rinky 712024 AORJ113575Document7 pagesRinky 712024 AORJ113575sazzad suvroNo ratings yet
- Wa0024 PDFDocument5 pagesWa0024 PDFmr copy xeroxNo ratings yet
- 1 s2.0 S2405632423000197 MainDocument11 pages1 s2.0 S2405632423000197 Mainsaros22568No ratings yet
- Comparison of Carbon Ion and Photon Reirradiation For Recurrent GlioblastomaDocument9 pagesComparison of Carbon Ion and Photon Reirradiation For Recurrent Glioblastomachanmaulana30No ratings yet
- Q 3 WedefDocument6 pagesQ 3 Wedefsupaidi97No ratings yet
- Post Treatment ADC Changes in The Periresectional Area in Patients With GBMDocument7 pagesPost Treatment ADC Changes in The Periresectional Area in Patients With GBMafdhal.888980No ratings yet
- The Evolving Role of Hypofractionated Radiotherapy in Older Adults With Gastrointestinal CancersDocument9 pagesThe Evolving Role of Hypofractionated Radiotherapy in Older Adults With Gastrointestinal CancersRaul Matute MartinNo ratings yet
- Ji-Hye Park2019Document9 pagesJi-Hye Park2019Naiadja Santana CerqueiraNo ratings yet
- Genot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaDocument8 pagesGenot-Klastersky2020 Article RetrospectiveEvaluationOfTheSaLarisssaa FerreiraNo ratings yet
- Radiotherapy of Liver CancerFrom EverandRadiotherapy of Liver CancerJinsil SeongNo ratings yet
- ASTRO17 Abdel-WahabDocument5 pagesASTRO17 Abdel-WahabRohit MaldeNo ratings yet
- Eligibility Guide - V29 - Non NeoadjuvantDocument1 pageEligibility Guide - V29 - Non NeoadjuvantRohit MaldeNo ratings yet
- Famous Indian Classical Musicians & Vocalists: OliveDocument8 pagesFamous Indian Classical Musicians & Vocalists: OliveRohit MaldeNo ratings yet
- STD 5 Civics Worksheet Indian CitizenshipDocument2 pagesSTD 5 Civics Worksheet Indian CitizenshipRohit MaldeNo ratings yet
- Instruction: Do Not Copy The Questions. Number The Questions Properly. Start The New Session On A New Page. Present Your Work NeatlyDocument3 pagesInstruction: Do Not Copy The Questions. Number The Questions Properly. Start The New Session On A New Page. Present Your Work NeatlyRohit MaldeNo ratings yet
- STD 5 TERM II Exam Time TableDocument1 pageSTD 5 TERM II Exam Time TableRohit MaldeNo ratings yet
- Smt. Sulochanadevi Singhania School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 ElectricityDocument2 pagesSmt. Sulochanadevi Singhania School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 ElectricityRohit MaldeNo ratings yet
- Smt. Sulochanadevi Singhanai School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 Human Body: Skeletal and Muscular SystemDocument2 pagesSmt. Sulochanadevi Singhanai School, Thane STD 5/Science/Practice Worksheet/ Term 2/2019-20 Human Body: Skeletal and Muscular SystemRohit MaldeNo ratings yet
- MeiosisDocument8 pagesMeiosisRohit MaldeNo ratings yet
- Gracia Arredondo - Symmetry-Gracia Arredondo (2019)Document230 pagesGracia Arredondo - Symmetry-Gracia Arredondo (2019)Rohit MaldeNo ratings yet
- 29-Article Text-180-1-10-20200430Document7 pages29-Article Text-180-1-10-20200430Drizella anatasyaNo ratings yet
- Stockleys 12e - 9780857113474 PDFDocument1 pageStockleys 12e - 9780857113474 PDFPark arimaNo ratings yet
- SPC - Ma130 00201Document6 pagesSPC - Ma130 00201Cassia FistulaNo ratings yet
- Kelompok 7 - 4b - Buku Saku Antibiotik Dan AntivirusDocument62 pagesKelompok 7 - 4b - Buku Saku Antibiotik Dan AntivirusWidya PratiwiNo ratings yet
- Web Non Subsidized Fully Manufactured LocallyDocument16 pagesWeb Non Subsidized Fully Manufactured LocallyA GhNo ratings yet
- MGH Bupe Home Induction Patient Final PDFDocument2 pagesMGH Bupe Home Induction Patient Final PDFben swaseyNo ratings yet
- Approved Price List of Medicine2007-08 (1) 07!09!07Document10 pagesApproved Price List of Medicine2007-08 (1) 07!09!07Anonymous m65TTcfOTNo ratings yet
- Principles of Practice For Pharmaceutical CareDocument29 pagesPrinciples of Practice For Pharmaceutical CareNgetwa TzDe TheWirymanNo ratings yet
- Umesh Pharma 669708399 - 9075Document24 pagesUmesh Pharma 669708399 - 9075Training and PlacementNo ratings yet
- Brochure - MagicTouch, Concept MedicalDocument6 pagesBrochure - MagicTouch, Concept MedicalBUSHRA ILYASNo ratings yet
- No Expired Dekat Exp Stok Menumpuk: Soal KadaluarsaDocument4 pagesNo Expired Dekat Exp Stok Menumpuk: Soal KadaluarsaAnnisa FitrianaNo ratings yet
- Laporan Pemakaian Dan Lembar Permintaan Obat Puskesmas: (Harus Diisi)Document12 pagesLaporan Pemakaian Dan Lembar Permintaan Obat Puskesmas: (Harus Diisi)Winda RosiNo ratings yet
- Fake Medicine Test 3asDocument2 pagesFake Medicine Test 3asSara EnglishNo ratings yet
- Calcium CarbonateDocument1 pageCalcium Carbonatecop_per0% (1)
- Lippincott Illustrated Reviews (PDFDrive) - Pages-396Document1 pageLippincott Illustrated Reviews (PDFDrive) - Pages-396Eman ShalabyNo ratings yet
- INJartesunate 60mg Booklet ENGDocument6 pagesINJartesunate 60mg Booklet ENGElly PetroNo ratings yet
- BLS Guidelines 2015Document9 pagesBLS Guidelines 2015Avicenna Zahara BungaNo ratings yet
- Introduction, Therapeutic Drug Monitoring & Patient CouncellingDocument22 pagesIntroduction, Therapeutic Drug Monitoring & Patient CouncellingSham Sakhare100% (1)
- 15 Mixing Medications Using One SyringeDocument2 pages15 Mixing Medications Using One SyringeMarky RoqueNo ratings yet
- 478 PeriodizationDocument13 pages478 Periodizationomarou1867% (3)
- Fact Sheets Graseby 1200Document10 pagesFact Sheets Graseby 1200Cherry EstradaNo ratings yet
- Coordinated Spontaneous Awakening and Breathing Trials ProtocolDocument6 pagesCoordinated Spontaneous Awakening and Breathing Trials ProtocolRidski D. MiruNo ratings yet
- Humalog Novolog Apidra: Type of Insulin & Brand Names Onset Peak Duration Role in Blood Sugar Management Rapid-ActingDocument2 pagesHumalog Novolog Apidra: Type of Insulin & Brand Names Onset Peak Duration Role in Blood Sugar Management Rapid-ActingkatrinasdNo ratings yet
- Module 2: Drug Classes and Schedules: Learning OutcomesDocument5 pagesModule 2: Drug Classes and Schedules: Learning OutcomesShaina JavierNo ratings yet
- 2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumDocument8 pages2024 American Society of Clinical Oncology Genitourinary (ASCO-GU) Cancers SymposiumJad DegheiliNo ratings yet
- CJR Isu OlahragaDocument15 pagesCJR Isu OlahragaDanang Dwi NopriandaNo ratings yet
- ATC Guidelines 2010Document139 pagesATC Guidelines 2010Chirag ChavdaNo ratings yet
- 10 MG 5 MG: Antasida Doen Chew-TabDocument9 pages10 MG 5 MG: Antasida Doen Chew-TabUlfa ErviliaNo ratings yet