Professional Documents
Culture Documents
Week 2 Case Study
Week 2 Case Study
Uploaded by
Melissa CernyCopyright:
Available Formats
You might also like
- STUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningDocument14 pagesSTUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningPeggy100% (12)
- 50 Most Commonly Prescribed MedicationsDocument2 pages50 Most Commonly Prescribed MedicationsGloryJane67% (3)
- Nursing Case Study Ch46 Med SurgDocument1 pageNursing Case Study Ch46 Med SurgPriyal ParikhNo ratings yet
- Junetta Cooper Vsim Prep 2Document5 pagesJunetta Cooper Vsim Prep 2Michelle Pinkhasova100% (2)
- STUDENT-Sickle - Cell-FUNDAMENTAL ReasoningDocument7 pagesSTUDENT-Sickle - Cell-FUNDAMENTAL ReasoningSharon Tanveer0% (1)
- Novel Coronavirus Disease (COVID-19) Part I: Emergency Department (ED)Document8 pagesNovel Coronavirus Disease (COVID-19) Part I: Emergency Department (ED)Uzumaki K100% (1)
- Small Bowel Obstruction System - DisorderDocument1 pageSmall Bowel Obstruction System - DisorderMarina Wasem Netzlaff0% (1)
- Chapter 13: Delirium and Dementia Linton: Medical-Surgical Nursing, 7th EditionDocument10 pagesChapter 13: Delirium and Dementia Linton: Medical-Surgical Nursing, 7th EditionnickNo ratings yet
- Memory Notebook of Nursing VolDocument170 pagesMemory Notebook of Nursing Voleric100% (1)
- Vsim Case Sara Lin Virtual ClinicalDocument12 pagesVsim Case Sara Lin Virtual ClinicalLivan Martell100% (4)
- Pediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)From EverandPediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)No ratings yet
- Ams 11Document702 pagesAms 11CrazyNo ratings yet
- Ekg Chart PDF 01Document5 pagesEkg Chart PDF 01YukiMaedaNo ratings yet
- Urosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFDocument11 pagesUrosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFOLga A. Thigpen100% (4)
- This Study Resource Was: Assessment & Reasoning Cardiac SystemDocument6 pagesThis Study Resource Was: Assessment & Reasoning Cardiac SystemSharon TanveerNo ratings yet
- Fundamentals of Nursing Nclex RNDocument71 pagesFundamentals of Nursing Nclex RNspartacuslivesNo ratings yet
- Shock Comparison ChartDocument2 pagesShock Comparison Chartlinnaete88% (8)
- HESI Case Study Older Adult With StrokeDocument2 pagesHESI Case Study Older Adult With StrokeAna Bienne100% (1)
- Simple Study Notes For Nursing - StrokeDocument5 pagesSimple Study Notes For Nursing - StrokeAshleigh Johnstone100% (1)
- VATI Funds RemediationDocument2 pagesVATI Funds RemediationestberryNo ratings yet
- Nursing Memory JoggersDocument2 pagesNursing Memory JoggersMarcus, RN96% (24)
- Vsim Isbar Activity Student Worksheet: Your Name, Position (RN), Unit You Are Working OnDocument2 pagesVsim Isbar Activity Student Worksheet: Your Name, Position (RN), Unit You Are Working OnA PNo ratings yet
- Ricci KeithRN Eating DisorderDocument14 pagesRicci KeithRN Eating DisorderMichelle RicciNo ratings yet
- CardiacDisorders StudyGuideLongDocument7 pagesCardiacDisorders StudyGuideLongYukiMaeda100% (1)
- PDF - VeinsDocument3 pagesPDF - VeinsjulialeoNo ratings yet
- VSim For NursingDocument21 pagesVSim For NursingDennis Mburu100% (1)
- TMendoza CriticalCareConceptMap2Document5 pagesTMendoza CriticalCareConceptMap2Theresa Fernandez Mendoza0% (1)
- HEENT Focused Exam Soap NoteDocument5 pagesHEENT Focused Exam Soap Noteariel sparkmanNo ratings yet
- Nurseslabs MedsurgDocument9 pagesNurseslabs MedsurgiamdarnNo ratings yet
- Summary Notes For Studying Fluid and ElectrolytesDocument8 pagesSummary Notes For Studying Fluid and ElectrolytesCandace Mead100% (1)
- OB NRSNG - Com BrainsheetsDocument4 pagesOB NRSNG - Com BrainsheetsD SchwartzlerNo ratings yet
- 1 - Yellow BookDocument49 pages1 - Yellow Booksushma.rayamajhi.bsc06No ratings yet
- Chest AuscultationDocument24 pagesChest AuscultationAtu KaushalNo ratings yet
- EKG Interpretation NursingDocument14 pagesEKG Interpretation NursingTanya ViarsNo ratings yet
- Cardiac Study GuideDocument9 pagesCardiac Study GuideJane DiazNo ratings yet
- Adult Health III Final Study GuideDocument12 pagesAdult Health III Final Study GuideRyanne JNo ratings yet
- 1) Nursing Careplan For FeverDocument9 pages1) Nursing Careplan For FeverY. Beatrice AbigailNo ratings yet
- Nurse Brain Sheet New Shift ReportDocument1 pageNurse Brain Sheet New Shift ReportJenny Anne100% (1)
- Cardiovascular Nursing Bullet Points I PDFDocument4 pagesCardiovascular Nursing Bullet Points I PDFKhalid Epping100% (3)
- Diabetes Med Surg Questions 1Document6 pagesDiabetes Med Surg Questions 1Trish Hồ0% (1)
- N205 - Basic EKG InterpretationDocument23 pagesN205 - Basic EKG InterpretationTinaHoNo ratings yet
- Resp Lecture NotesDocument18 pagesResp Lecture Notessurviving nursing schoolNo ratings yet
- Peds Unit 2 Study GuideDocument25 pagesPeds Unit 2 Study GuideKyptasticNo ratings yet
- NIH Stroke ScaleDocument29 pagesNIH Stroke ScaleEdRobertArnad100% (1)
- NotesDocument10 pagesNotesVu HauNo ratings yet
- Nursing Path o CardsDocument194 pagesNursing Path o CardsDanielle Shull100% (1)
- Template For NURSING NotesDocument2 pagesTemplate For NURSING Notesbngraham4No ratings yet
- Nurses Note DONEDocument1 pageNurses Note DONEjhenssineNo ratings yet
- A Nurse's Guide to Caring for Cardiac Intervention PatientsFrom EverandA Nurse's Guide to Caring for Cardiac Intervention PatientsNo ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Dimensional Analysis For Nursing StudentsFrom EverandDimensional Analysis For Nursing StudentsNo ratings yet
- The Call of Nursing: Stories from the Front Lines of Health CareFrom EverandThe Call of Nursing: Stories from the Front Lines of Health CareRating: 4.5 out of 5 stars4.5/5 (3)
- MEDICAL-SURGICAL NURSE: Passbooks Study GuideFrom EverandMEDICAL-SURGICAL NURSE: Passbooks Study GuideNo ratings yet
- CRITICAL THINKING IN CLINICAL NURSING PRACTICE (RN): Passbooks Study GuideFrom EverandCRITICAL THINKING IN CLINICAL NURSING PRACTICE (RN): Passbooks Study GuideNo ratings yet
- FATSDocument27 pagesFATSBer Anne Jaropojop TahilNo ratings yet
- Pathophysiology, Diagnosis, and Management of Dyslipidemia: Gerald T. Gau, MD, and R. Scott Wright, MD, FACC, FAHA, FESCDocument42 pagesPathophysiology, Diagnosis, and Management of Dyslipidemia: Gerald T. Gau, MD, and R. Scott Wright, MD, FACC, FAHA, FESCCalvin LitraNo ratings yet
- Appendix: Laboratory Reference Values : Reference Intervals For HematologyDocument10 pagesAppendix: Laboratory Reference Values : Reference Intervals For HematologynovikaneNo ratings yet
- NX600 FolletoDocument4 pagesNX600 FolletoValeria AlfaRoNo ratings yet
- Anatomy of Healing BookDocument72 pagesAnatomy of Healing BookSachin Karthik100% (2)
- PCOS Evidence-Based Guideline For Assessment and Management PcosDocument167 pagesPCOS Evidence-Based Guideline For Assessment and Management PcosJalajarani AridassNo ratings yet
- Ayusante CatalogueDocument12 pagesAyusante CatalogueAnkit Modi0% (1)
- Product ListDocument28 pagesProduct ListBibi MomoNo ratings yet
- Comparison of The Efficacy of Rosuvastatin Versus Atorvastatin, Simvastatin, and Pravastatin in Achieving Lipid Goals: Results From The STELLAR TrialDocument11 pagesComparison of The Efficacy of Rosuvastatin Versus Atorvastatin, Simvastatin, and Pravastatin in Achieving Lipid Goals: Results From The STELLAR Trialamit khanNo ratings yet
- 20 Rajarajeswari EtalDocument4 pages20 Rajarajeswari EtaleditorijmrhsNo ratings yet
- Swift 2018Document33 pagesSwift 2018Sam Steven Hernandez JañaNo ratings yet
- Ashish Sarraju Atherosclerotic Plaque StabilizationDocument11 pagesAshish Sarraju Atherosclerotic Plaque Stabilizationdarkangelmx1No ratings yet
- Effect of Galohgor Cookies and Powder Drinks On ViDocument8 pagesEffect of Galohgor Cookies and Powder Drinks On ViKhaerul FadlyNo ratings yet
- Abubakar and Naomi's Project 2022Document4 pagesAbubakar and Naomi's Project 2022Ahmad OlaiyaNo ratings yet
- JCEM Hypertriglyceridemia Endocrinology Society 2012Document36 pagesJCEM Hypertriglyceridemia Endocrinology Society 2012Paz VidaNo ratings yet
- Biochemical Tests in Diabetes: DR Joe Fleming PHD MCB Frcpath Dept of Clinical Biochemistry CMC VelloreDocument43 pagesBiochemical Tests in Diabetes: DR Joe Fleming PHD MCB Frcpath Dept of Clinical Biochemistry CMC VelloreTRINEL ANGGRIATI100% (1)
- Equipment Applications BTS 370Document32 pagesEquipment Applications BTS 370oscacaiNo ratings yet
- CME Slide Deck CardiacDocument53 pagesCME Slide Deck CardiacPragnesh ShahNo ratings yet
- Tanyut Huidrom - Assignment 4 - HUman PhysiologyDocument1 pageTanyut Huidrom - Assignment 4 - HUman PhysiologyTanyut HuidromNo ratings yet
- Jurnal FisiologiDocument8 pagesJurnal FisiologiRFALWNo ratings yet
- Haematology: Investigation Observed Value Unit Biological Reference IntervalDocument10 pagesHaematology: Investigation Observed Value Unit Biological Reference IntervalVanshitaNo ratings yet
- Is It Possible To Remove Heavy Metals From The Body by Wet Cupping Therapy (Al-Hijamah) ?Document6 pagesIs It Possible To Remove Heavy Metals From The Body by Wet Cupping Therapy (Al-Hijamah) ?yoshefarieNo ratings yet
- Robbins File For AnkiDocument13 pagesRobbins File For Ankiאיתי עוזרNo ratings yet
- Nej MR A 2311526Document11 pagesNej MR A 2311526lakshminivas PingaliNo ratings yet
- Yoga & HypothyroidismDocument6 pagesYoga & Hypothyroidismtttt45No ratings yet
- A Systematic Review of The Potential Effects of Propolis Extracts On Experimentally-Induced DiabetesDocument9 pagesA Systematic Review of The Potential Effects of Propolis Extracts On Experimentally-Induced DiabetesAmir MukmininNo ratings yet
- 13804-Article Text-50409-1-10-20130214Document6 pages13804-Article Text-50409-1-10-20130214Jose TeranNo ratings yet
- TACA Times Sept/Oct 2010Document6 pagesTACA Times Sept/Oct 2010Bruce WileyNo ratings yet
- Oils and Fats: Induction Training (Technical-1/2)Document27 pagesOils and Fats: Induction Training (Technical-1/2)Umesha shankra ShettyNo ratings yet
- Mode of Action of Snehapanam 2023Document8 pagesMode of Action of Snehapanam 2023Doctor KalarirasayanaNo ratings yet
Week 2 Case Study
Week 2 Case Study
Uploaded by
Melissa CernyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Week 2 Case Study
Week 2 Case Study
Uploaded by
Melissa CernyCopyright:
Available Formats
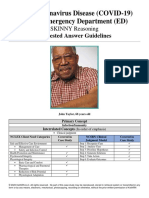
Hypertension
Mike Kelly, 51 years old
Primary Concept
Perfusion
Interrelated Concepts (In order of emphasis)
1. Glucose Regulation
2. Pain
3. Clinical Judgment
4. Patient Education
© 2016 Keith Rischer/www.KeithRN.com
FUNDAMENTAL Reasoning: STUDENT
History of Present Problem:
Mike Kelly is a 51-year-old Caucasian male who is 6 feet tall and weighs 275 pounds (BMI 37.3) with an abnormal
distribution of weight around his abdomen. He does not regularly exercise, does not like to cook, and eats fast food three
to five times during the week. He has smoked one pack per day since the age of 20 (31 pack years). He has a history of
hyperlipidemia, but is unable to afford his medication (atorvastatin), and has not taken since he was diagnosed 5 years
ago. He has no current diagnosed medical problems. He became concerned and came to the emergency department
because he is more easily fatigued and has had a headache the past three days that has not improved.
Personal/Social History:
Mike is self-employed and owns his own auto mechanic business. He has no health insurance. His father had hypertension
and died of a myocardial infarction (MI) at the age of 50. Angelina, his wife, came with him to urgent care. She shares
that he is usually stoic about health problems, so this must really bother him or he is afraid. He took Excedrin and Motrin
for pain and it didn’t help.
What data from the histories are RELEVANT and have clinical significance for the nurse?
RELEVANT Data from Present Problem: Clinical Significance:
BMI 37.3 Overall, unhealthy
Does not excercise
Unhealthy eating High Cholestrol left untreated
Smokes Consumes high fat/ sodium food contributing to his high
Hyperlipidemia
Does not take perscribed medication cholestrol
Easily Fatigured
Headache For 3 days
RELEVANT Data from Social History: Clinical Significance:
No health insurance Unable to afford treatments
Family history of hypertension and MI (heart Possiblitiy of hypertension or MI
attack)
Patient is usually quiet about problems Patient is fearful
Took OTC for pain with no relief
Developing Nurse Thinking by Identifying Significance of Clinical Data
Patient Care Begins:
Current VS: P-Q-R-S-T Pain Assessment (5th VS):
T: 98.9 F/37.2 C (oral) Provoking/Palliative: Nothing/Nothing
P: 88 (regular) Quality: Ache
R: 20 Region/Radiation: Global head ache (HA)
BP: 220/118 Severity: 8/10
O2 sat: 95% room air Timing: Continuous
What VS data are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT VS Data: Clinical Significance:
R:20 Respirations on higher end
BP: 220/118 Blood pressure is dangerously high
Pain 8/10 High pain levels
Continuous acheing Headache could be relavent to blood pressure
headache
© 2016 Keith Rischer/www.KeithRN.com
Current Assessment:
GENERAL Appears uncomfortable, body tense with occasional grimacing
APPEARANCE:
RESP: Breath sounds clear with equal aeration bilaterally ant/post, non-labored respiratory effort
CARDIAC: Pink, warm and dry, no edema, heart sounds regular–S1S2, pulses bounding, equal with
palpation at radial/pedal/post-tibial landmarks
NEURO: Alert and oriented to person, place, time, and situation (x4)
GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants
GU: Voiding without difficulty, urine clear/yellow
SKIN: Skin integrity intact, skin turgor elastic with no tenting
What assessment data are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Assessment Data: Clinical Significance:
Occasional grimacing Overall, patient is in pain
Normal heart and pulses Heart is not affected by high blood pressure
Alert Shows no signs of dementia, correct medical history given
No skin tenting Patient is not significantly dehydrated
Developing Nurse Thinking through APPLICATION of the Sciences
Fluid & Electrolytes/Lab/diagnostic Results:
Radiology Reports: Chest x-ray
What diagnostic results are RELEVANT and must be recognized as clinically significant to the nurse?
RELEVANT Results: Clinical Significance:
The cardiac size is Heart is enlarged and is working harder, making it weaker. Walls can become
enlarged with moderate to affected. Heart is still pumpimg normally.
severe cardiomegaly.
There are no focal
infiltrates or
consolidations or pleural
effusions.
Lab Results:
Complete Blood Count (CBC:) Current: High/Low/WNL?
WBC (4.5–11.0 mm 3) 10.5 WNL
Hgb (12–16 g/dL) 15.3 WNL
Platelets (150–450x 103/µl) 422 WNL
Neutrophil % (42–72) 68 WNL
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
Normal Blood Labs No signs of infection, all results in normal range
© 2016 Keith Rischer/www.KeithRN.com
Basic Metabolic Panel (BMP:) Current: High/Low/WNL?
Sodium (135–145 mEq/L) 136 WNL
Potassium (3.5–5.0 mEq/L) 4.0 WNL
Glucose (70–110 mg/dL) 188 HIGH
BUN (7–25 mg/dl) 32 HIGH
Creatinine (0.6–1.2 mg/dL) 1.5 HIGH
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
Glucose high High levels of sugars could be caused by diabetes or pancreas
BUN High High blood urea nitrogen could be sign of heart failure, GI issues, or heart
Creatinine High attack
High Creatinine could be sign of dehrdration, kidney failure/ disease, or UT
obstruction.
Cardiac Labs: Current: High/Low/WNL?
BNP (B-natriuretic Peptide) (<100 ng/L) 758 HIGH
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
High BNP Higher levels of BNP can indicate heart failure or weakening of the heart.
Lipid Panel: Current: High/Low/WNL?
Low density lipoprotein–LDL (<130 mg/dL) 260 High
High density lipoprotein–HDL (>40 mg/dL) 28 Low
Total cholesterol (<200 mg/dL) 290 High
Triglycerides (30–149 mg/dL) 484 High
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
High LDL High LDL can indicate high levels of cholestrol and/or cholestrol buildup in the
lowHDL arteries.
High Cholestrol Low HDL indicates not enough good cholestrol, higher risk of cardiovasuclar
issues.
High cholestrol increases risk for heart disease
© 2016 Keith Rischer/www.KeithRN.com
Urine Analysis (UA:) Current: High/Low/WNL?
Color (yellow) Yellow WNL
Clarity (clear) Clear WNL
Specific Gravity (1.015–1.030) 1.018 WNL
Protein (neg) Moderate High
Glucose (neg) Moderate High
Ketones (neg) Negative WNL
Bilirubin (neg) Negative WNL
Blood (neg) Positive High
Nitrite (neg) Negative WNL
LET (Leukocyte Esterase) (neg) Negative WNL
MICRO:
RBCs (<5) 3 WNL
WBCs (<5) 2 WNL
Bacteria (neg) Negative WNL
Epithelial (neg) Negative WNL
What lab results are RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT Lab(s): Clinical Significance:
Moderate Protein Sign of kideny disease, Kidneys did not fully filter proteins/ waste products
Moderate Glucose High glucose could be a sign of diabetes or also related to a kidney issue.
Postive Blood Blood in urine could be from a UTI or UT obstruction or also related to kidneys
function.
Lab Planning: Creating a Plan of Care with a PRIORITY Lab:
Lab: Normal Why Relevant? Nursing Assessments/Interventions Required:
Value:
Creatinine High creatinine More fluids to filter waste products.
could be a sign of
Value: Critical value: dehydration, kidney
Lower levels of creatinine through use of dialysis to remove
1.5 failue/ disease, or waste in kidneys.
UT obstruction.
Lab: Normal Value: Why Relevant? Nursing Assessments/Interventions
Required:
BNP Can indicate heart failure or Use of medication to treat.
(B-natriuretic weakend heart. Monitor vitals after medication
Peptide) administration.
Critical Value:
Value:
758
© 2016 Keith Rischer/www.KeithRN.com
Pharmacology:
Home Med: Classification: Mechanism of Action Nursing Considerations:
(in own words):
Atorvastatin Antilipidemic Reduces cholestrol, inhibits reductase Consider patients poor diet, lab
inhibitor. Reduces elevated levels of values. Be aware of theraputic
HMG-CoA triglycerides. response for lipid labs. Has
reductasae adverse affects in patients with
Inhibitor liver disease.
Pathophysiology:
1. What is the primary problem that your patient is most likely presenting?
High blood pressure
2. What is the underlying cause/pathophysiology of this primary problem?
(Relate initial manifestations to the pathophysiology of the primary problem)
Pathophysiology of Primary Problem: Rationale/Relationship to Manifestations:
Hyperlipidemia (high cholesterol) is the underlying cause of The high cholesterol creates buildup
patients issues in the arteries, making the arteries
narrow. This means that the heart
has to pump and work harder to be
ableto push the blood through those
arteries. The cholesterol can also
block renal arteries, reducing blood
flow available to kidneys, creating
loss of kidney function.
Developing Nurse Thinking by Identifying Clinical RELATIONSHIPS
1. What is the RELATIONSHIP of the past medical history and current medications?
(Which medication treats which condition? Draw lines to connect)
Past Medical History (PMH): Home Meds:
Hyperlipidemia --------------> Atorvastatin NOT currently taking
Obesity…abd fat distribution
Sedentary lifestyle
Smokes 1 ppd
Family history of heart disease
1. Is there a RELATIONSHIP between any disease in PMH that may have contributed to the development of the
current problem? (Which disease likely developed FIRST then began a “domino effect”?)
PMH: What Came FIRST:
Untreated hypertension and Hyperlipidemia came first. It created the need for the high blood
hyperlipidemia pressure by blocking arteries, making the heart pump harder.
© 2016 Keith Rischer/www.KeithRN.com
3. What is the RELATIONSHIP between the primary care provider’s orders and primary problem?
Care Provider Orders: How it Will Resolve Primary Problem/Nursing Priority:
Basic metabolic panel (BMP) Gives more information on patient and monitor lab levels after
treatment.
Complete cell count (CBC) CBC can see if infection is present.
BNP (B-natriuretic Peptide)
BNP can give an idea of the condition of the heart, we were able
to see that the heart is weakend.
Lipid profile
Lipid panel was able to see the true levels of cholestrol
Urine analysis (UA) Urine analysis was able to see how the kidney is not effectivly
filtering waste products
12-lead EKG 12- lead EKG would be able to see how the heart is working and
check to see the thickness of the walls. It would see how affeted
the heart is from working hard for the high blood pressure.
Chest X-ray
Chest xray we were able to see that the heart is enlarged and was
being affected by the high blood pressure
Labetalol 20 mg IV push every 10".
Maximum 300 mg dose. Will decrease blood pressure, treats hypertension
Goal-BP: 160/100
Developing Nurse Thinking by Identifying Clinical PRIORITIES
1. What nursing priority(ies) will guide your plan of care? (if more than one-list in order of PRIORITY)
Treatment for high blood pressure and cholesterol
Provide a fluids and healthy nutritional meals
Teach patient about importance of taking his medication.
2. What interventions will you initiate based on this priority?
Nursing Interventions: Rationale: Expected Outcome:
Provide medication for high blood Giving the patient his perscribed Lower cholesterol
pressure and cholesterol Atrovastatin will decrease his high
cholesterol and having an IV push of Lower blood
Labetatol will decrease his blood pressure
pressure
Alleviated
Headache
3. What are the PRIORITY psychosocial needs that this patient and/or family likely have that will need to be
addressed?
Patient needs to be educated on the importance of taking his medication as prescribed and to
take care of his body with proper nutrition and excercise.
© 2016 Keith Rischer/www.KeithRN.com
4. How can the nurse address these psychosocial needs?
Nurse can provide information on how to take the medication. If patient has issues with affording
medication, refer to a case manager. Provide information on nutrition and excercise.
5. What educational/discharge PRIORITIES will be needed to develop a teaching plan for this patient and/or family?
Give education on importance of taking prescribed medications. Education on healthy eating and
daily excercise.
Caring & the “Art” of Nursing
1. What is the patient likely experiencing/feeling right now in this situation?
The patient feels fearful and is experiencing discomfort and pain. Potentially anxious to know
what is going on
2. What can I do to engage myself with this patient’s experience, and show that he/she matters to me as a person?
Show sympathy for the issues that have shown. Let them know that as long as they adhear to the
treatments they will be okay and that were here to give you the care you deserve and need.
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention
in the moment as the events are unfolding to make a correct clinical judgment and transfer what is learned to improve
nurse thinking and patient care in the future.
1. What did I learn from this scenario?
That many issues can come from one underlying problem. Many issues can be treated with the
same thing.
2. How can I use what has been learned from this scenario to improve patient care in the future?
I can use this to be able to compare similar events to this case study. I now know how blood
pressure, cholesterol, and the heart are all in relation to each other. I can compare events that
may arise in future patient care and look for sign in this study.
© 2016 Keith Rischer/www.KeithRN.com
You might also like
- STUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningDocument14 pagesSTUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningPeggy100% (12)
- 50 Most Commonly Prescribed MedicationsDocument2 pages50 Most Commonly Prescribed MedicationsGloryJane67% (3)
- Nursing Case Study Ch46 Med SurgDocument1 pageNursing Case Study Ch46 Med SurgPriyal ParikhNo ratings yet
- Junetta Cooper Vsim Prep 2Document5 pagesJunetta Cooper Vsim Prep 2Michelle Pinkhasova100% (2)
- STUDENT-Sickle - Cell-FUNDAMENTAL ReasoningDocument7 pagesSTUDENT-Sickle - Cell-FUNDAMENTAL ReasoningSharon Tanveer0% (1)
- Novel Coronavirus Disease (COVID-19) Part I: Emergency Department (ED)Document8 pagesNovel Coronavirus Disease (COVID-19) Part I: Emergency Department (ED)Uzumaki K100% (1)
- Small Bowel Obstruction System - DisorderDocument1 pageSmall Bowel Obstruction System - DisorderMarina Wasem Netzlaff0% (1)
- Chapter 13: Delirium and Dementia Linton: Medical-Surgical Nursing, 7th EditionDocument10 pagesChapter 13: Delirium and Dementia Linton: Medical-Surgical Nursing, 7th EditionnickNo ratings yet
- Memory Notebook of Nursing VolDocument170 pagesMemory Notebook of Nursing Voleric100% (1)
- Vsim Case Sara Lin Virtual ClinicalDocument12 pagesVsim Case Sara Lin Virtual ClinicalLivan Martell100% (4)
- Pediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)From EverandPediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)No ratings yet
- Ams 11Document702 pagesAms 11CrazyNo ratings yet
- Ekg Chart PDF 01Document5 pagesEkg Chart PDF 01YukiMaedaNo ratings yet
- Urosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFDocument11 pagesUrosepsis-Sepsis - (KeithRN-Unfolding THIGPEN PDFOLga A. Thigpen100% (4)
- This Study Resource Was: Assessment & Reasoning Cardiac SystemDocument6 pagesThis Study Resource Was: Assessment & Reasoning Cardiac SystemSharon TanveerNo ratings yet
- Fundamentals of Nursing Nclex RNDocument71 pagesFundamentals of Nursing Nclex RNspartacuslivesNo ratings yet
- Shock Comparison ChartDocument2 pagesShock Comparison Chartlinnaete88% (8)
- HESI Case Study Older Adult With StrokeDocument2 pagesHESI Case Study Older Adult With StrokeAna Bienne100% (1)
- Simple Study Notes For Nursing - StrokeDocument5 pagesSimple Study Notes For Nursing - StrokeAshleigh Johnstone100% (1)
- VATI Funds RemediationDocument2 pagesVATI Funds RemediationestberryNo ratings yet
- Nursing Memory JoggersDocument2 pagesNursing Memory JoggersMarcus, RN96% (24)
- Vsim Isbar Activity Student Worksheet: Your Name, Position (RN), Unit You Are Working OnDocument2 pagesVsim Isbar Activity Student Worksheet: Your Name, Position (RN), Unit You Are Working OnA PNo ratings yet
- Ricci KeithRN Eating DisorderDocument14 pagesRicci KeithRN Eating DisorderMichelle RicciNo ratings yet
- CardiacDisorders StudyGuideLongDocument7 pagesCardiacDisorders StudyGuideLongYukiMaeda100% (1)
- PDF - VeinsDocument3 pagesPDF - VeinsjulialeoNo ratings yet
- VSim For NursingDocument21 pagesVSim For NursingDennis Mburu100% (1)
- TMendoza CriticalCareConceptMap2Document5 pagesTMendoza CriticalCareConceptMap2Theresa Fernandez Mendoza0% (1)
- HEENT Focused Exam Soap NoteDocument5 pagesHEENT Focused Exam Soap Noteariel sparkmanNo ratings yet
- Nurseslabs MedsurgDocument9 pagesNurseslabs MedsurgiamdarnNo ratings yet
- Summary Notes For Studying Fluid and ElectrolytesDocument8 pagesSummary Notes For Studying Fluid and ElectrolytesCandace Mead100% (1)
- OB NRSNG - Com BrainsheetsDocument4 pagesOB NRSNG - Com BrainsheetsD SchwartzlerNo ratings yet
- 1 - Yellow BookDocument49 pages1 - Yellow Booksushma.rayamajhi.bsc06No ratings yet
- Chest AuscultationDocument24 pagesChest AuscultationAtu KaushalNo ratings yet
- EKG Interpretation NursingDocument14 pagesEKG Interpretation NursingTanya ViarsNo ratings yet
- Cardiac Study GuideDocument9 pagesCardiac Study GuideJane DiazNo ratings yet
- Adult Health III Final Study GuideDocument12 pagesAdult Health III Final Study GuideRyanne JNo ratings yet
- 1) Nursing Careplan For FeverDocument9 pages1) Nursing Careplan For FeverY. Beatrice AbigailNo ratings yet
- Nurse Brain Sheet New Shift ReportDocument1 pageNurse Brain Sheet New Shift ReportJenny Anne100% (1)
- Cardiovascular Nursing Bullet Points I PDFDocument4 pagesCardiovascular Nursing Bullet Points I PDFKhalid Epping100% (3)
- Diabetes Med Surg Questions 1Document6 pagesDiabetes Med Surg Questions 1Trish Hồ0% (1)
- N205 - Basic EKG InterpretationDocument23 pagesN205 - Basic EKG InterpretationTinaHoNo ratings yet
- Resp Lecture NotesDocument18 pagesResp Lecture Notessurviving nursing schoolNo ratings yet
- Peds Unit 2 Study GuideDocument25 pagesPeds Unit 2 Study GuideKyptasticNo ratings yet
- NIH Stroke ScaleDocument29 pagesNIH Stroke ScaleEdRobertArnad100% (1)
- NotesDocument10 pagesNotesVu HauNo ratings yet
- Nursing Path o CardsDocument194 pagesNursing Path o CardsDanielle Shull100% (1)
- Template For NURSING NotesDocument2 pagesTemplate For NURSING Notesbngraham4No ratings yet
- Nurses Note DONEDocument1 pageNurses Note DONEjhenssineNo ratings yet
- A Nurse's Guide to Caring for Cardiac Intervention PatientsFrom EverandA Nurse's Guide to Caring for Cardiac Intervention PatientsNo ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Dimensional Analysis For Nursing StudentsFrom EverandDimensional Analysis For Nursing StudentsNo ratings yet
- The Call of Nursing: Stories from the Front Lines of Health CareFrom EverandThe Call of Nursing: Stories from the Front Lines of Health CareRating: 4.5 out of 5 stars4.5/5 (3)
- MEDICAL-SURGICAL NURSE: Passbooks Study GuideFrom EverandMEDICAL-SURGICAL NURSE: Passbooks Study GuideNo ratings yet
- CRITICAL THINKING IN CLINICAL NURSING PRACTICE (RN): Passbooks Study GuideFrom EverandCRITICAL THINKING IN CLINICAL NURSING PRACTICE (RN): Passbooks Study GuideNo ratings yet
- FATSDocument27 pagesFATSBer Anne Jaropojop TahilNo ratings yet
- Pathophysiology, Diagnosis, and Management of Dyslipidemia: Gerald T. Gau, MD, and R. Scott Wright, MD, FACC, FAHA, FESCDocument42 pagesPathophysiology, Diagnosis, and Management of Dyslipidemia: Gerald T. Gau, MD, and R. Scott Wright, MD, FACC, FAHA, FESCCalvin LitraNo ratings yet
- Appendix: Laboratory Reference Values : Reference Intervals For HematologyDocument10 pagesAppendix: Laboratory Reference Values : Reference Intervals For HematologynovikaneNo ratings yet
- NX600 FolletoDocument4 pagesNX600 FolletoValeria AlfaRoNo ratings yet
- Anatomy of Healing BookDocument72 pagesAnatomy of Healing BookSachin Karthik100% (2)
- PCOS Evidence-Based Guideline For Assessment and Management PcosDocument167 pagesPCOS Evidence-Based Guideline For Assessment and Management PcosJalajarani AridassNo ratings yet
- Ayusante CatalogueDocument12 pagesAyusante CatalogueAnkit Modi0% (1)
- Product ListDocument28 pagesProduct ListBibi MomoNo ratings yet
- Comparison of The Efficacy of Rosuvastatin Versus Atorvastatin, Simvastatin, and Pravastatin in Achieving Lipid Goals: Results From The STELLAR TrialDocument11 pagesComparison of The Efficacy of Rosuvastatin Versus Atorvastatin, Simvastatin, and Pravastatin in Achieving Lipid Goals: Results From The STELLAR Trialamit khanNo ratings yet
- 20 Rajarajeswari EtalDocument4 pages20 Rajarajeswari EtaleditorijmrhsNo ratings yet
- Swift 2018Document33 pagesSwift 2018Sam Steven Hernandez JañaNo ratings yet
- Ashish Sarraju Atherosclerotic Plaque StabilizationDocument11 pagesAshish Sarraju Atherosclerotic Plaque Stabilizationdarkangelmx1No ratings yet
- Effect of Galohgor Cookies and Powder Drinks On ViDocument8 pagesEffect of Galohgor Cookies and Powder Drinks On ViKhaerul FadlyNo ratings yet
- Abubakar and Naomi's Project 2022Document4 pagesAbubakar and Naomi's Project 2022Ahmad OlaiyaNo ratings yet
- JCEM Hypertriglyceridemia Endocrinology Society 2012Document36 pagesJCEM Hypertriglyceridemia Endocrinology Society 2012Paz VidaNo ratings yet
- Biochemical Tests in Diabetes: DR Joe Fleming PHD MCB Frcpath Dept of Clinical Biochemistry CMC VelloreDocument43 pagesBiochemical Tests in Diabetes: DR Joe Fleming PHD MCB Frcpath Dept of Clinical Biochemistry CMC VelloreTRINEL ANGGRIATI100% (1)
- Equipment Applications BTS 370Document32 pagesEquipment Applications BTS 370oscacaiNo ratings yet
- CME Slide Deck CardiacDocument53 pagesCME Slide Deck CardiacPragnesh ShahNo ratings yet
- Tanyut Huidrom - Assignment 4 - HUman PhysiologyDocument1 pageTanyut Huidrom - Assignment 4 - HUman PhysiologyTanyut HuidromNo ratings yet
- Jurnal FisiologiDocument8 pagesJurnal FisiologiRFALWNo ratings yet
- Haematology: Investigation Observed Value Unit Biological Reference IntervalDocument10 pagesHaematology: Investigation Observed Value Unit Biological Reference IntervalVanshitaNo ratings yet
- Is It Possible To Remove Heavy Metals From The Body by Wet Cupping Therapy (Al-Hijamah) ?Document6 pagesIs It Possible To Remove Heavy Metals From The Body by Wet Cupping Therapy (Al-Hijamah) ?yoshefarieNo ratings yet
- Robbins File For AnkiDocument13 pagesRobbins File For Ankiאיתי עוזרNo ratings yet
- Nej MR A 2311526Document11 pagesNej MR A 2311526lakshminivas PingaliNo ratings yet
- Yoga & HypothyroidismDocument6 pagesYoga & Hypothyroidismtttt45No ratings yet
- A Systematic Review of The Potential Effects of Propolis Extracts On Experimentally-Induced DiabetesDocument9 pagesA Systematic Review of The Potential Effects of Propolis Extracts On Experimentally-Induced DiabetesAmir MukmininNo ratings yet
- 13804-Article Text-50409-1-10-20130214Document6 pages13804-Article Text-50409-1-10-20130214Jose TeranNo ratings yet
- TACA Times Sept/Oct 2010Document6 pagesTACA Times Sept/Oct 2010Bruce WileyNo ratings yet
- Oils and Fats: Induction Training (Technical-1/2)Document27 pagesOils and Fats: Induction Training (Technical-1/2)Umesha shankra ShettyNo ratings yet
- Mode of Action of Snehapanam 2023Document8 pagesMode of Action of Snehapanam 2023Doctor KalarirasayanaNo ratings yet