Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
73 viewsCesar, Katyana Antoine - Common Laboratory and Diagnostics Procedures Used in Gi Disorders (Rle Worksheet No. 3)
Cesar, Katyana Antoine - Common Laboratory and Diagnostics Procedures Used in Gi Disorders (Rle Worksheet No. 3)
Uploaded by
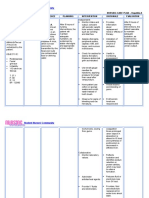
kdfhjfhfThis document discusses common non-invasive gastrointestinal diagnostic procedures, including liver function tests, hepatitis screening, and alpha-fetoprotein testing. Liver function tests measure blood levels of liver enzymes and proteins to screen for and monitor liver disease. Hepatitis screening determines infection status for hepatitis A, B, and C through antibody and antigen testing. Alpha-fetoprotein is a tumor marker that may indicate liver, ovarian, or testicular cancers when levels are elevated. Nursing responsibilities include educating patients, obtaining samples correctly, and monitoring for complications or abnormal results that require treatment.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Speaking Notes - OetDocument76 pagesSpeaking Notes - OetExam Materials94% (81)
- Tonsillitis: Case Presentation Related To Clients With Upper Respiratory ProblemsDocument54 pagesTonsillitis: Case Presentation Related To Clients With Upper Respiratory ProblemskdfhjfhfNo ratings yet
- Your Complete Guide To Liver He - Paul J. ThuluvathDocument216 pagesYour Complete Guide To Liver He - Paul J. ThuluvathSam Simons100% (1)
- NP3. Nursing Board Exam November 2008 Answer KeyDocument12 pagesNP3. Nursing Board Exam November 2008 Answer KeyAlyssa Mier Dacua Patalinjug100% (1)
- Philippine Handbook On Adult Immunization 2012 PDFDocument140 pagesPhilippine Handbook On Adult Immunization 2012 PDFLinius CruzNo ratings yet
- Nursingcrib Com NURSING CARE PLAN Hepatitis ADocument2 pagesNursingcrib Com NURSING CARE PLAN Hepatitis APravesh Verma100% (1)
- Viral HepatitisDocument20 pagesViral HepatitisShivam SoniNo ratings yet
- UntitledDocument43 pagesUntitledJovania B.No ratings yet
- ACG Abnormal Liver Chemistries Guideline SummaryDocument16 pagesACG Abnormal Liver Chemistries Guideline SummaryDanuNo ratings yet
- ACG Abnormal Liver Chemistries Guideline 2017Document18 pagesACG Abnormal Liver Chemistries Guideline 2017honeyworksNo ratings yet
- Diagnosis of HepatitisDocument19 pagesDiagnosis of HepatitisHrishikesh BangaleNo ratings yet
- Gallbladder-Liver and Pancreatic DisordersDocument7 pagesGallbladder-Liver and Pancreatic DisordersHasan A AsFourNo ratings yet
- Discharge PlanDocument12 pagesDischarge PlanPamela Shiermaine FilomenoNo ratings yet
- 13-11-2023Document40 pages13-11-2023vineeta.ashoknagarNo ratings yet
- GI 2007 Exam QuestionsDocument47 pagesGI 2007 Exam QuestionsRoh JitenNo ratings yet
- Diagnostic TestsDocument11 pagesDiagnostic TestsMae GabrielNo ratings yet
- Interpret Liver TestsDocument4 pagesInterpret Liver TestsKaram Ali ShahNo ratings yet
- Case Study 3Document2 pagesCase Study 3api-305352286No ratings yet
- New PPT For HepatitisDocument88 pagesNew PPT For HepatitisPriya100% (2)
- Project Nutrition Jasmin-2Document17 pagesProject Nutrition Jasmin-2JAs MineNo ratings yet
- Viral HepatitisDocument6 pagesViral HepatitisangelarainNo ratings yet
- Testing PositiveDocument3 pagesTesting PositiveAhmed GaberNo ratings yet
- Hepatitis BDocument48 pagesHepatitis BHari Suthan TNo ratings yet
- GI 2007 Exam QuestionsDocument47 pagesGI 2007 Exam QuestionsShadows BlameNo ratings yet
- IBD-Rough Road - Case Study in IBD From Presentation To ManagementDocument4 pagesIBD-Rough Road - Case Study in IBD From Presentation To ManagementBejan CorinaNo ratings yet
- Patogenesis Dan Manifestasi Klinik HepatitisDocument91 pagesPatogenesis Dan Manifestasi Klinik HepatitisFaulina Yosia PanjaitanNo ratings yet
- Evidence-Based Management of Common Gallstone-Related EmergenciesDocument11 pagesEvidence-Based Management of Common Gallstone-Related EmergenciesEva Puspita VaniNo ratings yet
- Case StudyDocument8 pagesCase StudyJan Clarisse RamosNo ratings yet
- PreeclampsiaDocument179 pagesPreeclampsiaJohn Wilbert Birung100% (3)
- Abnormal LTs 2014Document63 pagesAbnormal LTs 2014Robert G. Gish, MDNo ratings yet
- Guide For Pre-Clinical Practice Research and PlanningDocument5 pagesGuide For Pre-Clinical Practice Research and PlanningAnonymous ZSqTiYX7nNo ratings yet
- MT 6322 - Mycology and Virology 2nd Shifting OLADocument9 pagesMT 6322 - Mycology and Virology 2nd Shifting OLAlily bluesNo ratings yet
- Liver and Its Clinical SignificanceDocument59 pagesLiver and Its Clinical SignificanceazizNo ratings yet
- Diagnostic Tests A. Endoscopy: Nursing ConsiderationsDocument3 pagesDiagnostic Tests A. Endoscopy: Nursing ConsiderationsMae GabrielNo ratings yet
- Table 44-8 Nursing Assessment: Hepatitis Subjective Data Important Health InformationDocument7 pagesTable 44-8 Nursing Assessment: Hepatitis Subjective Data Important Health InformationAnggela kian puspaNo ratings yet
- Ziad Aro, MD Internal MedicineDocument100 pagesZiad Aro, MD Internal MedicineAli Aborges Jr.No ratings yet
- Week 8 Hepato Biliary 2Document94 pagesWeek 8 Hepato Biliary 2طفوف محمد.No ratings yet
- Viral Hepatitis and Alcoholic Liver Disease: Prepared By: Azhi Omer - F190219 Supervised By: Dr. Truska FaraidunDocument29 pagesViral Hepatitis and Alcoholic Liver Disease: Prepared By: Azhi Omer - F190219 Supervised By: Dr. Truska FaraidunMustafa Salam M.NooriNo ratings yet
- Acute Hepatitis: Dr.G.Indhumathi MD.Document39 pagesAcute Hepatitis: Dr.G.Indhumathi MD.Parthiban AnnaduraiNo ratings yet
- Bachelor of Science in Nursing: Ncmb316 Rle: RLE RLE Unit WeekDocument4 pagesBachelor of Science in Nursing: Ncmb316 Rle: RLE RLE Unit WeekMaica LectanaNo ratings yet
- Test #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyDocument47 pagesTest #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyJahangir AlamNo ratings yet
- Hepatitis ADocument15 pagesHepatitis Azakariah kamal0% (1)
- Liver TransplantationDocument6 pagesLiver TransplantationPriya0% (1)
- Diarrea Crónica Mar95Document5 pagesDiarrea Crónica Mar95apadronNo ratings yet
- GI (PBL3) - Mohamad Arbian Karim - FMUI20Document7 pagesGI (PBL3) - Mohamad Arbian Karim - FMUI20Mohamad Arbian KarimNo ratings yet
- Final Laboratory ProceduresDocument14 pagesFinal Laboratory ProceduresJosh BlasNo ratings yet
- Hepatitis, Viral: Type A (HAV) Type B (HBV) Type C (HCV)Document17 pagesHepatitis, Viral: Type A (HAV) Type B (HBV) Type C (HCV)herlindaNo ratings yet
- GlomerulonephritisDocument4 pagesGlomerulonephritisKim GarciaNo ratings yet
- Pi Is 1542356511012778Document6 pagesPi Is 1542356511012778Muhammad Rehan AnisNo ratings yet
- DyspepsiaDocument26 pagesDyspepsiaYaasin R NNo ratings yet
- Hepatic Encephalo & Viral Hep: Pathy AtitisDocument28 pagesHepatic Encephalo & Viral Hep: Pathy AtitisAdrian ArenasNo ratings yet
- 1B-Antenatal Care Case Protocol-1Document3 pages1B-Antenatal Care Case Protocol-1Mario EspinoNo ratings yet
- Note For H.Pylori Antigen TestDocument12 pagesNote For H.Pylori Antigen TestKrishna ShresthaNo ratings yet
- What Is Hepatitis A?: NCM 104 - CHN (Rle) 1Document3 pagesWhat Is Hepatitis A?: NCM 104 - CHN (Rle) 1Sue CañizaresNo ratings yet
- Evaluation Chronic DiarrheaDocument34 pagesEvaluation Chronic DiarrheaarthoclaseNo ratings yet
- 44 Year Old Man With Fatigue, Weight Loss, and LeuDocument5 pages44 Year Old Man With Fatigue, Weight Loss, and LeuRamiro Arraya MierNo ratings yet
- Hepatic, Pancreatic, and Rare Gastrointestinal Complications of Immune Checkpoint Inhibitor Therapy - UpToDateDocument29 pagesHepatic, Pancreatic, and Rare Gastrointestinal Complications of Immune Checkpoint Inhibitor Therapy - UpToDatemayteveronica1000No ratings yet
- Hepatitis A Virus - HAV: DiagnosisDocument6 pagesHepatitis A Virus - HAV: DiagnosisnurmaliarizkyNo ratings yet
- NURS 321/527 Unit 4 Review Digestion: GERD, Malabsorption, Pancreatitis, HepatitisDocument19 pagesNURS 321/527 Unit 4 Review Digestion: GERD, Malabsorption, Pancreatitis, HepatitisSamip PatelNo ratings yet
- Approach To Viral Hepatitis andDocument38 pagesApproach To Viral Hepatitis andVijay ShankarNo ratings yet
- Hepatology: Gatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2013Document50 pagesHepatology: Gatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2013niluhayusumbawatiNo ratings yet
- Module14 Content Nursing Care Management of AdultDocument21 pagesModule14 Content Nursing Care Management of AdultFranceska AntonioNo ratings yet
- American Family Physician - April 15, 2020 - Chronic Diarrhea in Adults - Evaluation and Differential DiagnosisDocument16 pagesAmerican Family Physician - April 15, 2020 - Chronic Diarrhea in Adults - Evaluation and Differential DiagnosismariaNo ratings yet
- Fecal Calprotectin in IBDDocument34 pagesFecal Calprotectin in IBDNathania Nadia BudimanNo ratings yet
- Name: Celajes, Ma. Lourdes Ann D. Group: D: Rarely (1) Sometimes (2) Usually (3) Almost AlwaysDocument3 pagesName: Celajes, Ma. Lourdes Ann D. Group: D: Rarely (1) Sometimes (2) Usually (3) Almost AlwayskdfhjfhfNo ratings yet
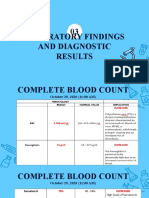
- Laboratory Findings and Diagnostic Results 03Document7 pagesLaboratory Findings and Diagnostic Results 03kdfhjfhfNo ratings yet
- Diagnostic Test Normal Findins Description Purpose Indication Procedure Nursing Implications Magnetic Resonance ImagingDocument5 pagesDiagnostic Test Normal Findins Description Purpose Indication Procedure Nursing Implications Magnetic Resonance ImagingkdfhjfhfNo ratings yet
- RRL LocalinternationalDocument11 pagesRRL LocalinternationalkdfhjfhfNo ratings yet
- Ella Sots and Research LocaleDocument2 pagesElla Sots and Research LocalekdfhjfhfNo ratings yet
- Laboratory Findings and Diagnostic Results 03Document4 pagesLaboratory Findings and Diagnostic Results 03kdfhjfhfNo ratings yet
- Synchronous Class Schedule For: Time 1 and 3 Week of The Month 2 and 4 Week of The Month Wednesday Friday Wednesday FridayDocument1 pageSynchronous Class Schedule For: Time 1 and 3 Week of The Month 2 and 4 Week of The Month Wednesday Friday Wednesday FridaykdfhjfhfNo ratings yet
- Name Name Name: AnswerDocument2 pagesName Name Name: AnswerkdfhjfhfNo ratings yet
- The Type of Cancer SuspectedDocument20 pagesThe Type of Cancer SuspectedkdfhjfhfNo ratings yet
- Normal Findings and MeaningDocument11 pagesNormal Findings and MeaningkdfhjfhfNo ratings yet
- Laboratory Test Normal Findings Description Purpose Indications Procedure Nursing Implications 1. Adrenocorticotropi C Hormone (Plasma) Pre-TestDocument11 pagesLaboratory Test Normal Findings Description Purpose Indications Procedure Nursing Implications 1. Adrenocorticotropi C Hormone (Plasma) Pre-TestkdfhjfhfNo ratings yet
- Tumor Marker Test A. Prostate Specific Antigen (Psa) TestDocument25 pagesTumor Marker Test A. Prostate Specific Antigen (Psa) TestkdfhjfhfNo ratings yet
- Laboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisordersDocument153 pagesLaboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisorderskdfhjfhfNo ratings yet
- Laboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisordersDocument145 pagesLaboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisorderskdfhjfhfNo ratings yet
- Nursing Care For A Family Caring For Children With Infectious DiseaseDocument4 pagesNursing Care For A Family Caring For Children With Infectious DiseasekdfhjfhfNo ratings yet
- Case Scenario 5 NCPDocument10 pagesCase Scenario 5 NCPkdfhjfhfNo ratings yet
- Cesar, Katyana Antoine - Vision & Hearing LecDocument17 pagesCesar, Katyana Antoine - Vision & Hearing LeckdfhjfhfNo ratings yet
- Cesar - Evaluation - ImciDocument3 pagesCesar - Evaluation - ImcikdfhjfhfNo ratings yet
- 4 Collab Ws VH KasDocument2 pages4 Collab Ws VH KaskdfhjfhfNo ratings yet
- NCM - 109 RLE Worksheet No. 4 Common Diagnostics - Laboratory and Nursing Procedures Related To Renal and Reproductive DisordersDocument10 pagesNCM - 109 RLE Worksheet No. 4 Common Diagnostics - Laboratory and Nursing Procedures Related To Renal and Reproductive DisorderskdfhjfhfNo ratings yet
- Cesar - Cardio & HemaDocument77 pagesCesar - Cardio & HemakdfhjfhfNo ratings yet
- Name of Structure Functio N Name of Structure Function Name of Structure Functio NDocument2 pagesName of Structure Functio N Name of Structure Function Name of Structure Functio NkdfhjfhfNo ratings yet
- Anatomy & Physiology of The EyesDocument4 pagesAnatomy & Physiology of The EyeskdfhjfhfNo ratings yet
- Example of An Interview EssayDocument7 pagesExample of An Interview Essayafhbebseg100% (2)
- Prevention of Hepatitis A To E - 014825Document15 pagesPrevention of Hepatitis A To E - 014825saadkhalid8No ratings yet
- Grid AbcdeDocument1 pageGrid AbcdeStephanieDardaNo ratings yet
- Presented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHDocument55 pagesPresented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHKailash Nagar100% (1)
- 3.0HEPATIT Lecture 5Document48 pages3.0HEPATIT Lecture 5Jiya MuhammadNo ratings yet
- Hepatitis PresentationDocument33 pagesHepatitis Presentationapi-286686446No ratings yet
- Hepatitis A Fact SheetDocument2 pagesHepatitis A Fact SheetKUER NewsNo ratings yet
- Foodborne PathogensDocument42 pagesFoodborne Pathogensabdiredha100% (1)
- Liver & Biliary DiseaseDocument41 pagesLiver & Biliary Diseasesaump3No ratings yet
- COVID-19 Vaccination PlanDocument52 pagesCOVID-19 Vaccination PlanFOX 17 NewsNo ratings yet
- Hepatitis A Treatment in Pune - Kaizen Gastro CareDocument4 pagesHepatitis A Treatment in Pune - Kaizen Gastro CareKaizen Gastro CareNo ratings yet
- June 26, 2015 Strathmore TimesDocument40 pagesJune 26, 2015 Strathmore TimesStrathmore TimesNo ratings yet
- Fen Otrimoxazole AlloDocument2 pagesFen Otrimoxazole AlloKristine AguilarNo ratings yet
- 9510 Enteric VirusesDocument18 pages9510 Enteric VirusesPenelope MeloNo ratings yet
- Viral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Document44 pagesViral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Eleni HagosNo ratings yet
- Case Presentation: Hepatitis ADocument57 pagesCase Presentation: Hepatitis Azahrara90No ratings yet
- Immunization - Dr. SarahDocument14 pagesImmunization - Dr. Sarahf6bk6xnppyNo ratings yet
- PhysAssessAbdomen 1Document21 pagesPhysAssessAbdomen 1David DvoskineNo ratings yet
- NCM 112 - HepatitisDocument8 pagesNCM 112 - HepatitisMara Jon Ocden CasibenNo ratings yet
- Viral Hepatitis TableDocument2 pagesViral Hepatitis TableJohnNo ratings yet
- Viral HepatitisDocument12 pagesViral HepatitisHeart Of Ayurveda Beatrice DNo ratings yet
- Hep ADocument13 pagesHep ARakesh SharmaNo ratings yet
- Obstructive JaundiceDocument54 pagesObstructive JaundiceJenine Ezra M. Conol50% (2)
- CHN ExamDocument16 pagesCHN ExamGlenn Daryll SantosNo ratings yet
- Liver FunctionDocument90 pagesLiver Functionapi-19641337100% (1)
Cesar, Katyana Antoine - Common Laboratory and Diagnostics Procedures Used in Gi Disorders (Rle Worksheet No. 3)
Cesar, Katyana Antoine - Common Laboratory and Diagnostics Procedures Used in Gi Disorders (Rle Worksheet No. 3)
Uploaded by
kdfhjfhf0 ratings0% found this document useful (0 votes)
73 views30 pagesThis document discusses common non-invasive gastrointestinal diagnostic procedures, including liver function tests, hepatitis screening, and alpha-fetoprotein testing. Liver function tests measure blood levels of liver enzymes and proteins to screen for and monitor liver disease. Hepatitis screening determines infection status for hepatitis A, B, and C through antibody and antigen testing. Alpha-fetoprotein is a tumor marker that may indicate liver, ovarian, or testicular cancers when levels are elevated. Nursing responsibilities include educating patients, obtaining samples correctly, and monitoring for complications or abnormal results that require treatment.
Original Description:
Original Title
CESAR, KATYANA ANTOINE - COMMON LABORATORY AND DIAGNOSTICS PROCEDURES USED IN GI DISORDERS (RLE WORKSHEET NO. 3)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses common non-invasive gastrointestinal diagnostic procedures, including liver function tests, hepatitis screening, and alpha-fetoprotein testing. Liver function tests measure blood levels of liver enzymes and proteins to screen for and monitor liver disease. Hepatitis screening determines infection status for hepatitis A, B, and C through antibody and antigen testing. Alpha-fetoprotein is a tumor marker that may indicate liver, ovarian, or testicular cancers when levels are elevated. Nursing responsibilities include educating patients, obtaining samples correctly, and monitoring for complications or abnormal results that require treatment.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
73 views30 pagesCesar, Katyana Antoine - Common Laboratory and Diagnostics Procedures Used in Gi Disorders (Rle Worksheet No. 3)
Cesar, Katyana Antoine - Common Laboratory and Diagnostics Procedures Used in Gi Disorders (Rle Worksheet No. 3)
Uploaded by
kdfhjfhfThis document discusses common non-invasive gastrointestinal diagnostic procedures, including liver function tests, hepatitis screening, and alpha-fetoprotein testing. Liver function tests measure blood levels of liver enzymes and proteins to screen for and monitor liver disease. Hepatitis screening determines infection status for hepatitis A, B, and C through antibody and antigen testing. Alpha-fetoprotein is a tumor marker that may indicate liver, ovarian, or testicular cancers when levels are elevated. Nursing responsibilities include educating patients, obtaining samples correctly, and monitoring for complications or abnormal results that require treatment.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 30
DOÑA REMEDIOS TRINIDAD ROMUALDEZ MEDICAL FOUNDATION, INC.
COLLEGE OF NURSING
2nd Semester, S.Y. 2019-2020
NCM 109: maternal and
Child Nursing
Worksheet on NCM 109 RLE
Nursing Care of a Family
When a Child has a
Gastrointestinal Disorder
Common Laboratory and
Diagnostic Procedures used in
Gastrointestinal Disorders
:
KATYANA ANTOINE D. CESAR
BSN – 2B
NON-INVASIVE PROCEDURES:
A. LIVER FUNCTION TEST
I. DESCRIPTION
Help determine the health of your liver by measuring the levels of proteins, liver enzymes, and bilirubin in your blood.
II. INDICATION
Liver function tests can be used to: Screen for liver infections, such as hepatitis. Monitor the progression of a disease, such
as viral or alcoholic hepatitis, and determine how well a treatment is working. Measure the severity of a disease, particularly
scarring of the liver (cirrhosis)
III. CONTRAINDICATION
Because LFTs are checked with a routine blood test, there are minimal risks and no contraindications.
IV. NORMAL VALUES/ FINDINGS
Normal blood test results for typical liver function tests include:
ALT. 7 to 55 units per liter (U/L)
AST. 8 to 48 U/L
ALP. 40 to 129 U/L
Albumin. 3.5 to 5.0 grams per deciliter (g/dL)
Total protein. 6.3 to 7.9 g/dL
Bilirubin. 0.1 to 1.2 milligrams per deciliter (mg/dL)
GGT. 8 to 61 U/L
LD. 122 to 222 U/L
PT. 9.4 to 12.5 seconds
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Elevated levels of bilirubin (jaundice) might indicate liver damage or disease or certain types of anemia. Gamma-
glutamyltransferase (GGT). GGT is an enzyme in the blood. Higher-than-normal levels may indicate liver or bile duct damage.
VI. PATIENT PREPARATION
The patient should be N.P.O. for 4 hours before you draw blood for bilirubin and ALP levels and be N.P.O. for 8 hours and
abstain from alcohol for 24 hours before a GGT level. Otherwise, no special preparation is needed.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Before the Study: Planning and Implementation
Teaching the Patient What to Expect
Inform the patient this test can assist with evaluation of liver function and help identify liver disease.
Explain that a blood sample is needed for the test.
After the Study: Potential Nursing Actions
Avoiding Complications
The patient with cirrhosis should be carefully observed for the development of ascites, in which case fluid and
electrolyte balance requires strict attention.
Treatment Considerations
Fluid Volume Deficit: Collaborate with health-care provider (HCP) regarding administration of IV fluids to support
optimal hydration. Monitor laboratory values that reflect alterations in fluid status: potassium, BUN, Cr, calcium,
Hgb, and Hct. Administer replacement electrolytes, as ordered, to manage underlying cause of fluid alteration;
monitor urine characteristics and respiratory status. Trend vital signs and daily weight, and perform strict intake
and output.
Fluid Volume Overload: Measure abdominal girth and trend size. Monitor and trend laboratory values: albumin,
protein, and globulin. Assess for dehydration and increase fluids if present (fluid shifts from intravascular to
extravascular can result in concerns related to hydration status). Administer ordered diuretics. Trend vital signs
and daily weight, and perform strict intake and output.
GI Problems: Perform nasogastric intubation to remove gastric secretions and decrease pancreatic secretions,
which may result in autodigestion. Monitor nasogastric tube for patency and amount of drainage, and assess
bowel sounds frequently. Measure abdominal girth to monitor degree of abdominal distention.
Pain: Collaborate with the patient and HCP to identify the best pain management modality. Refrain from activities
that may increase pain. Apply heat or cold to the best effect in managing pain, and monitor pain severity.
Nutritional Considerations
Increased ALT levels may be associated with liver disease. In general, patients should be encouraged to eat a well-
balanced diet that includes foods high in fiber. Dietary recommendations will vary depending on the condition and its
severity. For example, a soft foods diet is recommended if esophageal varices develop, fat substitutes are
recommended if bile duct disease is diagnosed, and salt intake should be limited if ascites develop.
Administer ordered enteral or parenteral nutrition; monitor laboratory values (albumin, protein, potassium) and
collaborate with HCP on replacement strategies; correlate laboratory values with IV fluid infusion, and collaborate with
the HCP and pharmacist to adjust to patient needs; ensure adequate pain c
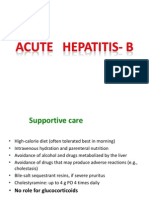
B. HEPATIC SEROLOGY (HEPATITIS SCREENING)
I. DESCRIPTION
Hepatitis serology (HepA, HepB, HepC) is a relatively complex set of tests to determine past infection, current infection,
immunity and infectivity relating to the Hepatitis viruses. These viruses all affect the liver, but behave quite differently from
each other
II. INDICATION
Screening test to determine hepatitis status, for example prior to childbirth, dialysis or a surgical procedure
Investigation of jaundice (yellow skin or eyes) or abnormal Liver Function Tests (LFTs)
Checking immunity to Hepatitis B, for healthcare workers or those with occupational (or non-occupational) exposure to body
fluids with infective potential – e.g. a needle stick injury
III. CONTRAINDICATION
N/A
IV. NORMAL VALUES/ FINDINGS
Any value between 1 and 5 s/c is indeterminate and should be repeated. For hepatitis B surface antibody (anti-HBs),
a level less than 5 mIU is considered negative, while a level more than 12 mIU is considered protective. Any value between 5
and 12 mIU is indeterminate and should be repeated.
V. SIGNIFICANT ABNORMAL VALUE/FINDING
There are different tests for hepatitis A and hepatitis B. A positive test is considered abnormal.
A positive test may mean:
You currently have a hepatitis infection. This may be a new infection (acute hepatitis), or it may be an infection
that you have had for a long time (chronic hepatitis).
You had a hepatitis infection in the past, but you no longer have the infection and can't spread it to others.
Hepatitis A test results:
IgM anti-hepatitis A virus (HAV) antibodies, you have had a recent infection with hepatitis A
Total (IgM and IgG) antibodies to hepatitis A, you have a previous or past infection, or immunity to hepatitis A
Hepatitis B test results:
Hepatitis B surface antigen (HBsAg): you have an active hepatitis B infection, either recent or chronic (long-term)
Antibody to hepatitis B core antigen (Anti-HBc), you have a recent or past hepatitis B infection
Antibody to HBsAg (Anti-HBs): you have a past hepatitis B infection or you have received the hepatitis B vaccine
and are unlikely to become infected
Hepatitis B type e antigen (HBeAg): you have a chronic hepatitis B infection and you are more likely to spread the
infection to others through sexual contact or by sharing needles
Antibodies to hepatitis C can most often be detected 4 to 10 weeks after you get the infection. Other types of tests may be
done to decide on treatment and monitor the hepatitis C infection.
VI. PATIENT PREPARATION
No special preparation is needed.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Prior to taking the blood sample, the nurse should inform the patient about the test(s) to be performed and the preparation
for the test. You should:
Define and explain the test
State the specific purpose of the test
Explain the procedure
Discuss test preparation, procedure, and posttest care
C. ALPHA FETO PROTEINS
I. DESCRIPTION
An AFP tumor marker test is a blood test that measures the levels of AFP in adults. Tumor markers are substances made
by cancer cells or by normal cells in response to cancer in the body. High levels of AFP can be a sign of liver cancer or cancer
of the ovaries or testicles, as well as noncancerous liver diseases such as cirrhosis and hepatitis
II. INDICATION
Help confirm or rule out a diagnosis of liver cancer or cancer of the ovaries or testicles.
Monitor cancer treatment. AFP levels often go up if cancer is spreading and go down when treatment is working.
See if cancer has returned after treatment.
Monitor the health of people with cirrhosis or hepatitis.
III. CONTRAINDICATION
N/A
IV. NORMAL VALUES/ FINDINGS
AFP is measured in nanograms per milliliter (ng/mL). An AFP level of less than 10 ng/mL is normal for adults. An extremely
high level of AFP in your blood—greater than 500 ng/mL—could be a sign of liver tumors.
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
If your results show high levels of AFP, it may confirm a diagnosis of liver cancer, or cancer of the ovaries or testicles.
Sometimes, high levels of AFP can be a sign of other cancers, including Hodgkin disease and lymphoma, or noncancerous
liver disorders.
VI. PATIENT PREPARATION
No special preparation is necessary before an AFP test.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Explain that the AFP tests helps in monitoring fetal development, screens for a need for further testing, helps detect possible
congenital defects in the fetus, and monitors the patient’s response to therapy by measuring a specific blood protein, as
appropriate.
Inform the patient that she need not restrict food, fluids, or medications.
Tell the patient that the test requires a blood sample. Explain who will perform the venipuncture and when.
Explain to the patient that she may experience slight discomfort from the tourniquet and needle puncture.
Perform a venipuncture and collect the sample in a 7 ml clot-activator tube.
Record the patient’s age, race, weight, and week of gestation on the laboratory request.
Handle the sample gently to prevent hemolysis.
Place the patient in comfortable position.
Encourage deep breathing exercise to alleviate fear.
Apply direct pressure to the venipuncture site until bleeding stops.
D. SERUM AMYLASE AND LIPASE
I. DESCRIPTION
Amylase and lipase are key digestive enzymes. Amylase helps your body break down starches. Lipase helps your body digest
fats. The pancreas is a glandular organ that sits behind the stomach and produces digestive juices that empty into the small
intestine. The pancreas also produces both amylase and lipase, as well as many other enzymes.
Serum amylase and lipase tests are used to diagnose and monitor treatment of acute pancreatitis and to differentiate
pancreatitis from other acute abdominal disorders (80% of patients with acute pancreatitis will have elevated amylase and
lipase levels; lipase stays elevated longer). Lipase assay provides better sensitivity and specificity and is best used with
amylase determination.
II. INDICATION
N/A
III. CONTRAINDICATION
The nurse or phlebotomist should follow standard precautions for the prevention of transmission of bloodborne pathogens.
Amylase and lipase should not be used as screening tests for future pancreatic disease. Neither enzyme is likely to be
elevated in chronic pancreatitis because enzyme production is decreased by chronic disease. Drugs that may increase
amylase include morphine, phenformin, ethanol, and contraceptives. Lipase may be increased by ethanol, codeine, and
narcotics. Results are dependent upon the method used and normal values may vary significantly among laboratories.
IV. NORMAL VALUES/ FINDINGS
Amylase:
Newborns: 6-65 U/L
Adults: 25-125 U/L
Elderly persons (>60 years):24-151 U/L
Lipase
Adults: 10-140 U/L
Elderly persons (>60 years):18-180 U/L
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
When levels of lipase and amylase are higher than normal it may indicate pancreatic injury or another disease. Most studies
show that levels of greater than three times the upper limit of normal usually lead to a diagnosis of pancreatitis, according
to guidelines from the American College of Gastroenterology (ACG).
Greatly increased amylase levels occur in acute pancreatic early in the course of the disease. The increase begins in 3-
6 hours after the onset of pain.
Increased amylase levels also occur in the following conditions:
Chronic pancreatitis, pancreatic trauma, pancreatic carcinoma, obstruction of pancreatic duct
Partial gastrectomy
Acute appendicitis, peritonitis
Perforated peptic ulcer
Cerebral trauma or shock
Obstruction or inflammation of salivary duct or gland and mumps
Acute cholecystitis (common duct stone)
Intestinal obstruction with strangulation
Ruptured tubal pregnancy and ectopic pregnancy
Ruptured aortic aneurysm
Macroamylasemia
Decreased amylase levels occur in the following conditions:
Pancreatic insuffieciency
Hepatitis, severe liver disease
Advance cystic fibrosis
Pancreatectomy
Elevated lipase levels occur in pancreatic disorders (e.g, pancreatitis, alcoholic and non-alcoholic; pancreatic
carcinoma).
Increased lipase values also are associated with the following conditions:
Cholecystitis
Hemodialysis
Strangulated or infarcted bowel
Peritonitis
Primary biliary cirrhosis
Chronic renal failure
VI. PATIENT PREPARATION
There’s no special preparation necessary for an amylase or lipase blood test.
VII. NURSING CONSIDERATION & RESPONSIBILITES
A nurse or phlebotomist usually collects blood for amylase and lipase tests by venipuncture.
Educate the patient on the proper collection and storage of a urine sample, and may also take a drug history to identify
medications which might interfere with the testing.
Explain test purpose and procedure. Amylase and lipase testing are done together in the presence of abdominal pain,
epigastric tenderness, nausea, and vomiting. These findings characterize acute pancreatitis as well as other acute surgical
emergencies.
If amylase/creatinine clearance testing is also being done, collect a single, random urine sample at the same time blood is
drawn.
Have patient resume normal activities.
Interpret results and monitor as appropriate for pancreatitis or other acute abdominal conditions.
E. HELICOBACTER PYLORI TEST
I. DESCRIPTION
Helicobacter pylori tests are used to detect a Helicobacter pylori (H. pylori) infection in the stomach and upper part of the
small intestine (duodenum). H. pylori can cause peptic ulcers. But most people with H. pylori in their digestive systems do
not develop ulcers.
Four tests are used to detect H. pylori:
Blood antibody test. A blood test checks to see whether your body has made antibodies to H. pylori bacteria. If you have
antibodies to H. pylori in your blood, it means you either are currently infected or have been infected in the past.
Urea breath test. A urea breath test checks to see if you have H. pylori bacteria in your stomach. This test can show if
you have an H. pylori infection. It can also be used to see if treatment has worked to get rid of H. pylori.
Stool antigen test. A stool antigen test checks to see if substances that trigger the immune system to fight an H.
pylori infection (H. pylori antigens) are present in your feces (stool). Stool antigen testing may be done to help support
a diagnosis of H. pylori infection or to find out whether treatment for an H. pylori infection has been successful.
Stomach biopsy. A small sample (biopsy) is taken from the lining of your stomach and small intestine during
an endoscopy. Several different tests may be done on the biopsy sample. To learn more, see the topic Upper
Gastrointestinal Endoscopy.
II. INDICATION
Assist in differentiating between H. pylori infection and nonsteroidal anti-inflammatory drug (NSAID) use as the cause of
gastritis or peptic or duodenal ulcer
Assist in establishing a diagnosis of gastritis, gastric carcinoma, or peptic or duodenal ulcer
III. CONTRAINDICATION
N/A
IV. NORMAL VALUES/ FINDINGS
Negative for H. pylori by ELISA indicated no detectable IgG antibody in serum or stool.
IgM:
≤30 U/mL (negative)
30.01-39.99 U/mL (equivocal)
≥40 U/mL (positive)
IgG
<0.75 (negative)
0.75-0.99 (equivocal)
≥1 (positive)
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
A positive result indicates the presence of detectable IgG antibody in serum or stool.
VI. PATIENT PREPARATION
Tell the doctor if you are pregnant, have a lung or heart condition or any other disease, or if you are allergic to
any medications.
Do not take any antibiotics for at least 4 weeks before the test.
Do not take any proton pump inhibitors (Prilosec, Prevacid, Aciphex, Nexium, Protonix) or Pepto-Bismol for at least 2 weeks
before the test.
Take only the medications approved by your doctor the day of the procedure. Take them only with a small sip of water if it
is within four hours of the procedure. Do not discontinue any medication without first consulting with your primary or
referring doctor.
Do not eat or drink anything (including water) for four hours before the procedure.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pretest:
Obtain a history of the patient’s complaints, including a list of known allergens.
Obtain a history of the patient’s gastrointestinal and immune systems, as well as results of previously performed tests
and procedures. For related tests, refer to the gastrointestinal and immune system tables.
Obtain a list of the medications the patient is taking, including herbs, nutritional supplements, and nutraceuticals. The
requesting health care practitioner and laboratory should be advised if the patient regularly uses these products so
that their effects can be taken into consideration when reviewing results.
There are no food, fluid, or medication restrictions unless by medical direction.
Inform the patient that each specimen collection takes approximately 5 to 10 minutes.
Intratest:
Direct the patient to breathe normally and to avoid unnecessary movement.
Observe standard precautions and follow the general guidelines in Appendix A. Perform a venipuncture, and collect the
specimen in a 5-mL red-top tube.
Label the specimen, and promptly transport it to the laboratory.
Post-test:
Observe venipuncture site for bleeding or hematoma formation. Apply pressure bandage.
Inform the patient that a positive test result constitutes an independent risk factor for gastric cancer.
Evaluate test results in relation to the patient’s symptoms and other tests performed. Related laboratory tests include
gastrin and gastric acid stimulation.
F. STOOL EXAMINATION
I. DESCRIPTION
Examination of a stool specimen can detect several types of intestinal parasites. Some of these parasites live in
nonpathogenic symbiosis; others cause intestinal disease.
II. INDICATION
Aid in diagnosing disorders related to gastrointestinal (GI) bleeding or medication therapy that results in bleeding
Assist in the diagnosis of pseudomembranous enterocolitis following the use of broad-spectrum antibiotic therapy
Help diagnose suspected inflammatory bowel syndrome (IBS)
Identify the cause of diarrhea of unknown origin
Investigate disorders of protein digestion
Screen for colorectal cancer
Screen for cystic fibrosis
Determine intestinal parasitic infestation, as indicated by diarrhea of unknown cause
Evaluate the effectiveness of therapeutic regimen for intestinal malabsorption or pancreatic insufficiency
III. CONTRAINDICATION
N/A
IV. NORMAL VALUES/ FINDINGS
No parasites or ova should appear in stool.
CHARACTERISTICS OF STOOL NORMAL FINDINGS
APPEARANCE SOLID AND FORMED
COLOR BROWN
EPITHELIAL CELLS FEW TO MODERATE
FECAL FAT LESS THAN 7 GRAMS OF FAT PER 24 HOURS
LEUKOCYTES (WHITE BLOOD CELLS) NEGATIVE
MEAT FIBERS NEGATIVE
OCCULT BLOOD NEGATIVE
REDUCING UBSTANCES NEGATIVE
TRYPSIN 2+ TO 4+
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Unusual appearance:
Mucous: Intestinal wall inflammation
Bloody: Excessive intestinal wall irritation or malignancy
Frothy or bulky: Malabsorption
Ribbonlike or slender: Obstruction
Unusual color:
Red: Beets and food coloring, lower GI bleed, phenazopyridine hydrochloride compounds, rifampicin
Black: Bismuth (antacid) or charcoal ingestion, iron therapy, upper GI bleeding
Yellow: Rhubarb
Green: Antibiotics, biliverdin, green vegetables
Grayish white: Barium ingestion, bile duct obstruction
Increased:
Blood: related to GI bleeding
Occult blood: Diverticular disease, esophagitis, gastritis, esophageal varices, anal fissure, hemorrhoids, infectious
diarrhea, inflammatory bowel disease, polyps, tumors, ulcers, Mallory-Weiss tears
Leukocytes: Inflammation of the intestines related to bacterial infections of the intestinal wall, ulcerative colitis,
shigellosis, or salmonellosis
Epithelial cells: Inflammatory bowel disorders
Carbohydrates/reducing substances: Inability to digest some sugar, malabsorption syndromes
Fats: Sprue (celiac disease), cystic fibrosis related to malabsorption, pancreatitis
pH: Related to inflammation in the intestine from colitis, cancer, or antibiotic use
Meat fibers: Pancreatitis, impaired protein digestion
Decreased:
Leukocytes: Disorders resulting from toxins, cholera, viral diarrhea, amebic colitis, parasites
Carbohydrates/reducing substances: Cystic fibrosis, sprue, malnutrition, medications such as colchicine or birth control
pills
pH: Related to poor absorption of carbohydrate or fat
Trypsin: Malabsorption syndrome, pancreatic deficiency, cystic fibrosis
VI. PATIENT PREPARATION
Tell your doctor if you are pregnant, have a lung or heart condition or any other disease, or if you are allergic to
any medications.
Do not take any antibiotics for at least 4 weeks before the test.
Do not take any proton pump inhibitors (Prilosec, Prevacid, Aciphex, Nexium, Protonix) or Pepto-Bismol for at least 2 weeks
before the test.
Take only the medications approved by your doctor the day of the procedure. Take them only with a small sip of water if it
is within four hours of the procedure. Do not discontinue any medication without first consulting with your primary or
referring doctor.
Do not eat or drink anything (including water) for four hours before the procedure.
VII. NURSING CONSIDERATIONS AND RESPONSIBILITIES
Before the procedure
Assess the patient’s level of comfort. Collecting stool specimen may produce a feeling of embarrassment and
discomfort to the patient.
Encourage the patient to urinate. Allow the patient to urinate before collecting to avoid contaminating the stool
with urine.
Avoid laxatives. Advise patient that laxatives, enemas, or suppositories are avoided three days prior to collection.
Instruct a red-meat free and high residue diet. The patient is indicated for an occult blood test, must follow a special
diet that includes generous amounts of chicken, turkey, and tuna, raw and uncooked vegetables and fruits such as
spinach, celery, prunes and bran containing cereal for two (2) days before the test.
After the procedure
Instruct patient to do handwashing. Allow the patient to thoroughly clean his or her hands and perianal area.
Resume activities. The patient may resume his or her normal diet and medication therapy unless otherwise specified.
Recommend regular screening. The American Cancer Society recommends yearly occult blood test as part of the
screening for colorectal cancer starting at the age of 45 years old for people with average risk.
G. FECAL OCCULT BLOOD TEST
I. DESCRIPTION
Occult blood tests for the presence of blood in the stool as an indicator of gastrointestinal bleeding. Since smaller amounts
of blood are not always visible (e.g., in earlier stages of some GI diseases), a chemical test will confirm its presence and cue
further testing and examination for pathophysiology.
II. INDICATION
Screens for carcinomas (particularly colon) and polyps of GI tract.
Identifies GI bleeding related to upper GI bleeding (gastric ulcer).
Screens for diverticulitis and colitis.
III. CONTRAINDICATION
Menstruation
Barium enema in the last 72 hrs.
IV. NORMAL VALUES/ FINDINGS
Negative for blood
V. SIGNIFICANT ABNORMAL VALUES/ FINDINGS:
Positive testing for occult blood may be caused by the following conditions:
Carcinoma of colon
Ulcerative colitis and other inflammatory lesions
Adenoma
Diaphragmatic hernia
Gastric carcinoma
Rectal carcinoma
Peptic ulcer
Gastritis
Vasculitis
Amyloidosis
Kaposi’s sarcoma (tumors caused by human herpesvirus 8 [HHV8] presenting with cutaneous lesions)
VI. PATIENT PREPARATION
Explain the test procedure and the purpose of the test.
Assess the client’s knowledge of the test.
Instruct client not to eat foods for 2 days that interfere with results.
Recommend that the patient consume a high-residue diet, starting 72 hours before and continuing throughout the
collection period. Roughage in diet can increase test accuracy by helping to uncover silent lesions that bleed
intermittently. The diet may include the following:
Meats: only small amounts of chicken, turkey, and tuna
Vegetables: generous amounts of both raw and cooked vegetables, including lettuce, corn, spinach, carrots, and celery;
avoid vegetables with high peroxidase activity (see 3b above)
Fruits: plenty of fruits, especially prunes
Cereals: bran and bran-containing cereals
Moderate amounts of peanuts and popcorn daily. If any of the above foods are known to cause discomfort, the patient
should consult the physician.
Inform client that one method of collecting the specimen is to place a loose film of plastic wrap across the toilet bowl
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pediatric: Infants and children will need assistance in obtaining stool specimen and age-appropriate comfort measures
following the test.
Gerontology: Elderly clients are more at risk for interfering factors associated with constipation and hemorrhoids.
Home Care: If home testing, advise the client to inform the health care provider of positive results. Instruct the client that if
sending specimens to laboratory, the sample kits should be kept closed after each random stool sampling and should not
be stored in refrigerator or near heat or light.
H. STOOL CULTURE AND ANALYSIS
I. DESCRIPTION
Stool cultures are used to diagnose pathogens, which may be causing abnormal bowel patterns, specifically diarrhea. Stool
cultures are most often used to identify enteric disease pathogens. Fecal material is a waste product of the gastrointestinal
system. It is normally assessed for its color, odor, and consistency after a rectal examination or after defecation.
II. INDICATION
Diagnoses and monitors Salmonella, Shigella, Campylobacter jejuni, enteropathogenic E. coli, Helicobacter, Clostridium
difficile, and Yersinia enterocolitica.
Evaluates and monitors pure cultures of S. aureus and various parasites.
III. CONTRAINDICATION
Feces from patients receiving barium, bismuth, mineral oil, or antibiotics are not satisfactory specimens for identifying
protozoa
IV. NORMAL VALUES/ FINDINGS
The following organisms may be present in the stool of apparently healthy people:
C. albicans
Enterococcus spp.
E. coli
Proteus spp.
Pseudomonas aeruginosa
Streptococcus spp.
Staphylococcus spp.
Positive results reported when Staphylococcus grows on the culture; no growth in 48 hr. indicates negative test.
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS:
A positive test result means that your poop was infected with a germ, virus, or other type of bacteria. The lab will tell your
doctor which type it is and which medicines will fight against it.
Positive results reported when Staphylococcus grows on the culture.
VI. PATIENT PREPARATION
Explain purpose and procedure. Obtain history of diarrhea, including type and length of time.
Instruct the patient to defecate into a clean, dry bedpan or large-mouthed container.
Do not allow patient to defecate into the toilet bowl or urinate into the bedpan or collecting container because urine has
an adverse effect on protozoa.
Do not place toilet paper into the bedpan or collection container; it may contain bismuth, which can interfere with testing.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pediatric: Usually only one stool culture ordered. It is not recommended to order stool cultures after 4 days of hospitalization.
Infants and children will need assistance in remaining still during the collection of the stool and age-appropriate comfort
measures following the test.
Gerontology: Precipitating factors leading to decreased bowel elimination in the older adult include lack of bulk in the diet,
decreased fluid intake, decreased activity, laxative abuse, and avoidance of the need to defecate. In addition, rectal neurons
may degenerate with age, which results in decreased sphincter control and fecal incontinence.
International: Diarrhea is the leading cause of death worldwide; parasites are frequently found in the gastrointestinal tracts
of persons living in third world countries.
I. STOOL OVA PARASITE TEST
I. DESCRIPTION
This test evaluates stool for the presence of intestinal parasites and their eggs. Some parasites are nonpathogenic; others,
such as protozoa and worms, can cause serious illness.
II. INDICATION
Assist in the diagnosis of parasitic infestation.
III. CONTRAINDICATION
N/A
IV. NORMAL VALUES/ FINDINGS
No presence of parasites, ova, or larvae.
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Amebiasis—Entamoeba infection histolytica
Ascariasis—Ascaris lumbricoides infection
Blastocystis—Blastocystis hominis infection
Cryptosporidiosis—Cryptosporidium parvum infection
Enterobiasis—Enterobius vermicularis (pinworm) infection
Giardiasis—Giardia lamblia infection
Hookworm disease—Ancylostoma duodenale, Necator americanus infection
Isospora—Isospora belli infection
Schistosomiasis—Schistosoma haemato- bium, Schistosoma japonicum, Schistosoma mansoni infection
Strongyloidiasis—Strongyloides stercoralis infection
Tapeworm disease—Diphyllobothrium, Hymenolepiasis, Taenia saginata, Taenia solium infection
Trematode disease—Clonorchis sinensis, Fasciola hepatica, Fasciolopsis buski infection
Trichuriasis—Trichuris trichiura infection
VI. PATIENT PREPARATION
Obtain a history of the patient’s complaints, and document any travel to foreign countries. Obtain a list of known allergens.
Obtain a history of the patient’s gastrointestinal and immune systems, as well as results of previously per- formed tests and
procedures. For related tests, refer to the gastrointestinal and immune system tables.
Obtain a list of the medications the patient is taking, including herbs, nutritional supplements, and nutraceuticals. The
requesting health care practitioner and laboratory should be advised if the patient regularly uses these products so their
effects can be taken into consideration when re- viewing results.
Instruct the patient to avoid medications that interfere with test results.
Note any recent therapies that can interfere with test results.
Instruct the patient on handwashing procedures, and inform the patient that the infection may be contagious.
There are no food or fluid restrictions unless by medical direction.
Review the procedure with the patient. Warn the patient not to contaminate the specimen with urine, toilet paper, or toilet
water.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pediatrics: Infants and children will need assistance in remaining still during the collection of the stool and age-appropriate
comfort measures following the test.
Rural: Rural settings are more likely to have unpurified drinking water, which is a common cause of parasite infestation.
Client education should be provided, especially if there is an outbreak of identified parasites in a given area.
International: Obtain information regarding any countries client has visited within the past 3 years. People traveling outside
the North American continent should be evaluated for a history of drinking unpurified drinking water, which can lead to
parasite infection
J. LACTOSE TOLERANCE TEST
I. DESCRIPTION
Lactose is a disaccharide found in dairy products. When ingested, lactose is broken down in the intestine, by the sugar-
splitting enzyme lactase, into glucose and galactose. When sufficient lactase is not available, intestinal bacteria metabolize
the lactose, resulting in abdominal bloating, pain, flatus, and diarrhea. The lactose tolerance test screens for lactose
intolerance by monitoring glucose levels after ingestion of a dose of lactose.
II. INDICATION
Evaluate patients for suspected lactose intolerance
III. CONTRAINDICATION
N/A
IV. NORMAL VALUES/ FINDINGS
Normal: greater than 30 mg/dL or greater than 1.7 mmol/L
Inconclusive: 20-30 mg/dL or 1.1-1.7 mmol/L
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Less than 20 mg/dl or less than 1.1 mmol/ L
Glucose levels decreased in: Lactose intolerance
VI. PATIENT PREPARATION
Obtain a history of the patient’s complaints, including a list of known allergens.
Obtain a history of the patient’s gastrointestinal system and results of previously performed tests and procedures. For related
tests, refer to the gastrointestinal system table.
Obtain a list of the medications the patient is taking, including herbs, nutritional supplements, and nutraceuticals. The
requesting health care practitioner and laboratory should be advised if the patient regularly uses these products so that their
effects can be taken into consideration when reviewing results.
There are no medication restrictions unless by medical direction.
Inform the patient that fasting for at least 12 hours before the test is required and that strenuous activity should also be
avoided for at least 12 hours before the test.
Review the procedure with the patient. Inform the patient that the test may produce symptoms such as cramps and diarrhea.
Instruct the patient not to smoke cigarettes or chew gum during the test.
Obtain the pediatric patient’s weight to calculate dose of lactose to be administered.
Inform the patient that multiple samples over a 90-minute interval will be collected and that each specimen collection takes
approximately 5 to 10 minutes.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pediatric: Infants and children will need assistance in remaining still during the venipuncture and age-appropriate comfort
measures following the test. Lactose intolerance is often a congenital condition and may be present in newborns. The child’s
weight determines strength of lactose mixture for treatment.
Home Care: Clients in the home settings need to be taught that symptoms such as IBS, gas, bloating, abdominal discomfort,
constipation, and diarrhea are indicative of lactose intolerance. Consequently, the clients should report these clinical
manifestations to their health care provider.
International: There is a higher prevalence of lactose tolerance in Native Americans, African Americans, Asians, and Jews.
INVASIVE PROCEDURES:
A. ABDOMINAL X-RAY
I. DESCRIPTION
The abdominal film is taken to aid in the diagnosis of gastrointestinal, biliary system, and urological diseases. It may provide
information on the size, shape, and position of the liver, spleen, and kidneys.
II. INDICATION
Evaluates abdominal masses and large tumors (e.g., ovarian or uterine).
Diagnoses intestinal obstruction and acute abdominal pain of unknown origin.
Identifies abnormal air (e.g., bowel perforation/obstruction), fluid (e.g., ascites), or objects in the abdomen.
Precursor to urological and gastrointestinal tract contrast-mediated studies.
Detects calcium deposits in the following; blood vessels and lymph nodes, cysts, tumors and stones.
Detects abnormal kidney/liver/spleen size, shape and position.
Differentiates between gastrointestinal and urological disorders.
III. CONTRAINDICATION
Abdominal films are not appropriate for some specific conditions, such as hemorrhaging gastrointestinal ulcers, or pregnancy
(unless the benefits outweigh the risks to the fetus).
IV. NORMAL VALUES/ FINDINGS
Differentiating the small and large bowel on an AXR is not always straightforward but there are a number of clues that can
help you:
The small bowel usually lies more centrally, with the large bowel framing it around the periphery.
The small bowel’s mucosal folds are called valvulae conniventes and are seen across the full width of the bowel.
The large bowel wall features pouches or sacculation that protrude into the lumen that are known as haustra. In between
the haustra are spaces known as plicae semilunaris. The haustra are thicker than the valvulae conniventes of the small
bowel. They also commonly do not appear to completely traverse the bowel. This distinction is unfortunately unreliable
as dilated large bowel can have a haustral pattern that does in fact traverse the bowel.
Feces have a mottled appearance and are most often seen in the colon, due to trapped gas within solid feces
There is considerable normal variation in the distribution of bowel gas.
The normal diameter of the intestines on an AXR do not usually exceed:
3 cm for small bowel
6 cm for colon (large bowel)
9 cm for caecum
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Small bowel obstruction
Small bowel obstruction can be visualized on an AXR as dilatation of the small bowel (>3cm).
The valvulae conniventes are much more visible and have what is referred to as a “coiled spring appearance”.
The most common cause (75%) of small bowel obstruction in the developed world is adhesions (mostly relating to
previous abdominal surgery). Some other causes include abdominal hernias (10%) and either intrinsic or extrinsic
compression by neoplastic masses.
You should inspect the inguinal regions on the x-ray if considering a hernia as a cause of small bowel obstruction, as
they are often fairly obvious even on plain abdominal x-rays
Large bowel obstruction
The most common causes of large bowel obstruction are colorectal carcinoma and diverticular strictures. Less common
causes are hernias and volvulus.
Volvulus is a twisting of the bowel on its mesentery and most commonly occurs at the sigmoid colon or caecum. Patients
with volvulus are at high risk of bowel perforation and/or bowel ischemia secondary to vascular compromise.
Sigmoid volvulus has a characteristic ‘coffee bean’ appearance
Caecal volvulus is often described as having a fetal appearance
Rigler’s (double wall) sign
Normally only the inner wall of the bowel is visible on an AXR.
Pneumoperitoneum may cause both sides of the bowel wall to be visible.
Causes of pneumoperitoneum include a perforated abdominal viscus (e.g. perforated bowel, perforated duodenal
ulcer) and recent abdominal surgery.
You should look closely for air under the diaphragm on an erect CXR if you suspect pneumoperitoneum.
Features of inflammatory bowel disease on AXR
Thumb-printing – mucosal thickening of the haustra due to inflammation and edema causing them to appear like thumb
prints projecting into the lumen
Lead-pipe (featureless) colon – loss of normal haustral markings secondary to chronic colitis
Toxic megacolon – colonic dilatation without obstruction associated with colitis
Other organs and structures
Although AXR isn’t well suited to imaging these structures, it’s useful to recognize them to help orientate yourself and
spot relevant pathology.
Lungs – check the lung bases if visible for pathology (e.g. consolidation) as abdominal pain can sometimes be caused
by basal pneumonia
Liver – large right upper quadrant (RUQ) structure
Gallbladder – rarely seen, look for calcified gallstones and cholecystectomy clips
Stomach – left upper quadrant (LUQ) to midline structure, containing a variable amount of air
Psoas muscles – lateral edge marked by a relatively straight line either side of the lumbar vertebrae and sacrum
Kidneys – often visible, right lower than left due to the liver
Spleen – LUQ, superior to left kidney
Bladder – variable appearance depending on fullness
Bones
Lots of bones are visible on an AXR and it’s important that you can identify each and screen for any pathology (which
may be expected or unexpected). In addition, bones on the AXR provide useful landmarks for where you might expect
to see a soft tissue structure (e.g. ischial spines are the usual level of the vesico-ureteric junction).
Bones commonly visible on AXR include:
Ribs
Lumbar vertebrae
Sacrum
Coccyx
Pelvis
Proximal femurs
A wide range of bony pathologies can be identified on abdominal x-rays including fractures, osteoarthritis, Paget’s
disease and bony metastases.
Calcification and artefact
Various high density (white) areas of calcification or artefact may be seen.
Examples include:
Calcified gallstones in the RUQ
Renal stones/staghorn calculi
Pancreatic calcification
Vascular calcification
Costochondral calcification
Contrast (e.g. following a barium meal)
Surgical clips
Naval jewelry artefact over the approximate location of the umbilicus
VI. PATIENT PREPARATION
Explain the test procedure and the purpose of the test. Assess the client’s knowledge of the test. Instruct the client that
during the procedure it may be uncomfortable to sit on the hard table or achieve some of the necessary positions; it is
important to remain as still as possible during the test; there are no dietary restrictions prior to the test; and it is necessary
to remove dental prosthesis, jewelry, eyeglasses, or other metal objects like hair clips before the procedure.
VII. NURSING CONSIDERATION & RESPONSIBILITES
During test: adhere to standard precautions. The client is instructed to take a deep breath and hold it or to exhale and not to
breathe as the x-ray is taken.
After test: monitor bowel sounds in clients who are experiencing pain (unrelated to the abdominal film procedure)
Pregnancy: Radiation should be avoided in pregnant women if possible (Note: appropriate lead shielding is done to protect
the fetus if it is determined this test is necessary).
Pediatric: infants and children will need assistance in remaining still during the x-ray and age-appropriate comfort measures
following the test.
Gerontology: The older person may find it difficult to maintain positions when required to do so for lengthy periods of time.
B. UPPER GASTROINTESTINAL SERIES (BARIUM SWALLOW & BARIUM MEAL)
I. DESCRIPTION
An upper GI series involves swallowing a barium mixture (or dye preparation) that shows up on x-ray. As the client swallows
this mixture, x-rays or fluoroscopic pictures are made of the upper GI tract. The form, position, peristaltic action, function, and
abnormalities can be visualized of the esophagus, duodenum, and upper portion of the jejunum. The barium passes through
the GI tract at a normal rate, and there should not be a reflux (which indicates a hiatal hernia or incompetent cardiac
sphincter) or leakage into the abdominal cavity.
II. INDICATION
Diagnoses ulcers, hiatal hernia, diverticula, gastritis, enteritis, strictures, varices, pyloric stenosis, and volvulus of the stomach.
Evaluates and monitors tumors.
Identifies esophageal reflux.
Detects foreign bodies.
III. CONTRAINDICATION
X-ray are usually avoided during pregnancy unless the benefit to the fetus outweights the potential risk; suspected ileus;
obstruction; gastrointestinal perforation. Interfering factors are retained food or fluids may interfere with visualization
during the study; it may be difficult to perform the test on a debilitated client.
IV. NORMAL VALUES/ FINDINGS
Normal esophageal, stomach, and small intestine motility; normal size and shape of the stomach and small intestine; no
ulcerations, inflammation, tumors, strictures, ruptures, foreign bodies, or hiatal hernia.
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Abnormal esophageal, stomach, and small intestine motility; Abnormal size and shape of the stomach and small intestine;
There are ulcerations, inflammation, tumors, strictures, ruptures, foreign bodies, or hiatal hernia.
VI. PATIENT PREPARATION
If you are pregnant or think you may be pregnant, you should notify your doctor. Notify the radiologist if you have had a
recent barium X-ray or cholangiography procedure, as this may interfere with obtaining an optimal X-ray exposure of the
upper GI series.
You must completely change into a patient gown. Please remove all piercings and leave all jewelry and valuables at home.
The night before the exam, do not eat or drink anything after midnight until the exam is over.
Based on the medical condition, the physician may request other specific preparation.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Before test: Explain the test procedure and the purpose of the test. Assess the client’s knowledge of the test. Instruct the
client that during the procedure it may be uncomfortable to sit on the hard table or achieve some of the necessary positions;
it is important to remain as still as possible during the test; and it is necessary to remove dental prosthesis, jewelry,
eyeglasses, or other metal objects like hair clips before the procedure. Instruct client to eat a light meal the evening before
the test and then fast for 12 hr prior to the procedure. Most medications are held after midnight before the test (particularly
those that affect GI motility). Diabetic clients should be scheduled early in the morning.
During test: Adhere to standard precautions. The barium is often found to have a chalky, unpleasant taste. The client is
instructed to take a deep breath and hold it or to exhale and not to breathe as the xray is taken.
After test: Instruct client to take a laxative or enema due to the constipation produced by the barium. Instruct the client to
rest after the procedure and explain that stools will be light colored for 24-72 hours.
Radiation should be avoided in pregnant women if possible (note: appropriate lead shielding is done to protect the fetus if
it is determined this test is necessary).
Sedation is recommended for infants and children. Place the infant or child on a blanket for comfort. After post-procedure
monitoring is completed and per health care provider’s order, the pediatric client is discharged with an adult who is given
instructions.
The older person may find it difficult to maintain positions when required to do so for lengthy periods of times during the
upper GI.
Advisable to arrange for transportation home after recovering from the upper GI
C. ENDOSCOPY
I. DESCRIPTION
Involves the direct visualization of internal structures of the body through the use of special fiber-optic instruments that
contain lights, and specialized tools such as suction, lavage, biopsy forceps, electrocautery, and even lasers. Scopes are
usually made from a flexible nylon that allows them to be introduced into a body cavity or organ.
II. INDICATION
Investigate signs and symptoms. An endoscopy may help your doctor determine what's causing digestive signs and
symptoms, such as nausea, vomiting, abdominal pain, difficulty swallowing and gastrointestinal bleeding
Diagnose. Your doctor may use an endoscopy to collect tissue samples (biopsy) to test for diseases and conditions, such as
anemia, bleeding, inflammation, diarrhea or cancers of the digestive system
Treat. Your doctor can pass special tools through the endoscope to treat problems in your digestive system, such as
widening a narrow esophagus, clipping off a polyp or removing a foreign object
III. CONTRAINDICATION
Some contraindications are fistulas, ileus, third-trimester pregnancy, bleeding disorders, acute peritonitis, and diverticulitis.
Examples of potential interfering factors are retained barium, when used as a contrast medium, and fixation of the bowel
from a previous radiation therapy or surgery.
IV. NORMAL VALUES/ FINDINGS
Procedures are performed using sterile technique, except for endoscopy of the colon. Endoscopic procedures usually take
approximately 30–60 min and do not usually require a general anesthetic
When you receive the results of your endoscopy will depend on your situation
V. SIGNIFICANT ABNORMAL VALLUE/FINDINGS
Fever
Chest pain
Shortness of breath
Bloody, black or very dark colored stool
Difficulty swallowing
Severe or persistent abdominal pain
Vomiting, especially if your vomit is bloody or looks like coffee grounds
VI. PATIENT PREPARATION
Before your upper endoscopy procedure, you'll be asked to lie down on a table on your back or on your side. Monitors may
be attached to your body to allow your health care team to keep tabs on your breathing, blood pressure and heart rate
At this time, you may receive a sedative medication. This medication, given through a vein in your forearm, helps you relax
during the endoscopy
Your doctor may also spray an anesthetic in your mouth, which will numb your throat in preparation for insertion of the
long, flexible tube (endoscope). You may be asked to wear a plastic mouth guard to hold your mouth open
VII. NURSING CONSIDERATION & RESPONSIBILITES
Often clients need to be positioned in a specific manner (e.g. Sims position)
The client should be informed that minor pain and discomfort are frequently associated with endoscopy
The client should be told what to expect and the analgesia discussed
Informed consent is usually required and should be obtained while the client is not under the effects of preoperative
sedation
Complications are rare, but include perforation, infection, bleeding, and allergic reactions to topical anesthetics, analgesics,
or contrast media
Some endoscopy procedures require NPO status to prevent aspiration
Client education regarding premedication for the procedure
Advising the client of clinical manifestations of infection (e.g. redness, warmth, swelling, pain) and to notify the health care
provider with any signs/symptoms of infection
D. ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY
I. DESCRIPTION
Endoscopic retrograde cholangiopancreatography (ERCP) allows direct visualization of the pancreatic and biliary ducts with
a flexible endoscope and, after injection of contrast material, with x-rays. It allows the physician to view the pancreatic,
hepatic, and common bile ducts and the ampulla of Vater.
II. INDICATION
Assess jaundice of unknown cause to differentiate biliary tract obstruction from liver disease
Identify obstruction caused by calculi, cysts, ducts, strictures, stenosis, and anatomic abnormalities
Retrieve calculi from the distal common bile duct and release strictures
Perform therapeutic procedures, such as sphincterotomy and placement of biliary drains
Collect specimens for cytology
III. CONTRAINDICATION
Inability of the patient to cooperate with the procedure because of age, significant pain, or mental status
Failure to follow dietary restrictions before the procedure
Previous surgery involving the stomach or duodenum, which can make locating the duodenal papilla difficult
Barium remaining in the stomach or bowel
A patient with Zenker’s diverticulum involving the esophagus, who may be unable to undergo ERCP
A patient with unstable cardiopulmonary status, blood coagulation defects, or cholangitis (test may have to be rescheduled
unless patient received antibiotic therapy before the test)
A patient with known acute pancreatitis
IV. NORMAL VALUES/ FINDINGS
Normal appearance of the duodenal papilla
Patency of the pancreatic and common bile ducts
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Duodenal papilla tumors
Pancreatic cancer
Pancreatic fibrosis
Pancreatitis
Sclerosing cholangitis
VI. PATIENT PREPARATION
Explain to the patient the purpose of the study and how the procedure is performed.
Obtain a written, informed consent for the procedure from the patient.
Obtain a history of suspected or existing disease of the pancreas, gallbladder, duct system, or other intestinal disorders. For
related tests, refer to the hepatobiliary and gastrointestinal system tables.
Determine if the patient has allergies or sensitivities to anesthetics, analgesics, antibiotics, or iodine.
Obtain results of other tests and procedures done to diagnose disorders of or to provide treatment for the pancreas,
gallbladder, biliary ducts, or intestinal system.
Explain that the procedure usually takes 30 to 60 minutes to complete and generally is performed in an endoscopy suite by
a physician and support staff. The physician interprets the results and sends the patient’s physician a written report, to be
discussed with the patient.
Inform the patient that a flushed feeling may be experienced when the contrast medium is injected.
Restrict food and fluids 8 to 12 hours before the procedure.
Note recent administration of barium because residual barium can obscure the organ to examined.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pregnancy: X-rays are usually avoided during pregnancy unless the benefit to the fetus outweighs the potential risk.
Pediatric: ERCP has been performed successfully in cholestatic neonates. A high level of technical expertise is required of
the physician performing this test on infants. Most neonates require general anesthesia during the examination. Specially
designed pediatric duodenoscopes are available, which allows for use of ERCP in infants with obstructive jaundice. Sedation
is recommended for infants and children undergoing an x-ray (abdominal). Place the infant or child on a blanket for comfort.
After postprocedure monitoring is completed and per health care provider’s order, the pediatric client is discharged with an
adult who is given instructions.
Gerontology: The older person may find it difficult to maintain positions when required to do so for lengthy periods of time
during the ERCP.
Rural: Advisable to arrange for transportation home after recovering from the ERCP.
E. PH MONITORING STUDIES
I. DESCRIPTION
Esophageal pH monitoring is a test that measures how often stomach acid enters the tube that leads from the mouth to
the stomach (called the esophagus). The test also measures how long the acid stays there.
II. INDICATION
Heartburn, primarily in patients who have failed medical treatment and are candidates for surgery
Uncommon symptoms of GERD (gastroesophageal reflux disease), such as chest pain, chronic cough, and asthma
III. CONTRAINDICATION
Patients with altered mental status or obtundation
Patients who cannot understand or follow instructions
Suspected or known pharyngeal or upper esophageal obstruction (e.g., tumors)
IV. NORMAL VALUES/ FINDINGS
Esophageal secretions: pH 5 to 6
Acid reflux: no regurgitation into the esophagus
Acid perfusion: no GER
Acid clearing: fewer than 10 swallows
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Achalasia (sphincter pressure of 50 mm Hg)
Chalasia
Esophageal scleroderma
Esophagitis
GER (sphincter pressure of 0 to 5 mmHg, pH of 1 to 3)
Hiatal hernia
Progressive systemic sclerosis (scleroderma)
Spasms
VI. PATIENT PREPARATION
Explain that the procedure is generally performed in an endoscopy suite by a physician with support staff and usually takes
30 to 60 minutes to complete.
Explain to the patient the purpose of the study and how the procedure is performed.
Obtain a written, informed consent for the procedure from the patient.
Obtain a history of upper GI distress or disorders, hiatal hernia, and related symptoms.
Obtain the results of previously performed tests, treatments, surgeries, and procedures done to diagnose or treat disorders
of the upper GI system. For related tests, refer to the gastrointestinal system table.
Determine date of last menstrual period and possibility of pregnancy in perimenopausal women.
Inform the patient that there will be some discomfort and gagging when the tube is inserted, but there are no complications
resulting from the procedure and the throat will be anesthetized with a spray or swab.
Inform the patient that dentures and eyewear will be removed before the test.
Inform the patient that he or she will not be able to speak during the procedure, but that breathing will not be affected.
Restrict food, fluids, and smoking for 8 hours before the procedure.
Ensure that medications are withheld for 24 hours before the study; special arrangements may be necessary for diabetic
patients.
Resuscitation and suctioning equipment should be readily available.
Obtain and record baseline vital signs.
VII. NURSING CONSIDERATION & RESPONSIBILITES
With the tube in place, a pH electrode probe is inserted into the esophagus with Valsalva maneuvers performed to stimulate
reflux of stomach contents into the esophagus.
If acid reflux is absent, 100 mL of 0.1% hydrochloric acid is instilled into the stomach during a 3-minute period, and then the
pH measurement is repeated.
To determine acid clearing, hydrochloric acid is instilled into the esophagus and the patient is asked to swallow while the
probe measures the pH.
A catheter is inserted through the nose into the esophagus and the patient is asked to inform the technician when pain is
experienced.
Normal saline solution is allowed to drip into the catheter at about 10 mL/min. Then hydrochloric acid is allowed to drip into
the catheter.
Pain experienced when the hydrochloric acid is instilled determines the presence of an esophageal abnormality. If no pain
is experienced, symptoms are the result of some other condition.
F. ESOPHAGEAL/GASTRIC MANOMETRY
I. DESCRIPTION
Consists of a group of invasive studies performed to assist in diagnosing abnormalities of esophageal muscle function and
esophageal structure. These studies measure esophageal pressure, the effects of gastric acid in the esophagus, lower
esophageal sphincter pressure, and motility patterns that result during swallowing. EM can be used to document and
quantify gastroesophageal reflux disease (GERD). It is indicated when a patient is experiencing difficulty swallowing,
heartburn, regurgitation, or vomiting or has chest pain for which no diagnosis has been found. Tests performed in
combination with EM include the acid reflux, acid clearing, and acid perfusion (Bernstein) tests.
II. INDICATION
Aid in the diagnosis of achalasia, evidenced by increased pressure in EM
Aid in the diagnosis of achalasia in children, evidenced by decreased pressure in EM
Aid in the diagnosis of esophageal scleroderma, evidenced by decreased motility
Aid in the diagnosis of GERD, evidenced by low pressure in EM, decreased pH in acidity test, and pain in acid reflux and
perfusion tests
Differentiate between esophagitis or cardiac condition as the cause of epigastric pain
Evaluate pyrosis and dysphagia to determine if the cause is GERD or esophagitis
III. CONTRAINDICATION
Patients with unstable cardiopulmonary status, blood coagulation defects, recent gastrointestinal surgery, esophageal
varices, or bleeding.
IV. NORMAL VALUES/ FINDINGS
Acid clearing: fewer than 10 swallows
Acid perfusion: no GERD
Acid reflux: no regurgitation into the esophagus
Bernstein test: negative
Esophageal secretions: pH 5 to 6
Esophageal sphincter pressure: 10 to 20 mmHg
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Achalasia (sphincter pressure of 50mmHg)
Chalasia
Esophageal scleroderma
Esophagitis
GER (sphincter pressure of 0 to 5 mmHg, pH of 1 to 3)
Hiatal hernia
Progressive systemic sclerosis (scleroderma)
VI. PATIENT PREPARATION
Do not eat or drink after midnight before the test.
Diabetics: Do not take your insulin or oral diabetic medications the morning of test.
The day of the procedure, you will be asked to sign an informed consent and provide information regarding any medicine
allergies.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pretest
Explain that the procedure is generally performed in an endoscopy suite by a physician with support staff and usually
takes 30 to 60 minutes to complete.
Explain to the patient the purpose of the study and how the procedure is performed.
Obtain a written, informed consent for the procedure from the patient.
Obtain a history of upper GI distress or disorders, hiatal hernia, and related symptoms.
Obtain the results of previously performed tests, treatments, surgeries, and procedures done to diagnose or treat
disorders of the upper GI system. For related tests, refer to the gastrointestinal system table.
Determine date of last menstrual period and possibility of pregnancy in perimenopausal women.
Inform the patient that there will be some discomfort and gagging when the tube is inserted, but there are no
complications resulting from the procedure and the throat will be anesthetized with a spray or swab.
Inform the patient that dentures and eyewear will be removed before the test.
Inform the patient that he or she will not be able to speak during the procedure, but that breathing will not be affected.
Restrict food, fluids, and smoking for 8 hours before the procedure.
Ensure that medications are withheld for 24 hours before the study; special arrangements may be necessary for
diabetic patients.
Resuscitation and suctioning equipment should be readily available.
Obtain and record baseline vital signs
Intratest
During the procedure, monitor the patient to prevent aspiration of stomach contents into the lungs. Note any change
in respirations (dyspnea, tachypnea, adventitious sounds).
Suction mouth, pharynx, and trachea, and administer oxygen as ordered.
Have the patient put on a hospital gown and void.
Place the patient on the examining table, and spray the throat with local anesthetic.
Wear gloves throughout the procedure
One or more small tubes are inserted through the nose into the esophagus and stomach.
A small transducer is attached to the ends of the tubes; pressures are measured at the lower esophageal sphincter,
and intraluminal pressures as well as regularity and duration or peristaltic contractions are measured.
The patient is asked to swallow small amounts of water or flavored gelatin.
Pressures are taken and recorded, and a motility pattern is recorded on a graph.
Post test
Tell the patient to expect some throat soreness and possible hoarseness. Advise the patient to use warm gargles,
lozenges, or ice packs to the neck; or to drink cool fluids to alleviate throat discomfort.
Monitor the patient for signs of respiratory depression (less than 15 respirations per minute). Resuscitation equipment
should be available.
Observe the patient for indications of perforation: painful swallowing with neck movement, substernal pain with
respiration, shoulder pain, dyspnea, abdominal or back pain, cyanosis, and fever.
Emphasize that any severe pain, fever, difficulty breathing, or expectoration of blood must be reported to the physician
immediately.
Do not allow the patient to eat or drink until the gag reflex returns then allow the patient to eat lightly for 12 to 24
hours.
Instruct the patient to resume normal activity, medication, and diet 24 hours after the examination or as tolerated,
unless otherwise indicated.
A physician specializing in this branch of medicine sends a written report to the ordering provider, who discusses the
results with the patient.
Inform the patient that an abnormal examination may indicate the need for further studies.
Evaluate test results in relation to the patient’s symptoms and any related tests performed.
Pediatrics: Infants and children will need assistance in remaining still during the procedure and age-appropriate comfort
measures following the test.
G. COLONOSCOPY
I. DESCRIPTION
Colonoscopy allows inspection of the mucosa of the entire colon, ileocecal valve, and terminal ileum using a flexible
fiberoptic colonoscope inserted through the anus and advanced to the terminal ileum. The colonoscope is a multichannel
instrument that allows viewing of the gastrointestinal (GI) tract lining, insufflation of air, aspiration of fluid, obtaining of
tissue biopsy samples, and passage of a laser beam for obliteration of tissue and control of bleeding. Mucosal surfaces of
the lower GI tract are examined for ulcerations, polyps, chronic diarrhea, hemorrhagic sites, neoplasms, and strictures.
During the procedure, tissue samples may be obtained for cytology, and some therapeutic procedures may be performed,
such as excision of small tumors or polyps, coagulation of bleeding sites, and removal of foreign bodies.
II. INDICATION
Determine cause of lower GI disorders, especially when barium enema and proctosigmoidoscopy are inconclusive
Determine source of rectal bleeding and perform hemostasis by coagulation
Remove foreign bodies and sclerosing strictures by laser
Confirm diagnosis of colon cancer and inflammatory bowel disease
Follow up on previously diagnosed and treated colon cancer
Detect Hirschsprung’s disease and determine the areas affected by the disease
Reduce volvulus and intussusception in children
Remove colon polyps
Investigate iron-deficiency anemia of unknown origin
Evaluate postsurgical status of colon resection
Evaluate stools that show a positive occult blood test, lower-GI bleeding, or change in bowel habits
Assess GI function in a patient with a personal or family history of colon cancer, polyps, or ulcerative colitis
III. CONTRAINDICATION
Patients with bleeding disorders or cardiac conditions
Patients with bowel perforation, acute peritonitis, acute colitis, ischemic bowel necrosis, toxic colitis, recent bowel surgery,
advanced pregnancy, severe cardiac or pulmonary disease, recent myocardial infarction, known or suspected pulmonary
embolus, and large abdominal aortic or iliac aneurysm
Patients who have had a colon anastomosis within the past 14 to 21 days, because an anastomosis may break down with
gas insufflation
IV. NORMAL VALUES/ FINDINGS
Normal intestinal mucosa with no abnormalities of structure, function, or mucosal surface in the colon or terminal ileum
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
Bleeding sites
Benign lesions
Bowel distention
Bowel infection or inflammation
Colon cancer
Crohn’s disease
Colitis
Diverticula
Foreign bodies
Hemorrhoids
Polyps
Proctitis
Tumors
Vascular abnormalities
VI. PATIENT PREPARATION
Follow a special diet the day before the exam. Typically, patient won't be able to eat solid food the day before the exam.
Drinks may be limited to clear liquids — plain water, tea and coffee without milk or cream, broth, and carbonated beverages.
Avoid red liquids, which can be confused with blood during the colonoscopy. Patient may not be able to eat or drink
anything after midnight the night before the exam.
Take a laxative. The doctor will usually recommend taking a laxative, in either pill form or liquid form. Patient may be
instructed to take the laxative the night before your colonoscopy, or may be asked to use the laxative both the night before
and the morning of the procedure.
Use an enema kit. In some cases, the patient may need to use an over-the-counter enema kit — either the night before the
exam or a few hours before the exam — to empty the colon. This is generally only effective in emptying the lower colon
and is usually not recommended as a primary way of emptying your colon.
Adjust your medications. Remind the doctor of your medications at least a week before the exam — especially if the patient
has diabetes, high blood pressure or heart problems or if the patient take medications or supplements that contain iron.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pretest
Explain to the patient the purpose of the study and how the procedure is performed.
Obtain a written, informed consent for the procedure from the patient.
Obtain a history of GI disorders, noting any information relating to lower bowel, anal, rectal, or coagulation disorders.
Note use of drugs that affect bleeding, such as aspirin and other salicylates.
Note intake of oral iron preparations 1 week before the procedure because these cause black, sticky feces that are
difficult to remove with bowel preparation.
Obtain the results of other tests (particularly hematologic or coagulation tests), treatments, surgeries, medication
usage, and procedures done to diagnose or treat disorders of the intestinal system. For related tests, refer to the
gastrointestinal system table.
Determine date of last menstrual period and possibility of pregnancy in perimenopausal women.
Explain that the procedure usually takes 30 to 60 minutes to complete and is generally performed in an endoscopy
suite by a physician and support staff.
Restrict the diet to clear liquids for 48 hours before beginning oral bowel preparation.
Ensure that ordered laxatives have been administered late in the afternoon of the day before the procedure.
Inform the patient that it is important that the bowel be cleaned thoroughly so that the physician can visualize the
colon and that the patient will have to receive enemas before the test.
Note recent administration of barium because it can obscure the area to be examined.
Resuscitation equipment should be readily available.
Intratest
Two hours before the procedure, administer a warm tap water or saline enema until the returns are clear or as ordered.
Have the patient put on a hospital gown and void.
An intravenous (IV) line may be started to allow infusion of a sedative or IV fluids.
Obtain baseline vital signs.
Administer ordered sedation.
The patient is placed on an examination table in the left lateral decubitus position and draped with the buttocks
exposed.
The physician performs a visual inspection of the perianal area and a digital rectal examination.
The patient is requested to bear down as if having a bowel movement as the fiberoptic tube is inserted through the
rectum.
The scope is advanced through the sigmoid. The patient’s position is changed to supine to facilitate passage into the
transverse colon. Air is insufflated through the tube during passage to aid in visualization.
The patient is instructed to take deep breaths to aid in movement of the scope downward through the ascending
colon to the cecum and into the terminal portion of the ileum.
Air is insufflated to distend the GI tract, as needed. Biopsies, cultures, or any endoscopic surgery is performed.
Foreign bodies or polyps are removed and placed in appropriate specimen containers, labeled properly, and sent to
the laboratory.
Photographs are obtained for future reference.
At the end of the procedure, excess air and secretions are aspirated through the scope, and the colonoscope is
removed.
Gloves and gowns are worn by the examiner throughout the procedure.
Monitor the patient for signs of respiratory depression. Resuscitation equipment should be available.
Post-test
Monitor for any rectal bleeding. Instruct the patient to expect slight rectal bleeding for 2 days after removal of polyps
or biopsy specimens, but that an increasing amount of bleeding or sustained bleeding should be reported to the
physician immediately.
Observe the patient until the effects of the sedation have worn off.
Observe the patient for indications of chest pain, abdominal pain or tenderness, or breathing problems. If these
symptoms are present or increase in frequency or severity, the change should be reported to a physician
immediately.
Inform the patient that belching, bloating, or flatulence is the result of air insufflation.
Emphasize that any severe pain, fever, difficulty breathing, or GI bleeding must be reported to the physician
immediately.
Resume normal activity, medication, and diet 2 hours after the procedure or as tolerated, unless otherwise indicated.
Encourage the patient to drink several glasses of water to help replace fluids lost during the preparation for the test.
A physician specializing in this branch of medicine sends a written report to the ordering provider, who discusses
the results with the patient.
Inform the patient that an abnormal examination may indicate the need for further studies.
Evaluate test results in relation to the patient’s symptoms and other tests performed. Related diagnostic tests
include barium enema and proctosigmoidoscopy.
Other considerations:
Failure to follow dietary restrictions before the procedure may cause the procedure to be canceled or repeated.
Bowel preparations that include laxatives or enemas should be avoided in pregnant patients or patients with
inflammatory bowel disease, unless specifically directed by a physician.
Pregnancy: X-rays are usually avoided during pregnancy unless the benefit to the fetus outweighs the potential risk.
Pediatric: ERCP has been performed successfully in cholestatic neonates. A high level of technical expertise is required of
the physician performing this test on infants. Most neonates require general anesthesia during the examination. Specially
designed pediatric duodenoscopes are available, which allows for use of ERCP in infants with obstructive jaundice. Sedation
is recommended for infants and children undergoing an x-ray (abdominal). Place the infant or child on a blanket for
comfort. After post-procedure monitoring is completed and per health care provider’s order, the pediatric client is
discharged with an adult who is given instructions.
Gerontology: The older person may find it difficult to maintain positions when required to do so for lengthy periods of time
during the ERCP.
Rural: Advisable to arrange for transportation home after recovering from the ERCP
H. BARIUM ENEMA
I. DESCRIPTION
This radiologic examination of the colon, distal small bowel, and occasionally the appendix follows installation of barium
using a rectal tube inserted into the rectum or an existing ostomy. The patient must retain the barium while a series of
radiographs are obtained. Visualization can be improved by using air or barium as the contrast medium (double-contrast
study). A combination of x-ray and fluoroscopy techniques is used to complete the study. This test is especially useful in the
evaluation of patients experiencing lower abdominal pain, changes in bowel habits, or the passage of stools containing
blood or mucus, and for visualizing polyps, diverticula, and tumors. A barium enema may be therapeutic; it may reduce an
obstruction caused by intussusception, or telescoping of the intestine. Barium enema should be performed before an upper
gastrointestinal study or barium swallow.
II. INDICATION
Determine the cause of rectal bleeding, blood, pus, or mucus in feces
Evaluate unexplained weight loss, anemia, or a change in bowel pattern
Identify and locate benign or malignant polyps or tumors
Evaluate suspected inflammatory process, congenital anomaly, motility disorder, or structural change
III. CONTRAINDICATION
Patients that are pregnant or suspected of being pregnant, unless the potential benefits of the procedure far outweigh the
risks to the fetus and mother.
Patients with intestinal obstruction, acute ulcerative colitis, acute diverticulitis, megacolon, or suspected rupture of the
colon.
IV. NORMAL VALUES/ FINDINGS
Normal size, filling, shape, position, and motility of the colon
Normal filling of the appendix and terminal ileum
V. SIGNIFICANT ABNORMAL VALLUE/FINDINGS
Appendicitis
Colorectal cancer
Congenital anomalies
Crohn’s disease
Diverticular disease
Fistulas
Gastroenteritis
Granulomatous colitis
Hirschsprung’s disease
Intussusception
Perforation of the colon
Polyps
Sarcoma
Sigmoid torsion
Sigmoid volvulus
Stenosis
Tumors
Ulcerative colitis
VI. PATIENT PREPARATION
Follow a special diet the day before the exam. The patient may be asked not to eat and to drink only clear liquids — such as
water, tea or coffee without milk or cream, broth, and clear carbonated beverages.
Fast after midnight. Usually, patient will be asked not to drink or eat anything after midnight before the exam.
Take a laxative the night before the exam. A laxative, in a pill or liquid form, will help empty the colon.
Use an enema kit. In some cases, patient may need to use an over-the-counter enema kit — either the night before the exam
or a few hours before the exam — that provides a cleansing solution to remove any residue in the colon.
Ask the doctor about your medications. At least a week before the exam, talk with the doctor about the medications
normally taken. He or she may ask the patient to stop taking them days or hours before the exam.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Pretest
Inform the patient about the purpose of the procedure, and the need to have contrast medium instilled into the rectum.
The procedure is not painful, but the patient may experience cramping, abdominal fullness, or an urge to defecate.
Obtain a history of the patient’s complaints and a list of any medications the patient is taking.
Obtain a history of the patient’s lower gastrointestinal system and the results of previously performed tests, surgery,
therapy, and procedures. For related tests, refer to the gastrointestinal system table.
Determine patient’s allergies, including barium and latex.
Assess for iodine allergy, including allergies to shellfish, if iodinated contrast medium is to be used.
The 30- to 60-minute procedure is done by a physician and/or technologist.
Instruct the patient to eat a lowresidue diet for several days before the procedure, to consume only clear liquids the
evening before the test, and to withhold food and fluids for 8 hours before the test.
Inform the patient that a laxative and cleansing enema may be needed the day before the procedure, with cleansing
enemas on the morning of the procedure, depending on the institution’s policy.
Determine date of last menstrual period and possibility of pregnancy in perimenopausal women.
Instruct patients with a colostomy to follow the same dietary preparation, take laxatives the evening before, and
perform colostomy irrigation before the study.
Assess for completion of bowel preparation according to the institution’s procedure.
Intratest
Remove clothing and metallic objects from the pelvic area.
Provide patient with a gown with tie closures and a robe to wear.
If appropriate, remove any wires connected to electrodes.
Place the patient on the x-ray table in a supine position or have the patient stand in front of an x-ray fluoroscopy screen.
An initial image is taken. The patient is helped to a side-lying position (Sims’ position). A rectal tube is inserted into the
anus while an attached balloon is inflated after it is situated against the anal sphincter.
Barium is instilled into the colon and then the movement is observed through the colon by fluoroscopy.
Images are taken at different angles and positions to aid in the evaluation of the patient’s problem.
For patients with a colostomy, an indwelling urinary catheter is inserted into the stoma and barium is administered.
The patient is returned to a position of comfort, and is placed on a bedpan or helped to the bathroom to expel the
barium.
After the expulsion of the barium, an additional film is taken of the intestine.
If a double-contrast barium enema has been ordered, air is then instilled in the intestine and additional films are taken.
Post-test
Instruct the patient to resume food, fluids, and medications withheld before the procedure.
Inform the patient of the possible need for further examinations to evaluate and determine the need for a change in
therapy or progression of the disease process.
If iodine is used, monitor for reaction to iodinated contrast medium including rash, urticaria, tachycardia, hyperpnea,
hypertension, or palpitations.
Instruct the patient to take a mild laxative and increase fluid intake (four glasses) to aid in elimination of barium, unless
contraindicated.
Instruct the patient that stools will be white or light in color for 2 to 3 days. If the patient is unable to eliminate the
barium, or if stools do not return to normal color, the patient should notify the physician.
Advise patients with a colostomy to administer tap water colostomy irrigation to aid in barium removal.
Carefully monitor the patient for fatigue and fluid and electrolyte imbalance.
Determine if the patient or patient’s family has any further questions or concerns.
A physician specializing in this branch of medicine will send a report to the ordering health care provider who will
discuss the results with the patient.
Evaluate test results in relation to the patient’s symptoms and other tests performed. Related diagnostic tests include
colonoscopy, as well as computed tomography and magnetic resonance imaging of the abdomen.
Pregnancy: Radiation should be avoided in pregnant women if possible (Note: appropriate lead shielding is done to protect
the fetus if it is determined this test is necessary).
Gerontology: The older person may find it difficult to maintain positions when required to do so for lengthy periods of time
during the barium enema.
I. ANORECTAL MANOMETRY
I. DESCRIPTION
A technique used to measure contractility in the anus and rectum. This technique uses a balloon in the rectum to distend
the rectum and a pressure sensor at the internal anal sphincter to measure the presence or absence of the rectosphincteric
reflex.
Useful for pre/post-surgical evaluation of anal sphincter tone, functional anorectal pain, pelvic floor dyssynergia, and
diagnosis of Hirschsprung’s Disease. Anorectal manometry measures the pressures of the anal sphincter muscles, sensation
in the rectum, and the neural reflexes that are needed for normal bowel movements.
II. INDICATION
Chronic constipation
Fecal incontinence
Differential diagnosis of the anal pain
Patients assessment before and during biofeedback training
Risk assessment of the rectoanal function disorders after rectal/anal surgeries
III. CONTRAINDICATION
Patients with known anal strictures or obstructions preventing insertion of the instrument
IV. NORMAL VALUES/ FINDINGS
Age is associated with lower (r = − 0.47, p < 0.01) anal resting [63[5] (≥50 y), 88[3] (<50 y)] but not squeeze pressures; higher
rectal pressure and rectoanal gradient during simulated evacuation (r = 0.3, p < 0.05); and a shorter (r = −0.4, p < 0.01) rectal
BET [17[9]s (≥50 y) vs 31[10]s (<50 y)]. Only 5 women had a prolonged (> 60 s) rectal BET but 52 had higher anal than rectal
pressures (ie, negative gradient) during simulated evacuation. The gradient was more negative in younger (−41[6] mm Hg)
than older (−12[6] mm Hg) women and negatively (r = −0.51, p <0.0001) correlated with rectal BET but only explained 16% of
the variation in rectal BET.
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
These observations provide normal values for anorectal pressures by HRM. Increasing age is associated with lower anal
resting pressure, a more positive rectoanal gradient during simulated evacuation, and a shorter BET in asymptomatic
women. While the rectoanal gradient is negatively correlated with rectal BET, this gradient is negative even in a majority of
asymptomatic women, undermining the utility of a negative gradient for diagnosing defecatory disorders by HRM.
VI. PATIENT PREPARATION
Ask your patient to:
Not eat or drink anything after midnight the night before the test
Give him/herself a Fleet enema two to three hours before the appointment. The patient can purchase Fleet enemas at
your local drug store or supermarket.
VII. NURSING CONSIDERATION & RESPONSIBILITES
After the procedure:
Discuss the results of the manometry test with the patient
Tell the patient he/she can continue his/her normal diet after going home
Instruct the patient to call his/her doctor if he/she starts experiencing any unusual symptoms or side effects
If the doctor finds something during the test, treatment depends on how severe the problem is and what’s causing it.
Generally, treatment options include:
Changes in diet.
Use of medications.
Muscle strengthening exercises.
Surgical repair.
J. BOTULINUM TOXIN INJECTION
I. DESCRIPTION
Botox is a drug that weakens or paralyzes muscle. In small doses, it can reduce skin wrinkles and help treat some muscle
conditions.
Botox is a protein made from botulinum toxin that the bacterium Clostridium botulinum produces. This is the same toxin
that causes botulism.
Botox is a toxin, but when people use it correctly and in small doses, it has a number of medical and cosmetic uses.
Botox injections are probably best known for reducing skin wrinkles. Botox can also help treat crossed eyes, eyelid spasms,
excessive sweating, and some bladder disorders.
II. INDICATION
Treat certain eye disorders such as crossed eyes (strabismus) and uncontrolled blinking (blepharospasm)
Treat muscle stiffness/spasms or movement disorders (such as cervical dystonia, torticollis)
Reduce the cosmetic appearance of wrinkles
Prevent headaches in people with very frequent migraines
Also used to treat overactive bladder by patients who do not respond to or who cannot tolerate the side effects of other
medications
Helps to reduce leaking of urine, feeling of needing to urinate right away, and frequent trips to the bathroom
Treat severe underarm sweating and drooling/excess saliva
III. CONTRAINDICATION
Botulism
Lou gehrig's disease
A disorder of the peripheral nerves that enable movement called peripheral motor neuropathy
Myasthenia gravis
A skeletal muscle disorder
Progressive muscle weakness with carcinoma
Condition where one object appears as two or more object
Double vision
Blurred vision
Drooping of the upper eyelid
Pneumonia due to accidental inhalation of vomit
Decreased lung function
Hoarseness
A type of speech disorder called dysarthria
Trouble breathing
Difficulty swallowing
Involuntary leakage of urine
IV. NORMAL VALUES/ FINDINGS
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
VI. PATIENT PREPARATION
Assess for mentioned contraindications and cautions (e.g. drug allergy, cardiac depression, rheumatic disorder, pregnancy
and lactation, etc.) to prevent untoward complications.
Conduct thorough physical assessment (temperature, skin color and lesion, CNS orientation, affect, reflexes, bilateral grip
strength, spasticity evaluation; bowel sounds and urine output) to obtain baseline data.
Monitor liver and renal function tests to detect potential adverse effects.
Assess area before administering botulinum toxins because area with active infection will be exacerbated by injection.
Monitor intravenous access sites of dantrolene for potential extravasation because drug is alkaline and very irritating to
tissues.
Periodically discontinue dantrolene for 2-4 days as ordered to monitor therapeutic effectiveness.
Discontinue drug at any sign of liver dysfunction to prevent adverse effects.
Provide comfort measures to help patient tolerate drug effects.
Provide safety measures (e.g. adequate lighting, raised side rails, etc.) to prevent injuries.
Educate client on drug therapy to promote understanding and compliance.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Monitor patient response to therapy (improvement in spasticity, movement and activities).
Monitor for adverse effects (e.g. CNS changes, diarrhea, liver toxicity, etc).
Evaluate patient understanding on drug therapy by asking patient to name the drug, its indication, and adverse effects to
watch for.
Monitor patient compliance to drug therapy.
K. LIVER BIOPSY
I. DESCRIPTION
The excision of a tissue sample from the liver for microscopic analysis to determine cell morphology and the presence of
tissue abnormalities. This test is used to assist in confirming a diagnosis of cancer or certain disorders of the hepatic
parenchyma. Biopsy specimen is usually obtained either percutaneously or after surgical incision
II. INDICATION
Assist in confirming suspected hepatic malignancy
Assist in confirming suspected hepatic parenchymal disease
Assist in diagnosing the cause of persistently elevated liver enzymes, hepatomegaly, or jaundice
III. CONTRAINDICATION
Patients with:
Bleeding disorders
Suspected vascular tumor of the liver
Ascites that may obscure proper insertion site for needle biopsy
Subdiaphragmatic or right hemothoracic infection
Biliary tract infection.
IV. NORMAL VALUES/ FINDINGS
Positive findings in:
Cancer
Cholesterol ester storage disease
Cirrhosis
Galactosemia
Hemochromatosis
Hepatic involvement with systemic lupus erythematosus, sarcoidosis, or amyloidosis
Hepatitis
Parasitic infestations (e.g., amebiasis, malaria, visceral larva migrans)
Reye’s syndrome
Wilson’s disease
V. SIGNIFICANT ABNORMAL VALUE/FINDINGS
N/A
VI. PATIENT PREPARATION
Obtain a history of the patient’s complaints especially fatigue and pain related to inflammation and swelling of the liver.
Obtain a list of known allergens.
Obtain a history of the patient’s hepatobiliary and immune system, any bleeding disorders, and results of previously
performed tests and procedures, especially bleeding time, clotting time, complete blood count, partial thromboplastin time,
platelets, and prothrombin time. For related tests, refer to the hepatobiliary and immune system tables.
Obtain a list of the medications the patient is taking, including anticoagulant therapy, acetylsalicylic acid, herbs, and
nutraceuticals known to affect coagulation. These products should be discontinued 14 days before dental or surgical
procedures. The requesting health care practitioner and laboratory should be advised if the patient regularly uses these
products so their effects can be taken into consideration when reviewing results.
There are no medication restrictions unless by medical direction.
Explain that food and fluids are restricted beginning midnight of the day before the test.
Review the procedure with the patient. Sensitivity to cultural and social issues, as well as concern for modesty, is important
in providing psychological support.
Address concerns about pain related to the procedure. Explain that a sedative and/or anesthetic will be administered before
the procedure to promote relaxation during the percutaneous biopsy, and that general anesthesia will be administered for
open biopsy.
Assess if the patient has an allergy to local anesthetics, and inform the health care practitioner accordingly.
Ensure that non-allergy to anesthesia is confirmed before the open biopsy procedure is performed under general
anesthesia.
Obtain written and informed consent before administering any medications prior to the procedure.
Inform the patient that the procedure is performed by a surgeon under sterile conditions and usually takes about 90
minutes to complete. Needle biopsy should take about 15 minutes.
VII. NURSING CONSIDERATION & RESPONSIBILITES
Instruct the patient to resume usual diet as directed by the health care practitioner.
After open biopsy, monitor vital signs every 15 minutes for 1 hour, then every 2 hours for 4 hours, and as ordered. Take
temperature every 4 hours for 24 hours.
After local anesthesia, monitor vital signs and compare with baseline values.
After percutaneous biopsy, instruct the patient to stay in bed lying on the affected side for at least 2 hours with a pillow or
rolled towel under the site to prevent bleeding. The patient will also need to remain on bed rest for 24 hours.
Instruct the patient in the care and assessment of the site, observe for bleeding, hematoma formation, bile leakage, and
inflammation. Note any pleuritic pain, persistent right shoulder pain, or abdominal pain.
Recognize anxiety related to test results and offer support. Provide teaching and information regarding the clinical
implications of the test results, as appropriate. Educate the patient regarding access to counseling services.
Evaluate test results in relation to the patient’s symptoms and other tests performed. Related laboratory tests include
alanine aminotransferase, albumin, alkaline phosphatase, 1- antitrypsin/phenotyping, ammonia, amylase, antimitochondrial
antibody, anti–smooth muscle antibody, aspartate aminotransferase, bilirubin, bilirubin fractions, cholesterol, coagulation
factor assays, complete blood count, copper, y-glutamyl transpeptidase, infectious mononucleosis screen, lipase,
prothrombin time, and urinalysis.
REFERENCES:
Daniels, Rick. (2003), Delmar's Manual of Laboratory and Diagnostic Tests, 2nd Edition.
Dunning, Marshall. B., & Fischbach, Frances. (2014). A Manual of Laboratory and Diagnostic Tests, 9th Edition.
Williamson, Mary A., & Snyder, L. Michael. (2015). Wallach's Interpretation of Diagnostic Tests, 10th Edition.
https://www.webmd.com/a-to-z-guides/what-is-a-stool-culture#2
https://www.mayoclinic.org/tests-procedures/colonoscopy/about/pac-
20393569#:~:text=Follow%20a%20special%20diet%20the,with%20blood%20during%20the%20colonoscopy.
https://www.mayoclinic.org/tests-procedures/barium-enema/about/pac-20393008
Schnell Z. B., Leeuwen A., Kranpitz T. (2003); Davis’s Comprehensive handbook of Laboratory and Diagnostic Test with Nursing Implication
https://www.mayoclinic.org/tests-procedures/endoscopy/about/pac-
20395197#:~:text=Endoscopy,your%20small%20intestine%20(duodenum).
https://www.medicalnewstoday.com/articles/153737#recovery
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/upper-gastrointestinal-series
https://geekymedics.com/abdominal-x-ray-interpretation/
https://www.encyclopedia.com/medicine/encyclopedias-almanacs-transcripts-and-maps/amylase-and-lipase-tests
https://www.healthline.com/health/amylase-and-lipase-tests#understanding-your-results
https://www.healthlinkbc.ca/medical-
tests/hw1531#:~:text=Helicobacter%20pylori%20tests%20are%20used%20to%20detect%20a%20Helicobacter%20pylori,available%20w
ithin%20a%20few%20hours.
https://www.uptodate.com/contents/indications-and-diagnostic-tests-for-helicobacter-pylori-
infection#:~:text=Indications%20for%20testing%20include%3A&text=Low%20grade%20gastric%20mucosa%20associated%20lymphoi
d%20tissue%20(MALT)%20lymphoma.&text=Active%20peptic%20ulcer%20disease%20or,infection%20has%20not%20been%20docume
nted.
https://www.ebmconsult.com/articles/lab-test-helicobacter-pylori-antibody-h-pylori-antibody-level
https://www.mayoclinic.org/tests-procedures/liver-function-tests/about/pac-20394595
https://nursing.unboundmedicine.com/nursingcentral/view/Davis-Lab-and-Diagnostic-Tests/425050/all/Alanine_Aminotransferase
https://medlineplus.gov/ency/article/003558.htm
https://medlineplus.gov/lab-tests/alpha-fetoprotein-afp-tumor-marker-test/
You might also like
- Speaking Notes - OetDocument76 pagesSpeaking Notes - OetExam Materials94% (81)
- Tonsillitis: Case Presentation Related To Clients With Upper Respiratory ProblemsDocument54 pagesTonsillitis: Case Presentation Related To Clients With Upper Respiratory ProblemskdfhjfhfNo ratings yet
- Your Complete Guide To Liver He - Paul J. ThuluvathDocument216 pagesYour Complete Guide To Liver He - Paul J. ThuluvathSam Simons100% (1)
- NP3. Nursing Board Exam November 2008 Answer KeyDocument12 pagesNP3. Nursing Board Exam November 2008 Answer KeyAlyssa Mier Dacua Patalinjug100% (1)
- Philippine Handbook On Adult Immunization 2012 PDFDocument140 pagesPhilippine Handbook On Adult Immunization 2012 PDFLinius CruzNo ratings yet
- Nursingcrib Com NURSING CARE PLAN Hepatitis ADocument2 pagesNursingcrib Com NURSING CARE PLAN Hepatitis APravesh Verma100% (1)
- Viral HepatitisDocument20 pagesViral HepatitisShivam SoniNo ratings yet
- UntitledDocument43 pagesUntitledJovania B.No ratings yet
- ACG Abnormal Liver Chemistries Guideline SummaryDocument16 pagesACG Abnormal Liver Chemistries Guideline SummaryDanuNo ratings yet
- ACG Abnormal Liver Chemistries Guideline 2017Document18 pagesACG Abnormal Liver Chemistries Guideline 2017honeyworksNo ratings yet
- Diagnosis of HepatitisDocument19 pagesDiagnosis of HepatitisHrishikesh BangaleNo ratings yet
- Gallbladder-Liver and Pancreatic DisordersDocument7 pagesGallbladder-Liver and Pancreatic DisordersHasan A AsFourNo ratings yet
- Discharge PlanDocument12 pagesDischarge PlanPamela Shiermaine FilomenoNo ratings yet
- 13-11-2023Document40 pages13-11-2023vineeta.ashoknagarNo ratings yet
- GI 2007 Exam QuestionsDocument47 pagesGI 2007 Exam QuestionsRoh JitenNo ratings yet
- Diagnostic TestsDocument11 pagesDiagnostic TestsMae GabrielNo ratings yet
- Interpret Liver TestsDocument4 pagesInterpret Liver TestsKaram Ali ShahNo ratings yet
- Case Study 3Document2 pagesCase Study 3api-305352286No ratings yet
- New PPT For HepatitisDocument88 pagesNew PPT For HepatitisPriya100% (2)
- Project Nutrition Jasmin-2Document17 pagesProject Nutrition Jasmin-2JAs MineNo ratings yet
- Viral HepatitisDocument6 pagesViral HepatitisangelarainNo ratings yet
- Testing PositiveDocument3 pagesTesting PositiveAhmed GaberNo ratings yet
- Hepatitis BDocument48 pagesHepatitis BHari Suthan TNo ratings yet
- GI 2007 Exam QuestionsDocument47 pagesGI 2007 Exam QuestionsShadows BlameNo ratings yet
- IBD-Rough Road - Case Study in IBD From Presentation To ManagementDocument4 pagesIBD-Rough Road - Case Study in IBD From Presentation To ManagementBejan CorinaNo ratings yet
- Patogenesis Dan Manifestasi Klinik HepatitisDocument91 pagesPatogenesis Dan Manifestasi Klinik HepatitisFaulina Yosia PanjaitanNo ratings yet
- Evidence-Based Management of Common Gallstone-Related EmergenciesDocument11 pagesEvidence-Based Management of Common Gallstone-Related EmergenciesEva Puspita VaniNo ratings yet
- Case StudyDocument8 pagesCase StudyJan Clarisse RamosNo ratings yet
- PreeclampsiaDocument179 pagesPreeclampsiaJohn Wilbert Birung100% (3)
- Abnormal LTs 2014Document63 pagesAbnormal LTs 2014Robert G. Gish, MDNo ratings yet
- Guide For Pre-Clinical Practice Research and PlanningDocument5 pagesGuide For Pre-Clinical Practice Research and PlanningAnonymous ZSqTiYX7nNo ratings yet
- MT 6322 - Mycology and Virology 2nd Shifting OLADocument9 pagesMT 6322 - Mycology and Virology 2nd Shifting OLAlily bluesNo ratings yet
- Liver and Its Clinical SignificanceDocument59 pagesLiver and Its Clinical SignificanceazizNo ratings yet
- Diagnostic Tests A. Endoscopy: Nursing ConsiderationsDocument3 pagesDiagnostic Tests A. Endoscopy: Nursing ConsiderationsMae GabrielNo ratings yet
- Table 44-8 Nursing Assessment: Hepatitis Subjective Data Important Health InformationDocument7 pagesTable 44-8 Nursing Assessment: Hepatitis Subjective Data Important Health InformationAnggela kian puspaNo ratings yet
- Ziad Aro, MD Internal MedicineDocument100 pagesZiad Aro, MD Internal MedicineAli Aborges Jr.No ratings yet
- Week 8 Hepato Biliary 2Document94 pagesWeek 8 Hepato Biliary 2طفوف محمد.No ratings yet
- Viral Hepatitis and Alcoholic Liver Disease: Prepared By: Azhi Omer - F190219 Supervised By: Dr. Truska FaraidunDocument29 pagesViral Hepatitis and Alcoholic Liver Disease: Prepared By: Azhi Omer - F190219 Supervised By: Dr. Truska FaraidunMustafa Salam M.NooriNo ratings yet
- Acute Hepatitis: Dr.G.Indhumathi MD.Document39 pagesAcute Hepatitis: Dr.G.Indhumathi MD.Parthiban AnnaduraiNo ratings yet
- Bachelor of Science in Nursing: Ncmb316 Rle: RLE RLE Unit WeekDocument4 pagesBachelor of Science in Nursing: Ncmb316 Rle: RLE RLE Unit WeekMaica LectanaNo ratings yet
- Test #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyDocument47 pagesTest #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyJahangir AlamNo ratings yet
- Hepatitis ADocument15 pagesHepatitis Azakariah kamal0% (1)
- Liver TransplantationDocument6 pagesLiver TransplantationPriya0% (1)
- Diarrea Crónica Mar95Document5 pagesDiarrea Crónica Mar95apadronNo ratings yet
- GI (PBL3) - Mohamad Arbian Karim - FMUI20Document7 pagesGI (PBL3) - Mohamad Arbian Karim - FMUI20Mohamad Arbian KarimNo ratings yet
- Final Laboratory ProceduresDocument14 pagesFinal Laboratory ProceduresJosh BlasNo ratings yet
- Hepatitis, Viral: Type A (HAV) Type B (HBV) Type C (HCV)Document17 pagesHepatitis, Viral: Type A (HAV) Type B (HBV) Type C (HCV)herlindaNo ratings yet
- GlomerulonephritisDocument4 pagesGlomerulonephritisKim GarciaNo ratings yet
- Pi Is 1542356511012778Document6 pagesPi Is 1542356511012778Muhammad Rehan AnisNo ratings yet
- DyspepsiaDocument26 pagesDyspepsiaYaasin R NNo ratings yet
- Hepatic Encephalo & Viral Hep: Pathy AtitisDocument28 pagesHepatic Encephalo & Viral Hep: Pathy AtitisAdrian ArenasNo ratings yet
- 1B-Antenatal Care Case Protocol-1Document3 pages1B-Antenatal Care Case Protocol-1Mario EspinoNo ratings yet
- Note For H.Pylori Antigen TestDocument12 pagesNote For H.Pylori Antigen TestKrishna ShresthaNo ratings yet
- What Is Hepatitis A?: NCM 104 - CHN (Rle) 1Document3 pagesWhat Is Hepatitis A?: NCM 104 - CHN (Rle) 1Sue CañizaresNo ratings yet
- Evaluation Chronic DiarrheaDocument34 pagesEvaluation Chronic DiarrheaarthoclaseNo ratings yet
- 44 Year Old Man With Fatigue, Weight Loss, and LeuDocument5 pages44 Year Old Man With Fatigue, Weight Loss, and LeuRamiro Arraya MierNo ratings yet
- Hepatic, Pancreatic, and Rare Gastrointestinal Complications of Immune Checkpoint Inhibitor Therapy - UpToDateDocument29 pagesHepatic, Pancreatic, and Rare Gastrointestinal Complications of Immune Checkpoint Inhibitor Therapy - UpToDatemayteveronica1000No ratings yet
- Hepatitis A Virus - HAV: DiagnosisDocument6 pagesHepatitis A Virus - HAV: DiagnosisnurmaliarizkyNo ratings yet
- NURS 321/527 Unit 4 Review Digestion: GERD, Malabsorption, Pancreatitis, HepatitisDocument19 pagesNURS 321/527 Unit 4 Review Digestion: GERD, Malabsorption, Pancreatitis, HepatitisSamip PatelNo ratings yet
- Approach To Viral Hepatitis andDocument38 pagesApproach To Viral Hepatitis andVijay ShankarNo ratings yet
- Hepatology: Gatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2013Document50 pagesHepatology: Gatot Sugiharto, MD, Internist Faculty of Medicine, UWKS Lecture - 2013niluhayusumbawatiNo ratings yet
- Module14 Content Nursing Care Management of AdultDocument21 pagesModule14 Content Nursing Care Management of AdultFranceska AntonioNo ratings yet
- American Family Physician - April 15, 2020 - Chronic Diarrhea in Adults - Evaluation and Differential DiagnosisDocument16 pagesAmerican Family Physician - April 15, 2020 - Chronic Diarrhea in Adults - Evaluation and Differential DiagnosismariaNo ratings yet
- Fecal Calprotectin in IBDDocument34 pagesFecal Calprotectin in IBDNathania Nadia BudimanNo ratings yet
- Name: Celajes, Ma. Lourdes Ann D. Group: D: Rarely (1) Sometimes (2) Usually (3) Almost AlwaysDocument3 pagesName: Celajes, Ma. Lourdes Ann D. Group: D: Rarely (1) Sometimes (2) Usually (3) Almost AlwayskdfhjfhfNo ratings yet
- Laboratory Findings and Diagnostic Results 03Document7 pagesLaboratory Findings and Diagnostic Results 03kdfhjfhfNo ratings yet
- Diagnostic Test Normal Findins Description Purpose Indication Procedure Nursing Implications Magnetic Resonance ImagingDocument5 pagesDiagnostic Test Normal Findins Description Purpose Indication Procedure Nursing Implications Magnetic Resonance ImagingkdfhjfhfNo ratings yet
- RRL LocalinternationalDocument11 pagesRRL LocalinternationalkdfhjfhfNo ratings yet
- Ella Sots and Research LocaleDocument2 pagesElla Sots and Research LocalekdfhjfhfNo ratings yet
- Laboratory Findings and Diagnostic Results 03Document4 pagesLaboratory Findings and Diagnostic Results 03kdfhjfhfNo ratings yet
- Synchronous Class Schedule For: Time 1 and 3 Week of The Month 2 and 4 Week of The Month Wednesday Friday Wednesday FridayDocument1 pageSynchronous Class Schedule For: Time 1 and 3 Week of The Month 2 and 4 Week of The Month Wednesday Friday Wednesday FridaykdfhjfhfNo ratings yet
- Name Name Name: AnswerDocument2 pagesName Name Name: AnswerkdfhjfhfNo ratings yet
- The Type of Cancer SuspectedDocument20 pagesThe Type of Cancer SuspectedkdfhjfhfNo ratings yet
- Normal Findings and MeaningDocument11 pagesNormal Findings and MeaningkdfhjfhfNo ratings yet
- Laboratory Test Normal Findings Description Purpose Indications Procedure Nursing Implications 1. Adrenocorticotropi C Hormone (Plasma) Pre-TestDocument11 pagesLaboratory Test Normal Findings Description Purpose Indications Procedure Nursing Implications 1. Adrenocorticotropi C Hormone (Plasma) Pre-TestkdfhjfhfNo ratings yet
- Tumor Marker Test A. Prostate Specific Antigen (Psa) TestDocument25 pagesTumor Marker Test A. Prostate Specific Antigen (Psa) TestkdfhjfhfNo ratings yet
- Laboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisordersDocument153 pagesLaboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisorderskdfhjfhfNo ratings yet
- Laboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisordersDocument145 pagesLaboratory/Diagnostic Exams: WORKSHEET ON Endocrine System DisorderskdfhjfhfNo ratings yet
- Nursing Care For A Family Caring For Children With Infectious DiseaseDocument4 pagesNursing Care For A Family Caring For Children With Infectious DiseasekdfhjfhfNo ratings yet
- Case Scenario 5 NCPDocument10 pagesCase Scenario 5 NCPkdfhjfhfNo ratings yet
- Cesar, Katyana Antoine - Vision & Hearing LecDocument17 pagesCesar, Katyana Antoine - Vision & Hearing LeckdfhjfhfNo ratings yet
- Cesar - Evaluation - ImciDocument3 pagesCesar - Evaluation - ImcikdfhjfhfNo ratings yet
- 4 Collab Ws VH KasDocument2 pages4 Collab Ws VH KaskdfhjfhfNo ratings yet
- NCM - 109 RLE Worksheet No. 4 Common Diagnostics - Laboratory and Nursing Procedures Related To Renal and Reproductive DisordersDocument10 pagesNCM - 109 RLE Worksheet No. 4 Common Diagnostics - Laboratory and Nursing Procedures Related To Renal and Reproductive DisorderskdfhjfhfNo ratings yet
- Cesar - Cardio & HemaDocument77 pagesCesar - Cardio & HemakdfhjfhfNo ratings yet
- Name of Structure Functio N Name of Structure Function Name of Structure Functio NDocument2 pagesName of Structure Functio N Name of Structure Function Name of Structure Functio NkdfhjfhfNo ratings yet
- Anatomy & Physiology of The EyesDocument4 pagesAnatomy & Physiology of The EyeskdfhjfhfNo ratings yet
- Example of An Interview EssayDocument7 pagesExample of An Interview Essayafhbebseg100% (2)
- Prevention of Hepatitis A To E - 014825Document15 pagesPrevention of Hepatitis A To E - 014825saadkhalid8No ratings yet
- Grid AbcdeDocument1 pageGrid AbcdeStephanieDardaNo ratings yet
- Presented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHDocument55 pagesPresented By:-Himanshu Dev DMLT VI TH Sem. VMMC & SJHKailash Nagar100% (1)
- 3.0HEPATIT Lecture 5Document48 pages3.0HEPATIT Lecture 5Jiya MuhammadNo ratings yet
- Hepatitis PresentationDocument33 pagesHepatitis Presentationapi-286686446No ratings yet
- Hepatitis A Fact SheetDocument2 pagesHepatitis A Fact SheetKUER NewsNo ratings yet
- Foodborne PathogensDocument42 pagesFoodborne Pathogensabdiredha100% (1)
- Liver & Biliary DiseaseDocument41 pagesLiver & Biliary Diseasesaump3No ratings yet
- COVID-19 Vaccination PlanDocument52 pagesCOVID-19 Vaccination PlanFOX 17 NewsNo ratings yet
- Hepatitis A Treatment in Pune - Kaizen Gastro CareDocument4 pagesHepatitis A Treatment in Pune - Kaizen Gastro CareKaizen Gastro CareNo ratings yet
- June 26, 2015 Strathmore TimesDocument40 pagesJune 26, 2015 Strathmore TimesStrathmore TimesNo ratings yet
- Fen Otrimoxazole AlloDocument2 pagesFen Otrimoxazole AlloKristine AguilarNo ratings yet
- 9510 Enteric VirusesDocument18 pages9510 Enteric VirusesPenelope MeloNo ratings yet
- Viral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Document44 pagesViral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2017Eleni HagosNo ratings yet
- Case Presentation: Hepatitis ADocument57 pagesCase Presentation: Hepatitis Azahrara90No ratings yet
- Immunization - Dr. SarahDocument14 pagesImmunization - Dr. Sarahf6bk6xnppyNo ratings yet
- PhysAssessAbdomen 1Document21 pagesPhysAssessAbdomen 1David DvoskineNo ratings yet
- NCM 112 - HepatitisDocument8 pagesNCM 112 - HepatitisMara Jon Ocden CasibenNo ratings yet
- Viral Hepatitis TableDocument2 pagesViral Hepatitis TableJohnNo ratings yet
- Viral HepatitisDocument12 pagesViral HepatitisHeart Of Ayurveda Beatrice DNo ratings yet
- Hep ADocument13 pagesHep ARakesh SharmaNo ratings yet
- Obstructive JaundiceDocument54 pagesObstructive JaundiceJenine Ezra M. Conol50% (2)
- CHN ExamDocument16 pagesCHN ExamGlenn Daryll SantosNo ratings yet
- Liver FunctionDocument90 pagesLiver Functionapi-19641337100% (1)