Professional Documents
Culture Documents
Clinical Use of Clopidogrel in Acute Coronary Syndrome: Reviewarticle
Clinical Use of Clopidogrel in Acute Coronary Syndrome: Reviewarticle
Uploaded by
magreaCopyright:
Available Formats
You might also like
- الخلاصه في 23 ورقهDocument23 pagesالخلاصه في 23 ورقهصلاح البازليNo ratings yet
- Stop Anticoagulation Neuraxial AnesthesiaDocument3 pagesStop Anticoagulation Neuraxial AnesthesiaGihan NakhlehNo ratings yet
- De Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IDocument43 pagesDe Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IAkhmad HidayatNo ratings yet
- Jamacardiology Rhee 2023 Oi 230014 1681134690.05816 PDFDocument10 pagesJamacardiology Rhee 2023 Oi 230014 1681134690.05816 PDFFernando DominguezNo ratings yet
- Antiplatelt Before During and Post PCIDocument8 pagesAntiplatelt Before During and Post PCIVivekanandGuptaNo ratings yet
- 2023 Kardio Aspirin Vs Clopidogrel For Long Term Maintenance AfterDocument10 pages2023 Kardio Aspirin Vs Clopidogrel For Long Term Maintenance AfterAuliya AndiNo ratings yet
- ClairDocument9 pagesClairMuhammad Imran MirzaNo ratings yet
- 1 s2.0 S0735109719300956 MainDocument9 pages1 s2.0 S0735109719300956 MainAlberto PolimeniNo ratings yet
- Propofol Vs MidazolamDocument8 pagesPropofol Vs MidazolamSergio NNo ratings yet
- Circulationaha.119.039253.PDF J 3Document3 pagesCirculationaha.119.039253.PDF J 3Yuni IndrianiNo ratings yet
- Yi Li Extended Clopidogrel Monotherapy Vs Dapt inDocument9 pagesYi Li Extended Clopidogrel Monotherapy Vs Dapt inCelebfan BoyNo ratings yet
- Tenecteplase For The Treatment of Acute Ischemic Stroke: A Review of Completed and Ongoing Randomized Controlled TrialsDocument8 pagesTenecteplase For The Treatment of Acute Ischemic Stroke: A Review of Completed and Ongoing Randomized Controlled TrialsyoggihermawanNo ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- Pharmacology Before, During and After Percutaneous Coronary InterventionDocument8 pagesPharmacology Before, During and After Percutaneous Coronary InterventionSharan SahotaNo ratings yet
- Pharmacology Before, During and After Percutaneous Coronary InterventioDocument8 pagesPharmacology Before, During and After Percutaneous Coronary InterventiosamuelNo ratings yet
- Tsoumani 2011Document5 pagesTsoumani 2011le.m4rtinezoNo ratings yet
- Acknowledgments: Competency in Medical KnowledgeDocument1 pageAcknowledgments: Competency in Medical KnowledgeTaniaNo ratings yet
- Endovascular Therapy For Ischemic Stroke With Perfusion-Imaging SelectionDocument10 pagesEndovascular Therapy For Ischemic Stroke With Perfusion-Imaging Selectioncitra dewiNo ratings yet
- Antiplatelets in acsDocument11 pagesAntiplatelets in acsrashm4455No ratings yet
- Ticagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Document4 pagesTicagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Atul DwivediNo ratings yet
- Cortez-Neuroradiology 2020Document10 pagesCortez-Neuroradiology 2020Pedro VillamorNo ratings yet
- AOMS_Art_27239-10Document7 pagesAOMS_Art_27239-10re septian IlhamsyahNo ratings yet
- CURE TrialDocument9 pagesCURE TrialCristina PazmiñoNo ratings yet
- Egred 2016Document1 pageEgred 2016he xuNo ratings yet
- Clinician CornerDocument10 pagesClinician CornerTeten SyahirahNo ratings yet
- Fassbender 2020Document10 pagesFassbender 2020widyadariNo ratings yet
- Hyperlipidemia in Stroke Pathobiology and Therapy: Insights and PerspectivesDocument6 pagesHyperlipidemia in Stroke Pathobiology and Therapy: Insights and Perspectivesputri aprilliaNo ratings yet
- Translation of Experimental Cardioprotective Capability of P2Y12 Inhibitors Into Clinical Outcome in Patients With ST-elevation Myocardial InfarctionDocument15 pagesTranslation of Experimental Cardioprotective Capability of P2Y12 Inhibitors Into Clinical Outcome in Patients With ST-elevation Myocardial InfarctionSol SolNo ratings yet
- Pan 2017Document1 pagePan 2017Arhip CojocNo ratings yet
- Lee 2015 Yonsei Med JDocument8 pagesLee 2015 Yonsei Med JCamilaNo ratings yet
- Variability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseDocument6 pagesVariability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseGono GenieNo ratings yet
- Eficacia Del Clopidogrel en Pacientes Con Fibrilacion Auricular y Sindrome Coronario AgudoDocument7 pagesEficacia Del Clopidogrel en Pacientes Con Fibrilacion Auricular y Sindrome Coronario AgudoElva MonserrathNo ratings yet
- Predictors of Functional Improvement in The Short Term After MitraClip Implantation in Patients With Secondary Mitral RegurgitationDocument16 pagesPredictors of Functional Improvement in The Short Term After MitraClip Implantation in Patients With Secondary Mitral Regurgitationjuajimenez55No ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- 215 FullDocument12 pages215 FullGusti AnisaNo ratings yet
- IndianJPharmacol484355-1876774 051247Document5 pagesIndianJPharmacol484355-1876774 051247Santhoshi Sadhanaa SankarNo ratings yet
- Diagnostics: Cardiac Resynchronization Therapy in Non-Ischemic Cardiomyopathy: Role of Multimodality ImagingDocument15 pagesDiagnostics: Cardiac Resynchronization Therapy in Non-Ischemic Cardiomyopathy: Role of Multimodality Imagingmarsim92No ratings yet
- Auricchio & Cols. (1999)Document6 pagesAuricchio & Cols. (1999)Luba D'AndreaNo ratings yet
- DACAMI TrialDocument6 pagesDACAMI TrialAlberto CardenasNo ratings yet
- Antiplaq y HsaDocument5 pagesAntiplaq y HsaWaldemar PiñaNo ratings yet
- AbstractsDocument2 pagesAbstractsAnisaNo ratings yet
- 1 s2.0 S1936879819304960 MainDocument16 pages1 s2.0 S1936879819304960 MainAlberto PolimeniNo ratings yet
- Ischemic 19Document8 pagesIschemic 19Adina Alexandra CNo ratings yet
- Sigaliptin 2Document8 pagesSigaliptin 2trinda ireneNo ratings yet
- Platelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionDocument9 pagesPlatelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionJanuar RezkyNo ratings yet
- Tpa SilverJubilee 2021 ReviewDocument13 pagesTpa SilverJubilee 2021 ReviewMuhammad Imran MirzaNo ratings yet
- Jaha 117 007288Document4 pagesJaha 117 007288Alberto PolimeniNo ratings yet
- Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!Document6 pagesHeart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!ayesha FalakNo ratings yet
- Cardiology Update 2018 The First QuarterDocument6 pagesCardiology Update 2018 The First QuarterAditya SutarNo ratings yet
- Ictromi 2017 NaomiDocument5 pagesIctromi 2017 NaomiNaomiNDalimuntheNo ratings yet
- Emanuel 2017Document4 pagesEmanuel 2017Kimberly Ann SumbillaNo ratings yet
- Critical Appraisal Meta AnalysisDocument2 pagesCritical Appraisal Meta Analysisk110235015No ratings yet
- High Dose Versus Low Dose Intravenous Nitroglycerine For Sympathetic Crashing Acute Pulmonary EdemaDocument36 pagesHigh Dose Versus Low Dose Intravenous Nitroglycerine For Sympathetic Crashing Acute Pulmonary EdemaNaiara PfbNo ratings yet
- TilemahDocument7 pagesTilemahAndreea TudurachiNo ratings yet
- Dilated CardiomyopathyDocument11 pagesDilated CardiomyopathyPaulaNo ratings yet
- FCVM 09 788503Document7 pagesFCVM 09 788503angiebarNo ratings yet
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Document11 pagesEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazNo ratings yet
- Editorial 2Document4 pagesEditorial 2david1086No ratings yet
- Antithrombotic and Thrombolytic Therapy For Ischemic StrokeDocument21 pagesAntithrombotic and Thrombolytic Therapy For Ischemic StrokeHabibie TifanNo ratings yet
- Cardiac Troponins For The Diagnosis of Acute Myocardial Infarction in Chronic Kidney Disease PDFDocument24 pagesCardiac Troponins For The Diagnosis of Acute Myocardial Infarction in Chronic Kidney Disease PDFDaniel Hernando Rodriguez PeraltaNo ratings yet
- Erp 18 0068Document17 pagesErp 18 0068Jose Ignacio Tarton SisimitNo ratings yet
- Arrhythmia Induction in the EP LabFrom EverandArrhythmia Induction in the EP LabGabriel CismaruNo ratings yet
- University of DundeeDocument10 pagesUniversity of DundeemagreaNo ratings yet
- Baron R, 2008, E Cacy and Safety of Pregabalin in Patients With Diabetic Peripheral Neuropathy or Postherpetic NeuralgiaDocument9 pagesBaron R, 2008, E Cacy and Safety of Pregabalin in Patients With Diabetic Peripheral Neuropathy or Postherpetic NeuralgiamagreaNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument7 pagesRevista Brasileira DE AnestesiologiamagreaNo ratings yet
- Al-Maharbi S, Prevalence of Depression and Its Association With Sociodemographic Factors in Patients With Chronic PainDocument7 pagesAl-Maharbi S, Prevalence of Depression and Its Association With Sociodemographic Factors in Patients With Chronic PainmagreaNo ratings yet
- Bouhassira D, 2008, Prevalence of Chronic Pain With Neuropathic Characteristics in The General PopulationDocument8 pagesBouhassira D, 2008, Prevalence of Chronic Pain With Neuropathic Characteristics in The General PopulationmagreaNo ratings yet
- Comparison of The Neuroprotective Effects and Recovery Profiles of Isoflurane, Sevoflurane and Desflurane As Neurosurgical Pre-ConditioningDocument9 pagesComparison of The Neuroprotective Effects and Recovery Profiles of Isoflurane, Sevoflurane and Desflurane As Neurosurgical Pre-ConditioningmagreaNo ratings yet
- General Anesthesia: Key InformationDocument20 pagesGeneral Anesthesia: Key InformationmagreaNo ratings yet
- The Vertis CV TrialDocument96 pagesThe Vertis CV TrialmagreaNo ratings yet
- Diabetes and Cardiovascular Disease: Inter-Relation of Risk Factors and TreatmentDocument19 pagesDiabetes and Cardiovascular Disease: Inter-Relation of Risk Factors and TreatmentmagreaNo ratings yet
- Interpretation of Cardiovascular Outcome TrialsDocument9 pagesInterpretation of Cardiovascular Outcome TrialsmagreaNo ratings yet
- Cardiovascular Outcome Study of Linagliptin Vs Glimepiride in Type 2 Diabetes - American College of CardiologyDocument3 pagesCardiovascular Outcome Study of Linagliptin Vs Glimepiride in Type 2 Diabetes - American College of CardiologymagreaNo ratings yet
- Cardiovascular Outcomes in Trials of Oral Diabetes MedicationsDocument22 pagesCardiovascular Outcomes in Trials of Oral Diabetes MedicationsmagreaNo ratings yet
- Cardiovascular Disease in Diabetes, Beyond GlucoseDocument27 pagesCardiovascular Disease in Diabetes, Beyond GlucosemagreaNo ratings yet
- Annals of Otology, Rhinology & Laryngology - V..Document4 pagesAnnals of Otology, Rhinology & Laryngology - V..magreaNo ratings yet
- An Old Drug For A New Application Carbazochrome Sodium Sulfonate in HHTDocument2 pagesAn Old Drug For A New Application Carbazochrome Sodium Sulfonate in HHTmagreaNo ratings yet
- OtitisanDocument54 pagesOtitisanmagreaNo ratings yet
- And PerspectivesDocument34 pagesAnd PerspectivesmagreaNo ratings yet
- Medication Adherence in The Real WorldDocument13 pagesMedication Adherence in The Real WorldCognizantNo ratings yet
- Dedicated To Life, Healing & Recovery: Product ListDocument4 pagesDedicated To Life, Healing & Recovery: Product ListsyedsajjadaliNo ratings yet
- Anticoagulants Preoperative InstructionsDocument3 pagesAnticoagulants Preoperative InstructionsDevaki VisvalingamNo ratings yet
- Proton Pump Inhibitors, Adverse Events and Increased Risk of MortalityDocument36 pagesProton Pump Inhibitors, Adverse Events and Increased Risk of MortalityMohammad Mahmudur RahmanNo ratings yet
- ATI Pharm TIPSDocument17 pagesATI Pharm TIPSmike Gee100% (3)
- Management Acute Ischemic Stroke: Rusdi LamsudinDocument121 pagesManagement Acute Ischemic Stroke: Rusdi LamsudinWilliam FrazierNo ratings yet
- Special Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersDocument6 pagesSpecial Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersRatri ReswitadewiNo ratings yet
- 01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFDocument26 pages01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFawinsyNo ratings yet
- Drugs Study of Omeprazole, Metoclopramide EtcDocument12 pagesDrugs Study of Omeprazole, Metoclopramide EtcMargaret Cortinas75% (4)
- 4564 2934 p436 Pages Deleted EditedDocument4 pages4564 2934 p436 Pages Deleted EditedHaniNo ratings yet
- Curriculum Vitae: Nama: Prof DR DR Hasan Sjahrir Sps (KDocument11 pagesCurriculum Vitae: Nama: Prof DR DR Hasan Sjahrir Sps (KUKM MargaasihNo ratings yet
- Proton Pump InhibitorDocument10 pagesProton Pump InhibitorFishIngNo ratings yet
- Scientific Discussion: 1/20 EMEA 2004Document20 pagesScientific Discussion: 1/20 EMEA 2004Donny Rahman KhalikNo ratings yet
- Antiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat VaskularDocument23 pagesAntiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat Vaskularmonyet65No ratings yet
- Duoplavin Epar Public Assessment Report - enDocument37 pagesDuoplavin Epar Public Assessment Report - enyasser ShaterNo ratings yet
- Ischemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractDocument9 pagesIschemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractLina SafitriNo ratings yet
- Clopidogrel Bisulfate (PLOGREL)Document2 pagesClopidogrel Bisulfate (PLOGREL)Kristine Young0% (1)
- Curcumae: Dosen Pengampu: Rohima Robby, S.PD., M.PDDocument14 pagesCurcumae: Dosen Pengampu: Rohima Robby, S.PD., M.PDRezkya HenantoNo ratings yet
- Informed Consent - Filler - RadiesseDocument7 pagesInformed Consent - Filler - RadiesseAshraf AboNo ratings yet
- Drugs Affecting Blood CoagulationDocument51 pagesDrugs Affecting Blood CoagulationMoxie Macado100% (1)
- Pegasus TIMI 54 TrialDocument13 pagesPegasus TIMI 54 TrialIsaac Aaron Enriquez MonsalvoNo ratings yet
- Eur Heart J 2016 Roffi 267 315Document59 pagesEur Heart J 2016 Roffi 267 315Putu Reza Sandhya PratamaNo ratings yet
- Torrent Pharmaceuticals LTDDocument13 pagesTorrent Pharmaceuticals LTDvineminaiNo ratings yet
- Acute Coronary SyndromeDocument59 pagesAcute Coronary SyndromeLouis EkaputraNo ratings yet
- Clopidogrel Bisulfate - PlavixDocument2 pagesClopidogrel Bisulfate - PlavixKristi WrayNo ratings yet
- Fluconazole - Drug InformationDocument21 pagesFluconazole - Drug InformationjjjkkNo ratings yet
Clinical Use of Clopidogrel in Acute Coronary Syndrome: Reviewarticle
Clinical Use of Clopidogrel in Acute Coronary Syndrome: Reviewarticle
Uploaded by
magreaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Use of Clopidogrel in Acute Coronary Syndrome: Reviewarticle
Clinical Use of Clopidogrel in Acute Coronary Syndrome: Reviewarticle
Uploaded by
magreaCopyright:
Available Formats
doi: 10.1111/j.1742-1241.2007.01315.
REVIEW ARTICLE
Clinical use of clopidogrel in acute coronary syndrome
R. Zambahari,1 O-H Kwok,2 S. Javier,3 K. H. Mak,4 S. Piyamitr,5 H. Q. Tri Ho,6 J. J. Hwang,7
R. Suryawan,8 W. H. Chow9
OnlineOpen: This article is available free online at www.blackwell-synergy.com
1
SUMMARY Department of Cardiology,
Review Criteria Institut Jantung Negara, Kuala
Several therapeutic approaches have been developed to improve the outcome
• A literature search of major trials on clopidogrel Lumpur, Malaysia
among patients with acute coronary syndrome (ACS). However, treatment with 2
Cardiac Catheterization and
in acute coronary syndrome was performed
antithrombotic therapies such as oral glycoprotein IIb/IIIa inhibitors has been lim- between January 2001 and December 2005 on Intervention Centre, Hong Kong
ited by the lack of efficacy and excess bleeding complications. As the publication PubMed. Sanatorium and Hospital, Hong
of the landmark study Clopidogrel in Unstable Angina to Prevent Recurrent Events Kong SAR
• Only randomised, double-blind, placebo-controlled 3
Makati Medical Center,
(CURE), the clinical benefit of early and intermediate-term use of combined anti- trials were included in the review.
Manila, Philippines
platelet agents – clopidogrel plus aspirin – in non-ST-segment elevation myocardial 4
Gleneagles Medical Centre,
infarction (NSTEMI) patients became evident. Pretreatment and intermediate-term Message for the Clinic School of Mechanical and
• CLARITY–TIMI 28 and COMMIT trials have Aerospace Engineering,
therapy with clopidogrel in NSTEMI ACS patients undergoing percutaneous coron-
confirmed the role of clopidogrel in patients with Nanyang Technological
ary intervention (PCI) was further supported by the PCI–CURE trial. Recently, the University, Singapore
ST-elevation myocardial infarction (STEMI).
results of two major trials Clopidogrel as Adjunctive Reperfusion Therapy–Throm- • Clopidogrel is a safe and effective ‘add-on’
5
Ramathibodi Hospital,
bolysis in Myocardial Infarction 28, Clopidogrel and Metoprolol in Myocardial therapy in the treatment of STEMI across a broad Bangkok, Thailand
6
Infarction Trial established the pivotal role of clopidogrel in the other spectrum of Emergency and Reanimation
range of STEMI patient demographics with no
Cardiology, Ho Chi Minh City
ACS–STEMI. Coupled with the results from previous multicentre trials, these two excess of bleeding events.
Heart Institute, Vietnam
studies provide a guide for the early and long-term use of clopidogrel in the whole 7
Yun-lin Branch Hospital,
spectrum of ACS. A review summarising the results of the recent clinical trials and National Taiwan University
a discussion on its implications for the clinical management of ACS is presented. Hospital, Taipei, Taiwan
8
Dr. Soetomo General Hospital,
Jakarta, Indonesia
9
Asia-Pacific Region, Sanofi-
marises those results and discusses their implications
Introduction Aventis
for clinical practice.
The pathophysiology of acute coronary syndrome Correspondence to:
Dato Seri Dr Robaayah
(ACS) is plaque disruption because of either athero-
Pathophysiology of ACS Zambahari, Department of
sclerotic plaque rupture or endothelial erosion, leading Cardiology, Institut Jantung
to acute thrombotic occlusion of the coronary artery Acute coronary syndrome is caused by an acute or sub- Negara, 145, Jalan Tun Razak,
50400 Kuala Lumpur, Malaysia
(1). From the time of first presentation, ACS patients acute primary reduction of myocardial oxygen supply Tel.: (603) 2617 8434
are at high risk of life-threatening atherothrombotic provoked by disruption of an atherosclerotic plaque Fax: (603) 2692 8425
events, including myocardial infarction (MI) and associated with inflammation, thrombus formation, Email: robaayah@ijn.com.my
stroke. Ongoing research on ACS has been aiming at vasoconstriction and microembolisation (3). Throm- Disclosures
reducing these cardiovascular risks and improving clin- bosis is induced at the site of plaque rupture or ero- None of the independent
ical outcome. Thus, antithrombotic therapies have been sion that leads to rapid compromise of coronary blood authors listed above have
accepted honoraria from Sanofi-
the focus of various research studies, particularly those flow. Different degrees of the superimposed thrombus Aventis specifically for the
targeting on platelet activation and aggregation. formation at the site of plaque disruption are associ- development of this manuscript.
The efficacy of aspirin as an antiplatelet agent has ated with different clinical presentations of ACS. Thus, Dr Weng Ho Chow is a Medical
Director of Sanofi-Aventis and
been widely accepted in various settings. The efficacy platelet activation, aggregation and associated inflam- with the exception of Dr J. J.
of clopidogrel as an adjunct antiplatelet agent in mation play a key role in the transformation of a stable Hwang, the refmaining authors
ACS patients without ST-segment elevation has been atherosclerotic plaque to an unstable lesion. are members of an advocacy
group sponsored by Sanofi-
well established in aspirin-treated patients in the Aventis.
large Clopidogrel in Unstable Angina to Prevent
Mechanisms of action of antiplatelet
Recurrent Events (CURE) study (2). Recent clinical
agents
trial results have also provided an evidence base for
the use of clopidogrel concomitantly with aspirin to All mediators of platelet activation cause conforma-
reduce further the risk of thrombotic events in ACS tional changes in the glycoprotein IIb/IIIa surface
patients with ST-segment elevation. This review sum- receptor of platelets, allowing it to bind to circulating
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481 473
474 Clinical use of clopidogrel in ACS
fibrinogen and to form platelet–fibrin aggregates. cardiovascular events, reinfarction and ischaemia in
Inhibitors of the glycoprotein IIb/IIIa receptor are ACS patients routinely treated with aspirin, in both
expected to be the most potent antiplatelet agents, as the short and long term.
they block the final common pathway for platelet Long-term treatment of ACS patients with oral
aggregation. glycoprotein IIb/IIIa inhibitors has been associated
Aspirin permanently acetylates platelet cyclooxyge- with increased mortality, no change in the incidence
nase 1, blocking the synthesis of thromboxane A2. of MI and increased bleeding complications (13). The
Thromboxane A2 promotes activation of other plate- addition of intravenous glycoprotein IIb/IIIa inhibitor
lets and is a potent vasoconstrictor. Aspirin has no (abciximab) to fibrinolytic therapy (together with
effect on other platelet activators, such as adenosine aspirin and heparin) in STEMI patients was reported,
diphosphate (ADP), thrombin or serotonin. in a meta-analysis of trials involving 23,166 patients.
When released from red blood cells, activated The reinfarction rates were 2.3% and 3.6% for the
platelets and damaged endothelial cells, ADP induces abciximab and the control groups (p < 0.001) respec-
platelet adhesion and aggregation (4,5). The platelet tively, and 30-day mortality rates were 5.8% for both
ADP receptor effects dense and a-granule release, groups (14). However, the rate of major bleeding
thromboxane A2 generation, glycoprotein IIb/IIIa complications was significantly higher among those
receptor activation and P-selectin expression (6). treated with abciximab (5.2%) compared with
Clopidogrel is a thienopyridine derivative that placebo (3.1%) (p < 0.001). This suggests that there
selectively and irreversibly inhibits the P2Y12 compo- is an additional role for antiplatelet therapy apart
nent of the platelet ADP receptor (7) and has no from the use of oral glycoprotein IIb/IIIa inhibitors.
direct effect on other mediators of platelet aggrega- Conversely, the use of clopidogrel has been shown
tion such as cyclooxygenase, thromboxane synthetase to be safe and efficacious in the long term. Compared
or adenoside. A thienopyridine derivative, clopidog- with aspirin 325 mg, clopidogrel was shown to pro-
rel is a prodrug which is metabolised by the hepatic vide a relative risk reduction of 8.7% [absolute risk
cytochrome P450-1A enzyme system to a short-lived reduction, 0.5% (NNT (number needed to treat) ¼
thiol that binds to the P2Y12 receptor. By blocking 200); p ¼ 0.043] for ischaemic stroke, MI or vascular
the ADP-dependent mechanisms of platelet activa- death among 19,185 patients with recent MI or isch-
tion, clopidogrel also limits the activation by other aemic stroke or peripheral artery disease (15). This
agonists and results in markedly decreased platelet benefit extended beyond the 25% relative risk reduc-
recruitment and aggregation. Maximal inhibition of tion provided by aspirin, and was associated with
ADP-induced platelet aggregation by clopidogrel ran- fewer bleeding complications during a follow-up per-
ges from 40% to 60%. This steady state is reached in iod of 1.91 years (15). Subsequently, early and inter-
3–5 days in healthy subjects at a standard dose of mediate-term (9 months–1 year) use of clopidogrel
75 mg/day or in 2–5 h after a 300 mg loading dose (300 mg loading dose, then 75 mg/day for a mean
(8). The antiplatelet effects of clopidogrel and aspirin duration of 9 months) plus aspirin in non-ST-seg-
are thus synergistic (9,10). ment elevation MI (NSTEMI) patients (n ¼ 12,562)
was shown being able to reduce the relative risk of
death from cardiovascular causes, non-fatal MI or
Rationale for the use of clopidogrel in
stroke by 20% (p < 0.001) compared with aspirin
ACS
alone in the CURE study (Figure 1) (2). Subgroup
The benefit of the use of aspirin was shown in the analysis of the trial results revealed that the rates of
Second International Study of Infarct Survival, which each component of the composite outcome also ten-
enrolled 17,187 subjects with acute ST-segment eleva- ded to be lower in the clopidogrel group, with the
tion MI (STEMI). Aspirin was shown to safely greatest difference observed for rates of reinfarction
reduce vascular mortality by about 25% and recur- (5.2% in the clopidogrel group vs. 6.7% in the pla-
rent non-fatal infarction by about 50% in the study cebo group). Although there were significantly more
(11). Subsequently, the Antithrombotic Trialists’ Col- patients with major bleeding in the clopidogrel group
laboration Group reviewed 287 studies which (3.7% vs. 2.7%; relative risk, 1.38; p ¼ 0.001), there
involved a wide variety of high-risk vascular patients were not significantly more patients with life-threat-
to compare the ability of various antiplatelet regi- ening bleeding or haemorrhagic strokes.
mens (n ¼ 77,000) vs. control (n ¼ 135,000) in Coronary stenting has improved the outcome of
reducing adverse cardiovascular events (12). Anti- percutaneous coronary intervention (PCI). However,
platelet therapy (usually aspirin) reduced the risk of stent thrombosis was a major limitation (16). Dual
vascular death, MI or stroke by about 25%. How- antiplatelet therapy has been shown to be consis-
ever, there was still a substantial risk of death from tently better than anticoagulation in preventing this
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
Clinical use of clopidogrel in ACS 475
Aspirin (n = 6303) thrombosis. In patients with STEMI, clinical practice
0.14 Clopidogrel + Aspirin (n = 6259) 11.4% guidelines recognise the importance of promptly
0.12 20% restoring normal epicardial blood flow and myocardial
Cumulative hazard rates
p < 0.001
perfusion in the infarct zone (24,25). The most effect-
0.10 9.3%
ive pharmacological reperfusion regimen appears to be
0.08 concurrent fibrinolytic therapy and platelet inhibition
0.06 and, up until recently, aspirin was the only antiplatelet
0.04 agent routinely used in this setting.
0.02
0.00 Clopidogrel reduces the risk of death,
0 3 6 9 12 recurrent MI and stroke
Follow-up (months) (COMMIT/CCS-2 trial results)
Cumulative events: MI, stroke, or CV, death
The Clopidogrel and Metoprolol in Myocardial
Figure 1 Early and long-term benefits of clopidogrel in
unstable angina (CURE study) (2). (Reproduced with Infarction Trial/Second Chinese Cardiac Study
permission from the Publishing Division of the (COMMIT/CCS-2) was a highly powered, random-
Massachusetts Medical Society) ised, double-blind, placebo-controlled trial jointly
co-ordinated by the Clinical Trial Service Unit of
complication. Indeed, clopidogrel plus aspirin treat- Oxford University, UK and the Fuwai Hospital,
ment (4 weeks) has become standard care for pre- Chinese Academy of Medical Sciences, Beijing, China
venting stent thrombosis in patients who received (26). Spanning 5 years, patients (n ¼ 45,852) in this
bare metal stents implantation (17–20). The PCI– study of the emergency treatment of acute MI were
CURE trial results demonstrated that extending recruited from 1250 hospitals throughout China. The
clopidogrel use to include pretreatment and long- objectives of the antiplatelet arm of the trial were to
term treatment (mean 8 months) in NSTEMI ACS investigate whether adding clopidogrel (75 mg/day)
patients (n ¼ 2658) undergoing PCI reduced the risk to aspirin and standard fibrinolytic and anticoagulant
of cardiovascular death or MI by about one-third therapy would further reduce the composite risk of
(21). These findings corroborated the results of death, recurrent MI or stroke, or improve mortality,
the prospective, randomised, placebo-controlled compared with placebo.
Clopidogrel for the Reduction of Events During Patients were enrolled if they presented with sus-
Observation trial (n ¼ 2116), which showed that a pected acute MI within 24 h of the onset of symp-
pretreatment dose of 300 mg clopidogrel 6–24 h toms, and the scheduled treatment period was
before PCI afforded the greatest effect (relative risk 4 weeks or prior hospital discharge. There were no
reduction, 38.6%; p ¼ 0.51) (22). age limits for inclusion in the study: patients had a
The results from the Antiplatelet therapy for Reduc- mean age of 61 years and 26% of patients were
tion of Myocardial Damage during Angioplasty study 70 years of age or older. The use of other therapies
which demonstrated that pretreatment with a higher was balanced between the clopidogrel and placebo
(600 mg) loading dose of clopidogrel significantly groups. About 55% of patients received fibrinolytic
reduced the risk of MI by 50% (odds ratio 0.48, p ¼ drugs (typically urokinase), which may not be com-
0.044) in patients undergoing PCI, suggests that there parable with the rate of thrombolysis in other West-
is potential benefit of using a higher loading dose ern countries. The average time from symptom onset
(600 mg) of clopidogrel in clinical practice (23). to presentation was just over 10 h, and the mean
Although clopidogrel had established a record of treatment duration was 15 days.
reducing ischaemic events without significantly The COMMIT study results (Figure 2) showed
increasing bleeding complications in a number of that the addition of clopidogrel to aspirin signifi-
settings, its role in STEMI patients remained unde- cantly reduced the relative risk of in-hospital death
fined until the results of the CLARITY–TIMI 28 and by 7% [absolute risk reduction, 0.6% (NNT ¼ 167);
COMMIT trials were published in 2005. p ¼ 0.03] and the risk of composite cardiovascular
events (death, reinfarction or stroke) by about 10%
[absolute risk reduction, 0.9% (NNT ¼ 111); p ¼
Clopidogrel reduces mortality in
0.002]. These benefits appeared to be independent
ST-segment elevation myocardial
of, and therefore additional to, those of other stand-
infarction
ard treatments. There was no apparent increase in
Platelet activation and aggregation are key processes major bleeding, even when clopidogrel was adminis-
in the initiation and propagation of coronary-artery tered with fibrinolytic agents or to older patients.
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
476 Clinical use of clopidogrel in ACS
12
Clopidogrel (n = 22,961)
2310
2121 (10.1%)
Clopidogrel improves the patency rate
10
Placebo (n = 22,891)
(9.2%) in the infarct-related artery and
Proportion of patients (%)
1845
1726 (8.1%)
8
(7.5%) reduces ischaemic complications
6
(CLARITY trial results)
4 Clopidogrel as Adjunctive Reperfusion Therapy–
270 330
127 142
Thrombolysis in Myocardial Infarction (CLARITY–
2 (1.2%) (1.4%)
(0.6%) (0.6%) TIMI 28) was designed to determine whether the
0
Reinfarction Stroke Death Death,
addition of clopidogrel is beneficial in STEMI patients
(survived) (survived) (any cause) reinfarction, who are receiving a standard fibrinolytic regimen,
or stroke
including aspirin (32). Patients (n ¼ 3491) aged
Figure 2 Absolute effects of clopidogrel on death, between 18 and 75 years were randomised to receive
reinfarction, or stroke (COMMIT study) (26). (Reproduced either clopidogrel (300 mg loading dose followed by
with permission from Elsevier)
75 mg once daily) or placebo in a double-blind setting.
This represents the first change in pharmacologi- The average time from symptom onset to fibrino-
cal reperfusion therapy for patients with STEMI in lytic administration was 2.7 h. Study medication was
more than 10 years that has achieved mortality administered up to and including the day of coronary
benefit. Earlier studies have shown that fibrinolytic angiography or, for patients who did not undergo
therapy failed to restore coronary flow in approxi- angiography, up to and including day 8 or hospital
mately 20% of STEMI patients (27–29). Among discharge, whichever came first. The protocol speci-
those who did not achieve reperfusion, mortality fied that coronary angiography be performed during
rates were doubled. Furthermore, angiographic re- index hospitalisation, 48–192 h after the start of study
occlusion occurred in 5–8% of patients during medication (or earlier if clinically indicated), to assess
index hospitalisation and these patients had an for late patency of the infarct-related artery. Patients
associated threefold increase in mortality (30). were followed up for 30 days for clinical events.
These adverse outcomes may have been overcome Treatment with clopidogrel resulted in a 36%
in the COMMIT study group by the synergistic relative reduction [absolute risk reduction, 6.7%
effects of clopidogrel and aspirin. Together, they (NNT ¼ 15); p < 0.001] in the composite odds of an
may have sufficiently reduced platelet activity so occluded infarct-related artery on the predischarge
that the threshold of aggregation was not exceeded, angiogram or death or recurrent MI by the time of
shifting the balance in favour of sustained reper- angiography. This benefit was consistent across a
fusion rather than reocclusion. broad range of subgroups (Table 1). At 30 days,
The benefits of adding clopidogrel were seen in a clopidogrel therapy led to a significant 20% relative
wide range of patients (Figure 3), even in older reduction in the odds of death from cardiovascular
patients aged over 70 and those presenting many causes, recurrent MI or ischaemia leading to the need
hours after the onset of symptoms. The findings for urgent revascularisation (p ¼ 0.03). Treatment
derived from the large population studied using a with clopidogrel was not associated with an increased
simple protocol, which allows management of rate of major bleeding or intracranial haemorrhage.
patients to approximate real world clinical practice, In a subgroup of patients from the CLARITY–TIMI
are likely to be applicable to STEMI patients in many 28 study, investigators sought to determine whether
other countries of the world. clopidogrel pretreatment before PCI in patients with
An unexpected observation during COMMIT was recent STEMI was superior to clopidogrel initiated at
that the benefit of clopidogrel emerged as early as the time of PCI in preventing major adverse events
the first day of therapy (Figure 4) even without a (PCI–CLARITY) (33). Patients were randomised to
loading dose. In the absence of a loading dose, max- receive clopidogrel as a 300 mg loading dose, fol-
imal antiplatelet effects with clopidogrel are expected lowed by 75 mg/day (n ¼ 933), or placebo (n ¼ 930)
to be seen days after initiation. No loading dose was in addition to a fibrinolytic agent and aspirin, for
given to patients in the COMMIT study because of 2–8 days until angiography. PCI was performed, at
concerns about potential bleeding complications. the discretion of the investigator, at an average of
Some antiplatelet activity does develop within a few 3 days after randomisation. Patients who underwent
hours of administering a 75 mg oral dose and may coronary stenting received a loading dose of at least
be adequate to provide the beneficial effect (31). It is 300 mg clopidogrel, followed by 75 mg daily.
possible that the results might have been more Pretreatment with clopidogrel significantly reduced
favourable had the patients received a 300 mg load- the odds of cardiovascular death, reinfarction or
ing dose of clopidogrel. stroke by 46% before and within 30 days following
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
Clinical use of clopidogrel in ACS 477
Events (%)
Heterogeneity
Clopidogrel Placebo or trend test
2
Baseline categorization (22,961) (22,891) Odds ratio (CI) (p)
Age at entry (years)
60 485 (5.0%) 512 (5.4%) 0.0 (0.9)
60–69 745 (10.1%) 835 (11.2%)
70 891 (14.9%) 963 (16.2%)
Sex
Male 1274 (7.7%) 1416 (8.6%) 1.0 (0.3)
Female 847 (13.3%) 894 (14.0%)
Time since onset (h)
6 709 (9.2%) 830 (10.8%) 5.7 (0.02)
6 to 13 738 (9.8%) 808 (10.8%)
13–24 674 (8.8%) 672 (8.8%)
Systolic blood pressure (mmHg)
120 797 (10.4%) 892 (11.6%) 1.0 (0.3)
120–139 693 (8.6%) 770 (9.5%)
140–159 388 (8.5%) 399 (8.9%)
160 243 (9.2%) 249 (9.6%)
Heart rate (bpm)
70 268 (5.3%) 315 (6.2%) 0.0 (1.0)
70–89 898 (8.1%) 952 (8.5%)
90–109 632 (12.3%) 683 (13.5%)
110 323 (19.9%) 360 (22.2%)
ECG at entry
Bundle branch block 270 (17.9%) 247 (17.4%) 1.8 (0.2)
ST elevation 1753 (8.8%) 1952 (9.8%)
ST depression 98 (6.2%) 111 (7.0%)
Killip class
I 1273 (7.3%) 1415 (8.2%) 0.6 (0.5)
II/III 848 (15.0%) 895 (16.0%)
Fibrinolytic agent given
Yes 1003 (8.8%) 1122 (9.9%) 0.7 (0.4)
No 1118 (9.7%) 1188 (10.3%)
Previous MI
Yes 177 (9.0%) 204 (11.1%) 1.6 (0.2)
No 1944 (9.3%) 2106 (10.0%)
Previous Aspirin use
Yes 399 (9.5%) 439 (10.4%) 0.0 (1.0)
No 1722 (9.2%) 1871 (10.0%)
Eligible for CLARITY trial
Yes 612 (8.2%) 717 (9.6%) 1.8 (0.2)
No 1509 (9.7%) 1593 (10.4%)
Metoprolol allocation
Yes 1063 (9.3%) 1110 (9.7%) 2.4 (0.1)
No 1058 (9.2%) 1200 (10.5%)
Prognostic index (3 equal groups)
Good 228 (3.0%) 282 (3.7%) 3.1 (0.08)
Average 574 (7.5%) 636 (8.3%)
Poor 1319 (17.3%) 1392 (18.2%)
Total 2121 (9.2%) 2310 (10.1%) 9% (SE 3)
proportional
Heterogeneity test: 2
22.9; p 0.3 reduction
21
(p 0.002)
0.5 0.75 1.0 1.25 1.5
Clopidogrel Placebo
better better
Figure 3 Effects of clopidogrel allocation on death, reinfarction, or stroke in different categories of patient (COMMIT
study) (26). (Reproduced with permission from Elsevier)
PCI, irrespective of the timing of PCI relative to gender, the presence of diabetes mellitus or infarct
randomisation (Table 2). Clopidogrel pretreatment location. The benefit of pretreatment was also similar
was consistently beneficial regardless of patient age, whether patients had PCI urgently for recurrent
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
478 Clinical use of clopidogrel in ACS
Events (%) ary artery procedures (PCI or stenting). The benefits
Days of Clopidogrel Placebo
event (22,961) (22,891) Odds ratio (CI)
demonstrated by the Clopidogrel vs Aspirin In
0 463 (2.0%) 524 (2.3%)
Patients at Risk of Ischemic Events (CAPRIE) and
1 482 (2.1%) 525 (2.3%) CURE studies led to the current recommendations
2–3 450 (2.0%) 451 (2.0%)
4–7 432 (1.9%) 463 (2.0%) for clopidogrel use in the American Heart Associ-
8–28 294 (1.3%) 347 (1.5%)
ation (AHA)/American College of Cardiology (24,34)
9% (SE 3)
Total 2121 (9.2%) 2310 (10.1%)
proportional and European Society of Cardiology (3) guidelines
reduction
(p = 0.002) on ACS management.
0.5 0.75 1.0 1.25 1.5 The improved mortality and reduced risks of rein-
Heterogeneity test: x2 = 3.0; p = 0.6 Clopidogrel Placebo farction and stroke seen in patients with acute MI in
4
better better
the COMMIT trial were achieved with short treat-
Figure 4 Effects of clopidogrel allocation on death, ment duration at fairly low cost. Clopidogrel could
reinfarction, or stroke by day of event in COMMIT study. therefore be used widely in populations with limited
Odds ratio in each period (black square with area
resources as well as in developed countries. Accord-
proportional to number of events) and 99% CI (horizontal
ing to the COMMIT results, early clopidogrel ther-
line); broken vertical line indicates oversall result, and
diamond indicates its 95% CI (26). (Reproduced with
apy has the potential to prevent about 5000 deaths
permission from Elsevier) and 5000 non-fatal reinfarctions and strokes if it
were given to 1 million of the 10 million patients
ischaemia or electively, and whether or not they worldwide who have an MI each year. The COMMIT
received glycoprotein IIb/IIIa inhibitor or a loading trialists recommended starting clopidogrel [probably
dose of open label clopidogrel at the time of PCI. with a loading dose as in the CURE study (2)] in
There was no significant increase in the risk of major almost all patients presenting with suspected acute
or minor bleeding, even though these patients had MI, irrespective of age, gender and the use of other
received intensive antiplatelet therapy. treatments (provided there are no strong contraindi-
cations). They also suggested that continuing clopi-
dogrel therapy after hospital discharge might lead to
Implications for future management further gains (35). Long-term benefit of dual anti-
of ACS
platelet therapy with clopidogrel plus low-dose aspi-
Increasingly, clopidogrel is included in the long-term rin was recently shown in subgroups of patients with
therapy for unstable angina (UA) and during coron- prior MI from a recent analysis of the Clopidogrel
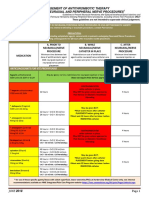
Table 1 Benefits of clopidogrel across subgroups in the CLARITY study: Reduced odds and event rates for the
composite of an occluded infarct-related artery on the pre-discharge angiogram, death, or recurrent MI by the time of
angiography [32].
Event rates (%)
Characteristic Number of patients Odds reduction (%) Clopidogrel Placebo
Overall 3491 36 15.0 21.7
Age
<65 years 2466 42 13.2 21.0
>65 years 1015 22 19.0 23.1
Gender
Male 2796 35 14.5 20.8
Female 685 38 16.9 24.7
Infarct location
Anterior 1416 33 15.0 20.7
Non-anterior 2065 38 15.0 22.0
Fibrinolytic agent
Fibrin-specific 2397 31 14.7 20.1
Non-fibrin-specific 1084 44 15.7 24.9
Predominant heparin
Low molecular weight 1429 31 11.4 15.7
Unfractionated 1431 42 17.8 27.1
None 621 26 17.1 21.9
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
Clinical use of clopidogrel in ACS 479
Table 2 Major cardiovascular outcomes according to allocation of clopidogrel pretreatment before PCI (PCI-CLARITY
study) [33].* (Reproduced with permission from American Medical Association)
No. (%)
Clopidogrel No
pretreatment pretreatment Adjusted odds ratio
Outcome (n ¼ 933) (n ¼ 930) (95% CI) p Value
Outcomes before PCI
MI or stroke 37 (4.0) 58 (6.2) 0.62 (0.40–0.95) 0.03
MI 37 (4.0) 57 (6.1) 0.60 (0.38–0.95)
Stroke 0 1 (0.1) –
Outcomes after PCI
Cardiovascular death, MI, or stroke 34 (3.6) 58 (6.2) 0.54 (0.35–0.85) 0.008
Cardiovascular death or MI 31 (3.3) 50 (5.4) 0.58 (0.36–0.94) 0.03
Cardiovascular death 13 (1.4) 24 (2.6) 0.49 (0.24–1.03)
MI 18 (1.9) 29 (3.1) 0.60 (0.33–1.11)
Stroke 4 (0.4) 11 (1.2) 0.35 (0.11–1.11)
Overall outcomes before and after PCI
Cardiovascular death, MI, or stroke 70 (7.5) 112 (12.0) 0.59 (0.43–0.81) 0.001
Cardiovascular death or MI 67 (7.2) 103 (11.1) 0.62 (0.45–0.86) 0.004
Cardiovascular death 13 (1.4) 24 (2.6) 0.49 (0.24–1.03)
MI 55 (5.9) 83 (8.9) 0.64 (0.44–0.92)
Stroke 4 (0.4) 12 (1.3) 0.32 (0.10–1.01)
Abbreviations: CI, confidence interval; MI, myocardial infarction; PCI, percutaneous coronary intervention.
*Patients may have had more than 1 outcome. Patients with cardiovascular events before and after PCI are counted in each category,
but counted only once for overall event rates.
Variables controlled for in adjusted analysis included type of fibrinolytic, initial type of heparin, infarct location, and a propensity score
for PCI.
for High Atherothrombotic Risk and Ischemic Stabil- alone. In practice, few patients presenting with
ization, Management, and Avoidance trial (36). The STEMI undergo urgent surgery (e.g. coronary artery
study had a median follow-up of 28 months. How- bypass grafting) during the index hospitalisation.
ever, as with all subgroup analyses, the results should Therefore, there is no need to delay clopidogrel
be interpreted with caution. Nevertheless, in STEMI administration because of the risk of major bleeding
patients, it is clear that current data supports the use during a surgical procedure and should be safe to
of clopidogrel for up to 28 days postevent. administer to suspected acute MI patients during the
The CLARITY–TIMI 28 study, which enrolled early acute phase.
STEMI patients mainly in western Europe and North Moreover, a recent extension of the CLARITY–
America, was different in design to the COMMIT TIMI 28 study has shown that it is feasible to treat
study, in that it incorporated a loading dose of clopi- STEMI patients with fibrinolytic agents, heparin,
dogrel, a fibrin-specific lytic agent was given to more aspirin and clopidogrel in medically-equipped ambu-
than two-thirds of patients with an average time lances without an increase in major bleeding compli-
from symptom onset to fibrinolytic administration of cations (37). Preliminary results indicate that
< 3 h, and angiography 2–8 days after the start of prehospital administration of clopidogrel significantly
study medication followed by PCI in more than half reduced the risk of an occluded infarct artery (TIMI
the patients. Nevertheless, current evidence showed flow grade 0/1), death and reinfarction prior to angi-
that the addition of clopidogrel to aspirin represents ography.
a major advance in the care of STEMI patients, with The benefit of clopidogrel pretreatment in the
clear benefit across a broad range of patient demo- PCI–CLARITY study was consistently maintained
graphics and practice patterns and no excess of across pretreatment periods ranging from 6 h to
bleeding events. 8 days, suggesting that even brief periods of pretreat-
The use of clopidogrel plus aspirin in acute MI ment with clopidogrel before PCI improved patient
requires no extra monitoring compared with aspirin outcomes. The event curves for the study and control
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
480 Clinical use of clopidogrel in ACS
groups continued to diverge following PCI, suggest- • a 300 mg oral dose of clopidogrel to emergency
ing that the benefit of clopidogrel pretreatment may department patients up to 75 years of age with
extend beyond the prevention of platelet aggregation STEMI who receive aspirin, heparin and fibrinoly-
during the procedure. According to the PCI–CLAR- sis.
ITY data, adopting a strategy of clopidogrel pretreat-
ment in 100 patients undergoing PCI should prevent
Acknowledgements
two MIs before PCI and two cardiovascular deaths,
MIs or strokes in the 30 days following PCI. We would like to acknowledge Sanofi-Aventis for
For those ACS patients who do not undergo PCI, providing editorial support for the development of
their reperfusion will be managed pharmacologically. this manuscript.
In this context, clopidogrel has been shown to reduce
the reoccurrence of thrombotic events without signi-
References
ficantly increasing major bleeding complications with
treatment of up to 30 days (STEMI patients) and 1 Yeghiazarians Y, Braunstein JB, Askari A et al. Unstable angina
pectoris. N Engl J Med 2000; 342: 101–14.
much longer (UA and NSTEMI patients). The fact 2 The Clopidogrel in Unstable Angina to Prevent Recurrent Events
that the COMMIT trial was conducted in China is Trial Investigators. Effects of clopidogrel in addition to aspirin in
noteworthy in that there was always a concern over patients with acute coronary syndromes without ST-segment eleva-
increased bleeding risk in Asians compared with tion. N Engl J Med 2001; 345: 494–502.
3 Bertrand ME, Simoons ML, Fox KA et al. Task Force on the Man-
Caucasians after intensive antiplatelet therapy. agement of Acute Coronary Syndromes of the European Society of
The results of both the COMMIT and CLARITY– Cardiology. Management of acute coronary syndromes in patients
TIMI studies have led to the approved extended use presenting without persistent ST-segment elevation. Eur Heart J
2002; 23: 1809–40.
of clopidogrel in STEMI patients from the US Food
4 Gardner A, Jonsen J, Laland S et al. Adenosine diphosphate in red
and Drug Administration and the European Medi- blood cells as a factor in the adhesiveness of human blood plate-
cines Evaluation Agency in August 2006. In future, lets. Nature 1961; 192: 531–2.
clopidogrel may be included as part of the long-term 5 Meyers KM, Holmsen H, Seachord CL. Comparative study of
platelet dense granule constituents. Am J Physiol 1982; 243: R454–
medical management of all ACS patients.
61.
6 Dorsam RT, Kunapuli SP. Central role of the P2Y12 receptor in
platelet activation. J Clin Invest 2004; 113: 340–5.
Conclusions 7 Quinn MJ, Fitzgerald DJ. Ticlopidine and clopidogrel. Circulation
1999; 348: 1329–39.
Both the COMMIT and the CLARITY–TIMI 28 trials
8 Savcic M, Hauert J, Bachmann F et al. Clopidogrel loading dose
have shown that clopidogrel is a safe and effective regimens: kinetic profile of pharmacodynamic response in healthy
‘add-on’ therapy in the early treatment of STEMI. subjects. Semin Thromb Hemost 1999; 25: 15–9.
Considering all the evidence, it may be reasonable to 9 Herbert J, Dol F, Bernat A et al. The antiaggregating and anti-
thrombotic activity of clopridogrel is potentiated by aspirin in sev-
prescribe clopidogrel 300 mg for patients < 75 years eral experimental models in the rabbit. Thromb Haemost 1998; 80:
old with STEMI upfront and clopidogrel 75 mg for 512–8.
patients > 75 years old with STEMI. Initiating clopi- 10 Moshfegh K, Redondo M, Julmy F et al. Antiplatelet effects of
dogrel therapy in the ambulance may further reduce clopidogrel compared with aspirin after myocardial infarction:
enhanced inhibitory effects of combination therapy. J Am Coll Car-
ischaemic times and promote faster and better reper- diol 2000; 36: 699–705.
fusion. 11 ISIS-2 (Second International Study of Infarct Survival) Collaborat-
The 2005 AHA Guidelines for Cardiopulmonary ive Group. Randomised trial of intravenous streptokinase, oral
Resuscitation and Emergency Cardiovascular Care aspirin, both or neither among 17,187 cases of suspected acute
myocardial infarction: ISIS-2. Lancet 1988; 2: 349–60.
have developed an algorithm for stabilisation of 12 Antithrombotic Trialists’ Collaboration. Collaborative meta-analy-
patients with ACS (38). The recommendations sis of randomised trials of antiplatelet therapy for prevention of
include giving: death, myocardial infarction, and stroke in high risk patients.
Br Med J 2002; 324: 71–86.
• a 300 mg loading dose of clopidogrel, in addition
13 Chew DP, Bhatt DL, Sapp S et al. Increased mortality with oral
to standard care, to emergency department patients platelet glycoprotein IIb/IIIa antagonists: a meta-analysis of phase
with ACS with elevated cardiac markers or new ECG III multicenter randomized trials. Circulation 2001; 103: 201–6.
changes consistent with ischaemia (excluding 14 De Luca G, Suryapranata H, Stone GW et al. Abciximab as adjunc-
tive therapy to reperfusion in acute ST-segment elevation myocar-
STEMI) in whom a medical approach or PCI is
dial infarction: a meta-analysis of randomized trials. JAMA 2005;
planned (class I); 293: 1759–65.
• a 300 mg oral dose of clopidogrel to emergency 15 CAPRIE Steering Committee. A randomised, blinded, trial of
department patients with suspected ACS (without clopidogrel versus aspirin in patients at risk of ischaemic events
(CAPRIE). Lancet 1996; 348: 1329–39.
ECG or cardiac marker changes) who are unable to 16 Mak KH, Belli G, Ellis SG et al. Subacute stent thrombosis:
take aspirin because of hypersensitivity or major gas- evolving issues and current concepts. J Am Coll Cardiol 1996; 27:
trointestinal intolerance (class IIa); 494–503.
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
Clinical use of clopidogrel in ACS 481
17 Bertrand ME, Legrand V, Boland J et al. Randomized multicenter 28 The GUSTO Angiographic Investigators. The effects of tissue
comparison of conventional anticoagulation versus antiplatelet plasminogen activator, streptokinase, or both on coronary-artery
therapy in unplanned and elective coronary stenting: The Full patency, ventricular function, and survival after acute myocardial
Anticoagulation versus Aspirin and Ticlopidine (FANTASTIC) infarction. N Engl J Med 1993; 329: 1615–22.
Study. Circulation 1998; 98: 1597–603. 29 Braunwald E. The open-artery theory is alive and well–again.
18 Leon MB, Baim DS, Popma JJ et al. A clinical trial comparing N Engl J Med 1993; 329: 1650–2.
three antithrombotic-drug regimens following coronary artery 30 Ohman EM, Califf RM, Topol EJ et al. Consequences of reocclu-
stenting. N Engl J Med 1998; 339: 1665–71. sion after successful reperfusion therapy in acute myocardial
19 Schömig A, Neumann F, Kastrati A et al. A randomized compar- infarction. Circulation 1990; 82: 781–91.
ison of antiplatelet and anticoagulant therapy after placement of 31 Cadroy Y, Bossavy JP, Thalamas C et al. Early potent antithrom-
coronary-artery stents. N Engl J Med 1996; 334: 1084–9. botic effect with combined aspirin and a loading dose of clopidog-
20 Urban P, Macaya C, Rupprecht H-J et al. Randomized evaluation rel on experimental arterial thrombogenesis in humans. Circulation
of anticoagulation versus antiplatelet therapy after coronary stent 2000; 101: 2823–28.
implantation in high-risk patients: the Multicenter Aspirin and 32 Sabatine MS, Cannon CP, Gibson CM et al. Addition of
Ticlopidine Trial after Intracoronary Stenting (MATTIS). Circula- clopidogrel to aspirin and fibrinolytic therapy for myocardial
tion 1998; 98: 2126–32. infarction with ST-segment elevation. N Engl J Med 2005; 352:
21 Mehta SR, Yusuf S, Peters RJG et al. Effects of pretreatment with 1179–89.
clopidogrel and aspirin followed by long-term therapy in patients 33 Sabatine MS, Cannon CP, Gibson CM et al. Effect of clopidogrel
undergoing percutaneous coronary intervention: the PCI-CURE pretreatment before percutaneous coronary intervention in patients
study. Lancet 2001; 358: 527–33. with ST-elevation myocardial infarction treated with fibrinolytics.
22 Steinhubl SR, Berger PB, Mann JT et al. Early and sustained dual The PCI–CLARITY study. JAMA 2005; 294: 1224–32.
oral antiplatelet therapy following percutaneous coronary interven- 34 Smith SC Jr, Dove JT, Jacobs AK et al. ACC/AHA guidelines for
tion: a randomized controlled trial. JAMA 2002; 288: 2411–20. percutaneous coronary intervention: a report of the American
23 Patti G, Colonna G, Pasceri V et al. Randomized trial of high load- College of Cardiology/American Heart Association Task Force on
ing dose of clopidogrel for reduction of periprocedural myocardial Practice Guidelines (Committee to Revise the 1993 Guidelines for
infarction in patients undergoing coronary intervention. Results Percutaneous Transluminal Coronary Angioplasty). J Am Coll
from the ARMYDA-2 (Antiplatelet therapy for Reduction of Myo- Cardiol 2001; 37: 2215–39.
cardial Damage during Angioplasty) Study. Circulation 2005; 111: 35 Bhatt DL, Topol EJ. Clopidogrel added to aspirin versus aspirin
2099–106. alone in secondary prevention and high-risk primary prevention:
24 Braunwald E, Antman EM, Beasley JW et al. ACC/AHA 2002 rationale and design of the Clopidogrel for High Atherothrombotic
guideline update for the management of patients with unstable Risk and Ischemic Stabilization, Management, and Avoidance
angina and non-ST-segment elevation myocardial infarction – (CHARISMA) Trial. Am Heart J 2004; 148: 263–8.
summary article: a report of the American College of Cardiology/ 36 Bhatt DL, Fox KAA, Hacke W et al. Clopidogrel and aspirin versus
American Heart Association task force on practice guidelines aspirin alone for the prevention of atherothrombotic events.
(Committee on the Management of Patients with Unstable N Engl J Med 2006; 354: 1706–17.
Angina). J Am Coll Cardiol 2002; 40: 1366–74. 37 Montalescot G, Verheugt F, Sabatine MS et al. Prehospital fibrino-
25 Van de Werf F, Ardissino D, Betriu A et al. The Task Force on the lysis with dual antiplatelet therapy in ST-elevation myocardial
Management of Acute Myocardial Infarction of the European Soci- infarction. The Prehospital CLARITY–TIMI 28 substudy. Circula-
ety of Cardiology. Management of acute myocardial infarction in tion 2005; 112: ??? (Abstract 2691).
patients presenting with ST-segment elevation. Eur Heart J 2003; 38 2005 American Heart Association Guidelines for Cardiopulmonary
24: 28–66. Resuscitation and Emergency Cardiovascular Care. Part 8: stabil-
26 COMMIT Collaborative Group. Addition of clopidogrel to aspirin ization of the patient with acute coronary syndromes. Circulation
in 45,852 patients with acute myocardial infarction: randomized 2005; 112: IV89–110.
placebo-controlled trial. Lancet 2005; 366: 1607–21.
27 The TIMI Study Group. The Thrombolysis in Myocardial Infarc-
tion (TIMI) trial: phase I findings. N Engl J Med 1985; 312: 932–6. Paper received August 2006, accepted December 2006
ª 2007 The Authors
Journal compilation ª 2007 Blackwell Publishing Ltd Int J Clin Pract, March 2007, 61, 3, 473–481
You might also like
- الخلاصه في 23 ورقهDocument23 pagesالخلاصه في 23 ورقهصلاح البازليNo ratings yet
- Stop Anticoagulation Neuraxial AnesthesiaDocument3 pagesStop Anticoagulation Neuraxial AnesthesiaGihan NakhlehNo ratings yet
- De Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IDocument43 pagesDe Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IAkhmad HidayatNo ratings yet
- Jamacardiology Rhee 2023 Oi 230014 1681134690.05816 PDFDocument10 pagesJamacardiology Rhee 2023 Oi 230014 1681134690.05816 PDFFernando DominguezNo ratings yet
- Antiplatelt Before During and Post PCIDocument8 pagesAntiplatelt Before During and Post PCIVivekanandGuptaNo ratings yet
- 2023 Kardio Aspirin Vs Clopidogrel For Long Term Maintenance AfterDocument10 pages2023 Kardio Aspirin Vs Clopidogrel For Long Term Maintenance AfterAuliya AndiNo ratings yet
- ClairDocument9 pagesClairMuhammad Imran MirzaNo ratings yet
- 1 s2.0 S0735109719300956 MainDocument9 pages1 s2.0 S0735109719300956 MainAlberto PolimeniNo ratings yet
- Propofol Vs MidazolamDocument8 pagesPropofol Vs MidazolamSergio NNo ratings yet
- Circulationaha.119.039253.PDF J 3Document3 pagesCirculationaha.119.039253.PDF J 3Yuni IndrianiNo ratings yet
- Yi Li Extended Clopidogrel Monotherapy Vs Dapt inDocument9 pagesYi Li Extended Clopidogrel Monotherapy Vs Dapt inCelebfan BoyNo ratings yet
- Tenecteplase For The Treatment of Acute Ischemic Stroke: A Review of Completed and Ongoing Randomized Controlled TrialsDocument8 pagesTenecteplase For The Treatment of Acute Ischemic Stroke: A Review of Completed and Ongoing Randomized Controlled TrialsyoggihermawanNo ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- Pharmacology Before, During and After Percutaneous Coronary InterventionDocument8 pagesPharmacology Before, During and After Percutaneous Coronary InterventionSharan SahotaNo ratings yet
- Pharmacology Before, During and After Percutaneous Coronary InterventioDocument8 pagesPharmacology Before, During and After Percutaneous Coronary InterventiosamuelNo ratings yet
- Tsoumani 2011Document5 pagesTsoumani 2011le.m4rtinezoNo ratings yet
- Acknowledgments: Competency in Medical KnowledgeDocument1 pageAcknowledgments: Competency in Medical KnowledgeTaniaNo ratings yet
- Endovascular Therapy For Ischemic Stroke With Perfusion-Imaging SelectionDocument10 pagesEndovascular Therapy For Ischemic Stroke With Perfusion-Imaging Selectioncitra dewiNo ratings yet
- Antiplatelets in acsDocument11 pagesAntiplatelets in acsrashm4455No ratings yet
- Ticagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Document4 pagesTicagrelor Vs Clopidogrel Clinical Outcomes in Stelevation Myocardial Infarction Patients March 2023 0716017862 7840249Atul DwivediNo ratings yet
- Cortez-Neuroradiology 2020Document10 pagesCortez-Neuroradiology 2020Pedro VillamorNo ratings yet
- AOMS_Art_27239-10Document7 pagesAOMS_Art_27239-10re septian IlhamsyahNo ratings yet
- CURE TrialDocument9 pagesCURE TrialCristina PazmiñoNo ratings yet
- Egred 2016Document1 pageEgred 2016he xuNo ratings yet
- Clinician CornerDocument10 pagesClinician CornerTeten SyahirahNo ratings yet
- Fassbender 2020Document10 pagesFassbender 2020widyadariNo ratings yet
- Hyperlipidemia in Stroke Pathobiology and Therapy: Insights and PerspectivesDocument6 pagesHyperlipidemia in Stroke Pathobiology and Therapy: Insights and Perspectivesputri aprilliaNo ratings yet
- Translation of Experimental Cardioprotective Capability of P2Y12 Inhibitors Into Clinical Outcome in Patients With ST-elevation Myocardial InfarctionDocument15 pagesTranslation of Experimental Cardioprotective Capability of P2Y12 Inhibitors Into Clinical Outcome in Patients With ST-elevation Myocardial InfarctionSol SolNo ratings yet
- Pan 2017Document1 pagePan 2017Arhip CojocNo ratings yet
- Lee 2015 Yonsei Med JDocument8 pagesLee 2015 Yonsei Med JCamilaNo ratings yet
- Variability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseDocument6 pagesVariability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseGono GenieNo ratings yet
- Eficacia Del Clopidogrel en Pacientes Con Fibrilacion Auricular y Sindrome Coronario AgudoDocument7 pagesEficacia Del Clopidogrel en Pacientes Con Fibrilacion Auricular y Sindrome Coronario AgudoElva MonserrathNo ratings yet
- Predictors of Functional Improvement in The Short Term After MitraClip Implantation in Patients With Secondary Mitral RegurgitationDocument16 pagesPredictors of Functional Improvement in The Short Term After MitraClip Implantation in Patients With Secondary Mitral Regurgitationjuajimenez55No ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- 215 FullDocument12 pages215 FullGusti AnisaNo ratings yet
- IndianJPharmacol484355-1876774 051247Document5 pagesIndianJPharmacol484355-1876774 051247Santhoshi Sadhanaa SankarNo ratings yet
- Diagnostics: Cardiac Resynchronization Therapy in Non-Ischemic Cardiomyopathy: Role of Multimodality ImagingDocument15 pagesDiagnostics: Cardiac Resynchronization Therapy in Non-Ischemic Cardiomyopathy: Role of Multimodality Imagingmarsim92No ratings yet
- Auricchio & Cols. (1999)Document6 pagesAuricchio & Cols. (1999)Luba D'AndreaNo ratings yet
- DACAMI TrialDocument6 pagesDACAMI TrialAlberto CardenasNo ratings yet
- Antiplaq y HsaDocument5 pagesAntiplaq y HsaWaldemar PiñaNo ratings yet
- AbstractsDocument2 pagesAbstractsAnisaNo ratings yet
- 1 s2.0 S1936879819304960 MainDocument16 pages1 s2.0 S1936879819304960 MainAlberto PolimeniNo ratings yet
- Ischemic 19Document8 pagesIschemic 19Adina Alexandra CNo ratings yet
- Sigaliptin 2Document8 pagesSigaliptin 2trinda ireneNo ratings yet
- Platelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionDocument9 pagesPlatelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionJanuar RezkyNo ratings yet
- Tpa SilverJubilee 2021 ReviewDocument13 pagesTpa SilverJubilee 2021 ReviewMuhammad Imran MirzaNo ratings yet
- Jaha 117 007288Document4 pagesJaha 117 007288Alberto PolimeniNo ratings yet
- Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!Document6 pagesHeart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!ayesha FalakNo ratings yet
- Cardiology Update 2018 The First QuarterDocument6 pagesCardiology Update 2018 The First QuarterAditya SutarNo ratings yet
- Ictromi 2017 NaomiDocument5 pagesIctromi 2017 NaomiNaomiNDalimuntheNo ratings yet
- Emanuel 2017Document4 pagesEmanuel 2017Kimberly Ann SumbillaNo ratings yet
- Critical Appraisal Meta AnalysisDocument2 pagesCritical Appraisal Meta Analysisk110235015No ratings yet
- High Dose Versus Low Dose Intravenous Nitroglycerine For Sympathetic Crashing Acute Pulmonary EdemaDocument36 pagesHigh Dose Versus Low Dose Intravenous Nitroglycerine For Sympathetic Crashing Acute Pulmonary EdemaNaiara PfbNo ratings yet
- TilemahDocument7 pagesTilemahAndreea TudurachiNo ratings yet
- Dilated CardiomyopathyDocument11 pagesDilated CardiomyopathyPaulaNo ratings yet
- FCVM 09 788503Document7 pagesFCVM 09 788503angiebarNo ratings yet
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Document11 pagesEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazNo ratings yet
- Editorial 2Document4 pagesEditorial 2david1086No ratings yet
- Antithrombotic and Thrombolytic Therapy For Ischemic StrokeDocument21 pagesAntithrombotic and Thrombolytic Therapy For Ischemic StrokeHabibie TifanNo ratings yet
- Cardiac Troponins For The Diagnosis of Acute Myocardial Infarction in Chronic Kidney Disease PDFDocument24 pagesCardiac Troponins For The Diagnosis of Acute Myocardial Infarction in Chronic Kidney Disease PDFDaniel Hernando Rodriguez PeraltaNo ratings yet
- Erp 18 0068Document17 pagesErp 18 0068Jose Ignacio Tarton SisimitNo ratings yet
- Arrhythmia Induction in the EP LabFrom EverandArrhythmia Induction in the EP LabGabriel CismaruNo ratings yet
- University of DundeeDocument10 pagesUniversity of DundeemagreaNo ratings yet
- Baron R, 2008, E Cacy and Safety of Pregabalin in Patients With Diabetic Peripheral Neuropathy or Postherpetic NeuralgiaDocument9 pagesBaron R, 2008, E Cacy and Safety of Pregabalin in Patients With Diabetic Peripheral Neuropathy or Postherpetic NeuralgiamagreaNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument7 pagesRevista Brasileira DE AnestesiologiamagreaNo ratings yet
- Al-Maharbi S, Prevalence of Depression and Its Association With Sociodemographic Factors in Patients With Chronic PainDocument7 pagesAl-Maharbi S, Prevalence of Depression and Its Association With Sociodemographic Factors in Patients With Chronic PainmagreaNo ratings yet
- Bouhassira D, 2008, Prevalence of Chronic Pain With Neuropathic Characteristics in The General PopulationDocument8 pagesBouhassira D, 2008, Prevalence of Chronic Pain With Neuropathic Characteristics in The General PopulationmagreaNo ratings yet
- Comparison of The Neuroprotective Effects and Recovery Profiles of Isoflurane, Sevoflurane and Desflurane As Neurosurgical Pre-ConditioningDocument9 pagesComparison of The Neuroprotective Effects and Recovery Profiles of Isoflurane, Sevoflurane and Desflurane As Neurosurgical Pre-ConditioningmagreaNo ratings yet
- General Anesthesia: Key InformationDocument20 pagesGeneral Anesthesia: Key InformationmagreaNo ratings yet
- The Vertis CV TrialDocument96 pagesThe Vertis CV TrialmagreaNo ratings yet
- Diabetes and Cardiovascular Disease: Inter-Relation of Risk Factors and TreatmentDocument19 pagesDiabetes and Cardiovascular Disease: Inter-Relation of Risk Factors and TreatmentmagreaNo ratings yet
- Interpretation of Cardiovascular Outcome TrialsDocument9 pagesInterpretation of Cardiovascular Outcome TrialsmagreaNo ratings yet
- Cardiovascular Outcome Study of Linagliptin Vs Glimepiride in Type 2 Diabetes - American College of CardiologyDocument3 pagesCardiovascular Outcome Study of Linagliptin Vs Glimepiride in Type 2 Diabetes - American College of CardiologymagreaNo ratings yet
- Cardiovascular Outcomes in Trials of Oral Diabetes MedicationsDocument22 pagesCardiovascular Outcomes in Trials of Oral Diabetes MedicationsmagreaNo ratings yet
- Cardiovascular Disease in Diabetes, Beyond GlucoseDocument27 pagesCardiovascular Disease in Diabetes, Beyond GlucosemagreaNo ratings yet
- Annals of Otology, Rhinology & Laryngology - V..Document4 pagesAnnals of Otology, Rhinology & Laryngology - V..magreaNo ratings yet
- An Old Drug For A New Application Carbazochrome Sodium Sulfonate in HHTDocument2 pagesAn Old Drug For A New Application Carbazochrome Sodium Sulfonate in HHTmagreaNo ratings yet
- OtitisanDocument54 pagesOtitisanmagreaNo ratings yet
- And PerspectivesDocument34 pagesAnd PerspectivesmagreaNo ratings yet
- Medication Adherence in The Real WorldDocument13 pagesMedication Adherence in The Real WorldCognizantNo ratings yet
- Dedicated To Life, Healing & Recovery: Product ListDocument4 pagesDedicated To Life, Healing & Recovery: Product ListsyedsajjadaliNo ratings yet
- Anticoagulants Preoperative InstructionsDocument3 pagesAnticoagulants Preoperative InstructionsDevaki VisvalingamNo ratings yet
- Proton Pump Inhibitors, Adverse Events and Increased Risk of MortalityDocument36 pagesProton Pump Inhibitors, Adverse Events and Increased Risk of MortalityMohammad Mahmudur RahmanNo ratings yet
- ATI Pharm TIPSDocument17 pagesATI Pharm TIPSmike Gee100% (3)
- Management Acute Ischemic Stroke: Rusdi LamsudinDocument121 pagesManagement Acute Ischemic Stroke: Rusdi LamsudinWilliam FrazierNo ratings yet
- Special Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersDocument6 pagesSpecial Care Dentistry Dental Management of Patients With Drug Related Acquired Bleeding DisordersRatri ReswitadewiNo ratings yet
- 01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFDocument26 pages01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFawinsyNo ratings yet
- Drugs Study of Omeprazole, Metoclopramide EtcDocument12 pagesDrugs Study of Omeprazole, Metoclopramide EtcMargaret Cortinas75% (4)
- 4564 2934 p436 Pages Deleted EditedDocument4 pages4564 2934 p436 Pages Deleted EditedHaniNo ratings yet
- Curriculum Vitae: Nama: Prof DR DR Hasan Sjahrir Sps (KDocument11 pagesCurriculum Vitae: Nama: Prof DR DR Hasan Sjahrir Sps (KUKM MargaasihNo ratings yet
- Proton Pump InhibitorDocument10 pagesProton Pump InhibitorFishIngNo ratings yet
- Scientific Discussion: 1/20 EMEA 2004Document20 pagesScientific Discussion: 1/20 EMEA 2004Donny Rahman KhalikNo ratings yet
- Antiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat VaskularDocument23 pagesAntiplatelet, Thrombolitik, Antikoagulan, Vasodilator Referat Vaskularmonyet65No ratings yet
- Duoplavin Epar Public Assessment Report - enDocument37 pagesDuoplavin Epar Public Assessment Report - enyasser ShaterNo ratings yet
- Ischemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractDocument9 pagesIschemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractLina SafitriNo ratings yet
- Clopidogrel Bisulfate (PLOGREL)Document2 pagesClopidogrel Bisulfate (PLOGREL)Kristine Young0% (1)
- Curcumae: Dosen Pengampu: Rohima Robby, S.PD., M.PDDocument14 pagesCurcumae: Dosen Pengampu: Rohima Robby, S.PD., M.PDRezkya HenantoNo ratings yet
- Informed Consent - Filler - RadiesseDocument7 pagesInformed Consent - Filler - RadiesseAshraf AboNo ratings yet
- Drugs Affecting Blood CoagulationDocument51 pagesDrugs Affecting Blood CoagulationMoxie Macado100% (1)
- Pegasus TIMI 54 TrialDocument13 pagesPegasus TIMI 54 TrialIsaac Aaron Enriquez MonsalvoNo ratings yet
- Eur Heart J 2016 Roffi 267 315Document59 pagesEur Heart J 2016 Roffi 267 315Putu Reza Sandhya PratamaNo ratings yet
- Torrent Pharmaceuticals LTDDocument13 pagesTorrent Pharmaceuticals LTDvineminaiNo ratings yet
- Acute Coronary SyndromeDocument59 pagesAcute Coronary SyndromeLouis EkaputraNo ratings yet
- Clopidogrel Bisulfate - PlavixDocument2 pagesClopidogrel Bisulfate - PlavixKristi WrayNo ratings yet
- Fluconazole - Drug InformationDocument21 pagesFluconazole - Drug InformationjjjkkNo ratings yet