Professional Documents
Culture Documents
Care For Critically Ill Patients With COVID-19: Clinical Update
Care For Critically Ill Patients With COVID-19: Clinical Update
Uploaded by
Nicole BatistaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Care For Critically Ill Patients With COVID-19: Clinical Update
Care For Critically Ill Patients With COVID-19: Clinical Update
Uploaded by
Nicole BatistaCopyright:
Available Formats
Clinical Review & Education
JAMA Insights | CLINICAL UPDATE
Care for Critically Ill Patients With COVID-19
Srinivas Murthy, MD, CM, MHSc; Charles D. Gomersall, MBBS; Robert A. Fowler, MD, CM, MSc
Initial reports suggest that COVID-19 is associated with severe dis-
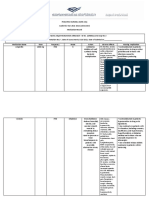
Figure. Summary of Caring for Critically Ill Patients With COVID-19
ease that requires intensive care in approximately 5% of proven
infections.1 Given how common the disease is becoming, as in prior Caring for critically ill patients with COVID-19 is based on the
usual management of viral pneumonia with respiratory failure with additional
majorsevereacuterespiratoryin-
precautions to reduce risk of transmission.
fection outbreaks—SARS (se-
Related article page 1502
vere acute respiratory syn- Usual critical care
drome), MERS (Middle East respiratory syndrome), avian influenza Many patients with severe COVID-19 develop acute respiratory distress
A(H7N9), and influenza A(H1N1)pdm09—critical care will be an inte- syndrome (ARDS). Evidence-based guidelines for ARDS in the context
of COVID-19 include treatments such as
gral component of the global response to this emerging infection. • Conservative intravenous • Lung-protective ventilation strategies
The rapid increase in the number of cases of COVID-19 in Wuhan, fluid strategies • Periodic prone positioning during
• Empirical early antibiotics mechanical ventilation
China, in late 2019 highlighted how quickly health systems can be chal-
for possible bacterial pneumonia • Consideration of extracorporeal
lengedtoprovideadequatecare.1 Case-fatalityproportionswere7-fold • Consideration for early membrane oxygenation
higher for patients in Hubei Province compared with those outside of invasive ventilation
the region, 2.9% vs 0.4%, emphasizing the importance of health sys-
tem capacity in the care of patients who are critically ill with COVID-19.1 Modifications to usual critical care
Thisarticlediscussesissuespertainingtoregionswherecriticalcare • Admission of patients with suspected disease to private rooms when possible
unitshavethecapacitytoprovidemechanicalventilation,acknowledg- • Use of medical face masks for symptomatic patients during assessment
and transfer
ing that this capacity does not exist in many regions and that capacity • Maintain distancing of at least 2 m between patients
could be exceeded in many places. This differential ability to manage • Caution when using high-flow nasal oxygen or noninvasive ventilation
the disease will likely have a substantial influence on patient outcomes. due to risk of dispersion of aerosolized virus in the health care environment
with poorly fitting masks
• Clinicians involved with aerosol-generating procedures should use additional
Factors Associated With Requiring Intensive Care airborne precautions including N95 respirators and eye protection
Appreciatingtypicalclinicalfeaturesanddiseasecoursearecrucialboth
to prepare for increasing numbers of patients and to determine how Facility planning
to best treat infected persons. Patients who have required critical care • Ensure staff have updated training in infection prevention and control
have tended to be older (median age ≈60 years), and 40% have had including personal protective equipment
comorbidconditions,commonlydiabetesandcardiacdisease.2 Children • Planning at local and regional levels for a potential surge in the need
for critical care resources
generally have been observed to experience a milder illness, although
perinatal exposure may be associated with substantial risk. The small COVID-19–specific considerations
numbersofpregnantwomeninfectedthusfarhavehadamildcourse,3
Antiviral or immunomodulatory therapies are not yet proven effective
but limited cases make predictions about disease course uncertain; for treatment of COVID-19. Patients should be asked to participate
however, severe illness in pregnant women was a major concern with in clinical trials of supportive or targeted therapies.
influenza A(H1N1)pdm2009. The median duration between onset of
symptoms and ICU admission has been 9 to 10 days, suggesting a The principal feature of patients with severe disease is the devel-
gradual deterioration in the majority of cases.4 The most documented opment of ARDS: a syndrome characterized by acute onset of hy-
reasonforrequiringintensivecarehasbeenrespiratorysupport,ofwhich poxemic respiratory failure with bilateral infiltrates. Evidence-
two-thirds of patients have met criteria for acute respiratory distress based treatment guidelines for ARDS should be followed, including
syndrome (ARDS).2 conservative fluid strategies for patients without shock following ini-
tial resuscitation, empirical early antibiotics for suspected bacterial
Differentiating From Other Diseases
Given the presence of a number of circulating respiratory viruses, dif- co-infection until a specific diagnosis is made, lung-protective ven-
ferentiating COVID-19 from other pathogens, particularly influenza, is tilation, prone positioning, and consideration of extracorporeal mem-
important and chiefly done using upper (nasopharyngeal) or lower brane oxygenation for refractory hypoxemia.5
(induced sputum, endotracheal aspirates, bronchoalveolar lavage) In settings with limited access to invasive ventilation or prior to pa-
respiratory tract samples for reverse transcriptase–polymerase chain tients developing severe hypoxemic respiratory failure, there may be
reactionandbacterialcultures.Therearesuggestivebutnonspecificra- a role for high-flow nasal oxygen or noninvasive ventilation.6 How-
diographic changes, such as ground-glass opacities on computed ever, the high gas flow of these 2 techniques is less contained than in
tomography.2 Rapidaccesstodiagnostictestingresultsisapublichealth the closed circuitry typical of invasive ventilators, which poses the risk
and clinical priority, allowing for efficient patient triage and implemen- of dispersion of aerosolized virus in the health care environment, such
tation of infection control practices. as in the setting of a poorly fitting face mask. Determining the magni-
tude of this risk, and mitigation strategies, is a crucial knowledge gap.
Clinical Management and Outcomes Septic shock and specific organ dysfunction such as acute kidney
Management of severe COVID-19 is not different from manage- injuryappeartooccurinasignificantproportionofpatientswithCOVID-
ment of most viral pneumonia causing respiratory failure (Figure). 19–related critical illness and are associated with increasing mortality,
jama.com (Reprinted) JAMA April 21, 2020 Volume 323, Number 15 1499
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/21/2020
Clinical Review & Education JAMA Insights
with management recommendations following available evidence- sources. Furthermore, if access to lifesaving interventions such as
based guidelines.7 hospital beds, ventilators, extracorporeal membrane oxygenation,
While no antiviral or immunomodulatory therapies for COVID-19 or renal replacement therapy is likely to be strained, clear resource
have yet proven effective, a majority of severely ill patients described allocation policies should be determined by clinicians, policy mak-
to date have received numerous potentially targeted therapies— ers, the general public, and ethicists. These active preparation mea-
most commonly neuraminidase inhibitors and corticosteroids— sures can be organized well before large numbers of infected pa-
and a minority of patients have been enrolled in clinical trials. tients require hospital preparation.
While mortality among all infected patients may be in the range
of 0.5% to 4%,1 among patients who require hospitalization, mor- Major Knowledge Gaps
tality may be approximately 5% to 15%, and for those who become COVID-19 is a novel disease with an incompletely described clinical
critically ill, there is currently a wide mortality range, from 22% to course, especially for children and vulnerable populations. Risk fac-
62% in the early Hubei Province case series.2,4 The exact cause of tors for severe illness remain uncertain (although older age and co-
death is unclear at this point, with progressive hypoxia and multi- morbidity have emerged as likely important factors), the safety of
organ dysfunction being the presumed causes. Case-fatality pro- supportive care strategies such as oxygen by high-flow nasal can-
portions, both among all COVID-19 patients and among severely ill nula and noninvasive ventilation are unclear, and the risk of mortal-
patients, will likely become more precise and generalizable with in- ity, even among critically ill patients, is uncertain. There are no proven
creased surveillance to better clarify the number of individuals in- effective specific treatment strategies, and the risk-benefit ratio for
fected and as greater numbers of infections occur around the globe. commonly used treatments such as corticosteroids is unclear.
It is essential to learn as much as possible through observational
Protecting Patients and Health Care Workers studiesandclinicaltrialsacrossabreadthofpatientpopulationsandcare
Reducing the risk of nosocomial outbreak amplification through trans- settings. These should incorporate clear measurements of severity of
mission of virus to other patients and health care workers is of critical criticalillnesssothatoutcomescanberiskadjusted,andusesufficiently
importance.Maintainingappropriatedistancingofatleast2mbetween common outcome measures to combine data and validly compare ob-
patients with suspected or confirmed to have COVID-19, consideration servations across regions.8 Ideally, clinical trials should be structured to
of use of medical masks for symptomatic patients, and, ideally, admis- promote maximum learning from around the world, such as through
sion of patients with suspected disease to private rooms are important the use of master protocols or adaptive platform designs.9,10
considerations.Ensuringhospitalstaffarewelltrainedinstandard,con-
tact, and droplet infection prevention and control precautions, includ- Conclusions
ingtheuseofrelevantpersonalprotectiveequipment,isanimperative. In a very short period, health care systems and society have been
Clinicians involved with aerosol-generating procedures such as endo- severely challenged by yet another emerging virus. Preventing trans-
tracheal intubation and diagnostic testing using bronchoscopy should mission and slowing the rate of new infections are the primary goals;
additionally use airborne precautions, including N95 respirators or however, the concern of COVID-19 causing critical illness and death
equivalent face masks and face shields or goggles for eye protection. is at the core of public anxiety. The critical care community has enor-
mous experience in treating severe acute respiratory infections ev-
Surge Preparation ery year, often from uncertain causes. The foundation for care of se-
If increasing numbers of patients with COVID-19 develop severe ill- verely ill patients with COVID-19 must be grounded in this evidence
ness, plans should be made at local and regional levels for how to base and, in parallel, ensure that learning from each patient is maxi-
best manage the potential surge in the need for critical care re- mized to help those who will follow.
ARTICLE INFORMATION REFERENCES tilation in adult patients with acute respiratory
Author Affiliations: University of British Columbia, 1. Wu Z, McGoogan JM. Characteristics of and distress syndrome. Am J Respir Crit Care Med. 2017;
Vancouver, British Columbia, Canada (Murthy); important lessons from the coronavirus disease 2019 195(9):1253-1263.
Chinese University of Hong Kong, Hong Kong (COVID-19) outbreak in China. JAMA. Published online 6. Alraddadi BM, Qushmaq I, Al-Hameed FM, et al.
(Gomersall); Sunnybrook Hospital, University of February 24, 2020. doi:10.1001/jama.2020.2648 Noninvasive ventilation in critically ill patients with
Toronto, Toronto, Ontario, Canada (Fowler). the Middle East respiratory syndrome. Influenza
2. Wang D, Hu B, Hu C, et al. Clinical characteristics
Corresponding Author: Srinivas Murthy, MD, CM, Other Respir Viruses. 2019;13(4):382-390.
of 138 hospitalized patients with 2019 novel
MHSc, University of British Columbia, 4500 Oak St, 7. De Backer D, Dorman T. Surviving Sepsis
coronavirus-infected pneumonia in Wuhan, China.
Vancouver, BC V6H 3V4, Canada (srinivas.murthy@ Guidelines: a continuous move toward better care
JAMA. Published online February 7, 2020. doi:10.
cw.bc.ca). of patients with sepsis. JAMA. 2017;317(8):807-808.
1001/jama.2020.1585
8. COVID-19 case record form. Accessed March 2,
Published Online: March 11, 2020. 3. Chen H, Guo J, Wang C, et al. Clinical
2020. https://isaric.tghn.org/novel-coronavirus/
doi:10.1001/jama.2020.3633 characteristics and intrauterine vertical
9. World Health Organization. Master Protocol:
Conflict of Interest Disclosures: Dr Gomersall transmission potential of COVID-19 infection in nine
A Multi-center, Adaptive, Randomized Controlled
reported that his department has received funding pregnant women. Lancet. Published online February
Trial of the Safety and Efficacy of Investigational
to develop educational material from Getinge, 12, 2020. doi:10.1016/S0140-6736(20)30360-3
Therapeutics for the Treatment of COVID-19 in
Draeger Medical, Hamilton Medical, and Fisher & 4. Yang X, Yu Y, Xu J, et al. Clinical course and Hospitalized Patients. Published February 24, 2020.
Paykel. No other disclosures were reported. outcomes of critically ill patients with SARS-CoV-2 Accessed March 2, 2020. https://www.who.int/
pneumonia in Wuhan, China. Lancet Respir Med. blueprint/priority-diseases/key-action/novel-
Additional Contributions: We thank the
2020;S2213-2600(20)30079-5. coronavirus/en/
International Forum of Acute Care Trialists (InFACT)
for assistance. 5. Fan E, Del Sorbo L, Goligher EC, et al. An official 10. REMAP-CAP: A Randomized, Embedded,
American Thoracic Society/European Society of Multifactorial, Adaptive Platform Trial for
Intensive Care Medicine/Society of Critical Care Community-Acquired Pneumonia. Accessed March
Medicine clinical practice guideline: mechanical ven- 3, 2020. http://www.remapcap.org
1500 JAMA April 21, 2020 Volume 323, Number 15 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/21/2020
You might also like
- Cardiac Arrest QuestionsDocument2 pagesCardiac Arrest Questionsmine251580% (5)
- Jama Murthy 2020 It 200008Document2 pagesJama Murthy 2020 It 200008jorgeNo ratings yet
- Mja2 50598Document10 pagesMja2 50598Andi Astrid AmaliaNo ratings yet
- Consensus Statement: Safe Airway Society Principles of Airway Management and Tracheal Intubation Specific To The COVID-19 Adult Patient GroupDocument10 pagesConsensus Statement: Safe Airway Society Principles of Airway Management and Tracheal Intubation Specific To The COVID-19 Adult Patient GroupMeska AmeliaNo ratings yet
- Severe Covid-19: Clinical PracticeDocument10 pagesSevere Covid-19: Clinical Practicemarcelocarvalhoteacher2373No ratings yet
- Rizal JournalDocument2 pagesRizal Journallindzy.amurao01No ratings yet
- Supporting The Health Care Workforce During The COVID-19 Global EpidemicDocument2 pagesSupporting The Health Care Workforce During The COVID-19 Global EpidemicDema AlsouqiNo ratings yet
- Clinical PracticeDocument10 pagesClinical PracticeCarlos AlvarezNo ratings yet
- Severe Covid-19Document10 pagesSevere Covid-19Gabriela ArvelaezNo ratings yet
- NEJM Severe COVIDDocument10 pagesNEJM Severe COVIDErick Roa GandicaNo ratings yet
- Severe Covid-19: Clinical PracticeDocument10 pagesSevere Covid-19: Clinical PracticejoelNo ratings yet
- HCQ Study JamaDocument7 pagesHCQ Study Jamathe kingfishNo ratings yet
- Reabilitação Após Doença Crítica de CovidDocument5 pagesReabilitação Após Doença Crítica de CovidCristina BoaventuraNo ratings yet
- 6MINUTEWALKTESTABERTODocument5 pages6MINUTEWALKTESTABERTOpv7j8j6q5rNo ratings yet
- Novel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited SettingsDocument8 pagesNovel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited Settingsdiah Bayu siswantiNo ratings yet
- 2389-Article Text-9837-6-10-20211201Document9 pages2389-Article Text-9837-6-10-20211201Sumendhe Hayuning SukmaraniNo ratings yet
- Covid 19 Hospital AcquiredDocument2 pagesCovid 19 Hospital AcquiredeliassssssNo ratings yet
- The Journal For Nurse PractitionersDocument5 pagesThe Journal For Nurse Practitionersagstri lestariNo ratings yet
- High Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019Document9 pagesHigh Incidence of Barotrauma in Patients With Severe Coronavirus Disease 2019AMBUJ KUMAR SONINo ratings yet
- Respiratory Support For Adult Patients With COVID-19Document7 pagesRespiratory Support For Adult Patients With COVID-19SekarNo ratings yet
- Evolution of Acute Respiratory Distress Syndrome IDocument14 pagesEvolution of Acute Respiratory Distress Syndrome InalgatronNo ratings yet
- Pneumonia and VAP PreventionDocument35 pagesPneumonia and VAP Preventionhendro harahapNo ratings yet
- Invasive and Non-Invasive Ventilation in Patients With COVID-19Document6 pagesInvasive and Non-Invasive Ventilation in Patients With COVID-19Augusto ManoelNo ratings yet
- Who 2019 Ncov Ipc Ppe Use 2020.3 EngDocument28 pagesWho 2019 Ncov Ipc Ppe Use 2020.3 EngKumanan1304No ratings yet
- Tx. COVID 19 en UCIDocument6 pagesTx. COVID 19 en UCIVictor Augusto Ávila HernándezNo ratings yet
- 1 s2.0 S0025712522000955 MainDocument12 pages1 s2.0 S0025712522000955 MainMonika Diaz KristyanindaNo ratings yet
- COVID-19: A Quick Look at Aspects of Critical CareDocument5 pagesCOVID-19: A Quick Look at Aspects of Critical CareJbarrianNo ratings yet
- Pi Is 0025619620311873Document5 pagesPi Is 0025619620311873Achmad RyandaNo ratings yet
- Dr. Hendri - Early Warning System & PPEDocument106 pagesDr. Hendri - Early Warning System & PPEViniFortunataNo ratings yet
- CCJM 87a ccc033 FullDocument4 pagesCCJM 87a ccc033 FullKamar Operasi Hermina BogorNo ratings yet
- 394 Full PDFDocument20 pages394 Full PDFHaltiNo ratings yet
- COVID-19 Disease Invasive VentilationDocument8 pagesCOVID-19 Disease Invasive VentilationfikriafisNo ratings yet
- Jamaotolaryngology Givi 2020 SC 200001Document6 pagesJamaotolaryngology Givi 2020 SC 200001dina ayu SeptianiNo ratings yet
- 10 1111@anae 15054 PDFDocument33 pages10 1111@anae 15054 PDFJuliana Rodriguez MariñoNo ratings yet
- Global Guidance For Surgical Care During The COVID-19 PandemicDocument7 pagesGlobal Guidance For Surgical Care During The COVID-19 PandemicSergio Losada AmayaNo ratings yet
- Recommendations For Prehospital Airway Management in Patients With Suspected COVID-19 InfectionDocument5 pagesRecommendations For Prehospital Airway Management in Patients With Suspected COVID-19 InfectionConnor StephensonNo ratings yet
- Internal Medicine Journal - 2009 - Ferguson - Preventing Healthcare Associated Infection Risks Healthcare Systems andDocument8 pagesInternal Medicine Journal - 2009 - Ferguson - Preventing Healthcare Associated Infection Risks Healthcare Systems andHamid ShahNo ratings yet
- Neurologic Emergencies During The Coronavirus DiseDocument17 pagesNeurologic Emergencies During The Coronavirus DiseCristina CalzadaNo ratings yet
- Final Seminar Manuscript Group 5 To PrintDocument30 pagesFinal Seminar Manuscript Group 5 To PrintGuenevere DamasinNo ratings yet
- How COVID-19 Has Changed The Management of Glomerular DiseasesDocument4 pagesHow COVID-19 Has Changed The Management of Glomerular DiseasesLouie MercadoNo ratings yet
- BMJ 2021 065871.fullDocument24 pagesBMJ 2021 065871.fullEfen YtNo ratings yet
- How COVID-19 Has Changed The Management of Glomerular DiseasesDocument4 pagesHow COVID-19 Has Changed The Management of Glomerular DiseasesHendri WahyudiNo ratings yet
- Covid 19 ProgramDocument12 pagesCovid 19 ProgramBAGUIO CATSNo ratings yet
- Novel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited SettingsDocument9 pagesNovel Coronavirus 2019 (2019-Ncov) Infection: Part Ii - Respiratory Support in The Pediatric Intensive Care Unit in Resource-Limited SettingsHanni HarahapNo ratings yet
- Recognition and Prevention of Nosocomial Pneumonia in The ICU and Infection Control in Mechanical VentilationDocument11 pagesRecognition and Prevention of Nosocomial Pneumonia in The ICU and Infection Control in Mechanical Ventilationandres felipe burgos granadosNo ratings yet
- Nac 2017Document18 pagesNac 2017Nataly CortesNo ratings yet
- The Central Role of Clinical Nutrition in COVID-19 Patients During and After Hospitalization in Intensive Care UnitDocument5 pagesThe Central Role of Clinical Nutrition in COVID-19 Patients During and After Hospitalization in Intensive Care UnitReaz MorshedNo ratings yet
- COVID en ObstetriciaDocument9 pagesCOVID en Obstetriciaantonio123valenciaNo ratings yet
- Guias JamaDocument2 pagesGuias JamaEliana TorresNo ratings yet
- The Interplay Between Coagulation and Inflammation Pathways in COVID-19-Associated Respiratory Failure: A Narrative ReviewDocument17 pagesThe Interplay Between Coagulation and Inflammation Pathways in COVID-19-Associated Respiratory Failure: A Narrative ReviewAlanNo ratings yet
- High Flow Nasal Cannula For Acute Respiratory Distress Syndrome Due To Covid 19Document5 pagesHigh Flow Nasal Cannula For Acute Respiratory Distress Syndrome Due To Covid 19Cesar C SNo ratings yet
- De Pascale 2012Document9 pagesDe Pascale 2012HellcroZNo ratings yet
- Healthcare Associated Pneumonia - Dr. Christian A. Johannes, SP - an.KICDocument30 pagesHealthcare Associated Pneumonia - Dr. Christian A. Johannes, SP - an.KICvenyNo ratings yet
- Jurding KLP A Anes 3Document18 pagesJurding KLP A Anes 3mreza26No ratings yet
- Pi Is 0099176720304220Document10 pagesPi Is 0099176720304220yasintameganabilaNo ratings yet
- 30794136: Aspiration Pneumonia in Older AdultsDocument7 pages30794136: Aspiration Pneumonia in Older AdultsNilson Morales CordobaNo ratings yet
- Nos InfecDocument6 pagesNos InfecMimi ElagoriNo ratings yet
- PIIS0003999320302951Document3 pagesPIIS0003999320302951Adiel CarrascoNo ratings yet
- 7.qiu2020 Article IntensiveCareDuringTheCoronaviDocument3 pages7.qiu2020 Article IntensiveCareDuringTheCoronaviM. TERESA TORNEL MARINNo ratings yet
- Whooping Cough Unveiled: From Pathogenesis to Promising TherapiesFrom EverandWhooping Cough Unveiled: From Pathogenesis to Promising TherapiesNo ratings yet
- 21 AdisaDocument6 pages21 AdisaTri UtariNo ratings yet
- Medication Sheet 2021-2022Document3 pagesMedication Sheet 2021-2022Attekah MohammedNo ratings yet
- Blood GroupsDocument5 pagesBlood GroupsMalik IrfanNo ratings yet
- ICD-10 CM All Diagnosis and Trigger Codes - Revised 9-17-2015Document6,507 pagesICD-10 CM All Diagnosis and Trigger Codes - Revised 9-17-2015Puskesmas MakaleNo ratings yet
- Appendix 4 - Example Birth HistoryDocument2 pagesAppendix 4 - Example Birth HistorySriMathi Kasi Malini ArmugamNo ratings yet
- Neurologist Doctor Near MeDocument2 pagesNeurologist Doctor Near MesnaayuNo ratings yet
- Final Course in The WardDocument4 pagesFinal Course in The WardMichael Boado100% (1)
- Ccare Pro Les Waye FeatureDocument10 pagesCcare Pro Les Waye Featureapi-604638740No ratings yet
- Oxygenation Problem Notes and Nursing InterventionsDocument7 pagesOxygenation Problem Notes and Nursing InterventionsAnna TaylorNo ratings yet
- Book-Based: Pathophysiology of Allergic RhinitisDocument2 pagesBook-Based: Pathophysiology of Allergic RhinitisJeraldine Corpuz PascualNo ratings yet
- APC-Associated Polyposis Conditions - GeneReviews® - NCBI BookshelfDocument38 pagesAPC-Associated Polyposis Conditions - GeneReviews® - NCBI BookshelfKostantinos EmmNo ratings yet
- Health CertificateDocument3 pagesHealth CertificateĐĂNG TRỊNH HẢINo ratings yet
- Compendium Dermatologie RomanaDocument207 pagesCompendium Dermatologie RomanaRusu Bianca Elena67% (3)
- 03 Muscle and Neuromuscular Junction Disorders PDFDocument325 pages03 Muscle and Neuromuscular Junction Disorders PDFOTTO JESUS VEGA VEGA100% (2)
- AIDS Is Real and It's in Our Church: HIV/AIDS and The Church in AfricaDocument327 pagesAIDS Is Real and It's in Our Church: HIV/AIDS and The Church in AfricaMike BlythNo ratings yet
- MCQs PulmonologyDocument2 pagesMCQs PulmonologySadia Batool86% (7)
- Children: Asthma's Impact On The NationDocument4 pagesChildren: Asthma's Impact On The NationNycoNo ratings yet
- Dr. Rasul Dr. Orencia: Surgery ER Orthopedics Ward OR ENT OPD Ophthalmology ClerkDocument12 pagesDr. Rasul Dr. Orencia: Surgery ER Orthopedics Ward OR ENT OPD Ophthalmology ClerkApmc Schwartz100% (1)
- Medsurg AdhdDocument3 pagesMedsurg AdhdminniprkNo ratings yet
- Tuberculosis of The Spine An OverviewDocument6 pagesTuberculosis of The Spine An OverviewSattvik SpineNo ratings yet
- 1.who Shall Be Considered As Having Community-Acquired Pneumonia?Document6 pages1.who Shall Be Considered As Having Community-Acquired Pneumonia?Kristine Jade OdtujanNo ratings yet
- Disorders of Speech & EmotionDocument10 pagesDisorders of Speech & EmotionBoris ThingbaijamNo ratings yet
- Stress Hyperglycemia: Anand MosesDocument4 pagesStress Hyperglycemia: Anand MosesDaeng Arya01No ratings yet
- Pediatric Traumatic Brain Injury: Characteristic Features, Diagnosis, and ManagementDocument12 pagesPediatric Traumatic Brain Injury: Characteristic Features, Diagnosis, and ManagementsylvetriNo ratings yet
- Intrathecal Injection (LP) ENGDocument1 pageIntrathecal Injection (LP) ENGAlina RadescuNo ratings yet
- (Impetigo) : Erbil Polythecnic University Soran Technical Insititute Nuraing Department First StageDocument14 pages(Impetigo) : Erbil Polythecnic University Soran Technical Insititute Nuraing Department First StageKubra ĖdrisNo ratings yet
- NSTP 2 Midterm ReviewerDocument6 pagesNSTP 2 Midterm ReviewerTrexy NorialNo ratings yet
- Fluids and Electrolytes IV FluidsDocument1 pageFluids and Electrolytes IV Fluidsnursing concept mapsNo ratings yet
- Thyroid DiseaseDocument17 pagesThyroid DiseaseCharlz ZipaganNo ratings yet