Professional Documents
Culture Documents
Annotated Albertcasemapping
Annotated Albertcasemapping
Uploaded by
api-518475553Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Annotated Albertcasemapping
Annotated Albertcasemapping
Uploaded by
api-518475553Copyright:
Available Formats
Student
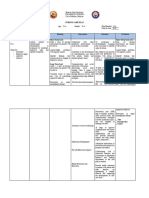
Name: Miranda Anderson Case: 7 Albert Date: 4/13/2020
1. Diagnosis, Referral, Setting, Reimbursement, LOS
Albert is an 18-year-old male diagnosed with schizophrenia/early psychosis.
He is being seen by an occupational therapist 2x/wk for 6 weeks in an early psychosis program that
he was referred to by a psychiatrist. Services are paid through ear-marked funding by the state
legislature for early psychosis programs.
2. Pragmatic Factors to Consider
-The scheduling of the program he is in and the limited amount of session may impact when I can
and can’t see him so I will need to be sure to work with the team to insure we all get our fair amount
of time spent with him without overlapping. If we do have to overlap, then the team needs to work
together to make sure all our goals are being addressed.
-Schizophrenia symptoms are widely variable so I need to be able to think on my feet and be trying
to make sure that my approach for therapy each day is going to work for whatever state Albert might
be in.
-I would still want his parents to be involved so I should make sure that I am somehow able to still
communicate with them and have them attend some of the sessions if possible.
- I need to research into the funding by the state legislature to ensure I write goals that are
appropriate for this type of funding.
5. Diagnosis and 6. Scientific Reasoning & Evidence
Expected Course List the barriers to performance typical of this diagnosis:
Schizophrenia is a -Being able to cope with both the positive and negative symptoms are
complex disorder. There things to address in therapy. These things may never completely go away,
are studies that provide even with medication, so learning to manage them is important.
evidence of a genetic -In the case of this client, making sure he is managing his medication
contribution to the properly is important. Medications for schizophrenia can also have
disorder. There is also varying side effects so understanding these can be important.
evidence to support that -cognition is often impaired and with this client we know he is at a 5.2
events affecting fetal Allen cognitive level. Because of this, we know that he has the ability to
development are related live on his own but there are still a lot of supports that need to be put into
to the diagnosis. To be place in order for this to work successfully. This can include but is not
diagnosed, an individual limit to weekly check-ins; creating a structured schedule for him to follow
must have at least two of to ensure things like daily grooming and hygiene, meals, and cleaning are
the following symptoms taking place; and setting up his environment to better ensure safety such
for at least 1 month: as visual cues for turning off the stove top or making sure he puts his
-delusions perishable foods away in the refrigerator after using them.
-hallucinations -Often times social skills or desire to be socially involved can be
-disorganized speech impacted. These are things to address in therapy.
-disorganized or -Because schizophrenia is very complex and often times difficult to
catatonic behavior understand, it would be good to educate and provide resources for both
-negative symptoms the client and family about the diagnosis and the best way to help the
The symptoms of client while also attempting to reduce stress. This can also include linking
schizophrenia are them up with support groups.
Page 1 of 10 Revised 1/9/17
classified as being
positive or negative.
Positive symptoms are
symptoms not typically
present in others such as
delusions, hallucinations
and disorganized speech
and behavior. Negative
symptoms are considered
the absence of typical
function such as flat
affect and social
withdrawal.
Symptoms vary widely
between people with
schizophrenia. Some
people experience
improvement in
symptoms over time
while others get worse.
Some individuals with
schizophrenia have
significant cognitive
impairments and others
do not.
(Brown and Stoffel book)
7. Practice Models Guiding Assessment and Rationale
Treatment
1. PEO Because Albert would like to do more things
independently, taking advantage of being able to
set up his environment to foster greater
independence would be very beneficial. For
example, we know that albert functions at a 5.2
Allen cognitive level (person), and he wants to
be able to use the light rail system (occupation),
so we can easily implement a schedule with
alarms in his phone (environment) so that he
takes the exact same route every day and has
reminders to get there on time and making the
correct transfers. His environment can be
manipulated in other areas of his life as well to
increase occupational performance such as
eliminating distractions when trying to complete
school work.
Page 2 of 10 Revised 1/9/17
2. Recovery Model The recovery model is one that is relevant for
people with schizophrenia. It focuses on the idea
that function is not necessarily an absence of
symptoms but instead being able to live with and
manage those symptoms. This is very pertinent
for Albert because we can assume that even on
medication, the likelihood of all of his
symptoms going away is very low. This model
also supports the use of a wellness recovery and
action plan which would be useful to implement
with Albert which can provide him with an
easily accessible tool box of skills and strategies
to use for maintaining his symptoms and also a
plan if things get out of control.
3. Allen’s cognitive disabilities frame of Because we know that Alberts cognition has
reference been impacted, I think that the Allen’s cognitive
disabilities frame of reference would be
beneficial. This would focus on helping families
to understand the cognitive function of their
loved one as well as help the client and family to
understand how their cognition is impacting
their occupations. It also focuses on using the
Allen cognitive levels to guide the therapy
process in terms of what the client can do, what
the client will do, and what the client may be
able to do in the future given this information.
Page 3 of 10 Revised 1/9/17
14. Evaluation: What Assessment tools and other means of assessment will you use?
Top Down Assessment: Prioritize one Occupation to observe the client perform
Observed Occupation Rationale/How will you use this information
Filling out/planning a week in a planner. The reason I would want to have Albert
Depending on how much he currently had going complete this task is because it would allow me
on that week I would either want to use his actual to see things like his reasoning, planning, and
schedule or I would supply him with a list of attention skills as well as if any of this triggers
hypothetical plans to organize and have things the voices in his head and what he is doing to
that would overlap or not get done on time if he cope with them. I would instruct him to walk me
didn’t schedule them correctly. through what he is thinking and feeling as we go
so I can better understand his thought process
and coping skills. This task is also relevant to his
life because he is a student and has difficulties
focusing while doing homework or while in
class. I would ask him to complete this task in a
place that he might typically do his homework.
This will allow me to better understand his
environment as well as begin thinking about
what parts of his environment are hindering his
performance and what aspects are helping.
Method/Tool Rationale/What is being Assessed
1. PASS meal prep CIADL Albert is at the age that he is probably starting to
make some meals for himself and having greater
independence is one of his goals. I think this
would be a great test of cognition while looking
at things like safety and judgement. This kind of
task will also require attention which we know
he struggles with so it will allow me to better
assess that.
2. Life Skills Profile This was developed to measure function and
disability in people with schizophrenia. It has 5
subscales including self-care, nonturbulence,
social contact, communication, and
responsibility. I think all of these areas are
appropriate to look at for Albert especially
considering his age and goals.
3. Action over Inertia Assessment. This assessment includes filling out worksheets
that such as a daily time-use log and evaluation
of current activity patterns. This may help to
guide therapy to see what his current activity
patterns are and his perspective on whether or
not they are beneficial or hindering.
Page 4 of 10 Revised 1/9/17
4. Social Profile We know that one of the symptoms of
schizophrenia can be social withdrawal. Albert
has a goal of making more friends at the
community college so gaining a better
understanding of his current social interactions
will help me to work on this goal at a level that
is appropriate for Albert.
5. Volitional Questionnaire while completing the I think this would be another appropriate
observed occupation of filling out the planner. assessment to use with Albert because it would
give me more insight into his volitional
behaviors rather than just focusing on the
environmental supports needed. This is intended
to be used when looking at someone’s work
skills so administering it while he is doing a task
such as using a planner would be beneficial.
6.
15. CPT Evaluation Code: Justification
Moderate complexity The client’s condition and medical history is moderately complex due to
97166 the amount many different signs, symptoms and medications involved.
We also know that there are at least 5 occupations in his life that
impacted by the symptoms involved with his diagnosis.
17. Resources and Team Members
Page 5 of 10 Revised 1/9/17
-Psychiatrist. We know that he already has a psychiatrist but it would be important to continue
working with them and make sure that Albert continues to be seen by them.
-Alberts parents are going to be an important part of the team. I can help show them the best way to
assist Albert while still letting him practice his independence.
-I would be interested in getting Alberts professor at the community college involved just so he can
be informed and also better understand when Albert advocates for learning needs.
- Center for disability services at the community college. This would be beneficial to gain more
information on the resources available to help Albert do well in his classes.
-Wellness and recovery action plan. I would want to provide Albert with a binder and organized
worksheets for creating a WRAP.
18. Intervention Plan
Barriers Supports
-Depending on the side-effects of the medications that Albert - He is on antipsychotic
is taking, this may be a barrier. medications that are working
-Because schizophrenia can constantly be changing in the well to decrease his
way that it presents, his symptoms can hinder or benefit our psychotic symptoms.
therapy sessions on any given day. - We are in a setting that we
-The scheduling of the program he is in may prove to be a are able to easily address the
barrier if he is seeing multiple disciplines in one day. This things he wants to work on
may cause addition exacerbation of symptoms or could both in the clinic and out in
negatively affect his ability to focus during occupational the community.
therapy. - He is at a cognitive level that
-Because Albert wants to be more independent, he may not be he does have the ability to
receptive to having his parents involved in the therapy live alone, he would just
process. need someone to do weekly
check-ins.
- It sounds like his parents are
pretty supportive
- He has very realistic and
achievable goals for himself.
- Albert has several interests
that can be used in therapy.
Goals Approach and deficit(s) for each goal
1. LTG: Approach:
In 6 weeks, Albert will independently utilize a wellness Prevent
recovery and action plan (WRAP) when in a situation that Establish
exacerbates his symptoms. Deficit:
Inability to manage schizophrenia
symptoms
1a.STG: Approach:
In 2 weeks, Albert will independently identify 3 triggers that Prevent
exacerbate his symptoms during his daily routine.
Deficit:
Inability to manage schizophrenia
symptoms
Page 6 of 10 Revised 1/9/17
1b.STG: Approach:
In 4 weeks, Albert will independently implement a daily Prevent
maintenance list for decreasing psychotic symptoms. Establish
Deficit:
Inability to manage schizophrenia
symptoms
2. LTG: Approach:
In 6 weeks, Albert will independently maintain focus on Establish
school related activities for 30 minutes with the use of Modify
compensatory strategies. Deficit:
Decreased attention
2a. STG: Approach:
In 2 weeks, Albert will independently identify and implement Modify
2 strategies for decreasing environmental distractions while Deficit:
studying. Decreased attention
2b. STG: Approach:
In 4 weeks, Albert will independently advocate for learning Establish
needs while in the classroom Deficit:
Decreased attention
3. LTG: Approach:
In 6 weeks, Albert will independently use public transit for Establish
commuting in order to attend school and social events. Deficit:
Difficulties with new learning and
coping with new situations.
3a.STG: Approach:
In 2 weeks, with minimal verbal cues, Albert will plan a trip Establish
on public transit with no more than 2 transfers to commute to Deficit:
his community college Difficulties with new learning and
coping with new situations.
3b. STG: Approach:
In 4 weeks, Albert will independently implement 2 calming Prevent
strategies when on a crowded bus. Deficit:
Difficulties with new learning and
coping with new situations.
Page 7 of 10 Revised 1/9/17
19. Treatment Sessions: Plan for first two 45 minute treatment sessions:
Page 8 of 10 Revised 1/9/17
1. What will you do? Identify Practice Based on which goal(s)?
I would want to start of this first session by working with Model Public transit
Albert to better understand his psychosis, potential triggers, Recovery WRAP
and what he currently does to cope. One of his goals is to be Allen’s Focusing
able to better cope with his symptoms and I think this will PEO
increase is occupational performance in several domains. We
could start by beginning to create a WRAP. The first step
would be to create a “wellness toolbox.” This would be a
beneficial session to have his parents attend if possible so that
we can all strategize this plan together. I would want him to
write down three strategies that have worked for him in the past
that help him to relieve troubling symptoms. Together, we
would come up with 3 additional strategies that he has not tried
and write them down. If he has a smart phone I would want
him to put these notes in his phone for easy access. Because he
stated that he experiences symptoms even when just
completing daily routines, I would expect that he may
experience symptoms no matter what we choose to do in
therapy. This would give him a great opportunity to practice
using his list. Any time throughout therapy that he started
experiencing hindering symptoms, I would prompt him to
choose a tool of his choice and take 1-2 minutes to implement
it. This would also give us the opportunity to reflect on what
did work or what didn’t work and adjust accordingly.
For the next part of this session I would want to have him plan
a trip to the community college and back to the clinic. This will
give him a chance to practice using schedules to help him
organize his day and exercise his independence. We again can
utilize his phone for planning and setting alarms. I would
introduce him to his local public transit website (if not
available I would provide him with a paper copy) and teach
him how to access the light rail and bus schedules. I would
teach him how to plan backwards by starting with the time he
wants to arrive somewhere and then finding the corresponding
bus times to figure out what time he would need to be at the
bus stop. Once we figured out the correct times, I would ask
him to schedule this trip in his phone for the following session
as well as set an alarm to ensure he will get to the bus stop on
time.
In the case that he does not have a phone, I would try using a
daily planner along with some sort of alarm system like on a
wrist watch.
During the scheduling task, this would be a great opportunity
for me to observe his attention span and identify what his
distractors are. I would be keeping this information in mind to
work on in a future session. However, there are some things I
would want him to implement during this session because
learning new information can be very difficult especially for
someone at a 5.2 level. We would practice being able to take
Page 9 of 10 Revised 1/9/17
breaks, move slowly, and go over the steps more than once.
2. What will you do? Identify Practice Based on which goal(s)?
Model
For this session, I would want to actually take the trip to the Recovery Public transit
community college that we had planned. I would begin by PEO WRAP
asking him if he remembered where we were going, why we
were going there and what time we needed to leave. If he
remembered where in his phone (or daily planner) to check for
this information then I would know that the system we set in
place was a good fit for him. If not, we would again work on
strategizing the best ways to store this information to make it
easy for him to access.
Next, we would take the public transit system as planned to get
to the community college. While traveling, we can strategize
what to do if he were to miss a bus, such as calling his parents,
choosing to always take an earlier bus so he can wait for the
next bus when running late, or have a backup route that he
could take (i.e light rail vs bus). This would also be a great
opportunity for him to continue working on his wellness plan.
Buses can often times be crowded so he may begin feeling
symptoms related to this. We can identify what those triggers
are and what action plans he needs to have in place to 1 prevent
exacerbated symptoms and 2 what to do if those symptoms
start to escalate.
Once we arrived at the college, I would explain that sometimes
going to a location before the day of an appointment or event
can help to alleviate stress and may decrease symptoms. We
could find his classroom by utilizing the school directory and
locate any other essential places he may need to go such as the
bathroom, disability center, or café. I could show him how to
organize any essential information in his phone such as the
classroom number or simple directions. We would then be
reminded by the alarm he set that we need to get back to the
bus stop to make it back to the clinic. Again, we could practice
coping strategies on the bus ride back.
Page 10 of 10 Revised 1/9/17
You might also like
- Sample of Intake Interview For CBTDocument11 pagesSample of Intake Interview For CBTalessarpon7557100% (3)
- PDSQ ForPatientsDocument9 pagesPDSQ ForPatientsCristina SelNo ratings yet
- M AdbbDocument10 pagesM AdbbAna PaulaNo ratings yet
- Motivation and Reinforcement - The Verbal Behavior Approach To ABA Autism Intervention PDFDocument5 pagesMotivation and Reinforcement - The Verbal Behavior Approach To ABA Autism Intervention PDFfonokariNo ratings yet
- Patterns of The Hypnotic Techniques of M PDFDocument237 pagesPatterns of The Hypnotic Techniques of M PDFjeanotte100% (2)
- Summary - Frogs Into PrincesDocument5 pagesSummary - Frogs Into PrincesMartinNo ratings yet
- Family Life Education PhilosophyDocument3 pagesFamily Life Education Philosophyapi-30085186950% (2)
- Neuropathic Pain Questionnaire-Short FormDocument2 pagesNeuropathic Pain Questionnaire-Short Formjoshis79100% (1)
- Aesthetics and ErgonomicsDocument17 pagesAesthetics and Ergonomicssiddharth_05No ratings yet
- Daycm 7Document8 pagesDaycm 7api-309879220No ratings yet
- 4cm Final YayDocument12 pages4cm Final Yayapi-518621879No ratings yet
- Script - What Is Applied Behaviour AnalysisDocument4 pagesScript - What Is Applied Behaviour AnalysisEmmaNo ratings yet
- Amaze Information Sheet Behaviour Support Strategies For Autistic PeopleDocument3 pagesAmaze Information Sheet Behaviour Support Strategies For Autistic PeopleRUIJIE JiangNo ratings yet
- 10 Common Misco-WPS OfficeDocument6 pages10 Common Misco-WPS OfficeAya AbouseifNo ratings yet
- Patient Care Written Practical Portion Case 1Document7 pagesPatient Care Written Practical Portion Case 1api-414657737No ratings yet
- The Resilient Mind Executive Functions, Emotion Regulation, And Mental Health in Children And AdolescentsFrom EverandThe Resilient Mind Executive Functions, Emotion Regulation, And Mental Health in Children And AdolescentsNo ratings yet
- Aspect Positive Behaviour Support: Behaviour Form Information SheetDocument4 pagesAspect Positive Behaviour Support: Behaviour Form Information SheetAna JaramilloNo ratings yet
- 139 146berneessayDocument8 pages139 146berneessayعلاء يحييNo ratings yet
- ReportDocument14 pagesReportSahan PereraNo ratings yet
- NCP Autism101Document5 pagesNCP Autism101Gio Padallan PisquizaNo ratings yet
- Sensory Stimulation in Dementia CareDocument12 pagesSensory Stimulation in Dementia CareNikki SwiftNo ratings yet
- Gale Researcher Guide for: The Frontal Lobe and Executive FunctionsFrom EverandGale Researcher Guide for: The Frontal Lobe and Executive FunctionsRating: 2 out of 5 stars2/5 (1)
- Teaching Plan: Involution (Bubble He)Document4 pagesTeaching Plan: Involution (Bubble He)Pamela BagabaldoNo ratings yet
- A Pastor's Communication Will Determine His Effectiveness To Help Others Change. by Sage Martin WilsonDocument3 pagesA Pastor's Communication Will Determine His Effectiveness To Help Others Change. by Sage Martin WilsonMartin C Wilson100% (1)
- Claudia AllenDocument16 pagesClaudia AllenFranciscaElizabethSandovalRochaNo ratings yet
- Scizophrenia NCP1Document13 pagesScizophrenia NCP1Kholid Abu Mohammad AlfaizinNo ratings yet
- Et - Week 4 - Reflection in Critical Thinking Process - 2023 - S2 - StudentsDocument4 pagesEt - Week 4 - Reflection in Critical Thinking Process - 2023 - S2 - StudentstansihuishNo ratings yet
- Aisyah Binti MD Nor NO. MATRIK: U2104435 Pensyarah: Dr. Siaw Yan LiDocument7 pagesAisyah Binti MD Nor NO. MATRIK: U2104435 Pensyarah: Dr. Siaw Yan LiEye SyahNo ratings yet
- CaseStudy - 10 Year Old Boy PDFDocument3 pagesCaseStudy - 10 Year Old Boy PDFRachelle SalcedoNo ratings yet
- NLP in MotionDocument3 pagesNLP in MotionSpeech & Language Therapy in PracticeNo ratings yet
- NCM 119 Assignment Galutan Kimberly Erika FDocument5 pagesNCM 119 Assignment Galutan Kimberly Erika Faaron tabernaNo ratings yet
- Submitted By: BS - Legal Management, LM3A: Penus, Queen Ivy JDocument19 pagesSubmitted By: BS - Legal Management, LM3A: Penus, Queen Ivy JApple Ple21No ratings yet
- Autiaid: A Learning Mobile Application For Autistic ChildrenDocument6 pagesAutiaid: A Learning Mobile Application For Autistic ChildrenSarmiento CarlosNo ratings yet
- Putting Treatment To PracticeDocument4 pagesPutting Treatment To PracticeFarah Allaik 1No ratings yet
- Bruce Lipton - Understanding The Conscious & Subconscious MindDocument27 pagesBruce Lipton - Understanding The Conscious & Subconscious MindszilviNo ratings yet
- Unit 01 Developing Effective Communication in Health and Social Care Teacher InstructionsDocument5 pagesUnit 01 Developing Effective Communication in Health and Social Care Teacher InstructionsValentinaCaramarinNo ratings yet
- How To Derive A Well Defined OutcomeDocument4 pagesHow To Derive A Well Defined Outcomesuccessunforgettable100% (1)
- COA Problem IdentifiedDocument1 pageCOA Problem IdentifiedMay Chelle ErazoNo ratings yet
- Moderate Autism (NCP-Drug)Document4 pagesModerate Autism (NCP-Drug)Laila V. MananonNo ratings yet
- 2011 - Otara - Perception A Guide For Managers and LeadersDocument4 pages2011 - Otara - Perception A Guide For Managers and LeadersBob SmithNo ratings yet
- CAT Manual FINAL 1-10-13Document105 pagesCAT Manual FINAL 1-10-13ainos80No ratings yet
- Treating Fluency DisordersDocument6 pagesTreating Fluency DisordersFarah Allaik 1No ratings yet
- Written Report - Group V - Control of AntecedentsDocument39 pagesWritten Report - Group V - Control of AntecedentsMJ FangoNo ratings yet
- Running Head: Intervention Plan For A Young Child AssignmentDocument8 pagesRunning Head: Intervention Plan For A Young Child AssignmentbdestineNo ratings yet
- RBT ManualDocument22 pagesRBT ManualScribdTranslationsNo ratings yet
- 188 - BULAN - Task For Week 1Document5 pages188 - BULAN - Task For Week 1Cyril BulanNo ratings yet
- Su - 5 Presentation Bswi 411Document5 pagesSu - 5 Presentation Bswi 411mabotshatebogoNo ratings yet
- DrugDocument39 pagesDrugNylia AtibiNo ratings yet
- Causes of AutismDocument29 pagesCauses of AutismMariakatrinuuhNo ratings yet
- 12.2 The Presupositions of NLPDocument7 pages12.2 The Presupositions of NLPmotaNo ratings yet
- Focus: Enhancer to Focus Your Mind, Energy Power (Easy Steps to Improve Concentration and Productivity)From EverandFocus: Enhancer to Focus Your Mind, Energy Power (Easy Steps to Improve Concentration and Productivity)No ratings yet
- Cognitive RestructuringDocument3 pagesCognitive Restructuringiulia9gavrisNo ratings yet
- CounsellorDocument19 pagesCounsellorBen CharlieNo ratings yet
- Memory Improvement: How to Boost Your Brain Power and Remember (The Beginner's Guide to Memory Training and Memory Improvement)From EverandMemory Improvement: How to Boost Your Brain Power and Remember (The Beginner's Guide to Memory Training and Memory Improvement)No ratings yet
- Nurs 3021h Final EvaluationDocument12 pagesNurs 3021h Final Evaluationapi-313097878No ratings yet
- DocumentDocument41 pagesDocumentNylia AtibiNo ratings yet
- Laziness The Job KillerDocument5 pagesLaziness The Job KillerWellchan MaquisoNo ratings yet
- Review of Paper Executive Functions by Adele DiamondDocument2 pagesReview of Paper Executive Functions by Adele DiamondRahula RakeshNo ratings yet
- Emotion PPT 09.1.2015Document59 pagesEmotion PPT 09.1.2015malathi kotaNo ratings yet
- Project Doc Personality PredictionDocument6 pagesProject Doc Personality PredictionRajale snehalNo ratings yet
- Seminar On ELT (Proposal Outline)Document6 pagesSeminar On ELT (Proposal Outline)Putri FadiyahNo ratings yet
- Hereditary Spastic Paraplegia - UpToDateDocument22 pagesHereditary Spastic Paraplegia - UpToDateMatheus AraújoNo ratings yet
- NvsDocument49 pagesNvsChong Uy AlawiNo ratings yet
- Chemotherapy-Induced Peripheral NeuropathyDocument22 pagesChemotherapy-Induced Peripheral Neuropathyapi-238658139No ratings yet
- Notes:: Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesNotes:: Time Allowed: Reading Time: 5 Minutes Writing Time: 40 Minutesmaimoona sulemanNo ratings yet
- Uhv qb2Document5 pagesUhv qb2Edu techNo ratings yet
- Classification of NeuropathyDocument16 pagesClassification of NeuropathysekiannNo ratings yet
- Neural Network Based Control: Dan Simon Cleveland State UniversityDocument11 pagesNeural Network Based Control: Dan Simon Cleveland State UniversityArioston JúniorNo ratings yet
- Psychiatric MedicinesDocument12 pagesPsychiatric MedicinesMr. Psycho Sam0% (1)
- BEFORE WATCHING THE FILM - Answer The Following Prompts:: FAT City Video Write-UpDocument4 pagesBEFORE WATCHING THE FILM - Answer The Following Prompts:: FAT City Video Write-UpGaby AlvaradoNo ratings yet
- Clark (2001) - Natural Born CyborgsDocument8 pagesClark (2001) - Natural Born CyborgsLeandro RivasNo ratings yet
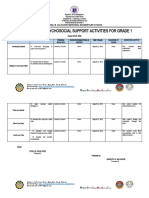
- Action Plan in Psychosocial Support Activities For Grade 1: Matias B. Salvador Memorial Elementary SchoolDocument3 pagesAction Plan in Psychosocial Support Activities For Grade 1: Matias B. Salvador Memorial Elementary SchoolMam NohryNo ratings yet
- NROSCIDocument2 pagesNROSCILiridon SopajNo ratings yet
- Psychiatric Mental Health Comprehensive Case StudyDocument13 pagesPsychiatric Mental Health Comprehensive Case Studyapi-592243628No ratings yet
- Critical Thinking SkillsDocument25 pagesCritical Thinking SkillsSamir BoucharefNo ratings yet
- No Erasures!: Disciplines and Ideas in The Social SciencesDocument2 pagesNo Erasures!: Disciplines and Ideas in The Social SciencesJoshua CorpuzNo ratings yet
- Proprioceptive Neuromuscular Facilitation PNF ItsDocument10 pagesProprioceptive Neuromuscular Facilitation PNF ItsKhaled RekabNo ratings yet
- Everything Is PredeterminedDocument6 pagesEverything Is PredeterminedOmSilence2651No ratings yet
- Nervous System Practice QuestionsDocument7 pagesNervous System Practice QuestionsOsama AlhumisiNo ratings yet
- Exam 1 PracticeDocument2 pagesExam 1 Practicejmkap13No ratings yet
- Holistic Research in SynopsDocument19 pagesHolistic Research in SynopsAMMAD FAZALNo ratings yet