Professional Documents
Culture Documents
Functional Co-Primary Measures For Clinical Trials in Schizophrenia: Results From The MATRICS Psychometric and Standardization Study
Functional Co-Primary Measures For Clinical Trials in Schizophrenia: Results From The MATRICS Psychometric and Standardization Study
Uploaded by
DrMartens AGCopyright:
Available Formats
You might also like
- Mayer-Salovey-Caruso Emotional Intelligence Test (Msceit)Document2 pagesMayer-Salovey-Caruso Emotional Intelligence Test (Msceit)DrMartens AG50% (2)
- Essay WritingDocument74 pagesEssay Writingtiendn92% (50)
- Davis Langdon Africa Handbook Jan 2009Document94 pagesDavis Langdon Africa Handbook Jan 2009Caesar 'Dee' Rethabile SerumulaNo ratings yet
- PSSR FormDocument16 pagesPSSR Formmythee100% (6)
- Evidence For Effective Interventions To Reduce Mental Health-Related Stigma and Discrimination in The Medium and Long Term: Systematic ReviewDocument51 pagesEvidence For Effective Interventions To Reduce Mental Health-Related Stigma and Discrimination in The Medium and Long Term: Systematic ReviewkinasihasyaNo ratings yet
- A Meta-Analysis of Cognitive Remediation in SchizophreniaDocument12 pagesA Meta-Analysis of Cognitive Remediation in Schizophreniamohitnet1327No ratings yet
- The Impact of Treatment Components SuggeDocument42 pagesThe Impact of Treatment Components Suggeaqsarajpoot2224No ratings yet
- A Meta-Analysis of Cognitive Remediation in SchizophreniaDocument12 pagesA Meta-Analysis of Cognitive Remediation in Schizophreniaisaacelias2509No ratings yet
- Estudio PilotoDocument9 pagesEstudio PilotoNina SalinasNo ratings yet
- CERQDocument21 pagesCERQsmacujaNo ratings yet
- Exercise and Sleep: A Systematic Review of Previous Meta-AnalysesDocument11 pagesExercise and Sleep: A Systematic Review of Previous Meta-AnalysesAlexPsrNo ratings yet
- Nihms 564241Document33 pagesNihms 564241Natalia BettancourtNo ratings yet
- The Efficacy of Cognitive Intervention in Mild Cognitive Impairment (MCI) : A Meta-Analysis of Outcomes On Neuropsychological MeasuresDocument45 pagesThe Efficacy of Cognitive Intervention in Mild Cognitive Impairment (MCI) : A Meta-Analysis of Outcomes On Neuropsychological MeasuresAlejandra GutiérrezNo ratings yet
- Clase 1 Lambert Et Al. - 1996 - The Reliability and Validity of The Outcome QuestionnaireDocument11 pagesClase 1 Lambert Et Al. - 1996 - The Reliability and Validity of The Outcome QuestionnaireLuis GaribottiNo ratings yet
- Ireland Clough Day 2017Document21 pagesIreland Clough Day 2017ShilpaNo ratings yet
- E025761 FullDocument6 pagesE025761 Full2021-110737No ratings yet
- Retest Reliabilities of Decision-Making and Cognitive Control Measures in Addictive DisordersDocument21 pagesRetest Reliabilities of Decision-Making and Cognitive Control Measures in Addictive DisordersRafael MartinsNo ratings yet
- Mindfulness SRDocument22 pagesMindfulness SRlea.clairetersouNo ratings yet
- FMCH 2021 001154Document7 pagesFMCH 2021 001154Vinayak NagriNo ratings yet
- 1 s2.0 S019188699900152X MainDocument12 pages1 s2.0 S019188699900152X MaingorkiptNo ratings yet
- Terapia BreveDocument18 pagesTerapia BreveFanny ZumárragaNo ratings yet
- The Transtheoretical Model's Processes of Change in The Heart of A Physical Activity Intervention A Series of N-Of-1 PDFDocument28 pagesThe Transtheoretical Model's Processes of Change in The Heart of A Physical Activity Intervention A Series of N-Of-1 PDFreymarkNo ratings yet
- 2 ManuscriptDocument66 pages2 ManuscriptRodrigo SilvaNo ratings yet
- Impact of Behavior ManagementPrograms On Exercise AdherenceDocument4 pagesImpact of Behavior ManagementPrograms On Exercise Adherencejhonnydm93No ratings yet
- Using Psychometric Techniques To Improve The Balance Evaluation Systems Test: The Mini-BestestDocument9 pagesUsing Psychometric Techniques To Improve The Balance Evaluation Systems Test: The Mini-BestestMochammad Syarif HidayatNo ratings yet
- SCM 37 371Document9 pagesSCM 37 371werazamaraNo ratings yet
- Improving Memory Performance in The Aged Through Mnemonic Training: A Meta-Analytic StudyDocument10 pagesImproving Memory Performance in The Aged Through Mnemonic Training: A Meta-Analytic Studypaulverhaeghen6877No ratings yet
- Borkovec93 CBT GadDocument15 pagesBorkovec93 CBT GadAlexa CiucăNo ratings yet
- Abnormal Psychology Cap4Document28 pagesAbnormal Psychology Cap4JuanNo ratings yet
- Art NueveDocument22 pagesArt NueveANTONIO REYES MEDINANo ratings yet
- VanWyk Possible (2003) PDFDocument8 pagesVanWyk Possible (2003) PDFLauren BrionesNo ratings yet
- ART 3 The Mental Health Literacy ScaleDocument6 pagesART 3 The Mental Health Literacy Scaleshireensaghir05No ratings yet
- ACT Psychosis Sistematic and MetaanalysisDocument13 pagesACT Psychosis Sistematic and MetaanalysisParla CardoNo ratings yet
- The Impact of Physical Activity On Brain Structure and Function in Youth - A Systematic ReviewDocument17 pagesThe Impact of Physical Activity On Brain Structure and Function in Youth - A Systematic ReviewSơn Đoàn TrungNo ratings yet
- Clinical Child and Family Psychology Review Volume 4 Issue 1 2001 (Doi 10.1023/a:1009528727345) Michael P. Bates - The Child and Adolescent Functional Assessment Scale (CAFAS) - Review and CurDocument22 pagesClinical Child and Family Psychology Review Volume 4 Issue 1 2001 (Doi 10.1023/a:1009528727345) Michael P. Bates - The Child and Adolescent Functional Assessment Scale (CAFAS) - Review and CurJesterJokerNo ratings yet
- Applied Behaviour Analysis and Standard Treatment in Intellectual Disability 2year OutcomesDocument2 pagesApplied Behaviour Analysis and Standard Treatment in Intellectual Disability 2year OutcomesAmira naser3579No ratings yet
- 2020 Cognition-Oriented Treatments For Older Adults - A Systematic Overview of Systematic Reviews2020Document27 pages2020 Cognition-Oriented Treatments For Older Adults - A Systematic Overview of Systematic Reviews2020maugelinNo ratings yet
- Joyce Et Al 2018.PMID - 29903782Document9 pagesJoyce Et Al 2018.PMID - 29903782Ara PalmaNo ratings yet
- 1 s2.0 S0920996414001698 MainDocument6 pages1 s2.0 S0920996414001698 MainJulieta AzevedoNo ratings yet
- Behavioral and Cognitive Impacts of Mindfulness-Based Interventions On Adults With ADHDDocument16 pagesBehavioral and Cognitive Impacts of Mindfulness-Based Interventions On Adults With ADHDDavid ZNo ratings yet
- MCQ 2Document9 pagesMCQ 2Munni KNo ratings yet
- The e Ect of Active Video Games On Cognitive Functioning in Clinical and Non-Clinical Populations A Meta-Analysis of Randomized Controlled TrialsDocument10 pagesThe e Ect of Active Video Games On Cognitive Functioning in Clinical and Non-Clinical Populations A Meta-Analysis of Randomized Controlled TrialsFaiz KunNo ratings yet
- Matrics - Confiabilidad y Validez pt1 PDFDocument11 pagesMatrics - Confiabilidad y Validez pt1 PDFDrMartens AGNo ratings yet
- The Use of The Theory of Planned Behavior To Predict Factors Influencing Physicians' Decision To Prescribe Extemporaneous Compounding Dosage Form For Pediatric OutpatientsDocument4 pagesThe Use of The Theory of Planned Behavior To Predict Factors Influencing Physicians' Decision To Prescribe Extemporaneous Compounding Dosage Form For Pediatric OutpatientsmeliNo ratings yet
- Using Generic Preferencebased Measures in Mental Health Psychometric Validity of The Eq5d and Sf6dDocument8 pagesUsing Generic Preferencebased Measures in Mental Health Psychometric Validity of The Eq5d and Sf6dJulaiha QosimNo ratings yet
- Satipatthana Mindfulness Meditation Annotated Bibliography 3-2024 2Document234 pagesSatipatthana Mindfulness Meditation Annotated Bibliography 3-2024 2bonduranNo ratings yet
- Study DrugsDocument22 pagesStudy Drugsnicole.mifsud.22No ratings yet
- Cognitive Interventions in Healthy Older Adults and People With Mild Cognitive Impairment - A Systematic ReviewDocument13 pagesCognitive Interventions in Healthy Older Adults and People With Mild Cognitive Impairment - A Systematic Reviewmadalena limaNo ratings yet
- Workplace StressDocument10 pagesWorkplace Stresspinku13No ratings yet
- ARandomized Controlled Pilot Studyofthe Effectivenessof Occupational Therapyfor Children With Sensory Modulation DisorderDocument12 pagesARandomized Controlled Pilot Studyofthe Effectivenessof Occupational Therapyfor Children With Sensory Modulation Disordertayna santosNo ratings yet
- The Functional Idiographic Assessment Template Ques - 2014 - Journal of ContextuDocument12 pagesThe Functional Idiographic Assessment Template Ques - 2014 - Journal of Contextudomingo jesus de la rosa diazNo ratings yet
- Types of Psychological TestsDocument4 pagesTypes of Psychological TestsScribdTranslationsNo ratings yet
- Evidence Based TableDocument13 pagesEvidence Based Tableneometal_86No ratings yet
- Ccoryn, Journal Editor, AllerDocument17 pagesCcoryn, Journal Editor, AllerKayu LowNo ratings yet
- Are We Improving? Update and Critical Appraisal of The Reporting of Decision Process and Quality Measures in Trials Evaluating Patient Decision AidsDocument6 pagesAre We Improving? Update and Critical Appraisal of The Reporting of Decision Process and Quality Measures in Trials Evaluating Patient Decision AidsThu ThảoNo ratings yet
- Development and Evaluation of A Scale To With Arthritis Measure Perceived Self-Efficacy in PeopleDocument8 pagesDevelopment and Evaluation of A Scale To With Arthritis Measure Perceived Self-Efficacy in PeopleSiti lestarinurhamidahNo ratings yet
- Using Psychometric Techniques To Improve The Balance Evaluation System's Test - The Mini-BESTestDocument17 pagesUsing Psychometric Techniques To Improve The Balance Evaluation System's Test - The Mini-BESTestizabelle paesNo ratings yet
- A Brief Measure For Assessing Generalized Anxiety Disorder: The GAD-7Document6 pagesA Brief Measure For Assessing Generalized Anxiety Disorder: The GAD-7Von Jezzrel Jumao-asNo ratings yet
- Emotional IntelligenceDocument13 pagesEmotional Intelligencedanamaria13No ratings yet
- Coelho - Ylvisaker - Turkstra Non-Stand Assess Sem 2005 PDFDocument19 pagesCoelho - Ylvisaker - Turkstra Non-Stand Assess Sem 2005 PDFGaoudam NatarajanNo ratings yet
- Basics of Psychological AssessmentsDocument35 pagesBasics of Psychological AssessmentsKarishma Tiwari100% (1)
- 1 s2.0 S1876201821004536 MainDocument7 pages1 s2.0 S1876201821004536 Mainwatch2303No ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet
- Dimensional PsychopathologyFrom EverandDimensional PsychopathologyMassimo BiondiNo ratings yet
- Ox B2 Test 2 AudioscriptDocument5 pagesOx B2 Test 2 AudioscriptDrMartens AGNo ratings yet
- Oxford Writing TipsDocument64 pagesOxford Writing TipsDrMartens AG100% (1)
- Oxfrod B2 Practice Test 1 Answer KeyDocument6 pagesOxfrod B2 Practice Test 1 Answer KeyDrMartens AGNo ratings yet
- Prepositional Phrase Examples: A Big List of 160+ Prepositional PhrasesDocument13 pagesPrepositional Phrase Examples: A Big List of 160+ Prepositional PhrasesDrMartens AGNo ratings yet
- EMDR Metaanlisis EstudioDocument12 pagesEMDR Metaanlisis EstudioDrMartens AGNo ratings yet
- Screening For Personality Disorders Among PDFDocument14 pagesScreening For Personality Disorders Among PDFDrMartens AGNo ratings yet
- Revising Axis V For A Review of Measures of Social FunctioningDocument9 pagesRevising Axis V For A Review of Measures of Social FunctioningDrMartens AGNo ratings yet
- Matrics - Confiabilidad y Validez pt1 PDFDocument11 pagesMatrics - Confiabilidad y Validez pt1 PDFDrMartens AGNo ratings yet
- Neuropsychological Profile in Early-Onset Schizophrenia-Spectrum Disorders: Measured With The MATRICS BatteryDocument8 pagesNeuropsychological Profile in Early-Onset Schizophrenia-Spectrum Disorders: Measured With The MATRICS BatteryDrMartens AGNo ratings yet
- Esquizo ITP 2011Document4 pagesEsquizo ITP 2011DrMartens AGNo ratings yet
- Wto 4Document24 pagesWto 4Tabish AhmedNo ratings yet
- Lecture 3: Solving Linear Systems: Elif TanDocument20 pagesLecture 3: Solving Linear Systems: Elif Tansercan egilmezkolNo ratings yet
- Meitei Mayek: Typeface Design (M. Thesis Presentation)Document53 pagesMeitei Mayek: Typeface Design (M. Thesis Presentation)ishanidayal536No ratings yet
- SPP No. 200 Code of Ethical ConductDocument24 pagesSPP No. 200 Code of Ethical ConductShann HortalezaNo ratings yet
- CadburyDocument12 pagesCadburymldc20110% (1)
- Lesson Plan Convection With AnswersDocument3 pagesLesson Plan Convection With AnswersQueencess Ara TorresNo ratings yet
- Sundram Fasteners Limited, HosurDocument38 pagesSundram Fasteners Limited, Hosurjaydeepsinh100% (1)
- CVS 4150 & 4160 Pressure Controller July 2012Document12 pagesCVS 4150 & 4160 Pressure Controller July 2012Zts MksNo ratings yet
- Presentation Alfa Laval Corrosion Charts For Plate Heat ExchangersDocument5 pagesPresentation Alfa Laval Corrosion Charts For Plate Heat ExchangersNasrin AkhondiNo ratings yet
- Emile Agnel Trio Oboe Cello PianoDocument52 pagesEmile Agnel Trio Oboe Cello PianoVíctor Lazo100% (1)
- Advances in Computer Entertainment: Dennis Reidsma Haruhiro Katayose Anton NijholtDocument692 pagesAdvances in Computer Entertainment: Dennis Reidsma Haruhiro Katayose Anton NijholtMauro GasparofNo ratings yet
- PRC Case Completion Form For Midwifery ExamsDocument2 pagesPRC Case Completion Form For Midwifery ExamsNoel84% (31)
- Categories Business-To-Consumer (B2C) (: Identify The Major Categories and Trends of E-Commerce Applications. E CommerceDocument9 pagesCategories Business-To-Consumer (B2C) (: Identify The Major Categories and Trends of E-Commerce Applications. E CommerceHajra NoorNo ratings yet
- Catalog CMT 2012Document302 pagesCatalog CMT 2012Cornelia BuriceaNo ratings yet
- CHAPTER 4 (Review Questions) : Direction: Read Each Question Carefully. Encircle The Letter of The Correct AnswerDocument11 pagesCHAPTER 4 (Review Questions) : Direction: Read Each Question Carefully. Encircle The Letter of The Correct AnswerChery PerialdeNo ratings yet
- Efficient Approach For ISL Using MLDocument4 pagesEfficient Approach For ISL Using MLsugar cubeNo ratings yet
- Ibs Company ProfileDocument52 pagesIbs Company ProfileFaeez ZainNo ratings yet
- Are You Fit For ISO 16890?: Thomas SchrothDocument16 pagesAre You Fit For ISO 16890?: Thomas SchrothUdhayakumar Venkataraman100% (1)
- Pigeonhole PrincipleDocument5 pagesPigeonhole PrincipleNoisyPoisyNo ratings yet
- Lesson 4 - History of Development Economics (First Part)Document12 pagesLesson 4 - History of Development Economics (First Part)Rose RaboNo ratings yet
- t2 M 5870 Differentiated Multistep Problems Involving Addition and Subtraction Activity Sheets - Ver - 1Document9 pagest2 M 5870 Differentiated Multistep Problems Involving Addition and Subtraction Activity Sheets - Ver - 1Chitra ThadaniNo ratings yet
- Rezene Business PlanDocument37 pagesRezene Business PlanMehari GebreyohannesNo ratings yet
- Bayview's Last Stand: Protecting Historic Black Neighborhoods - John William Templeton Speaker FilmmakerDocument5 pagesBayview's Last Stand: Protecting Historic Black Neighborhoods - John William Templeton Speaker FilmmakerJW TempletonNo ratings yet
- How Disruptive Technologies Are Opening Up Innovative Opportunities in ServicesDocument10 pagesHow Disruptive Technologies Are Opening Up Innovative Opportunities in ServicesSachin SengarNo ratings yet
- Barney Smca6 Tif 05Document31 pagesBarney Smca6 Tif 05p astelNo ratings yet
- 10 CarbohydratesDocument6 pages10 CarbohydratesBryanNo ratings yet
- WMO Guidelines On Surface Station Data Quality Assurance For Climate ApplicationsDocument74 pagesWMO Guidelines On Surface Station Data Quality Assurance For Climate ApplicationsGEMPFNo ratings yet
- Eddie The Carpet FitterDocument3 pagesEddie The Carpet Fittermaria praveenNo ratings yet
Functional Co-Primary Measures For Clinical Trials in Schizophrenia: Results From The MATRICS Psychometric and Standardization Study
Functional Co-Primary Measures For Clinical Trials in Schizophrenia: Results From The MATRICS Psychometric and Standardization Study
Uploaded by
DrMartens AGOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Functional Co-Primary Measures For Clinical Trials in Schizophrenia: Results From The MATRICS Psychometric and Standardization Study
Functional Co-Primary Measures For Clinical Trials in Schizophrenia: Results From The MATRICS Psychometric and Standardization Study
Uploaded by
DrMartens AGCopyright:
Available Formats
Article
Functional Co-Primary Measures for Clinical Trials
in Schizophrenia: Results From the MATRICS
Psychometric and Standardization Study
Michael F. Green, Ph.D. Objective: During the consensus meet- Results: Data are presented for each co-
ings of the National Institute of Mental primary measure for test-retest reliability,
Health Measurement and Treatment Re- utility as a repeated measure, relation-
Keith H. Nuechterlein, Ph.D.
search to Improve Cognition in Schizo- ship to cognitive performance, relation-
phrenia (NIMH-MATRICS) Initiative, the ship to functioning, tolerability/practical-
Robert S. Kern, Ph.D. U.S. Food and Drug Administration took ity, and number of missing data.
the position that a drug for this purpose Conclusions: Psychometric properties of
Lyle E. Baade, Ph.D. should show changes on 1) an accepted
all of the measures were considered ac-
consensus cognitive performance mea- ceptable, and the measures were gener-
Wayne S. Fenton, M.D. sure and 2) an additional measure (i.e., a
ally comparable across the various crite-
co-primary) that is considered function- ria, except that the functional capacity
James M. Gold, Ph.D. ally meaningful. The goal of the current
measures had stronger relationships to
study was to describe steps to evaluate cognitive performance and fewer missing
Richard S.E. Keefe, Ph.D. four potential co-primary measures for
data. The development and evaluation of
psychometric properties and validity. potential co-primary measures is still at
Raquelle Mesholam-Gately, Method: As part of the five-site MATRICS an early stage, and it was decided not to
Psychometric and Standardization Study endorse a single measure for clinical trials
Ph.D.
(PASS), two measures of functional capac- at this point. The current findings offer
ity and two interview-based measures of the initial steps to identify functionally
Larry J. Seidman, Ph.D. cognition were evaluated in 176 patients meaningful co-primary measures in this
with schizophrenia (167 of these patients area and will help to guide further evalu-
Ellen Stover, Ph.D. were retested 4 weeks later). ation of such measures.
Stephen R. Marder, M.D.
(Am J Psychiatry 2008; 165:221–228)
T he National Institute of Mental Health Measurement
and Treatment Research to Improve Cognition in Schizo-
One possible co-primary measure might be an assess-
ment of community functioning. However, change in
phrenia (NIMH-MATRICS) Initiative was created to stimu- community status (e.g., return to work, increased social
late the development of cognition-enhancing drugs for relationships, or higher degree of independent living) in-
schizophrenia (1–3). As described in two other articles (4, volves many intervening variables (both personal and so-
5), a key deliverable for the MATRICS Initiative was the se- cial factors) that act between underlying cognitive pro-
lection, through a broad-based multidisciplinary consen- cesses and these functional outcomes. These intermediate
sus process, of a standard cognitive battery: the MATRICS steps would make it difficult to see the functional benefits
Consensus Cognitive Battery (6). The U.S. Food and Drug of cognition-enhancing effects (7–10). Similarly, improve-
Administration (FDA) indicated at the MATRICS meetings ments in cognition would be expected to take consider-
that significant improvement on a consensus cognitive able time to translate into functional improvements (11).
performance endpoint would be necessary, but not suffi- Finally, changes in daily functioning would depend on
cient, for drug approval. In addition to changes in cogni- nonbiological factors that are typically uncontrolled in
tive performance, the FDA will require improvements on a clinical trial studies (e.g., the availability of psychosocial
functionally meaningful co-primary measure that would rehabilitation, social support networks, local employment
have more face validity for consumers and clinicians than rates, and training opportunities). Hence, alternative co-
cognitive performance measures (3). This requirement primary measures were considered that might change
presents a notable challenge because of the absence of ac- more directly and on a comparable time course with cog-
cepted or validated co-primary measures for this purpose. nitive improvement. Such measures include standardized
This article is featured in this month’s AJP Audio and discussed in an editorial by Drs. Harvey and Cornblatt on p. 163.
Am J Psychiatry 165:2, February 2008 ajp.psychiatryonline.org 221
RESULTS FROM THE MATRICS STUDY
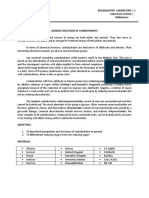
TABLE 1. Test-Retest Reliability of Measures in the MATRICS ability, utility as a repeated measure, relationship to cogni-
Psychometric and Standardization Study tive performance, relationship to outcome, practicality/
Test-Retest tolerability, and number of missing data.
Reliability
(intraclass
Co-Primary Measure correlation) Method
Maryland Assessment of Social Competence
Conversational content 0.68 The complete methods for this study are presented online (the
Nonverbal content 0.66 data supplement is available at http://ajp.psychiatryonline.org).
Effectiveness 0.69 A brief summary is presented here.
UCSD Performance-Based Skills Assessment
The data in this article are part of the five-site MATRICS PASS.
Total score 0.70
Phase 1 was conducted with 176 schizophrenia patients tested
Medication management 0.48
Schizophrenia Cognition Rating Scale twice at a 4-week interval (4), and phase 2 included 300 commu-
Overall impression (patient) 0.60 nity subjects to collect co-norming data for the tests in the final
Overall impression (informant) 0.77 battery (5). To evaluate the co-primary measures, we used a simi-
Overall impression (interviewer) 0.82 lar approach to that used to evaluate the cognitive performance
Clinical Global Impression of Cognition in measures and considered 1) test-retest reliability, 2) utility as a re-
Schizophrenia peated measure, 3) relationship to functional status, 4) tolerabil-
Neurocognitive state (patient) 0.76 ity/practicality, and 5) number of missing data. In addition, we
Neurocognitive state (caregiver) 0.85
evaluated the degree to which co-primary measures correlated
Neurocognitive state (composite) 0.80
with cognitive performance (3).
Global Assessment of Functioning (composite) 0.89
Based on discussions at consensus meetings and recommen-
dations of the MATRICS Outcomes Committee (1) (A. Bellack,
tests of functional capacity or interview-based assess- chair), two approaches to co-primary measures were considered:
ments of cognition. measures of functional capacity and self-report measures of cog-
nition. Two measures were selected from each approach. Unlike
Functional capacity refers to an individual’s capacity for
the large consensus and data collection process that was used to
performing key tasks of daily living. To assess functional select cognitive performance tests for the MATRICS Consensus
capacity, participants simulate in the clinic such real- Cognitive Battery, the selection of potential co-primary measures
world activities as holding a social conversation, prepar- was based on expert recommendations from the committee. The
ing a meal, or taking public transportation (12, 13). Good functional capacity measures were the Maryland Assessment of
Social Competence (13) and the University of California at San Di-
performance on such measures does not mean that a per-
ego (UCSD) Performance-Based Skills Assessment (18). The inter-
son will perform the tasks in the community, but it does view-based measures of cognition were the Schizophrenia Cogni-
mean that the person could perform the task if he or she tion Rating Scale (16) and the Clinical Global Impression of
had the opportunity and was willing. Because perfor- Cognition in Schizophrenia (17).
mance on measures of functional capacity do not depend Cognitive performance was assessed with the MATRICS Con-
sensus Cognitive Battery (4, 5). As described more fully in the first
on social and community opportunities, they are more
article (4), community functioning was assessed with variables
likely to be temporally linked with treatment-related from the Birchwood Social Functioning Scale (19), supplemented
changes in underlying cognition. with work and school items from the Social Adjustment Scale (20).
Another approach for co-primary measures was to con-
sider interview-based assessments of cognitive abilities. Results
Different interview-based approaches to cognition have
been used, including asking people to estimate their own Study Group
cognitive abilities or asking subjects to estimate the extent The study group for these analyses is the same as de-
to which their daily lives are affected by cognitive impair- scribed in the first article (4): across the five performance
ment. Interview-based approaches present a challenge sites, 176 patients were assessed at baseline and 167 were
because it is often difficult for individuals (healthy sub- assessed at the 4-week follow-up.
jects as well as patients) to estimate their own perfor-
mance abilities (14, 15). Recently, some cognitive assess- Test-Retest Reliability
ment interviews have been developed in which the ratings The results for test-retest reliability are shown in Table 1.
of psychotic patients are supplemented with ratings from The table shows the intraclass correlation coefficient (ICC),
informants (e.g., caregivers), an approach that might have which takes into account changes in mean level. Both the
advantages over previous assessments that used only self- ICC and Pearson’s r are shown in the online data supple-
reports (16, 17). ment; differences for the two statistics were minor. The test-
The goal of the current study was to evaluate the reli- retest reliability was good across measures; a correlation of
ability, validity, and appropriateness for use in clinical tri- 0.70 or greater is generally considered to be acceptable test-
als of four potential co-primary measures: two measures retest reliability for clinical trials, and most of the tests were
of functional capacity and two interview-based measures in that range or higher. The one exception was the medica-
of cognition. With this goal in mind, these four measures tion management component of the UCSD Performance-
were added to the MATRICS Psychometric and Standard- Based Skills Assessment that had relatively low reliability. As
ization Study (PASS) and assessed for their test-retest reli- mentioned above, this was a secondary measure of the
222 ajp.psychiatryonline.org Am J Psychiatry 165:2, February 2008
GREEN, NUECHTERLEIN, KERN, ET AL.
TABLE 2. Utility as a Repeated Measure in the MATRICS Psychometric and Standardization Study
Time2–Time1 Number of
Time1 Time2 Difference Scores at Analysis Effect Size
Co-Primary Measure Mean SD Mean SD Mean SD Floor/Ceiling t df p (Cohen’s d)
Maryland Assessment of
Social Competence
Conversational content 3.3 1.0 3.2 1.0 –0.1 0.8 8/9 –2.18 157 0.03 –0.10
Nonverbal content 3.3 1.1 3.1 1.0 –0.2 0.9 10/25 –3.16 157 0.002 –0.19
Effectiveness 3.2 1.0 3.1 1.0 –0.1 0.8 11/9 –2.29 165 0.02 –0.10
UCSD Performance-Based
Skills Assessment
Total score 86.1 11.3 88.6 10.2 2.5 7.2 0/23 4.54 165 0.0001 0.23
Medication managementa 7.4 6.6 6.5 6.3 –0.9 6.7 0/48 –1.64 165 0.10 –0.13
Schizophrenia Cognition
Rating Scale
Patienta 4.1 2.1 4.0 2.1 –0.1 1.9 3/38 –0.50 164 0.62 –0.03
Informanta 4.1 1.7 4.3 1.8 0.2 1.2 0/9 1.73 130 0.09 0.10
Interviewera 4.7 1.5 4.6 1.6 –0.1 0.9 0/2 –1.28 157 0.20 –0.06
Clinical Global Impression
of Cognition in
Schizophrenia
Neurocognitive state 3.2 0.9 3.1 0.9 –0.1 0.6 0/3 –1.35 164 0.18 –0.08
(patient)a
Neurocognitive state 3.0 1.0 3.1 0.9 0.1 0.5 0/8 1.34 131 0.18 0.06
(caregiver)a
Neurocognitive state 3.4 0.9 3.3 0.9 –0.1 0.6 0/2 –1.64 158 0.10 –0.08
(composite)a
Global Assessment of 59.2 9.3 59.6 9.2 0.4 4.3 0/0 1.08 160 0.28 0.04
Functioning (composite)
a Tests in which lower scores are better.
UCSD Performance-Based Skills Assessment. For the self- changes in cognition, it is important that they correlate
report measures, the reliability was slightly higher for the with cognitive performance. We examined the correla-
interviewers and informants than for the patients. tions of the co-primary measures with each of the compo-
nents of the MATRICS Consensus Cognitive Battery (in the
Utility as a Repeated Measure
data supplement), as well as a composite score from the 10
Tests are considered useful for clinical trials if they show a tests (shown in Table 3). For this purpose, the composite
relatively small practice effect or, if they have a practice ef- score was calculated by standardizing each of the cogni-
fect, the effect is not so large that subjects’ scores approach tive tests (mean of 0 and SD of 1) and then summing the
the ceiling. To examine a test’s utility as a repeated measure, standardized scores. The MATRICS Consensus Cognitive
we assessed scores at baseline and 4 weeks later, change Battery scoring program now has a more systematic way
scores, the variability of change, and the number of admin- to derive a composite score that involves two renorming
istrations at which the subjects performed at the ceiling or steps, first for each of the domain scores that have multi-
floor, defined as the best or worst score possible on the test
ple measures and second for the final composite score. We
(shown in Table 2). Note that in some of the tables, the di-
present the simplified composite score in this article be-
rection of scoring differs among test indices. Scores for
cause the PASS data were collected and analyzed before
which lower is better are noted. The practice effects were
the MATRICS Consensus Cognitive Battery scoring pro-
generally small, and the highest was for the UCSD Perfor-
gram existed, so the data in Table 4 are those that were re-
mance-Based Skills Assessment total score (Cohen’s d=
viewed by the MATRICS Neurocognition Committee and
0.23). Other effect sizes for practice effects with the co-pri-
mary measures were small, but some were statistically sig- submitted to NIMH and the FDA. To compare the strength
nificant with the large group size. Finally, a few tests showed of correlations among measures, we included only sub-
ceiling effects, including the medication management jects with complete data on all four measures (i.e., listwise
component of the UCSD Performance-Based Skills Assess- deletion, N=156). The correlation between the UCSD Per-
ment, the patient report on the Schizophrenia Cognition formance-Based Skills Assessment total score and cogni-
Rating Scale, the nonverbal score from the Maryland As- tive performance was significantly higher than for both
sessment of Social Competence, and the total score from interview-based summary measures (Schizophrenia Cog-
the UCSD Performance-Based Skills Assessment. nition Rating Scale—interviewer and Clinical Global Im-
pression of Cognition in Schizophrenia—neurocognitive
Relationship to Cognitive Performance state composite) (t=4.13, df=153, p=0.001). The UCSD Per-
Because the co-primary measures are intended to serve formance-Based Skills Assessment correlation with cogni-
as face valid indicators of the consequences of underlying tive performance was also higher than the one for the
Am J Psychiatry 165:2, February 2008 ajp.psychiatryonline.org 223
RESULTS FROM THE MATRICS STUDY
TABLE 3. Relationship to Cognitive Performance in the measures (4), the subjects were asked immediately after
MATRICS Psychometric and Standardization Studya each co-primary measure to point to a number on a 7-
Overall point Likert scale (1=extremely unpleasant, 7=extremely
Co-Primary Measure Cognition
pleasant) to indicate the degree to which they found the
Maryland Assessment of Social Competence
Conversational content 0.42 measure pleasant. Practicality refers to the administrator’s
Nonverbal content 0.32 view of the measure (i.e., how difficult it is to set up, train
Effectiveness 0.40
UCSD Performance-Based Skills Assessment
staff, administer, and score). Practicality was assessed with
Total score 0.61 a 7-point Likert scale for setup, administration, and scor-
Medicationb –0.53 ing, as well as a global score. The ratings were made by the
Schizophrenia Cognition Rating Scale
Patientb –0.18 administrators of the co-primary measures after comple-
Informantb –0.21 tion of data collection for the entire group.
Interviewerb –0.31
Clinical Global Impression of Cognition
Table 5 presents the data on tolerability and practicality,
in Schizophrenia as well as the mean length of time for administration. For
Neurocognitive state (patient)b –0.30 the two functional capacity measures, both tests were
Neurocognitive state (caregiver)b –0.24
Neurocognitive state (composite)b –0.31 considered to be practical and tolerable, with the UCSD
Global Assessment of Functioning (composite) 0.30 Performance-Based Skills Assessment generally rated
a Cognitive performance scores that were used: Trail Making Test higher than the Maryland Assessment of Social Compe-
part A: time to completion; Brief Assessment of Cognition in Schizo- tence. We did not record scoring as part of the practicality
phrenia symbol coding: total number correct; Hopkins Verbal
Learning Test—Revised: total number of words recalled over three rating for the Maryland Assessment of Social Competence
learning trials; Wechsler Memory Scale—III: spatial span: sum of because that test was scored centrally, not at the local
raw scores on forward and backward conditions; Letter-Number
sites. However, a practical consideration is that this test re-
Span: number of correct trials; Neuropsychological Assessment
Battery: mazes: total raw score; Brief Visuospatial Memory Test— quired the additional step of centralized scoring, a process
Revised: total recall score over three learning trials; Category Flu- that typically required 20–30 minutes per assessment. For
ency (animal naming): total number of animals named in 60 sec-
onds; Mayer-Salovey-Caruso Emotional Intelligence Test: managing
the two interview-based measures, both tests had accept-
emotions: branch score using general consensus scoring; Continu- able ratings, with the Schizophrenia Cognition Rating
ous Performance Test—identical pairs: mean d′ value across 2-, 3-, Scale generally rated higher than the Clinical Global Im-
and 4-digit conditions.
b Tests in which lower scores are better. pression of Cognition in Schizophrenia because it was
easier to score and could be administered in roughly half
the time. Of course, investigators desiring cognitive do-
Maryland Assessment of Social Competence Effectiveness
main coverage might nevertheless prefer the Clinical Glo-
score (t=2.50, df=153, p<0.03).
bal Impression of Cognition in Schizophrenia.
Relationship to Self-Reported Functional
Missing Data
Outcome
Table 6 shows the number of data missing across both
The sites differed substantially in the functional status
assessments, not counting the nine missing assessments
of the patients (e.g., one site had only a single subject
for the subjects who did not return for the retest. The
working, and another site consisted largely of patients in a
number of missing data is quite small for both functional
long-term residential program). Because of these cross-
capacity measures, with the UCSD Performance-Based
site differences in functional status, the correlations be-
Skills Assessment showing fewer missing data than the
tween co-primary measures and functional outcome var- Maryland Assessment of Social Competence. For the in-
ied from site to site. Given this variability, we present cor- terview-based measures, the data collection was nearly
relations two ways: a correlation for all subjects across complete for the patient interviews, but about 14% of the
sites and also the median correlation across the five sites. informant interviews (across both assessment periods)
Both of these methods tend to underestimate the correla- were missing. This pattern reflects the expected challenge
tions that would be observed if patients at all sites in- in identifying and locating suitable informants for the pa-
cluded a wide range of functional levels. However, the re- tient participants in clinical trials.
sults (Table 4) allow for direct comparisons among the
measures. Most of the correlations were modest, and there Site Differences
were no notable differences in the strength of the correla- We also evaluated site differences among representative
tions across co-primary measures. measures from each of the four co-primary measures (ef-
fectiveness from the Maryland Assessment of Social Com-
Tolerability/Practicality petence, total score from the UCSD Performance-Based
Tolerability refers to the participant’s perspective of a Skills Assessment, and the interviewer’s ratings from each
measure (i.e., how interesting, pleasant, or burdensome it self-report measure) with a series of one-way analyses of
is to take). Similar to what was done with the cognitive variance (ANOVAs). The UCSD Performance-Based Skills
224 ajp.psychiatryonline.org Am J Psychiatry 165:2, February 2008
GREEN, NUECHTERLEIN, KERN, ET AL.
TABLE 4. Relationships to Functional Status in the MATRICS Psychometric and Standardization Study
Relationship to Functional Outcome
Globala Sociala Independent Livinga Worka
Co-Primary Measure Median r Median r Median r Median r
Maryland Assessment of Social Competence
Conversational content 0.28 0.28 0.00 0.00 0.32 0.29 0.16 0.14
Nonverbal content 0.23 0.20 0.02 0.00 0.29 0.28 0.08 0.11
Effectiveness 0.27 0.28 0.00 0.03 0.31 0.26 0.15 0.10
UCSD Performance-Based Skills Assessment
Total score 0.23 0.29 0.04 0.00 0.19 0.09 0.17 0.19
Medication managementb –0.18 –0.18 –0.01 0.09 –0.07 –0.08 –0.23 –0.26
Schizophrenia Cognition Rating Scale
Patientb –0.23 –0.27 –0.28 –0.26 –0.06 –0.03 –0.06 –0.21
Informantb –0.24 –0.32 –0.16 –0.29 –0.22 –0.09 –0.05 0.05
Interviewerb –0.34 –0.37 –0.17 –0.08 –0.27 –0.23 –0.16 –0.08
Clinical Global Impression of Cognition in
Schizophrenia
Neurocognitive state (patient)b –0.31 –0.39 –0.20 –0.19 –0.24 –0.34 –0.10 –0.23
Neurocognitive state (caregiver)b –0.27 –0.40 –0.05 –0.07 –0.26 –0.37 –0.16 –0.02
Neurocognitive state (composite)b –0.30 –0.39 –0.12 –0.11 –0.26 –0.31 –0.14 –0.15
Global Assessment of Functioning 0.39 0.41 0.20 0.21 0.26 0.19 0.22 0.18
(composite)
a First value combines data across sites; second value is the median r of the five sites.
b Tests in which lower scores are better.
TABLE 5. Practicality and Tolerability in the MATRICS Psychometric and Standardization Study
Practicalitya Administration
Global Setup Administration Scoring Tolerabilityb Time
Co-Primary Measure Mean SD Mean SD Mean SD Mean SD Mean SD Mean SD
Maryland Assessment of 4.7 1.2 5.8 0.8 4.3 1.4 — 3.8 2.2 23.8 4.9
Social Competence
UCSD Performance-Based 5.8 0.8 5.2 1.2 5.8 1.2 6.2 1.0 6.2 1.0 25.7 8.7
Skills Assessment
Schizophrenia Cognition 6.0 0.9 7.0 0.0 6.2 0.8 5.8 0.8 5.7 1.0 13.3 3.8
Rating Scale
Clinical Global Impression of 3.5 0.8 6.0 1.1 3.5 1.0 3.0 0.6 3.5 0.8 25.8 3.8
Cognition in Schizophrenia
a Possible range=1 (very hard) to 7 (very easy).
b Possible range=1 (extremely unpleasant) to 7 (extremely pleasant).
Assessment did not show significant differences across different potential co-primary measures, two measures
sites, but the other three measures did (Maryland Assess- each from two distinctive approaches: measures of func-
ment of Social Competence effectiveness: F=3.39, df=4, tional capacity and interview-based measures of cognition.
161, p<0.03; Schizophrenia Cognition Rating Scale—inter- Several summary points can be drawn from these data.
viewer: F=6.67, df=4, 165, p<0.001; Clinical Global Impres- First, all four measures had acceptable test-retest reliabil-
sion of Cognition in Schizophrenia composite: F=20.73, ity. An added component of the UCSD Performance-Based
df=4, 165, p<0.001). The differences across sites on these Skills Assessment (medication management) had lower
co-primary measures may be partially a result of the fact reliability, perhaps because scores on this component
that the sites differed in terms of the average functional tended to be at or near the ceiling. Second, most tests had
level of the patients. Hence, we view the differences as a adequate range. A practice effect was noted for the UCSD
reflection of actual group differences as opposed to a fail- Performance-Based Skills Assessment total score. The
ure of cross-site reliability of administration. measures with the most prominent ceiling effects in-
cluded the medication management component of the
Discussion UCSD Performance-Based Skills Assessment (which is
separate from the main test) and the Schizophrenia Cog-
This article evaluated four potential co-primary mea- nition Rating Scale—patient rating (which is not the pri-
sures that may be used in clinical trials of cognition-en- mary rating for this interview). Third, the relationships to
hancing drugs for schizophrenia. Early discussions with the cognitive performance were notably higher for functional
FDA indicated that approval of a cognition-enhancing drug capacity measures (in particular the UCSD Performance-
for schizophrenia would require changes on a consensus Based Skills Assessment) than for the interview-based
measure of cognitive performance, as well as on a function- measures of cognition. This pattern is consistent with
ally meaningful co-primary measure. We considered four findings that interview-based assessments of cognition
Am J Psychiatry 165:2, February 2008 ajp.psychiatryonline.org 225
RESULTS FROM THE MATRICS STUDY
TABLE 6. Missing Data in the MATRICS Psychometric and munity functioning homogeneity. At some sites, the range
Standardization Study of community functioning was restricted by treatment set-
Tally of ting constraints (e.g., residential treatment) that were not
Missing
Co-Primary Measure Dataa simply due to cognitive or functional capacity levels. A re-
stricted range of within-site variance on the community
Maryland Assessment of Social Competence 18 functional status measure would be expected to reduce the
UCSD Performance-Based Skills Assessment 5 magnitude of the correlations with co-primary measures.
Schizophrenia Cognition Rating Scale—patient 3
Schizophrenia Cognition Rating Scale—informant 49 In this situation, it was difficult to obtain a representative
Clinical Global Impression of Cognition in 5 indication of the associations; however, the values do pro-
Schizophrenia—patient vide a reasonable basis for comparison of the four mea-
Clinical Global Impression of Cognition in 49
Schizophrenia—caregiver sures, all of which performed comparably.
a Missing data across both assessments. The MATRICS Neurocognition Committee reviewed the
data presented in this article and concluded that because
generally do not correlate well with objective cognitive all of the potential co-primary measures performed reason-
performance (15). Also, the UCSD Performance-Based ably well, it was difficult to make a narrow recommendation
Skills Assessment, the Maryland Assessment of Social to NIMH and the FDA. A clearly stated objective for the
Competence, and the MATRICS Consensus Cognitive Bat- MATRICS Initiative was to select a single consensus cogni-
tery can all be considered performance measures, and tive performance battery (the MATRICS Consensus Cogni-
therefore they share some method variance. Fourth, all tive Battery) for use in clinical trials of cognition-enhancing
measures had modest relationships to community func- drugs for schizophrenia. In contrast, the Neurocognition
Committee was not asked to recommend any particular co-
tional status that were somewhat lower than expected.
primary measure, and the committee did not do so. The
Fifth, missing data were more frequently observed for the
Neurocognition Committee noted that if one needed to
interview-based measures because of the difficulty in con-
choose a co-primary measure for a clinical trial at this time,
tacting individuals who could serve as informants.
the UCSD Performance-Based Skills Assessment (with
The blind across measures was not absolute. The raters
modifications to address the ceiling effect) had the advan-
who administered the functional capacity measures also
tage of a strong association with cognitive performance. A
administered the cognitive performance tests (although
revised version of the UCSD Performance-Based Skills As-
the scoring for the Maryland Assessment of Social Compe-
sessment with adjusted difficulty level is currently available.
tence was done centrally). The testers did not have access The two interview-based measures were similar in struc-
to any information on functional status or the interview- ture, and their summary scores were highly correlated (r=
based measures of cognition. The staff members who con- 0.68; in comparison, the correlation for the two functional
ducted the interview-based measures of cognition did not capacity measures was 0.30). If it was desirable to include
have access to the functional status interviews, but they an additional co-primary measure that reflects the inter-
were not fully blind to functional status because these view-based approach, the Schizophrenia Cognition Rating
measures include questions about the degree to which Scale has the advantage of better tolerability and practical-
cognitive impairment interferes with activities of daily liv- ity, although it lacks domain ratings.
ing. Another limitation of these data are that they were
The evaluation and selection of co-primary measures
collected in the absence of cognitive change. One would
raises questions about validity. The key concern of the
ideally want to know the sensitivity of these measures to FDA is demonstrating that a new cognition-enhancing
changes in cognition as opposed to measuring when the drug affects cognitive performance and meaningful func-
cognition was presumably stable. Questions about the tional abilities. At present, evidence of content validity of
sensitivity of co-primary measures to change in cognitive co-primary measures may be more available than evi-
performance will await identification of a potent cogni- dence of construct or external validity. That is, the content
tion-enhancing drug or perhaps could be examined in the of these measures can be evaluated for its functional
context of cognitive remediation programs. meaningfulness from the perspectives of patients, clini-
The relationships between the co-primary measures and cians, and families. Further establishment of construct or
functional status were somewhat lower than expected and external validity, including relationships to cognitive per-
lower than reported in other studies (10, 16). The ratings of formance and community functioning, will take time. A
community functioning were based entirely on subject related validity issue is whether co-primary measures
self-reports (not observation and not informants), which need to be sufficiently distinct (i.e., involve different con-
may have limited the validity of the ratings. In addition, the structs) from cognitive performance measures. For exam-
correlations may have been limited by substantial differ- ple, some functional capacity measures resemble neu-
ences in functional status across the five sites and consid- rocognitive tests in mode of administration. However, at
erable variability in the size of the correlations across sites this point, distinctiveness of cognitive performance and
that may be attributable to instances of within-site com- co-primary measures does not appear to be a concern of
226 ajp.psychiatryonline.org Am J Psychiatry 165:2, February 2008
GREEN, NUECHTERLEIN, KERN, ET AL.
the FDA. A co-primary measure could in theory be a mod- eth. Dr. Gold receives royalties from the Brief Assessment of Cogni-
tion. Dr. Neuchterlein has received a grant from Janssen.
ified version of a cognitive performance test (if it has con-
Funding for the MATRICS Initiative was provided through contract
tent of clear functional relevance) or a modified version of N01MH22006 from NIMH to the University of California, Los Angeles
a community functioning scale (if sufficiently sensitive to (Dr. Marder, principal investigator; Dr. Green, co-principal investiga-
tor; Dr. Fenton, project officer). Funding for MATRICS PASS came from
change within a clinical trial). At this stage of develop-
an option (Dr. Green, principal investigator; Dr. Nuechterlein, co-prin-
ment, associations between co-primary measures and cipal investigator) to the NIMH MATRICS Initiative.
cognitive performance may be more critical than those The authors thank Dr. Jim Mintz and the UCLA Semel Institute Bio-
with everyday functional outcome, given that improve- statistical Unit for developing the data entry systems and Bi-Hong
Deng for her help in data management and preparation of the ta-
ments in functional capacity may still require additional bles. The following staff members at the UCLA-VA site coordinated
rehabilitation in specific daily living or work skills to be the training and quality assurance procedures: Karen Cornelius,
Psy.D., Kimmy Kee, Ph.D., Mark McGee, Ayala Ofek, and Mark Sergi,
translated into community functioning.
Ph.D. Training and quality assurance for the co-primary measures
Representatives of the FDA indicated to the MATRICS was provided by Alan Bellack, Ph.D., Robert Bilder, Ph.D., Sherry
Neurocognition Committee that any of the four co-pri- Goldman, M.A., Thomas Patterson, Ph.D., Margaret Poe, Shannon
Thomas-Lohrman, M.S., and Joseph Ventura, Ph.D.
mary measures would be acceptable at this point for use in Dr. Fenton died in September 2006.
clinical trials. However, given the early stage of method de-
velopment in this area, the Neurocognition Committee ex-
pects that stronger measures using these approaches, or Acknowledgment
using entirely different approaches to assessment, might
Other members of the MATRICS Outcomes Committee included
be developed. This is a fertile area and one in which devel- Jean Addington, Robert Heinssen, Richard Mohs, Thomas Patter-
opments are occurring at a rapid pace. The importance of son, and Dawn Velligan.
functional assessment for serious mental disorders and its
role in drug evaluation has been reflected in several recent References
developments. For example, a new program at NIMH, 1. Marder SR, Fenton WS: Measurement and treatment research
Functional Assessment in Mental Disorders, has recently to improve cognition in schizophrenia: NIMH MATRICS initia-
been created. Also, a new academic/industry consortium tive to support the development of agents for improving cog-
(MATRICS-Co-Primary and Translation) has been formed nition in schizophrenia. Schizophr Res 2004; 72:5–10
2. Green MF, Nuechterlein KH, Gold JM, Barch DM, Cohen J, Es-
to facilitate the evaluation of potential co-primary mea-
sock S, Fenton WS, Frese F, Goldberg TE, Heaton RK, Keefe RSE,
sures for use in clinical trials. Finally, NIMH recently spon- Kern RS, Kraemer H, Stover E, Weinberger DR, Zalcman S,
sored a consensus meeting on functional assessment for Marder SR: Approaching a consensus cognitive battery for clin-
psychiatric disorders (21). Hence, the results presented in ical trials in schizophrenia: the NIMH-MATRICS conference to
the current article should be viewed as a good starting select cognitive domains and test criteria. Biol Psychiatry 2004;
56:301–307
point for evaluation, comparison, and discussion of poten-
3. Buchanan RW, Davis M, Goff D, Green MF, Keefe RSE, Leon AC,
tial functionally meaningful co-primary measures, with ex- Nuechterlein KH, Laughren T, Levin R, Stover E, Fenton W,
pectations that future developments will lead to improved Marder SR: A summary of the FDA-NIMH-MATRICS workshop
tools in this domain. on clinical trial design for neurocognitive drugs for schizophre-
nia. Schizophr Bull 2005; 31:5–19
4. Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch D, Cohen
Received Jan. 13, 2007; revisions received July 6 and Aug. 12, 2007;
accepted Aug. 16, 2007 (doi:10.1176/appi.ajp.2007.07010089). From J, Essock S, Fenton WS, Frese FJ, Gold JM, Goldberg T, Heaton R,
the Semel Institute for Neuroscience and Human Behavior and the Keefe RSE, Kraemer H, Mesholam-Gately R, Seidman LJ, Stover E,
Department of Psychology, Geffen School of Medicine, UCLA; the VA Weinberger DR, Young AS, Zalcman S, Marder SR: The MATRICS
Greater Los Angeles Healthcare System, Los Angeles; the University of Consensus Cognitive Battery: part 1, test selection, reliability,
Kansas School of Medicine, Wichita, Kan.; NIMH, Bethesda, Md.; the and validity. Am J Psychiatry (published online January 2,
Maryland Psychiatric Research Center, University of Maryland School 2008; doi: 10.1176/appi.ajp.2007.07010042)
of Medicine, Baltimore; the Department of Psychiatry and Behavioral 5. Kern RS, Nuechterlein KH, Green MF, Baade LE, Fenton WS, Gold
Sciences, Duke University, Durham, N.C.; the Public Psychiatry Divi-
JM, Keefe RSE, Mesholam-Gately R, Mintz J, Seidman LJ, Stover E,
sion, Department of Psychiatry, Beth Israel Deaconess Medical Center,
Marder SR: The MATRICS Consensus Cognitive Battery: part 2, co-
Massachusetts Mental Health Center, Boston; and the Department of
norming and standardization. Am J Psychiatry (published online
Psychiatry, Harvard Medical School, Boston. Address correspondence
and reprint requests to Dr. Green, Semel Institute for Neuroscience January 2, 2008; doi: 10.1176/appi.ajp.2007.07010043)
and Human Behavior, UCLA, 300 Medical Plaza, Rm. 2263, Los Ange- 6. Nuechterlein KH, Green MF: MATRICS Consensus Cognitive Bat-
les, CA 90095-6968; mgreen@ucla.edu (e-mail). tery. Los Angeles, MATRICS Assessment, 2006
Dr. Keefe has received funding from Abbot, AstraZeneca, Dainip- 7. Brekke JS, Kay DD, Kee KS, Green MF: Biosocial pathways to
pon Sumitomo, Forest, Gabriel, GlaxoSmithKline, Memory, Otsuka, functional outcome in schizophrenia. Schizophr Res 2005; 80:
Pfizer, Repligen, Saegis, Bristol-Myers Squibb, Cephalon, Eli Lilly, 213–225
Johnson & Johnson, Lundbeck, Merck, Orexigen, Sanofi-Aventis, Xe-
8. Vauth R, Rusch N, Wirtz M, Corrigan PW: Does social cognition
noport. He receives royalties from the Brief Assessment of Cognition
influence the relation between neurocognitive deficits and vo-
and the MATRICS Battery. He has received grants from Organon,
cational functioning in schizophrenia? Psychiatry Res 2004;
NIMH, Pfizer, Eli Lilly, and AstraZeneca. Dr. Green has consulted for Eli
Lilly, Otsuka, Lundbeck, Bristol-Myers Squibb, Abott, Sanofi-Aventis, 128:155–165
Memory, Solvay, and Astellas. Dr. Marder has received funds from 9. Sergi MJ, Rassovsky Y, Nuechterlein KH, Green MF: Social per-
Bristol-Myers Squibb, Otsuka, Solvay, Pfizer, Merck, Roche, and Wy- ception as a mediator of the influence of early visual process-
Am J Psychiatry 165:2, February 2008 ajp.psychiatryonline.org 227
RESULTS FROM THE MATRICS STUDY
ing on functional status in schizophrenia. Am J Psychiatry 16. Keefe RS, Poe M, Walker TM, Kang JW, Harvey PD: The Schizo-
2006; 163:448–454 phrenia Cognition Rating Scale: an interview-based assessment
10. Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD: and its relationship to cognition, real-world functioning, and
Determinants of real-world functional performance in schizo- functional capacity. Am J Psychiatry 2006; 163:426–432
phrenia subjects: correlations with cognition, functional capac- 17. Ventura J, Cienfuegos A, Boxer O, Bilder RM: Clinical Global Im-
ity, and symptoms. Am J Psychiatry 2006; 163:418–425 pression of Cognition in Schizophrenia (CGI-CogS): reliability
11. Brekke JS, Long JD, Nesbitt N, Sobel E: The impact of service and validity of a co-primary measure of cognition. Schizophr
characteristics from community support programs for persons Res (in press)
with schizophrenia: a growth curve analysis. J Consult Clin Psy- 18. Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV: UCSD
chol 1997; 65:464–475 Performance-Based Skills Assessment: development of a new
measure of everyday functioning for severely mentally ill
12. McKibbin CL, Brekke JS, Sires D, Jeste DV, Patterson TL: Direct
adults. Schizophr Bull 2001; 27:235–245
assessment of functional abilities: relevance to persons with
19. Birchwood M, Smith J, Cochran R, Wetton S, Copestake S: The
schizophrenia. Schizophr Res 2004; 72:53–67
Social Functioning Scale: the development and validation of a
13. Bellack AS, Sayers M, Mueser K, Bennett M: Evaluation of social new scale of social adjustment for use in family intervention
problem solving in schizophrenia. J Abnorm Psychol 1994; programs with schizophrenic patients. Br J Psychiatry 1990;
103:371–378 157:853–859
14. Dunning D, Heath C, Suls JM: Flawed self-assessment: implica- 20. Weissman M, Paykel E: The Depressed Woman: A Study of So-
tions for health, education, and the workplace. Psychol Science cial Relationships. Chicago, University of Chicago Press, 1974
in the Public Interest 2004; 5:69–106 21. Bellack AS, Green MF, Cook JA, Fenton W, Harvey PD, Heaton
15. Mortiz S, Ferahli S, Naber D: Memory and attention perfor- RK, Laughren T, Leon AC, Mayo D, Patrick DL, Patterson TL,
mance in psychiatric patients: lack of correspondence be- Rose A, Stover E, Wykes T: Assessment of community function-
tween clinician-rated and patient-rated functioning with neu- ing in people with schizophrenia and other severe mental ill-
ropsychological test results. J Int Neuropsychol Soc 2004; 10: nesses: a white paper based on an NIMH-sponsored workshop.
623–633 Schizophr Bull 2007; 33:805–822
228 ajp.psychiatryonline.org Am J Psychiatry 165:2, February 2008
You might also like
- Mayer-Salovey-Caruso Emotional Intelligence Test (Msceit)Document2 pagesMayer-Salovey-Caruso Emotional Intelligence Test (Msceit)DrMartens AG50% (2)
- Essay WritingDocument74 pagesEssay Writingtiendn92% (50)
- Davis Langdon Africa Handbook Jan 2009Document94 pagesDavis Langdon Africa Handbook Jan 2009Caesar 'Dee' Rethabile SerumulaNo ratings yet
- PSSR FormDocument16 pagesPSSR Formmythee100% (6)
- Evidence For Effective Interventions To Reduce Mental Health-Related Stigma and Discrimination in The Medium and Long Term: Systematic ReviewDocument51 pagesEvidence For Effective Interventions To Reduce Mental Health-Related Stigma and Discrimination in The Medium and Long Term: Systematic ReviewkinasihasyaNo ratings yet
- A Meta-Analysis of Cognitive Remediation in SchizophreniaDocument12 pagesA Meta-Analysis of Cognitive Remediation in Schizophreniamohitnet1327No ratings yet
- The Impact of Treatment Components SuggeDocument42 pagesThe Impact of Treatment Components Suggeaqsarajpoot2224No ratings yet
- A Meta-Analysis of Cognitive Remediation in SchizophreniaDocument12 pagesA Meta-Analysis of Cognitive Remediation in Schizophreniaisaacelias2509No ratings yet
- Estudio PilotoDocument9 pagesEstudio PilotoNina SalinasNo ratings yet
- CERQDocument21 pagesCERQsmacujaNo ratings yet
- Exercise and Sleep: A Systematic Review of Previous Meta-AnalysesDocument11 pagesExercise and Sleep: A Systematic Review of Previous Meta-AnalysesAlexPsrNo ratings yet
- Nihms 564241Document33 pagesNihms 564241Natalia BettancourtNo ratings yet
- The Efficacy of Cognitive Intervention in Mild Cognitive Impairment (MCI) : A Meta-Analysis of Outcomes On Neuropsychological MeasuresDocument45 pagesThe Efficacy of Cognitive Intervention in Mild Cognitive Impairment (MCI) : A Meta-Analysis of Outcomes On Neuropsychological MeasuresAlejandra GutiérrezNo ratings yet
- Clase 1 Lambert Et Al. - 1996 - The Reliability and Validity of The Outcome QuestionnaireDocument11 pagesClase 1 Lambert Et Al. - 1996 - The Reliability and Validity of The Outcome QuestionnaireLuis GaribottiNo ratings yet
- Ireland Clough Day 2017Document21 pagesIreland Clough Day 2017ShilpaNo ratings yet
- E025761 FullDocument6 pagesE025761 Full2021-110737No ratings yet
- Retest Reliabilities of Decision-Making and Cognitive Control Measures in Addictive DisordersDocument21 pagesRetest Reliabilities of Decision-Making and Cognitive Control Measures in Addictive DisordersRafael MartinsNo ratings yet
- Mindfulness SRDocument22 pagesMindfulness SRlea.clairetersouNo ratings yet
- FMCH 2021 001154Document7 pagesFMCH 2021 001154Vinayak NagriNo ratings yet
- 1 s2.0 S019188699900152X MainDocument12 pages1 s2.0 S019188699900152X MaingorkiptNo ratings yet
- Terapia BreveDocument18 pagesTerapia BreveFanny ZumárragaNo ratings yet
- The Transtheoretical Model's Processes of Change in The Heart of A Physical Activity Intervention A Series of N-Of-1 PDFDocument28 pagesThe Transtheoretical Model's Processes of Change in The Heart of A Physical Activity Intervention A Series of N-Of-1 PDFreymarkNo ratings yet
- 2 ManuscriptDocument66 pages2 ManuscriptRodrigo SilvaNo ratings yet
- Impact of Behavior ManagementPrograms On Exercise AdherenceDocument4 pagesImpact of Behavior ManagementPrograms On Exercise Adherencejhonnydm93No ratings yet
- Using Psychometric Techniques To Improve The Balance Evaluation Systems Test: The Mini-BestestDocument9 pagesUsing Psychometric Techniques To Improve The Balance Evaluation Systems Test: The Mini-BestestMochammad Syarif HidayatNo ratings yet
- SCM 37 371Document9 pagesSCM 37 371werazamaraNo ratings yet
- Improving Memory Performance in The Aged Through Mnemonic Training: A Meta-Analytic StudyDocument10 pagesImproving Memory Performance in The Aged Through Mnemonic Training: A Meta-Analytic Studypaulverhaeghen6877No ratings yet
- Borkovec93 CBT GadDocument15 pagesBorkovec93 CBT GadAlexa CiucăNo ratings yet
- Abnormal Psychology Cap4Document28 pagesAbnormal Psychology Cap4JuanNo ratings yet
- Art NueveDocument22 pagesArt NueveANTONIO REYES MEDINANo ratings yet
- VanWyk Possible (2003) PDFDocument8 pagesVanWyk Possible (2003) PDFLauren BrionesNo ratings yet
- ART 3 The Mental Health Literacy ScaleDocument6 pagesART 3 The Mental Health Literacy Scaleshireensaghir05No ratings yet
- ACT Psychosis Sistematic and MetaanalysisDocument13 pagesACT Psychosis Sistematic and MetaanalysisParla CardoNo ratings yet
- The Impact of Physical Activity On Brain Structure and Function in Youth - A Systematic ReviewDocument17 pagesThe Impact of Physical Activity On Brain Structure and Function in Youth - A Systematic ReviewSơn Đoàn TrungNo ratings yet
- Clinical Child and Family Psychology Review Volume 4 Issue 1 2001 (Doi 10.1023/a:1009528727345) Michael P. Bates - The Child and Adolescent Functional Assessment Scale (CAFAS) - Review and CurDocument22 pagesClinical Child and Family Psychology Review Volume 4 Issue 1 2001 (Doi 10.1023/a:1009528727345) Michael P. Bates - The Child and Adolescent Functional Assessment Scale (CAFAS) - Review and CurJesterJokerNo ratings yet
- Applied Behaviour Analysis and Standard Treatment in Intellectual Disability 2year OutcomesDocument2 pagesApplied Behaviour Analysis and Standard Treatment in Intellectual Disability 2year OutcomesAmira naser3579No ratings yet
- 2020 Cognition-Oriented Treatments For Older Adults - A Systematic Overview of Systematic Reviews2020Document27 pages2020 Cognition-Oriented Treatments For Older Adults - A Systematic Overview of Systematic Reviews2020maugelinNo ratings yet
- Joyce Et Al 2018.PMID - 29903782Document9 pagesJoyce Et Al 2018.PMID - 29903782Ara PalmaNo ratings yet
- 1 s2.0 S0920996414001698 MainDocument6 pages1 s2.0 S0920996414001698 MainJulieta AzevedoNo ratings yet
- Behavioral and Cognitive Impacts of Mindfulness-Based Interventions On Adults With ADHDDocument16 pagesBehavioral and Cognitive Impacts of Mindfulness-Based Interventions On Adults With ADHDDavid ZNo ratings yet
- MCQ 2Document9 pagesMCQ 2Munni KNo ratings yet
- The e Ect of Active Video Games On Cognitive Functioning in Clinical and Non-Clinical Populations A Meta-Analysis of Randomized Controlled TrialsDocument10 pagesThe e Ect of Active Video Games On Cognitive Functioning in Clinical and Non-Clinical Populations A Meta-Analysis of Randomized Controlled TrialsFaiz KunNo ratings yet
- Matrics - Confiabilidad y Validez pt1 PDFDocument11 pagesMatrics - Confiabilidad y Validez pt1 PDFDrMartens AGNo ratings yet
- The Use of The Theory of Planned Behavior To Predict Factors Influencing Physicians' Decision To Prescribe Extemporaneous Compounding Dosage Form For Pediatric OutpatientsDocument4 pagesThe Use of The Theory of Planned Behavior To Predict Factors Influencing Physicians' Decision To Prescribe Extemporaneous Compounding Dosage Form For Pediatric OutpatientsmeliNo ratings yet
- Using Generic Preferencebased Measures in Mental Health Psychometric Validity of The Eq5d and Sf6dDocument8 pagesUsing Generic Preferencebased Measures in Mental Health Psychometric Validity of The Eq5d and Sf6dJulaiha QosimNo ratings yet
- Satipatthana Mindfulness Meditation Annotated Bibliography 3-2024 2Document234 pagesSatipatthana Mindfulness Meditation Annotated Bibliography 3-2024 2bonduranNo ratings yet
- Study DrugsDocument22 pagesStudy Drugsnicole.mifsud.22No ratings yet
- Cognitive Interventions in Healthy Older Adults and People With Mild Cognitive Impairment - A Systematic ReviewDocument13 pagesCognitive Interventions in Healthy Older Adults and People With Mild Cognitive Impairment - A Systematic Reviewmadalena limaNo ratings yet
- Workplace StressDocument10 pagesWorkplace Stresspinku13No ratings yet
- ARandomized Controlled Pilot Studyofthe Effectivenessof Occupational Therapyfor Children With Sensory Modulation DisorderDocument12 pagesARandomized Controlled Pilot Studyofthe Effectivenessof Occupational Therapyfor Children With Sensory Modulation Disordertayna santosNo ratings yet
- The Functional Idiographic Assessment Template Ques - 2014 - Journal of ContextuDocument12 pagesThe Functional Idiographic Assessment Template Ques - 2014 - Journal of Contextudomingo jesus de la rosa diazNo ratings yet
- Types of Psychological TestsDocument4 pagesTypes of Psychological TestsScribdTranslationsNo ratings yet
- Evidence Based TableDocument13 pagesEvidence Based Tableneometal_86No ratings yet
- Ccoryn, Journal Editor, AllerDocument17 pagesCcoryn, Journal Editor, AllerKayu LowNo ratings yet
- Are We Improving? Update and Critical Appraisal of The Reporting of Decision Process and Quality Measures in Trials Evaluating Patient Decision AidsDocument6 pagesAre We Improving? Update and Critical Appraisal of The Reporting of Decision Process and Quality Measures in Trials Evaluating Patient Decision AidsThu ThảoNo ratings yet
- Development and Evaluation of A Scale To With Arthritis Measure Perceived Self-Efficacy in PeopleDocument8 pagesDevelopment and Evaluation of A Scale To With Arthritis Measure Perceived Self-Efficacy in PeopleSiti lestarinurhamidahNo ratings yet
- Using Psychometric Techniques To Improve The Balance Evaluation System's Test - The Mini-BESTestDocument17 pagesUsing Psychometric Techniques To Improve The Balance Evaluation System's Test - The Mini-BESTestizabelle paesNo ratings yet
- A Brief Measure For Assessing Generalized Anxiety Disorder: The GAD-7Document6 pagesA Brief Measure For Assessing Generalized Anxiety Disorder: The GAD-7Von Jezzrel Jumao-asNo ratings yet
- Emotional IntelligenceDocument13 pagesEmotional Intelligencedanamaria13No ratings yet
- Coelho - Ylvisaker - Turkstra Non-Stand Assess Sem 2005 PDFDocument19 pagesCoelho - Ylvisaker - Turkstra Non-Stand Assess Sem 2005 PDFGaoudam NatarajanNo ratings yet
- Basics of Psychological AssessmentsDocument35 pagesBasics of Psychological AssessmentsKarishma Tiwari100% (1)
- 1 s2.0 S1876201821004536 MainDocument7 pages1 s2.0 S1876201821004536 Mainwatch2303No ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet
- Dimensional PsychopathologyFrom EverandDimensional PsychopathologyMassimo BiondiNo ratings yet
- Ox B2 Test 2 AudioscriptDocument5 pagesOx B2 Test 2 AudioscriptDrMartens AGNo ratings yet
- Oxford Writing TipsDocument64 pagesOxford Writing TipsDrMartens AG100% (1)
- Oxfrod B2 Practice Test 1 Answer KeyDocument6 pagesOxfrod B2 Practice Test 1 Answer KeyDrMartens AGNo ratings yet
- Prepositional Phrase Examples: A Big List of 160+ Prepositional PhrasesDocument13 pagesPrepositional Phrase Examples: A Big List of 160+ Prepositional PhrasesDrMartens AGNo ratings yet
- EMDR Metaanlisis EstudioDocument12 pagesEMDR Metaanlisis EstudioDrMartens AGNo ratings yet
- Screening For Personality Disorders Among PDFDocument14 pagesScreening For Personality Disorders Among PDFDrMartens AGNo ratings yet
- Revising Axis V For A Review of Measures of Social FunctioningDocument9 pagesRevising Axis V For A Review of Measures of Social FunctioningDrMartens AGNo ratings yet
- Matrics - Confiabilidad y Validez pt1 PDFDocument11 pagesMatrics - Confiabilidad y Validez pt1 PDFDrMartens AGNo ratings yet
- Neuropsychological Profile in Early-Onset Schizophrenia-Spectrum Disorders: Measured With The MATRICS BatteryDocument8 pagesNeuropsychological Profile in Early-Onset Schizophrenia-Spectrum Disorders: Measured With The MATRICS BatteryDrMartens AGNo ratings yet
- Esquizo ITP 2011Document4 pagesEsquizo ITP 2011DrMartens AGNo ratings yet
- Wto 4Document24 pagesWto 4Tabish AhmedNo ratings yet
- Lecture 3: Solving Linear Systems: Elif TanDocument20 pagesLecture 3: Solving Linear Systems: Elif Tansercan egilmezkolNo ratings yet
- Meitei Mayek: Typeface Design (M. Thesis Presentation)Document53 pagesMeitei Mayek: Typeface Design (M. Thesis Presentation)ishanidayal536No ratings yet
- SPP No. 200 Code of Ethical ConductDocument24 pagesSPP No. 200 Code of Ethical ConductShann HortalezaNo ratings yet
- CadburyDocument12 pagesCadburymldc20110% (1)
- Lesson Plan Convection With AnswersDocument3 pagesLesson Plan Convection With AnswersQueencess Ara TorresNo ratings yet
- Sundram Fasteners Limited, HosurDocument38 pagesSundram Fasteners Limited, Hosurjaydeepsinh100% (1)
- CVS 4150 & 4160 Pressure Controller July 2012Document12 pagesCVS 4150 & 4160 Pressure Controller July 2012Zts MksNo ratings yet
- Presentation Alfa Laval Corrosion Charts For Plate Heat ExchangersDocument5 pagesPresentation Alfa Laval Corrosion Charts For Plate Heat ExchangersNasrin AkhondiNo ratings yet
- Emile Agnel Trio Oboe Cello PianoDocument52 pagesEmile Agnel Trio Oboe Cello PianoVíctor Lazo100% (1)
- Advances in Computer Entertainment: Dennis Reidsma Haruhiro Katayose Anton NijholtDocument692 pagesAdvances in Computer Entertainment: Dennis Reidsma Haruhiro Katayose Anton NijholtMauro GasparofNo ratings yet
- PRC Case Completion Form For Midwifery ExamsDocument2 pagesPRC Case Completion Form For Midwifery ExamsNoel84% (31)
- Categories Business-To-Consumer (B2C) (: Identify The Major Categories and Trends of E-Commerce Applications. E CommerceDocument9 pagesCategories Business-To-Consumer (B2C) (: Identify The Major Categories and Trends of E-Commerce Applications. E CommerceHajra NoorNo ratings yet
- Catalog CMT 2012Document302 pagesCatalog CMT 2012Cornelia BuriceaNo ratings yet
- CHAPTER 4 (Review Questions) : Direction: Read Each Question Carefully. Encircle The Letter of The Correct AnswerDocument11 pagesCHAPTER 4 (Review Questions) : Direction: Read Each Question Carefully. Encircle The Letter of The Correct AnswerChery PerialdeNo ratings yet
- Efficient Approach For ISL Using MLDocument4 pagesEfficient Approach For ISL Using MLsugar cubeNo ratings yet
- Ibs Company ProfileDocument52 pagesIbs Company ProfileFaeez ZainNo ratings yet
- Are You Fit For ISO 16890?: Thomas SchrothDocument16 pagesAre You Fit For ISO 16890?: Thomas SchrothUdhayakumar Venkataraman100% (1)
- Pigeonhole PrincipleDocument5 pagesPigeonhole PrincipleNoisyPoisyNo ratings yet
- Lesson 4 - History of Development Economics (First Part)Document12 pagesLesson 4 - History of Development Economics (First Part)Rose RaboNo ratings yet
- t2 M 5870 Differentiated Multistep Problems Involving Addition and Subtraction Activity Sheets - Ver - 1Document9 pagest2 M 5870 Differentiated Multistep Problems Involving Addition and Subtraction Activity Sheets - Ver - 1Chitra ThadaniNo ratings yet
- Rezene Business PlanDocument37 pagesRezene Business PlanMehari GebreyohannesNo ratings yet
- Bayview's Last Stand: Protecting Historic Black Neighborhoods - John William Templeton Speaker FilmmakerDocument5 pagesBayview's Last Stand: Protecting Historic Black Neighborhoods - John William Templeton Speaker FilmmakerJW TempletonNo ratings yet
- How Disruptive Technologies Are Opening Up Innovative Opportunities in ServicesDocument10 pagesHow Disruptive Technologies Are Opening Up Innovative Opportunities in ServicesSachin SengarNo ratings yet
- Barney Smca6 Tif 05Document31 pagesBarney Smca6 Tif 05p astelNo ratings yet
- 10 CarbohydratesDocument6 pages10 CarbohydratesBryanNo ratings yet
- WMO Guidelines On Surface Station Data Quality Assurance For Climate ApplicationsDocument74 pagesWMO Guidelines On Surface Station Data Quality Assurance For Climate ApplicationsGEMPFNo ratings yet
- Eddie The Carpet FitterDocument3 pagesEddie The Carpet Fittermaria praveenNo ratings yet