Professional Documents
Culture Documents
Title: The Effectiveness of Pulsed Radiofrequency On Joint Pain: A Narrative Review Running Title: PRF On Joint Pain
Title: The Effectiveness of Pulsed Radiofrequency On Joint Pain: A Narrative Review Running Title: PRF On Joint Pain
Uploaded by
Humberto Salas VelizOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Title: The Effectiveness of Pulsed Radiofrequency On Joint Pain: A Narrative Review Running Title: PRF On Joint Pain
Title: The Effectiveness of Pulsed Radiofrequency On Joint Pain: A Narrative Review Running Title: PRF On Joint Pain
Uploaded by
Humberto Salas VelizCopyright:
Available Formats
Accepted Article
DR. MATHIEU BOUDIER-REVÉRET (Orcid ID : 0000-0003-0259-8520)
DR. MIN CHEOL CHANG (Orcid ID : 0000-0002-7629-7213)
Article type : Review
Title: The Effectiveness of Pulsed Radiofrequency on Joint Pain: A Narrative Review
Running Title: PRF on Joint Pain
Mathieu Boudier-Revéret, MD 1; Aung Chan Thu, MD2; Ming-Yen Hsiao, MD3; Shaw-Gang Shyu,
MD3; Min Cheol Chang, MD4*
1Department of Physical Medicine and Rehabilitation, University of Montreal Health Center,
Montreal, Canada
2Department of Physical Medicine and Rehabilitation, Ministry of Health and Sports, Myanmar
3Department of Physical Medicine and Rehabilitation, National Taiwan University Hospital, College
of Medicine, National Taiwan University, Taipei, Taiwan
4Department of Rehabilitation Medicine, College of Medicine, Yeungnam University, Daegu,
Republic of Korea
This article has been accepted for publication and undergone full peer review but has not been through the
copyediting, typesetting, pagination and proofreading process, which may lead to differences between this
version and the Version of Record. Please cite this article as doi: 10.1111/PAPR.12863
This article is protected by copyright. All rights reserved
*Corresponding author: Min Cheol Chang
Accepted Article
Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University
317-1, Daemyungdong, Namku, Taegu, 705-717, Republic of Korea
Tel: +82-53-620-4682, E-mail: wheel633@gmail.com
Funding: The present study was supported by a National Research Foundation of Korea grant funded
by the Korean government (grant no. NRF-2019R1F1A1061348).
No conflicts of interest to declare
Keywords: Pulsed radiofrequency; Joint pain; Chronic pain
This article is protected by copyright. All rights reserved
Summary
Accepted Article
We reviewed the literature on the efficacy of pulsed radiofrequency (PRF) for controlling pain from
joint disorders. PRF seems to be a valid tool for controlling cervical and lumbar facet, sacroiliac, knee,
and glenogumeral joint pain. However, for more widespread application of PRF, more high-quality
studies are needed to confirm the benefits of PRF on pain originating from these joints.
Abstract
Background: PRF stimulation has been safely and effectively applied for controlling various types of
pain.
Purpose: We reviewed the literature on the efficacy of pulsed radiofrequency (PRF) for controlling
pain in joint disorders.
Methods and materials: We searched PubMed for papers published until Sep 7, 2019 that used PRF
to treat pain due to joint disorders. The key search phrases for identifying potentially relevant articles
were (PRF AND joint) OR (PRF AND arthritis) OR (PRF AND arthropathy). The following inclusion
criteria were applied for the selection of articles: 1) patients’ pain was caused by joint disorders; 2)
PRF stimulation was applied to manage joint-origin pain; and 3) after PRF stimulation, follow-up
evaluation was performed to assess the reduction in pain intensity. Moreover, joints with more than 3
reported PRF studies were included in our review.
Results: The primary literature search yielded 141 relevant papers. After reading their titles and
abstracts and assessing their eligibility based on the full-text articles, we finally included 34
publications in this review. Based on the positive therapeutic outcomes of previous studies, PRF
stimulation seems to be an effective treatment for cervical and lumbar facet, sacroiliac, knee, and
glenohumeral joint pain. PRF appears to be beneficial. For confirmation of the effectiveness of PRF
on joint pain, more high-quality studies are needed.
Conclusions: Our review provides insights on the degree of evidence according to pain in each joint,
which will help clinicians make informed decisions for using PRF stimulation in various joint pain
conditions.
This article is protected by copyright. All rights reserved
Abbreviations: pulsed radiofrequency; joint pain; chronic pain
Accepted Article
Introduction
Joint pain is a common problem in clinical practice, resulting in functional impairment and
decreased quality of life.1 This results from arthritis and injury, and factors like muscle weakness,
obesity, mechanical stress, and abnormal joint mechanics, which make joints vulnerable.1 For the
management of joint pain, several oral medications, modalities, and procedures are being used.
However, despite the use of various treatment methods, some patients still suffer from chronic joint
pain. To alleviate joint pain, corticosteroid injections (CSIs) are widely used in clinical practice.2-4
However, their effect is only sustained over the short-term and several adverse effects, including
tissue atrophy, fat necrosis, deterioration of the articular cartilage, crystal-induced synovitis,
hematoma, vascular necrosis, and sepsis, can occur.5, 6
Continuous radiofrequency (CRF) treatments have been used for approximately 40 years for
various medical conditions, including radicular pain, trigeminal neuralgia, joint pain, and myofascial
pain.7-9 It ablates the nerves or tissues by increasing the temperature around the RF needle tip.10
However, CRF causes diffuse tissue damage due to destructive temperatures.10 To overcome its
destructive adverse effect, pulsed radiofrequency (PRF) was developed. In PRF, the tissue
temperature reaches a maximum of 42°C, which prevents the unwanted adverse effect of irreversible
tissue damage.11-13 In the early days after its development, PRF stimulation was used to control
several types of neuropathic pain. Recently, several studies have demonstrated positive therapeutic
effects of PRF on joint pain.
Although the exact mechanism of PRF on reducing joint pain has not been clearly elucidated,
some possible mechanisms can be suggested. PRF alters the pain transmission secondary to the
phenomenon known as long-term depression and inhibits pain impulse propagation.14 Moreover, PRF
is reported to result in damage to mitochondria, microtubules, and microfilaments of the smaller
sensory nociceptors (C-fibers and A-delta fibers) without lesions on the larger non-pain related
sensory fibers (A-beta fiber).15 The 2 methods of PRF treatment are being applied to reduce joint pain.
First, PRF stimulation can be applied on nerves that transfer pain signals from joints to the spinal cord
This article is protected by copyright. All rights reserved
and brain.16 Second, intra-articular (IA) PRF stimulation can be used.17 These 2 methods of PRF
Accepted Article
treatment reduce pain through the same mechanism. Nerve and IA PRF stimulations would inhibit
transmission of pain information via the above-mentioned mechanisms.16 Regarding IA PRF
stimulation, the articular capsule is richly innervated by pain-generating afferent nerves or free nerve
endings.18 The electrical field produced by PRF could alter the pain signal from these nociceptive
nerve fibers and result in their microscopic damage. Moreover, the reflective character of bone could
enhance the effect of IA PRF stimulation on capsular nerve endings.17 Additionally, IA PRF
stimulation may reduce inflammation.17 The electrical field from PRF affects the production of pro-
inflammatory and inflammatory cytokines.17 After application of IA PRF, serum C-reactive protein
and cytokines were reported to be reduced.
In the current article, we reviewed studies to determine the effectiveness of PRF to manage
pain from joint disorders.
Methods and materials
The MEDLINE database (PubMed) was searched for articles published before Sep 7, 2019 by
using the following key phrase: (PRF AND joint) OR (PRF AND arthritis) OR (PRF AND
arthropathy). The following inclusion criteria were applied for the selection of articles: 1) patients’
pain was caused by joint disorders; 2) PRF stimulation was applied to manage joint-origin pain; and
3) after PRF stimulation, follow-up evaluation was performed to assess the reduction in pain intensity.
Review articles were excluded. Moreover, joints with more than 3 reported PRF studies were included
in our review.
Results
A total of 141 potentially relevant articles were found in the primary literature search. After
reading the titles and abstracts and assessing them for eligibility based on the full-text articles, 34
articles were finally included in the review (Table 1). Among the involved articles, PRF was used on
patients with pain from cervical joint in 6 studies16, 17, 19-22, lumbosacral joint in 10 studies19, 23-31,
sacroiliac joint (SI) in 5 studies12, 32-35, knee joint in 8 studies36-43, and glenohumeral (GH) joint in 6
This article is protected by copyright. All rights reserved
studies44-49. During the PRF procedure in all the previous studies except for 1 study33, the patients
Accepted Article
who received PRF treatment did not receive corticosteroid injection concomitantly to the PRF
treatment. In addition, in all the previous studies, the temperature of the catheter tip did not exceed
42°C.
Cervical facet and atlanto-occipital joint pain
To manage cervical joint pain (atlanto-occipital and cervical facet joints), 6 previous studies
evaluated the effectiveness of PRF stimulation.16, 17, 19-22
Of these studies, 2 were randomized trials. In 2017, Lim et al.17 performed IA PRF stimulation
on 20 patients and compared the effects with those of IA CSI in 20 patients. The pain of both groups
significantly decreased 1, 3, and 6 months after each treatment without any difference in therapeutic
effects. In 2018, Shin et al.20 investigated the effects of IA PRF stimulation in atlanto-occipital joint
pain. They performed IA PRF stimulation on 12 patients and IA CSI on 11 patients with atlanto-
occipital joint pain. After 2 procedures, the average pain degree in both groups was significantly
reduced and their effects persisted for at least 6 months, without significant intergroup differences. In
addition, in 2008, Liliang et al.16 performed a prospective observational study to investigate the effect
of PRF stimulation on the cervical medial branch in 14 patients with neck pain induced by whiplash
injuries. At 1-year post-PRF, nine patients (64.3%) showed significant pain reduction. Two
retrospective studies19, 22 and one case report21 also reported good treatment outcomes after medial
branch or intra-articular PRF stimulation.
Lumbosacral facet joint pain
Thus far, 10 previous studies have reported the effect of PRF stimulation on lumbosacral facet
joint pain.19, 23-31 Of these, 4 studies were randomized trials.26-28, 31 In 2007, Tekin et al.31 recruited 60
patients and performed PRF and CRF stimulations (temperature limitation: 80°C, 90 s, 22 gauge) on
the lumbar medial branch, dividing the recruited patients into 3 equal-sized groups (control, PRF, and
CRF groups). Six and 12 months after the procedures, the pain degree of the CRF group was
significantly reduced compared with that at pre-treatment, but the PRF group did not show a
significant pain reduction. In 2008, Kroll et al.28 performed PRF stimulation on the lumbar medial
This article is protected by copyright. All rights reserved
branches of 13 patients and CRF stimulation on lumbar medial branches in 13 patients. While the
Accepted Article
CRF group showed a positive treatment outcome 3 months after treatment, the PRF group showed
negative treatment outcomes at the follow-up evaluation. However, Tekin et al.31 performed the initial
follow-up evaluation only at 6 months after the PRF procedure. Accordingly, the PRF effect within
the first 6 months was not evaluated. Kroll et al.28 performed their study with a small sample size.
In 2014, Hashemi et al.27 compared the effect of PRF stimulation on the lumbar medial branch
(40 patients) with that of IA CSI (40 patients) with degenerative spondylolisthesis. Six weeks after
each procedure, both treatments significantly reduced the initial pain without a significant difference,
but 3 and 6 months after each procedure, the PRF group showed better treatment outcomes than the
IA CSI group. In 2017, Do et al.26 compared IA PRF stimulation and intra-facet joint CSI in 60
patients with lumbosacral facet-joint-origin pain. Both procedures effectively managed pain in both
groups, and their effects persisted for at least 6 months. However, one-month post-treatment, pain
reduction was larger after the CSI compared to IA PRF stimulation, but 3 and 6 months after
treatment, similar effects were shown. Therefore, the positive treatment outcome of PRF stimulation
on each lumbar medial branch and the intra-facet joint was reported in 1 randomized trial.
As for the other 6 previous studies, 2 prospective observational studies24, 25, 3 retrospective
studies19, 23, 29, and one case report30 were reported. In all 6 studies19, 23-25, 29, 30, after medial branch or
intra-articular PRF stimulation, significant pain reduction and functional improvement were observed.
Sacroiliac (SI) joint pain
Up to now, 5 studies have investigated the effect of PRF for SI joint pain, which accounts for
10 to 27% of chronic low back pain.50, 51 Of these, 2 were randomized trials33, 34, 2 were prospective
observational studies12, 35 and 1 was a retrospective study.32 All studies selected patients based on a
combination of history, physical examination, radiological tests, and response to an image-guided
diagnostic SI block with local anesthetics, as suggested by the IASP criteria.52 As for treatment, one
of two approaches have been used for PRF treatment of SI joint pain: IA PRF32, 35 or PRF targeted at
the nerves innervating the SI joint.12, 33, 34
In 2018, Ding et al.33 examined if CT-guided IA CRF (80°C, 180 s) or PRF had similar
efficacy for SI joint pain in 64 patients randomized into 2 groups. During the IA CRF and PRF
This article is protected by copyright. All rights reserved
procedures, one needle was used, and the needle tip was placed within the SI joint. Along with CRF
Accepted Article
or PRF stimulation, both groups were injected with betamethasone 5 mg. In both groups, the visual
analogue scale (VAS) score decreased at one week and the reduction was maintained at 6 and 12
months but was statistically more decreased in the CRF group. Also, in a prospective randomized trial
by Dutta et al.34, 30 patients with diagnostic-block confirmed SI joint pain were recruited and
allocated to 2 groups. The efficacy of PRF applied to sacral lateral branches, L4 medial branch, and
L5 dorsal rami was compared to that of IA CSI. Whereas both groups had a significant decrease in
pain at one month, this improvement was sustained at 3 and 6 months only in the PRF group, with a
proportion of 86.7% still reporting >50% pain relief.
In 2006, Vallejo et al.12 published a prospective study of 22 patients who had SI joint pain
confirmed by >75% relief lasting 1-8h with fluoroscopy-guided SI joint injection on 2 consecutive
occasions. These patients who were refractory to conservative treatment were offered PRF stimulation
on sacral lateral branches, L4 medial branch, and L5 dorsal rami. Out of 22 patients, 16 showed >50%
pain relief, however with variable duration of relief ranging from 6 to 32 weeks.
In 2017, Chang et al.32 retrospectively analyzed therapeutic results of IA PRF stimulation in
20 patients with SI joint pain confirmed by fluoroscopy-guided lidocaine SI injection. However, their
study revealed that IA PRF stimulation was limited in treating SI joint pain: at 3 months after
treatment, only 4/20 patients had a relief of >50%. These results are somewhat in contradiction with
those reported by Karaman et al.35: in a prospective non-randomized study of SI IA fluoroscopy-
guided PRF, 5 out of 9 patients had >50% pain relief at 10 months.
Knee joint pain
A total of 8 studies evaluated PRF for knee joint pain, with much heterogeneity in their
designs. Out of these studies, one was a randomized trial40, 4 were prospective observational studies38,
39, 42, 43 and 3 were retrospective studies.36, 37, 41 Regarding inclusion criteria, most of the patients
suffered from primary knee osteoarthritis (OA), but some had failed total knee arthroplasty with
This article is protected by copyright. All rights reserved
chronic knee pain. For treatment, PRF was either applied intraarticularly38, 40, 41 or periarticularly to
Accepted Article
various combinations of nerves involved in the knee joint innervation.36, 37, 39, 42, 43
In 2017, the effectiveness of IA knee PRF was evaluated by Gulec et al.40 in a randomized
trial of bipolar vs unipolar PRF for chronic knee pain in 100 patients with Kellgren-Lawrence (KL)
grade 2-3 OA. Under fluoroscopic guidance, a catheter was inserted in the medial or lateral sites of
the knee joint, and advanced to the cavity of the knee until the tip was placed in the middle of the joint
space in the transverse plane. At the 3-month outcome, 84% of patients in the bipolar PRF group
reported >50% pain relief as opposed to 50% in the unipolar group, favoring bipolar PRF in this study.
A different approach was adopted by Fucci et al.39 (2013) in a series 25 patients with 47
pathological knees with OA or post-surgical-related knee pain. They were treated by US-guided
sciatic nerve PRF at the level above the popliteal fossa in a prospective trial. The follow-up evaluation
was performed once at 4 weeks post-PRF, and the average VAS improved by 2.7 score. However, 10
out of the 47 procedures did not result in any improvement. In 2014, Vas et al.43 reported a technique
of US-guided PRF to the saphenous, tibial, femoral, and common peroneal nerves along with
subsartorial, peripatellar, and popliteal plexuses. A total of 10 patients with knee OA (KL grades 1 to
4), were enrolled prospectively and exhibited improvement for up to 6 months on both pain and
function scales. Interestingly, the authors performed standard knee X-rays of the participants before
PRF and 1-week post-PRF: they noticed an increase of the tibiofemoral and patellofemoral joint
spaces at 1-week post-PRF.
In 2015, IA PRF was evaluated in 21 patients with advanced knee OA in a prospective study
by Eyigor et al..38 Patients experienced a statistically significant improvement at week 4 on VAS both
at rest and during walking, but not in their walking distance on the 6-minute walk test. At week 12,
most of the benefits had disappeared, except for decreased pain during walking. In a prospective study
by Kesikburun et al. (2016) on ultrasound (US)-guided genicular nerve PRF of 9 patients (15 knees)
who had transiently responded to a lidocaine genicular nerve block (>50% transient relief) but still
had chronic medial knee pain, 6 out of the 9 patients had pain relief of >50% at 3 months.42
In 2011, Akbas et al.36 performed a retrospective study of 115 patients with radiographically
confirmed KL grade 1-3 knee OA on whom fluoroscopy-guided PRF was performed in the region of
This article is protected by copyright. All rights reserved
the infrapatellar branch of the saphenous nerve. They found >50% improvement in their chronic pain
Accepted Article
in all the patients at 6 months. The high level of relief obtained by treating only one of the nerves
responsible for knee-joint pain perception remained unexplained. In the same year, a retrospective
study of 31 patients with chronic knee pain treated with IA PRF revealed that 11 of them had >50%
pain relief at the 6-month follow-up, with a mean VAS decrease of 32.8%.41 Also, in a recently
published retrospective study (2019) on 23 patients with chronic knee pain, out of which 17 had
persistent pain after total knee arthroplasty (TKA), Erdem et al.37 conducted US-guided genicular
nerve PRF. The superior medial, inferior medial and superior lateral genicular nerves were all treated
with PRF. At 3 months, 15 out of 17 TKA patients and 4 out of 6 knee OA patients had >50% pain
relief.
Glenohumeral (GH) joint pain
When narrowing down shoulder pain to GH joint pain, a total of 6 studies were found
pertaining to the effect of PRF. Shoulder pain remains a complex condition with multiple potential
pain generators in a close vicinity. Many studies did not discriminate between intra and extraarticular
components of pain, or exclusively addressed extraarticular structures (e.g. subacromiodeltoid bursa)
and were therefore not included in this review. Most of the studies investigating the therapeutic effect
of PRF on GH joint pain included patients suffering from adhesive capsulitis or GH OA and targeted
the suprascapular nerve. Of the 6 studies, 2 were randomized controlled trials48, 49, 2 were prospective
observational studies45, 46, and 2 were case series.44, 47
In 2014, Wu et al.48 conducted a randomized controlled trial in which US-guided PRF on the
suprascapular nerve followed by 12 weeks of physical therapy was compared to simply 12 weeks of
physical therapy in 60 patients with GH adhesive capsulitis. A total of 42 patients completed the study
and were used for analysis: the PRF group had a significantly greater reduction of VAS at 1 week,
and at 3 months, they also had greater passive ROM gain, and improvement in shoulder pain and
disability index score. Also, in the same year, Yan et al.48 conducted a randomized double-blind
sham-controlled trial on 136 patients with adhesive capsulitis randomized to two groups: 68 were
allocated to the US-guided PRF to “target nerves” (not described in more detail in the article) whereas
This article is protected by copyright. All rights reserved
68 patients were allocated to the sham group in which the same US-guided procedure was carried out,
Accepted Article
but the PRF was never turned on. It is understood from the protocol that this procedure was conducted
on a weekly basis for a total of 12 weeks. After 12 weeks, both groups had improved compared to
baseline regarding pain and 36-items short form health survey scores, but the PRF group had a
statistically significant greater improvement.
In 2007, Kane et al.45 conducted a prospective observational study in which they recruited 12
patients with severe rotator cuff arthropathy unresponsive to IA GH CSI who were not medically fit
enough to be surgical candidates. They were treated with fluoroscopy-guided PRF to the
suprascapular nerve. The VAS score improved in 10 of the 12 patients at 3 months, and effects started
to wean out at 6 months. In 2011, in another prospective observational study performed by Luleci et
al.46, 12 out of 13 patients with GH OA (severity was not mentioned) had >50% improvement on the
numerical rating scale at 6 months after landmark-guided (verified by electrostimulation)
suprascapular nerve PRF.
A small case series (n=3) of patients stipulated to have GH joint pain based on history,
physical and radiological exams who received IA GH PRF was published in 2011.47 All patients
improved at 3 weeks but were back to baseline at 2 months. Another case series of 2 patients with GH
adhesive capsulitis who were treated with US-guided PRF to the suprascapular nerve resulted in
improved ROM and decrease in pain for a period of about 6 months.44
Discussion
Out of 34 previous studies, except for only 2 studies (Kroll et al.’s study28: PRF treatment on
lumbosacral facet joint pain, Chang et al.’s study32: PRF treatment on SI joint pain), PRF effectively
alleviated pain from joint disorders. On the basis of the results of these previous studies, PRF seems
to be effectively applied in patients with joint-origin pain.
For the cervical joint and lumbosacral facet joint pain, via 2 methods (medial branch
stimulation and intraarticular stimulation), researchers controlled the joint pain. PRF stimulation of
the medial branch of the posterior primary ramus inhibits pain signal transmission from the facet joint
This article is protected by copyright. All rights reserved
to the brain.16, 19 In IA PRF stimulation, PRF catheter was inserted into atlanto-occipital or facet
Accepted Article
joints.17, 20-22 Because the cervical joint and lumbosacral facet joint are relatively small, the electrical
fields produced by PRF seem to be able to affect the entire joint.21
Regarding the application of PRF for SI joint pain, despite the positive results in some
previous studies, all of these studies had small number of patients and none of them used a similar
design. Accordingly, it would be hard to draw conclusions on the use of PRF for SI-related pain. It is
nonetheless interesting to note that in the study by Ding at al.33, they obtained better results with IA
CRF compared with IA PRF. This application and safety of IA CRF will also have to be determined
in the future.
All previous studies have reported positive therapeutic effects of PRF on knee and shoulder
joint pain, which suggests that PRF stimulation can be a beneficial method to alleviate knee and
shoulder joint pain. However, similar results need to be reproduced in other well-designed
randomized controlled trials before PRF can become the standard of care for managing knee and
shoulder joint pain.
Conclusion
This review shows that PRF holds promise for treating various joint-related pains, but high-
quality evidence studies are generally lacking. In the 34 articles reviewed, no major adverse effects
were reported, and the trend was toward a positive effect in most of the published studies. In our
opinion, PRF seems to be a valid tool for controlling cervical and lumbar facet, SI, knee, and GH joint
pain. For more widespread application of PRF, more high-quality studies are needed to confirm the
benefits of PRF on pain originating from these joints. Our review provides insights on the degree of
evidence according to each joint, which can help clinicians make informed decisions for using PRF
stimulation in various joint-related pain. In the future, further studies to evaluate the most effective
mode for PRF stimulation and the effect of combination therapy with corticosteroid injection would
be warranted.
This article is protected by copyright. All rights reserved
References
Accepted Article
1. Guglielmo D, Murphy LB, Boring MA, et al. State-Specific Severe Joint Pain and Physical
Inactivity Among Adults with Arthritis - United States, 2017. MMWR Morb Mortal Wkly Rep.
2019;68(17):381-387.
2. Chang MC. The effects of ultrasound-guided corticosteroid injection for the treatment of
hemiplegic shoulder pain on depression and anxiety in patients with chronic stroke. Int J Neurosci.
2017;127(11):958-964.
3. Cushman DM, Ofek E, Syed RH, et al. The Effectiveness of Injected Corticosteroid Type, Dose,
and Volume for the Treatment of Pain in Small- and Intermediate-size Joints: A Systematic Review.
PM R. 2019;11(17):758-770.
4. Rice DA, McNair PJ, Lewis GN, et al. The effects of joint aspiration and intra-articular
corticosteroid injection on flexion reflex excitability, quadriceps strength and pain in individuals with
knee synovitis: a prospective observational study. Arthritis Res Ther. 2015;17:191.
5. Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician.
2002;5(2):182-199.
6. Manchikanti L, Boswell MV, Singh V, et al. Comprehensive evidence-based guidelines for
interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12(4):699-
802.
7. Cosman ER Jr, Gonzalez CD. Bipolar radiofrequency lesion geometry: implications for palisade
treatment of sacroiliac joint pain. Pain Pract. 2011;11(1):3-22.
8. Malik K, Benzon HT. Radiofrequency applications to dorsal root ganglia: a literature review.
Anesthesiology. 2008;109(3):527-542
9. Simopoulos TT, Nagda J, Aner MM. Percutaneous radiofrequency lesioning of the suprascapular
nerve for the management of chronic shoulder pain: a case series. J Pain Res. 2012;5:91-97.
10. Vatansever D, Tekin I, Tuglu I, et al. A comparison of the neuroablative effects of conventional
and pulsed radiofrequency techniques. Clin J Pain. 2008;24(8):717-724.
11. Podhajski RJ, Sekiguchi Y, Kikuchi S, et al. The histologic effects of pulsed and continuous
radiofrequency lesions at 42°C to rat dorsal root ganglion and sciatic nerve. Spine (Phila Pa 1976).
2005;30(9):1008-1013.
This article is protected by copyright. All rights reserved
12. Vallejo R, Benyamin RM, Kramer J, et al. Pulsed radiofrequency for the treatment of sacroiliac
Accepted Article
joint syndrome. Pain Med. 2006;7(5):429-434.
13. West M, Wu H. Pulsed radiofrequency ablation for residual and phantom limb pain: A case series.
Pain Practice. 2010;10(5):485-491.
14. Cosman ER Jr, Cosman ER Sr. Electric and thermal field effects in tissue around radiofrequency
electrodes. Pain Med. 2005;6(6):405–424.
15. Erdine S, Bilir A, Cosman ER, et al. Ultrastructural changes in axons following exposure to
pulsed radiofrequency fields. Pain Pract. 2009;9(6):407-417.
16. Liliang PC, Lu K, Hsieh CH, et al. Pulsed radiofrequency of cervical medial branches for
treatment of whiplash-related cervical zygapophysial joint pain. Surg Neurol. 2008;70 Suppl 1:S1:50-
55; discussion S1:55.
17. Lim JW, Cho YW, Lee DG, et al. Comparison of Intraarticular Pulsed Radiofrequency and
Intraarticular Corticosteroid Injection for Management of Cervical Facet Joint Pain. Pain Physician.
2017;20(6):E961-E967.
18. Chen C, Lu Y, Kallakuri S, et al. Distribution of A-delta and C-fiber receptors in the cervical facet
joint capsule and their response to stretch. J Bone Joint Surg Am. 2006;88(8):1807-1816.
19. Mikeladze G, Espinal R, Finnegan R, et al. Pulsed radiofrequency application in treatment of
chronic zygapophyseal joint pain. Spine J. 2003;3(5):360-362.
20. Shin SM, Kwak SG, Lee DG, et al. Clinical Effectiveness of Intra-articular Pulsed
Radiofrequency Compared to Intra-articular Corticosteroid Injection for Management of Atlanto-
occipital Joint Pain: A Prospective Randomized Controlled Pilot Study. Spine (Phila Pa 1976).
2018;43(11):741-746.
21. Sluijter ME, Teixeira A, Serra V, et al. Intra-articular application of pulsed radiofrequency for
arthrogenic pain--report of six cases. Pain Pract. 2008;8(1):57-61.
22. Tak HJ, Chang MC. Effect of Pulsed Radiofrequency Therapy on Chronic Refractory Atlanto-
Occipital Joint Pain. World Neurosurg. 2018;119:e638-642.
23. Chang MC, Cho YW, Ahn DH, et al. Intraarticular Pulsed Radiofrequency to Treat Refractory
Lumbar Facet Joint Pain in Patients with Low Back Pain. World Neurosurg. 2018;112:e140-144.
This article is protected by copyright. All rights reserved
24. Çetin A, Yektaş A. Evaluation of the Short- and Long-Term Effectiveness of Pulsed
Accepted Article
Radiofrequency and Conventional Radiofrequency Performed for Medial Branch Block in Patients
with Lumbar Facet Joint Pain. Pain Res Manag. 2018;2018:7492753.
25. Colini-Baldeschi G. Evaluation of pulsed radiofrequency denervation in the treatment of chronic
facetjoint pain: an observational study. Anesth Pain Med. 2012 Winter;1(3):168-173.
26. Do KH, Ahn SH, Cho YW, et al. Comparison of intra-articular lumbar facet joint pulsed
radiofrequency and intra-articular lumbar facet joint corticosteroid injection for management of
lumbar facet joint pain: A randomized controlled trial. Medicine (Baltimore). 2017;96:e6524.
27. Hashemi M, Hashemian M, Mohajerani SA, et al. Effect of pulsed radiofrequency in treatment of
facet-joint origin back pain in patients with degenerative spondylolisthesis. Eur Spine J.
2014;23(9):1927-1932.
28. Kroll HR, Kim D, Danic MJ, et al. A randomized, double-blind, prospective study comparing the
efficacy of continuous versus pulsed radiofrequency in the treatment of lumbar facet syndrome. J Clin
Anesth. 2008;20(7):534-537.
29. Lindner R, Sluijter ME, Schleinzer W. Pulsed radiofrequency treatment of the lumbar medial
branch for facet pain: a retrospective analysis. Pain Med 2006;7(5):435-439.
30. Schianchi PM. A new technique to treat facet joint pain with pulsed radiofrequency. Anesth Pain
Med. 2015;5(1):e21061.
31. Tekin I, Mirzai H, Ok G, et al. A comparison of conventional and pulsed radiofrequency
denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23(6):524-529.
32. Chang MC, Ahn SH. The effect of intra-articular stimulation by pulsed radiofrequency on chronic
sacroiliac joint pain refractory to intra-articular corticosteroid injection: A retrospective study.
Medicine (Baltimore). 2017;96:e7367.
33. Ding Y, Li H, Yao P, et al. Clinical observation of CT-guided intra-articular conventional
radiofrequency and pulsed radiofrequency in the treatment of chronic sacroiliac joint pain. J Pain Res.
2018;11:2359-2366.
This article is protected by copyright. All rights reserved
34. Dutta K, Dey S, Bhattacharyya P, et al. Comparison of Efficacy of Lateral Branch Pulsed
Accepted Article
Radiofrequency Denervation and Intraarticular Depot Methylprednisolone Injection for Sacroiliac
Joint Pain. Pain Physician. 2018;21(5):489-496.
35. Karaman H, Tüfek A, Kavak GO, et al. Would pulsed radiofrequency applied to different
anatomical regions have effective results for chronic pain treatment? J Pak Med Assoc.
2011;61(9):879-885.
36. Akbas M, Luleci N, Dere K, et al. Efficacy of pulsed radiofrequency treatment on the saphenous
nerve in patients with chronic knee pain. J Back Musculoskelet Rehabil. 2011;24(2):77-82.
37. Erdem Y, Sir E. The Efficacy of Ultrasound-Guided Pulsed Radiofrequency of Genicular Nerves
in the Treatment of Chronic Knee Pain Due to Severe Degenerative Disease or Previous Total Knee
Arthroplasty. Med Sci Monit. 2019;25:1857-1863.
38. Eyigor C, Eyigor S, Akdeniz S, et al. Effects of intra-articular application of pulsed
radiofrequency on pain, functioning and quality of life in patients with advanced knee osteoarthritis. J
Back Musculoskelet Rehabil. 2015;28(1):129-134.
39. E Djibilian Fucci R, Pascual-Ramírez J, Martínez-Marcos A, et al. Ultrasound-guided sciatic
nerve pulsed radiofrequency for chronic knee pain treatment: a novel approach. J Anesth.
2013;27(6):935-938.
40. Gulec E, Ozbek H, Pektas S, et al. Bipolar Versus Unipolar Intraarticular Pulsed Radiofrequency
Thermocoagulation in Chronic Knee Pain Treatment: A Prospective Randomized Trial. Pain
Physician. 2017;20(3):197-206.
41. Karaman H, Tüfek A, Kavak GÖ, et al. Intra-articularly applied pulsed radiofrequency can reduce
chronic knee pain in patients with osteoarthritis. J Chin Med Assoc. 2011;74(8):336-340.
42. Kesikburun S, Yaşar E, Uran A, et al. Ultrasound-Guided Genicular Nerve Pulsed Radiofrequency
Treatment For Painful Knee Osteoarthritis: A Preliminary Report. Pain Physician. 2016;19(5):E751-
759.
This article is protected by copyright. All rights reserved
43. Vas L, Pai R, Khandagale N, et al. Pulsed radiofrequency of the composite nerve supply to the
Accepted Article
knee joint as a new technique for relieving osteoarthritic pain: a preliminary report. Pain Physician.
2014;17(6):493-506.
44. Huang CC, Tsao SL, Cheng CY, et al. Treating frozen shoulder with ultrasound-guided pulsed
mode radiofrequency lesioning of the suprascapular nerve: two cases. Pain Med. 2010;11(12):1837-
1840.
45. Kane TP, Rogers P, Hazelgrove J, et al. Pulsed radiofrequency applied to the suprascapular nerve
in painful cuff tear arthropathy. J Shoulder Elbow Surg. 2008;17(3):436-440.
46. Luleci N, Ozdemir U, Dere K, et al. Evaluation of patients' response to pulsed radiofrequency
treatment applied to the suprascapular nerve in patients with chronic shoulder pain. J Back
Musculoskelet Rehabil. 2011;24(3):189-194.
47. Ozyuvaci E, Akyol O, Acikgoz A, et al. Intraarticular pulsed mode radiofrequency lesioning of
glenohumeral joint in chronic shoulder pain: 3 cases. Korean J Pain. 2011;24(4):239-241.
48. Wu YT, Ho CW, Chen YL, et al. Ultrasound-guided pulsed radiofrequency stimulation of the
suprascapular nerve for adhesive capsulitis: a prospective, randomized, controlled trial. Anesth Analg.
2014;119(3):686-692.
49. Yan J, Zhang XM. A randomized controlled trial of ultrasound-guided pulsed radiofrequency for
patients with frozen shoulder. Medicine (Baltimore). 2019;98:e13917.
50. Manchikanti L, Singh V, Pampati V, et al. Evaluation of the relative contributions of various
structures in chronic low back pain. Pain Physician. 2001;4(4):308-316.
51. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila
Pa 1976). 1995;20(1):31-37.
52. Merskey H. Bogduk N. International Association for the Study of Pain. Task Force on Taxonomy.
Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms.
Seattle; IASP Press, 1994.
This article is protected by copyright. All rights reserved
Accepted Article
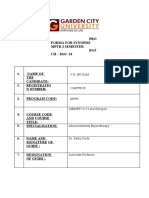
Table 1.The summary of the included previous studies
# First author, Study design Number of Treatment Stimulation site Stimulation mode Outcome Summary of outcome
year patients compared measurement
(E/C) with PRF time, months
Cervical joint
1 Mikeladze, Retrospective 31 - Medial branch 2Hz, 45-55V, 120s, - The average duration of the
200319 study 22G effect of PRF was 3.93
months
21
2 Sluijter, 2008 Case study 2 - Intraarticular Case 1: 10ms, 45V, Case 1: 1, 12 Case 1: No pain at 12-month
(cervical facet, 600s, 22G; Case 2: 10 Case 2: 1, 9 follow-up
atlanto-axial ms, 40V, 480s, 22G Case 2: VAS 6 → 1
joint)
(sustained for 8 months)
3 Liliang, 200816 Single-arm 14 - Medial branch 20ms, 45V, 180s, 2 1, 6, 12 Nine (64.3%) patients had
prospective cycles, 22G significant pain
study improvement at 12-month
follow-up
17
4 Lim, 2017 Prospective 40 (20/20) Intraaricular Intraarticular 5Hz, 5ms, 55V, 360s, 1, 3, 6 Ten (50%) patients showed a
randomized trial steroid (cervical facet) 23G pain relief of ≥ 50% at 6-
injection month follow up
20
5 Shin, 2018 Prospective 23 (12/11) Intraaricular Intraarticular 5Hz, 5ms, 55V, 360s, 1, 3, 6 Eight (66.7%) patients
randomized trial steroid (atlanto-occipital 22G showed a pain relief of ≥
injection joint) 50% at 6-month follow up
22
6 Tak, 2018 Retrospective 20 - Intraarticular 5Hz, 5ms, 55V, 360s, 1, 3 Sixteen (80%) patients
study (atlanto-occipital 22G showed a pain relief of ≥
This article is protected by copyright. All rights reserved
Accepted Article
joint) 50% at 3-month follow up
Lumbosacral facet joint
1 Mikeladze, Retrospective 83 - Medial branch 2Hz, 45-55V, 120s, - The average duration of the
19
2003 study 22G effect of PRF was 3.93
months
29
7 Lindner, 2006 Retrospective 47 - Medial branch 20ms, 120s, 2 cycles, 1, 4 Twenty-five (53%) patients
study 22G showed a pain relief of ≥
60% at 4-month follow up
31
8 Tekin, 2007 Randomized 60 (PRF: 20, CRF, sham Medial branch 45V, 240s, 22G 6, 12 CRF>PRF>control
controlled trial CRF: 20,
control: 20)
28
9 Kroll, 2008 Prospective 26 (13/13) CRF Medial branch 2Hz, 20ms, 120s, 3 Negative result, PRF < CRF
randomized trial 20/21G
10 Colini- Single-arm 300 - Medial branch 2 Hz, 20 ms, 240s, 1, 3, 6 NRS 6 (pre-treatment) → 2
Baldeschi, prospective 22G (3 and 6 months)
25
2012 study
11 Hashemi, Prospective 80 (40/40) Intraaricular Medial branch 20ms, 45V, 120s, 2 1.5, 3, 6 NRS 7.4 (pre-treatment) →
27
2014 randomized trial steroid cycles. 22G 2.4 (6 months), PRF >
injection Intraaricular steroid
injection
12 Schianchi, Case study 2 - Medial branch 2Hz, 10ms, 40V, 600s, Case 1: 0.3, Satisfactory pain relief for
30
2015 and Intraarticular 22G 1,24 two years
5Hz, 5ms, 40V, 600s, Case 2: 3, 24
22G
26
13 Do, 2017 Prospective 60 (30./30) Intraaricular Intraarticular 5Hz, 5ms, 55V, 360s, 0.5, 1, 3, 6 About 50% of patients
randomized trial steroid 23G showed a pain relief of ≥
This article is protected by copyright. All rights reserved
Accepted Article
injection 50% at 6-month follow up
23
14 Chang, 2018 Retrospective 20 - Intraarticular 5Hz, 5ms, 55V, 360s, 1, 3, 6 NRS 4.9 (pre-treatment) →
study 23G 2.3 (1 and 3 months) → 2.6
( 6 months)
24
15 Çetin,2018 Prospective 118 (75/43) CRF Medial branch 2 Hz, 20ms, 180s, 22G 1, 3, 6, 12, 24 PRF and CRF: significantly
study effective, PRF < CRF
Sacroiliac joint
16 Vallejo, 200612 Single-arm 22 - Medial branch 45V, 120s, 22G 6 Sixteen (72.7%) patients
prospective and lateral sacral
study branch
35
17 Karaman,2011 Retrospective 9 - Intraarticular 2Hz, 20ms, 900s, 22G - VAS 6.7 (pre-treatment) →
study 3.1 (average follow: 10.2
months)
32
18 Chang, 2017 Retrospective 20 - Intraarticular 5Hz, 5ms, 55V, 360s, 1, 2, 3 Negative result
study 22G
33
19 Ding, 2018 Prospective 64 (32/32) CRF Intraarticular 600s 0.25, 6, 12 PRF<CRF
randomized trial
34
20 Dutta, 2018 Prospective 30 (15/15) Intraaricular Medial branch 45V, 180s, 22G 0.5, 1, 3, 6 PRF: NRS 7.1 (pre-
randomized trial steroid and lateral sacral treatment) → 3.2 (6
injection branch months), Intraaricular
steroid injection NRS 7.1
(pre-treatment) → 5.4 (6
months), RRF> Intraaricular
steroid injection
Knee joint pain
21 Karaman, Retrospective 31 - Intraarticular 2Hz, 20ms, 900s, 22G 1, 6 VAS 6.1 (pre-treatment) →
This article is protected by copyright. All rights reserved
Accepted Article
201141 study 3.9 (1month) → 4.1 (6
months)
36
22 Akbas, 2011 Retrospective 115 - Saphenous nerve 2Hz, 20ms, 480s 0.3, 3, 6 All patients showed a pain
study relief of ≥ 50% at 6-month
follow up improvement in
VAS scores
23 E Djibilian Single-arm 25 - Sciatic nerve 45V, 480s, 23G 1, 3 VAS 8.1 (pre-treatment) →
39
Fucci, 2013 prospective 5.4 (3months)
study
43
24 Vas, 2014 Single-arm 10 - Saphenous, 480s, 22G 3, 6 Significant pain relief
prospective tibial, femoral,
study and common
peroneal nerves
38
25 Eyigor, 2015 Single-arm 21 - Intraarticular 45V, 600s, 22G 1, 3 VAS 7.6 (pre-treatment) →
prospective 6.1 (1month) → 5.9 (3
study months)
26 Kesikburun, Single-arm 9 - Genicular nerve 120s, 22G 0.25, 1, 3 Six (66.7%) patients showed
42
2016 prospective a pain relief of ≥ 50% at 6-
study month follow up
27 Gulec, 201740 Prospective 100 (50/50) Bipolar Intraarticular 2Hz, 10ms, 45V, 600s, 0.25, 1, 3 Fifty percent (monopolar)
randomized trial intraaricular 22G patients and 84% (bipolar)
patients showed a pain relief
of ≥ 50% at 6-month follow
up
37
28 Erdem, 2019 Retrospective 23 - Genicular nerve 120s, 3 cycles, 22G 0.75, 3 Eighteen (78%) patients
study showed satisfactory pain
This article is protected by copyright. All rights reserved
Accepted Article
relief
Shoulder joint pain
29 Kane, 200745 Single-arm 12 - Suprascapular 120s, 2 or 3 cycles, 3, 6 VAS 6.2 (pre-treatment) →
prospective nerve 22G 4.2 (3 months) → 3.9 (6
study months)
44
30 Huang, 2010 Case report 2 - Suprascapular 2Hz, 20ms, 120s, 2 Case 1: 5 Case 1: NRS 8 (pre-
nerve cycles, 22G months treatment) → 3 (5 months)
Case 2: 6
Case 2: NRS 9 (pre-
months
treatment) → 3 (6 months)
31 Luleci, 201146 Single-arm 13 - Suprascapular 2Hz, 20ms, 40V, 480s, 3, 6 Twelve (92.3%) patients
prospective nerve 21G showed a pain relief of ≥
study 50% at 6-month follow up
32 Ozyuvaci, Case study 3 - Intraarticular 240s 0.75 Case 1: VAS 6 → 3
47
2011
Case 2: VAS 7 → 4
Case 3: VAS 8 → 6
33 Wu, 201448 Randomized 60 (30/30) Sham Suprascapular 2Hz, 30ms, 180s 0.25, 1, 2, 3 PRF>control, Three months
controlled trial nerve after PRF, VAS 6.5 → 1.7
34 Yan, 201949 Randomized 136 (68/68) Sham Suprascapular 2Hz, 20ms, 40V, 22G Once weekly PRF>control, Three months
controlled trial nerve for 3 months after PRF, VAS 4.6 was
decreased
E: experimental group, C: comparison group, PRF: pulsed radiofrequency, CRF: continuous radiofrequency, VAS: visual analogue scale, NRS: numeric rating scale, G: gauge
This article is protected by copyright. All rights reserved
You might also like
- The Journal of ArthroplastyDocument6 pagesThe Journal of ArthroplastyKarla milNo ratings yet
- Radio ScriptDocument3 pagesRadio ScriptJason Raquin Roque84% (25)
- 2021 Article 2286Document8 pages2021 Article 2286Dido KamelNo ratings yet
- Abjs 11 666Document6 pagesAbjs 11 666Matej MilošNo ratings yet
- Park 2014Document7 pagesPark 2014Nurfitrianti ArfahNo ratings yet
- Assessment of The Effect of Epidural Steroid Injection in Patient Having Lumbar RadiculopathyDocument5 pagesAssessment of The Effect of Epidural Steroid Injection in Patient Having Lumbar RadiculopathyIJAR JOURNALNo ratings yet
- FisioterapiDocument7 pagesFisioterapiRidwan Hadinata SalimNo ratings yet
- Opioid Use For Postoperative Pain Control in Pediatric Supracondylar Humerus Fractures A Pain Diary Based Prospective StudyDocument7 pagesOpioid Use For Postoperative Pain Control in Pediatric Supracondylar Humerus Fractures A Pain Diary Based Prospective StudyAthenaeum Scientific PublishersNo ratings yet
- PRF PDFDocument10 pagesPRF PDFjuliusz koselNo ratings yet
- Long-Term Prognosis of Plantar FasciitisDocument9 pagesLong-Term Prognosis of Plantar FasciitisCambriaChicoNo ratings yet
- 2011 14 301 304 PDFDocument4 pages2011 14 301 304 PDFAngela PagliusoNo ratings yet
- Piriformis SyndromeDocument6 pagesPiriformis SyndromeChân Mệnh Thiên TửNo ratings yet
- ABJS Volume 8 Issue 4 Pages 479-501Document23 pagesABJS Volume 8 Issue 4 Pages 479-501Nurul Misna LestariNo ratings yet
- JPR 11 3151Document10 pagesJPR 11 3151Andani TNo ratings yet
- Does Ultrasonography Guided Steroid Injections Provide Better Outcome in Shoulder Impingement Syndrome? A Prospective StudyDocument12 pagesDoes Ultrasonography Guided Steroid Injections Provide Better Outcome in Shoulder Impingement Syndrome? A Prospective StudyIJAR JOURNALNo ratings yet
- 262+Jhrr+4 1+548+Compare+the+Effects+of+BowenDocument6 pages262+Jhrr+4 1+548+Compare+the+Effects+of+BowenBimma WahyuNo ratings yet
- Tratamiento TendinopatiaDocument16 pagesTratamiento TendinopatiasputnickNo ratings yet
- Chemical Hip Denervation For Inoperable Hip FractureDocument6 pagesChemical Hip Denervation For Inoperable Hip Fracturemanuel torresNo ratings yet
- Research ArticleDocument8 pagesResearch ArticleLUIZANo ratings yet
- The Relationship Between Rate of Algometer Application and Pain Pressure Threshold in TheDocument16 pagesThe Relationship Between Rate of Algometer Application and Pain Pressure Threshold in TheRafael BohnenbergerNo ratings yet
- Artigo - US Pra Dor CrônicaDocument12 pagesArtigo - US Pra Dor CrônicaJose Carlos CamposNo ratings yet
- Tens HNPDocument6 pagesTens HNPUniquaNo ratings yet
- 4Document4 pages4Amr Mohamed GalalNo ratings yet
- 116 239 1 SMDocument9 pages116 239 1 SMrizk86No ratings yet
- BBRC Vol 14 No 04 2021-80Document5 pagesBBRC Vol 14 No 04 2021-80Dr Sharique AliNo ratings yet
- Proloterapia Rev Sistemica 2021Document15 pagesProloterapia Rev Sistemica 2021Marcos FigueroaNo ratings yet
- Papr 12544Document11 pagesPapr 12544Michael HuntNo ratings yet
- Ijerph 18 04877Document10 pagesIjerph 18 04877aaNo ratings yet
- Heel Pain Plantar Fasciitis Revision 2023Document49 pagesHeel Pain Plantar Fasciitis Revision 2023martha sri astutiNo ratings yet
- APS Therapy Research DocumentsDocument60 pagesAPS Therapy Research Documentsherbs6No ratings yet
- 2016 Joint Mobilization Enhances Mechanisms of Conditioned Pain Modulation in Individuals With Osteoarthritis of The KneeDocument30 pages2016 Joint Mobilization Enhances Mechanisms of Conditioned Pain Modulation in Individuals With Osteoarthritis of The KneeGiancarlo Gardella MartínezNo ratings yet
- Feasibility and Estimated Efficacy of Blood Flow Restricted Training in Female Patients With Rheumatoid Arthritis A Randomized Controlled Pilot StudyDocument10 pagesFeasibility and Estimated Efficacy of Blood Flow Restricted Training in Female Patients With Rheumatoid Arthritis A Randomized Controlled Pilot StudyDaniel Andrés Bulla GarcíaNo ratings yet
- 2016 19 E1181 E1187Document8 pages2016 19 E1181 E1187Rafael FontesNo ratings yet
- Physiotherapy Management in Lumbar Facet Joint Syndrome - A Single Case StudyDocument5 pagesPhysiotherapy Management in Lumbar Facet Joint Syndrome - A Single Case StudyCambriaChicoNo ratings yet
- Relationship Between Pain Intensity, Pain Catastrophizing, and Self-Efficacy in Patients With Frozen Shoulder: A Cross-Sectional StudyDocument6 pagesRelationship Between Pain Intensity, Pain Catastrophizing, and Self-Efficacy in Patients With Frozen Shoulder: A Cross-Sectional Studyluisherrera1490No ratings yet
- SH 2Document14 pagesSH 2ع الNo ratings yet
- Characteristics of Myofascial Pain Syndrome of The Infraspinatus MuscleDocument9 pagesCharacteristics of Myofascial Pain Syndrome of The Infraspinatus Musclearia tristayanthiNo ratings yet
- Clinical StudyDocument8 pagesClinical Studylilis pratiwiNo ratings yet
- Jmu 26 194Document6 pagesJmu 26 194Arkar SoeNo ratings yet
- Effects of Dry Needling On Calf Muscle in Case of Myofascial Trigger Point With Mild Restriction of Knee Joint Movement: A Case StudyDocument4 pagesEffects of Dry Needling On Calf Muscle in Case of Myofascial Trigger Point With Mild Restriction of Knee Joint Movement: A Case StudyIJAR JOURNALNo ratings yet
- Headache Terapi RadiofrequencyDocument14 pagesHeadache Terapi RadiofrequencyHardiyanti HermanNo ratings yet
- TENS Literature - Review - and - Meta - Analysis - Of.99266Document9 pagesTENS Literature - Review - and - Meta - Analysis - Of.99266Adam ForshawNo ratings yet
- DOR - FENOL - Chemical Ablation of Genicular Nerve With Phenol For Pain Relief in Patients With Knee Osteoarthritis A Prospective Study - CompressedDocument7 pagesDOR - FENOL - Chemical Ablation of Genicular Nerve With Phenol For Pain Relief in Patients With Knee Osteoarthritis A Prospective Study - CompressedGustavo FredericoNo ratings yet
- Synopsis Template - MPTR 2022 - For Merge-1Document13 pagesSynopsis Template - MPTR 2022 - For Merge-1sriram gopalNo ratings yet
- Pages From SMJ 8, 2022 Id Link-6Document12 pagesPages From SMJ 8, 2022 Id Link-6Nakarit SangsirinawinNo ratings yet
- Brief Review Piriformis Syndrome Etiology DiagnosiDocument11 pagesBrief Review Piriformis Syndrome Etiology DiagnosiyonisfuadNo ratings yet
- 12Document9 pages12Kinjal SharmaNo ratings yet
- Pulsed Radiofrequency in Interventional Pain Management: Cellular and Molecular Mechanisms of Action - An Update and ReviewDocument9 pagesPulsed Radiofrequency in Interventional Pain Management: Cellular and Molecular Mechanisms of Action - An Update and ReviewYuyumNo ratings yet
- Low Back PainDocument6 pagesLow Back PainMuhammad Adzan Al QadriNo ratings yet
- Japre 22 71591Document3 pagesJapre 22 71591pramod aloorNo ratings yet
- Image-Guided Radiofrequency Ablation For Joint and Back Pain: Rationales, Techniques, and ResultsDocument13 pagesImage-Guided Radiofrequency Ablation For Joint and Back Pain: Rationales, Techniques, and ResultscontatoNo ratings yet
- Andrew IJTRRDocument8 pagesAndrew IJTRRsiddharthaNo ratings yet
- Assessing Pain Relief Following Medical and Surgical Interventions For Lumbar Disc HerniationDocument4 pagesAssessing Pain Relief Following Medical and Surgical Interventions For Lumbar Disc HerniationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- TEnsDocument10 pagesTEnsmarcelogascon.oNo ratings yet
- Effect of Adding Neural Mobilization Versus Myofascial Release To Stabilization Exercises After Lumbar Spine Fusion - A Randomized Controlled TrialDocument10 pagesEffect of Adding Neural Mobilization Versus Myofascial Release To Stabilization Exercises After Lumbar Spine Fusion - A Randomized Controlled TrialLuisa MendozaNo ratings yet
- Added Value of Gluteus Medius and Quadratus Lumborum Dry Needling in Improving Knee Pain and Function in Female Athletes With Patellofemoral Pain Syndrome: A Randomized Clinical TrialDocument10 pagesAdded Value of Gluteus Medius and Quadratus Lumborum Dry Needling in Improving Knee Pain and Function in Female Athletes With Patellofemoral Pain Syndrome: A Randomized Clinical Trialريما ميماNo ratings yet
- Prolo TherapyDocument14 pagesProlo TherapyrebeccaNo ratings yet
- Sports Pharmacology: Treating Pain and InflammationDocument49 pagesSports Pharmacology: Treating Pain and InflammationVLDs100% (1)
- Lumbar Trigger PointsDocument4 pagesLumbar Trigger PointsManoj KumarNo ratings yet
- Tangtiphaiboontana 2021Document8 pagesTangtiphaiboontana 2021翁嘉聰No ratings yet
- Consciousness Viewed in The Framework of Brain Phase SpaceDynamics, Criticality, and The Renormalization GroupDocument19 pagesConsciousness Viewed in The Framework of Brain Phase SpaceDynamics, Criticality, and The Renormalization GroupnikesemperNo ratings yet
- Integrated Principles of Zoology 17Th Edition Cleveland P Hickman Full ChapterDocument67 pagesIntegrated Principles of Zoology 17Th Edition Cleveland P Hickman Full Chaptermelissa.blankenship107100% (8)
- NCM 116 Perception NotesDocument8 pagesNCM 116 Perception NotesMarie HwangNo ratings yet
- 15 CortexDocument87 pages15 Cortexandreea_grama_11No ratings yet
- Lesson 2 Louise Joseph PeraltaDocument3 pagesLesson 2 Louise Joseph PeraltaLouise Joseph G. PeraltaNo ratings yet
- Neurohist of Cerebrum and CerebellumDocument70 pagesNeurohist of Cerebrum and CerebellumAisha YolaNo ratings yet
- Program and Proceedings - 7th International Regional "Stress and Behavior" Neuroscience and Biopsychiatry Conference (North America), June 22-24, 2016, Miami Beach, FL, USADocument33 pagesProgram and Proceedings - 7th International Regional "Stress and Behavior" Neuroscience and Biopsychiatry Conference (North America), June 22-24, 2016, Miami Beach, FL, USAISBS_SocietyNo ratings yet
- GEK1064 Lect 1 (Notes) AnnotatedDocument19 pagesGEK1064 Lect 1 (Notes) AnnotatedNg Jia ChengNo ratings yet
- Local Anesthetics VeterinaryDocument32 pagesLocal Anesthetics VeterinaryEssi Rehc100% (1)
- Myofascial Trigger PointsDocument11 pagesMyofascial Trigger PointsАлексNo ratings yet
- Review of Cerebral Anatomy:: DiencephalonDocument27 pagesReview of Cerebral Anatomy:: DiencephalonEJ GejonNo ratings yet
- Sensory Evaluation Notes 2010Document95 pagesSensory Evaluation Notes 2010Qi WeiNo ratings yet
- Posterior CorticalDocument24 pagesPosterior CorticalJ Alonso MejiaNo ratings yet
- The Stages of SleepDocument3 pagesThe Stages of Sleeptheamack100% (1)
- Amy Yu Grand Rounds Presentation - Feb 12, 2010Document20 pagesAmy Yu Grand Rounds Presentation - Feb 12, 2010Aulya ArchuletaNo ratings yet
- 02 Padure, L. Spastic Hip in Cerebral PalsyDocument4 pages02 Padure, L. Spastic Hip in Cerebral PalsyminichoixNo ratings yet
- Clinical Case Scenarios 3Document3 pagesClinical Case Scenarios 3Jei NacalabanNo ratings yet
- Cell Signaling - ImpDocument11 pagesCell Signaling - Impkrishnarajagopal2011No ratings yet
- Full Download PDF of Adams and Victor's Principles of Neurology 11th Edition (Ebook PDF) All ChapterDocument49 pagesFull Download PDF of Adams and Victor's Principles of Neurology 11th Edition (Ebook PDF) All Chaptersurzoelarbi100% (8)
- Control and Coordination Class 10 Notes PDF Science Biology CBSEDocument5 pagesControl and Coordination Class 10 Notes PDF Science Biology CBSEgooode100% (2)
- Pharmacology of Autonomic Nervous System 2013Document166 pagesPharmacology of Autonomic Nervous System 2013Adimera TsehayeNo ratings yet
- Contoh Soal Pat Bahasa Inggris Kelas XiDocument4 pagesContoh Soal Pat Bahasa Inggris Kelas XiRetno Haryanti, S.si.No ratings yet
- HNP CervicalDocument33 pagesHNP CervicalIndra RanteNo ratings yet
- Unit 5. Interaction and HealthDocument11 pagesUnit 5. Interaction and Healthtamarita90No ratings yet
- Presentation No. 2 - Sensory ImageryDocument8 pagesPresentation No. 2 - Sensory Imageryandie hinchNo ratings yet
- Ems UnitDocument28 pagesEms UnitKomang Tri Adi SuparwatiNo ratings yet
- Homeopathic Treatment of MigraineDocument3 pagesHomeopathic Treatment of MigraineRPh Krishna Chandra JagritNo ratings yet
- Nervous System IIIa-33Document2 pagesNervous System IIIa-33Dale Marie Renomeron0% (1)
- Ac en f31Document15 pagesAc en f31psychforallNo ratings yet