Professional Documents
Culture Documents
Doppler Arterial MsIS PDF
Doppler Arterial MsIS PDF
Uploaded by
Samantha AriasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Doppler Arterial MsIS PDF
Doppler Arterial MsIS PDF
Uploaded by
Samantha AriasCopyright:
Available Formats
Doppler ultrasonography of the lower
extremity arteries: anatomy and
scanning guidelines
Ji Young Hwang
REVIEW ARTICLE
Department of Radiology, Ewha Womans University School of Medicine, Seoul, Korea
https://doi.org/10.14366/usg.16054
pISSN: 2288-5919 • eISSN: 2288-5943
Ultrasonography 2017;36:111-119
Doppler ultrasonography of the lower extremity arteries is a valuable technique, although it is
less frequently indicated for peripheral arterial disease than for deep vein thrombosis or varicose
veins. Ultrasonography can diagnose stenosis through the direct visualization of plaques and
through the analysis of the Doppler waveforms in stenotic and poststenotic arteries. To perform
Received: December 30, 2016
Doppler ultrasonography of the lower extremity arteries, the operator should be familiar with the Revised: January 17, 2017
arterial anatomy of the lower extremities, basic scanning techniques, and the parameters used in Accepted: January 18, 2017
color and pulsed-wave Doppler ultrasonography. Correspondence to:
Ji Young Hwang, MD, Department
of Radiology, Ewha Womans
Keywords: Arteries; Lower extremity; Ultrasonography, Doppler, color; Ultrasonography, Doppler, University School of Medicine, 1071
Anyangcheon-ro, Yangcheon-gu, Seoul
pulsed; Peripheral arterial disease 07985, Korea
Tel. +82-2-2650-5687
Fax. +82-2-2650-5302
E-mail: mshjy@ewha.ac.kr
Introduction
Imaging modalities for evaluating peripheral arterial disease in the lower extremities include
computed tomography (CT) angiography, conventional angiography, and Doppler ultrasonography
(US). Three-dimensional CT angiography provides information about atherosclerotic calcifications and This is an Open Access article distributed under the
terms of the Creative Commons Attribution Non-
the extent of stenosis or occlusion of the arteries. CT angiography has some advantages, such as a Commercial License (http://creativecommons.org/
shorter examination time, the ability to evaluate the iliac artery, and the fact that it is less affected licenses/by-nc/3.0/) which permits unrestricted non-
commercial use, distribution, and reproduction in
by the operator’s experience. Conventional angiography is used for vascular interventions such as any medium, provided the original work is properly
cited.
angioplasty or stent application, as well as in the diagnosis of peripheral arterial disease. Doppler
US is the only noninvasive technique that does not require contrast enhancement, preparation of the Copyright © 2017 Korean Society of
patient before the study, or radiation exposure [1,2]. Doppler US is a good method for screening and Ultrasound in Medicine (KSUM)
follow-up, as well as for the definitive diagnosis of peripheral arterial disease [3-7]. Color Doppler US
can easily identify arteries by finding round objects with regular pulsation and can be used to detect
stenotic or occluded segments [4,8]. Pulsed-wave Doppler US can show the exact flow velocity of
each arterial segment and determine the degree of severity of the stenosis based on an analysis of
the pulsed-wave Doppler spectral waveform [9].
Knowledge of the ultrasonographic anatomy of the lower extremity arteries and the corresponding
anatomical landmarks is essential for performing Doppler US. In this article, we review the basic
How to cite this article:
scanning techniques of color and pulsed-wave Doppler US for the lower extremity arteries and the Hwang JY. Doppler ultrasonography of
the lower extremity arteries: anatomy and
spectral analysis of normal and stenotic arteries on pulsed-wave Doppler US. scanning guidelines. Ultrasonography. 2017
Apr;36(2):111-119.
e-ultrasonography.org Ultrasonography 36(2), April 2017 111
Ji Young Hwang
Anatomy of the Lower Extremity Arteries on the superficial femoral artery medially and the deep femoral artery
CT Angiography laterally [10]. The superficial femoral artery descends without
prominent branching between the quadratrus and adductor muscle
Each lower extremity artery is visible with an accompanying vein, groups in the anteromedial thigh. In the distal thigh, the superficial
extending from the iliac artery to the popliteal artery. The anterior femoral artery enters the adductor canal. On leaving the adductor
tibial artery, the posterior tibial artery, and the peroneal artery hiatus, the name of the artery becomes the popliteal artery in the
are seen with two homonymous veins. The overall anatomy of the popliteal fossa and ends by bifurcating into the anterior tibial artery
arteries in the lower extremities is shown on CT angiography in Fig. 1. and the tibioperoneal trunk in the posterior aspect of the proximal
The common iliac artery splits into the internal iliac artery and the calf [11].
external iliac artery in the pelvic cavity. The external iliac artery is Below the knee, the anterior tibial artery passes from the posterior
continuous with the common femoral artery (Fig. 1A). The inguinal to the anterior, and then descends along the interosseous membrane
ligament is a landmark for the junction of the external iliac artery behind the anterior tibialis muscle and the extensor muscles in the
and common femoral artery. The inguinal ligament is located more anterolateral leg. The tibioperoneal trunk divides into the posterior
proximally than the inguinal crease. The common femoral artery is tibial artery medially and the peroneal artery laterally (Fig. 1B). The
a short segment, generally about 4 cm long, and bifurcates into posterior tibial artery runs along the intermuscular space between
Aorta
Knee crease
POPA
CIA
EIA ATA Tibioperoneal trunk
IIA
CFA Inguinal crease
PA PTA
DFA
SFA
ATA PTA
POPA
Knee crease
A B
Fig. 1. The anatomy of the lower extremity arteries on computed tomography (CT) angiography.
A. On coronal maximal intensity projection (MIP) CT image above the knee, the external iliac artery (EIA) is continuous with the common
femoral artery (CFA) which bifurcates into the superficial femoral artery (SFA) and deep femoral artery (DFA). The SFA is continuous with the
popliteal artery (POPA). B. On coronal MIP CT image below the knee, the POPA splits anterior tibial artery (ATA) and tibioperoneal trunk
which bifurcates into posterior tibial artery (PTA) and peroneal artery (PA). CIA, common iliac artery; IIA, internal iliac artery.
112 Ultrasonography 36(2), April 2017 e-ultrasonography.org
Doppler ultrasonography of lower extremity arteries
the posterior tibialis muscle and the soleus muscles. The peroneal the transducer, arteries are partially compressed, while veins are
artery extends down between the posterior tibialis muscle and the completely collapsed [12].
flexor hallucis longus muscle. Doppler US of the lower extremity begins at the inguinal crease
In the ankle and foot region, the anterior tibial artery continues by putting a transducer on the common femoral artery in the
into the dorsalis pedis artery distal to the extensor retinaculum [11]. transverse plane with the patient in the supine position (Fig. 2). The
The dorsalis pedis artery forms the arcuate artery at the metatarsal common femoral artery is seen lateral to the femoral vein, which
base and gives rise to the dorsal metatarsal artery. The posterior is drained from the greater saphenous vein anteromedially at the
tibial artery passes behind the medial malleolus of the tibia and inguinal area (Fig. 3A). Just below the inguinal crease, the superficial
bifurcates, forming the medial and lateral plantar arteries. The deep femoral artery and the deep femoral artery are present alongside
plantar arch from the medial and lateral plantar arteries gives rise to the femoral vein, showing a shape reminiscent of Mickey Mouse’s
the plantar metatarsal and digital arteries of the foot [11]. face on a transverse scan (Fig. 3B). The common femoral artery, the
bifurcated superficial femoral artery and deep femoral artery are
US Anatomy of the Lower Extremity Arteries seen in a fallen-Y configuration in a longitudinal scan (Fig. 2). From
the proximal to distal thigh, scanning is performed by moving a
Arteries can be differentiated from veins on US by several transducer distally along the superficial femoral artery deep to the
characteristics. First, arteries are round in transverse images, while sartorius muscle. The superficial femoral artery goes together with
veins are somewhat oval. Second, arteries are smaller than veins. the femoral vein (Fig. 2).
Third, arteries have visible walls and sometimes have calcified The popliteal artery is evaluated from the knee crease level in
plaques on the walls. Fourth, when the vessels are compressed by the transverse plane and then traced proximally up to the adductor
Supine position Prone position
1 3
1 GSV CFA
2
SFA
3 FV CFA
2 DF FV
GSV SFA A
4 DFA
FV
4
SFA
5 FV 5
5 SSV 6
POPV
POPV
POPA POPA
Fig. 2. The steps of color Doppler ultrasonography (US) for the lower extremities above the knee, with the patient’s position indicated.
The red rectangular boxes are the essential scanning sites and planes for the femoral arteries and the popliteal artery. The numbers within
the boxes represent the general steps of scanning. The schema in the box demonstrates the typical US features of arteries and veins at each
scanning site. GSV, greater saphenous vein; FV, femoral vein; CFA, common femoral artery; SFA, superficial femoral artery; DFA, deep femoral
artery; SSV, small saphenous vein; POPV, popliteal vein; POPA, popliteal artery.
e-ultrasonography.org Ultrasonography 36(2), April 2017 113
Ji Young Hwang
SFA cm/sec
FV
CFA
DFA
FV
A B
Fig. 3. Normal color Doppler ultrasonography of the femoral arteries in the inguinal area.
A. The common femoral artery (CFA) is lateral to the femoral vein (FV) on a transverse scan at the inguinal crease. Note that the size of the
color box is as small as possible. B. The superficial femoral artery (SFA) and the deep femoral artery (DFA) make a shape like Mickey Mouse’s
ears, and the FV forms Mickey Mouse’s face.
canal at the supracondylar level of the femur (Fig. 2). The popliteal delicately to maintain visualization of the artery. Pulsed-wave
artery is seen in the central portion of popliteal fossa between Doppler US is performed in the longitudinal plane.
the medial and lateral heads of the gastrocnemius muscles. The The examination is usually performed with the patient placed
evaluation of the posterior tibial artery can be started from its in the supine position. The patient’s hip is generally abducted and
origins at the tibioperoneal trunk, if scanning distally, or from the externally rotated, and the knee is flexed like frog legs in order
ankle behind the medial malleolus, if scanning proximally (Fig. 4). to easily approach the popliteal artery in the popliteal fossa and
The peroneal artery is scanned along the lateral side of the posterior the posterior tibial artery in the medial calf (Fig. 2). The left lateral
calf and is visualized alongside the fibular bone (Fig. 4). decubitus position or the prone position are the alternatives for
The evaluation of the anterior tibial artery can be started from the evaluating the popliteal artery, the posterior tibial artery, and the
ankle anterior to the talus neck and continued proximally or started peroneal artery (Fig. 4). The anterior tibial artery and dorsalis pedis
from the proximal anterolateral leg between the tibia and the fibula artery are scanned in the supine position (Fig. 4).
and continued distally (Fig. 4). The transducer is traced from the
anterior ankle to the dorsal foot to evaluate the dorsalis pedis artery, Parameters and Optimization of Doppler US
continuing to the first dorsal metatarsal artery between the first and The operator should be aware of both color and pulsed-wave
second metatarsal bones (Fig. 4). Doppler parameters and how to adjust these parameters to obtain
an optimal Doppler image.
US Technique Among these parameters, the color box, color gain, color velocity
scale, and inversion are frequently used during color Doppler
Transducer and Patient Position US scanning. The color box is a square area within the grayscale
A linear transducer with a variable ultrasound frequency of 9-15 sonogram in which all color Doppler information is displayed (Fig.
MHz is generally used, but a convex transducer with a lower 3). The size and location of the box are adjustable, and the image
frequency can be selected for the evaluation of iliac arteries in resolution and quality are affected by the box size and depth [14].
the pelvic cavity [13]. The transducer is placed over an artery for The box should be made as small and placed as superficially as
transverse scanning, and then is rotated 90° for longitudinal possible, thereby maximizing the frame rate. The color box should be
scanning. The artery should be scanned on a longitudinal plane as tilted using the “steer” button according to the arterial axis during
long as possible. The operator should rotate or move the transducer longitudinal scanning (Fig. 5). Color gain refers to the amplification
114 Ultrasonography 36(2), April 2017 e-ultrasonography.org
Doppler ultrasonography of lower extremity arteries
Prone position Supine position
1 4
PTA
ATA
Ti
Ti F
2 5
PTA ATA DOA 4
MM
1
1
Ti
3 T
3 6 MA
PA
5
2 F 1 2
2
6
Fig. 4. The steps of color Doppler ultrasonography for the lower extremities below the knee, with the patient’s position indicated. The
posterior tibial artery (PTA) is seen along the tibia (Ti) at the medial side of the posterior calf (box 1) and behind the medial malleolus (MM)
of the ankle (box 2). The peroneal artery (PA) is depicted alongside the fibula (F) on the lateral side of posterior calf in the prone position
(box 3). The anterior tibial artery (ATA) is detected over interosseous memberane (black dashed line) between the tibia (Ti) and the fibula (F)
at the anterolateral side of the calf (box 4). At the ankle level, the ATA is seen anterior to the tibia plafond (Ti) and the talus (T) (box 5) and
continues to the dorsalis pedis artery (DOA) distal to the ankle and metatarsal artery (MA) between the metatarsal bones (box 6).
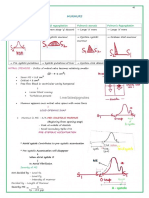
a θ SV cm/sec
cm/sec
cm/sec Fig. 5. Color and pulsed-wave Doppler sonograms of normal
lower extremity arteries with parameters. Top: In a color image
of a pulsed-wave Doppler sonogram, the color box is tilted to be
cm/sec parallel to the arterial axis using the “steer” key. Doppler angle (θ)
S is 60° in this case and is formed by the Doppler line of sight (S) and
the axis of arterial flow (a). SV, sample volume; LT FA, left femoral
artery; PSV, peak systolic velocity; EDV, end-diastolic velocity; MDV,
minimum diastolic velocity; RI, resistivity index. RI=(PSV-EDV)/PSV.
Bottom: On the Doppler spectrum, time (seconds) is represented on
the x-axis. Blood flow velocity (cm/sec) is shown on the y-axis (dashed
cm/sec
line). Flow direction relative to the transducer is shown in relation to
the spectrum baseline (arrow). The “high-Q” is the blue outline of
mm/sec the Doppler spectrum (arrowhead).
e-ultrasonography.org Ultrasonography 36(2), April 2017 115
Ji Young Hwang
of flow data to improve the depiction of flow [14]. Color gain (the direction of flow, which may complicate the interpretation of the
“gain” button on the US machine) should be set as high as possible flow direction. Therefore, the flow direction should be interpreted
without displaying background color noise. The color velocity is the based on the setting of the color bar. The wall filter (WF) eliminate
range of flow velocities that are depicted in color Doppler US [14]. the low frequency noise that may arise from vessel wall motion
If the velocity scale (the “scale” button on the US machine) setting below an operator-defined frequency threshold [9,14]. WF settings
is lower than the flow velocity of the artery, aliasing artifacts will are usually preset by manufacturer (Fig. 6).
be present. An operator can detect the color flow within an arterial It is important to understand the meaning of the parameters
lumen by increasing the gain or decreasing the scale. Color flow of pulsed-wave Doppler US and how to adjust them. The sample
artifacts outside an artery should be removed by decreasing the volume cursor is composed of parallel lines on both sides of the
gain. A homogeneous color of arterial flow can be obtained by arterial axis line. The sample volume should be placed within an
increasing the scale. Flow toward the transducer typically appears arterial lumen, and the range of the sample volume size is generally
red on color Doppler sonograms when a red color appears above from one-third to one-half of the luminal diameter [15]. The Doppler
the baseline on the color bar. Inversion can electronically invert the angle is formed by the Doppler line and the axis of arterial flow
cm/sec
cm/sec cm/sec
cm/sec cm/sec
cm/sec
cm/sec
cm/sec
cm/sec
cm/sec
cm/sec
cm/sec
cm/sec
Lower baseline Increase scale
cm/sec
Fig. 6. Adjustment of pulsed-wave Doppler ultrasonography in a stenotic arterial segment. The aliasing artifact on the Doppler spectrum
can be adjusted by lowering the baseline (arrowhead) and increasing the scale. Note the spectral broadening (arrow) in the Doppler
spectrum due to stenosis of the artery. Parameters for color flow (CF) and pulsed-wave (PW) Doppler are peak systolic velocity (PSV) 129 cm/sec,
end diastolic velocity (EDV) 15.4 cm/sec, minimum diastolic velocity (MDV) 8.9 cm/sec, resistivity index (RI) 0.88, and wall filter (WF) 120 Hz
in CF and 60 Hz in PW. SV, sample volume.
116 Ultrasonography 36(2), April 2017 e-ultrasonography.org
Doppler ultrasonography of lower extremity arteries
and should be between 45° and 60° for optimal accuracy [9]. On
Doppler US, the line in the center of the artery indicates of the axis
of arterial flow. The nearly vertical line is the Doppler line of sight
(Fig. 5). The Doppler spectrum is a graph showing the mixture of
frequencies over a short period of time [9]. The Doppler frequency
is defined as the difference between the received and transmitted
frequencies when blood cells are moving. The key elements of
the Doppler spectrum are the time and velocity scales [9]. On the
Doppler spectrum, time (seconds) is represented on the x-axis,
and the velocity scale (cm/sec) is shown on the y-axis (Fig. 5).
Flow direction relative to the transducer is shown in relation to
the spectrum baseline. Flow toward the transducer is represented
by positive velocity above the baseline (Fig. 5). The “high-Q” or
peak velocity envelope is the blue outline surrounding the Doppler
spectrum. Based on this envelope, peak systolic velocity (PSV), Fig. 7. A 56-year-old man with arterial occlusion. Color flow is
minimum diastolic velocity (MDV), end-diastolic velocity (EDV), absent in the superficial femoral artery (arrow) on color Doppler
and the resistivity index (RI) can be obtained numerically (Figs. 5, sonogram at the inguinal level, representing complete occlusion.
6). PSV is the highest systolic velocity, MDV is the lowest diastolic The red vessel is the deep femoral artery and the blue vessel is the
collapsed femoral vein.
velocity, and EDV is the highest end-diastolic velocity. The RI is one
of popular measurements of the pulsatility representing peripheral
flow resistance [9]. If an aliasing artifact is present in the Doppler
spectrum, the baseline can be reduced or the scale increased in
Abnormal US Findings
order to optimize the velocity range (Fig. 6). It can be automatically
optimized by pressing the “i-scan” button. Doppler US of the lower extremities can be performed by obtaining
grayscale images before the color Doppler study; however, grayscale
evaluations are sometimes optional and can be considered as a
Doppler Spectrum of Normal Lower
second step when a color Doppler study yields findings suspicious
Extremity Arteries
for stenosis or occlusion. On a grayscale image, the presence and
the size of a plaque should be described, as well as whether the
The Doppler waveform of the lower extremity arteries at rest is plaque is calcified or not. Plaque size can be measured in terms
classified as a high pulsatility waveform and is characterized by a of height and length obtained using transverse and longitudinal
triphasic flow pattern [9]. Over the course of each heartbeat, a tall, scans, respectively [16]. Three-dimensional US has been recently
narrow, and sharp systolic peak in the first phase is followed by early used for measuring plaque volume, with good intraobserver and
diastolic flow reversal in the second phase, and then by late diastolic interobserver reproducibility [17].
forward flow in the third phase (Fig. 5). Diastolic flow reversal On color Doppler US, if an occlusion is present in the artery, color
results from the high peripheral resistance of normal extremity flow is absent within the lumen (Fig. 7).
arteries [9]. In normal extremity arteries, flow acceleration in systole The Doppler spectrum at severely stenotic arterial segments and
is rapid, which means that the peak velocity is reached within a few poststenotic or post-obstructive distal arterial segments is briefly
hundredths of a second after ventricular contraction begins. Blood reviewed below. The peak systolic velocity at stenotic segments
in the center of the artery moves faster than blood at the periphery, increases until the diameter is reduced by 70%, which corresponds
which is described as laminar flow [9]. When the flow is laminar, the to a 90% reduction in area [18]. The area of flow disturbance
blood cells are moving at a similar speed. These features of normal showing spectral broadening occurs within 2 cm beyond the area
arteries produce a clear space, known as the spectral window, under of stenosis due to loss of the laminar flow pattern (Fig. 6). Spectral
the Doppler spectrum. broadening is prominent, with a diameter reduction of 20%-
50%. The lower extremity artery waveform may convert to a low-
resistance form with low pulsatility after exercise or as a result of
e-ultrasonography.org Ultrasonography 36(2), April 2017 117
Ji Young Hwang
the occlusion of more proximal arteries [18]. If the waveform is color flow duplex ultrasonography. J Vasc Technol 1996;20:93-98.
monophasic, that means that the entire waveform is either above or 7. Mohler ER 3rd, Bundens W, Denenberg J, Medenilla E, Hiatt WR,
below the Doppler spectrum baseline, depending on the orientation Criqui MH. Progression of asymptomatic peripheral artery disease
of the US transducer [9]. It is characterized by a “damped” pattern, over 1 year. Vasc Med 2012;17:10-16.
which means that systolic flow acceleration is slowed, peak 8. Hussain ST. Blood flow measurements in lower limb arteries using
systolic velocity is reduced, and diastolic flow is increased [19]. This duplex ultrasound. Ann R Coll Surg Engl 1997;79:323-330.
9. Zwiebel WJ, Pellerito JS. Basic concepts of Doppler frequency
monophasic waveform is seen at the stenotic site and in the distal
spectrum analysis and ultrasound blood flow imaging. In: Zwiebel
artery in cases of severe stenosis with a diameter reduction of more
WJ, Pellerito JS, eds. Introduction to vascular ultrasonography. 5th
than 50%.
ed. Philadelphia, PA: Elsevier Saunders, 2004;61-89.
10. Keck GM, Zwiebel WJ. Arterial anatomy of the extremities.
Conclusion In: Zwiebel WJ, Pellerito JS, eds. Introduction to vascular
ultrasonography. 5th ed. Philadelphia, PA: Elsevier Saunders,
Doppler US has been found to distinguish between stenosis with a 2004;265-274.
diameter reduction greater than or less than 50% (corresponding 11. Schuenke M, Schulte E, Schumacher U. Lower limb. In: Ross LM,
to an area reduction of 70%) with a sensitivity of 77%-82% and Lamperti ED, eds. Atlas of anatomy. New York: Thieme, 2006;464-
a specificity of 92%-98% [18,20-24]. Complete scanning of both 465.
lower extremities may require up to 2 hours depending on the 12. Hatsukami TS, Primozich J, Zierler RE, Strandness DE Jr. Color
operator’s experience [18]. However, if the operator is familiar with Doppler characteristics in normal lower extremity arteries.
the US anatomy of the lower extremity arteries and understands Ultrasound Med Biol 1992;18:167-171.
the parameters and Doppler waveforms of Doppler US, accurate 13. Zierler RE. Doppler techniques for lower extremity arterial diagnosis.
diagnostic results can be produced with less scanning time. Herz 1989;14:126-133.
14. Kruskal JB, Newman PA, Sammons LG, Kane RA. Optimizing
ORCID: Ji Young Hwang: http://orcid.org/0000-0001-5848-3429 Doppler and color flow US: application to hepatic sonography.
Radiographics 2004;24:657-675.
Conflict of Interest 15. Knox RA, Phillips DJ, Breslau PJ, Lawrence R, Primozich J,
No potential conflict of interest relevant to this article was reported. Strandness DE Jr. Empirical findings relating sample volume size
to diagnostic accuracy in pulsed Doppler cerebrovascular studies. J
Clin Ultrasound 1982;10:227-232.
References
16. Lee W. General principles of carotid Doppler ultrasonography.
1. Nzeh DA, Allan PL, McBride K, Gillespie I, Ruckley CV. Comparison Ultrasonography 2014;33:11-17.
of colour Doppler ultrasound and digital subtraction angiography 17. Landry A, Spence JD, Fenster A. Measurement of carotid plaque
in the diagnosis of lower limb arterial disease. Afr J Med Med Sci volume by 3-dimensional ultrasound. Stroke 2004;35:864-869.
1998;27:177-180. 18. Zierler RE. Ultrasound assessment of lower extremity arteries.
2. Karacagil S, Lofberg AM, Granbo A, Lorelius LE, Bergqvist D. Value In: Zwiebel WJ, Pellerito JS, eds. Introduction to vascular
of duplex scanning in evaluation of crural and foot arteries in limbs ultrasonography. 5th ed. Philadelphia, PA: Elsevier Saunders,
with severe lower limb ischaemia: a prospective comparison with 2004;341-356.
angiography. Eur J Vasc Endovasc Surg 1996;12:300-303. 19. Kotval PS. Doppler waveform parvus and tardus: a sign of proximal
3. Flanigan DP, Ballard JL, Robinson D, Galliano M, Blecker G, Harward flow obstruction. J Ultrasound Med 1989;8:435-440.
TR. Duplex ultrasound of the superficial femoral artery is a better 20. Jager KA, Phillips DJ, Martin RL, Hanson C, Roederer GO, Langlois
screening tool than ankle-brachial index to identify at risk patients YE, et al. Noninvasive mapping of lower limb arterial lesions.
with lower extremity atherosclerosis. J Vasc Surg 2008;47:789-792. Ultrasound Med Biol 1985;11:515-521.
4. Sensier Y, Bell PR, London NJ. The ability of qualitative assessment 21. Kohler TR, Nance DR, Cramer MM, Vandenburghe N, Strandness DE
of the common femoral Doppler waveform to screen for significant Jr. Duplex scanning for diagnosis of aortoiliac and femoropopliteal
aortoiliac disease. Eur J Vasc Endovasc Surg 1998;15:357-364. disease: a prospective study. Circulation 1987;76:1074-1080.
5. Gooding GA, Perez S, Rapp JH, Krupski WC. Lower-extremity vascular 22. Shaalan WE, French-Sherry E, Castilla M, Lozanski L, Bassiouny HS.
grafts placed for peripheral vascular disease: prospective evaluation Reliability of common femoral artery hemodynamics in assessing
with duplex Doppler sonography. Radiology 1991;180:379-386. the severity of aortoiliac inflow disease. J Vasc Surg 2003;37:960-
6. Sorrell K, Demasi R. Delayed vascular injury: the value of follow-up 969.
118 Ultrasonography 36(2), April 2017 e-ultrasonography.org
Doppler ultrasonography of lower extremity arteries
23. Hussain ST, Smith RE, Wood RF, Bland M. Observer variability in 24. Moneta GL, Yeager RA, Antonovic R, Hall LD, Caster JD, Cummings
volumetric blood flow measurements in leg arteries using duplex CA, et al. Accuracy of lower extremity arterial duplex mapping. J
ultrasound. Ultrasound Med Biol 1996;22:287-291. Vasc Surg 1992;15:275-283.
e-ultrasonography.org Ultrasonography 36(2), April 2017 119
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (350)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (824)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Kidney MCQDocument14 pagesKidney MCQNikita Nanwani86% (37)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- First Aid Q&A PDFDocument764 pagesFirst Aid Q&A PDFStephanie Williams100% (9)
- MC Case PDFDocument20 pagesMC Case PDFShivani KarkeraNo ratings yet
- CyclophosphamideDocument7 pagesCyclophosphamideFrances Ramos33% (3)
- (Alexei Lapkin, David Constable) Green Chemistry Me (B-Ok - CC) PDFDocument337 pages(Alexei Lapkin, David Constable) Green Chemistry Me (B-Ok - CC) PDFAlex Sustaita100% (1)
- Live Quiz - 3rd Month Birthday-Edited - WatermarkDocument13 pagesLive Quiz - 3rd Month Birthday-Edited - WatermarkNikita NanwaniNo ratings yet
- ADVT Admission Notice No.01 - 2020 AIIMS PG July 2020Document1 pageADVT Admission Notice No.01 - 2020 AIIMS PG July 2020Nikita NanwaniNo ratings yet
- Medicine Prepladder 2020-Pages-44-49Document6 pagesMedicine Prepladder 2020-Pages-44-49Nikita NanwaniNo ratings yet
- Antimicrobials in A Nutshell 27 JuneDocument37 pagesAntimicrobials in A Nutshell 27 JuneNikita NanwaniNo ratings yet
- Ecografia Toracica PDFDocument12 pagesEcografia Toracica PDFCristinaLucanNo ratings yet
- Usg 16054Document9 pagesUsg 16054Nikita NanwaniNo ratings yet
- ENTDocument2 pagesENTNikita Nanwani0% (1)
- Ikimono Gakari - HOT MILKDocument3 pagesIkimono Gakari - HOT MILKapi-3799292100% (1)
- Material Balance PDFDocument31 pagesMaterial Balance PDFApril Joy HaroNo ratings yet
- Base On Solid-Works Design of Compact High EfficieDocument15 pagesBase On Solid-Works Design of Compact High EfficieGorgeNo ratings yet
- Federal MogulDocument277 pagesFederal Mogulعبدالغني القباطي100% (1)
- Ciarrochi Fisher and Lane Link Between Values and Well-Being Among People With Cancer 2010 Psycho OncologyDocument9 pagesCiarrochi Fisher and Lane Link Between Values and Well-Being Among People With Cancer 2010 Psycho OncologyJuan C. VargasNo ratings yet
- LTE TDD - Network - Export - 2018 - 07 - 04Document3,760 pagesLTE TDD - Network - Export - 2018 - 07 - 04saadNo ratings yet
- Electronics Cooling: Mechanical Power Engineering DeptDocument22 pagesElectronics Cooling: Mechanical Power Engineering DeptneilNo ratings yet
- Coal Ash Dewatering SolutionDocument23 pagesCoal Ash Dewatering Solution류태하No ratings yet
- Veins and Hydrothermal DepositsDocument2 pagesVeins and Hydrothermal Depositsalimurtadha100% (1)
- Edible Oil - Case StudyDocument8 pagesEdible Oil - Case StudyVansh Raj GautamNo ratings yet
- Lecture 7 - Synchronous Generators 7 PDFDocument28 pagesLecture 7 - Synchronous Generators 7 PDFDorwinNeroNo ratings yet
- SOM016 - Hook Release System For Life Boats. Norsafe TOR mk2.Document20 pagesSOM016 - Hook Release System For Life Boats. Norsafe TOR mk2.arfaoui salimNo ratings yet
- Cne CatalogoDocument4 pagesCne CatalogoPaulo SergioNo ratings yet
- Battles Fought On The Great Wall of China Qin DynastyDocument2 pagesBattles Fought On The Great Wall of China Qin DynastySachin NagmotiNo ratings yet
- ProductSheet Iq200 Rackmount SatelliteModemDocument2 pagesProductSheet Iq200 Rackmount SatelliteModemAsim Penkar PenkarNo ratings yet
- Arthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832Document318 pagesArthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832cengizozakinciNo ratings yet
- Gennady Nesis, Leonid Shulman, Malcolm Gesthuysen - Tactics in The King's IndianDocument130 pagesGennady Nesis, Leonid Shulman, Malcolm Gesthuysen - Tactics in The King's Indiancodonauta100% (1)
- 4 Poisonous & Venomous AnimalsDocument47 pages4 Poisonous & Venomous AnimalsAnyi Yulieth AMPUDIA MURILLONo ratings yet
- A Clinical Audit Into The Success Rate of Inferior Alveolar Nerve Block Analgesia in General Dental PracticeDocument4 pagesA Clinical Audit Into The Success Rate of Inferior Alveolar Nerve Block Analgesia in General Dental PracticeGina CastilloNo ratings yet
- 130-87 InstructionsDocument7 pages130-87 InstructionsAlex GarciaNo ratings yet
- Tax System SriLankaDocument44 pagesTax System SriLankamandarak7146No ratings yet
- MCQ - AcousticsDocument16 pagesMCQ - AcousticsRomeo Espenida0% (1)
- 11 Chemistry Module 2Document19 pages11 Chemistry Module 2SpongeBob SquarePants Fidget ToysNo ratings yet
- Cacio e Pepe Pizza by Chef Uditi: Makes 4-5 Pizzas, About 250 GR Each Ingredients: For The Pizza DoughDocument1 pageCacio e Pepe Pizza by Chef Uditi: Makes 4-5 Pizzas, About 250 GR Each Ingredients: For The Pizza DoughPablo NameNo ratings yet
- T2T 32T BTC Master Manual enDocument10 pagesT2T 32T BTC Master Manual enRAMON RUIZNo ratings yet
- Combustion Engineering, Heat Transfer, Refrigeration Engineering, & Air ConditioningDocument17 pagesCombustion Engineering, Heat Transfer, Refrigeration Engineering, & Air ConditioningNicole Mae AllosadaNo ratings yet
- Soal PAS K13 Kelas 9 Ganjil Tp. 2019-2020Document5 pagesSoal PAS K13 Kelas 9 Ganjil Tp. 2019-2020Fairuz AbadiNo ratings yet