Professional Documents
Culture Documents
Pub - Clinical Outline of Oral Pathology Diagnosis and T PDF
Pub - Clinical Outline of Oral Pathology Diagnosis and T PDF
Uploaded by
TOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pub - Clinical Outline of Oral Pathology Diagnosis and T PDF
Pub - Clinical Outline of Oral Pathology Diagnosis and T PDF
Uploaded by
TCopyright:
Available Formats
CLINICAL OUTLINE OF ORAL
PATHOLOGY: DIAGNOSIS
AND TREATMENT
FOURTH EDITION
PMPH_Eversole_FM.indd i 1/25/2011 9:48:08 PM
PMPH_Eversole_FM.indd ii 1/25/2011 9:48:09 PM
CLINICAL OUTLINE OF ORAL
PATHOLOGY: DIAGNOSIS
AND TREATMENT
FOURTH EDITION
Lewis R. Eversole
2011
PEOPLE’S MEDICAL PUBLISHING HOUSE–USA
SHELTON, CONNECTICUT
PMPH_Eversole_FM.indd iii 1/25/2011 9:48:09 PM
People’s Medical Publishing House-USA
2 Enterprise Drive, Suite 509
Shelton, CT 06484
Tel: 203-402-0646
Fax: 203-402-0854
E-mail: info@pmph-usa.com
© 2011 PMPH-USA, Ltd.
All rights reserved. Without limiting the rights under copyright reserved above, no part of this publication may be reproduced,
stored in or introduced into a retrieval system, or transmitted, in any form or by any means (electronic, mechanical,
photocopying, recording, or otherwise), without the prior written permission of the publisher.
11 12 13 14/PMPH/9 8 7 6 5 4 3 2 1
ISBN: 978-1-60795-015-8
Printed in China by People’s Medical Publishing House
Editor: Jason Malley; Copyeditor/Typesetter: Newgen
Library of Congress Cataloging-in-Publication Data
Eversole, Lewis R.
Clinical outline of oral pathology : diagnosis and treatment / Lewis R. Eversole. — 4th ed.
p. ; cm.
ISBN 978-1-60795-015-8
1. Mouth—Diseases. 2. Teeth—Diseases. I. Title.
[DNLM: 1. Diagnosis, Oral. 2. Mouth Diseases—diagnosis. 3. Diagnosis, Differential.
4. Mouth Diseases—therapy. WU 140]
RC815.E9 2010
616.3’1—dc22
2010051383
Sales and Distribution
Canada United Kingdom, Europe, Middle East, Brazil
McGraw-Hill Ryerson Education Africa SuperPedido Tecmedd
Customer Care McGraw Hill Education Beatriz Alves, Foreign Trade Department
300 Water St Shoppenhangers Road R. Sansao Alves dos Santos, 102 | 7th floor
Whitby, Ontario L1N 9B6 Maidenhead Brooklin Novo
Canada Berkshire, SL6 2QL Sao Paolo 04571-090
Tel: 1-800-565-5758 England Brazil
Fax: 1-800-463-5885 Tel: 44-0-1628-502500 Tel: 55-16-3512-5539
www.mcgrawhill.ca Fax: 44-0-1628-635895 www.superpedidotecmedd.com.br
www.mcgraw-hill.co.uk
Foreign Rights India, Bangladesh, Pakistan, Sri Lanka,
People’s Medical Publishing House Singapore, Thailand, Philippines, Malaysia
Suzanne Robidoux, Copyright Sales Indonesia, CBS Publishers
Manager Vietnam, Pacific Rim, Korea 4819/X1 Prahlad Street 24
International Trade Department McGraw-Hill Education Ansari Road, Darya Ganj,
No. 19, Pan Jia Yuan Nan Li 60 Tuas Basin Link New Delhi-110002
Chaoyang District Singapore 638775 India
Beijing 100021 Tel: 65-6863-1580 Tel: 91-11-23266861/67
P.R. China Fax: 65-6862-3354 Fax: 91-11-23266818
Tel: 8610-59787337 www.mcgraw-hill.com.sg Email:cbspubs@vsnl.com
Fax: 8610-59787336
www.pmph.com/en/
Australia, New Zealand, Papua People’s Republic of China
New Guinea, Fiji, Tonga, Solomon Islands, People’s Medical Publishing House
Japan Cook Islands International Trade Department
United Publishers Services Limited Woodslane Pty Limited No. 19, Pan Jia Yuan Nan Li
1-32-5 Higashi-Shinagawa Unit 7/5 Vuko Place Chaoyang District
Shinagawa-ku, Tokyo 140-0002 Warriewood NSW 2102 Beijing 100021
Japan Australia P.R. China
Tel: 03-5479-7251 Tel: 61-2-9970-5111 Tel: 8610-67653342
Fax: 03-5479-7307 Fax: 61-2-9970-5002 Fax: 8610-67691034
Email: kakimoto@ups.co.jp www.woodslane.com.au www.pmph.com/en/
Notice: The authors and publisher have made every effort to ensure that the patient care recommended herein, including
choice of drugs and drug dosages, is in accord with the accepted standard and practice at the time of publication. However,
since research and regulation constantly change clinical standards, the reader is urged to check the product information
sheet included in the package of each drug, which includes recommended doses, warnings, and contraindications.
This is particularly important with new or infrequently used drugs. Any treatment regimen, particularly one involving
medication, involves inherent risk that must be weighed on a case-by-case basis against the benefits anticipated. The
reader is cautioned that the purpose of this book is to inform and enlighten; the information contained herein is not
intended as, and should not be employed as, a substitute for individual diagnosis and treatment.
PMPH_Eversole_FM.indd iv 1/25/2011 9:48:09 PM
Contents
1. THE DIAGNOSTIC PROCESS 1
Procurement of the Data Base 2 Assessment of the Findings 5
CHIEF COMPLAINT AND HISTORY OF THE Formulating a Differential
PRESENT ILLNESS 2
Diagnosis 5
MEDICAL AND DENTAL HISTORY 3
PHYSICAL EXAMINATION 4 Securing a Definitive Diagnosis 6
RADIOGRAPHIC EXAMINATION 4
CLINICAL LABORATORY TESTS 4 Formulating a Treatment Plan 7
2. WHITE LESIONS 9
Flat Plaques, Solitary 11 PROLIFERATIVE VERRUCOUS
LEUKOPLAKIA 31
FRICTIONAL BENIGN KERATOSES 11 VERRUCOUS CARCINOMA 33
LEUKOPLAKIA 12
ACTINIC CHEILITIS 14 Lacey White Lesions 34
SMOKELESS TOBACCO KERATOSES 14 LICHEN PLANUS 34
SANGUINARIA-INDUCED KERATOSES 16 LICHENOID REACTIONS 36
DYSKERATOSIS CONGENITA 17 LUPUS ERYTHEMATOSUS 37
FANCONI’S ANEMIA 18
HIV-ASSOCIATED HAIRY LEUKOPLAKIA 38
DYSPLASIA, CARCINOMA IN SITU,
SQUAMOUS CELL CARCINOMA, AND Papular Lesions 40
VERRUCOUS CARCINOMA 19
LICHEN PLANUS (HYPERTROPHIC TYPE) 21 KOPLIK SPOTS OF MEASLES 40
MUCOUS PATCHES (SECONDARY FORDYCE’S GRANULES 41
SYPHILIS) 22 DENTAL LAMINA CYSTS, BOHN’S NODULES,
EPSTEIN’S PEARLS 41
Flat Plaques, Bilateral or STOMATITIS NICOTINA 42
Multifocal 23
SPECKLED LEUKOPLAKIA 43
LEUKOEDEMA 23
GENOKERATOSES 24 Pseudomembranous Lesions 44
PLAQUE-FORM LICHEN PLANUS (SEE CHEMICAL BURNS 44
ABOVE) 30
CANDIDIASIS (MONILIASIS, THRUSH) 45
CHEEK/TONGUE BITE KERATOSIS 30
VESICULO-BULLOUS-ULCERATIVE
Verrucous/Rippled Plaques 31 DISEASES 47
PMPH_Eversole_FM.indd v 1/25/2011 9:48:09 PM
vi Contents
3. RED AND PIGMENTED LESIONS 49
Focal Erythemas 51 Petechiae 73
NONSPECIFIC (IRRITATIONAL) SUCTION PETECHIAE 73
MUCOSITIS 51 INFECTIOUS MONONUCLEOSIS 74
MEDIAN RHOMBOID GLOSSITIS 52 THROMBOCYTE DISORDERS 75
HEMANGIOMA 53 HEREDITARY HEMORRHAGIC
VARIX 54 TELANGIECTASIA 76
ERYTHROPLAKIA 55
Focal Pigmentations 77
Diffuse and Multifocal Red Lesions 56 AMALGAM AND GRAPHITE TATTOO 77
GEOGRAPHIC TONGUE (MIGRATORY MUCOCELE 78
GLOSSITIS) 56 HEMATOMA 79
ERYTHEMA MIGRANS (MIGRATORY NEVUS 80
STOMATITIS) 57 EPHELIS, ORAL MELANOTIC MACULE 81
ATROPHIC GLOSSITIS 58
RADIATION MUCOSITIS 59
Diffuse and Multifocal
Pigmentations 82
XEROSTOMIC MUCOSITIS 60
LUPUS ERYTHEMATOSUS 61 MALIGNANT MELANOMA 82
ALLERGIC MUCOSITIS, FOREIGN BODY RACIAL PIGMENTATION 83
GINGIVITIS 63 PIGMENTED LICHEN PLANUS 84
BULLOUS/EROSIVE DISEASES 64 PEUTZ-JEGHERS SYNDROME 85
CANDIDIASIS 65 MULTIPLE NEUROFIBROMATOSIS 86
LYMPHONODULAR PHARYNGITIS 67 ADDISON’S DISEASE 87
SCARLET FEVER 67 HEMOCHROMATOSIS 88
ATROPHIC LICHEN PLANUS 68 HIV-ASSOCIATED ORAL
PIGMENTATION 89
ECCHYMOSIS AND CLOTTING FACTOR
DEFICIENCIES 70 HEAVY METAL INGESTION 90
FIELD CANCERIZATION 71 DRUG-INDUCED PIGMENTATION 91
KAPOSI’S SARCOMA 72 HAIRY TONGUE 92
4. ORAL ULCERATIONS AND FISTULAE 95
Recurrent and Multiple ACUTE NECROTIZING ULCERATIVE
GINGIVITIS 105
Ulcerations 96
ACUTE STREPTOCOCCAL/
APHTHOUS STOMATITIS 96 STAPHYLOCOCCAL STOMATITIS 106
MAJOR SCARRING APHTHOUS CHRONIC ULCERATIVE STOMATITIS 107
STOMATITIS 97 GONOCOCCAL STOMATITIS 107
BEHÇET’S SYNDROME 99 HIV PERIODONTITIS AND ORAL
GLUTEN ENTEROPATHY 100 ULCERATIONS 108
AGRANULOCYTOSIS AND
IMMUNOSUPPRESSION 100 Focal Ulcerations 109
CYCLIC NEUTROPENIA 101 TRAUMATIC ULCER 109
UREMIC STOMATITIS 102 TRAUMATIC GRANULOMA WITH STROMAL
VIRAL VESICULAR STOMATITIS 103 EOSINOPHILIA 111
PMPH_Eversole_FM.indd vi 1/25/2011 9:48:09 PM
Contents vii
ATYPICAL HISTIOCYTIC GRANULOMA 112 OROANTRAL FISTULA 122
NECROTIZING SIALOMETAPLASIA 113 SOFT TISSUE ABSCESS 123
SPECIFIC GRANULOMATOUS ULCER 114 DEVELOPMENTAL ORAL SINUSES 124
CHANCRE (PRIMARY SYPHILIS) 115 FISSURED (SCROTAL) TONGUE 125
SQUAMOUS CELL CARCINOMA 116
Perioral and Commissural Necrotic and Osseous Destructive
Lesions 126
Ulcerations and Fistulae 117
FACTITIAL INJURY AND TRAUMA 126
COMMISSURAL PITS 117
WEGENER’S GRANULOMATOSIS 127
CONGENITAL LIP PITS 118
EXTRANODAL NK/T-CELL LYMPHOMA 128
ANGULAR CHEILITIS 119
TERTIARY SYPHILIS 129
Oral Fistulae 120 OSTEORADIONECROSIS 130
PERIAPICAL ABSCESS AND MUCORMYCOSIS 131
OSTEOMYELITIS 120 ANTRAL CARCINOMA 132
PERIODONTAL ABSCESS 121 BISPHOSPHONATE-RELATED
ACTINOMYCOSIS 122 OSTEONECROSIS OF THE JAWS 133
5. VESICULOBULLOUS AND DESQUAMATIVE LESIONS 137
Febrile-Associated Vesicular BULLOUS PEMPHIGOID 151
Eruptions 139 BENIGN MUCOUS MEMBRANE
PEMPHIGOID 152
HERPETIC GINGIVOSTOMATITIS 139 BULLOUS LICHEN PLANUS 154
HERPANGINA 140 ERYTHEMA MULTIFORME 155
HAND-FOOT-AND-MOUTH DISEASE 141 STEVENS-JOHNSON SYNDROME 156
PRIMARY VARICELLA-ZOSTER PARANEOPLASTIC PEMPHIGUS 157
(CHICKENPOX) 143 ANGINA BULLOSA HEMORRHAGICA 158
SECONDARY VARICELLA-ZOSTER EPIDERMOLYSIS BULLOSA 159
(SHINGLES) 144 DERMATITIS HERPETIFORMIS (GLUTEN
Nonfebrile-Associated Vesicular ENTEROPATHY) 161
Eruptions 145 Desquamative Lesions 161
RECURRENT HERPES STOMATITIS 145 GINGIVOSIS (DESQUAMATIVE
RECURRENT HERPES LABIALIS 146 GINGIVITIS) 161
CONTACT VESICULAR STOMATITIS 148 EROSIVE LICHEN PLANUS 163
IMPETIGO 149 LICHENOID CONTACT STOMATITIS 164
CHRONIC ULCERATIVE STOMATITIS 165
Bullous Diseases 150
PYOSTOMATITIS VEGETANS 166
PEMPHIGUS VULGARIS 150 TOOTHPASTE IDIOSYNCRATIC LESIONS 168
6. INTRAORAL SOFT TISSUE SWELLINGS 171
Localized Gingival Tumefactions 173 PERIPHERAL GIANT CELL GRANULOMA 176
PERIPHERAL FIBROMA 177
PARULIS 173 GIANT CELL FIBROMA 178
PYOGENIC GRANULOMA 175 PERIPHERAL OSSIFYING FIBROMA 179
PMPH_Eversole_FM.indd vii 1/25/2011 9:48:09 PM
viii Contents
JUVENILE SPONGIOTIC GINGIVAL CHEILITIS GLANDULARIS 217
HYPERPLASIA 180 ANGIONEUROTIC EDEMA 218
RETROCUSPID PAPILLAE 181 ACTINIC PRURIGO 219
TORUS MANDIBULARIS AND INFLAMMATORY FIBROUS HYPERPLASIA 220
EXOSTOSES 181 FOREIGN BODY GRANULOMA 220
GINGIVAL CYST 183 CROHN’S DISEASE 221
ERUPTION CYST 184 TRAUMATIC FIBROMA 222
EPULIS FISSURATA 185 TRAUMATIC (AMPUTATION) NEUROMA 224
CONGENITAL EPULIS 185 MESENCHYMAL NEOPLASMS 224
MESENCHYMAL TUMORS 187 HERNIATED BUCCAL FAT PAD 225
PERIPHERAL ODONTOGENIC TUMORS 188 REACTIVE LYMPHOID HYPERPLASIA 226
SQUAMOUS CELL CARCINOMA 189 HEMANGIOMA AND VARIX 227
SARCOMAS 190 SQUAMOUS CELL CARCINOMA 229
MUCOEPIDERMOID CARCINOMA 191 MONOMORPHIC ADENOMA 230
NON-HODGKIN’S LYMPHOMA 192 OTHER SALIVARY NEOPLASMS 231
METASTATIC CARCINOMA 193
LANGERHANS CELL HISTIOCYTOSIS 194 Tongue Swellings 232
Generalized Gingival Swellings 195 MEDIAN RHOMBOID GLOSSITIS 232
ECTOPIC LINGUAL THYROID 233
FIBROMATOSIS GINGIVAE 195 THYROGLOSSAL DUCT CYST 234
DRUG INDUCED HYPERPLASIA 196 LINGUAL CYST (ENTEROCYSTOMA, GASTRIC
NONSPECIFIC HYPERPLASTIC CYST) 235
GINGIVITIS 197 HYPERPLASTIC LINGUAL TONSIL 236
WEGENER’S GRANULOMATOSIS 198 LINGUAL ABSCESS 237
TYPE I DIABETES MELLITUS 199 REACTIVE LESIONS (FIBROMA, PYOGENIC
PUBERTY/PREGNANCY GINGIVITIS 200 GRANULOMA) 237
LEUKEMIA 201 MUCOCELE 238
Swellings of the Oral Floor 202 HEMANGIOMA AND LYMPHANGIOMA 239
NEURAL SHEATH TUMORS 241
RANULA AND SIALOCYSTS 202 GRANULAR CELL TUMOR 242
DISONTOGENIC CYSTS 203 LEIOMYOMA 243
LYMPHOEPITHELIAL CYST 204 OSTEOCARTILAGINOUS CHORISTOMA 244
SIALOLITHIASIS WITH SIALADENITIS 205 ECTOMESENCHYMAL CHONDROMYXOID
SALIVARY GLAND TUMORS 207 TUMOR 245
ADENOMATOID HYPERPLASIA 207 SARCOMAS 245
MESENCHYMAL NEOPLASMS 208 AMYLOID NODULES 246
LUDWIG’S ANGINA 209 SPECIFIC GRANULOMA 247
SQUAMOUS CELL CARCINOMA 210 SQUAMOUS CELL CARCINOMA 248
Swellings of the Lips and Buccal Palatal Swellings 250
Mucosa 211 TORUS PALATINUS 250
MUCOUS RETENTION (EXTRAVASATION) CYST OF THE INCISIVE PAPILLA 251
PHENOMENON (MUCOCELE) 211 PALATAL ABSCESS 251
SIALOCYST 213 REACTIVE LESIONS OF PALATAL
MINOR GLAND SIALOLITHIASIS 214 GINGIVAL 252
NASOALVEOLAR (KLESTADT) CYST 215 ADENOMATOUS HYPERPLASIA 252
CHEILITIS GRANULOMATOSA 216 PLEOMORPHIC ADENOMA 253
PMPH_Eversole_FM.indd viii 1/25/2011 9:48:09 PM
Contents ix
POLYMORPHOUS LOW-GRADE ADENOCARCINOMA, NOS 259
ADENOCARCINOMA 254 ATYPICAL LYMPHOPROLIFERATIVE
MISCELLANEOUS ADENOCARCINOMAS 255 DISEASE 259
ADENOID CYSTIC CARCINOMA 256 SQUAMOUS CELL CARCINOMA 261
MUCOEPIDERMOID CARCINOMA 258 CARCINOMA OF THE ANTRUM 262
7. PAPILLARY, PAPULAR, AND MULTIPLE POLYPOID LESIONS 265
Focal Papillary Lesions 267 PAPILLARY SQUAMOUS CELL
CARCINOMA 281
PAPILLOMA 267
VERRUCA VULGARIS 268
Diffuse Papular and Polypoid
Lesions 282
CONDYLOMA ACUMINATUM 269
VERRUCIFORM XANTHOMA 270 PAPILLARY HYPERPLASIA 282
SIALADENOMA PAPILLIFERUM 271 STOMATITIS NICOTINA 283
GIANT CELL FIBROMA 272 ACUTE LYMPHONODULAR
SQUAMOUS ACANTHOMA 273 PHARYNGITIS 284
KERATOSIS FOLLICULARIS 284
Focal and Umbilicated Papules 273 FOCAL EPITHELIAL HYPERPLASIA
(HECK’S DISEASE) 285
KERATOACANTHOMA 273
MULTIPLE HAMARTOMA (COWDEN)
WARTY DYSKERATOMA 274
SYNDROME 286
MOLLUSCUM CONTAGIOSUM 275 PYOSTOMATITIS VEGETANS 287
Diffuse and Multifocal Papillary CROHN’S DISEASE 288
Lesions 276 SPECIFIC GRANULOMATOUS
INFECTIONS 289
FOCAL DERMAL HYPOPLASIA (GOLTZ AMYLOIDOSIS 290
SYNDROME) 276 HYALINOSIS CUTIS ET MUCOSAE
NEVUS UNIUS LATERIS 277 (LIPOID PROTEINOSIS) 291
ACANTHOSIS NIGRICANS 278 HEMANGIOMA/LYMPHANGIOMA 292
ATYPICAL VERRUCOUS MULTIPLE ENDOCRINE NEOPLASIA,
LEUKOPLAKIA 278 TYPE IIB 293
VERRUCOUS CARCINOMA 280 DENTAL LAMINA CYSTS 294
8. SOFT TISSUE SWELLINGS OF THE NECK AND FACE 297
Lateral Neck Swellings 300 ACTINOMYCOSIS 306
REACTIVE PROLIFERATIONS 307
BRANCHIAL CLEFT CYST 300 SINUS HISTIOCYTOSIS 308
CERVICAL RIB AND TRANSVERSE BENIGN MESENCHYMAL TUMORS 309
PROCESS 301 CYSTIC HYGROMA (LYMPHANGIOMA) 310
NONSPECIFIC LYMPHADENITIS 301 CAROTID BODY TUMOR
INFECTIOUS MONONUCLEOSIS 303 (CHEMODECTOMA) 311
TUBERCULOUS LYMPHADENITIS METASTATIC CARCINOMA 312
(SCROFULA) 304 SARCOMAS 314
CAT-SCRATCH FEVER 305 MALIGNANT LYMPHOMA 315
PMPH_Eversole_FM.indd ix 1/25/2011 9:48:10 PM
x Contents
Unilateral Parotid and DYSGENETIC CYSTS OF THE PAROTID 338
Submandibular Swellings 316 METABOLIC SIALADENOSIS 339
ACUTE SIALADENITIS (SURGICAL Midline Neck Swellings 340
MUMPS) 316
THYROGLOSSAL TRACT CYST 340
SIALOLITHIASIS AND OBSTRUCTIVE
GOITER 341
SIALADENITIS 317
CHRONIC SIALADENITIS 318 THYROID NEOPLASIA 342
INTRAPAROTID MESENCHYMAL DERMOID CYST 343
TUMORS 319
LYMPHOMA 320
Growths and Swellings of the
Facial Skin 344
PLEOMORPHIC ADENOMA 322
PAPILLARY CYSTADENOMA NEVI 344
LYMPHOMATOSUM 323 SEBACEOUS CYST 345
ONCOCYTOMA 324 SEBORRHEIC KERATOSIS 346
MISCELLANEOUS ADENOMAS 325 ADNEXAL SKIN TUMORS 347
ADENOID CYSTIC CARCINOMA 326 BASAL CELL CARCINOMA 348
MUCOEPIDERMOID CARCINOMA 327 SQUAMOUS CELL CARCINOMA 350
ACINIC CELL CARCINOMA 329 KERATOACANTHOMA 351
ADENOCARCINOMA NOS AND MESENCHYMAL TUMORS 352
MISCELLANEOUS MALIGNANCIES 330
MALIGNANT MELANOMA 353
Bilateral Parotid and Submandibular
Swellings 332
Diffuse Facial Swellings 354
CELLULITIS AND SPACE INFECTIONS 354
ENDEMIC PAROTITIS (MUMPS) 332
SJÖGREN’S SYNDROME 333 EMPHYSEMA 355
MIKULICZ’S DISEASE 334 ANGIONEUROTIC EDEMA 356
SARCOID SIALADENITIS AND HEERFORDT’S CUSHING’S SYNDROME 357
SYNDROME 335 FACIAL HEMIHYPERTROPHY 358
TUBERCULOSIS 336 FIBROUS DYSPLASIA AND OTHER BONE
HIV SALIVARY DISEASE (DIFFUSE INFILTRATIVE LESIONS 359
LYMPHOCYTOSIS SYNDROME) 337 MASSETERIC HYPERTROPHY 360
9. RADIOLUCENT LESIONS OF THE JAWS 363
Periapical Radiolucencies 366 STATIC BONE CYST (SUBMANDIBULAR
GLAND DEPRESSION) 377
APICAL PERIODONTITIS (ABSCESS, SUBLINGUAL GLAND DEPRESSION 377
GRANULOMA, AND CYST) 366 PARADENTAL (BUCCAL INFECTED)
PERIAPICAL CEMENTAL DYSPLASIA 367 CYST 379
FOCAL CEMENTO-OSSEOUS CENTRAL GIANT CELL GRANULOMA 380
DYSPLASIA 369 MALIGNANCIES 380
FOCAL SCLEROSING OSTEOMYELITIS 371
BENIGN CEMENTOBLASTOMA 371 Interradicular Radiolucencies 383
INCISIVE CANAL CYST 372 LATERAL PERIODONTAL CYST 383
MEDIAN MANDIBULAR CYST 375 LATERALLY DISPLACED APICAL
TRAUMATIC (HEMORRHAGIC) CYST 375 PERIODONTAL CYST OR GRANULOMA 384
PMPH_Eversole_FM.indd x 1/25/2011 9:48:10 PM
Contents xi
RESIDUAL CYST 385 Multilocular Radiolucencies 423
ODONTOGENIC KERATOCYST 386
PRIMORDIAL CYST 386 ODONTOGENIC KERATOCYST 423
CALCIFYING CYSTIC ODONTOGENIC BOTRYOID ODONTOGENIC CYST 425
TUMOR 388 GLANDULAR ODONTOGENIC CYST 425
SQUAMOUS ODONTOGENIC TUMOR 389 CHERUBISM (FAMILIAL FIBROUS
SURGICAL CILIATED CYST 391 DYSPLASIA) 427
OSTEOPOROTIC BONE MARROW CENTRAL GIANT CELL GRANULOMA 429
DEFECT 392 ANEURYSMAL BONE CYST 429
CENTRAL OSSIFYING (CEMENTIFYING) HYPERPARATHYROIDISM 431
FIBROMA 393 AMELOBLASTOMA 432
ODONTOGENIC ADENOMATOID MYXOMA 433
TUMOR 394 CENTRAL NEUROGENIC NEOPLASMS 434
ODONTOGENIC FIBROMA 396 CENTRAL ARTERIOVENOUS
CENTRAL GIANT CELL GRANULOMA 397 MALFORMATION 436
Periodontal (Alveolar) Bone Loss 398 CENTRAL (LOW FLOW) HEMANGIOMA OF
BONE 437
CHRONIC PERIODONTITIS 398 CENTRAL LEIOMYOMA 438
DIABETIC PERIODONTITIS 400 PSEUDOTUMOR OF HEMOPHILIA 439
JUVENILE PERIODONTITIS AND PAPILLON- MYOFIBROMATOSIS (DESMOPLASTIC
LEFEVRE SYNDROME 401 FIBROMA OF BONE) 440
VANISHING BONE DISEASE (MASSIVE FIBROUS DYSPLASIA 442
OSTEOLYSIS) 402 INTRAOSSEOUS MUCOEPIDERMOID
LANGERHANS CELL HISTIOCYTOSIS 403 CARCINOMA 443
CYCLIC NEUTROPENIA 405 THALASSEMIA MAJOR 443
LEUKEMIA 406
Moth-Eaten Radiolucencies 443
Widened Periodontal Ligament OSTEOMYELITIS 443
Space 407
OSTEORADIONECROSIS 445
PERIODONTIC/ENDODONTIC BISPHOSPHONATE-RELATED
INFLAMMATION 407 OSTEONECROSIS OF THE JAWS
SCLERODERMA 409 (BRONJ) 446
OSTEOGENIC SARCOMA 410 PRIMARY INTRAOSSEOUS CARCINOMA 448
CYSTOGENIC CARCINOMA 449
Pericoronal Radiolucencies 411
METASTATIC CARCINOMA 450
DENTIGEROUS CYST 411 MALIGNANT ODONTOGENIC TUMORS 452
ODONTOGENIC KERATOCYST 413 OSTEOSARCOMA AND
GLANDULAR ODONTOGENIC CYST 414 CHONDROSARCOMA 453
UNICYSTIC AMELOBLASTOMA 414 EWING’S SARCOMA 455
CALCIFYING EPITHELIAL ODONTOGENIC PRIMARY LYMPHOMA OF BONE 456
TUMOR 417 BURKITT’S LYMPHOMA 457
ODONTOGENIC ADENOMATOID FIBROGENIC AND NEUROGENIC
TUMOR 417 SARCOMA 458
AMELOBLASTIC FIBROMA 419 MELANOTIC NEUROECTODERMAL TUMOR
ODONTOGENIC FIBROMA-LIKE OF INFANCY 459
HAMARTOMA/ENAMEL HYPOPLASIA 420
CENTRAL MUCOEPIDERMOID
Multifocal Radiolucencies 461
CARCINOMA 421 BASAL CELL NEVUS SYNDROME 461
PMPH_Eversole_FM.indd xi 1/25/2011 9:48:10 PM
xii Contents
LANGERHANS CELL HISTIOCYTOSIS 462 SENILE OSTEOPOROSIS 466
MULTIPLE MYELOMA 463 STEROID OSTEOPOROSIS 467
SICKLE CELL ANEMIA 468
Generalized Osteoporotic THALASSEMIA MAJOR 469
Lesions 465
OSTEOMALACIA 465
10. RADIOPAQUE LESIONS OF THE JAWS 473
Periapical Radiopacities 475 ANTRAL INVASIVE MYCOSES 506
FUNGUS BALL (ASPERGILLUS
PERIAPICAL CEMENTAL DYSPLASIA 475 MYCETOMA) 507
FOCAL CEMENTO-OSSEOUS DYSPLASIA 477 ALLERGIC FUNGAL SINUSITIS 508
FOCAL SCLEROSING OSTEOMYELITIS 479 DISPLACED TEETH, ROOTS, AND FOREIGN
FOCAL PERIAPICAL OSTEOSCLEROSIS 480 BODIES 509
BENIGN CEMENTOBLASTOMA 481 AUGMENTATION MATERIALS 510
ANTROLITH/RHINOLITH 511
Inter-Radicular Radiopacities 482
ODONTOGENIC TUMORS 512
RESIDUAL FOCAL OSTEITIS AND OSTEOMAS AND EXOSTOSES 513
CEMENTOMA 482 BENIGN MESENCHYMAL NEOPLASMS 515
IDIOPATHIC OSTEOSCLEROSIS 483 INVERTING PAPILLOMA 516
BISPHOSPHONATE-RELATED ANTRAL CARCINOMA 517
OSTEONECROSIS OF THE JAWS 484 ANTRAL SARCOMA 519
CALCIFYING AND KERATINIZING EPITHELIAL SILENT SINUS SYNDROME 520
ODONTOGENIC CYST/TUMOR 486
ODONTOGENIC ADENOMATOID Ground-Glass Radiopacities 521
TUMOR 486
ODONTOMA 489 FIBROUS DYSPLASIA 521
CENTRAL OSSIFYING OR CEMENTIFYING CHRONIC DIFFUSE SCLEROSING
FIBROMA 489 OSTEOMYELITIS 523
BENIGN OSTEOBLASTOMA 492 OSTEITIS DEFORMANS (PAGET’S DISEASE OF
BONE) 524
Pericoronal Radiopacities 493 HYPERPARATHYROIDISM 526
SEGMENTAL ODONTOMAXILLARY
ODONTOGENIC ADENOMATOID
DYSPLASIA 528
TUMOR 493
OSTEOPETROSIS 529
CALCIFYING EPITHELIAL ODONTOGENIC
TUMOR 494 Multifocal Confluent (Cotton-Wool)
AMELOBLASTIC FIBRODENTINOMA 496 Radiopacities 530
AMELOBLASTIC FIBRO-ODONTOMA 497
ODONTOMA 498 OSTEITIS DEFORMANS (PAGET’S DISEASE OF
ODONTOAMELOBLASTOMA 499 BONE) 530
FLORID OSSEOUS DYSPLASIA 531
Antral Opacities 500 GARDNER’S SYNDROME 533
MAXILLARY SINUSITIS 500 FAMILIAL GIGANTIFORM CEMENTOMA 534
ANTRAL POLYP 502 Cortical Redundancies (Onion-Skin
SINUS MUCOCELE 503 Patterns) 536
PERIAPICAL INFECTION WITH ANTRAL
POLYPS 504 GARRÉ’S PERIOSTITIS 536
PMPH_Eversole_FM.indd xii 1/25/2011 9:48:10 PM
Contents xiii
INFANTILE CORTICAL HYPEROSTOSIS 537 OSTEOGENIC AND CHONDROGENIC
GENERALIZED CORTICAL SARCOMA 545
HYPEROSTOSIS 538 METASTATIC CARCINOMA 546
JUXTACORTICAL OSTEOGENIC
SARCOMA 539
Superimposed Soft Tissue
Radiopacities 547
OSTEOID OSTEOMA 540
MANDIBULAR TORI AND EXOSTOSES 541 SIALOLITHIASIS 547
PHLEBOLITHIASIS 548
Irregular, Ill-Defined Expansile OSSEOUS/CARTILAGINOUS
Radiopacities 542 CHORISTOMA 549
CALCIFYING EPITHELIAL ODONTOGENIC FOREIGN BODIES 550
TUMOR 542 CALCIFIED LYMPH NODES 551
DESMOPLASTIC AMELOBLASTOMA 543 MYOSITIS OSSIFICANS 552
11. DENTAL DEFECTS 555
Alterations in Number: Missing EROSION 575
Teeth 558 HYPERCEMENTOSIS 576
HYPODONTIA 558 Alterations in Structure 577
INCONTINENTIA PIGMENTI 559 DENTAL CARIES 577
HYALINOSIS CUTIS ET MUCOSAE 559 ENAMEL HYPOPLASIA 579
MANDIBULO-OCULO-FACIAL CONGENITAL SYPHILIS 580
DYSCEPHALY 560
DENTAL FLUOROSIS 581
HEREDITARY ECTODERMAL DYSPLASIA 560
SNOW-CAPPED TEETH 582
CHONDROECTODERMAL DYSPLASIA 561
AMELOGENESIS IMPERFECTA, HYPOPLASTIC
Alterations in Number: TYPES 582
Supernumerary Teeth 562 AMELOGENESIS IMPERFECTA,
HYPOMATURATION/HYPOCALCIFICATION
HYPERDONTIA 562 TYPES 584
CLEIDOCRANIAL DYSPLASIA 563 SYNDROME-ASSOCIATED ENAMEL
GARDNER’S SYNDROME 564 DEFECTS 585
DENTINOGENESIS IMPERFECTA 587
Alterations in Morphology 565
OSTEOGENESIS IMPERFECTA 588
MICRODONTIA AND MACRODONTIA 565 DENTIN DYSPLASIA TYPE I 589
ACCESSORY CUSPS AND ROOTS 566 DENTIN DYSPLASIA TYPE II 590
DENTAL TRANSPOSITION 567 REGIONAL ODONTODYSPLASIA 591
ENAMEL PEARL 568 HYPOPHOSPHATASIA 593
DILACERATION 568 VITAMIN D REFRACTORY RICKETS 593
DENS INVAGINATUS (DENS IN DENTE) 570 DENTICLES AND PULP CALCIFICATION 595
TAURODONTISM 571 SEGMENTAL ODONTOMAXILLARY
GEMINATION 571 DYSPLASIA 595
FUSION 572 INTERNAL RESORPTION 597
CONCRESCENCE 573 EXTERNAL RESORPTION 598
ATTRITION 574 SUBCERVICAL RESORPTION 599
ABRASION 575 CORONAL FRACTURE 600
PMPH_Eversole_FM.indd xiii 1/25/2011 9:48:10 PM
xiv Contents
Alterations in Eruption/Exfoliation BILIARY ATRESIA 604
Times 601 POSTMORTEM PINK TEETH 605
PORPHYRIA 605
PREMATURE ERUPTION 601 DENTAL FLUOROSIS 606
DELAYED ERUPTION 601 TETRACYCLINE STAINING 607
IMPACTION 602 EXTRINSIC STAINING 608
PREMATURE EXFOLIATION 603 FOCAL PIGMENTATION 609
Pigmentations 603
ERYTHROBLASTOSIS FETALIS 603
12. FACIAL PAIN AND NEUROMUSCULAR DISORDERS 611
Ophthalmic Division Pain 614 Neck and Throat Pain 638
ODONTOGENIC INFECTION 614 STYLOHYOID SYNDROME (EAGLE’S
FRONTAL/ETHMOIDAL SINUSITIS 615 SYNDROME) 638
VASCULAR OCCLUSIVE DISEASE AND HYOID SYNDROME 638
ANEURYSMS 616 GLOSSOPHARYNGEAL NEURALGIA 639
CAROTIDYNIA 640
Maxillary Division Pain 616
SUPERIOR LARYNGEAL NEURALGIA 641
ODONTOGENIC INFECTION 616 LARYNGEAL NEOPLASMS 641
MAXILLARY SINUSITIS 617
PATHOLOGIC JAWBONE CAVITIES 619 TMJ Region Pain 642
ANTRAL AND MAXILLARY NEOPLASMS 620 MYOGENIC PAIN 642
CLUSTER HEADACHE 621 TYPE I INTERNAL DERANGEMENT
TRIGEMINAL NEURALGIA 623 (REDUCING) 644
POSTHERPETIC NEURALGIA 624 TYPE II INTERNAL DERANGEMENT
COMPLEX REGIONAL PAIN SYNDROME (TRANSIENT LOCK) 646
(CAUSALGIA) 625 TYPE III INTERNAL DERANGEMENT (CLOSED
CRANIAL BASE AND CNS NEOPLASMS 626 LOCK) 647
ATYPICAL FACIAL PAIN 628 MENISCUS PERFORATION 648
OSTEOARTHRITIS (DEGENERATIVE JOINT
Mandibular Division Pain 629 DISEASE) 649
ODONTOGENIC INFECTION 629 RHEUMATOID ARTHRITIS 650
OSTEOMYELITIS 630 ACUTE INFECTIOUS ARTHRITIDES 651
TRAUMATIC NEUROMA 631 MISCELLANEOUS ARTHRITIDES 652
SUBACUTE THYROIDITIS 632 CONDYLAR FRACTURE 653
STOMATODYNIA/GLOSSOPYROSIS 633 SYNOVIAL CHONDROMATOSIS 654
CARDIOGENIC FACIAL PAIN 634 PIGMENTED VILLONODULAR
SYNOVITIS 655
Otogenic Pain 634
ACUTE OTITIS MEDIA 634
Sialogenic Pain 656
CHRONIC OTITIS MEDIA 635 SIALOLITHIASIS 656
HERPES ZOSTER OTICUS 636 ENDEMIC PAROTITIS (MUMPS) 657
MIDDLE EAR NEOPLASMS 637 ACUTE SUPPURATIVE SIALADENITIS 658
PMPH_Eversole_FM.indd xiv 1/25/2011 9:48:10 PM
Contents xv
Temporal Pain 659 CONVERSION TRISMUS 671
ANKYLOSIS 671
MIGRAINE 659 HECHT-BEALS-WILSON SYNDROME 672
MYOGENIC PAIN (TENSION HEADACHE) 659 CORONOID HYPERPLASIA 673
GIANT CELL ARTERITIS 660 CONDYLAR HYPERPLASIA 673
Paresthesia 661 TMJ REGION NEOPLASMS 674
SCLERODERMA 676
MENTAL PARESTHESIA 661
ORAL SUBMUCOUS FIBROSIS 676
INFRAORBITAL PARESTHESIA 662
TETANUS 677
Localized Motor Deficits 664
Generalized Motor Function
FACIAL PARALYSIS 664 Disorders 678
HORNER’S SYNDROME 665
OPHTHALMOPLEGIA 666 AURICULOTEMPORAL SYNDROME 678
HYPOGLOSSAL PARALYSIS 667 JAW-WINKING PHENOMENON 679
SOFT PALATE PARALYSIS 668 MOTOR SYSTEM DISEASE 680
MULTIPLE SCLEROSIS 680
Limited and Deviant Mandibular MUSCULAR DYSTROPHIES 681
Opening 669 MYOTONIAS 682
MUSCLE SPLINTING 669 CONGENITAL FACIAL DIPLEGIA 683
POSTINJECTION/POSTINFECTION HEMIFACIAL ATROPHY 683
TRISMUS 670 MYASTHENIA GRAVIS 684
Appendix I 685
Appendix II 688
Appendix III 688
Appendix IV 689
Appendix V 694
Index 701
PMPH_Eversole_FM.indd xv 1/25/2011 9:48:10 PM
PMPH_Eversole_FM.indd xvi 1/25/2011 9:48:11 PM
The Diagnostic
Process 1
Procurement of the Data Base 2
CHIEF COMPLAINT AND HISTORY OF THE PRESENT ILLNESS 2
MEDICAL AND DENTAL HISTORY 3
PHYSICAL EXAMINATION 4
RADIOGRAPHIC EXAMINATION 4
CLINICAL LABORATORY TESTS 4
Assessment of the Findings 5
Formulating a Differential Diagnosis 5
Securing a Definitive Diagnosis 6
Formulating a Treatment Plan 7
PMPH_Eversole_Chapter-01.indd 1 1/17/2011 3:22:30 PM
The diagnostic process involves four sequen-
tial steps: (1) obtainment of a comprehensive Procurement of the Data Base
overview of the patient’s past and current
health status, referred to as the historical CHIEF COMPLAINT AND
data base; (2) evaluation of all the findings HISTORY OF THE PRESENT
to correlate the chief sign or symptoms with ILLNESS
the current history, other physical findings,
and the medical history; (3) formulation of a The initial contact with the patient should be
differential diagnosis to include all disease met with concern conveying a desire to be of
processes that could conceivably account assistance. Patients are often upset, fearful,
for the collective findings; and (4) arrival at annoyed, or short-tempered when they feel
a definitive diagnosis on the basis of inter- they are ill or have something wrong with
rogation and specific clinical and laboratory them, particularly when pain is the primary
tests that exclude specific diseases and point complaint or when they have sought help
to a definite disease process. Once the diag- from other health practitioners who were
nostic process is consummated, a plan for unable to arrive at a diagnosis. Nonverbal
treatment can be generated with establish- communication such as a hand on the
ment of a follow-up assessment program. shoulder, a look of kindness, or a comment
Thorough and open communication expressing concern and determination to
between doctor and patient is a prereq- help will open the doors to trust and com-
uisite to the diagnostic process. Because munication. Once these subtle gestures have
the ultimate goal is the definitive diagno- helped to establish rapport, an assessment
sis, the doctor is charged with the duty of of the patient’s problem or chief complaint
sleuth par excellence, meaning he or she can be explored. The chief complaint usu-
must develop the communication skills to ally emerges as a symptom, a sign, or both.
become an eminent interrogator. The ques- Symptoms are subjective, represent-
tioning process is as important as having ing a definite problem expressed by the
a large knowledge base regarding disease patient. Common symptoms of oral and
processes and the skills necessary to recog- maxillofacial disease processes include the
nize tissue changes. The process of interro- following:
gation helps to exclude diseases that, on the
basis of physical appearance or symptoms Discomfort: Pain, ache, numbness (hyp-
alone, would have been included as initial esthesia), tingling (paresthesia), itching
possibilities. What questions does one ask? (pruritus), burning, rawness, tenderness,
First, the clinician must have a reasonable and clicking/popping of temporoman-
comprehensive knowledge of the possible dibular joint (TMJ).
disease entities he or she may encounter. Textural changes: Roughness, dryness
Without this knowledge base, the appro- (xerostomia, xerophthalmia), and swelling
priate line of questioning may not be obvi- (growth, enlargement).
ous. Alternatively, the examiner who is Functional changes: Difficulty with swal-
aware of the various diseases sharing com- lowing, opening, or chewing: altered bite,
mon symptoms or physical signs can ask taste, or hearing; difficulty with speech:
appropriate questions to begin the process tooth clenching or grinding: joint sounds;
of elimination (i.e., limiting the differen- loose teeth and bleeding from mouth,
tial diagnosis). As we proceed through the gingiva, or nose.
sequential steps of the diagnostic process,
emphasis is placed on the development of a Once the chief symptom is recorded,
logical approach to interrogation. questioning helps to define the problem
PMPH_Eversole_Chapter-01.indd 2 1/17/2011 3:22:30 PM
The Diagnostic Process 3
more accurately. Interrogation revolving tissue changes that the patient observes
around the chief complaint should explore or changes that may be unknown to the
the nature of the problem, the duration, patient but have been detected during
the periodicity, the location, and associa- the course of the physical examination.
tion with factors known to the patient. For Signs should be characterized in detail by
example, if a patient complains of pain, the exploring their features and history. When
examiner should explore its nature (i.e., a patient states that he or she discovered a
sharp, dull, throbbing, etc.). How long has tissue change, the clinician should attempt
the symptom been a problem? Has it per- to uncover, through questioning, the nature
sisted for a few hours, a few days, or for of the disease from the patient’s perspec-
weeks, or months? What is the periodic- tive, the duration, the location, and any
ity of the pain? Is it constant, intermittent, associated factors. For example, a patient
only at night, only at mealtime? Where is may state that while looking in the mirror
the pain located? It is localized or does it he or she discovered a white patch on the
radiate? Can it be associated with hot liq- tongue. The examiner will want to know
uids, cold liquids, spicy foods, citrus fruits, how the patient perceives the change. Is
sugar, pressure, percussion? A similar line it sore? Can you feel its presence? How
of questioning can be pursued for other long ago did you first notice it? Is that the
subjective complaints or symptoms. only place in your mouth you’ve noticed a
Signs are objective changes that can change? Do you recall biting your tongue
be observed or detected by palpation, per- or burning it?
cussion, auscultation, or analysis of labo-
ratory data. Common signs of oral and
maxillofacial disease processes include the MEDICAL AND DENTAL
following: HISTORY
The recording of the problem—be it a
Soft-tissue changes: White, red, or pig- symptom, a sign, or both—along with the
mented spots or patches; ulcerations; history of the illness should have allowed
blisters; multiple small nodules (papules); the examiner to contemplate a partial list
nodules; papillary growths; localized of suspected disease processes. At this
swellings; and diffuse swellings. point, the chief complaint is put aside until
Hard-tissue changes (Clinical): Dental other aspects of the data base are procured.
changes in number, shape, or structure; The next step in the diagnostic process
localized or diffuse osseous swellings; is to evaluate the patient’s history of ill-
and facial asymmetry. ness. The patient’s general health status is
Hard-tissue changes (Radiographic): reviewed by determining how the patient
Dental changes, radiolucent or feels. Does he or she feel weak or febrile?
radiopaque lesions, and mixed radiolu- Any significant weight loss or loss of appe-
cent/radiopaque lesions. tite? A history of past illness according to
Neuromuscular functional changes: the body’s organ systems is reviewed; the
Paralysis or flaccidness, muscle spasm or examiner knows that certain medical prob-
hypertrophy, sensory deficits, and altera- lems require dental treatment precautions.
tion in salivation. Furthermore, many systemic diseases
manifest observable oral and facial lesions.
Not all patients relate a specific symp- Habits and medications can also affect the
tom. Often, they observe a change in the tissues of the head and neck. Previous hos-
tissues. Objective signs can be noticeable pitalizations and any complications from
PMPH_Eversole_Chapter-01.indd 3 1/17/2011 3:22:31 PM
4 Chapter 1
past medical treatment can have a bear- RADIOGRAPHIC
ing on the oral and maxillofacial tissues. EXAMINATION
Finally, the dental history might have some
influence with regard to the presenting When the patient’s history and physi-
problem. cal examination suggest pain of dental or
osseous origin, salivary occlusion, asym-
metry, or osseous enlargement, appropriate
PHYSICAL EXAMINATION radiographs are obtained to characterize
dental or intraosseous disease processes.
Provided the patient has no significant med- In general, periapical and panoramic films
ical problems that would militate against are used initially. The location of the sus-
proceeding with the physical examina- pected problem dictates the use of specific
tion, the examiner should begin a system- types of radiographs (Table 1.1). New tech-
atic evaluation of the tissues. In medicine, nology is emerging rapidly in radiology;
physical diagnosis involves examination of detailed tissue imaging is possible with
the organ systems. In dentistry, the primary the use of three-dimensional computerized
emphasis is examination of the head and tomography, radioisotopic scanning, xero-
neck. Usually, prior to a detailed evaluation radiography, and nuclear magnetic reso-
of these tissues, the vital signs, including nance imaging techniques. Many of these
blood pressure, pulse, respiration, and tem- techniques are costly, yet may be extremely
perature are assessed. Subsequently, physi- valuable diagnostically as well as for deter-
cal examination should include the external mining extent of disease. In most cases,
structures of the scalp, face, exposed skin, routine radiographs and tomograms are
and hands; the oral, nasal, and laryngeal obtained initially, and special radiographs
cavities; the tympanic membrane; the sali- are obtained as needed or when indicated.
vary glands and neck; the TMJ; and the Cone beam CT has become an extremely
dentition and periodontium. During the valuable tool for dental diagnostics.
physical examination, deviations from nor- The ability of the radiologist or the cli-
mal are recorded. nician to describe the radiomorphology and
Once the physical examination has list diseases known to exhibit specific pat-
been completed, the examiner should recall terns is of major importance. Radiographic
the chief complaint and focus attention on interpretation alone is rarely diagnostic.
physical changes associated with the pre-
senting signs and symptoms. Once a lesion
has been uncovered and clinically char- CLINICAL LABORATORY
acterized, the examiner should proceed TESTS
by ordering adjunctive diagnostic tests.
Many tests are available, and they should Clinical findings may indicate the need
be used discriminantly to avoid excessive for diagnostic clinical tests conducted by
cost to the patient. In general, a differen- the pathology laboratory. These tests are
tial diagnosis is established once the data used to evaluate blood chemistries, immu-
base from the history and physical exami- nologic reactivity (serology), hematologic
nation has been completed. When signs functions, urinalysis, microbiology, and
and symptoms point to a disease process genomic assays. Specific oral signs and
in bone, however, radiographs are usually symptoms may suggest a metabolic dis-
obtained prior to formulation of a differen- ease such as hyperparathyroidism whereby
tial diagnosis. testing for serum calcium, phosphate, and
PMPH_Eversole_Chapter-01.indd 4 1/17/2011 3:22:31 PM
The Diagnostic Process 5
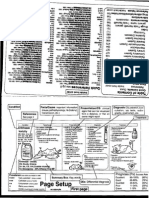
TABLE 1.1 Radiographs in Oral and Maxillofacial Medicine
Area of Investigation Radiography
Dental caries Bitewing
Infections of dental origin Periapicals
Impactions Panoramic, cone beam CT
Jaw lesions Panoramic, cone beam CT
Salivary stones (submandibular) Mandibular occlusal, sonograms, cone beam CT
Salivary stones (parotid) Panoramic, sonograms, cone beam CT
Salivary occlusion, inflammation, tumors Sialogram, radioisotope scan
Sinus lesions Water’s sinus, Caldwell sinus, sinus tomograms, cone beam CT
Other paranasal sinuses Paranasal sinus tomograms, CT scans
Facial deformities CT scans, cephalometric survey
Temporomandibular joints TMJ tomograms, arthrograms, CT scans, nuclear magnetic
resonance images, cone beam CT
Facial fractures Many different radiographs are available to visualize specific
sites, cone beam CT
Jaw and facial tumors Panoramic, CT scans, radioisotope scans, nuclear magnetic
resonance images, PET scans
Vascular jaw lesions Angiography
Dental implant sites Cone beam CT
parathormone levels support or confirm a examiner’s knowledge base is comprehen-
clinical impression; serologic testing for sive, the pieces of the puzzle usually fall
antinuclear antibodies may confirm an into place readily. Occasionally, however,
autoimmune process; a blood count in a some of these puzzles are quite complex
patient with swollen, inflamed gingiva and require more sophisticated diagnostic
may disclose leukemia; a urine sample may procedures. After all the data have been
show protein indicative of renal disease; a reviewed, collated, and correlated, the clini-
culture may be obtained to identify a sus- cian should be able to list possible disease
pected fungal infection; a gene rearrange- entities that could be responsible for the
ment study may confirm lymphoma. The findings. This list of entities represents the
tests performed in the clinical laboratory differential diagnosis.
may, therefore, be the means to a definitive
diagnosis.
Formulating a Differential
Diagnosis
Assessment of the Findings The list of entities subsumed under the
Once all the preliminary data, including designation “differential diagnosis” can be
initial radiographs, is secured, the clini- quite staggering, particularly when only
cian must return to the chief complaint the presenting signs or symptoms are taken
and physical findings. All these data must into account. To the astute clinician, the
be placed in perspective by focusing on interrogative process along with the review
the problems and correlating them with of all findings should have eliminated many
the overall findings. During this process, entities from the differential diagnosis list.
new lines of interrogation may emerge. In this regard, the “differential” has already
The problems and findings represent a been limited in scope. Perhaps only two or
mosaic that must achieve the best fit in three disease processes remain worthy of
order to arrive at a diagnosis. Provided the consideration.
PMPH_Eversole_Chapter-01.indd 5 1/17/2011 3:22:31 PM
6 Chapter 1
So far, the discussion has revolved
around principles and generalities. A spe- Securing a Definitive Diagnosis
cific example may help to clarify some Once a reasonable limited differential diag-
of these general considerations. Suppose nosis is formulated, specific tests are con-
a 40-year-old woman comes to you with ducted. These tests can further limit the
a chief complaint of painful sores in her differential by excluding some diseases
mouth. This is a presenting symptom. If (i.e., the rule out process). It is more advis-
you were to develop a differential diag- able, however, to rule in probable disease
nosis including all lesions that manifest processes. In oral medicine, the most use-
mouth sores, you would probably use up an ful diagnostic tool is biopsy. In most, yet not
entire notebook. This task might be a ter- all instances, the pathologist can provide a
rific academic exercise, but the patient is definitive diagnosis based on histologic
waiting for help. At this point, you would evaluation of the diseased tissue. Some dis-
want to obtain more history. She states that eases exhibit ambiguous or nonspecific his-
they appeared 2 weeks ago, she never had tologic changes, and clinical or laboratory
anything like this before, and they are get- findings are more germane to the process of
ting worse. Despite all this, she does not inclusion or exclusion.
feel tired or feverish. Review of her medi- Another important concept is the prin-
cal history is noncontributory, meaning she ciple of “cause and effect.” Just because two
has a clean bill of health. Furthermore, she factors occur simultaneously (i.e., they are
is not taking any medication. At this point, correlated) doesn’t mean one causes the
the long list in your differential diagnosis other. For example, an ulcer may occur on
may be somewhat shortened. the tongue adjacent to a fractured tooth
You conduct the physical examination cusp. Before concluding a cause-and-effect
and find multiple oral lesions that are red, relationship, the dentist should restore the
ulcerated, and sloughing. Furthermore, you tooth to normal contour and allow 2 weeks
discover a few large intact blisters. Being to pass. If the lesion persists, the initial
a sharp clinician, you conclude that this observation ascribing an irritational caus-
patient suffers from one of the bullous disor- ative role can no longer be substantiated. A
ders. You have now considerably shortened biopsy should then be performed, and it may
the list because less than a dozen bullous reveal an early cancerous lesion. Therefore,
diseases affect the oral tissues. Also, during a cause should be sought in all cases, and if
your examination, you failed to note any found, documentation is pursued to deter-
conjunctival, nasal, or skin lesions. What mine whether or not the observation was
you have is a limited, working differential indeed causative or merely correlative.
diagnosis. Furthermore, based on her age, In most instances, a definitive diagnosis
sex, and distribution of the oral lesions, you can be secured on a clinical, histologic, radio-
can eliminate some of the entities in the logic, and/or laboratory basis. Occasionally,
bullous disease category. a final diagnosis cannot be made because all
This example, then, helps to clarify definitive tests and criteria are ambiguous.
the process of limitation of the differen- Under these circumstances, therapeutic tri-
tial diagnosis. The final step in the diag- als may be in order. Perhaps the diagnosis is
nostic phase of the approach to the patient limited to two or three possibilities; if so, the
involves devising a plan to secure a defini- most likely disease is selected and treated
tive diagnosis. accordingly. If the treatment succeeds, then
PMPH_Eversole_Chapter-01.indd 6 1/17/2011 3:22:31 PM
The Diagnostic Process 7
one can usually conclude, on the basis of that has a potential for recurrence should
response to treatment, that the probable be placed on periodic recall. The length and
diagnosis was correct. periodicity are determined by the behavior
and natural history of the disease process.
Formulating a Treatment Plan Some diseases never recur, and initial ther-
apy is conclusive and complete; therefore,
Once a definitive diagnosis is made, the short-term follow-up and assessment are
most efficacious treatment must be selected. adequate. Alternatively, neoplastic diseases
Depending on the disease, the following and chronic illnesses may require frequent
management strategies are considered: (1) recall assessment and retreatment.
no treatment, (2) surgical removal, (3) phar- The diagnostic process must be thor-
macologic agents, (4) palliative treatment, ough and include history procurement,
(5) behavioral or functional treatment, and physical examination, and radiologic exam-
(6) psychiatric therapy. Referral to a medical ination when indicated. All patient find-
or dental specialist may be required. One ings are integrated to synthesize a differ-
should realize that many diseases cannot ential diagnosis. The differential diagnosis
be cured, and treatment is aimed at control is pared down with selective interrogation
and alleviation of symptoms. Some diseases and specific diagnostic procedures, such as
resolve of their own accord, some require a biopsy and clinical laboratory tests. With
single curative treatment, and others require establishment of a definitive diagnosis, a
prolonged or indefinite treatment. management plan can be devised; results of
After a management strategy has been therapy should be evaluated by follow-up
formulated and implemented, a plan for assessment, and preventive measures, when
prevention of recurrence should be devised. applicable, should be instituted.
For example, a patient with leukoplakia The remainder of this text is designed
showing microscopic evidence of premalig- to aid the clinician in the attainment of
nant change (i.e., dysplasia) may have been a definitive diagnosis; each disease is
successfully treated surgically. Failure to described so that the examiner can evaluate
eliminate important etiologic factors such efficiently the signs and symptoms to arrive
as continued alcohol and tobacco use could at a definitive diagnosis. Most chapters are
result in a recurrence of the disease in the arranged according to physical findings;
same site or in a new location. The clinician the final chapter, dealing with facial pain,
should advise the patient about these poten- being subjective, is outlined according to
tially harmful habits and help the patient to presenting symptoms. The recommended
curtail them. therapy is mentioned briefly, and the reader
The final consideration, and one of may find more detail regarding manage-
paramount importance, is patient follow-up ment by referring to the current references
and assessment. Patients with a disease listed for each disease.
PMPH_Eversole_Chapter-01.indd 7 1/17/2011 3:22:31 PM
a b
Normal mucosa Hyperkeratosis
c d
Acanthosis Lymphocytic infiltration
e f
Extrinsic coating Ulcerative pseudomembrane
White Lesions
PMPH_Eversole_Chapter-02.indd 8 1/17/2011 3:23:32 PM
White Lesions
2
Flat Plaques, Solitary 11 Verrucous/Rippled Plaques 31
FRICTIONAL BENIGN KERATOSES 11 PROLIFERATIVE VERRUCOUS
LEUKOPLAKIA 12 LEUKOPLAKIA 31
ACTINIC CHEILITIS 14 VERRUCOUS CARCINOMA 33
SMOKELESS TOBACCO
KERATOSES 14 Lacey White Lesions 34
SANGUINARIA-INDUCED LICHEN PLANUS 34
KERATOSES 16
LICHENOID REACTIONS 36
DYSKERATOSIS CONGENITA 17
LUPUS ERYTHEMATOSUS 37
FANCONI’S ANEMIA 18
HIV-ASSOCIATED HAIRY
DYSPLASIA, CARCINOMA IN SITU, LEUKOPLAKIA 38
SQUAMOUS CELL CARCINOMA,
AND VERRUCOUS CARCINOMA 19
LICHEN PLANUS
Papular Lesions 40
(HYPERTROPHIC TYPE) 21 KOPLIK SPOTS OF MEASLES 40
MUCOUS PATCHES FORDYCE’S GRANULES 41
(SECONDARY SYPHILIS) 22 DENTAL LAMINA CYSTS, BOHN’S
NODULES, EPSTEIN’S PEARLS 41
Flat Plaques, Bilateral STOMATITIS NICOTINA 42
or Multifocal 23 SPECKLED LEUKOPLAKIA 43
LEUKOEDEMA 23
GENOKERATOSES 24
Pseudomembranous Lesions 44
PLAQUE-FORM LICHEN CHEMICAL BURNS 44
PLANUS 30 CANDIDIASIS (MONILIASIS, THRUSH) 45
CHEEK/TONGUE BITE VESICULO-BULLOUS-ULCERATIVE
KERATOSIS 30 DISEASES 47
PMPH_Eversole_Chapter-02.indd 9 1/17/2011 3:23:34 PM
White lesions of oral mucous membranes Inflammatory lesions that may pro-
appear thus because one or more of the epi- duce thickened epithelium and/or a sur-
thelial layers is thickened or an extrinsic face pseudomembrane appear white; in
or intrinsic pseudomembrane is adherent these instances, the surface coating may be
to the surface mucosa. The white lesions rubbed away with gauze. The diagnosis of
encountered in practice may be subdivided inflammatory white lesions can be secured
into groups on the basis of pathogenesis by obtaining a thorough history, including
or etiologic factors. Developmental white questions regarding use of drugs, sexual
lesions are generally bilateral. Patients habits or promiscuity, recent contact with
relate that a familial pattern exists, because persons manifesting similar illness, or con-
most of the developmental white lesions are tact with injurious chemicals.
genetically inherited (genokeratosis). This chapter illustrates and enumer-
As a gardener’s hands become cal- ates the features of white lesions in the
loused from hours of friction from the hoe, context of clinical features as outlined ear-
so may the oral epithelium become calloused lier. The differential diagnosis for a given
or thickened in response to chronic trauma. white lesion depends on obtaining a his-
Tobacco in its many forms is also consid- tory, with primary considerations of (1) a
ered a local irritant and indeed is associated familial pattern; (2) presence or absence
with carcinomatous transformation in white of a causative agent with notations on oral
lesions of the oral mucosa. The white lesions habits, particularly tobacco use; (3) pres-
associated with physical or tobacco-product ence or absence of associated skin lesions;
irritation are grouped under the heading (4) questions relating to contact with indi-
leukoplakias, as are other white lesions of viduals showing similar lesions; (5) AIDS-
undetermined origin. Because tobacco-as- risk status; (6) presence or absence of fever;
sociated and idiopathic white lesions may and (7) exploration of the nature of the
show microscopic evidence of malignancy, white patch as to tenacity to underlying
biopsy must be performed when (1) a cause structures and ease of removal by rubbing.
cannot be detected or (2) the suspected trau- Based on responses and fi ndings regard-
matic agent is eliminated yet the lesion fails ing these considerations, a ranking of
to involute or regress. Leukoplakia of the entities in the differential diagnosis may
lateral tongue may be indicative of human ensue and, ultimately, biopsy—or in cer-
immunodeficiency virus (HIV) seropositiv- tain instances serology and blood count—
ity, particularly among patients who fall must be performed to obtain a defi nitive
into AIDS-risk categories. diagnosis.
White lesions of nonhereditary dis- The white lesions encountered most
eases may coexist with skin lesions. These frequently are (1) friction, idiopathic or
keratotic dermatoses may, however, occur tobacco-associated leukoplakias, (2) lichen
as oral lesions with skin involvement. As no planus, (3) candidiasis, and (4) Fordyce’s
etiologic agent can be discerned in oral ker- granules.
atotic dermatoses, biopsy must be under- White lesions associated with a poten-
taken to confirm the diagnostic impression tially lethal outcome include (1) premalig-
when classic clinical features of these disor- nant leukoplakias, (2) hairy leukoplakia,
ders are lacking. and (3) lupus erythematosus.
PMPH_Eversole_Chapter-02.indd 10 1/17/2011 3:23:35 PM
White Lesions 11
MICROSCOPIC FEATURES
Flat Plaques, Solitary Frictional irritation may cause thickening
FRICTIONAL BENIGN of any layer or combination of layers of
the epithelium with hyperorthokeratosis,
KERATOSES
hyperparakeratosis, and/or acanthosis.
Figure 2-1 Depending on the degree of irritation,
Age: No predilection
the underlying submucosa may show an
Sex: No predilection inflammatory cell infiltrate, which is usu-
ally chronic.
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
Frictional keratoses represent callus forma-
tion from chronic trauma with resultant White lesions arising from chronic irritation
thickening of one of the epithelial cell lay- may be diagnosed as such when a causative
ers. The white lesions are therefore associ- agent presents itself. Providing the cause can
ated with various etiologic agents, including be eliminated or reduced (e.g., leaving ill-fit-
ill-fitting dental prostheses, chronic irrita- ting dentures out of the mouth for 2 weeks,
tional habits such as cheek- or lip-biting, smoothing irritating tooth cusps, avoiding
overzealous tooth brushing, and white cal- habits), and the white lesion regresses or
luses formed from occluding on edentulous resolves; a cause-and-effect relationship can
ridges or the retromolar pads, a condition be substantiated. Failure of a white lesion
termed oral lichen simplex chronicus. The to regress subsequent to elimination of the
individual lesions may be smooth or irregu- causative agent(s) should arouse suspicion
lar in texture, and their location and con- with regard to precancerous leukoplakia,
figuration coincide with the corresponding and biopsy is then indicated. In addition,
location of the causative agent. Frictional other diseases manifesting white lesions
keratoses may also be multifocal. may coincidentally correspond to denture-
FIGURE 2-1
Frictional keratosis due to
irritation.
PMPH_Eversole_Chapter-02.indd 11 1/17/2011 3:23:35 PM
12 Chapter 2
bearing zones; however, diseases such as more often seen on the buccal mucosa,
lichen planus, moniliasis, or the genokera- mucobuccal fold, and oral floor. These leu-
toses are typically located in regions beyond koplakias may be smooth, ridged, rough,
the confines of a potential irritant. delineated, or diffuse. The smooth form or
planar type fails to exhibit surface irregu-
TREATMENT larity, being homogeneously white without
Elimination of the causative agent is indi- a verrucous texture, yet others may have a
cated. White lesions attributed to a chronic ridged or verrucous appearance. The term
irritant probably have a limited tendency leukoplakia is strictly clinical and has no
to undergo malignant change. Should the implications with regard to microscopy.
lesions fail to resolve after removal of the These lesions are usually benign yet may
irritant, however, a biopsy should be per- show microscopic evidence of premalig-
formed to rule out atypical cell changes that nant cellular change. Whereas leukoplakias
occur independently. as a collective group display microscopic
evidence of dysplasia, carcinoma in situ, or
squamous cell carcinoma in approximately
Additional Reading 20% of the cases, evidence suggests that
the atypical cell changes are less prevalent
Axell T, Holmstrup P, Kramer Irh, Pindborg JJ, Shear M. in the smooth planar form compared with
International seminar on oral leukoplakia and associat- the verrucous appearing lesions. Leukopla-
ed lesions related to tobacco habits. Community Dent kias of the oral floor manifest the highest
Oral Epidemiol. 1984;12:146. incidence of atypical cell change; approxi-
Cawson RA. Leukoplakia and oral cancer. Proc R Soc
Med. 1969;62:610. mately 40% harbor atypical cells.
Natarajan E, Woo SB. Benign alveolar ridge keratosis
(oral lichen simplex chronicus): a distinct clinicopatho- Microscopic features
logic entity. J Am Acad Dermatol. 2008;58(1):151-157.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral The clinical extent does not necessarily pre-
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders; dict the microscopic features. Idiopathic or
1983:92. tobacco-induced leukoplakias may merely
Waldron CA. In: Gorlin RJ and Goldman HM, eds. show hyperorthokeratosis, hyperparakera-
Thoma’s Oral Pathology. Vol 2. 6th ed. St Louis, MO:
C. V. Mosby; 1970:811.
tosis, acanthosis, or a combination. Alterna-
tively, and most important, cellular atypia,
dysplasia, carcinoma in situ, or frank super-
ficially invasive squamous cell carcinoma
LEUKOPLAKIA may be encountered microscopically.
Figure 2-2
Differential diagnosis
IDIOPATHIC/SMOKED TOBACCO-
ASSOCIATED LEUKOPLAKIA Idiopathic and tobacco-associated leukopla-
kia must be differentiated from frictional
Homogeneous Leukoplakia leukoplakia on the basis of history. Lichen
Age: Middle-aged and elderly adults planus, lupus erythematosus, the genokera-
Sex: Males predominantly toses, and inflammatory white lesions must
also be eliminated from consideration on
Clinical features the bases of history and biopsy findings.
White plaques of unknown etiology or
those encountered in smokers and tobacco Treatment
chewers are a common malady that may Biopsy should be performed in all instances
occur on any oral mucosal surface yet are of idiopathic or tobacco-associated leuko-
PMPH_Eversole_Chapter-02.indd 12 1/17/2011 3:23:45 PM
White Lesions 13
FIGURE 2-2
Thickened, diffuse white
lesions representing idio-
pathic leukoplakia.
plakia to ascertain whether or not prema- managed by combined radiotherapy and
lignant cell changes exist. Benign cellular surgery.
features do not preclude future malignant
change in the same location or in a new site.
About 2% to 3% of benign leukoplakias may
progress to carcinoma, whereas 17.5% of all
Additional Reading
oral leukoplakias, including cases with and Bánóczy J, Csiba A. Comparative study of the clinical
picture and histopathologic structure of oral leukopla-
without dysplastic change, progress to car-
kia. Cancer. 1972;29:1230.
cinoma over a mean follow-up period of 7½ Holmstrup P, Vedtofte P, Reibel J, et al. Long-term
years. Most dysplasias fail to progress to car- treatment outcome of oral premalignant lesions. Oral
cinoma and many spontaneously regress. Oncol. 2006;42:461-474.
Recent studies have disclosed that benign Hsue SS, Wang WC, Chen CH, et al. Malignant trans-
formation in 1458 patients with potentially malig-
leukoplakias may progress to carcinoma nant oral mucosal disorders: a follow-up study based
over time in almost comparable numbers in a Taiwanese hospital. J Oral Pathol Med. 2007;36:
to those that are dysplastic. For these rea- 25-29.
sons, patients should be subjected to peri- Mincer HH, Coleman SA, Hopkins KP. Observations on
the clinical characteristics of oral lesions showing his-
odic follow-up with rebiopsy, particularly tologic epithelial dysplasia. Oral Surg Oral Med Oral
when a change in the clinical character of Pathol. 1972;33:389.
a lesion evolves. Lesions with a microscopic Silverman S, Jr, Gorsky M, Lozada F. Oral leukoplakia
diagnosis of dysplasia or carcinoma in situ and malignant transformation. A follow-up study of
2157 patients. Cancer. 1984;53:563.
should be surgically stripped or removed Waldron CA, Shafer WG. Leukoplakia revisited. A clini-
in toto by standard surgery, cryosurgery, or copathologic study of 3256 oral leukoplakias. Cancer.
laser surgery. Invasive carcinoma is usually 1975;36:1386.
PMPH_Eversole_Chapter-02.indd 13 1/17/2011 3:23:45 PM
14 Chapter 2
ACTINIC CHEILITIS TREATMENT
Figure 2-3 A biopsy should be performed to deter-
mine whether or not dysplasia is present.
Age: Middle-aged and elderly adults A lack of premalignant cellular changes in
Sex: Males predominate actinic cheilitis does not preclude future
CLINICAL FEATURES evolvement. Protection from the sun with
solar protective cream containing p-amin-
Solar or ultraviolet light exposure may pre- obenzoic acid (PABA) is recommended.
dispose the vermilion border to keratotic Histologically, atypical change should be
change, and certain individuals whose managed by lip stripping with incontinuity
occupations or hobbies provide continu- wedge resection if a zone of superficial car-
ous exposure to sun are most prone to cinomatous invasion is coexistent.
develop actinic cheilitis. The lower lip If no foci of carcinoma exist, topical
is more prominent and, therefore, more application of 1% 5-fluorouracil cream twice
prone to actinic change than the upper. daily for 2 weeks will remove dysplastic epi-
The lesion is white and usually smooth thelium, allowing for regeneration of nor-
and diffuse. The borders may be sharply mal epithelium. Other effective treatments
delineated from uninvolved vermilion, or include 5% imiquimod cream and photody-
the transition may be gradual. Ulcerations namic therapy with methyl aminolevulinic
or focal zones of highly thickened keratin acid as the photosensitizer and red light at
plaque may indicate early carcinomatous 630 nm.
transformation.
MICROSCOPIC FEATURES Additional Reading
Solar cheilitis reflects a spectrum of micro- Bernier JL, Reynold MC. The relationship of senile elas-
scopic changes similar to leukoplakia. The tosis to actinic radiation and to squamous cell carci-
noma of the lip. Milit Med. 1955;117:209.
early limited changes are restricted to the
Castaño E, Comunión A, Arias D, et al. Photodynamic
keratin layer, which manifests thickening, therapy for actinic cheilitis. Actas Dermosifiliogr.
and the subjacent connective tissue zones, 2009;100:895-898.
which characteristically show clumping, Picascia DD, Robinson JK. Actinic cheilitis: a review of
fragmentation, and granulation of elastic etiology, differential diagnosis, and treatment. J Am
Acad Dermatol. 1987;17:255.
fibers known as solar or senile elastosis. Smith KJ, Germain M, Yeager J, Skelton H. Topical 5%
Progression to cytologic atypia, dysplasia, imiquimod for the therapy of actinic cheilitis. J Am
and frank invasive carcinoma can develop Acad Dermatol. 2002;47:497-501.
in actinic cheilitis. The earliest premalig- Warnock GR, Fuller RP, Jr, Pelleu GB, Jr. Evaluation of
5-fluorouracil in the treatment of actinic keratosis of
nant atypicality is represented by atrophy the lip. Oral Surg Oral Med Oral Pathol. 1981;52:501.
of the spinous cell layer, fragmentation of
the basement membrane, and mild hyper-
SMOKELESS TOBACCO
chromatism and/or pleomorphism of the
basal cells. KERATOSES
Figure 2-4
DIFFERENTIAL DIAGNOSIS
Age: No predilection
Habitual lip chewing must be differenti- Sex: No predilection
ated from actinic cheilitis. Tobacco irritants
CLINICAL FEATURES
(cigars, pipe stems, and reverse smoking)
may induce hyperkeratotic lesions of the White lesions caused by snuff and chewing
lips. tobacco usage are located under the area in
PMPH_Eversole_Chapter-02.indd 14 1/17/2011 3:23:53 PM
White Lesions 15
FIGURE 2-3
Actinic cheilitis of the lip.
FIGURE 2-4
Corrugated white plaques attributed to smokeless tobacco (snuff dipper’s keratosis).
PMPH_Eversole_Chapter-02.indd 15 1/17/2011 3:23:53 PM
16 Chapter 2
which these agents are habitually placed;
they are therefore encountered in the Additional Reading
mucobuccal fold region. The lesion is some- Brown RL, Suh JM, Scarborough JE, Wilkins SA, Jr,
what rough and may manifest an undulat- Smith RR. Snuff dipper’s intraoral cancer; clini-
ing or wrinkled surface. The white areas cal characteristics and response to therapy. Cancer.
are relatively well circumscribed and local- 1965;18:2.
Greer RO, Jr, Poulson TC. Oral tissue alterations asso-
ized to the area of snuff placement. Dur- ciated with the use of smokeless tobacco by teenag-
ing the 1980s and currently, the incidence ers. Part 1. Clinical findings. Oral Surg Oral Med Oral
of smokeless tobacco use by teenagers has Pathol. 1983;56:275.
increased. Rodu B, Jansson C. Smokeless tobacco and oral cancer:
A review of the risks and determinants.Crit Rev Oral
Biol Med. 2004;15:252-263.
MICROSCOPIC FEATURES
Roed-Petersen B, Pindborg JJ. A study of Danish
As with other forms of tobacco-induced snuff-induced oral leukoplakia. J Oral Pathol Med.
leukokeratosis, snuff keratosis may show 1973;2:301.
Rosenfeld L, Callaway J. Snuff dipper’s cancer. Am J
a thickening of one of the epithelial lay- Surg. 1963;106:840.
ers (i.e., hyperorthokeratosis, hyperparak-
eratosis, acanthosis), with a tendency for
“chevron”-shaped projections in the corni- SANGUINARIA-INDUCED
fied layer. Cytologic atypia is rarely seen, KERATOSES
and progression to invasive carcinoma is
Figure 2-5
rare among moist snuff users yet is signifi-
cantly more carcinogenic when dry snuff Age: no predilection
is used or when snuff is mixed with slaked Sex: no predilection
lime, a common additive in India and the
Middle East. CLINICAL FEATURES
Sanguinaria (blood root) is a chemical that
DIFFERENTIAL DIAGNOSIS has been shown to be antimicrobial and was
A white lesion in the mucobuccal fold may placed in dentifrice as well as in a mouth
represent frictional keratosis or leukoplakia rinse preparation to reduce microbial
related to tobacco products. A thorough his- plaque on tooth biofilms. A spurious find
tory will indicate whether or not the lesion among chronic and heavy users of these
is smokeless tobacco related. The “ebbing Sanguinaria products was the appearance
tide” effect on the white surface implicates of leukoplakias, particularly on the maxil-
snuff usage. lary anterior gingival and mucobuccal fold.
This localization has been attributed to the
TREATMENT physiology of mouth rinsing whereby the
All smokeless tobacco-associated white rinse is forcefully extended into the labial
lesions must be examined microscopi- compartment of pursed lips.
cally to rule out premalignancy. If atypi-
MICROSCOPIC FEATURES
cal cytologic changes are present in high
risk populations, complete excision is rec- Most biopsies from Sanguinaria-induced
ommended. Absence of cellular prema- leukoplakias exhibit benign keratosis with-
lignant changes does not preclude future out dysplasia. DNA ploidy studies, how-
evolution to cancer; therefore, the habit ever, have disclosed abnormal DNA content
should be curtailed. Tobacco-specific nit- in some of these lesions and, therefore, both
rosamines are thought to be the chief car- rinse and dentifrice have been withdrawn
cinogens in chewing tobacco and snuff. from the market.
PMPH_Eversole_Chapter-02.indd 16 1/17/2011 3:24:20 PM
White Lesions 17
FIGURE 2-5
Sanguinaria-induced keratoses of the anterior maxillary gingival and vestibule.
DIFFERENTIAL DIAGNOSIS complex (DKC1, TERC, TERT, NOP10,
Sanguinaria leukoplakia may simulate idio- NHP2) or shelterin (TINF2). The syndrome
pathic leukoplakias and plaque-form lichen is characterized by atrophic nail changes,
planus. telangiectatic pigmented reticular lesions of
skin, pancytopenia, and oral white lesions
TREATMENT associated with dorsal tongue depapillation
and atrophy. Premature aging is also fea-
Discontinuing the use of the product is tured. Forty percent of oral lesions progress
required, and many months may elapse to squamous cell carcinoma before the age
before the lesions resolve. of 50.
Additional Reading MICROSCOPIC FEATURES
A nonspecific thickening of the parakeratin
Allen CL, Loudon J, Mascarenhas AK. Sanguinaria- and spinous cell layer is seen. Dysplastic
related leukoplakia: epidemiologic and clinicopatho-
logic features of a recently described entity. Gen Dent. changes, absent in pachyonychia, evolve
2001;49:608-614. and progress to squamous cell carcinoma
Eversole LR, Eversole GM, Kopcik J. Sanguinaria- in dyskeratosis congenita.
associated oral leukoplakia: comparison with other
benign and dysplastic leukoplakic lesions. Oral Surg
DIFFERENTIAL DIAGNOSIS
Oral Med Oral Pathol Oral Radiol Endod. 2000;89:455-
464. The mucosal white lesions and constellation
of other clinical findings of dyskeratosis con-
genita may be confused with pachyonychia
DYSKERATOSIS CONGENITA congenita. Fanconi’s anemia is a significant
Figure 2-6 syndrome to consider in the differential
diagnosis since it presents with bone mar-
Age: Childhood onset
row suppression and oral white lesions that
Sex: No predilection
can progress to carcinoma. Other keratoses
CLINICAL FEATURES such as white sponge nevus, HBID, and
Dyskeratosis congenita (Zinsser-Engman- lichen planus should also be considered.
Cole syndrome) is inherited as either an
autosomal recessive, X-linked or autosomal TREATMENT
dominant disorder with telomere shorten- Close clinical follow-up of oral lesions is
ing mediated by mutations in six genes that mandatory since malignant transformation
encode either components of the telomerase will occur later in life.
PMPH_Eversole_Chapter-02.indd 17 1/17/2011 3:24:20 PM
18 Chapter 2
FIGURE 2-6
Dyskeratosis congenita. White lesions that progress to carcinoma.
deformed thumbs or agenesis. Pancytopenia
Additional Reading occurs with thrombocytopenia and neutro-
Alter BP, Giri N, Savage SA, Rosenberg PS. Cancer in penia. These events occur due to mutations
dyskeratosis congenita. Blood. 2009;113:6549-6557. in a group of core protein complexes (the FA
Armanios M. Syndromes of telomere shortening. Ann genes) whose function involves DNA repair
Rev Genomics Hum Genet. 2009;10:45-61. and antioxidant synthesis. These patients
Kirwan M, Dokal I. Dyskeratosis congenita, stem cells
and telomeres. Biochim Biophys Acta. 2009;1792(4D): may develop leukoplakias located on the
371-379. tongue or floor of the mouth that can later
Walne AJ, Dokal I. Advances in the understanding of transform to carcinoma.
dyskeratosis congenita. Br J Haematol. 2009;145:
164-172.
MICROSCOPIC FEATURES
The keratotic lesions in Fanconi’s anemia
FANCONI’S ANEMIA exhibit the same histology as those found
Figure 2-7 in idiopathic leukoplakias (i.e., benign kera-
tosis, dysplasia, carcinoma).
Age: Childhood onset
Sex: No predilection DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES The white lesions are similar to other leuko-
Fanconi’s anemia is an autosomal recessive plakias being flat plaques. The unique con-
genetic disorder involving as many as 13 stellation of syndromic characteristics usu-
genes of which mutations occur. If both par- ally allow for a straightforward diagnosis.
ents are carriers, there is a 25% risk of having
an affected child. Affected children develop TREATMENT
bone marrow suppression with erythrocyte The pancytopenia and leukemia can be
macrocytosis, and many will progress to managed by chemotherapy with greatest
acute myelogenous leukemia. Digital anom- response being seen after bone marrow
alies are characterized by anatomically transplantation. Importantly, many head
PMPH_Eversole_Chapter-02.indd 18 1/17/2011 3:24:24 PM
White Lesions 19
DYSPLASIA, CARCINOMA
IN SITU, SQUAMOUS
CELL CARCINOMA, AND
VERRUCOUS CARCINOMA
Figure 2-8
Age: Elderly adults
Sex: Males predominate
CLINICAL FEATURES
Early cancerous change within the oral epi-
thelium may initially manifest as a white
lesion or may arise in a preexisting leuko-
plakic area. Depending on the extent of the
tumor, the white lesion may be relatively
macular or plaque-like or, in larger lesions,
associated with tumefaction and indura-
tion. Whereas oral cancer is generally local-
ized, it may, on occasion, be multifocal with
numerous isolated separate white lesions
manifesting microscopic evidence of neo-
plastic transformation. Location is highly
significant when considering the possibility
of malignancy; although malignant change
may be seen on any surface, the most com-
mon locations are oral floor, alveolar ridge
FIGURE 2-7 and vestibule, and lateral posterior tongue.
Fanconi’s anemia. Thumb anomaly, oral carcinoma. The most important contributing etio-
logic factors regarding carcinogenesis of
and neck cancers have evolved in Fanconi oral epithelium are use of tobacco and a high
patients after marrow transplantation. intake of alcohol. Patients with untreated
syphilis and the Plummer-Vinson syndrome
are also prone to develop oral or oropharyn-
Additional Reading geal cancer. Recent research indicates that
a subpopulation of patients have tumors
Auerbach AD, Rogatko A, Schroeder-Kurth TM. associated with, and probably caused by,
International Fanconi Anemia Registry: relation of
clinical symptoms to diepoxybutane sensitivity. Blood. human papillomavirus (HPV) type 16. In
1989;3:391-396. this subset, the tumors are found at the
Garcia-Higuera I, Taniguchi T, Ganesan S, et al. base of the tongue and the tonsillar pillar.
Interaction of the Fanconi anemia proteins and BRCA1 As emphasized under the section on leuko-
in a common pathway. Mol Cell. 2001;7:249-262.
Masserot C, Peffault de Latour R, Rocha V, et al. Head plakias associated with tobacco, the appar-
and neck squamous cell carcinoma in 13 patients with ent clinical innocence of white patches can
Fanconi anemia after hematopoietic stem cell trans- be misleading; the most innocuous lesion
plantation. Cancer. 2008;113:3315-3322. may be cytologically malignant. One excep-
Reinhard H, Peters I, Gottschling S, et al. Squamous
cell carcinoma of the tongue in a 13-year-old girl
tion to clinical predictability regarding
with Fanconi anemia. J Pediatr Hematol Oncol. suspicion of potential malignancy may be
2007;29:488-491. encountered in the white lesion associated
PMPH_Eversole_Chapter-02.indd 19 1/17/2011 3:24:35 PM
20 Chapter 2
FIGURE 2-8
Dysplastic and neoplastic
white lesions. All showed
microscopic evidence of dys-
plasia or carcinoma.
with zones of erythema, so-called speckled subjacent connective tissue. Violations of
leukoplakia. Isolated mixed red and white the basement membrane integrity results
lesions should be considered malignant in superficially invasive carcinoma, which
until proven otherwise (i.e., by biopsy). then progresses to frank squamous cell
A variant form of oral squamous cell carcinoma.
carcinoma that is classically a warty-ap- Invasive squamous cell carcinoma
pearing keratotic white lesion is verrucous may contain islands and nests of tumor
carcinoma (see Chapter 6). cells that retain the characteristics of oral
epithelium by manufacturing the chief pro-
tective products of that organ, albeit dis-
MICROSCOPIC FEATURES organized, keratin and parakeratin. These
Epithelial dysplasia, carcinoma in situ, differentiated tissues are often arranged
and invasive squamous cell carcinoma are, in laminated whorls termed keratin pearls.
respectively, progressively advanced stages Tumors with this histologic morphology
of malignancy. When they are characterized are termed well-differentiated carcinomas
clinically as white lesions, they manifest and are associated with a slower course,
a thickening of the keratin or parakeratin lower metastatic potential, and thus a bet-
layer. The earliest changes, termed dysplasia, ter prognosis. A lack of, or a diminution in,
begin in the dividing cells of the basilar and keratin formation connotes a more rapidly
parabasilar layers. Initial changes include progressing lesion with a poor prognosis
nuclear hyperchromatism, pleomorphism, and is termed poorly differentiated carci-
and an increase in mitotic figures. By defi- noma. A moderately differentiated lesion
nition, all layers, top to bottom, must evince logically falls between these two extremes
atypical cell changes in carcinoma in situ; both morphologically and behaviorally.
however, the basement membrane remains Those tumors associated with HPV 16 tend
intact without evidence of invasion into the to show features that are differentiated
PMPH_Eversole_Chapter-02.indd 20 1/17/2011 3:24:41 PM
White Lesions 21
along the lines of tonsillar crypt epithe- El-Mofty SK, Lu DW. Prevalence of high-risk human
lium; they tend to have a better prognosis papillomavirus DNA in nonkeratinizing (cylindrical
cell) carcinoma of the sinonasal tract: a distinct clini-
than non-HPV carcinomas of the head and copathologic and molecular disease entity. Am J Surg
neck. P16 is an immunohistochemical sur- Pathol. 2005;29:1367-1372.
rogate marker for HPV 16. Eversole LR. Dysplasia of the upper aerodigestive
tract squamous epithelium. Head and Neck Pathol.
2009;3:63-68.
DIFFERENTIAL DIAGNOSIS Pindborg JJ, Restrup G, Poulsen HE, et al. Studies in
oral leukoplakias. V. Clinical and histologic signs of
White lesions associated with tumefaction malignancy. Acta Odontol Scand. 1963;20:407.
and induration present no problem in the Silverman S, Jr, Gorsky M, Lozada F. Oral leukoplakia
clinical diagnosis, yet biopsy is indicated and malignant transformation. A follow-up study of
to determine the grade of malignancy (i.e., 2157 patients. Cancer. 1984;53:563.
Waldron CA, Shafer WG. Leukoplakia revisited. A clini-
differentiation of tumor cells) prior to plan- copathologic study of 3256 oral leukoplakias. Cancer.
ning therapy. Early malignant change man- 1975;36:1386.
ifesting a plaque-like white lesion must be
differentiated primarily from frictional leu-
koplakias, benign leukoplakias, and lichen LICHEN PLANUS
planus. When a causative agent cannot be (HYPERTROPHIC TYPE)
identified or eliminated, an adequate his- Figure 2-9
tory and biopsy are necessary.
Age: No predilection
Sex: No predilection
TREATMENT
Dysplasia or carcinoma in situ, if local- CLINICAL FEATURES
ized, can be managed by wide local exci- Lichen planus is described in greater detail
sion, obtaining margins free from atypical later. The disease is a delayed hypersen-
changes; margins 1 cm away from clini- sitivity reaction in which an identifiable
cally involved tissue should be adequate, antigenic stimulus is usually not evident.
yet microscopic confirmation is mandatory. The hypertrophic form is typically located
Diffuse or multifocal dysplasia or carcinoma on the dorsal tongue that is pavemented
in situ may be treated by surgery or radia- in confluent thick white plaques. These
tion therapy. Invasive carcinoma requires plaque-like lesions may also occur on the
a complete work-up with evaluation of the palate and the buccal mucosa. There may
neck, chest radiographs, and the presence of be some areas with a lacey reticulated pat-
other symptoms. As treatment may include tern, but oftentimes these typical lichenoid
a variety of therapeutic methods either figures are not present.
alone or in combination, including surgery,
laser surgery, radiation, and chemotherapy, MICROSCOPIC FEATURES
invasive squamous cell carcinoma should A chronic interface mucositis is present,
be evaluated and managed by a physician characterized by a patchy or band-like lym-
experienced in head and neck oncology. phocytic infiltrate in juxtaposition to the
basal cell layer of the overlying epithelium.
The cells are a mixture of CD4 and CD8 T
Additional Reading lymphocytes. The infiltrated basal cell layer
Bánóczy J, Csiba A. Occurrence of epithelial dysplasia
shows cytoplasmic fragmentation or liq-
in oral leukoplakia: analysis and follow-up study of 12 uefaction. Tongue cancer occurs in 0.5% to
cases. Oral Surg Oral Med Oral Pathol. 1976;42:766. 1.0% of cases, and when dysplasia is evident
PMPH_Eversole_Chapter-02.indd 21 1/17/2011 3:24:49 PM
22 Chapter 2
FIGURE 2-9
Dorsal tongue and buccal
mucosa with plaque-form
(hypertrophic) lichen planus.
along with lichen planus features, the term MUCOUS PATCHES
lichenoid dysplasia has been used. (SECONDARY SYPHILIS)
Figure 2-10
DIFFERENTIAL DIAGNOSIS
The hypertrophic or plaque form of lichen MUCOUS PATCHES OF SYPHILIS
planus is easily confused with various Age: Adults
forms of leukoplakia. Sex: No predilection
Clinical Features
TREATMENT
Mucous patches are smooth-surfaced plaques
Close periodic follow-up is recommended
that manifest a glistening, opalescent charac-
and any zones of ulceration, redness, or
ter and are seen 6 to 8 weeks after formation
positive toluidine blue uptake should be
of the chancre. In addition to the mucosal
biopsied.
patches, split papules at the commissure
and a maculopapular rash may be present.
Additional Reading A history of promiscuous sexual activity can
usually be obtained, although some patients
Main JH, Birt BD, From L. Hypertrophic lichen planus may deny such activities. The lesions persist
of the oral mucosa. J Dent Assoc S Afr. 1992;47:216- for 1 to 3 weeks, after which they resolve.
218.
Setterfield JF, Black MM, Challacombe SJ. The man-
The lesions in this stage are infectious.
agement of oral lichen planus. Clin Exp Dermatol.
2000;25:176-182. Microscopic Features
Tan E, Malik R, Quirk CJ. Hypertrophic lichen planus
mimicking squamous cell carcinoma. Australas J Parakeratosis and fibrinous exudate over
Dermatol. 1998;39:45-47. both intact and focally ulcerated epithelium
PMPH_Eversole_Chapter-02.indd 22 1/17/2011 3:24:49 PM
White Lesions 23
FIGURE 2-10
Secondary syphilis, mucous patches, maculopapular rash, soles of feet.
can be seen. The submucosa contains an Fiumara NJ. Oral lesions of syphilis. Med Aspects Hum
avid plasma cell infiltrate. The spirochete is Sexuality. 1972;6:68.
Fiumara NJ. Venereal disease of the oral cavity. J Oral
not visible on routine staining; a Warthin- Pathol Med. 1976;31:36.
Starry silver stain will demonstrate the Herrero-González JE, Parera Amer ME, FerranFarrés
microorganism in tissue sections. M, et al. Syphilitic mucous patches: the resurgence of
an old classic. J Dermatol. 2008;47:1281-1283.
Meyer I, Shklar G. The oral manifestations of acquired
Differential Diagnosis syphilis. Oral Surg Oral Med Oral Pathol. 1967;23:34.
Mucous patches may resemble a variety of
white lesions of the oral cavity; because they
are highly infectious, the clinician should Flat Plaques, Bilateral or
always be aware of the fact that oral white Multifocal
lesions may be luetic. The primary consid-
erations in the clinical differential diagno- LEUKOEDEMA
sis include moniliasis, plaque-form lichen Figure 2-11
planus, or leukoplakia of one type or another.
An adequate history should elicit suspicion Age: No predilection
of syphilis, and the diagnosis may be con- Sex: No predilection
firmed by fluorescent treponemal antibody
CLINICAL FEATURES
test or Venereal Disease Research Labora-
tory test. A smear with dark-field micros- Leukoedema occurs in blacks and dark-
copy will demonstrate motile spirochetes. skinned whites and is encountered so
frequently that it should be considered a
Treatment normal variation in these individuals. The
lesion is bilateral and diffuse, involving the
Treatment for syphilis is penicillin. The
buccal mucosa, and shows a filmy, mother-
patient can be referred to a dermatologist or
of-pearl appearance, often with delicate
general physician for treatment.
overlapping curtain-like mucosal folds.
When the mucosa is stretched, the white
Additional Reading appearance is diminished.
Compilato D, Amato S, Campisi G. Resurgence of syphi- MICROSCOPIC FEATURES
lis: a diagnosis based on unusual oral mucosa lesions.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. The epithelium displays acanthosis, parak-
2009;108:e45-e49. eratosis, and spongiosis.
PMPH_Eversole_Chapter-02.indd 23 1/17/2011 3:25:01 PM
24 Chapter 2
FIGURE 2-11
Leukoedema covering entire buccal mucosa.
DIFFERENTIAL DIAGNOSIS Martin JL, Crump EP. Leukoedema of the buccal muco-
sa in Negro children and youth. Oral Surg Oral Med
The diffuse delicate mother-of-pearl sheen Oral Pathol. 1972;34:49.
and the propensity to affect blacks are char-
acteristics that permit differentiation from
other hereditary white lesions of the genok- GENOKERATOSES
eratosis group. The primary entities in the
differential diagnosis include white sponge WHITE SPONGE NEVUS
nevus and hereditary benign intraepithe- Figure 2-12
lial dyskeratosis (HBID), both of which Age: Childhood onset
are thicker, plaque-like, and show specific Sex: No predilection
microscopic features.
Clinical Features
TREATMENT White sponge nevus, inherited as an
autosomal dominant trait, appears, from
No treatment is necessary.
ultrastructural observations, to represent
a defect in epithelial maturation involv-
ing tonofilament formation with impaired
Additional Reading normal desquamation of the superficial
Archard HO, Carlson KP, Stanley HR. Leukoedema of
strata of cells. Mutations have been identi-
the human oral mucosa. Oral Surg Oral Med Oral fied in the genes coding for keratin 4 and
Pathol. 1968;25:717. 13. The condition is characterized by dif-
Durocher RT, Thalman R, Fiore-Donno G. Leukoedema fuse and, sometimes, patchy white lesions
of the oral mucosa. J Am Dent Assoc. 1972;85:1105.
Martin JL. Leukoedema: an epidemiological study in
of the buccal mucosa, bilaterally, with
white and African Americans. J Tenn Dent Assoc. involvement of the tongue and occasion-
1997;77:18. ally other oral mucosal sites. In severely
PMPH_Eversole_Chapter-02.indd 24 1/17/2011 3:25:05 PM
White Lesions 25
affected individuals, the buccal mucosal diagnosis. Biopsy will disclose characteristic
lesions are creased and exhibit corru- features.
gated vertical folds. The conjunctivas are
spared; however, vaginal, esophageal, Treatment
and anal mucous membranes may harbor
No treatment is necessary.
white lesions similar to those of the oral
tissues.
Additional Reading
Microscopic Features
Cannon AB. White sponge nevus of the mucosa (nae-
The epithelium shows parakeratosis and vus spongiosus albus mucosae). Arch Dermatol Syph.
acanthosis with spongiosis. Parallel striae 1935;31:365.
of condensed parakeratin traverse the sur- Martelli H, Jr, Pereira SM, Rocha TM, et al. White
sponge nevus: report of a three-generation family.
face layers in oblique planes. Individual cell Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
keratinization may be seen in the spinous 2007;103:43-47.
cell layer. Ultrastructurally, some spinous Richard G, De Laurenzi V, Didona B, et al. Keratin
layer cells differentiate early, becoming 13 point mutation underlies the hereditary mucosal
epithelial disorder white sponge nevus. Nat Genet.
enriched with tonofilaments that are com- 1995;11:453-455.
pacted in disarray. Rugg EL, McLean WH, Allison WE, et al. A mutation
in the mucosal keratin K4 is associated with oral white
sponge nevus. Nat Genet. 1995;11:450-452.
Differential Diagnosis Whitten JB. The electron microscopic examination of
Other white lesions do not tend to be as congenital keratosis of the oral mucous membranes. I.
White sponge nevus. Oral Surg Oral Med Oral Pathol.
thick and diffuse as white sponge nevus; 1970;29:69.
however, HBID, lichen planus, and candidi- Witkop CJ, Gorlin RJ. Four hereditary mucosal syn-
asis should be considered in the differential dromes. Arch Dermatol. 1961;84:762.
FIGURE 2-12
White sponge nevus.
Thick bilateral plaques
that cover most of
the buccal mucosa
and lateral tongue.
PMPH_Eversole_Chapter-02.indd 25 1/17/2011 3:25:17 PM
26 Chapter 2
HEREDITARY BENIGN
INTRAEPITHELIAL DYSKERATOSIS
Figure 2-13
Age: Childhood onset
Sex: No predilection
Clinical Features
HBID is inherited as an autosomal domi-
nant trait, and electron microscopic studies
have disclosed a defect in keratinization
characterized by cytoplasmic accumula-
tion of tonofilaments with loss of cellular
interdigitation and desmosomes. A dupli-
cation in chromosome 4q35 is associated
with HBID. As with the other genok-
eratoses, HBID manifests diffuse white FIGURE 2-13
plaques of the buccal mucosa and tongue, Hereditary benign intraepithelial dyskeratosis pres-
and secondary candidiasis is commonly ents with oral white lesions.
encountered. In addition to the oral signs
are coexistent conjunctival telangiectasias
and occasionally thickened plaques of the the muco-oculocutaneous syndromes in
bulbar conjunctiva, which may eventuate which the oral lesions are either ulcerative,
in blindness. The disease was originally bullous, or erythematous.
described in a racial isolate group in the
Carolina states.
Treatment
Microscopic Features No treatment is necessary. Because of the
potential for blindness, genetic counseling
Acanthosis with both hyperorthokeratosis may be in order.
and hyperparakeratosis is present within
the epithelium. The pathognomonic fea-
tures are benign dyskeratotic changes
consisting of the cell-within-a-cell phe-
Additional Reading
nomenon and individual cell keratiniza- Allingham RR, Seo B, Rampersaud E, et al. A duplica-
tion in chromosome 4q35 is associated with hereditary
tion, similar to those features encountered benign intraepithelial dyskeratosis. Am J Hum Genet.
in Darier-White’s disease; however, no 2001;68:491-494.
intraepithelial cleavage occurs. Periodic Haisley-Royster CA, Allingham RR, Klintworth GK,
acid-Schiff (PAS) staining may disclose the et al. Hereditary benign intraepithelial dyskeratosis:
report of two cases with prominent oral lesions. J Am
presence of Candida mycelia in the corni- Acad Dermatol. 2001;45:634-636.
fied layer. Sadeghi EM, Witkop CJ, Jr. Ultrastructural study of
hereditary benign intraepithelial dyskeratosis. Oral
Differential Diagnosis Surg Oral Med Oral Pathol. 1977;44:567.
Von Sallman L, Paton D. Hereditary benign intraepi-
The oral white lesions must be differenti- thelial dyskeratosis. I. Ocular manifestations. Arch
ated from those in white sponge nevus, Ophthalmol. 1960;63:421.
Witkop CJ, Shankle DH, Graham JB, et al. Hereditary
pachyonychia congenita, and lichen planus. benign intraepithelial dyskeratosis. II. Oral manifes-
The combination of eye and oral lesions in tations and hereditary transmission. Arch Pathol Lab
this disease should not be confused with Med. 1960;70:696.
PMPH_Eversole_Chapter-02.indd 26 1/17/2011 3:25:26 PM
White Lesions 27
KERATOSIS FOLLICULARIS
(DARIER-WHITE’S DISEASE)
Figure 2-14
Age: Generally adult onset
Sex: No predilection
Clinical Features
Keratosis follicularis is a dermatologic disor-
der manifesting orange-yellow papular and
white keratotic lesions of skin. It is inherited
as an autosomal dominant trait that affects
cell-to-cell adhesion and keratinization
resulting from numerous mutations in ade-
nosine triphosphate (ATP) calcium trans-
port proteins (ATP2A2). A coexistent defect
in cell-mediated immunity has also been
uncovered. Oral lesions are not seen in all
patients, yet when present, they are papular
and usually keratotic. Buccal mucosa, lips,
palate, and tongue are the favored oral loca-
tions. Other mucous membranes including
vulva, vagina, and anus may be involved.
Microscopic Features
Surface hyperkeratosis is present. Within FIGURE 2-14
the spinous cell layer are dyskeratotic Keratosis follicularis. Orange papular lesions and
changes represented by the cell-within-a- keratoses of skin with confluent white plaques.
(Courtesy of Dr. Dwight Weathers.)
cell phenomenon known as corps ronds and
pyknotic elongated nuclei termed grains. A
suprabasilar cleavage is present with acan- confused with other oral lesions showing
tholysis; formation of wandering rete ridges multiple polyps or papules, including pyos-
manifesting cleft-like spaces produces a vil- tomatitis vegetans, verrucous carcinoma,
lous pattern. The microscopic appearance and denture papillomatosis. Biopsy affords a
may be confused with pemphigus vulgaris definitive diagnosis.
and familial pemphigus (Hailey-Hailey dis-
ease). Ultrastructural evidence of defective Treatment
cell maturation involving the tonofilament/
Retinoids have been used in high doses, the
desmosomal apparatus is extant.
rationale being an attempt to eliminate the
degree of skin keratinization. This treat-
Differential Diagnosis ment is of limited value.
The multipapular or cobblestone appearance
and characteristic skin lesions differentiate
Darier-White’s disease from the other genok- Additional Reading
eratoses that generally manifest oral white
Gorlin RJ, Chaudhry AP. The oral manifestation of kera-
lesions in a more diffuse or plaque-like pat- tosis follicularis. Oral Surg Oral Med Oral Pathol.
tern. This white papular eruption may be 1959;12:1468.
PMPH_Eversole_Chapter-02.indd 27 1/17/2011 3:25:29 PM
28 Chapter 2
Spouge JD, Trott JR, Chesko G. Darier-White’s disease: sites, and are usually limited in terms of the
a cause of white lesions of the mucosa. Oral Surg Oral extent of mucosal tissues affected.
Med Oral Pathol. 1966;21:441.
Weathers DR, Driscoll RM. Darier’s disease of the
oral mucosa. Oral Surg Oral Med Oral Pathol. Microscopic Features
1974;37:711. A nonspecific thickening of the parakeratin
Gottlieb SK, Lutzner MA. Darier’s disease: an electron
microscopic study. Arch Dermatol. 1973;107:225. and spinous cell layer is seen. Dysplastic
Ren YQ, Gao M, Liang YH, et al. Five mutations of changes are absent in pachyonychia and do
ATP2A2 gene in Chinese patients with Darier’s dis- not evolve and progress to squamous cell
ease and a literature review of 86 cases reported in carcinoma
China. Arch Dermatol Res. 2006;298:58-63.
Differential Diagnosis
PACHYONYCHIA CONGENITA The bilateral mucosal white lesions of pachy-
Figure 2-15 onychia congenita may be confused with
Age: Childhood onset
white sponge nevus, HBID, and lichen planus;
Sex: No predilection however, the fingernail changes, when con-
sidered in conjunction with the oral lesions,
Clinical Features provide the diagnostic clinical features of
Pachyonychia congenita (Jadassohn-Le- the disease. Candidiasis of the oral mucosa
wandowsky syndrome) is an autosomal with fingernail involvement should be con-
dominant disorder manifesting oral white sidered in the differential diagnosis and can
lesions and laminated thickening of the be ruled out by obtaining an oral cytologic
finger- and toenails. This genokeratosis smear that can be stained for hyphae.
involves mutations in keratins K6a, K16,
and K17. The oral white lesions are bilateral Treatment
on the buccal mucosa, tongue, and other No treatment is necessary.
FIGURE 2-15
Pachyonychia congenita
showing thickened nails
(upper left) and surgi-
cally removed nail beds
(lower left) with white
lesions of oral mucosa.
PMPH_Eversole_Chapter-02.indd 28 1/17/2011 3:25:41 PM
White Lesions 29
may occur on the buccal mucosa, yielding
Additional Reading a patchy plaque or verrucous appearance.
Gorlin RJ, Chaudhry AP. Oral lesions accompanying Partial anodontia, strabismus with nystag-
pachyonychia congenita. Oral Surg Oral Med Oral mus, and epilepsy may also be seen.
Pathol. 1958;11:541.
Maser ED. Oral manifestations of pachyonychia congen-
ita: Report of a case. Oral Surg Oral Med Oral Pathol.
Microscopic Features
1977;43:373. Skin lesions in the vesicular stage show
Stieglitz JB, Centerwall WR. Pachyonychia congenita intraepithelial vesicle formation with
(Jadassohn-Lewandowsky syndrome): a seventeen-
member, four-generation pedigree with unusual numerous eosinophils. Pigmented zones
respiratory and dental involvement. Am J Med Genet. display incontinence of melanin granules
1983;14:21. from the basal cells with accumulation in
Leachman SA, Kaspar RL, Fleckman P, et al. Clinical dermal or submucosal macrophages. White
and pathological features of pachyonychia congenita.
J Investig Dermatol Symp Proc. 2005;10:3-17 lesions are characterized by hyperorthok-
Liao H, Sayers JM, Wilson NJ, et al. A spectrum of muta- eratosis, hyperparakeratosis, and acantho-
tions in keratins K6a, K16 and K17 causing pachyony- sis. Individual cell keratinization may be
chia congenita. J Dermatol Sci. 2007;48(3):199-205. present.
INCONTINENTIA PIGMENTI Differential Diagnosis
Figure 2-16
The white lesions encountered intraorally
Age: Begins during infancy
Sex: Females
may resemble those seen in other genokera-
toses yet are generally focal and patchy. The
Clinical Features other components of this disorder, includ-
Incontinentia pigmenti is inherited as a dom- ing skin discoloration and keratosis as well
inant trait, is lethal in males, and manifests as partial anodontia, separate this entity
both skin and dental defects. The disease is from other genetic diseases manifesting
caused by deletions in chromosome Xq28 IP. oral white lesions.
The skin lesions vary from reticulated slate-
gray pigmentations to vesicles and verru- Treatment
cous keratoses. Oral mucosal white lesions There is no treatment.
FIGURE 2-16
Oral lesions on buccal mucosa
in an infant with incontinentia
pigmenti along with keratoses
and focal pigmentations of
skin. (Courtesy of Dr. Sheldon
Rovin.)
PMPH_Eversole_Chapter-02.indd 29 1/17/2011 3:25:49 PM
30 Chapter 2
from anterior to posterior, following the
Additional Reading plane of dental occlusion. With appropriate
Schulze C. In Gorlin RJ, Goldman HM, eds. Thoma’s questioning and observation, the habit is
Oral Pathology. Vol 1. 6th ed. St Louis, MO: C. V. usually revealed.
Mosby; 1970:130.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral MICROSCOPIC FEATURES
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
1983:823. Severe parakeratosis is seen along with
Russell DL, Finn SB. Incontinentia pigmenti (Bloch- acanthosis. The parakeratotic layer is often
Sulzberger syndrome): a case report with emphasis on
edematous and the surface may be colo-
dental manifestations. J Dent Child. 1967;34:494.
Fusco F, Paciolla M, Pescatore A, et al. Microdeletion/ nized by basophilic bacterial organisms.
duplication at the Xq28 IP locus causes a de novo There is no carcinomatous tendency.
IKBKG/NEMO/IKKgamma exon4_10 deletion in
families with Incontinentia Pigmenti. Hum Mutat. DIFFERENTIAL DIAGNOSIS
2009;30:1284-1291.
The lesions should be differentiated from
other leukoplakias, hairy leukoplakia in
particular. Cheek- and tongue-bite kera-
PLAQUE-FORM LICHEN
toses do not harbor Epstein-Barr virus
PLANUS (SEE ABOVE) (EBV) DNA.
Figure 2-17
TREATMENT
CHEEK/TONGUE BITE
The lesions resolve when the habit is elimi-
KERATOSIS nated, and cessation may be facilitated by
Figure 2-18 fabrication of a bite splint.
Age: Children and young adults
Sex: No predilection Additional Reading
CLINICAL FEATURES Bouquot JE, Gorlin RJ. Leukoplakia, lichen planus, and
Chronic cheek and tongue biting is a form other oral keratoses in 23,616 white Americans over
the age of 35 years. Oral Surg Oral Med Oral Pathol.
of frictional benign keratosis yet is clinically 1986;61:373-381.
distinct. It evolves from a habit much like Woo SB, Lin D. Morsicatio mucosae oris—a chronic oral
nail biting. The lesions are white and often frictional keratosis, not a leukoplakia. J Oral Maxillofac
shaggy and have been termed morsicatio Surg. 2009;67:140-146.
Green TL, Greenspan JS, Greenspan D, De Souza YG.
mucosae oris. Despite this shaggy appear- Oral lesions mimicking hairy leukoplakia: a diag-
ance, the keratinized surface is tenacious. nostic dilemma. Oral Surg Oral Med Oral Pathol.
These white lesions are oriented linearly 1989;67:422-426.
FIGURE 2-17
Multiple pavement like ker-
atotic plaques in hypertro-
phic form of lichen planus.
PMPH_Eversole_Chapter-02.indd 30 1/17/2011 3:25:57 PM
White Lesions 31
FIGURE 2-18
Cheek- and tongue-biting
frictional keratoses along
the occlusal plane.
extensive. On long-term follow-up, many
Verrucous/Rippled Plaques of these lesions progress to verrucous car-
cinoma or squamous cell carcinoma. Some
PROLIFERATIVE VERRUCOUS of these lesions have been shown to harbor
LEUKOPLAKIA HPV DNA. Elderly females, most of whom
Figure 2-19 do not use tobacco, contract this condi-
tion and, despite excision, recurrence is
Age: Elderly probable.
Sex: Females predominate
CLINICAL FEATURES MICROSCOPIC FEATURES
Proliferative verrucous leukoplakia (PVL) There is a spectrum of histologic changes
is a clinically, rather than histologically, that are seen in PVL. The disease represents
defined entity characterized by a diffuse a continuum that progresses from benign
warty or papillary white appearance. Most warty change to invasive carcinoma, the
often, the lesions arise on the gingival, man- progression often taking 10 to 20 years to
dibular alveolar ridge and vestibular regions evolve. In the early benign phase of PVL,
and over time spread laterally, becoming the epithelium exhibits a verrucous pattern
PMPH_Eversole_Chapter-02.indd 31 1/17/2011 3:26:00 PM
32 Chapter 2
FIGURE 2-19
Proliferative verrucous
leukoplakia with lesions
representing a variety of
histologies varying from
atypical verrucous hyper-
plasia to verrucous carci-
noma to invasive squamous
cell carcinoma.
with alternating cryptic invaginations and or an exophytic papillary form of squamous
polypoid or acroform projections. The cancer. Biopsy is required.
cornified layer as represented by either par-
akeratin or orthokeratin is thickened, often TREATMENT
substantially. The spinous cell layer is gen-
Verrucous leukoplakia is notorious for recur-
erally acanthotic, and in the early stages,
rence subsequent to surgical excision. Indeed,
cytologic atypia is lacking. The subjacent
even when the margins appear normal,
fibrous tissue is usually infiltrated by lym-
this disease recurs. Some patients have had
phocytes. Temporally, the lesion can evolve
lesions totally excised as many as six times.
into verrucous lesions exhibiting marked
Verrucous leukoplakia is, therefore, a chronic,
acanthosis without cytologic atypia, and
persistent disease and all instances should
such changes are often designated atypical
be considered premalignant. Radiation ther-
verrucous hyperplasia (AVH) showing the
apy is contraindicated owing to the potential
typical thickened verrucous pattern with
to initiate dysplastic changes. Rather, each
parakeratin crypt formation. Over time, a
recurrence should be treated by conventional
classic verrucous carcinoma may evolve.
or laser surgery or cryosurgery.
Alternatively, some of these lesions develop
dysplastic cellular changes and progress to
either exophytic papillary or frankly inva-
sive squamous cell carcinoma.
Additional Reading
Eversole LR, Shopper TP. Oral leukoplakia: prevalence
DIFFERENTIAL DIAGNOSIS of dysplastic and carcinomatous change in verruciform
and planar patterns. Calif Dent Assoc J. 1981;9:45.
Verrucous leukoplakia cannot be differen- Shear M, Pindborg JJ. Verrucous hyperplasia of the oral
tiated clinically from verrucous carcinoma mucosa. Cancer. 1980;46:1855.
PMPH_Eversole_Chapter-02.indd 32 1/17/2011 3:26:09 PM
White Lesions 33
Slootweg PJ, Muller H. Verrucous hyperplasia or of the underlying connective tissue. Clini-
verrucous carcinoma, an analysis of 27 patients. cally verrucous carcinoma is exophytic with
J Craniomaxillofac Surg. 1983;11:1.
Hansen LS, Olson JA, Silverman S, Jr. Proliferative ver- a warty, shaggy white surface. While some
rucous leukoplakia. Oral Surg Oral Pathol Oral Med. patients use smoked or smokeless tobacco,
1985;60:285. many affected patients have no history of
van der Waal I, Reichart PA. Oral proliferative verrucous a tobacco habit. The lesions are most fre-
leukoplakia revisited. Oral Oncol. 2008;44:719-721.
quently encountered on the alveolar ridge,
gingiva, and mucobuccal fold.
VERRUCOUS CARCINOMA
Figure 2-20 MICROSCOPIC FEATURES
Age: Elderly Surface stratified squamous epithelium exhib-
Sex: No predilection its a warty verrucous pattern with a mark-
edly thickened parakeratin layer. Marked
CLINICAL FEATURES elongation and thickening of rete pegs is
Verrucous carcinoma is not a true cancer observed and parakeratin crypts descend
because it does not metastasize unless is into the acanthotic rete ridges, appearing as
undergoes anaplastic transformation. It is a “elephant feet.” The individual cells fail to dis-
proliferative lesion that often evolves from a play atypia, although basilar crowding and
preexisting verrucous leukoplakia or atypi- mild basal/parabasilar hyperchromatism are
cal verrucous leukoplakia. The lesion grows seen. The lesion is superficial and exophytic
and spreads laterally without true invasion without invasion of the submucosa.
FIGURE 2-20
Verrucous carcinoma,
warty thick white lesions.
PMPH_Eversole_Chapter-02.indd 33 1/17/2011 3:26:24 PM
34 Chapter 2
DIFFERENTIAL DIAGNOSIS are a common presentation of the disease.
Clinically, condylomata and papillary Whereas the etiology is unknown, lichen
variant of squamous cell carcinoma are planus–like lesions are occasionally asso-
considered in the differential. Similarly, the ciated with systemic medications (see
microscopic features must be differentiated Lichenoid Reactions). The classic appear-
from papillary squamous cell carcinoma, a ance is one of reticulated interconnected,
lesion with significant dysplastic changes. white thread-like lesions, striae of Wick-
On the opposite end of the microscopic ham, located bilaterally on the buccal
spectrum, AVH must be included in the dif- mucosa and vestibule. Other areas such
ferential diagnosis. as ventral tongue and gingiva may also be
involved; indeed, virtually any oral mucosal
TREATMENT tissue may evince manifestations of lichen
planus. Whereas the aforementioned fea-
Wide local excision with 1 cm margins is tures are most common, oral lichen planus
recommended. Anaplastic change with may have protean clinical signs. The plaque
progression to invasive carcinoma has form resembles leukoplakia with a multifo-
been known to occur following radiation cal distribution. Plaque-like lichen planus
therapy. is usually a smooth and slightly irregularly
surfaced white lesion found primarily on
dorsal tongue mucosa. A circinate variety
Additional Reading can be encountered. Circinate, oval, and tar-
Ackerman LV. Verrucous carcinoma of the oral cavity. get-appearing white lesions of lichen planus
Surgery. 1948;23:670. are seen most often on buccal mucosa.
Perez CA, Kraus FT, Evans JC. Anaplastic transforma- A pigmented form shows a mixture of stria
tion in verrucous carcinoma of the oral cavity after on a slate-gray base.
radiation therapy. Radiology. 1966;86:108.
McCoy JM, Waldron CA. Verrucous carcinoma; analy- Skin lesions, when present, are scaly
sis of fifty-six cases. Oral Surg Oral Med Oral Pathol. keratoses overlying an erythematous or
1981;52:623. violaceous base and are seen most fre-
Arduino PG, Carrozzo M, Pagano M, Gandolfo S, quently on the extensor surfaces of the
Broccoletti R. Verrucous oral carcinoma: clinical find-
ings and treatment outcomes in 74 patients in Northwest
extremities.
Italy. Minerva Stomatol. 2008;57:335-339, 339-341. Multifocal white lesions with an ery-
Fujita S, Senba M, Kumatori A, Hayashi T, Ikeda T, thematous component are seen in the ero-
Toriyama K. Human papillomavirus infection in sive and bullous forms of lichen planus,
oral verrucous carcinoma: genotyping analysis and
inverse correlation with p53 expression. Pathobiology.
which are considered separately elsewhere.
2008;75:257-264. Malignant transformation is uncommon,
being more often encountered among
patients with erosive or plaque forms of the
Lacey White Lesions disease.
LICHEN PLANUS MICROSCOPIC FEATURES
Figure 2-21
Hyperkeratosis or parakeratosis may or may
Age: Adults not be present. The basal cell layer is dis-
Sex: Females affected slightly more often rupted with loss of polarity; lymphocytes
may be interposed between basal cells. If
CLINICAL FEATURES
rete ridges are present, they taper off into the
Lichen planus is a dermatologic disorder, underlying connective tissue, imperceptibly
yet oral lesions without skin involvement blending into a subepithelial lymphocytic
PMPH_Eversole_Chapter-02.indd 34 1/17/2011 3:26:36 PM
White Lesions 35
infiltrate below, yielding a sawtooth pat- may mimic other oral white lesions, and
tern. The basement membrane is irregular biopsy is often necessary to render a defin-
and thickened. The juxtaposed lymphocytic itive diagnosis.
infiltrate is zonal, localized only in the sub-
mucosa without involvement of the deeper TREATMENT
connective tissue, representing a chronic Topical and systemic retinoid preparations
interface mucositis. Phenotyping has dis- have been used with limited improvement;
closed that the lymphocytes are T cells with however, the nonerosive, nonbullous forms
a preponderence of the CD4 subset. of lichen planus are generally asymptom-
atic, requiring no treatment.
DIFFERENTIAL DIAGNOSIS
The reticulated form is separated eas-
ily from other oral white lesions. Plaque
forms may be confused with leukoplakias
Additional Reading
or premalignant conditions, moniliasis, Andreason J. Oral lichen planus. Oral Surg Oral Med
or the genokeratoses. As mentioned, evi- Oral Pathol. 1968;25:31.
dence is emerging that some instances of Silverman S, Jr, Griffith M. Studies on oral lichen planus.
Oral Surg Oral Med Oral Pathol. 1974;37:705.
lichen planus are associated with malig- Krutchkoff DJ, Cutler L, Laskowski S. Oral lichen planus:
nant transformation. Whether or not these the evidence regarding potential malignant transfor-
cases represent true lichen planus under- mation. J Oral Pathol Med. 1978;7:1.
going malignant change or leukoplakias Scully C, El-Korm M. Lichen planus: review and update
on pathogenesis. J Oral Pathol Med. 1985;14:431.
and mucositis with a strong resemblance McCartan BE, Healy CM. The reported prevalence of
to oral lichen planus microscopically is oral lichen planus: a review and critique. J Oral Pathol
unknown. Regardless, the plaque form Med. 2008;37:447-453.
FIGURE 2-21
Reticulated lichen planus,
stria of Wickham.
PMPH_Eversole_Chapter-02.indd 35 1/17/2011 3:26:36 PM
36 Chapter 2
LICHENOID REACTIONS smokeless tobacco. Clinically, there is often
Figure 2-22 a symptom of mucosal pain and burning.
The lesions are usually white with erythema
Age: Adults resembling erosive lichen planus. In lichenoid
Sex: Slight female predilection drug eruptions, cutaneous lichenoid lesions
CLINICAL FEATURES
are also commonly encountered.
White lesions that lack classic features of MICROSCOPIC FEATURES
lichen planus or appear without stria yet show
A chronic interface mucositis is present
a chronic interface histology may be referred
with lymphocytic infiltration similar or
to as “lichenoid reactions.” Also included
identical to conventional lichen planus. In
are lichen planus–like lesions that can be
cinnamon allergies, the infiltrate is mixed
attributed to allergenic chemicals including
with perivascular lymphoid aggregates in
both topical and systemic drugs (lichenoid
the submucosa. In lichen sclerosis et atro-
drug eruption). The chief allergens under
phicus, subepithelilal fibrosis is featured.
scrutiny are (1) contact dental restorative
metals, chiefly mercury, that may leach out
DIFFERENTIAL DIAGNOSIS
of old corroding amalgam restorations and
trace metals from cast gold alloys, (2) a host Conventional lichen planus, leukoeryth-
of systemic medications, and (3) food stuff roplakia, and other white lesions included
antigens such as cinnamon found in a vari- here must be considered in the differen-
ety of breakfast food and even used to flavor tial diagnosis. Questioning patients about
FIGURE 2-22
Lichenoid reactions: contact lesions, cinnamon reaction, drug eruption, lichen sclerosis et atrophicus of lip.
PMPH_Eversole_Chapter-02.indd 36 1/17/2011 3:26:46 PM
White Lesions 37
drug intake, cinnamon consumption, and LUPUS ERYTHEMATOSUS
other dietary potential allergens will help Figure 2-23
reveal the true diagnosis. So-called con-
tact lesions adjacent to metal restorations Age: Young adults
should be managed by removal of the prob- Sex: Females
able antigen. CLINICAL FEATURES
TREATMENT Lupus erythematosus, the discoid type,
Removal of the antigenic source is essential, is a disorder manifesting erythematous
accompanied by topical steroid, tacrolimus, dermatologic scaly lesions of skin. A more
and/or cyclosporine and soothing mouth serious form, the systematic type, evinces
rinses for pain relief. lesions in the kidney and other visceral
organs as well as on skin, being one of
the collagen-vascular immunopathic dis-
Additional Reading eases. Oral lesions are sometimes seen
with lupus erythematosus, particularly
Eversole LR, Ringer M. The role of dental restorative
metals in the pathogenesis of oral lichen planus. Oral the systemic type. The lesions are white
Surg Oral Med Oral Pathol. 1984;57:383-387. and plaque-like, resembling lichen planus,
Al-Hashimi I, Schifter M, Lockhart PB, et al. Oral lichen and occasionally an erythematous compo-
planus and oral lichenoid lesions: diagnostic and thera- nent accompanies the white lesions. Disc
peutic considerations. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 2007;103(suppl S25):e1-e12. and circinate patterns are common, and
Lomaga MA, Polak S, Grushka M, Walsh S. Results of lesions often involve the vermilion border.
patch testing in patients diagnosed with oral lichen The facial butterfly pattern—a plaque of
planus. J Cutan Med Surg. 2009;13:88-95. erythema over the nasal bridge with bilat-
Ismail SB, Kumar SK, Zain RB. Oral lichen planus and
lichenoid reactions: etiopathogenesis, diagnosis, man-
eral flaring on the skin of the malar emi-
agement and malignant transformation. J Oral Sci. nence region—is a classic feature of lupus
2007;49:89-106. erythematosus.
FIGURE 2-23
Discoid and lichenoid
lesions of lupus erythe-
matosus.
PMPH_Eversole_Chapter-02.indd 37 1/17/2011 3:27:12 PM
38 Chapter 2
MICROSCOPIC FEATURES
The microscopic features are most char-
Additional Reading
acteristic when a biopsy is obtained from Andreasen JO. Oral manifestations of discoid and sys-
skin. Hyperkeratosis is accompanied by temic lupus erythematosus. 1. Clinical investigations.
Acta Odontol Scand. 1964;22:295.
some disruption of the basal cell layer. The
Schiodt, M, Holmstrup P, Dabelsteen E, Ullman S.
basement membrane is thickened with Deposits of immunoglobulins, complement, and
fibrinoid change. A lymphocytic infiltrate fibrinogen in oral lupus erythematosus, lichen planus,
prevails, is patchy in distribution, and typi- and leukoplakia. Oral Surg Oral Med Oral Pathol.
cally is localized in the vicinity of pilose- 1981;51:603.
Schiodt M. Oral discoid lupus erythematosus. II. Skin
baceous structures. Oral lesions manifest lesions and systemic lupus erythematosus in sixty-six
microscopic features reminiscent of those of patients with 6-year follow up. Oral Surg Oral Med
lichen planus, yet deeper zones of perivas- Oral Pathol. 1984;57:177.
cular lymphocytic infiltration can be noted Jonsson R, Heyden G, Westberg NG, Nyberg G. Oral
mucosal lesions in systemic lupus erythematosus—a
and the spinous layer is hyperplastic. Direct clinical, histopathological and immunopathological
immunofluorescence on oral biopsies dis- study. J Rheumatol. 1984;11:1.
closes IgG or IgM deposition along the base- Porter S, Scully C. Connective tissue disorders and
ment membrane. the mouth. Dent Update. 2008;35:294-296, 298-300,
302.
DIFFERENTIAL DIAGNOSIS
White lesions of lupus erythematosus must HIV-ASSOCIATED HAIRY
be differentiated from lichen planus, the LEUKOPLAKIA
genokeratoses, and leukoplakias. The char- Figure 2-24
acteristic skin lesions and butterfly pattern,
when present, are important diagnostic Age: Young adults
signs. Lupus erythematosus may also be Sex: Males
associated with erythematous and erosive CLINICAL FEATURES
oral lesions, usually admixed with a white
component. Antinuclear factor, anti-DNA Oral hairy leukoplakia is an HIV-associ-
antibodies, immunofluorescence micro- ated disease that involves the lateroven-
scopic tests, and the lupus erythematosus tral tongue, although other oral sites are
preparation (LE prep) are usually positive sometimes involved. Clinically, the lesion
in lupus, and elevated IgG may be seen. is relatively distinct in that parallel, fringe,
On direct immunofluorescence of patient or hair-like white lesions are vertically ori-
lesional material, basement membrane IgM ented along the lateral border of the tongue.
immunoreactants are usually deposited In some instances, the lesion consists of a
(lupus band test). diffuse white plaque with only occasional
hairy striae; other cases are almost exclu-
sively striated. The disease is asymptom-
TREATMENT
atic and may be bilateral. When hairy leu-
Patients with lupus erythematosus may koplakia involves mucosal sites other than
manifest systemic complications, particu- the tongue, it is smooth and homogeneous
larly in the kidney. Prolonged systemic without striated margins. Most cases are
use of steroids or other immunosuppres- colonized by Candida albicans; however,
sive drugs is the treatment of choice, and the etiology is viral. The EBV is associated
these patients should be under the care with the disease and is, in all probability,
of a physician, usually a dermatologist or causative, representing an opportunistic
rheumatologist. infection. Importantly, hairy leukoplakia
PMPH_Eversole_Chapter-02.indd 38 1/17/2011 3:27:25 PM
White Lesions 39
FIGURE 2-24
Hairy leukoplakia in HIV-
infected males.
should be considered an AIDS prodrome as HIV seropositive and fit into an AIDS-risk
it is highly predictive for progression from population group (homosexual male, intra-
asymptomatic HIV seropositivity to the venous drug abuser, transfusion recipient,
full-blown syndrome. etc). If the diagnosis is in doubt, DNA in
situ hybridization should be undertaken.
MICROSCOPIC FEATURES This lesion is extremely uncommon among
The parakeratin layer is thickened and is other forms of immunosuppression.
usually colonized by Candida hyphae. Char-
acteristically, a subcorneal, upper spinous TREATMENT
layer zone of cytopathically altered kerati- Generally, no treatment is required because
nocytes is evident. These subcorneal cells the lesions are not painful or otherwise
show cytoplasmic clearing and nuclear bothersome. Resolution follows acyclovir
vesiculation with chromatin margination. therapy; however, the lesions recur once the
The spinous layer is of moderate thickness medication is withdrawn. Patients receiv-
and the submucosa is generally devoid of ing triple drug therapy for the treatment of
inflammation. Using DNA in situ hybrid- AIDS frequently manifest regression of the
ization with an EBV molecular probe on tongue lesions. Because hairy leukoplakia
processed tissue sections or on cytospin is most often seen as a pre-AIDS condition,
preparations, upper spinous layer cells stain it is important to refer affected patients to a
positively. physician who cares for such individuals.
DIFFERENTIAL DIAGNOSIS
Ordinary leukoplakia associated with a Additional Reading
tongue-chewing habit should be consid- Greenspan D, Greenspan JS, Conant M, Petersen V,
ered in the differential diagnosis along Silverman S, Jr, de Souza Y. Oral ‘hairy’ leucoplakia
with lichen planus. These patients are in male homosexuals: evidence of association with
PMPH_Eversole_Chapter-02.indd 39 1/17/2011 3:27:26 PM
40 Chapter 2
both papillomavirus and a herpes-group virus. Lancet. diameter may be encountered on the buccal
1984;2:831. mucosa. Patients may have only one lesion
Greenspan D, Greenspan JS, Hearst NG, et al. Relation
of oral hairy leukoplakia to infection with the human or as many as 50 on each side of the mouth.
immunodeficiency virus and risk of developing AIDS. The lesions are plaque- or dome-like and
J Infect Dis. 1987;155:475. are oval to round. When the maculopapu-
Belton CM, Eversole LR. Oral hairy leukoplakia: ultra- lar skin rash appears, Koplik spots begin to
structural features. J Oral Pathol Med. 1986;15:493.
Eversole LR, Jacobson P, Stone CE, Freckleton V. Oral
disappear.
condyloma planus (hairy leukoplakia) among homosex-
ual men: a clinicopathologic study of thirty-six cases. MICROSCOPIC FEATURES
Oral Surg Oral Med Oral Pathol. 1986;61:249.
López-Pintor R, Hernández G, de Arriba L, de Andrés The epithelium shows superficial necrosis
A. Comparison of oral lesion prevalence in renal trans- with an avid neutrophilic inflammatory cell
plant patients under immunosuppressive therapy and infiltrate in the subjacent submucosa.
healthy controls. Oral Dis. 2010;16:89-95.
DIFFERENTIAL DIAGNOSIS
Papular Lesions Koplik spots are usually not difficult to
separate from other white lesions because
KOPLIK SPOTS OF MEASLES they are focal and seen most often in chil-
Figure 2-25 dren. Large Fordyce’s granules and cheek-
biting keratosis should be considered in
Age: Children the differential diagnosis. A diagnosis of
Sex: No predilection Koplik spots is confirmed upon appear-
CLINICAL FEATURES ance of the classic rubeola maculopapular
rash.
During the prodromal stages of rubeola
infection when fever and malaise are wax-
ing, focal white spots less than 1 cm in TREATMENT
Supportive care, including high fluid intake
and the use of salicylates to control fever,
with bed rest is recommended treatment.
The child’s physician should be notified;
complications, although uncommon, may
occur in measles.
Additional Reading
Hornstein OP, Gorlin RJ. In Gorlin RJ, Goldman HM,
eds. Thoma’s Oral Pathology. Vol 2. 6th ed. St Louis,
MO: C. V. Mosby; 1970:756.
Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral
Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger;
1978:325.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
1983:378.
Koplik H. The diagnosis of the invasion of measles from
a study of the exanthem as it appears on the buccal
mucous membrane. Arch Pediatr. 1896;13:981.
FIGURE 2-25 Steichen O, Dautheville S. Koplik spots in early measles.
Prodromal measles Koplik spots. CMAJ. 2009;180:583.
PMPH_Eversole_Chapter-02.indd 40 1/17/2011 3:27:37 PM
White Lesions 41
FORDYCE’S GRANULES Fordyce J. A peculiar affection of the mucous membrane
of the lip and oral cavity. J Cutan Genito-Urin Dis.
Figure 2-26 1896;14:413.
Miles AEW. Sebaceous glands in the lip and cheek
Age: All ages mucosa of man. Br Dent J. 1958;105:235.
Sex: No predilection Olivier JH. Fordyce granules on the prolabial and oral
mucous membranes of a selected population. SADJ.
CLINICAL FEATURES 2006;61:O72-O74.
Fordyce’s granules or ectopic sebaceous
glands are present in 90% of the popula-
tion. They are multifocal, less than 2 mm DENTAL LAMINA CYSTS,
in diameter, and actually more yellow than BOHN’S NODULES, EPSTEIN’S
white. They are located on the mucosal sur- PEARLS
faces of the lips and buccal mucosa.
Figure 2-27
HISTOLOGIC FEATURES
Age: Infants
Submucosal clusters of sebaceous acini are Sex: No predilection
present and communicate with the oral epi- CLINICAL FEATURES
thelium by way of ducts.
Focal white nodules seen on the alveo-
DIFFERENTIAL DIAGNOSIS lar ridges, palatal raphe area, or lateral
The small size, multiplicity, and yellow palatal mucosa represent dental lamina
color are characteristic and are unlikely to cysts, Bohn’s nodules, and Epstein’s pearls,
be confused with other mucosal diseases. respectively. These nodules are encoun-
tered in neonates and represent keratin
TREATMENT cysts that are remnants of embryonic pro-
cesses of dental or minor salivary gland
No treatment is necessary.
origin or, in the case of midpalatal Bohn’s
nodules, small cystic remnants of palatal
Additional Reading process fusion.
Gorlin RJ. In Gorlin RJ, Goldman HM, eds. Thoma’s
Oral Pathology. Vol 1. 6th ed. St Louis, MO: C. V. MICROSCOPIC FEATURES
Mosby; 1970:24.
Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral
Microscopically, all three entities are identi-
Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger; cal. They are characterized by submucosal
1978:374. epithelial cysts that contain no true lumen
FIGURE 2-26
Yellowish white Fordyce’s
granules are multiple and
clustered.
PMPH_Eversole_Chapter-02.indd 41 1/17/2011 3:27:38 PM
42 Chapter 2
STOMATITIS NICOTINA
Figure 2-28
Age: Middle-aged and elderly adults
Sex: Males predominate
CLINICAL FEATURES
Inveterate pipe and cigar smokers may
manifest multiple focal keratotic papules
restricted to the palatal mucosa, generally
the posterior hard palate and anterior soft
palate. The center of each papule in stom-
atitis nicotina evidences a pinpoint ery-
FIGURE 2-27 thematous depression with an umbilicated
Congenital cysts of newborns. appearance.
MICROSCOPIC FEATURES
but, instead, are filled with concentric swirls The epithelium surrounding the palatal
of keratin. minor salivary gland duct orifice is thick-
ened, with involvement of both keratin and
spinous cell layers. The excretory salivary
DIFFERENTIAL DIAGNOSIS
duct is acanthotic and may show mucous
Neonatal alveolar ridge nodules may be cell metaplasia. A periductal inflammatory
confused with natal teeth, but closer scru- cell infiltrate composed of lymphocytes and
tiny discloses the true nature of the spots as plasma cells accompanies capillary prolifer-
submucosal nodules and not prematurely ation and dilatation in this zone.
erupting teeth.
DIFFERENTIAL DIAGNOSIS
TREATMENT
The restriction of umbilicated papules to
No treatment is necessary, as these small the palate in pipe smokers is characteris-
cysts spontaneously regress within 1 to 3 tic for stomatitis nicotina. Oral keratotic
months. papules may also be seen in keratosis fol-
licularis (Darier-White’s disease). Stomatitis
nicotina differs from papillomatosis (papil-
Additional Reading lary hyperplasia) in that the papules of the
former are generally focal with clinically
Kreshover SJ. The incidence and pathogenesis of gingival normal-appearing intervening mucous
cysts. Presented at 35th General Meeting, International
Association for Dental Research, March, 1957.
membrane; in addition, papillary hyperpla-
Fromm A. Epstein’s pearls, Bohn’s nodules and sia is not keratotic and does not show a cen-
inclusion cysts of the oral cavity. J Dent Child. trally depressed area.
1967;34:275.
Cataldo E, Berkman M. Cysts of the oral mucosa in new- TREATMENT
borns. Am J Dis Child. 1968;116:44.
Maher WP, Swindle PF. Etiology and vascularization of The presence of stomatitis nicotina is an
dental lamina cysts. Oral Surg Oral Med Oral Pathol. indication that the patient is utilizing
1970;29:590.
Kumar A, Grewal H, Verma M. Dental lamina cyst of
tobacco to a level that is toxic to mucosa.
newborn: a case report. J Indian Soc Pedod Prev Dent. Although malignancy is not associated
2008;26:175-176. with this mucosal change, the patient may
PMPH_Eversole_Chapter-02.indd 42 1/17/2011 3:27:46 PM
White Lesions 43
FIGURE 2-28
Stomatitis nicotina of the
palate, umbilicated papules
surrounded by keratosis.
nevertheless manifest leukoplakia plaques roximately 20% (somewhat less preva-
in other mucosal locations. The habit should lent among planar forms, more prevalent
be eliminated or severely limited. among the verruciform type), speckled
leukoplakias are the most ominous in this
regard. Clinically, speckled leukoplakia
Additional Reading is a velvety red patch with multiple white
Saunders WH. Nicotine stomatitis of the palate. Ann papular foci. Therefore, it represents a com-
Otol Rhinol Laryngol. 1958;67:618. bined leukoplakia-erythroplakia. Speckled
Schwartz DL. Stomatitis nicotina of the palate. Oral Surg leukoplakia is usually encountered on the
Oral Med Oral Pathol. 1965;20:306. oral floor, ventrolateral tongue, and soft
Thoma KH. Stomatitis nicotina and its effect on the pal-
ate. Am J Orthod Oral Surg. 1941;27:38.
palate.
Gavarasana S, Susarla MD. Palatal mucosal changes
among reverse smokers in an Indian village. Jpn J MICROSCOPIC FEATURES
Cancer Res. 1989;80:209-211.
Foci of hyperkeratosis, parakeratosis, and
acanthosis alternate with zones of epithe-
SPECKLED LEUKOPLAKIA lial atrophy devoid of a cornified layer. The
atrophied foci correspond to those regions
Figure 2–29
that appear red clinically, and usually the
Age: Middle-aged and elderly adults cells occupying the attenuated spinous layer
Sex: Males predominantly show pleomorphism, hyperchromatism,
and increased mitotic activity. The kera-
tinized or parakeratinized regions repre-
CLINICAL FEATURES
senting the clinically evident white plaques
Whereas the prevalence of atypical and may also harbor atypical cells and Candida
malignant change in leukoplakia is app- hyphae may colonize the surface.
PMPH_Eversole_Chapter-02.indd 43 1/17/2011 3:27:47 PM
44 Chapter 2
FIGURE 2-29
Velvety red lesions with
white punctate papules
in dysplastic speckled
leukoplakia.
DIFFERENTIAL DIAGNOSIS leukoplakia: retrospective analysis of 13 cases. Braz J
Otorhinolaryngol. 2009;75:295-299.
Speckled leukoplakia, with its mixed red
and white appearance, may be confused
clinically with erosive lichen planus and
candidiasis. Whereas these two entities are
Pseudomembranous Lesions
usually multifocal, speckled leukoplakia CHEMICAL BURNS
is usually, yet not invariably, an isolated
Figure 2-30
lesion. Biopsy is required to obtain a defini-
tive diagnosis. Age: No predilection
Sex: No predilection
TREATMENT
CLINICAL FEATURES
Speckled forms of leukoplakia are usually
found to harbor atypical cells. Dysplastic or Burns caused by caustic chemical agents pro-
carcinoma-in-situ lesions require surgical duce coagulation necrosis of the epithelium
stripping, cryosurgery, or laser surgery with with subsequent inflammation. The necrotic
liberal margins of normal mucosa. Invasive tissue loses its translucency and appears
cancer is managed by surgery and/or radia- white. The white areas correspond to the
tion therapy. areas of contact with the caustic agent and
show a tendency to slough; initially, how-
ever, they may be adherent to the mucosa so
Additional Reading that scraping with an instrument may not
result in desquamation. The chief incrimi-
Pindborg JJ, Renstrup G, Jolst O, Roed-Petersen B.
Studies in oral leukoplakia: a preliminary report on the
nating agents include aspirin, phenol, acids,
period prevalence of malignant transformation in leu- and alkalies. The contactants may be intro-
koplakia based on a follow-up study of 248 patients. J duced on a factitial or iatrogenic basis.
Am Dent Assoc. 1968;76:767.
Mashberg A, Morrissey JB, Garfinkel L. A study of the
appearance of early asymptomatic oral squamous cell
MICROSCOPIC FEATURES
carcinoma. Cancer. 1973;32:1436. Chemical burns cause coagulation necrosis
Craig RM. Speckled leukoplakia of the floor of the
mouth. J Am Dent Assoc. 1981;102:690-692.
of the epithelium so that, microscopically,
Hosni ES, Salum FG, Cherubini K, Yurgel LS, the upper layers show a homogeneous
Figueiredo MA. Oral erythroplakia and speckled appearance with loss of structure and a
PMPH_Eversole_Chapter-02.indd 44 1/17/2011 3:28:04 PM
White Lesions 45
FIGURE 2-30
Aspirin burns, yellowish
silver nitrate burn.
failure of nuclei to take stains. Desquama- Kawashima Z, Flagg RH, Cox DE. Aspirin-induced oral
tion occurs, and an inflammatory cell infil- lesion: report of case. J Am Dent Assoc. 1975;91:10.
Isenberg SR, Hier LA, Chauvin PJ. Chemical burns of
trate within the underlying connective tis- the oral mucosa: report of a case. J Can Dent Assoc.
sue can be seen. 1996;62:262-264.
DIFFERENTIAL DIAGNOSIS
The white necrotic surface is smooth with
CANDIDIASIS (MONILIASIS,
regional fissuring; this shiny surface, seen THRUSH)
clinically, usually differentiates the necrotic Figure 2-31
surface from the keratotic lesions. Candidi-
asis should also be included in the differ- Age: Infants and adults
Sex: No predilection in oral form
ential diagnosis; however, the presence of
pain and procurement of an adequate his- CLINICAL FEATURES
tory will provide evidence for a diagnosis C. albicans is a superficial fungus that infects
of mucosal burn. the mucous membranes of infants whose
mothers display vaginal infestation at the
TREATMENT
time of parturition and of adults who have
Treatment is supportive, with a consid- experienced an upset in their oral micro-
eration of eliminating pain until healing flora from the use of conventional antibi-
occurs. Orabase gel may provide relief, or otics. In addition, oral candidiasis may be
palliation may result from the anesthetic associated with other systemic alterations,
effects of an antihistaminic mouth rinse including diabetes mellitus, hypoparathy-
in combination with Kaopectate (Upjohn; roidism, and immunodeficiency diseases.
Kalamazoo, MI). Instances are also commonly seen in the
absence of preexisting or intercurrent sys-
temic disease. The oral lesions consist of
Additional Reading either multifocal or diffuse white velvety-
appearing surfaces resulting from matted
Greither A, Hornstein OP. In Gorlin RJ, Goldman HM,
eds. Thoma’s Oral Pathology. Vol 2. 6th ed. St Louis, mycelia and parakeratotic cells. The lesions
MO: C. V. Mosby; 1970:781. may be wiped away with gauze; however,
Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral often they are tenacious and resist such
Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger; treatment. In elderly patients, moniliasis
1978:375.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
has been found occasionally to coexist
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders; with dysplastic or carcinomatous change.
1983:572. A cocarcinogenic effect has been suggested
PMPH_Eversole_Chapter-02.indd 45 1/17/2011 3:28:13 PM
46 Chapter 2
FIGURE 2-31
Candidiasis, pseudomem-
branous type.
for Candida in these instances, yet no cause- with PAS staining for mycelium will con-
and-effect relationship has been proven. firm the diagnosis. On culture, not all
While Candida is generally characterized instances are caused by the Calbicans spe-
by white lesions, an erythematous compo- cies; other Candida species or Geotrichium
nent may accompany the white areas. Deep may be responsible. Instances of Candida
or systemic and granulomatous infection infection without any predisposing fac-
by Candida may occur in severely debili- tors should arouse suspicion of underlying
tated states, such as uncontrolled diabe- systemic disease. Appropriate laboratory
tes or severe immunodeficiency diseases. tests for diabetes, hypoparathyroidism, and
Indeed, chronic oral candidiasis is a com- immunodeficiency states—fasting blood
mon finding in AIDS patients, and it is glucose and glucose tolerance tests, serum
commonly encountered in HIV-seroposi- calcium, and immunoglobulin complement
tive individuals who do not suffer from the and lymphocyte blast transformation stud-
full syndrome. ies, respectively—should then be obtained.
Lastly, it should be recalled that candidiasis
MICROSCOPIC FEATURES is the most common oral marker for HIV
Superficial infection is microscopically seropositivity.
represented by surface parakeratosis with Candida infection in older age groups
infiltration of the parakeratin and upper may coexist with precancerous or carcino-
to middle spinous cell layers by PAS-posi- matous change. Biopsy is then indicated.
tive mycelia and yeast forms. The submu-
cosa may be free from inflammation or TREATMENT
may contain a chronic inflammatory cell Referral to a physician for control of any sys-
infiltrate. temic derangement is mandatory. Manage-
ment of the local infection involves the use
DIFFERENTIAL DIAGNOSIS of antifungal agents: nystatin oral pastilles
The velvety surface is unique, yet the or clotrimazole troches (4 times daily for
lesions of candidiasis may resemble white 10-14 days) or ketoconazole (200-mg tablets
lesions of plaque-form lichen planus, leuko- once daily for 10 days), provided the patient
plakias, or even one of the genokeratoses, is free of any liver disease.
particularly since familial candidiasis has
been described. A complete history, par-
ticularly questions relating to the recent Additional Reading
use of antibiotics, will significantly limit Lehner T. Oral thrush, or acute pseudomembranous
the differential diagnosis. A cytologic smear candidiasis: a clinico-pathologic study of forty-
PMPH_Eversole_Chapter-02.indd 46 1/17/2011 3:28:20 PM
White Lesions 47
FIGURE 2-32
Grayish white fibrinous
exudates in vesiculo-
bullous-ulcerative diseases.
four cases. Oral Surg Oral Med Oral Pathol. VESICULO-BULLOUS-
1964;18:27.
Cawson RA. Chronic oral candidiasis and leukoplakia. ULCERATIVE DISEASES
Oral Surg Oral Med Oral Pathol. 1966;22:582. Figure 2-32
Eyre J, Nally FF. Oral candidosis and carcinoma. Br J
Dermatol. 1971;85:73. Age: Varies according to disease entity
Lozada F, Silverman S, Jr, Migliorati CA, Conant MA, Sex: Vareis according to disease entity
Volberding PA. Oral manifestations of tumor and
opportunistic infections in the acquired immunodefi- CLINICAL FEATURES
ciency syndrome (AIDS): findings in 53 homosexual A variety of diseases result in loss of the
men with Kaposi’s sarcoma. Oral Surg Oral Med Oral surface epithelium, and the underlying tis-
Pathol. 1983;56:491.
sues become surfaced with fibrin, yielding
Eversole LR, Reichart PA, Ficarra G, Schmidt-
Westhausen A, Romagnoli P, Pimpinelli N. Oral kera- a white-gray pseudomembrane. The specific
tinocyte immune responses in HIV-associated can- entities are more appropriately categorized
didiasis. Oral Surg Oral Med Oral Pathol Oral Radiol as vesiculobullous, desquamative, and ulcer-
Endod. 1997;84:372-380. ative diseases covered in Chapters 4 and 5.
PMPH_Eversole_Chapter-02.indd 47 1/17/2011 3:28:31 PM
a b c
Normal mucosa Epithelial atrophy Inflammatory vasodilation
d e f
Vascular proliferation Basilar melanosis Melanin incontinence
g h i
Melanocytic proliferation Hemosiderin pigment Metallic particles
Red and Pigmented Lesions
PMPH_Eversole_Chapter-03.indd 48 1/17/2011 3:24:22 PM
Red and Pigmented
Lesions 3
THROMBOCYTE DISORDERS 75
Focal Erythemas 51
HEREDITARY HEMORRHAGIC
NONSPECIFIC (IRRITATIONAL) TELANGIECTASIA 76
MUCOSITIS 51
MEDIAN RHOMBOID GLOSSITIS 52
HEMANGIOMA 53
Focal Pigmentations 77
VARIX 54 AMALGAM AND GRAPHITE
ERYTHROPLAKIA 55 TATTOO 77
MUCOCELE 78
Diffuse and Multifocal HEMATOMA 79
Red Lesions 56
NEVUS 80
GEOGRAPHIC TONGUE EPHELIS, ORAL MELANOTIC
(MIGRATORY GLOSSITIS) 56
MACULE 81
ERYTHEMA MIGRANS
(MIGRATORY STOMATITIS) 57
ATROPHIC GLOSSITIS 58 Diffuse and Multifocal
RADIATION MUCOSITIS 59 Pigmentations 82
XEROSTOMIC MUCOSITIS 60
MALIGNANT MELANOMA 82
LUPUS ERYTHEMATOSUS 61
KAPOSI’S SARCOMA*
ALLERGIC MUCOSITIS, FOREIGN
BODY GINGIVITIS 63 RACIAL PIGMENTATION 83
BULLOUS/EROSIVE DISEASES 64 PIGMENTED LICHEN PLANUS 84
CANDIDIASIS 65 PEUTZ-JEGHERS SYNDROME 85
LYMPHONODULAR PHARYNGITIS 67
MULTIPLE NEUROFIBROMATOSIS 86
SCARLET FEVER 67
ADDISON’S DISEASE 87
ATROPHIC LICHEN PLANUS 68
ECCHYMOSIS AND CLOTTING HEMOCHROMATOSIS 88
FACTOR DEFICIENCIES 70 HIV-ASSOCIATED ORAL
FIELD CANCERIZATION 71 PIGMENTATION 89
KAPOSI’S SARCOMA 72 HEAVY METAL INGESTION 90
DRUG-INDUCED PIGMENTATION 91
Petechiae 73
HAIRY TONGUE 92
SUCTION PETECHIAE 73
INFECTIOUS MONONUCLEOSIS 74 *See other listings in this chapter
PMPH_Eversole_Chapter-03.indd 49 1/17/2011 3:24:24 PM
Redness of the gingiva is the hallmark of A previously mentioned concept war-
plaque-related inflammatory disease, gin- rants reemphasis: Most individual diseases
givitis, and periodontitis. These two entities encompassed within the erythematous group
have been intentionally omitted because are inflammatory idiopathic disorders. Some
they are dealt with extensively in dental represent a response to physical and chemi-
practice and need no consideration here. cal irritants; others are a manifestation of
When dental plaque cannot be incriminated hypersensitivity to various allergens includ-
as a source of inflammation, the clinician ing foods and drugs. Importantly, prema-
is obliged to pursue other causes. Diffuse lignancy or incipient carcinomatous change
gingivitis, often exhibiting pronounced may appear red clinically. As with other oral
erythema, may be encountered in associa- diseases, thorough history procurement rel-
tion with systemic alterations (e.g., diabe- ative to both the present illness and medi-
tes, pregnancy). In these instances, gingival cal history is imperative when attempting to
enlargement accompanies the erythema; limit the differential diagnosis. Observation
systemically associated gingivitis is dis- of the distribution, longevity, and temporal
cussed in the chapter dealing with intraoral relationship of lesions to suspected caus-
tumefactions. ative agents will, in conjunction with the
Red lesions or erythemas of the oral case history, lead to a tentative diagnosis.
mucosa, including the gingiva, generally These features are detailed for each disease
present to the assessing eye of the clinician entity included in this discussion.
a promulgation of inflammation. This gen- Pigmentations other than red lesions
erality should not, however, be made to the are considered in this section; they may
point of excluding other disease processes, be black, brown, or blue. The discolor-
particularly malignant neoplasia. Intense ations may result from the accumulation of
erythema represents increased vascular- either intrinsic or extrinsic chemicals in the
ity as an expression of the inflammatory mucosal tissues. The primary intrinsic pig-
response, yet early oral cancer frequently mentations of the oral mucosa include the
heralds its own presence by accompanying melanins and hemoglobin or hemosiderin.
inflammatory changes that often coexist. Extrinsic pigments responsible for discol-
In this section, red lesions are classi- orations are usually heavy metal particles
fied according to the degree of involvement introduced either locally or systemically.
with regard to surface area and the size of Pigmented areas that blanch when pressed
the isolated erythematous zone (i.e., focal represent vascular lesions. The differential
erythemas, diffuse and multifocal erythe- diagnosis is based on extent; multiple pig-
mas, petechiae, and focal telangiectasia). mentations are associated with certain disor-
When considering a grouping of disease ders, whereas focal, isolated pigmentations
entities as collective components of the dif- encompass a different group of diseases.
ferential diagnosis, one must be constantly Common focal erythemas are nonspe-
cognizant of the fact that ulcerative and cific mucositis and erythroplakia (prema-
vesiculobullous lesions usually manifest lignant and malignant). Erythroplakia is
a circumlesional erythematous halo. The potentially lethal.
primary character of the early lesion is of The most common multifocal red lesions
utmost relevance in the development of a are geographic tongue, erosive lichen planus,
differential diagnosis. Lesions that evince an and moniliasis. Multifocal red lesions associ-
erythematous component yet are primarily ated with a potential lethal outcome include
ulcerative or vesiculobullous-desquamative field cancerization, lupus erythematosus, and
are considered in a separate chapter. ecchymosis from clotting factor deficiencies.
PMPH_Eversole_Chapter-03.indd 50 1/17/2011 3:24:24 PM
Red and Pigmented Lesions 51
The most common petechial lesions MICROSCOPIC FEATURES
usually found on the palate are suction The epithelium may be atrophic with
petechiae. Petechiae connoting a potentially regions bordering on ulceration. The sub-
lethal course are associated with leukemia mucosa displays capillary proliferation
and primary thrombocyte disorders. with dilation and a mixed inflammatory
The most common focal pigmentations cell infiltrate.
are amalgam or graphite tattoo and melan-
otic macule. Melanoma is a potentially lethal,
pigmented lesion that may be focal during DIFFERENTIAL DIAGNOSIS
the incipient phase, yet usually appears dif- In older individuals, precancerous erythro-
fuse. All diffuse pigmentations, with the plakia must be ruled out, particularly when
exception of racial melanosis, are rare. an immediate cause is indeterminate or
when removal of the suspected causative
Focal Erythemas agent fails to mitigate or limit the extent of
the lesion.
NONSPECIFIC (IRRITATIONAL)
MUCOSITIS TREATMENT
Figure 3-1 Elimination of the irritating agent is neces-
sary. If the area is painful, Orabase gel or an
Age: No predilection oral bandage may alleviate or palliate the
Sex: No predilection
symptoms until healing takes place.
CLINICAL FEATURES
Localized zones of redness are often related to
a physical agent that has irritated the mucosa. Additional Reading
Ill-fitting dental prostheses or factitial inju-
Gilvetti C, Porter SR, Fedele S. Traumatic chemical oral
ries from chronic habitual irritation are the ulceration: a case report and review of the literature.
chief contributing factors. The zone of ery- Br Dent J. 2010;208:297-300.
thema corresponds to the source of irritation. Greither A. In: Gorlin RJ, Goldman HM, eds. Thoma’s
Chemical burns may also produce a nonspe- Oral Pathology. Vol. 2. 6th ed. St Louis, MO: C. V.
Mosby; 1970:780.
cific erythematous mucositis. Incriminating Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral
chemical agents include acids, alkalies, caus- Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger;
tic organic compounds, and volatile oils. 1978:381.
FIGURE 3-1
Tooth pic injury (left); Pizza burn of palate (center); Linear focal erythema corresponding to a partial den-
ture gold connector that had mechanically irritated the palatal mucosa (right).
PMPH_Eversole_Chapter-03.indd 51 1/17/2011 3:24:24 PM
52 Chapter 3
MEDIAN RHOMBOID MICROSCOPIC FEATURES
GLOSSITIS Epithelial hyperplasia is evident with trans-
Figure 3-2 migration of leukocytes into the epithelial
layer. Periodic acid-Schiff (PAS) staining
Age: Adults reveals the presence of Candida hyphae. The
Sex: No predilection submucosa is infiltrated by lymphocytes
CLINICAL FEATURES and a hyalinized band of collagen repre-
senting the midline raphe of the tongue is
The lingual papillae on the posterior mid- frequently identified.
line dorsum of the tongue undergo atro-
phy leaving a smooth flat, or oftentimes
somewhat bosselated, surface that is red. DIFFERENTIAL DIAGNOSIS
The lesion was thought to represent failure Very few diseases enter into the differential
of the tuberculum impar to retract during diagnosis. If notable swelling is encoun-
embryogenesis; however, this theory is not tered, a mesenchymal tumor such as granu-
considered likely because median rhomboid lar cell tumor should be considered.
glossitis is only encountered in adults and
therefore cannot represent a developmental
TREATMENT
defect. The surface is typically colonized by
Candida organisms, yet not to the extent that Antifungal medication should be prescribed
a white pseudomembrane occurs. either systemically or as an oral lozenge.
FIGURE 3-2
Median rhomboid glossitis,
posterior dorsum.
PMPH_Eversole_Chapter-03.indd 52 1/17/2011 3:24:31 PM
Red and Pigmented Lesions 53
present. Patients with this syndrome often
Additional Reading suffer from epilepsy, contralateral hemiple-
Fowler JC, White P. A classic case of median rhomboid gia, and visual disturbances. The angioma-
glossitis. JAAPA. 2009;22(6):70. tous component may extend as a macular or
Nelson BL, Thompson L. Median rhomboid glossitis. tumorous lesion of the oral mucosa. Focal
Ear Nose Throat J. 2007;86:600-601. macular hemangiomas without evidence of
Terai H, Shimahara M. Atrophic tongue associated with
Candida. J Oral Pathol Med. 2005;34:397-400. skin involvement or central nervous system
manifestations are also encountered in the
oral cavity, although they are somewhat
HEMANGIOMA rare. The tumorous palpable type is more
Figure 3-3 common.
Age: Congenital or childhood onset MICROSCOPIC FEATURES
Sex: Female predilection The submucosal or dermal connective tis-
CLINICAL FEATURES sue underlying the surface epithelium dis-
plays randomly dispersed small-caliber
Macular hemangiomas of the facial skin
vessels, which are usually engorged with
have been termed port-wine stains or nevus
erythrocytes.
flammeus. They tend to follow the vascu-
lar components of neurovascular tracts of
DIFFERENTIAL DIAGNOSIS
the trigeminal nerve pathways. The Sturge-
Weber syndrome, encephalotrigeminal Nevus flammeus of the facial skin, when
angiomatosis, manifests nevus flammeus considered in conjunction with a history of
of the facial skin with accompanying vas- long duration, poses no problem in the dif-
cular hamartomas of the cerebrum and ferential diagnosis. A diagnosis of Sturge-
radiographically demonstrable serpentine Weber syndrome requires radiographic
calcifications. Ocular involvement may be demonstration of intracranial calcifications
FIGURE 3-3
Hemangiomas range from
purple to red. Upper right,
treated with radiation
therapy inducing severe
gross decay.
PMPH_Eversole_Chapter-03.indd 53 1/17/2011 3:24:41 PM
54 Chapter 3
and onset of the characteristic symptoma- Yukua RA, Cassingham RJ, Carr RF. Periodontal mani-
tology. Focal mucosal hemangiomas may festations and treatment in a case of Sturge-Weber syn-
drome. Oral Surg Oral Med Oral Pathol. 1979;47:408.
be confused with erythroplakia, mucosi-
tis, or chemical burns; however, history of
onset and duration provides helpful clues
as to the nature of the red lesion. Blanching VARIX
on pressure may be evoked, and biopsy will Figure 3-4
confirm the diagnosis.
Age: Middle-aged and elderly adults
Sex: No predilection
TREATMENT
CLINICAL FEATURES
Patients with Sturge-Weber syndrome
should seek the care of a physician for con- Varices are often seen as multiple conflu-
trol of epilepsy. Cosmetic surgery and tat- ent blue/purple lesions bilaterally on the
tooing may be indicated for the concerned ventral tongue among elderly patients. The
patient with nevus flammeus. Oral macular focal varix is typically seen on the lower
hemangiomas may spontaneously regress lip yet may also occur in the vestibule and
after puberty. Once the diagnosis is estab- buccal mucosa. The lesions are blue, red,
lished, no treatment is necessary for focal or purple and are typically raised nodules
mucosa macular hemangiomas. that are round or oval. They blanch under
pressure (diascopy) unless a thrombus has
formed within the vascular lumen. There is
Additional Reading often a precedent trauma such as biting.
Gorlin RJ, Pindborg JJ. Syndromes of the Head and
Neck. New York: Blakiston Division, McGraw-Hill MICROSCOPIC FEATURES
Book; 1964.
Ray BW, Matthew IR. Point of care. How do I manage A varix is simply a dilated vein that pur-
a suspected oral vascular malformation? J Can Dent sues a tortuous course throughout the
Assoc. 2009;75:575-577. connective tissue. Being a venule, the vas-
Royle HE, Lapp R, Ferrara ED. The Sturge-Weber syn- cular channels lack a muscular coat. Often,
drome. Oral Surg Oral Med Oral Pathol. 1966;22:490.
Watson WL, McCarthy WD. Blood and lymph vessel
an intraluminal thrombus develops and
tumors; a report of 1,056 cases. Surg Gynecol Obstet. may undergo organization by granulation
1940;71:569. tissue.
FIGURE 3-4
Focal nodular reddish pur-
ple lesions representing a
varix.
PMPH_Eversole_Chapter-03.indd 54 1/17/2011 3:24:50 PM
Red and Pigmented Lesions 55
DIFFERENTIAL DIAGNOSIS in this chapter. Premalignant or malignant
The other vascular lesions included here erythroplakia was originally described as
should be considered. Failure to blanch a penile cancerous lesion termed erythropla-
could indicate the presence of a thrombus. sia. The oral mucosal counterpart is clini-
cally similar in that a focal zone of redness
TREATMENT may exist alone or be accompanied by leu-
koplakic zones. When multifocal keratotic
Simple excision with cautery or laser is white patches are superimposed on an ery-
recommended. thematous base, the lesion is descriptively
termed speckled leukoplakia or erythropla-
Additional Reading kia. A focal red lesion with no identifiable
cause is a prime suspect for premalignant
Corrêa PH, Nunes LC, Johann AC, Aguiar MC, Gomez erythroplakia. Precancerous erythropla-
RS, Mesquita RA. Prevalence of oral hemangioma, kia is most prevalent in the oral floor, on
vascular malformation and varix in a Brazilian popula-
tion. Braz Oral Res. 2007;21:40-45.
the soft palate, buccal mucosa, and ventral
Johann AC, Aguiar MC, do Carmo MA, Gomez RS, tongue.
Castro WH, Mesquita RA. Sclerotherapy of benign
oral vascular lesion with ethanolamine oleate: an open MICROSCOPIC FEATURES
clinical trial with 30 lesions. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 2005;100(5):579-584. The epithelium may or may not possess
a cornified layer. The spinous cell layer is
atrophic, and rete ridge formation is either
ERYTHROPLAKIA absent or shows bulbous projections. The
Figure 3-5 spinous layer contains cells displaying aty-
pia, hyperchromatism, pleomorphism, and
Age: Middle-aged and elderly adults increased numbers of mitotic figures. The
Sex: Male predilection
underlying connective tissue is generally
CLINICAL FEATURES infiltrated by mononuclear inflammatory
Erythroplakia is the red counterpart to leu- cells.
koplakia and should be used strictly in the
clinical sense meaning, simply, red patch. DIFFERENTIAL DIAGNOSIS
Erythroplakia may therefore be repre- Focal erythemas representing precancerous
sented by any of the focal erythemas listed erythroplakia can be clinically confused
FIGURE 3-5
Erythoplakia and speckled erythroplakia histologically confirmed as carcinoma in situ.
PMPH_Eversole_Chapter-03.indd 55 1/17/2011 3:24:56 PM
56 Chapter 3
with irritational mucositis, macular heman-
gioma, or chemical burn. Absence of any Diffuse and Multifocal
identifiable irritants warrants biopsy. Red Lesions
TREATMENT GEOGRAPHIC TONGUE
Wide local excision of focal lesions, includ- (MIGRATORY GLOSSITIS)
ing 1 cm of clinically normal tissue, is rec- Figure 3-6
ommended. The specimen should be evalu-
ated microscopically for dysplastic-free Age: Onset in childhood or early adult life
margins. Sex: Slight female predilection
CLINICAL FEATURES
Additional Reading Multifocal circinate and irregular zones
of surface erosion characterized by loss of
Mashberg A. Erythroplasia. The earliest sign of asymp- the filiform papillae are seen on the dor-
tomatic oral cancer. J Am Dent Assoc. 1978;96:615. sum and lateral margins of the tongue. The
Mashberg A, Morrissey JB. A study of the appearance
of early asymptomatic oral squamous cell carcinomas.
fungiform papillae remain intact and may
Cancer. 1976;37:2149. show mild swelling with variable degrees
Reichart PA, Philipsen HP. Oral erythroplakia—a review. of erythema. The eroded zones are rimmed
Oral Oncol. 2005;41:551-561. by keratotic white circumlesional hypertro-
Shafer WG, Waldron CA. Erythroplakia of the oral cav-
ity. Cancer. 1975;36:1021.
phic filiform papillae. Whereas most cases
Shear M. Erythroplakia of the mouth. Int Dent J. are asymptomatic, some patients complain
1972;22:460. of glossodynia. The disease has been stated
FIGURE 3-6
Circinate red macules with
surrounding white halo in
geographic tongue.
PMPH_Eversole_Chapter-03.indd 56 1/17/2011 3:25:04 PM
Red and Pigmented Lesions 57
to occur in 1% to 2% of the population. The
term geographic tongue is descriptive in that Additional Reading
the foci of desquamation appear as islands Redman RS. Prevalence of geographic tongue, fissured
and continents in a sea of normal-appearing tongue, median rhomboid glossitis, and hairy tongue
glossal mucosa. The lesions wax and wane among 3,611 Minnesota school children. Oral Surg
with periods of remission. During recur- Oral Med Oral Pathol. 1970;30:390.
Weathers DR, Baker G, Archard HO, Burkes EF, Jr.
rent episodes, lesions appear in a different Psoriasiform lesions of the oral mucosa (with emphasis
location. on “ectopic geographic tongue”). Oral Surg Oral Med
Oral Pathol. 1974;37:872.
MICROSCOPIC FEATURES Kullaa-Mikkonen A, Mikkonen M, Kotilainen R.
Prevalence of different morphologic forms of the
The epithelium evinces loss of filiform human tongue in young Finns. Oral Surg Oral Med
papillae with spongiotic abscesses simi- Oral Pathol. 1982;53:152.
lar to those encountered in psoriasis with Eidelman E, Chosack A, Cohen T. Scrotal tongue and
geographic tongue: polygenic and associated traits.
migration of neutrophils into the spinous Oral Surg Oral Med Oral Pathol. 1976;42:591.
cell layer. The submucosa generally dis- Shulman JD, Carpenter WM. Prevalence and risk factors
plays a mild chronic inflammatory cell associated with geographic tongue among US adults.
infiltrate with variable degrees of capillary Oral Dis. 2006;12:381-386.
proliferation.
DIFFERENTIAL DIAGNOSIS ERYTHEMA MIGRANS
The clinical features, age, and history of
(MIGRATORY STOMATITIS)
chronicity with a tendency of the lesions Figure 3-7
to migrate are characteristic. Other diffuse
Age: Young adults
erythemas that may mimic geographic Sex: No predilection
tongue include moniliasis and erosive
lichen planus, both of which manifest CLINICAL FEATURES
lesions in extraglossal mucosa. Geographic Erythema migrans is probably the extra-
tongue shows microscopic features similar glossal counterpart to geographic tongue.
to psoriasis yet is not, in fact, an oral man- The lesions may actually accompany those
ifestation of psoriasis. of geographic tongue, or they may be inde-
pendent. They are found on the buccal
TREATMENT mucosa, lips, soft palate, oral floor, and ven-
No treatment is necessary. The patient tral tongue mucosa. Multifocal erythema-
should be reassured as to the benignity of tous patches are rimmed by a keratotic white
the condition. margin and have a circinate pattern. As with
FIGURE 3-7
Circinate red macules with white border in erythema migrans.
PMPH_Eversole_Chapter-03.indd 57 1/17/2011 3:25:12 PM
58 Chapter 3
geographic tongue, a history of migration is Burkes EJ. Ectopic geographic tongue. J N C Dent Soc.
elicited. The erythematous regions are usu- 1974;57:22.
Ray R, Pyle MA, Sawyer DR, Canion SB, Gordon
ally asymptomatic; however, stomatodynia EL. Prevalence and etiology of erythema migrans
may be a complaint in rare instances. among children in northeast Ohio. Quintessence Int.
2007;38(5):409-416.
MICROSCOPIC FEATURES Saprio SM, Shklar G. Stomatitis areata migrans. Oral
Surg Oral Med Oral Pathol. 1973;36:28.
The epithelium displays psoriasiform pat- Weathers DR, Baker G, Archard HO. Psoriasiform
terns; spongiosis with neutrophilic infiltra- lesions of the oral mucosa (with emphasis on “ectopic
tion is seen in the spinous cell layer. The geographic tongue”). Oral Surg Oral Med Oral Pathol.
1974;37:872.
epithelium may be atrophic or may mani-
fest elongated rete ridges with superficially
oriented submucosal papillae. ATROPHIC GLOSSITIS
DIFFERENTIAL DIAGNOSIS Figure 3-8
A history of migration, lack of pain, and Age: Children and elderly adults
a circinate appearance are characteristic. Sex: No predilection
Erythematous moniliasis, erosive lichen CLINICAL FEATURES
planus, lupus erythyematosus, and field
cancerization should be considered in the Vitamin deficiencies are endemic in some
clinical diagnosis; biopsy should be per- regions of the world; in western popu-
formed to rule out these diseases. lations, they are usually restricted to
alcoholics suffering from malnutrition.
TREATMENT Deficiency of the B vitamins such as ribo-
The cause is unknown and no treatment is flavin, niacin, and cyanocobalamine (B12)
necessary. Assurance as to the benignity of with pernicious anemia, as well as folic
the condition is indicated, particularly if the acid deficiency and sprue resulting from
patient is cancerophobic. an intolerance to gluten, may be accompa-
nied by atrophic glossitis. Atrophic glos-
sitis accompanying pernicious anemia has
Additional Reading been termed Hunter’s or Moeller’s glossitis.
Brooks JK, Balciunas BA. Geographic stomatitis: review
The tongue is smooth, devoid of papillae,
of the literature and report of five cases. J Am Dent and shows diffuse erythema. Bald tongue
Assoc. 1987;115:421. has also been reported to occur in patients
FIGURE 3-8
Bald tongue generally red-
dened in pernicious anemia
or B-complex deficiency.
PMPH_Eversole_Chapter-03.indd 58 1/17/2011 3:25:18 PM
Red and Pigmented Lesions 59
with xerostomia. The condition is revers- is managed by a nutritional diet, whereas
ible with adequate therapy. nontropical sprue may be controlled by a
gluten-free diet.
MICROSCOPIC FEATURES
Tongue papillae are absent; there is a flat-
tened epithelial layer. The submucosa Additional Reading
shows mild chronic inflammatory cell
Adlersberg D. Newer advances in sprue. Oral Surg Oral
infiltration. Med Oral Pathol. 1948;1:1109.
Cagnone LD. In: Gorlin RJ, Goldman HM, eds. Thoma’s
DIFFERENTIAL DIAGNOSIS Oral Pathology. Vol. 2, 6th ed. St Louis, MO: C. V.
Mosby; 1970:612.
Atrophic erythematous glossitis, when Pastore L, Lo Muzio L, Serpico R. Atrophic glossitis
diffuse, is usually indicative of vitamin-B leading to the diagnosis of celiac disease. N Engl J
complex, or B12, deficiency. Luetic glossitis Med. 2007;356:2547.
should be considered in the differential Shafer WG, Hine MK, Levy BM. A Textbook of Oral
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
diagnosis, yet usually lacks an erythema- 1983:649.
tous component. Hematogram, bone mar-
row aspiration, and gastric analysis dis-
close the presence of pernicious anemia.
Similar blood studies and stool analysis
RADIATION MUCOSITIS
for steatorrhea are necessary when sprue is Figure 3-9
suspected.
Age: Middle-aged and elderly adults
Sex: Male predilection
TREATMENT
CLINICAL FEATURES
The nutritional deficiency should be recti-
fied by proper diet and multiple vitamin Patients who have received external radia-
tablets. Pernicious anemia should be man- tion therapy to the oral mucosa in excess of
aged by a physician and can be treated 3500 to 4000 rad for the treatment of oral,
by vitamin B12 injections. Tropical sprue pharyngeal, or salivary malignant neo-
plasms often evince a painful diffuse ery-
thema with telangiectasia of the mucosa.
The red zones may initially be associated
with a white pseudomembrane and are
located in the zone of maximal radiation.
Candida colonization is commonly present
in association with these lesions.
MICROSCOPIC FEATURES
The surface epithelium may show ulcer-
ation or atrophy; depending on whether the
area examined was involved with neoplas-
tic change, residual cytologic atypia can be
observed. Later changes show an inflamma-
FIGURE 3-9 tory cell infiltrate in the submucosa with an
A pale red lesions on tongue with similar lesions in attenuated spinous cell layer. Telangiectasia
the oropharynx in a patient who received radiation with nuclear pleomorphism of endothe-
for a carcinoma of the tongue. lial cells is often encountered; intimal
PMPH_Eversole_Chapter-03.indd 59 1/17/2011 3:25:23 PM
60 Chapter 3
thickening and even thrombosis may be XEROSTOMIC MUCOSITIS
observed. Atypical cytologic features are Figure 3-10
no longer observed 6 weeks after radiation
unless recurrence has developed. Cytologic Age: Adults
smears stained with PAS help to determine Sex: Female predilection
whether candidiasis is superimposed. CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS Diffuse erythema from lack of salivary
secretion is painful, with dry mucous
A history of radiation therapy to the head membranes, and is severe on the gingiva.
and neck area points to a diagnosis of radia- The diagnosis of xerostomic mucositis is
tion mucositis. Persistence of the red lesion realized on manual palpation of the major
or increase in size should arouse suspicion salivary glands with resultant failure to
that an erythroplakia connoting recurrence elicit flow from Wharton’s and Stensen’s
of carcinoma is evolving. ducts. Objectively, salivary flow rates can
be assessed as can lacrimal flow with
TREATMENT
Schirmer strips. Xerostomic mucositis may
Radiation mucositis regresses with time. result from (1) radiation fields in the region
Persistence or an increase in topographic of the major salivary glands, (2) immu-
extent may herald recurrence of carcinoma. nopathologic sialadenitis as seen with
Cytologic smears are the method of choice collagen diseases, Sjögren’s syndrome,
for monitoring postradiation mucositis. or Mikulicz’s disease, or (3) prolonged
Unnecessary tissue breakdown, often use of antihistamines or antisialogogues.
evoked by surgical biopsy, can be avoided Rampant dental caries may accompany
by this procedure. A bland dentifrice is xerostomia, particularly when associated
recommended along with a soft diet. A with radiation injury or long-standing
soothing mouth rinse such as an antihis- Sjögren’s syndrome. Notably, xerostomia
taminic with Kaopectate will offer pain may occur in the absence of any mucosal
relief. When Candida hyphae are demon- alterations. Secondary candidiasis of the
strable, 1.2% chlorhexidine rinses, nystatin
pastilles, or clotrimazole troches should be
prescribed.
Additional Reading
Arun Maiya G, Sagar MS, Fernandes D. Effect of low
level helium-neon (He-Ne) laser therapy in the pre-
vention & treatment of radiation induced mucositis
in head & neck cancer patients. Indian J Med Res.
2006;124(4):399-402.
Chase LP, Toto PD, Magalotti MF. Radiation-induced
changes in the epithelium of the buccal mucosa.
J Dent Res. 1961;40:929.
Dreizen S, Daly TE, Drane JB, Brown LR. Oral com-
plications of cancer radiotherapy. Postgrad Med.
1977;61:85. FIGURE 3-10
Greenspan D, Silverman S, Jr. Study of bland dentrifice Generalized erythema of the oral mucous mem-
for persons with radiation-induced mucositis and vesic- branes occurring in severe xerostomia associated
ulo-erosive disease. J Am Dent Assoc. 1979;99:203. with Sjögren’s syndrome.
PMPH_Eversole_Chapter-03.indd 60 1/17/2011 3:25:25 PM
Red and Pigmented Lesions 61
erythematous foci is frequently identifi- Dreizen S, Brown LR, Daly TE, et al. Prevention of
able by cytologic smear. xerostomia-related dental caries in irradiated cancer
patients. J Dent Res. 1977;56:99.
Fox PC, van der Ven PF, Baum BJ, et al. Pilocarpine for
MICROSCOPIC FEATURES the treatment of xerostomia associated with salivary
gland dysfunction. Oral Surg Oral Med Oral Pathol.
Xerostomic mucositis shows a nonspecific
1986;61:243.
chronic inflammatory cell infiltrate with Hernández-Molina G, Avila-Casado C, Cárdenas-
capillary dilation in the submucosa. Velázquez F, et al. Similarities and differences
between primary and secondary Sjögren’s syndrome.
DIFFERENTIAL DIAGNOSIS J Rheumatol. 2010;37:800-808.
Nakamoto RY. Use of a saliva substitute in postradiation
Diffuse erythema of xerostomic mucosi- xerostomia. J Prosthet Dent. 1979;42:539.
tis must be differentiated from primary
mucosal damage by direct irradiation (radia-
tion mucositis). Failure to elicit salivary flow LUPUS ERYTHEMATOSUS
on palpation, symptoms of dry mouth, his- Figure 3-11
tory of radiation to salivary gland regions,
and bilateral parotid enlargement are all Age: Young and middle-aged adults
indicative of oral erythema from xerostomia. Sex: Female predilection
A definitive diagnosis can be made only by CLINICAL FEATURES
uncovering the cause of the condition.
The oral lesions seen in lupus erythema-
TREATMENT tosus may be red, white, or bullous. Often,
red and white zones are present bilaterally
Management of xerostomic mucositis due on buccal mucosa with diffuse or multifo-
to antisialogogues requires elimination or cal involvement. The characteristic lesion
limitation of the drug. Treatment of dry resembles that seen in erosive lichen planus.
mouth and mucositis due to compromised A discoid erythematous plaque is observed
salivary function as a result of organic dis- and is enveloped by a white halo with radi-
ease is problematic. Frequent rinsing with ating fringe-like striae. The dermatologic
water or a saliva substitute and use of soft- features are invariably present, and the
line denture bases with Orabase may afford “butterfly rash” over the nasal bridge and
some degree of comfort. Use of sialogogues malar eminence region bilaterally is diag-
is of some benefit, yet may cause gastro- nostic when other skin lesions coexist. The
intestinal irritability because of their cho- systemic form more frequently manifests
linergic properties. Salivary flow may be oral lesions. Antinuclear antibodies are
increased by administration of pilocarpine. typically present, being demonstrated more
Daily fluoride application and meticulous often in the systemic than in the discoid
oral hygiene will diminish the caries inci- form of the disease. The presence of circu-
dence. When Candida infection is present, lating antibodies to DNA is of more diag-
antifungal medication should be given, and nostic significance.
chlorhexidine rinses may be beneficial for
some patients.
MICROSCOPIC FEATURES
The oral mucosal changes in lupus ery-
Additional Reading thematosus may resemble those in lichen
planus. The basal lamina is thickened
Bernholt CH, Skaug N. Oral findings in irradiated
edentulous patients. Int J Oral Maxillofac Surg. with subepithelial and perivascular lym-
1985;14:416. phocytic infiltrates. Epithelial hyperplasia
PMPH_Eversole_Chapter-03.indd 61 1/17/2011 3:25:26 PM
62 Chapter 3
FIGURE 3-11
Diffuse red lesions of
the mucosa in lupus
erythematosus.
is a prominent finding with enlarged rete TREATMENT
ridges that appear to break away from the Lupus erythematosus is treated by systemic
surface epithelium. Immunofluorescence immunosuppressant therapy and should be
microscopy reveals the presence of granu- managed by a physician.
lar in vitro tissue-bound immunoglobulins
in the basal lamina.
Additional Reading
DIFFERENTIAL DIAGNOSIS
Andreasen JO. Oral manifestations in discoid and sys-
The red and mixed red and white lesions of temic lupus erythematosus. 1. Clinical investigation.
lupus erythematosus resemble those seen in Acta Odontol Scand. 1964;22:295.
Karjalainen TK, Tomich CE. A histopathologic study
erosive lichen planus. Candidiasis, allergic of oral mucosal lupus erythematosus. Oral Surg Oral
mucositis, erythema migrans, and multifo- Med Oral Pathol. 1989;67:547.
cal precancerous erythroplakia must also Marques ER, Lourenço SV, Lima DM, Nico MM. Oral
be considered in the differential diagnosis. lesions in lupus erythematosus-cytokines profiles of
inflammatory infiltrate. J Cutan Pathol. 2010;37:439-
Antinuclear antibody, anti-DNA antibody, 445.
lupus erythematosus preparation (LE Prep), Schiodt M. Oral discoid lupus erythematosus. II. Skin
and renal function tests, with a consider- lesions and systemic lupus erythematosus in sixty-six
ation of the dermatologic condition, limit patients with 6-year followup. Oral Surg Oral Med
Oral Pathol. 1984;57:177.
the differential diagnosis. Direct immuno- Schiodt M, Halberg P, Hentzer B. A clinical study of 32
fluorescence on unfixed sections is a useful patients with oral discoid lupus erythematosus. Int J
adjunctive test as well. Oral Maxillofac Surg. 1978;7:85.
PMPH_Eversole_Chapter-03.indd 62 1/17/2011 3:25:26 PM
Red and Pigmented Lesions 63
ALLERGIC MUCOSITIS, as toothpastes and mouth rinses. The lips
FOREIGN BODY GINGIVITIS and face may show erythematous lesions
Figure 3-12 when cosmetics are the cause of allergy. A
specific form of contact mucositis related
Age: No predilection to an allergen in chewing gum has been
Sex: No predilection observed and is characterized by severe
diffuse gingival erythema with ulceration
CLINICAL FEATURES
of the lips and commissure. This condition
Inflammatory oral red lesions from imme- has been termed plasmacytosis gingivae, so
diate systemic hypersensitivity to drugs named because of the profuse infiltration
(stomatitis medicamentosa) or contact of plasma cells into the submucosa of the
allergy (stomatitis venenata) may occur at gingiva. In both immediate and contact
any site on oral mucosa. Immediate anti- allergic reactions, pruritus or burning may
body-mediated hypersensitivity may be be a primary symptom. Some instances of
seen with any parenteral medication, but lichen planus represent allergies to drugs or
is most commonly associated with antibi- to specific metals. Foreign body gingivitis is
otics, sulfa drugs, iodine, and barbiturates. a nonimmunologic foreign body reaction to
Diffuse and multifocal red lesions are usu- dental abrasives causing localized marginal
ally accompanied by a pseudomembrane, gingival erythema.
desquamation, or, occasionally, bullae.
Contact allergy can be seen in the region
MICROSCOPIC FEATURES
in direct continuity with the incriminat-
ing allergen, which may be any dental The submucosa in immediate hypersensi-
material including heavy metals, topical tivity evinces capillary dilation and nonspe-
medications, or dental preparations such cific infiltration of the inflammatory cells.
FIGURE 3-12
Allergy to cinnamon show-
ing diffuse erythema (top)
and reaction to dental fin-
ishing abrasive particles
from crown margin finish-
ing (foreign body gingivitis)
(bottom).
PMPH_Eversole_Chapter-03.indd 63 1/17/2011 3:25:33 PM
64 Chapter 3
Eosinophils are present in variable numbers
yet are not usually a prominent feature. In Additional Reading
plasmacytosis gingivae, an avid plasma cell Crissey JT. Stomatitis, dermatitis and denture materials.
infiltrate prevails, producing myeloma-like Arch Dermatol. 1965;92:45.
features microscopically. Delayed reactions Eversole LR. Allergic stomatitides. J Oral Pathol Med.
are T-cell mediated and exhibit a lympho- 1979;34:93.
Kerr DA, McClatchey KD, Regezi JA. Allergic gingi-
cytic submucosal infiltrate with scattered vostomatitis (due to gum chewing). J Periodontol.
plasma cells and chronic epidermitis; the 1971;42:709.
histologic features may be similar to lichen Koutis D, Freeman S. Allergic contact stomatitis caused
planus. In foreign body gingivitis, small by acrylic monomer in a denture. Australas J Dermatol.
2001;42:203-206.
refractile particles can be identified under Tillman HH. Problems of allergy encountered in dentistry.
polarized light. Oral Surg Oral Med Oral Pathol. 1958;11:1372.
DIFFERENTIAL DIAGNOSIS
Hypersensitivity-related oral red lesions BULLOUS/EROSIVE DISEASES
may clinically mimic erosive lichen planus, Figure 3-13
lupus erythematosus, erythema migrans,
or any of the other diffuse red lesions out- Age: Variable
lined in this section. The differential diag- Sex: Variable
nosis may be limited by procuring a history CLINICAL FEATURES
of drug ingestion or occurrence of lesions
The bullous/desquamative diseases are
after use of a suspected allergenic sub-
detailed in Chapter 5. Suffice it to mention
stance. Biopsy shows nonspecific features.
here that most of these lesions show ery-
Epimucous patch testing may be accom-
thematous mucosal changes that occur in
plished by applying the suspected allergen
conjunction with the desquamative com-
on dried mucosa overlaid with an oral ban-
ponent. Thus, pemphigus vulgaris, benign
dage. Provided the material is not naturally
mucous membrane pemphigoid, erythema
caustic, a zone of erythema 24 to 48 hours
multiforme, epidermolysis bullosa, and
later generally denotes allergy if the pro-
erosive lichen planus can all appear as red
cedure can be reduplicated. Alternatively,
lesions; nevertheless, unlike the other ery-
most allergens causing mucositis evoke
thematous lesions listed in this chapter,
a positive cutaneous patch test, which is
sloughing of the mucosa is evident. The
easier to perform. Patch testing is reserved
reader is referred to the aforementioned
for delayed contact reactions. If immediate
chapter for detailed description of this
hypersensitivity is suspected, scratch tests
group of disorders. Of all the bullous/ero-
with suspected allergens can be performed
sive diseases, benign mucous membrane
or in vitro radioallergosorbant assays can
pemphigoid, erosive lichen planus, and
be used diagnostically.
erythema multiforme are more often rep-
resented by diffuse foci of erythema. In
TREATMENT
pemphigoid, the red lesions are primarily
Elimination of the allergen is necessary to localized to the attached gingiva; erosive
provide cure. Acute reactions and symp- and atrophic lichen planus involve the gin-
toms can be minimized by prescribing giva, vestibule, and buccal mucosa, and
antihistamines for systemic reactions or the hemorrhagic sloughing lesions in ery-
topical fluorinated steroids for contact thema multiforme are most prominent on
allergy. the lips.
PMPH_Eversole_Chapter-03.indd 64 1/17/2011 3:25:42 PM
Red and Pigmented Lesions 65
FIGURE 3-13
Bullous and desquamative
diseases with erythema.
MICROSCOPIC FEATURES Person JR, Rogers RS. III: Bullous and cicatricial pem-
phigoid: clinical, histopathologic and immunopatho-
The bullous diseases involve defects in cell- logic correlations. Mayo Clin Proc. 1977;52:54.
cell attachment or adhesion to the basement Scully C, El-Kom M. Lichen planus: review and update
membrane. The specific histopathologic fea- on pathogenesis. J Oral Pathol Med. 1985;14:431.
Silverman S, Jr, Gorsky M, Lozada-Nur F, Liu, A. Oral
tures for each of these conditions are given
mucous membrane pemphigoid. Oral Surg Oral Med
in Chapter 5. Oral Pathol. 1986;61:233.
TREATMENT
Because most of these diseases involve CANDIDIASIS
immunopathologic mechanisms and many Figure 3-14
are believed to be autoimmune, immuno-
Age: Infants and adults
suppressive therapy is used in their man-
Sex: No predilection
agement. In most patients, topically applied
steroid preparations suffice, whereas more CLINICAL FEATURES
severe instances may require systemic ste- The classic pseudomembranous white
roid therapy. lesions of Candida albicans infection may
occasionally be supplanted or obscured by
Additional Reading diffuse and multifocal red patches. A com-
mon clinical manifestation of erythematous
Altenburg A, Krahl D, Zouboulis CC. Non-infectious candidiasis has been termed denture sore
ulcerating oral mucous membrane diseases. J Dtsch mouth. The red lesions are confined to den-
Dermatol Ges. 2009;7:242-257.
ture-bearing mucosa, usually on the pal-
Lozada F, Silverman S, Jr. Erythema multiforme: clini-
cal characteristics and natural history in fifty patients. ate, and exhibit a patchy distribution often
Oral Surg Oral Med Oral Pathol. 1978;46:628. associated with speckled curd-like white
PMPH_Eversole_Chapter-03.indd 65 1/17/2011 3:25:42 PM
66 Chapter 3
FIGURE 3-14
Multifocal red lesions of candidiasis underlying an ill-fitting maxillary dental prosthesis.
lesions, which are generally easily displaced dermatitis herpetiformis, or malignancy.
by rubbing. Angular cheilitis often accom- Indeed, candidal infection may coexist
panies such changes. In addition to can- with carcinoma. A cytologic smear with
didal-induced red lesions under dentures, PAS stain will disclose mycelia, or culture
erythematous candidiasis occasionally may be performed. Failure to respond to
involves mucous membranes devoid of any antifungal therapy should be followed by
overlying dental prosthesis. The red patches biopsy and consideration of other possible
may be strictly erythematous or speckled as diseases in the differential diagnosis.
seen in denture sore mouth. The erythema-
tous component in this form of candidiasis TREATMENT
is a reflection of inflammation and may Nystatin cream or ointment may be applied
represent hypersensitivity to the organism. to the denture base for rapid resolution of ery-
Although rare, this mycosis may become thema followed by reconstruction or relin-
systemic with a granulomatous response, is ing. Erythematous candidiasis not related to
potentially lethal, and usually heralds the ill-fitting dentures can be managed by nys-
presence of an immunodeficiency disorder. tatin pastilles used 4 times per day for 7 to 10
days or oral clotrimazole troches to be used
MICROSCOPIC FEATURES
4 times daily. Alternatively, ketoconazole (a
The epithelium is attenuated, and PAS stain- single 200-mg tablet per day for 10 days) is
ing exhibits superficially oriented mycelia. generally effective provided the patient does
The underlying submucosa evinces a mild not suffer from liver disease.
to avid chronic or subacute inflammatory
cell infiltrate.
Additional Reading
DIFFERENTIAL DIAGNOSIS Cawson RA. Denture sore mouth and angular cheilitis.
Br Dent J. 1963;115:441.
Denture sore mouth candidiasis must be Davenport JC. Incidence of immediate and delayed
distinguished from a true allergic reac- hypersensitivity to Candida albicans in denture stoma-
tion to denture-base resin (an extremely titis. J Dent Res. 1971;50:892.
rare condition). Nondenture-related ery- Hoshi N, Mori H, Taguchi H et al. Management of oral
candidiasis in denture wearers. J Prosthodont Res.
thematous candidiasis may be confused 2010 (Apr 7).
with erythema migrans, radiation change, Reeve CM, Van Roekel N. Denture sore mouth.
lupus erythematosus, erosive lichen planus, Dermatol Clin. 1987;5:681.
PMPH_Eversole_Chapter-03.indd 66 1/17/2011 3:25:52 PM
Red and Pigmented Lesions 67
Roed-Peterson B, Renstrup G, Pindborg JJ. Candida in transmigration of neutrophils. The submu-
oral leukoplakia. Scand J Dent Res. 1970;78:323. cosa is infiltrated with nodular accumula-
tions of lymphocytes that distend the over-
lying epithelium.
LYMPHONODULAR
PHARYNGITIS DIFFERENTIAL DIAGNOSIS
Figure 3-15
The lesions differ from those of other oral
Age: Children and young adults viral infections in that they are erythematous
Sex: No predilection and nodular rather than vesicular. The coex-
istence of palatal and oropharyngeal lesions
CLINICAL FEATURES with fever allows segregation from other
Multifocal nodules with a pronounced ery- elements in the differential diagnosis, yet
thematous base localized primarily to the soft allergic mucositis and erythema multiforme
palate and oropharynx are seen in lympho- should be considered. In these diseases, tem-
nodular pharyngitis, a coxsackie virus type perature is not elevated over 37.8°C, whereas
A infection. Patients complain of sore throat in lymphonodular pharyngitis, it usually
and general malaise, are febrile, and mani- exceeds 38.4°C. Definitive diagnosis can be
fest regional nodal lymphadenitis. The nod- achieved by procuring a stool culture for
ules are multifocal and approximately 0.5 isolation of coxsackie virus.
cm in diameter with a wide erythematous
base. Similar lesions may occasionally be TREATMENT
seen anterior to the oropharynx. The disease Treatment of lymphonodular pharyngitis is
resolves spontaneously in 5 to 7 days. palliative. The symptoms may be mitigated
by prescribing a soothing oral rinse such as
MICROSCOPIC FEATURES an antihistaminic expectorant mixed with
The epithelium displays both intracyto- equal parts of Kaopectate, with subsequent
plasmic and intranuclear inclusions with swallowing for sedative affects.
Additional Reading
Lennette EH, Magoffin RL. Virologic and immunologic
aspects of major oral ulcerations. J Am Dent Assoc.
1973;87:1055.
Steigman AJ, Lipton MM, Braspennickx H. Acute
lymphonodular pharyngitis: a newly described condi-
tion due to coxsackie A virus. J Pediatr. 1963;61:331.
SCARLET FEVER
Figure 3-16
Age: Children
Sex: No predilection
CLINICAL FEATURES
FIGURE 3-15
Multiple red papules of the soft palate and orophar- Scarlet fever is caused by β-hemolytic strep-
ynx characteristic of lymphonodular pharyngitis, a tococci, which generate an erythrogenic
coxsackie virus infection. toxin. The toxin induces vascular dilation
PMPH_Eversole_Chapter-03.indd 67 1/17/2011 3:26:01 PM
68 Chapter 3
and damage with an erythematous macu- so-called strawberry tongue constitutes the
lar rash on the skin. A fiery red pharyngi- hallmark of the disease. The tongue lesion
tis is accompanied by cervical lymphade- may simulate a chemical burn. Atrophic
nopathy. The tongue similarly becomes glossitis seen in vitamin deficiency and
overtly erythematous with hypertrophy of pernicious anemia is usually mild and not
the fungiform papillae, termed strawberry nearly as bright red in appearance. Swab
tongue. Constitutional signs of infectious cultures of the oropharynx disclose the
disease are epitomized by fever and mal- presence of hemolytic streptococci, and
aise. Potential complications include rheu- antistreptolysin-O titers are elevated.
matic fever, otitis media, and pharyngeal
abscess. The disease was often fatal before TREATMENT
antibiotic treatment became available. Penicillin is preferred if no allergy to the
drug exists. Intramuscular injection of
MICROSCOPIC FEATURES
1,000,000 units is followed by oral penicillin
The pharyngeal mucosa may display super- daily. As dangerous complications occasion-
ficial necrosis, a pseudomembranous exu- ally occur, the patient should be referred to
date, and microbial colonies. The submucosa his or her physician.
evinces an acute or subacute inflamma-
tory cell infiltrate. The tongue is generally
devoid of ulceration yet shows vasodilation Additional Reading
with inflammatory cell infiltration, being a
Krugman S, Ward R. Chapter 25. Infectious Diseases of
nonspecific mucositis. Children. 4th ed. St Louis, MO: C. V. Mosby; 1968.
Schwentker FF, Janney JH, Gordon JE. The epidemiol-
DIFFERENTIAL DIAGNOSIS ogy of scarlet fever. Am J Hyg. 1943;38:27.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
The clinical tetrad of erythematous mac- Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
ules, pharyngitis, lymphadenopathy, and 1983:340.
Wesselhoeft C, Weinstein L. Scarlet fever. N Engl J Med.
1945;232:500, 531.
ATROPHIC LICHEN PLANUS
Figure 3-17
Age: Middle-aged adults
Sex: Predilection for females
CLINICAL FEATURES
When erythema, superficial ulceration, and
desquamation accompany the white com-
ponent, the term erosive lichen planus is used
or atrophic lichen planus when only red
lesions are extant. The buccal mucosa and
mucobuccal fold are favored locations, yet
other sites are generally involved as well.
Reticulated white lines or striae are often,
FIGURE 3-16 but not invariably, present and are super-
Acute erythematous pharyngitis, a feature of strep- imposed over a red base. The lesions are
tococcal sore throat. patchy, with or without an overt slough.
PMPH_Eversole_Chapter-03.indd 68 1/17/2011 3:26:02 PM
Red and Pigmented Lesions 69
FIGURE 3-17
Atrophic lichen planus show-
ing multifocal erythematous
erosions.
Bullae may sometimes be seen with a pre- staining fails to demonstrate precipitation
dominantly erosive form of lichen planus. of immunoglobulins. Rather, fibrinogen
Pain and burning are frequently encoun- globular deposits are demonstrated along
tered. Skin lesions are infrequently associ- the epidermal-submucosal interface corre-
ated with oral erosive lichen planus. Most sponding to the zones of desquamation and
patients are tense or anxiety prone, and basal lamina thickening.
the lesions wax and wane corresponding
to periods of emotional stress. The erosive DIFFERENTIAL DIAGNOSIS
form of lichen planus has been associated When a white component with reticulated
in rare instances with oral carcinoma. striae accompanies the red lesions, a clinical
diagnosis of erosive lichen planus should
MICROSCOPIC FEATURES
be the foremost consideration. Radiation
The epithelium is generally attenuated and mucositis, allergic mucositis, lupus erythe-
the basal cell layer is disorganized, with dif- matosus, and erythroplakic precancerous
fuse zones of degeneration. Transmigration lesions show similar clinical features. Oral
of lymphocytes into the basal and parabasi- red lesions with clinical and microscopic
lar cell regions is a prominant feature, and features of atrophic lichen planus may dis-
the basement membrane is eosinophilic close foci of cytologic atypia with potential
and thickened. A junctional separation at for carcinomatous transformation; such
the level of the basement membrane is gen- lesions have been termed lichenoid dyspla-
erally noted in multiple areas to the extent sia. If bullous lesions accompany the red
that the epithelial layer may be completely lesions, other bullous dermatoses should
detached or missing. The immediate sub- be considered in the differential diagnosis.
jacent connective tissue evinces a zonal Biopsy is indicated to secure a definitive
lymphocytic band. Immunofluorescence diagnosis.
PMPH_Eversole_Chapter-03.indd 69 1/17/2011 3:26:04 PM
70 Chapter 3
TREATMENT defective clotting mechanism should be
A topical fluorinated steroid application suspected. Without exhaustive explanation,
(0.05% fluocinonide gel four to five times the following causes should be considered in
daily) is the treatment of choice and results the pathogenesis: (1) hereditary clotting fac-
in a clearing of the painful erythematous tor deficiencies (e.g., hemophilia, Christmas
component. As erosive lichen planus is a disease), (2) use of medications with anti-
paroxysmal chronic disease, this medica- coagulant activity (e.g., coumarin), and (3)
tion can be used periodically during the primary liver disease. Gingival hemorrhage
more severe episodes. Because of the occa- and uncontrolled bleeding are also features
sional occurrence of carcinoma in this form associated with clotting factor deficiencies.
of lichen planus, patients should be sub- Purpura is encountered in various platelet
jected to periodic follow-up. Biopsy of areas disorders and leukemia as well.
that are refractory to treatment should be
performed. MICROSCOPIC FEATURES
Ecchymosis is characterized by submucosal
Additional Reading extravasation of erythrocytes with varying
amounts of hemosiderin pigment and orga-
Holmstrup P, Thorn JJ, Rindum J, Pindborg JJ. Malignant nization by fibrovascular and inflammatory
development of lichen planus-affected oral mucosa. cell elements.
J Oral Pathol Med. 1988;17:219.
Scully C, El-Korm M. Lichen planus: review and update DIFFERENTIAL DIAGNOSIS
on pathogenesis. J Oral Pathol Med. 1985;14:431.
Shklar G. Erosive and bullous oral lesions of lichen planus: Ecchymosis of the oral mucosa associated
histologic studies. Arch Dermatol. 1968;97:411. with clotting factor disorders is, in general,
Silverman S, Jr, Griffith M. Studies on oral lichen planus.
complicated by cutaneous manifestations or
Oral Surg Oral Med Oral Pathol. 1974;37:705.
Torrente-Castells E, Figueiredo R, Berini-Aytés L, hemarthrosis. The oral lesions often appear
Gay-Escoda C. Clinical features of oral lichen planus. as blood-filled diffuse bullae and, therefore,
A retrospective study of 65 cases. Med Oral Patol Oral are not readily confused with other diffuse
Cir Bucal. 2010;15(5):e685-90. or multifocal red lesions. Defective throm-
bocyte deficiencies are generally heralded
ECCHYMOSIS AND CLOTTING by petechial rather than ecchymotic hemor-
rhages; nevertheless, severe platelet anoma-
FACTOR DEFICIENCIES lies manifest ecchymotic lesions. Patients with
Figure 3-18 ecchymosis with no history of undue trauma
should be initially subjected to a coagulation
Age: No predilection
Sex: No predilection panel evaluation, including partial thrombo-
plastin time, prothrombin time, thrombocyte
CLINICAL FEATURES count, thrombocyte aggregation assay, bleed-
Red lesions caused by extravasation of blood ing and clotting time, and a tourniquet test.
will appear clinically as a submucosal ery-
thema or a diffuse slightly elevated smooth- TREATMENT
surfaced bruise. The color will range from Detection of an abnormal value in any of
red to brown to bluish black, depending these tests warrants referral to an internist
on the duration. Ecchymosis from trauma or hematologist. Oral surgical procedures
is common, yet when no traumatic inci- should be deferred until the coagulation
dent can be recalled or when the presence defect has been corrected or purified factor
of ecchymosis far outweighs the degree infusions can be administered just before
of trauma experienced by the patient, a initiation of any surgical procedures.
PMPH_Eversole_Chapter-03.indd 70 1/17/2011 3:26:12 PM
Red and Pigmented Lesions 71
FIGURE 3-18
Multiple reddish brown
ecchymotic pigmenta-
tions observed in hem-
orrhagic diatheses
associated with clotting
factor deficiencies.
Additional Reading
Archer WH. Oral and Maxillofacial Surgery. 5th ed.
Philadelphia, PA: W. B. Saunders; 1975:1558.
Curtis AB. Childhood leukemias: initial oral manifesta-
tions. J Am Dent Assoc. 1971;83:159.
Rettberg WAH. Symptoms and signs referable to the
oral cavity in blood dyscrasias. Oral Surg Oral Med
Oral Pathol. 1953;6:614.
Schelkun PM, Bellome J, Hiatt WR, DeBoom GW.
Multiple oral petechiae and ecchymoses in a
patient with osteoarthritis. J Am Dent Assoc. 1987;
115:735.
FIELD CANCERIZATION
Figure 3-19 FIGURE 3-19
Erythroplakia with occasional leukoplakic foci are
Age: Middle-aged and elderly adults representative of widespread carcinoma in situ.
Sex: Male predilection
CLINICAL FEATURES
parakeratosis. The individual epithelial cells
Multifocal erythroplakias show the same may evince changes ranging from atypia to
features as focal precancerous erythropla- frank invasive carcinoma. The submucosa
kia: velvety-red macules often accompanied is traversed by dilated capillaries with an
by a patchy or speckled leukoplakia com- accompanying dense diffuse inflammatory
ponent. As with leukoplakia, most patients cell infiltrate.
use tobacco and are heavy consumers of
alcoholic beverages. Importantly, patients DIFFERENTIAL DIAGNOSIS
with a history of oral cancer are at risk for
Multifocal red lesions in elderly patients,
developing not merely a recurrence in the
particularly those with tobacco and alcohol
previous site of involvement but multifocal
habits, should arouse suspicion of malig-
oral carcinomas. The larynx may also be the
nancy. Biopsy is indicated immediately if
site for other primary carcinomas.
no cause is discernible, even when other
diseases are considered likely components
MICROSCOPIC FEATURES
of the differential diagnosis. Field cancer-
The epithelium is invariably attenu- ization made manifest by multifocal eryth-
ated, with foci of hyperorthokeratosis or roplasia may mimic erythema migrans,
PMPH_Eversole_Chapter-03.indd 71 1/17/2011 3:26:12 PM
72 Chapter 3
radiation mucositis, lupus erythematosus, Moertel CG, Dockerty MB, Baggenstoss AH. Multiple
allergic mucositis, erythema multiforme, primary malignant neoplasms. III. Tumors of multi-
centric origin. Cancer. 1961;14:238.
erythematous candidiasis, or erosive lichen Shafer WG, Hine MK, Levy BM. A Textbook of Oral
planus. Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
1983:115.
TREATMENT Slaughter DP., Southwick HW, Smejkal W. “Field can-
cerization” in oral stratified squamous epithelium;
Field cancerization is an extremely difficult clinical implications of multicentric origin. Cancer.
management problem and is particularly 1953;6:963.
enigmatic when a preexisting carcinoma Waldron CA. In: Gorlin RJ, Goldman HM, eds. Thoma’s
Oral Pathology. Vol. 2. 6th ed. St Louis, MO: C. V.
was present and was managed by radiation Mosby; 1970:824, 826.
therapy. Surgical stripping of carcinoma in
situ and radiation therapy remain the treat-
ment methods of choice. Complete exami- KAPOSI’S SARCOMA
nation with work-up for other primary
Figure 3-20
lesions in the oropharynx and larynx is
indicated, with management by an experi- Age: Young adults
enced oncologist. Sex: Males
CLINICAL FEATURES
Additional Reading Kaposi’s sarcoma was rarely seen during the
Ge L, Meng W, Zhou H, Bhowmick N. Could stroma
pre-AIDS years, but afterward, oral and cuta-
contribute to field cancerization? Med Hypotheses. neous Kaposi’s sarcoma became common
2010;75(1):26-31. findings among human immunodeficiency
FIGURE 3-20
Red and purple mac-
ules and tumefactions in
HIV-associated Kaposi’s
sarcoma.
PMPH_Eversole_Chapter-03.indd 72 1/17/2011 3:26:17 PM
Red and Pigmented Lesions 73
virus (HIV)-infected males, predominantly Dterak D. Opportunistic infections and Kaposi’s sar-
homosexuals. The lesions are vascular, coma in homosexual men. N Engl J Med. 1981;305:
1465.
angiomatous neoplasms that begin as a red Eversole LR, Leider AS, Jacobsen PL, Shaber EP. Oral
macule and progress to large tumefactive Kaposi’s sarcoma associated with acquired immuno-
red and purple lesions. This neoplastic con- deficiency syndrome among homosexual males. J Am
dition is an opportunistic infection caused Dent Assoc. 1983;107:248.
Feller L, Lemmer J, Wood NH, Jadwat Y, Raubenheimer
by herpes virus type 8. Oral lesions may be EJ. HIV-associated oral Kaposi sarcoma and
multifocal and are typically seen on the pal- HHV-8: a review. J Int Acad Periodontol. 2007;9:
ate and gingiva. 129-136.
Silverman S, Jr. AIDS update: oral findings, diagno-
MICROSCOPIC FEATURES sis and precautions. J Am Dent Assoc. 1987;115:
559.
Underlying surface epithelium is a spindle
cell proliferation with many of the tumor
cells found adjacent to sinusoidal spaces. The
spindle cell nuclei show mild pleomorphism
Petechiae
and cells lining vascular channels show a SUCTION PETECHIAE
hobnail appearance. Hemosiderin pigment Figure 3-21
granules are found throughout the tumor.
Age: No predilection
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Pyogenic granuloma, giant cell granuloma, CLINICAL FEATURES
and other angiomatous lesions are consid-
Petechiae are characterized by pinpoint-
ered in the differential diagnosis.
sized red spots 1 to 3 mm in diameter,
are multifocal, and may show confluency.
TREATMENT
Suction petechiae are located either beneath
Lesions tend to resolve or are prevented a denture with a relief zone or on the soft
when triple AIDS therapy is instituted. palate in patients complaining of pruritus
Unsightly lesions can be removed by inject- in that region. They may begin as a pro-
ing sclerosing agents, cauterization, or laser dromal sign for sore throat, influenza, or
ablation. the common cold. Onset of “itchiness” in
the soft palate may induce the patient to
Additional Reading suck or click the area for relief, with resul-
tant microvascular rupture. Soft-palate
Alper RA, Wiggins HE. Hemorrhagic palatal lesion. petechiae are also the result of orogenital
J Oral Pathol Med. 1975;4:222. sexual activity.
FIGURE 3-21
Petechial hemorrhages
evolving as the result of
negative pressure on the
oral tissues.
PMPH_Eversole_Chapter-03.indd 73 1/17/2011 3:26:26 PM
74 Chapter 3
MICROSCOPIC FEATURES Giansanti JS, Cramer JR, Weathers DR. Palatal erythe-
ma: another etiologic factor. Oral Surg Oral Med Oral
Damaged vascular walls of small vessels in Pathol. 1975;40:379.
the submucosa manifest a juxtaposed zone Schlesinger SL, Borbotsina J, O’Neill L. Petechial hem-
of erythrocyte extravasation. orrhages of the soft palate secondary to fellatio. Oral
Surg Oral Med Oral Pathol. 1975;40:376.
DIFFERENTIAL DIAGNOSIS
Infectious mononucleosis may be present INFECTIOUS
with palatal petechiae, yet other clinical and
MONONUCLEOSIS
laboratory features provide data that elimi-
nate consideration in the differential diag- Figure 3-22
nosis. If the patient does not recall clicking Age: Young adults
his or her soft palate and if other mucocuta- Sex: No predilection
neous petechiae are observed, thrombocyte
deficiencies or leukemia should be ruled out CLINICAL FEATURES
by instituting appropriate laboratory stud- Palatal petechiae are commonly seen in
ies. Hereditary hemorrhagic telangiectasia infectious mononucleosis, located on the
shows other characteristics essential for the soft palate. The petechiae are probably
diagnosis. Scurvy may include petechiae as engendered by suction on a pruritic soft
a component of vitamin C deficiency, but palate by the tongue as outlined for suc-
this disease is encountered with extreme tion petechiae; however, other hemorrhagic
rarity in this day and age. manifestations such as epistaxis have been
reported. A generalized stomatitis with
TREATMENT erythema and ulceration may also be evi-
No treatment is necessary for nondenture- dent. Other clinical features implicating
related suction petechiae. Those lesions onset of infectious mononucleosis, a herpes
related to a denture relief zone resolve after virus infection (Epstein-Barr virus), include
relining or rebasing the prosthesis. extreme malaise with lethargy, lymphade-
nopathy, hepatosplenomegaly, sore throat,
Additional Reading and fever.
Damm DD, White DK, Brinker CM. Variations of pala- MICROSCOPIC FEATURES
tal erythema secondary to fellatio. Oral Surg Oral Med
Oral Pathol. 1981;52:417. Damaged vascular walls of small vessels in
the submucosa manifest a juxtaposed zone
of erythrocyte extravasation.
DIFFERENTIAL DIAGNOSIS
Palatal petechiae are seen in sore throat
independent from infectious mononucleo-
sis, in platelet disorders, and in hereditary
hemorrhagic telangiectasia. The diagno-
sis of infectious mononucleosis may be
confirmed when the heterophil antibody
titer exceeds 1:28. The monospot screen-
ing serologic test, although not as accurate
FIGURE 3-22 as the heterophil antibody titration, is rap-
Soft-palate petechiae in infectious mononucleosis. idly performed and is usually adequate
PMPH_Eversole_Chapter-03.indd 74 1/17/2011 3:26:33 PM
Red and Pigmented Lesions 75
diagnostically. The appearance of atypical mucosa, yet lesions are encountered on
lymphocytes (Downey cells) on the dif- skin surfaces as well. Various diseases may
ferential blood count is also a diagnostic inhibit platelet formation. Myelophthisic
finding. anemia with thrombocytopenia can occur
with leukemia, lymphoma, metastatic
TREATMENT carcinoma to bone, and marble bone dis-
Treatment for infectious mononucleosis is ease. Primary thrombocytopenic purpura,
supportive, with bed rest and high liquid pancytopenia, and bone marrow depres-
intake. A mild analgesic and antipyretic are sion from cytotoxic drugs result in lack of
recommended. platelets. Malfunctioning platelets may be
responsible for petechial hemorrhages in
thrombocytopathic purpura, thrombasthe-
Additional Reading nia, or secondary to overuse of salicylates.
In addition to these bleeding disorders, a
Cassingham RJ. Infectious mononucleosis: a review of
the literature, including recent findings on etiology. variety of nonthrombocytopenic purpuras
Oral Surg Oral Med Oral Pathol. 1971;31:610. exist, including anaphylactoid purpura,
Dunnett WN. Infectious mononucleosis. Br Med J. snake venom purpura, and certain infec-
1963;1:1187. tious diseases. In all thrombocyte disorders,
Holzel A. An early clinical sign in infectious mononucleo-
sis. Oral Surg Oral Med Oral Pathol. 1959;12:685. petechiae may be accompanied by gingival
Shafer WG, Hine MK, Levy BM. A Textbook of Oral hemorrhage or prolonged bleeding after
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders; extraction.
1983:736.
Shiver CB, Berg P, Frenkel EP. Palatine petechiae:
an early sign in infectious mononucleosis. J Am Med MICROSCOPIC FEATURES
Assoc. 1956;161:592.
Damaged vascular walls of small vessels in
the submucosa manifest a juxtaposed zone
THROMBOCYTE DISORDERS of erythrocyte extravasation.
Figure 3-23
DIFFERENTIAL DIAGNOSIS
Age: Children and young adults
Sex: No predilection Thrombocyte disorders may be differenti-
ated clinically from other petechia-produc-
CLINICAL FEATURES
ing diseases in that the lesions are not con-
Petechiae resulting from platelet deficiency fined to the palate yet may be ubiquitous
or malfunction may be present on oral with lesions on the skin of the extremities
FIGURE 3-23
Petechial hemorrhages in leukemic patients with secondary thrombocytopenia.
PMPH_Eversole_Chapter-03.indd 75 1/17/2011 3:26:34 PM
76 Chapter 3
and trunk. The tourniquet test is posi- HEREDITARY HEMORRHAGIC
tive. A work-up for the underlying cause TELANGIECTASIA
includes complete blood count and plate- Figure 3-24
let count and other clinical and laboratory
tests specific for the diseases enumerated Age: Begins in infancy
under clinical features. A history of drug Sex: No predilection
use is of utmost significance when consid-
CLINICAL FEATURES
ering causes of petechiae. Because evalu-
ation of disease entities producing pete- Hereditary hemorrhagic telangiectasia is
chiae involves manifold considerations and inherited as a dominant trait and is charac-
complex relationships, the patient should terized by the appearance of spider telangi-
be referred to a hematologist for definitive ectasias of skin, primarily on the face and
diagnosis and treatment. neck with petechia-like lesions of the oral
mucosa. Epistaxis is a prominent clinical
TREATMENT sign. Bleeding from the gingiva is also a
Management of platelet disorders is gov- feature. Platelet and clotting factor func-
erned by the underlying cause. Definitive tions are normal. Perivascular supportive
diagnosis and treatment should be deter- tissue appears to be defective.
mined by a physician.
MICROSCOPIC FEATURES
Submucosal dilated vessels are present
Additional Reading and evince leakage of the vascular contents
with fibrin deposition in the perivascular
Barrett AP. Oral changes as initial diagnostic indica-
tors in acute leukemia. J Oral Pathol Med. 1986; region.
41:234.
Linenberg WB. Idiopathic thrombocytopenic purpura. DIFFERENTIAL DIAGNOSIS
Oral Surg Oral Med Oral Pathol. 1964;17:22.
Lynch MA, Ship II. Oral manifestations of leukemia; The resemblance to petechial disease is
a post-diagnostic study. J Am Dent Assoc. 1967;75: striking; however, close scrutiny of the skin
1139. lesions discloses the spider-like angiomas
Stafford R, Sonis S, Lockhart P, Sonis A. Oral pathoses as rather than true petechial macules, and
diagnostic indicators in leukemia. Oral Surg Oral Med
Oral Pathol. 1980;50:134.
a hereditary history will generally lead
Wintrobe MM. Clinical Hematology. 7th ed. Philadelphia, to a diagnosis of hereditary hemorrhagic
PA: Lea & Febiger; 1974. telangiectasia. Bleeding and clotting times
FIGURE 3-24
Red papules in hereditary hemorrhagic telangiectasia.
PMPH_Eversole_Chapter-03.indd 76 1/17/2011 3:26:44 PM
Red and Pigmented Lesions 77
are normal. Platelets and clotting factors are Shah RK, Dhingra JK, Shapshay SM. Hereditary
within normal limits unless profuse hem- hemorrhagic telangiectasia: a review of 76 cases.
Laryngoscope. 2002;112:767-773.
orrhage has resulted in a blood-loss anemia
with thrombocytopenia.
TREATMENT
Focal Pigmentations
Genetic counseling is recommended. A AMALGAM AND GRAPHITE
normal life span can be expected; how- TATTOO
ever, death from epistaxis may occur. Figure 3-25
Hemorrhage can generally be controlled by
placement of pressure packs. Age: No predilection
Sex: No predilection
Additional Reading CLINICAL FEATURES
Tattoos caused either by traumatic implanta-
Austin GB, Quart AM, Novak B. Hereditary hemor- tion of dental amalgam or by graphite from a
rhagic telangiectasias with oral manifestations: report
of periodontal treatment in two cases. Oral Surg Oral lead pencil produce a gray to black pigment
Med Oral Pathol. 1981;51:245. in the mucosa. The borders are generally
Gorlin RJ, Pindborg JJ. Syndromes of the Head and Neck. somewhat diffuse, and the pigment does not
New York: Blakiston Division, McGraw-Hill; 1964. blanch on pressure. Amalgam tattoos are usu-
Everett FG, Hahn CR. Hereditary hemorrhagic telangi-
ectasia with gingival lesions: review and case reports. ally located on the gingiva, alveolar ridge, or
J Periodontol. 1976;47:295. buccal mucosa, whereas graphite tattoos are
Scopp IW, Quart A. Hereditary hemorrhagic telangiecta- more often seen on the palate where a pen-
sia involving the oral cavity. Oral Surg Oral Med Oral cil wound was self-inflicted. Large amalgam
Pathol. 1958;11:1138.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
tattoos can be demonstrated radiographi-
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders; cally. Amalgam tattoos are usually solitary
1983:157. but occasionally may be multiple.
FIGURE 3-25
Dark areas representing
amalgam tattoos.
PMPH_Eversole_Chapter-03.indd 77 1/17/2011 3:26:48 PM
78 Chapter 3
MICROSCOPIC FEATURES Peters E, Gardner DG. A method of distinguishing
between amalgam and graphite in tissue. Oral Surg
Brown or black foreign material is pres- Oral Med Oral Pathol. 1986;62:73.
ent yet fails to elicit a giant cell response. Weathers DR, Fine R M. Amalgam tattoo of oral muco-
Stippling of collagen, reticulin, and sa. Arch Dermatol. 1974;110:727.
perivascular connective tissues with par-
ticulate granules is a prominent feature,
and inflammatory cells are present in lim- MUCOCELE
ited number. Figure 3-26
Age: No predilection
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Amalgam tattoos must be differenti-
CLINICAL FEATURES
ated from nevi and superficial melanoma.
Pressure without blanching differentiates Mucoceles may appear as focal reddish blue
amalgam tattoos from vascular lesions. elevations if hemorrhage has occurred. As
with the conventionally appearing fluid-
TREATMENT filled mucous retention phenomena, hemor-
rhagic mucoceles follow trauma with rupture
Failure to demonstrate radiopaque particles or severance of a minor salivary duct with
on radiographs for suspected amalgam tat- pooling of mucus within the submucosa;
too necessitates biopsy to rule out nevus they are most frequently encountered on the
or melanoma. No treatment is necessary lips, buccal mucosa, and ventral tongue.
for those lesions that are radiographically
demonstrable. MICROSCOPIC FEATURES
The epithelium is distended by an under-
Additional Reading lying zone of pooled mucin encompassed
by a granulation tissue pseudocystic mem-
Buchner A, Hansen LS. Amalgam pigmentation (amal- brane. Extravasated erythrocytes and fibrin
gam tattoo) of the oral mucosa. A clinicopathologic
are admixed with mucin and inflammatory
study of 268 cases. Oral Surg Oral Med Oral Pathol.
1980;49:139. cells.
Harrison J, Rowley P, Peters P. Amalgam tattoos. Light
and electron microscopy and electron-probe micro- DIFFERENTIAL DIAGNOSIS
analysis. J Pathol. 1977;121:83.
Orban B. Discoloration of the oral mucous membrane by Hemorrhagic mucoceles may be indistin-
metallic foreign bodies. J Periodontol. 1946;17:55. guishable clinically from hemangioma,
FIGURE 3-26
Mucocele containing extravasated blood and appearing as brown pigmented masses.
PMPH_Eversole_Chapter-03.indd 78 1/17/2011 3:26:55 PM
Red and Pigmented Lesions 79
varix, hematoma, nevus, or even melanoma. intraluminal but extravasated, hematomas
A history of antecedent trauma can usually do not blanch on pressure.
be elicited.
MICROSCOPIC FEATURES
TREATMENT The submucosa evinces profuse erythro-
Local excision with extirpation of the cyte extravasation with fibrin deposition.
underlying minor salivary lobules is rec- Variable degrees of fibrovascular organiza-
ommended. Failure to remove the glandu- tion with inflammation are present.
lar tissue may contribute to recurrence.
DIFFERENTIAL DIAGNOSIS
Additional Reading Hematomas are the result of trauma yet
may be confused clinically with hemor-
Cataldo E, Mosadomi A. Mucoceles of the oral mucous rhagic mucocele, tattoo, hemangioma or
membrane. Arch Otolaryngol Head Neck Surg. varix, nevus, and melanoma. Ecchymosis
1970;91:360.
Granholm C, Olsson Bergland K, Walhjalt H, Magnusson
is identical, yet in blood dyscrasias, trauma
B. Oral mucoceles; extravasation cysts and retention is minor and the lesions are usually
cysts. A study of 298 cases. Swed Dent J. 2009;33:125- multifocal.
130.
Harrison JD. Salivary mucoceles. Oral Surg Oral Med
TREATMENT
Oral Pathol. 1975;39:268.
Robinson L, Hjorting-Hansen E. Pathologic changes A suspected hematoma should be
associated with mucous retention cysts of minor observed over a 2-week period. Failure to
salivary glands. Oral Surg Oral Med Oral Pathol.
1964;18:191. resolve indicates the clinical impression
was incorrect and biopsy should be per-
formed. Any hematoma observed without
HEMATOMA significant provocation or trauma should
Figure 3-27 arouse suspicion of associated with a blood
dyscrasia.
Age: No predilection
Sex: No predilection
CLINICAL FEATURES
Additional Reading
Mucosal hematomas or bruises result from Archer WH. Oral and Maxillofacial Surgery. 5th ed.
Philadelphia, PA: W. B. Saunders; 1975:1554.
vascular severance resulting from trauma. Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral
They are brown or blue and may be mac- Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger;
ular or swollen. Because the blood is not 1978:407.
FIGURE 3-27
Hematoma of the buccal
mucosa.
PMPH_Eversole_Chapter-03.indd 79 1/17/2011 3:27:05 PM
80 Chapter 3
NEVUS arranged in clumps or theques; junctional
Figure 3-28 nevi maintain continuity with the epithe-
lium, whereas intramucosal types are con-
Age: No predilection fined to the underlying connective tissue.
Sex: Female predilection Spindle cell nevi contain elongated spindle
CLINICAL FEATURES cells with a junctional (intraepithelial) com-
ponent. Melanocytic or blue nevi are con-
Oral nevi are rare and are characterized by a fined to the submucosa and are composed
plaque- or dome-shaped sessile nodule with of fibroblast-like spindle cells with fascicu-
blue or black pigmentation. Occasionally, lation. Melanin granules may be seen in all
nonpigmented forms occur intraorally. forms and may be sparse or pervasive.
They may be seen at any age, but are likely
to have been present since childhood. DIFFERENTIAL DIAGNOSIS
Pigmented nevi do not blanch on pressure
and are most frequently encountered on the Nevi do not blanch under pressure and
palate, gingiva, buccal mucosa, and lips. may clinically be indistinguishable from a
They generally reach a given size, and the tattoo, hematoma, or superficial melanoma.
growth becomes static. Various types exist, An ephelis is flat, lacking any tumefaction
including junctional, compound, intramu- yet is often indistinguishable clinically
cosal, blue nevus, and spindle cell nevus. from junctional nevi and tattoos.
MICROSCOPIC FEATURES TREATMENT
The histology of nevi is variable. Nevocellular Junctional nevi in adults may evolve into
nevi are composed of oval epithelioid cells malignant melanoma. For this reason, all
FIGURE 3-28
Pigmented nevi appear
brown, black, or blue
and may be papular or
macular.
PMPH_Eversole_Chapter-03.indd 80 1/17/2011 3:27:11 PM
Red and Pigmented Lesions 81
pigmented lesions in the mouth in which EPHELIS, ORAL MELANOTIC
nevus is a consideration in the differential MACULE
diagnosis should be excised and submitted Figure 3-29
for microscopic examination.
Age: No predilection
Sex: Female predilection
Additional Reading CLINICAL FEATURES
Bhaskar SN, Jacoway JR. Blue nevus of the oral
mucosa. Oral Surg Oral Med Oral Pathol. 1965;
Ephelis, or freckle, occurs on sun-exposed
19:678. skin and is common on the face, yet unusual
Buchner A, Hansen LS. Pigmented nevi of the oral on the vermilion border. The lesion is brown
mucosa: a clinicopathologic study of 36 new cas- or brownish black and macular; in most
es and review of 155 cases from the literature. I
cases, it is less than one half of 1 cm. The
& II. Oral Surg Oral Med Oral Pathol. 1987;63:
566, 676. melanotic macule occurs on oral mucosa and
Meleti M, Mooi WJ, Casparie MK, van der Waal therefore is not related to actinic radiation.
I. Melanocytic nevi of the oral mucosa—no evi- Oral melanotic macules are focal brown,
dence of increased risk for oral malignant mela- blue, or black spots that are most frequently
noma: an analysis of 119 cases. Oral Oncol. 2007;43:
976-981. observed on the gingiva and buccal mucosa.
Trodahl JN, Sprague WG. Benign and malignant mel-
anocytic lesions of the oral mucosa: an analysis of 135 MICROSCOPIC FEATURES
cases. Cancer. 1970;25:812.
Weathers DR. Benign nevi of the oral mucosa. Arch Melanotic macules do not evolve from
Dermatol. 1969;99:688. proliferation of melanocytes; rather, the
FIGURE 3-29
Oral melanotic macule.
PMPH_Eversole_Chapter-03.indd 81 1/17/2011 3:27:25 PM
82 Chapter 3
epithelium is unremarkable, and the basal Page LR, Coro RE, Crawford BE, Giansanti JS, Weathers
cells exhibit diffuse deposition of melanin DR. The oral melanotic macule. Oral Surg Oral Med
Oral Pathol. 1977;44:219.
pigment. Occasionally, melanin inconti- Shapiro L, Zegarelli DJ. The solitary labial lentigo: a clin-
nence is observed with pigment granules icopathologic study of 20 cases. Oral Surg Oral Med
identifiable in subepithelial melanophages. Oral Pathol. 1971;31:87.
Weathers DR, Corio RL, Crawford BE, Giansant JS,
Page LR. The labial melanotic macule. Oral Surg Oral
DIFFERENTIAL DIAGNOSIS Med Oral Pathol. 1976;42:196.
The focal macular appearance of ephelis of
the lip or melanotic macule of oral mucosa
may be identical to amalgam tattoo, junc- Diffuse and Multifocal
tional nevus, or early superficial spreading Pigmentations
melanoma. Pigmented lesions of this nature
cannot be diagnosed without microscopic MALIGNANT MELANOMA
evaluation. Figure 3-30
TREATMENT Age: Middle age and above
Sex: Male predilection
Excision is the treatment of choice.
CLINICAL FEATURES
Additional Reading Oral melanomas exhibit a striking predi-
lection for the palatal mucosa, chiefly ante-
Buchner A, Hansen LS. Melanotic macule of the oral rior palate and maxillary alveolar ridge or
mucosa: a clinicopathologic study of 105 cases. Oral gingiva. Most are pigmented, either bluish
Surg Oral Med Oral Pathol. 1979;48:244.
Nikitakis NG, Brooks JK. Diffuse oral mucosal pigmen-
black or dark brown. They begin as macu-
tations. Smoker’s melanosis. Gen Dent. 2010;58:151, lar focal lesions but may rapidly grow to
153-154 fungating diffuse tumefactions. Ulceration
FIGURE 3-30
Malignant melanoma of the
oral cavity, usually seen on
the anterior maxillary or
palatal mucosa. It begins as
a brown-black or blue pig-
mentation with irregular
borders and becomes pro-
gressively more diffuse.
PMPH_Eversole_Chapter-03.indd 82 1/17/2011 3:27:40 PM
Red and Pigmented Lesions 83
is a common finding. As proliferation to the papillary dermis are “thin” melano-
ensues, satellite lesions or streaking of pig- mas whereas those with deep invasion are
ment can be noted at the lateral margins. “thick” melanomas.
The tumor may or may not be indurated.
Survival rates for oral and cutaneous mela- DIFFERENTIAL DIAGNOSIS
nomas are extremely low; less than 5% live Early oral melanoma may be confused with
for 5 years. Widespread dissemination to other focal pigmentations. Because melanin
both nodes and distant sites is common. does not blanch, differentiation from a vas-
A superficial form known as malignant cular lesion can be made clinically. Because
freckle of Hutchinson has a more favorable melanoma must be detected at its earliest
prognosis; although usually located on stage to achieve cure, biopsies from all oral
facial skin, oral cases have been reported. focal pigmentations are recommended.
Malignant freckle is macular with mini-
mal tumefaction. Nonpigmented varieties TREATMENT
of melanoma occur and may be confused
clinically with inflammatory and other Radical surgery is indicated and should be
neoplastic swellings. There is a genetic performed by a cancer surgeon. Prophylactic
predilection for oral melanoma on certain neck dissection in the absence of clinically
islands in Japan. palpable nodes probably does not improve
the prognosis.
MICROSCOPIC FEATURES
Three specific microscopic patterns are Additional Reading
observed in melanoma. The Hutchinson’s
Chaudhry AP, Hampel A, Gorlin RJ. Primary malignant
freckle variety is a slowly growing lesion melanoma of the oral cavity; a review of 105 cases.
usually seen on the malar skin charac- Cancer. 1958;11:923.
terized by proliferation of pleomorphic, Kato T, Takematsu H, Tomita Y, Takahashi M, Abe R.
palisaded melanocytes distributed along Malignant melanoma of mucous membranes. A clini-
copathologic study of 13 cases in Japanese patients.
the epidermal/dermal junction with a Arch Dermatol. 1987;123:216.
horizontal or lateral direction of prolifera- Moreno MA, Hanna EY. Management of mucosal
tion. These atypical cells fail to invade the melanomas of the head and neck: did we make any
upper epithelial layers. The second vari- progress? Curr Opin Otolaryngol Head Neck Surg.
2010;18:101-106.
ety also proliferates along the epidermal/ Regezi JA, Hayward JR, Pickens TN. Superficial melano-
dermal junction and is termed the super- mas of oral mucous membranes. Oral Surg Oral Med
ficial spreading type. This type exhibits a Oral Pathol. 1978;45:730.
pagetoid appearance with ovoid tumor cell Trodahl JN, Sprague WG. Benign and malignant melan-
otic lesions of the oral mucosa; an analysis of 135 cases.
nests showing a propensity for invasion of Cancer. 1970;25:812.
the upper epithelial layers. The third vari-
ety is invasive melanoma. This form may
arise de novo or evolve from either of the RACIAL PIGMENTATION
aforementioned lesions. The invasive type
Figure 3-31
is usually nodular and exhibits a vertical
growth pattern that invades the underlying Age: Present at birth
connective tissues. The cells are spindle, Sex: No predilection
ovoid, or polygonal and are pleomorphic
CLINICAL FEATURES
with variable amounts of melanin pigment.
Invasive melanomas are graded depending The oral mucosa of blacks and many dark-
on their depth of growth: lesions confined skinned whites is often stippled with
PMPH_Eversole_Chapter-03.indd 83 1/17/2011 3:27:56 PM
84 Chapter 3
FIGURE 3-31
Racial melanosis can be
seen anywhere in the
mouth but is identified
more commonly on the
gingiva of blacks or dark-
skinned whites.
multifocal and diffuse macular pigmenta- PIGMENTED LICHEN PLANUS
tions, generally dark brown. These zones Figure 3-32
may occur anywhere in the mouth and are
more often encountered on the gingiva. Age: Adults
They are innocuous manifestations of racial Sex: Females more often affected
or ethnic origin and have no premalignant CLINICAL FEATURES
potential.
Whereas lichen planus is usually charac-
MICROSCOPIC FEATURES terized by either white striated lesions or
mixed red and white lesions in the erosive
Melanin granules are densely accumulated
form, a pigmented variety is occasionally
in the basal cell layer.
encountered. The pigmented zones are
macular with a black, brown, or slate-gray
DIFFERENTIAL DIAGNOSIS
appearance and are most prevalent on the
When the patient’s skin is heavily pig- buccal mucosa. Invariably, the pigmented
mented, oral pigmentation can be consid- mucosa is surrounded by a zone of white,
ered normal. In whites, other diseases must and reticulated striae can be discerned.
be considered, for example, Addison’s dis-
ease, neurofibromatosis, or heavy metal
MICROSCOPIC FEATURES
ingestion.
The surface keratin is thickened, and
TREATMENT transmigration of lymphocytes into the
No treatment is necessary. basilar and parabasilar zones occurs. The
basal cell layer contains melanin granules,
and this layer is disrupted with melanin
Additional Reading incontinence. The submucosa is occupied
by a band-like lymphocytic infiltrate with
Dummett CO. Oral pigmentation—physiologic and interposed free melanin granules and
pathologic. N Y State Dent J. 1959;25:407.
Dummett CO. Physiologic pigmentation of the oral melanophages.
and cutaneous tissues in the Negro. J Dent Res.
1946;25:421.
Mescon H, Grots IA, Gorlin RJ. In Gorlin RJ, Goldman DIFFERENTIAL DIAGNOSIS
HM, eds. Thoma’s Oral Pathology. Vol. 2. 6th ed. St The pigmented zones of this form of lichen
Louis, MO: C. V. Mosby; 1970:672.
Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral planus may be confused with other diffuse
Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger; pigmented lesions included here; however,
1978:382. one is usually able to detect the presence of
PMPH_Eversole_Chapter-03.indd 84 1/17/2011 3:27:56 PM
Red and Pigmented Lesions 85
FIGURE 3-32
Gray melanin deposition
associated with white
stria in pigmented lichen
planus.
FIGURE 3-33
Peutz-Jeghers syndrome:
melanotic macules of the
lips, melanotic macules
of the fingers, and benign
intestinal polyps.
accompanying white striae. A biopsy will PEUTZ-JEGHERS SYNDROME
confirm the diagnosis. Figure 3-33
TREATMENT Age: Childhood onset
Sex: No predilection
Provided an erosive component is lacking,
no treatment is necessary. CLINICAL FEATURES
Peutz-Jeghers syndrome is inherited as
Additional Reading an autosomal dominant trait and is char-
acterized by multifocal macular melanin
Murti PR, Bhousle RB, Daftary DK, Mehta FS. Oral pigmentation in perioral locations. These
lichen planus associated with pigmentation. J Oral macules or freckles stipple the vermilion
Pathol Med. 1979;34:23.
Scully C, Porter S. ABC of oral health. Swellings
and may extend into the facial skin as well
and red, white, and pigmented lesions. BMJ. as the oral mucosa. Intestinal polyposis
2000;321(7255):225-228. with no tendency for malignant change
PMPH_Eversole_Chapter-03.indd 85 1/17/2011 3:28:05 PM
86 Chapter 3
may contribute to colic pain in affected Jeghers H, McKusick VA, Katz KH. Generalized intes-
individuals. In addition to perioral lesions, tinal polyposis and melanin spots of the oral mucosa,
lips and digits. N Engl J Med. 1949;241:993, 1031.
the extremities may show dermal foci of Lucky AW. Pigmentary abnormalities in genetic disor-
pigmentation. ders. Dermatol Clin. 1988;6:193.
Tan VK, Koh PK, Loi CT, Eu KW, Tang CL. Peutz-
MICROSCOPIC FEATURES Jeghers syndrome: data from the Singapore Polyposis
Registry and a shifting paradigm in management. Ann
The basal cell layer contains a profusion of Acad Med Singapore. 2010;39:17-21.
melanin granules. Wesley RK, Delaney JR, Pensler L. Mucocutaneous mel-
anosis and gastrointestinal polyposis (Peutz-Jeghers
syndrome): clinical considerations and report of case.
DIFFERENTIAL DIAGNOSIS J Dent Child. 1977;44:131.
The perioral location is unique and diag-
nostic. Intestinal radiographic studies dis-
close the presence of polyps primarily in
MULTIPLE
the small intestine. NEUROFIBROMATOSIS
Figure 3-34
TREATMENT
Age: Childhood onset
Provided an erosive component is lack- Sex: No predilection
ing, no treatment is necessary. Patients can
CLINICAL FEATURES
be advised of the genetic character of the
disease. Referral to a gastroenterologist is An inheritable disease characterized by
recommended. multiple neurofibromatous nodules, von
Recklinghausen’s disease of skin also
manifests pigmented macules of skin
Additional Reading termed café-au-lait spots. The pigment is
Bartholomew LG, Moore CE, Dahlin DC, Waugh JM.
light brown and the macules vary consid-
Intestinal polyposis associated with mucocutaneous erably in size, displaying smooth demar-
pigmentation. Surg Gynecol Obstet. 1962;115:1. cated borders. The neurofibromas exist in
FIGURE 3-34
Café-au-lait pigmentations
and tumor nodules in neuro-
fibromatosis.
PMPH_Eversole_Chapter-03.indd 86 1/17/2011 3:28:27 PM
Red and Pigmented Lesions 87
two forms: nodular, with a putty-like feel
on palpation, or flabby pendulous folds. Additional Reading
The neurofibromas and macular pigmen- Crowe RW, Schull WJ. Diagnostic importance of café-
tations may involve the oral mucous mem- au-lait spots in neurofibromatosis. Arch Intern Med.
branes as well as the skin. The NF1 gene 1953;91:758.
is mutated in this disease. Similar muco- Kragh LV, Soule EH, Masson JK. Neurofibromatosis
(von Recklinghausen’s disease) of the head and neck;
cutaneous pigmentation is seen in the cosmetic and reconstructive aspects. Plast Reconstr
McCune-Albright syndrome consisting of Surg. 1960;25:565.
polyostotic fibrous dysplasia, endocrinopa- O’Driscoll PM. The oral manifestations of multiple neu-
thy, and skin pigmentations. rofibromatosis. Br J Oral Maxillofac Surg. 1965;3:22.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
MICROSCOPIC FEATURES 1983:206.
White AK, Smith RJ, Bigler CR, Brooke WF, Schauer
Café-au-lait pigmentation is represented PR. Head and neck manifestations of neurofibromato-
by diffuse deposition of melanin granules sis. Laryngoscope. 1986;96:732.
within the basal cell layer. Xavier SP, Ribeiro MC, Sicchieri LG, Brentegani LG,
Lacerda SA. Clinical, microscopic and imaging find-
ings associated to McCune-Albright syndrome: report
DIFFERENTIAL DIAGNOSIS of two cases. Braz Dent J. 2008;19:165-170.
Oral pigmentations of neurofibromatosis
are similar to those of Peutz-Jeghers syn-
drome, racial pigmentation, and Addison’s ADDISON’S DISEASE
disease. The accompanying neurofibroma- Figure 3-35
tous tumefactions on skin differentiate von
Recklinghausen’s disease from the afore- Age: Middle-aged adults
Sex: Slight female predilection
mentioned entities.
CLINICAL FEATURES
TREATMENT Addison’s disease is caused by adrenal cor-
When function is compromised, the neu- tical insufficiency of idiopathic origin or by
rofibromas can be excised. The pigmented cortical replacement as seen in granuloma-
areas have no malignant potential; however, tous infection by tuberculosis or the deep
sarcomatous change in preexisting benign mycoses. Decreased steroid levels stimulate
neurofibromas of von Recklinghausen’s pituitary corticotropin hormone (ACTH)
disease has been reported to occur in as output with increased levels of a melano-
many as 5% of the population with the cyte-stimulating factor. The skin becomes
disease. bronzed or shows brown pigmentation in
FIGURE 3-35
Progressive diffuse pig-
mentation of the mucosa in
regions previously devoid
of such change is sugges-
tive of Addison’s disease.
PMPH_Eversole_Chapter-03.indd 87 1/17/2011 3:28:36 PM
88 Chapter 3
skin folds or over joints. Oral pigmentation
is multifocal or diffuse and macular. Other Additional Reading
symptoms of the disease include weak- Lamey PJ, Carmichael F, Scully C. Oral pigmentation,
ness, hypotension, and cold intolerance. Addison’s disease and the results of screening for adre-
Anorexia, vomiting, and diarrhea are also nocortical insufficiency. Br Dent J. 1985;158:297.
common symptoms. Cushing’s syndrome Wilkins L. The Diagnosis and Treatment of Endocrine
Disorders of Childhood and Adolescence. 3rd ed.
associated with pituitary hyperfunction Springfield, IL: Charles C Thomas; 1965:342.
may also be associated with pigmentation Wood NK, Goaz PW. Differential Diagnosis of Oral
on mucocutaneous surfaces. Lesions. 2nd ed. St Louis, MO: C. V. Mosby;
1980:201.
MICROSCOPIC FEATURES
Pigmentation in Addison’s disease is a man-
ifestation of increased melanin production HEMOCHROMATOSIS
represented by diffuse melanin granule Figure 3-36
deposition in the basal cell layer.
Age: Adults
DIFFERENTIAL DIAGNOSIS Sex: Male predilection
Addisonian pigmentation in the mouth CLINICAL FEATURES
simulates that of racial pigmentation, Peutz- Characterized by excessive deposition of
Jeghers disease, and von Recklinghausen’s iron pigment within tissues, hemochro-
disease. The skin coloration particularly in matosis represents a primary heritable dis-
pressure areas, lack of lesions seen in other ease with a pronounced male predilection
diseases with oral pigmentations, history of or evolves as a secondary acquired defect
recent onset with progressive deepening of accompanying cirrhosis, chronic anemia,
the pigment, and the other clinical manifes- porphyria, excessive dietary iron intake, or
tations require work-up for adrenal cortical a postcaval shunt for portal hypertension.
insufficiency. Classic clinical signs include hepatomegaly,
diabetes, and bronze skin. Pigmentation
TREATMENT of the palate and, less frequently, the gin-
Addison’s disease is managed by the physi- giva is encountered. The pigmentation is
cian. Any underlying cause must be treated, slate-gray to brown with diffuse macu-
and maintenance levels of steroid therapy lar appearance. Oral and skin pigmenta-
are required. tions are attributable to iron deposition
FIGURE 3-36
Blood pigment deposition
in hemochromatosis.
PMPH_Eversole_Chapter-03.indd 88 1/17/2011 3:28:44 PM
Red and Pigmented Lesions 89
as well as melanosis, probably secondary HIV-ASSOCIATED ORAL
to adrenal cortical insufficiency related to PIGMENTATION
pathologic deposition of iron in the adre- Figure 3-37
nal cortex with subsequent elevations in
melanogenic ACTH secretion. Involvement Age: Young adults
of the major and minor salivary glands has Sex: Male predilection
been reported, yet no symptoms or signs
CLINICAL FEATURES
referable to glands are extant.
Progressive pigmentation of the skin and
MICROSCOPIC FEATURES nails is seen among HIV-positive patients
A biopsy of oral mucosa may disclose basi- with opportunistic infections of the adre-
lar melanosis with deposition of brown nal cortex culminating in Addison’s dis-
granular hemosiderin or ferritin pigment ease. In addition, cutaneous pigmentation
within connective tissue and underlying has been attributed to zidovudine therapy.
salivary acini. A Prussian blue iron stain Alternatively, oral pigmentation may occur
is especially useful for demonstrating the in HIV-seropositive individuals who show
nature of the pigment. An inflammatory no alterations in serum steroid or ACTH
reaction is usually not present. levels; furthermore, a drug-related etiology
can be ruled out, because pigmentation of
DIFFERENTIAL DIAGNOSIS this type has been reported among individ-
uals who are not taking any medications.
The macular diffuse slate-gray pigmenta- The lesions are diffuse, grey or brown, and
tion observed in hemochromatosis may generally multifocal. The buccal mucosa,
resemble early laterally spreading mela- gingiva, palate, and tongue are the sites
noma, diffuse tattoo, Addisonian pigmen- more often affected.
tation, and heavy metal ingestion. A his-
tory or documentation of cirrhosis with MICROSCOPIC FEATURES
concomitant diabetes and bronzing of the
skin should arouse suspicion of hemochro- Melanin granules are identifiable in the
matosis. A biopsy with demonstration of basal cell layer along with melanin incon-
diffuse iron deposition, in conjunction with tinence. Melanophages are present in the
the clinical findings and an elevated serum immediate subjacent lamina propria. No
iron level allows for a definitive diagnosis. melanocytic proliferation is evident.
TREATMENT
Hemochromatosis is a metabolic medical
problem with many causes and should be
managed by a physician.
Additional Reading
Dean DH, Hiramoto RN. Submandibular salivary gland
involvement in hemochromatosis. J Oral Pathol Med.
1984;39:197.
Frantzis TG, Sheridan PJ, Reeve CM, Young LL. Oral
manifestations of hemochromatosis. Report of a case.
Oral Surg Oral Med Oral Pathol. 1972;33:186. FIGURE 3-37
Powell LW. Changing concepts in haemochromatosis. Diffuse gray pigmentation of the mucosa in an HIV-
Postgrad Med J. 1970;46:200. seropositive patient.
PMPH_Eversole_Chapter-03.indd 89 1/17/2011 3:28:52 PM
90 Chapter 3
DIFFERENTIAL DIAGNOSIS
HIV-associated pigmentation may closely
resemble the other forms of diffuse pig-
mentation enumerated in this chapter. The
diagnosis can be confirmed only after a
thorough work-up for AIDS and HIV infec-
tion has been undertaken. Among AIDS
patients taking zidovudine, the pigmenta-
tion may be attributable to the medication.
TREATMENT
The lesions are asymptomatic and there is
no specific treatment for the pigmentation FIGURE 3-38
in HIV-positive patients. Heavy metal deposits in the marginal gingiva.
Additional Reading abdominal pain, vomiting, anorexia, tremor,
headaches, and mania.
Chernosky ME, Finley VK. Yellow nail syndrome in
patients with acquired immunodeficiency disease. MICROSCOPIC FEATURES
J Am Acad Dermatol. 1985;13:731.
Esposito R. Hyperpigmentation of skin in patients with Metallic crystals are located within the sub-
AIDS. Br Med J. 1987;294:840. mucosal fibrous connective tissue immedi-
Grover C, Kubba S, Bansal S, Nanda S, Reddy BS. ately subjacent to the oral epithelium.
Pigmentation: a potential cutaneous marker for AIDS?
J Dermatol. 2004;31:756-760.
Langford A, Pohle H-D, Zhang X, Reichart PA. Oral DIFFERENTIAL DIAGNOSIS
hyperpigmentation in HIV-infected patients. Oral
Surg Oral Med Oral Pathol. 1989;67:301.
The limitation of pigment to the gingival
margin is characteristic of heavy metal pig-
mentation. History of metal ingestion con-
HEAVY METAL INGESTION firms the visual clinical impression.
Figure 3-38
TREATMENT
Age: Adults No treatment is necessary for the pigmented
Sex: No predilection
lesions. Once a metallic line has formed,
CLINICAL FEATURES the patient should be considered in a state
Various heavy metals including lead, mer- of metal poisoning and exposure should be
cury, and bismuth may be ingested for immediately terminated. Advanced peri-
medicinal reasons or as an occupational odontal disease may accompany mercury
hazard. (Bismuth, lead, and mercury are poisoning.
the more common metals causing oral pig-
mentation.) The metal becomes deposited
diffusely along the free gingival margin
Additional Reading
that scallops around the cervix of the teeth. Bruggenkate CM, Cordozo EL, Maaskant P, van der
The metallic line is gray. Occasionally, other Waal I. Lead poisoning with pigmentation of the
oral mucosa. Oral Surg Oral Med Oral Pathol. 1975;
mucosal sites show macular pigmentation. 39:747.
Systemic symptoms are often encountered, Dreeson WC. Health of lead-exposed storage battery
particularly in lead poisoning. These include workers. J Invest Hyg Toxicol. 1943;25:60.
PMPH_Eversole_Chapter-03.indd 90 1/17/2011 3:28:54 PM
Red and Pigmented Lesions 91
Gordon NC, Brown S, Khosla VM, Hansen LS. Lead poi- minocycline used in the treatment of acne
soning; a comprehensive review and report of a case. vulgaris is also known to induce foci of pig-
Oral Surg Oral Med Oral Pathol. 1979;47:500.
Robinson HM. An evaluation of the bismuth blue line. mentation of the skin, bone, and thyroid.
J Invest Dermatol. 1952;18:341. Oral involvement is most often encoun-
tered on the palate and facial gingiva. Birth
control pills can be associated with brown
DRUG-INDUCED pigmentation of the facial skin and perioral
PIGMENTATION region (Malasma, Chloasma). Other drugs
Figure 3-39 that may cause pigmentation are tranquil-
izers, phenolphthalein, and estrogens.
Age: No predilection
Sex: Females MICROSCOPIC FEATURES
CLINICAL FEATURES Although not all instances of drug-induced
The antimalarial drugs are used for a vari- oral pigmentations have been evaluated
ety of diseases owing to their anti-inflam- microscopically, some have, and the typical
matory actions. Many of these drugs are finding is basilar melanosis with melanin
known to cause cutaneous, nail bed, and incontinence characterized by free melanin
mucosal pigmentation. Quinoline, hydroxy- in the connective tissue and pigment within
quinoline, and amodiaquine have been used melanophages.
to manage autoimmune diseases, and oral
pigmentation may occur in 10% of patients DIFFERENTIAL DIAGNOSIS
taking the drug on a long-term basis. The The diffuse distribution of pigment in
pigmentation is gray to blue and is usu- drug-induced lesions is similar to that seen
ally located on the hard palate as a diffuse in Addison’s disease and, in the palate, to
macule. The broad-spectrum antibiotic early superficial spreading melanoma. The
FIGURE 3-39
Minocycline pigmenta-
tions in the palate (top),
Chloasma, the mask of
pregnancy, may also be
seen with patients taking
birth control medication.
PMPH_Eversole_Chapter-03.indd 91 1/17/2011 3:28:59 PM
92 Chapter 3
history is, of course, of prime importance, elongate hair-like projections of the filiform
and biopsy is recommended. papillae is termed hairy tongue. The pig-
ment is extensive and probably represents
TREATMENT a combination of food products, tobacco
Withdrawal of the medication is recom- stain, and chromogenic bacteria. A host
mended, although the pigmentation may of causative agents have been considered;
persist for as long as 1 year after cessation however, the etiology remains obscure.
of medication.
MICROSCOPIC FEATURES
Additional Reading The filiform papillae are elongated, with
voluminous amounts of stratified parakera-
Beehner ME, Houston GD, Young JD. Oral pigmen- tin. Food and microbial debris are impacted
tation secondary to minocycline therapy. J Oral between papillae.
Maxillofac Surg. 1986;44:582.
Campbell CH. Pigmentation of the nail beds, palate and DIFFERENTIAL DIAGNOSIS
skin occurring during malarial suppressive therapy
with Camoquin. Med J Aust. 1960;47:956. Pigmentation localized to the dorsum of the
Fendrich P, Brooke RI. An unusual case of oral pigmen- tongue accompanied by elongated papillae
tation. Oral Surg Oral Med Oral Pathol. 1984;58:288. is pathognomonic. Hairy tongue should not
Giansanti JS, Tillery DE, Olansky S. Oral mucosal pig-
mentation resulting from anti-malarial therapy. J Oral
be confused with oral hairy leukoplakia, a
Maxillofac Surg. 1971;31:66. white lesion of the lateral margin among
Lewis DM. Diffuse pigmentation of the palate. J Okla HIV-seropositive individuals.
Dent Assoc. 2009;100:24-25.
TREATMENT
HAIRY TONGUE Podophyllum resin has been used success-
Figure 3-40 fully, painted over the affected area as 1%
solution. After application, the tongue is
Age: Middle-aged adults rinsed thoroughly and the rinse is expecto-
Sex: More common in males rated, as ingested podophyllum can produce
dangerous side effects. Three to five daily
CLINICAL FEATURES
treatments are satisfactory. Many patients
Diffuse brown or black pigment of the dor- respond to brushing of the tongue with a
sal surface of the tongue accompanied by hard-bristle toothbrush. This treatment
FIGURE 3-40
Hairy tongue characterized by elongation of the filiform papillae, which appear matted and pigmented,
brown or black coloration being most common.
PMPH_Eversole_Chapter-03.indd 92 1/17/2011 3:29:16 PM
Red and Pigmented Lesions 93
is preferable initially, with podophyllum Powell FC. Glossodynia and other disorders of the
reserved for cases that fail to resolve with tongue. Dermatol Clin. 1987;5:687.
Standish SM, Moorman WC. Treatment of hairy tongue
mechanical abrasion. with podophyllin resin. J Am Dent Assoc. 1964;
68:535.
Svejda J, Skach M, Plackova A. Hairlike variations of
Additional Reading filiform papillae in the human tongue. Oral Surg Oral
Med Oral Pathol. 1977;43:97.
Farman AG. Hairy tongue (lingua villosa). J Oral Med. Winer LH. Black hairy tongue. Arch Dermatol.
1977;32:85. 1958;77:97.
PMPH_Eversole_Chapter-03.indd 93 1/17/2011 3:29:28 PM
a b c
Normal mucosa Ulceration Granulomatous ulceration
d e f
Carcinoma with ulceration Fissure Oroantral fistula
g h i
Blind fistula Infectious sinus tract Osseous destructive ulceration
Ulcers, Fistulae, and Sinuses
PMPH_Eversole_Chapter-04.indd 94 1/20/2011 2:15:08 PM
Oral Ulcerations and
Fistulae 4
Recurrent and Multiple Perioral and Commissural
Ulcerations 96 Ulcerations and Fistulae 117
APHTHOUS STOMATITIS 96 COMMISSURAL PITS 117
MAJOR SCARRING APHTHOUS CONGENITAL LIP PITS 118
STOMATITIS 97 ANGULAR CHEILITIS 119
BEHÇET’S SYNDROME 99 CARCINOMA*
GLUTEN ENTEROPATHY 100
AGRANULOCYTOSIS AND Oral Fistulae 120
IMMUNOSUPPRESSION 100
PERIAPICAL ABSCESS AND
CYCLIC NEUTROPENIA 101
OSTEOMYELITIS 120
UREMIC STOMATITIS 102
PERIODONTAL ABSCESS 121
VIRAL VESICULAR STOMATITIS 103
ACTINOMYCOSIS 122
ACUTE NECROTIZING ULCERATIVE
OROANTRAL FISTULA 122
GINGIVITIS 105
SOFT TISSUE ABSCESS 123
ACUTE STREPTOCOCCAL/
STAPHYLOCOCCAL STOMATITIS 106 DEVELOPMENTAL ORAL SINUSES 124
CHRONIC ULCERATIVE FISSURED (SCROTAL) TONGUE 125
STOMATITIS 107
GONOCOCCAL STOMATITIS 107
Necrotic and Osseous
HIV PERIODONTITIS AND ORAL
Destructive Lesions 126
ULCERATIONS 108 FACTITIAL INJURY AND TRAUMA 126
WEGENER’S GRANULOMATOSIS 127
Focal Ulcerations 109 EXTRANODAL NK/T-CELL
LYMPHOMA 128
TRAUMATIC ULCER 109
TERTIARY SYPHILIS 129
TRAUMATIC ULCERATIVE
OSTEORADIONECROSIS 130
GRANULOMA WITH STROMAL
EOSINOPHILIA 111 MUCORMYCOSIS 131
ATYPICAL HISTIOCYTIC INVASIVE FUNGI**
GRANULOMA 112 ANTRAL CARCINOMA 132
NECROTIZING SIALOMETAPLASIA 113 BISPHOSPHONATE-RELATED
SPECIFIC GRANULOMATOUS OSTEONECROSIS OF THE JAWS 133
ULCER 114 *See Carcinoma under focal ulcers
CHANCRE (PRIMARY SYPHILIS) 115 **See above Specific Granulomatous
SQUAMOUS CELL CARCINOMA 116 Ulcer
PMPH_Eversole_Chapter-04.indd 95 1/20/2011 2:15:13 PM
Ulcerative lesions of the oral cavity are com- The traumatic ulcer from biting or den-
mon. Assessment of the nature of oral ulcers ture irritation is the most common focal oral
requires a thorough history of the present ill- ulceration. Carcinoma, tuberculous, and
ness. Certain ulcerations occur in multiples, mycotic ulcers are potentially lethal diseases.
and many are recurrent. Signs and symp- Common perioral ulcerations include
toms relative to general health with review angular cheilitis and cancer, the latter being
of organ systems will point to a diagnosis of most serious.
certain systematic problems that can mani- Parulis of pulpal or periodontal origin
fest oral ulceration. The nature of the ulcer is the most common form of oral fistula. All
itself is vitally important when a definitive necrotic and osseous destructive lesions
diagnosis is pursued. One should always with drainage are serious disorders.
remember that oral vesiculobullous dis-
eases are subject to trauma, with loss of the
characteristic vesicular nature of the lesions
clinically. For this reason, the patient should Recurrent and Multiple
be questioned concerning the nature of the Ulcerations
lesions at their outset, and attempts should
be made to search for an intact vesicle. If APHTHOUS STOMATITIS
the ulcerations prove to be, or to have been,
Figure 4-1
vesiculobullous, refer to the next chapter
for discussion of vesiculobullous diseases. Age: Teenagers and young adults
In this section, only diseases that begin as Sex: No predilection
ulcers are considered.
CLINICAL FEATURES
Draining tracts or fistulae are included
in this chapter because, clinically, they Aphthous ulcers may occur singly or in
may appear as areas of ulceration. By defi- crops. The lesions are shallow and flat with
nition, a fistula represents an epithelial- a central white fibrinous pseudomembrane
lined tract connecting two body cavities, surrounded by an erythematous halo.
whereas a sinus is a drainage tract asso- Commonly known as canker sores, these
ciated with an infection. Many clinicians lesions are prone to appear during times of
do not make this distinction and refer to stress; frequency of recurrence and multiplic-
all tracts as fistulae. This is the context ity are extremely varied. They are quite pain-
in which the term fistula is used here. ful, remain for 10 to 14 days, and then sponta-
Palpation of the underlying tissues usu- neously regress. They occur most often on the
ally elicits flow of purulent exudate from oral soft tissues that are not bound to bone, yet
an area of tissue breakdown suspected to occasionally the gingiva is involved. Aphthae
represent a fistula. Insertion of a probe or can be small, punctate, and present in great
gutta-percha point will also aid in detect- numbers; lesions of this nature have been
ing a tract. The exudate may be subjected referred to as herpetiform ulcers, despite the
to culture and sensitivity tests to identify fact that they are not caused by herpesvirus.
specific infectious agents. Aphthous ulcers are occasionally a concomi-
The most common recurring oral tant of chronic inflammatory bowel disease,
ulcerations are aphthae, whereas the most including both ulcerative colitis and regional
frequently encountered nonrecurring multi- enteritis. L-form streptococci have been iso-
focal ulcerative disease is acute necrotizing lated from the lesions, and cell-mediated
ulcerative gingivitis (ANUG). Potentially immune responses to oral epithelium have
lethal diseases with multifocal ulcerations been demonstrated, whereas others have
are agranulocytosis and uremia. found evidence for an immunoregulatory
PMPH_Eversole_Chapter-04.indd 96 1/20/2011 2:15:13 PM
Oral Ulcerations and Fistulae 97
FIGURE 4-1
Aphthous ulcers of the oral mucosa—oval, shallow, and displaying an erythematous halo.
defect among T lymphocytes. Although a applicator impregnated with silver nitrate for
specific etiology has not been definitively a few seconds, cauterizing the central core of
identified, food allergens may be responsible the ulcer. Tetracycline oral suspension may
in some instances. invoke early involution. Selective elimination
of suspected foods can be attempted.
MICROSCOPIC FEATURES
The epithelium is ulcerated, with an eosino-
philic fibrinous coagulum on the surface. The Additional Reading
connective tissue is infiltrated with mononu-
clear cells, chiefly lymphocytes, and the reac- Akintoye SO, Greenberg MS. Recurrent aphthous stom-
tion is superficial. atitis. Dent Clin North Am. 2005;49:31-47, vii-viii.
Antoon JW, Miller RL. Aphthous ulcers—a review of
the literature on etiology, pathogenesis, diagnosis and
DIFFERENTIAL DIAGNOSIS treatment. J Am Dent Assoc. 1980;101:803.
Recurrent aphthous stomatitis must be differ- Graykowski EA, Barile MF, Lee WB, Stanley HR Jr.
Recurrent aphthous stomatitis: clinical, therapeutic,
entiated from cyclic neutropenia by obtaining histopathologic and hypersensitivity aspects. JAMA.
periodic blood counts when the recurrence of 1966;196:637-644.
lesions is periodic and regular. Behçet’s syn- Lehner T. Pathology of recurrent oral ulceration and oral
drome should be investigated because oral ulceration in Behçet’s syndrome. Light, electron and
fluorescence microscopy. J Pathol. 1969;97:548.
lesions in that disease are indistinguishable Savage NW, Seymour GJ, Kruger BJ. Expression of class
from aphthae. I and class II major histocompatibility complex anti-
Viral infection can be ruled out if no gens on epithelial cells in recurrent aphthous stomati-
history of vesicle formation can be obtained. tis. J Oral Pathol Med. 1986;15:191.
With the exception of palatal secondary her-
pesvirus infection, herpes of the oral soft
tissues does not occur on a recurrent basis MAJOR SCARRING APHTHOUS
as do aphthae. Also, herpesvirus-induced STOMATITIS
lesions tend to cluster in geographic groups; Figure 4-2
aphthae show no such tendency, being ran-
domly distributed. Age: Young adults
Sex: No predilection
TREATMENT CLINICAL FEATURES
Single lesions or instances in which only a few Major aphthae, also known as periadeni-
ulcers appear can be treated by applying a wet tis mucosae necrotica recurrens or Sutton’s
PMPH_Eversole_Chapter-04.indd 97 1/20/2011 2:15:13 PM
98 Chapter 4
FIGURE 4-2
Major aphthous ulcers—extensive, often showing irregular margins, and with inflamed surrounding
mucosa. They leave depressed scars after healing.
disease, are similar in appearance to minor TREATMENT
aphthae. The ulcers, however, are more deep- Initial attempts to control the severity and
seated, exceed 0.5 cm (indeed, they may be distress of major aphthae include the use
1-2 centimeters in diameter), and like minor of gauze compresses soaked in tetracycline
aphthae, soft tissues not bound to bone are oral suspension and applied three times
predisposed to them. The faucial pillars and daily. A palliative mouth rinse such as an
oropharynx are often the initial sites of ulcer- antihistamine oral suspension mixed with
ation. After resolution, which may require equal parts of Kaopectate often minimizes
1 to 4 weeks, healing with scar formation is pain. If tetracycline is ineffective, predni-
seen. Remissions are short, with a new crop of sone (40 mg daily in divided doses for 10
ulcers appearing shortly after the older lesions days) usually induces regression of ulcer-
resolve. Most patients are tense and anxious, ations. These treatment regimens must be
and the lesions are extremely painful. The repeated when new lesions periodically
cause is unknown, but mounting evidence appear.
points to an immune defect. Both immuno-
globulin and cell-mediated responses to oral
epithelium have been demonstrated. Additional Reading
MICROSCOPIC FEATURES Chung JY, Ramos-Caro FA, Ford MJ, Mullins D.
Recurrent scarring ulcers of the oral mucosa.
The epithelium is ulcerated with an eosino- Sutton disease (periadenitis mucosa necrotica
philic fibrin surface. A mononuclear inflam- recurrens). Arch Dermatol. 1997;133:1162-1163,
matory cell infiltrate composed predomi- 1165-1166.
Hjørting-Hansen E, Siemssen SO. Stomatitis
nantly of lymphocytes extends deeply into aphthosa recurrens cicatricians. Odontol Tidskr.
the submucosa. 1961;69:294.
Lehner T. Pathology of recurrent oral ulceration and
DIFFERENTIAL DIAGNOSIS oral ulceration in Behçet’s syndrome. Light,
electron and fluorescence microscopy. J Pathol.
Major aphthae are differentiated from minor 1969;97:548.
aphthous stomatitis on the basis of size and Monoteleone L. Periadenitis mucosa necrotica
recurrens. Oral Surg Oral Med Oral Pathol.
tendency to heal with scarring. Cyclic neutro-
1967;23:586.
penia and agranulocytosis may be ruled out by Sutton RL Sr. Periadenitis mucosa necrotica recurrens.
obtaining a leukocyte and differential count. J Cutan Dis. 1911;29:65.
PMPH_Eversole_Chapter-04.indd 98 1/20/2011 2:15:25 PM
Oral Ulcerations and Fistulae 99
BEHÇET’S SYNDROME and scrotum; in females, the vulva is
Figure 4-3 frequently affected. Gastrointestinal
complaints such as diarrhea and pain
Age: Young and middle-aged adults are frequently encountered, as are joint
Sex: Significant male predilection pain and discomfort. Cutaneous macu-
CLINICAL FEATURES lar, papular, and plaque lesions are also
encountered in some patients.
One of the muco-oculocutaneous syn-
dromes, Behçet’s disease represents an MICROSCOPIC FEATURES
immunopathic disorder characterized
by oral aphthous ulcerations, uveocon- The epithelium shows ulceration, being
junctivitis, and genital ulceration. The replaced by an eosinophilic coagulum. The
disease is more often encountered in the connective tissue is infiltrated with mono-
Middle East, most patients being HLA- nuclear cells, chiefly lymphocytes.
B51 and HLA-DRw52 antigen positive.
L-form bacteria have been implicated DIFFERENTIAL DIAGNOSIS
in its pathogenesis; yet recent stud- The extraoral signs are sufficient to dif-
ies have detected circulating immune ferentiate Behçet’s syndrome from simple
complexes with herpesvirus specific- aphthae. When the dominant features are
ity. Not all components of the syndrome arthritis, dermatitis of the palms and soles,
triad are present at any given time. The conjunctivitis, and genital ulceration, the
oral ulcerations are small with a white disease is more correctly termed Reiter’s
pseudomembrane and erythematous syndrome. Both Behçet’s and Reiter’s syn-
halo, indistinguishable from ordinary dromes are probably variants of the same
aphthae. The eye lesions consist of recur- immunopathologic process.
rent conjunctivitis, ulceration, uveitis,
and hypopyon, with visual damage TREATMENT
being a common sequela. In males, the
genital lesions are located on the penis Systemic steroids are required for control.
Because of the multiplicity of defects, these
patients should be managed by a general
physician or dermatologist.
Additional Reading
Chae EJ, Do KH, Seo JB, et al. Radiologic and clini-
cal findings of Behçet disease: comprehensive
review of multisystemic involvement. Radiographics.
2008;28:e31.
Chajek T, Fainaru M. Behçet’s disease. Report of 41
cases and a review of the literature. Medicine.
1975;54:179.
Jorizzo JL. Behçet’s disease. Arch Dermatol.
1986;122:556.
Mason RM, Barns CG. Behçet’s syndrome with arthritis.
Ann Rheum Dis. 1969;28:95.
FIGURE 4-3 Rapidis AD, Langdon JD, Patel MF. Recurrent oral and
Oral ulcerations in Behçet’s syndrome, resembling oculogenital ulcerations (Behçet’s syndrome). Oral
aphthae. Surg Oral Med Oral Pathol. 1976;41:457.
PMPH_Eversole_Chapter-04.indd 99 1/20/2011 2:15:35 PM
100 Chapter 4
GLUTEN ENTEROPATHY DIFFERENTIAL DIAGNOSIS
Figure 4-4 Because the lesions are essentially identical
to those of recurrent aphthae, a consider-
Age: Young adults, adolescents
ation of celiac disease should be explored in
Sex: No predilection
those patients with pale buoyant stools and
CLINICAL FEATURES episodic upset bowel symptoms.
Gluten enteropathy is one of the intestinal
TREATMENT
malabsorption syndromes whereby lipids
are not readily absorbed to transport mol- A gliadin-free diet should be instituted.
ecules resulting, therefore, in steatorrhea.
Malabsorption of the fat-soluble vitamins
may occur with mild symptoms of hypovita- Additional Reading
minosis A, D, and K, the latter of which may
Campisi G, Di Liberto C, Carroccio A, et al. Coeliac
predispose such patients to a hemorrhagic
disease: oral ulcer prevalence, assessment of risk and
diathesis. Some patients complain of mouth association with gluten-free diet in children. Dig Liver
sores and, clinically, the lesions resemble Dis. 2008;40:104-107.
those encountered in recurrent aphthous Ferguson MM, Wray D, Carmichael HA, Russell RI,
ulcerations. These patients have circulat- Lee FD. Coeliac disease associated with recurrent
aphthae. Gut. 1980;2:223.
ing antigliadin antibodies. The recurring Veloso FT, Saleiro JV. Small-bowel changes in recur-
ulcerations subside once the patient follows rent ulceration of the mouth. Hepatogastroenterology.
a gluten-free diet. 1987;34:36.
Wray D. Gluten-sensitive recurrent aphthous stomatitis.
MICROSCOPIC FEATURES Dig Dis Sci. 1981;26:737.
The histologic changes are essentially iden-
tical to those of aphthous stomatitis. AGRANULOCYTOSIS AND
IMMUNOSUPPRESSION
Figure 4-5
Age: No predilection
Sex: No predilection
CLINICAL FEATURES
A deficiency in circulating blood granulo-
cytes may represent a primary idiopathic
disorder or may be secondary to bone mar-
row suppression by certain drugs that are
cytotoxic for hematopoietic tissue. Cancer
patients receiving antitumor chemo-
therapy are most often affected: however,
organ transplantation recipients receiving
immunosuppressive medications may also
develop oral ulcerations. Because the gran-
ulocytic series are vital to defense against
infection, patients with agranulocytosis
are extremely prone to develop infections,
FIGURE 4-4 pulmonary bacterial infections in particu-
Aphthous-like lesions in a patient with gluten sensitivity. lar. Death from uncontrollable infection is
PMPH_Eversole_Chapter-04.indd 100 1/20/2011 2:15:38 PM
Oral Ulcerations and Fistulae 101
of cellular defense mechanisms. If drug
induced, it is a sign of dangerous toxicity
levels and the dose of medication should
be decreased immediately; otherwise, the
patient is open to rapidly progressive infec-
tion. If no cause can be determined, the dis-
ease is of the idiopathic primary type, and
referral to a hematologist is essential.
Additional Reading
FIGURE 4-5 Andrews RG, Benjamin S, Shore N, Canter S. Chronic
Agranulocytic ulcers, flat with a necrotic center. benign neutropenia of childhood with associated oral
manifestations. Oral Surg Oral Med Oral Pathol.
1965;20:719.
common. The leukocyte count is usually Awbrey JJ, Hibbard ED. Congenital agranulocytosis.
Oral Surg Oral Med Oral Pathol. 1973;35:526.
under 2500/mm3, and the differential count
Copete MA, Sheridan DP. Large granular lymphocyte
shows severely depressed numbers of neu- leukemia and its association with oral neutropenic
trophilic granulocytes. The oral ulcers are ulcerations: a case report. Oral Surg Oral Med Oral
oval and variable in size. In addition, gin- Pathol Oral Radiol Endod. 2000;90:474-477.
givitis or periodontitis is a frequent finding Kander R, Mauer AM. Neutropenias of childhood.
J Pediatr. 1966;69:147.
with ulcerations located on the attached Ohishi M, Oobu K, Miyanoshita Y, Yamaguchi K. Acute
gingivae. Pain is a feature of these lesions. gingival necrosis caused by drug-induced agranulocy-
tosis. Oral Surg Oral Med Oral Pathol. 1988;66:194.
MICROSCOPIC FEATURES
The microscopic changes are pathogno-
CYCLIC NEUTROPENIA
monic. The epithelium is lacking, and there
is an eosinophilic fibrin surface. Underlying Figure 4-6
the pseudomembrane and imperceptibly Age: Childhood onset
merging with it is a zone of amorphous Sex: No predilection
necrotic tissue, which is strikingly devoid
of neutrophils. Indeed, other inflammatory CLINICAL FEATURES
cells, including round cells, are present in Oral ulcerations that are multifocal, are
only limited numbers, probably because the located primarily on movable mucosa,
lesions are detected and taken for biopsy appear every 20 to 25 days, persist for 5 to
early in their course. 8 days, and reappear on a periodic basis
probably represent oral manifestations of
DIFFERENTIAL DIAGNOSIS cyclic neutropenia. The ulcers are shallow,
Agranulocytic ulcers may appear identical may show an erythematous halo, and vary
to aphthae, major aphthae, and cyclic neu- in size. Coexistent severe premature peri-
tropenia. Differentiation from these entities odontal lesions are common. The gingival
requires biopsy and a complete blood count papillae are erythematous and edematous,
when the patient reports no history of cyto- and may be ulcerated. Vertical alveolar bone
toxic drug intake. loss with pocket formation is encountered in
many regions throughout both dental arches.
TREATMENT Otitis media, joint pain, and headache are
Oral ulceration in agranulocytosis is an often present during the neutropenic phase.
ominous sign denoting severe depression The leukocyte count is depressed, as are the
PMPH_Eversole_Chapter-04.indd 101 1/20/2011 2:15:45 PM
102 Chapter 4
FIGURE 4-6
Cyclic neutropenia, character-
ized by premature periodon-
titis and focal ulcerations that
appear every 20 or 25 days.
neutrophilic granulocytes during the period TREATMENT
of ulceration. Throughout the course of the Patients with cyclic neutropenia require
20-day remission, the hemogram is within management by a hematologist. Although
normal limits. During the agranulocytic the periodontal prognosis is poor, peri-
phase, susceptibility to infection is a com- odontal therapy is required for its own sake
plication. The cause of this mysterious par- as well as to eliminate a focus of infection.
oxysmal hematologic disorder is unknown
but is related to a maturation arrest in the
bone marrow with mutations in ELA2, gene
that encodes neutrophil granule protease,
Additional Reading
neutrophil elastase. Cohen L. Recurrent oral ulceration and cutaneous infec-
tions associated with cyclical neutropenia. Dental
MICROSCOPIC FEATURES Pract. 1966;16:97.
Gorlin RJ, Chandhry AP. The oral manifestations of cyclic
The ulcers are typically agranulocytic. (periodic) neutropenia. Arch Dermatol. 1960;82:344.
The epithelium is lacking, and there is an Horwitz MS, Duan Z, Korkmaz B, Lee HH, Mealiffe
ME, Salipante SJ. Neutrophil elastase in cyclic and
eosinophilic necrotic zone. The submucosa severe congenital neutropenia. Blood. 2007;109:1817-
is characterized by a paucity of inflamma- 1824.
tory cells in general and a complete lack of Rezaei N, Farhoudi A, Ramyar A, et al. Congenital neu-
neutrophils. tropenia and primary immunodeficiency disorders: a
survey of 26 Iranian patients. J Pediatr Hematol Oncol.
2005;27:351-356.
DIFFERENTIAL DIAGNOSIS Scully C, MacFadyen E, Campbell A. Oral manifesta-
The ulcers of cyclic neutropenia are indis- tions in cyclic neutropenia. Br J Oral Maxillofac Surg.
1982;20:96.
tinguishable from aphthae, major aphthae,
agranulocytosis, and Behçet’s syndrome.
The consistent cyclic nature of the lesions UREMIC STOMATITIS
is highly suggestive of cyclic neutropenia;
Figure 4-7
however, recurrent aphthae often show this
pattern in the absence of an altered hemo- Age: Young and middle-aged adults
gram. The presence of premature periodon- Sex: No predilection
tal lesions is another factor in favor of a diag-
CLINICAL FEATURES
nosis of cyclic neutropenia. The diagnosis
can be established by obtaining leukocyte Patients suffering end-stage renal disease
and differential blood counts every 3 days with elevated creatinine or blood urea
during periods of affliction and regression. nitrogen and electrolyte derangements
PMPH_Eversole_Chapter-04.indd 102 1/20/2011 2:15:49 PM
Oral Ulcerations and Fistulae 103
recurrent and may clinically simulate agran-
ulocytic ulcers. Similar appearing ulcers
may be encountered among renal transplant
recipients (as well as other organ transplan-
tations); these lesions are generally attribut-
able to immunosuppressive drug therapy.
TREATMENT
Uremia may be secondary to pyelonephritis,
glomerulonephritis, diabetic glomeruloscle-
rosis, or lupus erythematosus. Management
lies with a physician.
The oral ulcers, if painful, may be
treated by prescribing a palliative oral rinse
such as an antihistaminic oral suspension
50:50 with Kaopectate.
FIGURE 4-7
Diffuse stomatitis with zones of ulceration mani-
fested in renal failure.
Additional Reading
Halazonetis J, Harley A. Uremic stomatitis. Oral Surg
Oral Med Oral Pathol. 1967;23:572.
occasionally develop oral ulcerations. Hamid MJ, Dummer CD, Pinto LS. Systemic condi-
Uremic oral ulcers vary in size, are irregu- tions, oral findings and dental management of chronic
renal failure patients: general considerations and case
lar in shape, and are usually shallow. They report. Braz Dent J. 2006;17:166-170.
connote a poor prognosis, with death being Newell GB, Stone OJ. Irritant contact stomatitis in
imminent unless renal dialysis or kidney chronic renal failure. Arch Dermatol. 1974;109:53.
transplant is performed. The cause for Tyldesley WR, Rotter E, Sells RA. Oral lesions in
renal transplant patients. J Oral Pathol Med.
ulceration is unknown, yet one suggestion 1979;8:53.
is that it is the consequence of strongly alka-
line saliva, a result of ammonia formation
from retained urea secreted in the saliva. VIRAL VESICULAR
In other patients, the use of orally admin- STOMATITIS
istered alkaline solutions used to alleviate
Figure 4-8
metabolic acidosis may cause ulceration.
MICROSCOPIC FEATURES Age: Children and young adults
Sex: No predilection
The epithelium is lacking, having been
replaced by an eosinophilic coagulum with CLINICAL FEATURES
a subjacent inflammatory cell infiltrate. Viral infections that manifest oral ulcer-
ations do so secondarily, in that the early
DIFFERENTIAL DIAGNOSIS lesion is vesicular and, under masticatory
Patients with uremic ulcers manifest the trauma, the vesicles rupture and yield areas
clinical signs of the uremic syndrome: an of ulceration. Herpes virus, varicella-zoster
ammonia odor on the breath, weight loss, virus, and coxsackie viruses are the com-
anemia, cardiac arrhythmias, and, in many mon infectious agents. The specific features
instances, secondary hyperparathyroid- encountered in oral viral infections are enu-
ism. The oral ulcers are chronic rather than merated in the section on vesiculobullous
PMPH_Eversole_Chapter-04.indd 103 1/20/2011 2:16:09 PM
104 Chapter 4
FIGURE 4-8
Viral stomatitides. Vesicles
form and rupture within 24
hours, yielding shallow ulcers
as seen in these examples
recurrent intraoral her-
pes, primary herpetic gingi-
vostomatitis, shingles, and
cytomegalovirus.
and desquamative lesions. In general terms, and recurrent palatal herpes, which is uni-
oral ulcers that develop from viral infection laterally localized to the palatal gingiva
are shallow, small, multifocal, and painful. as microvesicles that ulcerate, leaving tiny
A constant finding is elevation in tempera- pinpoint ulcerative foci.
ture during primary infection.
TREATMENT
MICROSCOPIC FEATURES
Acyclovir analogues may result in early
The classic cytologic changes unique to resolution of herpetic lesions. Soft diet,
oral vesicular eruptions are usually not liquids, analgesic/antipyretic drugs, and a
apparent after the vesicles rupture to leave soothing oral rinse consisting of an antihis-
ulcers. The ulcerated zones may show bal- taminic oral suspension with equal parts of
looning degeneration of spinous cells in Kaopectate are recommended.
the marginal epithelium. Usually only an
area of ulceration with a subacute inflam-
matory cell infiltrate is seen, with evidence
of regenerating epithelium on the surface.
Additional Reading
Eversole LR. Clinical virology of the head and neck.
DIFFERENTIAL DIAGNOSIS Comp Contin Educ Dent. 1985;6:298.
Lennette EH, Magoffin RL. Virologic and immunologic
Viral ulcerations are most frequently con- aspects of major oral ulcerations. J Am Dent Assoc.
fused with aphthous stomatitis. If the oral 1973;87:1055.
ulcers are recurrent, then viral ulceration McCullough MJ, Savage NW. Oral viral infections and
the therapeutic use of antiviral agents in dentistry.
can be eliminated as a possibility; the Aust Dent J. 2005;50(4 suppl 2): S31-S35.
viruses causing oral infection do so only Ship II. Virus and viral-like diseases of the mouth.
as a primary disease and do not manifest Postgrad Med. 1965;38:499.
intraoral recurrent infections. Weathers DR, Griffin JW. Intraoral ulcerations of
recurrent herpes simplex and recurrent aphthae:
Exceptions to this maxim are recur- two distinct clinical entities. J Am Dent Assoc.
rent herpes labialis, which is not intraoral, 1970;81:81.
PMPH_Eversole_Chapter-04.indd 104 1/20/2011 2:16:14 PM
Oral Ulcerations and Fistulae 105
ACUTE NECROTIZING Bacterial colonies populate the necrotic
ULCERATIVE GINGIVITIS surface.
Figure 4-9
DIFFERENTIAL DIAGNOSIS
Age: Teenagers and young adults Localization to gingival papillae and pres-
Sex: Male predilection
ence of a foul odor are essentially diagnos-
CLINICAL FEATURES tic. These features differentiate this disease
ANUG, Vincent’s disease, manifests multi- from the other ulcerative disorders outlined
focal pseudomembranous ulcerations local- in this section.
ized primarily to the gingival interdental
papillae. The papillae are blunted, with TREATMENT
necrotic craters showing a marginal zone In severe cases, systemic antibiotics (e.g.,
of erythema. Pain is a chief complaint, and penicillin 250 mg 4 times daily for 1 week)
halitosis is a constant feature. Uncommonly, are recommended. Less severe forms
ulcerations extend beyond the gingiva to can be managed by 3% hydrogen perox-
include the palate and mucobuccal fold, ide rinses. Two to 3 days after therapy is
where they may be extensive. The infectious instituted, dental prophylaxis should be
microorganisms associated with ANUG performed.
are anaerobic fusiform and spirochetal
bacteria that are saprophytic members of
normal oral flora. They proliferate and may
be considered pathogenic when the patient Additional Reading
is under undue stress. In this context, it is Carter WJ, Ball DM. Results of a three-year study of
not surprising that the disease often occurs Vincent’s infection at the Great Lakes Naval Dental
among college students during final exami- Department. J Periodontol. 1953;24:187.
Coslet RS. The psychological factor in the
nation periods. It is also encountered in etiology of acute necrotizing gingivitis. Dent Hyg.
malnutrition. 1979;53:257.
Folayan MO. The epidemiology, etiology, and pathophys-
MICROSCOPIC FEATURES iology of acute necrotizing ulcerative gingivitis asso-
ciated with malnutrition. J Contemp Dent Pract.
Smears and dark-field scrapings disclose the 2004;5:28-41.
presence of fusiform and mobile spirochete Johnson BD, Engel D. Acute necrotizing ulcerative gin-
bacterial forms. Tissue sections show non- givitis: a review of diagnosis, etiology and treatment.
J Periodontol. 1986;57:141.
specific ulceration with superficial necrosis Schluger S. Necrotizing ulcerative gingivitis in the Army.
and a subacute inflammatory cell infiltrate. J Am Dent Assoc. 1949;38:174.
FIGURE 4-9
Gingivitis accompanied by
crateriform ulcers with
blunting of the papillae. The
multifocal ulcers of acute
necrotizing ulcerative gin-
givitis are generally con-
fined to the interdental
papillae.
PMPH_Eversole_Chapter-04.indd 105 1/20/2011 2:16:38 PM
106 Chapter 4
ACUTE STREPTOCOCCAL/
STAPHYLOCOCCAL
STOMATITIS
Figure 4-10
Age: Young adults
Sex: No predilection
CLINICAL FEATURES
Acute streptococcal or staphylococcal stoma-
titis is a rare disease characterized by gingi-
val, oral mucosal, and tonsillar inflammation FIGURE 4-10
associated with cervical lymphadenopathy Child with diffuse ulcer and pseudomembrane in
and occurring in the context of immuno- acute streptococcal stomatitis. (Courtesy of Dr. D.
suppression. The disease often represents Adams.)
a secondary bacterial infection following
primary herpetic gingivostomatitis. There streptococcal gingivitis fails to show this
is an increased risk for streptococcal septi- feature. Most of the other ulcerative dis-
cemia among patients with post–bone mar- eases are not accompanied by fever and
row transplant myelosuppression and oral lymphadenopathy. Definitive diagnosis
mucositis implying that streptococci are rests with a positive culture for β-hemolytic
harbored by the oral lesions. The lesions are streptococci with elevated antistreptolysin
ulcerative with an erythematous base and O titers in the convalescent period.
involve both fixed and movable mucosa.
The gingiva is boggy with diffuse erythema; TREATMENT
the ulcers do not confine themselves to the
intradental papilla, nor are they restricted Acute streptococcal stomatitis is managed by
only to marginal gingiva. Fetid odor is not prescribing penicillin or synthetic penicillin
a feature. β-Hemolytic streptococci can be analogs 250 mg every 6 hours for 2 weeks.
cultured, and antistreptolysin O titers are A palliative oral mouth rinse or tetracycline
elevated during the convalescent period. oral suspension is also recommended.
The white blood cell count is elevated with a
neutrophilic leukocytosis. Additional Reading
MICROSCOPIC FEATURES Blake GC, Trott JR. Acute streptococcal gingivitis. Dent
Pract. 1959;10:43.
The mucosa is ulcerated with a pseudomem- Littner MM, Dayan D, Kaffe I, et al. Acute streptococ-
branous fibrin surface. The ulcer bed is rep- cal gingivostomatitis: report of five cases and review
of the literature. Oral Surg Oral Med Oral Pathol.
resented by granulation tissue exhibiting 1982;53:144.
a nonspecific subacute inflammatory cell Ruescher TJ, Sodeifi A, Scrivani SJ, Kaban LB, Sonis
infiltrate. ST. The impact of mucositis on alpha-hemolytic strep-
tococcal infection in patients undergoing autologous
DIFFERENTIAL DIAGNOSIS bone marrow transplantation for hematologic malig-
nancies. Cancer. 1998;82:2275-2281.
Viral vesicular stomatitis, particularly pri- Shouval DS, Bilavsky E, Avitzur Y, Shapiro R, Amir J.
mary herpetic gingivostomatitis, exhibits Staphylococcus aureus bacteremia complicating herpes
simplex virus type 1 stomatitis: case report and review
almost identical clinical features. Whereas of the literature. J Periodontol. 2008;79:376-378.
primary herpes typically manifests a mar- Tyldesley WR. Infections of the oral mucosa. Br Dent J.
ginal gingivitis in addition to oral ulcers, 1973;20:449.
PMPH_Eversole_Chapter-04.indd 106 1/20/2011 2:16:44 PM
Oral Ulcerations and Fistulae 107
CHRONIC ULCERATIVE recalcitrant to topical steroids. Short-term
STOMATITIS systemic corticosteroid therapy may or may
Figure 4-11 not be effective. Hydroxychloroquine ther-
apy may be prescribed.
Age: Adults
Sex: No predilection
CLINICAL FEATURES
Additional Reading
Church LF Jr, Schosser RH. Chronic ulcerative stoma-
Chronic ulcerative stomatitis is a rare lichenoid titis associated with stratified epithelial specific anti-
disease of oral mucosa that is characterized nuclear antibodies. A case report of a newly described
by the presence of antinuclear antibodies disease entity. Oral Surg Oral Med Oral Pathol.
reactive with stratified squamous epithelial 1992;73:579-582.
Islam MN, Cohen DM, Ojha J, et al. Chronic ulcerative
nuclei. Clinically, the lesions are painful white, stomatitis: diagnostic and management challenges—four
red, ulcerative, and desquamative, appearing new cases and review of literature. Oral Surg Oral Med
primarily on the tongue and buccal mucosa. Oral Pathol Oral Radiol Endod. 2007;104: 194-203.
Solomon LW. Chronic ulcerative stomatitis. Oral Dis.
2008;14:383-389.
MICROSCOPIC FEATURES Solomon LW, Neiders ME, Zwick MG, Kirkwood KL,
A chronic lymphocytic interface mucosi- Kumar V. Autoimmunity to deltaNp63alpha in chronic
ulcerative stomatitis. J Dent Res. 2007;86:826-831.
tis is evident, resembling ordinary lichen Solomon LW, Stark PC, Winter L, Kumar V, Sinha S.
planus. On immunoflourescent testing, ELISA test for p63 antibodies in chronic ulcerative
fibrinogen may be localized along the base- stomatitis. Oral Dis. 2010;16:151-155.
ment membrane, but the singular feature is
the presence of IgG and/or IgM antinuclear GONOCOCCAL STOMATITIS
keratinocyte antibodies identified in the
Figure 4-12
lower strata keratinocytes.
Age: Young adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Lichen planus and lichenoid eruptions are CLINICAL FEATURES
the primary considerations in the differen-
Whereas gonorrhea is a common urethral
tial diagnosis.
infection, localization in the oral cavity and
TREATMENT
oropharynx is rare. When the oral mucosa is
infected, irregular ulcerations ranging from 0.5
The significance of the antinuclear antibod- to 2.0 cm are observed and are accompanied
ies is unknown and not related to lupus by a perilesional zone of erythema. Tonsillar
erythematosus. The condition is often and pharyngeal involvement is characterized
FIGURE 4-11
Red and ulcerative lesions
in chronic ulcerative
stomatitis associated with
stratified epithelial specific
antinuclear antibodies.
PMPH_Eversole_Chapter-04.indd 107 1/20/2011 2:16:47 PM
108 Chapter 4
infection. Penicillin-resistant cases should be
evaluated by culture and sensitivity testing.
Additional Reading
Bruce AJ, Rogers RS 3rd. Oral manifestations of sexually
transmitted diseases. Clin Dermatol. 2004;22:520-527.
Chue PWY. Gonorrhea—its natural history, oral mani-
festations, diagnosis, treatment, and prevention. J Am
Dent Assoc. 1975;90:1297.
Jamsky RJ, Christen AG. Oral gonococcal infections;
report of two cases. Oral Surg Oral Med Oral Pathol.
1982;53:358.
FIGURE 4-12 Kohn SR, Shaffer JF, Chomenko AG. Primary gonococ-
Irregularly outlined ulcer in gonococcal stomatitis. cal stomatitis. JAMA. 1972;219:86.
Simmons P. Gingival ulcer as an initial manifestation of
gonococcal stomatitis. Br Dent J. 1987;163:79.
by a pseudomembranous reaction with ton-
sillar enlargement accompanied by an ery- HIV PERIODONTITIS AND
thematous pharyngitis. Lymphadenopathy ORAL ULCERATIONS
and fever are also observed.
Figure 4-13
MICROSCOPIC FEATURES Age: Young adults
The mucosa may be intact or ulcerated with Sex: Male predilection
a fibrinous pseudomembrane. The submu- CLINICAL FEATURES
cosa displays a nonspecific subacute inflam-
matory cell infiltrate. Cytologic smears pre- Although any human immunodeficiency
pared with a Gram stain disclose free and virus (HIV)–infected individual may
intraepithelial gram-negative diplococci. develop periodontal disease, HIV periodon-
titis is a specific form of periodontal break-
DIFFERENTIAL DIAGNOSIS down resembling a fulminant, rapidly pro-
gressing ANUG. Although most instances
The ulcerations of gonococcal stomatitis have been seen in homosexual HIV-positive
may simulate other diseases included here males, other infected individuals may be
as ulcerative diseases. The variation in size affected. Early marginal gingivitis is char-
and configuration and elevated temperature acterized by a band-like zone of erythema
should arouse suspicion of gonorrhea along along the attached gingiva. Subsequently,
with a history of contact with a known car- the interdental papillae as well as the free
rier of the disease. A smear often, yet not marginal gingiva ulcerate, with appear-
invariably, discloses the presence of gram- ance of a gray-white pseudomembrane. The
negative diplococci. A culture is required to unique change in this disease is the rapidly
secure a definitive diagnosis. evolving periodontal stripping. Within a
few weeks, both soft and supportive hard
TREATMENT
tissues undergo necrosis, culminating in
Penicillin is the treatment of choice. One exposure of root cementum. Indeed, in
gram of probenecid followed 30 minutes some patients, the ulcerations progressively
later by 4.8 million units of intramuscu- extend onto the palate or adjacent vestibu-
lar procaine penicillin is recommended. lar soft tissues, resembling noma. The cul-
Alternatively, 500 mg oral penicillin every tivatable microbiota includes gram-positive
6 hours for 10 days generally eliminates the and -negative anaerobic rods, gram-positive
PMPH_Eversole_Chapter-04.indd 108 1/20/2011 2:16:55 PM
Oral Ulcerations and Fistulae 109
FIGURE 4-13
Left: multifocal gingival
ulcerations with strip-
ping of attached gingival
and necrotic bone in HIV
periodontitis. Right: apht-
hous-like ulceration in HIV
patient.
cocci, and uniquely, Candida species. Patients home care brushing, flossing, and importantly,
presenting with HIV periodontitis may or topical 1.2% chlorhexidine rinses. Severe dis-
may not harbor other opportunistic infec- ease warrants systemic antibiotics, either tetra-
tions or neoplastic lesions characteristic of cycline or metronidazole, for a 10-day period
AIDS. Another form of ulceration in HIV in addition to topical treatment techniques.
patients is the focal ulcers that appear iden-
tical to aphthous ulcers and may in fact rep-
resent simple aphthae unrelated to HIV.
Additional Reading
Delgado WA, Almeida OP, Vargas PA, León JE. Oral
MICROSCOPIC FEATURES ulcers in HIV-positive Peruvian patients: an immuno-
histochemical and in situ hybridization study. J Oral
The histologic findings are nonspecific. Pathol Med. 2009;38:120-125.
Ulceration with exposed fibrin, entrapped Murray PA, Holt S. Microbiology of HIV-associated gin-
leukocytes, and underlying granulation givitis and periodontitis. In Robertson PB, Greenspan
tissue are observed. The inflammatory cell JS, eds. Oral Manifestations of AIDS. Littleton, MA:
PSG Publishers; 1988:1053.
infiltrate is not particularly intense. Small Pindborg JJ, Holmstrup P. Necrotizing gingivitis related
osseous sequestra may be identifiable, and to human immunodeficiency virus (HIV) infection.
numerous polymorphic microbial colonies Afr Dent J. 1987;1:5.
adhere to the necrotic ulcerated regions Winkler JR, Grassi M, Murray PA. Clinical description
and etiology of HIV-associated periodontal diseases.
representing the sulcus. The aphthous- Calif Dent Assoc J. 1987;15:20.
like ulcerations are nonspecific ulcers with Winkler JR, Murray PA. Periodontal disease—potential
underlying chronic inflammation. intraoral expression of AIDS may be a rapidly progres-
sive periodontitis. In: Robertson PB, Greenspan JS,
DIFFERENTIAL DIAGNOSIS eds. Oral Manifestations of AIDS. Littleton, MA: PSG
Publishers; 1988:49.
The early changes are not particularly
unique, resembling ordinary gingivitis.
Early ulcerative changes are easily con-
fused with ANUG. Once rapidly progres- Focal Ulcerations
sive necrosis with exposure of cementum
occurs, HIV serologic testing should be
TRAUMATIC ULCER
considered. The oral aphthae must be dif- Figure 4-14
ferentiated from infectious ulcers with such
Age: No predilection
opportunistic pathogens as mycobacteria, Sex: No predilection
invasive fungi, and protozoal parasites.
CLINICAL FEATURES
TREATMENT The traumatic ulcer is by far the most com-
Periodontal debridement with povidone-io- mon type of focal ulceration. It may occur
dine irrigation is recommended followed by in response to a variety of traumatic insults
PMPH_Eversole_Chapter-04.indd 109 1/20/2011 2:16:57 PM
110 Chapter 4
FIGURE 4-14
Traumatic ulcers are focal.
including denture irritation, cheek- or marginal connective tissues evince a round
tongue-biting, pizza burn, or other forms cell infiltrate.
of self-inflicted trauma or iatrogenic injury
occurring in the dental office. The cause is DIFFERENTIAL DIAGNOSIS
usually readily determined by examining Traumatic ulcers may be extensive and asso-
for flange overextension on dentures using ciated with tumefaction. In these patients,
pressure-indicating paste, or by checking carcinoma, specific granulomatous inflam-
for jagged or malposed cusps and resto- mation, traumatic granuloma, and atypical
rations. The ulcer is generally shallow, histiocytic granuloma must be ruled out by
yet may show rolled borders as a result of biopsy.
granulation tissue response. Marginal ery-
thema is usually, yet not invariably, present. TREATMENT
Traumatic ulcers of the soft palate in the
If a history of trauma is present or irritational
region of the pterygoid hamulus in infants
factors are identified, they should be removed
have been referred to as Bednar’s aphthae.
and 10 days should be allowed for healing.
A traumatic ulcer of the lips in children
Failure to resolve necessitates a biopsy.
with erupting teeth has been termed Riga-
Fede disease. Deep traumatic ulcers of the
tongue associated with a granulomatous
tumefaction and a pronounced eosino-
Additional Reading
philic myositis have been termed trau- Abramson M, Dowrie JO. Sublingual granuloma in infan-
cy (Riga-Fede’s disease). J Pediatr. 1944;24:195.
matic ulcerative granuloma with stromal Elzay RP. Traumatic ulcerative granuloma with strom-
eosinophilia. al eosinophilia (Riga-Fede’s disease and traumatic
eosinophilic granuloma). Oral Surg Oral Med Oral
Pathol. 1983;55:497.
MICROSCOPIC FEATURES Neves BG, Roza RT, Castro GF. Traumatic lesions
The epithelium is lacking, exposing bare from congenital insensitivity to pain with anhidro-
sis in a pediatric patient: dental management. Dent
connective tissue with an eosinophilic sur- Traumatol. 2009;25:545-549.
face coagulum. The superficial layer is infil- Obermayer ME. Cheek biting (Morsicatio buccarum).
trated with neutrophils, and the deeper and Arch Dermatol. 1964;90:185.
PMPH_Eversole_Chapter-04.indd 110 1/20/2011 2:17:02 PM
Oral Ulcerations and Fistulae 111
TRAUMATIC GRANULOMA resemble lymphoma. The unusual histologic
WITH STROMAL findings account for the term atypical histio-
EOSINOPHILIA cytic granuloma. The lesion is probably a vari-
ant of the traumatic granuloma of the tongue
Figure 4-15
as its behavior is comparable. Similar lesions
Age: Adults may occur episodically in other intraoral
Sex: No predilection sites. Regardless, they eventually resolve
spontaneously and any provocation for their
CLINICAL FEATURES pathogenesis remains undetermined.
Traumatic granuloma is a large ulcerative
MICROSCOPIC FEATURES
lesion, often showing rolled margins, with a
predilection for the lateral of the tongue. The The traumatic granuloma of the tongue
ulcerated surface exceeds 1 cm and is gray- shows loss of surface epithelium with under-
white, and the margins fail to show a promi- lying deeply infiltrative sheets of histio-
nent erythematous halo. The lesion may feel cytes and scattered eosinophils. This infil-
indurated owing to the extension of inflam- trate extends into the intrinsic muscle fibers
mation into the underlying skeletal muscle of the tongue and, although not related,
layer. Although the lesion is referred to as a closely resembles the infiltrates seen in his-
“traumatic” granuloma, a history of trauma tiocytosis X. Atypical histiocytic granuloma
may be lacking, thereby obscuring the etiol- also shows surface ulceration and a histio-
ogy of this histopathologically defined lesion. cytic infiltrate; however, the histiocytes are
After an incisional biopsy, most of these cytologically pleomorphic and numerous
lesions involute, resolving within 4 to 5 weeks. mitotic figures are encountered. The histo-
A similar large ulcer with rolled mar- logic findings closely resemble those of lym-
gins can appear on the tongue, lips, or ves- phoma, and therefore, a medical work-up
tibule in elderly patients. The lesions are to rule out systemic lymphoma should be
clinically ominous and, histologically, they undertaken before a definitive diagnosis of
FIGURE 4-15
Traumatic ulcerative granu-
loma with stromal eosino-
philia.
PMPH_Eversole_Chapter-04.indd 111 1/20/2011 2:17:08 PM
112 Chapter 4
atypical histiocytic granuloma can be ren- Wright JM, Raukin KV, Wilson JW. Traumatic granu-
dered. Immunocytochemical marker stud- loma of the tongue. Head Neck. 1983;5:363.
ies on fresh tissue samples help to rule out
lymphoma because the atypical cells stain ATYPICAL HISTIOCYTIC
with histiocyte rather than lymphoid cell GRANULOMA
surface and cytoplasmic markers. Figure 4-16
DIFFERENTIAL DIAGNOSIS Age: Elderly
Clinically, both traumatic and atypical his- Sex: No predilection
tiocytic granulomas appear identical to CLINICAL FEATURES
squamous cell carcinoma or specific granu-
Some pathologists consider atypical histio-
lomatous inflammatory ulcerations. Biopsy
cytic granuloma to be a variant of traumatic
is therefore essential to determining the
ulcerative granuloma with stromal eosino-
diagnosis.
philia (TUGSE) since the two lesions share
TREATMENT similar clinical and microscopic features.
Atypical histiocytic granulomas are large
Once an incisional biopsy has been pro- with irregular margins occurring on the
cured and the diagnosis is established, no lips, vestibule, alveolar ridge, and rarely on
further treatment is required. The lesions the tongue, and microscopically, the cellular
resolve in 4 to 5 weeks. infiltrate is far more anaplastic than TUGSE,
mimicking a lymphoma (Hodgkin’s disease,
Additional Reading and lymphomatoid papulosis in particular).
These angry appearing ulcerations lack
Bhaskar SN, Lilly GE. Traumatic granuloma of the rolled borders and spontaneously resolve
tongue (human and experimental). Oral Surg Oral of their own accord. Some instances recur,
Med Oral Pathol. 1964;18:206. only to resolve again. They are only mildly
Elzay RP. Traumatic ulcerative granuloma with strom-
al eosinophilia (Riga-Fede’s disease and traumatic painful. No infectious agent has been asso-
eosinophilic granuloma). Oral Surg Oral Med Oral ciated with these ulcers.
Pathol. 1983;55:497.
Eversole LR, Leider AS, Jacobson PL, Kidd PM. Atypical MICROSCOPIC FEATURES
histiocytic granuloma. Cancer. 1985;55:1722. A loss of epithelium is evident and the ulcer
Hirshberg A, Amariglio N, Akrish S, et al. Traumatic
ulcerative granuloma with stromal eosinophilia: a bed exhibits a diffuse, often deep inflam-
reactive lesion of the oral mucosa. Am J Clin Pathol. matory cell infiltrate predominated by his-
2006;126:522-529. tiocytes with large nuclei and prominent
FIGURE 4-16
Atypical histiocytic granuloma appearing as large ulcers that eventually resolve.
PMPH_Eversole_Chapter-04.indd 112 1/20/2011 2:17:27 PM
Oral Ulcerations and Fistulae 113
nucleoli resembling Reed-Sternberg cells Romero-Ruiz MM, Torres-Lagares D, Alonso-Alejandro
of Hodgkin’s lymphoma. Plasma cells, lym- E, Serrano-González A, Gutiérrez-Pérez JL. Palatal
atypical histiocytic granuloma. Med Oral Pathol Oral
phocytes, and eosinophils are also included Cir Bucal. 2009;14:e480-e484.
in the infiltrate, yet show normal, benign Throndson RR, Wright JM, Watkins D. Atypical his-
features. Clinically, atypical histiocytic tiocytic granuloma of the oral mucosa: an unusual
granuloma resembles squamous cell carci- clinicopathologic entity simulating malignancy. J Oral
Maxillofac Surg. 2001;59(7):822-826.
noma and invasive fungal granulomas.
DIFFERENTIAL DIAGNOSIS
NECROTIZING
Some of these lesions show T-cell rearrange-
SIALOMETAPLASIA
ment with CD30 positivity using immuno-
histochemistry and should be considered Figure 4-17
as T-cell lymphomas. Molecular analysis is Age: Adults
required to make the differentiation. Sex: No predilection
TREATMENT CLINICAL FEATURES
Following biopsy, these ulcers tend to heal The hard and soft palates show focal deep-
within 3 to 4 weeks. Recurrence may occur, seated ulceration, occasionally bilateral.
yet these recurrences also spontaneously Occasionally, other mucosal sites bearing
involute. minor salivary glands are affected. The
ulcers are large, lack induration, and fail
Additional Reading to show rolled margins; the necrotic center
possesses a pebbly surfaced, gray mem-
Alobeid B, Pan LX, Milligan L, Budel L, Frizzera G.
brane. Despite their extensiveness, they are
Eosinophil-rich CD30+ lymphoproliferative disorder
of the oral mucosa. A form of “traumatic eosinophilic generally painless. After biopsy, the lesions
granuloma.” Am J Clin Pathol. 2004;121:43-50. generally heal spontaneously within 2
Eversole LR, Leider AS, Jacobsen PL, Kidd PM. Atypical months. The etiology is unknown, but vas-
histiocytic granuloma. Light microscopic, ultrastruc- cular occlusion of the arterioles supplying
tural, and histochemical findings in an unusual pseudo-
malignant reactive lesion of the oral cavity. Cancer. the palate and associated minor salivary
1985;55:1722-1729. glands has been suggested.
FIGURE 4-17
Necrotizing sialometa-
plasia, characterized by
relatively deep-seated
necrotic ulcers of the pala-
tal mucosa.
PMPH_Eversole_Chapter-04.indd 113 1/20/2011 2:17:32 PM
114 Chapter 4
MICROSCOPIC FEATURES
The ulcer bed is composed of necrotic
Additional Reading
debris and eosinophilic fibrinous material. Abrams AM, Melrose RJ, Howell FV. Necrotizing sialo-
The underlying salivary tissue is necrotic, metaplasia. Cancer. 1973;32:130.
Dunlap CL, Barker BF. Necrotizing sialometaplasia;
with maintenance of cellular outlines remi-
report of five additional cases. Oral Surg Oral Med
niscent of ischemic necrosis. The salivary Oral Pathol. 1974;37:722.
epithelium adjacent to the necrotic zone Dunley RE, Jacoway JR. Necrotizing sialometaplasia.
displays squamous metaplasia with loss of Oral Surg Oral Med Oral Pathol. 1979;47:169.
normal acinar morphologic characteristics. Lieberman J, Weinstein M. Necrotizing sialometaplasia.
Cutis. 1988;41:97.
The metaplastic islands are oval or linear Lynch DP, Crago CA, Martinez MG. Necrotizing sia-
with rounded margins. Lesions should not lometaplasia. Oral Surg Oral Med Oral Pathol.
be confused with mucoepidermoid or epi- 1979;47:63.
dermoid carcinoma.
DIFFERENTIAL DIAGNOSIS SPECIFIC GRANULOMATOUS
Clinically, necrotizing sialometaplasia may be ULCER
confused with carcinoma, adenocarcinoma, Figure 4-18
granulomatous ulcer, or traumatic ulcer. Lack
Age: Adults
of induration and rolled margins should Sex: No predilection
divert suspicion of malignancy. Biopsy is
required to obtain a definitive diagnosis. CLINICAL FEATURES
Specific granulomatous responses elicited by
TREATMENT
microorganisms are all primary pulmonary
Once a definitive diagnosis is secured, no infections that involve oral mucous mem-
treatment is required. The lesions sponta- branes secondarily by extrapulmonary dis-
neously regress in 6 to 8 weeks. Palliation semination; Mycobacterium tuberculosis and
is not necessary because pain is generally the deep fungi are specifically implicated.
not a problem. Of the fungal infections, histoplasmosis,
FIGURE 4-18
Granulomatous ulcers caused
by mycobacteria or inva-
sive fungi (histoplasmosis,
blastomycosis).
PMPH_Eversole_Chapter-04.indd 114 1/20/2011 2:17:47 PM
Oral Ulcerations and Fistulae 115
blastomycosis, cryptococcosis, and coccid- TREATMENT
iodomycosis are most common. The ulcers Because oral granulomatous lesions are
are always associated with a granulomatous, associated with pulmonary disease, refer-
firm swelling that characteristically evinces ral to an internist is indicated. Tuberculosis
a papillary or cobblestone surface pattern is treated with long-term isoniazid therapy.
with patchy erythema. Although any site Deep fungi are managed with amphoteri-
may be affected, the tongue and buccal cin B. HIV-associated granulomatous infec-
mucosa are favored. Often, more than one tions require administration of appropri-
lesion is present. Because pulmonary infec- ate antibiotics in addition to antiretroviral
tion is the dominant feature, chronic cough drugs.
is noted. Transmission of infection by phys-
ical contact with the lesions is remote but
possible.
Atypical mycobacteria, particularly
Additional Reading
Mycobacterium avium intracellulare and deep Birkholz H, Riegler HC. Tuberculosis of the tongue.
fungal infections manifesting as granu- J Am Dent Assoc. 1979;98:60.
Levy BM. Oral manifestations of histoplasmosis. J Am
lomatous ulcers of the oral mucous mem- Dent Assoc. 1945;32:215.
branes may herald the onset of pre-AIDS or Mincer HH, Oglesby R. Intraoral North American blasto-
AIDS. Such opportunistic infections occur mycosis. Oral Surg Oral Med Oral Pathol. 1966;22:36.
in the oral cavity subsequent to HIV infec- Pindborg JJ. Classification of oral lesions associated
with HIV infection. Oral Surg Oral Med Oral Pathol.
tion, and serologic testing for the virus is 1989;67:292.
warranted in high-risk patients. Yungco JC. Tuberculosis of the tongue in patients with
pulmonary tuberculosis. Dis Chest. 1963;44:638.
MICROSCOPIC FEATURES
Subjacent to the ulcerated zones are focal
condensations of chronically inflamed CHANCRE (PRIMARY SYPHILIS)
granulation tissue with epithelioid cells and Figure 4-19
multinucleated giant cells showing a horse-
shoe or wreath-like nuclear arrangement. Age: Young adults
Sex: No predilection
Caseous necrosis is often, yet not always,
seen in tuberculous granulomas. The deep CLINICAL FEATURES
fungal granulomas are noncaseating. Acid- Primary syphilitic chancre of the oral
fast stains disclose the presence of myco- mucosa arises subsequent to venereal con-
bacteria. Periodic acid-Schiff (PAS) or meth- tact as a consequence of orogenital sexual
enamine silver stain fungal cell walls. relationships. The lesion is most frequently
seen on the lips or tongue and is typically a
DIFFERENTIAL DIAGNOSIS painless fungating tumefaction with central
Specific granulomatous ulcers may simu- ulceration, firm to palpation. The examiner
late carcinoma or traumatic ulcers. When should wear gloves as the primary lesion is
predominantly papillary in appearance, teeming with Treponema pallidum, the caus-
they may be difficult to differentiate from ative spirochetal microorganism. Chancres
papillary hyperplasia or verrucous car- appear 5 to 6 weeks after sexual contact. The
cinoma. Biopsy reveals the characteristic Venereal Disease Research Laboratory test
features of granulomatous infection. Skin (VDRL), fluorescence treponemal antibody
tests may also be indicated to demon- test, or treponemal immobilization assay
strate delayed hypersensitivity to a specific usually are negative or only slightly reactive
microorganism. during the early stages of the disease and
PMPH_Eversole_Chapter-04.indd 115 1/20/2011 2:18:05 PM
116 Chapter 4
Most states require that venereal disease cases
be reported to the state board of health.
Additional Reading
Alexander WN. Venereal disease and the dentist. J Acad
Gen Dent. 1975;23:14.
Aloi F. Lip syphilitic chancre in a child. Pediatr Dermatol.
1987;4:63.
Meyer I, Shklar G. The oral manifestations of acquired
syphilis. Oral Surg Oral Med Oral Pathol. 1967; 23:45.
SQUAMOUS CELL
FIGURE 4-19 CARCINOMA
Chancre of primary syphilis. A central zone of Figure 4-20
ulceration is surrounded by indurated, rolled, or
swollen margins. Age: Elderly adults
Sex: Male predilection
CLINICAL FEATURES
therefore assays should be performed 1 to 2
weeks after appearance of the primary lesion. The most common presenting sign of oral
cancer is the focal ulceration with indurated
MICROSCOPIC FEATURES margins. Any oral ulcer without a readily
The epithelium is lacking over the clinically apparent cause should be considered carci-
ulcerated surface. Granulation tissue, which noma until proven otherwise, particularly if
evinces an intense plasma cell infiltrate with the lesion has persisted longer than 2 weeks.
a tendency for perivascular orientation, Carcinomatous ulcers may arise in preexist-
constitutes the bulk of the tumefaction. A ing leukoplakia or erythroplasia, but there
Warthin-Starry spirochete stain is required may be no history of a precedent precancer-
to visualize the microorganism. A smear ous lesion. The patients usually give a history
with dark-field illumination discloses the of smoking and show a proclivity for overim-
presence of mobile spirochetes. bibing alcoholic beverages. The lateral border
of the tongue, floor of the mouth, alveolar
DIFFERENTIAL DIAGNOSIS ridge, and lower lip are the sites of predilec-
tion; however, oral cancer can develop in any
The granulomatous ulcer may resemble carci- location. The ulcer is often, yet not always,
noma, specific granulomatous ulcer of tuber- painless. The growth rate is variable but usu-
culosis or the deep mycoses, and traumatic ally progresses relatively rapidly. The larger
ulcer. A history of venereal transmission the tumefactive ulceration, the more likely
with rapid onset and growth should arouse the chance for nodal metastasis. Oral cancer
suspicion of primary syphilis. VDRL, fluo- spreads first to the submandibular and cer-
rescence treponemal antibody, or trepone- vical lymph nodes. Regional metastatic dis-
mal immobilization tests are positive 1 to 2 ease in the neck, like the primary lesion, is
weeks after appearance of the chancre. indurated and fixed to adjacent tissues.
TREATMENT MICROSCOPIC FEATURES
Four million units of penicillin intramuscu- Subjacent and lateral to the zone of ulcer-
larly followed by 250 mg penicillin orally 4 ation are invasive islands, cords, and nests of
times daily for 2 weeks is usually curative. malignant epithelial cells that demonstrate
PMPH_Eversole_Chapter-04.indd 116 1/20/2011 2:18:06 PM
Oral Ulcerations and Fistulae 117
FIGURE 4-20
Squamous cell carcinoma
beginning as a focal ulceration
with rolled borders.
varying degrees of pleomorphism, hyper- Shafer WG, Hine MK, Levy BM. A Textbook of Oral
chromatism, and increased mitoses, many Pathology. 4th ed. Philadelphia: W. B. Saunders;
1983:112.
of which are bizarre. Keratin and parakera- Tiecke RW, Bernier JL. Statistical and morpho-
tin pearls are often present. logical analysis of four hundred and one cases of
intraoral squamous cell carcinoma. J Am Dent Assoc.
DIFFERENTIAL DIAGNOSIS 1954;49:684.
Carcinoma appearing as an oral ulcer may
be clinically indistinguishable from trau-
matic ulcer, chancre, or one of the specific Perioral and Commissural
granulomatous infections. Biopsy pro- Ulcerations and Fistulae
vides a definitive diagnosis. Certainly, any
ulcer without a cause, or one that fails to COMMISSURAL PITS
heal when a suspected cause is removed, Figure 4-21
requires microscopic examination.
Age: From infancy
TREATMENT Sex: No predilection
Cancer should be managed by an oncologist. CLINICAL FEATURES
Surgery, radiotherapy, or a combination of
Blind fistulae or pits located at the commis-
the two are the treatment methods of choice.
sure of the lips are 1 to 2 mm in diameter
and reach a depth of similar dimension.
Additional Reading They may be unilateral or bilateral, show
a familial tendency, and are more frequent
Kremen AJ, Arhelger SW. Early cancer of the oral cav-
among blacks than whites. Their incidence
ity with special reference to cancer of the tongue.
Postgrad Med. 1960;27:422. has been reported to vary from 1% to 20% of
Nakissa N, Hornback NB, Shidnia H, Sayoc ES. Carcinoma the population.
of the floor of the mouth. Cancer. 1978;45:2914.
Rossi EP, Hirsch SA. A survey of 4,793 oral lesions with MICROSCOPIC FEATURES
emphasis on neoplasia and premalignancy. J Am Dent
Assoc. 1977;94:883. Not applicable.
PMPH_Eversole_Chapter-04.indd 117 1/20/2011 2:18:07 PM
118 Chapter 4
FIGURE 4-22
Congenital lip pits. These may be bilateral blind
FIGURE 4-21 ducts or they may communicate with salivary con-
Commissural pits: bilateral blind fistulae devoid of duits. (Courtesy of Dr. Caesar Lopez.)
tumefactive margins.
side of the midline on the vermilion bor-
DIFFERENTIAL DIAGNOSIS
der. The fistulae may extend as deep as 2
Commissural pits are clean, uninflamed cm and communicate with minor salivary
depressions that can be easily differentiated ducts. The surrounding submucosa may
from inflammatory or neoplastic lesions be somewhat hyperplastic, producing a
involving the angles of the mouth. soft elevation of tissue around the broad
sinuses. Although lip pits may be an iso-
TREATMENT lated finding, they are more often associated
No treatment is necessary. with cleft palate-cleft lip. This syndrome is
inherited as an autosomal dominant trait.
Developmental pits have also occurred in
Additional Reading the buccal mucosa.
Baker WR. Pits of the lip commissures in
caucasoid males. Oral Surg Oral Med Oral Pathol. MICROSCOPIC FEATURES
1966;21:56. Not applicable.
Everett FG, Wescott WB. Commissural lip pits. Oral
Surg Oral Med Oral Pathol. 1961;14:202.
DIFFERENTIAL DIAGNOSIS
Lip pits lack ulceration and inflammation,
CONGENITAL LIP PITS allowing for easy recognition as a devel-
Figure 4-22 opmental anomaly, particularly in light of
their bilaterality and association with other
Age: From infancy developmental anomalies.
Sex: Slight female predilection
CLINICAL FEATURES TREATMENT
Developmental pits of the lower lip are Surgical removal may be undertaken for
blind fistulae located bilaterally on either cosmetic purposes.
PMPH_Eversole_Chapter-04.indd 118 1/20/2011 2:18:29 PM
Oral Ulcerations and Fistulae 119
Candida hyphae are aggregated in the super-
Additional Reading ficial layers. The subjacent fibrous connec-
Bocian M et al. Lip pits and deletion lq32—41. Am J Med tive tissue displays a subacute or chronic
Genet. 1987;26:437. inflammatory cell infiltrate.
Bowden DW. Bilateral congenital fistulae of the lower
lip. Br J Orthod. 1977;4:101.
Van Der Woude A. Fistula labii inferious congenita and DIFFERENTIAL DIAGNOSIS
its association with cleft lip and palate. Am J Hum
The bilateral, weeping inflamed lesions
Genet. 1954;6:244.
Watanabe Y, Igaku-Hakushi, Otake M, Tomida K. devoid of tumefaction are characteristic.
Congenital fistulas of the lower lip; report of five cases Underlying predisposing factors must be
with special reference to the etiology. Oral Surg Oral sought. A complete blood count and gas-
Med Oral Pathol. 1951;4(6):709-722. tric analysis should be performed when
pernicious anemia is suspected. Patients
with pernicious anemia usually manifest
ANGULAR CHEILITIS
atrophic glossitis in addition to angular
Figure 4-23 cheilitis.
Age: Adults
Sex: No predilection TREATMENT
CLINICAL FEATURES The predisposing factors, be they local or
systemic, must be eliminated or controlled.
Located bilaterally at the commissures of
Topical application of nystatin cream or
the lips, angular cheilitis is characterized
ointment three times daily eliminates com-
by weeping focal ulcerations showing
plicating candidal infection.
cracking, keratosis, and mild erythema.
In most instances, the disease is caused
by, or secondarily infected with, Candida
albicans. Predisposing factors are com- Additional Reading
monly encountered: decreased vertical Cawson RA. Denture sore mouth and angular cheilitis.
intermaxillary dimension, pronounced Br Dent J. 1963;115:441.
angular skin folds, vitamin B complex Finnerud C. Perleche: a study of 100 cases. Arch
deficiency, pernicious anemia, and HIV Dermatol Syph. 1929;20:454.
Lorentzer SH. Angular cheilitis. Northwest Dent.
infection. 1981;60:10.
Pindborg JJ. Oral candidiasis in HIV infection. In:
MICROSCOPIC FEATURES Robertson PB, Greenspan JS, eds. Oral Manifestations
of AIDS. Littleton, MA: PSG Publishing; 1988:28.
The surface epithelium shows zones of ulcer- Ritchie GM, Fletcher AM. Angular inflammation. Oral
ation alternating with focal hyperkeratosis. Surg Oral Med Oral Pathol. 1973;36:358.
FIGURE 4-23
Angular cheilitis char-
acterized by commis-
sural fissuring with
keratotic, weeping
lesions.
PMPH_Eversole_Chapter-04.indd 119 1/20/2011 8:26:50 PM
120 Chapter 4
ally may evince a squamous epithelial lin-
Oral Fistulae ing. In either case, communication with
inflamed granulation tissue in bone is
PERIAPICAL ABSCESS AND observed.
OSTEOMYELITIS
Figure 4-24 DIFFERENTIAL DIAGNOSIS
Age: No predilection A draining fistula may be clinically con-
Sex: No predilection fused with traumatic ulcer, aphthous ulcer,
or, rarely, carcinoma. Searching for an infec-
CLINICAL FEATURES tious source and probing the lesion with
Drainage tracts resulting from infection of a periodontal probe or gutta-percha point
odontogenic and periodontal origin are the will aid in obtaining a diagnosis.
most frequent forms of oral fistulae. They When radiographic evidence of osteo-
are most often encountered on the gingiva myelitis exists, culture and sensitivity of
in close proximity to the tooth, acting as the the exudate, particularly for actinomy-
source of infection or adjacent to a focus of cetes, should be pursued. When teeth are
destructive or sclerosing osteomyelitis as missing, search for a retained root tip is
evidenced radiographically. When a carious advisable.
or traumatized noncarious tooth is pres-
ent, it will test nonvital with a vitalome- TREATMENT
ter. The fistula contains a draining center Infected teeth must be treated endodonti-
from which a purulent exudate can often cally or, if nonrestorable, extracted. When
be expressed. Patients usually complain of osteomyelitis is present, antibiotic treatment
a foul or metallic taste. Occasionally, the fis- should be instituted and either maintained
tula is associated with a parulis. or altered depending on results of culture
and sensitivity testing. When the patient is
MICROSCOPIC FEATURES
febrile with malaise and cellulitis is present,
The drainage tract is lined by subacutely hospitalization and intravenous antibiotic
inflamed granulation tissue and occasion- treatment may be indicated.
FIGURE 4-24
Oral fistula associated with a periapi-
cal abscess.
PMPH_Eversole_Chapter-04.indd 120 1/20/2011 2:18:40 PM
Oral Ulcerations and Fistulae 121
Capillaries course through the abscess, and
Additional Reading both necrotic debris and microbial colo-
Shapiro HH et al. Spread of infection of dental origin. nies may be present. The fistula contains
Oral Surg Oral Med Oral Pathol. 1950;3: 1407. an acute inflammatory cell infiltrate and is
Smulson MH, Maggio JD, Hagen, JC. Diseases of the pulp usually lined by granulation tissue; how-
and periapex. In: Weine FS, ed. Endodontic Therapy. ever, epithelialization may develop.
3rd ed. St Louis, MO: C. V. Mosby; 1982:142.
DIFFERENTIAL DIAGNOSIS
PERIODONTAL ABSCESS
Fistulae of periapical origin must be ruled
Figure 4-25 out on a radiographic and clinical basis uti-
Age: Adults lizing methods to ascertain pulp viability.
Sex: No predilection Occasionally, a periodontal abscess may
coexist with, or indeed cause, pulp necrosis.
CLINICAL FEATURES
Specific infection by actinomycetes may be
An acute reaction to dental plaque irritants present and can be diagnosed by microbial
and bacteria may develop in periodontal anaerobic culture or biopsy.
pockets and in furcation areas. Whereas
many periodontal abscesses drain via the TREATMENT
sulcular pocket, others may spread through Periodontal curettage or flap surgery with
gingival tissues and perforate to form a fis- elimination of the abscess is required. Root
tula. The periodontally involved tooth may planing and periodontal therapy in gen-
or may not be sensitive to percussion, and eral should be undertaken. If periodontal
pain may be dull or severe. Constitutional abscess exists in conjunction with pulp
signs of infection, including fever, malaise, necrosis, either endodontic treatment or
and lymphadenopathy, may exist. Placing a extraction is indicated.
probe into the periodontal pocket with mild
manipulation often elicits drainage of exu-
date through the fistulous tract. When the
Additional Reading
pocket is deep and the abscess lies adjacent Glickman I. Chap. 18. Clinical Periodontology. 4th ed.
to lateral accessory root canals, retrograde Philadelphia, PA: W. B. Saunders; 1972.
pulpitis may ensue. Recurrent or multiple O’Brien JJ. Diagnosis and treatment of periodontal
and gingival abscesses. J Ontario Dent Assoc.
periodontal abscesses may be encountered 1970;47:16.
in uncontrolled diabetics. Ray HG, Orban F. Gingival structures in diabetes mel-
litus. J Periodontol. 1950;21:85.
MICROSCOPIC FEATURES Smith RG et al. Acute lateral periodontal abscesses. Br
Dent J. 1986;161:176.
The zone of abscess formation shows infil- Trott JR. The acute periodontal abscess. J Can Dent
tration by neutrophils and macrophages. Assoc. 1969;25:601.
FIGURE 4-25
Oral fistula associated with
a periodontal abscess.
PMPH_Eversole_Chapter-04.indd 121 1/20/2011 2:18:48 PM
122 Chapter 4
ACTINOMYCOSIS TREATMENT
Figure 4-26 The granulation tissue bed in bone should
be curetted and the patient should receive
Age: Young adults
Sex: Male predilection
antibiotic therapy. Penicillin (1 million units
intramuscularly, followed by 500 mg for 10
CLINICAL FEATURES days) is the drug of choice. In patients aller-
Either oral or extraoral fistulae may develop gic to penicillin, erythromycin may be pre-
in an area of infection by Actinomyces israelii. scribed. If the disease fails to respond, mas-
The disease is most frequently encountered sive intravenous doses of antibiotic may be
in the head and neck area and is acquired required to achieve cure.
subsequent to tooth extraction or trauma. It
usually manifests as an osteomyelitis with
formation of granulation tissue and abscess
Additional Reading
in the submandibular region, producing so- Benoliel R et al. Actinomycosis of the jaws. Int J Oral
called lumpy jaw. The infection may localize Surg. 1985;14:195.
Freeman LR, Zimmermann EE, Ferrillo PJ. Conservative
in periapical periodontal foci of inflammation. treatment of periapical actinomycosis. Oral Surg Oral
The organisms may be expressed through Med Oral Pathol. 1981;51:205.
the fistulae and appear as small yellow flecks Kapsimalis P et al. Actinomycosis of the periapical tis-
termed sulfur granules. Anaerobic methods sues. Oral Surg Oral Med Oral Pathol. 1968;26:374.
Porter IA. Actinomycosis in the North-East of Scotland.
are required to culture the organism. Br Med J. 1951;1:1360.
Weir JC, Buck WH. Periapical actinomycosis: Report
MICROSCOPIC FEATURES of a case and review of the literature. Oral Surg Oral
The granulation tissue in bone, or underly- Med Oral Pathol. 1982;54:336.
ing the fistulae, shows foci of epithelioid his-
tiocytes or localized abscesses. The microbial OROANTRAL FISTULA
colonies are clove shaped, display a peripheral Figure 4-27
fringe, and are PAS positive. They lie in the
center of a sea of neutrophilic granulocytes. Age: Adults
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
Actinomycosis manifesting oral fistulae
cannot be differentiated from nonspecific A fistula that traverses the maxillary alveo-
infection of pulpal or periodontal origin. lus, causing an oral-antral communication,
Culture and biopsy disclose the presence of may arise subsequent to tooth extraction
actinomycotic microorganisms. in which a perforation of the antral floor
FIGURE 4-26
Drainage tracts, which
develop either extraorally or
intraorally in actinomycotic
infection.
PMPH_Eversole_Chapter-04.indd 122 1/20/2011 2:18:52 PM
Oral Ulcerations and Fistulae 123
TREATMENT
The fistula should be curetted to disrupt the
epithelialized communication, and a pala-
tal flap can be rotated over the defect for
primary closure. Gold or platinum foil may
be employed during surgery to occlude the
opening and facilitate tissue closure.
Additional Reading
Clark HB, Jr. Practical Oral Surgery. 3rd ed. Philadelphia,
PA: Lea & Febiger; 1965:168.
FIGURE 4-27 Goldman EH, Stratigos GT, Arthur AL. Treatment of
Oroantral fistula representing a through-and- oroantral fistula by gold foil closure: Report of a case.
through communication between the oral cavity J Oral Maxillofac Surg. 1969;27:875.
and antrum. Killey HC, Kay LW. An analysis of 250 cases of oro-antral
fistula treated by buccal flap operation. Oral Surg Oral
Med Oral Pathol. 1967;24:726.
developed. The fistula usually opens on Wowren NV. Oroantral communications and displace-
the crest of the maxillary alveolar ridge, ments of roots into the maxillary sinus: A follow-up of
231 cases. J Oral Maxillofac Surg. 1971;29:622.
yet may exit in the mucobuccal fold area. Yih WY et al. Secondary closure of oroantral and oronasal
The opening may be narrow or large and fistulas: A modification of existing techniques. J Oral
is usually devoid of erythema and purulent Maxillofac Surg. 1988;46:357.
drainage. If residual inflammation exists
in the maxilla or antral cavity, an exudate
may be present. Occasionally, antral polyps SOFT TISSUE ABSCESS
herniate through the fistula as a fluctuant Figure 4-28
bulbous tumefaction.
Age: No predilection
Sex: No predilection
MICROSCOPIC FEATURES
The fistula is lined by stratified squamous CLINICAL FEATURES
and often respiratory epithelium. The sur- An abscess may develop in the submucosal
rounding fibrous connective tissue evinces connective tissues subsequent to a penetrat-
an inflammatory cell infiltrate of variable ing wound or introduction of a foreign body.
intensity. Rarely, Actinomyces may cause a soft tissue
abscess. Any tissue site may be involved;
DIFFERENTIAL DIAGNOSIS however, the tongue and buccal mucosa are
Oroantral fistulae must be differentiated most frequently affected. A tumefaction is
from fistulae developing from underlying usually palpable or visible subjacent to the
osteomyelitis or actinomycosis. The location site of drainage. Pain is often present, and
on the maxillary alveolus, history of extrac- compression of the area elicits exudation
tion, and ability to probe through the defect through the fistula.
into the antrum usually provide sufficient
evidence to make the diagnosis. The presence MICROSCOPIC FEATURES
of associated swelling or necrotic tissue could Granulation tissue with foci of neutrophilic
be indicative of a more serious disorder, such infiltration is observed. When a foreign
as maxillary sinus carcinoma or mucormyco- body is present, it is usually identifiable
sis. A biopsy should then be performed. under ordinary or polarized light. Giant
PMPH_Eversole_Chapter-04.indd 123 1/20/2011 2:19:00 PM
124 Chapter 4
FIGURE 4-28
Soft tissue abscess formation showing
swelling with a focus of drainage.
FIGURE 4-29
Left: Developmental sinus lat-
eral to the pterygomandibular
raphe. Right: Blind sinus in
external ear.
cells surround the foreign material. The fis- Tov YS et al. Facial cutaneous fistula due to a foreign body
tulous tract is lined by granulation tissue. in Wharton’s duct. J Laryngol Otol. 1988;102:370.
DIFFERENTIAL DIAGNOSIS
DEVELOPMENTAL ORAL
A draining fistula in the soft tissues, because SINUSES
it is often associated with tumefaction,
Figure 4-29
must be differentiated from specific granu-
lomatous diseases and neoplasms that have Age: From infancy
become inflamed. Sex: No predilection
TREATMENT CLINICAL FEATURES
Incision with curettage and drainage should A variety of developmental fistulae and
be performed and the tissue should be sub- sinuses occur within the oral cavity. Some
mitted for microscopic examination to con- of these pits and fistulae fail to com-
firm the clinical impression. municate with underlying structures or
If fever is present and the abscess is embryonic remnants, whereas others do
large, the patient should receive antibiotic communicate. Included in this group of
therapy while culture and sensitivity are developmental defects are (1) fistula of the
obtained. nasopalatine duct, (2) tonsillar faucial fistu-
lae, (3) pits of the pterygomandibular fold,
Additional Reading and (4) lingual thyroglossal sinus of the
foramen cecum area. Most of these sinuses
Archer WH. Oral and Maxillofacial Surgery. 5th ed. are blind and are devoid of inflammatory
Philadelphia, PA: W. B. Saunders; 1975:490, 492. changes. Occasionally, oral pits and sinuses
PMPH_Eversole_Chapter-04.indd 124 1/20/2011 2:19:01 PM
Oral Ulcerations and Fistulae 125
are associated with preauricular pits and Hill WC, Darlow HM. Bilateral perforate nasopalatine
deafness. communication in the human adult. J Laryngol Otol.
1945;60:160.
Leider AS, Lucas JW, Eversole, LR. Sebaceous choristo-
MICROSCOPIC FEATURES ma of the thyroglossal duct. Oral Surg Oral Med Oral
Pathol. 1977;44:261.
Not applicable.
DIFFERENTIAL DIAGNOSIS
FISSURED (SCROTAL) TONGUE
The bilateral nature, location, and Figure 4-30
healthy tissue appearance allow for easy
identification. Age: All ages
Sex: Slight male predilection
TREATMENT
CLINICAL FEATURES
No treatment is necessary.
Cracks and fissures may cover the surface
of the tongue, representing a developmental
Additional Reading innocuous, and rather common, condition.
In some instances a central linear fissure is
Campbell EH. Perforation of the faucial pillars. Arch seen with small contributories fanning lat-
Otolaryngol Head Neck Surg. 1925;1:503. erally. The fissures may be up to 8 mm deep
Claiborne JH, Jr. Hiatus in the anterior pillar of the fau-
ces of the right side with congenital absence of the and can entrap food, causing irritation and
tonsil on either side. Am J Med Sci. 1885;89:490. discomfort.
FIGURE 4-30
Fissures on dorsum (scrotal tongue).
PMPH_Eversole_Chapter-04.indd 125 1/20/2011 2:19:14 PM
126 Chapter 4
MICROSCOPIC FEATURES Zargari O. The prevalence and significance of fissured
tongue and geographical tongue in psoriatic patients.
The fissures are lined by normal appearing Clin Exp Dermatol. 2006;31:192-195.
stratified squamous epithelium and are in
fact not truly ulcerated.
Necrotic and Osseous
DIFFERENTIAL DIAGNOSIS Destructive Lesions
The clinical presentation is classic and not
confused with other oral ulcerations. Fissured FACTITIAL INJURY AND
tongue is a component of the Melkerson- TRAUMA
Rosenthall syndrome, a component of oro- Figure 4-31
facial granulomatosis in which the lips are
Age: No predilection
enlarged with granulomatous inflammation
Sex: No predilection
and patients develop facial nerve palsy.
CLINICAL FEATURES
TREATMENT
Self-inflicted wounds, chronic irritation, and
None. If irritation occurs, the fissures can be postsurgical defects may result in osseous
brushed out with a soft bristle brush. or soft tissue perforations of the palate.
Occasionally, the palate breaks down, leav-
Additional Reading ing a defect after cleft palate repair. A large
rhinolith may irritate the palatal roof, caus-
Binmadi NO, Jham BC, Meiller TF, Scheper MA. A case
of a deeply fissured tongue. Oral Surg Oral Med Oral ing palatal perforation. Habitual cocaine
Pathol Oral Radiol Endod. 2010;109:659-63. use may cause nasal osseous necrosis with
Hoexter DL. Melkerson Rosenthal syndrome. N Y State extension through the palate. The defects
Dent J. 2007;73:30-32. are usually clean with little evidence of
Yarom N, Cantony U, Gorsky M. Prevalence of fissured
tongue, geographic tongue and median rhomboid glos- erythema, granulation tissue, or necrosis.
sitis among Israeli adults of different ethnic origins. Patients may experience altered speech and
Dermatology. 2004;209:88-94. difficulty in eating.
FIGURE 4-31
Osseous destruction due to trauma.
Ulcer on right caused by irritation
during intubation.
PMPH_Eversole_Chapter-04.indd 126 1/20/2011 2:19:37 PM
Oral Ulcerations and Fistulae 127
MICROSCOPIC FEATURES
Not applicable.
DIFFERENTIAL DIAGNOSIS
Palatal perforations resulting from factitial
injury as a result of trauma or as sequelae
to surgical intervention may simulate other
osseous destructive lesions included in this
section. The clean noninflamed character
and a thorough history usually provide
information sufficient to secure the diag-
nosis. A biopsy rules out other entities of a FIGURE 4-32
more serious nature. Palatal perforation from nasal lesions in Wegener’s
granulomatosis. (Courtesy of Dr. T. Daniels.)
TREATMENT
The defect may be occluded with a dental granulomatosis is a systemic collagen dis-
prosthesis or may be closed surgically with ease that can manifest these destructive and
the aid of a palatal flap. ulcerative lesions of the face and oral cavity.
In addition, erythematous granular tume-
factions may be encountered on the gingiva
Additional Reading and other mucosal sites. Widespread mani-
festations are present with granulomatous
Archer WH. Oral and Maxillofacial Surgery. 5th ed.
Philadelphia, PA: W. B. Saunders; 1975:1616, 1621.
and destructive lesions of the kidneys and
Silvestre FJ, Perez-Herbera A, Puente-Sandoval A, lungs. Patients with Wegener’s are posi-
Bagán JV. Hard palate perforation in cocaine abusers: tive for a serum autoantibody known as
a systematic review. Clin Oral Investig. 2010. antineutrophil cytoplasmic antibodies
(ANCA).
WEGENER’S MICROSCOPIC FEATURES
GRANULOMATOSIS The granulomatous tissue surrounding the
Figure 4-32 defects is infiltrated with mononuclear cells
and a foreign-body type of multinucleated
Age: Adults
giant cell. Scattered eosinophils are occa-
Sex: Female predilection
sionally observed. The sine qua non of the
CLINICAL FEATURES histomorphologic findings is the presence
Midline lethal granuloma is a clinically of necrotizing vasculitis. Special stains fail
defined entity in which midfacial osseous to disclose the presence of specific bacterial
resorption and necrosis are seen, often or fungal microorganisms.
with palatal perforation and loss of the
nasal septum. Both Wegener’s granuloma- DIFFERENTIAL DIAGNOSIS
tosis and extranodal natural killer (NK)/T- The palatal perforation and midfacial
cell lymphoma (polymorphic reticulosis), destructive lesions of these granuloma-
a form of non-Hodgkin’s lymphoma, will tous inflammations must be differentiated
present with this clinical profile. With microscopically from malignant reticulosis,
time, the entire midface may be destroyed gummatous necrosis, mucormycosis, and
with involvement of the orbits. Wegener’s antral carcinoma.
PMPH_Eversole_Chapter-04.indd 127 1/20/2011 2:19:48 PM
128 Chapter 4
TREATMENT the latter, the disease is more often seen in
Wegener’s granulomatosis is potentially Asia, Mexico, and Central America. The
lethal if left untreated. It is treated with immu- malignancy causes nasal obstruction and
nosuppressive drugs such as high-dose ste- epistaxis and evolves into a destructive
roids, azathioprine, and cyclophosphamide lesion that erodes the midface structures as
and should be managed by a physician. invasion and extension into the nasophar-
ynx, paranasal sinuses, orbit, and oral cav-
Additional Reading ity. Distant metastases ultimately evolve,
and additional symptoms appear such as
Batsakis JG et al. Midfacial necrotizing lesions. Semin fever, malaise, and weight loss.
Diagn Pathol. 1987;4:90.
Brown HA, Woolner LG. Findings referable to the upper MICROSCOPIC FEATURES
part of the respiratory tract in Wegener’s granuloma-
tosis. Ann Otol Rhinol Laryngol. 1960;69:810. The lymphomatous infiltrate tends to be
Chen M, Kallenberg CG. New advances in the patho- angiocentric and angiodestructive. The cells
genesis of ANCA-associated vasculitides. Clin Exp
are small yet admixed with large and often-
Rheumatol. 2009;27(1 suppl 52):S108-S114.
Edwards MB, Buckerfield JP. Wegener’s granulomato- times anaplastic lymphoblasts. The nuclei
sis: a case with primary mucocutaneous lesions. Oral are granular without prominent nucleoli.
Surg Oral Med Oral Pathol. 1978;46:53. In many cases, the malignant infiltrate is
Kassel SH et al. Midline malignant reticulosis (so-called joined by normal inflammatory cells. The
lethal midline granuloma). Cancer. 1969;23:920.
immunohistochemical profile shows posi-
tivity for CD56, CD2, and granzyme B.
EXTRANODAL NK/T-CELL
LYMPHOMA DIFFERENTIAL DIAGNOSIS
Figure 4-33 Wegener’s is the chief entity in the differ-
ential diagnosis, yet trauma, cocaine abuse,
Age: Young adults
Sex: Males
other malignancies, and invasive fungi are
also considerations.
CLINICAL FEATURES
Midline lethal granuloma is a midface TREATMENT
osseous destructive process that can be Extranodal NK/T-cell lymphomas are man-
seen in Wegener’s granulomatosis and aged by radiation therapy and chemother-
polymorphic reticulosis, now termed extra- apy combined. Prognosis is variable with
nodal NK/T-cell lymphoma, nasal type. In potential for wide dissemination.
FIGURE 4-33
Osseous destructive ulcers in lymphoma (NK/T cell nasal type, large B cell lymphoma, central lymphoma
of bone).
PMPH_Eversole_Chapter-04.indd 128 1/20/2011 2:19:50 PM
Oral Ulcerations and Fistulae 129
of gummatous necrosis, aortic aneurysm,
Additional Reading peripheral neuropathy, and tabes dorsalis.
Avilés A, Díaz NR, Neri N, Cleto S, Talavera A. The VDRL is positive at this late stage; how-
Angiocentric nasal T/natural killer cell lymphoma: ever, the lesions are essentially noninfective.
a single centre study of prognostic factors in 108
patients. Clin Lab Haematol. 2000;22:215-220. MICROSCOPIC FEATURES
Cuadra-Garcia I, Proulx GM, Wu CL, et al. Sinonasal
lymphoma: a clinicopathologic analysis of 58 cases The tissue adjacent to the zone of pala-
from the Massachusetts General Hospital. Am J Surg tal perforation shows foci of eosinophilic
Pathol. 1999;23:1356-1369.
necrotic aggregates, and the surrounding
Harabuchi Y, Takahara M, Kishibe K, Moriai S, Nagato
T, Ishii H. Nasal natural killer (NK)/T-cell lymphoma: granulation tissue evinces a mononuclear
clinical, histological, virological, and genetic features. inflammatory cell infiltrate. Treponemal
Int J Clin Oncol. 2009;14:181-190. organisms are usually not demonstrable.
Kim J, Kim EY, Lee SK, et al. Extranodal nasal-type
NK/T-cell lymphoma: computed tomography find-
ings of head and neck involvement. Acta Radiol.
DIFFERENTIAL DIAGNOSIS
2010;51:164-169. Palatal perforation by syphilitic gumma
Li YX, Fang H, Liu QF, et al. Clinical Features and treat-
ment outcome of nasal-type NK/T-cell lymphoma of
may be confused clinically with Wegener’s
Waldeyer ring. Blood. 2008;112:3057-3064. granulomatosis, midline lethal granuloma,
malignant reticulosis, mucormycosis, and
TERTIARY SYPHILIS antral carcinoma. Other clinical signs and
Figure 4-34 symptoms that aid in arriving at a diagno-
sis of syphilis are usually present. A VDRL
Age: Elderly adults serologic evaluation should be obtained.
Sex: Male predilection
TREATMENT
CLINICAL FEATURES
Tertiary syphilis should be managed by a
Gummatous necrosis of the oral tissues fre- physician because many of its ramifications
quently involves the palate. The gumma is involve various organ systems.
rubbery with necrotic rolled margins and
often sloughs, leaving a relatively clean,
vacant perforation of the palate. After a
course of antibiotic therapy, large masses
Additional Reading
of necrotic tissue may be lost (Herxheimer’s Bains MK, Hosseini-Ardehali M. Palatal perforations:
past and present. Two case reports and a literature
reaction). Other signs of tertiary syphilis are review. Br Dent J. 2005;199:267-269.
encountered: psychotic behavior with delu- Gaikwad AV et al. Syphilitic palatal perforation and reha-
sions of grandeur, luetic glossitis, other foci bilitation denture. J Indian Dent Assoc. 1986;58:461.
FIGURE 4-34
Gummatous necrosis in
tertiary syphilis.
PMPH_Eversole_Chapter-04.indd 129 1/20/2011 2:19:57 PM
130 Chapter 4
Huebsch RF. Gumma of the hard palate with perfora- are observed. The risk of developing osteora-
tion. Oral Surg Oral Med Oral Pathol. 1955;8:690. dionecrosis is less with newer supravoltage
Meyer I, Shklar G. The oral manifestations of acquired
syphilis. Oral Surg Oral Med Oral Pathol. 1967;23:45. radiation sources such as the linear accelera-
Penneau M et al. Syphilitic necrosis of the incisive bone. tor, betatron, and cobalt-60 machines.
Rev Stomatol Chir Maxillofac. 1980;81:392.
MICROSCOPIC FEATURES
The soft tissues display necrosis with an
OSTEORADIONECROSIS
acute or subacute inflammatory cell infil-
Figure 4-35 trate. The osseous tissue lacks lacunar
Age: Elderly adults
osteocytes; the marrow spaces contain
Sex: Male predilection necrotic debris, microbial colonies, and a
neutrophilic infiltrate not unlike nonspe-
CLINICAL FEATURES cific acute osteomyelitis.
Patients who have received cancericidal
DIFFERENTIAL DIAGNOSIS
radiation to the jaws experience a vascu-
lar derangement in the osseous tissues Because osteoradionecrosis is located
that severely compromises the inflamma- chiefly in the mandible, it is not likely to be
tory defense of the tissue to the onslaught confused with the other osseous destructive
of infection. Odontogenic or periodontal draining lesions included in this section.
infection may become rampant and spread At any rate, a history of radiation therapy
quickly through the bone. The mandible in excess of 6000 rad confirms a diagnosis
is more susceptible than the maxilla. Oral of osteoradionecrosis. Recurrent tumor in
fistulae develop in the involved area, with the area must be ruled out by biopsy when
sequestration of large fragments of necrotic tumefaction surrounds or infiltrates the
bone. Indeed, the entire alveolar ridge may involved osseous tissue.
show ulceration and drainage with exposure
TREATMENT
of nearly one half the mandible. Lesions are
usually exudative with a foul odor. Pain is Sequestra should be carefully removed and
invariably present. Radiographically, moth- the area debrided. When extensive areas of
eaten radiolucencies with opaque sequestra necrosis are present, surgical intervention
FIGURE 4-35
Osseous sequestrum in
a patient who received
radiation for a mandibular
alveolar ridge squamous
cell carcinoma.
PMPH_Eversole_Chapter-04.indd 130 1/20/2011 2:20:05 PM
Oral Ulcerations and Fistulae 131
should be delayed. The patient requires unless the patient is suffering from debilitat-
hospitalization with supportive care and ing illness. Patients with diabetes or wide-
intravenous antibiotic therapy. Hyperbaric spread lymphoma and those receiving anti-
oxygen therapy has been shown to be effec- tumor chemotherapeutic agents are the most
tive in facilitating healing in some cases. frequent sufferers. The antrum is usually the
Prevention is the key to management. All site of origin of the infection. As the antrum
pulpally or periodontally infected teeth becomes progressively eroded by necrotic
should be extracted or treated before and granulation tissues, perforation ensues
radiation; posttherapeutically, a strict oral with osseous destruction and oroantral fis-
hygiene program should be instituted with tula formation. Anesthesia or paresthesia of
inclusion of daily topical application of fluo- the second division of the trigeminal nerve
ride gels to the remaining dentition. frequently occurs. The infected antrum is
opacified on panoramic or Water’s sinus
Additional Reading radiographs, and evidence of bony erosion of
the antral walls can be visualized, especially
Cook HP. Tooth extraction and radiation therapy of the on tomograms. Aspergillosis may manifest
mouth. Br Dent J. 1966;120:372. features identical to those of mucormycosis
Hart GB, Mainous EG. The treatment of radiation necrosis when the antrum is involved.
with hyperbaric oxygen (OHP). Cancer. 1976;37:2580.
Jacobson AS, Buchbinder D, Urken ML. Reconstruction
of bilateral osteoradionecrosis of the mandible using a MICROSCOPIC FEATURES
single fibular free flap. Laryngoscope. 2010;120:273-275.
Motila E, Westerholm N. Osteoradionecrosis of the jaw.
The granulation and necrotic tissues con-
Odontol Tidskr. 1965;73:239. tain colonies of large hyalinized baso-
Silverman S, Jr. Radiation effects. Oral Cancer. New philic hyphae that are devoid of septae.
York, The American Cancer Society; 1981:66. Inflammatory cells, chiefly neutrophils and
eosinophils, prevail in the granulation tis-
sue that is located peripheral to widespread
MUCORMYCOSIS zones of necrosis. Vascular invasion by the
Figure 4-36 microorganism is common and results in
ischemic necrosis with infarction.
Age: No predilection
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
Palatal osseous destructive lesions of
Mucormycosis is an infection caused by one mucormycosis may simulate nonspecific
of the phycomycetes and is not pathogenic oroantral fistula, midline lethal granuloma,
FIGURE 4-36
Necrotic osseous destruc-
tion of the palate in antral
mucormycosis.
PMPH_Eversole_Chapter-04.indd 131 1/20/2011 2:20:10 PM
132 Chapter 4
Wegener’s granulomatosis, and malignant ANTRAL CARCINOMA
disease. A history of diabetes should arouse Figure 4-37
suspicion of mucormycosis. Biopsy discloses
the presence of the infectious agent. Age: Elderly adults
Sex: Male predilection
TREATMENT
CLINICAL FEATURES
Because mucormycosis is a secondary
invader, the underlying medical illness Cancer of the maxillary sinus develops
must be treated concurrently with the infec- insidiously and is extensive when per-
tion. Intravenous administration of ampho- foration of bone occurs. The carcinoma
tericin B is the treatment of choice. may extend and perforate through any of
the antral walls. The palate is a frequent
site, with formation of osseous destruc-
Additional Reading tive zones rimmed by necrotic tissue.
Tumefaction may herniate through the
Blitzer A et al. Patient survival factors in paranasal sinus
mucormycosis. Laryngoscope. 1980;90:635. perforation; however, the oroantral com-
Brown OE et al. Mucormycosis of the mandible. J Oral munication is more often a simple ulcer-
Maxillofac Surg. 1986;44:132. ated perforation. The malar skin often
Rapidis AD. Orbitomaxillary mucormycosis (zygomyco- shows erythema with facial swelling.
sis) and the surgical approach to treatment: perspec-
tives from a maxillofacial surgeon. Clin Microbiol Displacement of the nasal septum and
Infect. 2009;15(suppl 5):98-102. globe is also frequently encountered.
Savetsky L, Waltner J. Aspergillosis of the maxil- Second-division anesthesia or paresthe-
lary antrum. Arch Otolaryngol Head Neck Surg. sia is a frequent symptom. Water’s sinus,
1961;74:695.
Taylor CG et al. Mucormycosis (polycomycosis) involv-
panographic, and antral tomograms show
ing the maxilla. Oral Surg Oral Med Oral Pathol. opacification and osseous destruction of
1969;27:806. the sinus walls.
FIGURE 4-37
Ulceration and palatal destruc-
tion in antral carcinoma.
PMPH_Eversole_Chapter-04.indd 132 1/20/2011 2:20:13 PM
Oral Ulcerations and Fistulae 133
MICROSCOPIC FEATURES Liu FC. A classification system for maxillary sinus carcino-
ma. Arch Otolaryngol Head Neck Surg. 1987;113: 409.
Tissue removed from around the site of per- Merrick RE, Rhone DP, Chilis TJ. Malignant fibrous
foration shows infiltrating islands, cords, histiocytoma of the maxillary sinus. Arch Otolaryngol
and nests of tumor cells. Their morpho- Head Neck Surg. 1980;106:365.
logic characteristics vary from squamous
to adenomatous differentiation. Metastatic
tumors and sarcomas may also arise in the
BISPHOSPHONATE-RELATED
antrum and invade the palate. OSTEONECROSIS OF
THE JAWS
DIFFERENTIAL DIAGNOSIS Figure 4-38
When antral carcinoma extends into the
Age: Elderly
oral cavity with palatal perforation, other Sex: No predilection
osseous destructive lesions including mid-
line lethal granuloma, syphilitic gumma, CLINICAL FEATURES
and mucormycosis must be considered in Patients with metastatic bone disease, mel-
the differential diagnosis. anoma, and generalized osteoporosis are
often treated with intravenous bisphopho-
TREATMENT nates such as zoledronate and pamidronate
Antral carcinoma carries an extremely poor in order to increase bone mass. A subpopu-
prognosis. It is treated surgically, radiothera- lation of these subjects develop osteonecro-
peutically, or with a combination of the two, sis of the jaws. Recently, patients taking oral
and should be managed by an oncologist. preparations of bisphosphonates have also
developed sequestrating lesions, usually
in the mandible, yet also in the palate and
Additional Reading maxillary alveolus. Prior trauma or extrac-
tions are reported in many of these patients,
Ahmad K, Cordoba RB, Fayos JV. Squamous cell carci-
noma of the maxillary sinus. Arch Otolaryngol Head yet a significant proportion develop the
Neck Surg. 1981;107:48. condition without any provocation. The
Chaudhry AP et al. Carcinoma of the antrum. Oral Surg lesions are painful and ulcerative without
Oral Med Oral Pathol. 1960;13:269. significant tumefaction, and at the time of
Huang JS, Kok SH, Lee JJ, Hsu WY, Chiang CP, Kuo YS.
Extensive maxillary sequestration resulting from mucormy- examination, sequestra can be seen in the
cosis. Br J Oral Maxillofac Surg. 2005;43: 532-534. base of the ulcers. Radiographs disclose
FIGURE 4-38
Ulceration and exposure
of underlying bone in
bisphosphonate-related
osteonecrosis of the jaws.
PMPH_Eversole_Chapter-04.indd 133 1/20/2011 2:20:24 PM
134 Chapter 4
irregular, ragged opacities usually sur- TREATMENT
rounded by a resorptive radiolucency. The Systemic antibiotics, sequestrectomy with
risk for developing osteonecrosis while tak- gentle nonaggressive debridement, and
ing bisphosphonates can be quite reliably betadine rinses are recommended along
predicted by ordering serum C-terminal with bisphosphonate withdrawal.
telopeptide (CTX). High levels are indica-
tive of decreased risk for jaw necrosis (150
pgm/ml).
Additional Reading
MICROSCOPIC FEATURES Almazrooa SA, Woo SB. Bisphosphonate and nonbispho-
sphonate-associated osteonecrosis of the jaw: a review.
Nonvital trabeculae show lacunae devoid J Am Dent Assoc. 2009;140:864-875.
of osteocyte nuclei with adherent microbial Colella G, Campisi G, Fusco V. American Association of
colonies. Many of the colonies are PAS posi- Oral and Maxillofacial Surgeons position paper: bis-
tive with a peripheral fringe and periph- phosphonate-related osteonecrosis of the Jaws-2009
update: the need to refine the BRONJ definition. J
eral neutrophils typical for actinomycotic
Oral Maxillofac Surg. 2009;67:2698-2699.
organisms. Marx RE. Pamidronate (Aredia) and zoledronate
(Zometa) induced avascular necrosis of the jaws: a
DIFFERENTIAL DIAGNOSIS growing epidemic. J Oral Maxillofac Surg. 2003;61:
1115-1117.
Sequestra of other etiologies must be consid- Marx RE, Cillo JE, Jr, Ulloa JJ. Oral bisphosphonate-
ered in the differential diagnosis, including induced osteonecrosis: risk factors, prediction of risk
odontogenic osteomyelitis, trauma, intuba- using serum CTX testing, prevention, and treatment. J
Oral Maxillofac Surg. 2007;65:2397-2410.
tion, if lesions are located on the posterior- Naik NH, Russo TA. Bisphosphonate-related osteone-
lingual mandibular mucosa and postradia- crosis of the jaw: the role of actinomyces. Clin Infect
tion osteonecrosis to mention a few. Dis. 2009;49:1729-1732.
PMPH_Eversole_Chapter-04.indd 134 1/20/2011 2:20:30 PM
PMPH_Eversole_Chapter-04.indd 135 1/20/2011 2:20:30 PM
a b
Normal mucosa Intraepithelial viral vesicle
c d
Suprabasilar bulla Sub-basilar bulla
e f
Intrabasilar bulla Erosion desquamation
Vesiculobullous Lesions
PMPH_Eversole_Chapter-05.indd 136 1/17/2011 3:30:04 PM
Vesiculobullous
and Desquamative
Lesions
5
BENIGN MUCOUS MEMBRANE
Febrile-Associated Vesicular PEMPHIGOID 152
Eruptions 139
BULLOUS LICHEN PLANUS 154
HERPETIC GINGIVOSTOMATITIS 139 ERYTHEMA MULTIFORME 155
HERPANGINA 140 STEVENS-JOHNSON SYNDROME 156
HAND-FOOT-AND-MOUTH PARANEOPLASTIC PEMPHIGUS 157
DISEASE 141 ANGINA BULLOSA
PRIMARY VARICELLA-ZOSTER HEMORRHAGICA 158
(CHICKENPOX) 143
EPIDERMOLYSIS BULLOSA 159
SECONDARY VARICELLA-ZOSTER
DERMATITIS HERPETIFORMIS
(SHINGLES) 144
(GLUTEN ENTEROPATHY) 161
Nonfebrile-Associated Desquamative Lesions 161
Vesicular Eruptions 145
GINGIVOSIS (DESQUAMATIVE
RECURRENT HERPES STOMATITIS 145
GINGIVITIS) 161
RECURRENT HERPES LABIALIS 146
EROSIVE LICHEN PLANUS 163
CONTACT VESICULAR
STOMATITIS 148 LICHENOID CONTACT
STOMATITIS 164
IMPETIGO 149
CHRONIC ULCERATIVE
STOMATITIS 165
Bullous Diseases 150
PYOSTOMATITIS VEGETANS 166
PEMPHIGUS VULGARIS 150 TOOTHPASTE IDIOSYNCRATIC
BULLOUS PEMPHIGOID 151 LESIONS 168
PMPH_Eversole_Chapter-05.indd 137 1/17/2011 3:30:07 PM
Vesicles are fluid-filled blisters measur- or inclusion bodies. The specific diagnosis
ing less than 5 mm; bullae are blisters in of viral vesicular eruptions is obtained by
excess of 5 mm. On skin, vesicles and bul- observing the pattern of distribution of the
lae are bleb-like and tense. In the oral cav- lesions. These features are enumerated for
ity, both vesicles and bullae are more flat- each entity.
tened, with a smooth gelatinous surface. The bullous dermatoses are skin dis-
Because of chronic masticatory forces and eases characterized by bulla formation.
a less rigid epithelial surface, oral vesicles All of the diseases included here manifest
and bullae are prone to rupture, leaving precedent or coexistent oral bullae. One
ulcerative and desquamative lesions later disease, benign mucous membrane pem-
in the course of disease. When ulcers, ero- phigoid (BMMP), is limited to the mucous
sions, and desquamations are observed membranes. The bullous lesions themselves
in the mouth, a search should be made to may appear identical from one disease to
detect intact fluid-filled surface lesions; the the next. Biopsy is mandatory to arrive at a
history should be investigated for indica- definitive diagnosis in most patients. Some
tions that the early lesions were blister-like of the entities in this group show specific
from onset. site distributions or are accompanied by
When attempting to differentiate skin manifestations that evince a diagnostic
between a disease that is primarily vesicu- pattern or configuration. These features are
lar and one that is bullous, the size of the detailed in the text. An immunopathogen-
individual lesions is the key to diagnosis. esis underlies the mechanism of bulla for-
One must, however, be cognizant of the mation in most of these disorders. Some of
fact that vesicles often cluster together and these diseases are T–cell–mediated, whereas
may appear bullous. Furthermore, a ten- others are antibody-mediated autoimmune
dency for clustering of vesicles in a local- processes.
ized area is most suggestive of herpesvirus A final group of disorders in this chap-
infection. ter include those in which large areas of
The vesicular diseases are primarily epithelial detachment occur. Bullae do not
infectious and, specifically, most are the form; rather, diffuse zones of sloughing or
result of assault by viral organisms that desquamation ensue and are often accom-
propagate in epithelial cells and are har- panied by intense erythema.
bored as dormant virus in sensory nerve The most common vesicular diseases
ganglion nuclei. Of utmost importance in are primary herpetic gingivostomatitis and
arriving at a definitive diagnosis is evalu- secondary herpes labialis. Frequent recur-
ation of the patient’s temperature. For this rences of shingles may accompany underly-
reason, vesicular eruptions of the mouth ing malignant lymphoma.
have been divided into those associated with Most of the bullous dermatoses are
elevated temperature and those in which rare. Erythema multiforme is the most
the patient is afebrile. The latter group may common disease in this group. Pemphigus
occasionally manifest mild elevation in vulgaris and certain forms of epidermolysis
temperature; if detected, it is invariably less bullosa are potentially lethal.
than 100°F. When viral infections are sus- All three diseases included with the
pected, a cytologic smear of intact vesicular desquamative group are relatively common,
contents often reveals the presence of viral- erosive lichen planus being most prevalent.
specific nuclear ballooning degeneration None is lethal.
PMPH_Eversole_Chapter-05.indd 138 1/17/2011 3:30:07 PM
Vesiculobullous and Desquamative Lesions 139
identical. The vesicles rapidly rupture, leav-
Febrile-Associated Vesicular ing a raw or white pseudomembranous ero-
Eruptions sion. Erythema surrounds the vesicular and
ulcerative zones. The oropharynx is involved
HERPETIC only occasionally. The lesions are painful,
GINGIVOSTOMATITIS and eating is a significant problem. The
Figure 5-1 temperature is elevated and may approach
103 to 104°F. Constitutional symptoms of
Age: Children and young adults inflammatory disease, including malaise
Sex: No predilection and cervical lymphadenopathy, are present.
The disease is contagious; however, most
CLINICAL FEATURES
individuals exposed to it are either already
Primary infection with herpesvirus homi- immune or suffer only subclinical manifes-
nis type 1 of the oral cavity is characterized tations, such as transient fever. During the
by multiple vesicular eruptions located on course of infection, antiherpes antibody
the attached gingiva and movable musosa, titer is elevated. The disease runs its course
chiefly the lips and buccal mucosa. Type 2 in 10 to 14 days, and healing develops with-
herpesvirus can also cause primary her- out scar formation. Rarely, complications
petic gingivostomatitis, being transmitted develop, particularly in debilitated children
by either oral-oral or genito-oral routes. and infants. The Pospischill-Feyrter syn-
Regardless of the genotypic forms of her- drome and Kaposi’s varicelliform eruption
pes simplex, the clinical manifestations are are disseminated herpes infections that are
FIGURE 5-1
Marginal gingivitis with
ulceration accompanied
by small vesicles with ery-
thematous halos that rap-
idly desquamate to yield
ulcers in primary herpetic
gingivostomatitis.
PMPH_Eversole_Chapter-05.indd 139 1/17/2011 3:30:07 PM
140 Chapter 5
potentially lethal. Herpesvirus infections soothing mouth rinse composed of equal
may also occur on the facial skin and con- parts of an antihistamine elixir with Kao-
junctiva. Contact with infected patients by pectate is useful in adults. One percent
dentists and oral health auxiliary personnel viscous lidocaine is recommended for chil-
who have never been exposed to the dis- dren. Acyclovir therapy shortens the dura-
ease may result in herpetic whitlow, a viral tion of disease. Severe orofacial herpes
dermatitis of the finger. infections may develop in immunocompro-
mised patients; in such instances, treatment
MICROSCOPIC FEATURES with acyclovir is recommended. Although
Intraepithelial vesicle formation is seen this antiviral medication is beneficial, an
with necrotic exudate and a neutrophilic acyclovir-resistant mutant organism that
infiltrate. Eosinophilic inclusion bodies escapes treatment may evolve. Preliminary
(Lipschütz bodies) in the vesicular space animal studies indicate that chlorhexidine
are accompanied by epithelial cells showing rinses may be virocidal.
nuclear ballooning degeneration. Immu-
noperoxidase staining with type-specific
antisera helps to differentiate types 1 and Additional Reading
2, provided the lesion is sampled before day Amir J. Clinical aspects and antiviral therapy in primary
4 of the infection. These viral infection-spe- herpetic gingivostomatitis. Paediatr Drugs. 2001;3:593-
cific changes are not obvious in ulcerated 597.
vesicles. Lennette EH, Magoffin, RL. Virologic and immunologic
aspects of major oral ulcerations. J Am Dent Assoc.
1973;87:1055.
DIFFERENTIAL DIAGNOSIS Saral R, Burns WH, Laskin OL, Santos GW, Lietman PS.
The vesiculoulcerative lesions of herpes Acyclovir prophylaxis of herpes-simplex-virus infec-
tions: a randomized, double-blind controlled trial in
are often confused with recurrent aphthae. bone-marrow-transplant recipients. N Engl J Med.
Aphthae are not associated with a highly 1981;305:63.
elevated temperature, and there is a history Scully C. Orofacial herpes simplex virus infections:
of recurrent episodes. Herpetic gingivos- current concepts in the epidemiology, pathogen-
esis, and treatment, and disorders in which the virus
tomatitis does not recur intraorally, with the may be implicated. Oral Surg Oral Med Oral Pathol.
exception of recurrent herpetic stomatitis, 1989;68:701.
which usually manifests microvesicles local- Silverman S Jr, Beumer J, III. Primary herpetic gingi-
ized unilaterally on the palatal gingiva. Pri- vostomatitis of adult onset. Oral Surg Oral Med Oral
Pathol. 1973;36:496.
mary herpes can be differentiated from cox-
sackievirus infections on the basis of lesional
distribution, the latter being localized to the
oropharynx. Shingles, seen in older individ-
HERPANGINA
uals and with unilateral lesions, can be ruled Figure 5-2
out on the basis of age and distribution. The
Age: Children
gingival lesions of primary herpes can be Sex: No predilection
confused with acute necrotizing ulcerative
gingivitis; however, the latter fails to show CLINICAL FEATURES
vesicles on nongingival mucosa. Infection with Group A coxsackieviruses
and enterovirus 71 (EV-71) may produce
TREATMENT
herpangina. The disease is limited to the
Supportive care consists of prescribing a oropharynx with vesicles located primarily
soft diet: milkshakes, baby foods, and liq- on the soft palate and faucial pillars. Exten-
uids. Aspirin reduces fever and pain. A sion anteriorly is rare. The lesions are pain-
PMPH_Eversole_Chapter-05.indd 140 1/17/2011 3:30:40 PM
Vesiculobullous and Desquamative Lesions 141
FIGURE 5-2
Multiple erythematous
vesicles limited to the soft
palate and oropharynx in
herpangina, a coxsackievi-
rus infection.
ful and are accompanied by generalized
oropharyngitis evidenced by erythema of Additional Reading
the throat. The vesicles tend to cluster and Chawareewong S, Kiangsiri S, Lokaphadhana K, et al.
become ulcerated 3 to 4 days after onset. Neonatal herpangina caused by Coxsackie A-5 virus.
Fever, malaise, lymphadenitis, headache, J Pediatr. 1978;93:492.
and sore throat develop. The disease shows Cherry JD, Hahn CL. Herpangina: the etiologic spec-
trum. Pediatrics. 1965;36:632.
an incubation period of 1 week or less and Kung CM, King CC, Lee CN, et al. Differences in
runs its course in the same amount of time. replication capacity between enterovirus 71 isolates
Meningitis is a complication but is usually obtained from patients with encephalitis and those
self-limited. The disease is contagious, and obtained from patients with herpangina in Taiwan.
J Med Virol. 2007;79(1):60-68.
outbreaks among school-age children are Lennette EH, Magoffin RL. Virologic and immunologic
common. EV-71, more often encountered aspects of major oral ulcerations. J Am Dent Assoc.
in Asian countries, may also cause severe 1973;87:1055.
neurologic damage when it infects the Wang SM, Liu CC. Enterovirus 71: epidemiology, patho-
genesis and management. Expert Rev Anti Infect Ther.
CNS. 2009;7:735-742.
MICROSCOPIC FEATURES
Intraepithelial vesicles contain an eosino- HAND-FOOT-AND-MOUTH
philic exudate, and nuclear ballooning DISEASE
degeneration of epithelial cells is a feature. Figure 5-3
DIFFERENTIAL DIAGNOSIS Age: Children and young adults
Sex: No predilection
Herpangina must be differentiated from
infection by herpesvirus and varicella- CLINICAL FEATURES
zoster virus and, when ulceration pre- Group A coxsackieviruses and enterovirus
dominates, from aphthae. The limitation 71 are responsible for the vesicular eruption
of lesions to the soft palate/faucial region of hand-foot-and-mouth disease with EV-71
is essentially diagnostic. Virus may be more often encountered in Asia. The disease
retrieved from stool specimens by tissue is more often seen in spring and summer in
culture techniques. preschool and school children and is mildly
contagious. The distribution of lesions is
TREATMENT pathognomonic in that, after a short incuba-
A palliative oral rinse, such as an antihista- tion period, vesicles with an erythematous
mine elixir mixed 50:50 with Kaopectate, is halo appear in the oral cavity, on the hands,
advised. Soft diet and antipyretics are rec- and on the feet. The oral lesions are located
ommended as well. primarily on the lips and buccal mucosa,
PMPH_Eversole_Chapter-05.indd 141 1/17/2011 3:30:40 PM
142 Chapter 5
FIGURE 5-3
Hand-foot-and-mouth dis-
ease, caused by a coxsacki-
evirus and showing vesicu-
loulcerative lesions of the
oral mucous membranes
accompanied by a vesicular
eruption of the hands and
feet.
sparing the oropharynx. Within 24 to 48 DIFFERENTIAL DIAGNOSIS
hours, the oral vesicles rupture, leaving The oral vesiculoulcerative lesions are simi-
erosions or ulcerations with a white or grey lar to those encountered in herpetic gin-
pseudomembrane. The extremity lesions givostomatitis, herpangina, varicella, and
are limited to the skin below the knees and aphthous stomatitis. The distribution of
elbows, are vesicular with circumferential lesions in hand-foot-and-mouth disease is
erythema, and are located on both dorsal diagnostic and eliminates these other enti-
and ventral surfaces of the hands and feet. ties from consideration. Coxsackie virus can
All lesions are painful, and constitutional be cultured from stool specimens.
signs of infection include elevated tempera-
ture, malaise, and lymphadenopathy. EV-17 TREATMENT
may also cause encephalitis.
Antipyretic-analgesics, soft or liquid diet,
fluids, and a soothing oral rinse such as an
MICROSCOPIC FEATURES
antihistamine elixir mixed 50:50 with Kao-
Intraepithelial vesicles are seen in the early pectate are recommended. Viscous lido-
stages with intracytoplasmic eosinophilic caine may be used in small children.
inclusion bodies. Later stages are character-
ized by shallow ulcerations and erosions
with regeneration of the marginal epithe- Additional Reading
lium. A superficial inflammatory cell infil- Buchner A. Hand, foot, and mouth disease. Oral Surg
trate is present in the submucosa. Oral Med Oral Pathol. 1976;41:333.
PMPH_Eversole_Chapter-05.indd 142 1/17/2011 3:31:00 PM
Vesiculobullous and Desquamative Lesions 143
Cawson RA, McSwiggan DA. An outbreak of hand, foot cella-zoster such that the disease is rarely
and mouth disease in a dental hospital. Oral Surg Oral encountered now in developed countries.
Med Oral Pathol. 1969;27:451.
Cherry JD, Jahn CL. Hand, foot and mouth syndrome. Nevertheless, many adults who contracted
Pediatrics. 1966;37:637. chickenpox during childhood harbor latent
Southam JC, Colley IT. Hand, foot, and mouth disease. VZV in ganglia and may develop shingles.
Br Dent J. 1968;125:298.
Wong SS, Yip CC, Lau SK, Yuen KY. Human enterovi-
rus 71 and hand, foot and mouth disease. Epidemiol MICROSCOPIC FEATURES
Infect. 2010;8:1-19.
Superficial intraepithelial vesicle forma-
tion is present. The vesicular contents con-
PRIMARY VARICELLA-ZOSTER tain eosinophilic exudate, inflammatory
cells, and epithelial cells. Nuclear balloon-
(CHICKENPOX)
ing degeneration is a feature. A superficial
Figure 5-4 submucosal inflammatory cell infiltrate is
Age: Children
discernible.
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
Oral vesiculoulcerative lesions of chicken-
Chickenpox is a dermal vesicular exan-
pox resemble those of herpes, the coxsacki-
them caused by the varicella-zoster virus.
eviruses, and aphthae. The skin lesions pre-
The incubation period lasts 2 to 3 weeks.
dominate and must be differentiated from
The lesions are located primarily on the
smallpox and Kaposi’s varicelliform erup-
trunk and face, are vesicular with an ery-
tion, the latter caused by dermatotrophic
thematous boundary, and are extremely
herpevirus. Antibody titers to varicella-
pruritic. Fever, malaise, and mild general-
zoster are elevated.
ized lymphadenopathy are present. Oral
manifestations are common, with early
TREATMENT
onset of vesicles that rapidly rupture and
leave erosions with a surface pseudomem- Although complications are rare, it is nev-
brane. These lesions are limited in extent. ertheless recommended that children with
The palatal mucosa is the predominant oral chickenpox be under the care of a pediatri-
location. The lesions resolve within 5 to 8 cian. Oral lesions may be treated palliatively
days. Most childhood vaccines include vari- with viscous lidocaine.
FIGURE 5-4
Focal vesicles seen in the
mouth, usually the soft pal-
ate area in children with
the typical dermal vesicular
exanthem of chickenpox.
PMPH_Eversole_Chapter-05.indd 143 1/17/2011 3:31:53 PM
144 Chapter 5
distribution of sensory nerves, being seg-
Additional Reading mental and unilateral. Prodromal neural-
Badger GR. Oral signs of chickenpox (Varicella): report gia is followed by clustered vesicular erup-
of two cases. ASDC J Dent Child. 1980;47:349. tions. Although the thoracic and abdominal
Blank H, Rake G. Viral and Rickettsial Diseases of the nerves are most frequently involved, the
Skin, Eye, and Mucous Membranes of Man. Boston, mucosa supplied by the second or third
MA: Little, Brown and Co; 1955.
Glanz JM, McClure DL, Magid DJ, et al. Parental refusal division of the trigeminal nerve may be the
of varicella vaccination and the associated risk of vari- site of infection if the virus is harbored and
cella infection in children. Arch Pediatr Adolesc Med. propagated within the Gasserian ganglion.
2010;164:66-70. The vesicles are unilaterally distributed,
Lennette EH, Magoffin RL. Virologic and immunologic
aspects of major oral ulcerations. J Am Dent Assoc.
stop at the midline, and are extremely pain-
1973;87:1055. ful. Patients experiencing multiple recur-
Myers MG. Varicella and herpes zoster: comparisons in rent episodes of shingles have been shown
the old and young. Geriatrics. 1977;32:77. to be at risk for lymphoma, leukemia, and
carcinomatosis; a single episode does not
connote any increased risk for malignancy.
SECONDARY VARICELLA- After healing of shingles, postherpetic neu-
ZOSTER (SHINGLES) ralgia may develop. The disease has a 1- to
Figure 5-5 3-week incubation period, and the vesicular
stage may persist for 1 to 5 weeks. Constitu-
Age: Adults and elderly people tional signs of infectious disease, including
Sex: Slight male predilection elevated temperature, malaise, and lymph-
adenitis, are apparent.
CLINICAL FEATURES
When trigeminal shingles occurs in
Shingles is caused by reactivation of varicel- young males, underlying human immuno-
la-zoster virus and may be conceptualized deficiency virus (HIV) infection should be
as a recurrent form of chickenpox. In the suspected. Indeed, any individual consid-
secondary or recurrent form, it is neuroder- ered to be at risk for AIDS showing classic
matropic. The virus propagates within gan- clinical features for shingles should be eval-
glia, and the vesicular eruption follows the uated serologically for HIV infection.
FIGURE 5-5
Reactivation by the vari-
cella-zoster virus, which
causes shingles. The lesions
begin as small vesicles that
are unilateral, with a ten-
dency to follow the sen-
sory nerve pathways.
PMPH_Eversole_Chapter-05.indd 144 1/17/2011 3:32:28 PM
Vesiculobullous and Desquamative Lesions 145
MICROSCOPIC FEATURES Schiødt M, Rindum J, Bygbjert I. Chickenpox with
oral manifestations in an AIDS patient. Dan Dent J.
The epithelium manifests intraepithelial vesi- 1987;91:316.
cles with epithelial nuclear ballooning degen-
eration. The subjacent submucosa contains a
mononuclear inflammatory cell infiltrate. Nonfebrile-Associated
DIFFERENTIAL DIAGNOSIS
Vesicular Eruptions
Oral vesiculoulcerative eruptions of shingles RECURRENT HERPES
mimic those observed in herpesvirus, cox- STOMATITIS
sackievirus, and aphthous stomatitis. Uni- Figure 5-6
lateral segmental distribution, prevalence
in adults, and severe pain are features that Age: Young adults
allow for clinical differentiation. Antibody Sex: No predilection
titers to varicella-zoster virus are elevated.
CLINICAL FEATURES
Systemic malignancy should be ruled out.
Recurrent infection of the oral mucosa by
TREATMENT herpesvirus hominis type 1 is uncommon.
When it occurs, it is usually restricted to the
Varicella-zoster virus infections in the form
palatal gingiva unilaterally and is charac-
of shingles restricted to the oral mucosa can
terized by the formation of microvesicles
be treated by prescribing soft or liquid diet,
that rapidly rupture to leave small punctate
analgesic-antipyretic medication, and a pal-
ulcerations with a tendency to cluster. Even
liative oral rinse such as an antihistamine
less common is the appearance of vesicles
elixir mixed with equal parts of Kaopectate.
of the buccal mandibular gingiva in the
Definitive antiviral therapy with 1000 mg
vicinity of the mental foramen or the buc-
acyclovir should be initiated at the onset
cal maxillary gingiva and adjacent buccal
of the eruption. Should multiple recurrent
mucosa. The lesions are slightly painful
episodes occur, referral to a physician or
and persist for only 5 to 7 days. Fever and
dermatologist is recommended; search for
malaise are usually not present.
underlying lymphoma, leukemia, wide-
Importantly, HIV-infected patients are
spread cancer, or HIV infection must be
subject to recurrent orofacial herpetic infec-
undertaken.
tion, and such infections, although vesicu-
lar, do not always show the usual patterns.
Additional Reading MICROSCOPIC FEATURES
Chaconas CP. Herpes zoster, a primary manifestation of
chronic lymphocytic leukemia. Oral Surg Oral Med The epithelium contains small vesicles with
Oral Pathol. 1961;14:942. epithelial nuclear ballooning degeneration.
Inoue H, Motani-Saitoh H, Sakurada K, et al. Detection The submucosa displays a mild mononu-
of varicella-zoster virus DNA in 414 human trigeminal
ganglia from cadavers by the polymerase chain reac-
clear inflammatory cell infiltrate.
tion: a comparison of the detection rate of varicella-
zoster virus and herpes simplex virus type 1. J Med DIFFERENTIAL DIAGNOSIS
Virol. 2010;82:345-349.
Nally FF, Ross IH. Herpes zoster of the oral and facial Recurrent oral herpetic vesicular eruptions
structures. Report of five cases and discussion. Oral are distributed unilaterally and must be
Surg Oral Med Oral Pathol. 1971;32:221.
Ragozzino MW, Melton LJ, Kurland LT, Chu CP, Perry
differentiated from the lesions of shingles.
HO. Risk of cancer after herpes zoster. A population- Because pain is not severe and resolution
based study. N Engl J Med. 1982;307:393. is rapid, the distinction can usually be
PMPH_Eversole_Chapter-05.indd 145 1/17/2011 3:33:08 PM
146 Chapter 5
FIGURE 5-6
Clustered painful microve-
sicles, which quickly rup-
ture in intraoral herpes.
Most cases are located on
the palatal gingiva but may
also follow the distribution
of the long buccal nerve.
made. Recall that the sine qua non for her-
pes simplex recurrent infection is cluster- Additional Reading
ing of vesicles, confined to a limited area of Griffin JW. Recurrent intraoral herpes simplex virus infec-
the mucosa. Antiherpes antibody titers are tions. Oral Surg Oral Med Oral Pathol. 1965;19:209.
elevated during the course of infection. Dif- Phelan JA, Saltzman BR, Friedland GH, Klein RS.
ferentiation from recurrent aphthae is not Oral findings in patients with acquired immunodefi-
ciency syndrome. Oral Surg Oral Med Oral Pathol.
difficult; intraoral recurrent herpes lesions 1987;64:50-56.
are microvesicles or tiny clustering punctate Sheridan PJ, Herrmann EC. Intraoral lesions of adults
ulcerations of attached mucosa, whereas associated with herpes simplex virus. Oral Surg Oral
aphthae do not tend to involve mucosa fixed Med Oral Pathol. 1971;32:390-397.
Southam JC. Recurrent intraoral herpes simplex infec-
to bone. Herpetic lesions that fail to resolve tions. Br Dent J. 1969;127:276.
within 4 weeks are highly suspected for HIV Weathers DR, Griffin JW. Intraoral ulcerations of recur-
infection. Indeed, orofacial herpes persist- rent herpes simplex and recurrent aphthae: two dis-
ing more than 30 days with HIV positivity tinct clinical entities. J Am Dent Assoc. 1970;81:81-87.
fulfills the criteria for a diagnosis of AIDS.
TREATMENT RECURRENT HERPES LABIALIS
Figure 5-7
No treatment is necessary. Elective palliative
mouth rinses may be employed. Alterna- Age: Adults
tively, persistant herpes associated with AIDS Sex: No predilection
should be treated with oral or intravenously
CLINICAL FEATURES
administered acyclovir. In some patients, the
lesions are nonresponsive and may require Recurrent infection of the lips by herpesvi-
therapy with other antiviral agents. rus hominis type 1 is herpes labialis. Vesicles
PMPH_Eversole_Chapter-05.indd 146 1/17/2011 3:33:08 PM
Vesiculobullous and Desquamative Lesions 147
FIGURE 5-7
Vesicular eruptions of the
lips with erythema and
edema typically encoun-
tered in recurrent herpes
labialis (cold sores). Early
lesions (left), crust stage
(right).
occur in clusters on the vermilion border tact dermatitis. Focal clustering of lesions,
and adjacent perioral skin of the lips. Edema, history of trauma or sun exposure, ten-
which may be severe, and erythema under- dency to occur in young adults, lack of
lie the vesicles. The patient is usually afe- linear streaking, and inability to correlate
brile. The vesicles are associated with pain. onset with contact by a potential allergen
Because of their location, they are unsightly. aid in eliminating these latter diseases from
The oral cavity is free of disease. Various fac- consideration. A cytologic smear of vesicu-
tors trigger the infection, including trauma lar contents discloses the presence of viral-
and sunlight (ultraviolet light) exposure, specific cytologic alterations.
even though the patients possess antiherpes
antibody. Evidence implicates a latent prop- TREATMENT
erty to the virus, which may remain seques- Photoactivated dye treatments are contrain-
tered from the immune system by residing dicated in light of studies implicating car-
in ganglia. During latent periods, no symp- cinogenic transformation. Topical antiviral
toms or lesions are encountered. agents, including acyclovir and its ana-
As noted previously with regard to logues are marginally effective in clearing
recurrent intraoral herpetic stomatitis, per- vesicles early. Alternatively, systemically
sistent herpes labialis may be indicative of administered acyclovir 400 mg taken daily
an immunocompromised status, including will prevent the occurrence of the infec-
HIV infection. In such instances, lesional tion among patients who initially pres-
involvement may be extensive. ent with severe and frequent recurrences.
Subsequent to rupture of the vesicles, a
MICROSCOPIC FEATURES
topical steroid cream with antibiotic can be
Cytologic smears of nonruptured vesicles applied. Steroid-antibiotic preparations can
disclose the presence of nuclear ballooning be combined with 1% anesthetics to achieve
degeneration. Microscopic sections are rep- pain control. Caution should be taken not
resented by the presence of intraepithelial to prescribe steroid creams during the early
vesicles with the same cytologic changes infective stage of the disease (i.e., the first
already specified for primary herpes. The 3 to 4 days). Oral or intravenous acyclovir
submucosa or dermis evinces an inflamma- therapy is indicated in immunocompro-
tory cell infiltrate. mised patients; even so, some individuals
harbor thymidine kinase-resistant strains
DIFFERENTIAL DIAGNOSIS
and may require other antiviral medica-
Recurrent herpes labialis shows vesicles tions to control the disease. Prophylactic
that may be confused with impetigo or con- use of antiviral agents is recommended for
PMPH_Eversole_Chapter-05.indd 147 1/17/2011 3:33:38 PM
148 Chapter 5
severely compromised patients (200 mg, 4 arise in areas of allergenic contact and
times daily taken orally). therefore are on perioral skin if cosmetics
are the offending substances. Intraorally,
various substances may elicit hypersensi-
Additional Reading tivity responses in patients who are aller-
gic. Specifically, mouthwashes, dentifrices,
Corey L, Nahmias AJ, Guinan ME, Benedetti JK,
Critchlow CW, Holmes KK. A trial of topical acyclo- acrylic, topical antibiotics, and foods can be
vir in genital herpes simplex virus infections. N Engl J incriminated. Perhaps more frequently, oral
Med. 1982;306:1313-1319. allergic eruptions of the immediate type
Hann IM, Prentice HG, Blacklock HA. Acyclovir pro- arise subsequent to a systemically intro-
phylaxis against herpes virus infection in severely
immunocompromised patients: randomized double- duced allergen such as shellfish, berries, or
blind trial. Br Med J. 1983;287:384-388. drugs. Allergic stomatitis is less common
Jaffe EC, Lehner T. Treatment of herpetic stomatitis than atopic dermatitis. The lesions regress
with idoxuridine. Br Dent J. 1968;125:392-395. within 3 to 5 days, providing repeated con-
Ship II. Virus and viral-like diseases of the mouth.
Postgrad Med. 1965;38:499.
tact with allergen is avoided.
Sklar SH, Buimovici-Klein E. Adenosine in the treat-
ment of recurrent herpes labialis. Oral Surg Oral Med
MICROSCOPIC FEATURES
Oral Pathol. 1979;48:416-417.
Intraepithelial vesicles are present. The
vesicular contents are composed of an
CONTACT VESICULAR eosinophilic exudate and an acute inflam-
STOMATITIS matory cell infiltrate composed of both neu-
Figure 5-8 trophils and eosinophils. The submucosa is
traversed by dilated capillaries and is infil-
Age: No predilection trated with leukocytes.
Sex: No predilection
CLINICAL FEATURES DIFFERENTIAL DIAGNOSIS
Immediate or humorally mediated immune The vesicular eruption of allergic mucositis
reactions to allergens contacting the oral may resemble primary herpes, hand-foot-
mucous membranes may manifest vesicle and-mouth disease, and erythema multi-
formation. The vesicles do not tend to clus- forme. Because the patient is afebrile, this
ter and are superimposed on a broad mat- feature tends to eliminate the aforemen-
ted erythematous base. Pain or burning, tioned diseases from the differential diag-
rather than pruritus, is present. Vesicles nosis. Questioning the patient with regard
FIGURE 5-8
Multiple vesicles and small
ulcers appearing as a
manifestation of allergy to
various mouth rinses, den-
tifrices, dental materials,
foods, and drugs.
PMPH_Eversole_Chapter-05.indd 148 1/17/2011 3:33:50 PM
Vesiculobullous and Desquamative Lesions 149
to the use of newly contacted materials or configuration of vesicles occurs. The dis-
chemicals usually provides the necessary ease is contagious.
clue to the nature of the allergen. Those sub-
stances suspected of being allergenic may MICROSCOPIC FEATURES
be applied to the mucosa for epimucous Intraepithelial vesicles are engorged with
patch testing. This testing is accomplished neutrophils. The submucosa evinces a sub-
by mixing suspected allergens with Ora- acute inflammatory cell infiltrate.
base and applying to the mucosa. A positive
reaction may be seen in 24 to 48 hours. DIFFERENTIAL DIAGNOSIS
TREATMENT Perioral vesicles of impetigo must be differ-
entiated from those seen in recurrent herpes
Suspected contact allergens should be dis- labialis and contact dermatitis. Involvement
continued. Antihistamines, 50 mg diphen- is usually more widespread with impetigo
hydramine hydrochloride (Benadryl), or 12.5 than with herpes, and the presence of lin-
mg promethazine hydrochloride (Phener- ear tracks of vesicles is highly suggestive
gan), twice daily will effect an early resolu- of impetigo. A cytologic smear of an intact
tion of vesicles and associated discomfort. vesicle rules out virus-specific cytologic
changes.
Additional Reading TREATMENT
Eversole LR. Allergic stomatitis. J Oral Pathol Med.
1979;34(4).
Topical application of bacitracin, neomy-
Goldman L, Farrington J. Stomatitis with glossitis follow- cin, and polymyxin is recommended. Sys-
ing oral therapy with penicillin tablets. Arch Dermatol. temically administered penicillin (500 mg 4
1958;57:399. times daily for 10 days) is recommended if
Laubach JL, Malkinson FD, Ringrose EJ. Cheilitis
lymphadenopathy or fever is present.
caused by cinnamon (Cassia) oil in toothpaste. J Am
Med Assoc. 1953;152:404-405.
Rickles NH. Allergy in surface lesions of the oral mucosa.
Oral Surg Oral Med Oral Pathol. 1972;33:744.
Zakon SJ, Goldberg AL, Kahn JB. Lipstick cheilitis. Arch
Additional Reading
Derm Syphilol. 1947;56:499-505. Fleisher G. Pediatric skin, soft tissue, and bone infec-
tions. Del Med J. 1980;52:587.
IMPETIGO
Figure 5-9
Age: Children
Sex: No predilection
CLINICAL FEATURES
Impetigo is a vesicular eruption on the peri-
oral skin and vermilion border. Oral mucosa
is not affected. The lesions are caused by
staphylococci or a mixed staphylococcal-
streptococcal infection. They are pain-
ful and pruritic and, because the patient
scratches the lesions, they are excoriated FIGURE 5-9
and eroded. Scratching causes implantation Excoriated clustering vesicles occurring in crops
of organisms, so that a linear or serpentine and linear streaks on the perioral skin in impetigo.
PMPH_Eversole_Chapter-05.indd 149 1/17/2011 3:34:15 PM
150 Chapter 5
Hughes WT. Impetigo contagiosa in children. GP. between keratinocytes. This antigen has
1969;36:78. been characterized electrophoretically.
Markowitz M, Bruton HD, Kuttner AG, Cluff LE. The
bacteriologic findings, streptococcal immune response, Oral lesions are invariably present at some
and renal complications in children with impetigo. time in the course of the disease and may
Pediatrics. 1965;35:393-404. actually precede the development of skin
Peter G, Smith AL. Group A streptococcal infections of lesions in as many as 50% of the affected
the skin and pharynx. N Engl J Med. 1977;297:311-
317.
population. The oral bullae begin as bleb-
like blisters or diffuse gelatinous plaques.
Rupture of the bullae occurs within a
Bullous Diseases few days, leaving broad areas of desqua-
mation with associated erythema. The
PEMPHIGUS VULGARIS lesions are usually painful. Generalized
desquamative lesions of the attached gin-
Figure 5-10
giva are commonly encountered. Rubbing
Age: Middle-aged and elderly adults uninvolved skin or mucosa may elicit the
Sex: No predilection formation of a bullous lesion (Nikolsky’s
sign). Instances of pemphigus-like lesions
CLINICAL FEATURES have been reported to evolve subsequent
Pemphigus vulgaris is an immunopatho- to administration of certain drugs, partic-
logic dermatologic disease characterized ularly penicillamine. If left untreated, the
by bulla formation. Affected patients disease may be fatal. Patients die of dehy-
develop autoantibodies to a normal pro- dration and septicemia through exposed
tein associated with cell-cell adhesion denuded bullae of the skin.
FIGURE 5-10
Bullous lesions accompa-
nied by a desquamative
gingivitis in pemphigus vul-
garis.
PMPH_Eversole_Chapter-05.indd 150 1/17/2011 3:34:39 PM
Vesiculobullous and Desquamative Lesions 151
MICROSCOPIC FEATURES
Biopsy should be performed on intact bul-
Additional Reading
lae when possible. The epithelium displays a Amagai M, Karpati S, Prussick R, Klaus-Kovtun V,
suprabasilar cleft with round, smooth epithe- Stanley JR. Autoantibodies against the amino-terminal
cadherin-like binding domain of pemphigus vulgaris
lial cells (acantholytic, Tzanck cells), found
antigen are pathogenic. J Clin Invest. 1992;90:919-
suspended in the bullous cavity. In vivo, 926.
bound immunoglobulins can be detected Beutner EH, Lever WF, Witebsky E, Jordon R, Chertock
in the intercellular cement regions, and B. Autoantibodies in pemphigus vulgaris: response to
patients with active disease have circulating intercellular substance of epidermis. J Am Med Assoc.
1965;192:682-688.
antibodies and complement directed to the Eisenberg E, Ballow M, Wolfe SH, Krutchkoff DJ,
desmosomal adhesion protein desmoglein 3. Tanzer JM. Pemphigus-like mucosal lesions: a side
Direct immunofluorescence shows perikera- effect of penicillamine therapy. Oral Surg Oral Med
tinocyte staining with IgG, IgM, and comple- Oral Pathol. 1981;51:409-414.
Laskaris G. Oral pemphigus vulgaris: an immunofluo-
ment fraction 3 yielding a “fish net” pattern. rescent study of fifty-eight cases. Oral Surg Oral Med
Oral Pathol. 1981;51:626-631.
DIFFERENTIAL DIAGNOSIS Shamim T, Varghese VI, Shameena PM, Sudha S.
Pemphigus vulgaris in oral cavity: clinical analysis of 71
When only oral bullae are present, per- cases. Med Oral Patol Oral Cir Bucal. 2008;13:E622-
phigus may be indistinguishable from the E626.
other bullous dermatoses listed in this sec-
tion. A biopsy is required to confirm the
diagnosis. Occasionally, pemphigus lesions BULLOUS PEMPHIGOID
are confined to the gingiva. If this is the Figure 5-11
case, gingivosis should be considered in the
Age: Adults
differential diagnosis.
Sex: No predilection
TREATMENT CLINICAL FEATURES
Pemphigus vulgaris should be treated by Bullous pemphigoid is an immunopatho-
a general physician or dermatologist; high- logic bullous dermatosis characterized
dose, long-term systemic steroid therapy by bulla formation of skin. The antigen in
is required for control of the disease. With bullous pemphigoid has been character-
severe dermal involvement, fluid/electrolyte ized and is a normal protein constituent of
balance must be controlled and septicemia the hemidesmosome-basement membrane
must be prevented. Levamisole in conjunc- complex. Lesions are located primarily in
tion with prednisone allows for lower ste- the axillary and inguinal and abdominal
roid dosage. Azathioprine with prednisone regions. They begin as erythematous and
may be effective as well. eczematous plaques that ultimately prog-
FIGURE 5-11
Bullous pemphigoid, a
bullous dermatosis of skin
occasionally accompanied
by oral bullae.
PMPH_Eversole_Chapter-05.indd 151 1/17/2011 3:35:23 PM
152 Chapter 5
ress to bullae. Occasionally, but not invari-
ably, the oral mucosa is affected. The bullae Additional Reading
are tense blebs or broad gelatinous plaques. Beutner EH, Jordon RE, Chorzelski TP. The immu-
As in the other oral bullous disorders, rup- nopathology of pemphigus and bullous pemphigoid.
ture with desquamation takes place shortly J Invest Dermatol. 1968;51:63-80.
after the lesions appear. The disease is Hodge L, Marsden RA, Black MM, Bhogal B, Corbett
MF. Bullous pemphigoid: the frequency of mucosal
annoying yet not usually fatal; nevertheless, involvement and concurrent malignancy related to
septicemia may be a complication. There is indirect immunofluorescent findings. Br J Dermatol.
some evidence that patients with bullous 1982;105:65-69.
pemphigoid accompanied by oral lesions Iwata H, Kamio N, Aoyama Y, et al. IgG from patients
with bullous pemphigoid depletes cultured kerati-
are more likely to develop malignancies nocytes of the 180-kDa bullous pemphigoid antigen
elsewhere in the body. (type XVII collagen) and weakens cell attachment.
J Invest Dermatol. 2009;129:919-926.
MICROSCOPIC FEATURES Katsumi S, Muramatsu T, Kobayashi N, Nakatani C,
Shirai T. Bullous pemphigoid preceded by recurrent
The bullae are subepithelial. The bulluos oral lesions: identification of autoantibodies against
roof in an early lesion possesses well- BP180 by immunoblot using epidermal extracts and
aligned and polarized basal cells, whereas BP180 fusion proteins. Br J Dermatol. 1999;141:157-
159.
the connective tissue floor is devoid of or Shklar G, Meyer I, Zacarian S. Oral lesions in bullous
shows only mild infiltration by mononu- pemphigoid. Arch Dermatol. 1969;99:663-670.
clear cells. Patients with active disease show
high antibody titers of immunoglobulins
that specifically bind to lamina lucida base- BENIGN MUCOUS MEMBRANE
ment membrane proteins BP230 and BP180. PEMPHIGOID
Direct immunofluorescence discloses a lin- Figure 5-12
ear pattern along the course of the basement
membrane with IgG, IgM, and complement Age: Middle-aged and elderly adults
Sex: Female predilection
fraction 3.
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
BMMP is a bullous disorder that resembles
Bullous pemphigoid must be differentiated bullous pemphigoid, yet the bullae have a
from the other bullous dermatoses listed predilection for mucous membranes. The
in this section. The restriction of lesions oral cavity and conjunctivas are favored
to the axillary and inguinal intertriginous sites, although pharyngeal, anal, and vagi-
zones is typical for pemphigoid. Biopsy is nal lesions are present in one half of the
required to arrive at a definitive diagnosis. patients. The BMMP antigen is unique and
Immunofluorescence antibody testing to differs from that of the bullous pemphig-
detect antibasement membrane antibodies oid antigen. Bullae of the facial neck, and
may be useful in the diagnosis. genital skin are also occasionally present.
The oral bullae develop slowly and vary in
TREATMENT size. They are tense or gelatinous plaques.
Bullous pemphigoid is treated by systemic Desquamation of the gingiva is also a fre-
steroids. Dapsone has also been shown to quent finding. The eye lesions are found on
be effective in the management of the dis- both palpebral and bulbar conjunctivas and
ease; however, red cell suppression may be a tend to heal with scarring. Fibrous bands
complication. The disease, being a primary extend from the lid to the sclera and are
cutaneous disorder, should be managed by termed symblepharon. This finding, in con-
a dermatologist. junction with oral bullae, is essentially diag-
PMPH_Eversole_Chapter-05.indd 152 1/17/2011 3:35:34 PM
Vesiculobullous and Desquamative Lesions 153
FIGURE 5-12
Benign mucous membrane
pemphigoid, a bullous dis-
order showing extensive
oral bullae on an erythema-
tous base. Symblepharon is
seen traversing palpebral
and bulbar conjunctivae.
nostic for BMMP. The disease is not lethal The eye lesions are characteristic, and when
and follows a protracted course. The major oral biopsy discloses subepithelial bul-
complication is entropion with blindness. lae, a clinicopathologic diagnosis can be
obtained.
MICROSCOPIC FEATURES
TREATMENT
The bullous lesions are subepithelial with
an intact basal cell layer on the roof. The Systemic steroid therapy, consisting of 40 mg
submucosa in early lesions shows minimal of prednisone in divided doses daily, can
inflammation. These features are identical be used until control of lesions is achieved,
to those encountered in bullous pemphig- after which medication is withdrawn until
oid. Antibasement membrane antibodies new lesions develop. Dapsone has also been
in serum can be detected, yet are present found to be effective. Topical 0.05% fluoci-
in very low titers. The target antigen in nonide (Lidex) or tacrolimus ointment can
mucous membrane pemphigoid (MMP) is be applied 4 to 6 times daily to oral bullous
heterogeneous and usually localized to the and desquamative lesions.
lamina lucida (laminin 5, collagen VII, and
other nonlaminin basement adhesion mol-
ecules). Direct immunofluorescence shows Additional Reading
basement membrane linear distribution of Dabelsteen E, Ullman S, Thomsen K, Rygaard J.
IgG, complement fraction 3, and IgA (linear Demonstration of basement membrane autoantibodies
IgA disease). in patients with benign mucous membrane pemphig-
oid. Acta Dermatol. Venereol (Stockh). 1974;54:189-
192.
DIFFERENTIAL DIAGNOSIS Person JR, Rogers RS, III. Bullous and cicatricial pem-
The oral lesions of BMMP are similar in phigoid: clinical, histopathologic, and immunopatho-
logic correlations. Mayo Clin Proc. 1977;52:54.
appearance to those of the other bullous Rogers RS, III, Seehafer JR, Perry HO. Treatment of
dermatoses, but they develop more slowly cicatricial (benign mucous membrane) pemphigoid
and tend to be smaller and less extensive. with dapsone. J Am Acad Dermatol. 1982;6:215.
PMPH_Eversole_Chapter-05.indd 153 1/17/2011 3:35:34 PM
154 Chapter 5
Shklar G, McMarthy PL. Oral lesions of mucous and mucosa. This condition is referred to as
membrane pemphigoid: a study of 85 cases. Arch lichen planus pemphigoides.
Otolaryngol Head Neck Surg. 1971;93:354.
Solomon LW, Yerke LM, Kumar V. Differentiation of
mucous membrane pemphigoid subgroups with con- MICROSCOPIC FEATURES
focal imaging. Oral Surg Oral Med Oral Pathol Oral
The diagnostic features of bullous lichen
Radiol Endod. 2007;104:790-795.
planus are most obvious on the margin
of the lesion. A subepithelial separation is
BULLOUS LICHEN PLANUS present. The roof of the bulla is composed of
Figure 5-13 disoriented fragmented basal cells lacking
polarization. The floor shows fragmented
Age: Middle-aged adults basal cells overlying fibrous tissue with a
Sex: Slight female predilection zonal superficial infiltrate of lymphocytes.
The margin of the bulla blends with mucosa
CLINICAL FEATURES
showing the microscopic features typical of
Although lichen planus is typically a white the conventional type of lichen planus. On
lesion, erosive and bullous variants occur. direct immunofluorescence, fibrinogen is
The latter is very rare, most cases being consistently identified along the basal lam-
desquamative without intact bullae. The ina with a fringe pattern. In lichen planus
oral bullae are most often encountered on pemphigoides, antibasement membrane
the buccal mucosa and appear as flattened IgG is also demonstrated.
gelatinous bullous plaques surrounded by
zones of erythema. Often, but not invari- DIFFERENTIAL DIAGNOSIS
ably, white lesions or striae can be found
When white striae are present in conjunc-
adjacent to bullae or in other intraoral loca-
tion with bullae, providing the microscopic
tions. Burning discomfort or mild pain may
features are typical, and the diagnosis is
be a complaint. Skin lesions are present in
easily determined. When only bullae are
some instances. The disease is benign and
present, bullous lichen planus may be clini-
chronic. A familial form affects the extremi-
cally indistinguishable from other bullous
ties, appears in early childhood and teen-
dermatoses. Biopsy is then required for a
age years, and is inherited as an autosomal
definitive diagnosis.
dominant trait.
Rarely, both lichen planus, a T cell-me-
diated disease process, and bullous pem- TREATMENT
phigoid, a humoral-mediated process, may Topical application of 0.05% fluocinonide
occur simultaneously, affecting both skin ointment (Lidex) or 0.05% clobetasol propri-
FIGURE 5-13
Bullous lesions in lichen
planus, a rare presentation
that proceeds to erosions.
PMPH_Eversole_Chapter-05.indd 154 1/17/2011 3:35:55 PM
Vesiculobullous and Desquamative Lesions 155
onate (Temovate) is useful in controlling the the lips are almost constantly affected, with
bullous and erythematous component of painful exudative erythematous erosions.
the disease but will not eliminate the white Occasionally, oral lesions are seen without
lesions that may be present. dermatologic manifestations. A slightly ele-
vated temperature is commonly detected.
The disease runs its course in 2 to 5 weeks.
Additional Reading
MICROSCOPIC FEATURES
Allen CM, Camisa C, Grimwood R. Lichen planus pem-
phigoides: report of a case with oral lesions. Oral Surg The bullae or desquamating regions gener-
Oral Med Oral Pathol. 1987;63:184. ally manifest a junctional separation. This
Goldstein BH. Immunofluorescent findings in oral
bullous lichen planus. J Oral Pathol Med. 1979;34:8.
feature is not consistent throughout; zones
Haselden FG. Bullous lichen planus. Oral Surg Oral of irregular intraepithelial separation are
Med Oral Pathol. 1967;24:4. usually encountered. The upper spinous
Huang C, Chen S, Liu Z, Tao J, Wang C, Zhou Y. Familial and parakeratin layers often contain vesicu-
bullous lichen planus (FBLP): pedigree analysis and
clinical characteristics. J Cutan Med Surg. 2005;9:217-
lar pools of eosinophilic coagulum (muco-
222. polysaccharide-keratin dystrophy). The
van Tuyll van Serooskerken AM, van Marion AM, de subjacent fibrous connective tissue evinces
Zwart-Storm E, Frank J, Poblete-Gutiérrez P. Lichen a subacute inflammatory cell infiltrate.
planus with bullous manifestation on the lip. Int J
Dermatol. 2007;46(suppl 3):25-26.
DIFFERENTIAL DIAGNOSIS
The bullous lesions of erythema multiforme
ERYTHEMA MULTIFORME are clinically similar to those of the other
Figure 5-14 bullous dermatoses. Severe involvement of
the lips, target lesions of skin, and slight
Age: Young adults elevation of temperature are indicative of
Sex: Male predilection erythema multiforme. Biopsy should be
CLINICAL FEATURES performed to rule out the other bullous der-
matoses. Localization of lesions on the oral,
Erythema multiforme is a dermatologic conjunctival, and genital mucous mem-
disorder that is often but not invariably pre- branes are typical for Stevens-Johnson syn-
cipitated by allergens such as sulfa drugs. drome, a variant of erythema multiforme.
Precedent herpes infection is a common
finding in many instances in which no
TREATMENT
allergen can be identified. Postherpetic ery-
thema multiforme has been shown to evolve Systemically administered antihistamines,
as a consequence of perivascular immune antipyretics, and a palliative oral rinse such
complex deposition of immunoglobulin, as antihistamine oral expectorant mixed
herpes virus antigen, and complement. The 50:50 with Kaopectate are recommended.
disease manifests a variety of lesions of In more severe cases, 20 mg of prednisone
skin and mucosa including bullae, macules, in divided doses may be required. Fluid
erosions, and, on skin, an erythematous cir- intake should be maintained and the patient
cular wheal with a circumferential halo, the should be placed on a soft diet. Among
so-called target or iris lesion. The oral cav- patients with precedent herpesvirus infec-
ity is usually involved. Bullae develop and tion, acyclovir (400 mg daily) prevents
rapidly burst, leaving raw erosions with recurrences of both herpetic lesions and the
desquamation and underlying erythema. associated erythema multiforme eruptions
Although any oral tissue can be involved, in most patients.
PMPH_Eversole_Chapter-05.indd 155 1/17/2011 3:36:06 PM
156 Chapter 5
FIGURE 5-14
Erythema multiforme with
vesiculobullous lesions
having a tendency to hem-
orrhage are seen through-
out the oral mucosa, with
predilection for the lips
and vermilion border.
erosive erythematous lesions are found in
Additional Reading the oral cavity, on the bulbar and palpebral
Buchner A, Lozada F, Silverman S Jr. Histopathologic conjunctivas, and on the external genitalia
spectrum of oral erythema multiforme. Oral Surg Oral (glans penis, vulva). Typical iris or target
Med Oral Pathol. 1980;49:221. skin erythematous wheals are often present
Lozada F, Silverman S Jr. Erythema multiforme: clini- as well. The oral manifestations of Stevens-
cal characteristics and natural history of fifty patients.
Oral Surg Oral Med Oral Pathol. 1978;46:628. Johnson syndrome may be confused with
Molin L. Oral acyclovir prevents herpes simplex virus- other bullous dermatoses. The oral lesions
associated erythema multiforme. Br J Dermatol. invariably involve the lips as a diffuse hem-
1987;116:109. orrhagic exudative bullous eruption. Sulfa
Shelley WB. Herpes simplex virus as a cause of erythema
multiforme. JAMA. 1967;201:153.
drugs are often found to precipitate this syn-
Wetter DA, Davis MD. Recurrent erythema multiforme: drome, which may be fatal if no treatment is
clinical characteristics, etiologic associations, and treat- rendered. As in erythema multiforme of the
ment in a series of 48 patients at Mayo Clinic, 2000 to minor type, this major syndrome may fol-
2007. J Am Acad Dermatol. 2010;62:45-53.
low herpes infection.
MICROSCOPIC FEATURES
STEVENS-JOHNSON
See Erythema Multiforme.
SYNDROME
Figure 5-15 DIFFERENTIAL DIAGNOSIS
Age: Young adults The bullous and erosive lesions of Stevens-
Sex: Male predilection Johnson syndrome may be confused with
other bullous dermatoses. The triad of oral,
CLINICAL FEATURES
eye, and genital involvement is classic for
Stevens-Johnson syndrome is a form of ery- Stevens-Johnson syndrome. This distribu-
thema multiforme often termed erythema tion should not present a problem when
multiforme major, in which bullous and differentiating this disease from the muco-
PMPH_Eversole_Chapter-05.indd 156 1/17/2011 3:36:06 PM
Vesiculobullous and Desquamative Lesions 157
FIGURE 5-15
The Stevens-Johnson syndrome, representing a specific form of erythema multiforme in which the oral
mucosa, conjunctiva, and genital mucosa manifest a vesiculobullous eruption.
oculocutaneous lesions of Behcet’s syn- Nethercott JR, Choi BCK. Erythema multiforme
drome and Reiter’s disease because these (Stevens-Johnson Syndrome)—chart review of 123
hospitalized patients. Dermatologica. 1985;171:383.
latter two disorders manifest aphthous-like Robinson HM Jr., McCrumb FR Jr. Comparative analy-
ulcerations rather than desquamating bul- sis of the mucocutaneous-ocular syndromes. Arch
lae of the oral cavity. Dermatol Syph. 1950;61:539.
Yetiv JZ, Bianchine JR, Owen JA Jr. Etiologic fac-
TREATMENT tors of the Stevens-Johnson syndrome. South Med J.
1980;73:599-602.
Any allergenic drug or food should be with-
drawn. The disease is then managed as out-
lined for erythema multiforme. Systemic PARANEOPLASTIC
steroids should be prescribed in severe
cases, because fatalities in Stevens-Johnson
PEMPHIGUS
syndrome associated with sulfa drugs have Figure 5-16
been recorded.
Age: Adults
Sex: No predilection
Additional Reading CLINICAL FEATURES
Coursin DB. Stevens-Johnson syndrome: nonspecific Paraneoplastic pemphigus is an oral/
parasensitivity reaction? JAMA. 1966;198:113.
Knowles S, Shear NH. Clinical risk management of
cutaneous condition that occurs as a con-
Stevens-Johnson syndrome/toxic epidermal necrolysis sequence of autoantibodies directed to des-
spectrum. Dermatol Ther. 2009;22:441-451. moplakin proteins in keratinocytes. The
PMPH_Eversole_Chapter-05.indd 157 1/17/2011 3:36:20 PM
158 Chapter 5
FIGURE 5-16
Oral and ocular lesions of
paraneoplastic pemphigus
in a patient with Castle-
man’s disease.
autoantibodies were generated in response of burning and pain. Most importantly, a
to a malignant lesion located viscerally. clandestine neoplastic process needs to be
More than 85% of cases have an associated uncovered with institution of appropriate
B cell lymphoma or Castleman’s disease. therapy.
The oral lesions are bullous, desquama-
tive, and ulcerated involving the lips, oral
mucosa, and conjunctiva. Patients complain
Additional Reading
of oral burning pain. Edgin WA, Pratt TC, Grimwood RE. Pemphigus vulgaris
and paraneoplastic pemphigus. Oral Maxillofac Surg
MICROSCOPIC FEATURES Clin North Am. 2008;20:577-584.
Kaplan I, Hodak E, Ackerman L, Mimouni D, Anhalt
The erosive/desquamative lesions of para- GJ, Calderon S. Neoplasms associated with para-
neoplastic pemphigus do not parallel those neoplastic pemphigus: a review with emphasis on
of pemphigus vulgaris; rather they are more non-hematologic malignancy and oral mucosal mani-
festations. Oral Oncol. 2004;40:553-562.
often lichenoid with a lymphocytic chronic Tilakaratne W, Dissanayake M. Paraneoplastic pemphi-
interface mucositis, or they may appear as gus: a case report and review of literature. Oral Dis.
a nonspecific chronic mucositis. On direct 2005;11:326-329.
immunofluorescence, a pericellular distribu- Yokokura H, Demitsu T, Kakurai M, et al. Paraneoplastic
pemphigus mimicking erosive mucosal lichen planus
tion is identified along with demonstration associated with primary hepatocellular carcinoma.
of basement membrane immunoreactants J Dermatol. 2006;33:842-845.
reflecting the location of desmoplakins in
both desmosomes and hemidesmosomes.
ANGINA BULLOSA
DIFFERENTIAL DIAGNOSIS HEMORRHAGICA
Paraneoplastic pemphigus often presents Figure 5-17
with ocular lesions, being confused with
Age: Middle-aged adults
mucous membrane pemphigoid. In some
Sex: No predilection
instances the patient is already aware of
a cancerous process, in yet others the oral CLINICAL FEATURES
and/or ocular lesions may be the initial pre- Hemorrhagic bullae are believed to evolve
sentation and an oncologic workup should as a consequence of trauma and are com-
be initiated. monly encountered on the hard or soft pal-
ate. There may only be a single bullae or
TREATMENT
multiple lesions can be seen and they are
Topical steroids will lessen the inflam- often painful in the early stage. They are
matory process with its accompaniment tense bullae that are ruby red or deep pur-
PMPH_Eversole_Chapter-05.indd 158 1/17/2011 3:36:57 PM
Vesiculobullous and Desquamative Lesions 159
FIGURE 5-17
Blood blisters in angina
bullosa haemorrhagica.
ple that, shortly after their formation, burst EPIDERMOLYSIS BULLOSA
to leave a broad erosion that heals over in 7 Figure 5-18
to 10 days.
Age: Infants (hereditary variants)
MICROSCOPIC FEATURES Sex: Varies with mode of inheritance
Unknown CLINICAL FEATURES
There are many forms of epidermolyis
DIFFERENTIAL DIAGNOSIS
bullosa (EB), most being inherited. This
Other bullous diseases must be included group of diseases has been subdivided on the
in the differential diagnosis because any basis of inheritance patterns, severity of dis-
blister can be hemorrhagic. A blood-filled ease, and histopathologic features of blister
mucocele should also be a consideration. formation. The “simplex” form is present at
birth and improves with ensuing years. The
TREATMENT disorder primarily affects the feet, hands,
The erosions left after the bullae burst and neck, with nail changes being variable;
resolve of their own accord. Soothing mouth scarring is nonexistent. Oral bullae are mild
rinses such as an antihistamine/Kaopectate and the teeth are not affected. In the “gen-
syrup will attenuate pain. eralisata gravis” form, an autosomal reces-
sive disease, blisters appear at the nail beds
shortly after birth and the nails are then
Additional Reading shed. Involvement of the trunk, umbilicus,
face, scalp, and extremities follow, and some
Deblauwe BM, van der Waal I. Blood blisters of the oral
mucosa (angina bullosa haemorrhagica). J Am Acad patients die as a consequence of septicemia.
Dermatol. 1994;31(2 Pt 2):341-344. Many patients survive and show fragile,
Giuliani M, Favia GF, Lajolo C, Miani CM. Angina hemorrhagic oral bullae, particularly of the
bullosa haemorrhagica: presentation of eight new palate. Hypoplastic, pitted enamel involv-
cases and a review of the literature. Oral Dis. 2002;8:
54-58. ing the molar teeth is a feature and, charac-
Porter K, Porter SR, Scully C. ‘Angina bullosa haemor- teristically, perioral and perinasal granular
rhagica: a complication of long-term steroid inhaler hemorrhagic crusted lesions evolve. The
use’. Br Dent J. 1988;165:279. dystrophic or hypertrophic form is inher-
Poskitt L. Angina bullosa haemorrhagica: associated ste-
roid inhaler use. N Z Med J. 1991;104(925):522.
ited as a dominant trait and the flattened
Yip HK. Angina bullosa haemorrhagica: a case report and bullae appear on the hands, elbows, ankles,
a concise review. Gen Dent. 2004;52:162-164. knees, and feet before the first year of life
PMPH_Eversole_Chapter-05.indd 159 1/17/2011 3:37:08 PM
160 Chapter 5
FIGURE 5-18
Oral lesions accompanying bullous, scarring lesions located on skin over joints, a manifestation of epider-
molysis bullosa (Courtesy of Dr. J. Mink).
with improvement after puberty. Oral bul- hypoplasia without significant submucosal
lae are occasionally seen. inflammation. In the scarring form, the level
The “scarring” variety is subdivided of cleavage is below the basal lamina.
into four autosomal recessive disease forms,
all of which occur in infants. The occipital DIFFERENTIAL DIAGNOSIS
and scapular skin is blistered, as is that on Most of the other bullous diseases included
the elbows, fingers, buttocks, and feet. Scar- in this section occur in adults. Blistering
ring with pigmentation and depigmenta- diseases of childhood that should be con-
tion are featured and the hands become sidered in the differential diagnosis include
claw-like. Bullae arise in the larynx and bullous impetigo, porphyria, and dermati-
esophagus leading to hoarseness/aphonia tis herpetiformis. Although biopsy is help-
and dysphagia, respectively. Oral bullae ful, the distribution of lesions and degree
are also generally present along with scar- of scarring are important features in the
ring and mucosal atrophy; the teeth show establishment of a definitive diagnosis.
hypoplastic enamel. The nonhereditary Referral to a dermatologist or pediatrician
acquisita form of the disease shows anti- is recommended.
bodies to type VII collagen; however, oral
lesions are rarely encountered. Other vari- TREATMENT
eties of the disease are not associated with
oral or dental manifestations. Prevention of septicemia is of paramount
importance in severely affected patients.
MICROSCOPIC FEATURES Those forms of EB with dental hypoplasia are
associated with severe caries and the affected
The histologic classification of EB does not teeth should be restored with full crowns.
necessarily correlate with the clinical forms
and includes four specific subgroups. This
classification is based on the microscopic Additional Reading
focus of bulla formation: type I, the split is
Album MM, Gaisin A, Lee KW, Buck BE, Sharrar
intraepithelial; type II, junctional cleavage WG, Gill FM. Epidermolysis bullosa dystrophica
at the level of the basal lamina; type III, der- polydysplastica. Oral Surg Oral Med Oral Pathol.
mal separation associated with atrophy and 1977;43:859.
scarring; type IV, the nonhereditary form, Atar M, Körperich EJ. Systemic disorders and their
influence on the development of dental hard tissues: a
also with junctional separation. The simplex literature review. J Dent. 2010;38:296-306.
and generalisata gravis varieties involve an Lowe LG Jr. Hereditary epidermolysis bullosa. Arch
intrabasilar split owing to hemidesmosome Dermatol. 1967;95:587.
PMPH_Eversole_Chapter-05.indd 160 1/17/2011 3:37:17 PM
Vesiculobullous and Desquamative Lesions 161
Sedano HO, Gorlin RJ. Epidermolysis bullosa. Oral Surg the eosinophil. Lumps of IgA can be dem-
Oral Med Oral Pathol. 1989;67:555. onstrated in the dermal papilla area with
Winstock D. Oral aspects of epidermolysis bullosa. Br J
Dermatol. 1962;74:431. immunofluorescence staining.
DIFFERENTIAL DIAGNOSIS
DERMATITIS HERPETIFORMIS The oral lesions of dermatitis herpetiformis
(GLUTEN ENTEROPATHY) are similar in appearance to those of the
Figure 5-19 other bullous dermatoses. The clustered
vesicles with pigmented base on the skin are
Age: Middle-aged adults highly suggestive but not pathognomonic
Sex: Male predilection for the disease. Biopsy discloses character-
CLINICAL FEATURES istic features.
Dermatitis herpetiformis is an immunop- TREATMENT
athologic vesiculobullous disease of skin
rarely showing oral manifestations. The con- Because the disease is primarily a derma-
dition represents the cutaneous expression tologic disorder, referral to a dermatologist
of gluten enteropathy (gliadin sensitivity). is recommended. Dermatitis herpetiformis
The skin lesions are pruritic and are located responds to sulfapyridine therapy; steroids
primarily on the extremities and buttocks. are not particularly useful.
They are vesicular with a tendency to rup-
ture and desquamate. Oral bullae may be
encountered and many patients present
Additional Reading
with aphthous like ulcers. The disease is Caproni M, Antiga E, Melani L, Fabbri P. Italian Group
for Cutaneous Immunopathology. Guidelines for the
chronic, lasting for many years, yet is not diagnosis and treatment of dermatitis herpetiformis.
life threatening. J Eur Acad Dermatol Venereol. 2009;23:633-638.
Fraser NG, Kerr NW, Donald D. Oral lesions in derma-
MICROSCOPIC FEATURES titis herpetiformis. Br J Dermatol. 1973;89:439.
Hall RP, Lawley TJ, Katz SI. Dermatitis herpetiformis.
The epithelium displays a sub-basilar sepa- Springer Semin Immunopathol. 1981;4:33.
ration with a subacute inflammatory infil- Katz SI, Hall RP 3rd, Lawley TJ, Strober W. Dermatitis
trate located in the dermal or submucosal herpetiformis: the skin and the gut. Ann Intern Med.
1980;93:857.
papilla zones. The predominant cell type is Russotto SG, Ship II. Oral manifestations of dermati-
tis herpetiformis. Oral Surg Oral Med Oral Pathol.
1971;31:42.
Desquamative Lesions
GINGIVOSIS (DESQUAMATIVE
GINGIVITIS)
Figure 5-20
Age: Middle-aged adults
Sex: Exclusive female predilection
CLINICAL FEATURES
FIGURE 5-19
Oral lesions in gluten enteropathy with cutaneous Gingivosis was, at one time, considered a
dermatitis herpetiformis. specific desquamative disease occurring
PMPH_Eversole_Chapter-05.indd 161 1/17/2011 3:37:36 PM
162 Chapter 5
FIGURE 5-20
Gingivosis characterized by
an erythematous gingivitis
accompanied by desqua-
mation. These lesions are
seen in pemphigoid (top),
erosive lichen planus (bot-
tom left), and pemphigus
vulgaris (bottom right).
after menopause and confined to the DIFFERENTIAL DIAGNOSIS
attached gingiva. Because the clinical and The desquamation of the gingiva as seen
microscopic features of the disease are sim- in BMMP may also occur in many of the
ilar to those encountered in BMMP, most bullous dermatoses, including pemphigus
investigators and clinicians have suggested vulgaris. Erosive lichen planus and tooth-
that gingivosis is a form of BMMP that is paste idiosyncrasy reactions may show fea-
merely confined to gingiva. Many of the dis- tures similar to gingivosis; however, the for-
eases classified previously as bullous disor- mer usually shows extragingival lesions and
ders can manifest desquamative lesions of the latter lacks an erythematous component.
the gingiva. Therefore, desquamative gingivi-
tis is a clinical term and is not specific for TREATMENT
any given disease; nevertheless, gingival
desquamation is most commonly seen in The patient should avoid spicy or acidic
patients with BMMP. foods. A palliative mouth rinse may be
used and topically applied 0.05% fluocino-
MICROSCOPIC FEATURES nide (Lidex) ointment is beneficial in mini-
mizing the inflammatory component.
In BMMP, a junctional separation occurs,
with maintenance of an intact basal cell
layer adherent to the desquamated tissue.
The underlying submucosa manifests an
Additional Reading
intense chronic inflammatory cell infiltrate Glickman I, Smulow JB. Chronic desquamative gingivitis:
its nature and treatment. J Periodontol. 1964;35:297.
with numerous dilated capillaries. The his- Lo Russo L, Fedele S, Guiglia R, et al. Diagnostic path-
tology for other bullous diseases is detailed ways and clinical significance of desquamative gingivi-
elsewhere in this chapter. tis. J Periodontol. 2008;79:4-24.
PMPH_Eversole_Chapter-05.indd 162 1/17/2011 3:37:47 PM
Vesiculobullous and Desquamative Lesions 163
Nisengard RJ, Alpert AM, Krestow V. Desquamative diabetes mellitus and hypertension, a triad
gingivitis: immunologic findings. J Periodontol. known as Grinspan’s syndrome. Instances
1978;49:27.
Scopp IW. Desquamative gingivitis. J Periodontol. of carcinomatous transformation in ero-
1964;35:149. sive lichen planus have been infrequently
Ziskin DE, Zegarelli EV. Chronic desquamative gingivi- reported; the incidence is higher than that
tis. Am J Orthod Oral Surg. 1945;31:1. seen in the nonaffected population. The
disease runs a protracted course and may
or may not be associated with skin mani-
EROSIVE LICHEN PLANUS festations. The oral lesions partially resolve
Figure 5-21 in one region only to reappear at some
new site. Many patients are prone to anxi-
Age: Middle-aged adults
ety. Oral and cutaneous lesions identical
Sex: Female predilection
to lichen planus are occasionally encoun-
CLINICAL FEATURES tered in patients receiving gold therapy and
The erosive form of lichen planus is as com- other drugs such as antimalarials and pen-
mon as the nonerosive type. The lesions icillamine. Bone marrow graft recipients
are most frequently located on the gingiva, may also develop lichenoid mucocutaneous
mucobuccal fold, and buccal mucosa. The lesions.
erosions and zones of desquamation are
MICROSCOPIC FEATURES
accompanied by erythema. Peripheral to the
erosive lesions are white plaques or typical At the margin of the erosions, the histomor-
reticulated striae. Mild to moderate pain or phologic features typical of lichen planus
burning is a common complaint. This form (chronic lymphocytic interface mucosis-
of lichen planus is also often associated with tis) are encountered. Transition is seen,
FIGURE 5-21
The erosive form of lichen
planus showing white striae
accompanied by intense
redness with superficial
sloughing of the mucosa.
PMPH_Eversole_Chapter-05.indd 163 1/17/2011 3:38:14 PM
164 Chapter 5
whereby the epithelium becomes detached LICHENOID CONTACT
from the underlying chronically inflamed STOMATITIS
submucosa. Damage with disorientation of Figure 5-22
the basal cell layer is an important diagnos-
tic feature. Age: Adults
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
When confined to gingiva, erosive lichen
Lichenoid reactions show clinical and micro-
planus may simulate gingivosis. Erosive
scopic features of classic, idiopathic lichen
lichen planus is usually, however, multifocal
planus yet often lack the reticular pattern
and not localized to gingiva. Careful exami-
with stria. In general, they represent delayed
nation usually discloses the presence of white
type hypersensitivity reactions to contac-
striae. A biopsy should be performed; the
tants or represent lichenoid drug eruptions
microscopic features are pathognomonic.
that are triggered by specific pharmaco-
TREATMENT logic agents. More than 60 drugs have been
shown to serve as allergens in susceptible
Topical application of 0.05% fluocinonide subjects. The lesions are typically mixed red
(Lidex) or 0.05% clobetasol (Temovate) oint- and white, often showing erosions and ulcer-
ment should be applied to lesional tissue ations. When the allergen is a metallic hapten,
4 to 6 times each day. Maximal effects are the metals become chelated to host proteins
observed if contact can be maintained over- making them immunogenic for certain peo-
night. Decadron oral rinses are also effec- ple. Lichenoid lesions that contact dental
tive. When erosive lichen planus is severe, amalgams are termed “contact lesions” and
a regimen of 40 mg prednisone for 1 week can usually be attributed to mercury sensi-
with tapering doses for the ensuing 5 to 7 tivity although other metals may be aller-
days may be initiated, followed thereafter genic. Cinnamon is a commonly consumed
with topical steroids for control of lesions. spice that can induce lichenoid oral lesions.
The white component is not controlled with Malignant transformation to squamous can-
topical steroids. cer occurs in 2% of lichen planus patients
and there is evidence supporting the notion
Additional Reading that lichenoid reactions may be more at risk
than classic lichen planus.
Carbone M, Arduino PG, Carrozzo M, et al. Topical clo-
betasol in the treatment of atrophic-erosive oral lichen
planus: a randomized controlled trial to compare two MICROSCOPIC FEATURES
preparations with different concentrations. J Oral A chronic interface lymphocytic mucositis is
Pathol Med. 2009;38:227-233.
Haselden FG. Bullous lichen planus. Oral Surg Oral seen, identical to conventional lichen planus
Med Oral Pathol. 1967;24:472. and direct immunofluorescence demon-
Lozada F, Silverman S Jr. Topically applied fluocinonide strates basement membrane fibrinogen
in an adhesive base in the treatment of oral vesiculo- deposition, thereby excluding the efficacy
erosive diseases. Arch Dermatol. 1980;116:898.
Seehafer JR, Rogers RS 3rd, Fleming CR, Dickson ER.
of this test when attempting to differentiate
Lichen planus-like lesions caused by penicillamine in conventional lichen planus from a lichenoid
primary biliary cirrhosis. Arch Dermatol. 1981;117:140- reaction. Therefore, the diagnosis is based
142. on clinical findings of a potential antigen.
Shulman HM, Sullivan KM, Weiden PL, et al. Chronic
graft-versus-host syndrome in man. A long-term clini-
A singular histology is seen in cinnamon
copathologic study of 20 Seattle patients. Am J Med. lichenoid reactions in that the chronic inter-
1980;69:204-217. face mucositis is mixed with lymphocytes,
PMPH_Eversole_Chapter-05.indd 164 1/17/2011 3:38:36 PM
Vesiculobullous and Desquamative Lesions 165
FIGURE 5-22
Erosive lesions in lichenoid
reactions that represent
local contact allergy (note
proximity to dental restor-
ative metals(top), or to
systemic drug eruptions).
plasma cells, and histiocytes and is accom- Ditrichova D, Kapralova S, Tichy M, et al. Oral lichenoid
panied by submucosal perivascular lym- lesions and allergy to dental materials. Biomed Pap
Med Fac Univ Palacky Olomouc Czech Repub.
phoid aggregates. Some of these aggregates 2007;151:333-339.
show germinal center formation. Kaomongkolgit R. Oral lichenoid drug reaction associ-
ated with antihypertensive and hypoglycemic drugs.
DIFFERENTIAL DIAGNOSIS J Drugs Dermatol. 2010;9:73-75.
Koch P, Bahmer FA. Oral lichenoid lesions, mercury
The chief entity in the differential diagno- hypersensitivity and combined hypersensitivity to mer-
sis is conventional lichen planus. Chronic cury and other metals: histologically-proven reproduc-
tion of the reaction by patch testing with metal salts.
ulcerative stomatitis, lupus erythematosis, Contact Dermatitis. 1995;33:323-328.
and erythroleukoplakia are also included van der Waal I. Oral lichen planus and oral lichenoid
in the differential diagnosis. lesions: a critical appraisal with emphasis on the
diagnostic aspects. Med Oral Patol Oral Cir Bucal.
2009;14:E310-E314.
TREATMENT
Withdrawal of the putative allergenic mate-
rial or pharmacologic agent should result CHRONIC ULCERATIVE
in resolution. Topical steroid gels and STOMATITIS
mouthrinses may facilitate clearance. Figure 5-23
Additional Reading Age: Adults
Sex: No predilection
Al-Hashimi I, Schifter M, Lockhart PB, et al. Oral lichen CLINICAL FEATURES
planus and oral lichenoid lesions: diagnostic and thera-
peutic considerations. Oral Surg Oral Med Oral Pathol Chronic ulcerative stomatitis is a rare
Oral Radiol Endod. 2007;103(suppl):S25.e1-12. lichenoid disease of oral mucosa that is
PMPH_Eversole_Chapter-05.indd 165 1/17/2011 3:38:36 PM
166 Chapter 5
FIGURE 5-23
Ulceration and desquama-
tion in chronic ulcerative
stomatitis with antinuclear
stratified squamous epi-
thelial antibodies.
characterized by the presence of antinu- nuclear antibodies. A case report of a newly described
clear antibodies reactive with stratified disease entity. Oral Surg Oral Med Oral Pathol.
1992;73:579-582.
squamous epithelial nuclei. Clinically, the Islam MN, Cohen DM, Ojha J, et al. Chronic ulcerative
lesions are painful white, red, ulcerative, stomatitis: diagnostic and management challenges—four
and desquamative, appearing primarily on new cases and review of literature. Oral Surg Oral Med
the tongue and buccal mucosa. Oral Pathol Oral Radiol Endod. 2007;104:194-203.
Solomon LW, Neiders ME, Zwick MG, Kirkwood KL,
Kumar V. Autoimmunity to deltaNp63alpha in chronic
MICROSCOPIC FEATURES ulcerative stomatitis. J Dent Res. 2007;86:826-831.
A chronic lymphocytic interface mucosi- Solomon LW, Stark PC, Winter L, Kumar V, Sinha S.
ELISA test for p63 antibodies in chronic ulcerative
tis is evident, resembling ordinary lichen stomatitis. Oral Dis. 2010;16:151-155.
planus. On immunoflourescent testing, Solomon LW. Chronic ulcerative stomatitis. Oral Dis.
fibrinogen may be localized along the base- 2008;14:383-389.
ment membrane, but the singular feature is
the presence of IgG and/or IgM antinuclear
keratinocyte antibodies identified in the PYOSTOMATITIS VEGETANS
lower strata keratinocytes. Figure 5-24
DIFFERENTIAL DIAGNOSIS Age: Adults
Sex: No Predilection
Lichen planus and lichenoid eruptions are
the primary considerations in the differen- CLINICAL FEATURES
tial diagnosis.
A subset of patients with ulcerative colitis
and regional enteritis (Crohn’s disease) may
TREATMENT
manifest cutaneous or mucosal lesions that
The significance of the antinuclear antibod- share a common histology. On the skin,
ies is unknown and not related to lupus the condition is known as pyodermatitis
erythematosus. The condition is often vegetans, in which multifocal white verru-
recalcitrant to topical steroids. Short-term cous patches may develop. In oral mucosa,
systemic corticosteroid therapy may or may the lesions of pyostomatitis vegetans are
not be effective. Hydroxychloroquine ther- yellowish shallow erosions that appear as
apy may be prescribed. willowy serpentine tracts, like the trail left
behind by a mollusk on the ocean floor.
Additional Reading These lesions are painful and burning.
Why only a small minority of patients with
Church LF Jr, Schosser RH. Chronic ulcerative stoma- inflammatory bowel disease manifest this
titis associated with stratified epithelial specific anti- complication is unknown.
PMPH_Eversole_Chapter-05.indd 166 1/17/2011 3:38:47 PM
Vesiculobullous and Desquamative Lesions 167
FIGURE 5-24
Erosions in pyostomatitis
vegetans, an oral manifes-
tation of ulcerative colitis.
MICROSCOPIC FEATURES the chief consideration; biopsy will confirm
There are alternating zones of thickening the clinical impression.
and atrophy of the epithelial layer with
spinous layer edema and transmigration TREATMENT
of leukocytes. The submucosa also shows Systemic corticosteroids (e.g., 50 mg of pred-
nonspecific inflammation. The hallmark nisone daily) will usually allow for clear-
of pyostomatitis vegetans is the appear- ance of lesions within 7 to 10 days. Topical
ance of eosinophilic abscesses located fluorinated steroid gels and high potency
within the spinous layer of the epithelium. rinses can then be used at the earliest onset
Direct immunofluorescence is negative. of recurrences.
A similar condition both clinically and
microscopically is Neuman type pemphi-
gus vegetans. This is a pemphigus vul- Additional Reading
garis variant that may show oral lesions, Damm DD, Fantasia JE. Chronic diffuse yellow erup-
yet there is no association with inflamma- tion. Pyostomatitis vegetans. Gen Dent. 2002;50:561-
tory bowel disease. Furthermore, autoan- 564.
tibodies to desmoglein 3 are present with Femiano F, Lanza A, Buonaiuto C, Perillo L, Dell’Ermo
A, Cirillo N. Pyostomatitis vegetans: a review of the lit-
a pemphigus-like direct immunofluores- erature. Med Oral Patol Oral Cir Bucal. 2009;14:E114-
cence pattern. E117.
Gonzalez-Moles MA, Gil-Montoya JA, Ruiz-Avila I,
DIFFERENTIAL DIAGNOSIS Esteban F, Bascones-Martinez A. Pyostomatitis veg-
etans: dramatic clinical response to clobetasol pro-
Other bullous diseases included here must pionate treatment in aqueous solution. J Eur Acad
be considered in the differential. When Dermatol Venereol. 2008;22:252-253.
Ruiz-Roca JA, Berini-Aytés L, Gay-Escoda C.
there is a history of inflammatory bowel Pyostomatitis vegetans. Report of two cases and review
disease or frequent complaints of gastroin- of the literature. Oral Surg Oral Med Oral Pathol Oral
testinal cramping, pyostomatitis should be Radiol Endod. 2005;99:447-54.
PMPH_Eversole_Chapter-05.indd 167 1/17/2011 3:38:51 PM
168 Chapter 5
FIGURE 5-25
Pale mucosal tissues that
show a superficial slough
of the mucosal cornified
layer in response to spe-
cific dentifrices.
TOOTHPASTE IDIOSYNCRATIC DIFFERENTIAL DIAGNOSIS
LESIONS Erosive lichen planus and gingivosis must
Figure 5-25 be considered in the differential diagno-
sis. Absence of white striae, erythema, and
Age: No predilection pain or burning should limit the diagnosis
Sex: No predilection to toothpaste idiosyncrasy reaction. The
CLINICAL FEATURES clinical diagnosis can be confirmed if the
desquamation resolves after withdrawal of
Certain dentifrices, usually those contain- the suspected causative dentifrice.
ing fluoride salts, cause a superficial desqua-
mation or slough of the cornified layer in TREATMENT
susceptible patients. The reaction does not
appear to represent a true form of allergy, The patient should abstain from the use
but is more consistent with a mild irritant of toothpaste for 1 week, after which a
reaction; it is rather uncommon. The buc- bland nonfluoride dentifrice should be
cal mucosa and mucosal surfaces of the lips prescribed.
show a thin, white membrane that is easily
dislodged by rubbing with gauze. Pain and
erythema are lacking. The disease resolves
Additional Reading
when the causative agent is withdrawn. Herlofson BB, Barkvoll P. Oral mucosal desquamation
of pre- and post-menopausal women. A comparison
MICROSCOPIC FEATURES of response to sodium lauryl sulphate in toothpastes.
J Clin Periodontol. 1996;23:567-571.
Biopsy at the margin of the zonal slough Kowitz G, Lucatorto F, Bennett W. Effects of dentifrices
reveals a separation beneath the stratum on soft tissues of the oral cavity. J Oral Pathol Med.
1973;28:105.
corneum without vesicle formation, and Kuttan NA, Narayana N, Moghadam BK. Desquamative
transmigration of leukocytes into epithe- stomatitis associated with routine use of oral health
lium and submucosa is not a feature. care products. Gen Dent. 2001;49:596-602.
PMPH_Eversole_Chapter-05.indd 168 1/17/2011 3:39:40 PM
PMPH_Eversole_Chapter-05.indd 169 1/17/2011 3:40:01 PM
a b
Pendunculated swelling Sessile swelling
c d
Hyperplasia, reactive Vascular proliferation
e f
Cyst Mesenchymal neoplasm
g h
Glandular neoplasm Osseous enlargement
Soft Tissue Swellings
PMPH_Eversole_Chapter-06.indd 170 1/20/2011 2:22:30 PM
Intraoral Soft
Tissue Swellings 6
TYPE I DIABETES MELLITUS 199
Localized Gingival PUBERTY/PREGNANCY
Tumefactions 173
GINGIVITIS 200
PARULIS 173 LEUKEMIA 201
PYOGENIC GRANULOMA 175
PERIPHERAL GIANT CELL Swellings of the Oral
GRANULOMA 176 Floor 202
PERIPHERAL FIBROMA 177
RANULA AND SIALOCYSTS 202
GIANT CELL FIBROMA 178
DISONTOGENIC CYSTS 203
PERIPHERAL OSSIFYING
FIBROMA 179 LYMPHOEPITHELIAL CYST 204
JUVENILE SPONGIOTIC GINGIVAL SIALOLITHIASIS WITH
HYPERPLASIA 180 SIALADENITIS 205
RETROCUSPID PAPILLAE 181 SALIVARY GLAND TUMORS 207
TORUS MANDIBULARIS AND ADENOMATOID HYPERPLASIA 207
EXOSTOSES 181 MESENCHYMAL NEOPLASMS 208
GINGIVAL CYST 183 LUDWIG’S ANGINA 209
ERUPTION CYST 184 SQUAMOUS CELL CARCINOMA 210
EPULIS FISSURATA 185
CONGENITAL EPULIS 185 Swellings of the Lips And
MESENCHYMAL TUMORS 187 Buccal Mucosa 211
PERIPHERAL ODONTOGENIC
MUCOUS RETENTION
TUMORS 188
(EXTRAVASATION)
SQUAMOUS CELL CARCINOMA 189 PHENOMENON (MUCOCELE) 211
SARCOMAS 190 SIALOCYST 213
MUCOEPIDERMOID MINOR GLAND SIALOLITHIASIS 214
CARCINOMA 191
NASOALVEOLAR (KLESTADT)
NON-HODGKIN’S LYMPHOMA 192 CYST 215
METASTATIC CARCINOMA 193 CHEILITIS GRANULOMATOSA 216
LANGERHANS CELL CHEILITIS GLANDULARIS 217
HISTIOCYTOSIS 194
ANGIONEUROTIC EDEMA 218
ACTINIC PRURIGO 219
Generalized Gingival INFLAMMATORY FIBROUS
Swellings 195 HYPERPLASIA 220
FIBROMATOSIS GINGIVAE 195 FOREIGN BODY GRANULOMA 220
DRUG INDUCED HYPERPLASIA 196 CROHN’S DISEASE 221
NONSPECIFIC HYPERPLASTIC TRAUMATIC FIBROMA 222
GINGIVITIS 197 TRAUMATIC (AMPUTATION)
WEGENER’S GRANULOMATOSIS 198 NEUROMA 224
PMPH_Eversole_Chapter-06.indd 171 1/20/2011 2:22:31 PM
MESENCHYMAL NEOPLASMS 224 SARCOMAS 245
HERNIATED BUCCAL FAT PAD 225 AMYLOID NODULES 246
REACTIVE LYMPHOID SPECIFIC GRANULOMA 247
HYPERPLASIA 226
SQUAMOUS CELL CARCINOMA 248
HEMANGIOMA AND VARIX 227
SQUAMOUS CELL CARCINOMA 229
Palatal Swellings 250
MONOMORPHIC ADENOMA 230
OTHER SALIVARY NEOPLASMS 231 TORUS PALATINUS 250
CYST OF THE INCISIVE PAPILLA 251
Tongue Swellings 232 PALATAL ABSCESS 251
MEDIAN RHOMBOID GLOSSITIS 232 REACTIVE LESIONS OF PALATAL
ECTOPIC LINGUAL THYROID 233 GINGIVAL* 252
THYROGLOSSAL DUCT CYST 234 ADENOMATOUS HYPERPLASIA 252
LINGUAL CYST (ENTERO PLEOMORPHIC ADENOMA 253
CYSTOMA, GASTRIC CYST) 235 POLYMORPHOUS LOW-GRADE
HYPERPLASTIC LINGUAL ADENOCARCINOMA 254
TONSIL 236 MISCELLANEOUS
LINGUAL ABSCESS 237 ADENOCARCINOMAS 255
REACTIVE LESIONS (FIBROMA, ADENOID CYSTIC CARCINOMA 256
PYOGENIC GRANULOMA) 237
MUCOEPIDERMOID
MUCOCELE 238 CARCINOMA 258
HEMANGIOMA AND
ADENOCARCINOMA, NOS 259
LYMPHANGIOMA 239
ATYPICAL LYMPHOPROLIFERATIVE
NEURAL SHEATH TUMORS 241
DISEASE 259
GRANULAR CELL TUMOR 242
SQUAMOUS CELL CARCINOMA** 261
LEIOMYOMA 243
OSTEOCARTILAGINOUS CARCINOMA OF THE ANTRUM 262
CHORISTOMA 244
ECTOMESENCHYMAL *Discussed under Gingival Masses
CHONDROMYXOID TUMOR 245 **Discussed elsewhere in this chapter
PMPH_Eversole_Chapter-06.indd 172 1/20/2011 2:22:31 PM
Both epithelial and mesenchymal lesions The most common tumefactions of the
can produce tumefaction in soft tissues. gingiva or alveolar ridge are the parulis of
The swellings may be of developmental, pulpal or periodontal origin, the pyogenic and
inflammatory, or neoplastic origin, or they peripheral giant cell granuloma, the periph-
may reflect an oral representation of a gen- eral fibroma, and the ossifying fibroma. Recall
eralized systemic disorder. When the clini- that a central jaw lesion may perforate bone
cian develops a differential diagnosis for a and manifest as a gingival growth or epulis.
given lump in the oral cavity, three param- The common swellings of the oral
eters are of paramount importance in the floor are the ranula, the dermoid cyst, and
limitation of the differential: location, con- the lymphoepithelial cyst. The common
sistency, and the presence or absence of swellings of the lips are mucoceles (lower
pain. In this section, diseases that appear lip) and benign salivary tumors (upper lip).
as tumefactions are categorized according Commonly encountered swellings of
to location. Although a disease is listed for the tongue include mesenchymal tumors,
a given topographic locale, that lesion is not chiefly benign hemangiomas or lymp-
limited exclusively to that region. To elimi- hangiomas, neural sheath tumors, and
nate redundancies, the grouping of lesions granular cell tumor. Lethal lesions include
according to location is based on prevalence carcinoma and sarcoma. Systemic diseases
or a tendency for that lesion to occur in a that may cause death and produce tongue
given site. swellings include amyloidosis and specific
When developing a differential diag- granulomatous diseases, such as tuberculo-
nosis, one must be aware both of the ten- sis and histoplasmosis.
dency for a lesion to arise in a given locale The more common palatal swellings
and of the tissues normally present in a are tori, palatal abscesses, and benign or
given region. For example, a swelling in malignant salivary tumors, the latter of
the palate should suggest a diagnosis of which are potentially lethal.
salivary tumor, because the palate is replete Common swellings in the cheek
with minor salivary glands. Nevertheless, include benign mesenchymal tumors,
salivary tissue is, with few exceptions, ubiq- fibrous hyperplasia, and salivary tumors.
uitous in oral mucous membranes. For this Malignant salivary tumors may cause
reason, a swelling in any of the oral tissues death. Retromolar swellings include pri-
could represent a salivary neoplasm. When marily dentigerous cysts from underlying
a disease entity is restricted exclusively to a impacted third molars, pericoronitis, and,
given location, this condition is specified in importantly, mucoepidermoid carcinoma.
the text.
The consistency of a swelling is of
utmost importance when one considers
diagnostic probabilities, determines pro-
Localized Gingival
cedures for securing a definitive diagno-
Tumefactions
sis, and provides treatment. Tumefactions
PARULIS
that are movable and firm, yet not indu-
rated, are most consistent with benign Figure 6-1
neoplasms; tumefactions that are fixed, Age: No predilection
indurated, and ulcerated are more likely Sex: No predilection
to be malignant neoplasms. Swellings that
CLINICAL FEATURES
are tender or painful and may manifest fis-
tulation are, in all probability, inflamma- Inflammation of pulpal or periodontal ori-
tory conditions. gin may drain peripherally, producing a
PMPH_Eversole_Chapter-06.indd 173 1/20/2011 2:22:31 PM
174 Chapter 6
fistula with submucosal abscess formation parulis and radiographed to disclose the
in the gingival tissues. The swelling is fluc- incriminating tooth when other clinical
tuant and may be sore or painless. A paru- findings are equivocal.
lis of odontogenic origin is associated with
a necrotic pulp, and periapical pathosis is TREATMENT
radiographically demonstrable. A parulis Elimination of the source of inflammation
of periodontal origin is found adjacent to a is curative; if pulpal, then endodontics or
deep periodontal pocket. extraction is required. If the source is peri-
odontal, curettage or surgery with debride-
MICROSCOPIC FEATURES
ment of calculus and granulation tissue is
Abscess formation, composed of loose indicated.
connective tissue, eosinophilic exudate,
and neutrophils, may be accompanied
by necrotic debris and scattered chronic Additional Reading
inflammatory cells, chiefly macrophages. Darling AI. In: Gorlin RJ, Goldman HM. Thoma’s Oral
Pathology. Vol 1. 6th ed. St Louis, MO: C. V. Mosby;
DIFFERENTIAL DIAGNOSIS 1970:344.
Hodges TP, Cohan DA., Deck D. Odontogenic sinus
Parulis can be differentiated from other tracts. Am Fam Physician. 1989;40:113.
gingival epulides by locating the source Mitchell DF, Standish SM, Fast TB. Oral Diagnosis/Oral
of infection. Periapical radiographs, pulp Medicine. 3rd ed. Philadelphia, PA: Lea & Febiger;
1978:394.
tests, and pocket probing are useful in Shafer WG, Hine MK, Levy BM. A Textbook of Oral
this respect. A gutta-percha point may be Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
inserted through the fistula feeding the 1983:794.
FIGURE 6-1
Gingival abscess or paru-
lis (gum boil) represents
drainage from an endo-
dontic infection.
PMPH_Eversole_Chapter-06.indd 174 1/20/2011 2:22:31 PM
Intraoral Soft Tissue Swellings 175
PYOGENIC GRANULOMA MICROSCOPIC FEATURES
Figure 6-2 The surface is usually ulcerated, and the
tumor mass is composed of erythrocyte-en-
Age: Teenagers and young adults gorged dilated vascular spaces. The inter-
Sex: Female predilection vening fibrous stroma is infiltrated with
CLINICAL FEATURES inflammatory cells.
The pyogenic granuloma is a reactive, exu-
DIFFERENTIAL DIAGNOSIS
berant overgrowth of granulation tissue
resulting from irritation. It may occur any- Unlike parulis, the pyogenic granuloma
where on the mucocutaneous surfaces but does not contain a purulent exudate nor
is most common on the gingiva. The lesion is there an inflammatory source of infec-
is smooth or bosselated, usually ulcerated, tion from dental origin. The lesion must be
hemorrhagic, and compressible. Pyogenic differentiated from other reactive gingival
granulomas often reach large proportions swellings and hemangioma.
yet generally emanate from a stalk origi-
TREATMENT
nating at a gingival papilla. This lesion is
common among gravid females, hence the Pyogenic granuloma is managed by excision
term pregnancy tumor. It has been suggested and thorough scaling and curettage of the
that the hormonal imbalance coincident adjacent teeth and root surfaces. In the gravid
with pregnancy heightens the organism’s patient, recurrence is likely and treatment, to
response to irritation. be successful, should await parturition.
FIGURE 6-2
Pyogenic granuloma of
maxillary gingiva are ery-
thematous and not related
to pulp disease.
PMPH_Eversole_Chapter-06.indd 175 1/20/2011 2:22:50 PM
176 Chapter 6
FIGURE 6-3
Peripheral giant cell granulo-
mas are reddish purple reac-
tive masses and may erode the
underlying alveolar bone.
ridges and is restricted in location only to these
Additional Reading regions of the mouth. The lesion may reach a
Angelopoulos AP. Pyogenic granuloma of the oral cav- large size and may have a sessile base. The sur-
ity: statistical analysis of its clinical features. J Oral face is either smooth or granular, often with
Maxillofac Surg. 1971;29:840. a blue or purple tinge. It is somewhat firm to
Bhaskar SN, Jacoway JR. Pyogenic granuloma—clinical fea- palpation. Giant cell granuloma is aggressive
tures, incidence, histology, and result of treatment; report
of 242 cases. J Oral Maxillofac Surg. 1966;24:391. and has the potential to erode into underly-
Gordón-Núñez MA, Carvalho MD, Benevenuto TG, Lopes ing alveolar bone. Like other reactive gingival
MF, Silva LM, Galvão HC. Oral Pyogenic Granuloma: growths, it is common in pregnant women
a retrospective analysis of 293 cases in a Brazilian popu- and has a tendency to recur after excision.
lation. J Oral Maxillofac Surg. 2010;68(9):2185-2188.
Lee DW. The fibrous epulis and related lesions.
Periodontics. 1968;6:277. MICROSCOPIC FEATURES
Vilmann A, Vilmann P, Vilmann H. Pyogenic granuloma: A hypercellular fibrovascular stroma pre-
evaluation of oral conditions. Br J Oral Maxillofac
Surg. 1986;24:376.
vails; numerous giant cells are present, many
of which line vascular spaces. The multinu-
cleated cells show a random distribution of
PERIPHERAL GIANT CELL nuclei within the cytoplasm. The lesion is
GRANULOMA often lobulated with heavy deposits of hemo-
Figure 6-3 siderin granules located about the periphery.
Osteoid is also a common feature, elaborated
Age: No predilection within the granulomatous stroma.
Sex: Female predilection
CLINICAL FEATURES DIFFERENTIAL DIAGNOSIS
Peripheral giant cell granuloma may arise Peripheral giant cell granuloma can clinically
on both dentulous and edentulous alveolar resemble any of the other gingival tumefac-
PMPH_Eversole_Chapter-06.indd 176 1/20/2011 2:22:56 PM
Intraoral Soft Tissue Swellings 177
tions, including reactive and neoplastic con- Sapp JP. Ultrastructure and histogenesis of peripheral
ditions. An infectious source is lacking. giant cell reparative granuloma of the jaws. Cancer.
1972;30:119.
TREATMENT
Giant cell granulomas originate from gin-
gival tissues (i.e., periosteum) and require PERIPHERAL FIBROMA
excision extending to bone. Recurrence can Figure 6-4
be anticipated if the lesion is not excised in
Age: Young adults
its entirety. The adjacent teeth should be
Sex: Female predilection
scaled to remove any irritants associated
with plaque. CLINICAL FEATURES
Peripheral fibroma is merely a focal
Additional Reading fibrous hyperplasia of the marginal gin-
giva and is analogous to the fibroma or
Bhaskar SN, Cutright DE. Giant cell reparative granu- inflammatory hyperplasia occurring else-
loma (peripheral): report of 50 cases. J Oral Maxillofac where in the mouth. Peripheral fibroma
Surg. 1971;29:110. may evolve as such or may represent a
Buchner A, Shnaiderman-Shapiro A, Vered M. Relative
frequency of localized reactive hyperplastic lesions of
late sclerosing stage of a pyogenic granu-
the gingiva: a retrospective study of 1675 cases from loma. It is usually smooth, nonulcerated,
Israel. J Oral Pathol Med. 2010. [Epub ahead of print] firm, and lacking discoloration. Although
Eversole LR, Sabes WR, Rovin S. Reactive lesions of the peripheral fibromas may become quite
gingiva. J Oral Pathol Med. 1972;1:30.
Giansanti JS, Waldron CA. Peripheral giant cell granu-
large, they usually emanate from a slen-
loma: Review of 720 cases. J Oral Maxillofac Surg. der stalk originating on a single gingival
1969;27:787. papilla.
FIGURE 6-4
Peripheral fibroma mani-
festing as a firm, normal-
colored tumefaction.
PMPH_Eversole_Chapter-06.indd 177 1/20/2011 2:23:29 PM
178 Chapter 6
MICROSCOPIC FEATURES more frequently than maxillary growths.
Surface epithelium is distended by a mass They also arise on the tongue, palate, buc-
of dense fibrous connective tissue that may cal mucosa, and lips. Similar lesions can be
contain mild diffuse inflammatory cell infil- found on the skin and genitalia.
trates or may be devoid of inflammation.
Occasionally, multinucleated fibroblasts are MICROSCOPIC FEATURES
encountered, the so-called giant cell fibroma. The mass may be papillary or smooth
and is covered by a thin layer of stratified
DIFFERENTIAL DIAGNOSIS squamous epithelium. The bulk of the spec-
The normal mucosal color and firm consis- imen is represented by irregular swirls of
tency help to differentiate the peripheral collagen fibers with interspersed plump ste-
fibroma from pyogenic or peripheral giant late and spindle-shaped fibroblasts. Many
cell granuloma. The clinical appearance may of these cells exhibit a “manta ray” appear-
be identical to that of ossifying fibroma, gingi- ance and possess 2 to 5 oval nuclei.
val cysts, or peripheral odontogenic tumors.
DIFFERENTIAL DIAGNOSIS
TREATMENT Papillary appearing lesions are clinically
Excision with root scaling of adjacent teeth indistinguishable from papilloma, con-
is recommended. dyloma, and other focal papillary lesions
described in the next chapter. Dome-
shaped lesions may be confused with the
Additional Reading other localized gingival swellings listed
in this chapter. Most giant cell fibromas
Bhaskar SN, Jacoway JR. Peripheral fibroma and periph-
arise on attached gingiva away from the
eral fibroma with calcification. J Am Dent Assoc.
1966;73:1312. interdental papilla and are normal in color,
Eversole LR, Rovin S. Reactive lesions of the gingiva. thereby eliminating most of the reactive
J Oral Pathol Med. 1972;1:30. proliferations from consideration. A biopsy
Lee KW. The fibrous epulis and related lesions. is required to obtain a diagnosis.
Periodontics. 1968;6:277.
Zhang W, Chen Y, An Z, Geng N, Bao D. Reactive
gingival lesions: a retrospective study of 2,439 cases. TREATMENT
Quintessence Int. 2007;38(2):103-110.
Most giant cell fibromas are pedunculated,
and simple surgical excision is the treat-
GIANT CELL FIBROMA ment of choice. Recurrence is rare.
Figure 6-5
Age: Teenagers and young adults
Sex: No predilection
CLINICAL FEATURES
The giant cell fibroma is basically a fibrous
proliferation with distinctive microscopic
features and may represent a reactive or
benign neoplastic process. It is smooth or
papillary and usually pedunculated. Most
lesions are small and normal in color. One FIGURE 6-5
half of these lesions are located on the gin- Small gingival nodule representing a giant cell
giva, with mandibular lesions occurring fibroma.
PMPH_Eversole_Chapter-06.indd 178 1/20/2011 2:23:59 PM
Intraoral Soft Tissue Swellings 179
on edentulous ridges. Like other reactive
Additional Reading proliferations of the gingivae, female predi-
Fletcher CD. Giant cell fibroblastoma of soft tis- lection and association with pregnancy are
sue: a clinicopathological and histochemical study. encountered. The lesion is firm, usually not
Histopathology. 1988;13:499. discolored. The surface is smooth, yet may
Houston GD. The giant cell fibroma. A review of 464 occasionally be ulcerated. It emanates from
cases. Oral Surg Oral Med Oral Pathol. 1982;53:582.
Kuo RC, Wang YP, Chen HM, Sun A, Liu BY, Kuo YS. one gingival papilla. It frequently recurs
Clinicopathological study of oral giant cell fibromas. after excision.
J Formos Med Assoc. 2009;108(9):725-729.
Regezi JA, Courtney RM, Kerr DA. Fibrous lesions of
the skin and mucous membrane which contain stellate MICROSCOPIC FEATURES
and multinucleated cells. Oral Surg Oral Med Oral Surface epithelium may be ulcerated, and
Pathol. 1975;39:605.
Weathers DR, Callihan MD. Giant-cell fibroma. Oral
the bulk of the tissue mass is composed of
Surg Oral Med Oral Pathol. 1974;37:374. collagenous fibers with hypercellular plump
fibroblasts. Osteoid or oval cementum-like
deposits are randomly oriented within the
PERIPHERAL OSSIFYING fibrous element.
FIBROMA
Figure 6-6 DIFFERENTIAL DIAGNOSIS
Age: Young adults Peripheral ossifying fibroma resembles the
Sex: Female predilection other focal swellings included here; however,
unlike pyogenic granuloma and peripheral
CLINICAL FEATURES
giant cell granuloma, it usually has a nor-
Peripheral ossifying fibroma is located mal coloration. Microscopic examination is
exclusively on the gingiva and is rarely seen required for a definitive diagnosis.
FIGURE 6-6
Peripheral ossifying
fibroma, which is a firm,
usually normal-colored
growth of the marginal
gingiva.
PMPH_Eversole_Chapter-06.indd 179 1/20/2011 2:24:06 PM
180 Chapter 6
TREATMENT a strawberry appearance, which may be
Because the lesion probably arises in the ulcerated and often emanate from the inter-
periodontal ligament, the excision should dental papillae. These lesions may be reac-
be deep, including periosteum and liga- tive in nature with clinical features of an
ment, and thorough root scaling of adjacent inflamed papillary pyogenic granuloma.
teeth should be performed.
MICROSCOPIC FEATURES
Additional Reading Epithelial hyperplasia is seen with spongi-
otic acanthosis characterized by anastomo-
Bhaskar SN, Jacoway JR. Peripheral fibroma and periph- sing rete pegs. The supportive connective
eral fibroma with calcification. J Am Dent Assoc. tissue fronds are represented by areolar,
1966;73:1312.
hypervascular connecitve tissue showing a
Eversole LR, Sabes WR, Rovin S. Reactive lesions of the
gingiva. J Oral Pathol Med. 1972;1:30. mixed leukocytic infiltrate.
Gardner DG. The peripheral odontogenic fibroma: an
attempt at clarification. Oral Surg Oral Med Oral DIFFERENTIAL DIAGNOSIS
Pathol. 1982;54:40.
Salum FG, Yurgel LS, Cherubini K, De Figueiredo MA, Inflamed papilloma and pyogenic granu-
Medeiros IC, Nicola FS. Pyogenic granuloma, periph- loma are the chief entities to be considered
eral giant cell granuloma and peripheral ossifying in the differential diagnosis. Microscopic
fibroma: retrospective analysis of 138 cases. Minerva
Stomatol. 2008;57(5):227-232.
examination is required for the final
diagnosis.
JUVENILE SPONGIOTIC TREATMENT
GINGIVAL HYPERPLASIA Focal gingivectomy (local excision) is the
Figure 6-7 treatment of choice.
Age: Children
Sex: Female predilection Additional Reading
CLINICAL FEATURES
Chang JY, Kessler HP, Wright JM. Localized juvenile
Papillary hyperplastic lesions occur on the spongiotic gingival hyperplasia. Oral Surg Oral Med
gingiva among children and appear “pasted Oral Pathol Oral Radiol Endod. 2008;106:411-418.
[Epub 2008 Jul 7].
on” to the gingival mucosa. Many of these Darling MR, Daley TD, Wilson A, Wysocki GP. Juvenile
lesions occur in children with braces. The spongiotic gingivitis. J Periodontol. 2007;78:1235-
lesions show a granular red surface with 1240.
FIGURE 6-7
Juvenile spongiotic gingival hyperplasia.
PMPH_Eversole_Chapter-06.indd 180 1/20/2011 2:24:27 PM
Intraoral Soft Tissue Swellings 181
FIGURE 6-8
The retrocuspid papilla, a developmental papule located on the lingual gingiva adjacent to mandibular
cuspids.
RETROCUSPID PAPILLAE
Figure 6-8
Additional Reading
D’Aoust P, Landry R, Ganske R, Carrier J. The prevalence
Age: Young adults of the retrocuspid papilla among three indigenous groups
Sex: No predilection of patients. Study of the subjects in Ecuador, Honduras
and Nicaragua. Ont Dent. 1991;68(8):39, 43, 45 passim.
CLINICAL FEATURES Easley JR, Weis RW. Incidence of the retrocuspid papil-
Retrocuspid papillae are 2- to 4-mm pap- la. J Dent Child. 1970;37:523.
Everett FG, Hall WB, Bennett JS. Retrocuspid papillae.
ules located bilaterally on the lingually Periodontics. 1965;3:81.
attached gingiva immediately posterior to Gorsky M, Begleiter A, Buchner A, Harel-Raviv M. The
the mandibular cuspids. They are soft, of retrocuspid papillae in Israeli Jews. Oral Surg Oral
normal color, and not associated with any Med Oral Pathol. 1986;62:240.
Hirschfeld I. The retrocuspid papillae. Am J Orthod
causative factor. They probably represent Dentofacial Orthop. (Oral Surg Sec.) 1947;33:447.
developmental anomalies and may merely
represent a variant of giant cell fibroma.
TORUS MANDIBULARIS AND
MICROSCOPIC FEATURES EXOSTOSES
An epithelium-covered papule is composed Figure 6-9
of fibrous connective tissue. Fibroblasts
may contain 2 or 3 nuclei being stellate or Age: Adults
Sex: Slightly more common among females
spindle in shape.
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS Whereas tori and exostoses are hard tis-
The small papules may resemble a parulis sue lesions, they are included with the soft
or fistula; however, lack of an infectious tissue swellings because of their clinical
source and bilateral location generally allow resemblance to other gingival swellings.
for a clinical diagnosis. Mandibular tori are located bilaterally
on the lingual mandibular gingiva in the
cuspid-premolar region. Being bosselated
TREATMENT and extremely hard, they represent bony
No treatment is necessary. excrescences. Unilateral instances occur less
PMPH_Eversole_Chapter-06.indd 181 1/20/2011 2:24:43 PM
182 Chapter 6
FIGURE 6-9
Lingual tori. These are usu-
ally small, yet may reach
the large proportions seen
here.
frequently. They are rather common among TREATMENT
all races and are encountered in one third No treatment is required. Tori can be
of the Eskimo population. Tori are inherited removed by chisel or burr should they inter-
as an autosomal dominant trait. Progres- fere with fabrication of a dental prosthesis.
sive slow growth occurs throughout adult-
hood. Exostoses are multiple similar lesions
located on the buccal aspect of the maxillary
and mandibular alveolus. Both may show
Additional Reading
oval radiopacities on dental radiographs. Blakemore JR, Eller DJ, Tomaro AJ. Maxillary exostoses.
Oral Surg Oral Med Oral Pathol. 1975;40:200.
Kolas S, Halprin V. The occurrence of torus palatinus
MICROSCOPIC FEATURES
and torus mandibularis in 2,478 dental patients. Oral
Mature osseous trabeculae emanate from an Surg Oral Med Oral Pathol. 1953;6:1134.
outer cortex and are admixed with fibrous Sawair FA, Shayyab MH, Al-Rababah MA, Saku T.
Prevalence and clinical characteristics of tori and jaw
or adipose marrow. exostoses in a teaching hospital in Jordan. Saudi Med J.
2009;30(12):1557-1562.
DIFFERENTIAL DIAGNOSIS Summers CJ. Prevalance of tori. J Oral Maxillofac Surg.
1968;26:718.
The bony, hard consistency and bilateral- Suzuki M, Sakai T. A familial study of torus palati-
ity of tori are features sufficiently unique to nus and torus mandibularis. Am J Phys Anthropol.
allow for a clinical diagnosis. 1960;18:263.
PMPH_Eversole_Chapter-06.indd 182 1/20/2011 2:24:55 PM
Intraoral Soft Tissue Swellings 183
GINGIVAL CYST MICROSCOPIC FEATURES
Figure 6-10 The cystic lining resembles that of nonkera-
tinizing lateral periodontal cyst. The micro-
Age: Middle-aged adults scopic features are unique. The lining
Sex: No predilection epithelium is cuboidal and pursues a tortu-
CLINICAL FEATURES ous course with a multicystic pattern. Focal
Submucosal cysts of the gingiva appear acanthotic excrescences are seen and are
as firm or compressible smooth-surfaced composed of clear cells. The multiple cys-
nodules with a blanched appearance. The tic cavities probably interconnect at various
mandibular gingiva adjacent to the pre- levels and are separated by dense fibrous
molars is the most common location. The tissue devoid of inflammation. Some gingi-
pathogenesis is variable; they may arise val cysts show ameloblastic differentiation
from rests of Serres or epithelial implanta- with ghost cells, keratinization, and cal-
tion, or they may be the peripheral coun- cification. Lesions of this nature represent
terpart of the central lateral periodontal peripheral calcifying and keratinizing (Gor-
cyst. Others may not be clinically obvious, lin) cysts.
but are discernible as microcysts in routine
DIFFERENTIAL DIAGNOSIS
gingival surgical specimens. Regardless
of their origin, all gingival cysts are rela- Reactive proliferations generally arise in
tively self-limited in terms of their growth the gingival papilla area, whereas cysts
potential. They are located in attached are oriented away from the gingival mar-
gingiva removed from the free gingival gin. Parulis and peripheral odontogenic
margin. tumors may show identical clinical fea-
FIGURE 6-10
Gingival cysts arising from
the dental lamina or rests
of Serres are either firm
or fluctuant.
PMPH_Eversole_Chapter-06.indd 183 1/20/2011 2:25:19 PM
184 Chapter 6
tures; the former can usually be eliminated deciduous or permanent tooth. Therefore, it
from consideration by ruling out a source of is seen directly overlying the alveolus at the
inflammation. site of eruption. It may be dark red when it
is blood filled.
TREATMENT
Gingival cysts can be excised or enucleated. MICROSCOPIC FEATURES
Lining stratified squamous or columnar
Additional Reading epithelium is present, and the follicular
wall evinces an avid inflammatory cell
Buchner A, Hansen LS. The histomorphologic spectrum infiltrate.
of the gingival cyst in the adult. Oral Surg Oral Med
Oral Pathol. 1979;48:532.
DIFFERENTIAL DIAGNOSIS
Freedman PD, Lumerman H, Gee JK. Calcifying odon-
togenic cyst. A review and analysis of seventy cases. The clinical features are diagnostic. Neo-
Oral Surg Oral Med Oral Pathol. 1975;40:93.
plasia has not been reported to arise from
Noonan V, Kemp S, Gallagher G, Kabani S. Gingival
cyst. J Mass Dent Soc. 2008;57(3):62. the lining of eruption cysts.
Reeve CM, Levy BP. Gingival cysts: a review of the
literature and a report of four cases. Periodontics. TREATMENT
1968;6:115.
Wysocki G, Brannon RB, Gardner DG, Sapp P. The soft tissue cap can be excised to uncover
Histogenesis of the lateral periodontal cyst and the the erupting tooth.
gingival cyst of the adult. Oral Surg Oral Med Oral
Pathol. 1980;50:327.
Additional Reading
ERUPTION CYST Anderson BB. Hemorrhagic cysts associated with erupt-
Figure 6-11 ing teeth. Ann Dent. 1942;1:114.
Clark CA. A survey of eruption cysts in the newborn.
Age: Children Oral Surg Oral Med Oral Pathol. 1962;14:917.
Sex: No predilection Koch H, Schwartz O, Klausen B. Indications for surgical
removal of supernumerary teeth in the premaxilla. Int
CLINICAL FEATURES J Oral Maxillofac Surg. 1986;15:273.
Puranik RS, Vanaki SS. Dentigerous cyst vs. eruption
The eruption cyst is a soft tissue dentiger- cyst. Aust Dent J. 2007;52(4):345.
ous cyst arising from the reduced enamel Seward MH. Eruption cyst: an analysis of its clinical fea-
epithelium and follicle of an erupting tures. J Oral Maxillofac Surg. 1973;31:31.
FIGURE 6-11
An eruption cyst appearing
as an inflamed mass of the
gingiva overlying an erupt-
ing tooth.
PMPH_Eversole_Chapter-06.indd 184 1/20/2011 2:25:37 PM
Intraoral Soft Tissue Swellings 185
FIGURE 6-12
Redundant tissue folds underlying a denture flange, representing fibrous hyperplasia secondary to
irritation.
EPULIS FISSURATA TREATMENT
Figure 6-12 The tissue should be excised and examined
microscopically. A new set of dentures or a
Age: Adults relining is required to prevent reestablish-
Sex: No predilection ment of the hyperplastic response.
CLINICAL FEATURES
Flabby, redundant soft tissue masses, which
are often fissured or bosselated, emanate Additional Reading
from the base of the alveolar ridge and Cutright DE. The histopathologic findings in 583 cases
extend into the mucobuccal fold, as hyper- of epulis fissuratum. Oral Surg Oral Med Oral Pathol.
plastic responses to ill-fitting dental pros- 1974;37:401.
theses. The hyperplastic tissue is located at Hatton ER, Gogan CM, Hatton MN. Common oral
conditions in the elderly. Am Fam Physician.
the contact area of the denture flange and
1989;40:149.
generally has a broad base of attachment. Passeri LA, de Abreu EM, de Carvalho AC, Line SR.
Epulis fissurata is usually of normal color, The use of tissue conditioner or zinc oxide and eugenol
yet may show foci of inflammation with impression paste in the excision of epulis fissurata.
ulceration. It is soft to palpation. J Nihon Univ Sch Dent. 1987;29:87.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
MICROSCOPIC FEATURES 1983:552.
Surface epithelium overlies masses of dense
fibrous connective tissue that contains vari-
able amounts of inflammatory cells. Focal CONGENITAL EPULIS
myxomatous zones and cartilaginous rests Figure 6-13
may be seen when the lesion is located on the
interior maxillary alveolus and mucobuccal Age: Present at birth
fold. Sex: Female predilection
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS The congenital epulis is a neoplasm of
Redundant hyperplastic tissue must be dif- unknown origin found exclusively on
ferentiated from the other gingival tume- the alveolar ridge. A large polypoid soft
factions, including carcinoma. Its soft mov- swelling, which may reach a diameter of
ability and broad base are usually sufficient several centimeters, emanates from a con-
to make this lesion clinically recognizable. stricted stalk that attaches the tumor to the
PMPH_Eversole_Chapter-06.indd 185 1/20/2011 2:25:48 PM
186 Chapter 6
FIGURE 6-13
Firm or rubbery gingival
masses emanating from a
constricted stalk in congen-
ital epulis of the newborn.
edentulous alveolus of newborns. Congeni- or teratoma, both of which are extre-
tal epulis is more common on the maxillary mely rare.
anterior alveolar ridge. The tumor is some-
what firm yet may be compressible. TREATMENT
Excision with inclusion of the stalk or base
MICROSCOPIC FEATURES
may be accomplished without danger of
The overlying epithelium is intact and recurrence.
unremarkable. The tumor is composed of
large swollen granular or foamy cells with a
round pyknotic nucleus. The fibrous stroma
is scant; only small vascular channels are
Additional Reading
seen. The cellular architecture is extremely Blair AE, Edwards DM. Congenital epulis of the new-
born. Oral Surg Oral Med Oral Pathol. 1977;43:687.
monomorphic with no cytologic atypia, and
Custer RP, Fust JA. Congenital epulis. Am J Clin Pathol.
organoid configurations are not featured. 1952;22:1044.
Recent evidence based on electron micro- Fuhr AH, Krough PH. Congenital epulis of the newborn:
scopic findings supports a pericyte origin centennial review of the literature and a report of case.
for this lesion. J Oral Maxillofac Surg. 1972;30:30.
Guven S, Kaymakci A, Bugday MS, Yilmaz M. Congenital
granular cell tumor. J Craniofac Surg. 2009;20(3):976-
DIFFERENTIAL DIAGNOSIS 977.
Rohrer MD, Young SK. Congenital epulis (gingival
Congenital epulis is infrequently found. A cell tumor): ultrastructural evidence of origin from
pedunculated mass in the newborn on the pericytes. Oral Surg Oral Med Oral Pathol. 1982;
gingiva may occur in congenital sarcoma 53:56.
PMPH_Eversole_Chapter-06.indd 186 1/20/2011 2:25:57 PM
Intraoral Soft Tissue Swellings 187
MESENCHYMAL TUMORS rocay bodies, the latter with delicate hap-
Figure 6-14 hazardly arranged fibrous tissue showing
S-100 nuclear and cytoplasmic localization.
Age: No predilection Leiomyomas are spindle cell benign prolif-
Sex: Depends on tumor type erations populated by spindle nuclei with
CLINICAL FEATURES blunt ends and stain with smooth muscle
actin. Solitary fibrous tumors are pattern-
A variety of soft tissue tumors may arise less spindle cell proliferations with wavy
on the gingival and alveolar ridges. The collagen and stain for CD34.
more common entities are hemangioma,
nerve sheath tumors, leiomyomas and soli- DIFFERENTIAL DIAGNOSIS
tary fibrous tumor. These lesions are far
less commonly encountered than the reac- The soft tissue tumors are clinically similar
tive lesions of fibrovascular and periodon- to reactive gingival lesions yet biopsy will
tal fibrous origin. As a group, they present disclose their mesenchymal differentia-
as dome shaped, sometimes multinodu- tion depending on the tissues they resem-
lar, submucosal tumefactions with normal ble. Neurofibromas may be multiple with
coloration except for angiomatous lesions, accompanying skin tumors and café-au-
which are red or purple. They are firm yet lait pigmentations in von Recklinghausen’s
not indurated and are usually fixed to the neurofibromatosis.
underlying periosteum.
TREATMENT
MICROSCOPIC FEATURES Simple local excision with clear margins is
the treatment of choice.
The mesenchymal tumors show micro-
scopic features that differentiate into pat-
terns that resemble their cells of origin.
Hemangiomas may show cavernous or cel-
Additional Reading
lular capillary structures that are engorged Perrotti V, Rubini C, Fioroni M, Piattelli A. Soft tissue
myxoma: report of an unusual case located on the gin-
with red cells. Angioleiomyomas show cen- giva. J Clin Periodontol. 2006;33:76-78.
tral vascular lumens surrounded by con- Rosenberg ES, Iravani F. Hemangioma of gingiva—a
centric layers of smooth muscle cells and case report. Quintessence Int Dent Dig. 1979;10:
collagenous tissues, the former positive for 17-21.
Safadi RA, Hellstein JW, Diab MM, Hammad HM. Nerve
smooth muscle actin. Nerve sheath tumors sheath myxoma (neurothekeoma) of the Gingiva, a
include neurilemmom and neurofibroma, case report and review of the literature. Head Neck
the former with Antoni A tissue and ver- Pathol. 2010;4(3):242-245.
FIGURE 6-14
Mesenchymal gingival tumors (nerve sheath tumor, hemangioma, leiomyoma) are firm submucosal
masses.
PMPH_Eversole_Chapter-06.indd 187 1/20/2011 2:26:16 PM
188 Chapter 6
PERIPHERAL ODONTOGENIC of tumor seen (see chapters dealing with
TUMORS radiolucencies and radiopacities). Two
Figure 6-15 odontogenic tumors are characteristically
extraosseous. The peripheral odontogenic
Age: Young adults hamartoma is composed of fibrous tissue
Sex: Depends on tumor type with linear epithelial cords and is synony-
CLINICAL FEATURES
mous with peripheral odontogenic fibroma.
The other gingival tumor, ameloblastic fibro-
Tumors that arise from the odontogenic appa- dentinoma, occurs in children and is repre-
ratus or remnants of the tooth germ are, as sented by dental lamina-like epithelial cell
a rule, intraosseous. Occasionally, they arise rests, some of which show stellate reticulum.
in the extraosseous tissues of the alveolus. These cell rests are dispersed throughout a
Clinically, they are nodular smooth-surfaced mesenchymal stroma that is poorly endowed
tumefactions of the gingiva that are firm to with collagen. An eosinophilic dentin-like
palpation. Soft tissue ossification may be amorphous product is found in juxtaposi-
detectable in radiographs in some of these tion to the epithelial cell component.
tumors. The odontogenic tumors that can
originate in the gingiva are the Gorlin cyst, DIFFERENTIAL DIAGNOSIS
Pindborg tumor, odontogenic adenomatoid
tumor, ameloblastoma, peripheral odonto- Extraosseous odontogenic tumors show
genic hamartoma, peripheral odontogenic clinical features in common with the reac-
fibroma, and ameloblastic fibrodentinoma. tive proliferations and gingival cysts.
MICROSCOPIC FEATURES TREATMENT
The tumor cells may or may not be encap- Simple excision is the treatment of choice.
sulated and vary, depending on the type Peripheral forms of odontogenic tumors,
FIGURE 6-15
Peripheral odontogenic
tumors (calcifying odon-
togenic cyst, ameloblastic
fibroma, calcifying epithe-
lial odontogenic tumor,
ameloblastoma).
PMPH_Eversole_Chapter-06.indd 188 1/20/2011 2:26:26 PM
Intraoral Soft Tissue Swellings 189
considered aggressive when located cen- MICROSCOPIC FEATURES
trally, behave nonaggressively, with little Invasive nests and islands of squamous epi-
tendency for recurrence. thelium are encountered, and most tumors
evince parakeratin pearls or squamous
Additional Reading eddies. The individual cells show vary-
ing degrees of pleomorphism, hyperchro-
Baden E, Moskow BS, Moskow R. Odontogenic gin- matism, and mitoses. The fibrous stroma
gival epithelial hamartoma. J Oral Maxillofac Surg. is frequently infiltrated by mononuclear
1968;26:702. cells.
Buchner A, Sciubba JJ. Peripheral epithelial odontogenic
tumors: a review. Oral Surg Oral Med Oral Pathol.
1987;63:688. DIFFERENTIAL DIAGNOSIS
Gardner DG. Peripheral ameloblastoma: a study of 21
cases, including 5 reported as basal cell carcinoma of Swellings of the gingiva or edentulous ridge
the gingiva. Cancer. 1977;39:1625. representing carcinoma may be confused
Gardner DG. The peripheral odontogenic fibroma: an with reactive proliferations included in this
attempt at clarification. Oral Surg Oral Med Oral section on gingival tumefactions. Usually
Pathol. 1982;54:40.
Ide F, Obara K, Mishima K, et al. Peripheral odontogen-
the patient’s age, when considered along
ic tumor: a clinicopathologic study of 30 cases. General with lesional induration, ulceration, and/or
features and hamartomatous lesions. J Oral Pathol keratosis, supports a clinical impression of
Med. 2005;34(9):552-557. cancer. An incisional biopsy is essential to a
definitive diagnosis.
SQUAMOUS CELL
TREATMENT
CARCINOMA
Figure 6-16 Squamous cell carcinoma must be treated
aggressively to achieve a cure. Radiother-
Age: Elderly apy and surgery are generally combined,
Sex: Male predilection along with regional node dissection in the
CLINICAL FEATURES
presence of palpable nodes. Prophylactic
neck dissection or radiation therapy is usu-
Squamous cancer of the gingiva and alve- ally indicated in the absence of palpable
olar ridge represents about 15% of all oral nodes. The prognosis is based on tumor
squamous cell carcinomas. The swelling size (T), the presence or absence of nodal
is either red or keratotic and may appear metastasis (N), and the presence or absence
granular or ulcerated. The lesion frequently of distant metastasis (M). The 5-year sur-
extends into the mucobuccal fold or oral vival for patients with lesions less than 3 cm
floor and is most prevalent on the mandib- is about 80%. Invasion of underlying bone
ular arch. In addition, the marginal tissue along with periosteal lymphatic invasion
is frequently leukoplakic or erythroplakic. worsen the prognosis; bone scanning may
The swelling is usually indurated. Palpation provide additional information regarding
of the submandibular and cervical regions extent of disease before planning surgical
is essential in order to detect any clinical intervention.
evidence of regional metastasis; a thorough
medical work-up should be pursued along
with a chest radiograph to evaluate for dis- Additional Reading
tant metastases. All squamous cell carcino-
Lubek J, El-Hakim M, Salama AR, Liu X, Ord RA.
mas in this location should be assessed for Gingival carcinoma: retrospective analysis of 72
bone invasion of the alveolus by procuring patients and indications for elective neck dissection. Br
panoramic and periapical radiographs. J Oral Maxillofac Surg. 2010. [Epub ahead of print.]
PMPH_Eversole_Chapter-06.indd 189 1/20/2011 2:26:43 PM
190 Chapter 6
FIGURE 6-16
Squamous cell carcinoma
of the gingiva.
Martin HE. Cancer of the gums (gingivae). Am J Surg. patients, neurogenic sarcoma, and leiomyo-
1941;54:765. sarcoma. As a group, they are rapidly grow-
Nathanson A, Jakobsson A, Wersall J. Prognosis
of squamous cell carcinoma of the gums. Acta ing, often ulcerated and indurated masses,
Otolaryngol. 1973;75:301. and many are friable and hemorrhagic.
Tiecke RW, Bernier JL. Statistical and morpho- Myelogenous leukemia may form extravas-
logical analysis of four hundred and one cases of cular infiltrates of the soft tissues accom-
intraoral squamous cell carcinoma. J Am Dent Assoc.
1954;49:684.
panied by leukocytosis and bone marrow
Willen R, Nathanson A, Moberger G, Anneroth G. infiltrates (granulocytic sarcoma).
Squamous cell carcinoma of the gingiva. Histological
classification and grading of malignancy. Acta
Otolaryngol. (Stockh.) 1975;79:146. MICROSCOPIC FEATURES
As mentioned earlier, the sarcoma nosol-
ogy is based on patterns of differentiation.
SARCOMAS
Immunohistochemical markers are of value
Figure 6-17 in refining or corroborating the histopatho-
Age: Young adults
logic features. As a group, most are spindle
Sex: Depends on tumor type cell proliferations that exhibit hypercellu-
larity, nuclear pleomorphism, and mitotic
CLINICAL FEATURES figures, many of which are atypical. Most
Like benign mesenchymal tumors, sarco- sarcomas stain positively for vimentin, a
mas differ according to their differentiation. connective tissue protein. Other markers
These malignancies are very rare in the oral are also assessed for aiding the diagnosis
cavity and may occur in any location. The such as muscle (desmin, actin), nerve sheath
more common are fibrosarcoma, malig- (S-100 protein), and hematologic (various
nant fibrous histiocytoma, angiosarcoma CD cell surface proteins). Granulocytic sar-
in human immunodeficiency virus (HIV) coma is characterized by a round cell infil-
PMPH_Eversole_Chapter-06.indd 190 1/20/2011 2:26:43 PM
Intraoral Soft Tissue Swellings 191
FIGURE 6-18
Mucoepidermoid carcinoma, often observed as a
swelling in the retromolar pad area.
FIGURE 6-17
Fibrosarcoma of the gingiva. Chi AC, Barnes JD, Budnick S, Agresta SV, Neville
B. Rhabdomyosarcoma of the maxillary gingiva.
J Periodontol. 2007;78:1839-1845.
trate, positive with myeloid markers and Matsushita K, Abe T, Takeda Y, et al. Granulocytic sarco-
chloracetate esterase. ma of the gingiva: two case reports. Quintessence Int.
2007;38(10):817-820.
DIFFERENTIAL DIAGNOSIS
The rapid growth, size, and induration seen MUCOEPIDERMOID
with sarcomas are also seen in primary CARCINOMA
squamous cell carcinomas, lymphomas,
Figure 6-18
and metastatic tumors. The use of the afore-
mentioned markers will assist the patholo- Age: Teenagers and adults
gist in determining what cell the tumor is Sex: No predilection
attempting to mimic.
CLINICAL FEATURES
TREATMENT Mucoepidermoid carcinoma is included
Radical surgery is usually required along with gingival tumefactions because of the
with resection of the jaws. Some types propensity of this tumor to arise at the pos-
respond to radiation therapy and adjunct terior confines of the mandibular alveolus,
chemotherapy. The specific type of sarcoma the retromolar pad. It arises from salivary
dictates the treatment. glands normally present in this location
and may be indurated or fluctuant and
cystic, resembling a mucocele. The surface
Additional Reading mucosa is generally intact. Occasionally,
Agnihotri R, Bhat KM, Bhat GS. A rare case of malig-
cystic, mucin-filled spaces occur superfi-
nant fibrous histiocytoma of the gingiva. J Periodontol. cially, giving the tumor a vesicular or bleb-
2008;79:955-960. like appearance.
PMPH_Eversole_Chapter-06.indd 191 1/20/2011 2:26:55 PM
192 Chapter 6
MICROSCOPIC FEATURES
Neoplastic ductal, cuboidal, and squamous
Additional Reading
epithelia are present, as are mucous cells. Bhaskar SN, Bernier JL. Mucoepidermoid tumors of
The neoplastic islands may be solid or cys- major and minor salivary glands. Cancer. 1962;15:801.
Eversole LR. Mucoepidermoid carcinoma; review of 815
tic with large dilated mucin-filled spaces.
reported cases. J Oral Maxillofac Surg. 1970;28:490.
Kahn MA, Lucas RM. Mucoepidermoid tumor: a case
DIFFERENTIAL DIAGNOSIS report involving the operculum of an erupting perma-
nent second molar. Oral Surg Oral Med Oral Pathol.
The other tumefactions of the gingiva 1989;68:375.
included in this section tend to occur ante- Melrose RJ, Abrams AM, Howell FV. Mucoepidermoid
riorly. Retromolar swellings, which appear tumors of the intraoral minor salivary glands: a clini-
copathologic study of 54 cases. J Oral Pathol Med.
clinically similar, include mucocele, erup-
1973;2:314.
tion cyst from an impacted third molar, and Triantafillidou K, Dimitrakopoulos J, Iordanidis F,
mesenchymal neoplasms. Koufogiannis D. Mucoepidermoid carcinoma of minor
salivary glands: a clinical study of 16 cases and review
of the literature. Oral Dis. 2006;12:364-370.
TREATMENT
Low-grade tumors are treated by wide local
excision. High-grade malignancy requires NON-HODGKIN’S LYMPHOMA
wide excision and block resection of the
Figure 6-19
underlying mandibular bone. Careful
evaluation of the neck is necessary because Age: Adults
nodal involvement requires in-continuity Sex: Male predilection
neck dissection or, at least, supraomohyoid
CLINICAL FEATURES
dissection when submandibular nodes are
palpable. Lymphomas in the oral cavity are extran-
odal and rare. When they occur, one should
be suspicious of HIV infection. Clinically,
HIV-associated lymphomas of the oral cavity
are most often encountered on the gingiva,
particularly the palatal gingiva. The lesions
are indurated, ulcerated, and erythematous
and manifest extremely rapid growth. Pain
and paresthesia are uncommon symptoms.
Gingival lesions may induce saucerization
of the underlying bone. Oral non-Hodgkin’s
lymphomas among non-HIV subjects often
arise centrally in the jaws. T-cell lymphomas
associated with human lymphotropic virus
are endemic on certain islands in Japan, yet
the head and neck lesions tend to arise in
Waldeyer’s ring rather than in the oral cav-
ity proper.
MICROSCOPIC FEATURES
FIGURE 6-19 As with nodal lymphomas, non-Hodgkin’s
Gingival mass representing HIV-associated extran- lymphomas of the oral regions are usually
odal lymphoma. of B-lymphocyte origin and can exhibit a
PMPH_Eversole_Chapter-06.indd 192 1/20/2011 2:27:02 PM
Intraoral Soft Tissue Swellings 193
variety of cytologic patterns depending histologic diagnosis has been established.
on the degree of differentiation. Therefore, Radiation therapy is recommended for
some lesions consist of large cleaved and localized oral lesions; disseminated disease
noncleaved lymphoblasts, whereas others requires multiregimen chemotherapy.
are represented by small lymphoblasts or
lymphocytes. A nodular pattern is not usu-
ally observed in these extranodal lesions, Additional Reading
and the periphery of the infiltrate is com-
Green TL, Eversole LR. Oral lymphomas in HIV-
monly represented by stringy, elongated infected patients: association with Epstein-Barr virus
degenerative lymphocytes. A Burkitt’s lym- DNA. Oral Surg Oral Med Oral Pathol. 1989;67:437.
phoma-like histologic pattern (starry-sky Handlers JP, Howell RE, Abrams AM, Melrose RJ.
pattern) is frequently noted, particularly Extranodal oral lymphoma. Part 1. A morphologic and
immunoperoxidase study of 34 cases. Oral Surg Oral
in HIV-associated oral lymphomas. Some Med Oral Pathol. 1986;61:362.
lesions contain Epstein-Barr virus genomic Kaugers GE, Burns JC. Non-Hodgkin’s lymphoma of the
DNA. oral cavity associated with AIDS. Oral Surg Oral Med
Oral Pathol. 1989;67:433.
DIFFERENTIAL DIAGNOSIS Keszler A, Piloni MJ, Paparella ML, Soler Mde D, Ron
PC, Narbaitz M. Extranodal oral non-Hodgkin’s lym-
Reactive gingival tumefactions, including phomas. a retrospective study of 40 cases in Argentina.
pyogenic granuloma and giant cell granu- Acta Odontol Latinoam. 2008;21(1):43-48.
Kurihara K, Kohno H, Miyamoto N, Chikamori Y,
loma, must be considered in the clinical Kondo T. Pathologic characteristics of human T-cell
diagnosis, because they too can display an lymphotropic virus (HTLV)-related extranodal oro-
extremely rapid growth rate. Most of the facial lymphomas. Oral Surg Oral Med Oral Pathol.
lesions appearing as localized tumefactions 1990;70:199.
of the gingiva do not spread laterally and
diffusely as does lymphoma.
METASTATIC CARCINOMA
TREATMENT Figure 6-20
Extranodal non-Hodgkin’s lymphomas in Age: Adults and elderly
the oral cavity convey variable prognoses Sex: Depends on tumor type
depending on the specific type. Often the
CLINICAL FEATURES
patient has disseminated disease, and it is
imperative to subject patients to a complete Metastatic tumors may be seen central in
work-up for lesions in other areas once a bone as well as in the soft tissues of the
FIGURE 6-20
Metastatic renal cell carcinoma, magnetic resonance imaging showing metastatic tumor infiltration of
mandible and abdominal images of primary tumor (arrow) involving kidney.
PMPH_Eversole_Chapter-06.indd 193 1/20/2011 2:27:04 PM
194 Chapter 6
gingiva. The most common primary sites requiring various combinations of surgery,
are breast, lung, colon, prostate, and kidney. radiation, and chemotherapy.
They appear as multinodular, often hemor-
rhagic ulcerated masses with rapid growth.
Oftentimes, at the time of biopsy, the pri- Additional Reading
mary site is unknown, and a metastatic Califano L, Sanguedolce F, Staibano S, et al. Large oral
work-up is required. soft tissue metastasis from anaplastic carcinoma of the
lung mimicking a primitive malignancy: case report
MICROSCOPIC FEATURES and brief review of the literature. Minerva Stomatol.
2008;57:447-451.
The microscopic features are unique to Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger
the patterns seen in the primary organs of R. Metastatic tumours to the oral cavity - pathogenesis
origin. The tumors usually comprise cyto- and analysis of 673 cases. Oral Oncol. 2008;44:743-
logically atypical cells that can represent 752. [Epub 2007 Dec 3.]
Pozzi EC, Altermatt HJ, Rees TD, Bornstein MM.
undifferentiated tumors, clear cell tumors, Exophytic mass of the gingiva as the first manifes-
adenocarcinomas, and squamous cell car- tation of metastatic pulmonary adenocarcinoma.
cinomas. Immunohistochemistry (IHC) J Periodontol. 2008;79:187-191.
markers are valuable in defining the organs
of origin including breast markers such as
progesterone and estrogen receptors as well
LANGERHANS CELL
as Her-2-Nu, prostate specific antigen, car- HISTIOCYTOSIS
cinoembryonic antigen, and cytokeratins to Figure 6-21
name but a few.
Age: Children
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Metastatic tumors clinically resemble pri- CLINICAL FEATURES
mary malignancies such as squamous cell The Langerhans cell is a specialized mac-
carcinoma, salivary malignancies, lympho- rophage that resides in the epithelium of
mas, and sarcomas. When assessed micro- skin and mucous membranes and functions
scopically and the tumor is thought to as an antigen-presenting cell in the context
represent a metastasis, a metastatic clinical, of the afferent limb of the immune response.
imaging, and laboratory work-up is required Clonal proliferation of Langerhans cells
in order to locate the primary focus. may be focal or multifocal. Acute dissemi-
nated Langerhans cell histiocytosis (LCH)
TREATMENT occurs in infants and toddlers presenting
Therapy is varied depending upon site of with multiorgan involvement, typically liver
origin and degree of dissemination usually and spleen along with a cutaneous papular
FIGURE 6-21
Langerhans histiocytosis is
primarily a bone lesion in
the jaws yet may extend
into the gingiva.
PMPH_Eversole_Chapter-06.indd 194 1/20/2011 2:27:11 PM
Intraoral Soft Tissue Swellings 195
rash. Chronic disseminated LCH occurs in Disseminated disease is successfully man-
children and teens in which infiltrates of aged by chemotherapy, usually Vinca alka-
Langerhans cells may result in intraosseous loids (vincristin, vinblastin).
lesions including radiolucencies of the
skull and jaws, retro-orbital infiltrates caus-
ing exophthalmos and posterior pituitary Additional Reading
lesions with resultant diabetes insipidis. In Annibali S, Cristalli MP, Solidani M, et al. Langerhans
young adults, localized LCH may present cell histiocytosis: oral/periodontal involvement in adult
with a single focus of tumor cells, often seen patients. Oral Dis. 2009;15:596-601. [Epub 2009 Sep
in the lungs or the jaws. Jaw lesions of LCH 16].
Bottomley WK, Gabriel SA, Corio RL, Jacobson RJ,
may appear as periradicular periodontal Rothchild N. Histiocytosis X: report of an oral soft tis-
radiolucenies yielding a “tooth floating in sue lesion without bony involvement. Oral Surg Oral
space” appearance, and the overlying gin- Med Oral Pathol. 1987;63(2):228-231.
giva is red, enlarged, and often ulcerated. Hicks J, Flaitz CM. Langerhans cell histiocytosis: current
insights in a molecular age with emphasis on clinical
oral and maxillofacial pathology practice. Oral Surg
MICROSCOPIC FEATURES Oral Med Oral Pathol Oral Radiol Endod. 2005;100
The Langerhans cell is dentrocytic when (2 suppl):S42-S66.
seen in the epithelium; however in LCH,
large mononuclear cells are seen and pos-
sess oval clear nuclei with surrounding Generalized Gingival
eosinophilic cytoplasms and an accompa- Swellings
niment of scattered eosinophils. Langer-
hans cells stain for CD1a and S-100 protein FIBROMATOSIS GINGIVAE
and on election microscopy Birbeck organ- Figure 6-22
elles, shaped like small tennis rackets, are
encountered. Age: Childhood onset
Sex: No predilection
DIFFERENTIAL DIAGNOSIS CLINICAL FEATURES
LCH may be confused with an inflamma- Transmitted as an autosomal dominant
tory reaction or Hodgkin’s lymphoma. IHC trait, hereditary fibromatosis gingivae
staining of S-100 and/or CD1a are useful becomes obvious soon after eruption of the
markers for the diagnosis of LCH. primary teeth. The gingiva shows multi-
nodular enlargement, most prominent in
TREATMENT the interdental papillar regions. The tissue
Surgical intervention and tooth extraction is firm and of normal color, and the hyper-
may be required for oral and jaw lesions. plasia may be so extensive that the entire
FIGURE 6-22
Generalized fibrotic enlarg-
ement of the gingival
tissues, a feature of heredi-
tary fibromatosis gingivae.
PMPH_Eversole_Chapter-06.indd 195 1/20/2011 2:27:18 PM
196 Chapter 6
coronal portion of the teeth is obliterated. Ye X, Shi L, Yin W, Meng L, Wang QK, Bian Z. Further
Elimination of dental plaque does not sig- evidence of genetic heterogeneity segregating with
hereditary gingival fibromatosis. J Clin Periodontol.
nificantly lessen the severity. The disorder 2009;36:627-633. [Epub 2009 Jun 22.]
has been linked to 2p21. Gingival fibroma-
tosis may be accompanied by other disor-
ders, including splenomegaly, enlarged DRUG INDUCED HYPERPLASIA
nasal and external ear soft tissues, short- Figure 6-23
ened terminal phalanges, hyperflexia of
joints, and hypoplasia of the nails, the so- Age: No predilection
called Laband syndrome. Sex: No predilection
CLINICAL FEATURES
MICROSCOPIC FEATURES
Gingival hyperplasia is encountered among
Gingival epithelium is distended by mas- patients receiving hydantoin, nifedipine,
sive accumulations of mature, dense collag- and cyclosporin A. Gingival enlargement
enous tissue. Inflammation is minimal. occurring in seizure patients receiving
sodium diphenylhydantoin is generalized.
DIFFERENTIAL DIAGNOSIS The gingiva shows bulbous fibrotic firm
Dilantin (phenytoin sodium) hyperplasia, nodules emanating from the papillar regions
hyperplastic gingivitis, and leukemic infil- and may be severe enough to obscure the
tration of the gingiva may show signs clini- crowns of the teeth. The condition is wors-
cally indistinguishable from fibromatosis ened when oral hygiene is poor and dental
gingivae. A history of familial involvement plaque accumulates. Hyperplastic tissue on
is of paramount importance in making the edentulous ridge areas is extremely rare,
diagnosis. yet has been reported to occur in edentu-
lous patients. In general, cyclosporin- and
nifedipine-induced hyperplasia are less
TREATMENT
severe and a pebbly surface is often encoun-
Periodic gingivectomy with placement of a tered. Recent research indicates that specific
gingival acrylic splint or prosthesis can be subpopulations of fibroblasts in the gingiva
done for both cosmetic and functional rea- respond to these drugs with increased pro-
sons. Recurrence to some degree should be liferation and fibrillogenesis.
anticipated.
MICROSCOPIC FEATURES
Additional Reading Surface epithelium is distended by dense
collagenous fibrous tissue. Long, slender
Emerson TG. Hereditary gingival hyperplasia; a fam- so-called test-tube rete ridges extend deeply
ily pedigree of four generations. Oral Surg Oral Med into the subjacent fibrous tissue. Inflamma-
Oral Pathol. 1965;19:1. tory cell infiltration is not a prominent or
Laband PF, Habib G, Humphreys GS. Hereditary gin-
gival fibromatosis. Report of an affected family with consistent finding.
associated splenomegaly and skeletal and soft-tissue
abnormalities. Oral Surg Oral Med Oral Pathol. DIFFERENTIAL DIAGNOSIS
1964;17:339.
Oikawa K, Cavaglia AMV, Lu D. Laband syndrome: A history of epilepsy controlled by diphe-
report of case. J Oral Maxillofac Surg. 1979;37:120. nylhydantoin is necessary for the diagno-
Xiao S, Wang X, Qu B, et al. Refinement of the locus
for autosomal dominant hereditary gingival fibroma-
sis. This drug-related gingival enlargement
tosis (GINGF) to a 3.8-cM region on 2p21. Genomics. may be indistinguishable from fibromatosis
2000;68:247-252. gingivae and may resemble that seen in leu-
PMPH_Eversole_Chapter-06.indd 196 1/20/2011 2:27:23 PM
Intraoral Soft Tissue Swellings 197
FIGURE 6-23
Generalized enlargement of the gingiva as a consequence of medications (hydantoin, cyclosporine, calcium
channel blockers).
kemia and nonspecific hyperplastic gingivi- Dreyer WP, Thomas CJ. Diphenylhydantoinate-induced
tis. Nifedipine is a calcium channel blocker hyperplasia of the masticatory mucosa in an eden-
tulous epileptic patient. Oral Surg Oral Med Oral
used in therapy for coronary artery disease, Pathol. 1978;45:701.
whereas cyclosporin is an immunosuppres- Hassell TM. Gingival overgrowth: hereditary consider-
sive agent prescribed for organ transplant ations. Comp Cont Educ Dent Suppl. 1990;14:S511.
patients.
TREATMENT NONSPECIFIC HYPERPLASTIC
Cosmesis and function may be restored by GINGIVITIS
gingivectomy followed by thorough prophy- Figure 6-24
laxis and institution of a conscientious oral
hygiene home care program. Recurrence is Age: Adults
Sex: No predilection
common, yet the degree of enlargement can
be lessened provided appropriate periodon- CLINICAL FEATURES
tal maintenance therapy is followed. Whereas most forms of nonspecific gingi-
vitis result in mild edema with erythema,
Additional Reading an occasional response is one of swelling
from edema, fibroplasia, and inflammatory
Angelopoulos AP, Goaz PW. Incidence of diphenylhy- cell infiltration. This hyperplastic form of
dantoin gingival hyperplasia. Oral Surg Oral Med Oral
Pathol. 1972;34:898.
gingivitis is characterized by generalized
Castro LA, Elias LS, Oton-Leite AF, et al. Long-term enlargement, particularly interdentally; the
effects of nifedipine on human gingival epithelium: tissues are boggy, and ulceration is not fre-
a histopathological and immunohistochemical study. quent. Erythema is generally present. Den-
J Oral Sci. 2010;52:55-62.
DeCamargo PM. Cyclosporin and nifedipine-induced
tal plaque is accumulated and periodontal
gingival enlargement: An overview. J West Soc disease with pocket formation is often pres-
Periodontol. 1989;37:57. ent as well. The hyperplastic form may be
PMPH_Eversole_Chapter-06.indd 197 1/20/2011 2:27:24 PM
198 Chapter 6
FIGURE 6-24
Nonspecific inflamma-
tory enlargement of the
gingiva.
uncomplicated by systemic disease; how- TREATMENT
ever, underlying medical problems such Dental prophylaxis with scaling and peri-
as uncontrolled diabetes mellitus or cyclic odontal curettage causes the hyperplastic
neutropenia must be ruled out. This form tissue to subside. If the problem is compli-
of gingivitis is frequently seen in gravid cated by systemic disease, systemic as well
women. as local factors must be controlled.
MICROSCOPIC FEATURES
Surface epithelium may be unremarkable, Additional Reading
whereas the crevicular epithelium evinces
Bartolucci EG, Parkes RB. Accelerated periodontal
anastomosing elongated rete ridges. The breakdown in uncontrolled diabetes. Pathogenesis
underlying tissues are fibrovascular with and treatment. Oral Surg Oral Med Oral Pathol.
nonspecific inflammatory cell infiltrates. 1981;52:387.
Fragments of calculus and microbial colo- Benvetiste R, Bixler D, Conneally PM. Periodontal dis-
ease in diabetics. J Periodontol. 1967;38:271.
nies are often found adherent to crevicular Orban B. Classification and nomenclature of periodontal
epithelium. diseases (based on pathology, etiology, and clinical pic-
ture). J Periodontol. 1942;13:88.
DIFFERENTIAL DIAGNOSIS Pandit IK, Pandit N. Non-specific inflammatory gingival
enlargement—a case report. J Indian Soc Pedod Prev
Leukemic infiltrates may show indistin- Dent. 2000;18:21-23.
guishable features. Fibromatosis gingivae Silness J, Low H. Periodontal disease in pregnancy.
and Dilantin hyperplasia can mimic hyper- I. Prevalence and severity. Acta Odontol Scand.
1963;21:532.
plastic gingivitis, yet the former two lesions
are usually not boggy or erythematous. A
blood count, fasting blood sugar, or, prefer- WEGENER’S
ably, a glucose tolerance test can be obtained
GRANULOMATOSIS
to rule out leukemia, cyclic neutropenia,
and diabetes. Figure 6-25
On rare occasions, granulomatous Age: Adults
inflammations such as Wegener’s granulo- Sex: No predilection
matosis or tuberculosis can manifest gen-
CLINICAL FEATURES
eralized gingival enlargement. In these
instances, the surface is pebbly or granular Wegener’s granulomatosis is a rare disorder
and ulceration is present. A biopsy differ- with pathogenic features akin to many of
entiates nonspecific hyperplastic gingivitis the collagen diseases. The pathologic mani-
from these lesions and from leukemia. festations include destructive granulomas
PMPH_Eversole_Chapter-06.indd 198 1/20/2011 2:27:34 PM
Intraoral Soft Tissue Swellings 199
FIGURE 6-25
Diffuse granular gingival
enlargement in Wegener’s
granulomatosis (straw-
berry gums).
of both upper and lower respiratory tract, TREATMENT
necrotizing angiitis, and glomerulonephri- Chemotherapy is the treatment of choice.
tis signaled by sinusitis and rhinitis, cough Combined cyclophosphamide and predni-
with hemoptysis, and uremia. Other tissues sone therapy achieves resolution of lesions
that may be involved include the middle ear, with remission in a few months. Some
urethra, skin, and salivary glands. Whereas patients enjoy fairly long-term remission
osseous destructive lesions are sometimes even after cessation of treatment.
observed in the nose, sinuses, and palate,
the gingival changes are unique and may,
in fact, be pathognomonic of the disease. A
generalized hyperplastic gingivitis is seen
Additional Reading
with a characteristic granular or pebbly Brooke RI. Wegener’s granulomatosis involving the gin-
telangiectatic appearance. Antineutrophil givae. Br Dent J. 1969;127:34.
Israelson H, Binnie WH, Hurt WC. The hyperplastic
cytoplasmic antibodies (ANCA) are classi- gingivitis of Wegener’s granulomatosis. J Periodontol.
cally present in serum. 1981;52:81.
Scott J, Finch LD. Wegener’s granulomatosis present-
MICROSCOPIC FEATURES ing as gingivitis. Review of the clinical and pathologic
features and report of a case. Oral Surg Oral Med Oral
A gingival biopsy discloses granulomatous Pathol. 1972;34:920.
inflammation with a mononuclear infiltrate. Stewart C, Cohen D, Bhattacharyya I, et al. Oral mani-
festations of Wegener’s granulomatosis: a report of
Multinucleated giant cells are present and
three cases and a literature review. J Am Dent Assoc.
in some patients the granulomas are infil- 2007;138:338-348; quiz 396, 398.
trated by numerous eosinophils. The sine Wolff SM, Fauci AS, Horn RG, Dale DC. Wegener’s
qua non on a microscopic basis is the pres- granulomatosis. Ann Intern Med. 1974;81:513.
ence of necrotizing vasculitis.
DIFFERENTIAL DIAGNOSIS TYPE I DIABETES MELLITUS
Although the other entities included here as Figure 6-26
diffuse gingival enlargements may be con- Age: Children
sidered, the granular telangiectatic appear- Sex: No predilection
ance is classic for Wegener’s granulomatosis.
Other symptoms of the disease may be pres- CLINICAL FEATURES
ent, and altered laboratory findings include The most severe form of diabetes (juvenile,
an elevated sedimentation rate and an ele- type I) is most apt to be associated with
vated creatinine level. Chest radiographs gingival enlargement although periodon-
disclose pulmonary involvement. tal lesions may also be encountered among
PMPH_Eversole_Chapter-06.indd 199 1/20/2011 2:27:38 PM
200 Chapter 6
FIGURE 6-26
Hyperplastic gingivitis with
abscess formation in type
1 diabetes.
adult onset cases that are severe. The juve- referral to the patient’s primary care physi-
nile form is an autoimmune disease with an cian should be undertaken, attempting to
immune response being generated to islets achieve improved metabolic control of their
of Langerhans cells and resultant insulin disease.
depletion. Patients develop hyperglyce-
mia, glycosuria, and ketoacidosis as well
as microangiopathic vascular lesions and Additional Reading
large vessel atherosclerotic disease. The
Kinane DF, Marshall GJ. Periodontal manifestations of
gingival enlargement may be diffuse or systemic disease. Aust Dent J. 2001;46:2-12.
multifocal with hyperplastic changes and Soory M. Hormonal factors in periodontal disease. Dent
striking erythema. In addition, periodontal Update. 2000;27:380-383.
abscesses may occur and pus may be com- Van Dis ML, Allen CM, Neville BW. Erythematous
gingival enlargement in diabetic patients: a report
pressed from periodontal pockets. of four cases. J Oral Maxillofac Surg. 1988;46:
794-798.
MICROSCOPIC FEATURES
There are no diabetes-specific changes as
a rule. Diffuse chronic inflammation is PUBERTY/PREGNANCY
encountered along with focal abscess for- GINGIVITIS
mation. Small vessels may show microan- Figure 6-27
giopathy with thickened vascular walls
exhibiting hyaline change. Age: Teens, pregnant women
Sex: Females
DIFFERENTIAL DIAGNOSIS CLINICAL FEATURES
Clinical laboratory tests will confirm diabe- During puberty and pregnancy, female hor-
tes. When gingival enlargement is encoun- monal changes are taking place and these
tered along with periodontal abscesses, metabolic events, in a subset of girls and
diabetes is usually overt. Fasting blood glu- expectant mothers, manifest generalized or
cose will be over 150 mg % (hyperglycemia) multifocal gingival enlargement. The endo-
and sugar will be found in the urine (glyco- crinologic mechanism for gingival lesions
suria). Prolonged glucose elevation is moni- is unknown. Why some females develop
tored by assay of glycosylated hemoglobin. inflammatory gingival enlargement and
others do not has not been determined. The
TREATMENT
gingival tissues are boggy, swollen, and
Antibiotic therapy and periodontal debride- fiery red. They tend to bleed freely upon
ment or surgery are usually necessary, and gingival probing.
PMPH_Eversole_Chapter-06.indd 200 1/20/2011 2:27:46 PM
Intraoral Soft Tissue Swellings 201
MICROSCOPIC FEATURES Tiainen L, Asikainen S, Saxén L. Puberty-associated gingi-
vitis. Community Dent Oral Epidemiol. 1992;20:87-89.
The epithelium is hyperplastic with elon-
gated anastomosing rete ridges. The underly-
ing connective tissue is highly vascularized LEUKEMIA
and an intense, diffuse, and nonspecific Figure 6-28
chronic inflammatory infiltrate prevails.
Age: Children and young adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
CLINICAL FEATURES
Other forms of gingival enlargement must
be considered, and when warranted, biopsy Infiltration of leukemic cells into the gingiva
will help to rule out ominous disease such occurs in approximately one half of patients
as Kaposi’s sarcoma, angiosarcoma, and suffering from acute leukemia, particularly
leukemia. acute monocytic leukemia. The interdental
papillae are enlarged, red or bluish, and
TREATMENT usually boggy, although they may occasion-
Periodontal therapy is the treatment of ally feel firm to palpation. Ulceration with
choice, and antibiotics may be administered pseudomembrane is often seen. Other signs
should any clinical evidence of abscess for- may accompany gingival enlargement: pal-
mation be encountered. lor of the skin and remaining mucosa, gin-
gival hemorrhage, formation of petechiae
and ecchymoses, joint swelling related to
Additional Reading hemarthrosis, and general malaise.
Barak S, Oettinger-Barak O, Oettinger M, Machtei MICROSCOPIC FEATURES
EE, Peled M, Ohel G. Common oral manifestations
during pregnancy: a review. Obstet Gynecol Surv. The fibrous tissue underlying surface and
2003;58:624-628. sulcular epithelium displays a monomor-
Boyarova TV, Dryankova MM, Bobeva AI, Genadiev
GI. Pregnancy and gingival hyperplasia. Folia Med
phic, monotonous infiltrate of leukemia
(Plovdiv). 2001;43:53-56. cells. In monocytic leukemia, the cells are
oval or round with vesicular nucleoplasm
and prominent nucleoli.
DIFFERENTIAL DIAGNOSIS
Nonspecific hyperplastic gingivitis may
show identical features. Fibromatosis gingi-
vae and phenytoin sodium (Dilantin) hyper-
plasia, although usually not associated
with inflamed tissue, should nevertheless
be considered in the differential diagnosis.
Other generalized signs and symptoms will
arouse suspicion of leukemia. A biopsy and
complete blood count should be obtained.
TREATMENT
Leukemia should be managed by a hema-
FIGURE 6-27 tologist. Oral signs diminish or resolve with
Pregnancy gingivitis. Similar lesions may be seen successful treatment of the disease, usually
during transition to puberty. with chemotherapeutic drugs.
PMPH_Eversole_Chapter-06.indd 201 1/20/2011 2:27:57 PM
202 Chapter 6
FIGURE 6-28
Leukemic cell infiltration
of the gingiva, producing
generalized enlargement.
Because the mucin accumulation is super-
Additional Reading ficial, the swelling appears fluid filled and
Demirer S, Ozdemir H, Sencan M, Marakoglu I. Gingival has a bluish cast; the thin membranous sur-
hyperplasia as an early diagnostic oral manifestation in face is traversed by obvious capillary mark-
acute monocytic leukemia: a case report. Eur J Dent. ings. It is compressible and usually located
2007;1:111-114. unilaterally in the vicinity of one of the
Duffy JH, Driscoll EJ. Oral manifestations in leukemia.
Oral Surg Oral Med Oral Pathol. 1958;11:484. submandibular ducts. Salivary flow on the
Lynch MA, Ship II. Oral manifestations of leuke- affected side cannot be elicited by milking
mia; a postdiagnostic study. J Am Dent Assoc. 1967; the gland when a major duct is involved.
75:1139. When minor glands in the floor of the
Michand M, Baehner RL, Bixler D, Kafrawy AH. Oral
manifestations of acute leukemia in children. J Am
mouth are affected, salivary flow may be
Dent Assoc. 1977;95:1145. normal. Many of the smaller cystic lesions
Tjwa E, Mattijssen V. Images in clinical medicine. are true sialocysts.
Gingival hypertrophy and leukemia. N Engl J Med.
2008;359:e21.
MICROSCOPIC FEATURES
Most ranulas are fluid (mucin)-filled spaces
Swellings of the Oral Floor lined by a granulation tissue wall repre-
senting a large mucocele. Less frequently,
RANULA AND SIALOCYSTS they may be lined by cuboidal ductal epi-
Figure 6-29 thelium with areas of oncocytic metaplasia
representing sialocysts.
Age: No predilection
Sex: No predilection DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
The ranula may be differentiated clinically
A ranula is a mucin-filled cystic or pseudo- from other oral floor swellings by virtue of
cystic cavity in the floor of the mouth. its compressible cystic nature, location lat-
PMPH_Eversole_Chapter-06.indd 202 1/20/2011 2:27:59 PM
Intraoral Soft Tissue Swellings 203
FIGURE 6-29
Ranula, a mucocele of the
oral floor, soft and fluctuant.
eral to the midline, and bluish, fluid-filled DISONTOGENIC CYSTS
character. It is conceivable that a low-grade Figure 6-30
cystic mucoepidermoid carcinoma in the
floor of the mouth could resemble ranula in Age: Adults
clinical appearance. Sex: No predilection
CLINICAL FEATURES
TREATMENT
The disontogenic cyst includes epidermoid
Ranula is conventionally managed by cyst, dermoid cyst, and teratoid cyst. They
marsupialization. have been suggested to be derived from
entrapped epithelium remaining from
Additional Reading fusion of the embryonic processes forming
the oral floor. These cysts are located in the
Catone GA, Merrill RG, Henny FA. Sublingual gland midline of the anterior floor of the mouth
mucous-escape phenomenon—treatment by exci- as a dome-shaped mass. They protrude
sion of sublingual gland. J Oral Maxillofac Surg.
orally when localized above the mylohyoid
1969;27:774.
Gormley MG, Jarrett W, Seldin R. Ranulas: a series of muscle, submentally when arising below
eighteen cases of extravasation cysts. J Acad Gen Dent. this muscle. Because disontogenic cysts are
1973;21:29. filled with semisolid keratin and sebum,
Harrison JD. Modern management and pathophysi- they are doughy on palpation.
ology of ranula: literature review. Head Neck.
2010;32(10):1310-1320.
Mandel L, Baurmash H. Bilateral ranulas: report of a MICROSCOPIC FEATURES
case. J Oral Maxillofac Surg. 1970;28:621.
Olech, E. Ranula. Oral Surg Oral Med Oral Pathol. The cyst lining is keratinizing stratified
1963;16:1169. squamous epithelium in the epidermoid
PMPH_Eversole_Chapter-06.indd 203 1/20/2011 2:28:18 PM
204 Chapter 6
FIGURE 6-30
Dermoid cysts arising from
the oral floor in the mid-
line—firm, rubbery tume-
factions that elevate the
tongue.
cyst, and the lumen may contain keratin. Colp R. Dermoid cysts of the floor of the mouth. Surg
The dermoid cyst shows histologic patterns Gynecol Obstet. 1925;40:183.
MacNeil SD, Moxham JP. Review of floor of mouth
from the ectodermal and mesodermal germ dysontogenic cysts. Ann Otol Rhinol Laryngol.
layers. The luminal contents are eosino- 2010;119:165-173.
philic, amorphous, and caseous. Respiratory New EB, Erich JG. Dermoid cysts of the head and neck.
epithelium is occasionally present. Within Surg Gynecol Obstet. 1937;65:48.
al-Khayat M, Kenyon GS. Midline sublingual dermoid
the fibrous wall are skin adnexal structures cyst. J Laryngol Otol. 1990;104:578.
such as sebaceous glands, sweat glands, and
hair follicles. Minor salivary tissue may be
present as well. When other connective tis- LYMPHOEPITHELIAL CYST
sues and neural elements are encountered, Figure 6-31
the cyst is classified as a teratoid cyst.
Age: Adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
CLINICAL FEATURES
Most of the other lesions listed in this sec-
tion as oral floor swellings arise lateral to the The lymphoepithelial cyst arising in the
midline. The central location, doughy con- oral floor is histologically analogous to its
sistency, and tendency to elevate the tongue extraoral counterpart, the branchial cleft
are classic signs of a disontogenic cyst. As cyst of the neck. The intraoral variety is gen-
the cyst contents are semisolid, little or no erally small, located in the anterior oral floor,
fluid can be obtained on aspiration. ventral tongue, or lingual frenum and is a
doughy, well-circumscribed nodule. Because
TREATMENT of the involved lymphoid tissue, it may have
The cyst can be delivered surgically by a yellowish cast. The origin is obscure but
simple enucleation. When it is superior may arise from confinement of salivary duct
to the mylohyoid, an intraoral approach epithelium in a small lymph node. Alterna-
is preferred. Submylohyoid dermoids are tively, oral lymphoepithelial cysts have been
removed by an extraoral approach. suggested to represent tonsillar tissue with
keratin-plugged cystic crypts.
Additional Reading MICROSCOPIC FEATURES
Chakravorty RC, Schatzki PF. Lateral sublingual der- Stratified squamous or, rarely, respiratory
moid. Oral Surg Oral Med Oral Pathol. 1975;39:862. epithelium lines the cyst. When squamous
PMPH_Eversole_Chapter-06.indd 204 1/20/2011 2:28:41 PM
Intraoral Soft Tissue Swellings 205
FIGURE 6-31
Benign lymphoepithelial
cysts, yellow modules with
a smooth surface usually
located in the oral floor or
ventral tongue.
epithelium is present, keratin fills the Knapp MJ. Oral tonsils: location, distribution, and histol-
lumen. The wall of the cyst contains sheets ogy. Oral Surg Oral Med Oral Pathol. 1970;29:155.
Seifert G. Lymphoid lesions of the oral cavity. Pathol Res
of lymphocytes with germinal centers. Pract. 1980;167:179-203.
Some examples show a microscopic com- Toto PD, Wortel JP, Joseph G. Lymphoepithelial cysts
munication with the oral epithelium. and associated immunoglobulins. Oral Surg Oral Med
Oral Pathol. 1982;54:59.
DIFFERENTIAL DIAGNOSIS
The small nodule of lymphoepithelial cyst SIALOLITHIASIS WITH
must be differentiated from salivary tumors, SIALADENITIS
benign mesenchymal neoplasms, mucocele,
Figure 6-32
and salivary stones.
Age: Adults
TREATMENT Sex: Male predilection
The nodule should be excised because a CLINICAL FEATURES
clinical diagnosis cannot unequivocably be
made. More than 90% of all sialoliths occur within
the submandibular duct. When they arise
in the distal aspect, they do so as oral floor
Additional Reading swellings. Duct occlusion produces swell-
ing and fibrosis of the affected gland. The
Buchner A, Hansen LS. Lymphoepithelial cysts of the duct is usually painless; however, pain on
oral cavity: a clinicopathologic study of thirty-eight
cases. Oral Surg Oral Med Oral Pathol. 1980;50:441.
the affected side is elicited when eating.
Giunta J, Cataldo E. Lymphoepithelial cysts of the oral Salivary flow from the sublingual orifice
mucosa. Oral Surg Oral Med Oral Pathol. 1973;35:77. cannot be initiated on milking of the gland.
PMPH_Eversole_Chapter-06.indd 205 1/20/2011 2:28:56 PM
206 Chapter 6
FIGURE 6-32
Salivary stones causing
swelling in the oral floor
with distension of the
submandibular salivary
duct, visible with occlusal
radiographs.
The dilated duct containing the stone is a TREATMENT
rock-hard nodule. Occasionally, an occluded Small stones may be delivered through the
gland becomes subject to secondary patho- duct orifice by manual manipulation. When
genic bacteria with development of acute they are large, surgical removal is indicated.
sialadenitis. The affected gland and duct Removal of the involved gland may be nec-
enlarge and are acutely tender to palpation. essary, particularly if fibrosis and second-
In addition, an exudate can often be milked ary infection exist. The use of lithotriptor
from the Wharton’s duct. destruction of salivary stones has proven
successful.
MICROSCOPIC FEATURES
The decalcified specimen shows a stone
with concentric laminations. The ductal
lining shows metaplasia within the epithe-
Additional Reading
lium so that stratified squamous, mucous Levy BM, ReMine WH, Devine KD. Salivary gland
cell formation, or oncocytic change may be calculi: pain, swelling associated with eating. JAMA.
1962;181:1115.
discerned. Respiratory epithelium may be
Marmary Y. A novel and non-invasive method for the
present. removal of salivary gland stones. Int J Oral Maxillofac
Surg. 1986;15:585.
DIFFERENTIAL DIAGNOSIS Narang R, Dixon RA. Surgical management of subman-
dibular sialadenitis and sialolithiasis. Oral Surg Oral
The oral floor swelling may mimic neo- Med Oral Pathol. 1977;43:210.
plasm or cyst; however, the symptoms and © Seldin HM, Seldin SD, Rakower W. Conservative
indurated calcific nature of sialolithiasis are surgery for removal of salivary calculi. Oral Surg Oral
usually present, providing the information Med Oral Pathol. 1963;6:579.
Zhang L, Escudier M, Brown J, Capaccio P, Pignataro L,
necessary to make a clinical diagnosis. An McGurk M. Long-term outcome after intraoral remov-
occlusal radiograph discloses the presence al of large submandibular gland calculi. Laryngoscope.
of a radiopacity in the floor of the mouth. 2010;120:964-966.
PMPH_Eversole_Chapter-06.indd 206 1/20/2011 2:29:14 PM
Intraoral Soft Tissue Swellings 207
SALIVARY GLAND TUMORS major forms are discussed under palatal
Figure 6-33 swellings.
Age: Adults DIFFERENTIAL DIAGNOSIS
Sex: Male predilection Benign salivary tumors must be differen-
CLINICAL FEATURES tiated from mesenchymal neoplasms and
Salivary neoplasms, benign or malignant, sclerosing sialadenitis. Indurated swellings
may on rare occasions arise within the major suspected of being salivary adenocarcino-
or minor sublingual glands in the floor of mas must be differentiated from subman-
the mouth. Salivary tumors of the oral floor dibular lymph node metastasis from a
are more commonly seen in the subman- primary oral carcinoma and from primary
dibular gland with evidence of a mass in sarcomas.
the lateroposterior region. Submandibu-
lar tumors may not be visually noticeable TREATMENT
intraorally but become obvious on biman- Benign tumors are treated by sialectomy.
ual palpation. If the tumor is benign, it will Malignant salivary neoplasms require
be firm but encapsulated and movable. The resection with radical neck dissection
most common tumor is the pleomorphic when cervical or supraomohyoid nodes are
adenoma; however, both submandibular palpable.
and sublingual gland neoplasms are more
apt to represent malignancies than are
parotid tumors. Adenocarcinomas may be Additional Reading
of any type, yet adenoid cystic carcinoma
Eneroth CM, Hjertman L. Benign tumors of the subman-
or cylindroma and mucoepidermoid car- dibular gland. Pract Otorhinolaryngol. 1967;29:166.
cinoma are the tumors more frequently Eneroth CM, Hjertman L, Moberger G. Malignant
encountered. Malignant salivary tumors tumors of the submandibular gland. Acta Otolaryngol.
are nonencapsulated, indurated, and may (Stockh.). 1967;64:514.
Hanna DC, Clairmont AA. Submandibular gland tumors.
or may not evince fixation. J Plast Reconstr Surg. 1978;61:198.
Martin VT, Salmaso R, Onnis GL. Tumors of salivary
MICROSCOPIC FEATURES glands. Review of 479 cases with particular reference
to histologic types, site, age and sex distribution. Appl
The microscopic features vary, depend-
Pathol. 1989;7:154.
ing on the type of tumor present. The Rapidis AD, Stavrianos S, Lagogiannis G, Faratzis G.
Tumors of the submandibular gland: clinicopatho-
logic analysis of 23 patients. J Oral Maxillofac Surg.
2004;62:1203-1208.
ADENOMATOID HYPERPLASIA
Figure 6-34
Age: Teens, adults
Sex: No Predilection
CLINICAL FEATURES
FIGURE 6-33 Adenomatous or adenomatoid hyperplasia
Salivary neoplasms of the submandibular and sub- of minor salivary glands occurs unilaterally
lingual glands can manifest as unilateral oral floor in the posterior hard palate and soft palate.
swellings. Clinically, the lesion is soft to palpation and
PMPH_Eversole_Chapter-06.indd 207 1/20/2011 2:29:27 PM
208 Chapter 6
TREATMENT
Once the diagnosis has been secured by
biopsy, no further treatment is required.
Additional Reading
Gnepp DR, Wang LJ, Brandwein-Gensler M, Slootweg
P, Gill M, Hille J. Sclerosing polycystic adenosis of the
salivary gland: a report of 16 cases. Am J Surg Pathol.
2006;30:154-164.
Herrera-Calvo G, García-Montesinos-Perea B, Saiz-
Bustillo R, Gallo-Terán J, Lastra-García-Barón P.
Unilateral submandibular gland aplasia with ipsilat-
eral sublingual gland hypertrophy presenting as a neck
mass. Med Oral Patol Oral Cir Bucal. 2010. [Epub
FIGURE 6-34 ahead of print.]
Adenomatous hyperplasia of the submandibular Mathison CC, Hudgins PA. Bilateral submandibu-
gland. lar gland aplasia with hypertrophy of sublingual
glands. Otolaryngol Head Neck Surg. 2008;138:
119-120.
Smith BC, Ellis GL, Slater LJ, Foss RD. Sclerosing
polycystic adenosis of major salivary glands. A clini-
asymptomatic appearing as a submucosal
copathologic analysis of nine cases. Am J Surg Pathol.
nodule. Similarly, glandular hyperplasia of 1996;20:161-170.
the sublingual or submandibular gland may
cause lobular swellings in the floor of the
mouth. This lesion is frequently mistaken MESENCHYMAL NEOPLASMS
for a salivary gland tumor. In fact, adenom- Figure 6-35
atoid hyperplasia is a non-neoplastic over-
growth of normal salivary glands. Sclerosing Age: More frequent in adults
polycystic adenosis may also arise in the sub- Sex: Slight male predilection
mandibular gland although it is more com- CLINICAL FEATURES
mon in the parotid. There is disagreement
as to whether this lesion is hyperplastic or Benign or malignant connective tissue
neoplastic, yet some develop dysplasia. tumors may arise in any location. Although
mesenchymal neoplasms are more fre-
MICROSCOPIC FEATURES quently seen in the tongue and buccal
mucosa, they nevertheless arise in the oral
These hyperplasias show histologic features floor and appear as smooth-surfaced eleva-
identical to that of the normal resident sali- tions. Reactive tumor-like proliferations,
vary glands. Seromucous acini with serous the fibromatoses, may also be located in
demilunes typical for submandibular gland the floor of the mouth. Benign mesenchy-
are seen along with ductal elements. Scle- mal tumors are encapsulated or well delin-
rosing polycystic adenosis is characterized eated, soft or firm, and movable. The more
by multiple cystic spaces lined by colum- common entities include lipoma, fibroma,
nar and cuboidal cells, often with apocrine hemangioma, and neural sheath tumors.
differentiation. A special form of lymphangioma, the cys-
tic hygroma, occurs in this location and
DIFFERENTIAL DIAGNOSIS
usually bulges extraorally. The sarcomas
Clinically, salivary tumors are the primary are multinodular, indurated, and usually
concern. fixed. Although all sarcomas are rare in this
PMPH_Eversole_Chapter-06.indd 208 1/20/2011 2:29:35 PM
Intraoral Soft Tissue Swellings 209
FIGURE 6-35
Mesenchymal neoplasms
in the oral floor (neurofi-
broma, hemangioma).
region, the entities most likely to be present Devi M, Nalin Kumar S, Ranganathan K, Saraswathi
include fibrosarcoma and lymphoma. TR. Oral intra vascular papillary endothelial hyper-
plasia in the floor of the mouth. Indian J Dent Res.
2004;15(4):149-151.
MICROSCOPIC FEATURES O’Day RA, Soule EH, Gores RJ. Soft tissue sarcomas of
the oral cavity. Mayo Clin Proc. 1964;39:169.
The histologic patterns found in mesen- Vindenes H. Lipomas of the oral cavity. Int J Oral
chymal neoplasms are extremely varied, Maxillofac Surg. 1978;7:162.
depending on the type of tumor and cell of Watson WL, McCarthy WD. Blood and lymph vessel
origin. Some are described in the section on tumors; a report of 1,056 cases. Surg Gynecol Obstet.
1940;71:569.
tongue swellings.
DIFFERENTIAL DIAGNOSIS LUDWIG’S ANGINA
Oral floor swellings representing mes- Figure 6-36
enchymal tumors are firm or indurated
and must be differentiated from salivary Age: No predilection
Sex: No predilection
tumors, sclerosing sialadenitis, and meta-
static lymphadenopathy. Those of vascular CLINICAL FEATURES
origin may be less encapsulated, particu- Odontogenic infection with drainage into
larly lymphangiomas, and therefore require the fascial spaces of the oral floor produces
wide excision. Sarcomas require radical swelling. When bilateral involvement of
excision. A diagnosis of lymphoma requires the submandibular and sublingual spaces
further work-up to detect dissemination; occurs in conjunction with cellulitis of the
the disease is managed by radiation and mylohyoid and tongue musculature, a dif-
chemotherapeutic methods. fuse boardhard swelling evolves and is
obvious both extraorally and intraorally.
TREATMENT The patient is febrile, with malaise. Pain is
Well-localized nodules representing benign severe. Death may ensue from encroach-
mesenchymal neoplasms are treated by ment of edema and cellulitis on the airway
simple surgical excision. or spread of infection into the paravertebral
space and mediastinum.
Additional Reading MICROSCOPIC FEATURES
Brandjord RM, Reaume CE, Wesley RK. Leiomyosarcoma
The tissues are avidly and diffusely infil-
of the floor of the mouth: Review of the literature and trated with neutrophils and scattered
report of case. J Oral Maxillofac Surg. 1977;35:590. histiocytes.
PMPH_Eversole_Chapter-06.indd 209 1/20/2011 2:29:38 PM
210 Chapter 6
Taffel M, Harvey SC. Ludwig’s angina. Surgery.
1942;11:841.
Williams AC, Guralnick WC. Diagnosis and treatment
of Ludwig’s angina; report of 20 cases. N Engl J Med.
1943;228:443.
SQUAMOUS CELL
CARCINOMA
Figure 6-37
Age: Middle-aged and elderly adults
Sex: Male predilection
FIGURE 6-36
Ludwig’s angina with diffuse swelling of the sub- CLINICAL FEATURES
mandibular area, also showing elevation of the oral Squamous cancer of the oral floor may
floor.
appear red, white, mixed red and white,
ulcerated, or tumefactive; the floor of the
DIFFERENTIAL DIAGNOSIS mouth represents the most common site for
oral cancer. Invasive tumefactive lesions are
The only other disease that can extend into indurated and usually ulcerated. They are
all regions of the oral floor as an indurated most frequently located anteriorly, overly-
swelling resembling Ludwig’s angina is ing Wharton’s duct. They may infiltrate
infiltrating carcinoma or sarcoma. In these laterally to involve the alveolar ridge or
instances, fever is not a dominant sign and ventral tongue. About one half of patients
conspicuous odontogenic infection with a present with nodal involvement of the sub-
carious or nonvital tooth is not featured, mandibular or cervical region.
unless it occurs as a coincidental finding.
Whereas streptococci are usually cultured
MICROSCOPIC FEATURES
from the tissue, anaerobic organisms may
be responsible, either as concomitants or as Oral floor squamous cell carcinoma is
primary agents. characterized by invasive cords, nests, and
islands comprising squamous cells showing
TREATMENT varying degrees of hyperchromatism, pleo-
morphism, and increased mitotic activity.
Antibiotic therapy with multiple incisions
Parakeratin pearl formation can usually be
for drainage is required to prevent respira-
identified. Many oral floor tumors, particu-
tory embarrassment. Intravenous antibiotic
larly smaller lesions, maintain carcinoma
therapy with hospitalization and support-
in-situ changes along the lateral margins.
ive care for infection are necessary.
These changes frequently extend along sali-
vary excretory ducts.
Additional Reading DIFFERENTIAL DIAGNOSIS
Holland CS. The management of Ludwig’s angina. Br J
Oral Maxillofac Surg. 1975;13:153. Most noncancerous oral floor swellings are
Juang YC, Cheng D, Wang L, Liu C, Duh R, Chang C. soft and exhibit an intact mucosal surface.
Ludwig’s angina: an analysis of 14 cases. Scand J Infect Any lesion that is indurated and ulcer-
Dis. 1989;21:121.
Reynolds SC, Chow AW. Severe soft tissue infections of
ated should be considered, in all prob-
the head and neck: a primer for critical care physicians. ability, a carcinoma; immediate biopsy is
Lung. 2009;187:271-279. [Epub 2009 Aug 5.] indicated.
PMPH_Eversole_Chapter-06.indd 210 1/20/2011 2:29:48 PM
Intraoral Soft Tissue Swellings 211
FIGURE 6-37
Squamous cell carcinomas
of the oral floor showing
keratotic and ulcerated
tumefaction.
TREATMENT Zini A, Czerninski R, Sgan-Cohen HD. Oral cancer
over four decades: epidemiology, trends, histology,
Combined radiation therapy and surgery and survival by anatomical sites. J Oral Pathol Med.
are preferable over a single method. Lymph 2010;39:299-305. [Epub 2009 Dec 15.]
node dissection is advocated when palpable
nodes are present and is usually advisable
in the absence of palpable nodes. Survival Swellings of the Lips and
depends on extent of disease. Resection of Buccal Mucosa
the adjacent mandible is often necessary
owing to periosteal extension of tumor. MUCOUS RETENTION
Overall 5-year survival for this site is about (EXTRAVASATION)
50%. PHENOMENON (MUCOCELE)
Figure 6-38
Additional Reading Age: Young adults
Sex: Slight male predilection
Ballard BR, Suess GR, Pickren JW, Greene GW,
Shedd DP. Squamous cell carcinoma of the floor of CLINICAL FEATURES
the mouth. Oral Surg Oral Med Oral Pathol. 1978;
45:568.
The mucocele is the most common swell-
Feind CR, Cole RM. Cancer of the floor of the mouth ing of the lower lip and arises secondary
and its lymphatic spread. Am J Surg. 1968;116:482. to traumatic severance of a minor salivary
Martin HE, Sugarbaker EL. Cancer of the floor of the duct with pooling of extraductal mucin in
mouth. Surg Gynecol Obstet. 1940;71:347.
Nason RW. Surgical management of squamous cell
the submucosa. It may be seen on the buc-
carcinoma of the floor of the mouth. Am J Surg. cal mucosa as well. It is a dome-shaped
1989;158:292. elevation, which, if superficial, has a
PMPH_Eversole_Chapter-06.indd 211 1/20/2011 2:29:52 PM
212 Chapter 6
FIGURE 6-38
Mucocele, generally seen
on the lower lip as fluctu-
ant fluid-filled blebs.
bluish fluid-filled appearance. If situated giving the appearance of hemangioma or
deep, it may be of normal color. A history varix.
of paroxysmal swelling and collapse is
common. TREATMENT
Mucoceles cannot be unroofed and be
MICROSCOPIC FEATURES expected to resolve. Excision with inclusion
The epithelium is distended by a pseudo- of the underlying salivary tissue helps to
cystic space filled with mucin infiltrated minimize the chance for recurrence.
with neutrophils and foamy histiocytes. The
wall is composed of granulation tissue.
Additional Reading
DIFFERENTIAL DIAGNOSIS Cataldo E, Mosadomi A. Mucoceles of the oral mucous
membrane. Arch Otolaryngol Head Neck Surg.
When mucoceles are superficial, they 1970;91:360.
may resemble bullae. The remaining oral Cohen L. Mucoceles of the oral cavity. Oral Surg Oral
tissues, conjunctivas, and skin must be Med Oral Pathol. 1965;19:365.
Hayashida AM, Zerbinatti DC, Balducci I, Cabral
examined to rule out bullous dermatoses. LA, Almeida JD. Mucus extravasation and reten-
Mucoepidermoid carcinoma may clinically tion phenomena: a 24-year study. BMC Oral Health.
resemble mucocele yet is extremely rare 2010;10(1):15.
in the lip. Deeply situated mucoceles may Standish SM, Shafer WG. The mucous retention phenom-
enon. J Oral Surg Oral Med Oral Pathol. 1959;17:15.
appear identical to fibrous hyperplasia or Yamasoba T, Tayama N, Syoji M, Fukuta M.
mesenchymal neoplasms. Occasionally, Clinicostatistical study of lower lip mucoceles. Head
blood enters the cystic cavity of a mucocele, Neck. 1990;12:316.
PMPH_Eversole_Chapter-06.indd 212 1/20/2011 2:30:17 PM
Intraoral Soft Tissue Swellings 213
SIALOCYST episodic release of the fluid contents. There-
Figure 6-39 fore, some sialocysts may arise from partial
duct blockage by mucous plugs. Clinically,
Age: Adults the lesions are fluctuant, nonulcerated, and
Sex: No predilection movable submucosal nodules. Although
CLINICAL FEATURES most are clearly visualized, deeper lesions
may only be detectable by palpation. Some
Sialocysts are fluid filled, well-localized patients have multiple lesions.
swellings of the submucosa. Whereas the
floor of the mouth is the favored site for
MICROSCOPIC FEATURES
most sialocysts, the lips and buccal mucosa
are also frequent locations, especially in Sialocysts occur in three variations: simple
elderly patients who have oncocytic cells mucous retention cysts lined by cuboidal
in their lining. Whether or not sialocysts epithelium, reactive oncocytoid cysts lined
are true blind cysts or merely represent by columnar ductal cells with foci of onco-
aneurysmal-like dilatation of an obstructed cytic metaplasia, and mucopapillary cysts
duct is not conclusive. The latter is more that are multilocated and tortuous, and con-
probable because many patients report tain papillary configurations with lining
fluctuations in the size of the lesions with columnar and mucous-secreting cells. Some
FIGURE 6-39
Sialocyst of the buccal
mucosa.
PMPH_Eversole_Chapter-06.indd 213 1/20/2011 2:30:42 PM
214 Chapter 6
pathologists think that the mucopapillary Eversole LR. Oral sialocysts. Arch Otolaryngol Head
cysts are true benign neoplasms and prefer Neck Surg. 1987;113:51.
Eversole LR, Sabes WR. Minor salivary gland duct
to label them as papillary cystadenomas. changes due to obstruction. Arch Otolaryngol Head
Neck Surg. 1971;94:19.
DIFFERENTIAL DIAGNOSIS Southam JC. Mucous retention cysts of the oral mucosa.
J Oral Pathol Med. 1983;3:197.
Sialocysts are clinically indistinguish- Tal H, Altini M, Lemmer J. Multiple mucous retention
able from mucoceles owing to their com- cysts of the oral mucosa. Oral Surg Oral Med Oral
pressible, fluctuant nature; fluctuation in Pathol. 1984;58:692.
size is also a common feature. Low-grade
mucoepidermoid carcinoma should be
considered in the differential diagnosis. MINOR GLAND
Indeed, microscopically, the mucopapillary SIALOLITHIASIS
cyst closely resembles low-grade mucoepi- Figure 6-40
dermoid carcinoma.
Age: Middle-aged adults
TREATMENT Sex: Slightly more common in males
Complete excision is the treatment of choice. CLINICAL FEATURES
Most sialocysts are easily enucleated. The Salivary stones occasionally form within
mucopapillary cyst is more tortuous and the ducts of minor glands, being most fre-
requires wider excision. Recurrences are quently detected in the buccal mucosa and
extremely rare. upper lip. They are not always visible yet are
easily detected by palpation. Larger stones
Additional Reading may produce a nodular bulge; in all cases,
the lesion is hard and may give the impres-
Collins EM. Papillary cystadenoma of accessory salivary sion of a foreign body such as a beebee or
glands. Am J Surg. 1958;96:749. shot. They are usually asymptomatic.
FIGURE 6-40
Small hard palpable nod-
ules representing minor
gland sialoliths.
PMPH_Eversole_Chapter-06.indd 214 1/20/2011 2:31:00 PM
Intraoral Soft Tissue Swellings 215
MICROSCOPIC FEATURES incisor and cuspid lying above the mucobuc-
Minor gland sialoliths are situated within cal fold. It is soft and fluctuant or tense and
a dilated duct that shows mucous, respira- often extends superiorly into the anterior
tory, or squamous metaplasia. The stone nasal floor, producing a bulge below, and
is composed of concentric acellular lami- anterior to, the inferior turbinate. Bilateral
nations of basophilic amorphous material cases have been reported. On aspiration, a
in decalcified specimens. Adjacent acini mucous fluid is obtained, and injection of
exhibit degenerative changes with fibrous radiopaque dye clearly demonstrates its
and inflammatory changes. cystic nature radiographically. This cyst is
believed to derive from entrapped embry-
onic epithelium.
DIFFERENTIAL DIAGNOSIS
These lesions are clinically typical in that a MICROSCOPIC FEATURES
hard movable nodule can be palpated. They
The cyst is lined by pseudostratified colum-
may, however, be confused with a foreign
nar epithelium. Cilia are demonstrable in
body.
most cases. Mucous metaplasia is frequently
encountered. The fibrous wall usually lacks
TREATMENT inflammatory cell infiltration.
Surgical excision is the treatment of choice.
DIFFERENTIAL DIAGNOSIS
Additional Reading A clinically cystic lesion in the location of
the maxillary cuspid is almost invariably
Bahn SL, Tabachnick TF. Sialolithiasis of minor sali- a nasoalveolar cyst. Nevertheless, it must
vary glands. Oral Surg Oral Med Oral Pathol. 1971; be differentiated from a salivary or mes-
32:371. enchymal neoplasm and an abscess (paru-
Eversole LR, Sabes WR. Minor salivary gland duct lis) related to drainage from odontogenic
changes due to obstruction. Arch Otolaryngol Head
Neck Surg. 1971;94:19. infection.
Krolls SO, Smith WE. Sialolithiasis of the minor salivary
glands. Ear Nose Throat J. 1988;67:296. TREATMENT
Lee LT, Wong YK. Pathogenesis and diverse histolog-
ic findings of sialolithiasis in minor salivary glands. Simple excision by enucleation generally is
J Oral Maxillofac Surg. 2010;60:465-470. [Epub 2010 not followed by recurrence.
Jan 15.]
Pullon PA, Miller AS. Sialolithiasis of accessory salivary
glands: review of 55 cases. J Oral Maxillofac Surg.
1972;30:832.
NASOALVEOLAR (KLESTADT)
CYST
Figure 6-41
Age: Adults
Sex: Female predilection
CLINICAL FEATURES
The nasoalveolar cyst is restricted in loca- FIGURE 6-41
tion to the submucosal tissues between, and Swelling with elevation of the ala of the nose in a
superior to, the roots of the maxillary lateral nasolabial cyst. (Courtesy of Charles Tomich.)
PMPH_Eversole_Chapter-06.indd 215 1/20/2011 2:31:14 PM
216 Chapter 6
granulomatosa. Twenty percent of patients
Additional Reading exhibit facial paralysis and 40% have fis-
Brandao GS, Ebling H, Souza IC. Bilateral nasolabial sured tongue; other oral sites, primarily the
cyst. Oral Surg Oral Med Oral Pathol. 1974;37:480. buccal mucosa and palate, are affected by
Crawford WH, Greskovich FJ. Nasolabial cysts: report of multinodular lesions or erythematous or
two cases. J Oral Maxillofac Surg. 1968;26:582. bluish edematous plaques. Cheilitis granu-
Klestadt WO. Nasal cysts and the facial cleft theory. Ann
Otol Rhinol Laryngol. 1953;62:84. lomatosa is of unknown origin but has been
Roed-Peterson B. Nasolabial cysts: a presentation of suggested to represent a regional form of
five patients and review of the literature. Br J Oral sarcoidosis or an atypical granulomatous
Maxillofac Surg. 1969;7:83. disease, possibly allergic in origin.
Yerli H, Cabbarpur C, Aydin E. CT findings of a nasoal-
veolar cyst. Br J Radiol. 2009;82(976):e76-e78.
MICROSCOPIC FEATURES
The swelling is accounted for by the pres-
CHEILITIS GRANULOMATOSA ence of granulomatous inflammation with
Figure 6-42 infiltration and replacement of the minor
salivary glands. The granulomas are mul-
Age: Young adults
Sex: Females tinodular, composed of swirled collagen
fascicles with interspersed multinucleated
CLINICAL FEATURES giant cells.
Either upper, lower, or both lips show a dif-
fuse nodular enlargement that involves not DIFFERENTIAL DIAGNOSIS
just a portion but the entire lip from one
The appearance is similar to that of angion-
commissure to the other. The lip is firm
eurotic edema or edema and cellulitis of
to palpation but devoid of any superficial
odontogenic infectious origin. These two
inflammation or discoloration. Cheilitis
lesions are diffuse and soft to palpation,
granulomatosa accompanied by fissured
whereas cheilitis granulomatosa is firm and
tongue and facial paralysis constitutes the
multinodular.
Melkersson-Rosenthal syndrome, a form of
orofacial granulomatosis. The fissured tongue
may also show nodular or papillary tume- TREATMENT
factions. In actuality, a spectrum of changes Intralesional injection of triamcinolone or
may be encountered in patients with cheilitis another steroid on 6 to 10 weekly occasions
FIGURE 6-42
Diffuse, firm enlargement of the upper lip seen in cheilitis granulomatosa: a lesion associated with orofa-
cial granulomatosis and the Melkersson-Rosenthal syndrome.
PMPH_Eversole_Chapter-06.indd 216 1/20/2011 2:31:18 PM
Intraoral Soft Tissue Swellings 217
may result in significant diminution in the Overexposure to sun with superimposed
size of the lip. Intralesional steroids are not infection has been suggested to give rise to
always effective, and surgical excision of this uncommon condition. The vermilion
lip granulomas may be followed by recur- border and mucosa may be of normal color,
rence. Surprisingly, elimination of odonto- or diffuse keratosis with scaling may be fea-
genic and periodontal sources of infection tured. The lower lip is affected and a mul-
often coincide with a diminution in signs tinodular enlargement is seen. Multiple pits
and symptoms. or fistulae representing dilated minor sali-
vary ducts stipple the lip surface, and exu-
date may be expressed from these openings
Additional Reading in some but not all instances. Carcinoma of
Krutchkoff D, James R. Cheilitis granulomatosa.
the lip has been reported to complicate a
Successful treatment with combined triamcinolone number of cases.
injections and surgery. Arch Dermatol. 1978;114:1203.
Nally FM. Melkersson-Rosenthal syndrome. Report MICROSCOPIC FEATURES
of two cases. Oral Surg Oral Med Oral Pathol.
1970;29:694. The surface epithelium may be unremark-
Shaikh AB. Granulomatous cheilitis. A review and able; more often, hyperkeratosis and actinic
report of a case. Oral Surg Oral Med Oral Pathol.
1989;67:527.
changes are observed. The underlying sali-
Worsaae N, Christensen KC, Schipdt M, Reibel J. vary gland lobules show hypertrophy and
Melkersson-Rosenthal syndrome and cheilitis granu- sialadenitis, often of an acute nature.
lomatosa. A clinicopathologic study of thirty-three
patients with special reference to their oral lesions.
Oral Surg Oral Med Oral Pathol. 1982;54:404. DIFFERENTIAL DIAGNOSIS
Zeng W, Geng S, Niu X, Yuan J. Complete Melkersson- Cheilitis glandularis may simulate the clini-
Rosenthal syndrome with multiple cranial nerve pal-
sies. Clin Exp Dermatol. 2010;35:272-274. cal features seen in cheilitis granulomatosa;
however, the multiple dilated duct orifices
along with multinodular enlargement are
CHEILITIS GLANDULARIS classic clinical findings. Actinic prurigo
Figure 6-43 is also a major consideration, yet tends to
occur in Amerindians. Biopsy should be
Age: Middle-aged and elderly adults performed, particularly in patients with
Sex: Male predilection foci of keratotic thickening or ulceration.
CLINICAL FEATURES
TREATMENT
Cheilitis glandularis is a disease of unknown
etiology that represents both a superficial Excision of the involved area can generally
and deep (salivary) inflammatory disorder. be accomplished without extending the
FIGURE 6-43
Cheilitis glandularis char-
acterized by enlargement
of the lower lip accompa-
nied by accentuation of the
salivary excretory duct
pores. (Courtesy of Dr. H.
Cherrick.)
PMPH_Eversole_Chapter-06.indd 217 1/20/2011 2:31:28 PM
218 Chapter 6
surgical margin onto the vermilion, thereby Often the periorbital skin is involved and
avoiding cosmetic deformity. the swelling may be such that the eyes can-
not open. A hereditary form exists and is
usually accompanied by generalized skin
Additional Reading urticaria. The inherited variety shows a bio-
Doku HC, Shklar G, McCarthy PL. Cheilitis glandularis.
chemical defect in the complement fixation
Oral Surg Oral Med Oral Pathol. 1965;20:563. pathway with a deficiency of C’l esterase
Nico MM, Nakano de Melo J, Lourenço SV. Cheilitis inhibitor.
glandularis: a clinicopathological study in 22 patients.
J Am Acad Dermatol. 2010;62:233-238. [Epub 2009
Dec 11.] MICROSCOPIC FEATURES
Oliver ID, Pickett AB. Cheilitis glandularis. Oral Surg Not applicable.
Oral Med Oral Pathol. 1980;49:526.
Stuller CB, Schaberg SJ, Stokos J, Pierce GL. Cheilitis
glandularis. Oral Surg Oral Med Oral Pathol. DIFFERENTIAL DIAGNOSIS
1982;53:602.
Weir TW, Johnson WC. Cheilitis glandularis. Arch The rapid onset of swelling often preceded
Dermatol. 1971;103:433. by pruritus is unique. The only other dis-
ease that may mimic angioneurotic edema
is diffuse cellulitis with edema resulting
ANGIONEUROTIC EDEMA from odontogenic infection in an anterior
Figure 6-44 maxillary tooth. The hereditary form fol-
lows an autosomal dominant pattern with
Age: No predilection both skin and visceral manifestations.
Sex: No predilection
CLINICAL FEATURES TREATMENT
Angioneurotic edema represents a hista- Any suspected allergens should be with-
mine-mediated immediate hypersensitiv- drawn. Systemically administered anti-
ity reaction to some allergenic substance, histamines cause resolution within hours.
usually a food or drug. An intraoral vesic- Repeated exposure to the allergen can result
uloerythematous reaction may accompany in Quincke’s edema and progress to ana-
the edematous episode, which consists phylactic shock. Patients with hereditary
of diffuse, often massive swelling of the angioneurotic edema should be referred
upper lip and face. The swelling, resulting to an allergist. Three daily 200-mg doses
from accumulation of edema fluid, is soft. of danazol on a maintenance schedule
FIGURE 6-44
Angioneurotic edema, an
allergic reaction, results
in soft edematous enlarge-
ment of the upper lip and
face.
PMPH_Eversole_Chapter-06.indd 218 1/20/2011 2:31:36 PM
Intraoral Soft Tissue Swellings 219
are effective in the hereditary form of the MICROSCOPIC FEATURES
disease. The lip is edematous with a diffuse mono-
nuclear infiltrate in the submucosa and may
Additional Reading show perivascular CD4 lymphoid aggre-
gates. It may be that UV-irradiated kerati-
Albright BW; Taylor CG. Hereditary angioneurot- nocytes develop neoantigens causing an
ic edema: report of case. J Oral Maxillofac Surg. autoimmune reaction.
1979;37:888.
Correll RW, DeBoom GW, Jensen JL. Rapidly develop-
ing, edematous swelling of the upper lip. J Am Dent DIFFERENTIAL DIAGNOSIS
Assoc. 1986;113:69.
Reinberg SM, Feinberg AR. Allergy to penicillin. JAMA.
Cheilitis glandularis, cheilitis granuloma-
1956;160:778. tosa and actinic cheilitis are the chief enti-
Stevenson HA, Steele JC, Field EA, Darroch CJ. ties to consider. Biopsy will exclude these
Angioedema of the lips and tongue induced by angio- processes.
tensin-converting enzyme inhibitor. A report of two
cases. Prim Dent Care. 2004;11:17-19.
Sturdy KA., Grisius RJ, Oatis GW. Hereditary angioede- TREATMENT
ma controlled with danazol. Oral Surg Oral Med Oral
Pathol. 1979;48:418. Topical steroid ointments and gels are effec-
tive, and sun screen should be used once
the inflammation and swelling resolve.
ACTINIC PRURIGO
Figure 6-45
Age: Teens, adults
Additional Reading
Sex: No predilection Gómez A, Umana A, Trespalacios AA. Immune respons-
es to isolated human skin antigens in actinic prurigo.
CLINICAL FEATURES Med Sci Monit. 2006;12(3):BR106-BR113. [Epub
2006 Feb 23.]
Actinic prurigo, also termed familial poly- Hojyo-Tomoka MT, Vega-Memije ME, Cortes-Franco
morphous light eruption of American Indians, R, Domínguez-Soto L. Diagnosis and treatment of
is more often seen in Central America and actinic prurigo. Dermatol Ther. 2003;16(1):40-44.
Asia than in North America and Europe, Mounsdon T, Kratochvil F, Auclair P, Neale J, Lee L.
Actinic prurigo of the lower lip. Review of the litera-
typically among individuals living at high ture and report of five cases. Oral Surg Oral Med Oral
altitude. Sun exposure is probably a major Pathol. 1988;65:327-332.
etiologic factor. The lower lip becomes Vega-Memije ME, Mosqueda-Taylor A, Irigoyen-
enlarged and tender without keratotic Camacho ME, Hojyo-Tomoka MT, Domínguez-Soto
L. Actinic prurigo cheilitis: clinicopathologic analysis
changes and cutaneous plaques, and nod- and therapeutic results in 116 cases. Oral Surg Oral
ules appear commonly on the face, arms, Med Oral Pathol Oral Radiol Endod. 2002;94(1):
and legs. 83-91.
FIGURE 6-45
Diffuse lip swelling in
actinic prurigo. Source:
Moundsdon T, Kratochvil
F, Auclair P, Neal J, Lee L.
Actinic prurigo of the lower
lip. Oral Surg Oral Med Oral
Pathol. 1988;65:327-332.
PMPH_Eversole_Chapter-06.indd 219 1/20/2011 2:32:03 PM
220 Chapter 6
INFLAMMATORY FIBROUS vestibule are features favoring inflamma-
HYPERPLASIA tory fibrous hyperplasia.
Figure 6-46
TREATMENT
Age: Adults, elderly Surgical excision is the treatment of choice
Sex: No predilection followed by fabrication of a new denture.
CLINICAL FEATURES
Ill-fitting dentures evolve over time as the
alveolar ridges slowly atrophy. The conse-
Additional Reading
quences of this atrophy are overextension of Bhattacharyya I. Case of the month. Epulis fissuratum.
the denture flanges into the vestibule, serv- Todays FDA. 2008;20:15, 17, 19.
ing as a chronic irritant. The host responds Canger EM, Celenk P, Kayipmaz S. Denture-related
hyperplasia: a clinical study of a Turkish population
by attempting to lay down a fibrous con- group. Braz Dent J. 2009;20(3):243-248.
nective tissue “pillow” that clinically is a Keng SB, Loh HS. The treatment of epulis fissuratum of
bosselated multinodular hyperplastic soft the oral cavity by CO 2 laser surgery. J Clin Laser Med
growth in the vestibular area. These reac- Surg. 1992;10:303-306.
Thomas GA. Denture-induced fibrous inflammatory
tive proliferations are soft and can become hyperplasia (epulis fissuratum): research aspects. Aust
ulcerated. They are often referred to as epu- Prosthodont J. 1993;7:49-53.
lis fissuratum.
MICROSCOPIC FEATURES FOREIGN BODY GRANULOMA
The surface epithelium is typically hyper- Figure 6-47
plastic with elongated thick rete ridges. The
surface is often lobulated, and underlying Age: No predilection
the epithelial is normal-appearing collag- Sex: No predilection
enous connective tissue. Minor salivary CLINICAL FEATURES
gland lobules are commonly seen along the A variety of foreign bodies may be intro-
base, exhibiting chronic sialadenitis. duced into the oral submucosal tissues.
Most foreign bodies are iatrogenic, whereby
DIFFERENTIAL DIAGNOSIS
a substance becomes implanted during an
Any of the swellings listed here are in the extraction or oral surgical procedure. Not
differential; however, the association with all foreign agents and chemicals elicit a
an ill-fitting denture and localization to the granulomatous response. Common reac-
FIGURE 6-46
Inflammatory fibrous
hyperplasia appears as
redundant soft tissue folds
associated with ill-fitting
dentures.
PMPH_Eversole_Chapter-06.indd 220 1/20/2011 2:32:15 PM
Intraoral Soft Tissue Swellings 221
foreign body reaction, biopsy is required to
obtain a definitive diagnosis.
TREATMENT
Local excisional biopsy is the treatment of
choice.
Additional Reading
Cataldo E, Santis H. Response of the oral tissue to exog-
FIGURE 6-47 enous foreign materials. J Periodontol. 1974;45:93.
Fine L, Mostofi R, Wiemann MR, Crinzi RA. Foreign
Lip augmentation hyaluronate foreign body granu-
body-type reaction following crown cementation.
loma that, after injection, migrated into sulcus J Periodontol. 1977;48:294.
forming a pale mass. McMillan MD, Kardos TB, Edwards JL, Thourburn DN,
Adams DB, Palmer DK. Giant cell hyalin angiopathy
or pulse granuloma. Oral Surg. 1981;52:178.
tions of this nature occur with handpiece Sage RJ, Chaffins ML, Kouba DJ. Granulomatous foreign
oil (oil granuloma), vegetable matter (pulse body reaction to hyaluronic acid: report of a case after
melolabial fold augmentation and review of manage-
granuloma), and dental cements. The true ment. Dermatol Surg. 2009;35(suppl 2):1696-1700.
nature of the foreign agent often cannot be Stewart CM, Watson RE. Experimental foreign
ascertained. The mucobuccal fold is prob- body reactions. Oral Surg Oral Med Oral Pathol.
ably the most common location; the lesions 1990;69:713.
are soft or firm and either dome shaped or
multinodular.
CROHN’S DISEASE
MICROSCOPIC FEATURES Figure 6-48
The submucosa is fibrotic with chronically Age: Teenagers and adults
inflamed granulation tissue evincing a mild Sex: No predilection
inflammatory cell infiltrate. Multinucleated CLINICAL FEATURES
giant cells are observed and usually phago-
cytosis of the foreign material can be seen. Crohn’s disease, also termed regional
Oil granulomas appear as large vacant vac- enteritis, is a segmental transluminal
uoles. Pulse granulomas exhibit compart- inflammatory bowel disease that most fre-
mentalized spaces with enveloping giant quently affects the distal ileum and colon.
cells. When a foreign material is not readily Patients generally complain of subumbili-
identifiable, polarized lenses may be used cal or lower right quadrant abdominal pain
to detect refractile materials. with diarrhea. Other complications include
chronic fever, general malaise, malabsorp-
tion, joint pain, and growth failure. Char-
DIFFERENTIAL DIAGNOSIS
acteristic segmental changes are observed
Foreign body granulomas are dome-shaped in radiographic gastrointestinal series.
nodules that cannot usually be differenti- Extracolonic manifestations are common
ated clinically from benign mesenchymal and include arthritis, skin, ocular and oral
neoplasms, salivary neoplasms, or other lesions, and hepatic involvement. Whereas
granulomatous lesions. Whereas a history oral ulcerations may occur, particularly
of trauma to, or previous surgery in, the in youngsters, adults more often manifest
area would certainly arouse suspicion of a tumefactive lesions of the buccal mucosa
PMPH_Eversole_Chapter-06.indd 221 1/20/2011 2:32:28 PM
222 Chapter 6
fissuratum, although many other inflam-
matory or even submucosal neoplastic
processes may show similar features. In a
patient with bowel symptoms, malaise, and
arthritis, the clinician should certainly sus-
pect Crohn’s disease. Biopsy is not diagnos-
tic; however, the presence of noncaseating
granulomas without an infectious etiology
should arouse suspicion of regional enteri-
tis, and a medical work-up for bowel dis-
ease is then indicated.
TREATMENT
The patient with suspected Crohn’s disease
should be referred to a gastroenterologist.
Most patients respond to systemic pred-
nisone, sulfasalazine, and metronidazole
therapy.
Additional Reading
Coenen C, Borsch G, Muller K, Fabry H. Oral inflam-
matory changes as an initial manifestation of Crohn’s
disease antedating abdominal diagnosis. Dis Colon
FIGURE 6-48 Rectum. 1988;31:548.
Multinodular mass of the submucosa representing Eisenbud L, Katska I, Platt N. Oral manifestations in
noncaseating granulomas of Crohn’s disease. Crohn’s disease. Oral Surg Oral Med Oral Pathol.
1972;34:770.
Estrin HM, Hughes RW. Oral manifestations in Crohn’s
and vestibule. The lesions may be multi- disease: Report of a case. Am J Gastroenterol.
1985;80:352.
nodular or fissured or possess a cobblestone Kim SK, Lee ES. Orofacial granulomatosis associated
surface pattern. Certain periodontopathic with Crohn’s disease. Ann Dermatol. 2010;22:203-205.
bacteria (Wolinella) have been implicated as [Epub 2010 May 18.]
potential pathogens. Van Dyke TE, Dowell VR, Offenbacher S, Snyder W,
Hersh T. Potential role of microorganisms isolated
from periodontal lesions in the pathogenesis of inflam-
MICROSCOPIC FEATURES matory bowel disease. Infect Immun. 1986;53:671.
The nodular lesions show a chronic inflam-
matory cell infiltrate with formation of
noncaseating granulomas characterized by TRAUMATIC FIBROMA
oval aggregates of epithelioid histiocytes Figure 6-49
surrounded by a halo of mature lympho-
cytes and histiocytes. No caseation necrosis Age: No predilection
is evident in the center of the granulomas. Sex: No predilection
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
The traumatic fibroma may arise in any
The nodular lesions are most often confused oral location. It represents the most com-
with simple fibrous hyperplasia or epulis mon swelling of the buccal mucosa and is
PMPH_Eversole_Chapter-06.indd 222 1/20/2011 2:32:29 PM
Intraoral Soft Tissue Swellings 223
FIGURE 6-49
Traumatic fibromas are very com-
mon in the buccal mucosa and
lips.
also extremely common on the mucosal plasms, benign salivary tumor, a deeply
surface of the lips. Traumatic fibroma rep- situated mucocele, or an epidermoid cyst.
resents reactive fibrous hyperplasia owing
to trauma and is not a true neoplasm. It is TREATMENT
a sessile, dome-shaped soft nodule, usually Excisional biopsy is recommended to rule
of normal color, and may be ulcerated from out the presence of a true neoplasm.
trauma as in cheek biting.
MICROSCOPIC FEATURES Additional Reading
The epithelium is distended by a mass of Barker DS, Lucas FB. Localized fibrous overgrowths of
dense collagenous tissue with interspersed the oral mucosa. Br J Oral Maxillofac Surg. 1967;5:86.
fibroblasts. Capillaries traverse the tissue, Bouquot JE, Gundlach KK. Oral exophytic lesions in
23,616 white Americans over 35 years of age. Oral
and few if any inflammatory cells are evi- Surg Oral Med Oral Pathol. 1986;62:284.
dent. When stellate multinucleated cells Fadavi S, Punwani I. Oral fibromas in children: reports
are seen, the lesion represents a giant cell of two cases. ASDC J Dent Child. 1987;54:126.
fibroma. Fernandez-Flores A. Solitary oral fibromas of the tongue
show similar morphologic features to fibrous papule
of the face: a study of 31 cases. Am J Dermatopathol.
DIFFERENTIAL DIAGNOSIS 2010;32:442-427.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
Traumatic fibroma may be clinically indis- Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
tinguishable from true mesenchymal neo- 1983:137.
PMPH_Eversole_Chapter-06.indd 223 1/20/2011 2:32:35 PM
224 Chapter 6
TRAUMATIC (AMPUTATION) A variant form is palisaded encapsulated neu-
NEUROMA roma characterized by palisaded spindle-
Figure 6-50 shaped cells invested by a descrete capsule.
S-100 protein is positive.
Age: No predilection
Sex: No predilection DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES The swelling observed with amputation
neuroma is identical to that seen in mes-
An amputation neuroma evolves subsequent
enchymal neoplasms, salivary tumors, or
to severance of a nerve, whereby the distal
foreign body granulomas. A parulis may
segment undergoes Wallerian degenera-
be considered in the differential diagno-
tion and the proximal segment attempts in
sis when the lesion lies directly below the
vain to reunite with the distal nerve sheath.
attached gingiva. Firmness with pain on
When the severed segments are displaced,
palpation should arouse clinical suspicion
the proximal portion proliferates, pursuing
of neuroma. When multiple neuromas are
a tortuous course, resulting in tumefaction.
identified, the neuropolyendocrine syn-
The swelling is most frequently encoun-
drome should be ruled out.
tered in the mucobuccal fold adjacent to
the mental foramen. The nodule is firm yet
TREATMENT
usually movable. Pain is often elicited when
pressure is applied: however, some patients Simple surgical excision is rarely followed
suffer from spontaneous facial pain. Most by recurrence.
amputation neuromas measure less than
0.5 cm in diameter.
Additional Reading
MICROSCOPIC FEATURES
Koutlas IG, Scheithauer BW. Palisaded encapsulated
A tortuous array of axis cylinders accompa- (“solitary circumscribed”) neuroma of the oral cavity:
nied by neurilemma sheath and enveloping a review of 55 cases. Head Neck Pathol. 2010;4:15-26.
[Epub 2010 Jan 23.]
perineurium is encountered, resembling Rasmussen OC. Painful traumatic neuromas in the
an overabundance of normal nerve tissue. oral cavity. Oral Surg Oral Med Oral Pathol. 1980;
49:191.
Robinson M, Slvakin HC. Dental amputation neuromas.
J Am Dent Assoc. 1965;70:662.
Sist TC, Jr, Greene GW. Traumatic neuroma of the
oral cavity. Report of thirty-one new cases and review
of the literature. Oral Surg Oral Med Oral Pathol.
1981;51:394.
Swanson HH. Traumatic neuromas; a review of the liter-
ature. Oral Surg Oral Med Oral Pathol. 1961;14:317.
MESENCHYMAL NEOPLASMS
Figure 6-51
Age: Young adults
Sex: No predilection
CLINICAL FEATURES
FIGURE 6-50
Traumatic neuroma, a small nodule that arose on Various neoplasms of mesenchymal origin
the lip after trauma. may arise in the buccal mucosa and lips.
PMPH_Eversole_Chapter-06.indd 224 1/20/2011 2:33:03 PM
Intraoral Soft Tissue Swellings 225
FIGURE 6-51
Benign mesenchymal neoplasms such as lipoma, neurofibroma, and neurilemmoma are common tumefac-
tions of the cheek.
Because of its prevalence, hemangioma is TREATMENT
considered separately. The most common Enucleation and excision are the treatments
mesenchymal tumors in this location are of choice for benign mesenchymal tumors.
neurofibroma, neurilemmoma, and lipoma. Sarcomas require radical wide excision.
Less frequently encountered benign neo-
plasms or neoplastic-like swellings of con-
nective tissue origin include leiomyoma, Additional Reading
fibrous histiocytoma, and oral focal muci-
Baderca F, Cojocaru S, Lazăr E, et al. Schwannoma of
nosis. As a group, they vary considerably
the lip: case report and review of the literature. Rom J
in size, may be soft or firm, movable, and Morphol Embryol. 2008;49:391-398.
well demarcated or encapsulated. Ulcer- Cherrick HM, Eversole LR. Benign neural sheath neo-
ation of the surface mucosa is unusual. In plasm of the oral cavity. Report on thirty-seven cases.
the cheek, a diffuse swelling composed Oral Surg Oral Med Oral Pathol. 1971;32:900.
DiLascio JP, Devlin GP, Doyle JL. Aggressive fibrous
of adipose tissue usually represents her- histiocytoma of perioral soft tissues: Report of case.
niation of the buccal fat pad rather than a J Oral Maxillofac Surg. 1981;39:134.
true lipoma. Sarcomas and lymphomas are Tomich CE. Oral focal mucinosis: a clinicopathologic
rarely encountered; ulceration and indura- and histochemical study of eight cases. Oral Surg Oral
Med Oral Pathol. 1974;38:714.
tion usually are present when the mass rep- Vindenes H. Lipomas of the oral cavity. Int J Oral
resents a mesenchymal malignancy. Maxillofac Surg. 1978;7:162.
MICROSCOPIC FEATURES
The microscopic patterns vary with the HERNIATED BUCCAL FAT PAD
tissue of origin. Neural sheath tumors are Figure 6-52
described under tongue swellings.
Age: Middle-aged and elderly adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
CLINICAL FEATURES
Swellings of the cheek and lips in mesen-
chymal tumors are identical to those of The buccal fat pad lies external to the buc-
salivary neoplasm, traumatic fibroma, or cinator muscle. Trauma to this thin muscle
deep mucocele. Indurated and ulcerated from cheek biting or surgery may weaken
sarcomatous tumors may clinically resem- or separate the muscle fibers, allowing adi-
ble squamous cell carcinoma or malignant pose tissue to herniate orally. Herniated fat
salivary neoplasms. pads are soft to palpation and may appear
PMPH_Eversole_Chapter-06.indd 225 1/20/2011 2:33:08 PM
226 Chapter 6
FIGURE 6-52
Soft masses, sometimes
yellow, in posterior aspect
of buccal mucosa are com-
posed of adipose tissue
that has herniated through
the buccinator muscle fol-
lowing trauma or a cheek-
biting episode.
faintly yellow. They either are dome-shaped Clawson RJ, Kline KK, Armbrecht EC. Trauma-induced
tumefactions or exhibit surface lobulation. avulsion of the buccal fat pad into the mouth. J Oral
Maxillofac Surg. 1968;26:546.
Haria S, Kidner G, Shepherd JP. Traumatic herniation
MICROSCOPIC FEATURES of the buccal fat pad into the oral cavity. Int J Paediatr
Dent. 1991;1:159-162.
The lesion is composed of normal-appear-
Messenger KL, Cloyd W. Traumatic herniation of the
ing adipose tissue traversed by capillary buccal fat pad: report of case. Oral Surg Oral Med
septae. They cannot usually be differenti- Oral Pathol. 1977;43:41.
ated histologically from lipoma; however,
scattered isolated muscle fibers are occa-
sionally admixed with the adipose tissue, a REACTIVE LYMPHOID
feature not encountered in lipoma. HYPERPLASIA
Figure 6-53
DIFFERENTIAL DIAGNOSIS
The buccal mucosal mass representing a Age: No predilection
Sex: No predilection
herniated fat pad may clinically resemble
the other mesenchymal and reactive lesions CLINICAL FEATURES
included in this section. The consistency Facial nodes located adjacent to the facial
and gross appearance do not allow for vein and buccinator muscle are present in
differentiation from lipoma. A history of about 20% of the population. The nodes are
trauma aids in arriving at a diagnosis in usually not palpable unless stimulated to
conjunction with biopsy. undergo reactive hyperplasia. Lymphoid
hyperplasia of the buccal nodes may not
TREATMENT be visible; yet the enlarged node is firm,
The excess fatty tissue should be excised; palpable, and movable, being located near
if the zone of buccinator perforation can be Stensen’s duct. The etiology is not always
located, the fibers should be juxtaposed and apparent yet may accompany generalized
sutured. lymphadenopathy in viral infections or rep-
resent local adenopathy secondary to oral
or facial skin infections. Occasionally, an
Additional Reading enlarged buccal node represents a specific
Brooke RI. Traumatic herniation of buccal pad of fat
infection, such as latent acquired toxoplas-
(traumatic pseudolipoma). Oral Surg Oral Med Oral mosis. Handling of contaminated cat litter is
Pathol. 1978;45:689. usually the route of transmission; in gravid
PMPH_Eversole_Chapter-06.indd 226 1/20/2011 2:33:30 PM
Intraoral Soft Tissue Swellings 227
FIGURE 6-53
Buccal lymph nodes will
undergo enlargement
when an antigenic chal-
lenge occurs.
females, this could significantly endanger
the developing fetus. Malignant lymphoma Additional Reading
is extremely rare in this location. Appel BN, Mendelow H, Pasqual HN. Acquired
Toxoplasma lymphadenitis. Oral Surg Oral Med Oral
MICROSCOPIC FEATURES Pathol. 1979;47:529.
Dorfman RF, Warnke R. Lymphadenopathy simulating
The node is enlarged and encapsulated. malignant lymphomas. Hum Pathol. 1974;5:519.
Hyperplastic germinal centers are impacted Doyle JL. Benign lymphoid lesions of the oral mucosa.
with active large immunoblasts. The para- Oral Surg Oral Med Oral Pathol. 1970;29:31.
cortical region may continue to possess a Graham RM, Thomson EF, Cousin GC, Kumar SN,
Awasthi A. A case of facial lymphoma mimicking den-
mature lymphocytic mantle; however, large tal infection. Dent Update. 2009;36:244-246.
blast cells may occupy this region. The med- Weidman B, Warman E. Lymph nodes of the head and
ullary zone is often congested; in addition neck. J Oral Pathol Med. 1980;35:39.
to mature lymphocytes, histiocytes show-
ing phagocytosis and plasma cells may be
present. Toxoplasma lymphadenitis is char- HEMANGIOMA AND VARIX
acterized by extrafollicular pale epithelioid Figure 6-54
histiocytes.
Age: Hemangiomas—children; Varix—adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Reactive lymphoid hyperplasia is indis- CLINICAL FEATURES
tinguishable clinically from mesenchy- Vascular lesions are commonly located on
mal neoplasms, benign salivary tumors, the lips and buccal mucosa. In children,
and focal granulomas. For this reason, a they represent hamartomatous proliferation
biopsy is required to arrive at a definitive of vascular channels (hemangiomas). Intra-
diagnosis. muscular hemangiomas may attain consid-
erable dimensions; being situated in deeper
TREATMENT
tissues, they do not necessarily impart a red
Provided no infectious source can be or bluish appearance to the distended over-
uncovered, further treatment, even for lying mucosa. In older patients, the clinical
toxoplasma lymphadenitis, is not required. features are nearly identical but vascular
Generalized or systemic disease should be growths generally represent aneurysma-
treated according to the nature of the pro- like dilations of venules known as varices.
cess. Rarely, lymphoma may arise in a buc- A localized varix may appear subsequent
cal node. to trauma. Both hemangiomas and varices
PMPH_Eversole_Chapter-06.indd 227 1/20/2011 2:33:57 PM
228 Chapter 6
FIGURE 6-54
Hemangioma and varix of the lip
and buccal mucosa. These benign
vascular red and blue lesions blanch
under pressure.
appear as smooth or slightly nodular, red to hemangiomas. Thrombi are frequently seen
purple soft swellings that blanch on pres- within the dilated vascular lumina.
sure. Hemangiomas of the oral mucosa Hemangioendotheliomas are cellular
may accompany facial skin angiomatoses with only slit-like vascular channels and
or port-wine stain and can be a component sheets of plump endothelial cells. Likewise,
of the Sturge-Weber syndrome. Angiomas hemangiopericytomas are hypercellular,
or varices of long duration may contain yet reticulum stains disclose that the neo-
radiographically demonstrable phleboliths. plastic cells proliferate beyond the confines
Aggressive, or even malignant, hemangio- of periendothelial reticulum. In addition,
endotheliomas or hemangiopericytomas the vascular spaces are irregular, evincing a
are rare, have a rapid growth rate, and are “stag-horn” pattern.
usually indurated. The caliber persistant
labial artery is another vascular lesion found DIFFERENTIAL DIAGNOSIS
on the lip and simply represents a superfi- Other swellings of the lips and cheek are
cially placed arteriole in the submucosa. not pigmented; however, deeply situated
vascular lesions may not show a red color
MICROSCOPIC FEATURES and therefore must be differentiated from
Hemangiomas may be capillary in type, mucocele, other mesenchymal neoplasms,
with numerous small-caliber vascular salivary neoplasms, and inflammatory
channels, or they may be cavernous with hyperplasia.
large dilated vessels. A varix may represent
TREATMENT
a single dilated tortuous venule, which,
on microscopic section, shows numer- Local excision is the treatment of choice
ous dilated channels similar to cavernous for small lesions; excessive hemorrhage is
PMPH_Eversole_Chapter-06.indd 228 1/20/2011 2:34:10 PM
Intraoral Soft Tissue Swellings 229
generally not encountered. Large diffuse Weathers DR, Fine RM. Thrombosed varix of the oral
hemangiomas may be excised or sclerosed. cavity. Arch Dermatol. 1971;104:427.
If they do not interfere with function or are
not a cosmetic problem, they may be left
untreated. Hemangiomas in children may SQUAMOUS CELL
show spontaneous regression before or dur- CARCINOMA
ing pubescence. Wide excision with liberal Figure 6-55
margins is in order for hemangioendothe-
lioma and hemangiopericytoma. When Age: Elderly adults
these tumors are encountered, a thorough Sex: Male predilection
medical work-up is necessary, as they occa- CLINICAL FEATURES
sionally metastasize.
Early squamous cell carcinoma may appear
as a focal ulcer on the lower lip and often
Additional Reading shows actinic cheilosis. As tumefaction
ensues, the surface may remain ulcerated
Kinni ME, Webb RI, Christensen RW. Intramuscular or be encrusted with keratin. Usually, but
hemangioma of the orbicularis oris muscle: report of not invariably, the mass is indurated and
case. J Oral Maxillofac Surg. 1981;39:780.
Kocyigit P, Kocyigit D, Akay BN, Ustuner E, Kisnisci R. fixed to the adjacent soft tissues. Meta-
Calibre persistent labial artery: clinical features and static deposits may be detected in the sub-
noninvasive radiological diagnosis. Clin Exp Dermatol. mental, submandibular, or cervical nodes.
2006;31:528-530. Squamous cell carcinoma in the buccal
Shklar G, Meyer I. Vascular tumors of the mouth and
jaws. Oral Surg Oral Med Oral Pathol. 1965;19:335.
mucosa is similarly ulcerated and indu-
Walike JW, Bailey BJ. Head and neck hemangiopericyto- rated. Not uncommonly, it may show a
ma. Arch Otolaryngol Head Neck Surg. 1971;93:345. white keratinized surface.
FIGURE 6-55
Squamous cell carcinoma
of the lower lip has a good
prognosis after complete
excision.
PMPH_Eversole_Chapter-06.indd 229 1/20/2011 2:34:43 PM
230 Chapter 6
MICROSCOPIC FEATURES
The neoplastic epithelium is well differenti-
Additional Reading
ated when it involves the lip, showing mini- Cross JE, Guralnick E, Daland EM. Carcinoma of the
mal hyperchromatism or pleomorphism. lip. Surg Gynecol Obstet. 1948;87:153.
Ellis GL, Corio RL. Spindle cell carcinoma of the oral
Tumor islands display central parakeratin
cavity: a clinicopathologic assessment of fifty-nine cas-
or keratin pearls. Two specific forms of es. Oral Surg Oral Med Oral Pathol. 1980;50:523.
squamous cancer occur on the lip and show Hasson O. Squamous cell carcinoma of the lower lip.
unique histomorphologic features. Adenoid J Oral Maxillofac Surg. 2008;66:1259-1262.
squamous cell carcinoma is characterized Nuutinen J, Karja J. Local and distant metastases in
patients with surgically treated squamous cell carci-
by acantholysis of cells, producing clefting noma of the lip. Clin Otolaryngol. 1981;6:415.
within tumor islands. This change imparts Tomich CE, Hutton CE. Adenoid squamous cell car-
an adenoid appearance. Spindle cell carci- cinoma of the lip: report of cases. J Oral Maxillofac
noma is another variant of squamous cell Surg. 1972;30:592.
carcinoma. Microscopically, the cells appear
sarcomatoid with streams of invasive spin-
dle cells that are usually in continuity with,
MONOMORPHIC ADENOMA
and emanate from, the basal layer. Buccal Figure 6-56
mucosa carcinomas may not necessarily be
Age: Middle-aged and elderly adults
well differentiated. Sex: Female predilection
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
A variety of histologically distinct salivary
Small squamous cell carcinomas may be neoplasms including canalicular adenoma,
well localized and clinically appear identi- basal cell adenoma, and membranous ade-
cal to keratoacanthoma. Larger lesions are noma are collectively grouped as monomor-
usually fungating and may resemble gran- phic adenomas. These tumors arise most
ulomatous lesions. Specific granulomatous frequently in the minor glands of the upper
infections of the lips and buccal mucosa lip, where they appear as movable nodules
are rare. Crusted or ulcerated lesions of the with either a fluctuant or soft consistency.
upper lip are more likely to represent basal Although usually solitary, this type of ade-
cell carcinomas. Because they usually origi- noma can be multifocal. This finding would
nate on the skin rather than on the vermil- support a hamartomatous pathogenetic
ion border, basal cell carcinomas are dealt nature.
with in the section on soft tissue swellings
of the neck and face. Ulcerated and indu- MICROSCOPIC FEATURES
rated carcinoma of the buccal mucosa must
be distinguished from malignant salivary Three primary variations are encountered.
or mesenchymal neoplasms. The canalicular adenoma is characterized
by anastomosing cords of basaloid cuboidal
cells with an intervening delicate mucoid
TREATMENT
vascular stroma. Multicentric foci are fre-
Biopsy must be performed to ensure a quently observed, and an intralobular ori-
diagnosis of squamous cell carcinoma. Lip gin can be documented in some cases. The
cancer is preferably treated with surgical basal cell adenoma is represented by cords
excision and lip shave. Buccal mucosal car- and islands of basaloid cells showing duct
cinoma should be managed by a cancer spe- formation. The stroma is fibrovascular
cialist and may require both irradiation and without chondroid, adipose, or myxoid dif-
surgery. ferentiation. The membranous adenoma is
PMPH_Eversole_Chapter-06.indd 230 1/20/2011 2:35:24 PM
Intraoral Soft Tissue Swellings 231
FIGURE 6-56
A basal cell adenoma (left)
and a canalicular (mono-
morphic) adenoma aris-
ing from minor salivary
glands.
histologically similar to the basal cell type; OTHER SALIVARY NEOPLASMS
however, the stroma is hyalinized. Interest- Figure 6-57
ingly, all three patterns may be identified
within a single specimen. Age: Middle-aged adults
Sex: Female predilection
DIFFERENTIAL DIAGNOSIS CLINICAL FEATURES
Clinically, monomorphic adenoma is indis- Salivary tumors are frequently seen in the
tinguishable from other salivary neoplasms cheek and upper lip; the lower lip is rarely
or encapsulated mesenchymal tumors. A the site of origin. The pleomorphic ade-
movable mass in the upper lip, however, noma, which is most common, is a well-
usually represents monomorphic adenoma. demarcated, encapsulated, soft-to-firm
movable mass. Malignant salivary tumors
TREATMENT
infrequently arise in labial glands, but are
Excision of the tumor with an attempt to often located in the buccal mucosa. They
remove some of the adjacent marginal tis- are firm or indurated and may or may not
sue is recommended. show ulceration. Specific tumors include
polymorphous low-grade adenocarcinoma,
adenoid cystic carcinoma, and mucoepider-
Additional Reading moid carcinoma. Acinic cell carcinoma is
seen most often in the parotid; when it arises
Christ TF, Crocker D. Basal cell adenoma of minor sali-
vary gland origin. Cancer. 1972;30:214. from oral minor glands, the buccal mucosa
Fantasia JE, Neville BW. Basal cell adenomas of the and lip are the more prevalent sites.
minor salivary glands: a clinicopathologic study of sev-
enteen new cases and a review of the literature. Oral MICROSCOPIC FEATURES
Surg Oral Med Oral Pathol. 1980;50:433.
Minicucci EM, de Campos EB, Weber SA, Domingues The histologic findings vary depending on
MA, Ribeiro DA. Basal cell adenoma of the upper the specific type of tumor. These features
lip from minor salivary gland origin. Eur J Dent. are separately enumerated in the section on
2008;2:213-216.
Mintz,GA, Abrams AM, Melrose RJ. Monomorphic ade- palatal swellings.
nomas of the major and minor salivary glands. Report
of twenty-one cases and review of the literature. Oral DIFFERENTIAL DIAGNOSIS
Surg Oral Med Oral Pathol. 1982;53:375.
Nelson JF, Jacoway JR. Monomorphic adenoma (canali- Salivary neoplasms appearing as upper
cular type): report at 29 cases. Cancer. 1973;31:1511. lip or buccal mucosal swellings resem-
PMPH_Eversole_Chapter-06.indd 231 1/20/2011 2:35:24 PM
232 Chapter 6
FIGURE 6-57
Benign or malignant salivary neoplasms of the buccal mucosa present as submucosal swellings, some of
which have a bluish cast due to mucin production in the tumor.
ble mucocele (which rarely occurs in the
upper lip), mesenchymal neoplasm, or Tongue Swellings
inflammatory hyperplasia. Ulcerated and
indurated adenocarcinomas must be differ- MEDIAN RHOMBOID
entiated from squamous cell carcinoma and GLOSSITIS
sarcomas. Figure 6-58
TREATMENT Age: Adults
Sex: Male predilection
Benign salivary tumors should be excised
rather than merely enucleated, because the CLINICAL FEATURES
latter procedure often results in recurrence. A smooth-surfaced, slightly nodular pink ele-
Wide and often radical excision is necessary vation that is devoid of papillae and is located
to eradicate malignant salivary tumors. immediately anterior to the foramen caecum
Depending on the histologic designation, and circumvallate papillae in the midline
neck dissection may be indicated. characterizes median rhomboid glossitis.
This anomaly could represent a develop-
mental defect: persistence of the tuberculum
Additional Reading impar with failure to retrude during embryo-
Gardner DG, Bell ME, Wesley RK, Wysocki GP. Acinic genesis. This theory is equivocal in light of
cell tumors of minor salivary glands. Oral Surg Oral evidence that suggests the lesion is not con-
Med Oral Pathol. 1980;50:545. genital but arises later in life. Candida organ-
Krolls SO, Hicks JL. Mixed tumors of the lower lip. Oral isms are associated with this lesion, and
Surg Oral Med Oral Pathol. 1973;35:212.
Owens OT, Calcaterra TC. Salivary gland tumors of
although some investigators think they play
the lip. Arch Otolaryngol Head Neck Surg. 1982; a causative role, this theory has not been
108:45. documented in all instances. It is innocuous,
Spiro RH, Koss LG, Hajdu SI, Strong EW. Tumors of painless, and rarely warrants removal.
minor salivary origin; a clinicopathologic study of 492
cases. Cancer. 1973;31:117.
Weber RS, Palmer JM, el-Naggar A, McNeese MD, MICROSCOPIC FEATURES
Guillamondegui OM, Byers RM. Minor salivary gland
tumors of the lip and buccal mucosa. Laryngoscope. The surface epithelium is devoid of papil-
1989;99:6-9. lae and shows rete ridge extension into the
PMPH_Eversole_Chapter-06.indd 232 1/20/2011 2:35:39 PM
Intraoral Soft Tissue Swellings 233
FIGURE 6-58
Median rhomboid glossitis,
characterized by a midline
swelling located on the
dorsum of the tongue.
submucosa. Candidal organisms are often Martin HE, Howe ME. Glossitis rhombica mediana. Ann
present within the parakeratin layer. The Surg. 1938;107:39.
Nelson BL, Thompson L. Median rhomboid glossitis.
subjacent fibrous tissue is mildly infiltrated Ear Nose Throat J. 2007;86:600-601
with leukocytes. Wright BA. Median rhomboid glossitis: not a misno-
mer. Review of the literature and histologic study of
DIFFERENTIAL DIAGNOSIS twenty-eight cases. Oral Surg Oral Med Oral Pathol.
1978;46:806.
Median rhomboid glossitis may clinically Wright BA, Fenwick BA. Candidiasis and atrophic tongue
resemble mesenchymal neoplasms, lingual lesions. Oral Surg Oral Med Oral Pathol. 1981;51:55.
cyst, and glossal-oriented thyroglossal duct
cyst. Generally, a clinical diagnosis is easily
rendered by virtue of its configuration, lack ECTOPIC LINGUAL THYROID
of growth potential, and midline location. Figure 6-59
TREATMENT Age: Early adulthood
Sex: Female predilection
If the tumefaction is large, a biopsy is indi-
cated to rule out neoplasia or cyst. When it CLINICAL FEATURES
is of limited size, periodic recall should be Ectopic thyroid tissue appears as a smooth,
instituted to determine that no growth is nodular, or occasionally cystic swelling pos-
taking place. terior to the foramen caecum. Dysphagia
may be a feature. In most patients, no thy-
Additional Reading roid tissue can be detected in the usual loca-
tion. For this reason, excision could result in
Baughman RA. Median rhomboid glossitis: a developmental postsurgical hypothyroidism. An 131I radio-
anomaly? Oral Surg Oral Med Oral Pathol. 1971;31:56. isotope scan is useful in the diagnosis of
PMPH_Eversole_Chapter-06.indd 233 1/20/2011 2:35:52 PM
234 Chapter 6
FIGURE 6-59
Lingual thyroid nodule at
base of tongue. Radioactive
iodine uptake is seen in
base of tongue rather than
in the normal region of the
anterior neck.
suspected lingual thyroid and serves as an
indication as to whether or not any thyroid Additional Reading
tissue is present in the usual location. The Ashhurst APC, White CY. Carcinoma in an aberrant thy-
ectopic location reflects the failure of normal roid at base of tongue. JAMA. 1925;85:1219.
developmental migration of the thyroglossal Baughman RA. Lingual thyroid and lingual thyroglossal
tract and gland primordium. Both adenoma tract remnants. A clinical and histopathologic study
with review of the literature. Oral Surg Oral Med Oral
and adenocarcinoma have been reported to Pathol. 1972;34:781.
arise in lingual thyroid nodules. Rahbar R, Yoon MJ, Connolly LP, et al. Lingual thy-
roid in children: a rare clinical entity. Laryngoscope.
MICROSCOPIC FEATURES 2008;118:1174-1179.
Reaume CE, Sofie VL. Lingual thyroid, review of the lit-
The oral epithelium is distended by mature erature and report of a case. Oral Surg Oral Med Oral
thyroid follicles filled with colloid and lined Pathol. 1978;45:841.
Wible LE, Freeman GR. Lingual thyroid. Arch
by cuboidal epithelium.
Otolaryngol Head Neck Surg. 1962;75:168.
DIFFERENTIAL DIAGNOSIS
The lingual thyroid nodule must be dif- THYROGLOSSAL DUCT CYST
ferentiated from thyroglossal duct cyst, Figure 6-60
a large superiorly displaced vallecular
cyst, and mesenchymal neoplasm. An 131I Age: Childhood onset
scan can outline the extent of the lesion Sex: No predilection
and identify any normally located thyroid CLINICAL FEATURES
tissue. Thyroglossal cysts arise from remnants of
the thyroid anlage and are generally seen
TREATMENT above the thyroid in the vicinity of the
Incisional biopsy may be performed to hyoid bone in the midline of the neck. They
aid in diagnosis; however, the entire mass may, however, arise in the substance of the
should not be removed if normally located tongue below the foramen caecum. They
thyroid tissue cannot be demonstrated. are compressible and yield a yellow fluid on
Should the lesion show a history of recent aspiration. Dysphagia may develop. Carci-
growth, biopsy is indicated to rule out thy- noma has been reported to arise from the
roid neoplasia. cyst lining.
PMPH_Eversole_Chapter-06.indd 234 1/20/2011 2:36:21 PM
Intraoral Soft Tissue Swellings 235
FIGURE 6-60
Thyroglossal cyst in the
tongue. Source: Macdonald
DM. Thyroglossal cysts and
fistulae. Int J Oral Maxillofac
Surg. 1974;3:342.
MICROSCOPIC FEATURES
The cyst is lined by columnar, respiratory,
or stratified squamous epithelium. Follicles
of thyroid glandular epithelium are fre-
quently located in juxtaposition to the cyst
lining.
DIFFERENTIAL DIAGNOSIS
Lingually localized thyroglossal duct cyst
has features similar to lingual thyroid nod-
ule, mesenchymal neoplasms, and even
a posteriorly located median rhomboid
glossitis.
FIGURE 6-61
TREATMENT Lingual developmental gastric cyst in the area of the
foramen ceacum.
The cyst should be surgically excised or
enucleated.
LINGUAL CYST
Additional Reading (ENTEROCYSTOMA, GASTRIC
CYST)
Burkart CM, Richter GT, Rutter MJ, Myer CM, 3rd. Figure 6-61
Update on endoscopic management of lingual
thyroglossal duct cysts. Laryngoscope. 2009;119:
2055-2060. Age: Insufficient data to determine
Gross RE, Connerly ML. Thyroglossal cysts and sinus- Sex: Insufficient data to determine
es; a study and report of 198 cases. N Engl J Med. CLINICAL FEATURES
1940;223:616.
MacDonald DM. Thyroglossal cysts and fistulae. Int J The lingual cyst is rare and is located in the
Oral Maxillofac Surg. 1974;3:342. anterior midline of the tongue. It is mov-
Nachlas NE. Thyroglossal duct cysts. Ann Otol Rhinol
Laryngol. 1950;59:381.
able and compressible. Few cases have been
Snedecor PA, Groshong LE. Carcinoma of the thyroglos- reported. It has been suggested to arise as
sal duct. Surgery. 1965;58:969. a result of epithelial entrapment during
PMPH_Eversole_Chapter-06.indd 235 1/20/2011 2:36:31 PM
236 Chapter 6
fissural closure of the lateral lingual pro- HYPERPLASTIC LINGUAL
cesses during development. Many of these TONSIL
lesions harbor gastric primordial epithe- Figure 6-62
lium; hence, the term enterocystoma.
Age: Adults
MICROSCOPIC FEATURES Sex: No predilection
Most lingual cysts are lined by aberrant gas- CLINICAL FEATURES
tric epithelium and are referred to as gastric
cysts or enterocystoma. Some lesions are The foliate papillae located at the postero-
simply lined by columnar, respiratory, or lateral tongue base represent lingual tonsils
stratified squamous epithelium. with epithelial lined crypts surrounded by
lymphoid tissue that may produce germi-
DIFFERENTIAL DIAGNOSIS nal centers. These tonsillar tissues become
enlarged during upper respiratory infec-
The smooth nodular swelling protrudes
tions or from trauma. The hyperplastic
dorsally so that confusion with dermoid
tissue is smooth, reddish yellow, and non-
cyst or ranula should be no problem. A
ulcerated. They are usually painless, yet in
lingual abscess or mesenchymal neoplasm
some patients discomfort is a complaint.
may clinically resemble a lingual cyst.
MICROSCOPIC FEATURES
TREATMENT
Surface stratified squamous epithelium is
Surgical excision is recommended.
hyperplastic and is distended by sheets of
lymphocytes with germinal centers that are
Additional Reading also hyperplastic. The epithelial lined ton-
sillar crypts blend imperceptibly with the
Arcand P, Granger J, Brochu P. Congenital dermoid cyst surrounding lymphocytes.
of the oral cavity with gastric choristoma. J Otolaryngol.
1988;17:219.
Gorlin RJ, Jirasek JE. Oral cysts containing gastric or DIFFERENTIAL DIAGNOSIS
intestinal mucosa; unusual embryologic accident or
heterotopia. J Oral Maxillofac Surg. 1970;28:9.
Hyperplastic lingual tonsils are common
Katz A, Aimi K, Skolnik EM. Enterocystoma of the head and occur in the same site as squamous
and neck. Laryngoscope. 1980;90:1441. cell carcinoma of the posterolateral tongue.
Lui B, Korman B. Congenital oral heterotopic gastroin- Unlike carcinoma, hyperplastic tissues
testinal cyst: case report and review of the literature.
J Otolaryngol Head Neck Surg. 2008;37:E151-E154.
are not indurated, being soft to palpation.
Quinn JH. Congenital epidermoid cyst of anterior half of Biopsy should be performed for patients
tongue. Oral Surg Oral Med Oral Pathol. 1960;13:1283. who smoke just to be certain.
FIGURE 6-62
Hyperplastic lymphoid
tissue is nodular, located
at the lateral tongue base
(foliate papillae).
PMPH_Eversole_Chapter-06.indd 236 1/20/2011 2:36:49 PM
Intraoral Soft Tissue Swellings 237
FIGURE 6-63
Submucosal abscesses are
firm and tender. Many occur
after trauma or a piercing
by a small fishbone.
TREATMENT DIFFERENTIAL DIAGNOSIS
Short-term follow-up is recommended. The Pain signals an acute infection in a tongue
hyperplastic tissues tend to regress over time. mass. Other reactive and neoplastic lesions
should be considered.
Additional Reading TREATMENT
Di Felice R, Lombardi T. Foliate papillitis occurring in a Excision with debridement should be
child: a case report. Ann Dent. 1993;52:17-18. undertaken. Antibiotic therapy is reserved
Parham K, Newman R. Recurrent lingual tonsil hyper- for patients with fever.
plasia. Arch Otolaryngol Head Neck Surg. 2003;129:
1010-1012.
Additional Reading
LINGUAL ABSCESS Eviatar E, Pitaro K, Segal S, Kessler A. Lingual abscess:
Figure 6-63 secondary to follicular tonsillitis. Otolaryngol Head
Neck Surg. 2004;131:558-559.
Age: Adults Kim HJ, Lee BJ, Kim SJ, Shim WY, Baik SK, Sunwoo
Sex: No predilection M. Tongue abscess mimicking neoplasia. AJNR Am J
Neuroradiol. 2006;27:2202-2203.
CLINICAL FEATURES
Trauma from a tongue bite or introduction
of a foreign object such as a fish bone can REACTIVE LESIONS (FIBROMA,
leave a laceration that can fester, becom- PYOGENIC GRANULOMA)
ing infected with pyogenic bacteria such Figure 6-64
as staphylococci or streptococci. Clinically,
the tongue becomes swollen, is exquisitely Age: Adults
Sex: No predilection
painful to touch, and often has a fistula.
CLINICAL FEATURES
MICROSCOPIC FEATURES The most common swelling of the tongue
A foreign object may be seen microscopi- is the traumatic fibroma. It appears as a
cally and when none is found, reexami- dome-shaped submucosal mass that shows
nation under polarized light may reveal normal mucosal coloration and is rarely
refractile particles. Muscle necrosis and ulcerated. They can be located anywhere
degeneration are evident with a suppura- on the tongue. Fibromas evolve secondary
tive infiltrate of leukocytes. to trauma, usually a tongue bite incident.
PMPH_Eversole_Chapter-06.indd 237 1/20/2011 2:37:02 PM
238 Chapter 6
FIGURE 6-64
Reactive lesions of the
tongue include pyogenic
granulomas that are red
or purple and traumatic
fibromas, usually of nor-
mal coral pink coloration.
Pyogenic granulomas are similarly reactive TREATMENT
proliferations that also appear as dome- Excision is the treatment of choice. Fibro-
shaped masses. They are typically red and mas do not tend to recure whereas pyogenic
usually show a whitish surface secondary granulomas sometimes do.
to ulceration. Pyogenic granulomas usually
proliferate rapidly, alarming patients that
they may have cancer. Additional Reading
MICROSCOPIC FEATURES Gordón-Núñez MA, Carvalho MD, Benevenuto TG,
Lopes MF, Silva LM, Galvão HC. Oral pyogenic
Fibromas show a layer of surface epithelium granuloma: a retrospective analysis of 293 cases
that may manifest hyperkeratosis and acan- in a Brazilian population. J Oral Maxillofac Surg.
2010;68:2185-2188. [Epub ahead of print.]
thosis. Comprising the bulk of the speci- Kuo RC, Wang YP, Chen HM, Sun A, Liu BY, Kuo YS.
men is mature fibrous connective tissue Clinicopathological study of oral giant cell fibromas.
that is traversed by capillaries. Scattered J Formos Med Assoc. 2009;108(9):725-729.
leukocytes are sometimes present. Giant cell
fibromas contain multinucleated fibroblasts
with a splayed “manta ray” cytoplasm. Pyo- MUCOCELE
genic granulomas are often ulcerated with a Figure 6-65
fibrinous surface membrane. The specimen
comprises granulation tissue, prominently Age: Children
Sex: No predilection
vascularized, and the vessels are often
arranged in a lobular pattern of growth. CLINICAL FEATURES
Most mucoceles occur on the lower lip and
DIFFERENTIAL DIAGNOSIS once excised, the recurrence rate is low pro-
Other mesenchymal tumors are easily mis- vided the underlying feeder glands are enu-
taken clinically for reactive growths. Biopsy cleated during surgical excision. Mucocels
is required to secure a definitive diagnosis. that arise from the glands of Blandin-Nuhn
PMPH_Eversole_Chapter-06.indd 238 1/20/2011 2:37:16 PM
Intraoral Soft Tissue Swellings 239
FIGURE 6-65
Mucoceles in the region of
the minor salivary glands
of Blandin-Nuhn tend to
recur following excision.
behave differently. They appear as unifocal gland of Blandin-Nuhn: histological and clinical find-
nodules on the ventral anterior tongue and ings. Clin Oral Investig. 2009;13:351-353. [Epub 2009
Jan 27.]
may be translucent or blue. They are fluc- Sugerman PB, Savage NW, Young WG. Mucocele of the
tuant to palpation and evolve subsequent anterior lingual salivary glands (glands of Blandin and
to trauma such as tongue biting or ventral Nuhn): report of 5 cases. Oral Surg Oral Med Oral
tongue lacerations. Since the minor glands Pathol Oral Radiol Endod. 2000;90:478-482.
of Blandin-Nuhn reside within the intrin-
sic muscle layers, they are often left behind HEMANGIOMA AND
during treatment, providing saliva leakage
LYMPHANGIOMA
that predispose to a recurrence.
Figure 6-66
MICROSCOPIC FEATURES
Age: Children
The epithelium is distended by pooled Sex: No predilection
mucin undergoing varying degrees of CLINICAL FEATURES
organization by granulation tissue. Minor
glands may be seen interposed between Vascular tumors often arise within the
muscle fibers. tongue and manifest a swelling of the mid-
line or lateral margins. When superficial,
DIFFERENTIAL DIAGNOSIS which is often the case, racemose nodules
are present; in hemangioma, they are red
The clinical appearance is quite classic, and blanch on pressure. Lymphangiomas
although in sclerosing lesions, a fibroma or do not impart a color change to the mucosa.
mesenchymal tumor may be expected. The entire tongue or only a portion of it may
be occupied by neoplastic vessels. Calcified
TREATMENT
thrombi or phleboliths are often present in
Excision of the mucocele, making sure to hemangiomas of long standing; the calci-
dissect out the intramuscular glands, is fied nodules are demonstrable as soft tissue
essential to avoid recurrence. radiopacities radiographically. The more
aggressive vascular tumors, hemangioen-
Additional Reading dothelioma and hemangiopericytoma, are
more firm to palpation, have a rapid growth
Adachi P, Soubhia AM, Horikawa FK, Shinohara EH. rate, and have metastatic potential.
Mucocele of the glands of Blandin-Nuhn-clinical, path-
ological, and therapeutical aspects. Oral Maxillofac MICROSCOPIC FEATURES
Surg. 2010 Apr 15. [Epub ahead of print.]
de Camargo Moraes P, Bönecker M, Furuse C, Thomaz Hemangioma and lymphangioma have
LA, Teixeira RG, de Araújo VC. Mucocele of the similar microscopic characteristics. Dilated
PMPH_Eversole_Chapter-06.indd 239 1/20/2011 2:37:34 PM
240 Chapter 6
FIGURE 6-66
Hemangiomas are common
in the tongue, appearing at
infancy or childhood. The
hemangioma in the upper
right was radiated, causing
advanced radiation caries
in the dentition. Case in
lower right is creamy white
being a lymphangioma.
endothelium-lined channels course throu- ture of vascular neoplasm. Deeply situated
ghout the tongue stroma and are often angiomas may be confused with other mes-
intramuscular. When superficially oriented, enchymal neoplasms.
exophytic extensions composed of vessels
distend the surface epithelium. The vascu- TREATMENT
lar channels of hemangioma contain eryth- When the lesions are small, local excision is
rocytes and occasionally thrombi. When recommended. Lingual hemangiomas may
the lesions are primarily cellular, they are bleed profusely. Extensive lesions, once
designated as cellular hemangioma or benign diagnosed by biopsy, may be left untreated
hemangioendothelioma. These lesions behave if asymptomatic. The aggressive angiomas
benignly, similar to simple hemangiomas. (hemangioendothelioma, hemangioperi-
Lymphangiomas contain lymph, an eosino- cytoma) require wide local excision with
philic coagulum. The aggressive hemangio- periodic follow-up. Metastasis may develop
endothelioma is highly cellular, composed late but metastatic predictability is difficult
of monomorphic, plump elongated nuclei if not impossible for aggressive angiomas
with little pleomorphism. These cells line based on microscopic evaluation.
vacant clefts resembling stag horns. Heman-
giopericytomas are composed of similar
cells but are arranged in swirls around a
small lumen.
Additional Reading
Brockbank J. Hemangiopericytoma of the oral cav-
DIFFERENTIAL DIAGNOSIS ity: report of case and review of the literature. J Oral
Maxillofac Surg. 1979;37:659.
Most vascular lesions are extensive so that Goldberg MH, Nemarich AN, Danielson P.
confusion with focal midline tongue lesions Lymphangioma of the tongue: medical and surgical
therapy. J Oral Maxillofac Surg. 1977;35:841.
such as median rhomboid glossitis, lingual Khanna JN, Khanapurkar CR. Bilateral vascular lesion
thyroid, or cystic lesions is not probable. A of the tongue, hemangioma, and lymphangioma. J Ind
racemose surface pattern is invariably a fea- Dent Assoc. 1979;51:139.
PMPH_Eversole_Chapter-06.indd 240 1/20/2011 2:37:48 PM
Intraoral Soft Tissue Swellings 241
Shklar G, Meyer L. Vascular tumors of the mouth and are associated with similar lesions of skin
jaws. Oral Surg Oral Med Oral Pathol. 1965;19:335. and café-au-lait pigmentations, they repre-
Watson WL, McCarthy WD. Blood and lymph vessel
tumors; a report of 1,056 cases. Surg Gynecol Obstet. sent a component of von Recklinghausen’s
1940;71:569. neurofibromatosis. Oral neurofibromas are,
however, most frequently solitary. Neural
tumors occurring as multiple small nod-
NEURAL SHEATH TUMORS ules may be a component of the Sipple syn-
Figure 6-67 drome (see papillary and multiple polypoid
swellings).
Age: Young adults
Sex: No predilection MICROSCOPIC FEATURES
CLINICAL FEATURES Neurilemmoma shows a fibrous capsule;
Benign neoplasms of cells that ensheath the tumor cells are arranged in parallel
nerves include those derived from the rows, demonstrating palisading of nuclei,
neurilemma, neurilemmomas, and those Antoni type A tissue. Palisaded nuclei are
derived by perineuronal fibroblasts, neuro- separated by a dense acellular fibrillar zone.
fibromas. Both types may arise anywhere Organoid swirls of Antoni A tissue consti-
in the mouth, but are encountered most fre- tute Verocay bodies. Antoni B tissue is com-
quently in the tongue, where they appear as posed of loosely arranged collagen with
smooth-surfaced firm or rubbery painless interfibrillar vacuolated foci. Neurofibromas
nodules. Neurilemmomas are encapsulated are composed of elongated nuclei randomly
yet may be multinodular. Neurofibromas dispersed in a fibrous background. The cel-
are well defined, yet lack true encapsula- lular pattern is winding, giving the appear-
tion. When multiple oral neurofibromas ance of intercoiled spaghetti noodles. Rare
FIGURE 6-67
Nerve sheath tumors of
the tongue. Most neuro-
fibromas are solitary; the
patient on the upper left
has neurofibromatosis.
Lower left: neurilemmoma
(Schwannoma).
PMPH_Eversole_Chapter-06.indd 241 1/20/2011 2:38:10 PM
242 Chapter 6
nerve sheath tumors include benign nerve Hatziotis JC, Asprides H. Neurilemmoma (schwannoma)
sheath myxoma, palisaded encapsulated of the oral cavity. Oral Surg Oral Med Oral Pathol.
1967;24:510.
neuroma, and ancient neurilemmoma. Karaca CT, Habesoglu TE, Naiboglu B, et al. Schwannoma
of the tongue in a child. Am J Otolaryngol. 2010;31:46-
DIFFERENTIAL DIAGNOSIS 48. [Epub 2009 Mar 26.]
O’Driscoll PM. The oral manifestations of multiple neu-
Neural sheath neoplasms tend to locate in rofibromatosis. Br J Oral Maxillofac Surg. 1965;3:22.
the anterior one third of the tongue, and the
swelling must be differentiated from other
mesenchymal neoplasms, lingual cysts, and GRANULAR CELL TUMOR
salivary tumors, which occasionally arise Figure 6-68
from minor glands of the tongue.
Age: No predilection
TREATMENT Sex: No predilection
Simple excision is rarely complicated by CLINICAL FEATURES
recurrence. Granular cell tumors are derived from cells
that ensheath other cells such as neuri-
Additional Reading lemma (Schwann) cells or sarcolemma. The
term granular cell myoblastoma was used in
Chen S, Miller AS. Neurofibroma and schwannoma the past because most of these lesions in the
of the oral cavity. Oral Surg Oral Med Oral Pathol. mouth are associated with muscle fibers.
1979;47:522.
Cherrick HM, Eversole LR. Benign neural sheath neo-
Nevertheless, many are clearly derived
plasm of the oral cavity; report of thirty-seven cases. from nerve sheath cells. The lesions appear
Oral Surg Oral Med Oral Pathol. 1971;32:900. as small elevated nodules on the dorsum
FIGURE 6-68
Granular cell tumors of
the tongue, generally pre-
senting as a smooth nod-
ule with a sessile base.
PMPH_Eversole_Chapter-06.indd 242 1/20/2011 2:38:29 PM
Intraoral Soft Tissue Swellings 243
or lateral border of the tongue. They are TREATMENT
painless and soft to palpation. The rhab- Simple excision is recommended. Recur-
domyoma, a rare tumor of muscle origin, rence is almost nonexistent.
also arises in the tongue. These tumors
are encapsulated and have limited growth
potential. Additional Reading
Corio RL, Lewis DM. Intraoral rhabdomyomas. Oral
MICROSCOPIC FEATURES Surg Oral Med Oral Pathol. 1979;48:525.
Eversole LR, Sabes WR, Rovin S. Granular sheath
Oval eosinophilic granular cells have cell lesions; report of cases. J Oral Maxillofac Surg.
pyknotic nuclei and are separated from one 1971;29:867.
another by scant stroma. When superficial, Nagaraj PB, Ongole R, Bhujanga-Rao BR. Granular cell
the epithelium may show extensive pseu- tumor of the tongue in a 6-year-old girl—a case report.
Med Oral Patol Oral Cir Bucal. 2006;11:E162-E164.
doepitheliomatous hyperplasia. The granu- Regizi JA, Batsakis JG, Courtney RM. Granular cell
lar cells may emanate from either muscle tumors of the head and neck. J Oral Maxillofac Surg.
fibers or neural sheath. Rhabdomyomas 1979;37:402.
are composed of large oval or elongated Stewart C, Watson RE, Eversole LR, Fischlschweiger W,
Leider AS. Oral granular cell tumors: a clinicopatho-
cells with eosinophilic granular cytoplasm
logic and immunocytochemical study. Oral Surg Oral
showing evidence of cross-striations. The Med Oral Pathol. 1988;65:427.
nuclei are eccentric.
DIFFERENTIAL DIAGNOSIS
LEIOMYOMA
Figure 6-69
Granular sheath cell lesions and rhabdomy-
oma may be clinically similar to median Age: Middle-aged adults
rhomboid glossitis or other mesenchymal Sex: Male predilection
neoplasms. CLINICAL FEATURES
Leiomyomas are smooth-surfaced tume-
factions that may arise in any location.
In the mouth, they are most frequently
encountered on the tongue. The tumor is
encapsulated, painless, firm, and may be
multinodular.
MICROSCOPIC FEATURES
The tumor cells possess elongated, blunt-
ended nuclei with a vesicular nucleoplasm.
The cells course in streams and fascicles,
often evolving from vessels showing perivas-
cular concentric laminations of spindle
cells. The fibrillar background may be dis-
tinguished from collagen with a trichrome
stain and smooth muscle actin IHC.
DIFFERENTIAL DIAGNOSIS
FIGURE 6-69
Leiomyoma. These are rare in the mouth; when Leiomyoma may be clinically indistinguish-
they occur, the tongue is the favored site. able from other mesenchymal neoplasms.
PMPH_Eversole_Chapter-06.indd 243 1/20/2011 2:38:48 PM
244 Chapter 6
TREATMENT the tongue. Whereas most are asymptomatic,
Simple surgical excision is recommended. some cause dysphagia. They may be located
Recurrence is unlikely after complete in the anterior, mid, or posterior regions and
excision. are more often visualized or palpable on the
dorsal aspect. They are firm or hard, ses-
sile or pedunculated, and freely movable.
Additional Reading Because no osteoprogenitor cells are within
the tongue, their origin is obscure; hence,
Cherrick HM, Dunlap CL, Klug OH. Leiomyomas of the
they represent choristomas. Their potential
oral cavity; review of the literature and clinicopatho-
logic study of seven new cases. Oral Surg Oral Med for growth is probably self-limited.
Oral Pathol. 1973;35:54.
de Faria PR, Batista JD, Duriguetto AF, Jr, et al. Giant MICROSCOPIC FEATURES
leiomyomatous hamartoma of the tongue. J Oral
Maxillofac Surg. 2008;66:1476-1480. Some lesions are entirely dense lamellar
Kelly DE, Harrigan WF. Leiomyoma of the tongue: osseous tissue with a paucity of fibrous
report of a case. J Oral Maxillofac Surg. 1977;35:316. marrow or stroma. Others exhibit enclaved
Leung KW, Wong DY, Li WY. Oral leiomyoma: case
report. J Oral Maxillofac Surg. 1990;48:735.
foci of chondroid tissue.
MacDonald DG. Smooth muscle tumors of the mouth.
Br J Oral Maxillofac Surg. 1969;6:207. DIFFERENTIAL DIAGNOSIS
Clinically, osseous or osteocartilaginous
choristomas may resemble traumatic fibro-
OSTEOCARTILAGINOUS
mas or other mesenchymal neoplasms. On
CHORISTOMA palpation, however, a movable rock-hard
Figure 6-70 nodule should arouse suspicion of osseous
choristoma. An occlusal radiograph will
Age: Young adults
show a radiopaque mass within the soft tis-
Sex: Female predilection
sue of the tongue.
CLINICAL FEATURES
Discrete nodules of osseous or osteocarti- TREATMENT
laginous tissue may form in the substance of Osseous and osteocartilaginous choris-
tomas are easily enucleated from adjacent
soft tissues. Pedunculated varieties can
simply be excised at the base of the stalk.
Additional Reading
Krolls SO, Jacoway JR, Alexander WN. Osseous cho-
ristomas (osteomas) of the intraoral soft tissues. Oral
Surg Oral Med Oral Pathol. 1971;32:588.
Landini G, Kitano M, Urago A, Sugihara K, Yamashita S.
Chondroma and osteochondroma of the tongue. Oral
Surg Oral Med Oral Pathol. 1989;68:206.
Tohill MJ, Green JG, Cohen DM. Intraoral osseous and
cartilaginous choristomas: report of three cases and
review of the literature. Oral Surg Oral Med Oral
Pathol. 1987;63:506.
Yaqoob N, Ahmed Z, Muzaffar S. Chondroid choristoma of
FIGURE 6-70 tongue—a rare entity. J Pak Med Assoc. 2002;52:584-585.
Cartilaginous choristoma appearing as blanched Zegarelli DJ. Chondroma of the tongue. Oral Surg Oral
nodule of ventral tongue. Med Oral Pathol. 1977;43:738.
PMPH_Eversole_Chapter-06.indd 244 1/20/2011 2:38:50 PM
Intraoral Soft Tissue Swellings 245
ECTOMESENCHYMAL Immunohistochemical markers that stain
CHONDROMYXOID TUMOR positively include cytokeratins, glial fibril-
Figure 6-71 lary acidic protein, S-100, and CD-57.
Age: Adults DIFFERENTIAL DIAGNOSIS
Sex: No predilection
Clinically, the other mesenchymal tumors
CLINICAL FEATURES listed here are in the differential, and the
The ectomesenchymal chondromyxoid consistency being soft resembles lipoma or
tumor (ECT) is a rare neoplasm found soft tissue myxoma.
almost exclusively on the tongue. It is most
commonly seen on the dorsum and is usu- TREATMENT
ally less than 2 cm in size. ECT appears as a
Local excision is the standard treatment
submucosal nodule that is soft and movable
with recurrence being rare.
with a nonulcerated intact surface mucosa.
MICROSCOPIC FEATURES
Surface epithelium is intact and overlies a
Additional Reading
well-demarcated submucosal mass with Allen CM. The ectomesenchymal chondromyxoid tumor:
a review. Oral Dis. 2008;14:390-395.
a variety of tissue patterns including epi-
de Camargo Moraes P, Bönecker M, Furuse C, Thomaz
thelial-like strands with eosinophilic cyto- LA, Teixeira RG, de Araújo VC. Mucocele of the gland
plasm and monomorphic nuclei. A myxoid of Blandin-Nuhn: histological and clinical findings.
element is prominent with immature chon- Clin Oral Investig. 2009;13(3):351-353. [Epub 2009
dromyxoid tissue. Hypercellularity is not Jan 27.]
Jinbu Y, Kusama M, Itoh H, Matsumoto K, Wang J,
a feature, and mitotic figures are absent. Noguchi T. Mucocele of the anterior lingual salivary
glands (glands of Blandin and Nuhn): report of 5 cases.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
2000;90:478-482.
Jinbu Y, Kusama M, Itoh H, Matsumoto K, Wang J,
Noguchi T. Mucocele of the glands of Blandin-Nuhn:
clinical and histopathologic analysis of 26 cases. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod.
2003;95:467-470.
Nigam S, Dhingra KK, Gulati A. Ectomesenchymal chon-
dromyxoid tumor of the hard palate—a case report.
J Oral Pathol Med. 2006;35:126-128.
SARCOMAS
Figure 6-72
Age: Varies with tumor type
Sex: No predilection
CLINICAL FEATURES
Sarcomas of the oral cavity are rare. They
FIGURE 6-71 may arise in any locality, including the
Ectomesenchymal chondromyxoid tumors are rare tongue. The more frequently encountered
and limited to the tongue. They appear as movable types include rhabdomyosarcoma and fibro-
soft-to-firm submucosal nodules. sarcoma. All sarcomas show a rapid growth
PMPH_Eversole_Chapter-06.indd 245 1/20/2011 2:38:55 PM
246 Chapter 6
FIGURE 6-72
Rhabdomyosarcoma of the
tongue. Upper left repre-
sents initial presentation.
Lower right is just prior to
death, just 1 month later.
rate, are indurated and fixed, and have a
tendency toward ulceration. Hematoge- Additional Reading
nous metastasis is the most frequent route Eley KA, Afzal T, Shah KA, Watt-Smith SR. Alveolar
of spread from sarcomas leading to pulmo- soft-part sarcoma of the tongue: report of a case and
nary and widespread metastatic foci. review of the literature. Int J Oral Maxillofac Surg.
2010;39:824-826.
Eversole LR, Schwartz D, Sabes WR. Central and periph-
MICROSCOPIC FEATURES
eral fibrogenic and neurogenic sarcomas of the oral
Histologic findings vary, depending on dif- regions. Oral Surg Oral Med Oral Pathol. 1973;36:49.
ferentiation of the tumor. Most sarcomas Masson JK, Soule EH. Embryonal rhabdomyosarcoma of
the head and neck; report on eighty-eight cases. Am J
are composed of spindle, pleomorphic, and Surg. 1965;110:585.
anaplastic cells with multiple and bizarre O’Day RA, Soule EH, Gores RJ. Soft tissue sarcomas of
mitotic figures. Invasion of adjacent tissues the oral cavity. Proc Mayo Clin. 1964;39:169.
is a constant feature. Microscopically, sar- Ryan MD, LaDow C. Primary fibrosarcoma of the tongue:
report of case. J Oral Maxillofac Surg. 1972;30:135.
comas must be differentiated from cellular
fibromatoses and pseudosarcomas.
AMYLOID NODULES
DIFFERENTIAL DIAGNOSIS Figure 6-73
Indurated fixed swellings in the tongue
must be differentiated from carcinoma and Age: Adults
Sex: No predilection
salivary adenocarcinoma.
CLINICAL FEATURES
TREATMENT Amyloidosis is a metabolic disorder char-
Radical excision or glossectomy is required. acterized by deposition of a starch-like pro-
Despite radical treatment, the prognosis is tein in the tissues. Solitary nodules may
poor. be deposited in the tongue, or widespread
PMPH_Eversole_Chapter-06.indd 246 1/20/2011 2:38:58 PM
Intraoral Soft Tissue Swellings 247
FIGURE 6-73
Amyloid nodules of the
tongue. (Courtesy of
Drs. S. Silverman and T.
Daniels.)
multifocal organ involvement may evolve. aged by control of the primary disease
It may be primary, secondary to chronic process. All forms should be managed by a
infection such as tuberculosis or osteomy- physician.
elitis, or associated with multiple myeloma.
A unique form of amyloid, β2-microglobulin
amyloidosis, is encountered in patients Additional Reading
undergoing long-term hemodialysis. The Barth WF. Primary amyloidosis. Ann Intern Med.
tongue is the most common oral location 1968;69:787.
for the accumulation of amyloid, and the Guccion JG, Redman RS, Winne CE. Hemodialysis-
areas of deposition appear as focal or mul- associated amyloidosis presenting as lingual nodules.
Oral Surg Oral Med Oral Pathol. 1989;68:618.
tiple nodular elevations that are normal in Kraut RA, Buhler JE, LaRue JR, Acevedo A. Amyloidosis
color, nonulcerated, and painless. Diffuse associated with multiple myeloma. Oral Surg Oral
involvement of the tongue musculature cul- Med Oral Pathol. 1977;43:63.
minates in macroglossia with stiffness and Schwartz HC. Amyloidosis: a rational approach to diag-
nosis by intraoral biopsy. Oral Surg Oral Med Oral
lack of mobility. Pathol. 1975;39:837.
Serdar A, Basak D, Sercan G, Ali V. Solitary amy-
MICROSCOPIC FEATURES loid tumor of the tongue base. Int J Otolaryngol.
2009;2009:515068. [Epub 2009 Jan 6.]
Normal connective tissue is displaced by
accumulations of amorphous eosinophilic
deposits. The amyloid material stains with SPECIFIC GRANULOMA
Congo red and exhibits dichroism with Figure 6-74
green birefringence under polarized light.
Frequently, the deposits are in perivascular Age: Adults
distribution. Sex: No predilection
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
Specific granulomatous infection is primary
Solitary amyloid nodules may resemble in the lungs and appears orally as a sec-
inflammatory hyperplasia or mesenchymal ondary manifestation of miliary spread. In
neoplasm. Multiple nodules may be con- the United States, the infections most often
fused with those encountered in the Sipple encountered include tuberculosis, histoplas-
syndrome or neurofibromatoses. mosis, and cryptococcosis. Less frequently,
blastomycosis and coccidioidomycosis have
TREATMENT
oral manifestations. The lesions may develop
Secondary amyloidosis and amyloidosis anywhere in the mouth and are frequently
associated with myeloma must be man- seen on the tongue. They are characterized
PMPH_Eversole_Chapter-06.indd 247 1/20/2011 2:39:17 PM
248 Chapter 6
FIGURE 6-74
Ulcerated nodules repre-
senting primary syphilis
(right) and histoplasmo-
sis (left), granulomatous
infections.
by elevated nodular swellings with rolled ance of the primary lesion. A darkfield
margins and an ulcerated central region, smear discloses the presence of spirochetes.
or they are pebbly granular swellings. Pain
is usually not a feature. Primary syphilitic TREATMENT
chancre also occurs on the tongue, showing Once a diagnosis of granulomatous infec-
the same clinical features as the secondary tion is confirmed, a work-up for pulmonary
granulomatous infections. Histoplasmosis disease is in order and the patient should
of the oral mucosa in an HIV-positive patient be placed under the care of a physician for
represents a sentinel of disseminated dis- management and therapy. Syphilis can be
ease and is diagnostic for AIDS. treated by penicillin therapy.
MICROSCOPIC FEATURES
Granulation and fibrous tissues are admixed
Additional Reading
with macrophages and multinucleated giant Flynn TR, Hunter GJ, Johnson MM. Case records of
cells. Fungi can usually be found free and the Massachusetts General Hospital. Case 6-2010. A
37-year-old man with a lesion on the tongue. N Engl J
within giant cells with routine stains. Acid-
Med. 2010;362:740-748.
fast preparations are required for identifi- Franenfelder D, Schwartz AW. Coccidioidomycosis
cation of tubercle bacilli, and periodic acid- involving head and neck. Plast Reconstr Surg.
Schiff or methenamine silver readily discloses 1967;39:549.
the presence of mycotic microorganisms. A Verma A, Mann SB, Radotra B: Primary tuberculosis of
the tongue. Ear Nose Throat J. 1989;68:718.
dense plasma cell infiltrate is suggestive of Weed LA, Parkhill EM. The diagnosis of histoplasmosis
syphilis; however, a Warthin-Starry stain is in ulcerative disease of the mouth and pharynx. Am J
required to demonstrate spirochetes. Clin Pathol. 1948;18:130.
Yusuf H, Craig GT, Allan D. Disseminated histoplasmo-
sis presenting with oral lesions—report of a case. Br J
DIFFERENTIAL DIAGNOSIS
Oral Maxillofac Surg. 1979;16:234.
The ulcerated granulomas of tuberculosis
or the deep mycoses may clinically resem- SQUAMOUS CELL
ble carcinoma or even sarcoma. Biopsy is
CARCINOMA
required to establish a definitive diagnosis.
When tuberculosis or deep mycotic infection Figure 6-75
is discovered, it should be recalled that the Age: Elderly adults
oral lesions represent secondary infection Sex: Predominantly males
with primary pulmonary disease. Syphi-
CLINICAL FEATURES
litic chancre is not accompanied by positive
serologic findings; serologic testing should The tongue is the second most common site
be performed 2 to 3 weeks after the appear- for squamous cancer in the mouth, exceeded
PMPH_Eversole_Chapter-06.indd 248 1/20/2011 2:39:22 PM
Intraoral Soft Tissue Swellings 249
only by floor of the mouth. The posterior lat- cosa and muscle. Keratin pearl formation
eral border is the most common location; is usually present, and the individual cells
however, carcinoma may also affect the exhibit pleomorphism, hyperchromatism,
mobile and ventral regions. The dorsum is and increased mitotic activity. The stroma
rarely involved; when it is, syphilitic glos- is infiltrated by plasma cells and lympho-
sitis is usually preexistent. Lesions showing cytes. The IHC marker p16 is a surrogate
poor differentiation in the base of the tongue, marker for HPV infection. The presence of
and tonsillar pillars are associated with, and HPV is associated with a more favorable
may be caused by, human papilloma virus treatment outcome.
(HPV), especially HPV 16, the same onco-
genic virus implicated in uterine cervix car- DIFFERENTIAL DIAGNOSIS
cinoma. The neoplasm may be red, white,
mixed red and white, ulcerated, or tumefac- Tongue swellings located on the lateral mar-
tive. Even tumefactive lesions are usually gin with ulceration and induration rarely
ulcerated and often have coexistent leuko- represent benign lesions. Immediate biopsy
plakia and/or erythroplakia on the mar- is indicated.
gins. The mass is fixed and indurated and
may have involved the oral floor or tonsillar TREATMENT
pillar. These tumors are staged according to Combined radiation therapy and radical
extent. Submandibular or cervical lymph- surgery, along with neck dissection and/
adenopathy is frequently observed, particu- or radiation to the neck, are indicated for
larly in association with larger tumors. large tumors. Indeed, bilateral neck dissec-
tion should be undertaken as contralateral
MICROSCOPIC FEATURES metastases are frequently found. Small stage
Invasive islands and cords of neoplastic I tumors are usually curable with either
cells extend into the underlying submu- wide local excision or radiation therapy.
FIGURE 6-75
Squamous cell carcinoma
of the tongue, indurated
ulcerated masses.
PMPH_Eversole_Chapter-06.indd 249 1/20/2011 2:39:31 PM
250 Chapter 6
mental hereditary overgrowth of bone and
Additional Reading is extremely hard to palpation. The surface
El-Mofty SK, Patil S. Human papillomavirus (HPV)-related mucosa is generally intact and often shows
oropharyngeal nonkeratinizing squamous cell carcinoma: lobulation. Tori vary considerably in size
characterization of a distinct phenotype. Oral Surg Oral and are common, occurring in 20% of the
Med Oral Pathol Oral Radiol Endod. 2006;101:339-345. population. Orientals show a greater inci-
Maddox WA, Sherlock EC, Evans WB. Cancer of the
tongue: review of thirteen years experience. Am Surg. dence than whites and blacks. The palatal
1971;37:642. torus may be quite small, or it may grow to
Martin HE, Munster H, Sugarbaker ED. Cancer of the fill the entire palatal vault.
tongue. Arch Surg. 1940;41:888.
Spiro RH, Strong EW. Surgical treatment of cancer of MICROSCOPIC FEATURES
the tongue. Surg Clin North Am. 1974;54:4.
Martis CS. Carcinoma of the tongue: evaluation of sur- The excrescence is composed of an outer
gical treatment of 123 cases. J Oral Maxillofac Surg. cortical plate with a central cancellous zone.
1982;40:340.
The osseous tissues show normal histologic
features.
Palatal Swellings DIFFERENTIAL DIAGNOSIS
The midline location, slow growth, and
TORUS PALATINUS bone-hard nature of palatal tori allow for dif-
Figure 6-76 ferentiation from palatal abscess or salivary
tumors, which are softer and usually located
Age: Young adults
somewhat lateral to the palatal raphe.
Sex: Female predilection
CLINICAL FEATURES TREATMENT
Palatal torus is a bone-hard excrescence Tori may be left untreated. When a torus
that develops after puberty in the midline interferes with fabrication of a maxillary
of the palatal vault. It represents a develop- dental prosthesis, it may be excised.
FIGURE 6-76
Torus palatinus, a bone-
hard bosselated swell-
ing located in the palatal
vault.
PMPH_Eversole_Chapter-06.indd 250 1/20/2011 2:39:53 PM
Intraoral Soft Tissue Swellings 251
FIGURE 6-77
Anterior palatal midline
swelling representing a
cyst of the incisive papilla.
(Courtesy of Dr. A. Leider.)
ratory epithelium is coexistent. The fibrous
Additional Reading wall is rich in neurovascular elements,
Barbujani G, Rolo M, Barrai I, Pinto J. Torus palatinus: a and an inflammatory cell infiltrate is not
segregation analysis. Hum Hered. 1986;36:317. uncommon.
Gould AW. An investigation of the inheritance of
torus palatinus and torus mandibularis. J Dent Res. DIFFERENTIAL DIAGNOSIS
1964;43:159.
King DR, Moore GE. An analysis of torus palatinus in a The location is characteristic; however, cysts
transatlantic study. J Oral Pathol Med. 1976;31:44. of the incisive papilla must be differenti-
Kolas S, Halperin V. The occurrence of torus palatinus
and torus mandibularis in 2,478 dental patients. Oral ated from a central incisive canal cyst with
Surg Oral Med Oral Pathol. 1953;6:1134. draining fistula and palatal abscess arising
Reichart PA, Neuhaus F, Sookasem M. Prevalence of from odontogenic infection.
torus palatinus and torus mandibularis in Germans and
Thai. Community Dent Oral Epidemiol. 1988;16:61.
TREATMENT
Simple excision is recommended.
CYST OF THE INCISIVE
PAPILLA
Figure 6-77 Additional Reading
Abrams AM, Howell FV, Bullock WK.. Nasopalatine
Age: Middle-aged adults cysts. Oral Surg Oral Med Oral Pathol. 1963;16:306.
Sex: No predilection Brown FH, Houston GD, Lubow RM, Sagan MA.
CLINICAL FEATURES Cyst of the incisive (palatine) papilla. J Periodontol.
1987;58:274.
When epithelial remnants of the nasopala- Small EW. Cysts. Dent Clin North Am. 1971;15:369.
tine duct or incisive canal reside immediately
subjacent to the incisive papilla and undergo
proliferation with cystic change, they are PALATAL ABSCESS
termed cysts of the incisive papilla. They there- Figure 6-78
fore represent the oral soft tissue counter-
part of the incisive canal cyst. The cysts are Age: No predilection
Sex: No predilection
usually small, soft, or fluctuant on palpation
and may develop a draining fistula. CLINICAL FEATURES
Palatal abscess is seen in the premolar-molar
MICROSCOPIC FEATURES region lateral to the midline and is a tense
The cyst lining is stratified squamous epi- yet compressible swelling. It represents
thelium, although on rare occasion, respi- palatally directed drainage of infection of
PMPH_Eversole_Chapter-06.indd 251 1/20/2011 2:40:22 PM
252 Chapter 6
Shapiro HH, Sleeper EL, Guralnick WC. Spread of
infection of dental origin. Oral Surg Oral Med Oral
Pathol. 1950;3:1407.
Wood NK, Goaz PW. Differential Diagnosis of Oral
Lesions. 2nd ed. St Louis, MO: C. V. Mosby; 1980:138,
144.
REACTIVE LESIONS OF
PALATAL GINGIVAL
Figure 6-79
See gingival tumefactions
FIGURE 6-78
Firm palatal swelling adjacent to a carious molar, ADENOMATOUS HYPERPLASIA
representing a subperiosteal abscess of odonto- Figure 6-80
genic infectious origin.
Age: Adults
odontogenic or periodontal origin. A pala- Sex: Male predilection
tal molar root is the most common source. CLINICAL FEATURES
Pain is a frequent finding. A purulent exu-
Occasionally, a sessile mass on either the
date may be aspirated from the swelling.
soft or hard palate, appearing to represent
MICROSCOPIC FEATURES a neoplasm, is found to consist of normal-
appearing mucous acini and accompanying
The palatal abscess is composed of necrotic
ducts. These lesions are soft to palpation
debris, exudate, and infiltration of neutro-
and usually do not exceed 2 cm. They are
phils and histiocytes. The abscess is usually
covered by normal-appearing mucosa and
enveloped by a granulation tissue wall.
may represent a developmental anomaly or
DIFFERENTIAL DIAGNOSIS a focal glandular hyperplasia.
Palatal abscess can be differentiated clini-
cally from salivary neoplasms by noting the MICROSCOPIC FEATURES
presence of pain and identifying an odonto- Lobules of normal-appearing palatal minor
genic infectious source by vitalometer test- mucous acini and associated ductal ele-
ing or a periapical lesion by radiographs. ments lie within the connective tissue under
normal surface epithelium.
TREATMENT
The source of infection must be identified DIFFERENTIAL DIAGNOSIS
and arrested by either extraction or pulpec-
tomy. The abscess may be incised and Benign salivary neoplasms and atypi-
drained to relieve pain. cal lymphoproliferative disease should be
considered in the differential diagnosis. A
palatal abscess can be ruled out by virtue
Additional Reading of location (adenomatous hyperplasia is
Shafer WG, Hine MK, Levy BM. Chap. 8. A Textbook
usually not confluent with palatal gingiva)
of Oral Pathology. 4th ed. Philadelphia, PA: W. B. and absence of an odontogenic source of
Saunders; 1983. infection.
PMPH_Eversole_Chapter-06.indd 252 1/20/2011 2:40:34 PM
Intraoral Soft Tissue Swellings 253
FIGURE 6-79
Fleshy growths represent
pyogenic granulomas.
FIGURE 6-80
Adenomatous hyperpla-
sia at hard-soft palate
junction.
TREATMENT PLEOMORPHIC ADENOMA
Biopsy of masses of this nature should be Figure 6-81
performed to rule out tumor. Once a diag-
nosis of adenomatous or glandular hyper- Age: Middle-aged adults
plasia is made, no further treatment is Sex: Female predilection
required. CLINICAL FEATURES
Pleomorphic adenomas may arise in any of
Additional Reading the major or minor salivary glands. When
intraoral, the palate is the site of predilection.
Arafat A, Brannon RB, Ellis GL. Adenomatoid hyper- The tumor is located lateral to the midline in
plasia of mucous salivary glands. Oral Surg Oral Med
the hard or soft palate, is firm to palpation,
Oral Pathol. 1981;52:51.
Buchner A, Merrell PW, Carpenter WM, Leider AS. and as a rule lacks surface ulceration.
Adenomatoid hyperplasia of minor salivary glands.
Oral Surg Oral Med Oral Pathol. 1991;71:583.
Devildos LR, Langlois CC. Minor salivary gland lesion MICROSCOPIC FEATURES
presenting clinically as tumor. Oral Surg Oral Med Pleomorphic adenoma possesses a circum-
Oral Pathol. 1976;41:657.
Giansanti JS, Baker GO, Waldron CA. Intraoral muci- ferential capsule. The tumor is composed
nous, minor salivary gland lesions, presenting clini- of nests and sheets of cuboidal epithe-
cally as tumors. Oral Surg Oral Med Oral Pathol. lium with ductal formations. Interspersed
1971;32:918. throughout are various mesenchymal tis-
Shimoyama T, Wakabayashi M, Kato T, Kaneko T, Horie
N, Ide F. Adenomatoid hyperplasia of the palate mim-
sues, which include fat, cartilage, and bone.
icking clinically as a salivary gland tumor. J Oral Sci. Myxoid tissue is common and may be
2001;43:135-138. accompanied by proliferation of spindle-
PMPH_Eversole_Chapter-06.indd 253 1/20/2011 2:40:37 PM
254 Chapter 6
FIGURE 6-81
Pleomorphic adenoma located in the lateral hard palate. Ulceration is not often seen.
shaped myoepithelial cells. Histologic vari- Waldron CA, el-Mofty SK, Gnepp DR. Tumors of the
ants are encountered, including those with intraoral minor salivary glands: a demographic and his-
tologic study of 426 cases. Oral Surg Oral Med Oral
“plasmacytoid” hyaline cells and tumors Pathol. 1988;66:323.
with tyrosine crystals.
DIFFERENTIAL DIAGNOSIS
POLYMORPHOUS LOW-GRADE
Pleomorphic adenoma can be differentiated ADENOCARCINOMA
from palatal abscess by failure to locate an
Figure 6-82
infectious source; pain is not a feature. Clin-
ically, it may simulate a malignant salivary Age: Elderly
tumor or a mesenchymal neoplasm; the lat- Sex: Female predilection
ter is relatively uncommon in this location.
CLINICAL FEATURES
TREATMENT As with most minor salivary tumors of the
oral cavity, the palate is the favored site for
Because tumor islands may actually per-
polymorphous low-grade adenocarcinoma,
forate the capsule, simple enucleation may
the most common of the minor salivary
result in recurrence. Excision of the tumor
gland malignancies. Tumors also frequently
and adjacent tissue is recommended. In
arise in the buccal mucosa and are less
the hard palate, the capsule may fuse with
commonly seen in the retromolar region,
periosteum, necessitating subperiosteal dis-
lips, and base of the tongue. The typical
section with excision.
lesion of the palate is asymptomatic, fixed
and firm without ulceration, arising off the
Additional Reading midline. Surface ulceration or telangiectasia
are not commonly seen with this low-grade
Chaudhry AP, Vickers RA, Gorlin RJ. Intraoral minor malignancy.
salivary gland tumors; analysis of 1,414 cases. Oral
Surg Oral Med Oral Pathol. 1961;14:1194.
Daniels JS, Ali I, Al Bakri IM, Sumangala B. Pleomorphic MICROSCOPIC FEATURES
adenoma of the palate in children and adolescents: a
report of 2 cases and review of the literature. J Oral The polymorphous low-grade adenocarci-
Maxillofac Surg. 2007;65:541-549. noma manifests two distinct microscopic
Fine G, Marshall RB, Horn RC. Tumors of the minor patterns: infiltrating cords and lobular
salivary gland. Cancer. 1960;13:653.
Naeim F, Forsberg MI, Waisman J, Coulson WF. Mixed
islands. In all tumors, the cells possess rela-
tumors of the salivary glands. Arch Pathol Lab Med. tively monomorphic oval or prolate nuclei
1976;100:271. without significant hyperchromatism. The
PMPH_Eversole_Chapter-06.indd 254 1/20/2011 2:41:07 PM
Intraoral Soft Tissue Swellings 255
FIGURE 6-82
Submucosal mass at hard-soft palate junction representing polymorphous low-grade adenocarcinoma.
lobular formations usually occupy the cen-
tral region of the tumor (the term lobular car- Additional Reading
cinoma has been applied to this lesion) and Evans HL, Batsakis JG. Polymorphous low-grade
may exhibit cribriform foci. The peripheral adenocarcinoma of minor salivary glands. Cancer.
aspects comprise tubular, duct-like cords of 1984;53:935.
cells with some tendency for streaming and Freedman PD, Lummerman H. Lobular carcinoma of
intraoral minor salivary gland origin. Oral Surg Oral
spindling of nuclei. The tumor is well cir- Med Oral Pathol. 1983;56:157.
cumscribed yet nonencapsulated. A some- Gnepp DR, Chen JC, Warren C. Polymorphous low-
what distinctive immunohistochemical grade adenocarcinoma of minor salivary gland origin:
staining pattern is identifiable, cells being an immunohistochemical and clinicopathologic study.
Am J Surg Pathol. 1988;12:461.
S-100 protein positive with weak actin Regezi JA., Zarbo RJ, Stewart JC, Courtney RM.
labeling. Polymorphous low grade adenocarcinoma of minor
salivary gland. A comparative histologic and immuno-
histochemical study. Oral Surg Oral Med Oral Pathol.
DIFFERENTIAL DIAGNOSIS 1991;71:469.
As with all palatal masses, palatal abscess Seethala RR, Johnson JT, Barnes EL, Myers EN.
Polymorphous low-grade adenocarcinoma: the
and other salivary tumors should be con- University of Pittsburgh experience. Arch Otolaryngol
sidered in the clinical differential diagnosis. Head Neck Surg. 2010;136:385-392.
Biopsy is required to arrive at a definitive
diagnosis, and the histologic characteristics
may be confused with those of adenoid cys- MISCELLANEOUS
tic carcinoma. ADENOCARCINOMAS
Figure 6-83
TREATMENT
Age: Adults
Wide local excision is the treatment of Sex: No predilection
choice, and local recurrence varies from
CLINICAL FEATURES
10% to 15%. Metastasis is uncommon;
when it occurs, spread is generally to A variety of salivary tumors occur in the oral
regional lymph nodes in the neck. Long- cavity that are rare or uncommon compared
term follow-up is advisable; recurrences to the other more commonly encountered
have been known to occur 10 years post- forms of adenocarcinoma. These variants are
operatively. malignancies that differ from one another in
PMPH_Eversole_Chapter-06.indd 255 1/20/2011 2:41:20 PM
256 Chapter 6
FIGURE 6-83
Miscellaneous rare ade-
nomas (left) and adeno-
carcinomas (right) also
tend to arise in the palatal
glands.
terms of metastatic potential, local aggres- some may metastasize, neck node clinical
siveness, and prognosis. Lower-grade tumors and magnetic resonance imaging evalu-
include cystadenocarcinoma, papillary cys- ation should be performed. High-grade
tadenocarcinoma, epithelial/myoepithelial tumors require surgical resection with neck
carcinoma of intercalated ducts, clear cell car- dissection when positive nodes are pres-
cinoma, minor gland acinic cell carcinoma, ent and some respond to adjunct radiation
and basal cell adenocarcinoma. High-grade and/or chemotherapy. Since some of these
tumors include salivary duct carcinoma, tumors are capable of distant metastases, a
squamous cell carcinoma of salivary origin, chest film should be ordered.
mucinous carcinoma, invasive carcinoma ex
mixed tumor, and anaplastic small and large
cell carcinomas. Most of these variants are
Additional Reading
more often seen in the major glands. Barthel JH, Gamble JW. Acinic cell carcinoma of the pal-
ate: report of case and review of the literature. J Oral
MICROSCOPIC FEATURES Surg. 1979;37:819-821.
Buchner A, Merrell PW, Carpenter WM. Relative fre-
Each specific variety of salivary carcinomas quency of intra-oral minor salivary gland tumors: a
exhibit unique, characteristic, and diagnos- study of 380 cases from northern California and com-
parison to reports from other parts of the world. J Oral
tic features. Outlining the microscopy for Pathol Med. 2007;36:207-214.
each of these lesions is beyond the scope of de Sousa SO, Schwarzschild M, de Araújo NS, de Araújo
this clinical atlas. Suffice it to say that these VC. Basal cell adenocarcinoma of the palate with
tumors, with exception of squamous cell squamous metaplasia. J Clin Pathol. 2000;53:153-156.
Foss RD, Ellis GL, Auclair PL. Salivary gland cystadeno-
carcinoma and the anaplastic lesions, show
carcinomas. A clinicopathologic study of 57 cases. Am
various patterns with salivary ductal and J Surg Pathol. 1996;20:1440-1447.
acinar cell types. Ponniah I, Murali GM, SureshKumar P, Kumaran MG,
Shaheen A. Salivary duct carcinoma of the palate.
Indian J Dent Res. 2005;16:167-170.
DIFFERENTIAL DIAGNOSIS
The rare adenocarcinoma variants clini-
cally resemble other salivary neoplasms ADENOID CYSTIC
being submucosal nodules in the palate CARCINOMA
or other oral sites where minor salivary Figure 6-84
glands occur. Some are ulcerated. Biopsy is
required to arrive at a definitive diagnosis. Age: Middle-aged adults
Sex: No predilection
TREATMENT CLINICAL FEATURES
The low-grade tumors are treated by surgi- Adenoid cystic carcinoma or cylindroma
cal excision with wide margins and because is a common intraoral malignant salivary
PMPH_Eversole_Chapter-06.indd 256 1/20/2011 2:41:35 PM
Intraoral Soft Tissue Swellings 257
neoplasm and is most often seen in the
hard palate. It appears as an indurated
swelling lateral to the midline and fre-
quently shows ulceration or surface telang-
iectasia. Pain is not uncommon. Despite
this malignant behavior, it may show a
lengthy growth progression. Metastasis is
common late in the course of the disease
and may not be detected for many years
after initial therapy. It has an equal ten-
dency for both regional and hematogenous
spread.
MICROSCOPIC FEATURES
The tumor lacks encapsulation and tends
to invade adjacent hard and soft tissues.
Tumor cells characteristically invade
perineural lymphatics and may progress
for extended distances along nerve sheaths.
The classic pattern shows hyperchromatic,
monomorphic cuboidal cells arranged in
islands forming multicystic cribriform pat-
terns resembling Swiss cheese. The cystic
lumina often contain a basophilic hyaline FIGURE 6-84
Adenoid cystic carcinoma with tumefaction show-
substance, and the stroma may display
ing surface ulceration.
eosinophilic hyalinization. When solid
basaloid islands predominate, the tumor
has a worse prognosis. and distant metastases become detectable.
The 5-year survival for palatal lesions is
DIFFERENTIAL DIAGNOSIS less than 35%; 10-year survival rate drops to
about 15%.
Cylindroma may be clinically identical to
other benign or malignant salivary tumors,
sarcomas, or antral carcinoma with palatal Additional Reading
invasion.
Carlinfante G, Lazzaretti M, Ferrari S, Bianchi B, Crafa
P. P53, bcl-2 and Ki-67 expression in adenoid cystic
TREATMENT carcinoma of the palate. A clinico-pathologic study of
21 cases with long-term follow-up. Pathol Res Pract.
Wide excision with partial maxillectomy 2005;200:791-799.
is necessary. Neck dissection is indicated Conley J, Dingman DL. Adenoid cystic carcinoma in the
when nodes are palpable. When they are head and neck. Arch Otolaryngol Head Neck Surg.
1974;100:81.
not palpable, node dissection may not be Eneroth CM, Hjertman L, Moberger G. Adenoid cystic
warranted as the tumor has great ten- carcinoma of palate. Acta Otolaryngol. 1968;66:248.
dency to spread to distant sites. All patients Spiro RH, Huvos A, Jr, Strong EW. Adenoid cystic car-
with cylindroma should be evaluated with cinoma of salivary origin; a clinicopathologic study of
242 cases. Am J Surg. 1974;128:512.
radiographs of the chest. Adenoid cystic Tarpley TM, Giansanti JS. Adenoid cystic carcinoma;
carcinoma pursues a slow rate of growth, analysis of fifty oral cases. Oral Surg Oral Med Oral
and many years elapse before recurrence Pathol. 1976;41:484.
PMPH_Eversole_Chapter-06.indd 257 1/20/2011 2:41:39 PM
258 Chapter 6
MUCOEPIDERMOID moid cells predominate, the prognosis is
CARCINOMA worse and the tumor is classified as high
Figure 6-85 grade. Low-grade tumors are cystic with a
preponderance of mucous and columnar
Age: Young and middle-aged adults cells.
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
Palatal abscess, other benign and malignant
When minor glands give rise to mucoepi-
salivary tumors, antral cancer, and mesen-
dermoid carcinoma, the palate is the most
chymal neoplasms are clinically similar
frequent location. The tumor may be cys-
in appearance to palatal mucoepidermoid
tic or indurated to palpation and usually
carcinoma.
fails to show ulceration. Telangiectasia is
frequently noted. The growth rate is often
TREATMENT
slow, and behavior is correlated with his-
tologic grade of malignancy. Despite gra- Low-grade tumors can be treated success-
dations, all mucoepidermoid carcinomas fully by wide local excision, making sure
have metastatic potential. Recent studies margins are free of tumor microscopically.
appear to indicate that low-grade tumors in High-grade lesions require more radical
the oral cavity do not metastasize; however, surgery. Maxillectomy is recommended for
this theory has not been completely docu- palatal tumors. Chest radiographs should
mented. The higher grade tumors spread by be obtained to rule out lung metastasis.
way of lymphatics; however, hematogenous
metastasis often occurs in addition to, or in
lieu of, nodal metastasis.
Additional Reading
Caccamese JF, Jr, Ord RA. Paediatric mucoepidermoid
MICROSCOPIC FEATURES carcinoma of the palate. Int J Oral Maxillofac Surg.
2002;31:136-139.
Tumor islands may be solid or may show Eversole LR, Rovin S, Sabes WR. Mucoepidermoid car-
large, dilated cystic formations. A capsule cinoma of minor salivary glands: report of 17 cases with
is lacking. The individual tumor cells show follow-up. J Oral Maxillofac Surg. 1972;30:107.
Melrose RJ, Abrams AM, Howell FW. Mucoepidermoid
a biphasic differentiation with both an epi- tumors of the intraoral minor salivary glands: a clini-
dermoid and a mucous cell component. copathologic study of 54 cases. J Oral Pathol Med.
When the tumor is less cystic and epider- 1973;2:314.
FIGURE 6-85
Sessile palatal masses rep-
resenting mucoepidermoid
carcinoma.
PMPH_Eversole_Chapter-06.indd 258 1/20/2011 2:42:00 PM
Intraoral Soft Tissue Swellings 259
Spiro RH, Huvos AG, Berk R, Strong EW. showing ductal formations. Some are mon-
Mucoepidermoid carcinoma of salivary gland origin; omorphic whereas others evince anaplasia
a clinicopathologic study of 367 cases. Am J Surg.
1978;136:461. and pleomorphism. Rarely, a benign pleo-
Spiro RH, Koss LG, Hajdu SI, Strong EW. Tumors of morphic adenoma undergoes adenocarci-
minor salivary origin; a clinicopathologic study of 492 nomatous transformation; these lesions are
cases. Cancer. 1973;31:117. referred to as carcinoma ex mixed tumor.
DIFFERENTIAL DIAGNOSIS
ADENOCARCINOMA, NOS
Figure 6-86 Adenocarcinomas clinically resemble other
salivary neoplasms, mesenchymal tumors,
Age: Middle-aged adults antral carcinoma, or a palatal abscess.
Sex: No predilection
CLINICAL FEATURES TREATMENT
Adenocarcinomas, not otherwise speci- Wide surgical excision with resection of
fied (NOS), are malignant salivary gland underlying bone is recommended. Radio-
tumors; they do not show microscopic graphs of the chest should be obtained to
features that allow specific classification rule out metastasis to lungs.
into one of the recognized salivary tumor
taxonomic categories. They appear as indu-
rated, often ulcerated swellings lateral to the Additional Reading
midline. Surface telangiectasia is common. Allen MS, Fitz-hugh GS, Marsh WL. Low-grade papillary
These tumors behave aggressively and may adenocarcinoma of the palate. Cancer. 1974;33:153.
metastasize regionally or distantly. Their Koss LG, Spiro RH, Hajdu S. Small cell (oat cell) car-
cinoma of minor salivary gland origin. Cancer.
behavior is similar to that of adenoid cystic
1972;30:737.
carcinoma. Livolsi VA, Perzin KH. Malignant mixed tumors aris-
ing in salivary glands. I. Carcinomas arising in benign
MICROSCOPIC FEATURES mixed tumors. A clinicopathologic study. Cancer.
1977;39:2209.
There is no capsule. Tumor cells show inva- Spiro RH, Koss LG, Hajdu SI, Strong EW. Tumors of
sion and are arranged in sheets and cords minor salivary origin; a clinicopathologic study of 492
cases. Cancer. 1973;31:117.
ATYPICAL
LYMPHOPROLIFERATIVE
DISEASE
Figure 6-87
Age: Elderly adults
Sex: No predilection
CLINICAL FEATURES
Lymphoid infiltration of salivary glands is
generally a feature of autoimmune sialad-
FIGURE 6-86
Adenocarcinoma NOS (not otherwise specified. enitis such as Sjögren’s syndrome or Miku-
This heterogeneous group of tumors fail to show licz’s disease, when the major salivary
microscopic features that would place them in a glands are involved. When the palatal sali-
specific category. vary glands manifest diffuse lymphoid
PMPH_Eversole_Chapter-06.indd 259 1/20/2011 2:42:09 PM
260 Chapter 6
FIGURE 6-87
Diffuse soft swelling of hard palate representing lymphoproliferative disease. Most are low-grade non-
Hodgkin’s lymphomas.
infiltration, however, the disease process in nant lymphoma will eventually develop,
most instances represents non-Hodgkin’s given sufficient time. Non-Hodgkin’s lym-
lymphoma. Atypical lymphoproliferative phomas among AIDS patients are rare in
disease of the palate is a unique entity the oral cavity, yet when they arise, the pal-
because the microscopic features often sug- ate and gingiva are the favored sites.
gest a benign lesion. The disease is charac-
terized by diffuse soft tissue enlargement
MICROSCOPIC FEATURES
located unilaterally in the hard palate.
Occasionally, the lesion extends into the The palatal salivary glands are infiltrated
soft palate area and may cross the midline by lymphocytes that may be monomorphic
with bilateral swelling. The lesion is soft or and well differentiated or mildly pleomor-
spongy on palpation, and the mucosa either phic and poorly differentiated. Interspersed
maintains normal coloration or manifests a thread-like basophilic strands with a ten-
bluish hue without evidence of ulceration dency for compaction are common and
or telangiectasia. Accompanying cervical probably represent degenerating lympho-
lymphadenopathy is generally not noted cytes. Reed-Sternberg cells are not encoun-
at the time of diagnosis. Once the diagno- tered. The overall pattern of the infiltrate
sis is secured, work-up for malignant lym- may be diffuse or nodular. The salivary
phoma is mandatory. Many patients show tissue shows acinar replacement; however,
evidence of lymphoma in other locations at ducts are often intact, embedded in a sea
the time that the palatal mass is detected; of lymphocytes. These residual ducts often
others may be free from disease in other show pronounced periductal hyalinization.
sites yet develop generalized lymphoma at Epimyoepithelial islands encountered in
a later date. In still other patients, the lesion benign lymphoepithelial lesions are rarely
remains static and progression to dissemi- encountered in lymphoproliferative disease
nated disease does not ensue, suggesting of the palate. Mucosa-associated lymphatic
the palatal mass may represent pseudolym- tissue (MALT) lymphomas show features
phoma. Insufficient long-term follow-up similar to autoimmune sialadenitis, yet the
information exists in this latter group of malignant lymphoid cells are monoclonal
patients to determine whether or not malig- plasmacytoid and monocytoid in appear-
PMPH_Eversole_Chapter-06.indd 260 1/20/2011 2:42:11 PM
Intraoral Soft Tissue Swellings 261
ance. Classic extranodal non-Hodgkin’s follow-up and reexamination semiannually
lymphomas are also encountered in the in anticipation of probable dissemination of
palate. Cell surface proteins termed CD disease. The palatal lesion has been shown
antigens are present in specific types of to respond favorably to radiation therapy; 8
lymphomas and can be identified with IHC to 10 Gy is generally adequate to cause reso-
stains. The chief ones are CD3 for T cells, lution. This treatment alone may not neces-
CD20 for B cells and CD 56 for natural killer sarily prevent the occurrence of lesions in
cells. AIDS-related lymphomas are clearly other anatomic sites. Other bona fide lym-
malignant histologically, being represented phomas are treated with chemotherapeutic
by large lymphoblasts. Plasmablastic lym- agents specific to a given histologic type
phoma is AIDS specific in the oral cavity combined with radiation therapy.
and resembles myeloma histologically.
DIFFERENTIAL DIAGNOSIS Additional Reading
A soft, spongy swelling of the hard palate Block P, van Delden L, van der Waal I. Non-Hodgkin’s
that is diffuse and sessile should arouse lymphoma of the hard palate. J Oral Maxillofac Surg.
suspicion of atypical lymphoprolifera- 1979;47:445.
tive disease, especially in elderly patients. Guggisberg K, Jordan RC. Mantle cell lymphoma of
the oral cavity: case series and comprehensive review
Malignant salivary neoplasms are gener- of the literature. Oral Surg Oral Med Oral Pathol
ally localized and indurated. Pleomorphic Oral Radiol Endod. 2010;109:98-104. [Epub 2009
adenoma and palatal abscess have clinical Oct 31.]
features in common with lymphoprolifera- Kaugars GE, Burns JC. Non-Hodgkin’s lymphoma of the
oral cavity associated with AIDS. Oral Surg Oral Med
tive disease; palatal abscess can be elimi- Oral Pathol. 1989;67:433.
nated from consideration when an infec- McNelis FL, Pai VT. Malignant lymphoma of the head
tious source is lacking. and neck. Laryngoscope. 1969;79:1076.
Tomich CE, Shafer WG. Lymphoproliferative disease of
TREATMENT the hard palate: A clinicopathologic entity. Oral Surg
Oral Med Oral Pathol. 1975;39:754.
Once a diagnosis of atypical lymphopro-
liferative disease is established, the patient
should be referred for complete evalu- SQUAMOUS CELL
ation to uncover evidence of malignant CARCINOMA
lymphoma in other reticuloendothelial Figure 6-88
tissues. Should the results prove negative,
the patient should be subjected to periodic See other locations in this chapter.
FIGURE 6-88
Palatal squamous cell car-
cinomas are uncommon.
PMPH_Eversole_Chapter-06.indd 261 1/20/2011 2:42:23 PM
262 Chapter 6
FIGURE 6-89
Carcinoma of the antral mucosa invading the antral floor and producing a palatal swelling with ulceration.
CARCINOMA OF THE ANTRUM DIFFERENTIAL DIAGNOSIS
Figure 6-89 Antral carcinoma resembles the other
malignant palatal swellings included here,
Age: Elderly adults necessitating biopsy with microscopic con-
Sex: Male predilection firmation. Sinus radiographs are of diag-
CLINICAL FEATURES nostic importance, and tomograms or com-
Cancer arising in the antrum generally puted tomographic scans help to determine
becomes advanced before signs or symp- the extent of the disease.
toms occur. The tumor may erode any of
TREATMENT
the antral bony walls including the orbital
floor, the lateral or medial wall, or often the Radiation therapy to the antrum and neck
palate. When the palate becomes eroded, may be coupled with maxillectomy. When
a mass protrudes and is invariably ulcer- nodes contain tumor, any treatment should
ated. A perforation or oroantral fistula is be considered palliative, as cures at this
frequently encountered. Toothache, max- stage are almost nonexistent.
illary division paresthesia, nasal obstruc-
tion, and loosening of teeth are common
clinical symptoms. Radiographically, antral Additional Reading
clouding and evidence of osseous erosion
Ahmad K, Cordoba RB, Fayos JV. Squamous cell carci-
can be demonstrated on Water’s views or noma of the maxillary sinus. Arch Otolaryngol Head
laminography. Neck Surg. 1981;107:48.
Chaudhry AP, Gorlin RJ, Mosser DG. Carcinoma of the
MICROSCOPIC FEATURES antrum. Oral Surg Oral Med Oral Pathol. 1960;13:269.
Kadish SP, Goodman ML, Wang CC. Treatment of
Antral cancer is either typical squamous minor salivary gland malignancies of the upper food
cell carcinoma or demonstrates glandu- and air passage epithelium. A review of 87 cases.
Cancer. 1972;29:1021.
lar differentiation as an adenocarcinoma. Larsson LG, Martensson G. Carcinoma of the para-
Occasionally, one of the salivary tumors nasal sinuses and the nasal cavities. Acta Radiol.
arises from antral submucosal glands. 1954;42:149.
PMPH_Eversole_Chapter-06.indd 262 1/20/2011 2:42:27 PM
PMPH_Eversole_Chapter-06.indd 263 1/20/2011 2:42:37 PM
a b c
Focal papillary proliferation Focal verrucous lesion Focal imbilicated lesion
d e
Diffuse papillary lesion Multifocal papillary lesion
f g
Diffuse verrucous lesion Papular of multiple polypoid lesion
Papillary, Papular, and Multiple Polypoid Lesions
PMPH_Eversole_Chapter-07.indd 264 1/20/2011 2:49:41 PM
Papillary, Papular,
and Multiple
Polypoid Lesions
7
PAPILLARY SQUAMOUS CELL
Focal Papillary Lesions 267 CARCINOMA 281
PAPILLOMA 267
VERRUCA VULGARIS 268 Diffuse Papular and
CONDYLOMA ACUMINATUM 269 Polypoid Lesions 282
VERRUCIFORM XANTHOMA 270 PAPILLARY HYPERPLASIA 282
SIALADENOMA PAPILLIFERUM 271 STOMATITIS NICOTINA 283
GIANT CELL FIBROMA 272 ACUTE LYMPHONODULAR
SQUAMOUS ACANTHOMA 273 PHARYNGITIS 284
KERATOSIS FOLLICULARIS 284
Focal and Umbilicated FOCAL EPITHELIAL HYPERPLASIA
(HECK’S DISEASE) 285
Papules 273
MULTIPLE HAMARTOMA
KERATOACANTHOMA 273 (COWDEN) SYNDROME 286
WARTY DYSKERATOMA 274 PYOSTOMATITIS VEGETANS 287
MOLLUSCUM CONTAGIOSUM 275 CROHN’S DISEASE 288
SPECIFIC GRANULOMATOUS
INFECTIONS 289
Diffuse and Multifocal AMYLOIDOSIS 290
Papillary Lesions 276
HYALINOSIS CUTIS ET MUCOSAE
CONDYLOMA ACUMINATUM* (LIPOID PROTEINOSIS) 291
FOCAL DERMAL HYPOPLASIA HEMANGIOMA/LYMPHANGIOMA 292
(GOLTZ SYNDROME) 276 MULTIPLE ENDOCRINE
NEVUS UNIUS LATERIS 277 NEOPLASIA, TYPE IIB 293
DENTAL LAMINA CYSTS 294
ACANTHOSIS NIGRICANS 278
ATYPICAL VERRUCOUS
LEUKOPLAKIA 278 *For Condyloma, see Focal Papillary
VERRUCOUS CARCINOMA 280 Lesions
PMPH_Eversole_Chapter-07.indd 265 1/20/2011 2:49:42 PM
Papillary lesions represent swellings with diseases of oral mucosa, some, particularly
finger-like projections imparting a cauli- diffuse papular and polypoid lesions, rep-
flower appearance; these microprojections resent oral markers of a systemic disor-
are rounded and blunt like the fungiform der. Biopsy is usually indicated to secure a
papillae of the tongue. Verrucous lesions definitive diagnosis; because some of these
are similar, yet possess a more irregular lesions herald the presence of an internal
surface. Indeed, differentiation between illness, the pathologist should be provided
papillary and verrucous lesions is based with data from the medical history.
more on microscopic features rather than Papilloma and giant cell fibroma are
on the clinical appearance. Umbilicated the most common focal papillary lesions.
nodules are oval dome-shaped lesions with All lesions listed as focal umbilicated pap-
rolled margins and a central pit, which may ules, extremely rare in the oral cavity, are
be plugged with keratin. Papules are small, more frequently encountered on skin.
usually less than 0.5 cm, elevations that tend Most of the diseases included as dif-
to occur in multiples or in crops. Polypoid fuse and multifocal papillary lesions are
lesions are similar in appearance to pap- rare with condyloma acuminatum or vene-
ules; however, they usually exceed 1.0 cm real wart being the exception. Such lesions
and, in the mouth, tend to be multifocal. are noted frequently in homosexual males.
Most of the lesions discussed in this Papillary hyperplasia, also termed
chapter represent proliferations of the sur- denture papillomatosis, is the most common
face epithelium. Alternatively, some are the entity observed as a diffuse papular lesion;
result of pathologic changes occurring in the stomatitis nicotina is also fairly common.
lamina propria with secondary elevation of Most of the other diseases in this group
the epithelium. Although most papillary are rare and are associated with either cuta-
and focal umbilicated lesions are primary neous or internal organ involvement.
PMPH_Eversole_Chapter-07.indd 266 1/20/2011 2:49:43 PM
Papillary, Papular, and Multiple Polypoid Lesions 267
MICROSCOPIC FEATURES
Focal Papillary Lesions The epithelium shows a thickened parakera-
PAPILLOMA tin layer and a papillary corrugated pattern.
The epithelial projections are supported by
Figure 7-1
fibrovascular cores, and inflammatory cells
Age: Young adults may be discernible.
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES A focal papilloma, by virtue of its papillary
Oral squamous papillomas are either cauliflower surface, is readily recognized.
pedunculated or sessile, show a cauliflower Larger lesions must be differentiated from
surface with finger-like projections, and verrucous carcinoma. On the lips, papilloma
may be white and keratotic or normal in may be indistinguishable from verruca vul-
color. These small epithelial neoplasms are garis. Multiple confluent papillomas must be
most often encountered on the palate, uvula, differentiated from condyloma acuminatum.
tongue, and lip; they tend to reach a certain
TREATMENT
size, after which the growth essentially
becomes arrested. Papillomavirus types 6 Simple excision is recommended. Recur-
and 11 are identifiable in some, yet not all, rence is extremely rare.
common squamous papillomas. A variant
form of papilloma, juvenile spongiotic hyper-
plasia, is found in children on the gingival Additional Reading
and presents with a brightly erythematous Abby LM, Page DG, Sawyer DR. The clinical and his-
papillary appearance. topathologic features of a series of 464 oral squamous
FIGURE 7-1
Squamous papillomas show-
ing a papillary cauliflower-like
surface. Juvenile spongiotic
hyperplasia is papillomatous
(lower right).
PMPH_Eversole_Chapter-07.indd 267 1/20/2011 2:49:43 PM
268 Chapter 7
cell papillomas. Oral Surg Oral Med Oral Pathol. verruca; yet viral genomes of these types
1980;49:419. are rarely seen in intraoral examples.
Eversole LR, Laipis PJ. Oral squamous papillomas:
detection of HPV DNA by in situ hybridization. Oral
Surg Oral Med Oral Pathol. 1988;65:545. MICROSCOPIC FEATURES
Greer RO, Goldman HM. Oral papillomas.
The epithelium possesses surface projec-
Clinicopathologic evaluation and retrospective exami-
nation for dyskeratosis in 110 lesions. Oral Surg Oral tions superficial to the normal tissue sur-
Med Oral Pathol. 1974;38:435. face and showing no invagination. The
Syrjänen S. Current concepts on human papillomavirus projections are acute, pointed angles rather
infections in children. APMIS. 2010;118:494-509. than bulbous or rounded, as with papillo-
Syrjänen K, Happonen R-P, Syrjanen S, Calonius B.
Human papilloma virus (HPV) antigens and local mas. Thickened keratin is a feature. Viral
immunologic reactivity in oral squamous cell tumors inclusion bodies are usually discernible in
and hyperplasias. Scand J Dent Res. 1984;92:358. the upper spinous layer.
DIFFERENTIAL DIAGNOSIS
VERRUCA VULGARIS
Verruca vulgaris is distinctive on vermil-
Figure 7-2
ion border or skin, yet intraorally, it may be
Age: Children and young adults clinically identical to papilloma.
Sex: No predilection
TREATMENT
CLINICAL FEATURES
Simple local excision is recommended.
Verruca vulgaris, the common wart, is a
virus-induced neoplasm of the skin caused
by human papillomavirus. It may be seen
on the vermilion border; lesions showing
Additional Reading
microscopic features indistinguishable Adler-Storthz K, Newland JR, Tessin BA, Yeudall WA,
from those of skin verrucae have been iden- Shillitoe EJ. Identification of human papillomavi-
rus types in oral verruca vulgaris. J Oral Pathol Med.
tified in the mouth. The lesion is white, with 1986;15:230.
a keratotic surface and a well-delineated Clausen FP. Rare oral viral disorders (molluscum con-
border. A stalk is not discernible. The pap- tagiosum, localized keratoacanthoma, verrucae, con-
illary excrescences are composed of finger- dyloma acuminatum, and focal epithelial hyperplasia).
Oral Surg Oral Med Oral Pathol. 1972;34:604.
like projections with a sharply angulated Eversole LR, Laipis PJ, Green TL. Human papilloma-
surface. Human papillomavirus types 2 virus type 2 DNA in oral and labial verruca vulgaris.
and 4 are consistently identifiable in labial J Cutan Pathol. 1987;14:319.
FIGURE 7-2
Verruca vulgaris, rarely
occurring on oral mucosa
yet not particularly uncom-
mon on the lip. The lesion is
raised with a verrucous sur-
face, which is white due to
hyperkeratosis.
PMPH_Eversole_Chapter-07.indd 268 1/20/2011 2:49:55 PM
Papillary, Papular, and Multiple Polypoid Lesions 269
Green TL, Eversole LR, Leider AS. Oral and labial tendency for multiplicity with clustering.
verruca vulgaris. Oral Surg Oral Med Oral Pathol. A history of sexual contact as a source of
1986;62:410.
Sivapathasundharam B, Shifa S. Oral verruca vulgaris: transmission can usually be obtained, and
report of a rare case. Indian J Dent Res. 2004;15: lesions are most often encountered among
32-34. prison inmates and homosexual males.
More than 85% of oral condylomata harbor
human papillomavirus types 6, 11, or both.
CONDYLOMA ACUMINATUM HIV-seropositive homosexual males are
Figure 7-3 commonly affected and their lesions may
harbor genotypes not ordinarily associated
Age: Adults with venereal warts (e.g., type 7).
Sex: No predilection
CLINICAL FEATURES MICROSCOPIC FEATURES
Condyloma acuminatum is a verrucous Surface-stratified squamous epithelium
papillary lesion caused by human papil- displays a papillary pattern with rounded
lomavirus types 6 and 11. The lesions are finger-like projections. A prominent par-
generally confined to the anogenital inter- akeratin layer is present, and acanthosis
triginous regions. They are autoinoculable is striking. Numerous mitotic figures can
and may also be transmitted as a vene- be encountered in the basal and parabasi-
real disease, accounting for the term vene- lar strata. Viral inclusion bodies are usu-
real warts. Oral condylomata are similar in ally discernible in the upper spinous layer.
appearance to anogenital condylomata. The The subjacent fibrous connective tissue is
resemblance to the common oral papilloma traversed by dilated vascular channels.
is striking; however, condyloma tends to HPV DNA can be demonstrated by in situ
appear more racemose and also shows a hybridization.
FIGURE 7-3
Condyloma acuminatum.
Large and multifocal cauli-
flower appearance.
PMPH_Eversole_Chapter-07.indd 269 1/20/2011 2:50:08 PM
270 Chapter 7
DIFFERENTIAL DIAGNOSIS Praetorius-Clausen F. Rare oral viral disorders (molluscum
contagiosum, localized keratoacanthoma, verrucae,
Condyloma acuminatum is most often con- condyloma acuminatum, and focal epithelial hyperpla-
fused with the common squamous papil- sia). Oral Surg Oral Med Oral Pathol. 1972;34:604.
loma. Differentiation can usually be made
clinically by a history of sexual transmis-
sion. Multiplicity with clustering of lesions VERRUCIFORM XANTHOMA
is also a feature in favor of a diagnosis of Figure 7-4
condyloma. In florid papillomatoses, the
entire oral cavity is involved; in the Goltz Age: Adults
syndrome, the dermal manifestations are Sex: Female predilection
characteristic. CLINICAL FEATURES
Verruciform xanthoma is most often encoun-
TREATMENT
tered on the alveolar ridge and buccal mucosa
Biopsy is necessary to obtain a definitive yet has also been reported in extraoral
diagnosis. Once the diagnosis is secured, mucosal sites. It is keratotic yet may show a
excision or cryotherapy with cotton appli- normal-colored pebbly surface. The lesion is
cators soaked in liquid nitrogen effectively well circumscribed, may be pedunculated,
removes the lesions. Recurrence is common, but more often is sessile and is less than 1.5
and the lesions are contagious. cm in diameter. There is no known relation-
ship between the occurrence of this lesion and
Additional Reading irritation, tobacco habits, or hyperlipidemia.
Eversole LR. Papillary lesions of the oral cavity: relation- MICROSCOPIC FEATURES
ship to human papillomaviruses. J Calif Dent Assoc.
2000;28:922-927. The surface epithelium is hypercornified
Eversole LR, Laipis PJ, Merrell P, Choi E. Demonstration and corrugated with small surface projec-
of human papillomavirus DNA in oral condyloma tions. The submucosal papillae extending
acuminatum. J Oral Pathol Med. 1987;16:266. between elongated rete ridges are diffusely
Greenspan D, de Villiers EM, Greenspan JS, de Souza
YG, zur Hausen H. Unusual HPV types in oral warts infiltrated with foam cell histiocytes.
in association with HIV infection. J Oral Pathol Med.
1988;17:482. DIFFERENTIAL DIAGNOSIS
Kui LL, Xiu HZ, Ning LY. Condyloma acuminatum and
human papilloma virus infection in the oral mucosa of Clinically, verruciform xanthoma cannot be
children. Pediatr Dent. 2003;25:149-153. distinguished from verruciform hyperkera-
FIGURE 7-4
Verruciform xanthoma. Flat,
sessile papillary lesions.
PMPH_Eversole_Chapter-07.indd 270 1/20/2011 2:50:17 PM
Papillary, Papular, and Multiple Polypoid Lesions 271
tosis. The lesion must also be differentiated face mucosa when origin is from oral minor
from verrucous carcinoma; however, age glands. Clinically, the lesion represents a
differences are helpful in this case. A sessile well-localized sessile or pedunculated pap-
papilloma may be grossly identical. illary growth, usually located on the hard
palate. This tumor has also been observed
TREATMENT to arise from the parotid gland and buccal
Verruciform xanthoma can be locally mucosa minor glands. Because the prolif-
excised. There is no known relationship eration extends down into the gland, the
between this type of xanthoma and the underlying base of the lesion is usually firm
hyperlipoproteinemias. or indurated.
MICROSCOPIC FEATURES
Additional Reading The papillary surface is usually represented
Miller AS, Elzay RP. Verruciform xanthoma of the gin- by stratified squamous epithelium. These
giva: report of six cases. J Periodontol. 1973;44:103. papillary folds extend into the deeper tis-
Neville B. The verruciform xanthoma. A review and sues undermining the surface. In this loca-
report of eight new cases. Am J Dermatopathol. tion, cystic channels are witnessed and the
1986;8:247.
Nowparast B, Howell FV, Rick GM. Verruciform xantho-
papillary projections protruding into the
ma. A clinicopathologic review and report of fifty-four lumina are lined by ductal pseudostratified
cases. Oral Surg Oral Med Oral Pathol. 1981;51:619. columnar epithelium. The individual cells
Philipsen HP, Reichart PA, Takata T, Ogawa I. are oncocytic with foci of mucous meta-
Verruciform xanthoma—biological profile of 282 oral
plasia. The base of the tumor lies directly
lesions based on a literature survey with nine new cas-
es from Japan. Oral Oncol. 2003;39:325-336. over normal-appearing acinar tissue. There
Shafer WG. Verruciform xanthoma. Oral Surg Oral Med are sporadic reports describing dysplastic
Oral Pathol. 1971;31:784. changes in the ductal components of the
tumor.
SIALADENOMA PAPILLIFERUM DIFFERENTIAL DIAGNOSIS
Figure 7-5 Sialadenoma papilliferum appears clinically
Age: Elderly adults similar to most of the other focal papillary
Sex: Male predilection lesions included in this discussion. Local-
ization to the palate along with palpation
CLINICAL FEATURES
of a firm submucosal base are findings that
Sialadenoma papilliferum is a benign sali- would support the clinical diagnosis. Nev-
vary tumor that presumably arises from ertheless, biopsy is required to secure the
the excretory duct system close to the sur- diagnosis.
FIGURE 7-5
Sialadenoma papilliferum is
an exophytic papilloma aris-
ing within a salivary excre-
tory duct.
PMPH_Eversole_Chapter-07.indd 271 1/20/2011 2:50:23 PM
272 Chapter 7
TREATMENT mas are usually multinodular or papillary.
Because the lesion extends submucosally They may be pedunculated or sessile and
into salivary ducts, superficial excision is are most frequently encountered on the
inadequate. Once the diagnosis is provided gingiva, tongue, and palate.
histologically, a deeper wedge resection
to include underlying glandular tissue is MICROSCOPIC FEATURES
advisable. The surface is multinodular and is cov-
ered by a thin layer of stratified squamous
epithelium, which is distended by swirls
Additional Reading of dense collagen fibers. The intervening
Abrams AM, Finck FM. Sialadenoma papilliferum. A fibroblasts are spindle or stellate, and many
previously unreported salivary gland tumor. Cancer. have copious basophilic cytoplasm with 2
1969;24:1057. to 5 oval nuclei.
Freedman PD, Lumerman H. Sialadenoma papilliferum.
Oral Surg Oral Med Oral Pathol. 1978;45:88.
DIFFERENTIAL DIAGNOSIS
McCoy JM, Eckert EF Jr. Sialadenoma papilliferum.
J Oral Maxillofac Surg. 1980;38:691. Papillary giant cell fibromas may be con-
Nasu M, Takagi M, Ishikawa G. Sialadenoma papil- fused clinically with papillomas, verrucae,
liferum: report of case. J Oral Maxillofac Surg.
1981;39:367. or condylomata. Biopsy is required to make
Papanicolaou SJ, Triantafyllou AG. Sialadenoma papillif- the diagnosis.
erum of the oral cavity: a case report and review of the
literature. J Oral Pathol Med. 1987;42:57. TREATMENT
Ponniah I. A rare case of sialadenoma papilliferum
with epithelial dysplasia and carcinoma in situ. Oral Complete surgical excision is the treatment
Surg Oral Med Oral Pathol Oral Radiol Endod. of choice.
2007;104(2):e27-e29.
GIANT CELL FIBROMA Additional Reading
Figure 7-6 Houston GD. The giant-cell fibroma: a review of 464
cases. Oral Surg Oral Med Oral Pathol. 1982;53:582.
Age: Teenagers and young adults Kuo RC, Wang YP, Chen HM, Sun A, Liu BY, Kuo YS.
Sex: No predilection Clinicopathological study of oral giant cell fibromas.
J Formos Med Assoc. 2009;108:725-729.
CLINICAL FEATURES Regezi JA, Courtney RM, Kerr DA. Fibrous lesions of
the skin and mucous membranes which contain stel-
Although most oral traumatic fibromas are late and multinucleated cells. Oral Surg Oral Med
smooth-surfaced nodules, giant cell fibro- Oral Pathol. 1975;39:605.
FIGURE 7-6
Giant cell fibromas are
small and often have a pap-
illary, corrugated surface.
PMPH_Eversole_Chapter-07.indd 272 1/20/2011 2:50:28 PM
Papillary, Papular, and Multiple Polypoid Lesions 273
Weathers DR, Callihan MD. Giant-cell fibroma. Oral
Surg Oral Med Oral Pathol. 1974;37:374. Additional Reading
Abbey LM, Sawyer DR, Syrop HM. Oral squamous acan-
thoma. Two additional cases with comments on etiolo-
SQUAMOUS ACANTHOMA gy. Oral Surg Oral Med oral pathol. 1978;45:255-260.
Figure 7-7 Chaudhry AP, Salman L, Ross S, Yamane GM, Wank F,
Reddi T. Multiple lesions of the so-called “squamous
acanthoma” of the oral mucosa (basosquamous cell
Age: Adults acanthoma). J Oral Med. 1986;41:114-116.
Sex: No predilection Tomich CE, Shafer WG. Squamous acanthoma of
CLINICAL FEATURES the oral mucosa. Oral Surg Oral Med Oral Pathol.
1974;38:755-759.
Squamous acanthomas are small focal
white lesions that often show a rough, cor-
rugated surface. They are commonly found Focal and Umbilicated
on the gingiva and palate appearing as flat Papules
warts. Although the etiology is unknown
and HPV association has not been found, KERATOACANTHOMA
they are probably a hyperplastic response Figure 7-8
to local mild trauma. Unlike leukoplakia,
squamous acanthoma is innocuous without Age: Adults
premalignant potential. Sex: Male predilection
CLINICAL FEATURES
MICROSCOPIC FEATURES
The facial skin and lower lip, sun-exposed
Focal hyperkeratosis is minimal whereas a areas, are the common sites for keratoacan-
localized acanthosis is prominent. The sur- thoma, which rarely evolves from mucous
face may be somewhat verrucous. There are membranes. Keratoacanthoma is a benign
no dysplastic changes. focal proliferation of surface epithelium
that is classically dome shaped with a cra-
DIFFERENTIAL DIAGNOSIS teriform appearance. The lesion is round
Verruca vulgaris flat wart appears clinically with rolled margins and possesses a central
identical. pit or core filled with a keratin plug that
is frequently discolored, yellowish brown.
Oral examples usually possess a white core.
TREATMENT
Occasionally, the keratin plug exhibits a
Local excision is the treatment of choice. verrucous surface.
FIGURE 7-7
Squamous acanthoma is
a focal, localized benign
keratosis.
PMPH_Eversole_Chapter-07.indd 273 1/20/2011 2:50:40 PM
274 Chapter 7
FIGURE 7-8
Oral keratoacanthoma
of the lip present as focal
keratotic lesions with rolled
borders.
MICROSCOPIC FEATURES Goodwin RE, Fisher GH. Keratoacanthoma of the head
and neck. Ann Otol Rhinol Laryngol. 1980;89:72.
Keratoacanthoma is characterized by an Kohn MW, Eversole LR. Keratoacanthoma of the
abrupt marginal change with acanthosis lower lip. Report of cases. J Oral Maxillofac Surg.
and hyperparakeratosis or hyperorthok- 1972;30:522.
Ramos LM, Cardoso SV, Loyola AM, Rocha MA,
eratosis. The surface is verrucous. On low
Durighetto-Júnior AF. Keratoacanthoma of the infe-
power, the lesion has a flask-shaped con- rior lip: review and report of case with spontaneous
figuration with a superficial collarette and a regression. J Appl Oral Sci. 2009;17:262-265.
bulbous expanded base. The individual cells Scofield HH, Werning JT, Shukes RC. Solitary intraoral
are unremarkable, with one exception: the keratoacanthoma. Oral Surg Oral Med Oral Pathol.
1974;37:889.
parabasilar cells may be hyperchromatic.
Rarely, cytologic atypia may be a prominent
feature, so-called squamous cell carcinoma
with keratoacanthoma features. WARTY DYSKERATOMA
Figure 7-9
DIFFERENTIAL DIAGNOSIS
Age: Adults
Squamous cancer may show similar clini-
Sex: No predilection
cal features; however, cancerous lesions
usually fail to exhibit a smooth round regu- CLINICAL FEATURES
larity. Warty dyskeratoma and molluscum Warty dyskeratoma, a localized lesion of
have gross features in common with kera- skin, is occasionally encountered in the
toacanthoma; yet, they are usually small mouth. The oral lesion is usually found on
(less than 0.5 cm) and keratoacanthoma can the palate or alveolar ridge and appears as
attain dimensions of 1.0 to 2.0 cm. a small papule with a depressed central
pit or as focal verrucous nodules. A vari-
TREATMENT
ant, termed focal acantholytic dyskeratosis,
The lesion usually regresses spontaneously manifests a similar appearance with two
within 1 or 2 years. Despite this fact, it can- or three discrete lesions arising adjacent to
not be definitively diagnosed clinically, is one another.
unsightly, and if allowed to regress, often
leaves a depressed scar. Surgical excision is MICROSCOPIC FEATURES
the treatment of choice. Both warty dyskeratoma and focal acan-
tholytic dyskeratosis display microscopic
Additional Reading features that are nearly identical to those
Eversole LR, Leider AS, Alexander G. Intraoral and labi-
observed in keratosis follicularis. These
al keratoacanthoma. Oral Surg Oral Med Oral Pathol. two focal lesions have a keratinized sur-
1982;54:663. face with an invaginated central depres-
PMPH_Eversole_Chapter-07.indd 274 1/20/2011 2:50:44 PM
Papillary, Papular, and Multiple Polypoid Lesions 275
MOLLUSCUM CONTAGIOSUM
Figure 7-10
Age: Children and young adults
Sex: No predilection
CLINICAL FEATURES
Molluscum contagiosum represents a
unique type of viral wart, resulting from
infection by a member of the poxvirus fam-
FIGURE 7-9 ily. The disease is usually encountered on the
Warty dyskeratoma appearing as crateriform lesion skin of children or in the anogenital region
on the tongue. in adults. It appears as a dome-shaped nod-
ule that is usually, yet not invariably, char-
acterized by a central pit or depressed core.
sion. The spinous layer is thickened and The lesion is rare on the lips or in the mouth
contains individually keratinized cells. The and when it does occur it is usually in an
pathognomonic change is observed inferi- immunocompromised host.
orly where villous rete ridges pervade and
exhibit acantholysis.
MICROSCOPIC FEATURES
DIFFERENTIAL DIAGNOSIS The histologic findings are unique and
Other umbilicated or crateriform lesions diagnostic. The epithelium exhibits an
listed here resemble, or are clinically iden- abrupt zone of acanthosis with a central
tical to, warty dyskeratoma. When a pitted parakeratinized invagination. Large promi-
papule fails to show tumefaction, a trau- nent eosinophilic globules, referred to as
matic lesion may be suspected clinically; molluscum bodies, are located as conglom-
therefore, the diagnosis requires a biopsy. erates in the upper and middle spinous
layers. Coalescing bulbous rete ridges are
TREATMENT present, and the underlying connective tis-
sue is often chronically inflamed.
Surgical excision of these small lesions is
usually accomplished during biopsy. DIFFERENTIAL DIAGNOSIS
Molluscum may clinically resemble a fistula
Additional Reading or parulis, keratoacanthoma, or warty dys-
keratoma when it occurs on lips or mucosa.
Cohen D, Bhattacharyya I. Case of the month. Warty Biopsy is required to make the diagnosis.
dyskeratoma (isolated Darier’s disease). Todays FDA.
2008;20:17-19.
Freedman, P. D., Lumerman, H., and Kerpel, S. M.: TREATMENT
Oral focal acantholytic dyskeratosis. Oral Surg. Oral Excisional biopsy is the treatment of choice.
Med. Oral Pathol. 52:66, 1981.
Leider AS, Eversole LR. Focal acantholytic dyskeratosis
of the oral mucosa. Oral Surg Oral Med Oral Pathol.
1984;58:64.
Szymanski FJ. Warty dyskeratoma, a benign cutaneous
Additional Reading
tumor resembling Darier’s disease microscopically. Barsh LI. Molluscum contagiosum of the oral mucosa.
Arch Dermatol. 1957;75:567. Oral Surg Oral Med Oral Pathol. 1966;22:42.
Tomich CE, Burkes EJ. Warty dyskeratoma (isolated Ficarra G, Gaglioti D. Facial molluscum contagiosum
dyskeratosis follicularis) of the oral mucosa. Oral Surg in HIV-infected patients. Int J Oral Maxillofac Surg.
Oral Med Oral Pathol. 1971;31:798. 1989;18:200.
PMPH_Eversole_Chapter-07.indd 275 1/20/2011 2:50:52 PM
276 Chapter 7
FIGURE 7-10
Multiple lesions of mollus-
cum contagiosum in HIV-
infected patients.
Lynch PJ, Minkin W. Molluscum contagiosum of the kled pigmented surfaces and represent her-
adult. Arch Dermatol. 1968;98:141. niation of the subcutaneous tissues through
Nelson JF, Tsaknis PJ. Molluscum contagiosum of
the lower lip: report of a case. J Oral Pathol Med. a genetically deficient dermal layer. Other
1980;35:62. features of the syndrome include mental
Scherer P, Fries J, Mischkowski RA, Neugebauer J, retardation, strabismus, syndactyly, and
Scheer M, Zöller JE. Intraoral molluscum contagio- colobomas of the iris.
sum imitating a squamous-cell carcinoma in an immu-
nocompetent person—case report and review of the
literature. Int J Oral Maxillofac Surg. 2009;38:802- MICROSCOPIC FEATURES
805. The oral papillomas of the Goltz syndrome
show histomorphologic features indistin-
guishable from the ordinary squamous
Diffuse and Multifocal papilloma.
Papillary Lesions
DIFFERENTIAL DIAGNOSIS
FOCAL DERMAL HYPOPLASIA The various components of the syndrome
(GOLTZ SYNDROME) allow differentiation from other diseases
Figure 7-11 manifesting oral papillary or polypoid
lesions.
Age: Children
Sex: No predilection TREATMENT
CLINICAL FEATURES
The papillomas should be excised, as they
Many defects accompany the skin lesions can be traumatized by mastication and thus
of the Goltz syndrome, including multiple hemorrhage.
papillomas of the lips and oral mucosa.
The oral lesions consist of exophytic pap-
illary outgrowths that are identical to the Additional Reading
ordinary oral squamous papilloma, yet
Goltz RJ et al. Focal dermal hypoplasia syndrome. Arch
are prone to be multiple with tendency for Dermatol. 1962;86:708.
confluency. The skin lesions located on the Gorlin RJ et al. Focal dermal hypoplasia syndrome. Acta
extremities are rubbery nodules with wrin- Dermatol. 1963;43:421.
PMPH_Eversole_Chapter-07.indd 276 1/20/2011 2:50:53 PM
Papillary, Papular, and Multiple Polypoid Lesions 277
FIGURE 7-11
FIGURE 7-12
Orolabial papillomas in focal dermal hypoplasia syn-
Unilateral extensive papillary proliferations involv-
drome. (Courtesy of Dr. Juan Seoane.)
ing oral mucosa in nevus unius lateris. (Courtesy of
Dr. Giuseppe Ficarra.)
Seoane J, Gibson RL, Almagro M, Pintos E. Oral mani-
festations associated with focal dermal hypoplasia. DIFFERENTIAL DIAGNOSIS
Dermatology. 2009;219:368-370.
Nevus unius lateris must be differentiated
from verrucous carcinoma, pyostomati-
NEVUS UNIUS LATERIS tis vegetans, and florid papillomatosis.
Figure 7-12 The linear configuration, extension onto
facial skin, and development during child-
Age: Children hood allow for differentiation from these
Sex: No predilection entities.
CLINICAL FEATURES
TREATMENT
A developmental verrucous lesion of skin,
nevus unius lateris (also termed the epi- After microscopic confirmation of the diag-
dermal nevus syndrome) usually occurs nosis, the lesion may be removed surgically
on the arm as a keratotic washboard- or with electrocautery in stages. The facial
rough lesion that conforms to a narrow lesions should be managed by a plastic
linear configuration. When the face is surgeon.
involved, extension into the oral cavity
may occur. The lesion continues its linear
orientation, yet its appearance assumes Additional Reading
a pebbly papillary pattern identical to Brown HM, Gorlin RJ. Oral mucosal involvement in
papilloma. nevus unius lateris (ichthyosis hystrix). Arch Dermatol.
1960;81:509.
MICROSCOPIC FEATURES Ephraim A, Skeer J. Nevus unius lateris on the left
cheek, scalp, and neck. Arch Dermatol Syph.
The skin lesion demonstrates acutely 1944;50:222.
angulated verrucous epithelial hyperk- Haberland-Carrodeguas C, Allen CM, Lovas JG, et al.
eratotic projections not unlike those of Review of linear epidermal nevus with oral mucosal
involvement—series of five new cases. Oral Dis.
verruca vulgaris. The oral lesion is micro- 2008;14:131-137.
scopically indistinguishable from simple Kelly JE, Hibbard ED, Giansanti JS. Epidermal
papilloma. nevus syndrome; report of a case with unusual oral
PMPH_Eversole_Chapter-07.indd 277 1/20/2011 2:51:02 PM
278 Chapter 7
manifestations. Oral Surg Oral Med Oral Pathol.
1972;34:774.
Muller JT, Pickett AB, Frederick FD. Facial
hemihypertrophy associated with nevus unius lat-
eris syndrome. Oral Surg Oral Med Oral Pathol.
1980;50:226.
ACANTHOSIS NIGRICANS
Figure 7-13
Age: Adults, maligna form older adults
Sex: No predilection
CLINICAL FEATURES FIGURE 7-13
Acanthosis nigricans of the lips. (Courtesy of Dr.
Acanthosis nigricans is a localized large Heddie Sedano.)
papillary lesion with variable amounts of
pigmentation. It exists in two forms: benign
and malignant. These two forms are clini- TREATMENT
cally indistinguishable being broad-based The lesion may be excised or removed by
velvety papillary lesions that occur on the laser if cosmetically problematic. Systemic
skin, lips, or mucous membranes and are work-up for diabetes, other endocrinopa-
usually solitary. They do not progress to thies, and internal malignancy should be
carcinoma. The benign form may be associ- undertaken.
ated with various endocrinopathies includ-
ing hypo- or hyperthyroidism, acromegaly,
insulin-dependent diabetes, and Cushing’s
Additional Reading
syndrome. The malignant form represents a Pentenero M, Carrozzo M, Pagano M, Gandolfo S. Oral
paraneoplastic syndrome whereby affected acanthosis nigricans, tripe palms and sign of leser-
trélat in a patient with gastric adenocarcinoma. Int
patients will suffer from an internal malig- J Dermatol. 2004;43(7):530-532.
nancy, most frequently of the stomach Schnopp C, Baumstark J. Images in clinical medicine. Oral
(adenocarcinomas). acanthosis nigricans. N Engl J Med. 2007;357(9):e10.
Tyler MT, Ficarra G, Silverman S Jr, Odom RB, Regezi
JA. Malignant acanthosis nigricans with florid papil-
MICROSCOPIC FEATURES lary oral lesions. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 1996;81(4):445-449.
A diffuse papillary pattern is observed
with parakeratosis and acanthosis. There
are melanin pigment granules in the ATYPICAL VERRUCOUS
basal cell layer with incontinence into the LEUKOPLAKIA
submucosa. Dysplastic changes are not Figure 7-14
encountered.
Age: Middle-aged and elderly adults
DIFFERENTIAL DIAGNOSIS Sex: Female predilection
On skin the pigmented velvety papillary CLINICAL FEATURES
appearance is clinically distinct. In the Verrucous leukoplakia, also referred to as
mucous membrane, these lesions may verrucous hyperplasia or verruciform leu-
resemble other papillary lesions discussed koplakia, is a precancerous lesion that rep-
here, however, any papillary lesion with resents the benign end of the Prolferative
brown pigmentation should be suspect. Verrucous Leukoplakia spectrum and may
PMPH_Eversole_Chapter-07.indd 278 1/20/2011 2:51:06 PM
Papillary, Papular, and Multiple Polypoid Lesions 279
FIGURE 7-14
Atypical verrucous leuko-
plakia, a histologic variant
of proliferative verrucous
leukoplakia.
progress to carcinoma. Clinically, the lesion DIFFERENTIAL DIAGNOSIS
is a localized yet often diffuse verrucous The clinical appearance of verrucous leuko-
or papillary lesion found most often on the plakia is similar, if not identical, to verru-
gingiva, alveolar ridge, or mucobuccal fold. cous carcinoma, particularly when a white
It may be white, pink, or speckled. Planar keratotic surface is present. Furthermore,
leukoplakia is frequently observed in asso- occurrence in the elderly differentiates this
ciation with the verrucous lesion, either in lesion from other diffuse papillary lesions
continuity or in separate locations. Some that occur in children.
patients give a history of smokeless tobacco
usage, although others deny any tobacco
TREATMENT
habits whatsoever. Some lesions harbor
human papillomavirus DNA; however, most Once the diagnosis is made, biopsy of
are devoid of any known genotypes. other areas of a large lesion should be per-
formed, with examination for the presence
MICROSCOPIC FEATURES of carcinoma. Wide local excision is recom-
mended with periodic follow-up. If coex-
Some examples exhibit sharp verrucous istent carcinoma is detected, the treatment
projections (acrokeratotic) or blunt rounded must be more aggressive. This disease is
projections (polypoid and cryptic). The extremely difficult to eradicate and recur-
surface is frequently hyperortho- or hyper- rence is the rule rather than the exception.
parakeratotic, and acanthosis is usually
observed. There is a high incidence of
dysplastic cytologic change, and many of
these lesions lie adjacent to zones of verru- Additional Reading
cous carcinoma or invasive squamous cell Adkins KF, Monsour FN. Verrucous leukoplakia. N Z
carcinoma. Dent J. 1976;72:28.
PMPH_Eversole_Chapter-07.indd 279 1/20/2011 2:51:11 PM
280 Chapter 7
Chen HM, Yu CH, Tu PC, Yeh CY, Tsai T, Chiang CP. MICROSCOPIC FEATURES
Successful treatment of oral verrucous hyperplasia and
oral leukoplakia with topical 5-aminolevulinic acid- The histomorphologic characteristics are
mediated photodynamic therapy. Lasers Surg Med. distinctive. Massively enlarged bulbous acan-
2005;37:114-122. thotic rete ridges invaginate into the connec-
Shear M, Pindborg JJ. Verrucous hyperplasia of the oral
tive tissue, yet extensions from the basal cell
mucosa. Cancer. 1980;46:1855-1862.
Wang YP, Chen HM, Kuo RC, et al. Oral verrucous layer showing invasion do not exist. Apart
hyperplasia: histologic classification, prognosis, and from basilar and parabasilar hyperchroma-
clinical implications. J Oral Pathol Med. 2009;3: tism, cytologic atypia is not featured; rather,
651-656. a normal maturation of epithelium exists.
Yeh CJ. Treatment of verrucous hyperplasia and
verrucous carcinoma by shave excision and simple Deep crypts, filled with parakeratin, extend
cryosurgery. Int J Oral Maxillofac Surg. 2003;32: downward from the surface into the center
280-283. of the bulbous rete ridge invaginations.
DIFFERENTIAL DIAGNOSIS
VERRUCOUS CARCINOMA Verrucous carcinoma may clinically simu-
Figure 7-15 late papillary hyperplasia, pyostomatitis
vegetans, and, importantly, squamous cell
Age: Elderly adults carcinoma that may be clinically verrucous
Sex: Male predilection in appearance. Only biopsy can differenti-
CLINICAL FEATURES ate between true verrucous carcinoma and
a clinically verrucoid-appearing squamous
Verrucous carcinoma is a nonmetastasiz- cell carcinoma.
ing, laterally spreading epithelial tumor,
sometimes associated with tobacco chew- TREATMENT
ing or snuff dipping. The lesion is typically Wide surgical excision is recommended;
fungating with a white verrucoid keratotic recurrence is common. In the past, radia-
surface that has a shaggy appearance. It is tion therapy was contraindicated in verru-
most often encountered in the mucobuccal cous carcinoma because anaplastic trans-
fold and buccal mucosa. In the later stages formation occurred after such treatment.
of disease, extensive lateral spread becomes The higher energy radiation sources used
manifest. Human papillomavirus type 2 today minimize this complication; inop-
DNA has been demonstrated in a minority erable lesions have shown resolution with
of cases. radiation therapy.
FIGURE 7-15
Verrucous carcinoma, a
nonmetastasizing neoplasm
of oral mucosa that shows
a shaggy, verrucous kera-
totic surface, an end stage
of proliferative verrucous
leukoplakia.
PMPH_Eversole_Chapter-07.indd 280 1/20/2011 2:51:23 PM
Papillary, Papular, and Multiple Polypoid Lesions 281
FIGURE 7-16
Papillary exophytic
squamous cell carcinoma,
may also be an end-stage
lesion of proliferative ver-
rucous leukoplakia.
with white keratoses. They show polypoid
Additional Reading extensions across the surface. The tumor
Ackerman LV. Verrucous carcinoma of the oral cavity. evolves slowly, proliferating superficially,
Surgery. 1948;23:670. and may reach 3 cm or more before foci of
Jacobson S, Shear M. Verrucous carcinoma of the mouth. invasion into the submucosal connective tis-
J Oral Pathol Med. 1972;1:66. sue occurs. Only late stage lesions of T4 size
McCoy JM, Waldron CA. Verrucous carcinoma; analy-
sis of fifty-six cases. Oral Surg Oral Med Oral Pathol. and long duration may metastasize locally.
1981;52:623.
Perez CA, Kraus FT, Evans JC, Powers WE. Anaplastic MICROSCOPIC FEATURES
transformation in verrucous carcinoma of the oral cav-
ity after radiation therapy. Radiology. 1966;86:108. Stratified squamous epithelium shows an
Rekha KP, Angadi PV. Verrucous carcinoma of the oral cav- exophytic papillary growth pattern with
ity: a clinico-pathologic appraisal of 133 cases in Indians. elongated wide rete pegs. Cytologically,
Oral Maxillofac Surg. 2010 Apr 16. [Epub ahead of print.] dysplastic changes are seen, particularly in
lower strata keratinocytes. In larger lesions
of longer duration, invasive foci of carci-
PAPILLARY SQUAMOUS CELL noma may be encountered in the connec-
CARCINOMA tive tissue.
Figure 7-16
DIFFERENTIAL DIAGNOSIS
Age: Elderly
Sex: Slight female predilection The papillary appearance in this specific
form of carcinoma may be quite similar
CLINICAL FEATURES
to the other benign entities in this chap-
Papillary squamous cell carcinoma is a ter. They mirror verrucous carcinoma and
unique tumor that tends to be exophytic atypical verrucous hyperplasia; however,
without extensive invasion. The lesions are papillary squamous cancer tends to be less
diffuse and may be red, pink, or speckled keratotic.
PMPH_Eversole_Chapter-07.indd 281 1/20/2011 2:51:30 PM
282 Chapter 7
FIGURE 7-17
Papillomatosis in the vault is
found under ill-fitting maxil-
lary dentures.
TREATMENT
Tumors in stage T1 and T2 rarely metas-
Diffuse Papular and
tasize whereas nodal spread is com- Polypoid Lesions
mon among T3 and T4 stage tumors.
Wide local excision is the treatment of PAPILLARY HYPERPLASIA
choice and neck radiation or dissection is Figure 7-17
recommended when nodes are detected Age: Adults
clinically or by magnetic resonance Sex: No predilection
imaging.
CLINICAL FEATURES
Confined to the palatal vault, papillary
Additional Reading hyperplasia or papillomatosis is most often
associated with a maxillary denture. Occa-
Ishiyama A, Eversole LR, Ross DA, et al. Papillary
squamous neoplasms of the head and neck. sionally, it occurs in dentulous mouths in
Laryngoscope. 1994;104:1446-1452. association with a partial denture. The lesion
Jo VY, Mills SE, Stoler MH, Stelow EB. Papillary displays a cobblestone appearance and is
squamous cell carcinoma of the head and neck: fre- either normal in color or erythematous.
quent association with human papillomavirus infec-
tion and invasive carcinoma. Am J Surg Pathol.
When the papillary lesions are reddened,
2009;33:1720-1724. secondary infection with Candida is com-
Suarez PA, Adler-Storthz K, Luna MA, El-Naggar AK, mon. The cause is unknown but is probably
Abdul-Karim FW, Batsakis JG. Papillary squamous related to trauma and may arise in response
cell carcinomas of the upper aerodigestive tract: a
to negative pressure placed on the palatal
clinicopathologic and molecular study. Head Neck.
200l;22:360-368. tissues. The lesion is not premalignant.
Takeda Y, Satoh M, Nakamura S, Yamamoto H.
Papillary squamous cell carcinoma of the oral MICROSCOPIC FEATURES
mucosa: immunohistochemical comparison with
other carcinomas of oral mucosal origin. J Oral Sci. The epithelium manifests multiple dome-
2001;43:165-169. shaped papules with elongated rete ridges
PMPH_Eversole_Chapter-07.indd 282 1/20/2011 2:51:36 PM
Papillary, Papular, and Multiple Polypoid Lesions 283
and pseudoepitheliomatous hyperplasia. STOMATITIS NICOTINA
The submucosa contains a diffuse chronic Figure 7-18
inflammatory cell infiltrate.
Age: Middle-aged and elderly adults
DIFFERENTIAL DIAGNOSIS Sex: Male predilection
The combination of dental prosthesis and CLINICAL FEATURES
palatal vault papillary outgrowth allows Pipe and cigar smokers occasionally develop
for a clinical diagnosis. If the lesion extends multiple white keratotic papules with red
onto the alveolar ridge, it must be differenti- depressed centers that represent dilated,
ated from verrucous carcinoma or a specific inflamed minor salivary ducts on the hard
granulomatous infection. and soft palate. The papules do not coalesce
and are separated by intervening normal-
TREATMENT appearing mucosa. It is not known whether
these multifocal keratotic papules arise as
The hyperplastic tissue may resolve after
a consequence of heat or tobacco tars. The
removal of the old denture. If not, surgical
lesion is rarely seen in cigarette smokers;
removal is recommended before fabrication
evidence does not support a premalignant
of a new prosthesis.
potential.
MICROSCOPIC FEATURES
Additional Reading The surface epithelium is hyperkeratotic
Miller EL. Clinical management of denture-induced and usually acanthotic. The salivary excre-
inflammations. J Prosthet Dent. 1977;38:362. tory ducts are dilated and evince a periduc-
O’Driscoll PM. Papillary hyperplasia of the palate. Br
Dent J. 1965;118:77. tal mononuclear inflammatory infiltrate.
Schmitz JF. A clinical study of inflammatory papillary
hyperplasia. J Prosthet Dent. 1964;14:1034. DIFFERENTIAL DIAGNOSIS
Uohara GI, Federbush MD. Removal of
papillary hyperplasia. J Oral Maxillofac Surg. White papules with a red center located on
1968;26:463. the palate of a pipe or cigar smoker are usu-
Vargas PA, Perez DE, Jorge J, Rangel AL, ally sufficient findings to permit establish-
León JE, Almeida OP. Denture hyperplasia with
areas simulating oral inverted ductal papilloma. Med
ment of the diagnosis on a clinical basis.
Oral Patol Oral Cir Bucal. 2005;10(suppl 2):E117- Other papular lesions fail to show this com-
E121. bination of findings.
FIGURE 7-18
Stomatitis nicotina, multiple
crateriform papules.
PMPH_Eversole_Chapter-07.indd 283 1/20/2011 2:51:42 PM
284 Chapter 7
pharyngitis is unique and is usually diag-
nosed clinically, based on morphologic char-
acteristics and location of the lesion. Multiple
yellowish pink papules are distributed over
the soft palate, tonsillar fauces, and orophar-
ynx. The patient fails to show a cutaneous
exanthem. Fever, lymphadenopathy, and
sore throat are the typical symptoms. Epi-
demics among school children are common.
MICROSCOPIC FEATURES
Surface epithelium is distended by focal
aggregates of lymphocytes, and attempts at
germinal center formation can be observed
FIGURE 7-19 in some of these lymphoid papules.
Multiple red papules of the soft palate and orophar-
ynx characteristic of lymphonodular pharyngitis, a DIFFERENTIAL DIAGNOSIS
coxsackie virus infection.
None of the other entities listed as papular
or multiple polypoid lesions are restricted
to the oropharynx, nor are they associated
TREATMENT
with constitutional symptoms of infectious
Abating the tobacco habit allows resolution. disease. A clinical diagnosis can be made. If
The oral cavity should be examined thor- confirmation is required, a stool culture for
oughly to detect leukoplakic or erythropla- coxsackie virus can be ordered.
kic foci, which may coexist.
TREATMENT
Additional Reading The disease is self-limited and resolves in 7 to
10 days. Antipyretic medication may be used
dos Santos RB, Katz J. Nicotinic stomatitis: positive cor- along with a palliative mouth rinse or gargle.
relation with heat in maté tea drinks and smoking.
Quintessence Int. 2009;40:537-540.
Saunders WH. Nicotine stomatitis of the palate. Ann
Otol Rhinol Laryngol. 1958;67:618.
Additional Reading
Schwartz DL. Stomatitis nicotina of the palate. Oral Surg Lennette EH, Magoffin RL. Virologic and immunologic
Oral Med Oral Pathol. 1965;20:306. aspects of major oral ulcerations. J Am Dent Assoc.
Thoma KH. Stomatitis nicotina and its effect on the pal- 1973;87:1055.
ate. Am J Orthod Oral Surg. 1941;27:38. Steigman AJ, Lipton MM, Braspennickx H. Acute
lymphonodular pharyngitis: a newly described condi-
tion due to coxsackie A virus. J Pediatr. 1963;61:331.
ACUTE LYMPHONODULAR
PHARYNGITIS KERATOSIS FOLLICULARIS
Figure 7-19 Figure 7-20
Age: Children and young adults Age: Adults
Sex: No predilection Sex: Male predilection
CLINICAL FEATURES CLINICAL FEATURES
Coxsackie virus infections manifest a vari- A primary disease of skin, keratosis folli-
ety of clinical presentations. Lymphonodular cularis or Darier-White’s disease frequently
PMPH_Eversole_Chapter-07.indd 284 1/20/2011 2:51:47 PM
Papillary, Papular, and Multiple Polypoid Lesions 285
affects the oral mucous membranes. This
autosomal dominantly inherited disorder Additional Reading
affects epithelial maturation and keratiniza- Miller RL, Bernstein ML, Arm RN. Darier’s disease of
tion and is associated with mutations in the the oral mucosa: clinical case report with ultrastruc-
ATP2A2 gene that encodes calcium pump tural evaluation. J Oral Pathol Med. 1982;11:79.
proteins. Orange-brown keratotic papules Prindville DE, Stern D. Oral manifestations of Darier’s
disease. J Oral Maxillofac Surg. 1976;34:1001.
appear on the skin and often keratinize pro- Spouge JD, Trott JR, Chesko G. Darier-White’s disease:
gressively, resulting in diffuse white verru- a cause of white lesions of the mucosa. Report of four
coid plaques. The oral lesions may be white cases. Oral Surg Oral Med Oral Pathol. 1966;21:441.
or may exhibit normal coloration; they dif- Weathers DR, Driscoll RM. Darier’s disease of the
oral mucosa. Oral Surg Oral Med Oral Pathol.
fusely affect the buccal mucosa and palate, 1974;37:711.
thus appearing as multiple confluent pap-
ules with a cobblestone pattern.
FOCAL EPITHELIAL
MICROSCOPIC FEATURES
HYPERPLASIA (HECK’S
DISEASE)
Hyperkeratosis occurs, and the spinous
Figure 7-21
cell layer contains individually keratinized
cells, many of which are enveloped by Age: Children
spinous layer cells (corps ronds). The rete Sex: No predilection
ridges assume a villous pattern with supra-
CLINICAL FEATURES
basilar acantholytic cleavage.
Focal polypoid nodules that appear primar-
DIFFERENTIAL DIAGNOSIS ily on the lips and buccal mucosa during the
prepubescent period are characteristic of
The cobblestone pattern resembles that seen
Heck’s disease. These peculiar lesions occur
in Cowden’s disease, papillary hyperplasia,
in clusters and in isolated crops, which
and pyostomatitis vegetans. The occur-
eventually spontaneously regress. They are
rence of papular and keratotic cutaneous
pale to normal in color and show a flattened
lesions suggests keratosis follicularis clini-
surface. American Indians and other ethnic
cally, and the microscopic features confirm
groups of Athapaskan descent are often
this impression.
afflicted, but this disorder has also been
reported in other ethnic groups, including
TREATMENT Europeans. Similar-appearing lesions may
Retinoids have been employed with mod- be encountered among HIV-seropositive
erate success for the cutaneous lesions. homosexual males. Focal epithelial hyper-
No effective treatment exists for the oral plasia is caused by human papillomavirus
lesions. types 13 and 32.
FIGURE 7-20
Keratosis follicularis. Oral
papular lesions and cutane-
ous scaly papules.
PMPH_Eversole_Chapter-07.indd 285 1/20/2011 2:51:48 PM
286 Chapter 7
FIGURE 7-21
Multiple sessile papules of the
lips and buccal mucosa char-
acteristic of focal epithelial
hyperplasia.
MICROSCOPIC FEATURES Indian children. Oral Surg Oral Med Oral Pathol.
1965;20:201.
The epithelium displays an exophytic nodu- Beaudenon S. A new type of human papillomavirus asso-
lar surface with thickened parakeratin. The ciated with oral focal epithelial hyperplasia. J Invest
major portion of the outgrowth is accounted Dermatol. 1987;88:130.
Cohen PR, Hebert AA, Adler-Storthz K. Focal epithe-
for by epithelial hyperplasia with acantho-
lial hyperplasia: Heck disease. Pediatr Dermatol.
sis and elongated anastomosing rete ridges. 1993;10:245-251.
Inclusion bodies may be seen in cells occu- Pfister H, Hettich I, Runne U, Gissmann L, Chilf GN.
pying the spinous cell layer. Characterization of human papillomavirus type
13 from focal epithelial hyperplasia Heck lesions.
Virology. 1983;47:363.
DIFFERENTIAL DIAGNOSIS Witkop CJ Jr, Niswander JD. Focal epithelial hyperplasia
The appearance of multifocal polypoid in Central and South American Indians and Latinos.
Oral Surg Oral Med Oral Pathol. 1965;20:213.
lesions on the lips of Indian children is
characteristic. Lack of total confluency aids
in differentiating Heck’s disease from the MULTIPLE HAMARTOMA
other lesions included in this section. (COWDEN) SYNDROME
Figure 7-22
TREATMENT
No treatment is required; spontaneous Age: Adults
regression occurs. Sex: No predilection
CLINICAL FEATURES
Additional Reading Also known as Cowden’s disease, the mul-
tiple hamartoma syndrome represents an
Archard HO, Heck JW, Stanley HR. Focal epithelial autosomal dominant hereditary disease with
hyperplasia: an unusual oral mucosa lesion found in mutations in a candidate tumor suppressor
PMPH_Eversole_Chapter-07.indd 286 1/20/2011 2:51:50 PM
Papillary, Papular, and Multiple Polypoid Lesions 287
gene, PTEN. It is characterized by wide-
spread hamartomas and neoplasms of skin, Additional Reading
mucosa, and internal organs. The oral lesions Bagan JV, Peñarrocha M, Vera-Sempere F.
are found on the attached gingiva. Multiple Cowden syndrome: clinical and pathological consid-
papular nodules yield a cobblestone pebbly erations in two new cases. J Oral Maxillofac Surg.
surface. Cutaneous papulonodular lesions 1989;47:291.
Farooq A, Walker LJ, Bowling J, Audisio RA. Cowden
are seen around the nares, lip commissures, syndrome. Cancer Treat Rev. 2010. May 22. [Epub
and palmar surface of the hands. Patients ahead of print.]
with Cowden’s disease also develop goiter Gentry WC Jr, Eskritt NE, Gorlin RJ. Multiple hama-
or thyroid adenomas and fibrocystic disease rtoma syndrome (Cowden disease). Arch Dermatol.
1974;109:521.
of the breast, which may progress to malig- Gertzman GBR, Clark M, Gaston G. Multiple
nancy. Other organs may also be involved. hamartoma and neoplasia syndrome (Cowden’s
syndrome). Oral Surg Oral Med Oral Pathol.
MICROSCOPIC FEATURES 1980;49:314.
Weary PE, Gorlin RJ, Gentry WC Jr, Comer JE, Greer
The oral papules exhibit microscopic fea- KE. Multiple hamartoma syndrome (Cowden’s dis-
tures of fibroepithelial polyps. The epi- ease). Arch Dermatol. 1972;106:682.
thelium is somewhat hyperplastic with
acanthosis and elongated, anastomosing
rete ridges. Supporting this epithelium is a PYOSTOMATITIS VEGETANS
mature fibrous connective tissue core. Figure 7-23
DIFFERENTIAL DIAGNOSIS Age: Middle-aged adults
Sex: Slight female predilection
The cobblestone lesions of multiple hamar-
toma syndrome may appear similar to the CLINICAL FEATURES
papular lesions observed in Sipple syn- Pyostomatitis vegetans is a vegetating dis-
drome, pyostomatitis vegetans, keratosis ease of oral mucosa characterized by both
follicularis, and focal epithelial hyperplasia. erosive and multifocal polypoid lesions of
Localization to the gingiva, observed pap- the lips and buccal mucosa. Although it may
ules on the facial skin, and a history of thy- occur in the absence of systemic disease, it is
roid or breast disease in conjunction with more often associated with either ulcerative
familial involvement lead to the diagnosis. colitis or regional enteritis, thereby repre-
senting the oral mucosal counterpart to the
TREATMENT skin disease pyodermatitis vegetans of Hal-
No treatment is necessary for the oral lesions. lopeau. The individual polyps vary in size
A complete medical work-up for organ-sys- and are usually inflamed. Pain is a promi-
tem involvement is recommended. nent feature when erosions are present.
FIGURE 7-22
Gingival papules in Cowden
syndrome.
PMPH_Eversole_Chapter-07.indd 287 1/20/2011 2:51:55 PM
288 Chapter 7
MICROSCOPIC FEATURES to bowel disease. Oral Surg Oral Med Oral Pathol.
1983;55:363.
The surface epithelium is acanthotic with McCarthy FP, Shklar G. A syndrome of pyostomati-
polypoid extensions of submucosal connec- tis vegetans and ulcerative colitis. Arch Dermatol.
tive tissue. A subacute inflammatory cell 1963;88:913.
Nigen S, Poulin Y, Rochette L, Lévesque MH, Gagné
infiltrate prevails, with foci of eosinophilic
E. Pyodermatitis-pyostomatitis vegetans: two cases
abscesses located in the papillae and at the and a review of the literature. J Cutan Med Surg.
epithelial connective tissue junction. 2003;7(3):250-255.
Thornhill MH, Zakrzewska JM, Gilkes JJ. Pyostomatitis
DIFFERENTIAL DIAGNOSIS vegetans: report of three cases and review of the litera-
ture. J Oral Pathol Med. 1992;21(3):128-133.
The lesion must be differentiated from ver-
rucous carcinoma, oral florid papillomato-
sis, mycotic granuloma, and focal epithelial CROHN’S DISEASE
hyperplasia (Heck’s disease). Biopsy with Figure 7-24
identification of eosinophilic abscesses and
medical work-up for ulcerative colitis are Age: Middle-aged adults
recommended to aid in arriving at a defini- Sex: No predilection
tive diagnosis. CLINICAL FEATURES
Regional enteritis or Crohn’s disease is a
TREATMENT
segmental granulomatous disease of the
Treatment is empiric. Systemic steroids ileum and ascending colon. Oral lesions are
(25-30 mg prednisone daily) with standard occasionally present and consist of bosse-
care for ulcerative colitis usually results in lated multiple polyps usually located in the
diminution of the oral lesions. Ulcerative buccal mucosa or mucobuccal fold. They
colitis is managed by a general physician or are firm, usually normal in color, and pain-
gastroenterologist. less. Gingival swellings and erythematous
pebbly lesions may also be encountered.
Additional Reading Patients complain of gastrointestinal irreg-
ularity, mild chronic diarrhea, and abdomi-
Forman L. Two cases of pyodermite vegetante nal discomfort.
(Hallopeau); an eosinophilic pustular and vegetating
dermatitis with conjunctival, oral and colonic involve- MICROSCOPIC FEATURES
ment. Proc R Soc Med. 1965;58:244.
Hansen LA, Silverman S Jr, Daniels TE. The differen- The epithelium is distended by an under-
tial diagnosis of pyostomatitis vegetans and its relation lying mass of organized granulation tis-
FIGURE 7-23
Multiple papules and ero-
sions in pyostomatitis
vegetans associated with
ulcerative colitis.
PMPH_Eversole_Chapter-07.indd 288 1/20/2011 2:51:58 PM
Papillary, Papular, and Multiple Polypoid Lesions 289
FIGURE 7-24
Multiple polypoid tumefac-
tions of the buccal mucosa
and mucobuccal fold are
oral manifestations of
Crohn’s disease.
sue with lymphoid infiltration, epithelioid Snyder MB, Cawson RA. Oral changes in Crohn’s dis-
histiocytes, and giant cells yielding a non- ease. J Oral Maxillofac Surg. 1976;34:594.
caseating specific granulomatous reaction.
Special stains fail to disclose the presence of
microorganisms. SPECIFIC GRANULOMATOUS
DIFFERENTIAL DIAGNOSIS INFECTIONS
Figure 7-25
The polypoid masses in Crohn’s disease are
broader and, overall, larger than most of the Age: Adults
other polypoid or papillary lesions included Sex: Equal distribution
in this section. They must be differentiated CLINICAL FEATURES
from denture hyperplasia, pyostomatitis
vegetans, and mycotic granuloma. Infectious and noninfectious granuloma-
tous inflammatory lesions of the oral mucous
TREATMENT membranes are usually localized and
exhibit a granular or papillary surface. The
The oral lesions may be excised. Crohn’s
lesions are usually raised and firm and may
disease is managed by a general physician
appear somewhat erythematous. Most of
or gastroenterologist.
them are infectious, representing hematog-
enous spread from a primary pulmonary
Additional Reading focus. The deep fungal diseases such as his-
toplasmosis and blastomycosis are more apt
Boraz RA. Oral manifestations of Crohn disease: update to show pebbly granular lesions. The inher-
of the literature and report of case. ASDC J Dent ited disorder known as chronic granuloma-
Child. 1988;55:72.
Bottomley WK, Giorgini GL, Julienne CH. Oral exten- tous disease may manifest similar lesions.
sion of regional enteritis (Crohn’s disease). Oral Surg This disorder is characterized by ineffective
Oral Med Oral Pathol. 1972;34:417. phagocytolysis by leukocytes with recur-
Eisenbud L, Katzka I, Platt N. Oral manifestations in rent and persistent infections accompa-
Crohn’s disease. Oral Surg Oral Med Oral Pathol.
1972;34:770. nied by granulomatous inflammation. Oral
Kim SK, Lee ES. Orofacial granulomatosis associated with lesions of sarcoidosis may also present in
Crohn’s disease. Ann Dermatol. 2010;22(2):203-205. similar fashion clinically. Granulomatous
PMPH_Eversole_Chapter-07.indd 289 1/20/2011 2:52:02 PM
290 Chapter 7
those patients presenting with a history of
risk factors.
TREATMENT
Depending on the organism identified, if
any, the treatment is medical. Fungal infec-
tions are generally treated with amphoteri-
cin B or ketoconazole.
Additional Reading
Kerr MW. Sarcoidosis. Oral Surg Oral Med Oral Pathol.
1965;20:166.
FIGURE 7-25 Kruse AL, Zwahlen RA, Bredell MG, Gengler C,
Granulomatous inflammation due to blastomycosis Dannemann C, Grätz KW. Primary blastomycosis of
with cobblestone appearance. oral cavity. J Craniofac Surg. 2010;21(1):121-123.
Pindborg JJ. Classification of oral lesions associated
with HIV infection. Oral Surg Oral Med Oral Pathol.
1989;67:292.
infections with Mycobacterium avium intra- Tiecke RW, Baron HJ, Casey DE. Localized oral his-
cellulare, Histoplasma capsulatum, and other toplasmosis. Oral Surg Oral Med Oral Pathol.
parasites occur in the submucosa among 1963;16:441.
Wysocki GP, Brooke RI. Oral manifestations of chronic
human immunodeficiency virus (HIV)-se- granulomatous disease. Oral Surg Oral Med Oral
ropositive patients, many of whom have no Pathol. 1978;46:815.
pulmonary involvement with the specific
organism in question.
AMYLOIDOSIS
MICROSCOPIC FEATURES Figure 7-26
The epithelium may exhibit pseudoepithe-
liomatous hyperplasia; foci of granuloma- Age: Middle-aged adults
tous inflammation are located within the Sex: Male predilection
underlying connective tissue. Epithelioid CLINICAL FEATURES
histiocytes predominate, and multinucle- Amyloidosis is a systemic disease in which
ated giant cells can be identified. Specific a heterologous group of glycoproteins accu-
histochemical stains such as acid-fast, peri- mulates within the connective tissues and
odic acid-Schiff (PAS), and methenamine around vascular walls. The disease may
silver demonstrate the presence of microor- be primary or secondary. Secondary forms
ganisms in the infectious granulomas. are more common and arise in conjunction
with multiple myeloma or, occasionally, in
DIFFERENTIAL DIAGNOSIS
association with a chronic granulomatous
Most of the focal papillary lesions included disease. The tongue is the most common
here are small and fail to evince surface intraoral site, yet deposits of amyloid pro-
erythema. Granulomatous lesions are often tein may also be identified in the lips and
large and invariably sessile. A history of buccal mucosa. The lesions are usually mul-
pulmonary disease or persistent cough tifocal and appear as sessile, deep nodules
and dyspnea should arouse suspicion of that are indurated. Amyloid A, deposited in
systemic granulomatous inflammatory dis- senile and familial amyloidosis, is a protein
ease. HIV infection should be suspected in derived from prealbumin, whereas amyloid
PMPH_Eversole_Chapter-07.indd 290 1/20/2011 2:52:08 PM
Papillary, Papular, and Multiple Polypoid Lesions 291
FIGURE 7-26
Multiple tongue nodules in
amyloidosis.
L, seen in myeloma, originates from immu-
noglobulin light chains. A third type, Additional Reading
AB2M derived from β2-microglobulin, is Akin RK, Barton K, Walters PJ. Amyloidosis, macroglos-
encountered in patients undergoing long- sia and carpal tunnel syndrome associated with myelo-
term hemodialysis. ma. J Oral Maxillofac Surg. 1975;33:690.
Cengiz IM, Wang HL, Yildiz L. Oral involvement in
a case of AA amyloidosis: a case report. J Med Case
MICROSCOPIC FEATURES Reports. 2010;4(1):200. [Epub ahead of print.]
Flick WG, Lawrence FR. Oral amyloidosis as initial
Globular aggregates of acellular eosino- symptom of multiple myeloma. A case report. Oral
philic proteinaceous material distend Surg Oral Med Oral Pathol. 1980;49:18.
the surface epithelium and are deposited Guccion FG, Redman RS, Winne CE. Hemodialysis-
within the underlying connective tis- associated amyloidosis presenting as lingual nodules.
Oral Surg Oral Med Oral Pathol. 1989;68:618.
sues. Amyloid with β-pleated structure Kraut RA, Buhler JE, LaRue JR, Acevedo A. Amyloidosis
shows Congo red staining with polar- associated with multiple myeloma. Oral Surg Oral
ization microscopy resulting in green Med Oral Pathol. 1977;43:63.
birefringence.
DIFFERENTIAL DIAGNOSIS HYALINOSIS CUTIS
Large nodular deposits causing macroglos- ET MUCOSAE (LIPOID
sia are usually observed, and these features PROTEINOSIS)
do not closely parallel those seen in the Figure 7-27
other papular or multiple polypoid lesions
listed here. Microscopically, amyloidosis Age: Young adults
resembles hyalinosis cutis et mucosae. A Sex: No predilection
biopsy along with Congo red staining pro- CLINICAL FEATURES
vide a definitive diagnosis.
Also known as lipoid proteinosis or the
Urbach-Wiethe syndrome, hyalinosis cutis
TREATMENT
et mucosae represents a rare autosomal
Once amyloidosis is diagnosed, a thorough recessive disorder involving many organ
medical work-up is indicated to uncover systems. It is caused by a mutation in the
myeloma or granulomatous disease. In the ECM1 gene (extracellular matrix). Diffuse
former, cytologic chemotherapeutic drugs deposits of hyaline glycoprotein and acid as
are prescribed. Large amyloid nodules well as neutral glycosaminoglycans occur in
interfering with speech or deglutition can the mucosal tissues, skin, and vessel walls.
be removed surgically. Deposits are also found in the brain with
PMPH_Eversole_Chapter-07.indd 291 1/20/2011 2:52:10 PM
292 Chapter 7
be performed. The clinical findings in con-
junction with microscopic and histochemi-
cal findings provide a definitive diagnosis.
TREATMENT
There is no known treatment for this syn-
drome. Most patients enjoy normal longev-
ity of life. Gingivectomy is recommended
when diffuse hyperplastic-appearing gin-
gival infiltration is present.
Additional Reading
FIGURE 7-27 Finkelstein MW, Hammond HL, Jones RB. Hyalinosis
Multiple gingival papules in hyalinosis cutis et cutis et mucosae. Oral Surg Oral Med Oral Pathol.
mucosae. 1982;54:49.
Laymon CW, Hill EM. An appraisal of hyalinosis cutis et
mucosae. Arch Dermatol. 1967;75:55.
Lupo I, Cefalu AB, Bongiorno MR, et al. A novel muta-
calcifications of the dorsum sellae. The oral tion of the extracellular matrix protein 1 gene (ECM1)
in a patient with lipoid proteinosis (Urbach-Wiethe
tissues show infiltrated plaques, papules, disease) from Sicily. Br J Dermatol. 2005;153(5):
and nodules that are yellowish white and 1019-1022.
are distributed in multiple array over the Simpson HE. Oral manifestations in lipoid proteinosis.
lips, tongue, buccal mucosa, and pharynx Oral Surg Oral Med Oral Pathol. 1972;33:528.
Williams R. Lipoid proteinosis (report of a case). Oral
with occasional gingival involvement. The Surg Oral Med Oral Pathol. 1971;31:624.
larynx is frequently involved as well. Cuta-
neous lesions may commence as vesicles;
on healing, acneform scars develop. Sub-
sequently, pale yellow nodules may form. HEMANGIOMA/
The face, neck, and eyelids are most often LYMPHANGIOMA
involved. Hypodontia involving the maxil- Figure 7-28
lary lateral incisors and premolars is also a
feature of the syndrome. Age: Children and young adults
Sex: No predilection
CLINICAL FEATURES
MICROSCOPIC FEATURES
A biopsy of one of the mucosal nodules Both blood and lymph vessel hamartomas
shows diffuse connective tissue hyaliniza- may appear as diffuse polypoid masses
tion with prominent hyaline perivascular yielding a grape cluster configuration.
cuffing. These deposits are PAS positive These lesions are most often observed on
and show equivocal reactions for amyloid. the tongue and buccal mucosa. Heman-
giomas are red, blue, or purple, whereas
lymphangiomas often mimic a mass of clus-
DIFFERENTIAL DIAGNOSIS tered vesicles. Most vascular hamartomas
Neuropolyendocrine syndrome, focal epi- are present from early childhood; however,
thelial hyperplasia, Cowden syndrome, and some lesions do not begin to proliferate
amyloidosis may show similar clinical fea- until the patient is in the second decade of
tures. A dermatologic examination should life.
PMPH_Eversole_Chapter-07.indd 292 1/20/2011 2:52:13 PM
Papillary, Papular, and Multiple Polypoid Lesions 293
MICROSCOPIC FEATURES Goldberg MH, Nemarich AN, Danielson P.
Lymphangioma of the tongue: medical and surgical
Racemose exophytic papules are covered therapy. J Oral Maxillofac Surg. 1977;35: 841.
by a thin layer of stratified squamous epithe- Shklar G, Meyers I. Vascular tumors of the mouth
lium, which is distended by dilated, endothe- and jaws. Oral Surg Oral Med Oral Pathol.
1965;19:335.
lium-lined vascular channels. These channels
Toida M, Hasegawa T, Watanabe F, et al. Lobular cap-
usually extend into the deeper connective tis- illary hemangioma of the oral mucosa: clinicopatho-
sues and may course between skeletal mus- logical study of 43 cases with a special reference to
cle fibers. In hemangioma, the vascular chan- immunohistochemical characterization of the vascu-
nels are filled with erythrocytes, whereas lar elements. Pathol Int. 2003;53(1):1-7.
lymphangiomas are represented by ectatic
vessels filled with an eosinophilic coagulum.
MULTIPLE ENDOCRINE
DIFFERENTIAL DIAGNOSIS
NEOPLASIA, TYPE IIB
Most of the vascular hamartomas are Figure 7-29
distinctive and are not often confused
clinically with other diffuse papular and Age: Teenagers and young adults
polypoid lesions. The clustered grape pat- Sex: No predilection
tern and localization are typical features. CLINICAL FEATURES
Nevertheless, a biopsy should be procured
to confirm the clinical impression. Inherited as an autosomal dominant trait,
the neuropolyendocrine syndrome or multi-
TREATMENT ple endocrine neoplasia, type IIb represents
one of the phakomatoses in that the lesions
Hemangiomas and lymphangiomas may be
do not evolve until the second decade or late
treated by injection of sodium morrhuate
childhood. There is a mutation in the RET
as a sclerosing agent or excised by scalpel
gene. Numerous forms of multiple endo-
or electrocautery. The surgeon should bear
crine neoplasia (MEN) are known; type IIb
in mind the tendency for these lesions to
shows oral lesions. The oral manifestations
extend into underlying muscle.
are multiple isolated polyps or nodules on
the lips, tongue, and eyelids that represent
Additional Reading plexiform neuromatous hamartomas. These
neural tumors are also seen on the eyelids.
Dingman RO, Grabb WC. Lymphangioma of the tongue. A Marfanoid facies is present. The impor-
Plast Reconstr Surg. 1961;27:214.
Flaitz CM. Oral and maxillofacial pathology case of the
tance of uncovering this syndrome lies with
month. Lymphangioma. Tex Dent J. 2000;117(4):65, the more serious manifestations that coex-
112-113. ist, including malignant tumors of various
FIGURE 7-28
Lymphangioma with pebbly
surface (left), hemangioma
showing grape-like clus-
tered papules (right).
PMPH_Eversole_Chapter-07.indd 293 1/20/2011 2:52:13 PM
294 Chapter 7
FIGURE 7-29
Multiple papular neuromas
of the tongue accompanied
by medullary carcinoma
of the thyroid and adrenal
pheochromocytoma.
endocrine glands. Adrenal pheochromocy- mas, pheochromocytoma, and medullary thyroid
toma and medullary carcinoma of the thy- carcinoma. Oral Surg Oral Med Oral Pathol.
1971;31:206.
roid are the most frequently encountered Kouvaraki MA, Shapiro SE, Perrier ND, et al. RET
cancers. proto-oncogene: a review and update of genotype-
phenotype correlations in hereditary medullary thy-
roid cancer and associated endocrine tumors. Thyroid.
MICROSCOPIC FEATURES
2005;15:531-544.
The oral neuromas are characterized by an Raue F, Frank-Raue K. Update multiple endocrine neo-
plasia type 2. Fam Cancer. 2010 Jan 20. [Epub ahead
organoid, plexiform arrangement of nerve
of print.]
and nerve sheath elements similar to those Schimke RN, Hartmann WH, Prout TE, Rimoin DL.
of traumatic neuroma. The neural elements Syndrome of bilateral pheochromocytoma, medullary
are enveloped by perineurium and are thyroid carcinoma and multiple neuromas. A possible
separated from one another by intervening regulatory defect in the differentiation of chromaffin
tissue. N Engl J Med. 1968;279:1.
fibrous stroma. Williams ED, Pollack DJ. Multiple mucosal neuroma-
ta with endocrine tumors; a syndrome allied to von
DIFFERENTIAL DIAGNOSIS Recklinghausen’s disease. J Pathol. 1966;91:71.
Multiple mucosal neuromas of the Sipple
syndrome may clinically simulate focal DENTAL LAMINA CYSTS
epithelial hyperplasia and Crohn’s disease.
Biopsy discloses their true nature. Figure 7-30
Age: Infancy
TREATMENT Sex: No predilection
The oral lesions may be excised or left CLINICAL FEATURES
untreated once a diagnosis is obtained.
Developmental soft tissue cysts arise in var-
Referral to an internist is recommended to
ious locations of the oral mucosa and ulti-
detect or anticipate the occurrence of endo-
mately involute or are shed within 6 months.
crine malignancies.
They appear as small white pearly nodules
measuring less than 2 to 4 mm and tend to
Additional Reading be multiple. When on the alveolar mucosa
prior to tooth eruption they are referred
Bartlett RC, Myall RW, Bean LR, Mandelstam P. A to as dental lamina cysts where they are
neuropolyendocrine syndrome: mucosal neuro- thought to originate from epithelial rests of
PMPH_Eversole_Chapter-07.indd 294 1/20/2011 2:52:18 PM
Papillary, Papular, and Multiple Polypoid Lesions 295
FIGURE 7-30
Multiple alveolar ridge pap-
ules in a neonate represent-
ing dental lamina cysts.
the nascent tooth germ, the dental lamina. TREATMENT
Epstein’s pearls are multiple and are located None necessary
in the midline of the palate whereas Bohn’s
nodules are similar yet reside in the palate
off the midline. Additional Reading
Alves KM, Peixoto V, Gomide MR, de Carvalho Carrara
MICROSCOPIC FEATURES CF, Costa B. Prevalence of palatal and alveolar cysts in
These tiny cysts are represented by multiple babies with cleft lip and palate. Cleft Palate Craniofac
J. 2004;41:490-493.
nodules of stratified squamous epithelium Faridi MM, Adhami S. Prepucial Epstein pearls. Indian
with lumens filled with keratin. J Pediatr. 1989;56:653-655.
Hayes PA. Hamartomas, eruption cyst, natal tooth and
DIFFERENTIAL DIAGNOSIS Epstein pearls in a newborn. ASDC J Dent Child.
2000;67:365-368.
MENIIb may be considered as may focal Kumar A, Grewal H, Verma M. Dental lamina cyst of
epithelial hyperplasia. Nevertheless the newborn: a case report. J Indian Soc Pedod Prev Dent.
2008;26(4):175-176.
confinement to the alveolus, small size, Lewis DM. Bohn’s nodules, Epstein’s pearls, and gingi-
and occurrence at birth allow for easy val cysts of the newborn: a new etiology and classifica-
recognition. tion. J Okla Dent Assoc. 2010;10:32-33.
PMPH_Eversole_Chapter-07.indd 295 1/20/2011 2:52:21 PM
a b c
Cyst Mesenchymal neoplasm Adnexal skin tumor
d e f
Glandular neoplasm Epithelial neoplasm Sialadenitis
g h i
Lymphadenitis Lymph node metastasis Expansile osseous neoplasm
Extraoral Swellings
PMPH_Eversole_Chapter-08.indd 296 1/17/2011 3:38:34 PM
Soft Tissue Swellings
of the Neck and Face 8
MISCELLANEOUS ADENOMAS 325
Lateral Neck Swellings 300
ADENOID CYSTIC CARCINOMA 326
BRANCHIAL CLEFT CYST 300 MUCOEPIDERMOID
CERVICAL RIB AND TRANSVERSE CARCINOMA 327
PROCESS 301 ACINIC CELL CARCINOMA 329
NONSPECIFIC LYMPHADENITIS 301 ADENOCARCINOMA NOS AND
INFECTIOUS MONONUCLEOSIS 303 MISCELLANEOUS
TUBERCULOUS LYMPHADENITIS MALIGNANCIES 330
(SCROFULA) 304
CAT-SCRATCH FEVER 305 Bilateral Parotid and
ACTINOMYCOSIS 306 Submandibular Swellings 332
REACTIVE PROLIFERATIONS 307
ENDEMIC PAROTITIS (MUMPS) 332
SINUS HISTIOCYTOSIS 308
SJÖGREN’S SYNDROME 333
BENIGN MESENCHYMAL
MIKULICZ’S DISEASE 334
TUMORS 309
SARCOID SIALADENITIS AND
CYSTIC HYGROMA
HEERFORDT’S SYNDROME 335
(LYMPHANGIOMA) 310
TUBERCULOSIS 336
CAROTID BODY TUMOR
(CHEMODECTOMA) 311 HIV SALIVARY DISEASE (DIFFUSE
INFILTRATIVE LYMPHOCYTOSIS
METASTATIC CARCINOMA 312
SYNDROME) 337
SARCOMAS 314
DYSGENETIC CYSTS OF THE
MALIGNANT LYMPHOMA 315 PAROTID 338
METABOLIC SIALADENOSIS 339
Unilateral Parotid and PAPILLARY CYSTADENOMA
Submandibular Swellings 316 LYMPHOMATOSUM*
ACUTE SIALADENITIS (SURGICAL
MUMPS) 316
Midline Neck Swellings 340
SIALOLITHIASIS AND OBSTRUCTIVE THYROGLOSSAL TRACT CYST 340
SIALADENITIS 317 GOITER 341
CHRONIC SIALADENITIS 318 THYROID NEOPLASIA 342
INTRAPAROTID MESENCHYMAL DERMOID CYST 343
TUMORS 319
LYMPHOMA 320 Growths and Swellings
PLEOMORPHIC ADENOMA 322 of the Facial Skin 344
PAPILLARY CYSTADENOMA
LYMPHOMATOSUM 323 NEVI 344
ONCOCYTOMA 324 SEBACEOUS CYST 345
PMPH_Eversole_Chapter-08.indd 297 1/17/2011 3:38:39 PM
SEBORRHEIC KERATOSIS 346 EMPHYSEMA 355
ADNEXAL SKIN TUMORS 347 ANGIONEUROTIC EDEMA 356
BASAL CELL CARCINOMA 348 CUSHING’S SYNDROME 357
SQUAMOUS CELL CARCINOMA 350 FACIAL HEMIHYPERTROPHY 358
KERATOACANTHOMA 351 FIBROUS DYSPLASIA AND OTHER
MESENCHYMAL TUMORS 352 BONE LESIONS 359
MALIGNANT MELANOMA 353 MASSETERIC HYPERTROPHY 360
Diffuse Facial Swellings 354
*See Unilateral Parotid and Submandib-
CELLULITIS AND SPACE ular Swellings
INFECTIONS 354
PMPH_Eversole_Chapter-08.indd 298 1/17/2011 3:38:39 PM
As with swellings located anywhere in the duce asymmetry and may be caused by
body and particularly in the subcutaneous soft tissue enlargement or expansion of the
tissues, neck and facial swellings may rep- underlying osseous tissue of the maxilla or
resent neoplasms, inflammatory disorders, mandible.
hyperplastic reactions, or developmental When extraoral swellings are encoun-
defects. If the mass is painful or tender, soft tered, a source of disease should be sought.
and movable, and associated with fever, the Infections of the upper air passages or
process is probably inflammatory. If the odontogenic infection are the most com-
mass is painless, well circumscribed, soft or mon causes of lymphadenopathy in the
firm yet not indurated, and can be grasped neck. The work-up should consist of physi-
and moved freely, a benign neoplastic or cal evaluation of the mass itself, noting its
reactive process should be foremost in the location, consistency, relationship to adja-
mind of the examiner. Indurated fixed swell- cent tissues, and whether or not it is ten-
ings with a history of progressive enlarge- der. The patient’s temperature should be
ment are prime suspects for malignancy. obtained. A complete oral soft tissue exami-
Anatomic localization of the tumefac- nation should be performed; if it yields neg-
tion is perhaps the most germane consider- ative results, the larynx, nasopharynx, and
ation when attempting to diagnose masses nasal cavity should be inspected. The denti-
in the head and neck region. In this chap- tion should be evaluated for necrotic teeth
ter, the nosology of extraoral swellings is and periodontal abscesses. Radiographs of
approached in this fashion. The rationale for the jaw and, if all else proves negative or if
grouping lesions according to site rests with symptoms warrant, sinus radiographs and
regional anatomic considerations. For exam- tomograms may be ordered. If no source
ple, the lateral neck is riddled with lymph of disease can be found and the mass fails
nodes; most swellings in the lateral neck, to resolve in 2 weeks, the patient should
located along the course of the sternomas- be referred to an appropriate specialist for
toid muscle, include developmental cysts, biopsy.
specific infectious diseases of lymphoid The most frequently encountered lat-
tissue, and various mesenchymal and lym- eral neck swellings are lymphadenitis of
phoid neoplasms. Midline neck swellings dental origin, infectious mononucleosis,
are more likely to represent thyroid disease. lipoma, metastatic tumor, and lymphoma.
Swellings located at the mandibular angle The latter two, as well as sarcoma and
or just anterior to the ear in the parotid tuberculosis, are potentially lethal.
region are usually salivary neoplasms or The most common midline neck swell-
inflammatory diseases of the parotid gland. ings are goiter and thyroglossal tract cyst.
When a swelling of the parotid region is Thyroid carcinoma is potentially lethal.
detected and the mass is clinically consis- Common parotid region swellings include
tent with neoplasia, fine-needle aspiration obstructive sialadenitis, pleomorphic
cytology should be considered. If the cyto- adenoma, and adenocarcinoma, the latter
logic findings are equivocal, the preferred being potentially life-threatening. Local-
approach is to perform a partial lobectomy ized facial swellings generally represent
and obtain frozen sections at the time of the nevi, sebaceous cyst, seborrheic keratosis,
operation. Depending on the diagnosis, this or basal cell carcinoma. The latter may be
procedure may be adequate or further sur- lethal if left untreated. The most common
gery may be indicated. diffuse facial swellings are cellulitis and
Localized swellings on the facial skin underlying expansile bone lesions such as
often represent skin adnexal or dermal fibrous dysplasia or benign intraosseous
neoplasms. Diffuse facial swellings pro- neoplasms.
PMPH_Eversole_Chapter-08.indd 299 1/17/2011 3:38:39 PM
300 Chapter 8
has been reported to occur from the lining
Lateral Neck Swellings of such cysts; however, the probability that
the carcinoma represents metastatic dis-
BRANCHIAL CLEFT CYST ease to nodal tissue from an upper respira-
Figure 8-1 tory or facial skin primary tumor must be
considered.
Age: Onset in childhood or early adulthood
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
The compressible, movable mass of bran-
The lymphoepithelial or branchial cleft cyst chial cleft cyst must be differentiated from
is believed to be derived from epithelial benign mesenchymal neoplasms, spe-
remnants of the embryonic branchial clefts cific infectious lymphadenitis, and carotid
that become entrapped within cervical body tumors. Lymphomas may also,
lymph nodes. An alternative theory impli- albeit rarely, show clinical features of a
cates intranodal entrapment of salivary benign lesion. Biopsy affords a definitive
epithelial elements. The cyst may reach diagnosis.
impressive proportions and can be located
anywhere along the anterior surface of the TREATMENT
sternomastoid muscle within the subcu-
The lesion may be excised.
taneous tissues. It is doughy or firm and
movable on palpation. Rarely, cysts similar
to the branchial cleft cyst, yet derived from Additional Reading
cervically migrating thymus or parathyroid
Bhaskar SN, Bernier JL. Histogenesis of branchial cysts;
anlagen, localize in the lateral neck.
a report of 468 cases. Am J Pathol. 1959;35:407.
Khafif RA, Prichep R, Minkowitz S. Primary branchio-
MICROSCOPIC FEATURES genic carcinoma. Head Neck. 1989;11:153.
Pietarinen-Runtti P, Apajalahti S, Robinson S, Passador-
The cyst lining consists of either stratified Santos F, Leivo I, Mäkitie AA. Cystic neck lesions:
squamous or respiratory epithelium or clinical, radiological and differential diagnostic consid-
alternating zones of both. The cyst wall is erations. Acta Otolaryngol. 2010;130:300-304.
Proctor B. Lateral vestigial cysts and fistulas of the neck.
composed of lymphoid tissue, which often Laryngoscope. 1955;65:355.
contains germinal centers. Carcinomatous Rickles NH, Little JW. The histogenesis of the branchial
change (so-called branchiogenic carcinoma) cyst. Am J Pathol. 1967;50:533, 765.
FIGURE 8-1
Branchial cleft cyst, a compress-
ible, movable mass overlying the
sternomastoid.
PMPH_Eversole_Chapter-08.indd 300 1/17/2011 3:38:40 PM
Soft Tissue Swellings of the Neck and Face 301
CERVICAL RIB AND DIFFERENTIAL DIAGNOSIS
TRANSVERSE PROCESS The rock-hard character of a cervical rib may
Figure 8-2 allow for easy confusion with lymphoma,
primary sarcoma, or metastatic carcinoma.
Age: Childhood onset A radiograph of the neck quickly eliminates
Sex: No predilection these from consideration.
CLINICAL FEATURES
Although rare, an extension of the transverse TREATMENT
process of a cervical vertebra may appear as No treatment is necessary.
an anomalous rib. Clinically, a bone-hard
swelling can be palpated directly behind
the sternomastoid muscle or in the parotid
region. To the unwary examiner, the lump
Additional Reading
has all the features of malignant or meta- Einstein RA, Katz AD. Parotid area swelling caused
by a prominent transverse process of atlas. Arch
static disease. An anteroposterior radio- Otolaryngol. 1975;101:558.
graph through the neck discloses the pres- Flemming MC, Kellman GM, Haggar AM. Cervical rib:
ence of the elongated transverse process. a cause of supraclavicular mass on MR imaging. AJR A
Occasionally, symptoms may accompany J Roentgenol. 1989;153:1102.
Gray H, Goss CM. Anatomy of the Human Body (Gray’s
this anomaly as a result of neurovascular
Anatomy). 29th ed. Philadelphia, PA. Lea & Febiger;
compression in the region of the branchial 1973:119, 132.
plexus and subclavian vessels. Neural com- Leong SC, Karkos PD. A “hard” neck lump. Singapore
pression may result in neuralgia, paresthe- Med J. 2009;50:e141-e142.
sia, and paralysis of the skin in the areas Match RM. Neck mass caused by a cervical rib. J Pediatr.
1978;92:508.
supplied by the eighth cervical and first
thoracic nerves. These latter symptoms are
usually seen with a cervical rib from C7, NONSPECIFIC
which is not palpable.
LYMPHADENITIS
MICROSCOPIC FEATURES Figure 8-3
Not applicable. Age: No predilection
Sex: No predilection
CLINICAL FEATURES
Tender soft-to-firm swellings of the lat-
eral neck are usually indicative of regional
lymphadenopathy subsequent to upper
respiratory or odontogenic infection. The
swellings are often bilateral when upper
respiratory inflammation occurs and are
generally unilateral in the face of acute
odontogenic or periodontal inflamma-
tion. The upper cervical nodes located just
inferior to the angle of the mandible are
FIGURE 8-2 most frequently affected by this reactive
Cervical rib emanating from lower cervical verte- hyperplastic swelling. The patient is usu-
bra. Similar anomalies on the upper cervical verte- ally slightly or moderately febrile. A search
brae are palpable. should be made for inflammatory change
PMPH_Eversole_Chapter-08.indd 301 1/17/2011 3:38:54 PM
302 Chapter 8
in the pharynx or oropharynx; tonsillar of necrosis are seen along with histiocytic
enlargement is often present. A variety of infiltration of the node. In Kawasaki dis-
specific viral or bacterial infectious diseases ease, sinus histiocytosis is observed along
may be responsible. In the absence of upper with necrotizing arteritis.
respiratory infection, the dentition should
be evaluated clinically and radiographically DIFFERENTIAL DIAGNOSIS
to disclose the presence of pulpal or peri- Soft tender swellings, typical of cervical
odontal inflammatory disease. Two specific lymphadenopathy, must be differentiated
diseases with cervical lymphadenitis and from specific inflammatory lymphaden-
fever are Kikuchi-Fujimoto disease, a lesion itides such as infectious mononucleosis,
with specific histology that is probably viral cat-scratch fever, actinomycosis, and tuber-
in origin and can persist for many months, culous lymphadenitis. The latter two dis-
and Kawasaki disease. Both of these condi- eases are often accompanied by fistulous
tions are probably viral induced and tend to tracts onto the skin surface. Failure of the
occur in Asian children. Kawasaki disease neck swellings to subside after conventional
is associated with potentially fatal coronary treatment for cervical lymphadenopathy
aneurysms and thrombosis; erythematous (i.e., control of upper respiratory infection
oral and lip lesions may be seen as well or odontogenic infection) warrants further
(mucocutaneous lymph node syndrome). work-up to rule out the aforementioned
entities. Fine-needle aspiration cytology is a
MICROSCOPIC FEATURES
less invasive diagnostic method than open
The lymph node is grossly enlarged and biopsy and has proven to be efficacious.
shows enlargement of the germinal centers.
The reticulum cells may show evidence of TREATMENT
mitosis, and a prominent lymphoid mantle Cervical lymphadenitis is a secondary reac-
is obvious. The medullary sinusoids are tive manifestation of infectious disease
impacted with small and large lympho- elsewhere. Throat infections should be
cytes. In Kikuchi-Fujimoto disease, areas managed by an otolaryngologist or gen-
eral physician. Periodontal infection should
be managed by surgery and/or curettage,
whereas pulpal infection can be treated by
therapeutic pulp canal exposure with sub-
sequent endodontics or extraction. If fever
is present, the patient should receive antibi-
otics, preferably penicillin (250 mg 4 times
daily for 7 days), and local control of the
infection should be instituted.
Additional Reading
Archibald DJ, Carlson ML, Gustafson RO. Kikuchi-
fujimoto disease in a 30-year-old caucasian female. Int
J Otolaryngol. 2009;2009:901537.
Parisi E, Glick M. Cervical lymphadenopathy in the den-
tal patient: a review of clinical approach. Quintessence
FIGURE 8-3 Int. 2005;36:423-436.
Nonspecific lymphadenitis associated with a Weidman B, Warman E. Lymph nodes of the head and
necrotic mandibular molar. neck. J Oral Pathol Med. 1980;35:39.
PMPH_Eversole_Chapter-08.indd 302 1/17/2011 3:38:56 PM
Soft Tissue Swellings of the Neck and Face 303
Hutchinson CB, Wang E. Kikuchi-Fujimoto disease. Persistent adenopathy and malaise, lasting
Arch Pathol Lab Med. 2010;134:289-293. for months or years, has been termed the
Yanagi S, Nomura Y, Masuda K, et al. Early diagnosis of
Kawasaki disease in patients with cervical lymphade- “chronic fatigue syndrome,” and although
nopathy. Pediatr Int. 2008;50:179-183. Epstein-Barr virus has been implicated as
a causal agent, a retrovirus has recently
become a suspect.
INFECTIOUS
MONONUCLEOSIS MICROSCOPIC FEATURES
Figure 8-4 Lymph nodes show hypertrophy with
hyperplasia of the germinal centers. Both
Age: Teenagers and young adults the germinal centers and medullary sinu-
Sex: No predilection soids contain epithelioid-appearing atypi-
CLINICAL FEATURES cal lymphocytes.
Caused by the Epstein-Barr virus, a form of
DIFFERENTIAL DIAGNOSIS
herpesvirus, infectious mononucleosis is a
relatively common infectious disease that is The enlarged nodes in infectious mononu-
transmitted by oral droplet contamination cleosis are usually bilateral. The presence
and frequently develops after kissing. It is of lymphadenopathy in conjunction with
not as contagious as many of the childhood intense pharyngitis and malaise must
exanthems. The disease is characterized by be differentiated from streptococcal sore
extreme malaise, intense painful pharyngi- throat, scarlet fever, diphtheria, and lym-
tis, and moderate-to-severe lymphadenopa- phoma. A swab culture may be obtained to
thy. The submandibular, upper cervical, rule out bacterial infection. The peripheral
and occipital lymph nodes may be enlarged, blood in infectious mononucleosis shows
are painful, and are usually soft or rubbery. atypical “Downey” lymphocytes, and the
Tonsillar enlargement and pharyngeal Paul-Bunnell or heterophil antibody titer
ulceration with formation of a pseudomem- is positive by the second or third week of
brane are evident. Petechial lesions of the the disease. EBER is detectable by DNA
soft palate are present in nearly one half in situ hybridization and confirms the
of the instances. The patients are febrile. diagnosis.
The disease persists from 2 to 5 weeks.
TREATMENT
Bed rest and supportive care with fluids,
soft diet, an anesthetic gargle, an analge-
sic-antipyretic, and systemic antibiotics to
control secondary bacterial pharyngitis are
recommended.
Additional Reading
Dunnett WN. Infectious mononucleosis. Br Med J.
1963;1:1187.
Fraser-Moodie W. Oral lesions in infectious mono-
nucleosis. Oral Surg Oral Med Oral Pathol.
1959;12:685.
FIGURE 8-4 Gulley ML, Tang W. Laboratory assays for Epstein-
Lymphadenitis in a patient with infectious mono- Barr virus-related disease. J Mol Diagn. 2008;10:
nucleosis. 279-292.
PMPH_Eversole_Chapter-08.indd 303 1/17/2011 3:39:02 PM
304 Chapter 8
Minagawa K, Okada T. Primary Epstein-Barr virus infec-
tion and cervical lymphadenopathy in childhood. Josai
Shika Daigaku Kiyo. 1986;15:450.
Ragab AH, Vietti TJ. Infectious mononucleosis, lym-
phoblastic leukemia, and the E B virus. Cancer.
1969;24:261.
TUBERCULOUS
LYMPHADENITIS (SCROFULA)
Figure 8-5
Age: Children and young adults
Sex: No predilection
CLINICAL FEATURES
The lateral neck is the most common loca- FIGURE 8-5
tion for tuberculous inflammation of lymph Tuberculous lymphadenopathy of cervical nodes.
nodes. As opposed to other mucocutaneous
manifestations of tuberculosis that are sec-
ondary to pulmonary disease, cervical node other specific granulomatous lymphadeniti-
tuberculosis or scrofula is often primary and des or benign neoplasms. The exudate can be
may be associated with a portal of entry in smeared and stained for acid-fast organisms,
the throat. It may be contracted by ingestion and definitive identification can be obtained
of contaminated milk. Although Mycobacte- by culture. A complete work-up to define the
rium tuberculosis is usually responsible, atypi- systemic extent of the disease is warranted.
cal tuberculosis may be acquired by infection
with less common strains of mycobacteria. TREATMENT
The lesion is located in the submandibular
The caseating granuloma can be excised;
or cervical nodes, is usually unilateral, and
however, this does not necessarily remove
eventually manifests exudative drainage
all infectious microorganisms. The patient
via a fistula. The swelling is initially pain-
requires conventional isoniazid therapy
less and on palpation is firm, generally mov-
and the care of a physician.
able, and of normal temperature, hence the
designation cold abscess. Mycobacteria can be
cultured from the exudate.
Additional Reading
MICROSCOPIC FEATURES Dandapat MC, Mishra BM, Dash SP, Kar PK. Peripheral
The lymph node is replaced by focal granu- lymph node tuberculosis: a review of 80 cases. Br J
Surg. 1990;77:911.
lomas evincing epithelioid cells and Lang- Kato T, Kimura Y, Sawabe M, Masuda Y, Kitamura K.
han’s giant cells. Caseation necrosis with Cervical tuberculous lymphadenitis in the elderly:
neutrophil infiltration is seen in fistulating comparative diagnostic findings. J Laryngol Otol.
lesions. Acid-fast bacilli are detected with 2009;123:1343-1347.
Knewitz FW, Devine KD, Waite DE. Differential diag-
the appropriate special stains. nosis of cervicofacial swellings. Oral Surg Oral Med
Oral Pathol. 1968;25:43.
DIFFERENTIAL DIAGNOSIS Mulay SG Hiranandani LH. A clinical study: surgi-
cal management of 250 cases of tuberculous cervical
The isolated swelling with fistula must be lymphadenitis. J Laryngol Otol. 1970;89:781.
differentiated from actinomycosis. When a Popowich L, Heydt S. Tuberculous cervical lymphadeni-
fistula is not present, scrofula may simulate tis. J Oral Maxillofac Surg. 1982;40:522.
PMPH_Eversole_Chapter-08.indd 304 1/17/2011 3:39:06 PM
Soft Tissue Swellings of the Neck and Face 305
CAT-SCRATCH FEVER nucleated giant cells that surround central
Figure 8-6 zones of granular eosinophilic necrotic
material. The organism may be demon-
Age: Children and young adults strable with a Wharthin-Starry or Giemsa’s
Sex: No predilection stain.
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
As the term implies, the disease is con-
tracted after scratch by a cat. Many patients The cervical swelling of cat-scratch fever
do not report a scratch, yet have been in must be differentiated from actinomyco-
contact with cats. The causative agent is sis, scrofula, and other rare granulomatous
Bartonella henselea, a cell-wall–defective lymphadenitides such as tularemia, lym-
gram-negative bacillus. A papule devel- phogranuloma venereum, atypical tuber-
ops in the zone of contact, with subsequent culosis, and neoplasms. A history of scratch
lymph node swelling in the region draining or contact with a cat is, of course, helpful in
the scratch site; other nodes may enlarge as making the diagnosis. A definitive diagno-
well. In the head and neck area, the sub- sis is obtained by noting a positive intracu-
mandibular, cervical, or occipital nodes are taneous reaction with Mollaret’s antigen or
involved. The nodes are sore, somewhat a positive complement-fixation test.
firm, and movable. Occasionally, a fistula is
encountered. Fever, malaise, headache, and TREATMENT
nausea become manifest early in the course
of the disease. The disease does not always respond to
antibiotics, although some patients may
benefit from gentamicin or cefoxitin. Sup-
MICROSCOPIC FEATURES
portive care with fluids, good diet, bed rest,
The involved node or nodes are replaced by and administration of antipyretics are rec-
focal granulomas that are characterized by ommended. Extremely tender nodes may
epithelioid histiocyte infiltration and multi- require incision with drainage.
FIGURE 8-6
Cervical lymphadenopathy
in cat-scratch fever.
PMPH_Eversole_Chapter-08.indd 305 1/17/2011 3:39:10 PM
306 Chapter 8
cervical-facial actinomycosis. Caused by
Additional Reading infection with Actinomyces israelii, actino-
English CK, Wear DJ, Margileth AM, Lissner CR, Walsh mycosis is characterized by a firm, often
GP. Cat-scratch disease. Isolation and culture of the indurated multinodular tumefaction that
bacterial agent. JAMA. 1988;259:1347. has a tendency to develop drainage. The
Florin TA, Zaoutis TE, Zaoutis LB. Beyond cat scratch exudate contains clumped colonies of the
disease: widening spectrum of Barto-nella henselae
infection. Pediatrics. 2008;121:e1413-e1425. microorganisms that appear crystalline
Gross BD, Case D. Cat scratch disease. Report of a case. and yellow, hence the term sulfur granules.
Oral Surg Oral Med Oral Pathol. 1977;43:698. The mass usually develops after trauma or
Margileth AM. Cat scratch disease: nonbacterial regional tooth extraction, which apparently provides
lymphadenitis. Pediatrics. 1968;42:803.
Rickles NH, Bernier JR. Cat-scratch disease. Oral Surg
a portal of entry for the fungus-like bacillus.
Oral Med Oral Pathol. 1960;13:282. The lesion develops within a few weeks to
months with slow progressive enlargement.
It is more frequently encountered among
ACTINOMYCOSIS
rural than urban inhabitants.
Figure 8-7
Age: Young adults MICROSCOPIC FEATURES
Sex: Male predilection The focus of inflammation is character-
CLINICAL FEATURES ized by surrounding fibroplasia with
extensive vascular proliferation. Focal
The submandibular and lateral neck regions
abscesses are distributed throughout and
are the most commonly involved areas in
are characterized by sheets of neutrophils
that surround amphophilic club-shaped
colonies that manifest a peripheral fringe.
These colonies are positively stained with
the periodic acid-Schiff technique. In the
early stages, microbial colonies may elicit
a granulomatous response with epithe-
lioid histiocytes and multinucleated giant
cells.
DIFFERENTIAL DIAGNOSIS
The indurated swelling of the neck seen
in actinomycosis is often “woody” and
must be differentiated from a neoplasm by
biopsy. Once a fistula has developed, suspi-
cion of actinomycosis is high. Nevertheless,
other lateral neck swellings with drainage,
such as scrofula or less common granu-
lomatous infections, must be considered as
possibilities. Identification of tiny yellow
sulfur granules (usually measuring less
than 2 mm) from the exudate or curettage
of the lesion is of diagnostic aid. Anaero-
FIGURE 8-7 bic methods of culture provide a definitive
Swollen cervical fistula in actinomycosis. diagnosis.
PMPH_Eversole_Chapter-08.indd 306 1/17/2011 3:39:32 PM
Soft Tissue Swellings of the Neck and Face 307
TREATMENT eral neck. These swellings are multinodular
Actinomyces infection responds to penicil- and firm but are usually somewhat mov-
lin therapy. High-dose therapy—10 to 20 mil- able within the surrounding tissues. They
lion units intravenously for 5 to 6 weeks—is often grow rapidly and may become large
required in many instances. Erythromycin if not removed. Clinically, they appear to
may be prescribed for patients with allergy represent neoplasms, yet are more likely to
to penicillin. evolve as a reaction to injury.
MICROSCOPIC FEATURES
Additional Reading All of the fibroproliferative reactions are
similar in their histomorphologic char-
Allen HA, Scatarige JC, Kim MH. Actinomycosis:
acteristics. Spindle cells are grouped into
CT findings in six patients. AJR Am J Roentgenol.
1987;149:1255. fascicles or form pinwheel-like swirls (sto-
Jones JE, Ladenheim S. Actinomycosis presenting as riform pattern) with variable amounts of
a deep neck infection. Trans Pa Acad Ophthalmol collagen. Epithelioid or foam cell histiocytes
Otolaryngol. 1987;39:643. are often present but are usually sparse and
Perlstein WH. Cervico-facial actinomycosis. N Engl J
Med. 1963;248:67. randomly distributed among fibroblastic
Rud J. Cervicofacial actinomycosis. J Oral Maxillofac cells. Many of these tumors are cellular and,
Surg. 1967;25:229. under these circumstances, may closely
Vernon V, Pranav G, Palande D. Actinomycosis of the mimic sarcoma.
neck causing cervical epidural cord compression. ‘A
case report and review of literature’. Spinal Cord.
2007;45:787-789. DIFFERENTIAL DIAGNOSIS
Reactive proliferations are clinically indis-
tinguishable from a variety of mesenchy-
REACTIVE PROLIFERATIONS mal neoplasms, actinomycosis, or specific
Figure 8-8 granulomatous enlargements. They may
be indurated and suggest lymphoma, sar-
Age: Children and young adults
coma, or metastatic disease. Multinodu-
Sex: No predilection
larity is suggestive of a reactive prolifera-
CLINICAL FEATURES tion. A biopsy is required for a definitive
Various fibroproliferative lesions such as diagnosis.
fibromatosis, myofibromatosis, pseudos-
arcomatous fasciitis, and dermatofibrosar- TREATMENT
coma protuberans, collectively grouped Although encapsulation is common, a
as the fibrous histiocytomas, often arise merging with adjacent fascia or connective
within the subcutaneous tissues of the lat- tissue is also frequently encountered. For
FIGURE 8-8
Fibrous histiocytoma of the
lateral neck (left), fibroma-
tosis with calcification (right
radiograph).
PMPH_Eversole_Chapter-08.indd 307 1/17/2011 3:39:37 PM
308 Chapter 8
this reason, wide local excision is gener- anorexia and malaise, are not present. Neu-
ally required to eradicate the disease and trophilic leukocytosis, elevated erythrocyte
circumvent recurrence. Combination radia- sedimentation rate, normocytic anemia, and
tion and chemotherapy has been successful hypergammaglobulinemia are present.
in patients with extensive disease. The disease persists for months or even
years, shows no tendency for malignant
Additional Reading change, and eventually undergoes sponta-
neous resolution. Elevated antibodies to the
Beck JC, Devaney KO, Weatherly RA, Koopmann CF, Epstein-Barr virus have been demonstrated
Jr, Lesperance MM. Pediatric myofibromatosis of the in this disease, yet a cause-and-effect rela-
head and neck. Arch Otolaryngol Head Neck Surg. tionship has not been proven.
1999;125:39-44.
Price EG, Jr, Silliphant WM, Shuman R. Nodular fascii-
tis; a clinicopathologic analysis of 65 cases. Am J Clin MICROSCOPIC FEATURES
Pathol. 1961;35:122.
Taylor HB, Helwig EB. Dermatofibrosarcoma protuber- Capsular fibrosis is a constant finding. The
ans; a study of 115 cases. Cancer. 1962;15:717. lymph node architecture is obliterated by
Werning JT. Nodular fascitis of the orofacial region. Oral dilated sinusoids lined by oval histiocytes
Surg Oral Med Oral Pathol. 1979;48:441.
West CB, Jr, Shagets FW, Mansfield MT. Nonsurgical
with abundant granular or foamy cytoplasm;
treatment of aggressive fibromatosis in the head and multinucleated forms are common. A hall-
neck. Otolaryngol Head Neck Surg. 1989;101:338. mark of the disease is a tendency for phagocy-
tosis of both lymphocytes and erythrocytes.
SINUS HISTIOCYTOSIS
DIFFERENTIAL DIAGNOSIS
Figure 8-9
Bilateral multinodular lymphoid swelling
Age: Children seen in sinus histiocytosis must be differ-
Sex: No predilection entiated from similar changes encountered
CLINICAL FEATURES
Sinus histiocytosis with massive lymphade-
nopathy is a childhood disease that occurs
more frequently among Blacks than among
Whites. The affected children show enlarge-
ment of the cervical and submandibular
nodes, usually bilaterally, and these nodal
swellings often reach massive proportions.
The neck is distended by bosselated, nodu-
lar confluent masses that are firm, pain-
less, and may become fixed to adjacent tis-
sues. Other node groups (axillary, inguinal,
hilar, and retroperitoneal lymph nodes)
often show enlargement; however, the size
is not comparable to that of the cervical
adenopathies. Cutaneous nodules and lytic
FIGURE 8-9
lesions of long bones occur in 30% to 40%
Sinus histiocytosis with massive lymphadenopathy of
of affected individuals and gallium scan- the cervical lymph nodes. Source: Rosai J, Dorfman
ning often discloses skeletal lesions. Fever RF. Sinus histiocytosis with massive lymphade-
is a constant finding; however, other consti- nopathy: a pseudolymphomatous benign disorder.
tutional signs of infectious disease, such as Analysis of 34 cases. Cancer. 1972;30:1174.
PMPH_Eversole_Chapter-08.indd 308 1/17/2011 3:39:49 PM
Soft Tissue Swellings of the Neck and Face 309
in other infectious lymphadenitides such as Rosai J, Dorfman RF. Sinus histiocytosis with
tuberculosis or cat-scratch fever, malignant massive lymphadenopathy: a pseudolymphoma-
tous benign disorder. Analysis of 34 cases. Cancer.
lymphoma, and metastatic carcinoma. The 1972;30:1174.
absence of positive skin tests for specific Walker PD, Rosai J, Dorfman RF. The osseous manifes-
microorganisms, presence of fever without tations of sinus histiocytosis with massive lymphade-
malaise, and laboratory data as designated nopathy. Am J Clin Pathol. 1981;75:131.
earlier point to a diagnosis of sinus histio-
cytosis. Biopsy discloses the characteristic
features. BENIGN MESENCHYMAL
TUMORS
TREATMENT
Figure 8-10
Neither antibiotics nor steroids show any
therapeutic value. Radiation therapy like- Age: Adults
wise is of no benefit in reducing the size of Sex: Depends on specific histologic type
the tumefactions. Because the etiology is CLINICAL FEATURES
essentially unknown, no treatment can be
rendered. The lesions eventually regress, A variety of connective tissue tumors arise
even though the disease persists for many in the lateral neck region. The more com-
months or even years. mon forms are lipoma, neurilemmoma,
neurofibroma, and lymphangioma (cystic
hygroma). Plexiform neurofibromas and
Additional Reading schwannomas may present in the context
of neurofibromatosis type 1. The mass is
Azoury FJ, Reed RJ. Histiocytosis. N Engl J Med. either soft or firm, yet not indurated, and is
1966;274:928.
La Barge DV, 3rd, Salzman KL, Harnsberger HR, et movable on palpation. The neoplasms are
al. Sinus histiocytosis with massive lymphadenopa- slow growing and are usually painless. If
thy (Rosai-Dorfman disease): imaging manifesta- left untreated, they may become quite large.
tions in the head and neck. AJR Am J Roentgenol. Ulceration, surface telangiectasia, and fistu-
2008;191:W299-W306.
McAlister WH, Herman T, Dehner LP. Sinus histiocy-
lization of the overlying skin are extremely
tosis with massive lymphadenopathy (Rosai-Dorfman rare with benign mesenchymal neoplasms.
disease). Pediatr Radiol. 1990;20:425. Computed tomography (CT), magnetic
FIGURE 8-10
Neurofibroma in NF1
appearing as a lateral neck
mass (left); lipoma (right).
PMPH_Eversole_Chapter-08.indd 309 1/17/2011 3:39:50 PM
310 Chapter 8
resonance imaging (MRI), and sonography CYSTIC HYGROMA
are useful diagnostic tools for determining (LYMPHANGIOMA)
location and extent of disease. Figure 8-11
MICROSCOPIC FEATURES Age: Infancy and childhood
Sex: No predilection
The histomorphologic features vary depend-
ing on the tissue cell of origin. Nearly all are CLINICAL FEATURES
well differentiated and have well-defined Cystic hygroma is considered separately
margins or are encapsulated. Lipomas are from the other benign mesenchymal neo-
tumor masses composed of normal adipose plasms because of its propensity to arise
tissue, whereas the neural sheath neoplasms in the soft tissues of the neck in children.
are composed of benign-appearing spindle The tumor mass may be present at birth or
cells associated with varying amounts of develop during the early childhood years.
collagen. It may reach large proportions, becoming
pendulous. The mass is soft and pliable on
DIFFERENTIAL DIAGNOSIS palpation. The neoplastic lymphatic chan-
nels may infiltrate between muscle and the
The firm or soft movable nonulcerated
contiguous soft tissues, thus making it dif-
mass representing a benign mesenchymal
ficult to determine the extent of the condi-
neoplasm must be differentiated from bran-
tion; however, CT, MRI, and lymphatic scin-
chial cleft cyst, carotid body tumor, and
tigraphy are useful in the determination of
nonfistulating granulomatous inflamma-
extent of disease. Patients with Down’s and
tions of lymph nodes. Biopsy is required to
Turner syndromes have a predilection for
obtain a definitive diagnosis.
cystic hygroma of the neck.
TREATMENT
Practically all benign mesenchymal neo-
plasms of the neck can be treated by con-
servative surgical excision. For most, recur-
rence rates after simple excision are low.
Additional Reading
Batsakis JG, Regezi JA, Rice DH. The pathology of head
and neck tumors: fibroadipose tissue and skeletal mus-
cle. Part 8. Head Neck Surg. 1980;3:45.
Berg JC, Scheithauer BW, Spinner RJ, Allen CM, Koutlas
IG. Plexiform schwannoma: a clinicopathologic over-
view with emphasis on the head and neck region. Hum
Pathol. 2008;39:633-640.
Gritzmann N, Schratter M, Traxler M, Helmer M.
Sonography and computed tomography in deep cervi-
cal lipomas and lipomatosis of the neck. J Ultrasound
Med. 1988;7:451.
Hawkins DB, Luxford WM. Schwannomas of the
head and neck in children. Laryngoscope. 1980;90:
1921. FIGURE 8-11
Oberman HA, Sullenger G. Neurogenous tumors of the Lymphangioma (cystic hygroma) of the neck in an
head and neck. Cancer. 1967;20:1992. infant.
PMPH_Eversole_Chapter-08.indd 310 1/17/2011 3:40:09 PM
Soft Tissue Swellings of the Neck and Face 311
MICROSCOPIC FEATURES hygroma. Biopsy is required for a definitive
Cystic hygroma is composed of dilated diagnosis.
endothelium-lined lymphatic channels.
The channels lie in juxtaposition to one TREATMENT
another with little intervening fibrous The mass requires surgical excision with
stroma. Infiltration of adjacent tissues is careful dissection from surrounding tis-
common; however, the endothelial cells sues, which it may infiltrate. Intralesional
show no signs of cellularity, pleomorphism, injection with OK-432 sclerosing agent has
or hyperchromatism. shown favorable results.
DIFFERENTIAL DIAGNOSIS
Cystic hygroma must be differentiated Additional Reading
from branchial cleft cyst, sinus histiocyto- Batsakis JG, Rice DH. The pathology of head and neck
sis, and lipoma. When the mass is small, tumors: vasoformative tumors, Part 9A, B. Head Neck
it may simulate one of the specific granu- Surg. 1981;3:231, 326.
lomatous inflammations such as tubercu- Bill AH, Jr, Summer DS. A unified concept of lymp-
hangioma and cystic hygroma. Surg Gynecol Obstet.
losis. When a large, soft, pliable mass is 1965;120:79.
detected in the lateral neck in a child, the Charabi B, Bretlau P, Bille M, Holmelund M. Cystic
foremost diagnostic consideration is cystic hygroma of the head and neck—a long-term follow-up
of 44 cases. Acta Otolaryngol Suppl. 2000;543:248-250.
Mahboubi S, Potsic WP. Computed tomography of
cervical cystic hygroma in the neck. Int J Pediatr
Otorhinolaryngol. 1989;18:47.
Watson WL, McCarthy WD. Blood and lymph vessel
tumors; a report of 1,056 cases. Surg Gynecol Obstet.
1940;71:569.
CAROTID BODY TUMOR
(CHEMODECTOMA)
Figure 8-12
Age: Middle-aged adults
Sex: No predilection
CLINICAL FEATURES
Neoplasms originating in the carotid body
are rarely malignant. Tumors are located in
the upper lateral neck adjacent to the angle
of the mandible. They are firm and movable
anteroposteriorly, yet cannot be manipu-
lated in a superoinferior direction because
of their attachment to the carotid bifurca-
tion. The tumors are generally asymptom-
atic, yet a bruit may be detected, the overly-
ing skin may be warm, and medial growth
FIGURE 8-12 may constrict the airway. Rarely, paralysis
Carotid body tumor causing large tumefaction of cranial nerves X or XII may be observed.
overlying carotid bifurcation. Occasionally, chemodectomas arise more
PMPH_Eversole_Chapter-08.indd 311 1/17/2011 3:40:12 PM
312 Chapter 8
inferiorly from other chemoreceptors Parry DM, Li FP, Strong LC, et al. Carotid body tumors
located along the carotid and aortic arter- in humans: genetics and epidemiology. J Natl Cancer
Inst. 1982;68:573.
ies. The mass may be somewhat tender, yet Valagni R, Amichetti M. Radiation therapy of carotid
is usually asymptomatic. body tumors. Am J Clin Oncol. 1990;13:45.
Wilson H. Carotid body tumors. Surgery. 1966;59:483.
MICROSCOPIC FEATURES
Carotid body tumors typically mimic, mor-
phologically, the normal carotid body with METASTATIC CARCINOMA
organoid nests of polygonal cells. Two cell Figure 8-13
types are seen: the more prevalent vesicular
Age: Teenagers (nasopharyngeal) and elderly
with similarly vesicular oval nuclei, the other
adults (squamous cell carcinoma)
pyknotic and hyperchromatic. The organoid Sex: Male predilection
nests are separated from one another by a
prominent vascular network. Synaptophysin CLINICAL FEATURES
and chromogranin IHC are positive. The first depot of metastatic carcinoma
from primary lesions of the upper respira-
DIFFERENTIAL DIAGNOSIS tory tract and face is the regional cervical
Carotid body tumors, by virtue of their loca- and submandibular group of lymph nodes.
tion, must be differentiated from lymphade- Although usually unilateral, malignant
nopathy, other mesenchymal tumors, and disease with more longevity may manifest
lymphoma. Their unique clinical features bilateral metastases. The mass is usually, yet
with regard to limited movement in a ver- not invariably, fixed to the adjacent fascia or
tical plane with movability in the horizon- sternomastoid muscle and is almost always
tal plane, although not pathognomonic, are indurated. Nasopharyngeal carcinomas
certainly highly suggestive. Angiography occur more frequently in teenagers than
discloses a well-circumscribed vascular in adults. The neck metastases may be the
“blush” in the carotid bifurcation area. first sign of disease, as they may be consid-
erably larger than the primary tumor itself.
TREATMENT When an indurated swelling is detected in
the lateral neck, a diligent search for a pri-
Surgical excision is recommended. The
mary tumor in the oral cavity, nose, throat,
tumor must be removed with great care
nasopharynx, and paranasal sinuses is
to avoid carotid perforation and, therefore,
mandatory. Carcinomas of the skin of the
should be managed by an experienced head
face and scalp may also metastasize to cer-
and neck surgeon. Recent evidence indi-
vical lymph nodes. When nodal metastases
cates that radiation therapy may be effective
are encountered, the prognosis is consider-
for these tumors. Embolization of head and
ably worsened. It should be noted that pri-
neck paragangliomas with n-butyl cyano-
mary adenocarcinomas of salivary origin
acrylate or onyx shows favorable results.
and melanoma of the head and neck fre-
quently manifest cervical metastasis. CT
Additional Reading and MRI detect metastatic disease that may
not be evident clinically.
McGuirt WF, Harker LA. Carotid body tumors. Arch
Otolaryngol Head Neck Surg. 1975;101:58.
Ozyer U, Harman A, Yildirim E, Aytekin C, Akay TH, MICROSCOPIC FEATURES
Boyvat F. Devascularization of head and neck para-
gangliomas by direct percutaneous embolization.
The metastatic tumor is essentially identical
Cardiovasc Intervent Radiol. 2010 Jan 22. [Epub microscopically to the primary lesion. Tumor
ahead of print.] cells tend to localize first in the subcapsular
PMPH_Eversole_Chapter-08.indd 312 1/17/2011 3:40:19 PM
Soft Tissue Swellings of the Neck and Face 313
FIGURE 8-13
Metastatic cancer in cervical
nodes from a primary carci-
noma of the oral cavity.
region and later replace the entire node. Infil- disease to nodes may be treated by cervical
tration into the adjacent tissues ensues. node dissection, often in continuity with the
primary lesion, or may be radiated. These
DIFFERENTIAL DIAGNOSIS treatment methods must be selected care-
The indurated fixed node containing meta- fully for each case by the oncologist or head
static cancer must be differentiated from and neck team.
malignant lymphoma, primary sarcoma,
and certain inflammatory diseases such
as actinomycosis and scrofula, which may
Additional Reading
also be hard and immovable. Detection of a Mustard RA, Rosen IB. Cervical lymph node involvement
in oral cancer. AJR Am J Roentgenol. 1963;90:978.
primary tumor in the head and neck region
Park JM, Jung CK, Choi YJ, et al. The use of an immu-
determines the diagnosis. Occasionally, no nohistochemical diagnostic panel to determine the
primary tumor can be found when intra- primary site of cervical lymph node metastases of occult
nodal carcinoma is discovered on biopsy. squamous cell carcinoma. Hum Pathol. 2010;41:431-437.
Most lesions of this nature arise in the Robertson MS, Snape L. The malignant gland in the
neck as a presenting sign in head and neck cancer. N Z
nasopharynx, which must again be exam- Med J. 1980;92:303.
ined with scrutiny. Roseman JM, James AG. Metastatic cancers to the neck
from undetermined primary sites: long-term follow-
TREATMENT up. J Surg Oncol. 1982;19:247.
Sharpe DT. The pattern of lymph node metastases in
The primary tumor may be treated surgi- intra-oral squamous cell carcinoma. Br J Plast Surg.
cally or with radiation therapy. Metastatic 1981;34:97.
PMPH_Eversole_Chapter-08.indd 313 1/17/2011 3:40:19 PM
314 Chapter 8
SARCOMAS DIFFERENTIAL DIAGNOSIS
Figure 8-14 Primary sarcomas of the neck, being fixed
and indurated, must be differentiated from
Age: Children and young adults lymphoma, metastatic carcinoma, some
Sex: No predilection of the reactive proliferations, and specific
CLINICAL FEATURES granulomatous inflammations, which are
Primary sarcomas of the head and neck occasionally hard to palpation. Biopsy is
region are rare, yet when they occur, the required to determine the diagnosis and
orbit and lateral neck are the most fre- ascertain the tissue of origin.
quently affected sites. In the neck, the most
TREATMENT
frequently encountered tumors are fibrosar-
coma, malignant fibrous histiocytoma, rhab- Wide radical excision is required and
domyosarcoma, and synovial sarcoma. The should be undertaken by an oncologic
swellings are firm or indurated and fixed surgeon. Even with radical surgery, recur-
to adjacent tissues. They may or may not rences may ensue and the prognosis is gen-
be painful. When large, telangiectasia and erally poor.
erythema of the overlying skin may be seen.
Growth is progressive and often rapid.
Additional Reading
MICROSCOPIC FEATURES Barnes L, Kanbour A. Malignant fibrous histiocytoma of
The histomorphology varies depending on the head and neck. Arch Otolaryngol Head Neck Surg.
1988;114:1149.
the cell of origin. The mesenchymal malig- Harb WJ, Luna MA, Patel SR, Ballo MT, Roberts DB,
nancies are, as a group, spindle cell neo- Sturgis EM. Survival in patients with synovial sar-
plasms with significant cellularity, pleomor- coma of the head and neck: association with tumor
phism, and nuclear hyperchromatism or location, size, and extension. Head Neck. 2007;29:
731-740.
vesiculation. Encapsulation is lacking, and Healy GB. Malignant tumors of the head and neck in
invasion of muscle and fascia is an almost children: diagnosis and treatment. Otolaryngol Clin
constant feature. North Am. 1980;13:483.
FIGURE 8-14
Periorbital indurated neck
mass is rhabdomyosarcoma
(left); fibrosarcoma (right).
PMPH_Eversole_Chapter-08.indd 314 1/17/2011 3:40:49 PM
Soft Tissue Swellings of the Neck and Face 315
Masson JD, Soule EH. Embryonal rhabdomyosarcoma lar clinical features, yet differ in prognosis;
of the head and neck; report on eighty-eight cases. Am Hodgkin’s lymphomas, as a group, prog-
J Surg. 1965;110:585.
Otte T, Kleinsasser O. Liposarcoma of the head and ress more slowly, and longevity is greatly
neck. Arch Otorhinolaryngol. 1981;232:285. increased over the non-Hodgkin’s group.
As the disease progresses, more extensive
node involvement occurs with axillary and
MALIGNANT LYMPHOMA inguinal enlargement. Hilar node enlarge-
ment becomes apparent radiographically.
Figure 8-15
Hepatosplenomegaly eventually occurs,
Age: Young and middle-aged adults and extranodal involvement with visceral,
Sex: Male predilection central nervous system, and osseous tumor
is seen in the terminal stages. Low-grade
CLINICAL FEATURES fever, malaise, weight loss, frequent night
Two basic types of lymphoid malignancy, sweats, and pruritus are common symp-
Hodgkin’s disease and non-Hodgkin’s toms. Shingles is a frequent complication.
lymphoma, involve the cervical lymph Lymphoma is the second most common
nodes. Indeed, the cervical nodes are one of malignancy seen in human immunodefi-
the most frequently involved node groups ciency virus (HIV) infection.
in the entire body. The swelling is occasion-
ally unilateral, but is more often bilateral. MICROSCOPIC FEATURES
The tumor masses may be multinodular The microscopic changes in the lymph
and are, as a rule, fixed and indurated. nodes are highly variable. The sine qua non
Growth is progressive and may be rapid. for Hodgkin’s disease is the presence of a
The two forms of lymphoma manifest simi- binucleated large histiocyte with prominent
FIGURE 8-15
Cervical masses in malignant
lymphoma.
PMPH_Eversole_Chapter-08.indd 315 1/17/2011 3:41:11 PM
316 Chapter 8
central nucleoli known as the Reed-Stern-
berg cell. The non-Hodgkin’s lymphomas Unilateral Parotid and
show either well- or poorly differentiated Submandibular Swellings
lymphocytes arranged in follicular patterns
or in monotonous cell sheets. The various ACUTE SIALADENITIS
subtypes in both groups have different nat- (SURGICAL MUMPS)
ural histories and prognoses. In the head Figure 8-16
and neck area, large B-cell lymphoma is the
most common type. Immunohistochemical Age: Elderly adults
markers and gene rearrangement studies Sex: Male predilection
for B- and T-cell lineages are crucial for typ- CLINICAL FEATURES
ing these tumors and determining appro-
priate chemotherapy. Acute inflammatory disease of the major
salivary glands most commonly affects the
DIFFERENTIAL DIAGNOSIS parotid. Unilateral involvement is more
Unilateral neck node enlargement in lym-
phoma must be differentiated from sarcoma,
metastatic carcinoma, and certain inflam-
matory enlargements such as scrofula and
actinomycosis. Bilateral enlargements must
be differentiated from sinus histiocyto-
sis, metastatic carcinoma, and nonspecific
lymphadenopathy. A complete physical
examination, which includes hematologic
studies, chest radiographs, and lymp-
hangiography, is required to determine the
extent of the disease.
TREATMENT
Lymphomas should be treated by a hema-
tologist, oncologic chemotherapist, and/or
radiotherapist. The disease is managed by
radiotherapy in combination with multi-
phasic antitumor chemotherapy.
Additional Reading
Aisenberg AC. Malignant lymphoma. N Engl J Med.
1973;288:883.
Butler JJ. Relationship of histological findings to survival
in Hodgkin’s disease. Cancer Res. 1971;31:1770.
Evans C. A review of non-Hodgkin’s lymphomata of the
head and neck. Clin Oncol. 1981;7:23.
Gaini RM, Romagnoli M, Sala A, Garavello W.
Lymphomas of head and neck in pediatric patients. Int
J Pediatr Otorhinolaryngol. 2009;73(suppl 1):S65-S70.
Levine AM. Non-Hodgkin’s lymphomas and other malig-
nancies in the acquired immune deficiency syndrome. FIGURE 8-16
Semin Oncol. 1987;14:34. Parotitis developing shortly after abdominal surgery.
PMPH_Eversole_Chapter-08.indd 316 1/17/2011 3:41:40 PM
Soft Tissue Swellings of the Neck and Face 317
frequent than bilateral. Staphylococci and Gomez-Rodrigo J, Mendelson J, Black M, Dascal A.
streptococci are the causative organisms. Streptococcus pneumoniae acute suppurative parotitis
in a patient with Sjögren’s syndrome. J Otolaryngol.
The disease is uncommon; when present, it 1990;19:195.
is seen primarily in debilitated patients and Rousseau P. Acute suppurative parotitis. J Am Geriatr
those who are recovering from major sur- Soc. 1990;38:897.
gery. It has also been reported to occur in Sermoneta D, Lodoli C, Di Mugno M, De Cosmo G, Gui
D. An unusual case of acute unilateral parotitis follow-
patients with xerostomia complicating the ing abdominal surgery. Report of a case and review of
use of phenothiazine drugs. The patients the literature. Ann Ital Chir. 2009;80:221-223.
are febrile, the swelling is painful, and a
purulent exudate can be milked from the
salivary ducts. SIALOLITHIASIS AND
OBSTRUCTIVE SIALADENITIS
MICROSCOPIC FEATURES Figure 8-17
The acinar parenchyma shows degenera-
Age: Middle-aged adults
tion and necrosis with diffuse infiltration Sex: Male predilection
by neutrophils. The ducts display ectasia
and are impacted with necrotic debris and CLINICAL FEATURES
neutrophils. The formation of salivary calculi within the
ducts of the major salivary glands is over-
DIFFERENTIAL DIAGNOSIS whelmingly more common in the subman-
Acute parotitis of bacterial origin must be dibular ducts. The stone develops on some
differentiated from endemic parotitis and sort of nidus, perhaps a mucous plug, and
duct occlusion phenomenon (sialolithiasis). calcium salts become deposited in a con-
Pain and swelling are common to all three centric fashion. When the stone reaches
disorders. Purulent drainage from the duct sufficient size, the duct becomes occluded,
orifice is more common in acute parotitis; mucin is retained, and the gland develops
bacteria can be cultured from this exudate sclerosing sialadenitis. Clinically, the gland
and, in addition, a history of recent surgery becomes enlarged and firm but is still mov-
or a predisposing debilitating condition can able. Pain is often severe or stabbing during
be obtained. mealtime, when salivation is stimulated.
The stone can often be palpated within the
TREATMENT duct or demonstrated radiographically. The
parotid duct is only occasionally involved.
Fluid and electrolyte balance should be main- Rarely, the intraoral minor glands develop
tained in postsurgical patients. Efforts to con- a calculus. Occasionally, developmental or
trol any debilitating disease should be made posttraumatic strictures develop in the duct
in consultation with the patient’s physician. system. The clinical signs and symptoms
The parotitis is treated with penicillin ther- simulate sialolithiasis, and sialography aids
apy in nonallergic patients while waiting for in identifying the stricture. Ultrasonogra-
results from culture and sensitivity testing. phy can be a useful diagnostic approach to
the diagnosis of sialolithiasis.
Additional Reading MICROSCOPIC FEATURES
Banning GL. Postoperative suppurative parotitis. Arch The stone, when decalcified, is composed
Surg. 1964;89:653.
Carlson RG, Glas WE. Acute suppurative parotitis;
of concentric laminations of amorphous
twenty-eight cases at a county hospital. Arch Surg. basophilic matrix. The occluded gland
1963;86:659. shows acinar degeneration with replace-
PMPH_Eversole_Chapter-08.indd 317 1/17/2011 3:41:46 PM
318 Chapter 8
pain, induration, and lack of function per-
sist, particularly in cases of long-standing
occlusion, sialectomy is indicated. Litho-
tripsy may prove to be a valuable method
for managing large stones.
Additional Reading
Bullock KN. Parotid and submandibular duct calculi in
three successive generations of one family. Postgrad
Med J. 1982;58:35.
Harrison GR. Calculi of the salivary glands and ducts.
Surg Gynecol Obstet. 1926;43:431.
Lustmann J, Regev E, Melamed Y. Sialolithiasis. A sur-
vey on 245 patients and a review of the literature. Int J
Oral Maxillofac Surg. 1990;19:135.
Seldin HM, Seldin SD, Rakower W. Conservative sur-
gery for removal of salivary calculi. Oral Surg Oral
Med Oral Pathol. 1953;6:579.
Yuasa K, Nakhyama E, Ban S, et al. Submandibular gland
FIGURE 8-17 duct endoscopy. Diagnostic value for salivary duct dis-
Submandibular swelling in sialadenitis secondary to orders in comparison to conventional radiography, sia-
duct blockage by a sialolith. lography, and ultrasonography. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod. 1997;84: 578-581.
ment by fibrous tissue and mononuclear
cells. Ducts are dilated, contain impacted CHRONIC SIALADENITIS
mucin, and show oncocytic, mucous, and Figure 8-18
squamous metaplasia.
Age: Adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Sclerosing sialadenitis associated with sialo- CLINICAL FEATURES
lithiasis may show features that can be con- Chronic sialadenitis is caused by retrograde
fused with endemic parotitis, salivary neo- infection with bacteria up the salivary duct
plasm, or mesenchymal neoplasm. Presence tree. Infections of this nature are usually the
of pain that is increased at mealtime, failure consequence of duct blockage from ductal
to obtain flow when milking the gland, and atresia, stricture, a mucous plug, or a stone.
presence of a palpable indurated mass in the The gland enlarges and is usually tender to
complementary duct lead to a diagnosis of palpation as salivary flow becomes blocked
sialolithiasis. Submandibular duct stones are and accumulates in the ductal system. Exu-
visualized with mandibular occlusal radio- date and inflammatory cells within acinar
graphs; parotid duct stones can be detected lobules also account for the swelling. If the
on panographic jaw radiographs. In addition, infectious flora changes, the inflammation
endoscopy can be performed to detect stric- may become acute with elevated tempera-
tures and mucous plugs as well as stones. ture and leakage of a purulent exudates
from the ductal opening.
TREATMENT
The stone can often be digitally manipu- MICROSCOPIC FEATURES
lated out of the duct orifice. If this cannot be A chronic sclerosing sialadenitis is observed
achieved, surgical removal is indicated. If with loss of acini, mononuclear infiltration,
PMPH_Eversole_Chapter-08.indd 318 1/17/2011 3:41:46 PM
Soft Tissue Swellings of the Neck and Face 319
Additional Reading
Bradley PJ. Microbiology and management of sialadeni-
tis. Curr Infect Dis Rep. 2002;4:217-224.
Johnson A. Inflammatory conditions of the major salivary
glands. Ear Nose Throat J. 1989;68:94-102.
Teymoortash A, Tiemann M, Schrader C, Werner JA.
Characterization of lymphoid infiltrates in chronic
obstructive sialadenitis associated with sialolithiasis.
J Oral Pathol Med. 2004;33:300-304.
INTRAPAROTID
MESENCHYMAL TUMORS
Figure 8-19
Age: Infants and children
Sex: Female predilection
CLINICAL FEATURES
Neoplasms arising from the supportive
stroma of the salivary glands are less com-
mon than parenchymal tumors. When they
do occur, they are primarily seen in children.
Vascular tumors are the most frequently
encountered mesenchymal tumors. Juve-
FIGURE 8-18 nile nevoxanthogranulomas and neurilem-
Chronic parotitis, duct blockage with bacterial momas also arise from salivary stromal
infection. progenitor cells. Sarcomas in major glands
are extremely rare. The benign tumor(s)
and interstitial fibrosis. In acute lesions, may be present at birth or develop slowly
abscess pockets may occur both within during childhood. The gland substance is
ducts and in the parenchyma. unilaterally affected and may evince a soft-
to-firm diffuse swelling, or the neoplasm
DIFFERENTIAL DIAGNOSIS may be well localized and encapsulated.
The masses are painless, and no erythema
Neoplastic lesions should be considered. or skin surface changes are found. Spon-
Milking the ducts may elicit the flow of taneous regression of cutaneous vascular
pus from the orifice indicating the infec- tumors by puberty is a frequent occurrence;
tious nature of the process during an acute however, intraparotid lesions do not tend to
phase. Ultrasound imaging is also useful in involute.
arriving at a definitive diagnosis. Venous aneurysms, although not
neoplastic, represent other mesenchymal
TREATMENT
lesions occurring within parotid tissue.
If possible, saliva should be milked from the They are nonpulsatile soft swellings that
gland and subjected to culture and sensitiv- appear when the head is lowered below the
ity in order to select the appropriate antibi- level of the heart. The swelling resolves in
otic. A search must be made to uncover any 2 to 3 minutes after the patient elevates the
possibility of duct blockage. head.
PMPH_Eversole_Chapter-08.indd 319 1/17/2011 3:42:07 PM
320 Chapter 8
FIGURE 8-19
Intraparotid hemangioma, arterio-
gram.
MICROSCOPIC FEATURES prone to involute spontaneously than are
Intraparotid hemangiomas and lymp- angiomas of skin. Neurilemmomas may be
hangiomas are characterized by infiltrative locally excised.
endothelium-lined channels of variable
cellularity that tend to course between
lobules and acini. Neurilemmomas are Additional Reading
typically encapsulated and are composed Bhaskar SN, Lilly GE. Salivary gland tumors of
of spindle-shaped nuclei and condensed infancy; report of 27 cases. J Oral Maxillofac Surg.
collagen with foci of microcyst formation 1963;21:305.
(Antoni B) and nuclear palisading (Antoni Jensen JL, Reingold IM. Venous aneurysms of the
parotid gland. Arch Otolaryngol Head Neck Surg.
A) zones. 1977;103:493.
Krolls SO, Trodahl JN, Boyers RC. Salivary gland
DIFFERENTIAL DIAGNOSIS lesions in children. A survey of 430 cases. Cancer.
1972;30:459.
The slowly enlarging tumor mass seen Lack EE, Upton MP. Histopathologic review of salivary
with mesenchymal neoplasms must be gland tumors in childhood. Arch Otolaryngol Head
differentiated from tuberculosis and Neck Surg. 1988;114:898.
unilateral mumps. The latter has an Muenscher A, Diegel T, Jaehne M, Ussmüller J, Koops
S, Sanchez-Hanke M. Benign and malignant salivary
acute course with pain and fever. Pri- gland diseases in children A retrospective study of 549
mary parenchymal salivary tumors, par- cases from the Salivary Gland Registry, Hamburg.
ticularly benign lesions, show identical Auris Nasus Larynx. 2009;36:326-331.
clinical features, but are rarely seen in
children. Biopsy is required to provide a
defi nitive diagnosis. LYMPHOMA
Figure 8-20
TREATMENT
Age: Middle-aged adults
Vascular tumors, being infiltrative, lack Sex: Male predilection
encapsulation and, therefore, require lobec-
CLINICAL FEATURES
tomy or parotidectomy, depending on the
extent. Treatment should be deferred until Whereas lymphomas generally make their
after puberty, as regression may occur; initial appearance in the cervical nodes of
however, parotid vascular tumors are less the lateral neck, intraparotid nodes may also
PMPH_Eversole_Chapter-08.indd 320 1/17/2011 3:42:11 PM
Soft Tissue Swellings of the Neck and Face 321
islands as seen in benign autoimmune
sialadenitis are also identifiable in MALT
lymphomas. Other types of lymphomas are
diagnosed on the basis of pattern, lympho-
cyte morphology, and immunohistochemi-
cal markers.
DIFFERENTIAL DIAGNOSIS
Bilateral parotid swellings seen in acute
sialadenitis and endemic parotitis may
be differentiated from lymphoma on the
basis of high fever, pain, lack of induration,
and rapid onset. Lymphoma may be con-
fused clinically with Sjögren’s syndrome,
Mikulicz’s disease, Heerfordt’s syndrome,
and tuberculosis. In these disorders, how-
ever, the glandular swellings are soft or only
moderately firm and lack fixation. Biopsy is
required to obtain a definitive diagnosis.
FIGURE 8-20 Once a diagnosis of malignant lymphoma
Intraparotid MALT type malignant lymphoma. is established, thorough physical examina-
tion, laboratory evaluation, and radiologic
survey are required to determine the extent
of disease.
be the site of original tumefaction, produc-
ing enlargements anterior to the ears and TREATMENT
over the mandibular angle. They are indu-
rated and may be bilateral. Salivary flow The patient should be under the care of
is usually not affected and can be milked an oncologist, a hematologist, and a radio-
from the ducts. Pain is uncommon. When therapist. Combination chemotherapy and
both parotids are enlarged in conjunction radiotherapy are used in treatment.
with lymphomatous swelling of the lacri-
mal glands, the disease is said to represent
Mikulicz’s syndrome (not to be confused Additional Reading
with Mikulicz’s disease, which is one of
Colby TV, Dorfman RF. Malignant lymphomas involving
the benign lymphoepithelial lesions). Most the salivary glands. Pathol Annu. 1979;14:307.
instances of intraparotid lymphoma are Freedman SI. Malignant lymphomas of the major
of the non-Hodgkin’s type and many are salivary glands. Arch Otolaryngol Head Neck Surg.
MALT lymphomas. Patients with Sjögren’s 1971;93:123.
Gravanis MB, Giansanti JS. Malignant histopathologic
syndrome are prone to develop lymphoma, counterpart of the benign lymphoepithelial lesion.
both in the affected parotid and other body Cancer. 1970;26:1332.
sites. Hu S, Zhou M, Jiang J, et al. Systems biology analysis of
Sjögren’s syndrome and mucosa-associated lymphoid
tissue lymphoma in parotid glands. Arthritis Rheum.
MICROSCOPIC FEATURES 2009;60:81-92.
Hyman GA, Wolfe M. Malignant lymphomas of the sali-
In lymphoma both acini and ducts within vary glands. Review of the literature and report of 33
salivary lobules are replaced by diffuse new cases, including four cases associated with the lym-
sheets of lymphocytes. Epimyoepithelial phoepithelial lesion. Am J Clin Pathol. 1976;65:421.
PMPH_Eversole_Chapter-08.indd 321 1/17/2011 3:42:33 PM
322 Chapter 8
PLEOMORPHIC ADENOMA basophilic epithelial cells grow in diffuse
Figure 8-21 sheets or are grouped into clusters show-
ing duct formation. A spindle cell element
Age: Middle-aged adults is seen to proliferate in juxtaposition to the
Sex: Female predilection epithelial cell component and may actu-
CLINICAL FEATURES ally be the predominant cell type. These
myoepithelial spindle cell proliferations
The pleomorphic adenoma or mixed tumor merge with stromal components that dif-
is the most common neoplasm of the major ferentiate into myxomatous, cartilaginous,
salivary glands. Over 80% arise in the osseous, or adipose tissues. Some tumors
parotid, and most of the remaining 20% contain myoepithelial hyaline cells with a
involve submandibular gland and minor plasmacytoid appearance, and occasion-
salivary glands. The tumor is generally ally, tyrosine crystals are encountered.
located superficially overlying the angle Encapsulation is a constant fi nding; how-
of the mandible. It is firm or soft, movable, ever, multiple extracapsular satellite cell
slow growing, and usually free from pain, nests or a multinodular pattern are fre-
even on palpation. It has a great growth quently noted.
potential in that long-standing tumors may
become so enormous that they hang to the DIFFERENTIAL DIAGNOSIS
shoulders. Malignant transformation is
uncommon but does occur. Pleomorphic adenoma must be differen-
tiated from papillary cystadenoma lym-
phomatosum, oncocytoma, mesenchymal
MICROSCOPIC FEATURES
neoplasms, and adenocarcinomas, all of
The term pleomorphic refers to the stromal which may appear well circumscribed.
element of the tumor and is the para- Although the clinical features may appear
mount pathologic feature. Monomorphic to be typical for pleomorphic adenoma,
FIGURE 8-21
Pleomorphic adenoma of the parotid
gland.
PMPH_Eversole_Chapter-08.indd 322 1/17/2011 3:42:39 PM
Soft Tissue Swellings of the Neck and Face 323
biopsy is required to rule out these other
entities. Aspiration cytology is less inva-
sive and is often diagnostic; however, cel-
lular mixed tumors may be confused with
adenocarcinomas.
TREATMENT
Simple excision is contraindicated, as recur-
rence is a common complication. Lobectomy
or in-continuity gland extirpation is the
treatment of choice. Facial nerve palsy and
the auriculotemporal syndrome are com- FIGURE 8-22
mon complications subsequent to parotid Parotid nodule representing papillary cystadenoma
gland surgery. lymphomatosum.
Additional Reading 4 cm, growth ceases in most cases. Another
feature supporting the concept of a hamar-
Clairmont AA, Richardson GS, Hanna DC. The pseudo- tomatous lesion is its frequent bilateral occur-
capsule of pleomorphic adenomas (benign mixed
tumors). Am J Surg. 1977;134:242.
rence. The tumor is restricted to the parotid
Eneroth CM. Histological and clinical aspects gland(s) and is not found in other major or
of parotid tumors. Acta Otolaryngol (Stockh). minor glands. It tends to be superficial, well
1964;191(suppl.):5. circumscribed, and movable, and classically
Jayaram N, Ashim D, Rajwanshi A, Radhika S, Banerjee
feels doughy and compressible on palpation.
CK. The value of fine-needle aspiration biopsy in
the cytodiagnosis of salivary gland lesions. Diag
Cytopathol. 1989;5:349. MICROSCOPIC FEATURES
Krolls SO, Boyers RC. Mixed tumors of salivary glands:
long-term follow-up. Cancer. 1972;30:276. The lesion is well encapsulated and shows
Redaelli de Zinis LO, Piccioni M, Antonelli AR, Nicolai cystic spaces lined by papillary projections
P. Management and prognostic factors of recurrent of columnar oncocytes with a double row
pleomorphic adenoma of the parotid gland: personal
experience and review of the literature. Eur Arch
of nuclei. The stroma is composed of lym-
Otorhinolaryngol. 2008;265:447-452. phocytes with scattered germinal centers. A
variant contains nests of squamous epithelial
islands showing cyst formation and sebaceous
PAPILLARY CYSTADENOMA acinar differentiation. The variant is termed
LYMPHOMATOSUM sebaceous lymphadenoma. Although extremely
Figure 8-22 rare, adenocarcinoma and squamous cell car-
cinoma have been reported to arise in papil-
Age: Middle-aged and elderly adults lary cystadenoma lymphomatosum.
Sex: Significant male predilection
CLINICAL FEATURES DIFFERENTIAL DIAGNOSIS
Papillary cystadenoma lymphomatosum or Warthin’s tumor must be differentiated
Warthin’s tumor is a benign tumor of salivary from other benign salivary neoplasms
origin that probably represents a hamartoma- of parenchymal and stromal origin and
tous enlargement rather than a true neoplasm. enlarged parotid lymph nodes. Occurrence
Credence is given to this concept on the basis in males, doughy compressible consistency,
of the clinical features of the lesion. It is slow and indolent growth are typical features.
growing and self-limited. Once it reaches 2 to Bilateral swellings with these characteristics
PMPH_Eversole_Chapter-08.indd 323 1/17/2011 3:42:55 PM
324 Chapter 8
are almost invariably Warthin’s tumors; before the age of 60 years. It arises most
nevertheless, biopsy should be performed frequently in the parotid gland but may
to confirm the clinical diagnosis. be located in the submandibular region as
well. The mass is firm, well demarcated,
TREATMENT and movable. It has a slow growth rate.
Simple local excision is recommended.
MICROSCOPIC FEATURES
Solid sheets or trabecular cords of rectangu-
Additional Reading lar cells show voluminous amounts of gran-
ular eosinophilic cytoplasm with pyknotic
Chaudhry AP, Gorlin RJ. Papillary cystadenoma lympho-
matosum (adenolymphoma); a review of the literature. or small nuclei containing a central nucleo-
Am J Surg. 1958;95:923. lus. Cystic spaces or duct formations may
Dietert SE. Papillary cystadenoma lymphomatosum be encountered, yet rarely predominate.
(Warthin’s tumor) in patients in a general hospital over Oncocytic metaplasia in ductal cells is com-
a 24-year period. Am J Clin Pathol. 1975;63:866.
McGavran MH, Bauer WC, Ackerman LV. Sebaceous mon in both major and minor salivary glands
lymphadenoma of the parotid salivary gland. Cancer. with ensuing age; however, this represents
1960;13:1185. reactive rather than neoplastic change. A
Morrison GA, Shaw HJ. Squamous carcinoma aris- rare variant with clear cells admixed with
ing within a Warthin’s tumour of the parotid gland.
J Laryngol Otol. 1988;102:1189.
oncocytes has been described.
Rizzi MD, Thompson LD. Papillary cystadenoma lym-
phomatosum (Warthin tumor). Ear Nose Throat DIFFERENTIAL DIAGNOSIS
J. 2003;82:920-922.
Shugar JM, Som PM, Biller HF. Warthin’s tumor, a multi- The well-localized movable swelling of
focal disease. Ann Otol Rhinol Laryngol. 1982;91:246. oncocytoma must be differentiated from
Warthin’s tumor, pleomorphic adenoma,
mesenchymal neoplasm, and enlarged
ONCOCYTOMA parotid lymph node. Age is highly signifi-
Figure 8-23 cant, and a swelling of this nature in an
elderly patient is strongly suggestive of
Age: Elderly adults oncocytoma. Microscopic examination is
Sex: Female predilection required to make the diagnosis.
CLINICAL FEATURES
TREATMENT
Oncocytoma or oxyphilic adenoma is a rare
benign salivary tumor that rarely occurs Simple local excision is recommended.
FIGURE 8-23
Oncocytoma of the parotid
in an elderly female.
PMPH_Eversole_Chapter-08.indd 324 1/17/2011 3:42:58 PM
Soft Tissue Swellings of the Neck and Face 325
sis is rare. Sialadenoma papilliferum may
Additional Reading extend through skin with an overlying cuta-
Chaudhry AP, Gorlin RJ. Oxyphilic granular cell adeno- neous cauliflower-like papillomatous mass.
ma (oncocytoma). Oral Surg Oral Med Oral Pathol.
1958;11:897.
Ellis GL. “Clear cell” oncocytoma of salivary gland. Hum MICROSCOPIC FEATURES
Pathol. 1988;19:862. Each tumor exhibits characteristic histo-
Eneroth CM. Oncocytoma of major salivary glands.
J Laryngol Otol. 1965;79:1064.
morphologic patterns. Basal cell adenomas
Hamperl H. Benign and malignant oncocytoma. Cancer. are composed of tumor islands, which com-
1962;15:1019. prise polygonal monomorphic cells with
Zhou CX, Gao Y. Oncocytoma of the salivary glands: a oval or round nuclei. Ductal elements are
clinicopathologic and immunohistochemical study.
Oral Oncol. 2009;45(12):e232-e238.
often encountered. Membranous adenomas
appear similar to basal cell adenomas with
zones of hyalinization encompassing indi-
MISCELLANEOUS ADENOMAS vidual nests or islands of monomorphic-ap-
pearing cells; such lesions are often associ-
Figure 8-24
ated with cutaneous tumors and are referred
Age: Adults to as dermal analogue tumors. Sialadenoma
Sex: Female predilection papilliferum shows cystic areas lined by
papillary interconnecting projections lined
CLINICAL FEATURES
by oncocytic columnar cells. When sur-
A variety of histologically distinct benign face skin is involved, the ductal-appearing
glandular tumors, other than the more com- cells merge with papillary projections cov-
mon types included in this chapter, arise ered with stratified squamous epithelium.
within the major salivary glands, usually the Myoepitheliomas are characterized by
parotid. Most of them are rare. Included in diffuse sheets of spindle cells resembling
this group are basal cell adenoma, membra- mesenchymal cells; thorough search of
nous adenoma, sialadenoma papilliferum, the specimen reveals streaming of spindle
myoepithelioma, sebaceous lymphadenoma, cells around small ducts. Sebaceous lymph-
and papillary cystadenoma. Generally located adenomas, a variant of Warthin’s tumor,
within the superficial parotid, they appear show ducts, sebaceous acini, and lymphoid
as movable soft or somewhat firm nodules. stroma. Papillary cystadenomas are cystic
Facial nerve compression resulting in paraly- with papillary projections into the lumina.
FIGURE 8-24
Basal cell adenoma of the
parotid gland.
PMPH_Eversole_Chapter-08.indd 325 1/17/2011 3:43:06 PM
326 Chapter 8
DIFFERENTIAL DIAGNOSIS ADENOID CYSTIC
These miscellaneous adenomas are soft CARCINOMA
or firm movable masses that are clinically Figure 8-25
indistinguishable from the other benign
adenomas included here.
Age: Middle-aged adults
Sex: Slight female predilection
TREATMENT
The recurrence rate after excision is not CLINICAL FEATURES
known for most of these less commonly Adenoid cystic carcinoma or cylindroma
encountered tumors. It would probably be occurs more frequently in adults than in
advisable to perform excision with in-conti- children. Unlike other malignant tumors of
nuity lobectomy. the salivary glands, it is just as likely to be
encountered in the submandibular as in the
Additional Reading parotid gland. The tumor mass is firm or
indurated, often fixed, and does not neces-
Abrams AM, Finck FM. Sialadenoma papilliferum: a sarily grow rapidly. Unlike benign tumors,
previously unreported salivary gland tumor. Cancer. pain is often a symptom. In the parotid
1969;24:1057. gland, facial nerve paralysis is encoun-
Batsakis JG, Brannon RB. Dermal analogue of the major
salivary glands. J Laryngol Otol. 1981;95:155. tered in nearly one third of the patients.
Headington JT, Batsakis JG, Beals TF, Campbell TE, When the tumor lies in close proximity to
Simmons JL, Stone WD. Membranous basal cell the overlying skin, erythema, telangiecta-
adenoma of parotid gland, dermal cylindromas, and sia, and ulceration may be seen. The tumor
trichoepitheliomas: Comparative histochemistry and
ultrastructure. Cancer. 1977;39:2460.
metastasizes to regional cervical nodes and
Liess BD, Lane RV, Frazier S, Zitsch RP, 3rd. Bilateral distantly by hematogenous spread with
canalicular adenoma of the parotid gland. Arch about equal frequency. A feature typical of
Otolaryngol Head Neck Surg. 2006;132:339-341. adenoid cystic carcinoma is its slow rate of
Stanley MW, Horwitz CA, Henry MJ, Burton LG,
Lowhagen T. Basal cell adenoma of the salivary gland:
metastasis. Many tumors have been known
a benign adenoma that cytologically mimics adenoid to manifest metastatic foci 10 or 15 years
cystic carcinoma. Diagn Cytopathol. 1988;4:342. after treatment.
FIGURE 8-25
Adenoid cystic carcinoma
of the parotid gland appear-
ing as an indurated ery-
thematous mass below the
ear lobe.
PMPH_Eversole_Chapter-08.indd 326 1/17/2011 3:43:21 PM
Soft Tissue Swellings of the Neck and Face 327
MICROSCOPIC FEATURES when wide excision (not gland extirpation)
The tumor cells are cuboidal, uniform, and is performed. The determinate 5-year sur-
hyperchromatic. Pleomorphism is uncom- vival is about 30%; 10-year survival, 20%;
mon. The cells are arranged in cords, solid and 15-year survival, 10%. Histologic grad-
sheets, or, typically, a multicystic honey- ing is not highly correlated with progno-
combed or cribriform pattern. The cys- sis. Recurrent disease is usually managed
tic areas contain a basophilic secretion by radiation therapy in conjunction with
product; the outer margin of the tumor hyperthermia.
islands, in the basal lamina region, evince
a thickened hyaline rim. Tumor cells show
a tendency for invasion of perineural lym-
Additional Reading
phatic vessels. The leading margins lack Barnett TA, Kapp DS, Goffinet DR. Adenoid cystic carci-
encapsulation, and invasion of contiguous noma of the salivary glands. Management of recurrent,
tissues is a constant finding. Histologic advanced, or persistent disease with hyperthermia and
radiation therapy. Cancer. 1990;65:2648.
grading has been undertaken whereby the Conley J, Dingman DL. Adenoid cystic carcinoma in the
typical cribriform pattern is grade I, cribri- head and neck (cylindroma). Arch Otolaryngol Head
form with admixed solid sheets is grade II, Neck Surg. 1974;100:81.
and basaloid or anaplastic predominance Eby LS, Johnson DS, Baker HW. Adenoid cystic carci-
noma of the head and neck. Cancer. 1972;29:1160.
is grade III. Eneroth CM, Hjertman L. Adenoid cystic carci-
noma of the submandibular gland. Laryngoscope.
DIFFERENTIAL DIAGNOSIS 1966;76:1639.
Iseli TA, Karnell LH, Preston TW, et al. Facial nerve sac-
Because cylindromas are not always sol- rifice and radiotherapy in parotid adenoid cystic carci-
idly fixed, they may simulate benign noma. Laryngoscope. 2008;118:1781-1786.
Spiro RH, Huvos AG, Strong EW. Adenoid cystic car-
salivary neoplasms and mesenchymal
cinoma of salivary origin, a clinicopathologic study of
tumors. When indurated and fixed, they 242 cases. Am J Surg. 1974;128:512.
must be differentiated from other malig-
nant salivary tumors such as mucoepider-
moid carcinoma, acinic cell carcinoma, and MUCOEPIDERMOID
adenocarcinoma. Microscopic examination
CARCINOMA
is required to make the diagnosis.
Figure 8-26
TREATMENT Age: Middle-aged adults
Sex: Slight female predilection
Depending on location, total parotidec-
tomy or excision of the entire submandibu- CLINICAL FEATURES
lar gland is mandatory. If the gland capsule Mucoepidermoid carcinoma is most com-
is invaded, inclusion of adjacent tissues is mon in adults; however, a significant number
necessary. Postoperative radiation therapy of cases involve children. The parotid gland
is recommended. In-continuity neck dis- is by far the most frequent site of origin. The
section should be performed when nodes tumors are divided microscopically into
are palpable; because hematogenous low- and high-grade varieties. Low-grade
spread is frequent, chest radiographs must tumors are cystic and may be soft and com-
be obtained. Twenty percent of patients pressible on palpation, whereas the more cel-
with major gland tumors exhibit nodal lular high-grade lesions are often fixed and
metastasis, whereas 50% present with, or indurated. The skin overlying a superficially
eventually develop, distant metastases. oriented tumor may be ulcerated, erythema-
The recurrence rate is high (over 50%) tous, and telangiectatic. Low-grade tumors
PMPH_Eversole_Chapter-08.indd 327 1/17/2011 3:43:29 PM
328 Chapter 8
have metastatic potential if left untreated, ferentiate diploid from atypical chromatin,
yet as a group the prognosis is good when the latter predicting an unfavorable course.
treatment is adequate. High-grade tumors Rarely, a pure epidermoid carcinoma arises
show a more rapid growth rate and metas- from salivary epithelium.
tasize by both lymphatic and hematogenous
routes. It should be noted that nearly 15% DIFFERENTIAL DIAGNOSIS
of patients have other salivary primaries or
Cystic or low-grade mucoepidermoid car-
cancer of other organs.
cinomas are soft, compressible, and often
demarcated and movable. In these instances,
MICROSCOPIC FEATURES clinical differentiation from pleomor-
phic adenoma and other benign tumors is
Low-grade tumors show a tendency for impossible. Indurated fixed carcinomas are
demarcation but lack a capsule. The tumor clinically identical to other salivary adeno-
nests show large cystic spaces lined by carcinomas. Biopsy is necessary to obtain a
stratified squamous epithelium, columnar definitive diagnosis.
ductal cells, and mucus-secreting cells.
Pleomorphism is not a feature. High-grade
TREATMENT
tumors contain a preponderance of epider-
moid cells with a low population of mucous Surgical removal of the entire gland with
cells. Cyst formation is less frequent, with a the tumor is required for both low- and
tendency for tumor cells to grow in sheets. high-grade tumors. Nearly one third of
Clear cells are commonly seen admixed both varieties recur after simple excision.
with the epidermoid component. In fact, Nodal metastases are observed at admis-
some tumors are predominantly clear cell sion in 30% of patients with parotid tumors
tumors and closely resemble renal cell car- and over 50% when the tumor arises in
cinoma. Cytophotometric analysis can dif- the submandibular gland. According to
FIGURE 8-26
Nodular mass of parotid rep-
resenting a mucoepidermoid
carcinoma.
PMPH_Eversole_Chapter-08.indd 328 1/17/2011 3:43:29 PM
Soft Tissue Swellings of the Neck and Face 329
histologic grade, less than 10% with low- A clinicopathologic study of 367 cases. Am J Surg.
grade tumors present with positive nodes, 1978;136:461.
whereas almost 60% of patients with high-
grade tumors exhibit positive palpable
ACINIC CELL CARCINOMA
nodes. If palpable nodes are present, a neck
dissection should be performed. Radia- Figure 8-27
tion therapy is not as effective as surgery Age: Middle-aged adults
in obtaining a cure. Five-year survival for Sex: Female predilection
low-grade tumors is good, exceeding 90%.
Five-year survival for high-grade tumors is CLINICAL FEATURES
less than 50%. Ten-year survival rates are Acinic cell carcinoma occurs primarily in
lower, but the precipitous decrease seen in the substance of the parotid gland, appear-
other salivary malignancies is not a feature ing as a firm nodule, which may be fixed
of mucoepidermoid carcinoma. or somewhat movable. Vague pain is often a
symptom, as is some degree of facial muscle
weakness on the affected side. The duration
Additional Reading is often long, with a history of slow progres-
Boukheris H, Curtis RE, Land CE, Dores GM. Incidence sive enlargement. Despite its early indolent
of carcinoma of the major salivary glands according to course, the tumor is prone to recur after
the WHO classification, 1992 to 2006: a population- simple excision and is capable of both nodal
based study in the United States. Cancer Epidemiol and distant metastases.
Biomarkers Prev. 2009;18:2899-2906.
Eversole LR. Mucoepidermoid carcinoma; review of 815
reported cases. J Oral Maxillofac Surg. 1970;28:490. MICROSCOPIC FEATURES
Jakobsson PA, Blanck C, Eneroth CM. Mucoepidermoid
carcinoma of the parotid gland. Cancer. 1968;22:111. Neoplastic tumor cells are arranged in aci-
Prior P, Waterhouse AH. Second primary cancers nus-like clusters, and cystic spaces are often
in patients with tumors of the salivary glands. Br J a prominent feature. When present, these
Cancer. 1977;36:302.
Spiro RH, Huvos AG, Berk R, Strong EW.
cystic cavities are lined by cells that are not
Mucoepidermoid carcinoma of salivary gland origin. ductal cell types, but have a cobblestone
FIGURE 8-27
Acinic cell carcinoma of the
parotid.
PMPH_Eversole_Chapter-08.indd 329 1/17/2011 3:43:41 PM
330 Chapter 8
pattern and resemble those cells arranged glands; a clinicopathologic study of 77 cases. Cancer.
in the acinar organoid groupings. The indi- 1965;18:1145.
Al-Zaher N, Obeid A, Al-Salam S, Al-Kayyali BS.
vidual cells contain copious amounts of Acinic cell carcinoma of the salivary glands: a litera-
clear or finely granular cytoplasm or may ture review. Hematol Oncol Stem Cell Ther. 2009;2:
be filled with zymogen granules. Whereas 259-264.
the tumor margins are often well defined, Chong GC, Beahrs OH, Woolner LB. Surgical manage-
ment of acinic cell carcinoma of the parotid gland.
neoplastic islands extend beyond the body Surg Gynecol Obstet. 1974;138:65.
of the tumor mass. Dardick I, George D, Jeans MT, et al. Ultrastructural
morphology and cellular differentiation in acinic
cell carcinoma. Oral Surg Oral Med Oral Pathol.
DIFFERENTIAL DIAGNOSIS 1987;63:325.
Because of its slow growth potential, acinic Spiro RH, Huvos AG, Strong EW. Acinic cell carcinoma
of salivary origin, a clinicopathologic study of 67 cases.
cell carcinoma may mimic the clinical fea- Cancer. 1978;41:924.
tures of benign salivary neoplasms, stromal
tumors, and enlarged lymph nodes. When a
firm, slowly enlarging mass in the parotid is
accompanied by pain and facial weakness,
ADENOCARCINOMA NOS
acinic cell carcinoma should be the primary AND MISCELLANEOUS
consideration. Biopsy must be performed to MALIGNANCIES
secure a definitive diagnosis. Figure 8-28
Age: Middle-aged adults
TREATMENT
Sex: Female predilection
Local excision, or even superficial parotidec- CLINICAL FEATURES
tomy, results in recurrence in over 50% of
the cases, whereas total parotidectomy sig- Adenocarcinomas not otherwise specified
nificantly lowers the propensity for recur- (NOS) do not show microscopic features
rence. Overall 5-year survival exceeds 75%. that allow classification with the other
salivary tumors included here. Their fre-
quency of occurrence is on a parity with
Additional Reading adenoid cystic carcinoma with a predilec-
tion for the parotid gland. They are indu-
Abrams AM, Cornyn J, Scofield HH, Hansen LS. rated and fixed to adjacent tissue, may be
Acinic cell adenocarcinoma of the major salivary associated with erythema and telangiecta-
FIGURE 8-28
Adenocarcinoma, not otherwise specified (NOS). Submandibular mass, sialogram showing ductal com-
pression and sialectasia (left and center); extension on to skin (right).
PMPH_Eversole_Chapter-08.indd 330 1/17/2011 3:43:50 PM
Soft Tissue Swellings of the Neck and Face 331
sia of the overlying facial skin, and may illary cystadenocarcinomas are cystic with
compress the facial nerve, thus causing papillary proliferations of columnar cells
paralysis. Approximately 2% of pleomor- displaying pleomorphism, hyperchroma-
phic adenomas develop adenocarcinoma- tism, and mitotic figures.
tous transformation (carcinoma ex pleo-
morphic adenoma), are malignant from DIFFERENTIAL DIAGNOSIS
onset, or metastasize despite a benign his- Adenocarcinoma and the other rare sali-
tologic appearance. Among the adenocar- vary malignancies (epidermoid carcinoma,
cinomas not associated with mixed tumors melanoma, and sarcoma) are indurated and
are histologically distinct subcategories, fixed. They must be differentiated from the
which have been more clearly defined dur- other specific malignant salivary neoplasms
ing the last decade. They include primary and malignant lymphoma by microscopic
squamous cell carcinoma of salivary origin, evaluation.
small (oat) cell carcinoma, clear cell myoep-
ithelioma of intercalated ducts, and papil-
TREATMENT
lary cystadenocarcinoma. Other malignant
tumors arising in salivary glands are quite Wide surgical excision including the entire
rare. Primary melanomas and sarcomas of gland is required. Neck dissection should
stromal origin are included among these be performed in continuity when palpable
rarities. These uncommon salivary neo- nodes are detected clinically. Adenocarci-
plasms all show rapid growth, fixation, and noma NOS is moderately radiosensitive, so
induration. combined radiation therapy and surgery
may be considered in the treatment plan.
Chest radiographs should be procured,
MICROSCOPIC FEATURES
as adenocarcinoma shows a tendency for
Adenocarcinoma NOS is infiltrative, lacking both regional and distant metastasis. The
a capsule. The histomorphology is protean. survival figures for most adenocarcinomas
Tumor cells may be arranged in trabecu- NOS are similar to those for adenoid cystic
lar cords, sheets, or ductal formations. The carcinoma.
cytologic features are also variable, some
tumors showing hyperchromatic mono-
morphic cells, others being pleomorphic or Additional Reading
anaplastic. Malignant mixed tumors (car- Corio RL, Sciubba JJ, Brannon RB, Batsakis JG.
cinoma ex pleomorphic adenoma) show Epithelial-myoepithelial carcinoma of intercalated
the classic features of benign pleomorphic duct origin. A clinicopathologic and ultrastructural
adenoma with foci of malignant trans- assessment of sixteen cases. Oral Surg Oral Med Oral
Pathol. 1982;53:280.
formation displaying the aforementioned Greene GW, Jr, Bernier JL. Primary malignant melano-
characteristics. Salivary squamous cell car- mas of the parotid gland. Oral Surg Oral Med Oral
cinomas exhibit similar features to those of Pathol. 1961;14:108.
surface mucosa origin. Small (oat) cell carci- Rosenfeld L, Sessions DG, McSwain B, Graves H, Jr.
Malignant tumors of salivary gland origin: 37-year
nomas are characterized by solid islands of review of 184 cases. Ann Surg. 1966;163:726.
small pleomorphic hyperchromatic nuclei Spiro RH, Huvos AG, Strong EW. Malignant mixed
without overt evidence of ductal differen- tumor of salivary origin. A clinicopathologic study of
tiation. Clear cell myoepitheliomas fail to 146 cases. Cancer. 1977;39:388.
Takahama Junior A, Almeida OP, Kowalski LP. Parotid
show pleomorphism; rather, they manifest neoplasms: analysis of 600 patients attended at a
small ducts lined by eosinophilic cuboidal single institution. Braz J Otorhinolaryngol. 2009;75:
cells enveloped by sheets of clear cells. Pap- 497-501.
PMPH_Eversole_Chapter-08.indd 331 1/17/2011 3:43:59 PM
332 Chapter 8
Bilateral Parotid and
Submandibular Swellings
ENDEMIC PAROTITIS (MUMPS)
Figure 8-29
Age: Children
Sex: No predilection
CLINICAL FEATURES
Mumps virus, a paramyxovirus, has an
incubation period of 2 to 3 weeks. The ini-
tial parotid swelling is usually unilateral;
enlargement of the opposite gland follows
shortly thereafter. Frequently, only one
gland remains involved. The swelling is dif-
fuse and soft and causes elevation of the ear
lobe. Submandibular involvement is also
common. The swelling is accompanied by
moderate-to-severe pain. An exudate may
be expressed from the parotid duct in some
cases, but not always. Sour foods are intoler-
able, eliciting severe pain. Patients manifest
other signs of infectious disease, including FIGURE 8-29
malaise, headache, and fever. The virus is Endemic parotitis showing diffuse parotid enlarge-
ment in a febrile child.
not limited to salivary tissue; pancreati-
tis and meningitis are complications, and
orchitis may lead to sterility in males. Orchi-
tis develops within 3 to 5 days after parotid in childhood. Serum amylase levels are ele-
swelling if spread to the testes occurs. vated early in mumps, and leukopenia is a
common finding.
MICROSCOPIC FEATURES
TREATMENT
The parotid ducts are dilated and contain
secretion products with inflammatory cells. The patient is infectious and should be con-
The acini manifest degenerative changes fined to bed. A bland diet with added liq-
such as degranulation and vacuolization with uids and prescription of antipyretics and
a mononuclear inflammatory cell infiltrate. analgesics are recommended. Because of
the possibility of orchitis and meningitis,
DIFFERENTIAL DIAGNOSIS the patient’s physician should be consulted.
Mumps must be differentiated from bac-
terial or occlusive salivary inflamma-
tory disease, the benign lymphoepithelial
Additional Reading
lesions (Sjögren’s syndrome, Mikulicz’s dis- Banks P. Nonneoplastic parotid swellings: a review. Oral
Surg Oral Med Oral Pathol. 1968;25:732.
ease), Heerfordt’s syndrome, and parotid Barskey AE, Glasser JW, LeBaron CW. Mumps resur-
lymphoma. Most of these entities occur in gences in the United States: a historical perspective on
adults, whereas mumps is more common unexpected elements. Vaccine. 2009;19;27:6186-6195.
PMPH_Eversole_Chapter-08.indd 332 1/17/2011 3:43:59 PM
Soft Tissue Swellings of the Neck and Face 333
Boodley CA, Jaquis JL. Measles, mumps, rubella and yarteritis nodosa, and scleroderma, such
chickenpox in the adult population. Nurse Pract. instances being referred to as secondary
1989;14:12.
Marcy SM, Kibrick S. Mumps. In: Hoeprich PD. Sjögren’s syndrome. Malignant lymphoma
Infectious Diseases. 2nd ed. Hagerstown, MD: Harper is more common among patients with
& Row; 1977:621. Sjögren’s syndrome, and the lymphoid
malignancies are usually found within the
gland and in extrasalivary locations.
SJÖGREN’S SYNDROME
Figure 8-30 MICROSCOPIC FEATURES
Age: Middle-aged adults The acini are replaced by diffuse infiltra-
Sex: Significant female predilection tive sheets of well-differentiated small and
large lymphocytes. Ductal elements are not
CLINICAL FEATURES
destroyed but manifest cellular prolifera-
Sjögren’s syndrome is a collagen disease tion in the form of epimyoepithelial islands.
of the rheumatoid group of immunopatho- This histology is referred to as autoimmune
logic disorders. The syndrome triad con- lymphoepithelial sialadenitis. Fluorescence
sists of xerostomia, xerophthalmia, and antibody studies show immunofluores-
rheumatic joint disease. The parotid glands cence of ductal epithelium. Intraoral minor
show slight to moderate enlargement bilat- salivary glands show multifocal lymphoid
erally, and milking the glands fails to elicit aggregates dispersed throughout the gland
flow from the ducts. Pain is occasionally lobules and in periductal arrangement.
a symptom. The mouth feels dry, the oral These infiltrates are quantitatively graded
mucosa is often erythematous, and even- from 0 to 4+, whereby 1+ is suspected and
tually cervical dental decay develops. The 2+ or above is typical for the syndrome.
conjunctivas are also dry because of the
lacrimal gland involvement with cessation
DIFFERENTIAL DIAGNOSIS
of secretion, producing keratoconjunctivitis
sicca. Classic signs of rheumatoid arthritis, Diffuse enlargement of the parotid glands
including joint pain and swelling, are pres- in Sjögren’s syndrome is clinically similar to
ent in most patients. All three components that seen in Mikulicz’s disease, Heerfordt’s
of the syndrome are not necessarily coexis- syndrome, parotid lymphoma, and meta-
tent in any one patient. Sjögren’s syndrome bolic sialadenosis. The occurrence in females
may accompany other collagen-immune and existence of other components of the
diseases such as lupus erythematosus, pol- syndrome are essentially classic features of
FIGURE 8-30
Bilateral parotid enlarge-
ment associated with
xerostomia, xerophthalmia,
and rheumatoid arthritis
characterizing Sjögren’s
syndrome.
PMPH_Eversole_Chapter-08.indd 333 1/17/2011 3:44:03 PM
334 Chapter 8
Sjögren’s syndrome. The disease may be con- Henderson JW. Keratoconjunctivitis sicca; review with
firmed by evaluation of parotid flow rates, use survey of 121 additional cases. Am J Ophthalmol.
1950;33:197.
of the Shirmer lacrimation test, and evalua- Scharf J, Scharf Y, Nahir M. Sjögren’s syndrome. Compr
tion of serum for the presence of rheumatoid Ther. 1982;8:40.
(RA) factor as well as specific autoantibodies
(anti-Ro, anti-La). Sialograms reveal multifo-
cal microsialectasia with a “birdshot” appear- MIKULICZ’S DISEASE
ance of contrast medium retention. Labial Figure 8-31
gland biopsy is also useful in diagnosis.
Age: Middle-aged and elderly adults
TREATMENT Sex: Male predilection
Patients with Sjögren’s syndrome should CLINICAL FEATURES
be thoroughly evaluated for the presence Mikulicz’s disease is a benign lymphoe-
of malignant lymphoma and other collagen pithelial lesion of the parotid and lacrimal
diseases. Their care should be managed by glands that occurs in males and is probably
a physician. The disease is treated with ste- a localized form of Sjögren’s syndrome. The
roids or other immunosuppressive therapeu- disease in males is not associated with rheu-
tic agents. Rituximab immunotherapy offers matoid arthritis. The parotid swellings are
some degree of control particularly when soft, movable, and painless. Xerostomia is
some exocrine function is still present. present, yet is rarely as severe as in women
with Sjögren’s syndrome. The term Miku-
Additional Reading licz’s disease is synonymous with local-
ized benign lymphoepithelial lesion and
Bertram U, Halberg P. A specific antibody against the should not be confused with Mikulicz’s syn-
epithelium of the salivary ducts in sera from patients drome, which refers to parotid and lacrimal
with Sjögren’s syndrome. Acta Allergol. 1964;19:458. enlargement due to malignant lymphoma.
Dijkstra PF. Classification and differential diagnosis
of sialographic characteristics in Sjögren syndrome.
Semin Arthritis Rheum. 1980;10:10. MICROSCOPIC FEATURES
Fauchais AL, Ouattara B, Gondran G, et al. Articular
manifestations in primary Sjögren’s syndrome: The microscopic changes in Mikulicz’s dis-
clinical significance and prognosis of 188 patients. ease are identical to those encountered in
Rheumatology (Oxford). 2010;49:1164-1172. Sjögren’s syndrome with the addition of
FIGURE 8-31
Bilateral benign
lymphoepithe-
lial lesions of the
parotid in Mikulicz’s
disease; sialogram
showing a lack of
ductal arboriza-
tion in Mikulicz’s
disease.
PMPH_Eversole_Chapter-08.indd 334 1/17/2011 3:44:15 PM
Soft Tissue Swellings of the Neck and Face 335
IgG4+ plasma cells and elevated IgG4 lev-
els in serum. Additional Reading
Bernier JL, Bhaskar SN. Lymphoepithelial lesions of
DIFFERENTIAL DIAGNOSIS salivary glands. Histogenesis and classification based
on 186 cases. Cancer. 1958;11:1156.
Mikulicz’s disease is differentiated from Kahn LB. Benign lymphoepithelial lesion (Mikulicz’s
Sjögren’s syndrome on the basis of gender disease) of the salivary gland: an ultrastructural study.
Hum. Pathol. 1979;10:99.
and limitation of extent, rheumatoid disease Morgan WS, Castleman BC. Clinicopathologic study of
and systemic autoimmune conditions being “Mikulicz’s disease.” Am J pathol. 1953;29:471.
absent. In all probability, both diseases Romero RW, Nesbitt LT, Jr, Ichinose H. Mikulicz dis-
are merely variations of the same process. ease and subsequent lupus erythematosus develop-
ment. J Am Med Assoc. 1977;237:2507.
Other disorders that must be considered Yamamoto M, Takahashi H, Sugai S, Imai K. Clinical
in the differential diagnosis are malignant and pathological characteristics of Mikulicz’s disease
lymphoma, Heerfordt’s syndrome, dissemi- (IgG4-related plasmacytic exocrinopathy). Autoimmun
nated tuberculosis, and metabolic sialad- Rev. 2005;4:195-200.
enosis. Parotid biopsy discloses the clas-
sic benign lymphoepithelial morphology.
Sialographic changes are identical to those
SARCOID SIALADENITIS AND
seen in Sjögren’s syndrome. HEERFORDT’S SYNDROME
Figure 8-32
TREATMENT
Age: Middle-aged adults
Moderate doses of steroids (e.g., 20-30 mg Sex: No predilection
prednisone daily) may help control the
immune process. The patient may require CLINICAL FEATURES
the use of a water bottle periodically to Sarcoidosis of the salivary glands occurs
relieve xerostomia. in less than 5% of patients suffering from
FIGURE 8-32
Parotid swelling in sarcoidosis.
PMPH_Eversole_Chapter-08.indd 335 1/17/2011 3:44:22 PM
336 Chapter 8
the generalized form of the disease. When Kveim test uses specific antigen to detect
the sarcoid granulomas are present within delayed hypersensitivity and is positive in
the salivary tissue, parotid and lacrimal most cases. Fine-needle aspiration can yield
enlargement and induration are the pri- diagnostic findings.
mary signs. The enlarged glands are firm
to palpation and free from pain, and the TREATMENT
patients are often slightly febrile. The Because generalized sarcoidosis is often
enlargement evolves slowly, requiring present, a thorough physical examination
many months to manifest clinically obvi- is required. The disease is treated with ste-
ous signs. It is usually bilateral but rarely roids or other immunosuppressive agents
symmetric. Diminished flow of saliva from and should be managed by an internist or
the involved glands is a common find- general physician.
ing, and if the granulomatous infiltration
is extensive, xerostomia with widespread
cervical caries may be seen. Sialography
discloses pathologic findings with defi-
Additional Reading
cient secondary and tertiary ducts and dye Chisholm DM, Lyell A, Haroon TS, Mason DK, Beeley
pooling, which yields a clouded pattern JA. Salivary gland function in sarcoidosis. Oral Surg
that represents terminal ectasia. Extensive Oral Med Oral Pathol. 1971;31:766.
Hamner JE, III, Scofield HHL. Cervical lymphadenopa-
lacrimal infiltration leads to xerophthalmia thy and parotid swelling in sarcoidosis; a study of 31
and conjunctivitis. Other manifestations cases. J Am Dent Assoc. 1967;74:1224.
of generalized sarcoidosis, such as hilar Michelson HE. Uveoparotitis. Arch Dermatol Syph.
node enlargement on chest radiographic 1939;39:329.
Nitzan DW, Shteyer A. Sarcoidosis of the parotid salivary
examination, are frequently identifiable. glands. J Oral Maxillofacial Surg. 1982;40:443.
The cause for this tuberculoid granuloma- Kittisupamongkol W. Heerfordt syndrome. QJM.
tous disease is unknown. It is most com- 2009;102:149.
monly encountered in middle European
countries.
TUBERCULOSIS
MICROSCOPIC FEATURES Figure 8-33
Sarcoid sialadenitis is characterized by
multifocal granulomatous infiltration of Age: Middle-aged and elderly adults
Sex: Male predilection
the gland. The epithelioid histiocytes are
admixed with multinucleated giant cells, CLINICAL FEATURES
and the former are arranged in fasciculated Both the parotid and submandibular
whorls. The granulomas are devoid of case- glands may show involvement with Myco-
ation necrosis. bacterium tuberculosis. Diffuse enlargement
occurs in conjunction with disseminated
DIFFERENTIAL DIAGNOSIS
or miliary tuberculosis, along with exten-
The enlargement seen in Heerfordt’s syn- sive pulmonary disease. The enlargement
drome may clinically resemble that seen may be unilateral or bilateral and is more
in Sjögren’s syndrome, Mikulicz’s dis- common in the parotid gland. Pain and
ease, tuberculosis, or lymphoma. A search fistula formation are unusual findings. As
for other signs of generalized sarcoidosis in the case of cervical node scrofula, pri-
should be pursued. Serum calcium levels mary tuberculosis in the absence of pul-
are often elevated. Biopsy reveals the fea- monary infection may develop in parotid
tures of noncaseating granulomas. The lymph nodes. In this form of the disease,
PMPH_Eversole_Chapter-08.indd 336 1/17/2011 3:44:36 PM
Soft Tissue Swellings of the Neck and Face 337
TREATMENT
Isoniazid therapy is the treatment of choice
for typical tubercular lesions.
Additional Reading
Allen-Mersh MG, Forsyth DM. Primary tuberculosis of
the parotid gland. Tubercle. 1958;39:108.
Kant R, Sahi RP, Mahendra NN, Agarwal PK, Shankhdhar
R. Primary tuberculosis of the parotid gland. J Indian
Med Assoc. 1977;68:212.
Mastronikolis NS, Papadas TA, Marangos M, Karkoulias
FIGURE 8-33 KP, Tsamandas AC, Goumas PD. Tuberculosis of the
Tuberculous granulomas in parotid lymph nodes parotid gland. Tuberk Toraks. 2009;57:84-88.
Patey DH, Thackray AC. Tuberculosis of the parotid
and cutaneous fistula.
gland. Arch Middlesex Hosp. 1954;4:256.
Taher AA. Tuberculosis of the parotid salivary
gland—case report. Br J Oral Maxillofac Surg.
the enlargement is unilateral and mani- 1988;26:514.
fests as a firm circumscribed tumefaction.
A drainage tract may appear on the skin.
The tonsil or pharynx is the probable por-
tal of entry in this form. HIV SALIVARY DISEASE
(DIFFUSE INFILTRATIVE
MICROSCOPIC FEATURES LYMPHOCYTOSIS SYNDROME)
Tuberculosis granulomas with epithelioid Figure 8-34
histiocytes and Langhans giant cells are
present. Zones of caseous necrosis are often Age: Children, young adults
but not invariably present. Focal abscess Sex: No predilection
formation with neutrophilic infiltrates is CLINICAL FEATURES
often present, particularly in the localized
Bilateral salivary enlargement has been
primary form.
noted in 10% to 15% of children with AIDS.
Although most children contract the HIV
DIFFERENTIAL DIAGNOSIS
infection perinatally, some have acquired
The firm parotid swelling of disseminated the infection from contaminated blood
tuberculosis must be differentiated from products. Adults can also manifest HIV sal-
Mikulicz’s disease, Sjögren’s syndrome, ivary disease. In both children and adults,
Heerfordt’s syndrome, and malignant lym- the swellings are bilateral and somewhat
phoma. Sialography reveals lakes of pooled firm to palpation; induration is not gener-
contrast medium and foci of ductal stenosis. ally a feature. The overlying skin is of nor-
Tuberculin skin tests and chest radiographs mal color without ulceration, and pain is
are required to obtain a definitive diagno- not a common complaint. Some patients
sis and determine the extent of disease. The present with a Sjögren’s-like disease in
localized form of intrasalivary tuberculosis which the parotid swellings are associated
must be differentiated from salivary tumor, with xerostomia. When the glands are eval-
mesenchymal neoplasms, or sclerosing uated with CT or MRI scanning, soft tissue
sialadenitis. Biopsy discloses specific gran- enlargements are seen in the gland proper
ulomatous inflammation. Acid-fast stains and are riddled with multicystic radiolu-
demonstrate the bacilli. cent foci.
PMPH_Eversole_Chapter-08.indd 337 1/17/2011 3:44:37 PM
338 Chapter 8
HISTOLOGIC FEATURES
The microscopic changes accompanying
HIV-associated salivary disease are pro-
tean and are not well defined, particularly
in children. In adult patients who have been
examined, diffuse lymphocytic infiltration
by CD8 lymphocytes is seen along with fol-
licular hyperplasia and epithelially lined
cystic spaces, the latter two features being
different than those seen in benign lymphoe-
pithelial lesion. Some patients with salivary
enlargement, however, particularly adults,
suffer from non-Hodgkin’s lymphoma.
DIFFERENTIAL DIAGNOSIS
The enlargement seen in HIV infection sim-
ulates the other bilateral salivary enlarge-
ments listed here. Certainly, suspicion
should be heightened among individuals
that constitute HIV-risk groups. CT or MRI FIGURE 8-34
Cystic parotid swelling in HIV sialadenitis.
may be useful owing to the unique multi-
cystic nature of the enlargement. Lower lip
minor gland biopsy may show lymphocytic Kreisel FH, Frater JL, Hassan A, El-Mofty SK. Cystic
infiltrates akin to those seen in Sjögren’s lymphoid hyperplasia of the parotid gland in HIV-
syndrome. Biopsy should be performed positive and HIV-negative patients: quantitative
immunopathology. Oral Surg Oral Med Oral Pathol
in adult patients because lymphoma does Oral Radiol Endod. 2010;109:567-574.
occur in AIDS-risk patients. Shugar JMA, Som PM, Jacobson AL, Ryan JR, Bernard
PJ, Dickman SH. Multicentric parotid cysts and cervi-
TREATMENT cal adenopathy in AIDS patients. A newly recognized
entity: CT and MR manifestations. Laryngoscope.
There is no treatment for HIV salivary 1988;98:772.
disease. In some cases, the enlargement Ulirsch RC, Jaffe ES. Sjögren’s syndrome-like
illness associated with the acquired immunodefi-
diminishes once patients are placed on ciency syndrome-related complex. Hum Pathol.
antiretroviral medications. Unsightly, large 1987;18:1063.
swellings may be surgically excised. When
dry mouth is extant, prevention of dental
caries is essential with institution of a topi- DYSGENETIC CYSTS OF
cal fluoride regimen. THE PAROTID
Figure 8-35
Additional Reading Age: Children
Sex: Females
Gordon JJ, Golbus J, Kertides ES. Chronic lymphade-
nopathy and Sjögren’s syndrome in a homosexual man.
CLINICAL FEATURES
N Engl J Med. 1984;311:1441. Dysgenetic cysts are developmental cysts
Ioachim HL, Ryan JR, Blaugrund SM. Salivary gland
lymph nodes. The site of lymphadenopathies and lym-
that arise from salivary duct epithelium.
phomas associated with human immunodeficiency They appear as bilateral soft fluctuant
virus infection. Arch Pathol Lab Med. 1988;112:1224. parotid swellings, although occasional
PMPH_Eversole_Chapter-08.indd 338 1/17/2011 3:44:38 PM
Soft Tissue Swellings of the Neck and Face 339
Ficarra G, Sapp JP, Christensen RE, Polyakov V.
Dysgenetic polycystic disease of the parotid gland:
report of case. J Oral Maxillofac Surg. 1996;54:1246-
1249.
Ortiz-Hidalgo C, Cervantes J, de la Vega G. Unilateral
polycystic (dysgenetic) disease of the parotid gland.
South Med J. 1995;88:1173-1175.
Seifert G, Thomsen S, Donath K. Bilateral dysgenet-
ic polycystic parotid glands. Morphological analy-
sis and differential diagnosis of a rare disease of the
salivary glands. Virchows Arch A Pathol Anat Histol.
1981;390:273-288.
Work WP. Cysts and congenital lesions of the
parotid gland. Otolaryngol Clin North Am.
1977;10:339-343.
METABOLIC SIALADENOSIS
Figure 8-36
FIGURE 8-35 Age: Middle-aged and elderly adults
Bilateral dysgenetic cysts of the parotid in an adult. Sex: Female predilection
CLINICAL FEATURES
unilateral instances have occurred. On sia-
Metabolic sialadenosis is not a single spe-
lograms pockets of dye are retained and on
cific disorder but, rather, an alteration both
MRI a polycystic pattern is seen within the
clinically and functionally of the salivary
parotid parenchyma.
glands that accompanies a variety of gen-
eralized metabolic disorders. The most
MICROSCOPIC FEATURES
common of these diseases are hormonal
Multiple dilated cysts are seen and are lined imbalances (including changes evolving in
by cuboidal cells that are reminiscent of conjunction with menopause, pregnancy,
intercalated ducts of normal glands. There and menarche), alcoholism, and a salivary
is no inflammatory element present. manifestation of diabetes mellitus. Simi-
lar changes may also be seen in hypothy-
DIFFERENTIAL DIAGNOSIS roidism, cirrhosis, and uremia. In all of
HIV salivary disease is included in the these disorders, the parotid is the salivary
differential diagnosis. Otherwise, there gland most often affected. Preauricular
are very few disorders that cause bilateral soft movable swellings are seen bilaterally
parotid swellings in children. in sex hormonal sialadenosis, whereas the
swellings are more prominent below and
TREATMENT behind the mandibular angle in diabetic
sialadenosis. Salivary flow is diminished,
No treatment is necessary unless a bacterial
there is no pain, and the patients are
sialadenitis occurs for which antibiotics and
afebrile.
ductal dilation are recommended.
MICROSCOPIC FEATURES
Additional Reading Both acinar and ductal cells appear edema-
Batsakis JG, Raymond AK. Sialocysts of the parotid tous with cloudy swelling. Degranulation of
glands. Ann Otol Rhinol Laryngol. 1989;98:487-489. zymogen secretory granules is a prominent
PMPH_Eversole_Chapter-08.indd 339 1/17/2011 3:44:40 PM
340 Chapter 8
cal evaluation are required to uncover the
underlying, coexisting metabolic disorder.
TREATMENT
Treatment consists of correcting the under-
lying metabolic disturbance and should be
managed by a physician.
Additional Reading
Chilla R. Sialadenosis of the salivary glands of the
head. Studies on the physiology and pathophysiology
of parotid secretion. Adv Otorhinolaryngol. 1981;
26:1.
Lyon E. Swelling of parotid gland and diabetes mellitus.
Gastroenterologia. 1943;68:139.
Nassour DN, Patel SV, Kosseifi SG, Jordan RM, Peiris
AN. Marked bilateral parotid enlargement in metabol-
ic syndrome: a case report and review of the literature.
Tenn Med. 2007;100:39-41.
Rauch S, Gorlin RJ. In: Gorlin RJ, Goldman HM.
Thoma’s Oral Pathology. Vol. 2. 6th ed. St Louis, MO:
C. V. Mosby; 1970:986.
Scott J, Burns J, Flower EA. Histological analysis of
parotid and submandibular glands in chronic alcohol
abuse: a necropsy study. J Clin Pathol. 1988;41:837.
FIGURE 8-36
Metabolic sialadenosis associated with diabetes.
Midline Neck Swellings
THYROGLOSSAL TRACT CYST
Figure 8-37
feature, and extensive fatty infiltration of
the stroma is observed. Age: Children and young adults
Sex: No predilection
DIFFERENTIAL DIAGNOSIS CLINICAL FEATURES
The slow-growing soft enlargement seen in Derived from epithelium that coursed
metabolic diseases with salivary involve- through the neck during thyroid organo-
ment is unusual; however, the disease genesis, the thyroglossal tract cyst may be
must be differentiated from other chronic localized anywhere between the foramen
sialadenopathies manifesting bilateral caecum at the base of the tongue and the
enlargement such as Sjögren’s syndrome, mature thyroid gland in the lower midline
Mikulicz’s disease, Heerfordt’s syndrome, of the neck. The cyst is firm or soft and com-
tuberculosis, and lymphoma. Sialograms pressible, freely movable (unless entwined
may appear normal; however, close scrutiny with the hyoid bone), and frequently devel-
usually discloses a filamentous, fine net- ops a fistula. Most are located below the
work of ducts. Analysis of parotid electro- hyoid bone. If localized in the tongue or
lytes is helpful, as potassium levels are ele- hyoid region, dysphagia may be a symp-
vated and sodium values are decreased in tom. Rarely, thyroid carcinoma may arise
sialadenosis. A thorough history and physi- from remnants of the tract.
PMPH_Eversole_Chapter-08.indd 340 1/17/2011 3:44:40 PM
Soft Tissue Swellings of the Neck and Face 341
FIGURE 8-37
Thyroglossal tract cysts appearing as a small nodule in the flexure of the midline of the neck.
MICROSCOPIC FEATURES and methods for resection. Ann Otol Rhinol Laryngol.
1988;97:483.
The cyst is lined by stratified squamous or Iwata T, Nakata S, Tsuge H, et al. Anatomy-based sur-
respiratory epithelium. The fibrous wall gery to remove thyroglossal duct cyst: two anomalous
may evince a mild mononuclear inflamma- cases. J Laryngol Otol. 2010;124:443-446.
tory cell infiltrate, and both mucous glands
and thyroid follicles can be observed.
GOITER
DIFFERENTIAL DIAGNOSIS Figure 8-38
Cysts located high in the midline of the
Age: Middle-aged adults
neck must be differentiated from the
Sex: Female predilection
dermoid cyst; if they are located low in
the neck, goiter and thyroid neoplasms CLINICAL FEATURES
must be considered in the differential Goiter refers to benign thyroid enlargement.
diagnosis. Many forms exist, including iodine deficiency
goiter, adenomatous goiter, and hyperthy-
TREATMENT roidism with exophthalmos (Graves’ dis-
Simple excision is the treatment of choice. ease). When hypothyroidism accompanies
When the cyst is intimately associated goiter, the patients are dull and lethargic,
with the hyoid bone, it may be necessary to and if the condition is severe, they show
remove a portion of the bone to ensure com- diffuse myxedema of the soft tissues. The
plete excision and avoid recurrence. enlargement, located below the thyroid car-
tilage in the midline, is firm or compressible,
movable, and in adenomatous goiter, mul-
Additional Reading tinodular. In Graves’ disease, the metabolic
rate is elevated, the patients are nervous and
Bollock WF, Stevenson EO. Cysts and sinuses of the thy- tense, and the goitrous swelling lacks nodu-
roglossal duct. Am J Surg. 1966;112:225. larity, being diffuse. Large goiters in elderly
Butler EC, Dickey JR, Shill OS, Jr, Shalak E. Carcinoma
patients may cause airway obstruction.
of the thyroglossal duct remnant. Laryngoscope.
1969;79:264.
Gross RE, Connerly ML. Thyroglossal cysts and sinus- MICROSCOPIC FEATURES
es; a study and report of 198 cases. N Engl J Med.
1940;223:616.
The histologic findings vary depending on
Hoffman MA, Schuster SR. Thyroglossal duct remnants the type of goiter. In iodine deficiency and
in infants and children: reevaluation of histopathology adenomatous goiter, the thyroid follicles are
PMPH_Eversole_Chapter-08.indd 341 1/17/2011 3:44:43 PM
342 Chapter 8
enlarged and impacted with thyroglobulin. Bell GO, Eisenbeis CH, Jr. The nontoxic nodular hyper-
In Graves’ disease, the follicular epithelium plastic goiter. N Engl J Med. 1955;253:812.
Hennemann G. Non-toxic goitre. Clin Endocrinol Metab.
shows hyperplasia. 1979;8:167.
Taylor S. Genesis of the thyroid nodule. Br Med Bull.
1960;16:102.
DIFFERENTIAL DIAGNOSIS
Zorrilla L, Tsai J, Freedman M. Airway obstruction
The goitrous conditions must be differenti- due to goiter in older patients. J Am Geriatr Soc.
ated from one another on the basis of clinical 1989;37:1153.
signs and symptoms. Metabolic studies evalu-
ating 131iodine uptake and radioactive thyroid
scans are useful, as is evaluation of serum THYROID NEOPLASIA
T3 and T4 levels. The diffuse nature of the Figure 8-39
swelling usually allows differentiation from
tumor; however, when the swelling is small Age: Middle-aged adults
or located just lateral to the midline, neoplasia Sex: Female predilection
in the thyroid gland must be considered. CLINICAL FEATURES
TREATMENT Thyroid neoplasms may be benign ade-
nomas or malignant adenocarcinomas.
Some goiters can be treated surgically, oth-
They are classified according to their his-
ers medically. Referral to an internist or
tomorphology. The benign adenomas arise
endocrinologist is recommended.
in one pole of the gland so that they are
located slightly lateral to the laryngeal car-
Additional Reading tilage. The tumors are generally small and
may not be visually obvious; rather, they
Barczyński M, Konturek A, Hubalewska-Dydejczyk A, are often detected by palpation. They are
Gołkowski F, Cichoń S, Nowak W. Five-year follow- soft or slightly firm and movable. Adeno-
up of a randomized clinical trial of total thyroidectomy
versus dunhill operation versus bilateral subtotal thy- carcinomas manifest a similar localization,
roidectomy for multinodular nontoxic goiter. World J but tend to be firm or indurated and fixed
Surg. 2010;34:1203-1213. to adjacent tissues. They, too, may be small
FIGURE 8-38
Diffuse swelling in the
thyroid area represent-
ing nontoxic goiter (right)
and Graves’ disease with
exophthalmos (left).
PMPH_Eversole_Chapter-08.indd 342 1/17/2011 3:44:54 PM
Soft Tissue Swellings of the Neck and Face 343
when first detected. Indeed, cervical node manage the care of patients with thyroid
metastasis may be detected before a notice- neoplasms.
able thyroid enlargement presents itself.
MICROSCOPIC FEATURES
Additional Reading
Harwick RD. Thyroid cancer—surgical decision making.
It is beyond the scope of this book to out- Semin Oncol. 1980;7:392.
line the microscopic features of thyroid Hawk WA, Hazard JB. The many appearances of pap-
tumors. The more common benign neo- illary carcinoma of the thyroid. Cleve Clin J Med.
plasms are fetal and follicular adenomas. 1976;43:207.
Liechty RD, Graham M, Freemeyer P. Benign
Papillary carcinoma is the most common
solitary thyroid nodules. Surg Gynecol Obstet.
form of thyroid cancer. Medullary carci- 1965;121:571.
noma may arise in conjunction with oral Sippel RS, Chen H. Controversies in the surgical man-
neuromas and other endocrine neoplasms agement of newly diagnosed and recurrent/residual
as a component of the neuropolyendocrine thyroid cancer. Thyroid. 2009;19:1373-1380.
Willis J. Incidence and aetiology of thyroid carcinoma. Br
syndrome. Med J. 1961;1:1646.
DIFFERENTIAL DIAGNOSIS
DERMOID CYST
Neoplastic swellings in the thyroid region Figure 8-40
must be differentiated from one another by
microscopic evaluation. Rarely, they must Age: Adults
be differentiated from goiter. Sex: No predilection
CLINICAL FEATURES
TREATMENT The dermoid cyst is usually encountered
Most thyroid tumors are treated surgically. in the oral floor. When it arises inferior to
Those that take up iodine may be treated the mylohyoid muscle, it protrudes inferi-
with 131iodine radiotherapy. An onco- orly, as an extraoral swelling in the upper
logic surgeon or otolaryngologist should midline of the neck in the submental flex-
FIGURE 8-39
Thyroid adenoma (left); papillary
carcinoma (right).
PMPH_Eversole_Chapter-08.indd 343 1/17/2011 3:45:06 PM
344 Chapter 8
ure area. The mass is movable and has a New EB, Erich JB. Dermoid cysts of the head and neck.
doughy consistency on palpation. Surg Gynecol Obstet. 1937;65:48.
Seward GR. Dermoid cysts of the floor of the mouth. Br
J Oral Surg. 1965;3:36.
MICROSCOPIC FEATURES
The cyst is lined by keratinizing stratified
squamous epithelium. Skin adnexal tissues Growths and Swellings of
such as sebaceous glands, sweat glands, and the Facial Skin
hair follicles are present within the fibrous
wall. When all three germ layers can be NEVI
demonstrated, the lesions are termed tera- Figure 8-41
toid cysts.
Age: Childhood onset
DIFFERENTIAL DIAGNOSIS Sex: No predilection
A superiorly located thyroglossal tract cyst CLINICAL FEATURES
may simulate the dermoid cyst. Sebaceous Moles or nevi are the most common swell-
cysts should also be considered in the dif- ings of the facial skin. They are usually less
ferential diagnosis. than 1 cm in diameter, may be multiple, and
are either brown, blue, or nonpigmented.
TREATMENT
Most importantly, benign nevi are symmet-
Simple excision using an extraoral approach rically round or oval with smooth nonjag-
is recommended for dermoid cysts located ged borders. Once they reach a certain size,
below the mylohyoid muscle. they stop growing.
MICROSCOPIC FEATURES
Additional Reading Nevi may be junctional, compound, or
al-Khayat, M, Kenyon GS. Midline sublingual dermoid
intradermal. The nevus cells contain vari-
cyst. J Laryngol Otol. 1990;104:578. able amounts of melanin pigment if clini-
Burger MF, Holland P, Napier B. Submental midline cally pigmented. Nonpigmented nevi are
dermoid cyst in a 25-year-old man. Ear Nose Throat J. composed of sheets and theques of polygo-
2006;85:752-753.
nal epithelioid cells devoid of melanin gran-
Kinnman J, Suh KW. Dermoid cysts of the floor of the
mouth: report of three cases. J Oral Maxillofac Surg. ules. A unique lesion, common on the face,
1968;26:190. is the deep penetrating nevus, which shows
FIGURE 8-40
Midline swelling of neck and sub-
mandibular region representing
a dermoid cyst; contrast media
showing cystic wall.
PMPH_Eversole_Chapter-08.indd 344 1/17/2011 3:45:12 PM
Soft Tissue Swellings of the Neck and Face 345
melanoma-like cells that extend deeply into the recent literature. Am J Med Sci. 1955;229:444,
the dermis. 583.
Castilla EE, da Graca Dutra M, Orioli-Parreiras
IM. Epidemiology of congenital pigmented naevi.
DIFFERENTIAL DIAGNOSIS I. Incidence rates and relative frequencies. Br J
Dermatol. 1981;104:307.
Pigmented nevi are differentiated from
Jacobs AH. Birthmarks: II. Melanocytic and epidermal
melanoma on the basis of history and nevi. Pediatrics. 1979;64:47.
clinical appearance. A long duration with Kamino H, Ackerman AB. A histologic atlas of some com-
arrested growth and lack of ulceration are mon benign pigmented lesions of the skin. J Dermatol
indicators of a benign lesion. Should a pig- Surg Oncol. 1979;5:718.
Margulis A, Adler N, Bauer BS. Congenital melano-
mented lesion continue to grow or ulcer- cytic nevi of the eyelids and periorbital region. Plast
ate, a biopsy is indicated. Nonpigmented Reconstr Surg. 2009;124:1273-1283..
nevi must be differentiated from basal cell
carcinoma, adnexal skin tumors, and seba-
ceous cysts. Basal cell carcinomas show SEBACEOUS CYST
progressive growth and often ulcerate. If Figure 8-42
they are not ulcerated, they usually show
surface telangiectasia. Age: Young adults
Sex: No predilection
TREATMENT CLINICAL FEATURES
Skin nodules that are pigmented or non- Sebaceous and epidermoid cysts are derived
pigmented and lack ulceration or telangi- from the pilosebaceous apparatus. Similar
ectasia, if they have persisted unchanged cysts result from implantation of surface epi-
for many years, are probably nevi. No treat- thelium after a cut or laceration. The cysts are
ment is required. Excisional biopsy is rec- often quite superficial and small; however,
ommended if recent growth has occurred, they can exceed 2 to 3 cm in diameter. When
if the lesion is ulcerated, or if surface telang- superficial, they have a pearly, blanched
iectasia is encountered. quality. Larger cysts are fixed to the dermis
yet can be moved about over the subcutane-
Additional Reading ous tissues and are compressible; they have
a doughy consistency. When multiple seba-
Beerman H, Lane RAG, Shaffer B. Pigmented nevi and ceous cysts are encountered, work-up for
malignant melanoma of the skin. A survey of some of Gardner’s syndrome should be undertaken.
FIGURE 8-41
Benign nevi with smooth
borders.
PMPH_Eversole_Chapter-08.indd 345 1/17/2011 3:45:20 PM
346 Chapter 8
MICROSCOPIC FEATURES Holmes R, Black MM. Steatocystoma multiplex with
unusually prominent cysts on the face. Br J Dermatol.
The lumen is filled with an eosinophilic 1980;102:711.
caseous material, and shredded keratin Klin B, Ashkenazi H. Sebaceous cyst excision with mini-
fibers desquamate from the keratinizing mal surgery. Am Fam Physician. 1990;41:1746.
McGavran MH, Binnington B. Keratinous cysts of the
stratified squamous epithelium. The wall
skin. Arch Dermatol. 1966;94:499.
is often ruptured with keratin and epi- Yang HJ, Yang KC. A new method for facial epider-
thelial cells embedded within the fibrous moid cyst removal with minimal incision. J Eur Acad
wall. A foreign-body reaction with multi- Dermatol Venereol. 2009;23:887-890.
nucleated giant cells is seen under these
circumstances. A specific type of cyst is
derived from the hair follicle, which con- SEBORRHEIC KERATOSIS
tains basophilic epithelial cells and lumi- Figure 8-43
nally oriented ghost cells (eosinophilic
epidermal cells with vacuolated spaces in Age: Middle-aged and elderly adults
place of nuclei). This specific type of pilar Sex: No predilection
cyst is known as the calcifying epithelioma CLINICAL FEATURES
of Malherbe. Seborrheic keratoses usually occur in mul-
tiples. They are focal papular or nodular
DIFFERENTIAL DIAGNOSIS lesions with a brown waxy character, so
superficial that they appear to have been
Sebaceous and epidermoid cysts, particu-
“stuck on” to the skin. They are not encoun-
larly when superficial, resemble basal cell
tered in young individuals, but become
carcinoma, adnexal skin tumors, or benign
more numerous with advancing age. Etiol-
mesenchymal tumors.
ogy is unknown.
TREATMENT MICROSCOPIC FEATURES
Surgical enucleation of the cyst is the treat- The epithelium evinces acanthosis that is
ment of choice, although a minimal-incision exophytic, with a smooth surface. Invagi-
technique has proven successful. nation of epidermal cells into the dermis
is not a feature. The acanthotic epithelium
Additional Reading may contain keratin pearls and cysts or
may evince a retiform pattern with accom-
Erich JB. Sebaceous, mucous, dermoid and epidermoid panying dermal connective tissue papillae.
cyst. Am J Surg. 1940;50:672. Acantholysis is typically observed.
FIGURE 8-42
Sebaceous cyst of the skin.
PMPH_Eversole_Chapter-08.indd 346 1/17/2011 3:45:26 PM
Soft Tissue Swellings of the Neck and Face 347
DIFFERENTIAL DIAGNOSIS Chen M, Shinmori H, Takemiya M, Miki Y. Acantholytic
variant of seborrheic keratosis. J Cutan Pathol.
Because of their pigmentation, seborrheic 1990;17:27.
keratoses may be confused with nevi. Molokhia MM, Portnoy B. A study of dendritic cells in
Nevi are not as superficial, lack the waxy seborrheic warts. Br J Dermatol. 1971;85:254.
Rowe L. Seborrheic keratosis. I. “Pseudoepitheliomatous
or oily character of seborrheic keratosis,
hyperplasia” (Weidman). J Invest Dermatol.
and do not become prevalent with advanc- 1957;29:165.
ing age.
TREATMENT ADNEXAL SKIN TUMORS
No treatment is necessary. If cosmesis is a Figure 8-44
problem, the keratosis can be shaved super-
ficially or cauterized. Age: Middle-aged and elderly adults
Sex: Male predilection
CLINICAL FEATURES
Additional Reading Tumors of skin that are derived from, or
Becker SW. Seborrheic keratosis and verruca, with spe- differentiate along, the lines of the skin
cial reference to the melanotic variety. Arch Dermatol appendages commonly arise on the face.
Syph. 1951;63:358. Hair follicle tumors (trichoepithelioma),
Brodsky J. Management of benign skin lesions commonly
affecting the face: actinic keratosis, seborrheic kera-
sebaceous cell adenomas, and sweat gland
tosis, and rosacea. Curr Opin Otolaryngol Head Neck adenomas (eccrine acrospiroma, hidrade-
Surg. 2009;17:315-320. noma) are all benign neoplasms. Malignant
FIGURE 8-43
Scaly nodule of scalp in an elderly
male representing seborrheic
keratosis.
PMPH_Eversole_Chapter-08.indd 347 1/17/2011 3:45:30 PM
348 Chapter 8
counterparts occur but are rare. The adn- Kligman AM, Pinkus H. The histogenesis of nevoid
exal skin tumors as a group may be either tumors of the skin. Arch Dermatol. 1960;81:922.
Mellette JR, Amonette RA, Gardner JH, Chesney TM.
uninodular or multinodular. Most are firm, Carcinoma of sebaceous glands on the head and
painless, and nonulcerated; however, malig- neck. A report of four cases. J Dermatol Surg Oncol.
nant varieties are often ulcerated with sur- 1981;7:404.
face telangiectasia. Ntomouchtsis A, Vahtsevanos K, Patrikidou A, Andreadis
C, Tsobanidou C, Antoniades K. Adnexal skin
carcinomas of the face. J Craniofac Surg. 2009;20:
MICROSCOPIC FEATURES 134-137.
The adnexal skin tumors vary considerably
in their histomorphologic characteristics.
They are composed of epithelial cells that BASAL CELL CARCINOMA
differentiate along pilar, sebaceous, or ade- Figure 8-45
nomatoid lines.
Age: Middle-aged and elderly adults
DIFFERENTIAL DIAGNOSIS Sex: Male predilection
The nodular swellings of adnexal skin CLINICAL FEATURES
tumors must be differentiated microscopi- The basal cell carcinoma is an aggressive yet
cally from one another. Clinically, they have nonmetastasizing neoplasm of the skin; rare
features in common with basal cell carcino- instances of metastasis have been reported.
mas, mesenchymal dermal neoplasms, and Over 90% of all basal cell carcinomas are
sebaceous cysts. encountered on the skin of the upper face
and forehead. The tumor may be solitary or
TREATMENT multiple; it tends to occur in patients with
Surgical excision is the treatment of choice. fair complexions and in those who are con-
stantly exposed to solar radiation. The early
tumor may be a smooth-surfaced nodule
Additional Reading with telangiectasia, a focal ulcer, or a nod-
ule with central keratosis. Large lesions
Johnson BL, Helwig EB. Eccrine acrospiroma; a clinico- are ulcerative with rolled, indurated mar-
pathologic study. Cancer. 1969;23:641.
King AI, Klima M, Johnson P. Sweat gland tumors of the
gins. Multiple basal cell tumors that show a
head and neck. Arch Otolaryngol Head Neck Surg. slow growth rate or reach a given size and
1982;108:48. become static may be seen in children and
FIGURE 8-44
Adnexal skin tumors. Syringoma (top), microcystic adenocarcinoma (bottom left), sebaceous cell carci-
noma (bottom right).
PMPH_Eversole_Chapter-08.indd 348 1/17/2011 3:45:44 PM
Soft Tissue Swellings of the Neck and Face 349
young adults suffering from odontogenic which is significantly less prevalent on the
keratocysts of the jaws and a bifid rib. This face. Specific granulomatous infection must
triad, in conjunction with other anomalies, also be considered in the differential diag-
constitutes the nevoid basal cell carcinoma nosis. Biopsy is required to obtain a defini-
syndrome. tive diagnosis.
MICROSCOPIC FEATURES TREATMENT
Surface epithelium shows a transition, Basal cell carcinoma requires excision with
whereby neoplastic cords and islands of a 1-cm margin from the clinically obvious
hyperchromatic monomorphic basaloid- tumor. This is necessary to avoid recurrence,
appearing epithelial cells demonstrate because the neoplasm commonly displays
invasion into the dermis. The center of the microscopic invasion or multicentricity that
neoplastic cell nests may contain keratin is often not visually detectable clinically.
pearls; however, acanthotic squamous cells Mohs surgical technique is used to obtain
mimicking the normal spinous cell layer are clear margins.
not typically present. Adenoid forms with
tubular rete-ridge cords and ductal patterns
are occasionally encountered. The morphea
Additional Reading
type shows extensive desmoplasia. Creschickter CF, Koehler HP. Ectodermal tumors of the
skin. Am J Cancer. 1935;23:804.
Gellin GA, Kopf AW, Garfinkel L. Basal cell epithelioma.
DIFFERENTIAL DIAGNOSIS Arch Dermatol. 1965;91:38.
Early basal cell carcinomas lacking ulceration Gorlin RJ. Nevoid basal-cell carcinoma syndrome.
Medicine. 1987;66:98.
must be differentiated from nonpigmented Levine HL, Bailin PL. Basal cell carcinoma of the
nevi, adnexal skin tumors, mesenchymal head and neck: identification of the high risk patient.
dermal tumors, and sebaceous cysts. Sur- Laryngoscope. 1980;90:955.
face telangiectasia is strongly indicative of Mosterd K, Krekels GA, Nieman FH, et al. Surgical
excision versus Mohs’ micrographic surgery for pri-
basal cell carcinoma. Larger lesions with mary and recurrent basal-cell carcinoma of the face:
ulceration and rolled margins must be dif- a prospective randomised controlled trial with 5-years’
ferentiated from squamous cell carcinoma, follow-up. Lancet Oncol. 2008;9:1149-1156.
FIGURE 8-45
Basal cell carcinoma of the face showing rolled margins with central ulceration.
PMPH_Eversole_Chapter-08.indd 349 1/17/2011 3:45:53 PM
350 Chapter 8
SQUAMOUS CELL show hyperchromatism, pleomorphism,
CARCINOMA and mitotic activity. Spindle cell variants
Figure 8-46 may occur and there are lesions that show
acantholytic change termed pseudoglanular
Age: Adults squamous cell carcinoma.
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES
Included in the differential are basal cell car-
Squamous cancers of the face usually occur
cinoma, metastatic carcinoma, adnexal car-
above the level of the lower lip; many arise
cinomas, and amelanotic melanoma. Biopsy
from a preexisting actinic keratosis that has
is required for a definitive diagnosis.
undergone dysplastic changes. The lesions
are tumefactive and indurated with surface
TREATMENT
ulceration and telangiectasia. As with basal
cell carcinoma, actinic radiation is a pri- Wide excision is required with 1.5-cm mar-
mary carcinogenic factor. Unlike basal cell gins, or Moh’s surgery can be performed,
carcinoma, cutaneous squamous cell carci- ensuring that margins are clear. The
nomas have metastatic potential, spreading regional nodes should be assessed clinically
regionally to the intraparotid and cervi- and by MR or positron emission tomogra-
cal lymph nodes. Perineural invasion may phy imaging.
occur and lesions on the lip may spread to
the mental and inferior alveolar nerve pre-
senting with a numb lip. Additional Reading
MICROSCOPIC FEATURES Ebrahimi A, Moncrieff MD, Clark JR, et al. Predicting
the pattern of regional metastases from cutaneous
Surface stratified squamous epithelium squamous cell carcinoma of the head and neck based on
shows dysplastic changes, and islands of location of the primary. Head Neck. 2010;32(10):1288-
1294.
neoplastic squamous epithelium invade Mohammed AM, Bagatin M, Orihovac Z. Perineural inva-
the underlying dermis. Keratin pearl for- sion by carcinoma of the lower lip. J Craniomaxillofac
mation is usually seen and individual cells Surg. 1995;23:155-159.
FIGURE 8-46
Squamous cell carcinoma
of facial skin.
PMPH_Eversole_Chapter-08.indd 350 1/17/2011 3:46:06 PM
Soft Tissue Swellings of the Neck and Face 351
Mourouzis C, Boynton A, Grant J, et al. Cutaneous head MICROSCOPIC FEATURES
and neck SCCs and risk of nodal metastasis—UK expe-
rience. J Craniomaxillofac Surg. 2009;37:443-447. The histologic features are similar to those
Peterson E, Murphy RX, Jr, Risch VR, Hallock GG. of a well-differentiated squamous cell car-
Regional lymphatic dissemination of squamous cinoma. A central zone composed of volu-
cell carcinoma of the face. Plast Reconstr Surg.
minous strata of keratin and parakeratin is
2009;123(1):21e-22e.
observed. The spinous cell layer is thick-
ened and rete-ridge formation is present,
yet invasion of the dermis is not observed.
KERATOACANTHOMA Pathognomonic features of this tumor are
Figure 8-47 identifiable at the lateral margins. The acan-
thotic central core shows lipping at the mar-
Age: Middle-aged adults gins, and at this point, an abrupt transition
Sex: Male predilection
into normal epithelium is observed.
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
Keratoacanthoma is a benign tumor of
epithelial origin. It may be solitary or multi- The umbilicated nodule with a keratin plug,
focal. Multiple keratoacanthoma is a domi- typical for keratoacanthoma, may also be
nantly inherited disorder. The tumor is encountered with basal and squamous cell
characterized by an elevation with rolled carcinomas and with some adnexal tumors
margins and a central keratotic core; the of skin.
margins are sharply delineated. The lesion
TREATMENT
may occur anywhere, but is most frequently
seen on the extremities and the face. The Excision is the treatment of choice. Waiting
tumor proliferates rapidly, becomes static for spontaneous involution is not advisable
with regard to growth, and within 6 to 12 for two reasons: (1) one cannot be assured
months spontaneously involutes, leaving a clinically that the lesion does indeed rep-
depressed scar. resent keratoacanthoma rather than cancer,
FIGURE 8-47
Keratoacanthoma of facial
skin showing rolled bor-
ders with a central kera-
totic plug.
PMPH_Eversole_Chapter-08.indd 351 1/17/2011 3:46:20 PM
352 Chapter 8
and (2) the scar remaining after surgery is sheath neoplasms arise on the facial skin.
often more cosmetic than that which devel- The former are quite soft, compressible,
ops after spontaneous regression. and movable. The latter are uninodular or
multinodular, firm, and movable. Multiple
Additional Reading neurofibromatous nodules and brown café-
au-lait macules are encountered in von
Flannery GR, Muller HK. Immune response to human Recklinghausen’s disease of skin. Other
keratoacanthoma. Br J Dermatol. 1979;101:625. mesenchymal tumors also arise here, but
Ghadially FN, Barton BW, Kerridge DF. The etiology of
keratoacanthoma. Cancer. 1963;16:603.
are rare.
Goodwin RE, Fisher GH. Keratoacanthoma of the
head and neck. Ann Otol Rhinol Laryngol. MICROSCOPIC FEATURES
1980;89:72.
Reed RJ. Actinic keratoacanthoma. Arch Dermatol. The benign connective tissue tumors are
1972;106:858. encapsulated or well localized and fail to
Yazdani N, Khorsandi-Ashtiani M, Rabbani-Anari M, show pleomorphism. Their differentiation
Bassam A, Kouhi A. Nasal vestibular huge keratoacan- depends on the tissue cells of origin.
thoma: an unusual site. Pak J Biol Sci. 2009;12:1385-
1387.
DIFFERENTIAL DIAGNOSIS
Benign mesenchymal tumors have a
MESENCHYMAL TUMORS smooth surface and are soft or firm. These
Figure 8-48 features may be seen with sebaceous cysts,
nonpigmented nevi, and adnexal tumors of
Age: Young and middle-aged adults skin. Microscopic examination is required
Sex: No predilection to determine the cell of origin.
CLINICAL FEATURES
TREATMENT
Mesenchymal neoplasms arising in the der-
mal and subcutaneous connective tissues Local excision is the treatment of choice.
of the face are uncommon. The superficial Recurrence rate for most mesenchymal neo-
dermatofibroma shows a smooth or slightly plasms of the skin is quite low.
keratotic surface and is pale brown or pink,
which may blanch on pressure. Heman-
giomas are also seen on the face, may be Additional Reading
flat or tumefactive, are reddish purple, and Adair FE, Pack GT, Farrior JH. Lipomas. Am J Cancer.
blanch on pressure. Lipomas and neural 1932;16:1104.
FIGURE 8-48
Mesenchymal tumors
(left), hemangioma (right),
CT scan, dermatofibro-
saracoma protuberans.
PMPH_Eversole_Chapter-08.indd 352 1/17/2011 3:46:30 PM
Soft Tissue Swellings of the Neck and Face 353
Mandal RV, Duncan LM, Austen WG, Jr, Nielsen GP. spread. The prognosis is based on depth of
Infiltrating intramuscular spindle cell lipoma of the invasion as assessed microscopically.
face. J Cutan Pathol. 2009;36(suppl 1):70-73.
Meigel WN, Ackerman AB. Fibrous papule of the face.
Am J Dermatopathol. 1979;1:329.
MICROSCOPIC FEATURES
Ross DE. Skin manifestations of von Recklinghausen’s Melanomas show a variety of histomor-
disease and associated tumors (neurofibromatosis).
Am Surg. 1965;31:729.
phologic features. In superficial spread-
Watson WL. Blood and lymph vessel tumors in children. ing melanoma the malignant melanocytes
J Pediatr. 1939;15:401. proliferate along the basal layer of the epi-
thelium, spreading laterally. The cells show
nuclear atypia, a feature that differentiates
MALIGNANT MELANOMA them from junctional nevi. As lesions prog-
Figure 8-49 ress, they invade into the papillary dermis
and later into the reticular dermis. In skin,
Age: Elderly the Breslow method of invasion depth is
Sex: No predilection used as a prognosticator among other fac-
CLINICAL FEATURES tors. The invasive lesions may comprise
Melanocyte malignancy in the facial spindle cells, round cells, or pleomorphic
region, typically the malar region, most cells and most, yet not all, show melanin
often begins as superficial spreading mela- pigment granules. The early invasive lesions
noma characterized by a variegated color- are considered as thin melanomas whereas
ation of black, blue, brown, and white with the late, more extensive, tumors are referred
irregular margins. Ultimately, nodules may to as thick melanomas. The immunohis-
evolve indicating progression to invasive tochemical markers positive in melanoma
disease. Some melanomas of facial skin are HMB45, S-100, Vimentin, and Melan A.
are amelanotic, showing no clinical evi-
DIFFERENTIAL DIAGNOSIS
dence of pigmentation. Melanomas have a
marked tendency for both regional lymph Early melanomas may resemble pigmented
node metastasis and distant hematogenous nevi or basal cell carcinomas when nonpig-
FIGURE 8-49
Malignant melanoma, flat macular superficial spreading lesions; nodular invasive lesions.
PMPH_Eversole_Chapter-08.indd 353 1/17/2011 3:46:37 PM
354 Chapter 8
mented types occur. Most benign nevi have is present. The patient is febrile and com-
smooth borders with homogeneous color- plains of malaise, and cervical lymphade-
ation while melanomas are multicolored nopathy is a frequent finding. Examination
and manifest irregular margins. There are of the teeth or dental radiographs discloses
also cases reported of squamous cell and a carious tooth and periapical radiolucency.
basal cell carcinomas that synthesize mela- Cellulitis localizes in the soft tissue adja-
nin pigment. cent to the infected tooth. When a ques-
tion exists with regard to the incriminating
TREATMENT tooth, vitalometer testing is in order. Ante-
Wide local excision with 3- to 4-cm margins rior maxillary teeth may drain into the soft
is recommended and a work-up for meta- tissues of the upper face and orbit; poste-
static spread should be performed. Thin rior maxillary and mandibular teeth are
melanomas have a much more favorable associated with cellulitis in the masseter
prognosis than thick melanomas. Mela- region. The soft tissue inflammation may
noma of the scalp and neck carries a 10-year ultimately point and drain, or may prog-
survival (60%). Melanomas of the ear, face, ress through fascial planes and spaces. If
and eyelid have 10-year survival rates of the mediastinum becomes involved, the
70%, 80%, and 90%, respectively. process may be lethal.
MICROSCOPIC FEATURES
Additional Reading Muscle and fascial connective tissue fibers
Hajdarbegovic E, van der Leest RJ, Munte K, Thio HB, are diffusely infiltrated with neutrophils
Neumann HA. Neoplasms of the facial skin. Clin Plast and scattered histiocytes. Tissue edema is
Surg. 2009;36(3):319-334. not prominent.
Plaza JA, Torres-Cabala C, Evans H, Diwan HA, Suster
S, Prieto VG. Cutaneous metastases of malignant
melanoma: a clinicopathologic study of 192 cases DIFFERENTIAL DIAGNOSIS
with emphasis on the morphologic spectrum. Am J Because of its induration, cellulitis may
Dermatopathol. 2010;32:129-136.
Woods JE. Management of malignant melanoma simulate malignant neoplasm or underly-
of the head and neck. Mayo Clin Proc. 1989;64: ing bone disease. Fever, constitutional signs
861-863. of infectious disease, and localization of
infectious sources, either in the dentition or
Diffuse Facial Swellings periodontium, allow for a clinical diagnosis
of cellulitis.
CELLULITIS AND SPACE TREATMENT
INFECTIONS
The patient should be placed on a regimen
Figure 8-50 of analgesics and antipyretics. Penicillin
Age: No predilection
is the drug of choice, provided the patient
Sex: No predilection is not allergic to it. The source of infection
should be eliminated either by pulp expo-
CLINICAL FEATURES sure or extraction. Hot packs can be applied
Cellulitis of the facial tissues usually arises to the swelling in an attempt to localize the
subsequent to spread of odontogenic infec- infection, after which incision and drainage
tion. The swelling is diffuse, firm, or indu- can be performed. Failure of the processes
rated and warm. The overlying skin may to show resolution in 48 hours requires
display erythema. Moderate-to-severe pain routine and anaerobic culture and sensitiv-
PMPH_Eversole_Chapter-08.indd 354 1/17/2011 3:46:45 PM
Soft Tissue Swellings of the Neck and Face 355
FIGURE 8-50
Diffused soft tissue swellings of face subsequent to spread of odontogenic infection represents space
infection (left), Ludwig’s angina (center) and cellulites (right).
ity tests of an aspirate from the inflamed wound, periodontal pocket, surgical flap,
tissues. or root canal. As the air becomes trapped
within tissues, it causes diffuse swelling,
which yields a bubbly sensation with soft
Additional Reading crepitus when palpated. Pain is often a
Kent HA. Cellulitis. Am J Orthod Oral Surg. complaint.
1939;25:172.
Moose SM, Marshall KJ. Ch. 11. In: Kruger GO, ed. MICROSCOPIC FEATURES
Textbook of Oral and Maxillofacial Surgery. 5th ed. St
Louis, MO: C. V. Mosby Co; 1979. Not applicable.
Rush DE, Abdel-Haq N, Zhu JF, Aamar B, Malian M.
Clindamycin versus Unasyn in the treatment of facial
cellulitis of odontogenic origin in children. Clin Pediatr DIFFERENTIAL DIAGNOSIS
(Phila). 2007;46:154-159.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral
Soft tissue emphysema is easily differ-
Pathology. 3rd ed. Philadelphia, PA: W. B. Saunders; entiated from other diffuse facial swell-
1974:464. ings on the basis of the bubbly consis-
Shapiro HH, Sleeper EL, Guralnick WC. Spread of tency detected on palpation. Occasionally,
infection of dental origin. Oral Surg Oral Med Oral
emphysema may be confused with the
Pathol. 1950;3:1407.
soft swellings seen in edema, particularly
angioneurotic edema. A complete history
EMPHYSEMA with consideration of potential etiologic
Figure 8-51 factors allows differentiation on a clinical
basis.
Age: No predilection
Sex: No predilection TREATMENT
CLINICAL FEATURES Soft tissue emphysema may be complicated
Emphysema of the oral and facial soft tis- by venous air embolism, which is often
sues arises as the result of entrapment of fatal, or by soft tissue abscess; in the lat-
air introduced into tissue or fascial spaces. ter, antibiotic therapy is indicated. Emphy-
This phenomenon is usually iatrogenic, fol- sema generally resolves in 4 to 7 days with
lowing some dental or surgical procedure no treatment. If the swelling is significant,
rendered in conjunction with application negative-pressure needle aspiration may
of positive-pressure air introduction into a aid in resolution.
PMPH_Eversole_Chapter-08.indd 355 1/17/2011 3:46:45 PM
356 Chapter 8
FIGURE 8-51
Diffuse soft swelling
of the cheek due to
air entrapment in
the facial tissues.
lip, face, and periorbital area. The tissue
Additional Reading is soft, pliable, and usually pruritic. The
Finlaysen RS, Stevens FD. Subcutaneous facial emphy- reaction is a manifestation of immediate
sema secondary to use of the Cavi-Jet. J Periodontol. immunoglobulin-mediated hypersensi-
1988;59:315. tivity that takes place within 1 or 2 hours
Lantz B. Cervicofacial emphysema. A report of three after antigenic challenge, which is usually
cases with periodontal etiology. Odontol Revy.
1964;15:279. venom from a localized spider bite or bee
Longenecker CG. Venous air embolism during opera- sting to the face. Ingestion of food allergens
tions on the head and neck; report of a case. Plast may also result in angioneurotic edema. A
Reconstr Surg. 1965;36:619. hereditary form of angioneurotic edema
Pousios D, Panagiotopoulos N, Sioutis N, Piyis A,
Gourgiotis S. Iatrogenic pneumomediastinum and
occurs. Patients with this form are geneti-
facial emphysema after surgical tooth extraction. Ann cally deficient in an enzyme that inhibits an
Thorac Surg. 2010;89:640. esterase responsible for a certain reaction in
Rhymes R, Jr. Postextraction subcutaneous emphysema. the complement-fixation process.
Oral Surg Oral Med Oral Pathol. 1964;17:271.
MICROSCOPIC FEATURES
ANGIONEUROTIC EDEMA Not applicable.
Figure 8-52
DIFFERENTIAL DIAGNOSIS
Age: No predilection
Sex: No predilection The diffuse swelling of angioneurotic
edema must be differentiated from emphy-
CLINICAL FEATURES
sema and facial cellulitis associated with
Patients allergic to certain foods or drugs spread of odontogenic infection. Celluli-
exhibit urticaria in most instances; how- tis may show an early edematous phase
ever, for unknown reasons, the allergic prior to cellular infiltration with indura-
manifestations may be localized to the tion. Infection of dental origin should be
facial area. The facial swelling may also be ruled out with appropriate radiologic and
accompanied by urticaria. The facial swell- clinical evaluation. Diligent question-
ing of angioneurotic edema is the result of ing is required to uncover the suspected
histamine-mediated profuse capillary per- allergen, and reexposure to the suspected
meability with a resultant diffuse, often agent may be necessary to confirm the
massive, edematous swelling of the upper etiology.
PMPH_Eversole_Chapter-08.indd 356 1/17/2011 3:46:53 PM
Soft Tissue Swellings of the Neck and Face 357
FIGURE 8-52
Diffuse soft swelling of the
lips in angioneurotic edema.
TREATMENT upper torso adiposity (buffalo hump),
The suspected allergen should be withdrawn abdominal stria, hypertension, and hyper-
and avoided in the future. The disease can glycemia. These signs and symptoms are
be treated by prescribing 50 mg of diphenhy- the result of adrenal hypercorticism. The
dramine or 12.5 mg of promethazine 4 times disease may be associated with an adrenal
daily for 3 days. Progression to anaphylac- cortical adenoma or hyperplasia, pituitary
tic shock may develop but is not a frequent adenoma, or steroid-secreting malignancies
complication. In hereditary angioedema, of other organs. The most common cause
subcutaneous icatibant, a bradykinin recep- is prolonged steroid drug therapy, produc-
tor antagonist, is the treatment of choice ing the so-called moon facies or cushingoid
facies. The soft tissues of the cheeks are
bilaterally puffy and edematous, yielding a
Additional Reading round face.
Albright WB, Taylor CG. Hereditary angioneurotic edema: MICROSCOPIC FEATURES
Report of a case. J Oral Maxillofac Surg. 1979;37:888.
Bork K, Frank J, Grundt B, Schlattmann P, Nussberger J, Not applicable.
Kreuz W. Treatment of acute edema attacks in heredi-
tary angioedema with a bradykinin receptor-2 antagonist DIFFERENTIAL DIAGNOSIS
(Icatibant). J Allergy Clin Immunol. 2007;119:1497-1503.
Donaldson VH, Rosen FS. Hereditary angioneurotic The soft bilateral swellings of slow onset
edema: A clinical survey. Pediatrics. 1966;37:1017. are quite characteristic. A history of steroid
Loria RC, Wedner HJ. Facial swelling secondary to therapy confirms the impression. Cush-
bronchodilator abuse. Catecholamine-induced sialad- ing’s syndrome occurring in patients who
enosis. Ann Allergy. 1989;62:289.
Sturdy KA, Beastall RH, Grisius RJ, Oatis GW, Jr.
are not taking steroid medication requires a
Hereditary angioedema controlled with danazol. Oral complete medical work-up with laboratory
Surg Oral Med Oral Pathol. 1979;48:418. studies to determine the cause of elevated
steroid levels. Obtaining a high blood pres-
sure reading (secondary to mineralocorti-
CUSHING’S SYNDROME coids) and fasting sugar (elevated because
Figure 8-53 of glucocorticoids) represents the initial
phase of the work-up.
Age: Adults
Sex: No predilection
TREATMENT
CLINICAL FEATURES
The cause of the disease must be deter-
Cushing’s syndrome is characterized by mined initially; treatment rests with medi-
bilateral edematous swelling of the face, cal and/or surgical intervention.
PMPH_Eversole_Chapter-08.indd 357 1/17/2011 3:47:04 PM
358 Chapter 8
FIGURE 8-53
Cushing’s syndrome with
diffuse facial edema.
the tongue is enlarged, and the cheek tissues
Additional Reading are thickened. The enlarged osseous tissues
Bertagna X, Guignat L, Groussin L, Bertherat J. do not show an alteration of trabeculation on
Cushing’s disease. Best Pract Res Clin Endocrinol radiographs. Teeth on the affected side may
Metab. 2009;23:607-623. be larger than those on the normal side. In
Hunder GG. Pathogenesis of Cushing’s disease. Mayo nearly one half of patients with this peculiar
Clin Proc. 1966;41:29.
McArthur RG, Cloutier MD, Hayles AB, Sprague RG. syndrome, the remainder of the body shows
Cushing’s disease in children. Findings in 13 cases. a similar unilateral involvement. Syndac-
Mayo Clin Proc. 1972;47:318. tyly and polydactyly are present in some
Rovitt RL, Duane TD. Cushing’s syndrome and pituitary instances, and one fifth of the patients with
tumors. Pathophysiology and ocular manifestations
of ACTH-secreting pituitary adenomas. Am J Med.
hemihypertrophy are retarded. A familial or
1969;46:416. genetic trend is not encountered.
MICROSCOPIC FEATURES
FACIAL HEMIHYPERTROPHY The affected tissues do not show any histo-
Figure 8-54 pathologic changes.
Age: Childhood onset DIFFERENTIAL DIAGNOSIS
Sex: Male predilection
The history of long-standing facial asymme-
CLINICAL FEATURES try helps to limit the differential diagnosis.
Hypertrophy of the facial tissues is a devel- Facial hemihypertrophy must be differenti-
opmental defect of unknown origin, which ated from fibrous dysplasia and other osseous
has been suggested to be related to an anom- enlargements. This can be accomplished by
alous vascular supply. The disease is unilat- obtaining radiographs, because no radiologic
eral, with enlargement of both osseous and changes in osseous trabeculation occur in
soft tissues. The opposite side of the face is facial hemihypertrophy. In neurofibromato-
normal, whereas the affected side shows sis (NF1), facial plexiform neurofibromas may
enlargement of the facial bones and mandi- cause facial asymmetry that can be confused
ble. The eye is laterally displaced. One half of with congenital facial hemihypertrophy.
PMPH_Eversole_Chapter-08.indd 358 1/17/2011 3:47:13 PM
Soft Tissue Swellings of the Neck and Face 359
FIGURE 8-54
Facial hemihypertrophy. A:
Unilateral enlargement of
the maxilla and mandible.
B: Panorex shows osseous
asymmetry.
TREATMENT other entities included in this section. Any
The disease is self-limiting but is certainly central lesion of the jaws that induces cor-
a cosmetic dilemma. Cosmetic surgical tical expansion can distort the facial con-
osseous contouring may be performed, tour, producing enlargement and asymme-
with plastic surgical correction for the soft try. Fibrous dysplasia of bone is one of the
tissue enlargement. more frequent diseases to appear in such a
fashion. The maxilla is more often affected
than the mandible. The swelling is usually
Additional Reading obvious over the malar eminence, zygoma,
or lateroinferior orbital rim. The other fea-
Horswell BB, Holmes AD, Barnett JS, Hookey SR.
tures of fibrous dysplasia are discussed
Primary hemihypertrophy of the face: review and report
of two cases. J Oral Maxillofac Surg. 1987;45:217. in the chapter on radiopaque lesions of
Kirks DR, Shackeford GD. Idiopathic hemihypertro- the jaws. Neoplasms of mesenchymal
phy with associated ipsilateral benign nephromegaly. or odontogenic origin often cause bony
Radiology. 1975;115:145. expansion and facial enlargement. These
Overdiek A, Feifel H, Schaper J, Mayatepek E,
Rosenbaum T. Diagnostic delay of NF1 in hemifacial specific neoplasms are also described in
hypertrophy due to plexiform neurofibromas. Brain detail in subsequent chapters, which cate-
Dev. 2006;28:275-280. gorize lesions on the basis of radiographic
Urban PP, Bruening R. Congenital isolated hemifacial characteristics.
hyperplasia. J Neurol. 2009;256:1566-1569.
Ward J, Lerner HH. A review of the subject of con- MICROSCOPIC FEATURES
genital hemihypertrophy and a complete case report.
J Pediatr. 1947;31:403. The microscopic features vary according to
the specific disease actually represented.
Refer to the chapters on radiolucent and
FIBROUS DYSPLASIA AND radiopaque lesions in which descriptions of
OTHER BONE LESIONS fibro-osseous lesions and central jaw neo-
plasms are presented.
Figure 8-55
DIFFERENTIAL DIAGNOSIS
Age: Children and young adults
Sex: No predilection Osseous enlargements are differentiated
from one another on the basis of clini-
CLINICAL FEATURES
cal, radiologic, and microscopic features.
Diffuse facial swellings not related to soft Osseous enlargements may simulate other
tissue enlargement are included here for diffuse facial swellings included here.
the sake of differential diagnosis because By merely palpating the area, the clini-
their clinical appearance may simulate the cian can determine the osseous nature of
PMPH_Eversole_Chapter-08.indd 359 1/17/2011 3:47:29 PM
360 Chapter 8
FIGURE 8-55
Enlargement of the jaws due
to underlying bone lesions.
Fibrous dysplasia (top), Garré
osteomyelitis (bottom left),
ameloblastoma (bottom right).
the enlargement and essentially rule out Waldron CA, Giansanu JS. Benign fibroosseous lesions
enlargements of soft tissue origin. of the jaws: a clinical-radiologic-histologic review of
sixty-five cases. I. Fibrous dysplasia of the jaws. Oral
Surg Oral Med Oral Pathol. 1973;35:190.
TREATMENT
The treatment varies considerably, based on
the final diagnosis. MASSETERIC HYPERTROPHY
Figure 8-56
Additional Reading Age: Onset in young adulthood
Sex: No predilection
Blomgren I, Lilja J, Lauritzen C, Magnusson B. Multiple
craniofacial surgical interventions during 25 years of CLINICAL FEATURES
follow-up in a case of giant fibrous dysplasia. Scand J Bilateral swellings located over the ascend-
Plast Reconstr Hand Surg. 1986;20:327.
Chen YR, Chang CN, Tan YC. Craniofacial fibrous dys-
ing ramus of the mandible character-
plasia: an update. Chang Gung Med J. 2006;29:543- ize benign muscular hypertrophy of the
549. masseters. The enlargement may be con-
Gardner AF, Halpert L. Fibrous dysplasia of the skull fused with parotid disease; however, if
with special reference to the oral regions. Dent Prac
Dent Rec. 1963;13:337.
the patient is asked to clench his teeth, the
Lewin ML. Nonmalignant maxillofacial tumors in chil- enlargements increase in size and become
dren. Plast Reconstr Surg. 1966;38:186. firm as the result of muscular contraction.
PMPH_Eversole_Chapter-08.indd 360 1/17/2011 3:47:36 PM
Soft Tissue Swellings of the Neck and Face 361
Pain is not a feature. The cause for this
condition is not always apparent. Some
instances appear to represent congenital
disease, whereas others may be related to
physiologic hypertrophy of muscle fibers
from overuse of the jaws, as in bruxism.
MICROSCOPIC FEATURES
Normal skeletal muscle fibers are present;
some may show enlarged diameters.
DIFFERENTIAL DIAGNOSIS
The bilateral distribution differentiates
masseteric hypertrophy from other facial FIGURE 8-56
swellings such as cellulitis, emphysema, or Masseteric hypertrophy.
facial hemihypertrophy. Because the loca-
tion is such that parotid disease may be
confused with this entity, such disorders as
Sjögren’s syndrome, Mikulicz’s disease, and
Additional Reading
Heerfordt’s syndrome should be considered Baş B, Ozan B, Muğlali M, Celebi N. Treatment of
masseteric hypertrophy with botulinum toxin: a
in the differential diagnosis. These can gen- report of two cases. Med Oral Patol Oral Cir Bucal.
erally be eliminated on the basis of other 2010;15:e649-e652.
clinical findings (a lack of xerostomia and Bloem JJ, Van Hoof RF. Hypertrophy of the masseter
increase in induration on clenching), which muscles. Plast Reconstr Surg. 1971;47:138.
Buchner A, David R, Temkin D. Unilateral enlargement
are features of masseteric hypertrophy. of the masseter muscle. Int J Oral Maxillofac Surg.
1979;8:140.
TREATMENT Lash H. Benign masseteric hypertrophy. Surg Clin North
Am. 1963;43:1357.
Botulinum toxin type A injection directly Wade WM, Roy EW. Idiopathic masseter muscle
into affected muscles reduces their size in hypertrophy: report of cases. J Oral Maxillofac Surg.
3 months. 1971;29:196.
PMPH_Eversole_Chapter-08.indd 361 1/17/2011 3:47:51 PM
a b c d
Unilocular, corticated Unilocular, noncorticated Unilocular, expansile Unilocular, cortical erosion
e f g
Multilocular Scalloped Motheaten
h i j
Periapical Interradicular Edentulous zone
k l m
Alveolar bone loss Pericoronal Multifocal
Radiolucent Lesions
PMPH_Eversole_Chapter-09.indd 362 1/20/2011 2:54:56 PM
Radiolucent Lesions
of the Jaws 9
SQUAMOUS ODONTOGENIC
Periapical TUMOR 389
Radiolucencies 366 SURGICAL CILIATED CYST 391
APICAL PERIODONTITIS (ABSCESS, OSTEOPOROTIC BONE MARROW
GRANULOMA, AND CYST) 366 DEFECT 392
PERIAPICAL CEMENTAL CENTRAL OSSIFYING
DYSPLASIA 367 (CEMENTIFYING) FIBROMA 393
FOCAL CEMENTO-OSSEOUS ODONTOGENIC ADENOMATOID
DYSPLASIA 369 TUMOR 394
ODONTOGENIC FIBROMA 396
FOCAL SCLEROSING
OSTEOMYELITIS 371 CENTRAL GIANT CELL
GRANULOMA ‡ 397
BENIGN CEMENTOBLASTOMA 371
INCISIVE CANAL CYST 372
MEDIAN MANDIBULAR CYST 375
Periodontal (Alveolar)
Bone Loss 398
TRAUMATIC (HEMORRHAGIC)
CYST 375 CHRONIC PERIODONTITIS 398
STATIC BONE CYST DIABETIC PERIODONTITIS 400
(SUBMANDIBULAR GLAND JUVENILE PERIODONTITIS AND
DEPRESSION) 377 PAPILLON-LEFEVRE
SUBLINGUAL GLAND SYNDROME 401
DEPRESSION 377 VANISHING BONE DISEASE
PARADENTAL (BUCCAL (MASSIVE OSTEOLYSIS) 402
INFECTED)CYST 379 LANGERHANS CELL
HISTIOCYTOSIS 403
CENTRAL GIANT CELL
GRANULOMA 380 CYCLIC NEUTROPENIA 405
MALIGNANCIES 380 LEUKEMIA 406
Interradicular Widened Periodontal
Radiolucencies 383 Ligament Space 407
PERIODONTIC/ENDODONTIC
LATERAL PERIODONTAL CYST 383
INFLAMMATION 407
LATERALLY DISPLACED APICAL
SCLERODERMA 409
PERIODONTAL CYST OR
OSTEOGENIC SARCOMA 410
GRANULOMA 384
RESIDUAL CYST 385
ODONTOGENIC KERATOCYST 386
Pericoronal
Radiolucencies 411
PRIMORDIAL CYST 386
CALCIFYING CYSTIC DENTIGEROUS CYST 411
ODONTOGENIC TUMOR 388 ODONTOGENIC KERATOCYST 413
PMPH_Eversole_Chapter-09.indd 363 1/20/2011 2:55:00 PM
GLANDULAR ODONTOGENIC OSTEORADIONECROSIS 445
CYST† 414 BISPHOSPHONATE-RELATED
UNICYSTIC AMELOBLASTOMA 414 OSTEONECROSIS OF THE JAWS
CALCIFYING EPITHELIAL (BRONJ) 446
ODONTOGENIC TUMOR 417 PRIMARY INTRAOSSEOUS
ODONTOGENIC ADENOMATOID CARCINOMA 448
TUMOR 417
CYSTOGENIC CARCINOMA 449
AMELOBLASTIC FIBROMA 419
METASTATIC CARCINOMA 450
ODONTOGENIC FIBROMA-
LIKE HAMARTOMA/ENAMEL MALIGNANT ODONTOGENIC
HYPOPLASIA 420 TUMORS 452
CENTRAL MUCOEPIDERMOID OSTEOSARCOMA AND
CARCINOMA 421 CHONDROSARCOMA 453
EWING’S SARCOMA 455
Multilocular PRIMARY LYMPHOMA OF BONE 456
Radiolucencies 423 BURKITT’S LYMPHOMA 457
ODONTOGENIC KERATOCYST 423 FIBROGENIC AND NEUROGENIC
BOTRYOID ODONTOGENIC SARCOMA 458
CYST 425 MELANOTIC NEUROECTODERMAL
GLANDULAR ODONTOGENIC TUMOR OF INFANCY 459
CYST 425
CHERUBISM (FAMILIAL FIBROUS Multifocal Radiolucencies 461
DYSPLASIA) 427
CENTRAL GIANT CELL BASAL CELL NEVUS SYNDROME 461
GRANULOMA 429 LANGERHANS CELL
ANEURYSMAL BONE CYST 429 HISTIOCYTOSIS 462
HYPERPARATHYROIDISM 431 MULTIPLE MYELOMA 463
AMELOBLASTOMA 432 CHERUBISM†
MYXOMA 433 PERIAPICAL CEMENTAL DYSPLASIA ‡
CENTRAL NEUROGENIC SQUAMOUS ODONTOGENIC
NEOPLASMS 434
TUMOR§
CENTRAL ARTERIOVENOUS
MALFORMATION 436
CENTRAL (LOW FLOW)
Generalized Osteoporotic
HEMANGIOMA OF BONE 437 Lesions 465
CENTRAL LEIOMYOMA 438 OSTEOMALACIA 465
PSEUDOTUMOR OF
SENILE OSTEOPOROSIS 466
HEMOPHILIA 439
STEROID OSTEOPOROSIS 467
MYOFIBROMATOSIS
(DESMOPLASTIC FIBROMA OF SICKLE CELL ANEMIA 468
BONE) 440 THALASSEMIA MAJOR 469
FIBROUS DYSPLASIA 442
INTRAOSSEOUS MUCOEPIDERMOID
CARCINOMA* 443
THALASSEMIA MAJOR** 443
*See Pericoronal Radiolucencies
**See Generalized Osteoporotic Lesions
Moth-Eaten †See Multilocular Radiolucencies
Radiolucencies 443
‡See Periapical Radiolucencies
OSTEOMYELITIS 443 §See Interradicular Radiolucencies
PMPH_Eversole_Chapter-09.indd 364 1/20/2011 2:55:00 PM
The diseases that affect the osseous marrow Because arteriovenous malformations
and cortex of the jaw bones are included are radiolucent, surgical biopsy should not
both in this chapter and in the succeeding be performed on radiolucent lesions of the
chapter dealing with radiopaque lesions. jaws before needle aspiration of the defect
Central lesions of the jaws may manifest is attempted.
signs and symptoms such as pain, discom- The most common periapical radiolu-
fort, paresthesia, and swelling, or they may cency is apical periodontitis secondary to
be discovered serendipitously when full- pulp necrosis. Periapical cemental dyspla-
mouth radiographs or panographic surveys sia and traumatic cyst are less common yet
are procured. are by no means rare. The lateral periodon-
It should be stressed from the onset that tal cyst and odontogenic keratocyst are the
a definitive diagnosis can rarely be secured most common interradicular radiolucent
on the basis of radiologic features alone; a lesions.
thorough case history and a bone biopsy are Alveolar bone loss is the hallmark of
required in most instances. The radiolucent periodontal disease and is seen in nearly
lesions are grouped according to location one half of the adult population. Neverthe-
and configuration. It is axiomatic that this less, the clinician should be aware of the
categorization is not all-inclusive; the enti- fact that many life-threatening diseases
ties listed in a given category are not always (diabetes, histiocytosis X, leukemia, and
represented by the radiographic headings malignant neoplasms) can manifest identi-
under which they are listed. Rather, the dis- cal radiographic features.
eases have been placed under a given pat- The most common multilocular radio-
tern heading because it is that particular lucencies are the odontogenic keratocyst,
configuration that the disease most often central giant cell granuloma, and amelo-
assumes. blastoma. Central arteriovenous malforma-
Some generalizations can be put for- tions are potentially lethal if traumatized or
ward with regard to radiolucent lesions of tampered with surgically. Osteomyelitis is
the jaws. A unilocular radiolucency with the most common disease showing a moth-
well-demarcated boundaries or cortication eaten pattern. A variety of sarcomas and
is usually indicative of a benign, slow-grow- metastatic carcinomas show similar radio-
ing process. Radiolucencies with ill-defined logic features; however, these malignancies,
or irregular margins may be either benign as opposed to osteomyelitis, are represented
or malignant. by expansion of the cortical plates.
Radiolucencies surrounding the crown The most common multifocal radio-
of a tooth are, as a rule, cystic or neoplastic lucency is periapical cemental dysplasia;
lesions of odontogenic origin. Multilocular this is included among the periapical radio-
radiolucencies with well-defined margins lucencies. The acute disseminated form of
frequently show cortical expansion. Lesions histiocytosis X and multiple myeloma, both
with this configuration are generally benign manifesting multiple radiolucent lesions,
yet aggressive reactive or neoplastic disor- are potentially lethal diseases. Generalized
ders. When evaluating unilocular radiolu- rarefaction or osteoporotic lesions involv-
cencies, one should remember that those ing the entire skeleton usually exhibit
diseases categorized as multilocular radiolu- jawbone changes. Senile osteoporosis is
cencies must initially appear as unilocular the most common condition, whereas the
lesions, with or without expansion depend- genetic hemolytic anemias are potentially,
ing on the size of the growth. yet rarely, lethal.
PMPH_Eversole_Chapter-09.indd 365 1/20/2011 2:55:00 PM
366 Chapter 9
scribed and are located directly below the
Periapical Radiolucencies apex of the involved teeth. If the source
of infection emanates from an accessory
APICAL PERIODONTITIS root canal, the radiolucency may be later-
(ABSCESS, GRANULOMA, ally displaced. Any tooth with a carious
AND CYST) pulp exposure can develop periapical dis-
Figure 9-1 ease; however, incisors and first molars are
most frequently involved. Radiographi-
Age: Adults
Sex: No predilection cally, abscesses, granulomas, or cysts have
the same features and cannot be differen-
CLINICAL AND RADIOGRAPHIC tiated without microscopic examination.
FEATURES
Acute periapical abscess is accompanied by
Inflammatory lesions of bone resulting severe pain that often interferes with sleep.
from apical progression of dental pulp Pain on percussion is a feature. Granulomas
inflammation evolve subsequent to dental and cysts may be asymptomatic or associ-
caries or trauma to the teeth. Radiographi- ated with a dull ache or, occasionally, severe
cally, the lesions are usually well circum- pain. If the periapical lesion resolves with
FIGURE 9-1
Apical periodontal cysts and granulomas associated with nonvital teeth. Cone beam computed tomo-
graphic sections on the right.
PMPH_Eversole_Chapter-09.indd 366 1/20/2011 2:55:00 PM
Radiolucent Lesions of the Jaws 367
treatment yet is not replaced by bone, a presence of deep carious lesions or a his-
residual periapical fibrous scar may persist. tory of a traumatic episode implicates an
Even after extraction of the necrotic tooth, infectious or inflammatory lesion of pul-
a through-and-through fibrous defect may pal origin. The diagnosis is confirmed by
persist and be radiographically demonstra- a negative response to vitalometer testing.
ble as an ill-defined radiolucency. Infection Many other primary cysts and tumors of
may spread, with intraoral fistulation and the jaws often lie in juxtaposition to tooth
parulis formation. Infected maxillary teeth roots; however, the teeth are vital.
may drain into the maxillary sinus, into tis-
sues of the face, producing a cellulitis, or, TREATMENT
rarely, inflammation may spread via the Teeth with periapical inflammation are
facial veins and progress to cavernous sinus nonvital and require endodontic therapy or
thrombosis. Mandibular teeth may drain extraction. Should the periapical radiolucency
buccally, causing space infections or Lud- fail to resolve within 6 to 12 months, apical
wig’s angina, which, if left untreated, may curettage with apicoectomy is indicated.
progress into the parapharyngeal spaces
and ultimately into the mediastinum. This
in turn may be fatal, because constriction is
caused by edema of the airway. Treponema
Additional Reading
denticola and Enterococcus faecalis are culti- Bhaskar SN. Periapical lesions—types, incidence, and
vated from periapical lesions with previ- clinical features. Oral Surg Oral Med Oral Pathol.
1966;21:657.
ous pain, while Porphyromonas gingivalis is Cogulu D, Uzel A, Oncag O, Eronat C. PCR-based iden-
associated with tenderness to percussion in tification of selected pathogens associated with endo-
both deciduous and permanent teeth. dontic infections in deciduous and permanent teeth.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
2008;106:443-449.
MICROSCOPIC FEATURES Lineberg WB, Waldron CA, Delanne GF. A clinical,
Periapical abscess shows loose areolar roentgenographic and histopathologic evaluation of
periapical lesions. Oral Surg Oral Med Oral Pathol.
granulation tissue and diffuse sheets of 1972;17:467.
neutrophils with scattered macrophages. Orstavik D, Farrants G, Wahl T, Kerekes K. Image anal-
Granulomas are composed of fibrous and ysis of endodontic radiographs: digital subtraction and
granulation tissue with a diffuse or patchy quantitative densitometry. Endodont Dent Traumatol.
1990;6:6.
subacute or chronic inflammatory cell infil-
Rohlin M, Kullendorff B, Ahlqwist M, Henrikson CO,
trate. The apical periodontal cyst is lined by Hollender L, Stenström B. Comparison between
nonkeratinizing squamous epithelium, often panoramic and periapical radiography in the diagno-
fragmented and with elongated anastomos- sis of periapical bone lesions. Dentomaxillofac Radiol.
ing rete ridges. Hyaline bodies are often pres- 1989;18:151.
ent within the spinous layer. Transmigration
of neutrophils into the spinous cell layer is
common. The fibrous and granulation tissue PERIAPICAL CEMENTAL
wall is infiltrated with inflammatory cells DYSPLASIA
and often contains cholesterol clefts. Figure 9-2
DIFFERENTIAL DIAGNOSIS Age: Middle-aged adults
Sex: Female predilection
Apical periodontitis may be radiographically
identical to immature periapical cemental CLINICAL AND RADIOGRAPHIC FEATURES
dysplasia, focal condensing osteitis, benign More common among blacks than whites,
cementoblastoma, and traumatic cyst. The periapical cemental dysplasia or cemen-
PMPH_Eversole_Chapter-09.indd 367 1/20/2011 2:55:11 PM
368 Chapter 9
FIGURE 9-2
Multiple apical radiolucencies underlying vital teeth represent periapical cemental dysplasia. Some show
early calcifications in the center of a radiolucent halo.
toma appears radiographically as a non- not invariably, circumscribed and located
expansile radiolucency in its early or subjacent to an intact apical periodontal
immature stage. The lesion may be single ligament space. The overlying teeth are
or multiple and is considerably more com- vital, clinical evidence of expansion is lack-
mon in the anterior mandible. Incisors and ing, and pain is not a feature. The etiology
premolars are more often associated with is unknown.
the periapical radiolucencies, and peria-
pical cemental dysplasia does not involve MICROSCOPIC FEATURES
molar teeth unless multiple lesions are The early stage of periapical cemental dys-
present. Periapical cemental dysplasia and plasia is characterized by the presence of
focal cemento-osseous dysplasia probably hypercellular fibrous tissue with irregular,
represent the same pathologic process, the small osseous trabeculae or curvilinear
latter found in the posterior mandibular cemental trabeculae. Droplet calcifications
quadrants. The radiolucency is usually, but are frequently observed.
PMPH_Eversole_Chapter-09.indd 368 1/20/2011 2:55:11 PM
Radiolucent Lesions of the Jaws 369
DIFFERENTIAL DIAGNOSIS Krausen AS, Pullon PA, Gulmen S, Schenck NL,
Ogura JH. Cementomas—aggressive or innocu-
Periapical cemental dysplasia can be differen- ous neoplasms? Arch Otolaryngol Head Neck Surg.
tiated from apical periodontitis on the basis 1977;103:349.
of vitalometer testing, as the pulp is vital in Leal RM, Santiago Mde O, Silveira FF, Nunes E,
Capistrano HM. Periapical cemental dysplasia in twin
the former disease. Focal condensing osteitis
sisters: a case report. Quintessence Int. 2009;40:e89-
and cementoblastoma are usually associated e92
with molars rather than with anterior teeth. Tanaka H, Yoshimoto A, Toyama Y, Iwase T, Hayasaka
N, Moro I. Periapical cemental dysplasia with multiple
TREATMENT lesions. Int J Oral Maxillofac Surg. 1987;16:757.
Zegarelli EV, Kutscher AH, Napoli N, Iurono F,
Nonexpansile periapical radiolucencies asso- Hoffman P. The cementoma, a study of 230 patients
ciated with vital anterior teeth are clinically with 435 cementomas. Oral Surg Oral Med Oral
Pathol. 1964;17:219.
considered to represent periapical cemen-
tal dysplasia. No treatment is required. The
patient should be recalled for periodic radio- FOCAL CEMENTO-OSSEOUS
graphic evaluation, to assure that the lesion fol-
lows the usual progression into mature stages
DYSPLASIA
with opacification. If the lesion progressively Figure 9-3
enlarges or causes expansion, it probably repre-
Age: Adults
sents another disease and biopsy is indicated. Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Additional Reading FEATURES
Chaudhry AP, Spink JH, Gorlin RJ. Periapical fibrous
Focal cemento-osseous dysplasia is a fibro-
dysplasia (cementoma). J Oral Maxillofac Surg. osseous hamartoma that begins central in
1958;16:483. bone as a radiolucency. Over time the lesion
FIGURE 9-3
Focal cemento-osseous dysplasia begin-
ning as apical radiolucent lesions in early
stages.
PMPH_Eversole_Chapter-09.indd 369 1/20/2011 2:55:22 PM
370 Chapter 9
undergoes ossification, becoming a radiolu- DIFFERENTIAL DIAGNOSIS
cency with a central opacity. These lesions Ossifying fibroma should be considered and
are commonly seen in the molar areas. They can be ruled out when osseous expansion is
grow to a given size without expansion of abscent. Focal sclerosing osteomyelitis can
bone and become quiescent. The pathogen- be eliminated when an odontogenic source
esis is therefore very similar to their ante- of infection (i.e., caries, nonvital teeth, large
rior jaw counterpart, periapical cemental restorations) is identifiable.
dysplasia. Importantly, in both lesions, the
overlying teeth are vital. TREATMENT
No treatment after biopsy is required.
MICROSCOPIC FEATURES
The lesion is typically curetted away from
a bony crypt and appears as multiple small
Additional Reading
lobules. A fibro-osseous pattern is observed Macdonald-Jankowski DS. Focal cemento-osseous dys-
with a hypercellular monomorphic fibro- plasia: a systematic review. Dentomaxillofac Radiol.
2008;37:350-360.
blastic proliferation throughout which lie Slootweg PJ. Maxillofacial fibro-osseous lesions: classifi-
irregular trabeculae. Cemental-like oval cation and differential diagnosis. Semin Diagn Pathol.
calcifications are also present. 1996;13:104-112.
FIGURE 9-4
Focal sclerosing osteomyelitis showing early lucent stage compared with later stages with opacification.
Teeth manifest pulpitis from caries and are usually vital.
FIGURE 9-5
Benign cementoblastoma in the early immature radiolucent stage and late calcified stage.
PMPH_Eversole_Chapter-09.indd 370 1/20/2011 2:55:29 PM
Radiolucent Lesions of the Jaws 371
Su L, Weathers DR, Waldron CA. Distinguishing fea- The two can be differentiated on clinical
tures of focal cemento-osseous dysplasia and cemento- grounds. Focal osteitis arises in associa-
ossifying fibromas. II. A clinical and radiologic spec-
trum of 316 cases. Oral Surg Oral Med Oral Pathol tion with posterior teeth with a large cari-
Oral Radiol Endod. 1997;84:540-549. ous lesion, whereas periapical cemental
Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia involves noncarious vital ante-
dysplasia: a clinicopathologic study of 221 cases. Oral rior teeth. Benign cementoblastoma may
Surg Oral Med Oral Pathol. 1994;78(5):611-620.
show similar features in the radiolucent
stage. This lesion is not associated with
FOCAL SCLEROSING caries and pulpitis. In addition, cortical
expansion is a feature of cementoblastoma
OSTEOMYELITIS but is rarely seen in focal osteitis. The
Figure 9-4 microscopic appearance may be indistin-
guishable from that of other fibro-osseous
Age: Teenagers and young adults
Sex: No predilection
lesions of the jaws, so that the diagnosis
depends on clinical features.
CLINICAL AND RADIOGRAPHIC
FEATURES TREATMENT
Whereas focal sclerosing osteomyelitis is Because the pulp is inflamed and may
most often observed as a radiopaque lesion, progress into an acute phase, with ultimate
it may evolve from a radiolucent stage, which necrosis, endodontic therapy is indicated.
becomes progressively opacified. This rare
form is characterized by a well-circum-
scribed periapical radiolucency in associa- Additional Reading
tion with a carious mandibular molar. The
Boyne PJ. Incidence of osteosclerotic areas in the mandi-
caries are usually deep, and the crown may ble and maxilla. J Oral Maxillofac Surg. 1960;18:486.
appear gutted. The pulp from the overlying Eversole LR, Stone CE, Strub D. Focal sclerosing
tooth is vital with a chronic inflammatory osteomyelitis and focal periapical osteopetrosis:
cell infiltrate (i.e., chronic pulpitis). The area Radiographic patterns. Oral Surg Oral Med Oral
Pathol. 1984;58:456.
may be asymptomatic or a dull ache may Farman AG, de V. Joubert JJ, Nortjé CJ. Focal osteoscle-
be present. Response to vitalometer test- rosis and apical periodontal pathoses in “European”
ing is often altered; however, the overlying and Cape coloured dental outpatients. Int J Oral
tooth rarely tests nonvital because the pulp Maxillofac Surg. 1978;7:549.
Kessler HP. Oral and maxillofacial pathology case of the
is inflamed rather than necrotic.
month. Condensing osteitis. Tex Dent J. 2003;120:178,
188-189.
MICROSCOPIC FEATURES Marmary Y, Kutiner G. A radiographic survey of periapi-
cal jawbone lesions. Oral Surg Oral Med Oral Pathol.
Hypercellular or moderately cellular 1986;61:405.
fibrous connective tissue is stippled with
small, irregular osseous trabeculae that are
usually rimmed by osteoblasts. Curvilinear BENIGN CEMENTOBLASTOMA
cemental trabeculae and ovoid calcifications Figure 9-5
may also be seen. The pulp from the overly-
ing tooth is vital, with a chronic inflamma- Age: Teenagers and young adults
tory cell infiltrate. Sex: No predilection
CLINICAL AND RADIOGRAPHIC
DIFFERENTIAL DIAGNOSIS FEATURES
Focal osteitis is most frequently con- A true neoplasm of cementoblastic origin,
fused with periapical cemental dysplasia. the benign cementoblastoma, is seen to arise
PMPH_Eversole_Chapter-09.indd 371 1/20/2011 2:55:38 PM
372 Chapter 9
in association with tooth roots. Molar teeth, ing fused tumor mass should be excised in
particularly the mandibular first molar, are toto. If left untreated, the lesion may pro-
the predominant sites for this lesion, usu- gressively enlarge and expand the encasing
ally encountered in a radiopaque stage. bone.
Early lesions may be radiolucent. They are
well circumscribed and envelop one or
both roots, usually extending midway up Additional Reading
the root surface. They are well demarcated
Brannon RB, Fowler CB, Carpenter WM, Corio RL.
and may be totally lucent or contain calcific Cementoblastoma: an innocuous neoplasm? A clinico-
flecks. Expansion of the buccal and/or lin- pathologic study of 44 cases and review of the literature
gual cortical plates occurs and, if of signifi- with special emphasis on recurrence. Oral Surg Oral
cant magnitude, may be demonstrated on Med Oral Pathol Oral Radiol Endod. 2002;93:311-
320.
occlusal radiographs. The tooth tests vital, Cherrick HM, King OH, Jr, Lucatorto FM, Suggs DM.
pain is not a feature, and a dull, ankylo- Benign cementoblastoma: a clinicopathologic evalua-
sed sound is produced when the tooth is tion. Oral Surg Oral Med Oral Pathol. 1974;37:54.
percussed. Corio RL, Crawford BE, Schaberg SJ, et al. Benign
cementoblastoma. Oral Surg Oral Med Oral Pathol.
1976;41:524.
MICROSCOPIC FEATURES
Eversole LR, Sabes WR, Dauchess VG. Benign
Linear-radiating trabeculae of osseous tis- cementoblastoma. Oral Surg Oral Med Oral Pathol.
sue are dispersed throughout a fibrous mar- 1973;36:824.
Farman AG, Köhler WW, Nortjé CJ, Van Wyk CW.
row and are intimately associated with, and Cementoblastoma: report of case. J Oral Maxillofac
fused to, the root cementum. These trabe- Surg. 1979;37:198.
culae generally show polarization patterns
more consistent with osseous tissue than
with cementum; rimming by osteoblasts is INCISIVE CANAL CYST
a prominent feature. Figure 9-6
DIFFERENTIAL DIAGNOSIS Age: Adults
Cementoblastoma in its immature radio- Sex: No predilection
lucent stage must be differentiated from CLINICAL AND RADIOGRAPHIC
focal sclerosing osteomyelitis, apical perio- FEATURES
dontitis, and periapical cemental dyspla- The incisive canal cyst is a developmental
sia. These latter entities do not produce an nonodontogenic cyst derived from embry-
ankylosed sound when percussed and fail onic epithelial remnants of the nasopalatine
to expand the cortical plates. Periapical duct or incisive canal. It is a well-delineated
cemental dysplasia involves anterior teeth, oval or heart-shaped radiolucency located
whereas cementoblastoma arises from the between, and apical to, the two maxillary
root area of posterior teeth. central incisors directly in the midline. It
rarely causes facial expansion, yet pala-
TREATMENT
tal swelling is common. Occasionally, the
A vital posterior tooth with an expansive incisors evince root resorption. The cyst
periapical radiolucency probably represents is asymptomatic and the teeth test vital. It
cementoblastoma in its early stage. Surgical is sometimes difficult to ascertain radio-
exploration with biopsy is advisable. If a graphically whether the radiolucency is
gritty or cartilage-like tissue is encountered truly pathologic or merely represents a
during surgery and appears to be fused to large incisive foramen. Cystic unilocular
the root surface, the tooth and accompany- lesions of the palatal midline (median pala-
PMPH_Eversole_Chapter-09.indd 372 1/20/2011 2:55:38 PM
Radiolucent Lesions of the Jaws 373
FIGURE 9-6
Incisive canal cysts are prolate or heart-shaped midline radiolucencies that may cause root divergence.
tal cyst) may represent true fissural cysts mordial cysts, and odontogenic keratocysts
from epithelial entrapment of the fusing arise in this location.
secondary palatal processes. Alternatively,
these lesions may represent posterior exten- TREATMENT
sion of an incisive canal cyst. When a radiologic diagnosis of incisive
canal cyst is made, treatment may consist
MICROSCOPIC FEATURES of surgical enucleation or periodic radio-
The cyst may be lined by stratified graphic follow-up. Progressive enlargement
squamous epithelium, respiratory epithe- warrants surgical intervention.
lium, or both. When respiratory epithe-
lium is present, mucous goblet cells may be
seen.
Additional Reading
The fibrous wall characteristically is Abrams AM, Howell FV, Bullock WK. Nasopalatine
traversed by large neurovascular bundles. cysts. Oral Surg Oral Med Oral Pathol. 1963;16:306.
Campbell JJ, Baden E, Williams AC. Nasopalatine cyst
of unusual size: report of case. J Oral Maxillofac Surg.
DIFFERENTIAL DIAGNOSIS 1973;31:776.
Nelson BL, Linfesty RL. Nasopalatine duct cyst. Head
A midline radiolucency of the maxilla Neck Pathol. 2010;4:121-122.
almost invariably represents incisive canal Taintor JF, Fahid A. Case report: Median palatine cyst.
cyst. Rarely, lateral periodontal cysts, pri- Dent Survey. 1977;53:33.
PMPH_Eversole_Chapter-09.indd 373 1/20/2011 2:55:38 PM
374 Chapter 9
FIGURE 9-7
Median mandibular cyst underlying vital teeth.
FIGURE 9-8
Traumatic or hemorrhagic
bone cyst appears as a
nonexpansile periapical
radiolucency. The overly-
ing molars test vital. The
lesion tends to scallop
into the furcation region
and between contiguous
teeth.
PMPH_Eversole_Chapter-09.indd 374 1/20/2011 2:55:54 PM
Radiolucent Lesions of the Jaws 375
MEDIAN MANDIBULAR CYST
Figure 9-7
Additional Reading
Blair AE, Wadsworth W. Median mandibular develop-
Age: Adults mental cyst. J Oral Maxillofac Surg. 1968;26:735.
Sex: No known predilection Buchner A, Ramon Y. Median mandibular cyst—a rare
lesion of debatable origin. Oral Surg Oral Med Oral
CLINICAL AND RADIOGRAPHIC Pathol. 1974;37:431.
FEATURES Gardner DG. An evaluation of reported cases of median
mandibular cysts. Oral Surg Oral Med Oral Pathol.
The median mandibular cyst is theoretically 1988;65:809.
a fissural cyst that evolves from entrapped Soskolne WA, Sheteyer A. Median mandibular cyst. Oral
epithelial remnants enclaved in the man- Surg Oral Med Oral Pathol. 1977;44:84.
dibular symphysis region subsequent to Tilson HB, Bauerle JE. Median mandibular cyst: report
of case. J Oral Maxillofac Surg. 1970;28:519.
fusion of the mandibular processes. Some
authors dispute this theory and ascribe the
cystic lesion to various other pathogenetic TRAUMATIC (HEMORRHAGIC)
derivations from odontogenic sources (i.e.,
primordial cyst from a supernumerary
CYST
bud, lateral periodontal cyst, odontogenic Figure 9-8
keratocyst). It appears as a unilocular, often
Age: Young adults
expansile, radiolucency underlying vital Sex: Slight male predilection
mandibular incisors.
CLINICAL AND RADIOGRAPHIC
MICROSCOPIC FEATURES FEATURES
Some cases represent odontogenic kerato- The traumatic cyst does not represent a
cyst. Others are lined by nonkeratinizing true epithelial cyst; rather, it is an empty
stratified squamous epithelium, whereas or fluid-filled cavity of bone lined with a
others have been reported with a respira- fibrous or granulation tissue membrane.
tory lining. This feature does not neces- The term traumatic was used to implicate
sarily support a fissural origin, since other trauma as a causative factor; however, less
odontogenic cysts may exhibit respiratory than half of the instances are associated
metaplasia. Furthermore, this region does with any significant trauma to the jaw.
not typically harbor respiratory epithe- The etiology remains unknown. Clinically,
lium during the embryonic morphogenetic pain and expansion are unusual. The lesion
period. is located most often in the body or anterior
portion of the mandible, and radiographi-
DIFFERENTIAL DIAGNOSIS cally, it is radiolucent. A classic feature is
its tendency to scallop between the tooth
Traumatic cyst may occur in this location, roots. Portions of the cystic lesion are well
yet rarely expands bone. Likewise, the demarcated from the neighboring bone,
sublingual salivary gland depression, also whereas in other areas the margins are ill
nonexpansile, is characterized by a radiolu- defined. The teeth that overlie the lesion
cency in the anterior mandible. Apical cysts test vital.
and granulomas can be ruled out when pul-
pal necrosis is documented. MICROSCOPIC FEATURES
When biopsy is attempted, an empty space
TREATMENT in the medullary bone is encountered. A thin
Surgical enucleation or curettage is the membrane may line the cavity and is char-
treatment of choice. acterized microscopically by the presence
PMPH_Eversole_Chapter-09.indd 375 1/20/2011 2:56:02 PM
376 Chapter 9
of fibrous granulation tissue that usually should be made to induce hemorrhage into
shows mild-to-moderate inflammation. the bone cavity. The clot organizes, ossi-
fies, and remodels within 6 to 12 months.
DIFFERENTIAL DIAGNOSIS Although evidence has been forwarded
Traumatic cysts must be differentiated from that traumatic cysts may resolve spontane-
apical periodontitis on the basis of vital- ously, surgical exploration is recommended
ity testing. The teeth overlying traumatic for diagnostic confirmation.
cysts are vital. Because these lesions may be
extensive and show peripheral scalloping,
they could be mistaken for one of the lesions Additional Reading
included as multilocular radiolucencies, for
Cortell-Ballester I, Figueiredo R, Berini-Aytés L, Gay-
example, keratocyst, central giant cell gran- Escoda C. Traumatic bone cyst: a retrospective
uloma, and certain odontogenic tumors. study of 21 cases. Med Oral Patol Oral Cir Bucal.
These lesions are usually expansile, whereas 2009;14:E239-E243.
traumatic cysts generally do not expand the Davis WM, Buchs AV, Davis WM. Extravasation cyst
diagnostic curettement: a treatment. Report of 15 cas-
cortex. Aspiration of a traumatic cyst may be
es and suggested treatment. Oral Surg Oral Med Oral
negative or yield a blood-tinged fluid. Pathol. 1979;47:2.
Hansen LS, Sapone J, Sproat RC. Traumatic bone
TREATMENT cysts of the jaws. Oral Surg Oral Med Oral Pathol.
1974;37:899.
After aspiration, the area should be entered Howe GL. “Haemorrhagic cysts” of the mandible. Br J
surgically. A portion of the lining membrane Oral Maxillofac Surg. 1965;3:55.
FIGURE 9-9
Unilocular, well-circum-
scribed radiolucency lying
below the inferior alveolar
canal represents a sub-
mandibular gland depres-
sion on the lingual aspect
of the mandible.
PMPH_Eversole_Chapter-09.indd 376 1/20/2011 2:56:03 PM
Radiolucent Lesions of the Jaws 377
Sapp JP, Stark ML. Self-healing traumatic bone cysts.
Oral Surg Oral Med Oral Pathol. 1990;69:597. Additional Reading
Anneroth G, Berglund G, Kahnberg KE. Intraosseous
STATIC BONE CYST salivary gland tissue of the mandible mimicking a peri-
apical lesion. Int J Oral Maxillofac Surg. 1990;19:74.
(SUBMANDIBULAR GLAND Barker GR. A radiolucency of the ascending ramus of
DEPRESSION) the mandible associated with invested parotid salivary
gland material and analogous with a Stafne bone cav-
Figure 9-9 ity. Br J Oral Maxillofac Surg. 1988;26:81.
Bsoul SA, Terezhalmy GT, Riley CK, Moore WS.
Age: Onset in childhood Developmental submandibular salivary gland depres-
Sex: Female predilection sion. Quintessence Int. 2002;33:242-243.
Choukas NC. Developmental submandibular gland
CLINICAL AND RADIOGRAPHIC
defect of the mandible. J Oral Maxillofac Surg.
FEATURES 1973;31:209.
The static bone cyst or submandibular sali- Stafne EC. Bone cavities situated near the angle of the
mandible. J Am Dent Assoc. 1942;29:1969.
vary gland depression is usually discov-
ered coincidentally on dental radiographs
because no symptoms are associated with
SUBLINGUAL GLAND
this benign developmental process. The
lesion is a well-circumscribed corticated DEPRESSION
oval radiolucency situated periapical to Figure 9-10
the second or third mandibular molar. The
Age: Onset in childhood
defect is not in continuity with root tips;
Sex: No known predilection
rather, it is located below the inferior alve-
olar canal. It is often bilateral. The lesion CLINICAL AND RADIOGRAPHIC
reflects a lingual depression of the cortical FEATURES
plate in which normal salivary gland tis- The sublingual glands may reside within
sue rests. A sialogram may be obtained and a lingual bone depression, similar to the
discloses the presence of ductal elements static bone cyst in relation to the subman-
converging in the region of the radiolucent dibular glands. The lesion lies apical to the
defect. Similar lesions of the mandibular anterior mandibular teeth and is a well-
ramus may encase parotid tissue. circumscribed unilocular radiolucency.
Bilateral defects may be witnessed. The
MICROSCOPIC FEATURES lucent foci may show progressive enlarge-
The contents of salivary depressions consist ment, which arrests in the teenage years.
of normal submandibular salivary tissue, There is no evidence of cortical expansion.
depending on the site of involvement.
MICROSCOPIC FEATURES
DIFFERENTIAL DIAGNOSIS A biopsy discloses the presence of normal-
The localization of submandibular gland appearing sublingual gland tissue.
depressions below the alveolar canal in the
absence of expansion or pain is characteris- DIFFERENTIAL DIAGNOSIS
tic, allowing for a radiologic diagnosis. The teeth are vital, and periapical cemen-
tal dysplasia may be considered. Usually
TREATMENT
the radiolucent area encompasses the api-
No treatment is required. Periodic radio- cal one third of the root. There is no racial
graphic follow-up is recommended to predilection. Because the disease is rare, an
ensure that no growth is taking place. exploratory biopsy is usually performed to
PMPH_Eversole_Chapter-09.indd 377 1/20/2011 2:56:07 PM
378 Chapter 9
FIGURE 9-10
Periapical radiolucency underlying mandibular cuspid and premolars representing sublingual gland
depression.
FIGURE 9-11
The paradental cyst lies
buccal to vital tooth roots
being superimposed over
the roots. These cysts are
often expansile.
rule out some other disease process that sublingual gland depression should be con-
may coincide in this location. In a young- sidered; a lingual surgical approach can be
ster with no clinical evidence of expansion, used for exploratory purposes.
PMPH_Eversole_Chapter-09.indd 378 1/20/2011 2:56:07 PM
Radiolucent Lesions of the Jaws 379
TREATMENT and develop a pericoronitis. Pain and puru-
Once a definitive diagnosis is obtained by lent discharge are common complaints.
exploration and/or biopsy, no treatment is
necessary. MICROSCOPIC FEATURES
The paradental cyst is an inflammatory
lesion and shares histologic features with
Additional Reading other odontogenic cysts; as mentioned
Batsakis JG. Heterotopic and accessory salivary tissues.
previously, it probably originates from a
Ann Otol Rhinol Laryngal. 1986;95:434. laterally displaced follicle, thereby being
Friedman J. Ectopic sublingual glands. Oral Surg Oral an inflamed dentigerous cyst. The lesion
Med Oral Pathol. 1964;18:219. is lined by nonkeratinizing stratified
Kaffe I, Littner MM, Arensburg B. The anterior buccal
mandibular depression: physical and radiologic fea-
squamous epithelium that is hyperplastic
tures. Oral Surg Oral Med Oral Pathol. 1990;69:647. with anastomosing, elongated rete ridges.
Solomon LW, Pantera EA, Jr, Monaco E, White SC, The cyst wall is thickened, exhibiting a dif-
Suresh L. A diagnostic challenge: anterior variant fuse mononuclear inflammatory cell infil-
of mandibular lingual bone depression. Gen Dent.
trate, and foci of acute inflammation may
2006;54:336-340.
Stene T, Pedersen KN. Aberrant salivary gland tissue be seen.
in the anterior mandible. Oral Surg Oral Med Oral
Pathol. 1977;44:72. DIFFERENTIAL DIAGNOSIS
Radiographically, paradental cyst differs
from most of the other interradicular lesions
PARADENTAL (BUCCAL
listed here in that the radiolucency is fre-
INFECTED) CYST quently superimposed over the tooth rather
Figure 9-11 than being solely interposed between the
roots. Biopsy is required to rule out other
Age: Young adults
more serious lesions.
Sex: No predilection
CLINICAL AND RADIOGRAPHIC TREATMENT
FEATURES
Enucleation and curettage can be under-
The paradental or buccal cyst is an odon- taken without sacrificing the adjacent teeth.
togenic cyst located buccal to an erupted Recurrence is not problematic.
to partially erupted vital molar tooth, or
according to some others, it can appear
interradicularly or distal to a tooth. Many
pathologists are of the belief that the para-
Additional Reading
dental cyst is merely a variant of dentiger- Ackerman G, Cohen MA, Altini M. The paradental cyst:
a clinicopathologic study of 50 cases. Oral Surg Oral
ous cyst in which the lesion became laterally Med Oral Pathol. 1987;64:308.
displaced during tooth eruption. These Craig GT. The paradental cyst. A specific inflammatory
cysts are by far most commonly encoun- odontogenic cyst. Br Dent J. 1976;141:9.
tered in the mandibular molar region and Philipsen HP, Reichart PA, Ogawa I, Suei Y, Takata T.
The inflammatory paradental cyst: a critical review
often show clinical, as well as radiographic, of 342 cases from a literature survey, including 17
evidence of buccal expansion. The radiolu- new cases from the author’s files. J Oral Pathol Med.
cency is unilocular and well marginated, 2004;33:147-155.
often superimposed over the affected tooth Stoneman DW, Worth HM. The mandibular infect-
ed buccal cyst-molar area. Dent Radiogr Photogr.
roots, yet many times the lesion projects 1983;56:1.
between contiguous teeth. Many paradental Vedtofte P, Praetorious F. The inflammatory paradental
cysts communicate with the gingival sulcus cyst. Oral Surg Oral Med Oral Pathol. 1989;68:182.
PMPH_Eversole_Chapter-09.indd 379 1/20/2011 2:56:15 PM
380 Chapter 9
CENTRAL GIANT CELL lished, appropriate laboratory tests should
GRANULOMA be performed to rule out brown tumor of
Figure 9-12 hyperparathyroidism.
Age: Young adults
Sex: Female predilection Additional Reading
CLINICAL AND RADIOGRAPHIC
Austin LT, Jr, Dahlin DC, Royer RA. Giant-cell
FEATURES reparative granuloma and related conditions affect-
Central giant cell granuloma is a neoplastic- ing the jawbones. Oral Surg Oral Med Oral Pathol.
1959;12:1285.
like reactive proliferation of the jaws that de Lange J, van den Akker HP, van den Berg H. Central
usually exhibits a multilocular pattern as giant cell granuloma of the jaw: a review of the litera-
observed radiographically. Early smaller ture with emphasis on therapy options. Oral Surg Oral
lesions are usually unilocular and fre- Med Oral Pathol Oral Radiol Endod. 2007;104:603-
615.
quently lie apical to vital teeth. The lesion High AS, Mathews A. The importance of radiography in
is more common in the mandible than in assessing the behaviour of an aggressive giant cell lesion
the maxilla underlying anterior or premo- of the jaws. Dentomaxillofac Radiol. 1989;18:36.
lar teeth. Buccal or lingual cortical expan- Horner K. Central giant cell granuloma of the jaws: a
clinicoradiological study. Clin Radiol. 1989;40:622.
sion can often be detected both clinically
Waldron CA, Shafer WG. The central giant cell repara-
and radiographically; expansile lesions can tive granuloma of the jaws: an analysis of 38 cases. Am
cause root divergence or resorption. J Clin Pathol. 1966;45:437.
MICROSCOPIC FEATURES
Multinucleated giant cells, dispersed MALIGNANCIES
throughout a hypercellular fibrovascular Figure 9-13
stroma, possess randomly arranged nuclei
that are either pyknotic and hyperchromatic Age: Adults
Sex: Depends on primary tumor location and
or oval and stippled with prominent nucle-
diagnosis
oli. Erythrocyte engorgement of vessels and
extravascular hemosiderin pigment are fre- CLINICAL AND RADIOGRAPHIC
quently observed as are occasional osseous FEATURES
trabeculae. The most common malignant tumor of
the jaws is metastatic carcinoma. Metasta-
DIFFERENTIAL DIAGNOSIS
tis to the jaws may arise from primary
The overlying teeth are generally vital, a tumors of the breast, colon, lungs, kidney,
feature that eliminates apical periodonti- prostate, and other organs less frequently.
tis. When expansion is present, most of the The mets tend to localize to the posterior
other lesions listed here can be eliminated, mandible and ramus, often causing mental
with the exception of cementoblastoma, nerve paresthesia. They are usually radio-
which is rarely encountered in the incisor- lucent but may induce osteogenesis and
premolar region. Other neoplastic processes are typically found adjacent to the roots of
and keratocysts can coincidentally arise posterior teeth. Although most metastatic
in periapical locations and expand bone. carcinomas manifest moth-eaten margins,
Biopsy is required to make the diagnosis. some may appear to be well delineated
yet punched out. Primary malignancies
TREATMENT
of bone can also present as apical radio-
Thorough curettage is the treatment of lucencies and include both sarcomas and
choice. When the diagnosis has been estab- carcinomas that arise from odontogenic
PMPH_Eversole_Chapter-09.indd 380 1/20/2011 2:56:15 PM
Radiolucent Lesions of the Jaws 381
FIGURE 9-12
Central giant cell granuloma appearing as periapical radiolucencies with root resorption.
epithelium. They are discussed elsewhere gen, progesterone, and Her2Nu for breast
in this chapter. cancer; carcinoembryonic antigen and
specific cytokeratins for colon cancer; and
MICROSCOPIC FEATURES S-100 protein for melanoma to mention but
Most metastatic tumors are adenocarci- a few).
nomas and will show ductal differentia-
DIFFERENTIAL DIAGNOSIS
tion, or the individual tumor cells will be
cuboidal or columnar. When metastasis is The other lesions listed here as apical radio-
suspected, immunohistochemical markers lucencies should be considered; metastatic
can be employed to assist in finding the tumors typically occur in association with
primary site of the tumor (e.g., prostate- vital teeth, and lip paresthesia is a telling
specific antigen for prostate cancer; estro- symptom for malignancy.
PMPH_Eversole_Chapter-09.indd 381 1/20/2011 2:56:15 PM
382 Chapter 9
FIGURE 9-13
Malignant lesions: meta-
static carcinoma of the
breast (upper left), multi-
ple myeloma (upper right),
primary intra-alveolar car-
cinoma (lower).
FIGURE 9-14
Lateral periodontal cyst
interposed between two
vital mandibular teeth.
PMPH_Eversole_Chapter-09.indd 382 1/20/2011 2:56:18 PM
Radiolucent Lesions of the Jaws 383
TREATMENT buccal cortical plate may or may not show
First and foremost is the detection of the moderate bulging when examined clini-
primary tumor in cases of metastasis. Che- cally. Pain is not a feature.
motherapy is usually required and most
cases have a poor prognosis. MICROSCOPIC FEATURES
The cyst lining is either nonkeratinizing
stratified squamous, or stratified cuboidal,
Additional Reading epithelium that shows a tendency for con-
Akinbami BO. Metastatic carcinoma of the jaws: a review volution and irregularity. The fibrous wall
of literature. Niger J Med. 2009;18:139-142. manifests minimal inflammation.
Baykul T, Aydin U, O Carroll MK. Unusual combina-
tion of presenting features in multiple myeloma. DIFFERENTIAL DIAGNOSIS
Dentomaxillofac Radiol. 2004;33:413-419.
Divya KS, Moran NA, Atkin PA. Numb chin syndrome: Lateral periodontal cyst may be differenti-
a case series and discussion. Br Dent J. 2010;208:157- ated from a laterally displaced apical peri-
160. odontal cyst on the basis of vitalometer
Selden HS, Manhoff DT, Hatges NA, Michel RC.
Metastatic carcinoma to the mandible that mimicked testing because the former arise develop-
pulpal/periodontal disease. J Endod. 1998;24:267- mentally, having no relationship to pulpal
270. disease. The radiographic features may be
Zwetyenga N, Pinsolle J, Rivel J, Majoufre-Lefebvre C, identical to those of keratocyst, primordial
Faucher A, Pinsolle V. Primary intraosseous carci-
noma of the jaws. Arch Otolaryngol Head Neck Surg. cyst, globulomaxillary cyst, incisive canal
2001;127:794-797. cyst, and calcifying epithelial odontogenic
(Gorlin) cyst. Biopsy is required to differen-
tiate among most of these entities.
Interradicular Radiolucencies TREATMENT
LATERAL PERIODONTAL CYST Surgical enucleation or curettage with pres-
Figure 9-14 ervation of adjoining teeth is the treatment
of choice.
Age: Adults
Sex: Slight female predilection
CLINICAL AND RADIOGRAPHIC Additional Reading
FEATURES
Eliasson S, Isacsson G, Kondell PA. The lateral periodon-
The lateral periodontal cyst may arise from tal cysts. Clinical, radiographical and histopathological
epithelial rests in the periodontal ligament findings. Int J Oral Maxillofac Surg. 1989;18:191.
or may represent a primordial cyst originat- Fantasia JE. Lateral periodontal cyst. Oral Surg Oral
Med Oral Pathol. 1979;48:237.
ing from a supernumerary tooth bud. The Formoso Senande MF, Figueiredo R, Berini Aytés L,
fact that this cyst is most frequently encoun- Gay Escoda C. Lateral periodontal cysts: a retrospec-
tered in the mandibular premolar region, a tive study of 11 cases. Med Oral Patol Oral Cir Bucal.
common location for supernumerary teeth, 2008;13:E313-E317.
Moskow BS, Siegel K, Zegarelli EV, Kutscher AH,
lends credence to this latter hypothesis. Rothenberg F. Gingival and lateral periodontal cysts.
Radiographically, the lateral periodontal J Periodontol. 1970;41(5):249-260.
cyst is an interradicular radiolucency with Standish SM, Shafer WG. The lateral periodontal cyst.
well-defined or corticated margins. The J Periodontol. 1958;29:27.
Wysocki GP, Brannon RB, Gardner DG, Sapp P.
adjacent teeth usually show some degree Histogenesis of the lateral periodontal cyst and the
of root divergence, and they are vital when gingival cyst of the adult. Oral Surg Oral Med Oral
evaluated with an electric pulp tester. The Pathol. 1980;50:327.
PMPH_Eversole_Chapter-09.indd 383 1/20/2011 2:56:21 PM
384 Chapter 9
LATERALLY DISPLACED also contain cholesterol clefts. Apical granu-
APICAL PERIODONTAL CYST lomas comprise inflamed granulation tissue
OR GRANULOMA and may have foreign material from endo-
dontic sealers in previously treated teeth.
Figure 9-15
Age: Adults DIFFERENTIAL DIAGNOSIS
Sex: No predilection The most common considerations in the dif-
CLINICAL AND RADIOGRAPHIC ferential are lateral periodontal cyst and odon-
FEATURES togenic keratocyst. The globulomaxillary cyst
Apical or radicular cysts are usually located was at one time considered to be a fissural
directly distal to the tooth root apex as a cyst located between a divergent maxillary
consequence of endodontic infection. When lateral incisor and cuspid. Most of these are
teeth harbor accessory root canals that are apical cysts from endodontic infection, others
oriented from the pulp chamber to the lat- are lateral periodontal cysts or keratocysts.
eral aspect of the root or when an infected Vitality testing should be undertaken.
root fracture is present, the spread of infec-
tion can progress laterally and occur as far TREATMENT
as midway up the root. Pain may be a fea- If the incriminated tooth is nonvital, endo-
ture, or in low virulence infections the tooth dontic therapy along with cystectomy is the
may be asymptomatic. treatment of choice.
MICROSCOPIC FEATURES
Apical periodontal cysts show a nonkerati- Additional Reading
nized, often hyperplastic, stratified squamous Kanas RJ, DeBoom GW, Jensen JL. Inverted heart-
epithelial lining along with a fibrous cyst shaped, interradicular radiolucent area of the anterior
wall that is infiltrated by leukocytes; many maxilla. J Am Dent Assoc. 1987;115:887-889.
FIGURE 9-15
Laterally displaced endodontic infec-
tions are found when infection spreads
through a lateral root fracture or
accessory canal.
PMPH_Eversole_Chapter-09.indd 384 1/20/2011 2:56:21 PM
Radiolucent Lesions of the Jaws 385
Lim AA, Peck RH. Bilateral mandibular cyst: lateral tooth was removed; whereas most are
radicular cyst, paradental cyst, or mandibular infected asymptomatic, some are associated with
buccal cyst? Report of a case. J Oral Maxillofac Surg.
2002;60:825-827. pain. Radiographically, the lesion is a well-
Prockt AP, Schebela CR, Maito FD, Sant’Ana-Filho M, circumscribed, often corticated, radiolu-
Rados PV. Odontogenic cysts: analysis of 680 cases in cency located in an edentulous region once
Brazil. Head Neck Pathol. 2008;2:150-156. occupied by a tooth.
Steiner DR. A lesion of endodontic origin misdiagnosed
as a globulomaxillary cyst.
J Endod. 1999;25:277-281. MICROSCOPIC FEATURES
Residual cysts are lined by noncornified
stratified squamous epithelium that may
RESIDUAL CYST contain hyaline bodies within the spinous
Figure 9-16 cell layer. The fibrous wall generally shows
an inflammatory cell infiltrate.
Age: Adults
Sex: Male predilection DIFFERENTIAL DIAGNOSIS
CLINICAL AND RADIOGRAPHIC The residual cyst is easily confused radio-
FEATURES graphically with primordial cyst. The lat-
A residual cyst is any type of odontogenic ter arises in lieu of a tooth, whereas the
cyst that persists in bone after the tooth with former arises in relation to an extracted
which it was associated has been removed. tooth. Residual cyst may also be confused
Therefore, a residual cyst may represent an radiographically with keratocyst, lateral
apical periodontal cyst if a necrotic tooth periodontal cyst, and calcifying epithelial
overlying the lesion was extracted, or it may odontogenic cyst. Biopsy is required to
represent a dentigerous cyst if an impacted arrive at a definitive diagnosis.
FIGURE 9-16
Residual periapical
cysts are located in a
site previously occu-
pied by a carious non-
vital tooth.
PMPH_Eversole_Chapter-09.indd 385 1/20/2011 2:56:23 PM
386 Chapter 9
TREATMENT In general, the fibrous wall is free from
Surgical enucleation or curettage is the inflammation.
treatment of choice.
DIFFERENTIAL DIAGNOSIS
Additional Reading Lateral odontogenic keratocyst must be
differentiated by biopsy from lateral peri-
Ahlstrom U, Johnson CC, Lautz B. Radicular and residu- odontal cyst, primordial cyst, residual cyst,
al cysts of the jaws: a long term roentgenographic study incisive canal cyst, and calcifying epithelial
following cystectomies. Odontol Rev. 1969;20:11. odontogenic cyst. In addition, the odonto-
Cabrini RL, Barros RE, Albano H. Cysts of the jaws: a sta-
genic adenomatoid tumor and any of those
tistical analysis. J Oral Maxillofac Surg. 1970;28:485.
Gardner DG. Residual cysts. Oral Surg Oral Med Oral lesions classified with the multilocular radi-
Pathol Oral Radiol Endod. 1997;84:114-115. olucencies may begin as unilocular radiolu-
High AS, Hirshmann PN. Age changes in residual radic- cencies in an interradicular location.
ular cysts. J Oral Pathol Med. 1986;15:524.
Murmura G, Traini T, Di Iorio D, Varvara G, Orsini G,
Caputi S. Residual and inflammatory radicular cysts. TREATMENT
Clinical and pathological aspects of 2 cases. Minerva Surgical enucleation is indicated. At sur-
Stomatol. 2004;53:693-701.
gery, the keratocyst is represented by a thin
delicate membrane. Small cysts have a low
ODONTOGENIC KERATOCYST recurrence rate, probably less than 20%,
whereas large expansile lesions commonly
Figure 9-17
recur following curettage.
Age: Adults
Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Additional Reading
FEATURES Brannon RB. The odontogenic keratocyst. A clinico-
pathologic study of 312 cases. Part I. Clinical features.
The odontogenic keratocyst is a specific Oral Surg Oral Med Oral Pathol. 1976;42:54.
form of odontogenic cyst that is microscopi- Browne RM. The odontogenic keratocyst. Br Dent J.
cally distinct. It may assume the character 1970;128:225.
Eliasson S, Isacsson G, Kondell PA. Lateral periodon-
of any of the odontogenic cysts and there-
tal cysts. Clinical radiographical and histopathological
fore may represent a keratinizing variant findings. Int J Oral Maxillofac Surg. 1989;18:191.
of the lateral periodontal cyst. Radiographi- Madras J, Lapointe H. Keratocystic odontogenic tumour:
cally, when interradicular, it is a well-mar- reclassification of the odontogenic keratocyst from cyst
ginated radiolucency with a propensity for to tumour. Tex Dent J. 2008 ;125:446-454.
Wright JM. The odontogenic keratocyst: Orthokeratinized
root divergence and cortical expansion. It is variant. Oral Surg Oral Med Oral Pathol.
not found in relation to nonvital teeth; pain 1981;51:609.
is not a symptom. When multiple kerato-
cysts of the jaws are observed, the nevoid
basal cell carcinoma syndrome should be PRIMORDIAL CYST
investigated. Figure 9-18
MICROSCOPIC FEATURES Age: Onset in young adulthood
Sex: No predilection
The lumen is often filled with desquamated
keratin. The lining, stratified squamous CLINICAL AND RADIOGRAPHIC
epithelium, possesses a corrugated par- FEATURES
akeratin layer, an attenuated spinous cell Primordial cysts arise from a developing
layer, and a polarized basal cell layer. tooth that fails to differentiate; rather, the
PMPH_Eversole_Chapter-09.indd 386 1/20/2011 2:56:24 PM
Radiolucent Lesions of the Jaws 387
FIGURE 9-17
Interradicular radiolu-
cencies with mild root
divergence represent
odontogenic keratocysts.
odontogenic epithelium becomes cystic DIFFERENTIAL DIAGNOSIS
prior to the formation of dental hard tis- The primordial cyst may be radiographi-
sues. Radiographically, the primordial cyst cally differentiated from the residual cyst
is unilocular, radiolucent, and well demar- because the former arises in lieu of a tooth,
cated. The lesion is interradicular or adja- whereas the latter is seen after tooth extrac-
cent to teeth and is always present in an tion. The primordial cyst must also be dif-
area where a tooth would normally have ferentiated from lateral periodontal cyst
developed. The most common locations and calcifying epithelial odontogenic cyst.
are third molar regions and the midline
of the maxilla, apparently from the tooth
TREATMENT
germ of a mesiodens. Despite the afore-
mentioned features, many oral patholo- Surgical enucleation is the treatment of
gists disclaim the existence of primordial choice.
cyst as defined here. Other pathologists in
Africa and Europe define primordial cysts
as keratocysts. Additional Reading
Forssell K, Kallioniemi H, Sainio P. Microcysts and epi-
MICROSCOPIC FEATURES thelial islands in primordial cysts. Proc Finn Dent Soc.
Primordial cysts are lined by stratified 1979;75:99.
Robinson HBG. Classification of cysts of the jaws. Am J
squamous epithelium, and most of them Orthod Dentofacial Orthop. 1945;31:370.
represent keratocysts. The fibrous wall usu- Shear M. Primordial cysts. J Dent Assoc S Afr.
ally lacks an inflammatory cell infiltrate. 1960;15:211.
PMPH_Eversole_Chapter-09.indd 387 1/20/2011 2:56:24 PM
388 Chapter 9
FIGURE 9-18
Unilocular radiolucencies
arising in lieu of a tooth
representing primordial
cysts.
Soskolne WA, Shear M. Observations on the pathogen- was first recognized, it was discovered that
esis of primordial cysts. Br Dent J. 1967;123:321. there are solid tumor forms, also benign in
their behavior. Nearly one fourth of these
cysts are located peripheral to bone on the
CALCIFYING CYSTIC attached gingiva. The teeth test vital, and
ODONTOGENIC TUMOR pain is not a feature.
Figure 9-19
MICROSCOPIC FEATURES
Age: No predilection
Sex: No predilection The lining epithelium shows distinct
pathognomonic features. The basal cell layer
CLINICAL AND RADIOGRAPHIC is polarized, assuming the posture of amelo-
FEATURES
blasts. The spinous cell layer resembles that
The calcifying odontogenic cyst, or Gor- of stratified squamous epithelium or may
lin cyst, arises most often in the premolar acquire the features of stellate reticulum.
region of the mandible, appearing as a well- Melanin pigment has been reported to occur
demarcated unilocular radiolucency located in these lesions. The spinous cells undergo
interproximally. The lesion may be entirely keratinization toward the luminal surface;
radiolucent or may contain radiopaque cal- large eosinophilic cells with vacuoles replac-
cific flecks. Divergence of the juxtaposed ing nuclei are apparent, termed ghost cells.
roots is a common finding. After this lesion An eosinophilic dentinoid material is often
PMPH_Eversole_Chapter-09.indd 388 1/20/2011 2:56:26 PM
Radiolucent Lesions of the Jaws 389
found within the fibrous wall in juxtaposi-
tion to the basal cells. Occasionally, the epi-
thelium proliferates along the differentiated
lines just enumerated yet fails to form a true
cyst. Many Gorlin cysts are therefore benign
neoplastic proliferations rather than true
cysts. The features of this cyst on occasion
are found in association with odontomas or
even in other types of odontogenic tumors.
Two variants include the dentinogenic ghost
cell tumor and the malignant ghost cell tumor.
The former shows sheets of odontogenic epi-
thelium with focal aggregates of ghost cells
and deposition of induced dentine; the latter
is similar histologically yet is highly cellular
with mitotic figures.
DIFFERENTIAL DIAGNOSIS
Calcifying cystic odontogenic cysts and
tumors in the entirely radiolucent stage
may be confused radiographically with lat-
eral periodontal cyst, odontogenic kerato-
cyst, primordial cyst, residual cyst, or one of
the nonodontogenic developmental cysts if FIGURE 9-19
located in specific areas in which confusion The calcifying cystic odontogenic tumor may be
may occur. Apical periodontal cysts arising predominantly cystic or it may be a solid tumor. It
from a necrotic lateral pulp canal can be is usually a well-circumscribed radiolucency located
ruled out on the basis of vitalometry. in the anterior segments.
TREATMENT
Surgical excision or curettage is the treat- dentinogenic ghost cell tumour and ghost cell odonto-
ment of choice. Recurrence is rare, although genic carcinoma. J Oral Pathol Med. 2008;37:302-308.
Soames JV. A pigmented calcifying odontogenic cyst.
the aggressive malignant ghost cell tumor
Oral Surg Oral Med Oral Pathol. 1982;53:395.
may require resection.
Additional Reading SQUAMOUS ODONTOGENIC
Abrams AM, Howell FW. The calcifying odontogenic
TUMOR
cyst. Oral Surg Oral Med Oral Pathol. 1968;25:594. Figure 9-20
Ellis GL, Shmookler BM. Aggressive (malignant?) epi-
thelial odontogenic ghost cell tumor. Oral Surg Oral Age: Young adults
Med Oral Pathol. 1986;61:471. Sex: Female predilection
Gorlin RJ, Pindborg JJ, Clausen FP, Vickers RA. The cal-
cifying odontogenic cyst—a possible analogue of the CLINICAL AND RADIOGRAPHIC
cutaneous calcifying epithelioma of Malherbe. Oral FEATURES
Surg Oral Med Oral Pathol. 1962;15:1235.
Ledesma-Montes C, Gorlin RJ, Shear M, et al.
Squamous odontogenic tumor is a hama-
International collaborative study on ghost cell odonto- rtomatous proliferation of odontogenic
genic tumours: calcifying cystic odontogenic tumour, epithelium, probably arising from the rests
PMPH_Eversole_Chapter-09.indd 389 1/20/2011 2:56:33 PM
390 Chapter 9
FIGURE 9-20
Interradicular defect in
squamous odontogenic
tumor. (Courtesy of Dr. A.
Jonker.)
of Malassez. The maxillary incisor-canine and some of the squamous nests exhibit
area and mandibular molar area are the ovoid crystalloid structures.
primary sites of involvement. Most cases
are unifocal with well demarcated mar- DIFFERENTIAL DIAGNOSIS
gins and shaped like a wine flask. Tooth
The radiographic features simulate a local-
mobility is the chief presenting sign; radio-
ized periodontal defect enveloping roots.
graphically, a localized radiolucency inter-
Langerhans disease should also be consid-
posed between contiguous teeth appears
ered in the differential diagnosis.
as a well-circumscribed periodontal defect.
Most cases are either triangular or semi-
TREATMENT
circular in configuration. Some lesions
exhibit an intact overlying alveolar crest; Most cases fail to recur after extraction of
most, however, extend coronally with loss the involved tooth and thorough curet-
of crestal bone. Although usually a soli- tage of the lesional tissue. Maxillary lesions
tary lesion, familial multifocal lesions have may be more extensive, involving the
been reported. sinus; resection may be required to prevent
recurrence.
MICROSCOPIC FEATURES
Oval, round, and curvilinear nests of
squamous epithelial cells are dispersed Additional Reading
throughout a mature collagenous stroma. Doyle JL, Grodjesk JE, Dolinsky HB, Rafel SS.
The basilar stratum fails to show polariza- Squamous odontogenic tumor: Report of three cases.
tion. Cystic degeneration is commonly seen, J Oral Maxillofac Surg. 1977;35:994.
PMPH_Eversole_Chapter-09.indd 390 1/20/2011 2:56:34 PM
Radiolucent Lesions of the Jaws 391
Goldblatt LI, Brannon RB, Ellis GL. Squamous odon- maxilla. The lesion lies within the alveo-
togenic tumor. Report of five cases and review of lar bone subjacent to the antral floor and
the literature. Oral Surg Oral Med Oral Pathol.
1982;54:187. is generally confined to an edentulous or
Leider AS, Jonker JA, Cook HE. Multicentric familial interradicular area in the posterior maxilla.
squamous odontogenic tumor. Oral Surg Oral Med Pain or discomfort may be present.
Oral Pathol. 1989;68:175.
Lin YL, White DK. Squamous odontogenic tumor. Oral
MICROSCOPIC FEATURES
Maxillofac Surg Clin North Am. 2004;16:355-357.
Pullon PA, Shafer WG, Elzay RP, Kerr DA, Corio RL. The cyst is lined by pseudostratified colum-
Squamous odontogenic tumor. Report of six cases of nar ciliated epithelium. The connective tis-
a previously undescribed lesion. Oral Surg Oral Med
Oral Pathol. 1975;40:616. sue wall may display an inflammatory cell
infiltrate.
SURGICAL CILIATED CYST DIFFERENTIAL DIAGNOSIS
Figure 9-21 By virtue of its location, the surgical cili-
ated cyst may radiographically resemble
Age: Adults an apical periodontal cyst, residual odonto-
Sex: Male predilection genic cyst, or low sinus extension. Indeed,
CLINICAL AND RADIOGRAPHIC loculations of the maxillary sinus are com-
FEATURES mon. A history of previous sinus surgery
After a Caldwell-Luc operation, fragments coupled with biopsy allows for a definitive
of sinus epithelial lining may become diagnosis.
entrapped in the maxillary surgical site. If
this epithelium undergoes benign cystic TREATMENT
proliferation, a unilocular well-delineated Surgical enucleation is the treatment of
radiolucency becomes discernible in the choice.
FIGURE 9-21
Well-circumscribed radiolucency in the posterior maxilla subsequent to a Caldwell-Luc procedure or a
postosteotomy is typical for surgical ciliated cysts.
PMPH_Eversole_Chapter-09.indd 391 1/20/2011 2:56:39 PM
392 Chapter 9
MICROSCOPIC FEATURES
Additional Reading Adipose tissue is seen with multiple foci
Gregory GT, Shafer WG. Surgical ciliated cysts of the of hematopoietic blast cells of myeloid,
maxilla: Report of cases. J Oral Maxillofac Surg. erythroid, lymphoid, and megakaryocytic
1958;16:251.
cell lines. Thin osseous trabeculae are also
Kaneshiro S, Nakajima T, Yoshikawa Y, Iwasaki H,
Tokiwa N. The postoperative maxillary cyst: report of encountered.
71 cases. J Oral Maxillofac Surg. 1981;39:191.
Miller R, Longo J, Houston G. Surgical ciliated cyst of DIFFERENTIAL DIAGNOSIS
the maxilla. J Oral Maxillofac Surg. 1988;46:310.
Shafer WG, Hine MK, Levy BM. A Textbook of Oral A nonexpansile poorly marginated radio-
Pathology. 4th ed. Philadelphia, PA: W. B. Saunders; lucency in an edentulous or interproxi-
1983:545. mal area is probably an osteoporotic bone
Sugar AW, Walker DM, Bounds GA. Surgical ciliated marrow defect. The other interradicular
(postoperative maxillary) cysts following mid-face
osteotomies. Br J Oral Maxillofac Surg. 1990;28: radiolucencies listed in this chapter show
264-267. well-defined borders. Other nonexpansile
poorly demarcated radiolucencies include
multiple myeloma, histiocytosis X, and met-
OSTEOPOROTIC BONE astatic cancer. For this reason, even though
MARROW DEFECT suspicion is high for bone marrow defect, a
Figure 9-22 biopsy should be performed.
Age: Middle-aged adults TREATMENT
Sex: Female predilection Once the diagnosis is confirmed by biopsy,
CLINICAL AND RADIOGRAPHIC no further treatment is needed.
FEATURES
After tooth extraction, the socket may heal
by formation of hematopoietic marrow
Additional Reading
rather than cancellous bone. This results Crawford BE, Weathers DR. Osteoporotic mar-
row defects of the jaws. J Oral Maxillofac Surg.
in a radiolucency located in the edentulous 1970;28:600.
region previously occupied by a tooth. The Schneider LC, Mesa ML, Fraenkel D. Osteoporotic
radiolucency characteristically shows ill- bone marrow defect: radiographic features and
defined ragged margins that blend into the pathogenic factors. Oral Surg Oral Med Oral Pathol.
1988;65:127.
normal adjacent cancellous bone. Cortical Shankland WE, Bouquot JE. Focal osteoporotic marrow
expansion does not occur, and pain is not defect: report of 100 new cases with ultrasonography
a feature. scans. Cranio. 2004;22:314-319.
FIGURE 9-22
Radiolucency in previous extraction site representing an osteoporotic bone marrow defect.
PMPH_Eversole_Chapter-09.indd 392 1/20/2011 2:57:01 PM
Radiolucent Lesions of the Jaws 393
Standish SM, Shafer WG. Focal osteoporotic bone expansion, and the mandible is affected
marrow defects of the jaws. J Oral Maxillofac Surg. far more frequently than the maxilla.
1962;20:123.
Radiographically, the lesion is unilocu-
lar, although multilocular patterns are
CENTRAL OSSIFYING also encountered. Expansion with clearly
demarcated borders is typical: in the man-
(CEMENTIFYING) FIBROMA dible, a smooth bowing expansion of the
Figure 9-23 inferior border is commonly observed. The
lesion usually extends between teeth and
Age: Children and young adults
Sex: Female predilection causes root divergence. In the early growth
stage, the lesion may appear entirely radio-
CLINICAL AND RADIOGRAPHIC lucent; with time, the center becomes pro-
FEATURES
gressively radiopaque as more calcified
Ossifying fibroma of bone is a neoplasm product is elaborated. If left untreated,
representing one of the benign fibro-os- the tumor may reach massive proportions
seous lesions of the jaws. When the tumor and result in significant facial disfigure-
synthesizes cementum rather than osteoid, ment. Ossifying fibromas are found in
the lesion is referred to as a cementifying hyperparathyroidism among patients with
fibroma. Clinically, the lesion manifests a mutation in the HRPT2 gene: the hyper-
as a painless enlargement with cortical parathyroidism-jaw tumor syndrome.
FIGURE 9-23
Radiolucencies with expan-
sion extending between
molar roots represent
central ossifying fibromas.
One instance shows two
separate lesions, a rare
finding.
PMPH_Eversole_Chapter-09.indd 393 1/20/2011 2:57:03 PM
394 Chapter 9
MICROSCOPIC FEATURES Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
2006;101(2):212-218.
A highly cellular fibroblastic stroma pre- Chang CC, Hung HY, Chang JY, et al. Central ossify-
vails, with the presence of delicate colla- ing fibroma: a clinicopathologic study of 28 cases.
gen fibers. Capillaries course throughout J Formos Med Assoc. 2008;107:288-294.
Eversole LR, Leider AS, Nelson K. Ossifying fibroma: a
this stroma, and foci of osteoid trabeculae
clinicopathologic study of sixty-four cases. Oral Surg
are observed. In radiolucent lesions, the Oral Med Oral Pathol. 1985;60:505.
fibrous element is predominant and the Waldron CA. Fibro-osseous lesions of the jaws. J Oral
osteoid matrix is poorly calcified. When Maxillofac Surg. 1970;28:58.
ovoid or curvilinear trabeculae prevail and Waldron CA, Giansanti JS. Benign fibro-osseous lesions
of the jaws: a clinical-radiologic-histologic review of
show polarization patterns consistent with sixty-five cases. Part II. Benign fibro-osseous lesions of
cementum, then the lesion is differentiat- periodontal ligament origin. Oral Surg Oral Med Oral
ing along periodontal ligament progeni- Pathol. 1973;35:340.
tor cell lines. These cementifying patterns
are more often seen in black than in white
patients. ODONTOGENIC
ADENOMATOID TUMOR
DIFFERENTIAL DIAGNOSIS Figure 9-24
Ossifying and cementifying fibromas in
Age: Teenagers
the early radiolucent stage must be dif- Sex: Female predilection
ferentiated from various cysts appearing
as interradicular radiolucencies and from CLINICAL AND RADIOGRAPHIC
FEATURES
other fibro-osseous and central neoplasms
included in the section on multilocular Although the odontogenic adenomatoid
radiolucencies, because any of those lesions tumor typically arises in association with
may begin as a unilocular radiolucency. the crown of an impacted tooth, 25% are
Differentiation from fibrous dysplasia is not located laterally. The maxilla is more often
difficult when microscopic and radiologic affected, with radiolucency interposed
features are considered together. Fibrous between contiguous teeth. They typically
dysplasia evinces poorly demarcated bor- localize to the premolar or anterior regions.
ders radiographically, whereas ossifying The radiolucency often contains radiopaque
and cementifying fibromas show well-mar- flecks because portions of the tumor can
ginated borders. calcify. It is almost invariably unilocular
and is well demarcated or corticated. Pain-
TREATMENT less cortical expansion is often the present-
Surgical enucleation is rarely followed by ing sign.
recurrence. Nevertheless, aggressive behav-
MICROSCOPIC FEATURES
ior is encountered, and some cases manifest
multiple recurrences. In these instances, en The tumor is surrounded by a dense
bloc resection may be required to eradicate fibrous capsule. The epithelial neoplas-
the disease. tic tissue often assumes the appearance
of a cyst with luminal proliferation. The
epithelial cells are elongated and arrange
Additional Reading themselves in swirls. This growth pattern
Aldred MJ, Talacko AA, Savarirayan R, et al. Dental
yields a granuloma-like configuration.
findings in a family with hyperparathyroidism-jaw Admixed with the spindle cell component
tumor syndrome and a novel HRPT2 gene mutation. are oval nests of columnar epithelial cells
PMPH_Eversole_Chapter-09.indd 394 1/20/2011 2:57:12 PM
Radiolucent Lesions of the Jaws 395
FIGURE 9-24
Interradicular odontogenic
adenomatoid tumors are
radiolucent and over time
develop calcifications.
with ameloblastic cytologic features. These TREATMENT
cells are oriented about an eosinophilic Simple enucleation of the neoplasm is ade-
secretion product and in classic examples quate treatment. Sometimes one or both of
assume ductal patterns with a central the adjacent teeth will require extraction.
lumen. Hyaline eosinophilic elements are The tumor rarely recurs.
also present, and in many areas, these cell
products undergo a dystrophic type of cal-
cification. Rarely, melanin pigment may
be present. Other coexistent odontogenic
Additional Reading
tumor histologic patterns are occasionally Abrams AM, Melrose RJ, Howell FV.
encountered. Adenoameloblastoma; a clinical pathologic study of
ten new cases. Cancer. 1968;22:175.
Courtney RM, Kerr DA. The odontogenic adenoma-
DIFFERENTIAL DIAGNOSIS toid tumor. Oral Surg Oral Med Oral Pathol.
Odontogenic adenomatoid tumors seen as 1975;39:424.
Giansanti JS, Someren A, Waldron CA. Odontogenic
interradicular radiolucencies must be dif- adenomatoid tumor (adenoameloblastoma). Oral Surg
ferentiated from other lesions that arise Oral Med Oral Pathol. 1970;30:69.
between teeth. The young age, anterior loca- Ide F. Inter-radicular adenomatoid odontogenic tumor
tion, and tendency for the calcifications to of the anterior mandible. Oral Maxillofac Surg.
2010;68:490-491.
occur are highly suggestive of odontogenic Siar CH, Nof KH. Adenomatoid odontogenic tumor:
adenomatoid tumor. Biopsy is required to a survey of 44 new cases in Malaysia. Ann Dent.
obtain a definitive diagnosis. 1986;45:11.
PMPH_Eversole_Chapter-09.indd 395 1/20/2011 2:57:13 PM
396 Chapter 9
ODONTOGENIC FIBROMA the crowns of impacted teeth and are
Figure 9-25 multiple and associated with hypoplastic
enamel in the odontogenic fibroma/hamar-
Age: Wide range toma enamel hypoplasia syndrome (see peri-
Sex: Female predilection coronal radiolucencies).
CLINICAL AND RADIOGRAPHIC
FEATURES MICROSCOPIC FEATURES
The odontogenic fibroma is classified A mature collagenous proliferation is pres-
as a mesenchymal odontogenic tumor. ent with monomorphic-appearing fibro-
It is typically interradicular and may blasts and a small vessel network. The
be located anywhere in the jaws. As the lesion is relatively hypocellular. Dispersed
tumor enlarges it can resorb the roots of throughout are small oval and linear odon-
adjacent teeth. In maxilla tumors, a dim- togenic epithelial islands with prominent
ple may be seen on the palate adjacent to eosinophilic, or sometimes clear, cytoplasm.
where the tumor is located. The lesion is Some cases may show amyloid deposits,
usually asymptomatic. This tumor also and the epithelial islands are wrapped
occurs peripherally on the gingiva. Odon- with dentritic cells positive for CD1a. Some
togenic fibromas may also occur around cases of odontogenic fibroma were found
FIGURE 9-25
Odontogenic fibromas often cause root resorption. A palatal “dimple” may also occur adjacent to the
tumor.
PMPH_Eversole_Chapter-09.indd 396 1/20/2011 2:57:25 PM
Radiolucent Lesions of the Jaws 397
to contain granular cells both in the epi- frequently lie adjacent to vital teeth. The
thelium and the stroma. This variant has lesion is more common in the mandible
been reclassified as granular cell odontogenic than in the maxilla underlying anterior
tumor. Another variation is the coexistence or premolar teeth. Buccal or lingual corti-
of odontogenic fibroma with central giant cal expansion can often be detected both
cell granuloma. clinically and radiographically; expan-
sile lesions can cause root divergence or
DIFFERENTIAL DIAGNOSIS resorption.
The presence of root resorption and palatal
MICROSCOPIC FEATURES
dimpling are highly suggestive of odonto-
genic fibroma. Other entities included here Multinucleated giant cells, dispersed
must be considered. throughout a hypercellular fibrovascular
stroma, possess randomly arranged nuclei
TREATMENT that are either pyknotic and hyperchromatic
Curettage is the treatment of choice. Teeth or oval and stippled with prominent nucle-
exhibiting resorption will usually require oli. Erythrocyte engorgement of vessels and
extraction. extravascular hemosiderin pigment are fre-
quently observed as are occasional osseous
trabeculae.
Additional Reading DIFFERENTIAL DIAGNOSIS
Brannon RB, Goode RK, Eversole LR, Carr RF. The
central granular cell odontogenic tumor: report of The adjacent teeth are generally vital, a fea-
5 new cases. Oral Surg Oral Med Oral Pathol Oral ture that eliminates an endodontic infection.
Radiol Endod. 2002;94:614-621. When expansion is present, other lesions
Dunlap CL. Odontogenic fibroma. Semin Diagn Pathol.
1999;16:293-296.
listed here must be considered. Other neo-
Handlers JP, Abrams AM, Melrose RJ, Danforth R. plastic processes and keratocysts can coin-
Central odontogenic fibroma: clinicopathologic fea- cidentally arise in interradicular locations
tures of 19 cases and review of the literature. J Oral and expand bone. Biopsy is required to
Maxillofac Surg. 1991;49:46-54.
make the diagnosis.
Younis RH, Scheper MA, Lindquist CC, Levy B. Hybrid
central odontogenic fibroma with giant cell granulo-
ma-like component: case report and review of litera- TREATMENT
ture. Head Neck Pathol. 2008;2:222-226.
Thorough curettage is the treatment of
choice. When the diagnosis has been estab-
CENTRAL GIANT CELL lished, appropriate laboratory tests should
GRANULOMA be performed to rule out brown tumor of
hyperparathyroidism.
Figure 9-26
Age: Young adults
Sex: Female predilection
Additional Reading
CLINICAL AND RADIOGRAPHIC Austin LT, Jr, Dahlin DC, Royer RA. Giant-cell
FEATURES reparative granuloma and related conditions affect-
ing the jawbones. Oral Surg Oral Med Oral Pathol.
Central giant cell granuloma is a neoplas- 1959;12:1285.
tic-like reactive proliferation of the jaws de Lange J, van den Akker HP, van den Berg H. Central
giant cell granuloma of the jaw: a review of the lit-
that usually exhibits a multilocular pat- erature with emphasis on therapy options. Oral Surg
tern as observed radiographically. Early Oral Med Oral Pathol Oral Radiol Endod. 2007;104:
smaller lesions are usually unilocular and 603-615.
PMPH_Eversole_Chapter-09.indd 397 1/20/2011 2:57:45 PM
398 Chapter 9
FIGURE 9-26
Root divergence is com-
mon with central giant cell
granulomas.
High AS, Mathews A. The importance of radiography in chronic periodontitis. Indeed, it is the
assessing the behaviour of an aggressive giant cell lesion most common oral disease of adulthood.
of the jaws. Dentomaxillofac Radiol. 1989;18:36.
Horner K. Central giant cell granuloma of the jaws: a Whereas overt manifestations are encoun-
clinicoradiological study. Clin Radiol. 1989;40:622. tered during middle age, early features of
Waldron CA, Shafer WG. The central giant cell repara- the disease are often apparent in teenag-
tive granuloma of the jaws: an analysis of 38 cases. Am ers and young adults. Periodontal pockets
J Clin Pathol. 1966;45:437.
in excess of 3 mm are indicative of early
periodontitis. Radiographically, the alveo-
Periodontal (Alveolar) Bone lar bone evinces either a uniform apical
migration (horizontal bone loss) or multifo-
Loss cal sharply demarcated trenching (vertical
bone loss). The earliest stage is a V-shaped
CHRONIC PERIODONTITIS wedge seen on the alveolar process in the
Figure 9-27 interproximal region. The gingiva may be
edematous and hyperemic. Itching is often
Age: Middle-aged adults
Sex: No predilection
a symptom; however, the disease may
become severe without any symptoms of
CLINICAL AND RADIOGRAPHIC pain. The precise etiology is unknown, but
FEATURES the severity of inflammation and bone loss
The most common cause of alveolar bone is proportional to the amount of accumu-
loss, as evidenced radiographically, is lated plaque and calculus.
PMPH_Eversole_Chapter-09.indd 398 1/20/2011 2:57:45 PM
Radiolucent Lesions of the Jaws 399
FIGURE 9-27
Alveolar bone loss in chronic periodontitis.
MICROSCOPIC FEATURES instituting periodic dental prophylaxis
The crevicular epithelium lacks a cornified in conjunction with daily toothbrushing
layer and shows elongation of rete ridges and flossing. Diets low in refined sugar
with transmigration of neutrophils into the and carbohydrate also aid in minimizing
spinous layer. The subjacent fibrous and plaque accumulation. Once alveolar bone
granulation tissues are avidly infiltrated loss with pocket formation develops, root
with plasma cells and lymphocytes. planing, curettage, or periodontal surgery
is indicated.
DIFFERENTIAL DIAGNOSIS
Rapid alveolar bone loss may occur in
conjunction with juvenile diabetes, cyclic
Additional Reading
neutropenia, Langerhans disease, and leu- Goldman HM, Cohen DW. The infrabony pocket: clas-
sification and treatment. J Periodontol. 1958;29:272.
kemia. These diseases should be strongly Prichard JF. The role of the roentgenogram in the diag-
considered in the differential diagnosis of nosis and prognosis of periodontal disease. Oral Surg
alveolar bone loss in young adults and teen- Oral Med Oral Pathol. 1961;14:182.
agers. Periodontosis must be included in the Ruquet M, Bonfil JJ, Tardivo D, et al. Characteristics and
prediction of the alveolar bone loss: essay of modeling.
differential diagnosis yet shows a specific Odontostomatol Trop. 2009;32:5-16.
distribution of bone loss. Sheridan PJ, Reeve CM. Ch. 8. Periodontal disease. In:
Stafne EC, Gibilisco JA, eds. Oral Roentgenographic
TREATMENT Diagnosis. Philadelphia, PA: W. B. Saunders; 1975.
Theilade J. An evaluation of the reliability of radiographs
Prevention is the key to control of peri- in the measurement of bone loss in periodontal dis-
odontal disease. This is accomplished by ease. J Periodontol. 1960;31:143.
PMPH_Eversole_Chapter-09.indd 399 1/20/2011 2:57:48 PM
400 Chapter 9
DIABETIC PERIODONTITIS panied by premature periodontal disease
Figure 9-28 is usually overt, and patients show elevated
fasting blood glucose and glycosuria.
Age: Young and middle-aged adults
Sex: No predilection MICROSCOPIC FEATURES
CLINICAL AND RADIOGRAPHIC The microscopic features of diabetic perio-
FEATURES dontitis are the same as those described for
Nonspecific chronic periodontitis develops uncomplicated chronic periodontitis. Occa-
at an early age in diabetics, particularly in sionally, hyaline arteriolosclerosis can be
those with hyperglycemia of childhood demonstrated.
onset. As a result of microangiopathic
DIFFERENTIAL DIAGNOSIS
lesions throughout the body, including the
periodontium, in conjunction with deficient Premature alveolar bone loss is occasionally
fibroblastic energy metabolism resulting seen in uncomplicated periodontitis yet is
from decreased intracellular glucose uti- also a feature of periodontosis, Langerhans
lization, wound healing is impaired. Peri- disease, cyclic neutropenia, and leukemia.
odontal disease progresses rapidly with When severe or premature bone loss is
widespread horizontal or vertical alveo- encountered, a fasting blood glucose test and
lar bone loss. Multiple foci of periodontal urinalysis should be performed. If the blood
abscess formation often accompany the glucose is within normal limits, a 5-hour
chronic disease process. Diabetes accom- glucose tolerance test can be performed.
FIGURE 9-28
Premature horizontal and
vertical bone loss in a dia-
betic. Also note coinciden-
tal dentigerous cyst around
mandibular third molar.
PMPH_Eversole_Chapter-09.indd 400 1/20/2011 2:57:54 PM
Radiolucent Lesions of the Jaws 401
TREATMENT JUVENILE PERIODONTITIS
Once diabetes is diagnosed, the patient AND PAPILLON-LEFEVRE
requires medication in the form of oral SYNDROME
hypoglycemic drugs or parenteral insulin. Figure 9-29
Referral to a physician is indicated. The
periodontal disease should be managed Age: Childhood onset
the same as that uncomplicated by diabe- Sex: No predilection
tes; however, if arteriolar vascular disease CLINICAL AND RADIOGRAPHIC
is widespread, the prognosis for controlling FEATURES
or preventing continuation of the periodon-
A disease of obscure etiology, periodon-
tal lesions is not particularly good.
tosis, or juvenile periodontitis represents
an inflammatory lesion of the perodon-
Additional Reading tium with the formation of periodontal
pockets, loosening of teeth, and rapidly
Awartani F. Evaluation of the relationship between type progressive alveolar bone loss. Local fac-
2 diabetes and periodontal disease. Odontostomatol tors such as tooth-accumulated material
Trop. 2009;32:33-39.
Bartolucci EG, Parkes RB. Accelerated periodontal and calculus are not significant etiologi-
breakdown in uncontrolled diabetes. Pathogenesis cally. Immunopathic mechanisms, a gran-
and treatment. Oral Surg Oral Med Oral Pathol. ulocyte disorder, and anaerobic bacteria
1981;52:387. have been implicated as etiologic factors.
Benvetiste R, Bixler D, Conneally PM. Periodontal dis-
ease in diabetics. J Periodontol. 1967;38:271. In the generalized form, a leukocyte adhe-
Hugoson A, Thorstensson H, Falk H, Kuylenstierna J. sion deficiency occurs; however, the local-
Periodontal conditions in insulin-dependent diabetics. ized form has no known association with
J Clin Periodontol. 1989;16:215. a hematologic disorder. The subgingival
McMullen JA, Legg M, Gottsegen R, Camerini-Davalos
R. Microangiopathy within gingival tissues of diabetic
gram-negative anaerobic flora is specific
subjects with special reference to the prediabetic state. and unique to juvenile periodontosis and
Periodontics. 1967;5:61. differs considerably from the flora isolated
FIGURE 9-29
Alveolar bone loss con-
fined to incisor and molar
regions in juvenile perio-
dontitis (Papillon-LeFevre).
Bottom: nonsyndrome case
of juvenile periodontitis.
PMPH_Eversole_Chapter-09.indd 401 1/20/2011 2:57:58 PM
402 Chapter 9
from the pockets of adult chronic inflam-
matory periodontal disease—Actinobacillus Additional Reading
and Bacteroides being predominant organ- Gorlin RJ, Sedano H, Anderson JE. The syndrome of pal-
isms. Whether these organisms are patho- mar-plantar hyperkeratosis and premature periodontal
gens and play a causative role is unknown. destruction of the teeth. J Pediatr. 1964;65:895.
Radiographically, a classic topography of Ingle JI. Papillon-Lefevre syndrome; precocious
periodontosis with associated epidermal lesions.
alveolar osseous recession is encountered J Periodontol. 1959;30:230.
in the generalized form. The periodontal Pallos D, Acevedo AC, Mestrinho HD, Cordeiro I, Hart
tissues around the molars and incisors are TC. Novel cathepsin C mutation in a Brazilian fam-
selectively lost and replaced by granulation ily with Papillon-Lefèvre syndrome: case report and
mutation update. J Dent Child (Chic). 2010;77:36-41.
tissue, whereas the cuspids and premolars Prabhu SR, Daftary DK, Dholakia HM. Hyperkeratosis
are spared or involved only to a minimal palmoplantaris with periodontosis (Papillon-Lefevre
degree. Not all instances of childhood-onset syndrome): report of three cases; two occurring in sib-
periodontal disease manifest this pattern. lings. J Oral Maxillofac Surg. 1979;37:262.
Watanabe K. Prepubertal periodontitis: a review of diag-
When this pattern of bone loss is accom- nostic criteria, pathogenesis, and differential diagnosis.
panied by hyperkeratosis of the palms and J Periodontol Res. 1990;25:31.
soles, the condition is termed the Papillon-
Lefevre syndrome. The disease has an
autosomal recessive genetic pattern with a VANISHING BONE DISEASE
mutation in cathepsin C. (MASSIVE OSTEOLYSIS)
Figure 9-30
MICROSCOPIC FEATURES
Biopsy specimens of pocket tissue show Age: Teenagers and young adults
granulation tissue with nonspecific chronic Sex: No predilection
inflammation composed chiefly of lympho- CLINICAL AND RADIOGRAPHIC
cytes and plasma cells. FEATURES
DIFFERENTIAL DIAGNOSIS
Vanishing bone disease (also known as
massive osteolysis, phantom bone disease,
Periodontitis, diabetic periodontitis, cyclic and Gorham’s disease) is one of the most
neutropenia, Langerhans cell histiocyto- enigmatic processes in medicine and den-
sis, and leukemia must all be considered in tistry. Entire bones, for no apparent rea-
the differential diagnosis. Onset at a young son, undergo massive resorption until the
age and classic incisor-molar alveolar bone entire osseous membrane has completely
loss in conjunction with nonspecific chronic disappeared radiographically, grossly, and
inflammation as evidenced microscopically histologically. Virtually any bone may be
lead to a diagnosis of periodontosis. affected by this idiopathic resorptive pro-
cess, including the jaws. Symptoms are lack-
TREATMENT ing until resorption proceeds to the extent
The dental prognosis is poor. Teeth that pathologic fracture becomes a compli-
lose periodontal support despite efforts cation. Normal osseous tissues are replaced
directed toward plaque control. The teeth by fibrous connective tissue. The process
involved in alveolar bone degeneration pursues a protracted course, with disap-
should be maintained without resorting to pearance of the affected bone after many
heroic surgical procedures; when they are years. Radiographically, the lesions begin
no longer functional, extraction becomes as localized, ill-defined osteoporotic foci,
necessary. Metronidazol helps to stop which coalesce to yield massive zones of
progression. osteolysis with noncorticated borders. The
PMPH_Eversole_Chapter-09.indd 402 1/20/2011 2:58:00 PM
Radiolucent Lesions of the Jaws 403
FIGURE 9-30
Widespread alveolar bone
loss in the absence of tumor
or any identifiable etiologic
agent, representing massive
osteolysis.
loss of bone may begin at the alveolar crest, tive process. Because the etiology remains
with an appearance resembling progres- unknown, no successful treatment has been
sive advanced periodontitis. Often, more realized.
than one jaw quadrant is involved. Eventu-
ally, the entire mandible, hemimandible, or
maxilla may virtually disappear from view Additional Reading
radiographically. Serum calcium and phos- Cherrick HM, King OH, Jr, Dorsey JN, Jr. Massive
phorus levels are within normal limits. osteolysis (disappearing bone, phantom bone, acute
absorption of bone) of the mandible and maxilla.
MICROSCOPIC FEATURES J Oral Pathol Med. 1972;27:67.
El-Mofty S. Atrophy of the mandible (massive
Normal osseous trabeculae are present and osteolysis). Oral Surg Oral Med Oral Pathol.
show foci of resorption. In the resorbed 1971;31:690.
zones, fibrous tissue predominates with pro- Gorham LW, Stout AP. Massive osteolysis (acute sponta-
neous absorption of bone, phantom bone, disappear-
liferation of capillaries. A chronic inflamma- ing bone). J Bone Joint Surg [Am]. 1955;37:985.
tory cell infiltrate is often encountered. Pro- Murphy JB, Doku HC, Carter BL. Massive osteoly-
nounced osteoclastic activity is not a feature. sis: phantom bone disease. J Oral Maxillofac Surg.
1978;36:318.
Raghuveer HP, Jayalekshmy R. Gorham’s massive osteol-
DIFFERENTIAL DIAGNOSIS
ysis of the mandible—a progressive radiographic pre-
The radiographic appearance of massive sentation. Dentomaxillofac Radiol. 2009;38: 292-295.
osteolysis may resemble that seen in perio-
dontitis, Langerhans disease, malignancy,
and diabetes. The diagnosis is generally LANGERHANS CELL
made when cultures are negative and the HISTIOCYTOSIS
aforementioned entities are excluded on the Figure 9-31
basis of histologic examination. Thus, the
diagnosis rests on the process of exclusion. Age: Children and teenagers
Sex: Male predilection
Often, long-term follow-up is required before
a definitive diagnosis can be rendered. CLINICAL AND RADIOGRAPHIC
FEATURES
TREATMENT Langerhans cell histiocytosis is a disease
Bone grafts are usually unsuccessful, as process with a wide spectrum of severity.
they too become involved in the resorp- The basic pathologic process is a neoplasia-
PMPH_Eversole_Chapter-09.indd 403 1/20/2011 2:58:00 PM
404 Chapter 9
like disorder whereby normal tissues are cally, the lesions of histiocytosis appear as
infiltrated with Langerhans histiocytes, well-demarcated, yet noncorticated, radio-
hence the synonymous term Langerhans lucencies. The lesions often simulate peri-
cell granulomatosis. The younger the odontal disease. Multifocal zones of verti-
patient, the worse the prognosis. Infants cal alveolar bone loss are encountered and
show soft tissue histiocytic infiltrates of the may actually completely engulf the apices,
skin, spleen, liver, and lymph nodes. This giving the impression that the involved
form, known as acute disseminated histio- teeth are floating in space.
cytosis or Letterer-Siwe disease, is usually
fatal. Older children develop the chronic
MICROSCOPIC FEATURES
disseminated form, also known as Hand-
Schuller-Christian disease. Histiocytic Bone defects contain diffuse sheets of histio-
infiltration of the pituitary and retro-orbital cytes that possess voluminous amphophilic
soft tissue leads to diabetes insipidus and cytoplasm with an oval or kidney-shaped
exophthalmos, respectively. Intraosseous vesicular nucleus. Being Langerhans cells,
lesions and otitis media are also features of these histiocytes are positive for CD1 and
the chronic disseminated form. The chronic S-100 protein markers. Multinucleated giant
limited form is more common among teen- cells are often seen; in the chronic forms,
agers and young adults, is restricted to foam cells may predominate, yielding a
bone, and is termed eosinophilic granuloma lipogranulomatous picture. Scattered or
of bone. Pulmonary infiltration by histio- clustered eosinophils are more numerous
cytes may occur in all three forms and can in the chronic limited form (eosinophilic
be detected radiographically. Radiographi- granuloma).
FIGURE 9-31
Localized vertical alveolar
bone loss in Langerhans
cell histiocytosis, some
with “tooth floating in
space” appearance.
PMPH_Eversole_Chapter-09.indd 404 1/20/2011 2:58:02 PM
Radiolucent Lesions of the Jaws 405
DIFFERENTIAL DIAGNOSIS Stewart JC, Regezi JA, Lloyd RV, McClatchey KD.
Immunohistochemical study of idiopathic histiocytosis
When histiocytosis manifests multifocal of the mandible and maxilla. Oral Surg Oral Med Oral
zones of periodontal destruction, periodon- Pathol. 1986;61:48.
titis, diabetic periodontitis, cyclic neutro-
penia, and leukemia must be considered.
Signs and symptoms of extraosseous dis- CYCLIC NEUTROPENIA
ease are encountered in the disseminated Figure 9-32
forms, and biopsy discloses the character-
istic microscopy of histiocytosis. When the Age: Teenagers and young adults
diagnosis is rendered, a skeletal survey and Sex: No predilection
physical examination should be performed CLINICAL AND RADIOGRAPHIC
to determine the extent of disease. FEATURES
Cyclic neutropenia is a blood dyscrasia in
TREATMENT
which a selective diminution in neutrophilic
Teeth may be saved if the osseous lesions granulocytes develops on a predictably
are not too extensive. When alveolar bone is recurrent periodic basis. The neutrophils
resorbed significantly, it will not regenerate disappear from the circulation as a result
after treatment. Treatment of choice is curet- of a bone marrow maturation defect of
tage and Vinca alkaloid chemotherapy. unknown etiology, although in one third of
cases, it appears to be inherited as an auto-
somal dominant trait. The leukocyte count
Additional Reading drops for 5 to 7 days at regular 21-day inter-
Chase DC, Eversole LR, Hall HD. Histiocytosis X with vals. In the interim, the white and differen-
jaw involvement. J Oral Maxillofac Surg. 1974;32:494. tial counts are virtually normal; however,
dos Anjos Pontual ML, da Silveira MM, de Assis Silva neutrophils are rarely present in numbers
Lima F, Filho FW. Eosinophilic granuloma in the exceeding 50% of the total leukocyte pop-
jaws. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 2007;104:e47-e51.
ulation. During neutropenia, ragged oral
Hartmen KS. Histiocytosis X: a review of 114 cases with aphthous-like ulcerations appear; when the
oral involvement. Oral Surg Oral Med Oral Pathol. white count returns to normal, the ulcers
1980;49:38. heal. During the granulocytopenic phase,
Sedano HO, Cernea P, Hosxe G, Gorlin RJ. Histiocytosis
X. Clinical, radiologic, and histologic findings with spe-
malaise, fever, and cervical lymphadenopa-
cial attention to oral manifestations. Oral Surg Oral thy occur. The other chief oral manifestation
Med Oral Pathol. 1969;27:760. is premature, or precocious, alveolar bone
FIGURE 9-32
Horizontal alveolar bone
loss in cyclic neutropenia.
PMPH_Eversole_Chapter-09.indd 405 1/20/2011 2:58:07 PM
406 Chapter 9
loss with classic clinical manifestations of LEUKEMIA
periodontitis. Figure 9-33
MICROSCOPIC FEATURES Age: Childhood and adult forms
Curettage from periodontal pockets shows Sex: No predilection
granulation tissue with a mononuclear CLINICAL AND RADIOGRAPHIC
inflammatory cell infiltrate. The oral ulcers FEATURES
are notably devoid of neutrophils. Leukemias are classified according to the
leukocyte blast cell of origin. The more
DIFFERENTIAL DIAGNOSIS
common forms are myelogenous (granulo-
Precocious periodontal bone loss may be cyte precursors) and lymphocytic. Further-
seen in diabetic periodontitis, periodon- more, both acute and chronic forms exist.
tosis, Langerhans disease, and leukemia The former pursues a rapid, often fatal,
as well as in cyclic neutropenia. Regularly course; however, cures can be achieved
recurring ulcerations of the mucosa should with combination drug chemotherapy. The
arouse suspicion. The diagnosis can be chief clinical signs and symptoms include
secured by obtaining complete blood counts malaise, low-grade fever, pallor, and dysp-
every 4 days for a 3-week period in order to nea. Gingival hemorrhage, petechiae, and
demonstrate the neutropenic phase. ecchymoses develop when the platelet
count drops subsequent to bone marrow
TREATMENT replacement by malignant leukocytes. Gin-
Efforts to control plaque, to institute home- gival enlargement is a feature, with boggy
care oral hygiene, and to palliate the oral erythematous swellings beginning in the
ulcerations with an antihistamine/Kao- interdental papilla area; these oral manifes-
pectate oral rinse should be made. The tations do not often occur, however. Never-
patient should be referred to a hematolo- theless, it is important to recognize the fact
gist to manage the blood dyscrasia and that leukemic infiltration may involve the
watch for complications such as recurrent periodontium, producing a radiographic
infection. Recombinant granulocyte stim- picture reminiscent of periodontal disease
ulating factor may prove to be of thera- with vertical pocket formation.
peutic value.
MICROSCOPIC FEATURES
Additional Reading Curettage or an incisional biopsy discloses
the presence of diffuse sheets of poorly dif-
Dale DC, Hammond WP. Cyclic neutropenia: a clinical ferentiated leukocyte blast cells. Regardless
review. Blood Rev. 1988;2:178. of whether the leukemia is myeloid, eryth-
Gates GF. Chronic neutropenia presenting with
oral lesions. Oral Surg Oral Med Oral Pathol.
roid, or lymphoid, the blast cells are mono-
1969;27:563. nuclear and usually monomorphic. Zones
Gorlin RJ, Chaudhry AP. The oral manifestations of of necrosis may be encountered.
cyclic (periodic) neutropenia. Arch Dermatol.
1960;82:344.
Rylander H, Ericsson I. Manifestations and treatment of
DIFFERENTIAL DIAGNOSIS
periodontal disease in a patient suffering from cyclic Radiographic evidence of alveolar bone
neutropenia. J Clin Periodontol. 1981;8:77.
Zaromb A, Chamberlain D, Schoor R, Almas K, Blei F.
loss in leukemia may be identical to that
Periodontitis as a manifestation of chronic benign neu- seen in nonspecific periodontitis, diabetic
tropenia. J Periodontol. 2006;77:1921-1926. periodontitis, periodontosis, histiocytosis,
PMPH_Eversole_Chapter-09.indd 406 1/20/2011 2:58:09 PM
Radiolucent Lesions of the Jaws 407
FIGURE 9-33
Leukemic infiltrate with advanced periodontal bone loss in the anterior mandible. Hyperplastic gingivitis
is also a feature.
or cyclic neutropenia. Other symptoms, Păunică SC, Dumitriu A, Mogoş M, Georgescu O, Mogoş
such as fatigue, malaise, petechia, ecchy- I. The evaluation of the periodontium in patients with
leukemia using thermographic imaging. Hematology.
mosis, and gingival hemorrhage, warrant 2009;14:341-346.
work-up for leukemia. A complete blood
count should be obtained.
TREATMENT
Widened Periodontal
Ligament Space
Chemotherapeutic control should be insti-
tuted as soon as possible by an oncologist PERIODONTIC/ENDODONTIC
or hematologist. Oral lesions respond to INFLAMMATION
systemic medications used for control of
Figure 9-34
leukemia.
Age: Adults
Sex: No predilection
Additional Reading CLINICAL AND RADIOGRAPHIC
FEATURES
Appel BN, Miggantz RJ. Acute nonlymphocytic leuke-
mia, monocytic variant. Report of a case. J Periodontol. Infection of periodontal origin may spread
1988;59:464. down the entire periodontal ligament, pro-
Burket LW. A histopathologic explanation for the oral
lesions in acute leukemias. Am J Orthod Dentofacial
ducing a localized widening of the peri-
Orthop. 1944;30:516. odontal ligament space. This may be cir-
Curtis AB. Childhood leukemias: Osseous changes in cumradicular or localized to only the mesial
jaws on panoramic dental radiographs. J Am Dent or only the distal root region. The periodon-
Assoc. 1971;83:844.
Michand M, Baehner RL, Bixler D, Kafrawy AH. Oral
tal defect can be probed and often induces
manifestations of acute leukemia in children. J Am exudation through the gingival sulcus. The
Dent Assoc. 1977;95:1145. infection can progress through lateral acces-
PMPH_Eversole_Chapter-09.indd 407 1/20/2011 2:58:09 PM
408 Chapter 9
FIGURE 9-34
Widened periodontal
ligament space involving
nonvital lateral incisor
representing combined
periodontic-endodontic
inflammation.
sory canals or proceed in retrograde fashion ally allows for a clinical diagnosis. More
through the apical foramen to initiate pulp advanced cases may radiographically
necrosis. Alternatively, pulpal infection resemble histiocytosis. When no exudate
may progress both apically and laterally via appears after probing or when the defect
accessory canals to involve the lateral peri- resists insertion of the periodontal probe, a
odontal ligament, and the infection may biopsy should be procured.
spread coronally with sulcular drainage.
TREATMENT
MICROSCOPIC FEATURES Advanced cases with pulp necrosis and
Tissue removed from the widened peri- excessive mobility usually require extrac-
odontal ligament is granulation tissue, usu- tion. In some instances, endodontic therapy
ally exhibiting a subacute inflammatory with splinting to adjacent teeth is success-
cell infiltrate. ful, thus avoiding extraction.
DIFFERENTIAL DIAGNOSIS
The localized widening of the periodontal
Additional Reading
ligament space in endodontic/periodontic Reeh ES, ElDeeb M. Rapid furcation involvement asso-
ciated with a devitalizing mandibular first molar. A case
infection may radiographically resemble report. Oral Surg Oral Med Oral Pathol. 1990;69:95.
incipient osteogenic sarcoma. Periodon- Rubach WC, Mitchell DF. Periodontal disease, accessory
tal probing and pulp vitality testing usu- canals, and pulp pathosis. J Periodontol. 1965;36:34.
PMPH_Eversole_Chapter-09.indd 408 1/20/2011 2:58:16 PM
Radiolucent Lesions of the Jaws 409
Seltzer S, Bender IB, Ziontz M. The interrelationship disease progresses, virtually all body sur-
of pulp and periodontal disease. Oral Surg Oral Med faces become involved. The periodontium is
Oral Pathol. 1963;16:1474.
Sunitha VR, Emmadi P, Namasivayam A, Thyegarajan affected in a limited number of instances.
R, Rajaraman V. The periodontal—endodontic The crestal alveolar bone is not compro-
continuum: A review. J Conserv Dent. 2008;11(2): mised; rather, a uniform generalized wid-
54-62. ening of the periodontal ligament space is
Whyman RA. Endodontic-periodontic lesions. N Z Dent
J. 1988;84:74.
observed. A pronounced notching of the
inferior border of the mandible just anterior
to the angle region is also a feature in scle-
roderma and resorption of the mandibular
SCLERODERMA condyle has been reported to occur.
Figure 9-35
MICROSCOPIC FEATURES
Age: Middle-aged adults
The periodontal ligament contains dense
Sex: Female predilection
collagen fibers similar to those seen in the
CLINICAL AND RADIOGRAPHIC normal ligament.
FEATURES
The systemic form of scleroderma is a col- DIFFERENTIAL DIAGNOSIS
lagen-immune disease affecting fibrous Uniform widening of the periodontal liga-
tissues of the dermis, submucosa of the ment space is seen when a tooth is in severe
gastrointestinal tract, and various internal traumatic occlusion or partially avulsed
organs. The skin becomes stiff and board- or, rarely, in periodontitis. If the condi-
like, losing its flexibility. This change is tion is localized to one or two teeth, early
most obvious on the face, which becomes osteogenic sarcoma must be considered in
wrinkle-free and expressionless. As the the differential diagnosis. When uniform
FIGURE 9-35
Generalized widening
of periodontal ligament
spaces in scleroderma.
Raynaud vasoconstriction
of fingers.
PMPH_Eversole_Chapter-09.indd 409 1/20/2011 2:58:27 PM
410 Chapter 9
widening involves the entire dentition, the MICROSCOPIC FEATURES
classic skin changes of scleroderma are Osteogenic sarcoma may be predominantly
invariably encountered. fibroblastic, chondroblastic, or osteoblastic.
The cellular elements display hypercellular-
TREATMENT
ity, hyperchromatism, and pleomorphism.
The involved teeth are generally secure Osteoid is elaborated in irregular fashion
and not prone to exfoliation. The disease is and is profusely endowed with lacunar
treated with steroids or immunosuppres- spaces containing pleomorphic nuclei. The
sive drugs and should be managed by a trabeculae are similarly rimmed by angu-
dermatologist. lar malignant osteoblasts. When cartilage
is present, lacunae are numerous and often
Additional Reading encase multiple nuclei.
Caplan HI, Benny RA. Total osteolysis of the mandibu- DIFFERENTIAL DIAGNOSIS
lar condyle in progressive systemic sclerosis. Oral Surg
Oral Med Oral Pathol. 1978;46:362. Localized widening of the periodontal liga-
Robbins JW, Craig RM, Jr, Correll RW. Symmetrical ment space should always arouse suspicion
widening of the periodontal ligament space in a patient of osteogenic sarcoma. Similar changes are
with multiple systemic problems. J Am Dent Assoc. seen in localized traumatic occlusion and
1986;113:307.
Scully C. Aspects of human disease: 46. Scleroderma. traumatically avulsed teeth. When clinical
Dent Update. 2010;37(3):197. features of these latter two conditions are
Stafne EC, Austin LT. Characteristic dental findings in not apparent, biopsy is indicated.
acrosclerosis and diffuse scleroderma. Am J Orthod
Dentofacial Orthop. 1944;30:25.
White SC, Frey NW, Blaschke DD, et al. Oral radiograph- TREATMENT
ic changes in patients with progressive systemic sclero- Osteogenic sarcoma requires resection of
sis (scleroderma). J Am Dent Assoc. 1977;94:1178.
the jaw, hemimandibulectomy, or partial
maxillectomy, and should be managed by a
OSTEOGENIC SARCOMA head and neck tumor surgeon. Metastases
Figure 9-36 are usually hematogenous; nodal spread is
uncommon. The 5-year survival is less than
Age: Adults 35%.
Sex: Slight male predilection
CLINICAL AND RADIOGRAPHIC
FEATURES
Additional Reading
Azizi T, Motamedi MH, Jafari SM. Gnathic osteosarco-
Primary osteogenic sarcoma of the jaws
mas: a 10-year multi-center demographic study. Indian
may manifest a variety of radiographic J Cancer. 2009;46:231-233.
alterations ranging from radiolucent to Forteza G, Colmenero B, Lopez-Barea F. Osteogenic
radiopaque. It is included in this section sarcoma of the mandible and maxilla. Oral Surg Oral
because of its tendency to manifest local- Med Oral Pathol. 1986;62:179.
Gardner DG, Mills DM. The widened periodontal liga-
ized symmetric widening of the periodontal ment of osteosarcoma of the jaws. Oral Surg Oral Med
ligament space when the lesion is incipient. Oral Pathol. 1976;41:652.
At this stage, mild cortical expansion may Garrington GE, Scofield HH, Cornyn J, Hooker SP.
be observed. The medullary bone adjacent Osteosarcoma of the jaws. Analysis of 56 cases. Cancer.
1967;20(3):377-391.
to the widened ligament spaces may be nor- Kragh LV, Dahlin DC, Erich JB. Osteogenic
mal or show a ragged moth-eaten pattern. sarcoma of the jaws and facial bones. Am J Surg.
Usually, patients do not complain of pain. 1958;96:496.
PMPH_Eversole_Chapter-09.indd 410 1/20/2011 2:58:41 PM
Radiolucent Lesions of the Jaws 411
FIGURE 9-36
Localized symmetric wid-
ening of the periodontal
ligament space in a patient
with incipient osteogenic
sarcoma.
impacted tooth. The pericoronal radiolu-
Pericoronal Radiolucencies cency is typically well demarcated and
may be extensive. The third molars and
DENTIGEROUS CYST cuspids are most frequently involved. Cor-
Figure 9-37 tical expansion and multilocularity may
occasionally occur with simple dentiger-
Age: Young adults
ous cysts; however, these features are more
Sex: No predilection
often indicative of neoplastic transforma-
CLINICAL AND RADIOGRAPHIC tion or keratinizing metaplasia within the
FEATURES cyst lining.
The follicular or dentigerous cyst is the
most common type of developmental
MICROSCOPIC FEATURES
odontogenic cyst. By definition, it is a cys-
tic lesion derived from the reduced enamel A lining composed of eosinophilic colum-
epithelium encompassing the crown of an nar (reduced enamel) epithelium is encoun-
PMPH_Eversole_Chapter-09.indd 411 1/20/2011 2:58:41 PM
412 Chapter 9
FIGURE 9-37
Dentigerous cysts.
tered in dentigerous cyst removed from from the epithelial lining, all dentigerous
younger patients. In older individuals, the cysts should be removed and examined
lining is composed of stratified squamous microscopically.
epithelium, which is devoid of a cornified
layer and fails to display significant rete- TREATMENT
ridge formation. Mucous metaplasia, surface The impacted tooth should be removed if it
cilia, and hyaline bodies are often present cannot be orthodontically erupted, and the
within the lining epithelium. The fibrous cyst should be thoroughly curetted.
wall may be devoid of inflammation or may
possess a chronic inflammatory cell infil-
trate. Varying numbers of oval or elongated
Additional Reading
odontogenic cell rests are usually seen, and Dachi SF, Howell FV. A survey of 3,874 routine full-
cholesterol clefts may occupy focal regions mouth radiographs. II. A study of impacted teeth. Oral
Surg Oral Med Oral Pathol. 1961;14:1165.
of the fibrous wall.
Gorlin RJ. Potentialities of oral epithelium manifest by
mandibular dentigerous cysts. Oral Surg Oral Med
Oral Pathol. 1957;10:271.
DIFFERENTIAL DIAGNOSIS
Main DW. Follicular cysts of mandibular third molar
A nonexpansile pericoronal radiolucency is teeth: radiological evaluation of enlargement.
Dentomaxillofac Radiol. 1989;18:156.
usually a simple dentigerous cyst. Because
Mourshed F. A roentgenographic study of dentigerous
many odontogenic tumors, keratocysts, cysts. I. Incidence in a population sample. Oral Surg
and even malignant neoplasms can arise Oral Med Oral Pathol. 1964;18:47.
PMPH_Eversole_Chapter-09.indd 412 1/20/2011 2:58:50 PM
Radiolucent Lesions of the Jaws 413
Zhang LL, Yang R, Zhang L, Li W, Macdonald-Jankowski to produce cortical expansion with notice-
D, Poh CF. Dentigerous cyst: a retrospective clini- able deformity. The impacted tooth is often
copathological analysis of 2082 dentigerous cysts in
British Columbia, Canada. Int J Oral Maxillofac Surg. displaced to the outer margin of the radio-
2010;39(9):878-882. lucency, and root development is usually
incomplete. The mandibular third molar
area is the most common location. Large
ODONTOGENIC KERATOCYST cysts tend to be multilocular. If multiple
Figure 9-38 pericoronal radiolucencies are present and
are microscopically keratinizing, the nevoid
Age: Adults basal cell carcinoma syndrome should be
Sex: No predilection considered. Odontogenic keratocysts both
CLINICAL AND RADIOGRAPHIC solitary and syndrome associated are asso-
FEATURES ciated with PTCH1 gene mutations.
Because of its protean radiographic mani-
festations, the odontogenic keratocyst, MICROSCOPIC FEATURES
also termed keratocystic odontogenic tumor, The lining epithelium is attenuated, dis-
is included under many categories in this playing a corrugated parakeratin or keratin
chapter. Perhaps its most common radio- surface, and the basal cell layer is polarized
graphic presentation is that of a pericoronal without manifestations of rete-ridge forma-
radiolucency. The cyst is often encoun- tion. The fibrous wall rarely contains signif-
tered when it has reached a size sufficient icant inflammation. Epithelial cell rests are
FIGURE 9-38
Odontogenic keratocyst
appearing as a pericoronal
radiolucency.
PMPH_Eversole_Chapter-09.indd 413 1/20/2011 2:59:36 PM
414 Chapter 9
present within the fibrous wall, and satellite UNICYSTIC AMELOBLASTOMA
or daughter cysts are frequently observed. Figure 9-40
DIFFERENTIAL DIAGNOSIS Age: Young adults
Expansile or loculated pericoronal radio- Sex: No predilection
lucencies typical of keratocysts are also CLINICAL AND RADIOGRAPHIC
featured when neoplastic transformation FEATURES
develops in a dentigerous cyst. Biopsy is
Ameloblastomas may arise from any source
required to differentiate among the various
of odontogenic epithelium. Approximately
lesions presenting this radiographic pattern.
20% are associated with the crown of an
TREATMENT impacted tooth, usually a mandibular third
molar. Although invasive ameloblastomas
Thorough curettage should be instituted, usually affect middle-aged adults, those
along with extraction. Neighboring teeth that arise from the linings of dentigerous
may need to be sacrificed if significant root cysts are typically encountered during the
resorption has developed. Odontogenic second or third decades. Whereas the peri-
keratocysts are aggressive lesions and may coronal radiolucency may be small, most
be difficult to eradicate. Recurrence rates in cystogenic ameloblastomas exhibit a clas-
excess of 30% have been recorded. Recur- sic radiographic pattern characterized by
rent lesions may require en bloc resection. a large unilocular radiolucency involving
Cysts that are characterized histologically the entire ramus, extending to the coro-
by orthokeratin are termed Orthokeratotic noid process. They are most frequently
Odontogenic Cyst and show a lower rate of associated with an impacted, displaced
recurrence. third molar showing incomplete root for-
mation. Occasionally, these tumors are
Additional Reading multilocular or evince scalloped margins.
When expansion occurs, clinically observ-
Brannon RB. The odontogenic keratocyst. A clinico- able deformity or facial asymmetry may be
pathologic study of 312 cases. Part I. Clinical features. apparent. Pain and paresthesia are gener-
Oral Surg Oral Med Oral Pathol. 1976;42:54. ally not evident.
Madras J, Lapointe H. Keratocystic odontogenic tumour:
reclassification of the odontogenic keratocyst from cyst
MICROSCOPIC FEATURES
to tumour. Tex Dent J. 2008;125:446-454.
Payne TF. An analysis of the clinical and histopathologic Most pericoronal ameloblastomas arise
parameters of the odontogenic keratocyst. Oral Surg
from the odontogenic epithelial lining of
Oral Med Oral Pathol. 1972;33:538.
Pindborg JJ, Hansen J. Studies on odontogenic cyst epi- dentigerous cysts. The earliest evidence of
thelium. II. Clinical and roentgenographic aspects of transformation is characterized by polar-
odontogenic keratocysts. Acta Pathol Microbiol Scand. ization of basal cells, superior displacement
1963;58:283. of nuclei, hyperchromatism, and cytoplas-
Wright JM. The odontogenic keratocyst, orthokera-
tinized variant. Oral Surg Oral Med Oral Pathol. mic vacuolization. Slender tube-like rete
1981;51:609. ridges extend into the fibrous wall, and the
overlying spinous layer resembles stellate
reticulum. When the bulk of the tumor pro-
GLANDULAR ODONTOGENIC trudes luminally, the designation luminal
CYST ameloblastoma is used; when the majority of
Figure 9-39 tumor cells invade the fibrous wall, mural
ameloblastoma is the designation. The term
Discussed under Multilocular Radiolucencies unicystic ameloblastoma has been applied to
PMPH_Eversole_Chapter-09.indd 414 1/20/2011 2:59:45 PM
Radiolucent Lesions of the Jaws 415
FIGURE 9-39
Pericoronal glandular odon-
togenic cysts.
FIGURE 9-40
Unicystic ameloblastomas
with inferiorly displaced
molars.
PMPH_Eversole_Chapter-09.indd 415 1/20/2011 2:59:46 PM
416 Chapter 9
those lesions in which ameloblasts line the rence. Maxillary tumors that have perfo-
entire cyst. The later stages of oncogenesis rated the antrum are extremely difficult
manifest typical histomorphologic features to control with curettage. A partial max-
of ameloblastoma. illary resection is recommended in these
instances.
DIFFERENTIAL DIAGNOSIS
Ameloblastomas arising from dentigerous
cysts are radiographically indistinguish-
Additional Reading
able from odontogenic keratocysts, other Eversole LR, Leider AS, Strub D. Radiographic charac-
teristics of cystogenic ameloblastoma. Oral Surg Oral
odontogenic tumors included in this section, Med Oral Pathol. 1984;57:572.
and carcinoma arising in a dentigerous cyst. Kahn MA. Ameloblastoma in young persons: a clinico-
Biopsy is required for a definitive diagnosis. pathologic analysis and etiologic investigation. Oral
Surg Oral Med Oral Pathol. 1989;67:706.
TREATMENT Pogrel MA, Montes DM. Is there a role for enucleation
in the management of ameloblastoma? Int J Oral
Luminal ameloblastomas do not invade Maxillofac Surg. 2009;38:807-812.
the encasing bony crypt. The initial ther- Robinson L, Martinez MG. Unicystic ameloblastoma. A
prognostically distinct entity. Cancer. 1977;40:2278.
apy should be curettage when lesions Vickers RA, Gorlin RJ. Ameloblastoma: delineation of
arise in the mandible. Intramural spread early histopathologic features of neoplasia. Cancer.
of tumor will increase the odds for recur- 1970;26:699.
FIG 9-41
Calcifying epithelial odon-
togenic tumor.
PMPH_Eversole_Chapter-09.indd 416 1/20/2011 3:00:02 PM
Radiolucent Lesions of the Jaws 417
CALCIFYING EPITHELIAL DIFFERENTIAL DIAGNOSIS
ODONTOGENIC TUMOR Calcifying epithelial odontogenic tumors
Figure 9-41 with irregular, poorly demarcated expan-
sile borders may give the radiographic
Age: Young and middle-aged adults appearance of osteogenic and chondrogenic
Sex: No predilection sarcoma or osteolytic metastatic tumor.
CLINICAL AND RADIOGRAPHIC Identification of an impacted tooth in asso-
FEATURES ciation with such a lesion is more sugges-
The calcifying epithelial odontogenic (Pin- tive of odontogenic neoplasm. More clearly
dborg) tumor is rare: when it occurs, it is usu- demarcated tumors must, by biopsy, be dif-
ally found in association with an impacted ferentiated from keratocyst, ameloblastoma,
tooth. Because the tumor contains foci of mixed odontogenic tumor, and dentigerous
calcification, it may show radiopaque flecks, cyst with carcinomatous transformation.
powder-like opacities, or irregular confluent
calcific globules. Many tumors, however, TREATMENT
are predominantly or entirely radiolucent. The Pindborg tumor is aggressive and
Cortical expansion is a regular feature, and requires total or en bloc resection. Simple
the radiolucency may be traversed by thin enucleation or curettage is generally inad-
opaque septae. The margins are generally equate, and the tumor recurs.
well demarcated, although radiographic
zones of poor margination are encountered
in which lesion tends to blend imperceptibly Additional Reading
into the adjacent normal medullary bone.
Franklin CD, Pindborg JJ. The calcifying epithelial
As with odontogenic keratocysts, there are odontogenic tumor. Oral Surg Oral Med Oral Pathol.
reports of PTCH 1 gene mutations in CEOT. 1976;42:753.
Krolls SO, Pindborg JJ. Calcifying epithelial odonto-
MICROSCOPIC FEATURES genic tumor. A survey of 23 cases and discussion of
histomorphologic variations. Arch Pathol Lab Med.
The neoplastic epithelial cells grow in a vari- 1974;98:206.
ety of patterns, ranging from diffuse sheet- Peacock ZS, Cox D, Schmidt BL. Involvement of PTCH1
like arrangements to islands and invasive mutations in the calcifying epithelial odontogenic
tumor. Oral Oncol. 2010;46:387-392.
cords. The individual cells bear little resem- Pindborg JJ. The calcifying epithelial odontogenic tumor;
blance to components of the tooth germ. review of literature and report of an extra-osseous
They are polygonal, eosinophilic, and con- case. Acta Odontol Scand. 1966;24:419.
tain large nuclei that are often hyperchro- Sadeghi EM, Hopper TL. Calcifying epithelial odonto-
genic tumor. J Oral Maxillofac Surg. 1982;40:225.
matic; significant pleomorphism may be
present despite the benignity of the tumor. A
clear-cell variant exists and is distinguished ODONTOGENIC
by sheets and islands of tumor cells that are
devoid of stainable cytoplasm. Eosinophilic
ADENOMATOID TUMOR
hyaline is associated with epithelium, and Figure 9-42
stains are positive for amyloid. Both dys-
Age: Teenagers
trophic and concentrically laminated Leise- Sex: Female predilection
gang calcifications are encountered. The
radiolucent lesions contain less calcification CLINICAL AND RADIOGRAPHIC
FEATURES
than the tumors with opacities. Other odon-
togenic tumor elements such as adenoma- Although the odontogenic adenomatoid
toid odontogenic tumor may coexist. tumor may arise between teeth, more than
PMPH_Eversole_Chapter-09.indd 417 1/20/2011 3:00:20 PM
418 Chapter 9
FIGURE 9-42
Impacted teeth with expansile well-circumscribed pericoronal radiolucencies, representing odontogenic
adenomatoid tumor.
75% are associated with the crown of an uloma-like configuration. Admixed with
impacted tooth. The maxilla is more often the spindle cell component are oval nests of
affected, with a pericoronal radiolucency columnar epithelial cells with ameloblastic
enveloping the crown of a cuspid. The radi- cytologic features. These cells are oriented
olucency often contains radiopaque flecks about an eosinophilic secretion product and
because portions of the tumor can calcify. in classic examples assume ductal patterns
Whereas simple dentigerous cysts emanate with a central lumen. Hyaline eosinophilic
from the cervix of the tooth, the odontogenic elements are also present, and in many
adenomatoid tumor often manifest a peri- areas, these cell products undergo a dystro-
coronal radiolucency that almost completely phic type of calcification. Rarely, melanin
engulfs the entire tooth, including the root. pigment may be present. Other coexistent
It is almost invariably unilocular and is well odontogenic tumor histologic patterns are
demarcated or corticated. Painless cortical occasionally encountered.
expansion is often the presenting sign.
DIFFERENTIAL DIAGNOSIS
MICROSCOPIC FEATURES Odontogenic adenomatoid tumors seen as
The tumor is surrounded by a dense fibrous pericoronal radiolucencies must be differen-
capsule. The epithelial neoplastic tissue tiated from ordinary dentigerous cysts, ker-
often assumes the appearance of a cyst with atocysts, and other odontogenic tumors that
luminal proliferation. The epithelial cells may arise from cyst lining. The young age,
are elongated and arrange themselves in anterior location, and tendency for the radi-
swirls. This growth pattern yields a gran- olucency to envelop the lower root region of
PMPH_Eversole_Chapter-09.indd 418 1/20/2011 3:00:20 PM
Radiolucent Lesions of the Jaws 419
the impacted tooth are highly suggestive of Rick GM. Adenomatoid odontogenic tumor. Oral
odontogenic adenomatoid tumor. Biopsy is Maxillofac Surg ClinNorth Am. 2004;16:333-354.
Siar CH, Nof KH. Adenomatoid odontogenic tumor:
required to obtain a definitive diagnosis. a survey of 44 new cases in Malaysia. Ann Dent.
1986;45:11.
TREATMENT
Extraction with simple enucleation of the
neoplasm is adequate treatment. The tumor AMELOBLASTIC FIBROMA
rarely recurs. Figure 9-43
Age: Children and teenagers
Additional Reading Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Abrams AM, Melrose RJ, Howell FV. FEATURES
Adenoameloblastoma; a clinical pathologic study of
ten new cases. Cancer. 1968;22:175. The mixed odontogenic tumors include
Courtney RM, Kerr DA. The odontogenic adenomatoid ameloblastic fibroma, ameloblastic fibro-
tumor. Oral Surg Oral Med Oral Pathol. 1975;39:424.
Giansanti JS, Someren A, Waldron CA. Odontogenic
dentinoma, ameloblastic fibro-odontoma,
adenomatoid tumor (adenoameloblastoma). Oral Surg and odontoma. Only ameloblastic fibroma
Oral Med Oral Pathol. 1970;30:69. is entirely radiolucent. Although all of the
FIGURE 9-43
Ameloblastic fibroma, a mixed odontogenic tumor appearing as a pericoronal radiolucency surrounding
the crowns of unerupted molars.
PMPH_Eversole_Chapter-09.indd 419 1/20/2011 3:00:25 PM
420 Chapter 9
mixed odontogenic tumors may begin as odontogenic keratocyst, ameloblastoma,
radiolucent lesions, the remainder eventu- Pindborg tumor, or carcinoma arising from
ally develop radiopaque foci. Over 90% of a dentigerous cyst. These latter lesions tend
ameloblastic fibromas are associated with to arise in adults rather than in youngsters.
an impacted tooth and therefore appear Biopsy is required to obtain a definitive
as pericoronal radiolucencies. They may diagnosis.
be unilocular or multilocular, expansile or
nonexpansile, and when initially detected, TREATMENT
they may be large or small. The ameloblastic Enucleation with extraction of the impacted
fibroma grows slowly, yet, if left untreated, it tooth is recommended. The ameloblastic
has a significant growth potential. A micro- fibroma has a limited tendency to recur.
scopically malignant, clinically aggres- Whereas ameloblastic fibrosarcomas are
sive mixed odontogenic tumor has been apparently nonmetastasizing, they are
described as ameloblastic fibrosarcoma. aggressive and recurrence after curettage is
commonplace; furthermore there is a 10 per-
MICROSCOPIC FEATURES cent transformation rate from preexistant
The mixed odontogenic tumors possess benign ameloblastic fibromas. These tumors
both epithelial and mesenchymal tumor ele- should be treated by en bloc resection.
ments, and they mimic the histiogenic dif-
ferentiation of the developing tooth germ.
The least differentiated is the ameloblastic Additional Reading
fibroma. It is composed of a diffuse mass of Chen Y, Wang JM, Li TJ. Ameloblastic fibroma: a review
embryonic mesenchyme, which is traversed of published studies with special reference to its nature
by elongated cords of cuboidal or columnar and biological behavior. Oral Oncol. 2007;43(10):960-
odontogenic epithelial cells that resemble the 969.
Hansen LS, Ficarra G. Mixed odontogenic tumors: an anal-
dental lamina. These cords terminate in bul- ysis of 23 new cases. Head Neck Surg. 1988;10:330.
bous projections that contain a central stellate Leider AS, Nelson JF, Trodahl JN. Ameloblastic fibro-
reticulum. Ameloblastic fibrodentinomas are sarcoma of the jaws. Oral Surg Oral Med Oral Pathol.
similar, yet a dense eosinophilic dentinoid 1972;33:559.
material lies in juxtaposition to the epithelial Regezi JA, Kerr DA, Courtney RM. Odontogenic
tumors: An analysis of 706 cases. J Oral Maxillofac
element. Ameloblastic fibro-odontomas are Surg. 1978;36:771.
further differentiated in that both dentin and Trodahl JN. Ameloblastic fibroma: A survey of cases
enamel matrix are formed and are admixed from the Armed Forces Institute of Pathology. Oral
with zones identical to simple ameloblastic Surg Oral Med Oral Pathol. 1972;33:547.
fibroma. The odontoma contains all elements
of the mature tooth germ yet does not evince
a significant soft tissue cellular overgrowth. ODONTOGENIC FIBROMA-
Ameloblastic fibrosarcoma exhibits a LIKE HAMARTOMA/ENAMEL
sarcomatoid mesenchymal element that is HYPOPLASIA
hypercellular; the individual fibroblasts are Figure 9-44
pleomorphic and hyperchromatic with dis-
cernible mitotic figures. Age: Children
Sex: No predilection
DIFFERENTIAL DIAGNOSIS CLINICAL AND RADIOGRAPHIC
Pericoronal radiolucencies representing FEATURES
ameloblastic fibroma may be radiographi- Occurring primarily among South African
cally identical to simple dentigerous cyst, black children, the odontogenic fibroma/
PMPH_Eversole_Chapter-09.indd 420 1/20/2011 3:00:29 PM
Radiolucent Lesions of the Jaws 421
FIGURE 9-44
Pericoronal radiolucen-
cies in the odontogenic
fibroma/hamartoma syn-
drome.
hamartoma with enamel hypoplasia syn-
drome, also termed enamel dysplasia with Additional Reading
hamartomatous atypical follicular hyper- Feller L, Jadwat Y, Bouckaert M, Buskin A, Raubenheimer
plasia, shows unerupted posterior teeth EJ. Enamel dysplasia with odontogenic fibroma-like
with peridental radiolucencies with bony hamartomas: review of the literature and report of a
expansion. Enamel hypoplasia resembles case. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 2006;101:620-624.
amelogenesis imperfecta and there is gin- Feller L, Kramer B, Raubenheimer EJ, Lemmer J.
gival hyperplasia, pulp calcifications, and Enamel dysplasia with hamartomatous atypical follicu-
hypodontia. lar hyperplasia (EDHFH) syndrome: suggested patho-
genic mechanisms. SADJ. 2008;63:102-105.
Raubenheimer EJ, Noffke CE. Central odontogenic
MICROSCOPIC FEATURES
fibroma-like tumors, hypodontia, and enamel dys-
The microscopic features of the enlarged plasia: review of the literature and report of a case.
peridental follicles mirror that of the soli- Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
2002;94:74-77.
tary odontogenic fibroma with delicate yet
mature collagen fibers and a moderately
cellular monomorphic fibroblast popula- CENTRAL MUCOEPIDERMOID
tion. Linear and oval odontogenic epithelial CARCINOMA
islands are dispersed throughout. Figure 9-45
DIFFERENTIAL DIAGNOSIS Age: Young adults
Enlarged follicles may also be seen in the Sex: No predilection
mucopolysaccharidoses yet histologically CLINICAL AND RADIOGRAPHIC
excessive ground substance is present as FEATURES
glycosaminoglycans without resemblance Mucoepidermoid carcinoma arising cen-
to odontogenic fibroma. trally in bone is rare. When it does, it is
often, but not always, associated with an
TREATMENT impacted tooth. Many instances have been
Extractions and curettage are sometimes reported in which the neoplasm could be
necessary and restorative dental procedure demonstrated to arise from the epithelial
are in order for enamel defective teeth. lining of a dentigerous cyst. The pericoronal
PMPH_Eversole_Chapter-09.indd 421 1/20/2011 3:00:29 PM
422 Chapter 9
radiolucency is well demarcated and tends been reported to arise from the lining of
to be multilocular. The posterior mandible odontogenic cysts.
is the most frequent location. Expansion is
encountered. Pain is generally not a feature, MICROSCOPIC FEATURES
but paresthesia may develop with large Evidence of a dentigerous cyst lining may
lesions. Squamous cell carcinoma has also be encountered or the neoplastic tissue
FIGURE 9-45
Impacted third molar with
associated radiolucency
filling the sinus, represent-
ing a central mucoepider-
moid carcinoma arising
from the lining of a denti-
gerous cyst. (Courtesy of
Dr. H. Cherrick.)
FIGURE 9-46
Multilocular keratocysts.
PMPH_Eversole_Chapter-09.indd 422 1/20/2011 3:00:30 PM
Radiolucent Lesions of the Jaws 423
may be so dominant that demonstrable ori-
gin from a cyst is obscured. The tumors are Multilocular Radiolucencies
usually low grade with cystic spaces lined
by columnar and mucus-secreting cells ODONTOGENIC KERATOCYST
admixed with epidermal spinous cells. Figure 9-46
Squamous cell carcinomas show the same
Age: Adults
features as those derived from surface
Sex: No predilection
mucosa.
CLINICAL AND RADIOGRAPHIC
DIFFERENTIAL DIAGNOSIS FEATURES
Pericoronal radiolucencies representing cen- The odontogenic keratocyst is probably the
tral mucoepidermoid carcinoma may show most common lesion to produce an expan-
radiographic features in common with den- sile multilocular radiolucency of the jaws. It
tigerous cysts, keratocysts, or odontogenic has been included in the differential diag-
neoplasms. The true nature of the disease nosis of pericoronal and interradicular radi-
can be ascertained only after microscopic olucencies because it is commonly seen in
evaluation, although glandular odontogenic those relationships as well. When the kera-
cyst must be considered in the differential tocyst is multilocular, it generally manifests
diagnosis microscopically. clinically obvious expansion. The posterior
body and ramus of the mandible are the
TREATMENT most frequent areas of involvement. The
Central mucoepidermoid carcinoma of the lesion is aggressive and, if left untreated,
jaws is usually of the low-grade variety. it may destroy large areas of bone. Corti-
High-grade tumors in this location are cal expansion is usually seen; however, the
unusual. When the tumor is low grade, cortex may actually be perforated. When
the disease can be cured by resection. multiple keratocysts are detected, exami-
Lymph node dissection should be per- nation of the skin for basal cell nevi and a
formed when clinically palpable nodes are radiograph of the chest or demonstration
encountered. of a bifid rib should be undertaken. Odon-
togenic keratocysts, both solitary and mul-
tiple, involve mutations in the patch gene of
Additional Reading the sonic hedgehog growth pathway. The
orthokeratoic odontogenic cyst shows similar
Eversole LR, Sabes WR, Rovin S. Aggressive growth and features as the odontogenic keratocyst yet
neoplastic potential of odontogenic cysts; with special
reference to central epidermoid and mucoepidermoid
is far less aggressive with lower recurrence
carcinoma. Cancer. 1975;35:270. rates.
Fredrickson C, Cherrick HM. Central mucoepider-
moid carcinoma of the jaws. J Oral Pathol Med. MICROSCOPIC FEATURES
1978;33:80.
Schultz W, Whitten JB. Mucoepidermoid carcinoma in The cyst lumen is usually filled with kera-
the mandible: Report of case. J Oral Maxillofac Surg. tin. The stratified squamous epithelial lin-
1969;27:337.
Smith RL, Dahlin DC, Waite DE. Mucoepidermoid
ing possesses a corrugated parakeratin
carcinomas of the jaw bones. J Oral Maxillofac Surg. layer, an attenuated spinous layer, and a
1968;26:387. polarized basal cell layer with no rete-ridge
Waldron CA, Koh ML. Central mucoepidermoid car- formation. Occasionally, however, bulbous
cinoma of the jaws: report of four cases with analysis
of the literature and discussion of the relationship to
epithelial extensions invaginate into the
mucoepidermoid sialodontogenic and glandular odon- fibrous wall where they proliferate and
togenic cysts. J Oral Maxillofac Surg. 1990;48:871. give rise to satellite (daughter) cysts. The
PMPH_Eversole_Chapter-09.indd 423 1/20/2011 3:00:36 PM
424 Chapter 9
orthokeratotic odontogenic cysts are lined by 30%. The orthokeratinized odontogenic
epithelium synthesizing orthokeratin with cyst rarely recurs after curettage. Recur-
a granular cell layer. rent cysts can be recuretted or excised en
bloc. Marsupialization, cryotherapy, and
DIFFERENTIAL DIAGNOSIS Carnoy solution lavage are also employed
A multilocular radiolucency representing in treatment.
keratocyst must be differentiated from all
of the other lesions listed in this section. If
an impacted tooth is present in association Additional Reading
with the radiolucency, the lesion is odon- Brannon RB. The odontogenic keratocyst: a clinicopatho-
togenic and the entities listed as pericoro- logic study of 312 cases. I. Clinical features. Oral Surg
nal radiolucencies must be included in the Oral Med Oral Pathol. 1981;51:609.
differential diagnosis. Aspiration usually Payne TG. An analysis of the clinical and histopathologic
parameters of the odontogenic keratocyst. Oral Surg
yields negative results with keratocysts Oral Med Oral Pathol. 1972;33:538.
because they are filled with caseous keratin Shear M. The aggressive nature of the odontogen-
rather than fluid. ic keratocyst: is it a benign cystic neoplasm? Part
2. Proliferation and genetic studies. Oral Oncol.
TREATMENT 2002;38(4):323-331.
Shear M. The aggressive nature of the odontogenic
Initial therapy should consist of thorough keratocyst: is it a benign cystic neoplasm? Part 3.
enucleation and curettage. Recurrence Immunocytochemistry of cytokeratin and other epi-
thelial cell markers. Oral Oncol. 2002;38:407-415.
rates for large multilocular keratocysts Wright JM. The odontogenic keratocyst: Orthokeratinized
are more than 50%, whereas recurrence variant. Oral Surg Oral Med Oral Pathol.
for lesions smaller than 2 cm is less than 1981;51:609.
FIGURE 9-47
Botryoid odontogenic
cysts can be microlocu-
lar or have a soap-bubble
appearance.
PMPH_Eversole_Chapter-09.indd 424 1/20/2011 3:00:36 PM
Radiolucent Lesions of the Jaws 425
BOTRYOID ODONTOGENIC CYST Phelan JA, Kritchman D, Fusco-Ramer M, Freedman
PD, Lumerman H. Recurrent botryoid odontogen-
Figure 9-47 ic cyst. Oral Surg Oral Med Oral Pathol. 1988;66:
345.
Age: Predilection unknown Weathers DR, Waldron CA. Unusual multilocular cysts
Sex: Predilection unknown of the jaws (botryoid odontogenic cysts). Oral Surg
Oral Med Oral Pathol. 1973;36:235.
CLINICAL AND RADIOGRAPHIC Wysocki GP, Brannon RB, Gardner DG, Sapp P.
FEATURES Histogenesis of the lateral periodontal cyst and the
gingival cyst of the adult. Oral Surg Oral Med Oral
The botryoid odontogenic cyst is a rare lesion
Pathol. 1980;50:327.
that grossly resembles a cluster of grapes. It
is found central in bone and may appear
unilocular or multilocular radiographically. GLANDULAR ODONTOGENIC
A soft tissue location for this lesion has been
CYST
observed as well. Expansion is observed
in central lesions. The origin of this cyst is Figure 9-48
unknown, yet it is probably odontogenic. Age: Adults
Microscopically, it closely resembles gingi- Sex: No predilection
val and lateral periodontal cysts.
CLINICAL AND RADIOGRAPHIC
FEATURES
MICROSCOPIC FEATURES
The lesion is multicystic, and each cystic cav- The glandular or sialo-odontogenic cyst is
ity is separated from others by fibrous sep- a central jaw lesion derived from epithelial
tae. The lining epithelium is low cuboidal or remnants of the odontogenic apparatus, yet
squamous, being only 1 or 2 cells thick. Focal capable of glandular differentiation. This
acanthotic clear-cell clusters are randomly cyst is developmental, although an apical
scattered along the lining, a finding identi- periodontal cyst may rarely contain a few
cal to that of lateral periodontal cyst and not mucus-secreting cells in its lining. Like
a pathognomonic feature for botryoid cyst. most other odontogenic cysts, those with
glandular histologic features are asymp-
DIFFERENTIAL DIAGNOSIS tomatic and may present with a variety of
radiologic patterns, ranging from unilocular
This unusual cyst may radiographically to multilocular; all show a well-delineated,
resemble lateral periodontal cyst; when corticated border. Certainly, young lesions
multilocular or scalloped, it cannot be dif- are probably unilocular only to become
ferentiated from the other lesions listed in racemose with progressive growth. Some
this section. instances of glandular odontogenic cyst are
pericoronal, although most are not. Growth
TREATMENT is probably steady and slow, yet these cysts
Enucleation is the treatment of choice. Altho- are capable of attaining large dimensions.
ugh not common, these cysts can recur. The anterior aspect of the mandible appears
to be the site of origin more often than the
Additional Reading maxilla.
Chi AC, Neville BW, Klinger BJ. A multilocular radio-
MICROSCOPIC FEATURES
lucency. Botryoid odontogenic cyst. J Am Dent Assoc. The histologic findings of glandular dif-
2007;138(8):1102-1103.
Greer RO, Jr, Johnson M. Botryoid odontogenic cyst:
ferentiation are what distinguish this cyst
clinicopathologic analysis of ten cases with three recur- from other odontogenic cysts. The lining
rences. J Oral Maxillofac Surg. 1988;46:574. is often tortuous and consists of nonkera-
PMPH_Eversole_Chapter-09.indd 425 1/20/2011 3:00:38 PM
426 Chapter 9
FIGURE 9-48
Expansile, loculated lucency
representing glandular odon-
togenic cyst.
tinizing stratified squamous epithelium. confused with central mucoepidermoid car-
Compartmentalization into multiple con- cinoma of the jaws.
fluent cyst cavities is not uncommon. Char-
acteristically, foci of mucous metaplasia are TREATMENT
encountered within the cyst wall and orga-
Surgical curettage is the favored approach.
nization into acinar-like clusters within the
The number of reported instances is too few to
spinous layer is observed. These mucinous
establish a rate of recurrence for these cysts.
cells are readily stained with mucin stains.
Some of the superficial cells confronting
the lumen are cuboidal or columnar.
Additional Reading
DIFFERENTIAL DIAGNOSIS Boffano P, Cassarino E, Zavattero E, Campisi P, Garzino-
Demo P. Surgical treatment of glandular odontogenic
Radiographically, the glandular odonto- cysts. J Craniofac Surg. 2010;21(3):776-780.
genic cyst exhibits large loculations when Gardner DG, Kessler HP, Morency R, Schaffner DL.
multilocular and may therefore resemble The glandular odontogenic cyst: an apparent entity.
J Oral Pathol Med. 1988;17:359.
keratocysts, ameloblastoma, aneurysmal Macdonald-Jankowski DS. Glandular odontogenic
bone cyst, and giant cell granuloma. Micro- cyst: systematic review. Dentomaxillofac Radiol.
scopically, a highly loculated cyst can be 2010;39(3):127-139.
PMPH_Eversole_Chapter-09.indd 426 1/20/2011 3:00:38 PM
Radiolucent Lesions of the Jaws 427
Padayachee A, Van Wyk CW. Two cystic lesions with ular radiolucencies occupy the entire ramus
features of both the botryoid odontogenic cyst and the and posterior body of the mandible on both
central mucoepidermoid tumour: sialo-odontogenic
cyst? J Oral Pathol Med. 1987;16:499. sides. Delicate septae course throughout
Patron M, Colmenero C, Larrauri J. Glandular odonto- the radiolucent lesion, and the anterior lim-
genic cyst: clinicopathologic analysis of three cases. its are generally ill defined. The maxillary
Oral Surg Oral Med Oral Pathol. 1991;72:71. tuberosity regions often contain expansile
multilocular radiolucencies as well. Pre-
mature exfoliation of deciduous teeth or
CHERUBISM (FAMILIAL impaction and displacement may be fea-
FIBROUS DYSPLASIA) tures. The progressive expansion begins in
Figure 9-49 early childhood and eventually the growth
becomes static, usually shortly after puberty.
Age: Childhood onset Recently, cherubism has been reported to
Sex: Slight male predilection occur in conjunction with the Noonan syn-
CLINICAL AND RADIOGRAPHIC drome, which is characterized by congenital
FEATURES heart disease, chest deformity, mental retar-
Cherubism is familial and there is evidence dation, short stature, facial bone anomalies,
that it represents an autosomal dominant and cryptorchidism. It may also be found in
trait with variable expressivity. The gene the Ramon syndrome that consists of mental
maps to chromosome 4p16, site of the 3BP2 deficiency, epilepsy, gingival fibromatosis,
adapter protein involved in mast cell acti- hypertrichosis, and rheumatoid arthritis.
vation. The term is descriptive of the clini-
cal appearance. The posterior mandible is MICROSCOPIC FEATURES
expanded bilaterally, yielding a cherubic Loose areolar fibrous connective tissue or
facies. Radiographically, extensive multiloc- even hypercellular fibrous tissue is pres-
FIGURE 9-49
Bilateral multilocular radi-
olucencies of the posterior
mandible in a patient with
familial fibrous dysplasia.
PMPH_Eversole_Chapter-09.indd 427 1/20/2011 3:00:41 PM
428 Chapter 9
ent and contains isolated, poorly formed may actually be activated by the procedure.
osseous tissue and multinucleated giant When growth has ceased, cosmetic osseous
cells. Vascular channels evince perivascular contouring may be instituted.
collagenous condensation or cuffing.
DIFFERENTIAL DIAGNOSIS Additional Reading
The clinicoradiologic features are pathog- Dunlap C, Neville B, Vickers RA, O’Neil D, Barker B.
nomonic when a familial tendency can be The Noonan syndrome/cherubism association. Oral
demonstrated. A biopsy should be per- Surg Oral Med Oral Pathol. 1989;67:698.
Hamner JE, III, Ketcham AS. Cherubism: an analysis of
formed because multiple keratocysts or treatment. Cancer. 1969;23:1133.
brown tumors of hyperparathyroidism Kuepper RC, Harrigan WF. Treatment of mandibular
could show similar characteristics, par- cherubism. J Oral Maxillofac Surg. 1978;36:638.
ticularly if no familial tendency can be Suhanya J, Aggarwal C, Mohideen K, Jayachandran
S, Ponniah I. Cherubism combined with epilep-
ascertained. sy, mental retardation and gingival fibromatosis
(Ramon syndrome): a case report. Head Neck Pathol.
TREATMENT 2010;4(2):126-131.
Topazian RG, Costich ER. Familial fibrous dyspla-
Surgical intervention during childhood is sia of the jaws (cherubism). J Oral Maxillofac Surg.
not recommended. The lesion recurs and 1965;23:559.
FIGURE 9-50
Expansile multilocular radi-
olucency of anterior man-
dible representing central
giant cell granuloma.
PMPH_Eversole_Chapter-09.indd 428 1/20/2011 3:00:46 PM
Radiolucent Lesions of the Jaws 429
CENTRAL GIANT CELL TREATMENT
GRANULOMA Surgical enucleation is the treatment of
Figure 9-50 choice. Teeth may need to be sacrificed to
eradicate the disease completely. If the lesion
Age: Young adults is not totally excised, it may recur. Intral-
Sex: Female predilection
esional steroid injection has been reported
CLINICAL AND RADIOGRAPHIC to cause resolution; however, a large series
FEATURES with follow-up documentation is lacking.
The central giant cell granuloma is an
aggressive reactive process of the jaw bones
that arises most often in the mandible ante-
Additional Reading
rior to the first molars. Indeed, it is the most de Lange J, van den Akker HP, van den Berg H. Central
common anteriorly located multilocular giant cell granuloma of the jaw: a review of the litera-
ture with emphasis on therapy options. Oral Surg Oral
expansile radiolucency. Smaller lesions may Med Oral Pathol Oral Radiol Endod. 2007;104:603-
be unilocular, and most are detected when 615.
clinical expansion alerts the patient to the Horner K. Central giant cell granuloma of the jaws. Clin
disease. When radiographs are obtained, Radiol. 1989;40:622.
Leban SG, Lepow H, Stratigos GT, Chu F. The giant
a soap-bubble loculated radiolucency is cell lesion of jaws: neoplastic or reparative? J Oral
encountered. Cortical expansion is seen Maxillofac Surg. 1971;29:398.
radiographically, and the margins of the Shklar G, Meyer I. Giant cell tumors of the mandi-
radiolucency are well demarcated. Root ble and maxilla. Oral Surg Oral Med Oral Pathol.
1961;14:809.
divergence and resorption are frequent find- Waldron CA, Shafer WG. The central giant cell reparative
ings. The overlying teeth remain vital, and granuloma of the jaws. Am J Clin Pathol. 1966;45:437.
pain or paresthesia is generally not present.
The lesion is capable of rapid growth.
ANEURYSMAL BONE CYST
MICROSCOPIC FEATURES Figure 9-51
A highly cellular fibrovascular stroma
Age: Young adults
prevails. Dispersed throughout are multi-
Sex: No predilection
nucleated giant cells that tend to lie in jux-
taposition to vascular channels. Osteoid CLINICAL AND RADIOGRAPHIC
or osseous trabeculae are present in most FEATURES
lesions, and hemosiderin granules may be The aneurysmal bone cyst is not a true
deposited in profusion. cyst. It is closely related pathogenically to
the giant cell granuloma, being an aggres-
DIFFERENTIAL DIAGNOSIS sive reactive process. Because the lesion
Brown tumor of hyperparathyroidism is is composed of large vascular sinusoids,
clinically, radiographically, and micro- blood can be aspirated with a syringe. The
scopically indistinguishable from giant cell blood coursing through the lesion is under
granuloma. A serum calcium determina- low pressure so that a bruit cannot be aus-
tion should be obtained to check for para- cultated. The lesion has a great potential
thyroid adenoma. Radiographically, giant for growth and may produce significant
cell granuloma may be confused with the expansion and deformity. The multilocu-
other lesions listed in this section. Aspi- lar radiolucency is traversed by thin septae,
ration may be negative or, because of the and cortical expansion is radiographically
vascularity of the lesion, small amounts of demonstrable. The mandibular body is the
blood may be obtained. most frequent site for this lesion and, when
PMPH_Eversole_Chapter-09.indd 429 1/20/2011 3:00:55 PM
430 Chapter 9
FIGURE 9-51
Multilocular radiolucencies
with expansion represent
aneurysmal bone cyst.
it is large, the inferior border shows a signif- of aid when attempting to differentiate
icant blowout expansile bulge. Aneurysmal aneurysmal bone cyst from arteriovenous
bone cyst is occasionally encountered in malformation, in that blood traverses the
association with other fibro-osseous lesions former slowly but progresses through the
of the jaws such as giant cell granuloma and latter at a rapid rate.
fibrous dysplasia.
TREATMENT
MICROSCOPIC FEATURES Despite the rapid growth and aggressive-
Large tortuous blood-filled sinusoidal chan- ness of the aneurysmal bone cyst, simple
nels are lined by a flat endothelial layer. enucleation rarely results in recurrence.
The surrounding tissue is fibroblastic and Intraoperatively, the lesion may hemorrhage
hypercellular. Multinucleated giant cells lie profusely; however, the blood is not under a
adjacent to the sinusoids, and osteoid tra- great degree of pressure.
beculae tend to orient themselves in close
proximity to the vascular spaces.
Additional Reading
DIFFERENTIAL DIAGNOSIS Bhaskar SN, Bernier JL, Godby F. Aneurysmal bone cyst
and other giant cell lesions of the jaws: report of 104
Radiographically, the aneurysmal bone cases. J Oral Maxillofac Surg. 1959;17:30.
cyst may demonstrate features indistin- Biesecker JL, Marcove RC, Huvos AG, Miké V.
guishable from the other multilocular Aneurysmal bone cysts: a clinicopathologic study of 66
radiolucencies included in this section. cases. Cancer. 1970;26:615.
Daugherty JW, Eversole LR. Aneurysmal bone cyst of
Aspiration of blood allows for limitation the mandible: report of case. J Oral Maxillofac Surg.
of the differential diagnosis; however, 1971;29:737.
central arteriovenous malformation or Iyogun CA. Aneurysmal bone cyst of the jaws: histologi-
hemangioma of bone also yields a bloody cal report of four cases and review of the literature.
Cent Afr J Med. 1987;33:249.
aspirate. A bruit is usually present in the Sun ZJ, Zhao YF, Yang RL, Zwahlen RA. Aneurysmal
latter, but not in aneurysmal bone cyst. bone cysts of the jaws: analysis of 17 Cases. J Oral
Carotid time-lapse angiography may be Maxillofac Surg. 2010;68:2122-2128.
PMPH_Eversole_Chapter-09.indd 430 1/20/2011 3:00:55 PM
Radiolucent Lesions of the Jaws 431
HYPERPARATHYROIDISM sia. In addition to parathyroid adenoma
Figure 9-52 and renal secondary hyperparathyroidism,
certain malignant neoplasms, such as oat
Age: Middle-aged adults cell carcinomas of the lung, secrete excess
Sex: Female predilection parathormone with the development of
CLINICAL AND RADIOGRAPHIC hyperparathyroidism. Late in the course
FEATURES of the disease, lesions may develop in any
bone, including the jaws. These are giant
A parathyroid adenoma secretes excessive
cell tumors known as brown tumors. In the
amounts of parathormone, which mobilizes
jaws, they appear as expansile multilocular
calcium into the serum and leads to osteo-
radiolucencies. Ossifying fibromas may also
porosis with elevated serum calcium levels.
occur in the jaws among genetically predis-
The poorly mineralized bone is replaced
posed patients with hyperparathyroidism.
by fibrous tissue, resulting in the condition
known as osteitis fibrosa cystica. Calcium
MICROSCOPIC FEATURES
salts precipitate in the kidneys with uro-
lithiasis, which in turn contributes to pyelo- The microscopic features of brown tumor
nephritis. Secondary hyperparathyroidism are indistinguishable from those of central
may occur in association with renal disease giant cell granuloma. Fibrovascular tissue is
in which calcium is lost in the urine, caus- admixed with numerous multinucleated giant
ing a compensatory parathyroid hyperpla- cells. Trabeculae of bone may be present.
FIGURE 9-52
Multilocular radiolucen-
cies are brown tumors of
hyperparathyroidism.
PMPH_Eversole_Chapter-09.indd 431 1/20/2011 3:01:00 PM
432 Chapter 9
DIFFERENTIAL DIAGNOSIS tumor syndrome and a novel HRPT2 gene mutation.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
The brown tumor of hyperparathyroidism 2006;101(2):212-218.
is clinically, radiographically, and micro- Carlotti AE, Camitta FD, Connor TB. Primary hyper-
scopically indistinguishable from central parathyroidism with giant cell tumors of the maxilla:
Report of case. J Oral Maxillofac Surg. 1969;27:722.
giant cell granuloma. For this reason, a bone
Karabekmez FE, Duymaz A, Keskin M, Tosun Z. Huge
chemistry panel must be evaluated. Testing deforming brown tumour at the maxilla and mandi-
reveals serum levels of calcium are elevated, ble in a patient with secondary hyperparathyroidism.
phosphorus is low, and alkaline phosphatase J Plast Reconstr Aesthet Surg. 2008;61(11):1404-1405.
is within normal limits. Radiographically, McWhorter AG, Layton S. Giant cell lesion associated
with secondary hyperparathyroidism: case report.
brown tumor may resemble the other radio- Pediatr Dent. 1989;11:55.
lucencies included in this section. Silverman S, Jr, Ware WH, Gillooly C, Jr. Dental aspects
of hyperparathyroidism. Oral Surg Oral Med Oral
TREATMENT Pathol. 1962;15(suppl 2):84.
After the diagnosis has been established,
the patient should be referred to a surgeon AMELOBLASTOMA
for excision of the parathyroid adenoma or Figure 9-53
for evaluation of renal function when sec-
ondary hyperparathyroidism is suspected. Age: Middle-aged adults
Sex: No predilection
When this work-up is negative, an endo-
crine-secreting carcinoma should be ruled CLINICAL AND RADIOGRAPHIC
out. The jaw lesions resolve after treatment; FEATURES
however, expansion may be maintained. The ameloblastoma is classically a multiloc-
Elective cosmetic osseous contouring may ular radiolucency with a predilection for
then be performed. the posterior mandible. Radiographs show
a well-circumscribed, expansile soap-bub-
Additional Reading ble radiolucency with clearly demarcated
borders. The neoplasm may arise from the
Aldred MJ, Talacko AA, Savarirayan R, et al. Dental lining of a dentigerous cyst but more often
findings in a family with hyperparathyroidism-jaw arises independent of any association with
FIGURE 9-53
Multilocular radiolucency with
root divergence and resorption in
ameloblastoma.
PMPH_Eversole_Chapter-09.indd 432 1/20/2011 3:01:01 PM
Radiolucent Lesions of the Jaws 433
impacted teeth. It shows a progressive mod- are high. Larger lesions, particularly those
erate growth rate and, if left untreated, may extending to the inferior border, require
reach enormous proportions. Expansion is en bloc resection or hemimandibulec-
seen clinically and radiographically. Pain is tomy. Maxillary ameloblastomas require
generally not a symptom. Maxillary tumors resection because they tend to invade the
frequently perforate into the antrum and antrum; any attempt to eradicate tumor by
may grow freely, with extension into the curettage will fail and importantly, recur-
nasal cavity, ethmoid sinuses, and cranial rences may not be controlled by subsequent
base. A small number of microscopically surgical resection. Less than 1% of benign-
benign ameloblastomas have been reported appearing ameloblastomas metastasize to
to undergo distant metastases. distant sites. These metastatic tumors are
frequently the granular cell type.
MICROSCOPIC FEATURES
Ameloblastomas show various growth pat-
terns; however, none of these histomorpho-
Additional Reading
logic variations has any bearing on predicting Carr RG, Halperin V. Malignant ameloblastomas from
growth potential, metastatic potential, or 1953 to 1966. Review of the literature and report of a
prognosis. The classic microscopic features case. Oral Surg Oral Med Oral Pathol. 1968;26:514.
Gomes CC, Duarte AP, Diniz MG, Gomez RS. Current
of ameloblastoma are represented by sheets concepts of ameloblastoma pathogenesis. J Oral Pathol
and islands of tumor cells showing an outer Med. 2010 Jul 2. [Epub ahead of print.]
rim of columnar ameloblasts with nuclei Hartman KH. Granular cell ameloblastoma. A survey
polarized away from the basement mem- of twenty cases from the Armed Forces Institute
of Pathology. Oral Surg Oral Med Oral Pathol.
brane. The center of these nests is composed 1974;38:241.
of stellate epithelial cells that mimic the stel- Pradhan SA, Soman CS, Patel A. Well-differentiated
late reticulum. Occasionally, these cells show metastasizing ameloblastoma. Report of a case with
squamous metaplasia or contain eosinophilic review of literature. Indian J Cancer. 1989;26:255.
Small IA, Waldron CA. Ameloblastoma of the jaws. Oral
granular cells. Plexiform, cystic, and basa-
Surg Oral Med Oral Pathol. 1955;8:281.
loid patterns are often dominant. Rarely, an
ameloblastoma exhibits cytologic features of
malignancy. Tumors of this nature maintain MYXOMA
histologic resemblance to benign amelo- Figure 9-54
blastoma with an outer columnar stratum
and a central stellate reticulum zone with Age: Young and middle-aged adults
squamous differentiation. These tumors are Sex: No prediction
diagnosed as ameloblastic carcinoma. CLINICAL AND RADIOGRAPHIC
FEATURES
DIFFERENTIAL DIAGNOSIS
The myxoma, because of its limitation to
The expansile multilocular pattern of amelo- jaw bones, is included as an odontogenic
blastoma is also encountered in other odon- neoplasm, which probably originates from
togenic and nonodontogenic lesions listed the dental papilla or follicular mesenchyme.
in this section. Aspiration is negative, and It is typically multilocular and expansile,
biopsy is required to obtain a definitive and sometimes is associated with impacted
diagnosis. teeth. The septae coursing through the radi-
olucency are extremely delicate and look like
TREATMENT
a finely reticulated spiderweb. The border
Curettage may be attempted for small man- may be clearly delineated, but occasionally,
dibular ameloblastomas. Recurrence rates the marginal limits of the tumor are indis-
PMPH_Eversole_Chapter-09.indd 433 1/20/2011 3:01:03 PM
434 Chapter 9
FIGURE 9-54
Finely reticulated septate
pattern in odontogenic
myxoma. (Courtesy of Dr.
James Shemke.)
crete. Myxomas are slow growing but are mucoid consistency. En bloc resection should
aggressively invasive; if left untreated, they be performed, particularly in larger gelati-
may become huge. The body of the mandi- nous lesions, to circumvent recurrence.
ble is the favored site. Maxillary myxomas
may perforate and invade the antrum.
Additional Reading
MICROSCOPIC FEATURES Barros RE, Cabrini RL. Myxoma of the jaws. Oral Surg
The microscopic pattern is distinctive. Spin- Oral Med Oral Pathol. 1969;27:225.
Ghosh BC, Huvos AG, Gerold FP, Miller TR. Myxoma
dle and stellate fibroblasts are associated of the jaws. Cancer. 1973;31:237.
with basophilic ground substance and deli- Happonen RP, Peltola J, Ylipaavalniemi P, Lamberg M.
cate immature collagen fibers representing Myxoma of the jaw bones. An analysis of 13 cases. Proc
myxomatous tissue. Oval odontogenic epi- Finn Dent Soc. 1988;84:45.
Martínez-Mata G, Mosqueda-Taylor A, Carlos-Bregni
thelial cell rests may or may not be present. R, et al. Odontogenic myxoma: clinico-pathological,
immunohistochemical and ultrastructural findings of a
DIFFERENTIAL DIAGNOSIS multicentric series. Oral Oncol. 2008;44(6):601-607.
White DK, Chen S, Mohnac AM, Miller AS. Odontogenic
A delicate reticulated pattern of septae, as
myxoma: a clinical and ultrastructural study. Oral Surg
seen radiographically in a multilocular Oral Med Oral Pathol. 1975;39:901.
radiolucency, is highly suggestive of myx-
oma. Regardless, the other lesions in this
section must be included in the differential CENTRAL NEUROGENIC
radiographic diagnosis. Aspiration is nega- NEOPLASMS
tive, and biopsy is indicated. Figure 9-55
TREATMENT Age: No predilection
Sex: No predilection
Myxomas are grossly gelatinous or mucoid;
so curettage is untenable in most instances. CLINICAL AND RADIOGRAPHIC
FEATURES
Occasionally, myxomas are more fibrous
and can be managed by curettage with less Neurilemmomas and neurofibromas arising
chance for recurrence than those with a from the sheath cells of the inferior alveolar
PMPH_Eversole_Chapter-09.indd 434 1/20/2011 3:01:04 PM
Radiolucent Lesions of the Jaws 435
FIGURE 9-55
Multilocular radiolucency
due to a central neural
sheath neoplasm (upper
left). Source: Sugimura M,
Shirasuna K, Yoshimura
Y, Fujimoto K, Nakajo Y.
A case of neurilemmoma
in the mandible. Int J Oral
Surg. 1974;3:194.
nerve appear as unilocular or multilocular wavy delicate collagen fibers with myx-
radiolucencies along the course of the nerve. omatous regions. Plexiform or organoid
Of all bones in the body, excluding the tem- patterns are commonly observed. Even rare
poral bone, the mandible is the most com- instances of neurogenic sarcoma have been
mon site for central nerve sheath neoplasms, reported with nuclear pleomorphism and
probably because no other bone transports a high mitotic rate. S-100 nuclear and cyto-
nerve for such a distance. Expansion of the plasmic staining assist in the diagnosis of
buccal plate is common, yet pain is not a fea- neural sheath tumors.
ture. Paresthesia may or may not be present.
Central neurofibromas are more likely to be DIFFERENTIAL DIAGNOSIS
solitary than to represent stigmata of von Multilocular central neural tumors must
Recklinghausen’s neurofibromatosis. be differentiated from the other lesions
included here. They often show widening
MICROSCOPIC FEATURES of the inferior alveolar canal with scalloped
Nerve sheath tumors of bone display the margins that make radiographic distinc-
same microscopic features as their soft tion from the traumatic cyst impossible.
tissue counterparts. Neurilemmomas are Biopsy is required to arrive at a definitive
composed of spindle cells arranged in pali- diagnosis.
sading columns and swirls separated by
TREATMENT
finely fibrillar vacuolated connective tissue.
Neurofibromas contain fibroblastic nuclei Simple surgical enucleation is the treatment
haphazardly arranged and admixed with of choice. Recurrence is uncommon.
PMPH_Eversole_Chapter-09.indd 435 1/20/2011 3:01:07 PM
436 Chapter 9
tiny locules represent small arterial chan-
Additional Reading nels. Bright-red fresh blood is obtained
Chi AC, Carey J, Muller S. Intraosseous schwannoma on aspiration. Indeed, the plunger of the
of the mandible: a case report and review of the lit- syringe may be forced out as a result of
erature. Oral Surg Oral Med Oral Pathol Oral Radiol the pressure within the lesion. Feeder ves-
Endod. 2003;96(1):54-65. sels are derived from the ipsilateral infe-
Ellis GL, Abrams AM, Melrose RJ. Intraosseous benign
neural sheath neoplasms of the jaws. Report of seven rior alveolar artery; however, contralateral
new cases and review of the literature. Oral Surg Oral vascular communications are common.
Med Oral Pathol. 1977;44:731. Unfortunately, vertebral vessels some-
Eversole LR. Central benign and malignant neu- times anastomose with the arterial chan-
ral neoplasms of the jaws. J Oral Maxillofac Surg.
1969;27:716.
nels of the jaw lesion. Angiography clearly
Sampter TG, Vellios F, Shafer WG. Neurilemmoma of demonstrates these anastomoses. Occa-
bone. Report of 3 cases with a review of the literature. sionally, central vascular anomalies are
Radiology. 1960;75:215. under low pressure. In these instances,
Wright BA, Jackson D. Neural tumors of the oral cav-
ity. A review of the spectrum of benign and malignant
they are perhaps more aptly termed cen-
neural tumors of the oral cavity and jaws. Oral Surg tral hemangiomas.
Oral Med Oral Pathol. 1980;49:509.
MICROSCOPIC FEATURES
Biopsy should not be performed when
CENTRAL ARTERIOVENOUS aspiration is positive and a bruit is det-
MALFORMATION ected. Resected mandibles show large-cal-
Figure 9-56 iber muscular vascular channels, which
course profusely throughout the medul-
Age: Children and teenagers lary bone.
Sex: Female predilection
CLINICAL AND RADIOGRAPHIC DIFFERENTIAL DIAGNOSIS
FEATURES Central AV malformations show radio-
An arteriovenous (AV) malformation of graphic features in common with the other
the mandible is potentially lethal and multilocular radiolucencies included here.
extremely dangerous when teeth are sur- A blood aspirate and detectable bruit allow
rounded by the lesion, because they will for a clinical diagnosis. A central AV mal-
become loose and, if extracted, uncontrol- formation may exist in the absence of a
lable hemorrhage often results. Spontane- bruit or cortical expansion. In these cases,
ous gingival hemorrhage or seeping of because aspiration is positive, differentia-
blood from the gingival sulci is a common tion from an aneurysmal bone cyst is criti-
sign. The malformation develops from cal. Time-lapse angiography is indicated as
the central vessels of the mandible dur- blood passes through an AV malformation
ing early childhood. High arterial pres- rapidly, whereas the time phase of aneurys-
sure is exerted within the vessels because mal bone cysts is not much different from
of direct communication of arteries with that of a normal arterial-capillary-venous
veins (an interposed capillary bed fails clearance.
to develop). This often causes compensa-
tory expansion of the cortices, and a bruit TREATMENT
can be heard on auscultation. The overly- Iatrogenic embolization with autologous
ing skin may be warmer than that on the muscle chips or other materials is con-
uninvolved side. Radiographically, AV traindicated, as pulmonary embolism may
malformations are microloculated. These occur (the vascular lumina may remain
PMPH_Eversole_Chapter-09.indd 436 1/20/2011 3:01:10 PM
Radiolucent Lesions of the Jaws 437
FIGURE 9-56
Upper: micro multilocu-
lar radiolucency (worm
hole pattern) of mandible,
an arteriovenous malfor-
mation, bloody aspirate.
Lower: angiogram showing
that blood clears the man-
dibular lesion before the
meningeal vessels enter
the venous phase of filling.
patent and equal in size through the CENTRAL (LOW FLOW)
course of the defect). The external carotids HEMANGIOMA OF BONE
should be ligated bilaterally with resec- Figure 9-57
tion of the involved portion of mandible.
Even then, hemorrhage may be profuse. Age: Infants, children
Ten units of donor blood should be avail- Sex: No predilection
able if needed. CLINICAL AND RADIOGRAPHIC
FEATURES
Additional Reading Whereas blood pressure is at arterial sys-
tolic levels in arteriovenous malformations,
Greene MW, Nishioka GJ, Triplett RG, Holt GR.
low flow intraosseous hemangiomas are at,
Arteriovenous malformation of the mandible: survey
of previously unreported cases and case report. J Oral or below, venous pressure. Low flow cen-
Maxillofac Surg. 1989;47:1322. tral hemangiomas of the mandible develop
Halzonitis JA, Kountouris J, Halzonitis NA. Arteriovenous within the inferior alveolar canal and usu-
aneurysm of the mandible. Oral Surg Oral Med Oral ally show a honeycomb or worm hole mul-
Pathol. 1982;53:454.
Lund BA, Dahlin DC. Hemangiomas of the mandible tilocular pattern with bony expansion of
and maxilla. J Oral Maxillofac Surg. 1964;22:234. the cortical plates. There may also be a soft
Tao Q, LV B, Bhatia KS, Qiao B, Zheng CQ, Chen ZF. tissue component with erythema of overly-
Three-dimensional CT angiography for the diagnosis ing skin or mucosa. A bruit is not evident.
and assessment of arteriovenous malformations in the
oral and maxillofacial region. J Craniomaxillofac Surg.
2010;38(1):32-37. MICROSCOPIC FEATURES
Worth HM, Stoneman DW. Radiology of vascular abnor-
malities in and about the jaws. Dent Radiogr Photog. Low flow hemangiomas and venous mal-
1979;52:1. formations comprise cavernous blood-filled
PMPH_Eversole_Chapter-09.indd 437 1/20/2011 3:01:10 PM
438 Chapter 9
FIGURE 9-57
Low pressure central
hemangiomas.
spaces that course among thin osseous tra- head and neck: MR characterization. AJNR Am J
beculae. These vessels lack muscular coats Neuroradiol. 1993;14(2):307-314.
Cheng NC, Lai DM, Hsie MH, Liao SL, Chen YB.
yet may show advential thickening. Small Intraosseous hemangiomas of the facial bone. Plast
capillary clusters are often interposed. Reconstr Surg. 2006;117(7):2366-2372.
Eliot CA, Castle JT. Intraosseous hemangioma of the
DIFFERENTIAL DIAGNOSIS anterior mandible. Head Neck Pathol. 2010;4(2):123-
125.
Multilocular lesions should be aspirated Hansen T, Kunkel M, Katenkamp D, Eletr S, Wagner W.
before biopsy, and if blood fills the syringe, Hemangioma of the mandible: case report with special
vascular imaging studies are in order. emphasis on bone degradation. Oral Maxillofac Surg.
2009;13(4):239-342.
Ultrasound and time-lapse angiographic
techniques can disclose flow levels aiding
in the differentiation between hemangioma
and AV malformation. CENTRAL LEIOMYOMA
Figure 9-58
TREATMENT
Age: Adults
Blood loss during surgery can be a signifi- Sex: No predilection
cant complication, yet not the life-threat-
ening event that could occur attempting CLINICAL AND RADIOGRAPHIC
FEATURES
to curette or resect an AV malformation.
Feeder vessel ligation and embolization Smooth muscle tumors central in the man-
techniques are employed in addition to dible derive from the vascular smooth
curettement or resection. muscle along the inferior alveolar canal
vasculature (vascular leiomyomas). They
Additional Reading are asymptomatic and result in uni- or mul-
tilocular radiolucencies with well-defined
Baker LL, Dillon WP, Hieshima GB, Dowd CF, Frieden margins. Cortical expansion is usually seen
IJ. Hemangiomas and vascular malformations of the in these rare tumors.
PMPH_Eversole_Chapter-09.indd 438 1/20/2011 3:01:12 PM
Radiolucent Lesions of the Jaws 439
Liang H, Frederiksen NL, Binnie WH, Cheng YS.
Intraosseous oral leiomyoma: systematic review
and report of one case. Dentomaxillofac Radiol.
2003;32(5):285-290.
Suresh L, Matsumura E, Calixto LE, Ruckert E, Aguirre
A. Intraosseous angiomyoma of the mandible. Gen
Dent. 2007;55(2):132-135.
PSEUDOTUMOR OF
FIGURE 9-58 HEMOPHILIA
Intraosseous leiomyoma.
Figure 9-59
MICROSCOPIC FEATURES Age: Children
Sex: Males
Leiomyomas are benign spindle cell neo-
CLINICAL AND RADIOGRAPHIC
plasms with streaming and fasciculation of FEATURES
the cells that show elongated, cigar-shaped
nuclei. Since most of these tumors arise from Hemophilia, an X-linked recessive disease,
vessel wall smooth muscle, they show a ten- affects males primarily and results in a
dency for perivascular, circumferential lay- deficiency of coagulation factor VIII. Gingi-
ering of tumor cells. Mitotic figures are not val bleeding, ecchymosis, and hemarthrosis
encountered. The cells are positive for muscle are the major findings. Two percent of the
markers, smooth muscle actin in particular. patients experience subperiosteal hemor-
rhage after trauma. Patients with factor IX
DIFFERENTIAL DIAGNOSIS deficiency may experience similar prob-
The clinical and radiographic features may lems. The subperiosteal focus of hemor-
simulate many of the other lesions listed rhage may progress to involve medullary
here as multilocular. Microscopically, myo- bone. Clinically, a firm expansile mass is
fibroma is a consideration, and both myofi- observed over the body and angle of the
broma and leiomyoma are smooth muscle mandible. Radiographically, a multilocular
actin positive. Importantly, fine collagen is radiolucency is observed and is expansile.
identified between spindle cells in myofi-
broma whereas leiomyoma is strictly smooth MICROSCOPIC FEATURES
muscle as seen on trichrome staining. The lesion shows foci of granulation tissue,
fibrous tissue, hematoma with extravasated
TREATMENT erythrocytes, and reactive new bone forma-
Thorough enucleation is required. The neu- tion. Cystic spaces without an epithelial lin-
rovascular bundle is sacrificed with resul- ing are also frequently encountered.
tant lip paresthesia, a symptom that may
ultimately resolve. DIFFERENTIAL DIAGNOSIS
A multicystic expansile mass in the man-
Additional Reading dible of a patient with a genetic coagulation
disorder and a history of trauma suggest
Bertolini F, Bianchi B, Corradi D, Caradonna L, Sesenna the diagnosis of hemophilic pseudotu-
E. Mandibular intraosseous leiomyoma in a child: report mor. Alternatively, a hemophiliac could,
of a case. J Clin Pediatr Dent. 2003;27(4):385-387.
Goldblatt LI, Edesess RB. Central leiomyoma of
of course, develop any of the other lesions
the mandible. Oral Surg Oral Med Oral Pathol. included here. A biopsy is recommended
1977;43(4):591-597. for securing a definitive diagnosis.
PMPH_Eversole_Chapter-09.indd 439 1/20/2011 3:01:13 PM
440 Chapter 9
FIGURE 9-59
Hemophilic pseudotumor
involving the mandible.
TREATMENT the inferior maxilla. Report of a case. Oral Surg Oral
Med Oral Pathol. 1982;53:347.
Biopsy and definitive surgery must be per- Stoneman DW, Beierl C, Douglas C. Pseudotumor of
formed after administration of the appro- hemophilia in the mandible. Oral Surg Oral Med Oral
priate factor cryoprecipitate. Curettage is Pathol. 1975;40:811.
the treatment of choice. The mandible may
heal yet remain expanded.
MYOFIBROMATOSIS
(DESMOPLASTIC FIBROMA OF
Additional Reading BONE)
Abell JM, Jr, Bayley RW. Hemophilic pseudotumors of Figure 9-60
the mandible. Arch Surg. 1960;81:569.
Bryan GW, Leibold DG, Triplett RG. Hemophilic Age: Teenagers and young adults
pseudotumor of the mandible. Report of case. Oral Sex: No predilection
Surg Oral Med Oral Pathol. 1990;69:550.
Lee DW, Jee YJ, Ryu DM, Kwon YD. Changes in a CLINICAL AND RADIOGRAPHIC
hemophilic pseudotumor of the mandible that devel- FEATURES
oped over a 20-year period. J Oral Maxillofac Surg.
2009;67(7):1516-1520.
Aggressive juvenile myofibromatosis is a
Marquez JL, Vinageras E, Dorantes S, Nussbaumer C, reactive fibroblastic proliferation of the soft
Flores A, Perez Rolon G. Hemophilic pseudotumor of tissues. Rarely, histologically similar lesions
PMPH_Eversole_Chapter-09.indd 440 1/20/2011 3:01:14 PM
Radiolucent Lesions of the Jaws 441
FIGURE 9-60
Intraosseous myofibromatosis.
arise centrally in the jawbones and are rem- long bones, some of these fibroblastic pro-
iniscent of central desmoplastic fibromas liferations synthesize more mature, dense
that arise in the long bones. Rapid expan- collagen bundles. Osseous trabeculae are
sion with facial asymmetry is the usual pre- either lacking or are a minor element. This
senting sign, and the mandible is more often myofibroblastic lesion is positive for smooth
the site of origin. Radiographically, a well- muscle actin and vimentin using immuno-
delineated multilocular or unilocular pat- histochemistry staining.
tern is encountered with concomitant root
resorption or divergence. Perforation of the DIFFERENTIAL DIAGNOSIS
cortex is by no means rare, and when large Myofibromatosis central in bone cannot
lesions occur it may be difficult to determine be differentiated with certainty from the
whether the lesion arose centrally with per- other aggressive neoplasms included here.
foration or peripherally with bony invasion. A history of rapid expansion and ability to
clinically and radiographically detect corti-
MICROSCOPIC FEATURES cal perforation in a teenage patient should
The lesion is hypercellular, being composed arouse suspicion of fibromatosis.
of fibroblasts and varying amounts of colla-
TREATMENT
gen. The collagen fibers are usually thin and
delicate with fasciculations and herring- Myofibromatosis is aggressive with sig-
bone, chevron, or storiform configurations. nificant potential for growth despite its
In keeping with desmoplastic fibroma of benignity. Indeed, some pathologists prefer
PMPH_Eversole_Chapter-09.indd 441 1/20/2011 3:01:17 PM
442 Chapter 9
to refer to these lesions as nonmetastasiz- illa as a ground-glass radiopacity, when
ing fibrosarcomas. Small lesions with total the mandible is involved, the lesion often
osseous confinement may be successfully assumes a multilocular radiolucent pat-
managed by thorough enucleation and tern. Characteristically, expansion is evi-
curettage. Large or massive tumors with dent and the radiographic margins of
cortical perforation usually require mar- the growth are indiscrete. The expansion
ginal or en bloc resection. develops insidiously during the early teen-
age years with progressive slow growth.
The growth potential begins to wane as
Additional Reading skeletal maturity ensues. In rare instances,
fibrous dysplasia shows a rapid enlarge-
Fisher AV, Philipsen HP. Desmoplastic fibroma of the
jawbones. Int J Oral Maxillofac Surg. 1976;5:285. ment with an aggressive clinical course.
Freedman PD, Cardo VA, Kerpel SM. Desmoplastic Polyostotic lesions should be sought by
fibroma (fibromatosis) of the jawbones. Oral Surg means of skull radiographs and a skeletal
Oral Med Oral Pathol. 1978;46:386. survey.
Foss RD, Ellis GL. Myofibromas and myofibromatosis of
the oral region: a clinicopathologic analysis of 79 cases.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. MICROSCOPIC FEATURES
2000;89(1):57-65.
Melrose RJ, Abrams AM. Juvenile fibromatosis affecting A hypercellular proliferative fibrous tissue
the jaws. Report of three cases. Oral Surg Oral Med element predominates the sections. Dis-
Oral Pathol. 1980;49:317. persed throughout are irregular, poorly
Peed LF, Epker BN. Aggressive juvenile fibromatosis formed osseous trabeculae that are usually,
involving the mandible: surgical excision with immedi-
ate reconstruction. Oral Surg Oral Med Oral Pathol.
but not invariably, fetal or woven. These tra-
1977;43:651. beculae are often devoid of any osteoblastic
rimming.
FIBROUS DYSPLASIA DIFFERENTIAL DIAGNOSIS
Figure 9-61 When fibrous dysplasia appears as a mul-
tilocular radiolucency, it must be differenti-
Age: Teenagers
Sex: No predilection ated from the other diseases included here
as multilocular lesions. The lack of defini-
CLINICAL AND RADIOGRAPHIC tion at the lesional borders is highly sugges-
FEATURES
tive of fibrous dysplasia, yet biopsy must be
Whereas fibrous dysplasia of the jaws is performed to confirm the clinicoradiologic
more frequently encountered in the max- impression.
FIGURE 9-61
Diffuse, poorly marginated
multicystic lesion of poste-
rior mandible in monosto-
tic fibrous dysplasia.
PMPH_Eversole_Chapter-09.indd 442 1/20/2011 3:01:21 PM
Radiolucent Lesions of the Jaws 443
TREATMENT
Treatment should be postponed until
Moth-Eaten Radiolucencies
growth of the lesion subsides. Surgical OSTEOMYELITIS
intervention before cessation of growth
Figure 9-63
may actually result in activation of the
lesion. In those lesions showing a rapidly Age: No predilection
proliferative course, close follow-up should Sex: No predilection
be instituted. If the lesion begins to mani-
CLINICAL AND RADIOGRAPHIC
fest massive growth potential, resection
FEATURES
should be considered. In the ordinary, less
aggressive and common form of the dis- Osteomyelitis of the jaws usually originates
ease, cosmetic osseous contouring can be from odontogenic infection. It may be acute,
undertaken when growth ceases. Radiation subacute, or chronic, the first being most
therapy has been shown to predispose to painful. The patient is usually only slightly
postradiation sarcoma. febrile, and cervical lymphadenopathy is a
frequent finding. Staphylococci and strepto-
cocci are the predominant causative organ-
Additional Reading isms; however, actinomycetes and anaerobic
gram-negative bacilli are cultured in many
Bessho K, Tagawa T, Murata M, Komaki M. Monostotic
fibrous dysplasia with involvement of the man-
instances. Clinically, in acute and subacute
dibular canal. Oral Surg Oral Med Oral Pathol. stages, multiple fistulae with draining puru-
1989;68:396. lent exudate are encountered. Paresthesia
Eversole LR, Sabes WR, Rovin S. Fibrous dysplasia: a and pain are associated with acute infec-
nosologic problem in the diagnosis of fibro-osseous
lesions of the jaw. J Oral Pathol Med. 1972;1:189.
tions. Radiographically, the cortices rarely
Eversole R, Su L, ElMofty S. Benign fibro-osseous show expansion. The lesion may be mul-
lesions of the craniofacial complex. A review. Head tilocular or show approximating multifocal
Neck Pathol. 2008;2:177-202. radiolucencies with ill-defined, moth-eaten
Waldron CA, Giansanti JS. Benign fibro-osseous lesions
margins. Radiopaque sequestrae are fre-
of the jaws: a clinical-radiologic-histologic review of
sixty-five cases. I. Fibrous dysplasia of the jaws. Oral quently seen to “float” within radiolucent
Surg Oral Med Oral Pathol. 1973;35:190. crypts. Specific forms of chronic osteomy-
Zimmerman DC, Dahlin DC, Stafne EC. Fibrous dys- elitis (phosphorus poisoning, syphilis, and
plasia of the maxilla and mandible. Oral Surg Oral tuberculosis) may involve the jaws. Another
Med Oral Pathol. 1958;11:55.
specific osseous inflammation, osteoradion-
ecrosis, develops in jaws of patients under-
going radiation therapy for oral carcinoma.
INTRAOSSEOUS
Patients with Paget’s disease of bone and
MUCOEPIDERMOID osteopetrosis are prone to develop wide-
CARCINOMA spread osteomyelitis of the jaws from odon-
Figure 9-62 togenic infection.
See description under Pericoronal Radio- MICROSCOPIC FEATURES
lucencies
Osseous trabeculae and necrotic bone are
surrounded by granulation tissue, necrotic
THALASSEMIA MAJOR debris, and inflammatory cells. The inflam-
matory cell infiltrate varies depending on
See description under Generalized Osteo- whether the process is acute, subacute, or
porotic Lesions chronic. Syphilitic osteomyelitis may dis-
PMPH_Eversole_Chapter-09.indd 443 1/20/2011 3:01:23 PM
444 Chapter 9
FIGURE 9-62
Intraosseous mucoepidermoid car-
cinoma.
FIGURE 9-63
Osteomyelitis showing a diffuse moth-eaten radiolucent pattern.
PMPH_Eversole_Chapter-09.indd 444 1/20/2011 3:01:23 PM
Radiolucent Lesions of the Jaws 445
play foci of gummatous necrosis. Tubercu- OSTEORADIONECROSIS
lous osteomyelitis is characterized by the Figure 9-64
presence of specific granulomatous inflam-
mation with Langhans’ giant cells. Age: Adults, elderly
Sex: Male predilection (oral cancer is more fre-
DIFFERENTIAL DIAGNOSIS quent in males)
When an offending necrotic tooth over- CLINICAL AND RADIOLOGIC FEATURES
lies the radiographic defect, when pain is Patients receiving more than 20 gray of
present and the patient is febrile, a clinical radiation to the jaws are subject to osteomy-
diagnosis can usually be made. Neverthe- elitis secondary to odontogenic/endodontic
less, moth-eaten radiolucencies occur in infection. In most instances, the radiation
metastatic and primary epithelial and mes- dosage is higher when used as a radio-
enchymal malignant neoplasms. Failure therapeutic regimen for treatment of oral
to respond within 2 weeks to therapeutic and oropharyngeal squamous cancer or in
measures to control infection necessitates some instances certain radiosensitive sali-
biopsy. vary gland malignancies. Radiographically,
a moth-eaten pattern is seen and clinically
TREATMENT alveolar ridge ulceration with bony seques-
Nonspecific osteomyelitis requires elimina- tration may be identified. Bacterial infection
tion of the source of infection (tooth extrac- spreads throughout the marrow spaces, and
tion), incision and drainage if spaces are fistulae are usually present. Pain is often
involved, and antibiotic therapy. Penicillin severe.
is the drug of choice. Before antibiotic ther-
apy is instituted, a sterile aspirate should MICROSCOPIC FEATURES
be obtained and submitted for both routine Simply put, osteoradionecrosis is osteomy-
and anaerobic culture and sensitivity tests. elitis of radiated bone and as such, is micro-
In patients with high fever, space infection, scopically similar to subacute osteomyelitis
or accompanying cellulitis, hospitalization with inflammatory infiltration of marrow
with intravenous antibiotic therapy and spaces along with bony sequestra. The
supportive care may be required. Surgi- vasculature may show endothelial pleo-
cal debridement with removal of seques- morphism as a consequence of radiation-
tra is indicated when widespread osseous induced cellular change.
involvement is seen.
DIFFERENTIAL DIAGNOSIS
Additional Reading Clinically, osteoradionecrosis must be dif-
ferentiated from recurrent carcinoma in
Hudson JW. Osteomyelitis of the jaws: a 50-year perspec- bone by obtaining biopsies from the lesional
tive. J Oral Maxillofac Surg. 1993;51(12):1294-1301.
Krutchkoff DJ, Runstad L. Unusually aggressive osteo- tissue.
myelitis of the jaws. A report of two cases. Oral Surg
Oral Med Oral Pathol. 1989;67:499. TREATMENT
Kinnmann JEG, Lee HS. Chronic osteomyelitis of the
mandible: clinical study of thirteen cases. Oral Surg Of utmost importance is prevention. Extrac-
Oral Med Oral Pathol. 1968;25:6. tion or root canal therapy of infected teeth
Mowlem R. Osteomyelitis of the jaw. Proc R Soc Med. and elimination of periodontal sepsis must
1945;38:452.
Musser LM, Tulumello TN, Hiatt WR. Actinomycosis of
be undertaken prior to administration of
the anterior maxilla. Oral Surg Oral Med Oral Pathol. radiation. Lead shields are used to prevent
1977;44:21. salivary damage and can be used over bony
PMPH_Eversole_Chapter-09.indd 445 1/20/2011 3:01:34 PM
446 Chapter 9
FIGURE 9-64
Postradiation osteoradionecrosis.
areas that are not involved with tumor. Oth- BISPHOSPHONATE-RELATED
erwise for active disease, antibiotic therapy, OSTEONECROSIS OF THE
debridement, and hyperbaric oxygen ther- JAWS (BRONJ)
apy are recommended.
Figure 9-65
Additional Reading Age: Elderly
Sex: No predilection
Bessereau J, Annane D. Treatment of osteoradionecro-
sis of the jaw: the case against the use of hyperbaric
CLINICAL AND RADIOLOGIC FEATURES
oxygen. J Oral Maxillofac Surg. 2010;68(8):1907- During the last century, people who worked
1910.
Cannady SB, Dean N, Kroeker A, Albert TA, Rosenthal in phosphorous mines were prone to develop
EL, Wax MK. Free flap reconstruction for osteoradi- osteomyelitis of their jaws and were said to
onecrosis of the jaws—outcomes and predictive fac- suffer from “phossy jaw.” Recently it was
tors for success. Head Neck. 2010 Jul 19. [Epub ahead discovered that bisphosphonate salts could
of print.]
Freiberger JJ, Feldmeier JJ. Evidence supporting the
be useful in promoting osteogenesis among
use of hyperbaric oxygen in the treatment of osteo- osteoporotic patients. Furthermore it was
radionecrosis of the jaw. J Oral Maxillofac Surg. found that bone formation in patients with
2010;68(8):1903-1906. intraosseous malignancies such as mul-
Lyons A, Ghazali N. Osteoradionecrosis of the jaws:
current understanding of its pathophysiology and
tiple myeloma and metastatic cancer can
treatment. Br J Oral Maxillofac Surg. 2008;46(8):653- be improved with bisphosphonate therapy.
560. In a subgroup of patients taking bisphos-
PMPH_Eversole_Chapter-09.indd 446 1/20/2011 3:01:34 PM
Radiolucent Lesions of the Jaws 447
FIGURE 9-65
Bisphosphonate-related osteonecrosis of the jaws.
phonates intravenously, bone necrosis and levels are indicative of decreased risk for jaw
sequestion were witnessed in the mandi- necrosis (>150 pgm/ml).
ble and maxilla. Subsequently, cases were
reported in patients taking bisphosphonates MICROSCOPIC FEATURES
orally. There is usually pain, ulceration of Necrotic bone characterized by lamellar
the alveolus, and exposed bony sequestra sequestra showing lacunae devoid of osteo-
that were spontaneously extruded. These cyte nuclei are identified and are surrounded
osseous destructive lesions presented, often by necrotic debris and microbial colonies.
without any provocation, as radiolucent foci In many instances these colonies show a
with moth-eaten ragged borders and float- radial fringe consistent with actinomycetes.
ing sequestra. In many instances, actinomy- Viable soft tissues are often absent.
cetes are cultivatable. The risk for developing
osteonecrosis while taking bisphosphonates DIFFERENTIAL DIAGNOSIS
can be quite reliably predicted by ordering The features are similar to those of osteo-
serum C-terminal telopeptide (CTX). High myelitis and osteoradionecrosis. The fact
PMPH_Eversole_Chapter-09.indd 447 1/20/2011 3:01:42 PM
448 Chapter 9
that the patients are being medicated for Sawatari Y, Marx RE. Bisphosphonates and bisphospho-
bone cancer or senile osteoporosis with bis- nate induced osteonecrosis. Oral Maxillofac Surg Clin
North Am. 2007;19(4):487-498, v-vi.
phosphonates underlies the diagnosis.
TREATMENT
PRIMARY INTRAOSSEOUS
Careful, nonaggressive sequestrectomy is CARCINOMA
required along with antiseptic lavage and
Figure 9-66
antibiotic therapy.
Age: Middle-aged adults
Additional Reading Sex: Male predilection
CLINICAL AND RADIOGRAPHIC
Bagan J, Scully C, Sabater V, Jimenez Y. Osteonecrosis FEATURES
of the jaws in patients treated with intravenous bis-
phosphonates (BRONJ): a concise update. Oral Oncol. Primary malignant epithelial tumors cen-
2009;45(7):551-554. tral in bone are extremely rare, but may
Ruggiero SL. Bisphosphonate-related osteonecrosis of arise from odontogenic epithelium enclosed
the jaw (BRONJ): initial discovery and subsequent
development. J Oral Maxillofac Surg. 2009;67(5
within the periodontal ligament or other
suppl):13-18. intraosseous locations. The chief clinical
Ruggiero SL, Dodson TB, Assael LA, Landesberg R, manifestations are the same as those for
Marx RE, Mehrotra B; American Association of Oral metastatic carcinomas of the jaws. Clinically
and Maxillofacial Surgeons. American Association of
Oral and Maxillofacial Surgeons position paper on bis-
demonstrable expansion, paresthesia, pain,
phosphonate-related osteonecrosis of the jaws—2009 and, occasionally, unexplained loosening of
update. J Oral Maxillofac Surg. 2009;67(5 suppl):2-12. teeth occur. Radiographically, the lesion is
FIGURE 9-66
Nondiscrete diffuse radio-
lucencies of jaws in primary
intraosseous carcinoma.
PMPH_Eversole_Chapter-09.indd 448 1/20/2011 3:01:53 PM
Radiolucent Lesions of the Jaws 449
multilocular with poorly defined borders. ing in an odontogenic cyst or de novo: a clinicopatho-
Expansion or cortical perforation is encoun- logic study of six new cases. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 2006;101:194-200.
tered. Primary squamous cell carcinomas of Lindquist C, Teppo L. Primary intraosseous carci-
the jaws may also arise from the linings of noma of the mandible. Int J Oral Maxillofac Surg.
odontogenic cysts, usually residual cysts. 1986;15:209.
Shear M. Primary intra-alveolar epidermoid carcinoma
MICROSCOPIC FEATURES of the jaw. J Pathol. 1969;97:645.
Sirsat MV, Sampat MB, Shrikhande SE. Primary intra-al-
Intraosseous carcinoma shows sheets and veolar squamous cell carcinoma of the mandible. Oral
islands of neoplastic epithelium manifesting Surg Oral Med Oral Pathol. 1973;35:366.
Van Wyk CW. Primary intraosseous carcinoma involv-
the cardinal signs of malignancy—hyper- ing the anterior mandible. Br J Oral Maxillofac Surg.
chromatism, pleomorphism, and mitoses. 1987;25:427.
Acanthotic regions resembling pearl for-
mation are occasionally present. Thus, the
tumor closely resembles squamous cell car- CYSTOGENIC CARCINOMA
cinoma. A distinctive feature is the odonto- Figure 9-67
genic nature of the tumor cells. An outer rim
of ameloblastic cells occupies the position Age: Elderly
usually assumed by basal cells in an ordi- Sex: Male predilection
nary squamous cell carcinoma. Carcinomas CLINICAL AND RADIOGRAPHIC
arising from odontogenic cysts usually do FEATURES
not show odontogenic features; rather, they Squamous cell carcinoma may, on rare
represent typical squamous cell carcinoma. occasions, arise from the lining of odonto-
genic cysts. Central mucoepidermoid carci-
DIFFERENTIAL DIAGNOSIS
noma, a malignant salivary neoplasm, may
The moth-eaten radiolucent pattern of also evolve from odontogenic cyst linings.
intraosseous carcinoma is similar to that of Whereas squamous cancers are more often
osteomyelitis; however, cortical expansion associated with residual cysts of the man-
is not common in infectious processes. Pri- dibular body, mucoepidermoid tumors are
mary malignant mesenchymal tumors must generally observed in the posterior mandi-
also be included in the differential diag- ble, and tumorigenesis from a dentigerous
nosis. Metastatic carcinoma must be ruled cyst can often be speculated or even docu-
out, even after biopsy, by thorough physical mented. Maxillary cases have also been
examination and diagnostic radiologic sur- reported; however, documented origin
veys. Only then may the tumor be consid- from cyst lining is problematic when antral
ered a primary carcinoma of the jaws. involvement exists. Clinically, paresthesia
is a frequent, yet certainly not invariable,
TREATMENT symptom. Radiographically, a poorly mar-
Resection of the involved segment with ginated unilocular or moth-eaten pattern is
regional node dissection is recommended. observed.
Chest radiographs should be evaluated for
distant spread. Survival rates are less than MICROSCOPIC FEATURES
30% for 5 years. Remnants of ordinary stratified squamous
epithelial lining are seen with both mural
Additional Reading and luminal proliferation of squamous cell
carcinoma exhibiting nuclear hyperchro-
Chaisuparat R, Coletti D, Kolokythas A, Ord RA, Nikitakis matism, pleomorphism, increased mitotic
NG. Primary intraosseous odontogenic carcinoma aris- activity, and keratin pearl formation. Cys-
PMPH_Eversole_Chapter-09.indd 449 1/20/2011 3:02:01 PM
450 Chapter 9
FIGURE 9-67
Residual and radicular
cysts with carcinomatous
transformation from the
cyst lining.
togenic mucoepidermoid tumors are usu- Muglali M, Sumer AP. Squamous cell carcinoma arising
ally of the low-grade variety with solid and in a residual cyst: a case report. J Contemp Dent Pract.
2008;9:115-121.
cystic islands consisting of mucous, epider- Waldron CA, Mustoe TA. Primary intraosseous car-
moid, and intermediate cells. cinoma of the mandible with probable origin in an
odontogenic cyst. Oral Surg Oral Med Oral Pathol.
DIFFERENTIAL DIAGNOSIS 1989;67:716.
Cystogenic cancers, especially when par-
esthesia is present, radiographically and
clinically, simulate other malignant bone METASTATIC CARCINOMA
tumors including metastatic carcinoma, Figure 9-68
intraosseous carcinoma, and primary sar-
Age: Adult predilection
comas. Biopsy with documented evidence
Sex: Male predilection
of typical cyst lining is required for the
diagnosis. CLINICAL AND RADIOGRAPHIC
FEATURES
TREATMENT Metastasis to the jaws from primary carci-
Complete block resection is required; noma located in visceral or parenchymal
should any palpable nodes be discovered, organs (usually the lung, breast, colon, or
a neck dissection is indicated. Because of prostate) may reach the medullary bone
insufficient data on these lesions, the prog- by hematogenous spread via arterial dis-
nosis remains unknown. semination from tumor foci located in
the lungs or via retrograde migration of
tumor emboli through Batson’s paraverte-
Additional Reading bral plexus, thereby bypassing the lungs.
Metastatic cancer is the most common
Eversole LR, Sabes WR, Rovin S. Aggressive growth and
neoplastic potential of odontogenic cysts, with special
malignancy of the jawbones. Whereas most
reference to central epidermoid and central mucoepi- instances of osseous metastasis to the jaws
dermoid carcinoma. Cancer. 1975;35:270. appear as irregular moth-eaten expansile
Gardner AG. The odontogenic cyst as a potential carci- radiolucencies, some metastatic carcino-
noma, a clinicopathologic appraisal. J Am Dent Assoc.
1969;78:746.
mas may induce ossification so that areas
Lapin R. Squamous cell carcinoma arising in a dentiger- of radiolucency are admixed with irregu-
ous cyst. J Oral Maxillofac Surg. 1973;31:354. lar radiopaque foci. Prostatic and thyroid
PMPH_Eversole_Chapter-09.indd 450 1/20/2011 3:02:01 PM
Radiolucent Lesions of the Jaws 451
FIGURE 9-68
Diffuse irregular radiolu-
cencies representing met-
astatic carcinomas. Some
mets induce osteogenesis
as seen in lower right.
tumors are more prone to demonstrate osteo- morphologic characteristics depending on
blastic foci. Juxtaposed teeth may show root the site of origin of the primary tumor.
resorption; however, large areas of osseous
destruction with no resorptive changes of DIFFERENTIAL DIAGNOSIS
the teeth are more common. The angle and The irregular poorly marginated expansile
body of the mandible are the favored sites radiolucencies encountered in metastatic car-
of deposition, probably because of the rich cinoma may also be seen in other malignant
intraosseous vascularity in these areas. The tumors of the jaws: reticulum cell sarcoma;
most important and consistent clinical find- Ewing’s sarcoma; Burkitt’s lymphoma; and
ings include swelling, paresthesia of the lip, osteogenic, chondrogenic, or fibrogenic sar-
and deeply situated bone pain. Loosening comata. Osteomyelitis rarely shows expan-
of teeth is also a frequent finding. sion. A history of cancer elsewhere or the
presence of paresthesia is highly suggestive
MICROSCOPIC FEATURES
of metastatic cancer. Primary intra-alveolar
Nests, islands, and cords of neoplastic epi- carcinoma shows microscopic features that
thelium are supported by a fibrous stroma. are somewhat unusual; however, the diag-
In the case of osteoblastic metastasis, exten- nosis should be reserved for those patients
sive osteoplasia may be demonstrated micro- in whom exhaustive examination proce-
scopically. The individual tumor cells may dures fail to disclose the presence of a pri-
display keratinizing, adenoid, or anaplastic mary carcinoma located elsewhere.
PMPH_Eversole_Chapter-09.indd 451 1/20/2011 3:02:03 PM
452 Chapter 9
TREATMENT ameloblastic carcinoma, the clear-cell odon-
The discovery of a metastatic deposit in the togenic tumor, and the malignant ghost cell
jaws carries an extremely poor prognosis. tumor, all of which are distinguished on the
Once the diagnosis is rendered, a complete basis of histologic features. The chief clini-
work-up is indicated to locate the primary cal finding is jaw enlargement without pain,
tumor, as is a metastatic radiographic series although loosening of teeth in the affected
to search for other sites of osseous metas- area may be a complaint. Cortical expan-
tasis. In most cases, the disease is treated sion is clinically detected. Radiographically,
palliatively, and radiation therapy may the lesions are radiolucent, destructive, and
be indicated to relieve pain. Rarely, the poorly marginated. Teeth in the area of these
jaw lesion may represent a single focus of tumors tend to be displaced, except for clear-
metastasis and the disease may be treatable cell lesions that rarely exhibit root resorp-
by surgical and/or radiation therapy to both tion, and the teeth appear to be suspended
the primary tumor and jaw metastasis. within the lesion.
MICROSCOPIC FEATURES
Additional Reading Ameloblastic carcinomas retain the mor-
Castigliano SG, Rominger CJ. Metastatic malignancy of phologic structure of ameloblastoma with a
jaws. Am J Surg. 1954;87:496. peripheral stratum of ameloblasts surround-
Cash CD, Royer RQ, Dahlin DC. Metastatic tumors of the ing stellate reticulum. Of note is the pres-
jaws. Oral Surg Oral Med Oral Pathol. 1961;14:897. ence of cytologic atypia and mitotic activity.
Divya KS, Moran NA, Atkin PA. Numb chin syndrome:
a case series and discussion. Br Dent J. 2010;208:157-
Ameloblastomas without evidence of atypia
160. have been reported to metastasize, and such
Hashimoto N, Kurihara K, Yamasaki H, Ohba S, Sakai lesions are referred to as malignant amelo-
H, Yoshida S. Pathological characteristics of metastatic blastomas as opposed to ameloblastic carci-
carcinoma in the human mandible. J Oral Pathol Med.
1987;16:362.
noma, a term reserved for lesions exhibiting
Perriman AO, Figures KH. Metastatic retinoblastoma cytologic atypia. The malignant ghost cell
of the mandible. Oral Surg Oral Med Oral Pathol. tumor resembles the calcifying and kerati-
1978;45:741. nizing odontogenic cyst yet shows atypia.
The clear-cell tumor is characterized by
nests and islands of epithelial cells that tend
MALIGNANT ODONTOGENIC to anastomose with one another. Most of
TUMORS these lesions are biphasic with nests of basi-
Figure 9-69 loid cells alternating with nests comprising
exclusively clear cells. The basal or outermost
Age: Adults stratum of cells are flattened without polar-
Sex: No predilection ization. The basaloid cells contain slightly
CLINICAL AND RADIOGRAPHIC pleomorphic nuclei without mitotic figures.
FEATURES A mature fibrous stroma intervenes.
Whereas primary intraosseous carcinoma
and carcinoma ex odontogenic cyst derive DIFFERENTIAL DIAGNOSIS
from odontogenic epithelium, both retain Radiographically, malignant odontogenic
the morphologic characteristics of squamous tumors resemble histiocytosis, metastatic dis-
cell carcinoma. Other odontogenic tumors ease, or other central jaw malignant tumors.
are extremely aggressive and some may be Microscopically, when clear cells are extant,
malignant with metastatic potential. Included renal cell carcinoma is the chief consideration
in this group of odontogenic carcinomas are and a primary kidney tumor should be ruled
PMPH_Eversole_Chapter-09.indd 452 1/20/2011 3:02:11 PM
Radiolucent Lesions of the Jaws 453
FIGURE 9-69
Poorly marginated lesion
with root divergence rep-
resenting clear-cell odon-
togenic tumor. Bone scan
showing high activity in
maxilla.
out by imaging studies before accepting clear- OSTEOSARCOMA AND
cell jaw tumors as primary disease. CHONDROSARCOMA
Figure 9-70
TREATMENT
These poorly marginated aggressive tumors Age: Adults
are generally managed by en bloc resection. Sex: No predilection (female predilection in
These lesions are extremely rare and there- mandibular tumors)
fore no information is available on their CLINICAL AND RADIOGRAPHIC
susceptibility to radiation or chemothera- FEATURES
peutic agents.
Whereas both osteogenic and chondro-
genic sarcomas are capable of calcifi-
Additional Reading cation, with resultant opacification on
radiographs, many forms fail to show sig-
Corio RL, Goldblatt LI, Edwards PA, Hartman KS. nificant calcification and appear as irregu-
Ameloblastic carcinoma: a clinicopathologic study and
assessment of eight cases. Oral Surg Oral Med Oral lar, poorly delineated, expansile radiolu-
Pathol. 1987;64:570. cencies. Both tumors are rare in the jaws;
Eversole LR. Malignant epithelial odontogenic tumors. as opposed to osteosarcoma of other bones,
Semin Diagn Pathol. 1999;16:317-324. jaw lesions tend to occur in older individu-
Eversole LR, Belton CM, Hansen LS. Clear cell odon-
togenic tumor: histochemical and ultrastructural fea-
als as well as in teenagers. The mandible
tures. J Oral Pathol Med. 1985;14:603. is affected more often than the maxilla.
Hansen LS, Eversole LR, Green TL, Powell NB. Clear Both osteo- and chondrosarcomas are rap-
cell odontogenic tumor—a new histologic variant with idly growing neoplasms with a propensity
aggressive potential. Head Neck Surg. 1985;8:115.
Kunze E, Donath K, Luhr HG, Engelhardt W, De Vivie
for distant rather than nodal metastasis.
R. Biology of metastasizing ameloblastomas. Pathol Expansion, pain, and paresthesia are com-
Res Pract. 1985;180:526. mon features.
PMPH_Eversole_Chapter-09.indd 453 1/20/2011 3:02:12 PM
454 Chapter 9
FIGURE 9-70
Poorly marginated radiolu-
cencies of the mandible in
osteogenic sarcoma.
MICROSCOPIC FEATURES reticulum cell sarcoma, Ewing’s sarcoma,
Osteogenic sarcoma exists in three histo- neurosarcoma, and fibrosarcoma of bone.
morphologic variations: osteoblastic, chon- Biopsy is required to obtain a definitive
droblastic, and fibroblastic. The latter is diagnosis.
most often radiolucent. The histology can-
not be correlated with prognostic predict- TREATMENT
ability. Chondrosarcomas generally contain Hemimandibulectomy or maxillectomy is
hyaline cartilage with pleomorphic chon- required. Radium needle implants, followed
droblasts. A specific histologic variant, the by resection, have also been employed. The
mesenchymal chondrosarcoma, has a pre- 5-year survival for osteogenic sarcoma of the
dilection for the jaws. These tumors contain jaws is less than 50%. Mandibular tumors
little identifiable hyaline cartilage, but are show a better prognosis than those arising
composed of immature hypercellular spin- in the maxilla. Because regional metastases
dle and stellate cells with intervening baso- are extremely rare, prophylactic neck dis-
philic ground substance. Focal areas are section is not indicated.
traversed by cleft-like channels reminiscent
of hemangiopericytoma.
Additional Reading
DIFFERENTIAL DIAGNOSIS Azizi T, Motamedi MH, Jafari SM. Gnathic osteosarco-
Osteo- and chondrosarcomas of moth-eaten mas: a 10-year multi-center demographic study. Indian
J Cancer. 2009;46:231-233.
radiolucent pattern resemble metastatic Chaudhry AP, Robinovitch MR, Mitchell DF, Vickers
carcinoma, intra-alveolar carcinoma, and RA. Chondrogenic tumors of the jaws. Am J Surg.
other mesenchymal malignancies such as 1961;102:403.
PMPH_Eversole_Chapter-09.indd 454 1/20/2011 3:02:18 PM
Radiolucent Lesions of the Jaws 455
Christensen RE. Mesenchymal chondrosarcoma of the reaction or cortical redundancy (onion
jaws. Oral Surg Oral Med Oral Pathol. 1982;54:197. skinning) is demonstrable. If left untreated,
Garrington GE, Collett WK. Chondrosarcoma I & II.
J Oral Pathol Med. 1988;17:1:12. widespread metastasis to other bones and
Garringon GE, Scofield HH, Cornyn J, Hooker SP. visceral organs ensues rapidly. In Ewing’s,
Osteosarcoma of the jaws. Analysis of 56 cases. Cancer. the (11;22)(q24;q12) chromosomal transloca-
1967;20:377. tion that encodes the EWS/FLI oncoprotein
is involved in most cases.
EWING’S SARCOMA MICROSCOPIC FEATURES
Figure 9-71
The tumor is composed of diffuse sheets of
Age: Teenagers hyperchromatic round cells with virtually
Sex: Male predilection no fibrous stroma. Septae traverse the neo-
plastic element, and tumor cells tend to ori-
CLINICAL AND RADIOGRAPHIC
FEATURES ent themselves about blood vessels. Multi-
focal zones of necrosis are commonly seen
Ewing’s sarcoma is a rare primary malig- CD99 is positive.
nant mesenchymal neoplasm of bone. The
true cell of origin is unknown, but it is prob- DIFFERENTIAL DIAGNOSIS
ably an undifferentiated osseous mesen-
Ewing’s sarcoma may radiographically and
chymal cell. The disease is most frequently
clinically resemble osteomyelitis. Particu-
encountered in the long bones of the lower
larly when onion skinning is present, con-
extremities, but may appear initially in the
fusion with Garré’s periostitis may arise.
jaws, usually the mandible. Expansion with
The moth-eaten expansile radiographic
pain, paresthesia, or anesthesia usually con-
appearance may also be seen in a variety
stitutes the chief complaint. Unexplained
of bone malignancies, including metastatic
loosening of teeth may also be a feature,
carcinoma, lymphoma, and other bone
and leukocytosis with elevated temperature
sarcomas. Biopsy is required to provide a
is often encountered. Radiographically, the
definitive diagnosis.
tumor is radiolucent with ill-defined mar-
gins. Expansion or erosion of the cortex is TREATMENT
observed, and occasionally, an osteophyte
Ewing’s sarcoma is a highly malignant neo-
plasm with a 5-year survival of less than
10%. The disease is treated by multidrug
chemotherapy and should be managed by
an oncologist. Treatment is usually by radi-
ation and chemotherapy. Surgical interven-
tion is occasionally attempted. Teeth should
be extracted before radiation therapy when
they are embedded in tumor.
Additional Reading
Bacchini P, Marchetti C, Mancini L, Present D, Bertoni
F, Stea G. Ewing’s sarcoma of the mandible and max-
illa. A report of three cases from the Instituto Beretta.
FIGURE 9-71 Oral Surg Oral Med Oral Pathol. 1986;61:278.
Moth-eaten radiolucent lesion of tuberosity in a Carl W, Schaaf NG, Gaeta J, Sinks LF. Ewing’s sarcoma.
child with Ewing’s sarcoma. J Oral Maxillofac Surg. 1971;31:472.
PMPH_Eversole_Chapter-09.indd 455 1/20/2011 3:02:26 PM
456 Chapter 9
Crowe WW, Harper JC. Ewing’s sarcoma with pri- clinical features include expansion, pain
mary lesion in mandible. J Oral Maxillofac Surg. or paresthesia, and unexplained loosening
1965;23:156.
Potdar GG. Ewing’s tumors of the jaws. Oral Surg Oral of teeth. Radiographically, the medullary
Med Oral Pathol. 1970;29:505. bone shows significant osseous destruc-
Toomey EC, Schiffman JD, Lessnick SL. Recent advanc- tion or merely a loss of trabeculation with
es in the molecular pathogenesis of Ewing’s sarcoma. ill-defined margins. Cortical expansion or
Oncogene. 2010;29:4504-4516.
perforation is often demonstrable radio-
graphically. In HIV-infected patients, cen-
PRIMARY LYMPHOMA OF tral jaw lymphomas may resemble Burkitt’s
BONE or may represent plasmablastic lymphoma, an
AIDS-specific oral lymphoma.
Figure 9-72
Age: Young adults MICROSCOPIC FEATURES
Sex: Male predilection The biopsy specimen shows diffuse sheets
CLINICAL AND RADIOGRAPHIC of oval-to-round nucleated cells separated
FEATURES by scant or often undiscernible stroma. The
nuclei are larger than those of mature lym-
Primary lymphoma that originates from
phocytes, and the nucleoplasm is moderately
bone marrow lymphoid precursor cells
stained with stippling. Most are classified as
is generally of the non-Hodgkin’s variety,
diffuse large B-cell lymphomas. Plasmablas-
lymphocytic and/or histiocytic type. This
tic lymphoma shows microscopic features
form was, in the past, referred to as reticu-
similar to anaplastic multiple myeloma.
lum cell sarcoma of bone. The pelvis and
long bones of the lower extremities are the
DIFFERENTIAL DIAGNOSIS
usual sites of origin, yet the jaws may be
involved initially or jaw lesions may accom- Ill-defined moth-eaten radiolucencies with
pany tumor in other osseous sites. The pain, typical of primary lymphoma of bone,
FIGURE 9-72
Irregular, poorly defined
radiolucencies representing
primary lymphoma of bone.
PMPH_Eversole_Chapter-09.indd 456 1/20/2011 3:02:28 PM
Radiolucent Lesions of the Jaws 457
are also features of osteomyelitis. In the lat- Sarode SC, Sarode GS, Patil A. Plasmablastic lymphoma
ter, an infectious source, usually odonto- of the oral cavity: a review. Oral Oncol. 2010;46(3):146-
153.
genic, is detectable; expansion of the cortex Wen BC, Zahra MK, Hussey DH, Doornbos JF, Vigliotti
is unusual. These same radiographic fea- A. Primary malignant lymphoma of the mandible.
tures are seen with Ewing’s sarcoma, other J Surg Oncol. 1988;39:39.
primary sarcomas of osteogenic mesenchy-
mal tissue, and metastatic carcinoma. The
diagnosis requires microscopic evaluation. BURKITT’S LYMPHOMA
Once the diagnosis has been secured, a Figure 9-73
complete blood count should be performed
to rule out leukemia with infiltration into Age: Children
bone. Sex: Male predilection
CLINICAL AND RADIOGRAPHIC
TREATMENT FEATURES
Radiation therapy with or without chemo- Burkitt’s (African) lymphoma is a unique
therapy is the treatment of choice and should form of lymphoma found primarily in
be performed by an oncologist or radia- Uganda and Kenya. Clinically similar cases
tion therapist. Teeth should be extracted have been discovered in the United States.
from the radiation field before therapy. The The unique character of the disease rests
prognosis is poor and even worse for plas- with the predilection for tumor to involve
mablastic lymphoma. certain organs and locations, namely the
jaws, abdominal nodes, and ovaries. Other
Additional Reading visceral tissues may be infiltrated as well.
The disease occurs in a specific geographic
Djavanmardi L, Oprean N, Alantar A, Bousetta K, Princ locale and at specific ranges in altitude,
G. Malignant non-Hodgkin’s lymphoma (NHL) of the implicating an insect vector of transmis-
jaws: a review of 16 cases. J Craniomaxillofac Surg. sion. Accumulating evidence suggests that
2008;36(7):410-414.
Gerry RG, Williams SF. Primary reticulum cell sarcoma
the Epstein-Barr virus may be causative
of the mandible. Oral Surg Oral Med Oral Pathol. (the same virus that causes the benign
1955;8:568. lymphoproliferative disorder infectious
Keszler A, Piloni MJ, Paparella ML, Soler Mde D, mononucleosis). Clinically, the tumor is
Ron PC, Narbaitz M. Extranodal oral non-Hodg-
kin’s lymphomas. A retrospective study of 40 cases
capable of massive growth with signifi-
in Argentina. Acta Odontol Latinoam. 2008;21(1): cant expansion and facial disfigurement
43-48. with loosening and displacement of teeth.
FIGURE 9-73
Diffuse, destructive lesion
in Burkitt’s lymphoma.
(Courtesy of Dr. George
Chew.)
PMPH_Eversole_Chapter-09.indd 457 1/20/2011 3:02:39 PM
458 Chapter 9
Abdominal distention from node and vis- The care of the patient should be managed
ceral lesions is common. Radiographically, by a medical oncologist.
massive destruction of bone is observed
with a moth-eaten, poorly marginated, pat-
tern. The cortex shows expansion or erosion Additional Reading
and perforation. Destruction of developing
Adatia AK. Significance of jaw lesions in Burkitt’s lym-
tooth buds is commonly seen. There is evi- phoma. Br Dent J. 1978;145:263.
dence that Epstein-Barr virus may induce a Anavi Y, Kaplinsky C, Calderon S, Zaizov R. Head, neck,
translocation of the MYC gene, forming a and maxillofacial childhood Burkitt’s lymphoma: a ret-
fusion protein with immunoglobulin pro- rospective analysis of 31 patients. J Oral Maxillofac
Surg. 1990;48:708.
moter sequences. Burkitt D. A sarcoma involving the jaws in African chil-
dren. Br J Surg. 1958;48:218.
MICROSCOPIC FEATURES Lehner T. The jaws and teeth in Burkitt’s tumor (African
lymphoma). J Pathol. 1964;88:581.
Diffuse sheets of mature lymphocytes are Terril DG, Lee A, LeDonne MA, Nusbaum TG. American
seen, and the tumor is essentially devoid Burkitt’s lymphoma in Pittsburgh, Pennsylvania. Oral
of fibrous stroma. Reticulum stains show a Surg Oral Med Oral Pathol. 1977;44:411.
profuse network of reticulum around tumor
cells. The pathognomonic microscopic pat-
tern of Burkitt’s lymphoma, referred to as FIBROGENIC AND
the “starry-sky” appearance, is character- NEUROGENIC SARCOMA
ized by multiple foci of large pale-staining Figure 9-74
histiocytic cells with vesicular nuclei and
generous amounts of cytoplasm dispersed Age: Young and middle-aged adults
randomly within a sea of darker staining Sex: No predilection
lymphoid cells. CLINICAL AND RADIOGRAPHIC
FEATURES
DIFFERENTIAL DIAGNOSIS
Sarcomas derived from fibroblasts or nerve
The combination of jaw lesions with sheath (Schwann cells, perineural fibro-
abdominal masses in an African child is blasts) are occasionally encountered in
classic for Burkitt’s lymphoma. In other bone. Indeed, central neurogenic sarcomas
geographic areas, the moth-eaten expan- are encountered more frequently in the
sile radiolucency of Burkitt’s lymphoma mandible than in any other bone, probably
must be differentiated from other lesions because of the unique anatomy by which
occurring with equal or greater frequency. the alveolar nerve traverses a long distance
Osteomyelitis may show similar features, while encased in bone. The chief clini-
but expansion is uncommon. Other sarco- cal findings include paresthesia, swelling,
mas of bone as well as metastatic childhood and loosening of teeth. Both fibrosarcomas
tumors (e.g., neuroblastoma, nephroblas- and neurosarcomas manifest as ill-defined
toma) must be included in the differential radiolucencies, which may cause root
diagnosis. Biopsy discloses the character- resorption or divergence. Expansion may
istic histomorphologic features of Burkitt’s be obvious; however, large areas of osseous
lymphoma. destruction may evolve in the absence of
any expansion. Neurosarcomas often pro-
TREATMENT
duce a fusiform widening of the inferior
This form of lymphoma is fatal, but chemo- alveolar canal, tending to grow along the
therapy effects remarkable tumor shrink- course of the nerve as high as the Gasserian
age and accounts for extended remissions. ganglion.
PMPH_Eversole_Chapter-09.indd 458 1/20/2011 3:02:49 PM
Radiolucent Lesions of the Jaws 459
FIGURE 9-74
Ill-defined radiolucency in mandible representing a central fibrosarcoma. Computed tomography showing
invasive myofibrosarcoma with skull base invasion.
MICROSCOPIC FEATURES pling for microscopic evidence of tumor, is
Both fibrogenic and neurogenic sarco- advisable. Central fibrosarcoma has a better
mas are hypercellular spindle cell prolif- prognosis in the jaws than it does in other
erations displaying little or only moderate bones. The 5-year survival exceeds 50%.
pleomorphism. Mitotic figures are usually
numerous. The tumor cells grow in parallel
fascicles, and palisading may be a feature of
Additional Reading
neural sheath malignancies. This feature is David DJ, Speculand B, Vernon-Roberts B, Sach RP.
not a constant, however, and proof of origin Malignant schwannoma of the inferior dental nerve.
Br J Plast Surg. 1978;31:323.
from nerve sheath requires the demonstra- Eversole LR, Schwartz WD, Sabes WR. Central and
tion of continuity between an intact nerve peripheral fibrogenic and neurogenic sarcoma of
and the circumneural tumor mass. the oral regions. Oral Surg Oral Med Oral Pathol.
1973;36:49.
Pereira CM, Jorge J, Jr, Di Hipólito O, Jr, Kowalski LP,
DIFFERENTIAL DIAGNOSIS
Lopes MA. Primary intraosseous fibrosarcoma of jaw.
An ill-defined enlargement of the inferior Int J Oral Maxillofac Surg. 2005;34(5):579-581.
alveolar canal in conjunction with paresthe- Sadoff RS, Rubin MM. Fibrosarcoma of the mandible: a
case report. J Am Dent Assoc. 1990;121:247.
sia is highly suggestive of central neurogenic Van Blarcom CW, Masson JK, Dahlin DC. Fibrosarcoma
sarcoma. Because both fibrosarcoma and of the mandible: a clinicopathologic study. Oral Surg
neurosarcoma may show an expansile moth- Oral Med Oral Pathol. 1972;32:428.
eaten radiolucency with or without resorp-
tion of adjacent teeth, other malignant tumors
including metastatic cancer and primary sar- MELANOTIC
comas of bone must be included in the dif- NEUROECTODERMAL TUMOR
ferential diagnosis. Microscopic evaluation is OF INFANCY
necessary to secure a definitive diagnosis. Figure 9-75
TREATMENT Age: Infancy
Sex: No predilection
Surgical resection, hemimandibulectomy,
or partial maxillectomy, including at least 3 CLINICAL AND RADIOGRAPHIC
cm of tumor-free margin, is the treatment FEATURES
of choice. In the case of neurosarcoma, dis- Melanotic neuroectodermal tumor of infancy
section of the inferior alveolar nerve, sam- is a benign neoplasm derived from neural
PMPH_Eversole_Chapter-09.indd 459 1/20/2011 3:02:49 PM
460 Chapter 9
FIGURE 9-75
Displaced developing inci-
sor with underlying, poorly
marginated radiolucency in
melanotic neuroectodermal
tumor of infancy.
crest cells with a propensity to involve tooth- neuroblast, with a round hyperchromatic
bearing regions in the maxilla. The precise nucleus with sparse or unidentifiable cyto-
origin is controversial. At one time, this neo- plasm. These two types coexist in the alve-
plasm was classified with the odontogenic olar clusters.
tumors; however, cases have been reported
in the skull, shoulder region, testes, and DIFFERENTIAL DIAGNOSIS
uterus. Some cells within the dental papil- The poorly marginated borders of melan-
lae have been shown to derive from neural otic neuroectodermal tumor would appear
crest precursors, so the tumor may repre- to support a radiologic diagnosis of malig-
sent a neuroectodermal odontogenic lesion nancy. Similar features may, of course, be
when it arises in the jaws. Early theories sug- seen in any of the malignant bone tumors
gested origin from ectopic retinal tissues. included among the moth-eaten radiolucen-
These theories account for the various terms cies; however, none of the malignant osseous
applied to this neoplasm (pigmented amelo- neoplasms shows a tendency to arise in
blastoma, retinal anlage tumor, progonoma). infants. Therefore, a maxillary aggressive-
The neoplasm is rarely encountered after 6 appearing radiolucent lesion in a neonate
months of age and, as previously stated, is should arouse suspicion that one is dealing
more often seen in the maxilla than the man- with neuroectodermal tumor. Because sar-
dible. Clinically, the edentulous alveolus of comas do occasionally arise in early child-
the infant shows a smooth-surfaced bulging hood, biopsy confirmation is mandatory.
and is generally nonpigmented. Radiograph-
ically, the lesion is radiolucent with irregu- TREATMENT
lar, ill-defined margins. Developing teeth
may lie within the radiolucent area or are Local curettage is the treatment of choice
significantly displaced by the neoplasm. As for this benign neoplasm. Recurrences have
with other neoplasms of neuroblastic origin, been recorded; however, most lesions can
vanillylmandelic acid may be detected in be cured without resorting to en bloc resec-
the urine. Apparently, some of these tumors, tion. Because metastasis has occurred in a
albeit few, are capable of metastasis. few cases, a complete radiologic evaluation
should be performed, and close periodic
MICROSCOPIC FEATURES follow-up is recommended.
The tumor is composed of alveolar nests
of cells oriented about cleft-like spaces,
with a surrounding dense fibrous stroma.
Additional Reading
Two cell types are encountered: an epithe- Allen MS, Jr, Harrison W, Jahrsdoerfer RA. “Retinal
anlage” tumors; melanotic progonoma, melanotic ada-
lioid polygonal cell with an oval vesicular mantinoma, pigmented epulis, melanotic neurecto-
nucleus is seen to contain melanin gran- dermal tumor of infancy, benign melanotic tumor of
ules, and the other cell type resembles a infancy. Am J Clin Pathol. 1969;51:309.
PMPH_Eversole_Chapter-09.indd 460 1/20/2011 3:02:56 PM
Radiolucent Lesions of the Jaws 461
Borello E, Gorlin RJ. Melanotic neuroectodermal tumor secondary anomalies. The chief features
of infancy—a neoplasm of neural crest origin; report of include nevoid basal cell carcinomas, one or
a case associated with high urinary excretion of vanil-
mandelic acid. Cancer. 1966;19:196. more bifid ribs, and multiple odontogenic
Chaudhary A, Wakhlu A, Mittal N, Misra S, Mehrotra keratocysts of the jaws. The basal cell lesions
D, Wakhlu AK. Melanotic neuroectodermal tumor have limited growth potential, arise during
of infancy: 2 decades of clinical experience with 18 childhood or early adulthood, and appear in
patients. J Oral Maxillofac Surg. 2009;67(1):47-51.
Gotcher JE, Jaffrey BJ, Hudson JW, Lozzio B, Chase
regions of the skin not necessarily exposed to
DC. Recurrent melanotic neuroectodermal tumor of solar radiation. The keratocysts are multiple;
infancy: report of case and tumor heterotransplanta- they may be interradicular or pericoronal
tion studies. J Oral Maxillofac Surg. 1980;38:702. well-delineated unilocular radiolucencies;
Judd PL, Harrop K, Becker J. Melanotic neuroectoder-
mal tumor of infancy. Oral Surg Oral Med Oral Pathol.
some may be multilocular. Cortical expan-
1990;69:723. sion in larger cysts is obvious clinically as
well as radiographically. Other anomalies
seen in the syndrome include frontal boss-
Multifocal Radiolucencies ing, hypertelorism, calcified falx cerebri,
prognathism, and palmar-plantar hyperker-
BASAL CELL NEVUS atosis. Individuals with this disorder are also
SYNDROME prone to develop medulloblastomas, malig-
Figure 9-76 nant posterior fossa brain tumors. Perturba-
tions in the sonic hedgehog growth pathway
Age: Teenagers involve mutations in the PTCH gene, molecu-
Sex: No predilection
lar lesions that are found in both keratocysts
CLINICAL AND RADIOGRAPHIC and nevoid basal cell tumors.
FEATURES
The basal cell nevus syndrome is an auto- MICROSCOPIC FEATURES
somal dominant genetic disease charac- The keratocysts of the basal cell nevus syn-
terized by a primary triad with variable drome do not differ from those seen as
FIGURE 9-76
Basal cell nevus syndrome with bifid rib and multiple odontogenic keratocysts.
PMPH_Eversole_Chapter-09.indd 461 1/20/2011 3:03:03 PM
462 Chapter 9
solitary lesions. The lumen contains lami- LANGERHANS CELL
nations of keratin. The lining epithelium HISTIOCYTOSIS
displays a corrugated surface, attenuated Figure 9-77
spinous layer, and polarized basal cell
layer. Age: Children and young adults
Sex: Male predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL AND RADIOGRAPHIC
The multifocal radiolucencies, particularly FEATURES
when many of them are pericoronal, in
Histiocytosis or Langerhans cell granulo-
conjunction with bifid ribs and basal cell
matosis, a histiocytic proliferative disor-
tumors are classic for the basal cell nevus
der of the reticuloendothelial system and
syndrome. From the radiographs of the jaw
bone, exists in three forms: acute dissemi-
alone, the multifocal radiolucencies may
nated, chronic disseminated, and chronic
resemble multiple keratocysts without other
limited variants. The latter two, previously
features of the syndrome, multiple dentiger-
termed Hand-Schuller-Christian disease
ous cysts, or even histiocytosis. The latter
and eosinophilic granuloma, respectively,
rarely shows expansion.
are dealt with here because they are more
TREATMENT apt to involve the jaws. Chronic dissemi-
nated histiocytosis manifests a classic triad
Thorough curettage of the jaw cysts is of features: exophthalmos from retro-orbital
required. Chemical cautery of the bony infiltration, diabetes insipidus owing to pos-
crypt may be performed. Recurrences are terior pituitary histiocytic infiltrates, and
common and require repeated surgical osseous lesions. Otitis media and lung infil-
intervention. The basal cell nevi may be trations are also common. This form occurs
too numerous to remove; however, they in children and teenagers. Chronic limited
generally are not aggressive as are ordi- histiocytosis is more often seen in young
nary basal cell carcinomas. Most cases adults, is generally limited to bone with
are sporadic yet hereditary linked cases either solitary or multifocal osseous defects,
are occasionally encountered. A thorough and occasionally manifests pulmonary infil-
neurologic work-up with periodic exami- trates. Jaw lesions in all forms of the disease
nations should be carried out to rule out show similar features. Pain and expansion
medulloblastoma. are usually absent. Teeth may become loose
for no apparent reason, and the gingiva
Additional Reading may appear inflamed in involved areas.
The lesions are more common in the man-
Anderson DE, Cook WA. Jaw cysts and the basal cell dible than maxilla and are often, yet not
nevus syndrome. J Oral Maxillofac Surg. 1966;24:15.
Giansānti JS, Baker GO. Nevoid basal cell carcinoma
invariably, multifocal irregular radiolucen-
syndrome in Negroes: report of five cases. J Oral cies lacking marginal cortication. When the
Maxillofac Surg. 1974;32:138. alveolus is involved, the teeth may give the
Gorlin RJ, Vickers RA, Kellen E, Williamson JJ. The mul- impression that they are floating in space,
tiple basal-cell nevi syndrome. Cancer. 1965;18:89.
Koutnick AW, Kolodny SC, Hooker SP, Roche WC.
because they may be entirely encompassed
Multiple nevoid basal cell epithelioma, cysts of the by a radiolucent defect. The skull often con-
jaws, and bifid rib syndrome: report of case. J Oral tains punched-out radiolucencies.
Maxillofac Surg. 1975;33:686.
Saran A. Basal cell carcinoma and the carcinogen- MICROSCOPIC FEATURES
ic role of aberrant Hedgehog signaling. Future
Oncol. 2010;6(6):1003-1014. Pediatr Dermatol. Diffuse sheets of histiocytes with pale nuclei
2008;25(3):291-295. and abundant cytoplasm prevail. These
PMPH_Eversole_Chapter-09.indd 462 1/20/2011 3:03:17 PM
Radiolucent Lesions of the Jaws 463
FIGURE 9-77
Radiolucent lesions in
both jaws in a patient
with Langerhans cell
histiocytosis.
cells represent CD1a+ Langerhans cells.
Occasionally, multinucleated histiocytes Additional Reading
and foam cells are encountered. Multiple Chase DC, Eversole LR, Hall H. D. Histiocytosis X with
foci of eosinophilic abscesses are encoun- jaw involvement. J Oral Maxillofac Surg. 1974;32:494.
tered. Fibrous stroma is scant. Granada FM, McDaniel RK. Multiple progressive
eosinophilic granuloma of the jaws. J Oral Maxillofac
Surg. 1982;40:174.
DIFFERENTIAL DIAGNOSIS
Hartman KS. Histiocytosis X: a review of 114 cases with
Multifocal noncorticated radiolucencies of oral involvement. Oral Surg Oral Med Oral Pathol.
1980;49:38.
the jaws may occur in diseases other than the
Rapidis AD, Langdon JD, Harvey PW, Patel MF.
histiocytoses, including multiple myeloma, Histiocytosis X. Analysis of 50 cases. Int J Oral
the basal cell nevus syndrome, and, occa- Maxillofac Surg. 1978;7:76.
sionally, multifocal metastatic carcinoma Satter EK, High WA. Langerhans cell histiocytosis:
and primary lymphoma of bone. Multiple a review of the current recommendations of the
Histiocyte Society. Pediatr Dermatol. 2008;25:291-295.
early-stage periapical cemental dysplasia
must be considered in the differential diag-
nosis when lesions are located at the apex MULTIPLE MYELOMA
of teeth. Biopsy is required for definitive Figure 9-78
diagnosis. A skeletal radiographic survey
should be obtained to check for disease in Age: Middle-aged adults
other bones. Sex: No predilection
CLINICAL AND RADIOGRAPHIC
TREATMENT FEATURES
Chronic disseminated histiocytosis has a Multiple myeloma is a malignant osseous
guarded prognosis. The disease responds to neoplastic disorder of immunoglobulin-se-
chemotherapy, particularly the vinca alka- creting plasma cells. It probably represents a
loids. The chronic limited form with jaw multicentric malignancy, as multiple osseous
lesions can be treated by local curettage. foci of disease may be detected simultane-
PMPH_Eversole_Chapter-09.indd 463 1/20/2011 3:03:17 PM
464 Chapter 9
FIGURE 9-78
Multifocal punched-out
lesions of the jaws, typically
seen in multiple myeloma.
A γ-spike is seen on elec-
trophoresis and immuno-
electrophoresis portrays
light chain restriction for λ.
ously. The jaws, usually the mandible, are As opposed to chronic inflammation with
involved in over one fourth of the cases. a predominance of plasma cells, myeloma
Immunoglobulins, usually of a single class infiltrates lack dense stroma or granulation
and allotype, are detected in serum. Bence- tissue, and other inflammatory cells in vir-
Jones protein, representing globulin frag- gin lesions are not encountered. Amyloid
ments, is often detectable in the urine. When deposits are frequently present. Immu-
the jaw is involved, bone pain and paresthe- noperoxidase techniques can be performed
sia are common complaints. The tumor cells on formalin-fixed sections; the demon-
may perforate the cortex, causing a soft tissue stration of monotypic antibody employ-
bulge or antral invasion. Loosening of teeth ing techniques for class immunoglobulin
may be observed. Radiographically, multiple heavy chains, a single type of light chain,
oval well-demarcated, but noncorticated, or the presence of J-protein is specific for
radiolucencies are observed. Cortical expan- myeloma. Immunoglobulin gene rearrange-
sion is rare, perforation being more common ment assays demonstrate the monoclonal
when the lesions extend to the periphery of nature of the malignancy.
bone. Root resorption may occur. A skel-
etal survey discloses similar lesions in other DIFFERENTIAL DIAGNOSIS
bones, particularly the skull. The punched-out well-defined radiolucen-
cies typical of myeloma may also occur in
MICROSCOPIC FEATURES
histiocytosis, disseminated metastatic car-
Monotonous sheets of relatively well-differ- cinoma, and primary lymphoma of bone.
entiated plasma cells prevail. Mitoses and Multiple keratocysts should be included
multinucleated cells are frequent findings. in the radiographic differential diagnosis.
PMPH_Eversole_Chapter-09.indd 464 1/20/2011 3:03:28 PM
Radiolucent Lesions of the Jaws 465
Microscopic examination is required for a rickets). In both cases, lack of active vitamin
definitive diagnosis. D results in deficient calcium absorption
and incorporation into osteoid. Malabsorp-
TREATMENT tion syndromes such as biliary cirrhosis and
various forms of steatorrhea encountered in
Multiple myeloma has a grave prognosis,
adults are characterized by hypocalcemia.
with 5-year survival of less than 10%. The dis-
Renal osteodystrophy develops in late-
ease is treated by chemotherapy and should
stage glomerular disease as a consequence
be managed by a medical oncologist.
of renal calcium diuresis. Certain drugs,
particularly anticonvulsants, interfere with
Additional Reading enzymatic activation of vitamin D. Onco-
genic osteomalacia is a rare paraneoplastic
Bruce KW, Royer RQ. Multiple myeloma occurring in the syndrome in which certain mesenchymal
jaws. Oral Surg Oral Med Oral Pathol. 1953;6:729. tumors secrete phosphaturic factors lead-
Elias HG, Scott J, Metheny L, Quereshy FA. Multiple
myeloma presenting as mandibular ill-defined radio-
ing to hypophosphatemia. Regardless of
lucent lesion with numb chin syndrome: a case report. the mechanism, osteomalacia is the result
J Oral Maxillofac Surg. 2009;67(9):1991-1996. of hypocalcemia. Radiographically, diffuse
Monje F, Gil-Diez JL, Campano FJ, Alonso del Hoyo rarefaction is observed in both the maxilla
JR. Mandibular lesion as the first evidence of mul-
tiple myeloma. Case report. J Craniomaxillofac Surg.
and the mandible. The density of trabeculae
1989;17:315. per unit area is diminished, and the lamina
Smith DB. Multiple myeloma involving the jaws; review dura may be quite thin. These radiographic
with report of an additional case. Oral Surg Oral Med alterations are often subtle and are not
Oral Pathol. 1957;10:911.
always observed. Pathologic fractures may
Wright BA, Wysocki GP, Bannerjee D. Diagnostic use of
immunoperoxidase techniques for plasma cell lesions of also complicate the condition.
the jaws. Oral Surg Oral Med Oral Pathol. 1981;52:615.
MICROSCOPIC FEATURES
Generalized Osteoporotic Routine histologic examination is not par-
ticularly revealing. During processing,
Lesions decalcification occurs quickly. Otherwise,
the histologic appearance of trabeculae in
OSTEOMALACIA osteomalacia is usually unremarkable.
Figure 9-79
Age: Varies according to pathogenesis
Sex: No predilection
CLINICAL AND RADIOGRAPHIC
FEATURES
Osteomalacia represents a collective of dis-
orders, whereby osteoid is not thoroughly
mineralized. Genetic and acquired deficien-
cies in calcium absorption and incorporation
into bone matrix are responsible. Dietary
vitamin D deficiency, or rickets, occurs in
children as does the hereditary form of
rickets, whereby an enzyme deficiency pre- FIGURE 9-79
cludes the normal activation of vitamin D Diffuse granular trabeculation in osteomalacia sec-
(hypophosphatemic or vitamin D refractory ondary to advanced renal disease.
PMPH_Eversole_Chapter-09.indd 465 1/20/2011 3:03:39 PM
466 Chapter 9
DIFFERENTIAL DIAGNOSIS hormones, particularly estrogen in post-
The diffuse rarefaction of osteomalacia is menopausal women. Mineral content is
basically identical to that seen in osteoporo- not problematic as in osteomalacia; rather,
sis and is similar to the changes observed in the total bone matrix volume decreases.
the other systemic diseases included here. The axial skeleton is involved primarily,
Because many pathogenic mechanisms are and a decrease in stature is evident. Back
involved, a complete medical evaluation pain may be a feature; as the appendicular
is imperative. A biochemical bone panel skeleton becomes progressively involved, a
to evaluate alkaline phosphatase, calcium, minor fall may result in fracture. Jaw radio-
and phosphorus levels is necessary. The graphs in advanced cases show thinning
work-up usually includes renal function of the cortices, being most obvious in the
tests, a renal panel, urinalysis, a liver panel, mandible with a generalized loss of defined
and a skeletal survey. trabeculation. This loss of trabecular defi-
nition may yield a somewhat ground-glass
TREATMENT or granular pattern with an overall general
radiolucent appearance. The biochemical
Referral to an internist is recommended. bone panel generally is within normal lim-
Treatment consists of establishing an appro- its. Studies comparing mandibular corti-
priate calcium balance and is based on ces on panoramic films fail to differentiate
determining the underlying pathogenetic osteoporosis from normal bone densities.
mechanism of the problem.
MICROSCOPIC FEATURES
Additional Reading In osteoporosis, low-power assessment dis-
closes a thinning of the cortical bone with a
Dupond JL, Mahammedi H, Prié D, et al. Oncogenic decreased ratio of trabeculae to marrow. The
osteomalacia: diagnostic importance of fibroblast medullary trabeculae are thin and atrophic
growth factor 23 and F-18 fluorodeoxyglucose PET/
CT scan for the diagnosis and follow-up in one case. without evidence of osteoblastic rimming.
Bone. 2005;36(3):375-378.
McCarthy JT, Kumar R. Renal osteodystrophy. DIFFERENTIAL DIAGNOSIS
Endocrinol Metab Clin North Am. 1990;19:65.
Reynolds WA, Karo JJ. Radiologic diagnosis of metabolic
Senile or postmenopausal osteoporosis is
bone disease: symposium on metabolic bone disease. radiographically indistinguishable, in the
Orthop Clin North Am. 1972;3:521.
Sparagana M. Tumor-induced osteomalacia: Long-term
follow-up of two patients cured by removal of their
tumors. J Surg Oncol. 1987;36:198.
Stafne EC. Dental roentgenologic manifestations of sys-
temic disease. Radiology. 1952;58:507, 820.
SENILE OSTEOPOROSIS
Figure 9-80
Age: Elderly adults
Sex: Predominantly females
CLINICAL AND RADIOGRAPHIC
FEATURES
FIGURE 9-80
Senile osteoporosis develops with ensuing Senile osteoporosis with loss of cortical promi-
age in conjunction with decreased anabolic nence and altered trabeculation.
PMPH_Eversole_Chapter-09.indd 466 1/20/2011 3:03:40 PM
Radiolucent Lesions of the Jaws 467
jaws, from osteomalacia or steroid osteo- gus, or mixed collagen diseases is usually
porosis. The hemolytic anemias generally effected by using steroid medication. High
have a distinctive altered and unusual tra- doses over a prolonged period result in
becular pattern. cushingoid changes. Prolonged elevation
of cortisone or steroid analogues result in
TREATMENT generalized osteoporosis affecting both the
These elderly patients should limit their axial and appendicular skeleton, including
physical activities while maintaining proper the skull and jaws. Radiographically, the
and balanced nutrition. Referral to a physi- changes mimic those seen in senile osteopo-
cian is recommended. rosis with thin cortices, attenuated lamina
dura, and generalized granular rarefaction.
Additional Reading MICROSCOPIC FEATURES
The cortices are thin, and the medullary
Conacher WD. Metabolic bone disease in the elderly.
Practitioner. 1973;210:351.
trabeculae are scant with abundant soft tis-
Drozdzowska B, Pluskiewicz W, Tarnawska B. Panoramic- sue marrow.
based mandibular indices in relation to mandibular
bone mineral density and skeletal status assessed by DIFFERENTIAL DIAGNOSIS
dual energy X-ray absorptiometry and quantitative
ultrasound. Dentomaxillofac Radiol. 2002;31(6):361- The diffuse rarefaction of steroid osteopo-
367. rosis is essentially identical to that seen in
Kribbs PJ. Comparison of mandibular bone in normal and senile osteoporosis. A history of systemic
osteoporotic women. J Prosthet Dent. 1990;63:218.
steroid medication or Cushing’s syndrome
Warren R. Osteoporosis. J Oral Pathol Med.
1977;32:113. establishes the diagnosis.
Watson L. Endocrine bone disease. Practitioner.
1973;210:376. TREATMENT
Cushing’s syndrome can be treated by sur-
gical removal of the adrenal or pituitary
STEROID OSTEOPOROSIS
tumor. Osteoporosis secondary to steroid
Figure 9-81 administration can be minimized to some
Age: Varies according to pathogenesis extent by prescribing the drug during early
Sex: No predilection morning hours, which coincide with physi-
ologic secretion peaks.
CLINICAL AND RADIOGRAPHIC
FEATURES
Osteoporotic changes develop in patients
with elevated blood corticosteroids. In
Cushing’s syndrome, either an adrenal
cortical adenoma or a pituitary corticotro-
pin-secreting tumor with adrenal cortical
hyperplasia exists. Clinically, the facial tis-
sues are edematous, yielding the so-called
moon facies; other features include upper
trunk adiposity, hypertension, and hyper-
glycemia. Elevated urine 17-ketosteroid
and elevated serum cortisol levels can be
detected. Treatment of immunopathic disor- FIGURE 9-81
ders such as lupus erythematosus, pemphi- Cushing’s syndrome with loss of trabecular markings.
PMPH_Eversole_Chapter-09.indd 467 1/20/2011 3:03:43 PM
468 Chapter 9
HbC) may be encountered in sickle cell dis-
Additional Reading ease. Oxygen tension is low, and erythrocytes
Crilly RG, Horsman A, Marshall DH, Nordin BE. Post- carrying this abnormal reduced hemoglobin
menopausal and corticosteroid-induced osteoporosis. assume altered morphology (sickled forms).
Front Horm Res. 1977;5:53. During a crisis, sludging of cells occurs with
Duncan H. Osteoporosis in rheumatoid arthritis and formation of microthrombi. A severe crisis
corticosteroid-induced osteoporosis: symposium
on metabolic bone disease. Orthop Clin North Am. can be fatal. A compensatory bone marrow
1972;3:571. erythroblastic hyperplasia develops and
Liu RH, Werth VP. What is new in the treatment of leads to generalized osteoporotic changes
steroid-induced osteoporosis? Semin Cutan Med Surg. radiographically. The clinical features
2007;26(4):203-209.
Lukert BP, Raisz LG. Glucocorticoid-induced osteopo-
include weakness, dyspnea, pallor, and gen-
rosis: pathogenesis and management. Ann Intern Med. eralized body pains. Jaw radiographs show a
1990;112:352. reduction in the number of trabeculae; those
Stafne EC, Lovestedt SA. Osteoporosis of the jaws asso- that remain are clearly defined and appear
ciated with hypercortisonism. Oral Surg Oral Med
Oral Pathol. 1960;13:1445.
thickened. Some cases show a so-called step-
ladder appearance with parallel horizontal
trabeculation in the interradicular zone. The
SICKLE CELL ANEMIA cortices are thin.
Figure 9-82
MICROSCOPIC FEATURES
Age: Childhood onset The microscopic features are not particu-
Sex: No predilection
larly diagnostic. Careful search for sick-
CLINICAL AND RADIOGRAPHIC led erythrocytes within vessels should be
FEATURES undertaken.
Sickle cell anemia is an autosomal recessive
inherited disease that affects less than 1% of DIFFERENTIAL DIAGNOSIS
the black population, in which a defective The step-ladder effect and reduced trabe-
hemoglobin molecule is synthesized. This culation may be seen in normal patients.
abnormal hemoglobin (HgS) can be detected Similar radiographic changes may also
with the use of hemoglobin electrophoresis. be encountered in thalassemia. The other
Other abnormal hemoglobin molecules (e.g., osteoporoses appear more granular on jaw
radiographs. When the aforementioned
radiographic features are encountered in
black children, sickle cell anemia should be
considered; a complete blood count, testing
for sickle cell phenomenon, and hemoglo-
bin electrophoresis should be ordered.
TREATMENT
There is no effective treatment. Parental
genetic counseling is recommended.
FIGURE 9-82
Additional Reading
Step-ladder trabeculation in sickle cell anemia. Demirbaş AK, Ergün S, Güneri P, Aktener BO,
(Courtesy of Dr. R. Sanger.) Boyacioğlu H. Mandibular bone changes in sickle cell
PMPH_Eversole_Chapter-09.indd 468 1/20/2011 3:03:44 PM
Radiolucent Lesions of the Jaws 469
anemia: fractal analysis. Oral Surg Oral Med Oral prominent malar region, incisor flaring,
Pathol Oral Radiol Endod. 2008;106(1):e41-e48. and depressed nasal bridge are common
Mourshed F, Tuckson CR. A study of the radiographic
features of the jaws in sickle-cell anemia. Oral Surg findings. Jaw and dental radiographic
Oral Med Oral Pathol. 1974;37:812. changes are not seen in every case; when
Reynolds J. An evaluation of some roentgenographic present, the patient usually suffers from
signs in sickle-cell anemia and its variants. South Med the β-major form of the disease. Various
J. 1962;55:1123.
Sanger RO, Greer RO, Auerbach RE. Differential diag-
radiographic changes have been reported
nosis of some simple osseous lesions associated with and include thinning of cortices, spiked
sickle-cell anemia. Oral Surg Oral Med Oral Pathol. roots, taurodonts, calcified inferior alveolar
1977;43:538. canal, diffuse rarefaction with decreased
Sears RS. The effects of sickle-cell disease on dental and
skeletal maturation. ASDC J Dent Child. 1981;48:275.
yet prominent trabeculation, and in some
instances, a diffuse and unmarginated
honeycomb appearance. Skull radiographs
THALASSEMIA MAJOR often show vertical osteophytes emanating
Figure 9-83 from the inner table of the calvarium pro-
ducing the hair-on-end effect.
Age: Childhood onset
Sex: No predilection
MICROSCOPIC FEATURES
CLINICAL AND RADIOGRAPHIC
FEATURES Biopsy that includes hematopoietic marrow
or bone marrow aspiration smears discloses
Thalassemia, found predominantly among hypochromic microcytes with poikilocy-
Italians and Greeks, is a hemoglobinopa- tosis and anisocytosis. Large numbers of
thy with resultant hemolytic anemia that immature erythroblastoid cells are present,
represents a heritable defect in either indicating a maturation arrest.
the α- or β-hemoglobin chain. Elevated
fetal hemoglobin (HbF) level is present
DIFFERENTIAL DIAGNOSIS
in erythrocytes and can be quantitated,
using hemoglobin electrophoretic tech- The radiographic features simulate, to some
niques. Major and minor β- (Cooley’s ane- extent, those changes observed in sickle
mia) and α-forms exist with full expres- cell anemia. Serum levels of unconjugated
sion in the homozygous forms. Clinically, bilirubin are elevated, and hemoglobin
homozygotes are affected from birth or electrophoresis discloses elevated amounts
early childhood; pallor, malaise, and par- of HbF. The aforementioned bone marrow
oxysmal fever occur. Splenomegaly and and peripheral blood changes are also of
appearance of mongoloid features with diagnostic importance.
FIGURE 9-83
Multifocal honeycomb tra-
beculation in thalassemia
major. (Courtesy of Dr.
H.G. Poyton.)
PMPH_Eversole_Chapter-09.indd 469 1/20/2011 3:03:46 PM
470 Chapter 9
TREATMENT Cannell H. The development of oral and facial signs in
beta-thalassaemia major. Br Dent J. 1988;164:50.
No effective treatment exists. Iron chelating Choremis C, Liakakos D, Tseghi C, Moschovakis
agents are administered orally to remove C. Pathogenesis of osseous lesions in thalassemia.
excessive iron. Genetic counseling is rec- J Pediatr. 1965;66:962.
Hazza’a AM, Al-Jamal G. Radiographic features of the
ommended for parents.
jaws and teeth in thalassaemia major. Dentomaxillofac
Radiol. 2006;35(4):283-288.
Additional Reading Poyton HG, Davey KW. Thalassemia: changes visible
in radiographs used in dentistry. Oral Surg Oral Med
Oral Pathol. 1968;25:564.
Alexander WN, Bechtold WA. Alpha thalassemia minor
trait accompanied by clinical oral signs. Oral Surg Oral
Med Oral Pathol. 1977;43:892.
PMPH_Eversole_Chapter-09.indd 470 1/20/2011 3:03:55 PM
PMPH_Eversole_Chapter-09.indd 471 1/20/2011 3:03:55 PM
a b c
Focal opacity Target lesion, floccular Target lesion, dense
d e f
Multifocal confluent Irregular Cortical redundancy
g h i
Ground glass Mixed lucent-opaque Soft tissue opacity
j k
Periapical Interradicular
l m
Edentulous zone Pericoronal
Radiopaque Lesions of the Jaws
PMPH_Eversole_Chapter-10.indd 472 1/20/2011 3:04:49 PM
Radiopaque Lesions
of the Jaws 10
ODONTOMA 498
Periapical Radiopacities 475
ODONTOAMELOBLASTOMA 499
PERIAPICAL CEMENTAL
DYSPLASIA 475 Target Lesions*
FOCAL CEMENTO-OSSEOUS
DYSPLASIA 477 PERIAPICAL CEMENTAL DYSPLASIA
FOCAL SCLEROSING FOCAL CEMENTO-OSSEOUS
OSTEOMYELITIS 479 DYSPLASIA
FOCAL PERIAPICAL FOCAL SCLEROSING
OSTEOSCLEROSIS 480 OSTEOMYELITIS
BENIGN CEMENTOBLASTOMA 481 CALCIFYING AND KERATINIZING
EPITHELIAL ODONTOGENIC CYST
AND TUMOR
Inter-Radicular ODONTOGENIC ADENOMATOID
Radiopacities 482 TUMOR
RESIDUAL FOCAL OSTEITIS AND ODONTOMA AND VARIANTS
CEMENTOMA 482 OSSIFYING FIBROMA
IDIOPATHIC OSTEOSCLEROSIS 483 OSTEOID OSTEOMA
BISPHOSPHONATE RELATED
OSTEONECROSIS OF THE JAWS 484 Antral Opacities 500
CALCIFYING AND KERATINIZING
EPITHELIAL ODONTOGENIC MAXILLARY SINUSITIS 500
CYST/TUMOR 486 ANTRAL POLYP 502
ODONTOGENIC ADENOMATOID SINUS MUCOCELE 503
TUMOR 486 PERIAPICAL INFECTION WITH
ODONTOMA 489 ANTRAL POLYPS 504
CENTRAL OSSIFYING OR ANTRAL INVASIVE MYCOSES 506
CEMENTIFYING FIBROMA 489 FUNGUS BALL (ASPERGILLUS
BENIGN OSTEOBLASTOMA 492 MYCETOMA) 507
ALLERGIC FUNGAL SINUSITIS 508
Pericoronal DISPLACED TEETH, ROOTS, AND
Radiopacities 493 FOREIGN BODIES 509
AUGMENTATION MATERIALS 510
ODONTOGENIC ADENOMATOID
ANTROLITH/RHINOLITH 511
TUMOR 493
ODONTOGENIC TUMORS 512
CALCIFYING EPITHELIAL
ODONTOGENIC TUMOR 494 OSTEOMAS AND EXOSTOSES 513
AMELOBLASTIC BENIGN MESENCHYMAL
FIBRODENTINOMA 496 NEOPLASMS 515
AMELOBLASTIC FIBRO- INVERTING PAPILLOMA 516
ODONTOMA 497 ANTRAL CARCINOMA 517
PMPH_Eversole_Chapter-10.indd 473 1/20/2011 3:04:51 PM
ANTRAL SARCOMA 519 OSTEOID OSTEOMA 540
SILENT SINUS SYNDROME 520 MANDIBULAR TORI AND
EXOSTOSES 541
Ground-Glass
Radiopacities 521 Irregular, Ill-Defined
Expansile Radiopacities 542
FIBROUS DYSPLASIA 521
CHRONIC DIFFUSE SCLEROSING CALCIFYING EPITHELIAL
OSTEOMYELITIS 523 ODONTOGENIC TUMOR 542
OSTEITIS DEFORMANS (PAGET’S DESMOPLASTIC
DISEASE OF BONE) 524 AMELOBLASTOMA 543
HYPERPARATHYROIDISM 526 OSTEOGENIC AND
CHONDROGENIC SARCOMA 545
SEGMENTAL ODONTOMAXILLARY
DYSPLASIA 528 METASTATIC CARCINOMA 546
OSTEOPETROSIS 529 FIBROUS DYSPLASIA†
INVERTED PAPILLOMA+++
Multifocal Confluent ANTRAL CARCINOMA+++
(Cotton-Wool) ANTRAL SARCOMA+++
Radiopacities 530
Superimposed Soft Tissue
OSTEITIS DEFORMANS (PAGET’S Radiopacities 547
DISEASE OF BONE) 530
FLORID OSSEOUS DYSPLASIA 531 SIALOLITHIASIS 547
GARDNER’S SYNDROME 533 PHLEBOLITHIASIS 548
FAMILIAL GIGANTIFORM OSSEOUS/CARTILAGINOUS
CEMENTOMA 534 CHORISTOMA 549
FOREIGN BODIES 550
Cortical Redundancies CALCIFIED LYMPH NODES 551
(Onion-Skin Patterns) 536 MYOSITIS OSSIFICANS 552
GARRÉ’S PERIOSTITIS 536
INFANTILE CORTICAL
HYPEROSTOSIS 537 *Detailed descriptions of target lesions
GENERALIZED CORTICAL appear in the text under the other head-
HYPEROSTOSIS 538 ings included in this chapter.
JUXTACORTICAL OSTEOGENIC †See ground-glass radiopacities.
SARCOMA 539 +++See antral opacities
PMPH_Eversole_Chapter-10.indd 474 1/20/2011 3:04:51 PM
Radiopacities portrayed on radiographs In some instances, a radiographic
are a reflection of the potential for a dis- diagnosis can be made; however, a bone
ease to elaborate calcified products. They biopsy is generally necessary for definitive
can also represent foreign objects lodged diagnosis or confirmation of the clinical
within bone or soft tissues superimposed impression.
on the normal osseous structures. The cal- The most common periapical radiopac-
cifiable matrices within the jaws include ities are periapical cemental dysplasia, focal
osseous tissue, cartilage, cementum, den- sclerosing osteomyelitis, and focal periapi-
tin, and enamel. Any lesions capable of cal osteopetrosis.
forming these cell products may appear The most common inter-radicular
radiopaque. Because the matrix for cal- radiopacities include osteopetrotic scar and
cification may be elaborated prior to any odontoma. Odontoma and odontogenic
mineralization, many of the lesions with adenomatoid tumor are the more frequently
a radiopaque radiographic pattern may encountered pericoronal radiopacities.
at an early stage in their development Fibrous dysplasia is the most common
appear radiolucent. As mineralization of disease to manifest a ground-glass pattern;
the matrices develops, the lesion becomes tori and florid cemento-osseous dysplasia
progressively opaque. For this reason, are the most common lesions yielding mul-
many calcifying tumors or diseases show tifocal confluent radiopacities.
a radiolucency with central opaque flecks Garré’s periostitis is the primary dis-
or conglomerates. Many of the bone lesions ease showing cortical layering. Potentially
presented in the previous chapter on radi- fatal diseases with an opaque radiographic
olucencies are included here because the appearance include the malignant bone neo-
later stages, for reasons just mentioned, plasms, Ewing’s sarcoma, osteogenic and
appear as radiopacities. chondrogenic sarcomas, and metastatic car-
General radiologic considerations cinoma. Gardner’s syndrome is accompa-
should be taken into account when one nied by gastrointestinal tract malignancy.
evaluates radiopaque lesions. Well-circum- Diffuse antral opacification is usually
scribed corticated borders usually repre- a radiographic sign of inflammatory aller-
sent benign slow-growing diseases. Target gic disease. Importantly, antral carcinoma
lesions, opacities with a well-delineated causes the antrum to appear clouded; this
radiolucent halo, are benign and are, as a is potentially fatal.
rule, odontogenic. Likewise, opacities asso-
ciated with the crown of an impacted tooth
are invariably odontogenic.
Periapical Radiopacities
Diffuse radiopacities with ill-defined PERIAPICAL CEMENTAL
borders are difficult to interpret because
they represent a wide range of both benign
DYSPLASIA
and malignant conditions. Multifocal Figure 10-1
radiopacities or those involving multiple
Age: Middle-aged adults
quadrants of the jaws are generally benign Sex: Female predilection
fibro-osseous disorders.
Opacification of the antrum is usually, CLINICAL AND RADIOGRAPHIC
FEATURES
yet not invariably, the result of a soft tissue
proliferation or represents the presence of Periapical cemental dysplasia or cemen-
fluid accumulation. toma is most commonly encountered
PMPH_Eversole_Chapter-10.indd 475 1/20/2011 3:04:51 PM
476 Chapter 10
in blacks. Solitary lesions are limited to lesion is larger than the usual 0.5 to 1 cm,
anterior teeth. Multiple lesions are also yet expansion is not detectable. The lesion
located anteriorly, usually in the mandible begins as a radiolucency; with ensuing
but sometimes extending to the apices of time, calcification progresses so that a solid
first molars. Pain and expansion are lack- opaque mass becomes the dominant radio-
ing, and the teeth are vital. The etiology is graphic feature.
unknown. Radiographically, single or mul-
tiple opacities are encountered apical to the
MICROSCOPIC FEATURES
incisors, cuspids, or premolars. They may
appear with a target pattern or merely as Mature lesions are composed of compact
well-delineated opacities. The apical lam- lamellar bone, quilted cementum, lamel-
ina dura is often intact. Occasionally, the lar cementum, or a combination of these,
FIGURE 10-1
Periapical radiopacities underlying vital teeth representing periapical cemental dysplasia.
PMPH_Eversole_Chapter-10.indd 476 1/20/2011 3:04:51 PM
Radiopaque Lesions of the Jaws 477
with little fibrous stroma. Those detected FOCAL CEMENTO-OSSEOUS
midway in development manifest a fibro- DYSPLASIA
osseous pattern with a hypercellular fibrous Figure 10-2
element containing multiple ovoid or linear
trabeculae of bone and cementum. Age: Young adults
Sex: No predilection
DIFFERENTIAL DIAGNOSIS CLINICAL AND RADIOGRAPHIC
Periapical cemental dysplasia presents a FEATURES
radiopaque pattern similar to that encoun- Focal cemento-osseous dysplasia (FCOD)
tered with focal condensing osteitis, focal is a benign dysplastic, nonpremalignant
periapical osteopetrosis, and benign cemen- lesion of bone that represents the poste-
toblastoma. All these conditions tend to rior jaw counterpart to periapical cemen-
involve posterior teeth. Focal osteitis is asso- tal dysplasia. Unlike periapical cemental
ciated with a deep carious lesion or restora- dysplasia, FCOD is typically a single soli-
tion, and cementoblastomas are expansile. tary lesion identified apical to or adjacent
In the absence of expansion, a well-circum- to the roots of the mandibular premolars,
scribed opacity apical to anterior mandib- and first and second molars. This lesion is
ular teeth can be considered to represent asymptomatic and nonexpansile being an
PACD, and no biopsy is necessary. endosseous pathologic process of unknown
etiology. Some studies show a predilection
TREATMENT for African descent subjects; however, the
lesion can occur in any race. The classic
No treatment is necessary. When biopsy is appearance radiologically is that of a tar-
deferred, the patient should be subjected to get lesion (radiolucent with opaque central
periodic radiographic follow-up to ensure foci).
that the lesion is not a proliferative one
that coincidentally involves the periapi- MICROSCOPIC FEATURES
cal region. Biopsy is indicated if growth is
observed. Multiple small curetted fragments are seen
and demonstrate a fibro-osseous element
and usually an accompanying osteoscle-
Additional Reading rotic focus. The fibro-osseous component
is typically hypercellular and the trabe-
Chaudhry AP, Spink JH, Gorlin RJ. Periapical fibrous cular elements may be linear or ovoid and
dysplasia (Cementoma). J Oral Maxillofac Surg. some confluent, yielding a “ginger-root”
1958;16:483.
Neville BW, Albenesius RJ. The prevalence of benign
morphology.
fibro-osseous lesions of periodontal ligament origin in
black women: a radiographic survey. Oral Surg Oral DIFFERENTIAL DIAGNOSIS
Med Oral Pathol. 1986;62:340.
Stafne EC. Cementoma, a study of 35 cases. Dent Surv. The primary lesion to consider in the differ-
1933;9:27. ential is ossifying fibroma, a neoplastic pro-
Su L, Weathers DR, Waldron CA. Distinguishing fea- cess that expands bone and, unlike FCOD,
tures of focal cemento-osseous dysplasias and cemen- continues to enlarge.
to-ossifying fibromas: I. A pathologic spectrum of 316
cases. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 1997;84(3):301-319. TREATMENT
Zegarelli EV, Kutscher AH, Napoli N, Iurono F,
Hoffman P. The cementoma, a study of 230 patients
No treatment is necessary. Progressive clini-
with 475 cementomas. Oral Surg Oral Med Oral cal and imaging follow-up is recommended
Pathol. 1964;17:219-224. and if expansion evolves, excisional biopsy
PMPH_Eversole_Chapter-10.indd 477 1/20/2011 3:04:55 PM
478 Chapter 10
FIGURE 10-2
Focal cemento-osseous dysplasia. Juxtaradicular target lesions.
with a provisional diagnosis of ossifying Macdonald-Jankowski DS. Focal cemento-osseous dys-
fibroma should be considered. plasia: a systematic review. Dentomaxillofac Radiol.
2008;37:350-360.
Su L, Weathers DR, Waldron CA. Distinguishing
features of focal cemento-osseous dysplasia and
Additional Reading cemento-ossifying fibromas. II. A clinical and radio-
logic spectrum of 316 cases. Oral Surg Oral Med Oral
Kawai T, Hiranuma H, Kishino M, Jikko A, Sakuda M. Pathol Oral Radiol Endod. 1997;84:540-549.
Cemento-osseous dysplasia of the jaws in 54 Japanese Summerlin DJ, Tomich CE. Focal cemento-osseous
patients: a radiographic study. Oral Surg Oral Med dysplasia: a clinicopathologic study of 221 cases. Oral
Oral Pathol Oral Radiol Endod. 1999;87:107-114. Surg Oral Med Oral Pathol. 1994;78(5):611-620.
PMPH_Eversole_Chapter-10.indd 478 1/20/2011 3:04:55 PM
Radiopaque Lesions of the Jaws 479
FOCAL SCLEROSING and occasionally extends up the root for a
OSTEOMYELITIS limited distance. The opacity does not merge
Figure 10-3 with root cementum, so that a periodontal
ligament space is usually discernible. The
Age: Young adults opacity may or may not be enveloped by a
Sex: No predilection radiolucent halo. Cortices do not expand.
CLINICAL AND RADIOGRAPHIC
FEATURES MICROSCOPIC FEATURES
Low-grade pulpal inflammation, usu- Depending on the degree of calcification,
ally located in the first mandibular molar, the tissue may be composed of compact
induces a reactive osteosclerotic response bone or cementum with scant stroma. In
at the apex. The tooth tests vital because less calcified specimens, a fibro-osseous
pulp necrosis is not present; rather, the pulp pattern with a hypercellular stroma pre-
is vital yet inflamed. There is generally no vails. Oval, linear, or curved trabeculae are
pain; however, the patient sometimes com- dispersed throughout this stroma. The pulp
plains of a dull ache. The most obvious may appear histologically unremarkable, or
clinical feature is the presence of gross car- a vital pulp exhibiting a mild mononuclear
ies or a large restoration with a deep pulpal inflammatory infiltrate may be encountered.
floor. Radiographically, a well-demarcated Occasionally, pulpal necrosis is observed in
radiopacity is located below the root apices, teeth with periapical sclerotic foci.
FIGURE 10-3
Focal sclerosing osteomyelitis. Apical radiodensities, pulpal inflammation.
PMPH_Eversole_Chapter-10.indd 479 1/20/2011 3:04:58 PM
480 Chapter 10
DIFFERENTIAL DIAGNOSIS FOCAL PERIAPICAL
The appearance of a well-circumscribed or OSTEOSCLEROSIS
target radiopacity at the apex of a first molar Figure 10-4
may be confused with periapical cemental
dysplasia, focal periapical osteopetrosis, Age: Adults
or benign cementoblastoma. Focal osteitis Sex: No predilection
is the result of pulp disease with caries, CLINICAL AND RADIOGRAPHIC
whereas cementoma and focal osteopetro- FEATURES
sis are not. Cementoblastoma shows fusion Well-localized radiopacities lying below
with the tooth root and expands bone, the apices of vital, noncarious molar teeth
whereas neither of these features is encoun- represent focal osteopetrosis. The etiology
tered in focal sclerosing osteomyelitis. is obscure because no pulp inflammation
TREATMENT is present; the teeth are asymptomatic
and test vital with a vitalometer. Many
Pulp extirpation with endodontic therapy is oral radiologists prefer to include lesions
recommended. of this nature with focal sclerosing osteo-
myelitis; because no clinical or radiologic
Additional Reading evidence of pulpal insult can be detected,
they have been arbitrarily segregated as
Boyne PJ. Incidence of osteosclerotic areas in the mandi- a separate entity. The lesion is usually
ble and maxilla. J Oral Maxillofac Surg. 1960;18:486. detected with routine periapical or pano-
Eversole LR, Stone CE, Strub D. Focal sclerosing osteo-
myelitis and focal periapical osteopetrosis: radiographic graphic views. The opacity generally lacks
patterns. Oral Surg Oral Med Oral Pathol. 1984;58:456. a radiolucent halo, yet is well demarcated
Farman AG, de Joubert JJ, Nortjé CJ. Focal osteosclero- with respect to the surrounding bone. Any
sis and apical periodontal pathoses in “European” and of the three mandibular molars may over-
Cape coloured dental outpatients. Int J Oral Maxillofac
Surg. 1978;7:549. lie the opacity.
Kessler HP. Oral and maxillofacial pathology case of the
month. Condensing osteitis. Tex Dent J. 2003;120:178, MICROSCOPIC FEATURES
188-189.
Marmary Y, Kutiner G. A radiographic survey of periapi-
Bone biopsy shows dense viable lamellar
cal jawbone lesions. Oral Surg Oral Med Oral Pathol. bone with fibrous marrow canals. Inflam-
1986;61:405. matory cells are lacking.
FIGURE 10-4
Focal periapical osteosclerosis. Idiopathic focal opacities without pulpal insult.
PMPH_Eversole_Chapter-10.indd 480 1/20/2011 3:04:59 PM
Radiopaque Lesions of the Jaws 481
DIFFERENTIAL DIAGNOSIS with either central opacities or a solid opac-
Periapical osteopetrosis can be distinguished ity. A thin, radiolucent halo can be seen
from cementoma by virtue of its posterior around densely calcified lesions. The tumor
location and lack of racial, sex, or age predi- is expansile when visualized with occlusal
lection. Cementoblastoma can be eliminated radiographs, and on periapical views, the
because no continuity with the root can be mass extends occlusally to encompass and
demonstrated radiographically or by means become confluent with the lower third of
of percussion. Expansion is also lacking. Focal the molar roots.
condensing osteitis must rank high in the
differential diagnosis; however, neither deep MICROSCOPIC FEATURES
caries, large restorations, nor other sources of Radially oriented trabeculae emanate from
pulp inflammation can be demonstrated. the attached root cementum. In most speci-
mens, the trabeculae polarize like bone
TREATMENT rather than cementum. Osteoblasts rim the
The diagnosis is clinicoradiologic, and no trabeculae, often to the point of stratifica-
treatment is required. tion. The marrow is fibrous.
DIFFERENTIAL DIAGNOSIS
Additional Reading Benign cementoblastoma must be differen-
Boyne PJ. Incidence of osteosclerotic areas in the mandi- tiated from periapical cemental dysplasia,
ble and maxilla. J Oral Maxillofac Surg. 1969;18:486. focal sclerosing osteomyelitis, and peria-
Damm DD. Oral diagnosis. Mandibular radiopacities. pical osteopetrosis. Radiographic demon-
Idiopathic osteosclerosis. Gen Dent. 2007;55:591-595.
Eversole LR, Stone CE, Strub D. Focal sclerosing
stration of confluency with tooth roots, the
osteomyelitis and focal periapical osteopetrosis: radio- presence of expansion, a dull sound on per-
graphic patterns. Oral Surg Oral Med Oral Pathol. cussion, and lack of pulp disease allow for
1984;58:456. a clinicoradiologic diagnosis.
TREATMENT
BENIGN CEMENTOBLASTOMA
Figure 10-5 Because cementoblastomas are somewhat
aggressive, they require excision. Removal
Age: Teenagers and young adults cannot be achieved without sacrificing the
Sex: No predilection ankylosed tooth.
CLINICAL AND RADIOGRAPHIC
FEATURES Additional Reading
A true neoplasm of cementoblasts, the
Barker GL, Begley A, Balmer C. Cementoblastoma in the
benign cementoblastoma, arises most often maxilla: a case report. Prim Dent Care. 2009;16(4):154-
on the first mandibular molars. Other 156.
molar teeth and premolars are involved less Cherrick HM, King OH, Lucatorto FM, Suggs DM.
frequently. Clinically, there is no pain; the Benign cementoblastoma. Oral Surg Oral Med Oral
Pathol. 1974;37:54.
cortex is slightly expanded both buccally Eversole LR, Sabes WR, Dauchess VG. Benign
and lingually. The tooth is vital and usually cementoblastoma. Oral Surg Oral Med Oral Pathol.
noncarious. The involved tooth is ankylo- 1973;36:824.
sed to the tumor mass; on percussion, an Townes TM, Marks RB, Carr RF. Benign (true) cemen-
toblastoma: report of cases. J Oral Maxillofac Surg.
audible difference between affected and 1979;37:342.
unaffected teeth can be discerned. Radio- Wiggins HE, Karian BK. Cementoblastoma of the maxil-
graphically, the apical mass may be lucent la: report of case. J Oral Maxillofac Surg. 1975;33:302.
PMPH_Eversole_Chapter-10.indd 481 1/20/2011 3:05:01 PM
482 Chapter 10
FIGURE 10-5
Benign cementoblastoma. Expansile lesions encompassing roots.
resolution. As the alveolar bone resorbs, the
Inter-Radicular Radiopacities lesion appears to lie in an inter-radicular
location in the edentulous zone. Radio-
RESIDUAL FOCAL OSTEITIS graphically, anterior focal opacities retain
AND CEMENTOMA their features of periapical cemental dyspla-
Figure 10-6 sia, whereas posterior opacities represent
focal osteitis. In both instances, pain and
Age: Adults expansion are lacking, and the lesion is well
Sex: Osteitis—no predilection; cementoma— delineated with or without a circumferen-
female predilection
tial radiolucent rim. As the alveolar bone
CLINICAL AND RADIOGRAPHIC atrophies, both lesions may sequestrate.
FEATURES
When teeth overlying periapical cemental MICROSCOPIC FEATURES
dysplasia (cementoma) or focal sclerosing With both lesions, dense lamellar bone or
osteomyelitis are extracted, the radiopaque cementum is seen, with scant interven-
mass often remains without undergoing ing fibrous marrow. When sequestration
PMPH_Eversole_Chapter-10.indd 482 1/20/2011 3:05:01 PM
Radiopaque Lesions of the Jaws 483
FIGURE 10-6
Opacities in edentulous
areas following tooth
extractions for teeth with
periapical cemental dys-
plasia or focal cemento-
osseous dysplasia.
ensues, the calcified tissue is accompanied excessive ossification. The result is a radio-
by inflamed granulation tissue. graphically demonstrable opacity that
lies within the edentulous space between
DIFFERENTIAL DIAGNOSIS contiguous teeth or is found in an inter-
Residual osteitis or cementoma is more radicular location between permanent
regular, round, or oval than postextraction teeth when deciduous tooth loss elicited
osteopetrotic scar. When a radiolucent halo the reaction. The premolar and first molar
is present, the lesion cannot be differentiated regions are favored. Pain and expansion
radiographically from the calcifying odonto- are lacking. Radiographically, the opaque
genic tumors included in this section. Biopsy lesion is elongated vertically or may
is required to ascertain the true nature of the assume an irregular yet well-delineated
radiographically demonstrable process. configuration.
TREATMENT MICROSCOPIC FEATURES
Once the diagnosis has been established by Dense viable lamellar bone with scant
trephinement or excisional bone biopsy, no fibrous marrow spaces is seen.
further treatment is required.
DIFFERENTIAL DIAGNOSIS
Additional Reading In the absence of expansion or other symp-
Boyne PJ. Incidence of osteosclerotic areas in the mandi-
toms, most lesions included in this sec-
ble and maxilla. J Oral Maxillofac Surg. 1969;18:486. tion on inter-radicular radiopacities can
Eversole LR, Sabes WR, Rovin S. Fibrous dysplasia: a be eliminated when the lesion assumes an
nosologic problem in the diagnosis of fibro-osseous elongated or irregular outline devoid of a
lesions of the jaws. J Oral Pathol Med. 1972;1:189.
radiolucent halo. If pain is present or if a fis-
tula is observed, sequestration with osteo-
IDIOPATHIC OSTEOSCLEROSIS myelitis should be considered.
Figure 10-7
TREATMENT
Age: Adults
Sex: No predilection In the absence of pain or expansion with
an elongated or irregular inter-radic-
CLINICAL AND RADIOGRAPHIC ular opacity, a clinicoradiologic diag-
FEATURES
nosis can be rendered. No treatment is
After tooth extraction or, occasionally, loss required other than periodic radiographic
of deciduous teeth, the socket heals with follow-up.
PMPH_Eversole_Chapter-10.indd 483 1/20/2011 3:05:14 PM
484 Chapter 10
FIGURE 10-7
Idiopathic osteosclerosis. Nonexpansile opacities.
nates such as zoledronate and pamidronate
Additional Reading to increase bone mass. A subpopulation of
Boyne PJ. Incidence of osteosclerotic areas in the mandi- these subjects develop osteonecrosis of the
ble and maxilla. J Oral Maxillofac Surg. 1960;18:486. jaws. Recently, patients taking oral prepara-
Brzovic FR, Belvederessi ME, Faivovich GW. Localized tions of bisphosphonates have also developed
osteosclerosis in the jaws. Quintessence. 1971;3:9. sequestrating lesions, usually in the mandi-
Geist JR, Katz JO. The frequency and distribution of
idiopathic osteosclerosis. Oral Surg Oral Med Oral ble, yet also in the palate and maxillary alve-
Pathol. 1990;69:388. olus. Prior trauma or extractions are reported
in many of these patients, yet a significant
proportion develop the condition without
BISPHOSPHONATE-RELATED any provocation. The lesions are painful and
OSTEONECROSIS OF THE ulcerative without significant tumefaction
and at the time of examination, sequestra can
JAWS
be seen in the base of the ulcers. Radiographs
Figure 10-8 disclose irregular, ragged opacities usually
Age: Elderly surrounded by a resorptive radiolucency.
Sex: No predilection The risk for developing osteonecrosis while
taking bisphosphonates can be quite reliably
CLINICAL FEATURES
predicted by ordering serum C-terminal
Patients with metastatic bone disease, mel- telopeptide (CTX). High levels are indica-
anoma, and generalized osteoporosis are tive of decreased risk for jaw necrosis (150
often treated with intravenous bisphopho- pg/mL).
PMPH_Eversole_Chapter-10.indd 484 1/20/2011 3:05:15 PM
Radiopaque Lesions of the Jaws 485
FIGURE 10-8
Sequestra and surrounding radiolucency in bisphosphonate-related osteonecrosis of the jaws.
MICROSCOPIC FEATURES betadine rinses are recommended along
Nonvital trabeculae show lacunae devoid with bisphosphonate withdrawal.
of osteocyte nuclei with adherent microbial
colonies. Many of the colonies are periodic
acid-Schiff (PAS) positive with a peripheral
Additional Reading
fringe and adherent neutrophils typical for Almazrooa SA, Woo SB. Bisphosphonate and nonbispho-
actinomycotic organisms. sphonate-associated osteonecrosis of the jaw: a review.
J Am Dent Assoc. 2009;140:864-875.
Colella G, Campisi G, Fusco V. American Association
DIFFERENTIAL DIAGNOSIS of Oral and Maxillofacial Surgeons position paper:
bisphosphonate-related osteonecrosis of the jaws-2009
Sequestra of other etiologies must be consid-
update: the need to refine the BRONJ definition.
ered in the differential diagnosis including J Oral Maxillofac Surg. 2009;67:2698-2699.
odontogenic osteomyelitis, trauma, intuba- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa)
tion if lesions are located on the posterior- induced avascular necrosis of the jaws: a growing epi-
lingual mandibular mucosa, and postradia- demic. J Oral Maxillofac Surg. 2003;61:1115-1117.
Marx RE, Cillo JE Jr, Ulloa JJ. Oral bisphosphonate-
tion osteonecrosis to mention a few. induced osteonecrosis: risk factors, prediction of risk
using serum CTX testing, prevention, and treatment.
TREATMENT J Oral Maxillofac Surg. 2007;65:2397-2410.
Naik NH, Russo TA. Bisphosphonate-related osteone-
Systemic antibiotics, sequestrectomy with crosis of the jaw: the role of actinomyces. Clin Infect
gentle nonaggressive debridement and Dis. 2009;49:1729-1732.
PMPH_Eversole_Chapter-10.indd 485 1/20/2011 3:05:19 PM
486 Chapter 10
CALCIFYING AND including the odontogenic adenoma-
KERATINIZING EPITHELIAL toid tumor, mixed odontogenic tumors,
ODONTOGENIC CYST/TUMOR odontoma, and ossifying or cementifying
fibroma. Microscopic evaluation is required
Figure 10-9
to arrive at a defi nitive diagnosis.
Age: No predilection
TREATMENT
Sex: No predilection
CLINICAL AND RADIOGRAPHIC Enucleation with curettage is rarely compli-
FEATURES cated by recurrence.
The calcifying and keratinizing epithelial
odontogenic or Gorlin cyst is a tumor-like Additional Reading
cyst found predominantly in the mandibu-
Freedman PD, Lumerman H, Gee JK. Calcifying
lar premolar region. Nearly one quarter of
odontogenic cyst. Oral Surg Oral Med Oral Pathol.
such cysts are peripheral, producing radio- 1975;40:93.
graphically evident calcification above the Gorlin RJ, Pindborg JJ, Clausen FP, Vickers RA. The cal-
underlying cortex and manifesting a gin- cifying odontogenic cyst—a possible analogue of the
gival swelling. Intrabony lesions may cause cutaneous calcifying epithelioma of Malherbe. Oral
Surg Oral Med Oral Pathol. 1962;15:1235.
expansion. The teeth are vital, and pain is Houg SP, Ellis GL, Hartman KS. Calcifying odontogenic
not a feature. Radiographically, the lesion cyst. A review of 92 cases with re-evaluation of their
begins as a radiolucency and progressively nature as cysts or neoplasms, the nature of ghost cells
calcifies, yielding a target lesion (opaque, and subclassification. Oral Surg Oral Med Oral Pathol.
1991;71:56.
with a circumferential lucent halo). Mid- Soames JV. A pigmented calcifying odontogenic cyst.
stage cysts may be predominantly lucent Oral Surg Oral Med Oral Pathol. 1982;53:395.
with centrally located calcific opaque flecks. Wang YP, Chang YF, Wang JT, Liu BY, Sun A, Chiang
Root divergence is a common finding. CP. Characteristics of calcifying odontogenic cyst in
Taiwanese. J Formos Med Assoc. 2003;102:715-721.
MICROSCOPIC FEATURES
The cyst lining is composed of stratified ODONTOGENIC
squamous epithelium with a rigidly polar- ADENOMATOID TUMOR
ized basal layer assuming ameloblastoid fea- Figure 10-10
tures. The spinous layer is often spongiotic,
mimicking stellate reticulum. The luminal Age: Teenagers
surface contains eosinophilic keratinized Sex: Female predilection
cells devoid of nuclei, so-called ghost cells. CLINICAL AND RADIOGRAPHIC
These cells undergo calcification. Melanin FEATURES
pigment may occasionally be encountered in
Although usually associated with the crown
these lesions. The fibrous wall often contains
of an impacted anterior tooth, the odonto-
eosinophilic cell products resembling osteoid
genic adenomatoid tumor may also arise
or dentinoid. When the cyst wall ruptures,
between tooth roots. Painless expansion is
an avid foreign-body reaction may ensue.
often the chief complaint. The maxillary
incisor-cuspid region is the site of predilec-
DIFFERENTIAL DIAGNOSIS
tion. Radiographically, the tumor is well
The intercellular target lesion seen with delineated, expansile with root divergence,
calcifying epithelial odontogenic cyst may and radiolucent with calcific flecks (target
be featured by other odontogenic tumors, appearance).
PMPH_Eversole_Chapter-10.indd 486 1/20/2011 3:05:42 PM
Radiopaque Lesions of the Jaws 487
FIGURE 10-9
Calcifying and keratinizing
odontogenic cyst/tumor
involving inter-radicular
area, typically occurring in
premolar regions.
FIGURE 10-10
Radiolucency with opaque foci in odontogenic adenomatoid tumor.
PMPH_Eversole_Chapter-10.indd 487 1/20/2011 3:05:42 PM
488 Chapter 10
MICROSCOPIC FEATURES logic diagnosis of odontogenic adenomatoid
The odontogenic adenomatoid tumor dis- tumor; however, microscopic confirmation
plays a thick fibrous capsule with an inner is mandatory.
epithelial neoplastic component composed
of organoid clusters of spindle cells. Colum- TREATMENT
nar cells are arranged in rosettes or ductal Simple surgical enucleation is recom-
patterns dispersed throughout the organoid mended. Recurrence is extremely rare.
cell proliferation. Dystrophic calcifications
are deposited throughout. Some of these
tumors contain melanin pigment. Additional Reading
Aldred MJ, Gray AR. A pigmented adenomatoid odon-
DIFFERENTIAL DIAGNOSIS togenic tumor. Oral Surg Oral Med Oral Pathol.
The expansile radiolucent lesion with central 1990;70:86.
Bhaskar SN. Adenoameloblastoma: its histogenesis
opacities or target appearance assumed by and report of 15 new cases. J Oral Maxillofac Surg.
the odontogenic adenomatoid tumor is sim- 1964;22:218.
ilar to or indistinguishable from that of the Courtney RM, Kerr DA. The odontogenic adenomatoid
calcifying epithelial odontogenic cyst, other tumor. A comprehensive study of twenty new cases.
Oral Surg Oral Med Oral Pathol. 1975;39:424.
mixed odontogenic tumors, odontomas, and Garg D, Palaskar S, Shetty VP, Bhushan A. Adenomatoid
central ossifying or cementifying fibroma. odontogenic tumor—hamartoma or true neoplasm: a
The age, sex, and location favor a radio- case report. J Oral Sci. 2009;51:155-159.
FIGURE 10-11
Odontomas.
PMPH_Eversole_Chapter-10.indd 488 1/20/2011 3:05:49 PM
Radiopaque Lesions of the Jaws 489
Giansanti JS, Someren A, Waldron CA. Odontogenic DIFFERENTIAL DIAGNOSIS
adenomatoid tumor (adenoameloblastoma). Oral Surg
Oral Med Oral Pathol. 1970;30:69. The compound composite variety with tooth
forms is easily recognized radiographically.
The compound complex type may present
ODONTOMA radiologic features in common with the
Figure 10-11 other odontogenic tumors included here,
as well as residual osteitis and cementoma,
Age: Teenagers, young adults ossifying or cementifying fibroma, and
Sex: Slight male predilection
Gorlin cyst. Both types may develop a den-
CLINICAL AND RADIOGRAPHIC tigerous cyst from the follicular wall.
FEATURES
A mixed odontogenic tumor emulating all the TREATMENT
hard tissue products of a mature tooth germ, Odontomas are generally encapsulated
the odontoma is probably the most common by a fibrous lining and can be enucleated.
type of odontogenic tumor or hamartoma. Because dentigerous cysts and even other
Although usually located pericoronal to an odontogenic neoplasms can arise from the
impacted tooth, the odontoma may also arise odontogenic epithelial component of odon-
from odontogenic progenitor cells within the tomas, they should be removed.
periodontal ligament and become located
between tooth roots. There is no pain, and
cortical expansion is either not discernible Additional Reading
or present only to a limited degree. Radio-
Bordini J Jr, Contar CM, Sarot JR, Fernandes A,
graphically, the lesion may present one of two Machado MA. Multiple compound odontomas in the
patterns. When a target pattern with a lucent jaw: case report and analysis of the literature. J Oral
halo prevails, the central opacities assume Maxillofac Surg. 2008;66:2617-2620.
tooth-form configurations. This variety has Budnick SD. Compound and complex odontomas. Oral
Surg Oral Med Oral Pathol. 1976;42:501.
been called compound composite odontoma Gorlin RJ, Chaudhry AP, Pindborg JJ. Odontogenic
and is frequently interposed between ante- tumors. Cancer. 1961;14:73-101.
rior teeth. The compound complex odontoma is Kaugers GE, Miller ME, Abbey LM. Odontomas. Oral
more common in the posterior region, is less Surg Oral Med Oral Pathol. 1989;67:172.
Slootweg PG. An analysis of the interrelationship of the
commonly inter-radicular, and manifests a mixed odontogenic tumors—ameloblastic fibroma,
well-localized opacity with frayed margins, ameloblastic fibro-odontoma, and the odontomas.
a “sunburst” pattern. On rare occasions, mul- Oral Surg Oral Med Oral Pathol. 1981;51:266.
tiple odontomas may be encountered.
MICROSCOPIC FEATURES CENTRAL OSSIFYING OR
Enamel matrix, dentin, cementum, and
CEMENTIFYING FIBROMA
bone are arranged in tooth-germ-like con- Figures 10-12A & 10-12B
figurations or admixed in haphazard fash-
Age: Teenagers, young adults
ion. Odontogenic epithelium, odontoblasts, Sex: No predilection
and pulp mesenchyme are also present. The
soft tissue components show no prolifera- CLINICAL AND RADIOGRAPHIC
FEATURES
tive activity. Some odontomas exhibit a cen-
tral radiolucent zone, being cystic (dilated The ossifying and cementifying fibromas
odontome). Oftentimes, the features of a are mesenchymal neoplasms of the jaws;
Gorlin cyst are present in addition to the they may differentiate along osseous,
odontoma. cemental, or both osseous and cemental
PMPH_Eversole_Chapter-10.indd 489 1/20/2011 3:06:07 PM
490 Chapter 10
FIGURE 10-12A
Central ossifying fibromas often initiate root divergence or resorption.
lines. The neoplasm is usually located in occasionally these tumors are extremely
the body or anterior region of the mandible aggressive with rapid growth, a tendency
or maxilla and classically produces expan- for expansion, and a potential for reaching
sion, usually in a buccal plane. Pain is not massive proportions. This type of lesion
a feature; the overlying alveolar mucosa has been referred to as aggressive juvenile
is generally intact, devoid of ulceration. ossifying fibroma for which there are two
Radiographically, expansion is usually microscopic variants: psammomatoid and
demonstrable along the inferior border of trabecular types both of which are aggres-
the mandible; on occlusal films, the buc- sive and may grow rapidly. Psammoma-
cal plate is bulged. The tumor displays toid ossifying fibroma is associated with a
sharply delineated margins and is usually specific gene translocation, t(X;2)(q26;q38).
unilocular, although multilocular patterns There is a tendency for the psammomatoid
are noted on occasion. The central zone type to arise in the facial/sinonasal bones.
contains opaque calcific flecks or a dense These tumors are expansile and radiolu-
radiopaque conglomerate mass. Divergence cent with central floccular calcifications
of adjacent tooth roots is a common find- and may reach 5 to 6 cm in diameter.
ing. Although most ossifying and cemen- Ossifying fibromas may be multifocal
tifying fibromas are slow-growing lesions, and some are affiliated with familial hyper-
PMPH_Eversole_Chapter-10.indd 490 1/20/2011 3:06:07 PM
Radiopaque Lesions of the Jaws 491
FIGURE 10-12B
Juvenile aggressive ossifying fibroma, expansile destructive lesions of psammomatoid, and trabecular
types.
parathyroidism in which there is a mutation sive behavior. Aggressive juvenile ossifying
in the HRPT2 tumor suppressor gene. fibromas exhibit a hypercellular fibroblastic
element. The psammomatoid type shows
MICROSCOPIC FEATURES ovoid psammoma bodies throughout,
A fibro-osseous microscopic pattern with whereas the trabecular type shows sheets of
a hypercellular fibroblastic stroma pre- fibroblastic regions with pockets of multi-
vails. Ossifying fibroma contains irregular nucleated giant cells similar to those of
osteoid spicules or retiform trabeculae often giant cell granuloma, and yet other regions
rimmed by osteoblasts. Ovoid and curvilin- of immature osteoid trabeculae.
ear trabeculae that polarize with a micro-
DIFFERENTIAL DIAGNOSIS
lamellar or quilted pattern are typical of
cementifying fibromas. Alternatively, some The expansile target pattern typical of ossi-
lesions show both types of trabeculae. The fying and cementifying fibromas may be
active juvenile variant may not be readily seen with the calcifying epithelial odonto-
segregated on the basis of histopathologic genic cyst, odontogenic adenomatoid tumor,
features. Although pronounced hypercellu- and some of the mixed odontogenic tumors.
larity is an indication of rapid proliferation, Lesions at an early stage may not show
it is not necessarily predictive of aggres- dense opacities; rather, faint calcified flecks
PMPH_Eversole_Chapter-10.indd 491 1/20/2011 3:06:13 PM
492 Chapter 10
float within an expanding radiolucency. In van Heerden WFP, Raubenheimer EJ, Weir RG, Kreidler
these cases, the differential diagnosis should J. Giant ossifying fibroma: a clinicopathologic study of
8 tumors. J Oral Pathol Med. 1989;18:506-509.
include Pindborg tumor as well as the afore-
mentioned entities. Biopsy discloses the
characteristic histomorphologic features.
BENIGN OSTEOBLASTOMA
TREATMENT Figure 10-13
Surgical enucleation is rarely followed by Age: Children and teenagers
recurrence for relatively small lesions. Large Sex: Male predilection
expansile tumors with root divergence or CLINICAL AND RADIOGRAPHIC
resorption and thin cortical boundaries FEATURES
may require en bloc resection to prevent
recurrence. The juvenile aggressive ossify- A tumor that generally arises in the long
ing fibroma, as determined histologically bones and vertebrae, the osteoblastoma may
and radiographically with clinical observa- occasionally arise in the maxillofacial com-
tion of rapid growth, should be resected. plex. It is a benign neoplasm of osteoblas-
tic origin with a rapid growth rate capable
of expansion and facial deformity. Radio-
Additional Reading graphically, it is relatively well circum-
scribed, although the tumor margins may
Eversole LR, Merrell PW, Strub D. Radiographic char-
be scalloped. Centrally, radiopaque foci are
acteristics of central ossifying fibroma. Oral Surg Oral
Med Oral Pathol. 1985;59:522. encountered. Adjacent teeth are displaced
Eversole LR, Sabes WR, Rovin S. Fibrous dysplasia: a and root resorption is usually encountered.
nosologic problem in the diagnosis of fibro-osseous Although the disease is rare, there may be a
lesions of the jaws. J Oral Pathol Med. 1972;1:189. predilection for the maxilla.
Fujikawa M, Okamura K, Sato K, et al. Familial iso-
lated hyperparathyroidism due to multiple adenomas
associated with ossifying jaw fibroma and multiple MICROSCOPIC FEATURES
uterine adenomyomatous polyps. Eur J Endocrinol.
1998;138:557-561.
Dispersed throughout an areolar fibrous
Sciubba JJ, Younai F. Ossifying fibroma of the mandible marrow are irregular or retiform arrange-
and maxilla: review of 18 cases. J Oral Pathol Med. ments of thin osteoid trabeculae rimmed
1989;18:315. to the point of stratification by plump
Thankappan S, Nair S, Thomas V, Sharafudeen KP.
Psammomatoid and trabecular variants of juvenile
basophilic osteoblasts. Osteoclasts are also
ossifying fibroma-two case reports. Indian J Radiol present, and the marrow is generally well
Imaging. 2009;19:116-119. vascularized.
FIGURE 10-13
Benign osteoblastoma,
well circumscribed mixed
lucent/opaque pattern.
PMPH_Eversole_Chapter-10.indd 492 1/20/2011 3:06:18 PM
Radiopaque Lesions of the Jaws 493
DIFFERENTIAL DIAGNOSIS Clinically, expansion of the buccal and pala-
Expansile inter-radicular radiopacities as tal or lingual plates is seen in the absence of
seen in benign osteoblastoma may be pain. Radiographically, the lesion is usually
encountered in central ossifying or cemen- a well-delineated, corticated radiolucency
tifying fibromas and certain mixed odonto- containing calcific flecks. The pericoronal
genic tumors. Biopsy is required to achieve lesion, as opposed to a simple dentiger-
a definitive diagnosis. ous cyst, tends to originate low on the root
rather than from the dentinoenamel junc-
TREATMENT tion. Occasionally, a classic target pattern
is seen, whereby a circumferential halo
Benign osteoblastoma is an aggressive envelops a dense, central, round radiodense
neoplasm; although enucleation may be mass.
attempted, recurrence is a distinct possibil-
ity. If the lesion recurs, en bloc resection is MICROSCOPIC FEATURES
recommended to eradicate the disease.
The tumor is composed of swirled spindle-
shaped epithelial cell conglomerates with
Additional Reading focal duct-like configurations lined by
columnar cells. Dystrophic calcifications
Angiero F, Mellone P, Baldi A, Stefani M. Osteoblastoma are distributed throughout. A dense fibrous
of the jaw: report of two cases and review of the litera-
ture. In Vivo. 2006;20(5):665-670. wall confines the neoplastic element. Occa-
Borello ED, Sedano HO. Giant osteoid osteoma sionally, other histologic patterns repre-
of the maxilla. Oral Surg Oral Med Oral Pathol. senting various other odontogenic tumors
1967;23:563. are coexistent.
el-Mofty S, Refai H. Benign osteoblastoma of the max-
illa. J Oral Maxillofac Surg. 1989;47:60.
Miller AS, Rambo HM, Bowser MW, Gross M. Benign DIFFERENTIAL DIAGNOSIS
osteoblastoma of the jaws: report of three cases. J Oral A pericoronal radiolucency with an opaque
Maxillofac Surg. 1980;38:694.
Smith RA, Hansen LS, Resnick D, Chan W. Comparison
center occurring in the anterior segment of
of the osteoblastoma in gnathic and extragnathic sites. the jaws in teenage females invariably rep-
Oral Surg Oral Med Oral Pathol. 1982;54:285-298. resents odontogenic adenomatoid tumor.
Nevertheless, the differential diagnosis must
include other odontogenic tumors included
Pericoronal Radiopacities in this section, because they may assume
similar radiologic characteristics. Biopsy is
ODONTOGENIC necessary for a definitive diagnosis.
ADENOMATOID TUMOR
Figure 10-14 TREATMENT
Simple surgical excision is curative. Recur-
Age: Teenagers
rence is almost nonexistent.
Sex: Female predilection
CLINICAL AND RADIOGRAPHIC
FEATURES Additional Reading
More than three quarters of all odontogenic Abrams AM, Melrose RJ, Howell FW.
adenomatoid tumors arise from reduced Adenomeloblastoma. A clinical pathologic study of ten
enamel epithelium surrounding the crown new cases. Cancer. 1968;22:175.
Bingham RA, Adrian JC. Combined epithelial odonto-
of an impacted anterior tooth; some lesions genic tumor-adenomatoid odontogenic tumor and cal-
have been extraosseous. The maxillary cus- cifying epithelial odontogenic tumor: report of a case.
pid is the most commonly affected tooth. J Oral Maxillofac Surg. 1986;44:574.
PMPH_Eversole_Chapter-10.indd 493 1/20/2011 3:06:20 PM
494 Chapter 10
FIGURE 10-14
Odontogenic adenomatoid tumor
tends to be a peridental lucency
with central opaque flecks.
Courtney RM, Kerr DA. The odontogenic adenomatoid neoplasm of epithelial derivation. Most
tumor. A comprehensive study of twenty new cases. lesions are associated with an impacted
Oral Surg Oral Med Oral Pathol. 1975;39:424.
Giansanti JS, Someren A, Waldron CA. Odontogenic tooth, and the mandibular body or ramus
adenomatoid tumor (adenoameloblastoma). Oral Surg is by far the most common site of origin.
Oral Med Oral Pathol. 1970;30:69. Pain is usually not a complaint. The chief
Rick GM. Adenomatoid odontogenic tumor. Oral sign is cortical expansion. Radiographically,
Maxillofac Surg Clin North Am. 2004;16:333-354.
expanded cortices can be visualized in buc-
cal, lingual, and vertical dimensions. The
CALCIFYING EPITHELIAL lesion is usually radiolucent with poorly
defined or, at the least, noncorticated bor-
ODONTOGENIC TUMOR ders. It may appear unilocular, multilocu-
Figure 10-15 lar, or moth-eaten. Multiple radiopaque foci
can be detected within the radiolucent zone
Age: Middle-aged adults
Sex: No predilection
in the form of flecks, conglomerates, or dif-
fuse opacities yielding a “driven-snow”
CLINICAL AND RADIOGRAPHIC appearance. Root divergence and resorp-
FEATURES tion are common findings. The impacted
The calcifying epithelial odontogenic (Pin- tooth usually shows arrested root develop-
dborg) tumor is an aggressive odontogenic ment and is often significantly displaced by
PMPH_Eversole_Chapter-10.indd 494 1/20/2011 3:06:20 PM
Radiopaque Lesions of the Jaws 495
FIGURE 10-15
Calcifying epithelial odon-
togenic tumor (Pindborg
tumor) is an aggressive
expansile tumor.
the tumor. A mutation in the ameloblastin ferentiated from osteogenic and chondro-
gene has been identified. genic sarcomas; however, these malignan-
cies are rarely associated with an impacted
MICROSCOPIC FEATURES tooth.
Sheets, nests, and cords of eosinophilic
TREATMENT
epithelial cells prevail, bearing no resem-
blance to tooth germ primordia. Nuclear Calcifying epithelial odontogenic tumors
pleomorphism may be significant despite are aggressive and may reach large pro-
the benignity of the tumor. Neoplastic portions. Their behavior is reminiscent of
cells are oriented about amyloid droplets, that of ameloblastoma. En bloc resection,
conglomerates of odontogenic ameloblast- hemimandibulectomy, or partial maxil-
associated protein (ODAM). Concentrically lectomy, depending on tumor size, are the
laminated Leisegang calcifications similar treatment methods required to eradicate
to psammoma bodies are a classic finding. the disease.
A variety of so-called atypical variants are
encountered; the primary variant is a clear
cell lesion that is composed of sheets and Additional Reading
islands of cells with vacuolated cytoplasm
Franklin CD, Pindborg JJ. The calcifying epithelial odon-
and associated amyloid deposits with togenic tumor. A review and analysis of 113 cases. Oral
calcification. Surg Oral Med Oral Pathol. 1976;42:753.
Kestler DP, Foster JS, Macy SD, Murphy CL, Weiss DT,
DIFFERENTIAL DIAGNOSIS Solomon A. Expression of odontogenic ameloblast-as-
sociated protein (ODAM) in dental and other epithe-
The radiographic appearance of Pindborg lial neoplasms. Mol Med. 2008;14:318-326.
tumor may simulate a variety of both Krolls SE, Pindborg JJ. Calcifying epithelial odonto-
genic tumor. A survey of 23 cases and discussion of
benign and malignant lesions of the jaws. histomorphologic variations. Arch Pathol Lab Med.
The more well-delineated tumors must 1974;98:206.
be microscopically differentiated from Maranda G, Gourgi M. Calcifying epithelial odontogenic
the other benign odontogenic neoplasms tumor (Pindborg tumor). Review of the literature and
case report. Can Dent Assoc J. 1986;52:1009.
included in this section. Lesions with Pindborg JJ. The calcifying epithelial odontogenic tumor;
expansile mixed radiolucent/radiopaque review of the literature and report of an extraosseous
patterns lacking margination must be dif- case. Acta Odontol Scand. 1966;24:419.
PMPH_Eversole_Chapter-10.indd 495 1/20/2011 3:06:33 PM
496 Chapter 10
AMELOBLASTIC ment are linear cords of cuboidal epithelium
FIBRODENTINOMA that tend to open, creating tooth germ con-
Figure 10-16 figurations with a central stellate reticulum
element. In juxtaposition to these epithelial
Age: Teenagers, young adults nests are sheets of eosinophilic hyalinized
Sex: No predilection material representing dentinoid. Occasion-
CLINICAL AND RADIOGRAPHIC ally, tubules are demonstrable. Cell nuclei
FEATURES may be entrapped within this product.
This rare mixed odontogenic tumor repre- DIFFERENTIAL DIAGNOSIS
sents an ameloblastic fibroma that has differ-
entiated to the extent that dentin is elaborated. Pericoronal lucencies with central opacities
Expansion is often present, but pain is not a as seen in ameloblastic fibrodentinoma are
feature. The lesion invariably arises in asso- also typical of other odontogenic neoplasms
ciation with an impacted tooth; depending included in the section. Biopsy is required
on the degree of dentinal calcification, it to secure a definitive diagnosis.
may appear radiolucent with central opaque
TREATMENT
flecks or may assume a target configuration.
It may be unilocular or multilocular with Simple surgical nucleation is the treatment
well-defined margins. A variant form occurs of choice. Recurrence is uncommon.
in children and is located peripherally as a
gingival swelling. Some pathologists believe
that this lesion is simply an early phase in Additional Reading
the development of an odontoma. Azaz B, Ulmansky M, Lewin-Epstein J. Dentinoma.
Report of a case. Oral Surg Oral Med Oral Pathol.
MICROSCOPIC FEATURES 1967;24:659.
Eversole LR, Tomich CA, Cherrick HM. Histogenesis of
Dispersed throughout an embryonic hyper- odontogenic tumors. Oral Surg Oral Med Oral Pathol.
cellular hypocollagenous mesenchymal ele- 1971;32:569.
FIGURE 10-16
Ameloblastic fibroden-
tinoma, a nonaggressive
tumor.
PMPH_Eversole_Chapter-10.indd 496 1/20/2011 3:06:35 PM
Radiopaque Lesions of the Jaws 497
Karasu HA, Akman H, Uyanik LO, Sayan NB. crown of an impacted tooth. The lesion may
Ameloblastic fibrodentinoma. A case report. N Y State reach large proportions yet is well demar-
Dent J. 2004;70:22-23.
McKelvy BD, Cherrick HM. Peripheral amelo- cated. It may be unilocular or multilocular
blastic fibrodentinoma. J Oral Maxillofac Surg. and contains multiple radiopaque foci with
1976;34:826. irregular configurations.
Pindborg JJ, Clausen F. Classification of odonto-
genic tumors: suggestion. Acta Odontol Scand.
1958;16:293.
MICROSCOPIC FEATURES
Calcified and uncalcified matrices of den-
tin, enamel, and cementum prevail in hap-
AMELOBLASTIC FIBRO- hazard arrangement. A significant portion
ODONTOMA of the tumor is composed of proliferating
Figure 10-17 epithelial and mesenchymal soft tissue
with features identical to those of amelo-
Age: Teenagers blastic fibroma. Inductive changes with
Sex: No predilection dentinoid and a mantle of enamel matrix
CLINICAL AND RADIOGRAPHIC are interposed between the epithelial and
FEATURES mesenchymal tissues in focal regions.
The ameloblastic fibro-odontoma, referred
to in the past simply as ameloblastic odon- DIFFERENTIAL DIAGNOSIS
toma, is an aggressive mixed odontogenic Large, well-defined radiolucencies with
neoplasm that is analogous to an amelo- multifocal central opacities in association
blastic fibroma capable of elaborating all of with an impacted tooth, usually a molar,
the hard tissues found in a mature tooth. are typically seen with ameloblastic fibro-
Clinically, the mandibular body and ramus dentinoma and odontoameloblastoma as
regions are the most frequent sites of ori- well as with ameloblastic fibro-odontoma.
gin, and expansion is the chief sign. Radio- Microscopic examination is therefore
graphically, most are associated with the required.
FIGURE 10-17
Ameloblastic fibro-od-
ontoma showing expan-
sile well-circumscribed
radiolucency with mul-
tiple opaque tooth-like
foci in association with
an impacted molar. These
tumors represent an
ameloblastic fibroma pro-
liferation in conjunction
with an odontoma.
PMPH_Eversole_Chapter-10.indd 497 1/20/2011 3:06:37 PM
498 Chapter 10
TREATMENT ODONTOMA
Surgical enucleation is the treatment of Figure 10-18
choice. Recurrence may develop, but is
uncommon. Age: Teenagers, young adults
Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Additional Reading FEATURES
Hanna PJ, Regezi JA, Hayward JR. Ameloblastic fibro- The odontoma, a mixed odontogenic tumor
odontoma: report of case with light and electron with the capability of elaborating all dental
microscopic observations. J Oral Maxillofac Surg. tissues found in a mature tooth, is self-lim-
1976;34:820.
Hooker SP. Ameloblastic odontoma: an analysis of iting in its growth potential. It is the most
twenty-six cases. Oral Surg Oral Med Oral Pathol. common pericoronal radiopacity. Expan-
1967;24:375 (abstract). sion, if present at all, is limited. Lesions
Miller AS, López CFA, Pullon PA, Elzay RP. Ameloblastic located high in the alveolus may tend to
fibro-odontoma. Report of seven cases. Oral Surg Oral
Med Oral Pathol. 1976;41:354-365.
erupt, with ulceration, fistulization, and
Piette EM, Tideman H, Wu PC. Massive maxil- inflammation. Radiographically, a pericoro-
lary ameloblastic fibro-odontoma: case report nal radiolucency with well-defined or cor-
with surgical management. J Oral Maxillofac Surg. ticated borders is seen. The center contains
1990;48:526.
Sumi M, Yonetsu K, Nakamura T. CT of ameloblastic
tooth-like calcified masses (composite type)
fibroodontoma. AJR Am J Roentgenol. 1997;169:599- or round, oval, or sunburst masses (complex
600. type). When odontoma are associated with
FIGURE 10-18
Odontomas frequently
arise in dental follicles of
impacted teeth.
PMPH_Eversole_Chapter-10.indd 498 1/20/2011 3:06:40 PM
Radiopaque Lesions of the Jaws 499
impacted teeth, they are usually mandibu- because odontomas may prevent eruption,
lar molars. displace adjacent teeth, or develop dentiger-
ous cysts.
MICROSCOPIC FEATURES
Enamel matrix, tubular dentin, and cemen-
tum are associated with their comple-
Additional Reading
mentary soft tissue elements, odontogenic Gardner DG, Dort LC. Dysplastic enamel in odontomas.
epithelium, odontoblasts, and cemento- Oral Surg Oral Med Oral Pathol. 1979;47:238.
Gorlin RJ, Chaudhry AP, Pindborg JJ. Odontogenic
blasts, respectively. The calcified compo- tumors. Cancer. 1961;14:73-101.
nents may or may not assume tooth-form Kaugers GE, Miller ME, Abbey LM. Odontomas. Oral
configurations. Surg Oral Med Oral Pathol. 1989;67:172.
Minderjahn A. Incidence and clinical differentia-
tion of odontogenic tumors. J Oral Maxillofac Surg.
DIFFERENTIAL DIAGNOSIS 1979;7:142.
When tooth-like opacities are present Regezi JA, Kerr DA, Courtney RM. Odontogenic
tumors: analysis of 706 cases. J Oral Maxillofac Surg.
within a unilocular radiolucency, a radio- 1978;36:771.
graphic diagnosis can often be rendered.
The complex varieties or larger pericoronal
lesions must be microscopically differenti- ODONTOAMELOBLASTOMA
ated from other odontogenic neoplasms Figure 10-19
such as Pindborg tumor, ameloblastic fibro-
dentinoma, ameloblastic fibro-odontoma, Age: Teenagers and young adults
and odontoameloblastoma. Sex: No predilection
CLINICAL AND RADIOGRAPHIC
TREATMENT FEATURES
Surgical enucleation is easily achieved An extremely rare mixed odontogenic
because of encapsulation by follicular tumor, the odontoameloblastoma is an
fibrous tissue. The lesion should be removed, aggressive neoplasm capable of producing
FIGURE 10-19
Odontoameloblastomas
show radiologic features
in common with amelo-
blastic fibro-odontomas
and represent an odon-
toma with proliferating
ameloblastoma.
PMPH_Eversole_Chapter-10.indd 499 1/20/2011 3:06:43 PM
500 Chapter 10
significant expansion and facial asymmetry.
The tumor is composed of all tissue compo- Additional Reading
nents of a normal tooth and can be consid- Clausen F. Les odontomes ameloblastiques. Rev Stomatol
ered an aggressive variant of the odontoma. Chir Maxillofac. 1959;60:590.
Radiographically, an impacted tooth with a Frissell GT, Shafer WG. Ameloblastic odontoma:
well-circumscribed expansile radiolucency report of a case. Oral Surg Oral Med Oral Pathol.
1953;6:1129.
containing multifocal radiopaque foci is Gupta DS, Gupta MK. Odontoameloblastoma. J Oral
demonstrated. The central opacities often Maxillofac Surg. 1986;44:146.
resemble malformed teeth. They may arise La Briola JD, Steiner M, Bernstein ML, Verdi GD,
in either jaw with a tendency to locate in the Stannard PF. Odontoameloblastoma. J Oral Maxillofac
Surg. 1980;38:139-143.
body area in association with an impacted Mosca RC, Marques MM, Barbosa SC, et al.
molar, which is usually displaced by the Odontoameloblastoma: report of two cases. Indian J
lesion. Root divergence or resorption may Dent Res. 2009;20:230-234.
be discernible.
MICROSCOPIC FEATURES Antral Opacities
Decalcified specimens show a diverse
array of calcified tissue matrices: enamel, MAXILLARY SINUSITIS
dentin, and cementum. These are often Figure 10-20
arranged in morphologic structures that
resemble developing anomalous teeth. Age: Adults
The hard tissues are admixed and associ- Sex: No predilection
ated with odontogenic epithelium, which CLINICAL AND RADIOGRAPHIC
in many regions is proliferative, display- FEATURES
ing ameloblastoma-like histomorpho-
Sinusitis is a common disease and is usu-
logic structure. These ameloblastomatous
ally allergic. Many cases of acute sinusitis
islands are embedded in mature collag-
and some cases of chronic sinusitis are
enous stroma.
associated with or caused by infectious
DIFFERENTIAL DIAGNOSIS organisms; chief among these are Hemophi-
lus influenzae, Streptococcus pneumoniae, and
Odontoma and odontogenic adenomatoid rhinovirus. Allergic sinusitis is generally
tumor are rarely as aggressive as odon- secondary to rhinitis, in which the lateral
toameloblastoma; nevertheless, they should nasal mucous membranes become edema-
be included in the differential radiographic tous, leading to blockage of the ostium. The
diagnosis. Ameloblastic fibro-odontoma, affected sinus fills with mucous secretion
ameloblastic fibrodentinoma, and calcify- and if also infected, a purulent aspirate
ing epithelial odontogenic tumor may all can be obtained. Repeated bouts of inflam-
appear radiographically indistinguishable mation with periodic blockage and drain-
from odontoameloblastoma. age can lead to a thickening of the sinus
membrane. Fluid-filled sinuses appear as
TREATMENT a diffuse opacification; transillumination
Because few cases of this tumor have been of the sinuses reveals a dull or opaque
reported, a reliable prognostic index cannot appearance when a fiberoptic light source
be based on previous experiences. Reported is placed against the palate in a darkened
cases often recur. Thorough enucleation is room. When the upper sinus is pneuma-
recommended and, if a recurrence devel- tized while fluid occupies the lower region,
ops, resection may be required. a discrete fluid level can be identified on
PMPH_Eversole_Chapter-10.indd 500 1/20/2011 3:06:44 PM
Radiopaque Lesions of the Jaws 501
FIGURE 10-20
Maxillary sinusitis with air/
fluid levels and complete
clouding fail to cause bone
erosion or expansion.
Water’s projections. Chronic recurrent acute or chronic infectious lesions contain
sinusitis often discloses patency with a a preponderance of mononuclear cells. The
thickened membrane. In general, a mem- mucous membranes in chronic sinusitis
brane thickening greater than 8 mm is are edematous with a leukocytic infiltrate
associated with symptoms. Many asymp- containing many eosinophils. Polypoid
tomatic patients exhibit mild to moder- excrescences are common and show similar
ate thickening radiographically. The chief histologic changes to hyperplastic mucosal
symptom of active chronic sinusitis is dull thickening.
pain that is referred to all posterior max-
illary teeth, which are sensitive to percus- DIFFERENTIAL DIAGNOSIS
sion. When the head is lowered, the pain Osseous destruction is not usually a feature
intensifies. Acute infectious sinusitis is of chronic sinusitis. Nevertheless, neoplas-
associated with moderate to severe maxil- tic processes may cause diffuse homoge-
lary pain and pressure, both of which occur neous opacification; however, pain is not
spontaneously and on palpation. usually featured. Failure of the opacifica-
tion to resolve after conventional therapy
MICROSCOPIC FEATURES
for sinusitis warrants exploration, sinos-
An aspirate in cases of acute infectious copy, and biopsy. Dental sources of infec-
sinusitis shows neutrophils, whereas sub- tion should be ruled out.
PMPH_Eversole_Chapter-10.indd 501 1/20/2011 3:06:44 PM
502 Chapter 10
TREATMENT ANTRAL POLYP
A therapeutic trial with nasal decon- Figure 10-21
gestants and antihistamines should be
initiated. Should the symptoms and radio- Age: Middle-aged adults
Sex: No predilection
graphic opacification fail to resolve within
4 or 5 days, an aspirate should be obtained CLINICAL AND RADIOGRAPHIC
to evaluate the presence of leukocytes. FEATURES
Furthermore, a culture and sensitivity test The so-called mucous retention cyst of
should be performed to explore the pos- the antrum represents an inflammatory
sibility of an infectious etiology; appropri- polyp without an epithelial lining and is,
ate antibiotic therapy, usually ampicillin or therefore, not a true cyst. Furthermore,
amoxicillin, should follow. this lesion should not be confused with
a true mucocele of the sinuses, which,
unlike the mucosal polyp, exhibits aggres-
Additional Reading sive behavior. The antral mucous retention
cyst should be referred to as an inflam-
Axelsson A, Jensen C. The roentgenologic demonstration matory mucosal polyp. Usually no symp-
of sinusitis. AJR Am J Roentgenol. 1974;122:621. toms are present; however, there may be
Evans FO Jr, Sydnor JB, Moore WEC, et al. Sinusitis of
the maxillary antrum. N Engl J Med. 1975;293:735- a history of nasal discharge, congestion,
739. or other symptoms of chronic sinusitis.
Fascenelli FW. Maxillary sinus abnormalities: radio- Radiographically, panoramic, Caldwell,
graphic evidence in an asymptomatic population. Arch and Water’s views reveal a smooth-sur-
Otolaryngol Head Neck Surg. 1969;90:190.
Rysz M, Bakoń L. Maxillary sinus anatomy variation faced, dome-shaped homogenous opacity
and nasal cavity width: structural computed tomog- that emanates from the antral floor and
raphy imaging. Folia Morphol (Warsz). 2009;68:260- in more advanced sinusitis, the polyps
264. may be multinodular. On anterioposterior
Shapiro GG, Furukawa CT, Pierson WE, Gilbertson E,
Bierman CW. Blinded comparison of maxillary sinus
views, an air space usually separates the
radiography and ultrasound for diagnosis of sinusitis. polyp from the lateral sinus bony wall.
J Allergy Clin Immunol. 1986;77:59-64. Neither bone erosion nor expansion is fea-
FIGURE 10-21
Inflammatory polyps are typically allergic and dome shaped.
PMPH_Eversole_Chapter-10.indd 502 1/20/2011 3:06:49 PM
Radiopaque Lesions of the Jaws 503
tured. The maxillary teeth underlying the Halstead CL. Mucosal cysts of the maxillary sinus: report
sinus lesion are vital. Antrochoanal polyp of 75 cases. J Am Dent Assoc. 1973;87:1435.
Vigneswaran N, Patel PY. Oral and maxillofacial pathol-
is a variant in which the polyp extends ogy case of the month. Antral pseudocyst Tex Dent J.
into the nasal cavity and posteriorly into 2007;124:1140-1141, 1146-1147.
the choanal region. Wright RW. Round shadows in the maxillary sinuses.
Laryngoscope. 1946;56:455.
MICROSCOPIC FEATURES
The antral retention polyp lacks an epithe- SINUS MUCOCELE
lial lining. The sinus respiratory epithelium
Figure 10-22
occupies the surface and is distended by
an underlying mass of areolar and myx- Age: Middle-aged adults
omatous fibrous or granulation tissue. Sex: No predilection
Mucoid lakes are often observed and are
CLINICAL AND RADIOGRAPHIC
compartmentalized by intervening deli- FEATURES
cate fibrovascular septa. Ductal ectasia of
the tubuloacinar glands is common, and a The sinus mucocele is usually located in the
mild inflammatory cell infiltrate composed frontal or anterior ethmoidal sinus; occasion-
of lymphocytes, plasma cells, neutrophils, ally, the antrum is involved. Rare cases of
and eosinophils prevails throughout. pansinus involvement have been reported.
Although the etiology is unknown, the
DIFFERENTIAL DIAGNOSIS most plausible cause is blockage of the sinus
openings with mucous retention. There
Antral mucosal polyps appear identical is usually a history of surgery, trauma, or
to antral polyps associated with spread of recurrent sinusitis. Frontoethmoidal lesions
odontogenic infection. Periapical cysts or expand and displace the eye laterally and
granulomas with sinus extension can be inferiorly. A crepitant bulge can usually be
ruled out by vitalometer testing. Most neo- detected in the frontal region. Radiographi-
plasms fail to show a discrete dome-shaped cally, diffuse opacification is seen along
opacity emanating from the sinus floor. with effacement of the septate configura-
Osteomas, antroliths, and odontomas are tion. Erosion of the sinus walls may be
more discrete and are generally more opaci- preceded or accompanied by reactive oste-
fied than antral mucosal polyps. osclerosis. Rarely, proliferative osteomy-
elitis is observed with dense opacification
TREATMENT and obliteration of the sinus air spaces. An
Symptoms rarely exist; thus, no treatment is acute infection may also evolve (mucopyo-
necessary. Periodic follow-up radiographs cele). When the antrum is involved, diffuse
should be obtained; most lesions spontane- opacification is seen along with osseous
ously resolve within 1 year. destruction. Clinically, the teeth may loosen
and the ipsilateral eye may exhibit propto-
sis. Computerized tomography is extremely
Additional Reading useful for determining extent of disease.
Frosini P, Picarella G, De Campora E. Antrochoanal pol-
yp: analysis of 200 cases. Acta Otorhinolaryngol Ital.
MICROSCOPIC FEATURES
2009;29:21-26. Although the sinus lining usually main-
Gothberg KA, Little JW, King DR, Bean LR. A clini-
cal study of cysts arising from mucosa of the maxil-
tains a pseudostratified columnar ciliated
lary sinus. Oral Surg Oral Med Oral Pathol. 1976;41: appearance, foci of squamous metapla-
52-58. sia may be present. An inflammatory cell
PMPH_Eversole_Chapter-10.indd 503 1/20/2011 3:06:51 PM
504 Chapter 10
FIGURE 10-22
Sinus mucoceles are inva-
sive expansile aggressive
lesions that can erode
sinus walls.
infiltrate is frequently encountered in the Natrig K, Larsen TE. Mucocele of the paranasal sinus-
submucosa. es: a retrospective clinical and histological study.
J Laryngol Otol. 1978;92:1075.
Schuknecht HF, Lindsay JR. Benign cyst of the para-
DIFFERENTIAL DIAGNOSIS nasal sinuses. Arch Otolaryngol Head Neck Surg.
1949;49:609.
When a mucocele arises in the antrum, the
Sheth HG, Goel R. Diplopia due to maxillary sinus muco-
diffuse opacification with erosion of the coele. Int Ophthalmol. 2007;27:365-367.
sinus walls cannot be reliably differenti-
ated from tumor. Aspiration that reveals
a mucoid secretion suggests mucocele. A PERIAPICAL INFECTION WITH
Caldwell-Luc procedure with sinus explo- ANTRAL POLYPS
ration and biopsy should be performed. Figure 10-23
TREATMENT Age: Adults
Frontal sinus and ethmoidal mucoceles Sex: No predilection
may extend intracranially. A modified CLINICAL AND RADIOGRAPHIC
Lynch-Howarth surgical procedure is rec- FEATURES
ommended, along with establishment of a Because of the close proximity of the max-
wide and patent nasofrontal duct. Antral illary molar root apices to the antrum,
lesions should be treated in similar fashion, periapical spread of infection often results
employing a Caldwell-Luc approach and in perforation. Acute pulpal infections may
maintaining a large and patent antronasal drain, causing an acute sinusitis. Radio-
opening. graphically, the entire antrum becomes
opacified with intact bony margins. Api-
Additional Reading cal granulomas and cysts may expand the
antral floor cortex or erode and become
Crain MR, Dolan KD, Maves MD. Maxillary sinus muco- confluent with the mucosal lining, thus
cele. Ann Otol Rhinol Laryngol. 1990;99:321. creating an elevated dome-shaped soft
Hesselink JR, Weber AL, New PF, Davis KR, Roberson
GH, Taveras JM. Evaluation of mucoceles of the para-
tissue opacity. Radiographically, when
nasal sinuses with computed tomography. Radiology. cortices are expanded, a halo effect about
1979;133:397-400. the root apex is observed (apical radiolu-
PMPH_Eversole_Chapter-10.indd 504 1/20/2011 3:06:51 PM
Radiopaque Lesions of the Jaws 505
FIGURE 10-23
Endodontic infections may spread into the antrum with overlying polypoid configurations. The teeth test
nonvital.
cency with an eggshell-like cap). When the antrum may fuse with sinus lining so
inflammatory tissue perforates the cortex, that both stratified squamous and respira-
a smooth-surfaced, dome-shaped homog- tory epithelial tissues constitute the cyst
enous opacity emanates from the antral lining.
floor.
DIFFERENTIAL DIAGNOSIS
MICROSCOPIC FEATURES Antral polyps associated with necrotic
Antral polyps secondary to odontogenic teeth appear identical radiographically to
infection are composed of extremely loose antral mucosal cysts. Pulp vitality testing
mucoid areolar granulation tissue exhibit- is essential to uncover the etiology. The
ing a leukocytic infiltrate. The surface is apical periodontal ligament space is often,
covered by respiratory epithelium. Api- yet not invariably, widened in instances
cal periodontal cysts protruding into the involving infected teeth. Because both of
PMPH_Eversole_Chapter-10.indd 505 1/20/2011 3:06:52 PM
506 Chapter 10
these lesions appear as smooth-surfaced, ANTRAL INVASIVE MYCOSES
dome-shaped opacities arising from the Figure 10-24
antral floor, confusion with the more
generalized opacifications represented Age: Adults
by other antral lesions should not be Sex: No predilection
problematic. CLINICAL AND RADIOGRAPHIC
FEATURES
TREATMENT
Fungal sinusitis generally affects only
Once the incriminating tooth has been debilitated patients such as juvenile brittle
treated endodontically or extracted, the diabetics and immunosuppressed indi-
antral lesion resolves. Occasionally, how- viduals. The Phycomycetes and Aspergil-
ever, an osseous protuberance evolves dur- lus organisms may become opportunistic
ing healing. pathogens in the milieu of the immunolog-
ically compromised patient, particularly
in mucormycosis. Maxillary enlargement
Additional Reading with ocular displacement, loosening of
Ericson S, Welander N. Local hyperplasia of maxillary
maxillary teeth, and palatal perforation
sinus mucosa after elimination of adjacent periapical are later manifestations. Radiographi-
osteitis. Odont Rev. 1966;17:153. cally, the antral walls and orbital floor
Matilla, K. Roentgenological investigations into the may exhibit bony erosion, and the entire
relation between periapical lesions and conditions of
antrum is faintly opacified. In aspergillo-
the mucous membrane of the maxillary sinus. Acta
Odontol. Scand. 1965;23:5. sis, radiopaque concretions may be identi-
Nimigean VR, Nimigean V, Maru N, Andressakis D, fied. It has been shown that overfilled root
Balatsouras DG, Danielidis V. The maxillary sinus and canals may predispose to maxillary sinus
its endodontic implications: clinical study and review. aspergillosis.
B-ENT. 2006;2:167-175.
Quiney RE, Brimble E, Hodofe M. Maxillary sinusitis
from dental osseointegrated implants. J Laryngol Otol. MICROSCOPIC FEATURES
1990;104:333.
Worth HM, Stoneman DW. Radiographic interpreta-
The sinus membrane is infiltrated by mono-
tions of antral mucosal changes due to localized dental nuclear inflammatory cells, and the antral
infection. J Can Dent Assoc. 1972;38:111. contents are represented by necrotic debris
FIGURE 10-24
Mucormycosis with orbital
floor erosion.
PMPH_Eversole_Chapter-10.indd 506 1/20/2011 3:07:00 PM
Radiopaque Lesions of the Jaws 507
that is laced with hyphae. The organisms
are readily identifiable with PAS staining. Additional Reading
Spores are prominent in aspergillosis. Blitzer A, Lawson W, Meyers BR, Biller HF. Patient
survival factors in paranasal sinus mucormycosis.
DIFFERENTIAL DIAGNOSIS Laryngoscope. 1980;90:635-648.
DeFoer C, Fossion E, Vaillant JM. Sinus aspergillosis.
The opacification and osseous destruction J Craniomaxillofac Surg. 1990;18:33.
observed in mucormycosis and aspergil- Iwamoto H, Katsura M, Fujimaki T. Mycosis of the max-
illary sinuses. Laryngoscope. 1972;82:903.
losis are reminiscent of carcinoma. A his-
Legent F, Billet J, Beauvillain C, Bonnet J, Miegeville
tory of advanced overt diabetes or systemic M. The role of dental root canal fillings in the devel-
cancer in a patient receiving chemotherapy opment of Aspergillosis sinusitis. A report of 85 cases.
should arouse suspicion of antral mycosis. Arch Otorhinolaryngol. 1989;246:318-320.
Biopsy is the most rapid method of diagno- Odessey E, Cohn A, Beaman K, Schechter L. Invasive
mucormycosis of the maxillary sinus: extensive
sis; however, culture of the sinus contents destruction with an indolent presentation. Surg Infect
is recommended to specifically identify and (Larchmt). 2008;9:91-98.
differentiate the two organisms.
TREATMENT FUNGUS BALL (ASPERGILLUS
Aggressive therapy is indicated because
MYCETOMA)
widespread mycotic osteomyelitis can Figure 10-25
result in massive sequestration of bone.
Age: Adults
The underlying systemic problem should Sex: Female predilection
be controlled if at all feasible, and systemic
antifungal therapy with amphotericin B CLINICAL AND RADIOGRAPHIC
FEATURES
or ketokonazole should be administered.
Both Aspergillus and Phycomycete infec- Aspergillus mycetoma or fungus ball of
tions should also be treated by surgical the paranasal sinuses is a relatively innocu-
curettage. ous colonization of hyphae from Aspergillus
FIGURE 10-25
Polyps with calcification in
localized aspergillosis (fun-
gus ball).
PMPH_Eversole_Chapter-10.indd 507 1/20/2011 3:07:01 PM
508 Chapter 10
species that forms within the sinus lumen, treated with endoscopic surgery. Laryngoscope.
failing to invade the mucous membranes, 2009;119:2275-2279.
Pagella F, Matti E, De Bernardi F, et al. Paranasal sinus
submucosa, or bony wall. A well-demar- fungus ball: diagnosis and management. Mycoses.
cated radiopacity, usually round or oval, is 2007;50:451-456.
identified within the antral cavity.
MICROSCOPIC FEATURES
ALLERGIC FUNGAL SINUSITIS
Fungus ball is composed of matted colonies Figure 10-26
of hyphae without any host response other
than a few adherent leukocytes. The branch- Age: Adults
ing hyphae are distinguishable from phy- Sex: No predilection
comycetes and bipolaris fungi and readily CLINICAL AND RADIOGRAPHIC
stain with PAS or Grocott’s methenamine FEATURES
silver (GMS) fungal stains.
Inhalation of otherwise harmless soil fungi
of the Bipolaris genus results, among suscep-
DIFFERENTIAL DIAGNOSIS
tible patients, in a fulminant allergic reac-
The opacity of fungus ball must be differen- tion with pronounced tissue eosinophilia.
tiated from foreign body, misplaced teeth, The host response rather than the organism
and odontomas and antrolith. accounts for the symptoms of nasal stuffi-
ness and blockage. Imaging studies of the
TREATMENT maxillary sinus typically reveal unilateral
Endoscopic surgery with removal of the involvement with opacification of the sinus
fungal mass usually results in cure. and resorption, apposition, and erosion of
the sinus wall.
Additional Reading MICROSCOPIC FEATURES
Costa F, Polini F, Zerman N, Robiony M, Toro C, Politi The material curetted from the sinus has
M. Surgical treatment of Aspergillus mycetomas of the the gross appearance of “peanut butter.”
maxillary sinus: review of the literature. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 2007;103:e23-e29.
Microscopically, necrosis and eosinophils
Nicolai P, Lombardi D, Tomenzoli D, et al. Fungus ball are seen as layed smudge. Chacot-Leyden
of the paranasal sinuses: experience in 160 patients crystals are usually prominent and scat-
FIGURE 10-26
Allergic fungal sinusitis
showing bony invasion and
expansion is typically asso-
ciated with noninvasive
pleomorphic soil fungi.
PMPH_Eversole_Chapter-10.indd 508 1/20/2011 3:07:02 PM
Radiopaque Lesions of the Jaws 509
tered colonies of large pleomorphic hyphae Rupa V, Jacob M, Mathews MS, Seshadri MS. A
are evident and readily demonstrated with prospective, randomised, placebo-controlled tri-
al of postoperative oral steroid in allergic fungal
PAS or GMS fungal stains. sinusitis. Eur Arch Otorhinolaryngol. 2010;267:
233-238.
DIFFERENTIAL DIAGNOSIS Schubert MS. Allergic fungal sinusitis: pathophysiology,
diagnosis and management. Med Mycol. 2009;47(suppl.
The expansile and osseous resorptive 1):S324-S330.
changes seen on imaging studies in allergic
fungal sinusitis are ominous findings and
malignancy must be included in the differ- DISPLACED TEETH, ROOTS,
ential diagnosis. AND FOREIGN BODIES
TREATMENT Figure 10-27
Thorough sinus lavage and curettage are Age: Adults
indicated followed by a 12-week course of Sex: No predilection
systemic corticosteroids. CLINICAL AND RADIOGRAPHIC
FEATURES
Additional Reading Teeth or root fragments within the sinus
are usually readily identifiable by their
Chan Y, Kuhn FA. An update on the classifications, morphologic features and radiologic
diagnosis, and treatment of rhinosinusitis. Curr Opin identification of a pulp chamber or root
Otolaryngol Head Neck Surg. 2009;17:204-208.
Marfani MS, Jawaid MA, Shaikh SM, Thaheem K.
canal shadow. They may radiographically
Allergic fungal rhinosinusitis with skull base and orbit- appear in this location as a consequence
al erosion. J Laryngol Otol. 2009 3:1-5. of (1) traumatic displacement, (2) displace-
FIGURE 10-27
Displaced teeth in the sinuses.
PMPH_Eversole_Chapter-10.indd 509 1/20/2011 3:07:04 PM
510 Chapter 10
ment of fractured root tips after exodon- surgically. A longstanding asymptomatic
tia, (3) developmental displacement, or (4) displaced root fragment may be left in place
superior displacement by an enlarging and monitored on a regular basis.
dentigerous cyst. Water’s views are not as
efficacious as periapical, Caldwell, and lat-
eral sinus views. When teeth or roots lie Additional Reading
within the sinus cavity, they may change
Gupta AC, Murthy DP, Pulotu ML. Unusual type of
positions with head movement. More often, foreign body in the maxillary sinus. J Laryngol Otol.
the tooth fragment is trapped between the 1990;104:718.
antral bony floor and the lining membrane; Harvinder S, Jenny L, Gurdeep S. An arrow in the maxil-
in these instances, a change in head posi- lary sinus. Med J Malaysia. 2008;63:333-334.
Jones EH, Steel JS. Roots in the maxillary sinus. Aust
tion will not alter the localization radio- Dent J. 1969;14:8.
graphically. Unerupted teeth appearing to Lownie JF, Lemmer J, Sykes L. Chronic maxillary sinus-
lie within the sinus often are not, in actual- itis resulting from displacement of impression material
ity, within the sinus itself. Rather, they are into the maxillary antrum: a case report. Tyd Van Tand
Veren Van Suid Afrika. 1989;44:341.
encased in bone and show a periodontal Van Wowern N. Oroantral communications and dis-
ligament space with an eggshell-thin cor- placements of roots into the maxillary sinus. J Oral
tex interposed between tooth and sinus Maxillofac Surg. 1971;29:622.
cavity. Last, it should be stressed that dur-
ing surgery, a tooth may be displaced into
the infratemporal space, or a root tip may AUGMENTATION MATERIALS
become lodged between the periosteum Figure 10-28
and outer cortical table. A variety of radio-
graphic projections and tomography help Age: Adults
to pinpoint the precise location. Root tips Sex: No predilection
lying free within the sinus may serve as CLINICAL AND RADIOGRAPHIC
an infectious source with resultant sinus- FEATURES
itis and diffuse opacification. Rarely, other Sinus lift surgery is performed to cre-
foreign bodies may reside within the sinus. ate bone bulk in order to support dental
Impression material forced through an metallic implants. The mucosal sinus floor
oral-antral fistula and traumatically placed is elevated and a variety of augmentation
metals are more common. materials are placed between the sinus floor
bone and the elevated membrane. Autoge-
MICROSCOPIC FEATURES nous bone and synthetic calcific materials
Not applicable. used to stimulate osteogenesis are placed.
Radiographically, a floccular appearance is
DIFFERENTIAL DIAGNOSIS seen represented by multiple calcified par-
ticles. Most augmentations provide 8 to 10
Focal opacities representing teeth or roots mm of height.
may be confused radiographically with
osteoma, exostosis, or antrolith. Usually, MICROSCOPIC FEATURES
the opacity is recognizable by virtue of its
morphology as tooth structure. Inert calcified particles are observed or
intact lamellar bone fragments are seen
with surrounding mature collagenous con-
TREATMENT
nective tissue. Appositionally, neo-osteo-
Using a Caldwell-Luc approach, intrasinus genesis is seen and some of the nonviable
teeth and/or root tips should be removed materials are partially resorbed.
PMPH_Eversole_Chapter-10.indd 510 1/20/2011 3:07:12 PM
Radiopaque Lesions of the Jaws 511
FIGURE 10-28
Powdered calcifications in
sinus lift surgeries to aug-
ment bone support for
integrated dental implants.
DIFFERENTIAL DIAGNOSIS dental implants: radiographic appearance. AJR Am J
Roentgenol. 2000;174:1289-1292.
These augmentation sites must be differ- Tiwana PS, Kushner GM, Haug RH. Maxillary sinus
entiated from osteogenic and odontogenic augmentation. Dent Clin North Am. 2006;50:409-424,
tumors. Furthermore, the surgically placed vii.
materials lack encapsulation as seen in
many benign cysts and tumors. Of course,
ANTROLITH/RHINOLITH
history is the main revealing factor.
Figure 10-29
TREATMENT Age: Adults
No treatment. Sex: No predilection
CLINICAL AND RADIOGRAPHIC
FEATURES
Additional Reading Stones arising in the antral cavities are
Abrahams JJ. Augmentation procedures of the jaw in uncommon. They may develop around a
patients with inadequate bone for dental implants: nidus, which usually represents a foreign
radiographic appearance. J Comput Assist Tomogr.
2000;24:152-158.
body such as a tooth root; on the other
Abrahams JJ, Hayt MW, Rock R. Sinus lift procedure hand, no particular material may be iden-
of the maxilla in patients with inadequate bone for tified as serving as the nidus for mineral-
PMPH_Eversole_Chapter-10.indd 511 1/20/2011 3:07:12 PM
512 Chapter 10
FIGURE 10-29
Antroliths represent dys-
trophic calcifications.
ization. Microbial colonies in bacterial and
mycotic antral infections may serve as a Additional Reading
matrix for calcification as well. The antrolith Allen GA, Liston SL. Rhinolith: unusual appearance
may be associated with dull pain or ache, on panoramic radiograph. J Oral Maxillofac Surg.
mimicking sinusitis. Radiographically, a 1979;37:54.
dense, irregular yet well-defined mass can Blaschke DD, Brady FA. The maxillary antrolith. Oral
Surg Oral Med Oral Pathol. 1979;48:187.
be identified in the antrum, usually rest- Cohen MA, Packota GV, Hall MJ, Steinberg J. Large
ing on the antral floor. Stones may develop asymptomatic antrolith of the maxillary sinus. Report of
within the nasal cavity; they are obvious on a case. Oral Surg Oral Med Oral Pathol. 1991;71:155-
panoramic views, Water’s radiographs, and 157.
Karges MA, Eversole LR, Poindexter BJ Jr. Antrolith:
tomograms. report of case and review of literature. J Oral Maxillofac
Surg. 1971;29:813.
MICROSCOPIC FEATURES Lord OC. Antral rhinoliths. J Laryngol Otol.
1944;59:218.
Decalcified specimens are composed of
dystrophic calcified amorphous matrices.
The adjacent antral membrane may be poly- ODONTOGENIC TUMORS
poid with a submucosal inflammatory cell Figure 10-30
infiltrate.
Age: Teenagers and adults
DIFFERENTIAL DIAGNOSIS Sex: No predilection
A radiopacity with well-defined margins CLINICAL AND RADIOGRAPHIC
located in the antrum can be differentiated FEATURES
from an antral retention cyst. A root frag- Occasionally, a maxillary odontoma devel-
ment located in the antrum is perhaps more ops in the maxillary bones of the sinus wall.
common. The osteomas in Gardner’s syn- Alternatively, some odontomas actually lie
drome often localize within the sinuses as free within the sinus cavity without an envel-
well. oping osseous encasement. Free odontomas
within the sinus often manifest symptoms
TREATMENT
of dull aching pain and nasal discharge and
Antroliths should be removed because they predispose to a chronic sinusitis. Radio-
irritate the sinus lining and predispose to graphically, the opacity may be focal; more
sinusitis. often, multifocal confluent opacities are clus-
PMPH_Eversole_Chapter-10.indd 512 1/20/2011 3:07:24 PM
Radiopaque Lesions of the Jaws 513
FIGURE 10-30
Odontogenic tumors in
the maxilla may erode into
the sinuses.
tered, and a fully formed unerupted tooth tates biopsy. Soft tissue densities from other
lies juxtaposed to the hamartomatous ele- types of odontogenic tumors will simulate
ment. Free odontomas change position when the other sinuses lesions described here.
the head is moved during procurement of
various maxillary radiographs. If the odon- TREATMENT
toma is encased in bone or entrapped under A Caldwell-Luc approach with surgical
the sinus membrane, no positional change removal is the treatment of choice. Any associ-
occurs. Maxillary odontogenic tumors such ated tooth should be removed in continuity. In
as ameloblastoma, calcifying epithelial odon- addition, any polypoid lesions resulting from
togenic tumor, and odontogenic myxoma irritation by the tumor should be excised.
among others may proliferate and perforate
the antral floor where they may then grow
freely in the sinus showing a soft tissue den- Additional Reading
sity in the sinus cavity. Alternatively, there
Caton RB, Marble HB Jr, Topazian RG. Complex odon-
are some instances that have evolved within toma in the maxillary sinus. J Oral Maxillofac Surg.
the sinus, separate from the alveolus. 1973;36:658.
Clayman GL, Marentette LJ. Complex odontoma of the
MICROSCOPIC FEATURES maxillary sinus with a complete dentition. Otolaryngol
Head Neck Surg. 1989;101:581.
Haphazardly arranged dental hard tis- Ereño C, Etxegarai L, Corral M, Basurko JM, Bilbao FJ,
sues, including enamel matrix, dentin, and López JI. Primary sinonasal ameloblastoma. APMIS.
2005;113:148-150.
cementum, are present and often histologi- Osborne TP, Park JK, Levy BA, Tewes WD. Odontoma
cally mimic miniature tooth buds. Dental containing ghost cells in the maxillary sinus. Oral Surg
pulp with an odontoblastic layer is usually Oral Med Oral Pathol. 1974;38:819-823.
identifiable, and odontogenic epithelium Press SG. Odontogenic tumors of the maxillary sinus. Curr
Opin Otolaryngol Head Neck Surg. 2008;16:47-54.
lies adjacent to enamel matrix. A fibrous
follicle is also present. The microscopic
features of other odontogenic tumors are OSTEOMAS AND EXOSTOSES
described elsewhere in chapters 9 and 10. Figure 10-31
DIFFERENTIAL DIAGNOSIS Age: Adults
Sex: No predilection
Composite odontomas with multiple tooth-
like configurations are easily recognized CLINICAL AND RADIOGRAPHIC
FEATURES
radiographically. Complex varieties may be
confused radiographically with osteoma or Ossified bodies (osteomas) and bony excres-
antrolith; thus, a definitive diagnosis necessi- cences (exostoses) may be found within
PMPH_Eversole_Chapter-10.indd 513 1/20/2011 3:07:27 PM
514 Chapter 10
the antrum, although they are more com- DIFFERENTIAL DIAGNOSIS
mon in the frontal and ethmoidal sinuses. Osteomas may be radiographically indis-
Antral cases are quite rare, and the etiology tinguishable from antroliths or complex
is obscure. Identification of an osteoma in odontomas. Once biopsy has confirmed
the antrum should alert the clinician to the a diagnosis of osteoma, paranasal sinus
possibility of Gardner’s syndrome, charac- radiographic series and jaw radiographs
terized by supernumerary teeth, osteomas should be obtained to uncover osteoma-
of the jaws and sinuses, desmoid tumors tous lesions. Should they be discovered, a
of the skin, and premalignant adenoma- work-up for Gardner’s syndrome should be
tous polyposis coli. Antral osteomas may undertaken.
predispose to sinusitis with symptoms of
maxillary pain and nasal discharge. Radio- TREATMENT
graphically, osteomas may be seen as single
or multiple round or oval radiopacities. A The Caldwell-Luc approach should be used
concomitant sinusitis may show a fluid to remove the lesion along with hyperplastic
level or diffuse opacification of the affected sinus membrane or polyps. As mentioned
sinus. Exostoses are firmly adherent and previously, Gardner’s syndrome should
confluent with the sinus wall, usually the be ruled out by referral to an internist or
lateral wall. gastroenterologist.
MICROSCOPIC FEATURES
Additional Reading
Both osteomas and exostoses are com-
Fu YS, Perzin KH. Non-epithelial tumors of the nasal
posed of mature lamellar bone. They are
cavity, paranasal sinuses, and nasopharynx: a clinico-
usually ovoid bodies with an outer corti- pathologic study. Osseous and fibro-osseous lesions,
cal margin that encases a medullary trabe- including osteoma, fibrous dysplasia, ossifying fibro-
cular zone. The marrow spaces are repre- ma, osteoblastoma, giant cell tumor and osteosarcoma.
sented by areolar fibrous or adipose tissue. Cancer. 1974;33:1289.
Herd JR. Exostoses of the sinus wall: a diagnostic prob-
When multiple osteomas occur, the ossi- lem. Aust Dent J. 1974;19:269.
fied bodies are usually discrete, separated Karmody CS. Osteoma of maxillary sinus. Laryngoscope.
from one another by mature fibrous tissue. 1969;79:427.
Some sinus osteomas will demonstrate Liston LS, Barker BF, Cocayne DR. Multiple osteo-
mas of the maxillary sinus. J Oral Maxillofac Surg.
osteoblastoma-like histologic foci, a fea- 1979;37:113.
ture that does not portend a more aggres- McHugh JB, Mukherji SK, Lucas DR. Sino-orbital osteo-
sive potential. ma: a clinicopathologic study of 45 surgically treated
FIGURE 10-31
Osteomas of the antrum.
PMPH_Eversole_Chapter-10.indd 514 1/20/2011 3:07:30 PM
Radiopaque Lesions of the Jaws 515
cases with emphasis on tumors with osteoblastoma-like lateral sinus wall medially; ossifying and
features. Arch Pathol Lab Med. 2009;133:1587-1593. cementifying fibromas as well as maxillary
odontogenic tumors may behave in this
fashion. Ameloblastomas of the maxilla
BENIGN MESENCHYMAL can perforate into the antral space. Primary
NEOPLASMS benign neoplasms grow to fill the sinus air
Figure 10-32 space with symptoms of swelling and nasal
congestion. Radiographically, diffuse opaci-
Age: Adults fication is observed; in larger neoplasms,
Sex: No predilection the sinus walls may exhibit expansion with
CLINICAL AND RADIOGRAPHIC bowing in all dimensions, particularly obvi-
FEATURES ous along the medial wall on sinus films.
Benign neoplasms of connective tissue ori- Osseous erosion and perforation can also
gin arising in the antrum are rare. Vascu- occur with benign neoplasms.
lar and nerve sheath neoplasms are more
MICROSCOPIC FEATURES
frequently encountered; these lesions arise
primarily within the submucosa of the The histologic features vary depending on
sinus membrane. Intraosseous neoplasms the cell of origin. The reader is referred to
of the maxilla may expand and displace the the chapter on oral soft tissue swellings for
FIGURE 10-32
Benign mesenchymal
tumors, a nerve sheath
tumor (upper right), juve-
nile ossifying fibroma
(upper left), anuerysmal
bone cyst (below).
PMPH_Eversole_Chapter-10.indd 515 1/20/2011 3:07:35 PM
516 Chapter 10
microscopic descriptions of vascular and Shugar JM, Son PM, Biller HF, Som ML, Krespi YP.
neural sheath neoplasms. Peripheral nerve sheath tumors of the paranasal sinus-
es. Head Neck Surg. 1981;4:72.
DIFFERENTIAL DIAGNOSIS
The diffuse opacifications seen in benign INVERTING PAPILLOMA
mesenchymal neoplasms along with symp- Figure 10-33
toms of congestion may be confused with
sinusitis. When expansion and erosion are Age: Middle-aged adults
present, mycotic infections and malignant Sex: Male predilection
tumors must be considered, and immediate CLINICAL AND RADIOGRAPHIC
exploration with biopsy is recommended. FEATURES
Unlike the common inflammatory nasal and
TREATMENT
antral polyp, the inverting or Schneiderian
Most benign neoplasms of connective tissue papilloma represents a true neoplastic pro-
origin can be treated by curettage or exci- cess arising from the ectodermally derived
sion. Osseous invasion or large destructive epithelium. Human papillomaviruses are
lesions may require hemimaxillectomy. of etiologic importance in fungiform pap-
illomas of the nasal cavity yet are rarely
Additional Reading encountered in the inverting papilloma. It
arises from the lateral nasal wall, either in
Agarwal MK, Gupta OP, Samant HC, Gupta S. the region of the middle turbinate or ethmoi-
Neurilemmoma of the maxillary sinus. J Oral Maxillofac dal recess. The lesion invades the submucosa
Surg. 1980;38:698-699. and frequently, either via the ostium or by
Fu YS, Perzin KH. Non-epithelial tumors of the nasal bony erosion, extends into the antral or eth-
cavity, paranasal sinuses, and nasopharynx: a clini-
copathologic study. I. General features and vascular moidal sinus. Clinically, the most common
tumors. Cancer. 1974;33:1275. symptom is nasal obstruction. Radiographi-
LaBruna A, Reagan B, Papageorge A. Leiomyoma of cally, the affected sinus is opacified; maxil-
the maxillary sinus: a diagnostic dilemma. Otolaryngol lary tomograms often disclose destruction
Head Neck Surg. 1995;112:595-598.
Sheppard LM, Mickelson SA. Hemangiomas of the nasal
of the medial antral wall with opacification
septum and paranasal sinuses. Henry Ford Hosp Med of the nasal cavity. Importantly, carcinoma
J. 1990;38:25. is associated with inverting papilloma in 7%
FIGURE 10-33
Aggressive inverting pap-
illomas of the sinonasal
tract may transform into
carcinoma.
PMPH_Eversole_Chapter-10.indd 516 1/20/2011 3:07:43 PM
Radiopaque Lesions of the Jaws 517
of the cases. The common fungiform papil- Astor FC, Donegan JO, Gluckman JL. Unusual anatomic
loma is limited to the nasal septum and does presentations of inverting papilloma. Head Neck Surg.
1985;7:243-245.
not invade the maxillary sinus. Hyams VJ. Papillomas of the nasal cavity and paranasal
sinuses. A clinicopathological study of 315 cases. Ann
MICROSCOPIC FEATURES Otol Rhinol Laryngol. 1971;80:192.
Snyder RN, Perzin KH. Papillomatosis of nasal cavity
Inverting papillomas, as the term implies, and paranasal sinuses (inverted papilloma, squamous
grow in inverted fashion into the subjacent papilloma). A clinicopathologic study. Cancer.
sinus and nasal submucosa. Budding folds 1972;30:668.
of stratified squamous epithelium are fre- Suh KW, Facer GW, Devine KD, Weiland LH, Zujko
RD. Inverting papilloma of the nose and paranasal
quently covered by a single row of ciliated sinuses. Laryngoscope. 1977;87:35-46.
columnar cells. Microcysts with mucin are
located throughout the spinous cell layer. A
rare variant termed cylindric cell (oncocytic) ANTRAL CARCINOMA
papilloma may also invade the antrum. The Figure 10-34
inverted architecture prevails; however, the
tumor element is represented by eosino- Age: Elderly adults
philic columnar cells, which may show sur- Sex: Male predilection
face cilia. CLINICAL AND RADIOGRAPHIC
FEATURES
DIFFERENTIAL DIAGNOSIS
Maxillary sinus carcinoma rarely manifests
Complete antral opacification with invert- worrisome signs or symptoms in the early
ing papilloma may be encountered in many stages. Patients may complain of unilat-
other benign and malignant lesions of eral dull sinus pain along with nasal dis-
the maxillary sinus. A concurrent opaque charge, which masquerade as sinusitis. The
mass in the ipsilateral nasal cavity sug- majority of cases represent squamous cell
gests inverted papilloma; however, biopsy carcinoma; transitional cell or anaplastic
is required for a definitive diagnosis. carcinoma and adenocarcinoma of lining
cell origin are less common. Occasionally,
TREATMENT adenocarcinomas of tubuloacinus origin
Inverting papillomas are aggressive, and occur in the antrum and show histopatho-
more than 60% recur after simple excision logic features similar or identical to sali-
(polypectomy). Computed tomographic vary tumors. As these malignant tumors
(CT) scans or paranasal sinus tomograms proliferate, they fill the sinus cavity, and in
are recommended to determine the extent later stages, they induce osseous destruc-
of disease. Lateral rhinotomy offers the tive changes. Medial growth perforates the
greatest chance for cure. Interestingly, this nasal cavity, superior growth may displace
lesion tends to recur more often in females. the eye with diplopia, posterior extension
Carcinomatous transformation requires into the pterygopalatine and pterygoman-
hemimaxillectomy with extended margins dibular spaces may cause trismus, and
and radiation therapy. inferior extension causes loosening of max-
illary teeth with palatal enlargement or
perforation. Infraorbital paresthesia may be
Additional Reading featured, and facial expansion can occur.
Radiographically, opacification is observed;
Arendt DM, Platkajs MA, Lusby TF, Scofield HH.
Cylindrical cell papilloma. Report of a case with light
with conventional sinus radiographs, sinus
and ultrastructural analysis. Oral Surg Oral Med Oral tomograms, and CT scans, osseous destruc-
Pathol. 1986;61:382-387. tive changes can be identified in advanced
PMPH_Eversole_Chapter-10.indd 517 1/20/2011 3:07:46 PM
518 Chapter 10
FIGURE 10-34
Squamous cell carcinoma
and sinonasal undifferen-
tiated carcinoma (SNUC,
right) are osseous destruc-
tive, the latter being uni-
versally fatal.
cases. Extension into other sinuses and cra- Both adenoid cystic and mucoepidermoid
nial base involvement may be extant at the carcinoma may be encountered.
time of admission. Despite the advanced
stage and diffuse extent of disease, palpa- DIFFERENTIAL DIAGNOSIS
ble nodes in the submandibular and upper Early tumors may exhibit opacification
neck regions are encountered in less than without destruction of the bony walls and
20% of these patients. may therefore simulate sinusitis. When
Other carcinomas may arise within osseous destruction is witnessed, sarcomas
or invade the maxillary sinus including and mycotic infections must be included
ameloblastic carcinoma, primary adeno- in the radiographic diagnosis. Persistent
carcinoma, salivary gland carcinomas, and opacification following conventional ther-
metastatic carcinomas, renal cell carcinoma apy for sinusitis should be explored and
in particular. biopsied.
MICROSCOPIC FEATURES TREATMENT
Squamous cell carcinoma, which is most Most antral cancers are advanced (T3, T4)
common, shows proliferating islands and by the time they are discovered. Maxillec-
cords of epidermal cells with keratin forma- tomy with exploration and surgical excision
tion that is generally not abundant. Occa- of tumor in contiguous sinus cavities fol-
sionally, adjacent tissue represents inverted lowed by postoperative external radiation
papilloma that has undergone carcinoma- (7500 rad) offers the best chance for cure.
tous transformation. Adenocarcinomas Five-year survival for T3 and T4 lesions is
show tubular and ductal differentiation. about 75% and 35%, respectively.
PMPH_Eversole_Chapter-10.indd 518 1/20/2011 3:07:46 PM
Radiopaque Lesions of the Jaws 519
sionally, metastatic neoplasms are located
Additional Reading in the antrum. These malignant mesen-
Angiero F, Borloni R, Macchi M, Stefani M. Ameloblastic chymal neoplasms share common clinical
carcinoma of the maxillary sinus. Anticancer Res. and radiographic findings that are similar
2008;28:3847-3854. to those observed in antral carcinoma. As
Hata M, Tokuuye K, Shioyama Y, et al. Malignant myoep- the neoplasm proliferates with the sinus,
ithelioma in the maxillary sinus: case report and review
of the literature. Anticancer Res. 2009;29(2):497-501. expansion with facial swelling may be
Jackson RT, Fitz-hugh GS, Constable WC. Malignant encountered along with extension of a mass
neoplasms of the nasal cavities and paranasal sinuses into the nasal fossa, superior displacement
(retrospective study). Laryngoscope. 1977;87:726. of the eye, and palatal swelling with loosen-
Larsson LG, Mårtensson G. Maxillary antral cancers.
JAMA. 1972;219:342.
ing of the maxillary teeth. Infraorbital par-
Sakai S, Shigematzu Y, Fuchihata H. Diagnosis and esthesia and epistaxis are common signs
TNM classification of maxillary sinus carcinoma. Acta and symptoms, particularly with lymphoma
Otolaryngol (Stockh). 1972;74:123. and plasmacytoma. Radiographically, dif-
Spiro JD, Soo KC, Spiro RH. Squamous carcinoma of
the nasal cavity and paranasal sinuses. Am J Surg.
fuse opacification is seen with expansion
1989;158:328. and sinus wall osseous destruction. Water’s
views and tomograms often show opacifi-
cation of the ipsilateral nasal cavity, and CT
ANTRAL SARCOMA scans aid in determining extent of disease.
Figure 10-35
MICROSCOPIC FEATURES
Age: Adults
Sex: Male predilection Lymphomas are characterized by sheets of
neoplastic lymphoblasts and may be diffuse
CLINICAL AND RADIOGRAPHIC or nodular. Malignant reticulosis, which
FEATURES
represents a specific form of lymphoma that
Malignant lymphomas and extramedul- affects the upper air passages, may also be
lary plasmacytomas are the most common encountered. Extramedullary plasmacy-
malignant mesenchymal tumors found tomas are composed of diffuse sheets of
to arise in the maxillary sinus. Malignant plasma cells with a scant vascular stroma.
fibrous histiocytoma, rhabdomyosarcoma, Many lesions of this nature are associated
and fibrosarcoma may also occur; occa- with or progress to multiple myeloma.
FIGURE 10-35
Sarcomas are destructive expansile lesions that rarely arise in the sinus. Malignant fibrous histiocytoma is
the most common type to occur in the antrum.
PMPH_Eversole_Chapter-10.indd 519 1/20/2011 3:07:50 PM
520 Chapter 10
Malignant spindle cells with bizarre nuclei
are seen in fibrosarcoma, malignant fibrous
histiocytoma, and rhabdomyosarcoma.
DIFFERENTIAL DIAGNOSIS
Clinical evidence of epistaxis in conjunction
with antral disease represents an ominous
finding. Radiographically, expansile and
osseous destructive changes occurring in
malignant mesenchymal sinus tumors can-
not be differentiated from carcinoma. Biopsy
is required for a definitive diagnosis.
TREATMENT
Lymphoma and plasmacytoma respond to
6000 rad of external beam radiation ther-
apy. Spindle cell malignancies require radi- FIGURE 10-36
cal maxillectomy. A thorough work-up for In the silent sinus syndrome, a unilateral collapse of
involvement of other organ systems and the antrum is seen and in this instance, sinus polyps
bones should be undertaken. are evident.
Additional Reading sis of the maxillary sinus. Enophthalmos and
hypoglobus are secondary to thinning and
Fu YS, Perzin KH. Non-epithelial tumors of the nasal
cavity, paranasal sinuses and nasopharynx. A clinico- inward curvature of the maxillary sinus roof.
pathologic study. X. Malignant lymphoma. Cancer. There are no symptoms of intrinsic sinona-
1979;43:611. sal inflammatory disease. On imaging, the
Merrick RE, Rhone DP, Chilis TJ. Malignant fibrous affected sinus is atrophied and opacified.
histiocytoma of the maxillary sinus. Case report and
literature review. Arch Otolaryngol Head Neck Surg.
1980;106:365. MICROSCOPIC FEATURES
Prassanna NM, Mendelsohn M. Maxillary sinus sarco- The sinus is replaced by mature lamellar
mas. Can J Otolaryngol. 1975;4:704.
Schabel SI, Rogers CI, Rittenberg GM, Bubanj bone and fibrous marrow.
R. Extramedullary plasmacytoma. Radiology.
1978;128:625-628. DIFFERENTIAL DIAGNOSIS
Wang CP, Chang YL, Ting LL, Yang TL, Ko JY, Lou PJ.
Malignant fibrous histiocytoma of the sinonasal tract. The condition can be distinguished from
Head Neck. 2009;31:85-93. other sinus opacities based on the clinical
finding of atrophy with progressive change
that begins in teenage years.
SILENT SINUS SYNDROME
Figure 10-36 TREATMENT
Surgical correction is indicated.
Age: Teens, young adults
Sex: No predilection
CLINICAL AND RADIOLOGIC FEATURES Additional Reading
Silent sinus syndrome presents as a facial Brandt MG, Wright ED. The silent sinus syndrome is
asymmetry secondary to unilateral atelecta- a form of chronic maxillary atelectasis: a systematic
PMPH_Eversole_Chapter-10.indd 520 1/20/2011 3:07:54 PM
Radiopaque Lesions of the Jaws 521
review of all reported cases. Am J Rhinol. 2008;22: G protein that plays a role in coupling cAMP
68-73. to hormone receptors. It may exist as a soli-
Habibi A, Sedaghat MR, Habibi M, Mellati E. Silent
sinus syndrome: report of a case. Oral Surg Oral Med tary lesion (the monostotic form), as multiple
Oral Pathol Oral Radiol Endod. 2008;105(3):e32- lesions involving many bones of the jaws and
e35. cranium (the craniofacial form), or through-
Monos T, Levy J, Lifshitz T, Puterman M. The silent out the skeleton (the polyostotic variety).
sinus syndrome. Isr Med Assoc J. 2005;7:333-335.
The latter may be complicated by endocrine
defects, including precocious puberty, goiter,
Ground-Glass and café-au-lait macular pigmentations of the
skin. This form of polyostotic fibrous dyspla-
Radiopacities sia is known as Albright’s syndrome. When
long bones are affected, deformed limbs and
FIBROUS DYSPLASIA pathologic fractures are frequent findings.
(FIGURES 10-37A & 10-37B) The monostotic variant is by far the most
common type seen when the jaw is affected.
Age: Teenagers and young adults
Sex: No predilection
The disease is a painless expansile dysplastic
process of osteoprogenitor connective tissue.
CLINICAL AND RADIOGRAPHIC Slow growth is seen with progressive facial
FEATURES deformity. Pain and paresthesia are generally
Fibrous dysplasia is the most common dis- lacking. The maxilla is most often the site of
ease of the jaws to manifest a ground-glass involvement. When the mandible is affected,
radiographic pattern. It is molecularly char- the radiographic pattern is more apt to be
acterized by a mutation in the α-subunit of multicystic or mottled. The maxillary lesion
FIGURE 10-37A
Fibrous dysplasia showing ground-glass patterns.
PMPH_Eversole_Chapter-10.indd 521 1/20/2011 3:08:03 PM
522 Chapter 10
FIGURE 10-37B
Fibrous dysplasia showing mottled patterns.
is monotonously ground-glass or “orange- DIFFERENTIAL DIAGNOSIS
peel” in configuration, shows expansion, and The ground-glass pattern of fibrous dyspla-
characteristically lacks margination. Rather, sia may be encountered in the early stages
the dysplastic process appears to blend sub- of osteitis deformans and in hyperparathy-
tly into the adjacent trabecular bone. The roidism. Osteitis deformans characteristi-
lesion does not cross the midline and shows cally crosses the midline, is a disease of
a tendency to limit itself to one bone, cross- elderly people, and produces significantly
ing sutures only occasionally. The antrum elevated serum alkaline phosphatase lev-
is often obliterated, and involvement of the els. During early or active growth stages
orbital floor may displace the globe. of fibrous dysplasia, serum alkaline phos-
MICROSCOPIC FEATURES
phatase levels may be elevated as well.
Hyperparathyroidism is more apt to mani-
Dispersed throughout a hypercellular fest brown tumors of the jaws than ground-
fibrous stroma are irregular, haphazardly glass lesions. A skeletal survey should be
arranged osseous trabeculae with no struc- taken to rule out polyostotic lesions.
tural arrangement; however, a retiform pat-
tern may be discerned in some cases. With
TREATMENT
polarized light, most of the trabeculae show
a woven bone pattern, but the presence of Treatment should be deferred, if pos-
lamellar trabeculae does not militate against sible, until skeletal maturity is reached.
a diagnosis of fibrous dysplasia. Attempts to intervene surgically during
PMPH_Eversole_Chapter-10.indd 522 1/20/2011 3:08:24 PM
Radiopaque Lesions of the Jaws 523
the lesional growth phase may actually that parallel those of fibrous dysplasia in
activate the process. Fibrous dysplasia many respects. Patients complain of epi-
tends to become arrested and static at the sodic mandibular pain manifested as a
same time that the epiphyseal growth cen- mild nagging ache and clinical examination
ters close. A rare aggressive form of the reveals cortical expansion. Radiographi-
disease known as active juvenile fibrous dys- cally, a diffuse ground-glass opacification
plasia shows rapid aggressive growth, par- is seen with indistinct margins. Usually, on
ticularly in the maxilla, and may invade axial CT of occlusal images, cortical redun-
the cranial base. Extremely aggressive dancy (onion skinning) is identified (Garré’s
clinical behavior in the face of cellularly phenomenon). The etiology is unknown in
active disease requires partial maxillec- many instances whereas in others a possible
tomy to achieve control. Taking the afore- odontogenic source of infection is uncov-
mentioned features into consideration, ered (caries, pulpal inflammation, tooth
it is recommended that children with a fracture). In some, yet not all, instances a
diagnosis of fibrous dysplasia be followed trephine bone sample can be culture posi-
quarterly with clinical, radiographic, and tive for anaerobic bacteria.
periodic study-model evaluation to deter-
mine whether accelerated or diminished MICROSCOPIC FEATURES
growth is taking place.
A fibro-osseous pattern is seen with anas-
tomosing trabeculae along with other fields
Additional Reading of diffuse osteosclerosis. The fibrous ele-
ment is not as cellular as seen in other fibro-
Eversole LR, Sabes WR, Rovin S. Fibrous dysplasia: a osseous lesions. Paradoxically, a robust
nosologic problem in the diagnosis of fibro-osseous
lesions of the jaws. J Oral Pathol Med. 1972;1:189. inflammatory infiltrate is lacking although
Eversole R, Su L, ElMofty S. Benign fibro-osseous a few small clusters of lymphocytes may be
lesions of the craniofacial complex. A review. Head encountered.
Neck Pathol. 2008;2:177-202.
Obisesan AA, et al. The radiologic features of fibrous
dysplasia of the craniofacial bones. Oral Surg Oral DIFFERENTIAL DIAGNOSIS
Med Oral Pathol. 1977;44:949.
The chief entity in the differential is fibrous
Waldron CA, Giansanti JS. Benign fibro-osseous lesions
of the jaws: a clinical-radiologic-histologic review of dysplasia. Clinically, the occurrence of par-
sixty-five cases. I. Fibrous dysplasia of the jaws. Oral oxysmal dull pain, Garré’s phenomenon, a
Surg Oral Med Oral Pathol. 1973;35:190. potential source of infection and the micro-
Zimmerman DC, Dahlin DC, Stafne EC. Fibrous dys- scopic features of a more mature osteogen-
plasia of the maxilla and mandible. Oral Surg Oral
Med Oral Pathol. 1958;11:55. esis allow for establishment of a definitive
diagnosis of chronic diffuse sclerosing
osteomyelitis.
CHRONIC DIFFUSE
SCLEROSING OSTEOMYELITIS TREATMENT
Figure 10-38 Long-term or intravenous antibiotic therapy
usually only provides temporary relief, yet
Age: Children, teens
Sex: No predilection results improve among some patients who
also receive hyperbaric oxygen therapy. The
CLINICAL AND RADIOGRAPHIC use of bisphosphonates may be promising.
FEATURES
Some patients will manifest osteomyeli-
Occurring in youngsters, chronic diffuse tis elsewhere in the skeleton warranting a
osteomyelitis is a rare lesion with features bone scan.
PMPH_Eversole_Chapter-10.indd 523 1/20/2011 3:08:44 PM
524 Chapter 10
FIGURE 10-38
Diffuse sclerosing osteomyelitis with osseous expansion. Bone scan reveals activity in mandible.
OSTEITIS DEFORMANS
Additional Reading (PAGET’S DISEASE OF BONE)
Jacobsson S. Diffuse sclerosing ostemyelitis of the man- Figure 10-39
dible. Acta Otolaryngol Suppl. 1979;360:61-63.
Schneider LC, Mesa ML. Differences between flor- Age: Elderly adults
id osseous dysplasia and chronic diffuse scleros-
Sex: Male predilection
ing osteomyelitis. Oral Surg Oral Med Oral Pathol.
1990;70:308-312. CLINICAL AND RADIOGRAPHIC
Suei Y, Taguchi A, Tanimoto K. Radiographic evaluation FEATURES
of possible etiology of diffuse sclerosing osteomyelitis
of the mandible. Oral Surg Oral Med Oral Pathol Oral Osteitis deformans is a dysplastic bone
Radiol Endod. 1997;84:571-577. disease that classically occurs in elderly
Van Merkesteyn JP, Bakker DJ, Van der Waal I, et people and involves replacement of normal
al. Hyperbaric oxygen treatment of chronic osteo-
myelitis of the jaws. Int J Oral Surg. 1984;13:386- bone by an irregular osseous growth, with
395. an increase in osteoblastic activity. The
Yamazaki Y, Satoh C, Ishikawa M, Notani K, Nomura K, molecular underpinnings involve muta-
Kitagawa Y. Remarkable response of juvenile diffuse tions of the sequestosome gene and the
sclerosing osteomyelitis of mandible to pamidronate.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. tumor necrosis family gene TNFRSF11A
2007;104:67-71. (osteoprotegrin). The long bones, pelvis,
PMPH_Eversole_Chapter-10.indd 524 1/20/2011 3:08:44 PM
Radiopaque Lesions of the Jaws 525
FIGURE 10-39
Ground-glass opacification
of alveolar bone. Osteitis
circumscripta in skull.
and cranium are predilected sites that show MICROSCOPIC FEATURES
expansion and deformity. As skull lesions A fibro-osseous microscopic pattern is
develop, foramina become constricted, seen in the early stages of osteitis defor-
leading to cranial nerve neuropathies such mans; a hypercellular fibrous stroma sup-
as blindness, deafness, and facial palsy. ports irregular osteoid trabeculae rimmed
Skull lesions begin in early stages as focal by osteoblasts on one side with resorbing
radiolucencies, so-called osteitis circum- osteoclasts on the opposite side. Vascularity
scripta. Later, the cranium enlarges with is prominent, and osteoclastic giant cells are
fuzzy radiopaque conglomerates, produc- often encountered in fibrous areas removed
ing the classic cotton-wool pattern. In the from any osseous trabeculae. Mosaic bone
jaws, the maxilla is involved more often is usually encountered even in the early
than the mandible, and the early stages stages, yet is far more prevalent in lesions of
show a uniform ground-glass appearance long standing.
with faint, poorly demarcated periapical
clearing (ill-defined radiolucencies). The
DIFFERENTIAL DIAGNOSIS
teeth remain vital. The cotton-wool pat-
tern eventually replaces the ground-glass A uniform bilateral maxillary ground-glass
appearance, and teeth may develop hyper- pattern with expansion and periapical clear-
cementosis. The maxillary lesions cross ing in an elderly patient is nearly diagnostic
the midline to involve both quadrants and for Paget’s disease. Alkaline phosphatase,
clinically manifest progressive expan- calcium, and phosphorus levels should be
sion, which in turn leads to diastema for- obtained; bone biopsy is recommended.
mation in dentulous patients. Giant cell Alkaline phosphate is characteristically
tumors similar to giant cell granuloma are elevated, whereas calcium and phosphorus
occasionally encountered in patients with levels are within normal limits. Although
Paget’s disease, appearing as expansile fibrous dysplasia and hyperparathyroidism
multilocular radiolucencies. Osteomyelitis may show similar radiographic features,
and an increased risk for development of the former is seen in young persons and
sarcomas in bone are complications. is restricted to one quadrant, and the latter
PMPH_Eversole_Chapter-10.indd 525 1/20/2011 3:09:06 PM
526 Chapter 10
fails to expand bone and is characterized by a decreased level of phosphorus. Elevated
an elevated serum calcium level. calcium leads to precipitation of mineral
in tissues (metastatic calcification), par-
TREATMENT ticularly in the bladder; this action leads to
Calcitonin is effective only temporarily, yet nephrocalcinosis and urolithiasis. Elevated
intravenous administration of biphospho- calcium levels also cause muscular weak-
nates has shown promise. Patients develop- ness and lethargy. Mobilization of calcium
ing periapical inflammation or requiring from bone results in osteitis fibrosa cystica, a
tooth extraction should receive antibiotics generalized demineralization; subperiosteal
because widespread osteomyelitis, which is resorption in the middle phalanges is a char-
difficult to control, is a complication. acteristic finding. When the jaw is involved,
multilocular radiolucencies representing
giant cell brown tumors may be seen, or a
Additional Reading diffuse ground-glass nonexpansile pattern
may be encountered. The lamina dura is
Brady FA, Roser SM, Sapp JP. Osteomyelitis of the missing, and the teeth become mobile. The
mandible as a complicating factor in Paget’s disease of same changes can be seen in secondary
bone. Br J Oral Maxillofac Surg. 1979;17:33.
Mankin HJ, Hornicek FJ. Paget’s sarcoma: a histori- hyperparathyroidism, which evolves sub-
cal and outcome review. Clin Orthop Relat Res. sequent to renal insufficiency and in which
2005;438:97-102. excessive urinary loss of calcium evokes a
Morgan GA, Morgan PR. Oral and skull manifestations compensatory parathyroid hyperplasia.
of Paget’s disease. J Can Dent Assoc. 1969;35:208.
Som PM, Hermann G, Sacher M, Stollman AL, A rare subset of patients with second-
Moscatello AL, Biller HF. Paget disease of the calva- ary renal hyperparathyroidism develop
ria and facial bones with an osteosarcoma of the max- massive facial bone and calvarial enlarge-
illa: CT and MR findings. J Comput Assist Tomogr. ment deformities designated in the past as
1987;11:887-890.
Tillman HH. Paget’s disease of bone: a clinical, radiologi-
leontiasis ossea, and more recently as big head
cal, and histomorphological study of twenty-four cases disease, uglyfying face syndrome, or Sagliker
involving the jaws. Oral Surg Oral Med Oral Pathol. syndrome. Also, as mentioned previously in
1962;15:1225. this chapter, familial hyperparathyroidism
Whyte MP. Paget’s disease of bone and genetic disorders
of RANKL/OPG/RANK/NF-kappaB signaling. Ann
may have jaw area ossifying fibromas as an
NY Acad Sci. 2006;1068:143-164. accompaniment.
MICROSCOPIC FEATURES
HYPERPARATHYROIDISM A fibro-osseous pattern prevails in the
Figure 10-40 ground-glass lesion whereby fibrous stroma
replaces normal bone and is stippled with
Age: Middle-aged adults irregular osseous trabeculae showing exces-
Sex: Female predilection sive osteoclastic activity.
CLINICAL AND RADIOGRAPHIC
FEATURES DIFFERENTIAL DIAGNOSIS
The jaw manifestations of hyperparathyroid- Although the ground-glass pattern of
ism are rare and, when present, are encoun- hyperparathyroidism may be similar to
tered only late in the course of the disease. that seen in fibrous dysplasia and osteitis
The result of an adenoma of the parathyroid deformans, expansion is lacking. The loss
gland with increased output of parathor- of lamina dura in conjunction with the
mone, the characteristic laboratory finding ground-glass appearance in an isolated jaw
is an elevation in serum calcium levels with quadrant occasionally is seen in metastatic
PMPH_Eversole_Chapter-10.indd 526 1/20/2011 3:09:09 PM
Radiopaque Lesions of the Jaws 527
FIGURE 10-40
Secondary renal hyper-
parathyroidism with loss
of lamina dura.
carcinoma or even primary sarcomas of the ease, the ground-glass pattern in the jaws
jaws. A bone chemistry profile, including may persist.
calcium, phosphorus, and alkaline phos-
phatase levels, should be obtained, even
when clinical symptomatology (urolithia-
sis, muscular weakness) points to a diagno-
Additional Reading
sis of hyperparathyroidism. Fletcher PD, Scopp IW, Hersh RA. Oral manifestations
of secondary hyperparathyroidism related to long-
term hemodialysis therapy. Oral Surg Oral Med Oral
TREATMENT Pathol. 1977;43:218.
Once it has been determined that the cause Petti GH Jr. Hyperparathyroidism. Otolaryngol Clin
North Am. 1990;23:339.
for the ground-glass lesion is hyperparathy- Sagliker Y, Balal M, Ozkaynak P, et al. Sagliker syn-
roidism (usually by an elevated serum cal- drome: uglifying human face appearance in late and
cium level), the patient should be referred severe secondary hyperparathyroidism in chronic renal
to an internist to determine whether a pri- failure. Semin Nephrol. 2004;24:449-455.
Silverman S Jr, Gordan G, Grant T, Steinbach H,
mary neoplasm or renal disease is caus- Eisenberg E, Manson R. The dental structures in pri-
ative. Parathyroid adenomas are treated mary hyperparathyroidism. Oral Surg Oral Med Oral
surgically. Even after elimination of the dis- Pathol. 1962;15:425.
PMPH_Eversole_Chapter-10.indd 527 1/20/2011 3:09:09 PM
528 Chapter 10
Silverman S Jr, Ware WH, Gillooly C. Dental aspects be particularly noticeable. Radiographically,
of hyperparathyroidism. Oral Surg Oral Med Oral the area of alveolar enlargement shows a
Pathol. 1968;26:184.
Walsh RF, Karmiol M. Oral roentgenographic findings somewhat ground-glass appearance that is
in osteitis fibrosa generalisata associated with chron- vertically streaked yielding a “falling rain
ic renal disease. Oral Surg Oral Med Oral Pathol. or sleet” pattern. One or both premolar
1969;28:273. teeth are missing and retained deciduous
teeth are morphologically anomalous.
SEGMENTAL MICROSCOPIC FEATURES
ODONTOMAXILLARY Pathologic changes in the affected maxillary
DYSPLASIA bone are characterized by osteocytic hyper-
Figure 10-41 plasia (increased number of intralacunar
osteocytes per unit area of bone), lacunar
Age: Teens, adults enlargement, and sheet-like arrangements
Sex: No predilection of woven bone. Osteoblastic and osteoclas-
CLINICAL AND RADIOGRAPHIC tic activities appear decreased. The fibrous
FEATURES marrow element is hypocellular, mature, or
This anomaly is sporadic and is first noted myxoid. Affected teeth show variability in
during teenage years when routine dental dentinal tubule diameter.
or orthodontic radiographs are procured
or when facial asymmetry becomes appar- DIFFERENTIAL DIAGNOSIS
ent. Unilateral asymmetry with maxillary Fibrous dysplasia may be a consideration yet
enlargement is usually mild and may not does not show anomalous or missing teeth.
FIGURE 10-41
Segmental odontomaxil-
lary dysplasia showing
missing teeth and verti-
cal sleet-like osseous
changes.
PMPH_Eversole_Chapter-10.indd 528 1/20/2011 3:09:12 PM
Radiopaque Lesions of the Jaws 529
TREATMENT cell/bone interface. Unchecked osteoblas-
No treatment is necessary. Any unerupted tic activity leads to excessive osteogenesis.
teeth in the area of lesional bone should be Radiographically, trabeculation is obscured
extracted. If maxillary enlargement is a cos- by an extremely dense opacification of med-
metic concern, surgical contouring may be ullary bone. The bone may appear so dense
undertaken. that dental root morphology is obscured.
Excessive endosteal bone formation results
in a myelophthisic anemia and pancytope-
Additional Reading nia. Neural compression accounts for neu-
rologic sensory and motor function deficits,
Armstrong C, Napier SS, Boyd RC, Gregg TA. and the long bones become brittle and are
Histopathology of the teeth in segmental odontomax-
illary dysplasia: new findings. J Oral Pathol Med. subject to fracture. Hepatosplenomegaly
2004;33:246-248. with extramedullary hematopoiesis, hydro-
Becktor KB, Reibel J, Vedel B, Kjaer I. Segmental odon- cephalus, and mental retardation may be
tomaxillary dysplasia: clinical, radiological and histolog- encountered.
ical aspects of four cases. Oral Dis. 2002;8:106-110.
Bhatia SK, Drage N, Cronin AJ, Hunter ML. Case report:
segmental odontomaxillary dysplasia—a rare disorder. MICROSCOPIC FEATURES
Eur Arch Paediatr Dent. 2008;9:245-248. Medullary bone resembles cortex with thick
Danforth RA, Melrose RJ, Abrams AM, Handlers JP.
Segmental odontomaxillary dysplasia. Report of eight anastomosing lamellar trabeculae obliterat-
cases and comparison with hemimaxillofacial dyspla- ing soft tissue marrow.
sia. Oral Surg Oral Med Oral Pathol. 1990;70:81-85.
Koenig LJ, Lynch DP, Yancey KB. Segmental odon- DIFFERENTIAL DIAGNOSIS
tomaxillary dysplasia presenting with facial hyper-
trichosis, commissural lip clefting, and hyperlinear The other entities included as ground-
palms. Pediatr Dermatol. 2008;25:491-492. glass opacities are finely granular and
should not be confused radiographically
with osteopetrosis, which is strikingly
OSTEOPETROSIS radiodense. Familial historic genetic map-
Figure 10-42 ping may uncover affected relatives of the
propositus.
Age: Childhood onset
Sex: No predilection
TREATMENT
CLINICAL AND RADIOGRAPHIC
There is no effective treatment. Periapical
FEATURES
infections may progress to severe osteomy-
Osteopetrosis, also known as marble bone elitis. Dental sepsis and extraction of teeth
disease or Albers-Schönberg disease, is in affected individuals should be treated in
inherited as an autosomal dominant trait conjunction with antibiotic therapy.
(benign form) or as an autosomal reces-
sive trait (malignant form). The former may
develop later in life; the severe recessive Additional Reading
form is present from birth, and life expec-
Gomez LSA, et al. The jaws in osteopetrosis (Albers-
tancy rarely exceeds 20 years. The disease Schönberg disease): report of case. J Oral Maxillofac
is apparently the result of defective osteo- Surg. 1966;24:67.
clastic activity, engendered by mutations Nitzan DW, Marmary Y. Osteomyelitis of the mandible
in numerous genes (CA-II, TCIRG1, ClCN7, in a patient with osteopetrosis. J Oral Maxillofac Surg.
1982;40:377.
OSTM1, and PLEKHM1) that are all involved Smith NH. Albers-Schönberg disease (osteopetrosis):
in the effector function of mature osteo- report of case and review of the literature. Oral Surg
clasts, being linked to acidification of the Oral Med Oral Pathol. 1966;22:699.
PMPH_Eversole_Chapter-10.indd 529 1/20/2011 3:09:15 PM
530 Chapter 10
FIGURE 10-42
Osteopetrosis. Teeth are
obscured by opacification.
Villa A, Guerrini MM, Cassani B, Pangrazio A, Sobacchi C. that is uniformly symmetric. Osteoblas-
Infantile malignant, autosomal recessive osteopetrosis: tic hyperactivity prevails, with resultant
the rich and the poor. Calcif Tissue Int. 2009;84:1-12.
Younai F, Eisenbud L, Sciubba JJ. Osteopetrosis: a case excess secretion of osteoblastic alkaline
report including gross and microscopic findings in the phosphatase. The enzyme may be detected
mandible at autopsy. Oral Surg Oral Med Oral Pathol. in elevated serum levels often approaching
1988;65:214. 10-fold elevations over normal amounts. As
the craniofacial bones expand, the skull and
upper face enlarge, with resulting increase
Multifocal Confluent in hat size, inability to wear dentures, or, if
(Cotton-Wool) the patient is dentulous, diastema forma-
tion. Bone enlargement in the area of neu-
Radiopacities ral foramina results in bizarre nerve deficits
such as hearing loss, blindness, and facial
OSTEITIS DEFORMANS palsy. The early stages appear as ground-
(PAGET’S DISEASE OF BONE) glass radiopacities; as the disease progresses,
Figure 10-43 osteoblastic activity prevails, with the
appearance of multifocal radiopacities in the
Age: Elderly adults maxilla, yielding a cotton-wool pattern. The
Sex: Male predilection process is generalized throughout the max-
CLINICAL AND RADIOGRAPHIC illa and calvarium, and is bilateral. Hyperce-
FEATURES mentosis is a common finding. The jaws are
Osteitis deformans is a dysplastic bone dis- susceptible to odontogenic infection; there-
ease of older people that is more severe in fore, widespread osteomyelitis may develop.
females than in males, yet affects males Patients with Paget’s disease are at risk for
more frequently than females. The molecu- malignant transformation to osteogenic sar-
lar underpinnings involve mutations in the coma or fibrosarcoma central in bone.
sequestosome gene and the tumor necrosis
MICROSCOPIC FEATURES
family gene TNFRSF11A (osteoprotegrin).
It is polyostotic; when the long bones and A fibro-osseous pattern predominates with
spine are severely involved, deformity and irregular osseous trabeculae implanted in a
crippling results. The skull and maxilla are hypercellular vascular marrow. Concomitant
rarely spared, with expansile overgrowth osteoblastic and osteoclastic rimming trabe-
PMPH_Eversole_Chapter-10.indd 530 1/20/2011 3:09:15 PM
Radiopaque Lesions of the Jaws 531
FIGURE 10-43
Osteitis deformans with
ground-glass and confluent
dense ossifications.
culae is a dominant feature. Large dense and abscess occurs, necessitating extraction, anti-
compact trabeculae are riddled with baso- biotic coverage should be provided to cir-
philic resting and reversal lines, producing cumvent the complication of osteomyelitis.
a jigsaw-puzzle arrangement. Occasionally, Follow-up both clinically and radiographi-
giant cell lesions accompany Paget’s disease. cally for sarcomatous change is indicated.
DIFFERENTIAL DIAGNOSIS
The cotton-wool, multifocal radiodense Additional Reading
conglomerates seen in osteitis deformans
Feig HI, Edmunds WR, Beaubien R, Finkelman AA.
may also be encountered in florid cemen- Chronic osteomyelitis of the maxilla secondary to
to-osseous dysplasia and Gardner’s syn- Paget’s disease: a complication following dental extrac-
drome. The osseous lesions are restricted tion. Report of a case. Oral Surg Oral Med Oral Pathol.
to the maxillofacial complex in these dis- 1969;28:320-325.
Peris P, Alvarez L, Vidal S, et al. Biochemical response to
orders, whereas in Paget’s disease of bone, bisphosphonate therapy in pagetic patients with skull
the skull, long bones, and vertebrae are also involvement. Calcif Tissue Int. 2006;79:22-26.
usually involved. The jaw lesions of Paget’s Rosenmertz SK, Schare HJ. Osteogenic sarcoma aris-
are usually maxillary with only occasional ing in Paget’s disease of the mandible. Oral Surg Oral
Med Oral Pathol. 1968;28:304.
involvement of the mandible, as opposed to Stafne EC, Austin LR. A study of dental roentgeno-
florid cemento-osseous dysplasia, which is grams in cases of Paget’s disease (osteitis deformans),
more common in the mandible. The pres- osteitis fibrosa cystica and osteoma. J Am Dent Assoc.
ence of supernumerary teeth and other fea- 1938;25:1210.
tures of Gardner’s syndrome are unique,
allowing for differentiation on a clinicora-
diologic basis. Alkaline phosphatase level FLORID OSSEOUS DYSPLASIA
elevations are a feature of Paget’s disease; Figure 10-44
these values are not significantly elevated
Age: Middle-aged adults
in other diseases considered in the differen-
Sex: Female predilection
tial diagnosis. In addition, the mosaic bone
pattern observed microscopically is not fea- CLINICAL AND RADIOGRAPHIC
tured in other diseases. FEATURES
Florid cemento-osseous dysplasia occurs
TREATMENT
predominantly in middle-aged black
Osteitis deformans is managed by admin- women and has been postulated to repre-
istration of bisphophonates. When dental sent a low-grade inflammatory lesion of
PMPH_Eversole_Chapter-10.indd 531 1/20/2011 3:09:16 PM
532 Chapter 10
the jaws, resulting from pulpal or periapi- acute osteomyelitis with bony sequestration
cal infection; hence the term diffuse scleros- and fistula formation.
ing osteomyelitis. Alternatively, an infectious
source is usually not identifiable. For this MICROSCOPIC FEATURES
reason, the condition has been suggested to
A fibro-osseous histologic pattern prevails
represent a dysplastic process of periodon-
in areas devoid of acute inflammation. A
tal ligament (cementoblastic) origin com-
hypercellular fibrous stroma supports cur-
mon in black females. Nevertheless, it is
vilinear trabeculae that show the polariza-
occasionally seen in members of other races.
tion microscopic features of cementum;
Radiographically, one or all four jaw quad-
however, some examples are composed pre-
rants can be affected, although there is a
dominantly of bone. Mononuclear inflam-
tendency to be limited to or more extensive
matory cells, if present at all, are sparse.
in the mandible. The jaws possess multiple
confluent radiopacities yielding a cotton-
DIFFERENTIAL DIAGNOSIS
wool pattern. More often than not, the jaws
are edentulous. Sequestrum formation with The cotton-wool radiographic appearance
a surface nodularity may be demonstrable, of florid osseous dysplasia is easily con-
but expansion of the cortices is lacking or fused with that of osteitis deformans. The
present to a limited degree. The alkaline former is primarily mandibular, extrag-
phosphatase level is usually within normal nathic osseous lesions are absent, and the
limits. The pathologic osseous tissue is sus- alkaline phosphatase level is normal; in
ceptible to infection, with development of Paget’s disease, the dysplastic osseous
FIGURE 10-44
Florid osseous dysplasia.
Lower panels show expan-
sion, an uncommon finding,
with lucent and opaque
foci.
PMPH_Eversole_Chapter-10.indd 532 1/20/2011 3:09:18 PM
Radiopaque Lesions of the Jaws 533
process is polyostotic, the alkaline phos- supernumerary teeth, desmoid (fibrous)
phatase level is elevated, and the maxil- tumors of skin, epidermal inclusion cysts,
lary quadrants are affected exclusively or and intestinal polyps with a predilection
more extensively than those of the man- for malignant transformation into adeno-
dible. Gardner’s syndrome must also be carcinomas. A mutation in the AP1 tumor
included in the differential diagnosis. The suppressor gene (adenomatous/polyposis)
cotton-wool osteomas of this syndrome are is the underlying molecular lesion. The
rarely limited to the jaws, the sinuses being intestinal polyps are limited to colorectal
a common site of localization. In addition, mucosa and can be detected on gastrointes-
the other manifestations of Gardner’s syn- tinal radiologic analysis and proctoscopic
drome are diagnostic. examination. The skin lesions are multiple
and appear as nodular, smooth-surfaced
TREATMENT lesions located primarily on the trunk and
No treatment is required. Should osteomy- back. The manifestations include multiple
elitis of an acute nature evolve, antibiotic supernumerary teeth and odontomas, most
therapy with surgical removal of sequestra of which are impacted. The osteomas are
and debridement is recommended. demonstrable on jaw, panographic, and
Water’s sinus radiographs as multiple dif-
fuse and confluent radiopacities that may
Additional Reading involve all four jaw quadrants. The antra
and frontal sinuses often contain simi-
Jacobsson S, Heyden G. Chronic sclerosing osteomyelitis lar irregular radiodensities. Because the
of the mandible: histologic and histochemical findings.
Oral Surg Oral Med Oral Pathol. 1977;43:357.
osteomas may reside both centrally and
Melrose RJ, Abrams AM, Mills BG. Florid osseous dys- in parosteal locations, clinically detectable
plasia. A clinical-pathologic study of thirty-four cases. indurated protuberances can be identified
Oral Surg Oral Med Oral Pathol. 1976;41:62. on palpation.
Schneider LC, Mesa ML. Differences between flor-
id osseous dysplasia and chronic diffuse scleros-
MICROSCOPIC FEATURES
ing osteomyelitis. Oral Surg Oral Med Oral Pathol.
1990;70:308. The osteomas are composed of dense
Sedano HO, Kuba R, Gorlin RJ. Autosomal dominant lamellar Haversian bone with scant fibrous
cemental dysplasia. Oral Surg Oral Med Oral Pathol.
1982;54:643. stroma.
Waldron CA, Giansanti JS, Browand BC. Sclerotic
cemental masses of the jaws (so-called chronic scleros- DIFFERENTIAL DIAGNOSIS
ing osteomyelitis, sclerosing osteitis, multiple enosto-
sis, and gigantiform cementoma). Oral Surg Oral Med The multifocal cotton-wool radiodensities
Oral Pathol. 1975;39:590. of Gardner’s syndrome are similar radio-
logically to the lesions encountered in Pag-
et’s disease and florid osseous dysplasia.
GARDNER’S SYNDROME A tendency for localization of osteomas in
Figure 10-45 the sinuses, the presence of supernumer-
ary teeth, and the other features of the syn-
Age: Young adults drome are sufficient to rule out these other
Sex: No predilection entities.
CLINICAL AND RADIOGRAPHIC
FEATURES TREATMENT
Inherited as an autosomal dominant trait, The osteomas may be removed if they inter-
Gardner’s syndrome is characterized by fere with function or present a cosmetic
multiple osteomas of the jaws and sinuses, problem. Supernumerary teeth and odon-
PMPH_Eversole_Chapter-10.indd 533 1/20/2011 3:09:23 PM
534 Chapter 10
FIGURE 10-45
Gardner’s syndrome. Multiple osteomas.
tomas should be removed. Patients should FAMILIAL GIGANTIFORM
be referred to a gastroenterologist because CEMENTOMA
intestinal adenocarcinoma is the most seri- Figure 10-46
ous aspect of this syndrome.
Age: Evolves during childhood
Additional Reading Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Gardner EJ. Follow-up study of a family group exhibiting FEATURES
dominant inheritance for a syndrome including intesti-
nal polyposis, osteomas, fibromas, and epidermal cysts. The familial gigantiform cementoma is a
Am J Hum Genet. 1962;14:376. rare disease in which only a few family
Gorlin RJ, Chaudhry AP. Multiple osteomatosis, fibro-
mas and fibrosarcomas of the skin and mesentery,
pedigrees have been reported. Clinically,
epidermoid inclusion cysts of the skin, leiomyomas painless expansion of the jaws occurs.
and multiple intestinal polyposis. N Engl J Med. Although a single lesion may appear ini-
1969;236:1151. tially, multiple sites eventually become
Half E, Bercovich D, Rozen P. Familial adenomatous
evident either clinically or radiographi-
polyposis. Orphanet J Rare Dis. 2009;4:22.
Ida M, Nakamura T, Utsunomiya J. Osteomatous cally. Although both upper and lower jaws
changes and tooth abnormalities found in the jaws of may be involved, bilaterality is common
patients with adenomatosis coli. Oral Surg Oral Med as well. The radiographs disclose large,
Oral Pathol. 1981;52:2. sometimes huge, expansile lesions that
Kubo K, Miyatani H, Takenoshita Y, et al. Widespread
radiopacity of jaw bones in familial adenomatosis coli. are generally fairly well delineated. The
J Craniomaxillofac Surg. 1989;17:350-353. lesions are mixed radiolucent/radiopaque
PMPH_Eversole_Chapter-10.indd 534 1/20/2011 3:09:23 PM
Radiopaque Lesions of the Jaws 535
FIGURE 10-46
Gigantiform cementoma.
Multifocal massive lesions
with marked facial defor-
mity. Courtesy of Dr.
Samir ElMofty.
yet become more dense with ensuing fluent opacities of both jaws, only familial
years, and confluent opacities superim- gigantiform cementoma has the potential for
posed over dental roots may progress from massive enlargement with a hereditary dis-
one molar around to the next. The disease position. Paget’s disease may show similar
appears to be inherited as an autosomal features, yet does not begin at an early age.
dominant trait with considerable variabil-
ity of expressivity, particularly with regard TREATMENT
to the number and size of lesions. There
The lesions are often huge and disfiguring
are other instances of large, expansile ossi-
requiring surgical intervention. Although
fying fibromas that involve more than one
recurrence may be anticipated in younger
quadrant in which no familial tendency
patients, once they reach adult life, surgical
has been documented.
osseous recontouring, although not abla-
tive, is usually successful; lesional tissue
MICROSCOPIC FEATURES may persist, yet the potential for recurrent
Typical fibro-osseous histologic character- growth is often limited or nonexistent.
istics are observed whereby the stroma is
collagenous and somewhat cellular with
monomorphic appearing fibroblasts. Irreg- Additional Reading
ular and haphazardly arranged osseous
Abdelsayed RA, Eversole LR, Singh BS, Scarbrough FE.
trabeculae are present and may form into
Gigantiform cementoma: clinicopathologic presenta-
confluent sclerotic masses. Small ovoid cal- tion of 3 cases. Oral Surg Oral Med Oral Pathol Oral
cifications are also common. Radiol Endod. 2001;91:438-444.
Agazzi C, Belloni L. Gli odontomi duri dei mascellari
contributo clinco-rontgenologico e antomo-micro-
DIFFERENTIAL DIAGNOSIS scopico con particolare riguardo alle formle ad ampia
Familial gigantiform cementoma has been estensione e alla comparsa familiare. Arch Ital Otol.
1953;64(suppl. 16):3.
erroneously confused with florid osseous Norberg O. Zur kenntnis der dysontogenetischen
dysplasia. Although both manifest radio- geshwulste der kieferknochen. Vkrtljsschr Zahn.
graphically demonstrable diffuse and con- 1930;46:321.
PMPH_Eversole_Chapter-10.indd 535 1/20/2011 3:09:27 PM
536 Chapter 10
Yih WY, Pederson GT, Bartley MH. Multiple familial ossi- microbial source. A soft tissue or parotid
fying fibromas: relationship to other osseous lesions of abscess overlying periosteum may also stim-
the jaws. Oral Surg Oral Med Oral Pathol. 1989;68:754.
Young SK, Markowitz NR, Sullivan S, Seale TW, Hirschi ulate periosteal osteogenesis. As new bone is
R. Familial gigantiform cementoma: classification and formed, expansion becomes evident; radio-
presentation of a large pedigree. Oral Surg Oral Med graphically, a redundant cortical layering
Oral Pathol. 1989;68:740-747. phenomenon is usually but not invariably
encountered. A constant radiographic feature
Cortical Redundancies is preservation of the normal boundary of the
cortex subjacent to the expanded region. The
(Onion-Skin Patterns) disease is essentially confined to the mandib-
ular body when the jaws are affected. Tooth-
GARRÉ’S PERIOSTITIS ache or dull bone pain may cause the patient
Figure 10-47 to seek dental consultation.
Age: Children and teenagers MICROSCOPIC FEATURES
Sex: No predilection
A fibro-osseous histologic pattern prevails,
CLINICAL AND RADIOGRAPHIC with a cellular fibroblastic stroma interposed
FEATURES between irregular or parallel trabeculae of
Garré’s periostitis represents a reactive woven or lamellar bone. Scattered mononu-
periosteal proliferative inflammatory res- clear inflammatory cells are often observed.
ponse to infection or trauma. In the jaws,
DIFFERENTIAL DIAGNOSIS
proliferative periostitis is typically associated
with chronic diffuse sclerosing osteomyeli- The cortical layering with expansion seen
tis and may or may not have an odontogenic in Garré’s periostitis is also encountered
FIGURE 10-47
Diffuse sclerosing osteo-
myelitis with periosteal
onion skinning (Garré’s).
PMPH_Eversole_Chapter-10.indd 536 1/20/2011 3:09:32 PM
Radiopaque Lesions of the Jaws 537
in Caffey’s disease and Ewing’s sarcoma. Silverman disease begins before 6 months
Because Garré’s periostitis is an inflamma- of age as a polyostotic cortical hyperosto-
tory disorder, an infectious source, usually sis. The thickened cortices reflect exagger-
a carious molar tooth with a periapical radi- ated periosteal osteogenesis, which has been
olucency, can be identified. Caffey’s disease suggested to evolve subsequent to tissue
is seen in infants, is bilateral, and involves hypoxia resulting from genetically defective
numerous bones of the appendicular skel- periosteal vessels. It has been proposed that
eton. A biopsy is recommended to rule out all infants exhibit an accelerated appositional
Ewing’s sarcoma. bone growth spurt, and periosteal redun-
dancy is merely an exaggerated form of this
TREATMENT growth phase, which is radiographically
The periosteal proliferative response bec- demonstrable in some infants. Clinically,
omes arrested and remodels to normal con- the overlying soft tissues are tender, warm,
tour once the infectious process responsible and swollen. The swellings are bilateral and
for its genesis has been eliminated. are particularly obvious about the mandible.
Fever and leukocytosis are generally appar-
ent. Radiographically, the body and ramus
Additional Reading manifest expansion with onion-skin cortical
redundancy. Within a few months, the gen-
Ebihara A, Yoshioka T, Suda H. Garrè’s osteomyelitis eralized condition resolves spontaneously.
managed by root canal treatment of a mandibular sec-
ond molar: incorporation of computed tomography
MICROSCOPIC FEATURES
with 3D reconstruction in the diagnosis and monitor-
ing of the disease. Int Endod J. 2005;38:255-261. The microscopic features of the osseous
Eisenbud L, Miller J, Roberts IL. Garré’s proliferative
lesions have not been well delineated.
periostitis occurring simultaneously in four quad-
rants of the jaws. Oral Surg Oral Med Oral Pathol.
1981;51:172.
Eversole LR, Leider AS, Corwin JO, Karian BK.
Proliferative periostitis of Garré: its differentiation
from other neoperiostoses. J Oral Maxillofac Surg.
1979;37:725-731.
Nortje CJ, Wood RE, Grotepass F. Periostitis ossificans
versus Garré’s osteomyelitis. Part II. Radiologic analy-
sis of 93 cases in the jaws. Oral Surg Oral Med Oral
Pathol. 1988;66:249.
Pell GJ, Shafer WG, Gregery GT, Ping RS, Spear LB.
Garré’s osteomyelitis of the mandible. J Oral Maxillofac
Surg. 1955;13:248.
INFANTILE CORTICAL
HYPEROSTOSIS
Figure 10-48
Age: Infants
Sex: No predilection
CLINICAL AND RADIOGRAPHIC
FEATURES
FIGURE 10-48
Inherited as an autosomal dominant trait, Infantile cortical hyperostosis with periosteal neo-
infantile cortical hyperostosis or Caffey- osteogenesis.
PMPH_Eversole_Chapter-10.indd 537 1/20/2011 3:09:44 PM
538 Chapter 10
DIFFERENTIAL DIAGNOSIS dible. The hyperostotic changes become evi-
The polyostotic symmetric distribution of dent during the second decade of life. The
cortical redundancies of infancy permit dif- jaw is squared and enlarged. Thickening
ferentiation from other diseases manifesting of the cranial base may eventually lead to
similar radiographic features. Familial fibrous foramina narrowing with attending neuro-
dysplasia or cherubism shows bilateral man- logic deficits, including facial paralysis, optic
dibular expansion. Cortical redundancy atrophy, and hearing loss. Serum alkaline
is not a feature, however; the jaw lesions of phosphatase levels are elevated. Radiograph-
cherubism are multilocular and expansile. ically, the cortices show a two or threefold
thickening. Sclerostosis is a variant form that
TREATMENT favors the calvaria, mandible, and clavicles
along with syndactyly. Typical facies are
No treatment is necessary because the dis- observed in infancy and include a long face
ease spontaneously regresses. Despite this with high forehead, hypertelorism, enlarged
fact, some residual jaw deformity may pre- head, and mandibular prognathism.
dispose to malocclusion.
MICROSCOPIC FEATURES
Additional Reading Grossly, the cortices are thickened with
irregular grooving and osteophyte forma-
Burbank PM, Lovestedt SA, Kennedy RLJ. The dental
tion. The cortical Haversian bone is thick-
aspects of infantile cortical hyperostosis. Oral Surg
Oral Med Oral Pathol. 1958;11:1126. ened yet histologically unremarkable.
Ditkowsky SP, Goldman A, Barnett H, Baker M,
Sammett J. Normal periosteal reactions and associated DIFFERENTIAL DIAGNOSIS
soft tissue findings. Relationship to infantile colic and
to the Caffey syndrome. Clin Pediatr. 1970;9:515-524. Sclerostosis and Van Buchem’s disease are
Holman GH. Infantile cortical hyperostosis: a review. Q similar, but they can be differentiated on
Rev Pediatr. 1962;17:24. the basis of the digital anomalies observed
Kamoun-Goldrat A, le Merrer M. Infantile cortical hyper-
ostosis (Caffey disease): a review. J Oral Maxillofac
in sclerostosis. Osteopetrosis may manifest
Surg. 2008;66:2145-2150. similar changes, yet the entire medullary
Shopfer CE. Periosteal bone growth in normal infants; bone is hyperostotic and yields a diffuse,
preliminary report. AJR Am J Roenigenol. 1966;97:154. rather than strictly cortical, opacification.
TREATMENT
GENERALIZED CORTICAL
HYPEROSTOSIS There is no effective treatment. Cosmetic
surgery of the mandible has been under-
Figure 10-49
taken successfully.
Age: Childhood onset
Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Additional Reading
FEATURES Cook JV, Phelps PD, Chandy J. Van Buchem’s dis-
ease with classical radiological features and appear-
Generalized cortical hyperostosis or Van ances on cranial computed tomography. Br J Radiol.
Buchem’s disease is inherited as an auto- 1989;62:74.
somal recessive trait that maps to chromo- Fosmoe RJ, Holm RS, Hildreth RC. Van Buchem’s dis-
some 17q12-q21. The disease is characterized ease. Radiology. 1968;90:771-774.
Van Buchem FSP, Hadders HN, Ubbens R. An uncom-
by generalized thickening of the cortical mon familial systemic disease of the skeleton: hyper-
table throughout the skeleton, primarily the ostosis corticalis generalisata familaris. Acta Radiol.
tubular bones, the calvaria, and the man- 1955;44:109-120.
PMPH_Eversole_Chapter-10.indd 538 1/20/2011 3:09:47 PM
Radiopaque Lesions of the Jaws 539
FIGURE 10-49
Sclerostosis is
bilateral.
Van Buchem FS, Hadders HN, Hansen JF, Woldring appearance is usually not apparent; instead,
MG. Hyperostosis corticalis generalisata. Report of an irregular opacification is observed, and
seven cases. Am J Med. 1962;33:387-397.
Van Hul W, Balemans W, Van Hul E, et al. Van radially protruding osteophytic spicules
Buchem disease (hyperostosis corticalis generalisata) can be identified. Cortical invasion with
maps to chromosome 17q12-q21. Am J Hum Genet. erosion may be featured. Occasionally, the
1998;62:391-399. periosteal new growth is clearly demar-
cated from cortex by an interposed radio-
lucent band. Such lesions are referred to as
JUXTACORTICAL periosteal osteogenic sarcoma.
OSTEOGENIC SARCOMA
Figure 10-50 MICROSCOPIC FEATURES
Age: Adults Most of these neoplasms are well differen-
Sex: Male predilection tiated; others are anaplastic. Pleomorphic
osteoblasts and a hypercellular stroma are
CLINICAL AND RADIOGRAPHIC
FEATURES
observed with formation of irregular trabe-
culae, which are also hypercellular. Chon-
Also termed parosteal osteogenic sarcoma, the droid foci are present in one half the cases.
juxtacortical neoplasm apparently arises
from periosteal osteoblasts, and elaboration DIFFERENTIAL DIAGNOSIS
of tumor bone is peripheral. The mandible
is affected more often than the maxilla, and Both proliferative periostitis and infantile
the prognosis of this type of osteogenic cortical hyperostosis show onion-skin pat-
sarcoma is much more favorable than that terns as opposed to irregular osteophytic
of its endosteal counterpart. Pain may be changes. Myositis ossificans and fascii-
featured; however, the most common com- tis ossificans should be considered in the
plaint is alveolar swelling with a history of radiographic diagnosis.
rapid growth. Radiographically, a mottled
TREATMENT
appearance of opacification is observed on
periapical films. Occlusal radiographs reveal Despite the peripheral orientation of the
the characteristic features. An onion-skin tumor, an en bloc resection of the underlying
PMPH_Eversole_Chapter-10.indd 539 1/20/2011 3:09:47 PM
540 Chapter 10
FIGURE 10-50
Osteogenic sarcoma, sun-
burst patter, and periosteal
reaction.
FIGURE 10-51
Osteoid osteoma over
cortex.
mandible or maxilla should be performed. Unni KK, Dahlin DC, Beabout JW, Ivins JC. Parosteal
Adjunctive chemotherapy should be con- osteogenic sarcoma. Cancer. 1976;37:2466-2475.
sidered for those lesions with invasion of
the endosteum. Anaplastic invasive tumors OSTEOID OSTEOMA
behave poorly, similar to those lesions aris-
Figure 10-51
ing centrally. Patients with well-differenti-
ated peripheral tumors have shown a 75% Age: Middle-aged adults
5-year survival. Sex: No predilection
CLINICAL AND RADIOGRAPHIC
Additional Reading FEATURES
Osteoid osteoma is a benign self-limited
Ahuja SC, Villacin AB, Smith J. Juxtacortical (parosteal)
osteogenic sarcoma: histologic grading and prognosis.
bone lesion that arises in the cortex. The
J Bone Joint Surg. 1977;59:632-647. lesion may be painful if compressed. It usu-
Bras JM, Donner R, van der Kwast WAM, Snow GB, ally presents with a faint central radiolucency
van der Waal I. Juxtacortical osteogenic sarcoma of within a round radiopaque structure that is
the jaws. Review of the literature and report of a case.
generally around 1 cm in diameter. An outer
Oral Surg Oral Med Oral Pathol. 1980;50:535-544.
Hewitt KM, Ellis G, Wiggins R, Bentz BG. Parosteal lucent halo yields a target appearance.
osteosarcoma: case report and review of the literature.
Head Neck. 2008;30:122-126. MICROSCOPIC FEATURES
Millar BG, Browne RM, Flood TR. Juxtacortical oste-
osarcoma of the jaws. Br J Oral Maxillofac Surg. A central nidus of formative osteoid is
1990;28:73. encountered with a fibro-osseous appear-
PMPH_Eversole_Chapter-10.indd 540 1/20/2011 3:09:52 PM
Radiopaque Lesions of the Jaws 541
ance. The bone external to the nidus is more visible radiographically as multiple, usu-
mature and lamellar with prominent osteo- ally bilateral, ovoid radiodensities superim-
blastic rimming, becoming accentuated posed over the premolar and molar roots.
radially at the periphery. These lesions are quite common, occurring
in nearly 8% of the population, and have
DIFFERENTIAL DIAGNOSIS a familial tendency. They may continue to
Differentiation from cementoblastoma is grow slowly with advancing years.
based on the fact that osteoid osteoma is
MICROSCOPIC FEATURES
located on the cortex and not in continu-
ity with tooth roots as is cementoblastoma. The osseous nodules are composed of a
Within the nidus, the lesion shows histo- thickened outer cortical plate of Haversian
logic similarities to the aggressive tumor bone. Medullary trabeculae extend inter-
benign osteoblastoma. nally and are admixed with an intervening
fibroadipose marrow.
TREATMENT
DIFFERENTIAL DIAGNOSIS
Surgical excision is the preferred treatment.
Exostoses and mandibular tori may radio-
graphically simulate the jaw lesions of
Additional Reading osteitis deformans, osteomyelitis, and
Gupta OP, Jain RK, Agarwal MK, Khanna S, Shrivastava
Gardner’s syndrome. Tori and exostoses,
A. Osteoid osteoma of the mandible. Ear Nose Throat as opposed to these other diseases, mani-
J. 1985;64:206-208. fest radiopacities located near the crest of
Matsuzaka K, Shimono M, Uchiyama T, Noma H, Inoue the alveolus without extension below root
T. Lesions related to the formation of bone, cartilage
apices. When the radiographic findings
or cementum arising in the oral area: a statistical study
and review of the literature. Bull Tokyo Dent Coll. are compared with the clinical features, a
2002;43:173-180. definitive diagnosis is easily rendered.
Rahsepar B, Nikgoo A, Fatemitabar SA. Osteoid osteoma
of subcondylar region: case report and review of the TREATMENT
literature. J Oral Maxillofac Surg. 2009;67:888-893.
van der Waal I, Greebe RB, Elias EA. Benign osteoblas- No treatment is required unless the
toma or osteoid osteoma of the maxilla. Report of a bony nodules interfere with function or
case. Int J Oral Surg. 1983;12:355-358. placement of a prosthetic appliance. In
these instances, they may be removed
MANDIBULAR TORI AND surgically.
EXOSTOSES
Figure 10-52 Additional Reading
Age: Middle-aged adults Blakemore JR, Eller DJ, Tomaro AJ. Maxillary exostoses.
Sex: Female predilection Oral Surg Oral Med Oral Pathol. 1975;40:200.
Kolas S, Halperin V, Jefferis K, Huddleston S, Robinson
CLINICAL AND RADIOGRAPHIC HB. The occurrence of torus palatinus and torus man-
FEATURES dibularis in 2,478 dental patients. Oral Surg Oral Med
Oral Pathol. 1953;6:1134-1141.
Mandibular tori are bony excrescences Reichart PA, Neuhaus F, Sookasem M. Prevalence of
located in the premolar region on the lin- torus palatinus and torus mandibularis in Germans and
gual alveolus; exostoses are similar devel- Thai. Community Dent. Oral Epidemiol. 1988;16:61.
Sawair FA, Shayyab MH, Al-Rababah MA, Saku T.
opmental osseous nodules found at the Prevalence and clinical characteristics of tori and jaw
mucobuccal fold on the maxillary buccal exostoses in a teaching hospital in Jordan. Saudi Med J.
alveolar ridge. Both, if large enough, are 2009;30:1557-1562.
PMPH_Eversole_Chapter-10.indd 541 1/20/2011 3:10:08 PM
542 Chapter 10
FIGURE 10-52
Tori and exostoses superimposed over teeth.
Suzuki M, Sakai T. A familial study of torus palati- asymmetry heralds its presence. Radio-
nus and torus mandibularis. Am J Phys Anthropol. graphically, the tumor may manifest many
1960;18:263.
patterns, one of the predominant ones
being a mixed radiolucent-radiopaque
Irregular, Ill-Defined expansile lesion with irregular configura-
tion. The margins are poorly defined, and
Expansile Radiopacities osteophytic spicules may project outward,
yielding a sunray pattern. Most cases are
CALCIFYING EPITHELIAL associated with an impacted tooth, and the
ODONTOGENIC TUMOR body or ramus regions of the mandible are
Figure 10-53 favored sites.
Age: Middle-aged adults MICROSCOPIC FEATURES
Sex: No predilection
The neoplastic epithelial element exists in
CLINICAL AND RADIOGRAPHIC sheets or islands of eosinophilic or clear
FEATURES polygonal cells with vesicular nuclei. Often
The Pindborg or calcifying epithelial odon- bizarre and pleomorphic nuclear elements
togenic tumor is a neoplasm of epithelial are encountered, but this feature has no
origin. Clinically, depending on the size bearing on the prognosis. Within the stroma
and duration, cortical expansion or facial and often in intimate association with the
PMPH_Eversole_Chapter-10.indd 542 1/20/2011 3:10:08 PM
Radiopaque Lesions of the Jaws 543
FIGURE 10-53
Calcifying epithelial odontogenic tumor with irregular calcifications and expansion.
epithelial islands are amorphous globules Goode RK. Calcifying epithelial odontogenic tumor. Oral
of amyloid material. Circular and ovoid Maxillofac Surg Clin North Am. 2004;16:323-331.
Krolls SO, Pindborg JJ. Calcifying epithelial odonto-
laminated calcifications or Leisegang rings genic tumor. A survey of 23 cases and discussion of
are seen in most tumors. histomorphologic variations. Arch Pathol Lab Med.
1974;98:206.
DIFFERENTIAL DIAGNOSIS Pindborg JJ. A calcifying epithelial odontogenic tumor.
Cancer. 1958;11:838.
When the Pindborg tumor appears radio- Vap DR, Dahlin DC, Turlington EG. Pindborg tumor:
graphically as an expansile ill-defined lesion the so-called calcifying epithelial odontogenic tumor.
with irregular radiodense conglomerates Cancer. 1970;25:629.
and spicules, malignant neoplasms of bone
should be considered in the differential
DESMOPLASTIC
diagnosis. If an impacted tooth is encom-
passed by a lesion with the aforementioned AMELOBLASTOMA
features, Pindborg tumor should be the Figure 10-54
foremost consideration. Biopsy is required
Age: No predilection
in any case.
Sex: No predilection
TREATMENT CLINICAL AND RADIOGRAPHIC
FEATURES
Pindborg tumor is aggressive and recurs
if adequate therapy is not instituted. Large The desmoplastic ameloblastoma is a variant
lesions require resection, hemimandibulec- of ameloblastoma that has been segregated
tomy, or partial maxillectomy; smaller owing to its unique radiographic and his-
tumors may be cured by en bloc or mar- tologic features. Ameloblastomas are most
ginal resection. frequently found in the posterior body and
ramus of the mandible; however, the des-
moplastic variant is found with equal fre-
Additional Reading quency in the maxilla and mandible and has
a tendency to arise in the anterior regions.
Chaudhry AP, Hanks CT, Leifer C, Gargiulo EA.
Calcifying epithelial odontogenic tumor. A his-
Radiographically, many of these tumors are
tochemical and ultrastructural study. Cancer. 1972;30: mistaken for fibro-osseous lesions owing to
519-529. their mixed radiolucent-radiopaque appear-
PMPH_Eversole_Chapter-10.indd 543 1/20/2011 3:10:18 PM
544 Chapter 10
FIGURE 10-54
Desmoplastic ameloblas-
toma with a benign fibro-
osseous-like pattern.
ance. Although some are well delineated, sarcoma. Biopsy is required to obtain a
others show diffuse margins without any definitive diagnosis.
cortication. Clinically, painless expansion
is the chief complaint, although in many TREATMENT
instances, the patient is not aware of any Small lesions should be treated by surgi-
signs or symptoms. cal enucleation, whereas larger tumors
with poorly defined margins are probably
MICROSCOPIC FEATURES
better managed by en bloc or marginal
Characteristically, the stroma dominates resection with reconstruction. Although
over the epithelial neoplastic component. data are limited, these tumors appear
Thin cords of hyperchromatic epithelial to behave in similar fashion to ordinary
cells are seen and many islands fail to ameloblastoma.
show distinct ameloblastic columnar cells,
although careful perusal of the tissue gen-
erally reveals foci of stellate reticulum and Additional Reading
some attempts at ameloblastic differen-
Atalay B, Soluk M, Brkić A, Emes Y, Cetin O, Olgac
tiation. Adenoid structures are commonly V. Desmoplastic ameloblastoma. J Craniofac Surg.
found. The stroma is densely collagenous 2009;20:2256-2259.
and abundant. Eversole LR, Leider AS, Hansen LS. Ameloblastomas
with pronounced stromal desmoplasia. J Oral
DIFFERENTIAL DIAGNOSIS Maxillofac Surg. 1984;42:735.
Waldron CA, El-Mofty SK. A histopathological study
Radiographically, as mentioned previously, of 116 ameloblastomas with special reference to the
these tumors are often mistaken for benign desmoplastic variant. Oral Surg Oral Med Oral Pathol.
1987;63:441.
fibro-osseous lesions, especially fibrous Yoshimura Y, Saito H. Desmoplastic variant of amelo-
dysplasia. The lack of margination may be blastoma: report of a case and review of the literature.
suggestive of metastatic tumor or primary J Oral Maxillofac Surg. 1990;48:1231.
PMPH_Eversole_Chapter-10.indd 544 1/20/2011 3:10:29 PM
Radiopaque Lesions of the Jaws 545
OSTEOGENIC AND qua non of osteogenic sarcoma is the elabo-
CHONDROGENIC SARCOMA ration of neoplastic osteoid matrix. Tumor
Figure 10-55 osteoid is found in all osteogenic sarcomas,
including the chondroblastic variant. Chon-
Age: Teenagers and young adults drosarcomas fail to elaborate tumor osteoid.
Sex: Male predilection The cellular element is composed, in both
CLINICAL AND RADIOGRAPHIC instances, of pleomorphic angulated, polyg-
FEATURES onal, or spindle-shaped cells.
Both osteogenic and chondrogenic sarcomas
DIFFERENTIAL DIAGNOSIS
of the jaws are rare. They show similar radio-
graphic features, although sarcomas of chon- Irregular, poorly marginated radiopacities
droblastic origin tend to be more radiolucent. should always suggest a tentative diagno-
When the tumor cartilage or osteoid calcifies, sis of osteogenic or chondrogenic sarcoma.
both chondrosarcoma and osteosarcoma Pindborg tumor, particularly if an impacted
can manifest irregular, poorly marginated tooth is associated with the lesion, and
radiopaque foci. Osteogenic sarcomas show metastatic carcinoma must be considered
a sunray or sunburst pattern of osteophytic in the differential radiographic diagnosis.
radiodense spicules in 25% of the cases. Biopsy is required to arrive at a definitive
Expansion of the alveolar cortices is demon- diagnosis.
strable both clinically and radiographically.
The mandible is more often affected than TREATMENT
the maxilla. Pain, paresthesia, and loosening The prognosis for osteogenic sarcoma is
of teeth in the region of tumor are common better for mandibular (70% 5-year survival)
complaints. Both sarcomas tend to metasta- than for maxillary tumor (50% 5-year sur-
size via hematogenous routes. vival). Information of this nature does not
exist for chondrosarcoma of the jaws. The
MICROSCOPIC FEATURES
treatment consists of maxillectomy with
Osteogenic sarcomas are histologically preservation of the orbit if extent of disease
divided into three groups: osteoblastic, allows. Mandibular tumors are treated with
chondroblastic, and fibroblastic. This clas- intraosseous radium needles with external
sification has no bearing on prognosis. The radiation when soft tissues are involved
tumor may differentiate along all three cell (10,000 rad total dosage). After radiation, en
lines; yet, regardless of the preponderance of bloc resection or hemimandibulectomy is
fibrous and cartilaginous elements, the sine performed.
FIGURE 10-55
Osteogenic sarcoma.
PMPH_Eversole_Chapter-10.indd 545 1/20/2011 3:10:39 PM
546 Chapter 10
obvious, as are focal radiolucent zones
Additional Reading admixed with irregular radiopaque foci.
Azizi T, Motamedi MH, Jafari SM. Gnathic osteosarco- The margins of the metastatic lesion are
mas: a 10-year multicenter demographic study. Indian poorly defined. Metastatic carcinoma is
J Cancer. 2009;46:231-233. the most common malignant tumor of the
Chaudhry AP, Robinovitch MR, Mitchell DF, et jaws.
al. Chondrogenic tumors of the jaws. Am J Surg.
1961;102:403.
Garrington GE, Collett WK. Chondrosarcoma. II. MICROSCOPIC FEATURES
Chondrosarcoma of the jaws: analysis of 37 cases.
The microscopic features are variable,
J Oral Pathol Med. 1988;17:12.
Garrington GE, Scofield HH, Cornyn J, Hooker SP. depending on the tissue site of origin. In
Osteosarcoma of the jaws: analysis of 56 cases. Cancer. general, nests, cords, or sheets of neoplastic
1967;20:377-391. epithelial cells show pleomorphism, ana-
Russ JE, Jesse RH. Management of osteosarcoma of the plasia, and numerous mitotic figures. The
maxilla and mandible. Am J Surg. 1980;140:572.
tumor cells are dispersed within a fibrous
stroma and lie in juxtaposition to dense and
METASTATIC CARCINOMA irregular osseous trabeculae.
Figure 10-56
DIFFERENTIAL DIAGNOSIS
Age: Middle-aged and elderly adults The irregular, poorly marginated radiopaci-
Sex: Depends on primary site ties as seen in osteoblastic metastatic car-
CLINICAL AND RADIOGRAPHIC cinomas are also seen in Pindborg tumor,
FEATURES osteogenic sarcoma, and chondrosarcoma.
Carcinoma arising in the lung, breast, thy- A history of cancer elsewhere in the body
roid, prostate, and colon tends to metas- helps to limit the differential diagnosis;
tasize to bone. When the jaws become a however, microscopic confirmation is nec-
metastatic depot, these malignancies may essary. On the other hand, the jaw metasta-
become deposited in marrow spaces and sis may be the first indication of a primary
actually simulate osteoblastic activity. The tumor of internal organs.
body and ramus areas of the mandible are
TREATMENT
most frequently involved. The chief clini-
cal finding is paresthesia of the lower lip. The primary tumor must be identified, as
Radiographically, expansion is usually well as other sites of metastasis; a skeletal
FIGURE 10-56
Osteogenic reaction in
metastatic disease to the
mandible.
PMPH_Eversole_Chapter-10.indd 546 1/20/2011 3:10:40 PM
Radiopaque Lesions of the Jaws 547
survey is indicated to detect other osseous Mesa MC. Metastatic prostatic carcinoma to the
foci of disease. The prognosis is extremely mandible: report of case. J Oral Maxillofac Surg.
1977;35:133.
poor. An oncologist should manage patient
care.
Superimposed Soft Tissue
Additional Reading Radiopacities
Castigliano SG, Rominger CJ. Metastatic malignancy of
the jaws. Am J Surg. 1954;87:496.
SIALOLITHIASIS
Clausen F, Poulsen H. Metastatic carcinoma to the jaws. Figure 10-57
Acta Pathol Microbiol Scand. 1963;57:361.
Colella G, Giudice A, Siniscalchi G, Falcone U, Age: Middle-aged adults
Guastafierro S. Chin numbness: a symptom that should Sex: Male predilection
not be underestimated: a review of 12 cases. Am J Med
Sci. 2009;337(6):407-410. CLINICAL AND RADIOGRAPHIC
Hashimoto N, Kurihara K, Yamasaki H, Ohba S, Sakai FEATURES
H, Yoshida S. Pathological characteristics of metastatic
carcinoma in the human mandible. J Oral Pathol Med. Salivary stones are calcium phosphate
1987;16:362-367. salts that crystallize about a central nidus
FIGURE 10-57
Sialoliths and calcified submandibular gland (lower left).
PMPH_Eversole_Chapter-10.indd 547 1/20/2011 3:10:49 PM
548 Chapter 10
of gelled mucin, desquamated epithelial require surgical extirpation, although the
cells, or bacterial colonies. They are most use of a lithotripter is a nonsurgical alter-
frequently formed within the submandibu- native form of therapy. If recurrent sialad-
lar ducts, but may arise within the parotid enitis with a purulent discharge develops
gland or minor salivary gland ducts of the after removal, sialadenectomy is usually
lips or buccal mucosa. When a major duct indicated.
becomes occluded, swelling with sialad-
enitis ensues and pain while eating is a
common complaint. Many patients may be Additional Reading
asymptomatic. Milking the involved gland
El Deeb M, Holte N, Gorlin RJ. Submandibular salivary
fails to elicit flow. When submandibular gland sialoliths perforated through the oral floor. Oral
sialoliths become large, they produce a Surg Oral Med Oral Pathol. 1981;51:134.
radiopacity that may become superimposed Elmostehy MR. Parotid salivary calculus. Oral Surg Oral
over the mandible on dental films. They are Med Oral Pathol. 1968;26:18.
Levy BM, ReMine WH, De Vine KD. Salivary gland cal-
well circumscribed and oval or elongated; if culi: pain, swelling associated with eating. J Am Med
the entire gland becomes filled with intra- Assoc. 1962;181:1115.
ductal stones, they may show a cauliflower Tholen EF. Sialolithiasis. J Oral Maxillofac Surg.
pattern radiographically. An occlusal radio- 1949;7:63.
Zenk J, Koch M, Iro H. Extracorporeal and intracorpo-
graph helps to locate the stone in the soft real lithotripsy of salivary gland stones: basic investiga-
tissue of the oral floor. No relationship tions. Otolaryngol Clin North Am. 2009;42:1115-1137
exists between hyperparathyroidism and a
tendency to form salivary calculi.
PHLEBOLITHIASIS
MICROSCOPIC FEATURES Figure 10-58
The decalcified stone shows concentric
laminations without viable cellular ele- Age: No predilection
Sex: No predilection
ments. The ducts show sialodochitis with
squamous, mucous, or respiratory epithe- CLINICAL AND RADIOGRAPHIC
lial metaplasia. The gland displays acinar FEATURES
degeneration with fibrous and mononu- Phleboliths are calcified thrombi that form
clear leukocytic infiltration representing a within the lumina of dilated vascular chan-
chronic sclerosing sialadenitis. nels. They are most frequently encountered
in hemangiomas and varices. The vascular
DIFFERENTIAL DIAGNOSIS
lesions can be visualized clinically and are
When a stone is superimposed over the generally palpable, particularly when phle-
body of the mandible, a central lesion boliths are present. When these lesions arise
manifesting a radiopaque appearance in tissues such as the cheek, lips, and tongue,
must be included in the differential diag- the calcifications, which may be multiple,
nosis. Occlusal and soft tissue films rule are demonstrable on dental radiographs.
out the possibility of a central lesion. Other The stones appear as circular or oval, well-
soft tissue lesions, which may manifest a demarcated focal radiopaque foci.
superimposed radiopacity, must also be
considered. MICROSCOPIC FEATURES
Vascular channels are dilated and intralu-
TREATMENT
minal thrombi are present. Within these
Small stones may be manipulated manually thrombosed regions, dystrophic and lami-
through the duct orifice. Larger ones may nated calcific foci are observed.
PMPH_Eversole_Chapter-10.indd 548 1/20/2011 3:11:04 PM
Radiopaque Lesions of the Jaws 549
FIGURE 10-58
Pleboliths in a hemangioma
at the base of the tongue.
DIFFERENTIAL DIAGNOSIS OSSEOUS/CARTILAGINOUS
Phleboliths with radiographically demon- CHORISTOMA
strable calcifications must be differentiated Figure 10-59
from central osseous lesions. Occlusal and
soft tissue radiographs rule out this possi- Age: Adults
bility. Other soft tissue disorders manifest- Sex: No predilection
ing radiopacities must be included in the CLINICAL AND RADIOGRAPHIC
differential radiographic diagnosis. Clini- FEATURES
cal examination discloses the presence of a Benign nodular growths of cartilage or bone
vascular lesion unless it is deep seated; in occasionally encountered in the oral mucosa
these instances, biopsy is indicated. are self-limited choristomas. Such lesions
may occur in any submucosal location yet are
TREATMENT
most common in the tongue. Radiographi-
Because most hemangiomas show a ces- cally, depending on the view ordered, the cal-
sation in growth potential, no treatment is cified nature of the choristoma is evident as
required provided the diagnosis has been an opacity. In panoramic or periapical radio-
confirmed. Surgical removal may be indi- graphs, a round or oval opacification may
cated if function is compromised by the appear to overlie the mandible if the lesion is
tumor or if cosmesis is a concern. located in the tongue. Most of these calcified
choristomas can be palpated and an occlusal
film will disclose its soft tissue localization.
Additional Reading
MICROSCOPIC FEATURES
Lo Casto A, Salerno S, Cannizzaro F, et al. MRI find-
ings in lingual venous malformations. Dentomaxillofac These hard tissue choristomas may histo-
Radiol. 2003;32:333-336. logically consist of benign, mature bone,
O’Riordan B. Phleboliths and salivary calculi. Br J Oral
Maxillofac Surg. 1974;12:119.
cartilage, or both. A fibrous capsule is gen-
Parker LA, Frommer HH. Phleboliths; report of case. erally observed and fibrous tissue marrow-
Oral Surg Oral Med Oral Pathol. 1964;18:476. like spaces may be seen.
PMPH_Eversole_Chapter-10.indd 549 1/20/2011 3:11:05 PM
550 Chapter 10
FIGURE 10-59
Osseous choristomas in
the soft tissues.
FIGURE 10-60
Foreign bodies: amalgam
tattoos and tongue pierc-
ing (right).
DIFFERENTIAL DIAGNOSIS Mesa ML, Schneider LC, Northington L. Osteoma of the
buccal mucosa. J Oral Maxillofac Surg. 1982;40:684.
Osteocartilaginous choristomas may be con- Tohill MJ, Green JG, Cohen DM. Intraoral osseous and
fused radiographically with sialoliths and cartilaginous choristomas: report of three cases and
phleboliths, both of which tend to be oval or review of the literature. Oral Surg Oral Med Oral
Pathol. 1987;63:506.
round. Palpation of a mass in the tongue or
other mucosal sites warrants a biopsy.
TREATMENT FOREIGN BODIES
Figure 10-60
Simple excision is recommended. Recur-
rence is extremely rare. Age: No predilection
Sex: No predilection
Additional Reading CLINICAL AND RADIOGRAPHIC
FEATURES
Davis GB. Intraoral osseous choristoma: report of case.
J Oral Maxillofac Surg. 1980;38:144. Foreign objects are introduced into the oral
Johann AC, Garcia BG, Nacif TR, de Freitas JB, do Carmo soft tissues as a result of traumatic or iatro-
MA, Mesquita RA. Submandibular osseous choristoma. genic injuries. Dental amalgam and metal
J Craniomaxillofac Surg. 2006;34(1):57-59.
Krolls SO, Jacoway JR, Alexander WN. Osseous choris-
fragments from automobile accidents or
tomas (osteomas) of intraoral soft tissues. Oral Surg assault are the more frequently encountered
Oral Med Oral Pathol. 1971;32:588. foreign bodies that are demonstrable radio-
PMPH_Eversole_Chapter-10.indd 550 1/20/2011 3:11:14 PM
Radiopaque Lesions of the Jaws 551
graphically. When these metallic objects Stewart CM, Watson RE. Experimental oral foreign body
become lodged within the buccal mucosa, reactions. Commonly employed dental materials. Oral
Surg Oral Med Oral Pathol. 1990;69:713.
lips, tongue, alveolar ridges, or gingiva, they
appear as irregular ragged radiopacities
superimposed over the maxilla or mandible.
Many foreign bodies are easily visualized
CALCIFIED LYMPH NODES
clinically as discolorations or swellings, or Figure 10-61
they may be palpable. Tongue, lip, and buc-
Age: Adults
cal mucosal piercings have made for some Sex: No predilection
interesting radiographic artistry.
CLINICAL AND RADIOGRAPHIC
FEATURES
MICROSCOPIC FEATURES
Metallic foreign bodies cannot be processed In the head and neck area, submandibu-
for routine microscopy. The surrounding lar, cervical, and digastric nodes are most
tissue may be fibrous, granulomatous with often enlarged during infectious processes.
giant cells, or acutely inflamed, depending Occasionally, a node or group of nodes with
on the chemical and physical properties of longstanding lymphadenopathy undergoes
the foreign object. fibrosis and subsequently develops foci of
dystrophic calcification. Scrofula, or tuber-
DIFFERENTIAL DIAGNOSIS
culous lymphadenitis, is probably the most
prevalent disease process to eventuate in
Foreign-body radiopacities superimposed nodal calcification. Actinomycosis, cats-
over bone are usually readily identifiable cratch fever, and other chronic infectious
because of irregular outline or configuration diseases may also eventually become qui-
of the metal deposit. In addition, the opacity escent with dystrophic calcification of scle-
is generally more dense and homogeneous rotic nodes. Radiographically, a single ovoid
than that of calcific lesions. Soft tissue films calcification or clustered calcifications may
and biopsy provide a definitive diagnosis. be encountered in regions in which groups
of lymph nodes are typically found.
TREATMENT
The foreign body should be excised, par- MICROSCOPIC FEATURES
ticularly if a fistula or swelling is present. The normal architecture of the lymph node
Amalgam pigmentation seen clinically in is usually obliterated; however, the periph-
conjunction with a radiopacity does not ery may occasionally be represented by
require treatment. aggregates of lymphocytes and atrophic
germinal centers. The central zone is occu-
pied by dense collagenous connective tissue
Additional Reading with confluent deposits of calcification.
Blum T. Foreign bodies in and about the jaws. Dent
Cosmos. 1921;63:12227. DIFFERENTIAL DIAGNOSIS
Eliasson ST, Holte NO. Rubber base impression mate-
rial as a foreign body: report of case. Oral Surg Oral
Calcified lymph nodes radiographically
Med Oral Pathol. 1979;48:379. resemble sialoliths, phleboliths, or foreign
Shinohara EH, Horikawa FK, Ruiz MM, Shinohara MT. bodies. Sialography is often helpful in that
Tongue piercing: case report of a local complication. the calcified node is not associated with the
J Contemp Dent Pract. 2007;8:83-89.
Stafne EC, Gibilisco JA. Oral Roentgenographic
duct tree. A history of scrofula or other dis-
Diagnosis. 4th ed. Philadelphia, PA: W. B. Saunders; eases associated with chronic lymphadeni-
1975. tis aids in arriving at a definitive diagnosis,
PMPH_Eversole_Chapter-10.indd 551 1/20/2011 3:11:18 PM
552 Chapter 10
FIGURE 10-61
Calcified lymph nodes.
particularly when the radiopacities are with ensuing age. In this form, intestinal
located in an area known to be populated smooth muscle, skeletal muscle, and fascia
by lymph nodes. undergo calcification. The facial muscles
may be involved. The etiology is unknown.
TREATMENT The second form, seen in a single muscle,
No treatment is required. is more often encountered in the perioral
musculature and is secondary to trauma
(traumatic myositis ossificans). The trau-
Additional Reading matic episode is thought to produce an
intramuscular hematoma, which organizes
Kara I, Yeler D, Yeler H, Ay S. Panoramic radiographic
appearance of massive calcification of tuberculous
and subsequently calcifies. The masseter,
lymph nodes. J Contemp Dent Pract. 2008;9:108-114. temporal, pterygoid, and geniohyoid mus-
Keberle M, Robinson S. Physiologic and pathologic cal- cles have been reported to be involved by
cifications and ossifications in the face and neck. Eur this process. The affected muscle shows
Radiol. 2007;17(8):2103-2111.
Sakae T, Yamamoto H. Crystals and calcification patterns
rapid enlargement subsequent to trauma
in two lymph node calcifications. J Oral Pathol Med. and then becomes indurated. Motion may
1987;16:456. be limited. Radiographically, the muscle
Wood NK, Goaz PW, eds. Periapical radiopacities. In involved shows a radiopaque zone that may
Differential Diagnosis of Oral Lesions. St. Louis, MO;
be discrete or show frayed margins. Myo-
C. V. Mosby; 1980: 559.
Zohar Y, Talmi YP. Calcified mass in the submandibular sitis ossificans in the masseter, pterygoids,
region. Isr J Dent Sci. 1988;2:101. or muscles in the floor of the mouth mani-
fest a radiopacity superimposed over the
mandible.
MYOSITIS OSSIFICANS
Figure 10-62 MICROSCOPIC FEATURES
Osteoid trabeculae are rimmed by osteo-
Age: Adults
Sex: Male predilection blasts, and the intervening fibrous tissue is
hypercellular. The overall picture is one of
CLINICAL AND RADIOGRAPHIC extremely active osteoplasia that has been
FEATURES
mistaken for sarcoma. The ossified zone is
Ossification of muscle occurs in a general- surrounded by muscle fibers. Mononuclear
ized form that begins in childhood and inflammatory cells are occasionally present
becomes progressively more extensive in limited number.
PMPH_Eversole_Chapter-10.indd 552 1/20/2011 3:11:18 PM
Radiopaque Lesions of the Jaws 553
ularly with the aid of occlusal radiographs.
In addition, most sialoliths and phleboliths
are focal, small calcific structures, whereas
the opacity seen in myositis ossificans is
generally large and diffuse.
TREATMENT
Once a tentative diagnosis is established,
the muscle can be entered surgically and
the calcified mass is excised; a portion of
the adjacent normal-appearing muscle must
also be obtained. A biopsy is needed to con-
firm the clinical diagnosis. Recurrence is
uncommon.
FIGURE 10-62
Additional Reading
Myositis ossificans in masticatory muscles. (Right Goodsell JO. Traumatic myositis ossificans of the
photo from Plezia RA, Mintz SM, Calligaro P. masseter muscle: review of the literature and report of
Myositis ossificans traumatica of the masseter mus- a case. J Oral Maxillofac Surg. 1962;20:116.
cle. Oral Surg Oral Med Oral Pathol. 1977;44:351.) Kruse AL, Dannemann C, Grätz KW. Bilateral myositis
ossificans of the masseter muscle after chemoradio-
therapy and critical illness neuropathy—report of a
DIFFERENTIAL DIAGNOSIS rare entity and review of literature. Head Neck Oncol.
2009;1:30.Mulherin D, Schow CE Jr. Traumatic myo-
The history and clinical features usually sitis ossificans after genioplasty. J Oral Maxillofac
indicate that the radiopaque mass is external Surg. 1980;38:786.
to bone. Radiographic views from various Narang R, Dixon RA Jr. Myositis ossificans: medial ptery-
angles usually locate the lesion in the soft goid muscle—a case report. Br J Oral Maxillofac Surg.
1974;12:229.
tissues in the vicinity of muscle. Sialoliths Plezia RA, Mintz SM, Calligaro P. Myositis ossificans
can be eliminated from consideration on traumatica of the masseter muscle. Report of a case.
the basis of location and symptoms, partic- Oral Surg Oral Med Oral Pathol. 1977;44:351.
PMPH_Eversole_Chapter-10.indd 553 1/20/2011 3:11:20 PM
a b c d e
f g h i
j k l m n o p q
r s t u v
w x y z
aa bb cc dd ee ff gg hh ii jj
Dental Defects
a, Limited hypodontia; b, Severe hypodontia; c, Hyperdontia; d, Focal pigmentation; e, Generalized
pigmentation; f, Localized microdontia; g, Generalized microdontia; h, Localized macrodontia; i, General-
ized macrodontia; j, Enamel pearl; k, Accessory roots; I, Accessory cusps; m, Dilaceration; n, Dens-in-dente;
o, Taurodontia; p, Fusion; q, Gemination; r, Concrescence; s, Attrition; t, Abrasion; u, Erosion; v, Hyperce-
mentosis; w, Enamel hypoplasia; x, Congenital syphilis; y, Fluorosis; z, Snowcapped teeth; aa, Amelogenesis
imperfecta; bb, Dentinogenesis imperfecta; cc, Dentin dysplasia I; dd, Dentin dysplasia II; ee, Odontodyspla-
sia; ff, Cemental agenesis (hypophosphatasia); gg, Vitamin D refractory rickets; hh, Pulp stones; ii, Internal
resorption; jj, External resorption
PMPH_Eversole_Chapter-11.indd 554 1/20/2011 3:12:06 PM
Dental Defects
11
Alterations in Number: Alterations in
Missing Teeth 558 Structure 577
HYPODONTIA 558 DENTAL CARIES 577
INCONTINENTIA PIGMENTI 559 ENAMEL HYPOPLASIA 579
HYALINOSIS CUTIS ET MUCOSAE 559 CONGENITAL SYPHILIS 580
MANDIBULO-OCULO-FACIAL DENTAL FLUOROSIS 581
DYSCEPHALY 560 SNOW-CAPPED TEETH 582
HEREDITARY ECTODERMAL AMELOGENESIS IMPERFECTA,
DYSPLASIA 560 HYPOPLASTIC TYPES 582
CHONDROECTODERMAL AMELOGENESIS IMPERFECTA,
DYSPLASIA 561 HYPOMATURATION/
HYPOCALCIFICATION
Alterations in Number: TYPES 584
Supernumerary Teeth 562 SYNDROME-ASSOCIATED ENAMEL
DEFECTS 585
HYPERDONTIA 562 DENTINOGENESIS
CLEIDOCRANIAL DYSPLASIA 563 IMPERFECTA 587
GARDNER’S SYNDROME 564 OSTEOGENESIS IMPERFECTA 588
DENTIN DYSPLASIA TYPE I 589
Alterations in DENTIN DYSPLASIA TYPE II 590
Morphology 565 REGIONAL
ODONTODYSPLASIA 591
MICRODONTIA AND HYPOPHOSPHATASIA 593
MACRODONTIA 565 VITAMIN D REFRACTORY
ACCESSORY CUSPS AND RICKETS 593
ROOTS 566 DENTICLES AND PULP
DENTAL TRANSPOSITION 567 CALCIFICATION 595
ENAMEL PEARL 568 SEGMENTAL ODONTOMAXILLARY
DILACERATION 568 DYSPLASIA 595
DENS INVAGINATUS (DENS IN INTERNAL RESORPTION 597
DENTE) 570 EXTERNAL RESORPTION 598
TAURODONTISM 571 SUBCERVICAL RESORPTION 599
GEMINATION 571 CORONAL FRACTURE 600
FUSION 572
CONCRESCENCE 573 Enlarged Pulp Chambers/
ATTRITION 574 Root Canals*
ABRASION 575 VITAMIN D REFRACTORY
EROSION 575 RICKETS
HYPERCEMENTOSIS 576 DENTIN DYSPLASIA TYPE II
PMPH_Eversole_Chapter-11.indd 555 1/20/2011 3:12:07 PM
DENTINOGENESIS IMPERFECTA,
TYPE III
Pigmentations 603
PSEUDOHYPOPARATHYROIDISM ERYTHROBLASTOSIS FETALIS 603
REGIONAL ODONTODYSPLASIA BILIARY ATRESIA 604
POSTMORTEM PINK TEETH 605
Obliterated Pulp Chambers/ PORPHYRIA 605
Root Canals* DENTAL FLUOROSIS 606
TETRACYCLINE STAINING 607
DENTINOGENESIS IMPERFECTA
EXTRINSIC STAINING 608
DENTIN DYSPLASIA TYPE I
FOCAL PIGMENTATION 609
Alterations in Eruption/ DENTAL CARIES*
Exfoliation Times 601 DENTINOGENESIS IMPERFECTA*
DENTIN DYSPLASIA TYPE II*
PREMATURE ERUPTION 601 AMELOGENESIS IMPERFECTA*
DELAYED ERUPTION 601
IMPACTION 602 *Refer to other Headings in this Chap-
PREMATURE EXFOLIATION 603 ter for Detailed Description.
PMPH_Eversole_Chapter-11.indd 556 1/20/2011 3:12:07 PM
The anomalies of teeth have been catego- cases of hypodontia. Missing teeth are seen
rized conventionally to include defects in in incontinentia pigmenti, a potentially fatal
number, morphology, and hard tissue struc- disease of females.
ture. Most dental defects are strictly local; Supernumerary teeth are common.
others are inheritable disorders associated Gardner’s syndrome is a potentially lethal
with other anomalies of the jaws and/or disease associated with supernumerary
other organ systems. Most of the dental and impacted teeth.
defects outlined here are familial or follow Common defects in size and morphol-
definite Mendelian patterns of inheritance. ogy of teeth include accessory cusps, enamel
Some are associated with life-threatening pearl, dilaceration, and dens invaginatus.
diseases. The most common anomalies in
Age predilection has been omitted for dental structure are enamel hypoplasia,
many of the entities included in this chap- snowcapped teeth, and dental fluorosis.
ter. This omission is intentional, because Hypophosphatasia, associated with prema-
it can be inferred that the defect makes its ture exfoliation and cemental agenesis, is a
appearance at the time the dentition has potentially lethal metabolic bone disease.
completed development or the teeth have Alterations in eruption and exfolia-
erupted, thereby being initially observable tion processes are included in this chapter,
in children. as are diseases that cause the deposition
The most common disorders showing of pigments either in or on dental hard
missing teeth are simple, uncomplicated tissues.
PMPH_Eversole_Chapter-11.indd 557 1/20/2011 3:12:07 PM
558 Chapter 11
acterized by premature whitening of the
Alterations in Number: hair, hyperhidrosis of the palms and soles,
Missing Teeth and aplasia of the premolars and third
molars. It is inherited as an autosomal
HYPODONTIA dominant trait. Rieger’s syndrome, also
Figure 11-1 an autosomal dominant hereditary dis-
order, shows oligodontia and microdon-
Sex: No predilection tia associated with iridial hypoplasia and
CLINICAL FEATURES
anterior synechiae; occasionally, glaucoma
is a complication. Missing teeth also occur
Hypodontia may involve both deciduous in association with a variety of other rare
and permanent teeth but is far more often syndromes.
encountered in the latter. The third molars,
any or all of them, are the most frequently
observed congenitally missing teeth. The TREATMENT
maxillary lateral incisors and second man- When teeth are congenitally missing, the
dibular bicuspids are also frequently miss- occlusion is usually defective. Orthodontic
ing. Rarely does partial anodontia affect therapy may be indicated.
the mandibular lateral incisors and first
molars. When deciduous teeth are involved,
the maxillary lateral incisors are most often
affected. When this occurs, the correspond- Additional Reading
ing permanent succedaneous teeth are
Böök JA. Clinical and genetic studies of hypodontia. I.
also usually missing. Hypodontia shows Premolar aplasia, hyperhidrosis, and canities prema-
a definite familial tendency. Occasionally, tura. A new hereditary syndrome in man. Am J Hum
numerous congenitally missing teeth are Genet. 1950;2:240.
encountered in children who received radi- Brooks JK, Coccaro PJ, Zarbin MA. The Rieger anomaly
concomitant with multiple dental, craniofacial, and
ation to the jaws as infants for therapeutic somatic midline anomalies and short stature. Oral
reasons. Tooth germs are quite sensitive to Surg Oral Med Oral Pathol. 1989;68:717.
radiation and low doses may arrest or cause De Coster PJ, Marks LA, Martens LC, Huysseune A.
abortion of odontogenesis. Dental agenesis: genetic and clinical perspectives.
J Oral Pathol Med. 2009;38(1):1-17.
Two specific syndromes, both of Dolder E. Deficient dentition. Dent Res. 1937;56:142.
which are rare, are associated with local- Feingold M, Shiere F, Fogels HR, Donaldson D. Rieger’s
ized hypodontia. Böök’s syndrome is char- syndrome. Pediatrics. 1969;44:564-569.
FIGURE 11-1
Partial anodontia.
PMPH_Eversole_Chapter-11.indd 558 1/20/2011 3:12:07 PM
Dental Defects 559
INCONTINENTIA PIGMENTI oral and dental abnormalities. Clin Oral Investig.
2006;10(4):343-347. Epub 2006 Aug 8.
Figure 11-2 Russell DL, Finn SB. Incontinentia pigmenti (Bloch-
Sulzberger syndrome): a case report with emphasis on
Sex: Exclusively in females dental manifestations. J Dent Child. 1967;34:494.
CLINICAL FEATURES
Incontinentia pigmenti is transmitted as HYALINOSIS CUTIS ET
an X-linked dominant trait and is lethal for
males; only females with the disease sur-
MUCOSAE
vive infancy. Vesicular and erythematous Figure 11-3
skin lesions appear shortly after parturi-
Sex: No predilection
tion, becoming keratotic. The characteristic
lesions are diffuse, reticulated slate-gray CLINICAL FEATURES
macules that cover broad areas of the skin. Hyalinosis cutis et mucosae, also known as
Skeletal, ocular, and neurologic disorders lipoid proteinosis and the Urbach-Wiethe
accompany the disease. White lesions may syndrome, is inherited as an autosomal
be seen on the oral mucosa. Delayed erup- recessive disorder characterized by patho-
tion, conical crown forms, and oligodontia logic accumulation of glycoproteins in most
are the chief dental anomalies seen. bodily tissues. Hoarseness or a weak cry
from infancy develops because of vocal
TREATMENT cord infiltration. The skin develops vesicles
The disease cannot be treated. The dental that, after healing, appear as acneform scars
defects may be corrected with orthodontic with altered pigmentation; later, pale yellow
and prosthetic therapy. nodules evolve. Multiple papules or nod-
ules develop in the oral cavity, particularly
on the tongue, buccal mucosa, and soft pal-
Additional Reading ate. Intracranial calcifications, particularly
Baddour HM, Steed DL, Tilson HB. Incontinentia
of the dorsum sellae, and seizures occur, as
pigmenti: report of case. J Oral Maxillofac Surg. does decreased sensitivity to pain. Reported
1981;39:57. dental defects include hypodontia, primar-
Gorlin RJ, Anderson JA. The characteristic dentition of ily involving the maxillary lateral incisors
incontinentia pigmenti. J Pediatr. 1960;57:78.
Himelhoch DA, Scott BJ, Olsen RA. Dental defects in
and premolars.
incontinentia pigmenti. Pediatr Dent. 1987;9:236.
Minić S, Novotny GE, Trpinac D, Obradović M. Clinical TREATMENT
features of incontinentia pigmenti with emphasis on
There is no known treatment for the sys-
temic manifestations. Missing teeth may be
replaced prosthetically.
Additional Reading
Finkelstein MW, Hammond HL, Jones RB. Hyalinosis
cutis et mucosae. Oral Surg Oral Med Oral Pathol.
1982;54:49.
Hamada T. Lipoid proteinosis. Clin Exp Dermatol.
FIGURE 11-2 2002;27(8):624-629.
Hypodontia with coronal defects in incontinentia Hofer PA. Urbach-Wiethe disease. A review. Acta Derm
pigmenti. (Courtesy of Dr. R. Gorlin.) Venereol. 1971;53(suppl. 71):5.
PMPH_Eversole_Chapter-11.indd 559 1/20/2011 3:12:12 PM
560 Chapter 11
FIGURE 11-4
FIGURE 11-3 Mandibulo-oculo-facial dyscephaly. (Courtesy of Dr.
Missing lateral incisors in a child with hyalinosis Ray Stewart.)
cutis et mucosae.
malocclusion, which are common in this
Jensen AD, Khodadoust A, Emery JM. Lipoid proteino- syndrome, should be treated accordingly.
sis: report of a case with electron microscopic findings. The craniofacial anomalies can be treated
Arch Ophthalmol. 1972;88:273. by orthognathic and plastic surgery.
Lin J, Hurng JJ, Wong CK. Hyalinosis cutis et muco-
sae—a case report. J Dermatol. 1987;14:497.
Additional Reading
MANDIBULO-OCULO-FACIAL Hoefnagel D, Benirschke K. Dyscephalia mandibulo-oc-
DYSCEPHALY ulo-facialis (Hallermann-Streiff syndrome). Arch Dis
Child. 1965;40:57.
Figure 11-4 Hutchinson M. Oral manifestations of oculoman-
dibulodyscephaly with hypotrichosis (Hallermann-
Sex: No predilection Streiff syndrome). Oral Surg Oral Med Oral Pathol.
1971;31:234-244.
CLINICAL FEATURES
Judge C, Chakanouskis JE. The Hallermann-Streiff syn-
The mandibulo-oculo-facial dyscephaly drome. J Ment Defic Res. 1971;15:115.
syndrome, also known by the eponym
Hallermann-Streiff syndrome, is character- HEREDITARY ECTODERMAL
ized by brachycephaly with frontal bossing,
small face, beak-like nose, mandibular ret-
DYSPLASIA
rognathia, temporomandibular joint anom- Figure 11-5
alies, open sutures, and microphthalmia
Sex: Male predilection
with blue sclera. Hypotrichosis with absent
brows, cutaneous atrophy, spinal deformi- CLINICAL FEATURES
ties, and mild retardation are also featured. Ectodermal dysplasia is a group of disor-
Hypodontia is seen with retention of decid- ders with similar features and differing
uous teeth, although supernumerary teeth modes of inheritance. Usually inherited
can also be present. Dental malformations as an X-linked recessive trait, ectodermal
are also commonly encountered. The syn- dysplasia is seen in males. One of the few
drome is usually sporadic. inherited structural defects to show genetic
heterogenicity, ectodermal dysplasia may
TREATMENT
also show an autosomal dominant form
As long as the deciduous dentition remains of transmission, whereby females mani-
sound, it can be retained. Severe caries and fest the trait. A variety of forms are now
PMPH_Eversole_Chapter-11.indd 560 1/20/2011 3:12:13 PM
Dental Defects 561
FIGURE 11-5
Ectodermal dysplasia.
Multiple missing teeth
conical cusps, lanugo hair.
Complete anodontia on
right.
recognized. Ectodermal appendages includ-
ing hair, teeth, and sweat glands either fail Additional Reading
to develop or are rudimentary. Children Bartlett RC, Eversole LR, Adkins RS. Autosomal
may be completely bald or possess lanugo recessive hypohidrotic ectodermal dysplasia: den-
hair. Heat intolerance is a common finding tal manifestations. Oral Surg Oral Med Oral Pathol.
because of the sweat gland agenesis. Com- 1972;33:736.
Crawford PJ, Aldred MJ, Clarke A, Michael SY. Rapp-
plete anodontia is sometimes seen; how- Hodgkin syndrome: an ectodermal dysplasia involving
ever, in most cases, the cuspids are present, the teeth, hair, nails, and palate. Oral Surg Oral Med
albeit malformed, with conical crown struc- Oral Pathol. 1989;67:50-62.
ture. Salivary hypoplasia with xerostomia is Irvine AD. Towards a unified classification of the ecto-
dermal dysplasias: opportunities outweigh challenges.
sometimes seen. Other anomalies including Am J Med Genet A. 2009;149A(9):1970-1972.
pili torti (kinky hair), cleft palate, popliteal Nakata M, Koshiba H, Eto K, Nance WE. A genetic
pterygium, cleft lip, and ectrodactyly may study of anodontia in X-linked hypohidrotic ectoder-
occur in variant forms of ectodermal dys- mal dysplasia. Am J Hum Genet. 1980;32: 908.
Upshaw BY, Montgomery H. Hereditary anhidrotic ecto-
plasia (Rapp-Hodgkin syndrome, Rosselli-
dermal dysplasia: a clinical and pathologic study. Arch
Gulienetti syndrome). Dermatol Syph. 1949;60:1170.
TREATMENT
CHONDROECTODERMAL
In most affected children, prosthetic appli-
ances are well tolerated; if xerostomia is DYSPLASIA
severe, dentures with a soft liner may be Figure 11-6
used. In some cases, however, prostheses
Sex: No predilection
cannot be tolerated. Because affected chil-
dren cannot stand hot humid climates, CLINICAL FEATURES
relocation to cool climates and/or air-con- Inherited as an autosomal recessive
ditioned living quarters are recommended. trait, the Ellis-van Creveld syndrome or
PMPH_Eversole_Chapter-11.indd 561 1/20/2011 3:12:14 PM
562 Chapter 11
chondroectodermal dysplasia represents a
developmental disorder involving both epi-
dermal and mesodermal tissues. The skin
anomalies include dysplasia of the nails and
hair. Sweat glands may be normal. Congen-
ital absence of some or numerous teeth and
fusion of the upper lip to the anterior max-
illary alveolar ridge are noted. Eruption is
often retarded. As with ectodermal dys-
plasia, the teeth that do form often evince
conical crown forms. The mesodermal
defects are most prominent in endochon- FIGURE 11-6
dral bones. The limbs are short, and poly- Hypodontia in chondroectodermal dysplasia.
dactyly is observed on both hands and feet. (Courtesy of Dr. Stefan Levin.)
The same features are typical of chondro-
plastic dwarfism. Congenital heart defects
are present in one half of the individuals McKusick VA, Egeland JA, Eldridge R, Krusen DE.
affected with the syndrome. The dental Dwarfism in the Amish. I. The Ellis-van Creveld syn-
drome. Bull Hopkins Hosp. 1964;115:306-336.
anomalies are similar to those encountered
in ectodermal dysplasia. Chondroplastic
dwarfism in conjunction with ectodermal
defects and hypodontia are the diagnostic
Alterations in Number:
features of chondroectodermal dysplasia. Supernumerary Teeth
TREATMENT
HYPERDONTIA
Figure 11-7
If their root length is adequate, the exist-
ing teeth may be used as abutments for Sex: No predilection
either removable or fixed dental prostheses.
When congenital heart disease is present CLINICAL FEATURES
and oral surgical procedures are required, Simple hyperdontia is not uncommon.
prophylactic antibiotic coverage should The supernumerary teeth may be eumor-
be instituted to prevent subacute bacterial phic but are usually heteromorphic. The
endocarditis. most common supernumerary tooth is the
mesiodens, which is formed in the midline
of the maxilla, either erupted or impacted,
Additional Reading and may occur singly or in pairs. It is
Biggerstaff RH, Mazaheri M. Oral manifestations of
heteromorphic with conical crown form.
the Ellis-van Creveld syndrome. J Am Dent Assoc. Maxillary fourth molars, also generally
1968;77:1090. heteromorphic, may be located behind the
Blackburn MG, Belliveau RE. Ellis-van Creveld syn- third molars (distomolars), or they may
drome: a report of previously undescribed anomalies
in two siblings. Am J Dis Child. 1971;122:267.
erupt laterally on the buccal aspect of the
Hanemann JA, de Carvalho BC, Franco EC. Oral mani- normal maxillary molar dentition (para-
festations in Ellis-van Creveld syndrome: report of a molars). Maxillary lateral incisors, man-
case and review of the literature. J Oral Maxillofac dibular incisors, and bicuspids occasion-
Surg. 2010;68(2):456-460.
ally are supernumerary; extra cuspids are
Kagalwala TY, Vaidya VU, Joshi RM, Bharucha BA,
Kumta NB. Chondroectodermal dysplasia. Indian rarely encountered. Extra deciduous teeth
Pediatr. 1987;24:1045-1050. are rare.
PMPH_Eversole_Chapter-11.indd 562 1/20/2011 3:12:25 PM
Dental Defects 563
FIGURE 11-7
Supernumerary teeth,
mesiodens upper right.
TREATMENT bossing, and the maxillary sinuses are
Supernumerary teeth that have erupted rudimentary. The clavicles may be absent
usually are afunctional and should be or hypoplastic so that the patient may be
extracted. Impacted supernumerary teeth able to adduct the shoulders almost to the
may interfere with normal tooth position point of touching. Other bones may show
and can develop dentigerous cysts. For anomalous development as well. The oral
this reason, they too should be surgically manifestations are striking, particularly
extracted as soon as they are identified. on dental radiographs. The deciduous
teeth may show delayed exfoliation, and
both dental arches are virtually fi lled with
Additional Reading unerupted permanent and supernumer-
ary teeth. It has been suggested that the
Bodin I, Julin P, Thomsson M. Hyperodontia III. defect in eruption is linked to the absence
Supernumerary anterior teeth. Dentomaxillofac or paucity of cementum on the permanent
Radiol. 1981;10:35. tooth roots. The locus for this disease was
Järvinen S, Lehtinen L. Supernumerary and congenital
missing primary teeth in Finnish children. An epide- mapped to chromosome 6p21. RUNX2 is
miologic study. Acta Odontol Scand. 1981;39: 83. a member of the runt family of transcrip-
Proff P, Fanghänel J, Allegrini S Jr, Bayerlein T, Gedrange tion factors and its expression is restricted
T. Problems of supernumerary teeth, hyperdontia to developing osteoblasts and a subset of
or dentes supernumerarii. Ann Anat. 2006;188(2):
163-169.
chondrocytes.
Stafne EC. Supernumerary teeth. Dent Cosmos.
1932;74:653.
Webster RL. Two cases of hereditary supernumeraries in TREATMENT
same family. Int J Orthod. 1927;13:620.
Deciduous tooth retention and numer-
ous impactions provide for a monumental
CLEIDOCRANIAL DYSPLASIA orthodontic problem. Removal of the
Figure 11-8 deciduous teeth does not usually allow
for eruption of the secondary dentition.
Sex: No predilection Attempts to surgically uncover, wire, and
orthodontically erupt the impacted teeth
CLINICAL FEATURES
may be successful.
Cleidocranial dysplasia may occur sporad-
ically or as an autosomal dominant trait.
The disease affects the bones of the shoul-
der and craniofacial complex. The cra-
Additional Reading
nial fontanels remain open into adult life, Järvinen S. Dental findings in three cases of cleidocranial
the frontal eminence is prominent with dysostosis. Proc Finn Dent Soc. 1980;76:56.
PMPH_Eversole_Chapter-11.indd 563 1/20/2011 3:12:25 PM
564 Chapter 11
FIGURE 11-8
Multiple impactions and supernumerary teeth in cleidocranial dysplasia. Absence of clavicles.
Kalliala E, Taskinen PJ. Cleidocranial dysostosis; report decade; ultimately many of these polyps
of six typical cases and one atypical case. Oral Surg transform into adenocarcinoma. Extraint-
Oral Med Oral Pathol. 1962;15:808.
Miles PW. Cleidocranial dysostosis: a survey of six new estinal manifestations include osteomas
cases and 126 from the literature. J Kans Med Soc. and dental abnormalities (unerupted teeth,
1940;41:462. congenital absence of one or more teeth,
Otto F, Kanegane H, Mundlos S. Mutations in the supernumerary teeth, and odontomas).
RUNX2 gene in patients with cleidocranial dysplasia.
Hum Mutat. 2002;19(3):209-216.
In addition, congenital hypertrophy of
Trimble LD, West RA, McNeill RW. Cleidocranial dys- the retinal pigment epithelium, desmoid
plasia: comprehensive treatment of the dentofacial tumors, and extracolonic cancers includ-
abnormalities. J Am Dent Assoc. 1982;105:661. ing thyroid, liver, bile ducts, and central
nervous system are encountered. There is a
GARDNER’S SYNDROME less aggressive form in which fewer polyps
are present and cancerous transformation
Figure 11-9
is less frequent. Craniomandibular osteo-
mas, dental abnormalities, and fibromas
Sex: No predilection on the scalp, shoulders, arms, and back
typify the Gardner variant. Classic FAP is
CLINICAL FEATURES
inherited in an autosomal dominant man-
Familial adenomatous polyposis (FAP) is ner and results from a germline mutation
characterized by multiple colonic polyps in the adenomatous polyposis (APC) gene.
that make their appearance in the second A MUTYH mutation causes a recessively
PMPH_Eversole_Chapter-11.indd 564 1/20/2011 3:12:29 PM
Dental Defects 565
FIGURE 11-9
Supernumerary teeth in
Gardner’s syndrome, osteo-
mas, premalignant adenom-
atous intestinal polyps.
inherited polyposis condition, also at lower
risk than classic FAP for development of Alterations in Morphology
carcinoma.
MICRODONTIA AND
TREATMENT MACRODONTIA
The primary concern in Gardner’s syn- Figure 11-10
drome is detection of the entity so that the Sex: No predilection
patient can be referred to a gastroenter-
CLINICAL FEATURES
ologist for management of the potentially
malignant intestinal polyps. The maxillofa- Variations in the size of teeth may be gen-
cial osteomas may require surgical removal, eralized, involving the entire dentition, or
and orthodontic therapy may be instituted localized to one or a few teeth; the latter
to restore the occlusion. is more common. Generalized microdon-
tia, extremely rare, is encountered among
pituitary dwarfs, whereas macrodontia may
Additional Reading be a feature of pituitary gigantism. Mac-
rodontia restricted to one half the teeth in
Coli RD, Moore JP, La Marche PH, DeLuca FG,
Thayer WR Jr. Gardner’s syndrome. Am J Dig Dis. unilateral distribution is a feature of facial
1970;15:551-568. hemihypertrophy. Localized microdon-
Half E, Bercovich D, Rozen P. Familial adenomatous tia most often affects the maxillary lateral
polyposis. Orphanet J Rare Dis. 2009;4:22. incisors, with formation of conical crown
Ida M, Nakamura T, Utsanomiya J. Osteomatous chang-
es and tooth abnormalities in the jaw of patients with forms. The disorder is usually familial.
adenomatosis coli. Oral Surg Oral Med Oral Pathol. Third molars are commonly small and mal-
1981;52:2. formed as well. Localized macrodontia is
Jones K, Korzcak P. The diagnostic significance and man- less often observed than microdontia. The
agement of Gardner’s syndrome. Br J Oral Maxillofac
Surg. 1990;28:80.
incisors are most commonly affected, but
Rayne J. Gardner’s syndrome. Br J Oral Maxillofac Surg. geminated or fused teeth may show fea-
1968;6:11. tures that could be confused with true mac-
PMPH_Eversole_Chapter-11.indd 565 1/20/2011 3:12:41 PM
566 Chapter 11
FIGURE 11-10
Microdontia above, macrodon-
tia below.
rodontia. Syndromic associations are seen ACCESSORY CUSPS AND
such as the microdontia, microtia, and sen- ROOTS
sorineural hearing loss syndrome in which Figure 11-11
there is a mutation in the fibroblast growth
factor number 3 gene. Sex: No predilection
TREATMENT CLINICAL FEATURES
Microdontia and macrodontia of a local- Accessory cusps are commonly encoun-
ized nature are usually of no consequence. tered on the lingual surface of maxillary
Orthodontics may be required if an arch first molars as the so-called cusps of Car-
length problem develops. Crown and bridge abelli. Indeed, rudimentary forms may
prosthodontic reconstruction may help to affect as many as 90% of all such teeth in
achieve an esthetic appearance. whites, although they are extremely rare
among Eskimos and Asians. Buccal acces-
Additional Reading sory cusps are occasionally encountered on
both molars and premolars. Dens evagina-
Alsmadi O, Meyer BF, Alkuraya F, et al. Syndromic con- tus represents an accessory cusp emanat-
genital sensorineural deafness, microtia and micro- ing occlusally from the central groove of
dontia resulting from a novel homoallelic mutation in premolars and molars. This anomaly is
fibroblast growth factor 3 (FGF3). Eur J Hum Genet. rare and is most often encountered among
2009;17(1):14-21.
Bowden DE, Goose DH. Inheritance of tooth size in Eskimos. A pulp horn may extend into this
Liverpool families. J Med Genet. 1969;6:55. central occlusal cusp. Excluding the cusp
Burke RS. Megadontism and partial gemination. Oral of Carabelli, the most common accessory
Surg Oral Med Oral Pathol. 1976;42:703. cusp represents an anomalously enlarged
Gregory WA. A case of extreme microdontia. Oral Surg
Oral Med Oral Pathol. 1990;69:658. lingual tubercle on an incisor. Accessory
Hayward JR. Cuspid gigantism. Oral Surg Oral Med roots are most frequently seen on maxillary
Oral Pathol. 1980;49:500. molar teeth and secondly on mandibular
PMPH_Eversole_Chapter-11.indd 566 1/20/2011 3:12:50 PM
Dental Defects 567
FIGURE 11-11
Accessory cusps, roots, and
Dens evaginatus.
molars. Premolars and maxillary cuspids Kraus BX. Carabelli’s anomaly of the maxillary molar
and incisors may have accessory or appen- teeth. Am J Hum Genet. 1951;3:348.
Krolls SO, Donalhue AH. Double-rooted maxillary
dicial roots; however, mandibular cuspid primary canines. Oral Surg Oral Med Oral Pathol.
or incisor accessory roots are extremely 1980;49:379.
rare. Mavrodisz K, Rózsa N, Budai M, Soós A, Pap I, Tarján I.
Prevalence of accessory tooth cusps in a contemporary
and ancestral Hungarian population. Eur J Orthod.
TREATMENT 2007;29(2):166-169.Younes SA, al-Shammery AR, el-
Angbawi MF. Three-rooted permanent mandibular
Accessory cusps are rarely in occlusion so
first molars of Asian and black groups in the middle
that no treatment is required unless, in the east. Oral Surg Oral Med Oral Pathol. 1990;69:102-
case of buccal accessory cusps, periodontal 105.
pocket formation is encountered. In this
case, tooth reduction and placement of a
restoration to avoid exposure of dentin are DENTAL TRANSPOSITION
recommended. Dens evaginatus may pose Figure 11-12
a problem, because the cusps are in occlu-
sion. It must be remembered that pulp Sex: No predilection
horns extend into these areas. A knowl-
edge of the existence of accessory roots CLINICAL FEATURES
is significant when endodontic therapy is Teeth may erupt into inappropriate posi-
required. tions. A second premolar may be inter-
posed between a first and second molar, or
a cuspid may erupt into position between
Additional Reading the premolars. Although rare, a tooth may
Geist JR. Dens evaginatus. Case report and review
erupt into the opposite quadrant. Many
of the literature. Oral Surg Oral Med Oral Pathol. examples of so-called “transposition” are
1989;67:628. instances of supernumerary teeth, particu-
PMPH_Eversole_Chapter-11.indd 567 1/20/2011 3:12:59 PM
568 Chapter 11
ENAMEL PEARL
Figure 11-13
Sex: No predilection
CLINICAL FEATURES
Enamel pearls or droplets are white, dome-
shaped calcific concretions of enamel, usu-
ally located at the furcation areas of molar
teeth. Maxillary molars are most often
affected. Encountered fairly frequently,
enamel pearls probably represent a histo-
logic abnormality occurring in Hertwig’s
FIGURE 11-12
sheath. The sheath epithelium retains
Transposition of lateral incisor and canine. ameloblastic potential in a focal area so that
a nodule of enamel forms in place of cemen-
tum. Occasionally, a dentin core extends
larly in the molar region. These supernu- into the enamel-surfaced excrescence.
merary molars are small and malformed
and often show occlusal anatomy analo- TREATMENT
gous to premolars. Seventy-five percent of
transpositions involve the maxillary den- Treatment is necessary only when peri-
tition. Unilateral transposition accounts odontal disease involves a furcation area
for 88% of cases; the most common trans- with an enamel pearl. Because the region is
position involves the maxillary canine difficult to maintain in a hygienic state, the
and first premolar. Data regarding any pearl should be removed with dental burrs
genetic tendency for true transposition are or stones.
insufficient.
TREATMENT Additional Reading
If crowding and malocclusion are not sig- Cavanha AO. Enamel pearls. Oral Surg Oral Med Oral
nificant, no treatment is required. Other- Pathol. 1965;19:373.
wise, extraction and/or orthodontic therapy Chrcanovic BR, Abreu MH, Custódio AL. Prevalence
of enamel pearls in teeth from a human teeth bank.
may be indicated. J Oral Sci. 2010;52(2):257-260.
Risnes S. Ectopic tooth enamel. An SEM study of the
Additional Reading structure of enamel in enamel pearls. Adv Dent Res.
1989;3:258.
Turner JG. A note on enamel nodules. Br Dent
Abbott DM, Svirsky JA, Yarborough BH. Transposition J. 1945;78:39.
of the permanent mandibular canine. Oral Surg Oral
Med Oral Pathol. 1980;49:97.
Ely NJ, Sherriff M, Cobourne MT. Dental transposi-
tion as a disorder of genetic origin. Eur J Orthod.
DILACERATION
2006;28(2):145-151. Figure 11-14
Patel JR. Transposed and submerged teeth. Oral Surg
Oral Med Oral Pathol. 1978;46:599. Sex: No predilection
Raphael DM. Transposed supernumerary premolars.
Oral Surg Oral Med Oral Pathol. 1978;46:598. CLINICAL FEATURES
Shapira Y, Kuftinec MM. Tooth transposition—a review
of the literature and treatment considerations. Angle Dilaceration refers to a defect in root devel-
Orthod. 1989;59:271. opment, whereby a bend or curve develops.
PMPH_Eversole_Chapter-11.indd 568 1/20/2011 3:13:12 PM
Dental Defects 569
FIGURE 11-13
Molar teeth with enamel pearls.
FIGURE 11-14
Dilaceration of roots.
This flaw, which is not the result of a true procedures are performed on such anoma-
laceration of Hertwig’s sheath, probably lous teeth.
evolves subsequent to trauma or some defect
in development that alters the angulation of
the tooth germ during root formation. The
Additional Reading
angulation may occur at any location along Ligh RA. Coronal dilaceration. Oral Surg Oral Med Oral
the root. Any tooth, deciduous or perma- Pathol. 1981;51:567.
nent, may show this anomaly. Dilaceration Malcić A, Jukić S, Brzović V, Miletić I, Pelivan I, Anić I.
Prevalence of root dilaceration in adult dental patients
of the coronal portion of the tooth has also in Croatia. Oral Surg Oral Med Oral Pathol Oral
been reported. Radiol Endod. 2006;102(1):104-109.
Mattison GD, Bernstein ML, Fisher JW. Lateral root
TREATMENT dilaceration: a multi-disciplinary approach to treat-
ment. Endodout Dent Traumatol. 1987;3:135.
No treatment is required. When extraction Rengaswamy V. Bilateral dilaceration of maxillary
or endodontic therapy is necessary, knowl- central incisors. Oral Surg Oral Med Oral Pathol.
1979;47:200.
edge of this defect and its identification on Shafer WG, Hine MK, Levy BM. A Textbook of Oral
dental radiographs aids in circumventing Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
complications that could occur when these 1975.
PMPH_Eversole_Chapter-11.indd 569 1/20/2011 3:13:13 PM
570 Chapter 11
DENS INVAGINATUS (DENS IN ent; food debris with accompanying micro-
DENTE) organisms enter this canal, predisposing
Figure 11-15 the affected tooth to caries, pulp infection,
and periapical disease.
Sex: No predilection
TREATMENT
CLINICAL FEATURES
When dens invaginatus is encountered
Dens invaginatus represents a defect in mor-
shortly after eruption, prophylactic restora-
phologic development, whereby the coronal
tion of the invaginated channel is recom-
enamel and dentin become inverted into
mended to prevent pulpal necrosis.
the pulp chamber. The defect, which is gen-
erally localized to a single tooth, occasion-
ally involves multiple teeth and frequently
involves the same tooth bilaterally. The Additional Reading
coronal invagination may be limited to the Alani A, Bishop K. Dens invaginatus. Part 1: clas-
crown region, or it may extend deeply into sification, prevalence and aetiology. Int Endod J.
the radicular pulp. The defect is most often 2008;41(12):1123-1136.
encountered in the maxillary lateral inci- Burton DJ, Saffos RO, Scheffer RB. Multiple bilateral
dens in dente as a factor in the etiology of multiple
sor and in mesiodens. Clinically, the incisor periapical lesions. Oral Surg Oral Med Oral Pathol.
may manifest only an enlarged lingual pit. 1980;49:496.
The defect is easily demonstrated radio- Conklin WW. Bilateral dens invaginatus in the mandibu-
graphically as an invaginated radiopaque, lar incisor region. Oral Surg Oral Med Oral Pathol.
1978;45:905.
ribbon-like enamel structure, giving the Shafer WG. Dens in dente. NY Dent J. 1953;19:220.
impression of a small tooth within the coro- Tuzum MS, Bilge OM. Multiple dens invaginatus. Oral
nal pulp cavity. The invaginated core is pat- Surg Oral Med Oral Pathol. 1990;70:128.
FIGURE 11-15
Dens invaginatus.
PMPH_Eversole_Chapter-11.indd 570 1/20/2011 3:13:20 PM
Dental Defects 571
TAURODONTISM
Figure 11-16
Additional Reading
Sex: No predilection Crawford JL. Concomitant taurodontism and amelo-
genesis imperfecta in the American Caucasian. J Dent
CLINICAL FEATURES Child. 1970;37:83.
Holt RD, Brook AH. Taurodontism: a criterion for diag-
Taurodontism means bull teeth; the term nosis and its prevalence in mandibular first permanent
is appropriate because this human dental molars in a sample of 1,115 British school children. J
defect involves an elongated pulp chamber Int Assoc Dent Child. 1979;10:41.
with rudimentary root formation mimick- Jafarzadeh H, Azarpazhooh A, Mayhall JT. Taurodontism:
a review of the condition and endodontic treatment
ing, to some extent, the normal morphol- challenges. Int Endod J. 2008;41(5):375-388.
ogy of the ungulate dentition. The defect Mangion JJ. Two cases of taurodontism in modern human
is observable only in dental radiographs; jaws. Br Dent J. 1962;113:309.
there is no clinically obvious malformation. Seow WK, Lai PY. Association of taurodontism with hypo-
dontia: a controlled study. Pediatr Dent. 1989;11:214.
Molars are affected and give the appearance
of having been “stretched,” with the root fur-
cation occurring at the apical third. One or
more molars may show this change. Tauro-
GEMINATION
donts may be encountered in patients suffer- Figure 11-17
ing from various developmental craniofacial
Sex: No predilection
deformities. Specifically, in the trichodento-
osseous syndrome, hypoplastic-hypocal- CLINICAL FEATURES
cified amelogenesis imperfecta (AI), kinky Gemination is the result of either schizo-
hair, and cortical osteosclerosis are seen dontism, the splitting of a tooth germ
along with taurodontism. Among patients during development, or synodontism, the
with hypodontia, one third also have a tau- fusion of a normal tooth bud with one
rodont. Interestingly, similar dental mor- from a developing supernumerary tooth.
phology has been encountered among fossil Both forms represent abortive attempts at
hominoids, particularly the Neanderthals. forming supernumerary buds. The decidu-
ous mandibular incisors and permanent
TREATMENT
maxillary incisors are most often affected.
No treatment is required. The enlarged pulp Gemination may be distinguished from
chamber is of significance when endodontic fusion by the fact that the full complement
therapy is required. of teeth is present in the former, whereas
FIGURE 11-16
Taurodontism.
PMPH_Eversole_Chapter-11.indd 571 1/20/2011 3:13:29 PM
572 Chapter 11
FIGURE 11-17
Gemination.
a tooth is missing in the latter. Geminate Levitas TC. Gemination, fusion, twinning and concres-
teeth usually show doubling of both the cence. J Dent Child. 1965;32:93.
O’Carroll MK. Fusion and gemination in alternate
crown and root. The crown may be exces- dentitions. Oral Surg Oral Med Oral Pathol.
sively widened or may actually show an 1990;69:655.
indentation or groove delineating the two Tannenbaum KA, Alling EE. Anomalous tooth
crown forms. A hereditary pattern is some- development. Oral Surg Oral Med Oral Pathol.
1963;16:883.
times evident.
TREATMENT FUSION
Gemination of anterior teeth represents Figure 11-18
a prosthetic challenge. Depending on the
morphologic character of the defect, a fixed Sex: No predilection
anterior bridge may be constructed, using
CLINICAL FEATURES
the anomalous tooth as an abutment. Alter-
natively, to ensure an adequate esthetic Fusion represents a junction at the level of
result, the affected teeth are extracted and dentin between juxtaposed normal tooth
the cuspids are used as abutments. germs, so that one enlarged anomalous
crown form exists in place of two normal
teeth. A single, enlarged root or two roots
Additional Reading are observed. A hereditary pattern is often
encountered. Either deciduous or perma-
Clayton JM. Congenital dental anomalies occurring in nent teeth can be affected; however, the
3,557 children. J Dent Child. 1956;23:206.
Kremeier K, Pontius O, Klaiber B, Hülsmann M.
anomaly has been reported to be more com-
Nonsurgical endodontic management of a double mon in deciduous teeth. In both dentitions,
tooth: a case report. Int Endod J. 2007;40(11):908-915. the incisors are most often affected.
PMPH_Eversole_Chapter-11.indd 572 1/20/2011 3:13:32 PM
Dental Defects 573
FIGURE 11-18
Fusion.
FIGURE 11-19
Concrescence in molar
teeth.
TREATMENT Onçag O, Candan U, Arikan F. Comprehensive ther-
apy of a fusion between a mandibular lateral inci-
Depending on the morphologic features sor and supernumerary tooth: case report. Int Dent
of the fused teeth, a fixed prosthetic appli- J. 2005;55(4):213-216.
ance may include the anomalous tooth as
an abutment, or the tooth may be extracted
with subsequent bridge fabrication to CONCRESCENCE
achieve optimal esthetics. Figure 11-19
Sex: No predilection
Additional Reading CLINICAL FEATURES
Concrescence represents union between jux-
Clayton JM. Congenital dental anomalies occurring in
3,557 children. J Dent Child. 1956;23:206.
taposed teeth at the level of the cementum;
Eidelman E. Fusion of maxillary primary cen- there is no interdentinal combination. The
tral and lateral incisors bilaterally. Pediatr Dent. maxillary molars are usually affected by this
1981;3:346. developmental abnormality. Confluency of
Maibaum WW. Fusion or confusion? Oral Surg Oral
Med Oral Pathol. 1990;69:657.
cementum between adjacent teeth may occur
Moody E, Montgomery LB. Hereditary tendencies in with two normal molars, yet is perhaps more
tooth formation. J Am Dent Assoc. 1934;21:1774. often encountered between a normal molar
PMPH_Eversole_Chapter-11.indd 573 1/20/2011 3:13:42 PM
574 Chapter 11
and a supernumerary molar (i.e., paramolar Normal occlusal attrition has been calcu-
or distomolar). Concrescence may occur in lated at 30 μm/year for molar teeth. The
both impacted and erupted teeth. process is related to diet, and is more severe
in individuals who partake of a food such as
TREATMENT maize or use their teeth in the preparation
Concrescent teeth are either in malocclusion of hides. It is, therefore, common among
or impacted, usually necessitating extrac- older American Indians and Eskimos.
tion. If such a condition is suspected from Tooth wear has been correlated with ero-
radiographic features, care during extrac- sive degenerative changes in the temporo-
tion is necessary, particularly to avoid frac- mandibular joint among aboriginals. It may
turing excessive amounts of alveolar bone. be difficult to differentiate between attrition
and bruxism with abrasion by noting only
the pattern of tooth wear.
Additional Reading TREATMENT
Gernhofer KJ. Concrescence of a maxillary second
and third molar. J Calif Dent Assoc. 2009;37(7):479- No treatment is required as secondary den-
481. tin proceeds at a rate commensurate with the
Levitas TC. Gemination, fusion, twinning and concres- attritional wear. When the crowns are worn
cence. J Dent Child. 1965;32:93.
Schulze C. Developmental abnormalities of the teeth and
down to the gingival margin, an overdenture
the jaws. In RJ Gorlin, HM Goldman, eds. Thoma’s may be constructed to improve function.
Oral Pathology, Vol. I. 6th ed. St. Louis, MO: C.V.
Mosby; 1970:121.
Additional Reading
ATTRITION Goldman HM. An atlas of acquired dental defects.
Figure 11-20 Compend Cont Educ Dent. 1982;3:275.
Kreulen CM, Van’t Spijker A, Rodriguez JM, Bronkhorst
EM, Creugers NH, Bartlett DW. Systematic review of
Age: Adults, particularly elderly people
the prevalence of tooth wear in children and adoles-
Sex: No predilection cents. Caries Res. 2010;44(2):151-159.
Lambrechts P, Braem M, Vuylsteke-Wauters M, Vanherle
CLINICAL FEATURES
G. Quantitative in vivo wear of human enamel. J Dent
Attrition represents the physiologic loss Res. 1989;68:1752.
of tooth structure. The pattern of loss is Richards LC, Brown T. Dental attrition and degenera-
tive arthritis of the temporomandibular joint. J Oral
characteristic in that the enamel and den- Rehabil. 1981;8:293.
tin become abraded on their occlusal and Sicher H. The biology of attrition. Oral Surg Oral Med
incisal surfaces in a generalized fashion. Oral Pathol. 1953;6:406.
FIGURE 11-20
Physiologic tooth wear or attrition.
PMPH_Eversole_Chapter-11.indd 574 1/20/2011 3:13:47 PM
Dental Defects 575
FIGURE 11-21
Pathologic tooth wear or abrasion.
ABRASION TREATMENT
Figure 11-21 Limited forms of abrasion require elimina-
tion of the incriminating habit and restora-
Age: Adults tion of normal tooth contour if function or
Sex: No predilection esthetics is a problem. Abrasion related to
CLINICAL FEATURES malocclusion may require occlusal reha-
bilitation and a complete periodontal evalu-
Abrasion represents the pathologic wear ation. Night-guard appliances may limit
of tooth structure. The location of tooth abrasion in patients with bruxism.
structure loss is in keeping with the nature
of the etiology or habit responsible for
excessive abrasion. Notching of incisors is Additional Reading
seen in hairdressers who hold bobby pins
Ervin JC, Bucher EM. Prevalence of tooth root expo-
between their teeth; grooving of both max- sure and abrasion among dental patients. Dent Items
illary and mandibular incisors is observed Interest. 1944;66:760.
in pipe smokers; cervical abrasion occurs Goldman HM. An atlas of acquired dental defects.
in individuals who brush excessively in a Compend Cont Educ Dent. 1982;3:275.
Harrington JH, Terry IA. Automatic and hard tooth brush-
horizontal plane. In the last instance, pulp ing abrasion studies. J Am Dent Assoc. 1964;68:343.
exposure may ensue. Isolated foci of abra- Koksal T, Dikbas I, Kazaoglu E. Alternative restorative
sion are observed in patients with occlusal approach for treatment of patient with extremely worn
prematurities appearing as cuspal wear fac- dentition. N Y State Dent J. 2009;75(5):52-55.
Oilo G, Hatle G, Gad AL, Dahl BL. Wear of teeth in
ets. A common occlusal anomaly leading to
a mentally retarded population. J Oral Rehabil.
widespread abrasion occurs in patients who 1990;17:173.
show incisal guided protrusive movement.
The incisal portion of the mandibular inci-
sors shows abrasion, as do the incisal and EROSION
lingual surfaces of the maxillary incisors Figure 11-22
and cuspids. It is important to recognize
that abrasion related to occlusal dishar- Age: Adult predilection
mony may be associated with advancing Sex: No predilection
periodontal disease about the affected
CLINICAL FEATURES
teeth. Patients with bruxism display gen-
eralized abrasion that mimics physiologic Erosion represents the demineralization of
attrition in its distribution. Pathologic tooth tooth structure as a result of chemical action,
wear has been found to be prevalent among usually that of acidic compounds. Although
mentally retarded patients. a definite history of oral contact with acids
PMPH_Eversole_Chapter-11.indd 575 1/20/2011 3:13:51 PM
576 Chapter 11
FIGURE 11-22
Idiopathic erosion of facial enamel.
Lingual erosion in anorexia
nervosa/bulimia with chronic
vomiting.
can be elicited in most instances, occasion- House RC, Grisius R, Bliziotes MM, Licht JH.
ally a cause is not readily apparent. The Perimolysis: unveiling the surreptitious vomiter. Oral
Surg Oral Med Oral Pathol. 1981;51:152-155.
more common agents associated with ero- Stege P, Visco-Dangler L, Rye L. Anorexia nervosa:
sion are chronic vomiting, habitual carbonic review including oral and dental manifestations. J Am
acid intake from cola or soft drinks, or habit- Dent Assoc. 1982;104:648.
ual contact with citric acid as in lemon suck- Wang X, Lussi A. Assessment and management of
dental erosion. Dent Clin North Am. 2010;54(3):565-
ing. When vomiting is the cause, a smooth 578.
homogeneous loss of enamel with exposure
of dentin is observed on the lingual sur-
faces. Both facial and lingual loss of surface HYPERCEMENTOSIS
tooth structure can be seen in persons who
Figure 11-23
imbibe acidic fruits or beverages. Idiopathic
erosion occurs on the cervical and middle Age: Middle-aged and elderly adults
thirds of the incisors, cuspids, and bicuspids Sex: No predilection
as a smooth cupped-out depression.
CLINICAL FEATURES
TREATMENT Excessive deposition of secondary cemen-
Areas of erosion may be sensitive and tum may develop on one tooth or may be
should be restored with conventional oper- generalized. Generally no cause can be
ative procedures. found; occasionally, contributing factors
can be detected (periapical inflammation
and hypofunction as seen when an oppos-
Additional Reading ing tooth is missing). Pain is not a feature.
The roots show laminated layers of second-
Allan DN. Enamel erosion with lemon juice. Br Dent J. ary cementum, usually of the lamellar type,
1967;122:300.
Grobler SR, Senekal PJ, Kotze TJ. The degree of enamel
which is most extensive in the apical third
erosion by five different kinds of fruit. Clin Prev Dent. of the root. The radiographic features are
1989;11:23. characteristic, showing bulbous enlarged
PMPH_Eversole_Chapter-11.indd 576 1/20/2011 3:13:56 PM
Dental Defects 577
FIGURE 11-23
Hypercementosis.
roots. Generalized hypercementosis may
occur alone or may be seen in conjunction Alterations in Structure
with a ground-glass or cotton-wool-appear-
ing alveolar bone in osteitis deformans. DENTAL CARIES
A serum alkaline phosphatase assay is Figure 11-24
helpful.
Sex: No predilection
TREATMENT CLINICAL FEATURES
No treatment is required. Extraction of teeth Dental caries represents the most common
with hypercementosis may require section- disease to affect the teeth. Most evidence
ing to facilitate removal. supports a bacterial etiology, whereby teeth
accumulate material known as plaque that
provides a carbohydrate substrate for acid-
producing bacteria, primarily Streptococcus
Additional Reading mutans. Acid generation induces a chemi-
Gardner BS, Goldstein H. The significance of hyperce- cal demineralization of hydroxyapatite
mentosis. Dent Cosmos. 1931;73:1065. crystals in the enamel. When the enamel
Humerfelt A, Reitan K. Effects of hypercementosis on has been penetrated, other microorgan-
the movability of teeth during orthodontic treatment. isms gain access to the protoplasm of the
Angle Orthodont. 1966;6:179.
Leider AS, Garbarino VE. Generalized hyperce- dentinal tubules, and the carious process
mentosis. Oral Surg Oral Med Oral Pathol. proceeds pulpally. Once the pulp has been
1987;63:375. invaded by bacteria, inflammation ensues;
Seed R, Nixon PP. Generalised hypercementosis: a case ultimately, necrosis with spread of infec-
report. Prim Dent Care. 2004;11(4):119-122.
Weinberger A. The clinical significance of
tion occurs through the apical foramen or
hypercementosis. Oral Surg Oral Med Oral Pathol. accessory root canals. In children, pits and
1954;7:79. fissures are the most common sites along
PMPH_Eversole_Chapter-11.indd 577 1/20/2011 3:14:16 PM
578 Chapter 11
FIGURE 11-24
Dental caries. Upper right:
crystal meth caries in an
addict who consumes
sugar drinks and candy
while stoned. Middle right:
post radiation therapy
caries associated with
xerostomia.
with interproximal areas. Clinically, pit and caries occurs in children who eat exces-
fissure caries is characterized by either a sive amounts of candy and other sweets. In
chalky appearance or a brown discoloration. adults, severe caries occurs in xerostomia
A sharp dental explorer can be forced into secondary to the Sjögren’s syndrome or
a carious fissure or pit and will be retained, after radiation therapy for head and neck
requiring somewhat forceful removal. Inter- cancer.
proximal caries can often be detected as pits
or irregularities on instrument exploration; TREATMENT
however, bite-wing radiographs are the All carious enamel and dentin must be
major diagnostic aid. Immediately below removed before restoration with amalgam,
the point of tooth-to-tooth contact, a funnel- cast gold, or resin materials. Pit and fissure
shaped radiolucency can be detected with its sealants effectively prevent dental decay
apex directed toward the dentin. Dentinal among children. Patients with xerostomia
caries also appears triangular and under- from immunopathic sialadenitis or radiation
mines the overlying intact enamel. Cervical should be treated with daily fluoride gel.
and root caries on the facial or buccal gin-
gival one third of the crown are more fre-
quently encountered among adults. It may Additional Reading
involve cementum and extend below the
Beck J. The epidemiology of root surface caries. J Dent
marginal gingiva. Cervical caries begins as Res. 1990;69:1216.
white opaque areas that become discolored Darling AI. The pathology and prevention of caries. Br
brown or yellow-brown. Severe or rampant Dent J. 1959;107:287.
PMPH_Eversole_Chapter-11.indd 578 1/20/2011 3:14:41 PM
Dental Defects 579
FIGURE 11-25
Turner’s hypoplasia of
centrals. Enamel pitting
occurs in teeth at the
same stage of odontogen-
esis when a stressor on
the enamel organ occurs
during development.
Frank RM, Herdly J, Philippe E. Acquired dental defects yellow or brown, and the enamel surface is
and salivary gland lesions after irradiation for carcino- pitted or chalky. Occasionally, many teeth
ma. J Am Dent Assoc. 1965;70:868-883.
Losee FL. Dental caries in abutting or bilaterally corre- show pitting or rough, poorly calcified
sponding tooth surfaces. J Am Dent Assoc. 1947;35:323. enamel matrices. In these instances, one of
Savara BS, Suher T. Study of dental caries in children 1 the childhood infectious diseases associ-
to 6 years of age as related to socioeconomic level and ated with prolonged elevated temperature
food habits. J Dent Res. 1953;32:680.
may have resulted in ameloblastic injury,
in which case only that portion of the teeth
ENAMEL HYPOPLASIA under development at the time of infection
Figure 11-25 manifests hypoplastic changes. Children of
low birth weight have a high incidence of
Sex: No predilection enamel hypoplasia, which may be a conse-
CLINICAL FEATURES quence of oxygen deprivation and mineral
depletion during perinatal development.
Damage to ameloblasts during odontogen- Enamel hypoplasia with a similar distri-
esis, if severe, results in defective enamel bution as that seen with febrile childhood
formation. A variety of infectious, nutri- infections may occur in rickets, congenital
tional, chemical, and traumatic factors play hypoparathyroidism, and birth injuries.
a role. (Because of their unique characters, Enamel defects have been reported to be a
congenital syphilis and dental fluorosis are common accompaniment to celiac disease.
considered separately). Perhaps, the most
common form of enamel hypoplasia is seen
TREATMENT
in isolated permanent teeth, whereby car-
ies with periapical spread of infection or When the pulp chambers have receded to
trauma to a deciduous tooth results in dam- an appropriate level, permanent restorations
age to ameloblasts forming the crown of the may be fabricated. In the interim, resin restor-
subjacent developing permanent tooth. The ative materials may be periodically placed
affected tooth, so-called Turner’s tooth, is to achieve a desirable esthetic appearance.
PMPH_Eversole_Chapter-11.indd 579 1/20/2011 3:14:45 PM
580 Chapter 11
infection. The clinical manifestations are
Additional Reading protean, as the infection may involve virtu-
Aine L, Mäki M, Collin P, Keyriläinen O. Dental ally any tissue or organ, particularly bone,
enamel defects in celiac disease. J Oral Pathol Med. tooth, and nerve. Saber shins, rhagades,
1990;19:241. frontal bossing, and saddle nose are com-
Fearne JM, Bryan EM, Elliman AM, Brook AH, Williams mon structural anomalies. Hutchinson’s
DM. Enamel defects in the primary dentition of
children born weighing less than 2000 g. Br Dent J. triad consists of blindness, deafness, and
1990;168:433-437. dental anomalies. The classic dental changes
Morningstar CH. Effect of infection of deciduous molar involve the maxillary incisors and first per-
on the permanent tooth germ. J Am Dent Assoc. manent molars. The central incisors are
1937;24:786.
Porteous JR. Appearance of chronologic hypoplasia. Oral
notched, the laterals are peg shaped, and
Surg Oral Med Oral Pathol. 1979;48:282. the molars manifest a crumpled, discolored
Shelling DH, Anderson GM. Relation of rickets and vita- occlusal surface (so-called mulberry molars).
min D to the incidence of dental caries, enamel hyp- Not all patients manifest all components of
oplasia and malocclusion in children. J Am Dent Assoc.
1936;23:840.
Hutchinson’s triad, nor do they all show the
Via WF Jr. Enamel defects induced by trauma during three dental anomalies together. The fact
tooth formation. J Oral Maxillofac Surg. 1968;25:49. that children with congenital syphilis may
continue to carry spirochetes, may be infec-
tious, and may show any of the signs of
CONGENITAL SYPHILIS
acquired syphilis is extremely important.
Figure 11-26
TREATMENT
Sex: No predilection
Children should be referred to a pediatri-
CLINICAL FEATURES
cian to determine whether or not active dis-
Congenital syphilis is contracted in utero ease persists. The anomalous teeth may be
from a mother who has active treponemal restored by the usual operative procedures.
FIGURE 11-26
“Screwdriver” centrals
and “mulberry” molars in
congenital syphilis.
PMPH_Eversole_Chapter-11.indd 580 1/20/2011 3:14:53 PM
Dental Defects 581
FIGURE 11-27
Fluorosis prior to age 1
resulting in discoloration
and chalky enamel.
teeth, deciduous or permanent, vary con-
Additional Reading siderably regarding the extent of hypopla-
Brauer JC, Blackstone CH. Dental aspects of congenital sia. The surface may be chalky, opaque, and
syphilis. J Am Dent Assoc. 1941;28:1633. flecked, or the enamel may show extensive
Fiumara NJ, Lessell S. Manifestations of late congenital flaking, fracturing, and brown or black pig-
syphilis. Arch Dermatol. 1970;102:78. mentation. The condition is generalized,
Putkonen T. Dental changes in congenital syphilis. Acta
Derm Venereol (Stockh). 1962;42:44. affecting all teeth exposed to excess fluoride
Sarnat BG, Shaw NG. Dental development in congenital during development.
syphilis. Am J Orthodont. (Oral Surg. Sect). 1943;29:270.
TREATMENT
No treatment can remineralize the defec-
DENTAL FLUOROSIS tive surface. Temporary resin restorations
should be employed during childhood, and
Figure 11-27
full-coverage fixed prostheses can be fabri-
Sex: No predilection cated after the pulp chamber has sufficiently
receded. Treatment is elective because the
CLINICAL FEATURES teeth are not any more susceptible to decay
When fluoride levels in the drinking water than the normal dentition.
exceed 1 ppm, mottling of enamel may occur.
Certain regions of the world have natural
drinking water supplies in which the fluo- Additional Reading
ride content is extremely high. Fluoride in
Black GV, McKay FA. Mottled teeth: an endemic devel-
concentrated levels is toxic to ameloblasts; opmental imperfection of the enamel of teeth here-
during amelogenesis, cell damage leads to tofore unknown in the literature of dentistry. Dent
defective enamel formation. The affected Cosmos. 1916;58:129.
PMPH_Eversole_Chapter-11.indd 581 1/20/2011 3:14:59 PM
582 Chapter 11
FIGURE 11-28
Opaque regions on incisal one third of maxillary central incisors and cuspids representing snow-capped
teeth.
Dean HT, Arnold FA. Endemic dental fluorosis or mot- studies indicate a structural defect in the
tled teeth. J Am Dent Assoc. 1943;30:1278. outer prismless enamel layer.
Dean HT. Chronic endemic fluorosis. J Am Med Assoc.
1936;107:1269.
McClure FS, Lipkins RC. Fluorine in human teeth stud- TREATMENT
ied in relation to fluorine in the drinking water. J Dent
No treatment is required.
Res. 1951;30:172.
Pendrys DG, Stamm JW. Relationship of total fluo-
ride intake to beneficial effects and enamel fluorosis.
J Dent Res. 1990;69:529-556. Additional Reading
Escobar VH, Goldblatt LI, Bixler D. A clinical, genetic
and ultrastructural study of snow-capped teeth: amelo-
SNOW-CAPPED TEETH genesis imperfecta, hypomaturation type. Oral Surg
Figure 11-28 Oral Med Oral Pathol. 1981;52:607.
Winter GB, Brook AH. Enamel hypoplasia and anoma-
Sex: No predilection lies of the enamel. Dent Clin North Am. 1975;19:3.
Witkop CJ Jr, Sauk JJ Jr. Heritable defects of enamel. In
CLINICAL FEATURES Stewart RE, Prescott, GH, eds. Oral Facial Genetics.
St. Louis, MO: C. V. Mosby; 1976: 187.
This autosomal dominantly inherited dis- Witkop CJ Jr. Heterogeneity in inherited dental tracts,
order is relatively common. The incisors, gingival fibromatosis and amelogenesis imperfecta.
cuspids, and occasionally even posterior South Med J. 1971;64(suppl. 1):16.
Witkop CJ Jr. Snow-capped teeth (marker). In Bergsma
teeth manifest a white, chalky opaque dis- D, ed. Birth Defects Atlas and Compendium, The
coloration of the incisal and occlusal third National Foundation. Baltimore, MD: Williams and
of the crown. This opacified region of the Wilkins; 197: 812.
enamel reflects an anomaly of mineraliza-
tion; however, the involved hard tissue is
neither structurally weakened nor more AMELOGENESIS IMPERFECTA,
susceptible than normal tooth structure HYPOPLASTIC TYPES
to caries. Recently, a rare X-linked form of
Figure 11-29
snow-capped teeth has been described and
has been classified as a form of AI, hypoma- Sex: Predilection varies according to mode of
turation type. This form resembles the com- inheritance.
mon variety in that the incisal one third of
CLINICAL FEATURES
the teeth exhibit an opaque appearance; it
differs in that a brownish discoloration also The amelogenin gene encodes for enamel
is observed. Scanning electron microscopic matrix protein and is probably heritably
PMPH_Eversole_Chapter-11.indd 582 1/20/2011 3:15:08 PM
Dental Defects 583
FIGURE 11-29
Amelogenesis imperfecta,
smooth hypoplastic type,
no incisal flare, no enamel
seen radiographically.
Lower right: amelogenesis
imperfecta, local hypoplas-
tic type showing midcoro-
nal pitting.
defective in the various forms of AI. Two being smooth and approximately one fourth
major forms of AI exist; the hypoplastic normal thickness; clinically, newly erupted
types exhibit a deficient amount of surface teeth are yellow and later appear opaque
enamel, whereas the hypomaturation forms white or slightly brown. Radiographically,
show adequate enamel thickness with the teeth may appear to be devoid of enamel.
defective mineralization. This subdivision The autosomal dominant rough hypoplastic
is often confusing because both hypoplastic form is represented by hard granular white
and hypomineralized enamel may coexist. or yellow-white enamel, one fourth normal
The hypoplastic forms have been subcat- thickness, that chips away from the under-
egorized according to clinical, microscopic, lying dentin. There is some degree of incisal
and genetic features. This group has the fol- flare. Radiographically, the enamel layer
lowing general features. The enamel is thin, is readily identified, yet extremely thin. In
teeth fail to evince mesiodistal contacts, and contrast, the autosomal recessive rough hyp-
pitting or fissuring, either horizontal or ver- oplastic type is nearly devoid of enamel and
tical, occurs. The autosomal dominant pitted is also termed enamel agenesis. The surface
hypoplastic variety affects both primary and exhibits a granular, ground-glass appear-
secondary dentitions that manifest multiple ance and a yellow discoloration. Impaction
pinpoint pits randomly distributed over the with resorption is frequently witnessed.
crowns. Autosomal dominant local hypoplastic Last, X-linked dominant smooth hypoplastic AI
AI is characterized by horizontal rows of varies according to sex. Hemizygous males
pits located on the middle one third of the show smooth yellowish-brown thin enamel
crown; the immediately adjacent enamel with significant abrasion; a thin opaque
is hypocalcified, and the occlusal third is enamel capping is observed radiographi-
usually unaffected. The autosomal dominant cally. Female heterozygotes show vertically
smooth hypoplastic form is devoid of pits, banded fissures, alternating with enamel
PMPH_Eversole_Chapter-11.indd 583 1/20/2011 3:15:15 PM
584 Chapter 11
striations of normal thickness (Lyonization Weinman JP, Svoboda JR, Woods RW. Disturbances of
effect). These vertical striae are radiographi- enamel formation and calcification. J Am Dent Assoc.
1945;32:397.
cally evident. In all forms of AI, there is a Witkop CJ Jr, Rao S. Inherited defects of tooth structure.
tendency for development of anterior open Birth Defects Orig Artic Ser. 1971;11:153-184.
bite. In families with an X-linked form, Witkop CJ Jr, Sauk JJ Jr. Heritable defects of enamel. In
it has been shown that the disorder may Stewart RE, Prescott GH, eds. Oral Facial Genetics.
St. Louis, MO: C. V. Mosby; 1976: 151.
result from mutations in the amelogenin
gene, AMELX. The enamelin gene, ENAM,
is implicated in the pathogenesis of the
dominant forms of AI. AMELOGENESIS IMPERFECTA,
HYPOMATURATION/
TREATMENT HYPOCALCIFICATION TYPES
Full crown prostheses are recommended Figure 11-30
for esthetic reasons and to eliminate sen-
Age: Infants
sitivity. Dentitions affected by AI are not
Sex: Predilection varies according to mode of
inherently caries prone. inheritance.
CLINICAL FEATURES
Additional Reading Hypomaturation and hypocalcification
forms of AI exhibit normal enamel thick-
Crawford PJ, Aldred M, Bloch-Zupan A. Amelogenesis ness with mesiodistal contacts, yet are
imperfecta. Orphanet J Rare Dis. 2007;2:17.
Lau EC, Slavkin HC, Snead ML. Analysis of human
poorly mineralized, mottled, discolored,
enamel genes: insights into genetic disorders of enam- and tend to show chipping of enamel away
el. Cleft Palate J. 1990;27:121. from the dentin. The hypocalcified enamel
FIGURE 11-30
Amelogenesis imperfecta, pigmented hypomaturation type.
PMPH_Eversole_Chapter-11.indd 584 1/20/2011 3:15:20 PM
Dental Defects 585
is no more radiodense than dentin, hav- mize calculus deposition, which would other-
ing a higher protein content than normal wise predispose to periodontal inflammation.
enamel. Autosomal dominant hypocalcified
AI is the most common form, occurring
once in every 20,000 births. The enamel Additional Reading
is normal in thickness yet is soft, cheesy, Crawford PJ, Aldred M, Bloch-Zupan A. Amelogenesis
and crumbly, and is penetrable with a imperfecta. Orphanet J Rare Dis. 2007;2:17.
dental explorer. Newly erupted teeth are Sauk JJ Jr, Lyon HW, Witkop CJ Jr. Electron optic
without luster and are opaque white or microanalysis of two gene products in enamel of
females heterozygous for X-linked hypomatura-
orange. The enamel wears away rapidly, tion amelogenesis imperfecta. Am J Hum Genet.
and calculus deposition is often a striking 1972;24:267.
feature. Radiographically, multiple moth- Witkop CJ Jr, Sauk JJ Jr. Heritable defects of enamel. In
eaten foci are observed over the crowns. Stewart RE, Prescott GH, eds. Oral Facial Genetics.
St. Louis, MO: C. V. Mosby; 1976: 151.
An autosomal dominant hypomaturation-hy-
Witkop CJ Jr, Kuhlmann W, Sauk JJ Jr. Autosomal
poplastic form of AI occurs in conjunction recessive pigmented hypomaturation amelogen-
with taurodontism, which may represent esis imperfecta. Oral Surg Oral Med Oral Pathol.
a variation of expressivity of the tricho- 1973;36:367.
dento-osseous syndrome (see Syndrome- Wright JT, Butler WT. Alteration of enamel proteins in
hypomaturation amelogenesis imperfecta. J Dent Res.
Associated Enamel Defects). X-linked reces- 1989;68:1328.
sive hypomaturation AI affects both primary
and adult dentitions. Males show more
severe changes. The permanent teeth are SYNDROME-ASSOCIATED
nearly normal in thickness and are in con- ENAMEL DEFECTS
tact, yet are yellowish-brown and mottled. Figure 11-31
The cervical collar is minimally involved.
In females, wavy vertical banding is seen Sex: Predilection varies according to mode of
and has the appearance of dripping wax. inheritance.
These striae are not seen radiographically. CLINICAL FEATURES
Autosomal recessive pigmented hypomatura-
tion AI affects both primary and adult den- A vast number of rare syndromes have been
titions. Although thickness approaches described in which dental anomalies have
normalcy, the enamel chips, particularly been observed. Some of these syndromes
around restorations, and is brown. The show enamel defects as the sole dental
incisal and occlusal surfaces are usually anomaly; others affect enamel as well as
eroded. These teeth tend to accumulate other dental tissues. Epidermolysis bullosa
calculus that fluoresces red-violet. Radio- occurs in at least four genetic forms and is
graphically, the enamel layer is poorly a bullous disease of skin and mucous mem-
defi ned. In families with an X-linked form, branes. Dental defects are observed in some
it has been shown that the disorder may of these forms and consist of thin hypoplas-
result from mutations in the amelogenin tic enamel with random pitting, yielding a
gene, AMELX. The enamelin gene, ENAM, honeycomb pattern. The mucopolysacchari-
is implicated in the pathogenesis of the doses (MPS) are heritable diseases of defec-
dominant forms of AI. tive mucopolysaccharide metabolism. In
type IV, Morquio’s syndrome, the enamel is
hypoplastic with pointed peak-like cusp tips.
TREATMENT
The teeth are grey and pitted, and the pits
Full coverage prostheses are indicated for tend to be vertically oriented. The teeth in
esthetic reasons. In addition, full crowns mini- type III, Sanfilippo’s syndrome, exhibit loss
PMPH_Eversole_Chapter-11.indd 585 1/20/2011 3:15:26 PM
586 Chapter 11
FIGURE 11-31
A variety of syndromes are
associated with hypodon-
tia and defective enamel.
of enamel with excessive and defective den- Taurodontism is a feature, and many of
tinogenesis, yielding radiographic evidence the teeth remain unerupted. In vitamin D
of pulp obliteration. In tuberous sclerosis, lin- refractory rickets, the incisal or occlusal one
ear enamel pits may pock the facial enamel third is hypoplastic with granular enamel.
surfaces; these pits are usually apparent as The pulp chambers are large and pulp
punctate radiolucencies. Oculodento-osseous horns extend to the dentinoenamel junc-
dysplasia is characterized by microphthal- tion. Pseudohypoparathyroidism exists in two
mus, iridal anomalies, bony anomalies of forms. In both forms, parathyroid hormone
the digits and syndactyly, thickened man- levels are intact; however, there is an inabil-
dibular bone, and enamel hypoplasia. The ity to eliminate phosphate through the
teeth show large multifocal hypoplastic kidneys. Males are more severely affected
defects and pitting, yielding a moth-eaten in this X-linked disease. Features include
pattern radiographically. Oculodentodigital round facies, short neck, short fourth meta-
dysplasia is a subvariant of the former disor- carpals, falx cerebri and basal ganglia cal-
der and involves mutations in the Connexin cifications, and hypocalcemia with tetany.
43 gene (GJA1). The syndrome is character- In addition, isolated secondary teeth, usu-
ized by abnormal facial features, central ally molars and premolars, show pitted
nervous system involvement, syndactyly enamel defects, are wedge shaped, and
and clinodactyly of fourth and fifth fingers, have short roots with wide root canals and
dry and lusterless hair, generalized enamel open apices. In the odontogenic fibroma-
hypoplasia, and odontodysplasia. In the like hamartoma/enamel hypoplasia syn-
amelo-onychohypohidrotic syndrome, defective drome, enlarged pericoronal follicles are
nails with subungual hyperkeratosis are seen around unerupted molars and enamel
seen in conjunction with sweat gland hypo- resembles that of AI.
function, seborrheic dermatitis, and severe
hypoplastic-hypocalcified enamel. Many TREATMENT
resorbing unerupted teeth are observed in The dental defects included here are all
this syndrome. characterized by enamel hypoplasia with
The trichodento-osseous syndrome also pitting, and can be restored with full
shows enamel defects in conjunction with crowns.
morphologic dental anomalies. These
patients have tightly curled, kinky hair,
with osteosclerosis of bone cortices. The Additional Reading
enamel is hypoplastic and hypocalcified, Aminabadi NA, Ganji AT, Vafaei A, Pourkazemi M,
lacking mesiodistal contact with pitting. Oskouei SG. Oculodentodigital dysplasia: disease
PMPH_Eversole_Chapter-11.indd 586 1/20/2011 3:15:26 PM
Dental Defects 587
spectrum in an eight-year-old boy, his parents and a DENTINOGENESIS
sibling. J Clin Pediatr Dent. 2009;33(4):337-341.
Arwill T, Bergenholtz A, Olsson O. Epidermolysis bullo- IMPERFECTA
sa hereditaria. III. A histologic study of the teeth in the Figure 11-32
polydysplastic, dystrophic, and lethal forms. Oral Surg
Oral Med Oral Pathol. 1965;19:723. Sex: No predilection
Crawford PJ, Alfred MJ. Amelogenesis imperfecta with
taurodontism and the trichodentoosseous syndrome:
CLINICAL FEATURES
separate conditions or a spectrum of disease? Clin
Genet. 1990;38:44. Dentinogenesis imperfecta is inherited
Croft LK, Witkop CJ Jr, Glas JE. Pseudohypop- as an autosomal dominant trait and is
arathyroidism. Oral Surg Oral Med Oral Pathol.
1965;20:758. occasionally associated with osteogenesis
Gorlin RJ, Meskin LH, Geme JW. Oculo-dento-digital imperfecta (OI) with blue sclera. Not all OI
dysplasia. J Pediatr. 1963;63:69. syndromes are associated with dentinal
Hoff M, van Grunsven MF, Jongebloed WL, Gravenmade defects. Furthermore, there is no correla-
EJ. Enamel defects associated with tuberous sclerosis:
a clinical and scanning-electronmicroscope study. Oral tion between dentinogenesis imperfecta
Surg Oral Med Oral Pathol. 1975;40:261. and severity of the osseous diseases in OI;
Levin LS, Jorgenson RJ, Salinas CF. Oral findings in the rather, it appears that OI pedigrees either
Morquio syndrome (mucopolysaccharidosis IV). Oral consistently exhibit dentinogenesis imper-
Surg Oral Med Oral Pathol. 1975;39:390.
Witkop CJ Jr, Brearley LJ, Gentry WC Jr. Hypoplastic
fecta or show no evidence of heritable
enamel, onycholysis, and anhidrosis inherited as an dental disease. Dentinogenesis imperfecta
autosomal dominant trait: a review of ectodermal dys- without associated osseous disease is
plasia syndromes. Oral Surg Oral Med Oral Pathol. encountered more frequently than OI-as-
1975;39:71.
Wright JT. Epidermolysis bullosa: dental and anesthetic
sociated disease. Both deciduous and per-
management of two cases. Oral Surg Oral Med Oral manent dentitions are affected. The teeth
Pathol. 1984;57:155. show a yellowish to blue-gray opalescent,
FIGURE 11-32
Dentinogenesis imper-
fecta with opalescent
teeth, which are subject
to enamel fragmentation
and advanced abrasion.
Radiographs show oblit-
eration of root canals.
PMPH_Eversole_Chapter-11.indd 587 1/20/2011 3:15:30 PM
588 Chapter 11
polished appearance. The defective dentin Bixler D. Heritable disorders affecting dentin. In Stewart
pervades both the coronal and radicular RE, Prescott, GH, eds. Oral Facial Genetics. St. Louis,
MO: C. V. Mosby; 1976: 230.
regions. A severe form of dentinogenesis Heys FM, Blattner RJ, Robinson HBG. Osteogenesis
imperfecta was first described in a trira- imperfecta and odontogenesis imperfecta: clinical
cial isolate group in Maryland. Opalescent and genetic aspects in eighteen families. J Pediatr.
bell-shaped crowns are seen; radiographi- 1960;56:234.
Levin LS. The dentition in the osteogenesis imperfecta
cally, dentin is rudimentary with large pulp syndromes. Clin Orthop. 1981;159:65.
chambers (shell teeth, Brandywine type, Sauk JJ. Molecular basis among hereditary dentinal
Shields type III). Originally it was thought defects: pathobiology of dentinal phosphophoryn.
that a defective dentinoenamel junction Birth Defects. 1989;25:7.
was extant; scanning electron microscopic
studies have disclosed a normal junction. OSTEOGENESIS IMPERFECTA
There is a propensity for enamel loss, and
Figure 11-33
the cleavage of enamel likely occurs within
defective dentin underlying the dentinoe- Sex: No Predilection
namel junction. The exposed dentin rap-
idly abrades in many instances so that the OI is a genetic disease involving mutations
coronal surface may fail to extend beyond in collagen that have great impact on osteo-
the gingival crest. Radiographically, the genesis. There are numerous variants of the
cervix region is constricted, the roots disorder, one of which is associated denti-
are spiked, and the pulp chambers and nogenisis imperfecta type I. Fractures are
root canals manifest calcific obliteration. the most problematic aspect of the disease
Because dentinal tubules are haphazardly and may occur without traumatic provoca-
arranged and often devoid of odontoblas- tion. Hearing loss may occur in adult life.
tic processes, the teeth are not particularly A hallmark of the disease is the presence
sensitive, even when most of the enamel of blue sclera. The clinical spectrum ranges
surface has been lost. Microscopically, the from severe skeletal deformities and short
pulp chamber is nearly obliterated. The stature with mobility impairments to mild
dentinal tubules are poorly formed and forms with limited history of fractures. In
fail to radiate in parallel fashion; rather, all forms, most fractures occur in the lower
they are serpentine and haphazardly extremities. Seven variant types of OI are
arranged. now identified. Radiographically, fractures
are seen along with Wormian bones, “cod-
fish” vertebrae, and osteopenia. Assays of
TREATMENT
bone collagen type I demonstrate perturba-
Affected teeth are not more prone than nor- tions in 98% of the cases of OI type II and
mal teeth to dental caries. Full crowns can somewhat less in the other variants.
be fabricated, even at an early age, because About 90% of individuals with OI types
of the small, obliterated pulp chambers. I, II, III, and IV (but none with OI types V,
Root fractures are relatively common. When VI, and VII) have an identifiable mutation
severe abrasion exists, an overdenture may in either COL1A1 or COL1A2. Types I to V
be considered. are autosomal dominant, whereas type VII
is inherited in an autosomal recessive man-
ner, and the mode of inheritance of type VI
Additional Reading has yet to be illuminated. The features of
Bixler D, Conneally PM, Christen AG. Dentinogenesis
dentinogenesis imperfecta (DI) mirror those
imperfecta; genetic variations in a six-generation fam- cases without OI association (DI type II).
ily. J Dent Res. 1969;48:1196. There is also an OI phenotype in which
PMPH_Eversole_Chapter-11.indd 588 1/20/2011 3:15:32 PM
Dental Defects 589
FIGURE 11-33
Osteogenesis imperfecta
with type I dentinogenesis
imperfecta. Blue sclera.
benign fibro-osseous lesions similar to Steiner RD, Pepin MG, Byers PH. Osteogenesis imper-
florid osseous dysplasia are present in mul- fecta. In Pagon RA, Bird TC, Dolan CR, Stephens K,
eds. GeneReviews [Internet]. Seattle, WA: University
tiple jaw quadrants. of Washington, Seattle; 1993.
DIFFERENTIAL DIAGNOSIS
Various forms of dwarfism must be consid- DENTIN DYSPLASIA TYPE I
ered in severe forms and other conditions Figure 11-34
that predispose to fracture should be con-
Sex: No predilection
sidered (e.g., osteoporosis and osteomala-
cia). Pathologic fractures also occur with CLINICAL FEATURES
intraosseous tumors including cancers
Dentin dysplasia type I is a rare disease
metastatic to bone.
of dentin and is inherited as an auto-
somal dominant trait that affects both the
TREATMENT
deciduous and permanent dentitions. It
There is no preventive treatment for this represents a peculiar disturbance in the
genetic group of disease. Orthopedic man- development of radicular dentinogenesis
agement of fractures is required throughout in that the coronal morphologic and histo-
life. When dentinogenesis is present, full logic features are normal. Unlike dentino-
coverage prosthodontics can be performed genesis imperfecta, enamel fragmentation
for both functional and esthetic reasons. is not encountered. Clinically, the crowns
usually appear normal, yet in some indi-
viduals subtle opalescent gray discolor-
Additional Reading ation is noted. Radiographically, the roots
Levin LS, Wright JM, Byrd DL, et al. Osteogenesis
are rudimentary with tapering and blunt-
imperfecta with unusual skeletal lesions: report of ing. The root canals are obliterated and the
three families. Am J Med Genet. 1985;21(2):257-269. pulp chambers are malformed, appearing
PMPH_Eversole_Chapter-11.indd 589 1/20/2011 3:15:33 PM
590 Chapter 11
FIGURE 11-34
Dentin dysplasia type
I. Rootless teeth with
obliterated root canals
and pulp chambers.
as horizontal crescents. Periapical radiolu-
cencies of unknown origin underlie many Additional Reading
of the teeth. The microscopic appearance Barron MJ, McDonnell ST, Mackie I, Dixon MJ. Hereditary
of extracted teeth is pathognomonic. The dentine disorders: dentinogenesis imperfecta and den-
coronal dentin shows normal tubular ori- tine dysplasia. Orphanet J Rare Dis. 2008;3:31.
entation, whereas the radicular dentin is Kim JW, Simmer JP. Hereditary dentin defects. J Dent
Res. 2007;86(5):392-399.
whorled, giving the appearance of cascad- Rushton MA. A case of dentinal dysplasia. Guys Hosp
ing waterfalls. The pulp chamber and root Rep. 1939;89:369.
canal cannot be identified. The short roots Sauk JJ Jr, Lyon HW, Trowbridge HO, Witkop CJ Jr. An
are functionally unstable, so that loosening electron optic analysis and explanation for the etiology
of dentinal dysplasia. Oral Surg Oral Med Oral Pathol.
of teeth is a feature. Dentin dysplasia type 1972;33:763-771.
I has been reported to occur in conjunc- Wesley RK, Wysoki GP, Mintz SM, Jackson J. Dentin
tion with diffuse generalized osteosclero- dysplasia type I. Clinical, morphologic, and genetic
sis in some patients and radiographically studies of a case. Oral Surg Oral Med Oral Pathol.
1976;41:516-524.
anomalous teeth similar to that of den-
tin dysplasia may be seen in conjunction
with periarticular tumoral calcinosis. The
genetic basis of this disorder has not been
DENTIN DYSPLASIA TYPE II
elucidated. Figure 11-35
Sex: No predilection
TREATMENT
CLINICAL FEATURES
No specific treatment is recommended.
When teeth are lost as a result of shortened Dentin dysplasia type II, coronal type, is
roots, adjacent teeth should not be used as inherited as an autosomal dominant disor-
prosthetic abutments. der. The deciduous teeth are amber/gray
PMPH_Eversole_Chapter-11.indd 590 1/20/2011 3:15:37 PM
Dental Defects 591
FIGURE 11-35
Dentin dysplasia type II
showing denticles. Martini
glass or thistle shaped
pulps.
and translucent with radiographic evidence Lee SK, Hu JC, Lee KE, Simmer JP, Kim JW. A dentin
of pulp chamber and root canal obliteration, sialophosphoprotein mutation that partially disrupts
a splice acceptor site causes type II dentin dysplasia.
thereby resembling dentinogenesis imper- J Endod. 2008;34(12):1470-1473.
fecta. The permanent dentition is clinically Rauta H, Lukinmaa PL, Knif J. Dentin dysplasia type II:
normal; radiographically, pronounced cervi- absence of type III collagen in dentin. J Oral Pathol
cal constriction is not featured. Large, flame- Med. 1990;19:160.
Shields ED, Bixler D, El-Kafrawy AM. A proposed
shaped pulp chambers contain many denti- classification for heritable human dentine defects
cles; root canals may be partially obliterated. with a description of a new entity. Arch Oral Biol.
The dentin sialophosphoprotein (DSPP) gene 1973;18:543.
on chromosome 4q21.3 encodes the major Witkop CJ Jr. Hereditary defects of dentin. Dent Clin
North Am. 1975;19:25.
noncollagenous protein in tooth dentin and is
mutated in dentin dysplasia type 2 as well as
dentinogenesis imperfecta types II and III.
REGIONAL
TREATMENT ODONTODYSPLASIA
No special treatment is required, because Figure 11-36
enamel fracturing is not a problem and root Sex: No predilection
length is essentially normal.
CLINICAL FEATURES
Occurring as a sporadic anomaly, regional
Additional Reading odontodysplasia is a localized develop-
Giansanti JS, Allen JD. Dentin dysplasia type II, or den-
mental dental defect restricted to a single
tin dysplasia, coronal type. Oral Surg Oral Med Oral tooth or group of contiguous teeth in one
Pathol. 1974;38:911. quadrant. Although most instances fail to
PMPH_Eversole_Chapter-11.indd 591 1/20/2011 3:15:40 PM
592 Chapter 11
FIGURE 11-36
Ghost teeth in regional
odontodysplasia.
show gingival enlargement in the affected nective tissue contains many enameloid
area, patients with hyperplastic appearing droplet calcifications.
tissue have been reported. The involved
teeth are usually the central and lateral TREATMENT
incisors and cuspid in the maxilla. They The teeth are nonfunctional; because erup-
fail to erupt completely. On radiographs, tion is not evident or is only partial, extrac-
both enamel and dentin formation are defi- tion with fabrication of a prosthetic appli-
cient, yielding a subdued appearance with ance is recommended.
patent dilated pulp chambers. The appear-
ance accounts for the term ghost teeth. The
cause is unknown; however, the distribu-
tion in the maxilla often corresponds to the Additional Reading
neurovascular supply, suggesting that an Alexander WN, Lily GE, Irby WB. Odontodysplasia.
ischemic phenomenon may be responsible. Oral Surg Oral Med Oral Pathol. 1966;22:814.
In fact, many cases have been reported in Gardner DG, Sapp JP. Regional odontodysplasia. Oral
which vascular nevi involve the area of the Surg Oral Med Oral Pathol. 1973;35:351.
Neupert EA III, Wright JM. Regional odontodysplasia
face that harbors the hypoplastic teeth. Both presenting as a soft tissue swelling. Oral Surg Oral
permanent and deciduous predecessors Med Oral Pathol. 1989;67:193.
may be affected. Microscopically, large pulp Quindere LB, Cavalcante RB, Nonaka CF, Miguel MC,
chambers are noted and the dentin is thin da Souza LB. Regional odontodysplasia involving three
quadrants of the jaws: a case report. Quintessence Int.
and globular. The enamel layer is attenu- 2010;41(1):13-16.
ated and disrupted. The reduced enamel Rushton, MA. Odontodysplasia. “Ghost teeth.” Br Dent
epithelium persists, and the follicular con- J. 1965;119:109.
PMPH_Eversole_Chapter-11.indd 592 1/20/2011 3:15:42 PM
Dental Defects 593
HYPOPHOSPHATASIA layer of dentin is observed with cemental
Figure 11-37 agenesis. The serum alkaline phosphatase
level is lowered; in many cases, hypercalce-
Sex: No predilection mia and urinary phosphoethanolamine are
demonstrable. Mutations in ALPL, the gene
CLINICAL FEATURES
encoding alkaline phosphatase, and tissue-
Inherited as an autosomal recessive trait, nonspecific isozyme (TNSALP) ALPL occur
hypophosphatasia represents an enzyme- in hypophosphatasia.
deficiency metabolic bone disease char-
acterized by absence or diminution of TREATMENT
alkaline phosphatase in osteoblasts, intes- No successful treatment is available. High-
tines, and kidneys, among other tissues. dose vitamin D therapy has been used with
It occurs in infantile, juvenile, and adult limited success.
forms; the infantile form has the worst
prognosis. Those individuals capable of
survival show osteomalacia with hypomin- Additional Reading
eralization similar to that seen in acquired
Sobel EH, Clark LC, Fox RP, Robinow M. Rickets,
rickets. The chief dental manifestation is
deficiency of “alkaline” phosphatase activity and pre-
premature tooth loss from cemental agen- mature loss of teeth in childhood. Pediatrics. 1953;11:
esis with lack of secure periodontal fiber 309-322.
attachment to the teeth. In addition, the Poland E III, Eversole LR, Bixler D, Christian JC.
teeth are often hypocalcified with large Histochemical observations in hypophosphatasia. J
Dent Res. 1972;51:333-338.
pulp chambers resembling shell teeth or Kjellman M, Oldfelt V, Nordenram A, Olow-
odontodysplasia. Both primary and second- Nordenram M. Five cases of hypophosphatasia with
ary teeth are affected. Histologically, a thin dental findings. Int J Oral Maxillofac Surg. 1973;2:
152-158.
Macfarlane JD, Swart JGN. Dental aspects of hypophos-
phatasia: a case report, family study, and literature
review. Oral Surg Oral Med Oral Pathol. 1989;67:521.
Mornet E, Nunes ME. Hypophosphatasia. In Pagon RA,
Bird TC, Dolan CR, Stephens K, eds. GeneReviews
[Internet]. Seattle, WA: University of Washington;
1993-2007.
VITAMIN D REFRACTORY
RICKETS
Figure 11-38
Sex: Males are affected more severely
CLINICAL FEATURES
Vitamin D refractory or hypophosphatemic
rickets is a heritable disorder with X-linked
dominant transmission. The clinical fea-
tures, osteomalacia causing osseous defor-
FIGURE 11-37 mities similar to those seen in ordinary
Drawing depicting normal cementogenesis (left), rickets, do not show resolution with admin-
cemental agenesis in hypophosphatasia (right). istration of vitamin D. Serum phosphorus
PMPH_Eversole_Chapter-11.indd 593 1/20/2011 3:15:44 PM
594 Chapter 11
FIGURE 11-38 phatemic rickets, and the former disease
Elongated pulp responds rapidly to vitamin D therapy. A
horns in region of mutation in the vitamin D receptor gene
coronal fissures in
has been identified.
vitamin D refrac-
tory rickets.
DIFFERENTIAL DIAGNOSIS
Widespread dental abscess formation may
be seen in diabetes of juvenile onset, yet
diabetes rarely becomes severe enough to
produce these changes in young children.
Assessment of serum phosphorus levels
and a skeletal radiographic survey should
be done with children showing wide-
spread periapical disease in the absence
of dental caries. The presence of a familial
pattern also helps to limit the differential
diagnosis.
TREATMENT
Administration of 1α-25 dihydroxyvitamin
D3 results in significant improvement. The
levels are depressed. Patients lack an enzyme patient should be referred to an internist
necessary for conversion of intestinally or endocrinologist. Occlusal sealants will
absorbed vitamin D3 into the active 1α-25 not prevent pulpal and periapical infection.
dihydroxyvitamin D3. The resultant deficit Complete pulpectomy of affected teeth is
in active vitamin leads to poor phosphate recommended with placement of zinc oxide
absorption and deficient mineralization and engenol.
of osteoid. There is also some evidence to
support a defect in renal tubular handling
of phosphate. Affected children have dif- Additional Reading
ficulty walking. Globular dentin is promi-
Archard HO, Witkop CJ Jr. Hereditary hypophos-
nent; fissures develop and extend from the phatemia (vitamin D-resistant rickets) presenting pri-
pulp horns, which are elongated, to the mary dental manifestations. Oral Surg Oral Med Oral
cusp tips. These fissures are patent, allow- Pathol. 1966;22:184.
ing oral microorganism to gain access to Shafeghati Y, Momenin N, Esfahani T, Reyniers E,
Wuyts W. Vitamin D-dependent rickets type II: report
the pulp chamber in the absence of caries. of a novel mutation in the vitamin D receptor gene.
This exposure, in turn, leads to periapical Arch Iran Med. 2008;11(3):330-334.
disease, demonstrated radiographically, Shields ED, Scriver CR, Reade T, et al. X-linked hypo-
with clinical evidence of widespread fis- phosphatemia: the mutant gene is expressed in teeth
as well as in kidney. Am J Hum Genet. 1990;46:434-
tulae. The supportive alveolar bone often 442.
shows an osteoporotic pattern of trabecula- Tracy WE, Steen JC, Steiner JE, Buist NR. Analysis of
tion. The long-bone epiphyseal plates show dentin pathogenesis in vitamin D-resistant rickets.
pericartilaginous deposition with failure to Oral Surg Oral Med Oral Pathol. 1971;32:38-44.
Vasilakis GJ, Nygaard VK, DiPalma DM. Vitamin
mineralize.
D-resistant rickets. A review and case report of an ado-
Ordinary rickets fails to show the lescent boy with a history of dental problems. J Oral
dental defects encountered in hypophos- Pathol Med. 1980;35:19.
PMPH_Eversole_Chapter-11.indd 594 1/20/2011 3:15:45 PM
Dental Defects 595
FIGURE 11-39
Pulp stones.
DENTICLES AND PULP dystrophic calcifications that tend to align
CALCIFICATION themselves in a vertical plane throughout
Figure 11-39 the radicular pulp.
Age: Adults TREATMENT
Sex: No predilection No treatment is required.
CLINICAL FEATURES
Pulpal calcifications are identified on den- Additional Reading
tal radiographs and may be located either
Goga R, Chandler NP, Oginni AO. Pulp stones: a review.
within the pulp chamber, appearing as Int Endod J. 2008;41(6):457-468.
focal intrapulpal radiopacities, or within the Hill TJ. Pathology of dental pulp. J Am Dent Assoc.
root canals, as diffuse radiopacities giving 1934;21:820.
the appearance of calcific obliteration. The Johnson PL, Bevelander G. Histogenesis and histoc
hemistry of pulpal calcifications. J Dent Res.
calcifications in the coronal pulp chamber
1956;35:714.
are referred to as denticles or pulp stones; root Levin LS, Young RJ, Pyeritz RE. Osteogenesis imperfec-
canal calcification has been referred to as ta type I with unusual dental abnormalities. Am J Med
calcific metamorphosis of pulp. In either case, Genet. 1988;31:921.
no cause can be identified either locally or Stafne EC, Szabo SE. The significance of pulp nodules.
Dent Cosmos. 1933;75:160.
systemically. The teeth are vital, even when
canals appear to be obliterated, and there is
no relationship between pulp calcification SEGMENTAL
and facial pain. Denticles are classified as ODONTOMAXILLARY
“true” if composed of dentin or “false” if
DYSPLASIA
composed of laminated dystrophic calcific
concretions. Furthermore, either type may Figure 11-40
be attached or free, depending on whether Age: Teens
the calcified mass is confluent with the nor- Sex: No predilection
mal tooth dentin. Type II dentin dysplasia is
CLINICAL FEATURES
characterized by large pulp chambers with
denticle formation. Pulp stones are also fre- This anomaly is sporadic and is first noted
quently encountered in certain forms of OI. during teenage years when routine dental
Microscopically, calcific metamorphosis of or orthodontic radiographs are procured
the root canal is characterized by multifocal or when facial asymmetry becomes appar-
PMPH_Eversole_Chapter-11.indd 595 1/20/2011 3:15:46 PM
596 Chapter 11
FIGURE 11-40
Segmental odontomaxil-
lary dysplasia.
ent. Unilateral asymmetry with maxillary TREATMENT
enlargement is usually mild and may not No treatment is necessary. Any unerupted
be particularly noticeable. Radiographically, teeth in the area of lesional bone should be
the area of alveolar enlargement shows a extracted. If maxillary enlargement is a cos-
somewhat ground glass appearance that is metic concern, surgical contouring may be
vertically streaked yielding a “falling rain undertaken.
or sleet” pattern. One or both premolar
teeth are missing and retained deciduous
teeth are morphologically anomalous. Additional Reading
MICROSCOPIC FEATURES Armstrong C, Napier SS, Boyd RC, Gregg TA.
Histopathology of the teeth in segmental odontomax-
Pathologic changes in the affected maxillary illary dysplasia: new findings. J Oral Pathol Med.
bone are characterized by osteocytic hyper- 2004;33(4):246-248.
plasia (increased number of intralacunar Becktor KB, Reibel J, Vedel B, Kjaer I. Segmental odon-
tomaxillary dysplasia: clinical, radiological and histolog-
osteocytes per unit area of bone), lacunar
ical aspects of four cases. Oral Dis. 2002;8(2):106-110.
enlargement, and sheet-like arrangements Danforth RA, Melrose RJ, Abrams AM, Handlers JP.
of woven bone. Osteoblastic and osteoclas- Segmental odontomaxillary dysplasia. Report of eight
tic activity appears decreased. The fibrous cases and comparison with hemimaxillofacial dysplasia.
marrow element is hypocellular, mature, or Oral Surg Oral Med Oral Pathol. 1990;70(1):81-85.
Packota GV, Pharoah MJ, Petrikowski CG. Related articles,
myxoid. Affected teeth show variability in links radiographic features of segmental odontomaxil-
dentinal tubule diameter. lary dysplasia: a study of 12 cases. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod. 1996;82(5):577-584.
DIFFERENTIAL DIAGNOSIS Welsch MJ, Stein SL. A syndrome of hemimaxillary
enlargement, asymmetry of the face, tooth abnor-
Fibrous dysplasia may be a consideration, yet malities, and skin findings (HATS). Pediatr Dermatol.
does not show anomalous or missing teeth. 2004;21(4):448-451.
PMPH_Eversole_Chapter-11.indd 596 1/20/2011 3:15:47 PM
Dental Defects 597
INTERNAL RESORPTION where the vascularity of the pulp tissue is
Figure 11-41 observed through a thin dental hard tissue
layer with a pink appearance (pink tooth of
Age: Young adults Mummery). Radiographs show a circular or
Sex: No predilection ovoid radiolucency within the region of the
pulp chamber either in the coronal or, more
CLINICAL FEATURES
commonly, in the radicular region. The
As opposed to most of the diseases showing maxillary central incisors are most often
structural deformities, internal resorp- afflicted. Internal resorption may accom-
tion is acquired later in life and fails to fol- pany external resorption, particularly with
low any hereditary pattern. The cause is impacted teeth. Microscopically, the pulp
unknown, although trauma has been sug- chamber contains viable fibrous connective
gested. Caries with pulpitis may be pres- tissue, which in unexposed pulps is devoid
ent, but this is not a prerequisite. Pain is of inflammation. The dentin shows scallop-
not a feature when caries is absent. When ing with osteoclastic resorption. Attempts
internal resorption develops in the coronal at repair may exist, with deposition of osteo-
pulp, the tooth may resorb to the point dentin over zones of resorption.
FIGURE 11-41
Internal resorption manifesting an intra-
dental radiolucency.
PMPH_Eversole_Chapter-11.indd 597 1/20/2011 3:15:50 PM
598 Chapter 11
TREATMENT EXTERNAL RESORPTION
No treatment is required. Endodontic Figure 11-42
therapy is not feasible because of the
inaccessibility of the resorbed recesses Age: Adults
Sex: No predilection
to instrumentation. As the disease pro-
gresses, root fracture may occur, neces- CLINICAL FEATURES
sitating extraction. Often, the resorption
The cementum and underlying dentin may
becomes static.
show resorption as a consequence of pres-
sure or trauma generated by tumors and
Additional Reading cysts, orthodontic forces, reimplantation, or
periapical inflammation. Impacted teeth of
Eveson JW, Gibb DH. Multiple idiopathic internal long standing may also show internal and
resorption. Br Dent J. 1989;166:49.
Frank AL. External-internal progressive resorption
external resorption of both coronal and
and its nonsurgical correction. J Endodent. 1981;7: radicular hard tissues. Resorption of roots
473. on erupted teeth where no cause can be
Selley WG. Idiopathic internal resorption of upper cen- determined is termed idiopathic resorption.
tral incisor. Br Dent J. 1956;100:357.
Some degree of root resorption probably
Sweet APS. Internal resorption, a chronology. Dent
Radiogr Photogr. 1965;38:75. occurs in most adults; however, it is mini-
Toplis JW. Idiopathic internal resorption of deciduous mal. Occasionally, for no apparent reason,
teeth. Br Dent J. 1980;149:111. many teeth show advanced resorption
FIGURE 11-42
External root resorption.
PMPH_Eversole_Chapter-11.indd 598 1/20/2011 3:16:01 PM
Dental Defects 599
with blunting of the roots. The maxillary SUBCERVICAL RESORPTION
premolars, incisors, and molars are most Figure 11-43
often affected. Neither periodontal disease
nor periapical inflammation bears any rela- Age: Adults
tionship to idiopathic generalized resorp- Sex: No predilection
tion. The apices show osteoclast-mediated CLINICAL FEATURES
resorption of cementum and dentin, with
no alteration in the periodontal ligament or Subcervical resorptive foci may be isolated,
underlying periodontal bone that replaces yet usually multiple lesions are seen, even as
the zone previously occupied by dental root many as 20 in any given patient. The resorp-
structure. tive lesions may be focal, on only one side of
a tooth or they may become circumferential.
TREATMENT Their number increases with time. There is
No form of treatment has been shown to arrest no association with any specific systemic or
the process. Resorption may proceed progres- other dental disease and the resorptive foci
sively until the involved teeth become loose. are not carious. Radiographically, radiolu-
Extraction may then become necessary. cencies at the cervical region are seen and
are usually smooth and well demarcated.
Additional Reading MICROSCOPIC FEATURES
Kerr DA, Courtney RM, Burkes EJ. Multiple idiopath- Granulation tissue, chronically inflamed,
ic root resorption. Oral Surg Oral Med Oral Pathol. occupies the resorptive foci and osteoclastic
1970;29:552. activity is identifiable.
Massler M, Perreault JG. Root resorption in the
permanent teeth of young adults. J Dent Child. DIFFERENTIAL DIAGNOSIS
1954;21:158.
Patel S, Dawood A, Wilson R, Horner K, Mannocci F. Cervical/root caries is differentiated from
The detection and management of root resorption subcervical resorption on the findings of
lesions using intraoral radiography and cone beam
computed tomography—an in vivo investigation. Int hard tissue softness using a sharp probe.
Endod J. 2009;42(9):831-838.
Postlethwaite KR, Hamilton M. Multiple idiopathic TREATMENT
external root resorption. Oral Surg Oral Med Oral
Pathol. 1989;68:640.
Circumferential lesions may condemn the
Yaacob HB. Idiopathic external resorption of teeth. Can tooth to extraction. Focal lesions can be
Dent Assoc J. 1980;46:578. restored with composite or full crowns can
FIGURE 11-43
Subcervical erosion.
PMPH_Eversole_Chapter-11.indd 599 1/20/2011 3:16:04 PM
600 Chapter 11
be fabricated especially in teeth that may be their face. Incisal fractures are the most
in danger of fracture. common injuries. There are classifica-
tion systems for dental fractures that are
designed for determining the most appro-
Additional Reading priate restorative treatment. Fractures that
Bergmans L, Van Cleynenbreugel J, Verbeken E, Wevers do not intersect the pulp chamber may
M, Van Meerbeek B, Lambrechts P. Cervical exter- not predispose to pulpitis because of pulp
nal root resorption in vital teeth. J Clin Periodontol. exposure; however, if tooth luxation occurs,
2002;29(6):580-585. the pulp may be devitalized in the absence
Liang H, Burkes EJ, Frederiksen NL. Multiple idiopathic
cervical root resorption: systematic review and report of
of pulp exposure. Fractures that intersect
four cases. Dentomaxillofac Radiol. 2003;32(3): 150-155. and expose the pulp will result in pulpitis
Roig M, Morelló S, Mercadé M, Durán-Sindreu F. leading to necrosis and periapical spread of
Invasive cervical resorption: report on two cases. Oral infection.
Surg Oral Med Oral Pathol Oral Radiol Endod. 2010
Jun 24. [Epub ahead of print].
MICROSCOPIC FEATURES
Not applicable.
CORONAL FRACTURE
Figure 11-44 DIFFERENTIAL DIAGNOSIS
Age: Children and teens A history of trauma eliminates develop-
Sex: Male predilection mental defects.
CLINICAL FEATURES
Rambunctious kids engaging in dare- TREATMENT
devil feats, tend to fall off of bikes and Avulsed teeth may be reinserted into the
skateboards, many invariably landing on socket and immobilized. Pulpotomy in
FIGURE 11-44
Incisal trauma with
fractures.
PMPH_Eversole_Chapter-11.indd 600 1/20/2011 3:16:07 PM
Dental Defects 601
pulpally exposed deciduous teeth is recom-
mended; in permanent incisors and cus- Additional Reading
pids, root canal therapy is required. Bodenhoff J, Gorlin RJ. Natal and neonatal teeth; folk-
lore and fact. Pediatrics. 1963;32:1087.
Camm JH, Schuler JL. Premature eruption of the pre-
Additional Reading molars. ASDC J Dent Child. 1990;57:142.
Dixon GH, Stewart RE. In Stewart RE, Prescott GH,
eds. Oral Facial Genetics. St. Louis, MO: C. V. Mosby;
Flores MT, Andersson L, Andreasen JO, et al. I. Fractures
1976: 142.
and luxations of permanent teeth. International
Spouge JD, Feasby WH. Erupted teeth in the newborn.
Association of Dental Traumatology. Dent Traumatol.
Oral Surg Oral Med Oral Pathol. 1966;22:198.
2007;23(2):66-71.
Thorén H, Numminen L, Snäll J, et al. Occurrence and
types of dental injuries among patients with maxillo-
facial fractures. Int J Oral Maxillofac Surg. 2010;39:
774-778.
DELAYED ERUPTION
Yilmaz Y, Guler C, Sahin H, Eyuboglu O. Evaluation of Sex: No predilection
tooth-fragment reattachment: a clinical and laboratory
CLINICAL FEATURES
study. Dent Traumatol. 2010;26(4):308-314.
Great variation exists with regard to erup-
tion dates; thus, delayed eruption may
Alterations in Eruption/ not herald the presence of any underly-
Exfoliation Times ing disorder but may merely represent a
variation in normal physiology. Certain
PREMATURE ERUPTION systemic illnesses and syndromes may be
associated with generalized delayed erup-
Sex: No predilection tion, and these conditions must be consid-
ered when a patient exhibits alteration in
CLINICAL FEATURES
eruption dates. In particular, patients with
Early eruption of teeth may occur with cleidocranial dysostosis show hypoplas-
both deciduous and permanent dentitions tic or aplastic clavicles, cranial anomalies,
in the absence of any underlying systemic and multiple unerupted and supernumer-
disorder. Indeed, 10% of the population ary teeth. In cryptodontic brachymetacar-
may manifest precocious eruption as early pia, the metacarpals and metatarsals are
as 3 months for deciduous and 4 years for shortened and teeth fail to erupt. Many of
permanent dentitions. Natal or neonatal the syndromes described in conjunction
teeth are deciduous teeth, usually man- with enamel defects show retarded erup-
dibular incisors, that are present at birth tion or unerupted teeth. Hypothyroidism
or erupt soon thereafter. This condition and hypopituitarism (pituitary dwarfism)
seems to be genetically determined and is are often associated with delayed eruption.
most frequently encountered among iso- Multiple impacted teeth are encountered in
lated tribes and ethnic groups. Often, pre- cleidocranial dysplasia and Gardner’s syn-
maturely erupted deciduous teeth fail to drome. Generalized delayed eruption may
complete root development and are prema- also be encountered in Down’s syndrome,
turely exfoliated. A variety of craniofacial rickets, vitamin D refractory rickets, lead
syndromes are associated with premature poisoning, and osteopetrosis. Isolated or
eruption of teeth: clefts, oculomandibulo- individual teeth showing retarded erup-
dyscephaly, chondroectodermal dysplasia, tion often indicate the presence of an intra-
and hemifacial hypertrophy. Hyperthyroid- bony odontogenic neoplasm or cyst, requir-
ism of congenital or childhood onset may ing radiographs to determine whether
also be associated with early eruption. or not a radiolucent or radiopaque lesion
PMPH_Eversole_Chapter-11.indd 601 1/20/2011 3:16:14 PM
602 Chapter 11
is associated with the impacted tooth. In encountered in man. Failure of teeth to erupt
addition to impaction, congenitally missing may be the result of a physical barrier, unex-
teeth, of course, give the impression that plained loss of eruption force, or a tumor or
eruption is retarded. This may be general- cyst of the jaws arising from odontogenic
ized in hereditary ectodermal dysplasia or nonodontogenic tissues. The mandibu-
and chondroectodermal dysplasia. lar third molars and maxillary canines are
most frequently involved, followed by the
Additional Reading maxillary third molars. Maxillary central
incisors, mandibular canines, and premo-
Barberia LE, Marañes PJP, Mourelle MMR, Moreno lars in both arches are also retained with
GJP. Tooth eruption in children with growth deficit. some degree of frequency. Supernumerary
J Int Assoc Dent Child. 1988;19:29-35. teeth such as mesiodens and premolars
Dixon GH, Stewart RE. In Stewart RE, Prescott GH,
eds. Oral Facial Genetics. St. Louis, MO: C. V. Mosby; often fail to erupt. Multiple impactions and
1976: 142. supernumerary teeth are encountered in
Pearl M, Roland NM. Delayed primary dentition in a cleidocranial dysostosis, which is charac-
case of congenital lead poisoning. ASDC J Dent Child. terized by the aforementioned dental defect
1980;47:269.
Pindborg JJ. Pathology of the Dental Hard Tissues.
in conjunction with agenesis or hypoplasia
Philadelphia, PA: W. B. Saunders; 1970. of the clavicles and craniofacial anomalies
Shokeir MH. Complete failure of eruption of all per- including Wormian bones, open fontanels,
manent teeth: an autosomal dominant disorder. Clin hypoplastic sinuses, and other defects of
Genet. 1974;5:322.
both membranous and endochondral bones.
Gardner’s syndrome is also associated with
IMPACTION multiple dental impactions. Impacted teeth
Figure 11-45 are also seen in various forms of AI and in
syndromes associated with enamel defects.
Sex: No predilection The significance of impacted teeth rests with
the latent potential of the follicular tissues
CLINICAL FEATURES
to undergo cystic or neoplastic transforma-
Impaction or retention of teeth is one of the tion. A complication of impacted mandibu-
most common developmental dental defects lar third molar removal is paresthesia.
FIGURE 11-45
Impacted teeth. Arrows: odontomas.
PMPH_Eversole_Chapter-11.indd 602 1/20/2011 3:16:14 PM
Dental Defects 603
Additional Reading Additional Reading
Blum T. Malposed teeth; their classification, pathology Cohen DW, Morris AL. Periodontal manifestations of
and treatment. Int J Orthod. 1923;9:122. cyclic neutropenia. J Periodontol. 1961;32:159.
Dachi SF, Howell FV. A survey of 3,874 routine Gorlin RJ, Sedano H, Anderson VE. The syndrome of
full-mouth radiographs. II. A study of impacted palmar-plantar hyperkeratosis and premature peri-
teeth. Oral Surg Oral Med Oral Pathol. 1961;14: odontal destruction of the teeth. J Pediatr. 1964;
1165. 65:895.
Fielding AF, Douglass AF, Whitley RD. Reasons for Kjellman M, Oldfelt V, Nordenram A, Olow-Nordenram
early removal of impacted third molars. Clin Prevent M. Five cases of hypophosphatasia with dental findings.
Dent. 1981;3:19. Int J Oral Maxillofac Surg. 1973;2:152-158.
Miller CS, Nummikoski PV, Barnett DA, Langlais RP. Myers DR, O’Dell NL, Clark JW, Cross RL.
Cross-sectional tomography. A diagnostic technique Localized prepubertal periodontitis: literature review
for determining the buccolingual relationship of and report of case. ASDC J Dent Child. 1989;56:
impacted mandibular third molars and the inferior 107-111.
alveolar neurovascular bundle. Oral Surg Oral Med Ritchie BM. Hypophosphatasia. A metabolic disease
Oral Pathol. 1990;70:791-797. with important dental manifestations. Arch Dis Child.
Shaw BM, Schneider SS, Zeger J. Surgical management 1964;39:584.
of ankylosed impacted maxillary canines. J Am Dent
Assoc. 1981;102:497.
Pigmentations
PREMATURE EXFOLIATION
Sex: No predilection ERYTHROBLASTOSIS
CLINICAL FEATURES FETALIS
Figure 11-46
Premature loss of deciduous teeth in
conjunction with precocious eruption is Sex: No predilection
usually no clinical significance because
CLINICAL FEATURES
the succedaneous dentition also com-
monly erupts early. Premature exfoliation Hemolytic anemia develops in infants
limited to a localized region may be an when an Rh-positive fetus is nurtured in
ominous sign. Loosening of either decidu- the womb of an Rh-negative mother who
ous or permanent teeth in children, teen- has developed anti-Rh antibodies from
agers, or young adults may be indicative a previous pregnancy. When antibodies
of an underlying destructive process of pass the placental membrane and enter
the alveolar bone: leukemia, sarcoma, his- the fetal circulation, they agglutinate fetal
tiocytosis X, or a benign neoplasm. Gener- erythrocytes, bind complement, and cause
alized premature loss of the incisors and hemolysis. This same immunologic lesion
molars is a feature of periodontosis; when may evolve as a consequence of ABO
seen in conjunction with palmar-plantar isoantigen incompatibility, in which the
hyperkeratosis, the Papillon-Lefevre syn- fetus is A, B, or AB and the mother lacks
drome should be considered. Generalized A or B isoantigens. If the anemia is pro-
early tooth loss is also encountered in longed, hemolyzed erythrocytes liberate
hypophosphatasia, juvenile onset diabe- hemosiderin pigment, which may become
tes, cyclic neutropenia, agranulocytosis, deposited in developing dentin matrices.
acrodynia, scurvy, and dentin dysplasia. Teeth at a comparable stage of develop-
Full-mouth dental radiographs or a pan- ment (usually only deciduous) then show
orex radiograph should be obtained when pigmentation; they are brown, black,
teeth become loose prior to their normal green, or blue. The pigment is transmitted
exfoliation times. from the deeper layers of dentin. When
PMPH_Eversole_Chapter-11.indd 603 1/20/2011 3:16:19 PM
604 Chapter 11
Thursfield H. Green teeth subsequent to a prolonged
jaundice in the first weeks of life. Proc R Soc Med.
1912;5:147.
BILIARY ATRESIA
Figure 11-47
Sex: No predilection
CLINICAL FEATURES
Atresia of the biliary ducts, or other liver dis-
orders such as neonatal hepatitis, may cause
FIGURE 11-46 retention of either conjugated or unconjugated
Teeth in erythroblastosis fetalis darkened as a bilirubin. The bile pigments become elevated
result of hemosiderin pigment deposition in den- in serum and may then become incorporated
tin. (Courtesy of Drs. R. Abrams, R. Adams, and into the organic matrices of developing teeth.
R. Sobel.) In the icteric state, the deposited bilirubin
imparts a green hue to the deciduous teeth. If
the child is able to thrive and if the jaundice
icterus develops, hypoplasia of enamel can be corrected, he or she will have a normal
may be seen. secondary dentition. The prognosis with bil-
DIFFERENTIAL DIAGNOSIS
iary atresia is poor. Other forms of neonatal
jaundice such as erythroblastosis and hepati-
The pigment of erythroblastosis is not asso- tis are reversible in most cases.
ciated with a chalky enamel surface as is
often encountered in fluorosis. Staining DIFFERENTIAL DIAGNOSIS
from tetracycline occurs more often in per-
The diagnosis of biliary atresia is made
manent teeth, is yellow, and fluoresces with
on the basis of biochemical and radiologic
ultraviolet light. Red fluorescence is seen in
studies for liver function. A conjugated
porphyria. Bilirubin-stained teeth are also
hyperbilirubinemia prevails, and cholan-
green, so that various other forms of neona-
giograms disclose a rudimentary biliary
tal jaundice must be considered. Extrinsic
tree. Liver biopsy may also be required to
stains can be removed with scalers.
make the diagnosis. Fever with jaundice
TREATMENT in newborns may indicate neonatal hepati-
tis. Needle biopsies may aid in obtaining a
No treatment is required. On exfoliation, the definitive diagnosis. By the time the patient
permanent teeth are usually of normal color. is seen by the dentist, a diagnosis has usu-
ally been rendered.
Additional Reading TREATMENT
Atasu M, Genc A, Ercalik S. Enamel hypoplasia and
Provided that jaundice has been corrected,
essential staining of teeth from erythroblastosis fetalis.
J Clin Pediatr Dent. 1998;22(3):249-252. the secondary dentition will be normal.
Kesson CW. Green teeth following icterus gravis neona-
torum. Proc R Soc Med. 1949;42:561.
Marsland EA, Gerrard JW. Intrinsic staining of teeth fol-
lowing icterus gravis. Br Dent J. 1953;94:305.
Additional Reading
Tank G. Two cases of green pigmentation of deciduous Baden E. In Gorlin RJ, Goldman HM, eds. Thoma’s Oral
teeth associated with hemolytic disease of the new- Pathology, Vol. I.. 6th ed. St. Louis, MO: C. V. Mosby;
born. J Am Dent Assoc. 1951;42:302. 1970: 191.
PMPH_Eversole_Chapter-11.indd 604 1/20/2011 3:16:20 PM
Dental Defects 605
cal assays have disclosed that the pigment
is undegraded hemoglobin rather than
hemosiderin or bilirubin, and this pigment
collects in the pulp as well as in dentinal
tubules. Gross evidence of pigmentation
is more striking in the roots of extracted
teeth, yet histologic sections disclose that
more pigment actually accumulates in the
coronal dentin and fades distally from the
pulp chamber on out to the dentinoenamel
junction.
FIGURE 11-47 Additional Reading
Exfoliated teeth stained green by bilirubin pigment
in biliary atresia. Brondum N, Simonsen J. Postmortem red coloration of
teeth. A retrospective investigation of 28 cases. Am J
Forensic Med Pathol. 1987;8:127.
Kirkham WR, Andrews EE, Snow CC, Grape PM,
Herbert FL, Delcambre TJ. Unusual case of green teeth Lorenza S. Postmortem pink teeth. J Forensic Sci.
resulting from neonatal hyperbilirubinemia. ASDC J 1977;22:119-131.
Dent Child. 1987;54:54. Sainio P, Syrjänen S, Keijälä JP, Parviainen AP.
Shapiro BM, Gallagher RE, Needleman HL. Dental man- Postmortem pink teeth phenomenon: an experimental
agement of the patient with biliary atresia. Report of two study and a survey of the literature. Proc Finn Dent
cases. Oral Surg Oral Med Oral Pathol. 1975;40:742. Soc. 1990;86:28.
Shittaker DK, Thomas VC, Thomas RIM. Post-mortem
pigmentation of teeth. Br Dent J. 1976;140:100.
POSTMORTEM PINK TEETH Van Wyk CW. Postmortem pink teeth. Histochemical
identification of the causative pigment. Am J Forensic
Age: After death
Med Pathol. 1989;10:134.
Sex: No predilection
CLINICAL FEATURES
PORPHYRIA
The pink teeth phenomenon in corpses, Figure 11-48
although uncommon, is a well-recognized
postmortem change. Predisposing fac- Sex: No predilection
tors include unnatural death, exposure
to humid conditions or submersion of the CLINICAL FEATURES
corpse in water, and probable gravitational Accumulations of porphyrin compounds in
stasis of blood at the time of death. Thus, tissues may result from certain infections
postmortem pink teeth are most often, yet or from an inborn error in metabolism.
not exclusively, observed in drownings. The most important form associated with
Clinically, all, most, or just a few teeth may dental pigmentation is congenital eryth-
be discolored, ranging from pale pink to a ropoietic porphyria, which is inherited as
robust red. The pigmentation is most obvi- an autosomal recessive trait. The first sign
ous in the root, with the apical one third is red coloration of the urine by uropor-
being of normal color. The cervical areas of phyrin. Photosensitivity becomes pro-
the crowns are involved; the occlusal sur- gressively worse as the child ages and a
faces are not. In all cases, the radicular col- vesiculobullous dermatitis develops. Both
oration is of a darker hue than that seen in deciduous and permanent dentitions show
the crown. Furthermore, anterior teeth are pigmentation, usually brown. Under ultra-
darker than molars. Histologic and chemi- violet light, the teeth show a striking red
PMPH_Eversole_Chapter-11.indd 605 1/20/2011 3:16:20 PM
606 Chapter 11
DENTAL FLUOROSIS
Figure 11-49
Sex: No predilection
CLINICAL FEATURES
Fluorosis, a common cause of dental pig-
mentation, is discussed with structural
dental defects. In addition to the hypoplas-
tic changes, a mottled or blotchy brown pig-
mentation is present in the enamel layers.
FIGURE 11-48
Porphyrin deposits in porphyria. (Courtesy of Dr.
Both deciduous and permanent teeth are
R. Gorlin.) affected if excess fluoride is consumed in
drinking water during the period of tooth
development. Concentrations in excess
of 1 ppm are required to produce dental
fluorescence. Ground sections disclose por-
mottling. Severe pigmentation is usually
phyrin pigments deposited in enamel, den-
not seen unless the fluoride concentration
tin, and cementum.
exceeds 5 ppm.
DIFFERENTIAL DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
The stain in porphyria often has a reddish Dental fluorosis is usually associated with
tinge. Under fluorescent light, the red fluo- chalky enamel surfaces, and the pigmenta-
rescence is pathognomonic. The cutaneous tion is generally irregular and blotchy, as
manifestations of porphyria, in conjunction opposed to that of other dental pigmenta-
with other clinical features of the disease, tions. The pigment shows no fluorescent
allow for differentiation from other disor- properties. A history of residence in a geo-
ders that show dental pigmentation. graphic region known to contain high lev-
els of fluoride in the water is significant in
TREATMENT limiting the differential diagnosis.
No treatment is available. The discolored
teeth may be cosmetically restored with TREATMENT
porcelain-veneered crowns.
Teeth with fluorosis pigmentation can be
restored with esthetic porcelain crowns.
Additional Reading
Haining RG, Cowger ML, Shurtleff DB, Labbe RF.
Congenital erythropoietic porphyria. Am J Med.
Additional Reading
1968;45:624-637. Black GV McKay FS. Mottled teeth: an endemic devel-
Kooijman MM, Brand HS. Oral aspects of porphyria. Int opmental imperfection of the enamel of teeth here-
Dent J. 2005;55(2):61-66. tofore unknown in the literature of dentistry. Dent
Schmid R, Schwartz S, Sundberg RD. Erythropoietic Cosmos. 1916;58:129.
(congenital) porphyria: a rare abnormality of the nor- Dean HT, Arnold FA. Endemic dental fluorosis or mot-
moblasts. Blood. 1955;10:416. tled teeth. J Am Dent Assoc. 1943;30:1278.
Trodahl JN, Schwartz S, Gorlin RJ. The pigmentation of Eckersten C, Pylvänen L, Schröder U, Twetman S,
dental tissues in erythropoietic (congenital) porphyria. Wennhall I, Matsson L. Prevalence of dental fluorosis
J Oral Pathol Med. 1972;1:159. in children taking part in an oral health programme
Waldenstrom J, Haeger-Aronsen B. Different patterns of including fluoride tablet supplements from the age of
humans porphyria. Br Med J. 1963;2:272. 2 years. Int J Paediatr Dent. 2010;20:347-352.
PMPH_Eversole_Chapter-11.indd 606 1/20/2011 3:16:21 PM
Dental Defects 607
FIGURE 11-49
Teeth with fluorosis show-
ing brown pigmentation.
McClure FS, Lipkins RC. Fluorine in human teeth stud- DIFFERENTIAL DIAGNOSIS
ied in relation to fluorine in the drinking water. J Dent
Res. 1951;30:172. When staining is seen as a result of tetracy-
Pendrys DG, Stamm JW. Relationship of total fluo- cline administration, it is generally diffuse
ride intake to beneficial effects and enamel fluorosis. and uniform as opposed to that of fluorosis,
J Dent Res. 1990;69:529-556.
which is brown and mottled. Tetracycline
fluoresces yellow, whereas porphyria is
associated with red fluorescence. A history
TETRACYCLINE STAINING of drug use is, of course, the key in making
Figure 11-50 the diagnosis.
Sex: No predilection
TREATMENT
CLINICAL FEATURES Severely discolored anterior teeth may
Tetracycline antibiotics act as a vital dye, be cosmetically corrected by porcelain-
being incorporated into bone and dentin veneered crowns when bleaching methods
during osteogenesis and dentinogenesis, are unsuccessful.
respectively. The antibiotic becomes highly
concentrated in dentin and renders the
teeth yellow or yellowish brown. Under
ultraviolet light, a bright yellow or yellow-
Additional Reading
ish-green fluorescence is observed. Discol- Baden E. Environmental pathology of the teeth. In Gorlin
oration as seen clinically depends on dose RJ, Goldman HM, eds. Thoma’s Oral Pathology, Vol.
I. 6th ed. St. Louis, MO: C. V. Mosby; 1970: 189.
and duration of drug administration. The Lin LC, Pitts DL, Burgess LW Jr. An investigation into
drug is deposited only during dentinogen- the feasibility of photobleaching tetracycline-stained
esis. Most examples of severe discolorations teeth. J Endodont. 1988;14:293.
are seen in children requiring long-term Primosch RE. Tetracycline discoloration, enamel defects,
and dental caries in patients with cystic fibrosis. Oral
antibiotic therapy; relatively short courses Surg Oral Med Oral Pathol. 1980;50:301.
of drug use usually fail to produce any sig- Sánchez AR, Rogers RS 3rd, Sheridan PJ. Tetracycline
nificant clinical manifestations. Ground and other tetracycline-derivative staining of the teeth
sections of teeth examined under fluores- and oral cavity. Int J Dermatol. 2004;43(10):709-
715.
cence microscopy show linear deposits in Shafer WG, Hine MK, Levy BM. A Textbook of Oral
dentin corresponding temporally to drug Pathology. 4th ed. Philadelphia, PA: W. B. Saunders;
intake. 1983: 581.
PMPH_Eversole_Chapter-11.indd 607 1/20/2011 3:16:21 PM
608 Chapter 11
FIGURE 11-50
Brownish-yellow pigmen-
tation in teeth of patients
receiving tetracycline over
a long period of time.
Patient on left has porce-
lain-fused-to-metal (PFM)
crowns on lower anterior
teeth.
FIGURE 11-51
Right: extrinsic stain from
betel nut chewing. On the
left: chromogenic bacteria
impart a yellow stain to
the dental biofilm.
EXTRINSIC STAINING bacteria are probably responsible. In adults,
Figure 11-51 brown or black stains are usually attribut-
able to tobacco or caffeine.
Sex: No predilection
DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES Extrinsic stains can be differentiated from
Extrinsic staining is generally confined the other forms of dental pigmentation
to the cervical enamel, whereby extrinsic included here on the basis of location, being
pigments become incorporated into dental confined to the cervical one third of the
plaque or calculus deposits. The color of tooth crown, and the fact that they can be
the deposit varies according to the agent scaled from the tooth surface.
responsible. In children, green stain is most
frequent. It is common and most prominent
on maxillary anterior teeth. The cause has
Additional Reading
not clearly been identified but may repre- Ayers P. Green stain. J Am Dent Assoc. 1939;26:2.
sent chlorophyll or deposits of chromogenic Boyle PE, Dinnerman M. Natural vital staining of the
teeth of infants and children. Am J Orthod Dentofac
bacteria. Orange stain, also seen in children, Orthop. 1941;27:377.
is believed to evolve as a result of coloniza- Leung SW. Naturally occurring stains on the teeth of
tion by chromogenic bacteria. Neither green children. J Am Dent Assoc. 1950;41:191.
nor orange stains have any pathogenic con- Sutcliffe P. Extrinsic tooth staining in children. Dent
Pract. 1967;17:175.
sequences. Rarely, black or brown stains Van Reenen JF. Tobacco: the effects of its use with spe-
are encountered on deciduous teeth and, as cial reference to the mouth and dental elements: a sur-
with green or orange stains, chromogenic vey of the literature. J Dent Assoc S Afr. 1954;9:334.
PMPH_Eversole_Chapter-11.indd 608 1/20/2011 3:16:27 PM
Dental Defects 609
FIGURE 11-52
Focal dental pigmentation
in pulp necrosis of central
incisor, left, pink tooth
Mummery due to internal
resorption.
FOCAL PIGMENTATION Internal coronal resorption can be easily
Figure 11-52 differentiated from the pigmentation associ-
ated with pulp necrosis on the basis of color
Sex: No predilection differences, radiographs, and response to
CLINICAL FEATURES pulp testing.
Pigmentation of a single tooth is seen in pulp TREATMENT
necrosis and internal coronal resorption. In
pulp necrosis, the affected tooth shows a Because pink teeth with coronal internal
brown or gray discoloration, which results resorption fracture easily, pulp extirpation
from deposition of hemosiderin pigment with endodontic therapy and a prosthetic
and necrotic tissue products. Radiographs crown are indicated. Pigmented nonvital
usually disclose the presence of a periapi- teeth should be treated similarly, and the
cal radiolucency; coronal internal resorp- discoloration can be managed by peroxide
tion has no known etiology, yet may be the bleaching.
result of trauma. The affected tooth appears
pink (pink tooth of Mummery) because of
pulpal enlargement subsequent to internal Additional Reading
resorption of dentin. Radiography discloses Nuttling EB, Poe GS. Chemical bleaching of discolored
focal pulp chamber enlargement. endodontically treated teeth. Dent Clin North Am.
1967;Nov:655-662.
DIFFERENTIAL DIAGNOSIS Padayachee A. Pigmentation of teeth: a review. J Forensic
Odonto-Stomatol. 1988;6:67.
The other pigmentations listed here are Sweet APS. Internal resorption, a chronology. Dent
generalized or involve more than one tooth. Radiogr Photogr. 1965;38:75.
PMPH_Eversole_Chapter-11.indd 609 1/20/2011 3:16:33 PM
a
1 2 3 4
5 6 7
8 9 10
1 2
1 2 3
4 5 6
Pain and Neuromuscular Disorders
a-1, Ophthalmic division pain; a-2, Maxillary division pain; a-3, Mandibular division pain; a-4, Wandering
pain; a-5, Otologic pain; a-6, Myofascial pain; a-7, Upper cervical pain; a-8, TMJ internal derangement; a-9,
Sialogenic pain; a-10, Temporal pain; b-1, Mental nerve paresthesia/hypoesthesia; b-2, lnfraorbital paresthe-
sia/hypoesthesia; c-1, Peripheral nerve VII paralysis; c-2, CNS nerve VII paralysis; c-3, Horner’s syndrome;
c-4, Ophthalmoplegia; c-5, Nerve XII paralysis; c-6, V Motor paralysis, X paralysis
PMPH_Eversole_Chapter-12.indd 610 1/20/2011 3:18:37 PM
Facial Pain and
Neuromuscular
Disorders
12
STOMATODYNIA/GLOSSOPYROSIS 633
Ophthalmic Division Pain 614 ATYPICAL FACIAL PAIN†
ODONTOGENIC INFECTION 614 CARDIOGENIC FACIAL PAIN 634
FRONTAL/ETHMOIDAL SINUSITIS 615
MYOGENIC PAIN* Wandering Facial Pain
POSTHERPETIC NEURALGIA†
TRIGEMINAL NEURALGIA† ATYPICAL AND PSYCHOGENIC PAIN†
CRANIAL BASE AND CNS MYOGENIC PAIN*
NEOPLASMS†
VASCULAR OCCLUSIVE DISEASE Otogenic Pain 634
AND ANEURYSMS 616
ACUTE OTITIS MEDIA 634
Maxillary Division Pain 616 CHRONIC OTITIS MEDIA 635
HERPES ZOSTER OTICUS 636
ODONTOGENIC INFECTION 616
MIDDLE EAR NEOPLASMS 637
MAXILLARY SINUSITIS 617
ODONTOGENIC INFECTION‡
PATHOLOGIC JAWBONE CAVITIES 619
TRAUMATIC NEUROMA ‡
ANTRAL AND MAXILLARY
Neck and Throat Pain 638
NEOPLASMS 620 STYLOHYOID SYNDROME (EAGLE’S
CLUSTER HEADACHE 621 SYNDROME) 638
TRIGEMINAL NEURALGIA 623 HYOID SYNDROME 638
POSTHERPETIC NEURALGIA 624 SUBACUTE THYROIDITIS‡
COMPLEX REGIONAL PAIN GLOSSOPHARYNGEAL
SYNDROME (CAUSALGIA) 625 NEURALGIA 639
CRANIAL BASE AND CNS CAROTIDYNIA 640
NEOPLASMS 626
SUPERIOR LARYNGEAL
ATYPICAL FACIAL PAIN 628
NEURALGIA 641
LARYNGEAL NEOPLASMS 641
Mandibular Division Pain 629
ODONTOGENIC INFECTION 629 TMJ Region Pain 642
TRIGEMINAL NEURALGIA†
MYOGENIC PAIN 642
POSTHERPETIC NEURALGIA†
CAUSALGIA* TYPE I INTERNAL DERANGEMENT 644
PATHOLOGIC JAWBONE CAVITIES† TYPE II INTERNAL DERANGEMENT 646
OSTEOMYELITIS 630 TYPE III INTERNAL
TRAUMATIC NEUROMA 631 DERANGEMENT 647
SUBACUTE THYROIDITIS 632 MENISCUS PERFORATION 648
CRANIAL BASE AND CNS OSTEOARTHRITIS 649
NEOPLASMS† RHEUMATOID ARTHRITIS 650
PMPH_Eversole_Chapter-12.indd 611 1/20/2011 3:18:38 PM
ACUTE INFECTIOUS MYOGENIC PAIN*
ARTHRITIDES 651 INTERNAL TMJ DERANGEMENT*
MISCELLANEOUS ARTHRITIDES 652 POSTINJECTION/POSTINFECTION
CONDYLAR FRACTURE 653 TRISMUS 670
SYNOVIAL CHONDROMATOSIS 654 CONVERSION TRISMUS 671
PIGMENTED VILLONODULAR SUBCONDYLAR FRACTURE*
SYNOVITIS 655
ANKYLOSIS 671
TMJ REGION NEOPLASMS**
HECHT-BEALS-WILSON
ODONTOGENIC INFECTION‡ SYNDROME 672
OTITIS MEDIA§
CORONOID HYPERPLASIA 673
CONDYLAR HYPERPLASIA 673
Sialogenic Pain 656
TMJ REGION NEOPLASMS 674
SIALOLITHIASIS 656 SCLERODERMA 676
ENDEMIC PAROTITIS 657 ORAL SUBMUCOUS FIBROSIS 676
ACUTE SUPPURATIVE TETANUS 677
SIALADENITIS 658
Generalized Motor Function
Temporal Pain 659 Disorders 678
MIGRAINE 659
AURICULOTEMPORAL
MYOGENIC PAIN 659 SYNDROME 678
GIANT CELL ARTERITIS 660
JAW-WINKING PHENOMENON 679
MOTOR SYSTEM DISEASE 680
Paresthesia 661
MULTIPLE SCLEROSIS 680
MENTAL PARESTHESIA 661 MUSCULAR DYSTROPHIES 681
INFRAORBITAL PARESTHESIA 662 MYOTONIAS 682
CONGENITAL FACIAL DIPLEGIA 683
Localized Motor Deficits 664 HEMIFACIAL ATROPHY 683
FACIAL PARALYSIS 664 MYASTHENIA GRAVIS 684
HORNER’S SYNDROME 665
OPHTHALMOPLEGIA 666
HYPOGLOSSAL PARALYSIS 667
SOFT PALATE PARALYSIS 668 *Refer to TMJ Region Pain.
†Refer to Maxillary Division Pain.
Limited and Deviant ‡Refer to Mandibular Division Pain.
§Refer to Otogenic Pain.
Mandibular Opening 669
**Refer to Limited and Deviant Mandibular
MUSCLE SPLINTING 669 Opening
PMPH_Eversole_Chapter-12.indd 612 1/20/2011 3:18:38 PM
Pain in the maxillofacial region is usually, When no organic source for facial
and significantly, a symptom heralding pain can be detected, the clinician is always
the presence of an infectious or inflamma- concerned that a brain tumor or abscess is
tory disease process. The more prevalent potentially causative. Lethal nervous sys-
sources of facial pain include odontogenic tem malignancies rarely cause facial pain;
infections, trauma, periodontal infections yet, when they do, there is usually a persis-
(abscess), sinusitis, otitis, salivary obstruc- tent paresthesia with a concomitant deficit
tion, internal derangements of the temporo- in motor function of ocular, facial, or masti-
mandibular joint (TMJ), and myofascial catory muscles.
psychofunctional disorders. Most organic Many pain disorders share common
diseases manifest acute pain, whereas rare symptoms. The specific disorders can often
pain syndromes and psychogenic pain be differentiated on the basis of the char-
disorders are chronic. Patients who have acter, location, and duration of sensory
organic disorders usually present obvious alterations considered in conjunction with
clinical signs uncovered by a thorough den- the physical and radiographic findings.
tal, oral, and facial physical examination. A definitive diagnosis of some diseases
After appropriate tests have been performed requires an extensive work-up, cranial
(including sensitivity testing of teeth to nerve function tests, therapeutic trials, labo-
hot and cold stimuli, percussion of teeth, ratory data, and expert psychiatric analysis.
occlusal stressing and fiberoptic evaluation The characteristics allowing for a definitive
for cracked teeth, vitalometric testing, and diagnosis along with recommendations for
periodontal probing), a diagnosis can usu- the work-up protocol are outlined for each
ally be rendered. entity.
Many of the diseases included in this The diagnosis of chronic facial pain
chapter show no identifiable organic lesions. can be problematic and evasive. In addition,
They represent defects in sensory percep- those patients with psychiatric disorders are
tion, vasodilatory phenomena, or symp- frequently demanding, abrasive, and other-
toms associated with psychologic disorders wise difficult to manage; a team approach
such as endogenous depression, conversion is recommended in such cases. Further-
reactions, stress-associated myospasm, or more, the clinician should be advised that
delusionary phenomena. As mentioned more than one process may be involved,
previously, most of these disorders have not and therefore more than one diagnosis
been found to be associated with any his- may be made. For example, a given patient
topathologic alteration in the tissues and may suffer from concurrent myogenic pain,
are usually characterized by chronic pain. an internal derangement of the TMJ, and
Furthermore, paroxysmal chronic pain is migraine headaches.
more often seen as a symptom of trigemi- This chapter also includes motor func-
nal neuralgia or vasoactive pain (cluster or tion disorders that involve the muscles of
migrainous facial pain). facial expression and mastication. The gna-
To aid the clinician in developing a thologic apparatus may be affected by dis-
differential diagnosis, the pain symptoms eases causing pain in the TMJ area. Some
are classified according to location. The of these TMJ pain problems exhibit an
more common entities such as organic pain attending motor defect such as limitation in
of odontogenic, periodontal, sinus, and opening or deviant function. Alternatively,
salivary origin are described first, followed jaw functional movements may exist in the
by the more esoteric entities represent- absence of pain. TMJ diseases are included
ing vasoactive, neuralgic, and psychogenic here under both categories. In addition, rare
disorders. neurologic and muscular disease processes
PMPH_Eversole_Chapter-12.indd 613 1/20/2011 3:18:38 PM
614 Chapter 12
of a systemic nature can affect the facial referred solely to the medial supraorbital
musculature. Differentiation among the area. The frontal pain is a constant moder-
specific disorders requires evaluation of ate ache with or without throbbing. Patients
the muscle groups involved in paralysis or complaining of medial frontal pain should
deviant function. be examined for an incriminating anterior
maxillary tooth; thus, evaluation for den-
tal caries, tooth percussion sensitivity, pulp
Ophthalmic Division Pain test response, and periapical radiographic
changes are required. Rarely, an odonto-
ODONTOGENIC INFECTION genic infection may spread to the orbit,
Figure 12-1 resulting in orbital cellulitis.
Age: No predilection
DIFFERENTIAL DIAGNOSIS
Sex: No predilection
CLINICAL FEATURES Odontogenic infection is easily differenti-
ated from the other entities included here if
Frontal pain of odontogenic origin is rare. the clinician is aware that dental infections
It represents referred pain from an acute can refer pain to this region.
pulpitis or acute apical periodontitis associ-
ated with the maxillary incisors or canines. TREATMENT
Pain is usually experienced in the infected
tooth as well, yet occasionally may be The infected tooth should be treated endo-
dontically and subsequently restored with a
crown of porcelain fused to metal. When evi-
dence of suppuration is observed, it is advis-
able to obtain a culture with sensitivity. When
facial swelling and fever are present, antibi-
otic therapy is indicated: a 1-week course of
penicillin, or erythromycin for patients with
penicillin allergy. In the absence of response,
the possibility of staphylococcal or anaerobic
infection must be considered with selection
of appropriate antibiotics (e.g., cloxacillin or
clindamycin, respectively).
Additional Reading
Glick DH. Locating referred pulpal pains. Oral Surg
Oral Med Oral Pathol. 1962;15:613.
Hovinga J, Christiaans BJ. Odontogenic infection lead-
ing to orbital cellulitis as a complication of fracture
of the zygomatic bone. J Craniomaxillofac Surg.
1987;15:254.
Olsen RE, Morello JA, Keiff ED. Antibiotic treatment
of oral anaerobic infections. J Oral Maxillofac Surg.
1976;33:619.
Robertson S, Goodell H, Wolff HG. The teeth as a source
of headache and other pain. Arch Neurol Psychiatr.
FIGURE 12-1 1947;57:277.
Frontal pain referral from anterior maxillary odon- Sicher H. Problems of pain in dentistry. Oral Surg Oral
togenic infection. Med Oral Pathol. 1954;7:149.
PMPH_Eversole_Chapter-12.indd 614 1/20/2011 3:18:39 PM
Facial Pain and Neuromuscular Disorders 615
FRONTAL/ETHMOIDAL with frontal swelling and pain (Pott’s puffy
SINUSITIS tumor) and may progress to death.
Figure 12-2
DIFFERENTIAL DIAGNOSIS
Age: Primarily adults Acute frontal sinusitis may be confused with
Sex: No predilection referred pain of odontogenic origin. Dental
CLINICAL FEATURES examination and evaluation of sinus radio-
The frontal sinuses may be chronically graphs aid in arriving at a diagnosis. Myo-
inflamed because of allergy; patients are genic pain involving the frontalis muscle
generally asymptomatic, although some is usually bilateral, dull, and diffuse; elec-
complain of pressure or a mild dull ache. tromyographic readings from the frontalis
Allergic frontal sinusitis is rarely local- muscle are elevated. The other disorders
ized; the other sinus cavities are also listed here manifest specific symptoms,
inflamed, and chronic rhinitis is usually allowing for exclusion from the differential
observed. Acute frontal sinusitis is usu- diagnosis of acute ophthalmic division pain.
ally infectious; it frequently occurs after
TREATMENT
water is forced into the nose, thus affect-
ing swimmers. A deviated septum or pres- As the nasofrontal communication is usu-
ence of nasal polyps also may predispose ally blocked because of edema, a nasal
to frontal sinusitis. The patient complains decongestant spray should be used in con-
of severe throbbing pain in the medial junction with antibiotics. Penicillin or one
supraorbital region. Water’s sinus radio- of the cephalosporins is the antibiotic of
graphs generally exhibit opacification choice. When the patient’s response is poor,
as a result of accumulation of a purulent the sinus may require irrigation or surgical
exudate within the sinus cavity. Lowering intervention.
the head often exacerbates or intensifies the
pain. Hemophilus influenzae and anaerobic
organisms are the more prevalent microbial Additional Reading
agents. If left untreated, swelling and red-
Frederick J, Brande AI. Anaerobic infection of the para-
ness of the upper eyelid may be seen and nasal sinuses. N Engl J Med. 1974;290:135.
brain abscess can occur. Also, the infec- Kennedy DW, Loury MC. Nasal and sinus pain: current
tion may progress to an acute osteomyelitis diagnosis and treatment. Semin Neurol. 1988;8:303.
FIGURE 12-2
Clouded ethmoid sinuses in acute sinusitis.
PMPH_Eversole_Chapter-12.indd 615 1/20/2011 3:18:40 PM
616 Chapter 12
McDermott C, O’Sullivan R, McMahon G. An unusual system (CNS) vascular lesions cause pari-
cause of headache: Pott’s puffy tumour. Eur J Emerg etal or occipital headache, yet many patients
Med. 2007;14(3):170-173.
Singletary EM, Reilly JF, Jr. Acute frontal sinus barotrau- complain of unilateral frontal and retro-or-
ma. Am J Emerg Med. 1990;8:329. bital pain, which is frequently throbbing.
Wilson WR, Montgomery WM. Infections and granu-
lomas of the nasal airways and paranasal sinuses. In: DIFFERENTIAL DIAGNOSIS
Paparella MM, Shumrick DA, eds. Otolaryngology.
2nd ed. Philadelphia, PA: W. B. Saunders; 1980:1972. When the classic signs and symptoms of
both cluster and tension headache are lack-
ing and frontal sinus and odontogenic pain
VASCULAR OCCLUSIVE
sources have been excluded, a CNS lesion,
DISEASE AND ANEURYSMS either vascular or neoplastic, should be sus-
Figure 12-3 pected, particularly when other neurologic
deficits can be detected.
Age: Adults
Sex: No predilection TREATMENT
CLINICAL FEATURES
When other pain syndromes have been
Thrombosis of the internal or common eliminated and a vascular occlusive or
carotid may cause unilateral cranial edema aneurysmal source is suspected, referral
with headache occurring on the affected side. to a neurologist is recommended. A spinal
Transient ischemia may also be associated tap, computed tomographic (CT) scans, and
with pain. Aneurysms and arteriovenous carotid angiograms are of great importance
malformations have been associated with diagnostically for localizing the lesion.
headache often mimicking migraine with
contralateral visual disturbances; intracranial
bruit is usually detectable. Ruptured aneu- Additional Reading
rysms lead to subarachnoid hemorrhage and Grindal AB, Toole JF. Headache and transient ischaemic
often follow sexual intercourse or physical attacks. Stroke. 1974;5:603.
exertion. Other neurologic deficits are often Lance JW. Chap. 7. Mechanisms and Management of
encountered, including hemiparesis, third Headache. 3rd ed. London, Butterworths; 1978.
Mathew NT. Chap. 13. Headache of neurologic origin.
nerve palsy, or palsy involving other cranial In: Ryan RE, Sr, Ryan RE, Jr. Headache and Head
motor nerves. Some of these central nervous Pain. St Louis, MO: C. V. Mosby; 1978.
Mathys J, Lachat M, Herren T. Headache as a manifesta-
tion of a life-threatening vascular disorder. Headache.
2004;44(7):706-709.
Zachariades N, Papavassiliou D. Traumatic carotid-cavern-
ous sinus fistula. J Craniomaxillofac Surg. 1988;16:385.
Maxillary Division Pain
ODONTOGENIC INFECTION
Figure 12-4
Age: No predilection
Sex: No predilection
CLINICAL FEATURES
FIGURE 12-3
Frontal area pain is occasionally associated with A: Maxillary teeth with pulpitis or pulp
vascular occlusive disease or B: aneurysms (carotid necrosis with acute apical periodontitis
angiography). will exhibit pain in the maxilla. The pain
PMPH_Eversole_Chapter-12.indd 616 1/20/2011 3:18:45 PM
Facial Pain and Neuromuscular Disorders 617
is localized to the infected tooth or may be tion anesthesia, and favorable response
diffusely distributed over the malar region. to analgesic drugs allow for a definitive
It is a dull aching pain or may progress to diagnosis.
severe throbbing. The tooth is sensitive to
heat, cold, and/or percussion. Periapical TREATMENT
radiographs should be obtained to evalu-
ate for apical widening of the periodontal Root canal therapy or extraction, when the
ligament space or a gross periapical radio- affected tooth is nonrestorable, is the treat-
lucency. When radiographs yield negative ment of choice. When patients are febrile or
findings and no carious lesions are encoun- show facial swelling, 10-day treatment with
tered, fiberoptic examination for cracks penicillin or erythromycin, in the presence
should be performed. Local infiltration of penicillin allergy, is advisable. Patients
anesthesia may be used diagnostically. who do not respond should be reevaluated
for staphylococcal penicillinase-positive
DIFFERENTIAL DIAGNOSIS organisms or anaerobes, especially bacte-
A variety of pain syndromes affect the sec- roides. In these instances, penicillinase-
ond division region of the trigeminal nerve. resistant antibiotics or clindamycin should
These disorders generally manifest charac- be prescribed, respectively.
teristic symptoms, yet many mimic tooth-
ache. Identification of an acutely infected
or necrotic tooth, relief of pain by infiltra- Additional Reading
Chow AW, Roser SM, Brady FA. Oralfacial odontogenic
infections. Ann Intern Med. 1978;88:392.
Glick DH. Locating referred pulpal pains. Oral Surg
Oral Med Oral Pathol. 1962;15:613.
Kannangara DW, Thadepelli H, McQuiter JL.
Bacteriology and treatment of dental infections. Oral
Surg Oral Med Oral Pathol. 1980;50:103.
Oshima K, Ishii T, Ogura Y, Aoyama Y, Katsuumi I.
Clinical investigation of patients who develop neu-
ropathic tooth pain after endodontic procedures.
J Endod. 2009;35(7):958-961.
Robertson S, Goodell H, Wolff HG. The teeth as a source
of headache and other pain. Arch Neurol Psychiatr.
1947;57:277.
MAXILLARY SINUSITIS
Figure 12-5
Age: Adults
Sex: No predilection
CLINICAL FEATURES
Chronic maxillary sinusitis is usually aller-
gic in origin and develops secondary to
chronic rhinitis. As the nasal mucous mem-
branes become congested and edematous
FIGURE 12-4 secondary to allergen:IgE-mediated inflam-
Paranasal pain referred from maxillary odontogenic mation, the ostium of the maxillary sinus
infection. becomes occluded. The sinus membranes
PMPH_Eversole_Chapter-12.indd 617 1/20/2011 3:18:48 PM
618 Chapter 12
may become inflamed and thickened, or purulent nasal discharge may be experi-
the antral cavity may partially or entirely enced and should be cultured. Hemophilus
fill with secretions. The pain is dull, ach- influenzae, Streptococcus pneumoniae, and
ing, and constant. All posterior maxil- Staphylococcus aureus are the bacteria most
lary teeth on the affected side ache and frequently cultured. Occasionally, acute
are sensitive to percussion; malar tender- sinusitis is caused by odontogenic infec-
ness to percussion also may be witnessed. tion, thus necessitating a thorough dental
Pain increases when the head is lowered examination.
between the knees. Nasal examination
discloses edematous and erythematous DIFFERENTIAL DIAGNOSIS
mucous membranes over the lateral wall Chronic maxillary sinusitis may have fea-
and turbinates. Water’s sinus radiographs tures suggesting odontogenic infection.
or maxillary sinus tomograms fail to show Cluster headaches and trigeminal neural-
osseous destruction or expansion. The gia are severe and paroxysmal. Neoplasms
sinus membrane is thickened, a fluid level of sinus or cranial base origin generally
may be detected, or the entire antral cavity manifest a sensory and/or motor deficit.
may be diffusely opacified. Acute sinus- Dull aching pain with rhinitis, congestion,
itis, which is usually infectious in origin, and pandental percussion sensitivity in the
manifests similar radiographic changes; affected maxilla along with radiographic
the patient experiences intense acute evidence of nondestructive antral disease
throbbing pain. In addition, a periodic are usually adequate signs and symptoms
FIGURE 12-5
Clouded sinuses in chronic maxil-
lary sinusitis: air/fluid level (upper
left), diffuse opacification (upper
right), antral polyp (lower left),
diffuse opacification (lower right).
PMPH_Eversole_Chapter-12.indd 618 1/20/2011 3:18:49 PM
Facial Pain and Neuromuscular Disorders 619
for diagnosis. If osseous destruction or and mandibular pain; furthermore, while
expansion is noted radiographically, an most cases fail to show pathology, lucent foci
antral biopsy should be performed. may sometimes be seen. The focus is usually
located within one jaw with upper-to-lower
TREATMENT or lower-to-upper pain referral patterns.
Chronic sinusitis should be treated with Patients may complain of classic trigemi-
nasal decongestant sprays, such as phe- nal neuralgia symptoms with an identifi-
nylephrine hydrochloride, and antihista- able trigger zone, or they may present with
mines. Occasionally, sinus irrigation and constant, dull, aching, or burning pain with
lavage are necessary. Acute sinusitis should unilateral distribution. The pain develops
be treated promptly with penicillin or after tooth extraction either immediately or
erythromycin, in the presence of penicillin many years later. In the absence of odonto-
allergy; if a purulent exudate is present, cul- genic or antrogenic infection, radiographs
ture and sensitivity tests are required. are used to identify edentulous zones on
the ipsilateral side for diagnostic infiltra-
tion anesthesia. Three percent mepivicaine,
Additional Reading 0.25 ml, is injected subperiosteally over the
suspected site. Abolition of pain then war-
Berg O, Lejdeborn L. Experience of a permanent ven- rants surgical exploration of the edentu-
tilation and drainage system in the management of
purulent maxillary sinusitis. Ann Otol Rhinol Laryngol.
lous region. Failure to achieve pain relief
1990;99:192. by local infiltration anesthesia requires
Evans FO, Jr, Sydnor JB, Moore WE. Sinusitis of the readministration to a closely adjacent site
maxillary antrum. N Engl J Med. 1975;293:735. until pain ablation is achieved, thereby
Kennedy DW, Loury MC. Nasal and sinus pain: current
diagnosis and treatment. Semin Neurol. 1988;8:303.
precisely pinpointing the location of the
Marple BF, Stankiewicz JA, Baroody FM, et al; American suspected bone cavity. Surgery will reveal
Academy of Otolaryngic Allergy Working Group on cavitation of the medullary region with soft
Chronic Rhinosinusitis. Diagnosis and management tissue contents. Histologically, these bone
of chronic rhinosinusitis in adults. Postgrad Med.
cavities are represented by vascular con-
2009;121(6):121-139.
Ryan RE, Jr, Kern EB. Rhinologic causes of facial pain nective tissue and occasionally exhibit a
and headache. Headache. 1978;18:44. mononuclear inflammatory cell infiltrate.
Microbiologic studies have disclosed the
presence of a mixed aerobic-anaerobic flora.
PATHOLOGIC JAWBONE Some of these patients have an associated
CAVITIES coagulopathic hematologic disorder.
Figure 12-6
DIFFERENTIAL DIAGNOSIS
Age: Middle-aged and elderly adults
Sex: No predilection Odontogenic and antrogenic sources of pain
should be ruled out initially. Reported pain
CLINICAL FEATURES
referral patterns associated with pathologic
The existence of radiologically nondemon- bone cavities are often diffuse and may extend
strable bone cavities in extraction site foci beyond the alveolus to involve the maxillary,
within the jaws has been reported to be etio- temporal, or TMJ regions; therefore, myo-
logically related to both atypical facial pain genic facial pain, internal derangements of
and trigeminal neuralgia. This condition is the TMJ, and temporal arteritis should be con-
also termed neuralgia-inducing cavitational sidered in the differential diagnosis. Elimina-
osteonecrosis. Both jaws are affected and tion of pain with local infiltration anesthesia
many patients experience both maxillary over an extraction site supports a diagnosis
PMPH_Eversole_Chapter-12.indd 619 1/20/2011 3:18:55 PM
620 Chapter 12
FIGURE 12-6
Idiopathic bone cavitation:
vague radiolucent foci in
the mandible associated
with jaw pain.
of bone cavity–related neuralgia. It should be Shaber EP, Krol AJ. Trigeminal neuralgia—a new treatment
noted that this entity is controversial and is concept. Oral Surg Oral Med Oral Pathol. 1980;49:286.
not accepted by many surgeons.
ANTRAL AND MAXILLARY
TREATMENT
NEOPLASMS
The edentulous site is approached surgi- Figure 12-7
cally after a flap reflection. The contents are
curetted and the space is packed with gauze Age: Predilection depends on nature of disease
impregnated with 500 mg tetracycline/ml Sex: Male predilection
sterile water. This packing is replaced until CLINICAL FEATURES
healthy granulation tissue appears, after
which the packing is removed. Chloromy- Maxillary and antral neoplasms are often
cetin also has been used in the packing. It asymptomatic in the early stages of prolifer-
should be noted that most clinicians report- ation. Pain may develop later in the course
ing this form of treatment for facial pain of the disease and is usually accompanied
have not included follow-up evaluation by paresthesia. Infraorbital paresthesia
over 18 months for most patients; however, and pain occur when the neoplasm, usu-
a small number of patients have been pain ally a malignant tumor, grows superiorly
free for 2 to 5 years. to involve the sinus roof. Antral carcinomas
often undergo foci of necrosis with second-
ary infection, which can result in release
Additional Reading of endogenous pain mediators. The pain
is usually deep seated and may be maxil-
Bouquot JE. More about neuralgia-inducing cavitation-
al osteonecrosis (NICO). Oral Surg Oral Med Oral
lary, retro-orbital, or dental in distribution.
Pathol. 1992;74(3):348-350. Water’s radiographs, maxillary sinus tomo-
Gruppo R, Glueck CJ, McMahon RE, et al. The grams, and CT scans disclose diffuse antral
pathophysiology of alveolar osteonecrosis of the jaw: opacification with sinus wall erosion.
anticardiolipin antibodies, thrombophilia, and hypofi-
brinolysis. J Lab Clin Med. 1996;127(5):481-488.
Ratner EJ, Person P, Kleinman DJ, Shklar G, Socransky
DIFFERENTIAL DIAGNOSIS
SS. Jawbone cavities and trigeminal and atypical facial Pain associated with sinus cancer is usu-
neuralgias. Oral Surg Oral Med Oral Pathol. 1979;48:3.
Roberts AM, Person P. Etiology and treatment of idio-
ally coexistent with paresthesia. Occasion-
pathic trigeminal and atypical facial neuralgias. Oral ally, no sensory deficit is encountered. In
Surg Oral Med Oral Pathol. 1979;48:298. these instances, the pain symptoms mimic
PMPH_Eversole_Chapter-12.indd 620 1/20/2011 3:18:55 PM
Facial Pain and Neuromuscular Disorders 621
FIGURE 12-7
Antral carcinoma with
palatal bone perfora-
tion; magnetic resonance
imaging and computed
tomographic scans show-
ing opacification and bony
expansion.
odontogenic pain or acute sinusitis. Radio- Boles R. Paransal sinuses and facial pain. In Alling III,
graphic opacification along with sinus wall EC, Mahan PE, eds. Facial Pain. 2nd ed. Philadelphia,
PA: Lea & Febiger; 1977:120.
erosion or expansion warrants a Caldwell- Ellinger RF, Kelly WH. Maxillary sinus lymphoma: a
Luc access or endoscopy with biopsy. consideration in the diagnosis of odontogenic pain.
J Endodont. 1989;15:90.
TREATMENT Frazell EL, Lewis JS. Cancer of the nasal cavity and
accessory sinuses; a report of the management of 416
Most sinus tumors with pain and paresthe- patients. Cancer. 1963;16:1293.
sia are malignant. Squamous cell carcinoma Saund D, Kotecha S, Rout J, Dietrich T. Non-resolving
and adenocarcinoma are managed by hemi- periapical inflammation: a malignant deception. Int
Endod J. 2010;43(1):84-90.
maxillectomy. Because the tumor may per-
forate into the nasal cavity, other paranasal
sinuses, or the cranium, a thorough clini- CLUSTER HEADACHE
cal and radiographic evaluation is needed Figure 12-8
to determine the extent of disease and the
form of treatment. Age: Middle-aged adults
Sex: Male predilection
Additional Reading CLINICAL FEATURES
Barat M, Rybak LP, Mann JL. Fibrous dysplasia mas-
A variety of eponymic designations, which
querading as chronic maxillary sinusitis. Ear Nose relate to the precise location of pain, have
Throat J. 1989;68:42. been applied to a group of midface vasoac-
PMPH_Eversole_Chapter-12.indd 621 1/20/2011 3:18:56 PM
622 Chapter 12
tive headaches (Vail’s syndrome, Horton’s nial or internal maxillary artery branches
headache, Sluder’s neuralgia, Charlin’s syn- is thought to be pathogenetically related
drome). Sphenopalatine neuralgia, vidian to the condition. Platelet-rich plasma sero-
neuralgia, petrosal neuralgia, and ciliary tonin and histamine levels are elevated,
neuralgia are all forms of midface cluster and the platelet count is decreased during
or vasoactive headaches. Two clinical pre- attacks. Electroencephalograms, CT scans,
sentations are observed. The chronic form and radionuclide brain scans are usually
persists throughout the year, whereas the normal.
episodic form is seasonal with pain attacks
being more frequent in the spring. In both DIFFERENTIAL DIAGNOSIS
forms, the nature of the pain attacks is simi- Cluster headaches, being paroxysmal, may
lar. The pain is severe and sharp, lasting 15 to be confused with trigeminal neuralgia
20 minutes, being unilaterally located in the involving the maxillary division. Absence
maxilla, retro-orbital, or supraorbital region. of a trigger zone, presence of autonomic
There is no trigger zone. The attacks occur signs and symptoms (lacrimation, nasal
once or twice daily, and nocturnal episodes stuffiness, conjunctival erythema), and
following random eye movement sleep are other aforementioned features are char-
common. Patients report no visual scoto- acteristic for cluster headache. The other
mata or other “aura” prodromal changes lesions causing maxillary pain fail to mani-
as seen in classic migraines. The concur- fest the episodic paroxysmal symptoms of
rent observation of ipsilateral conjunctival cluster headache.
erythema, palpebral edema, lacrimation,
and nasal stuffiness is significant diagnos- TREATMENT
tically. Patients with cluster headache often
exhibit a ruddy facial complexion. Alco- In the past, the treatment of choice was sub-
holism, peptic ulcer, and hypertension are lingual ergotamine tartrate or ergotamine
also common concomitants. Although the tartrate and caffeine rectal suppositories,
cause is unknown, vasodilation of the cra- which are used during a pain attack. Meth-
ysergide and prednisone are effective in the
prevention of cluster headache, and lithium
carbonate has been shown to be efficacious.
Administration of 100% oxygen at 7 L/
minute flow is more effective for aborting
pain if given at the onset of the attack. Ergot
alkaloids are contraindicated in patients
with hypertension, cardiac, or cerebral vas-
cular occlusive disease. Recently, calcium
channel blockers such as nifedipine (10 mg
t.i.d.) have been successful in relief of pain
from classic, seasonal-type of cluster head-
ache. Verapamil has proved efficacious in
patients with chronic cluster headaches.
FIGURE 12-8
Vessels involved in vasodilation cluster headache:
Additional Reading
sphenopalatine (Sluder’s neuralgia); middle menin- Bussone G, Leone M, Peccarisi C, et al. Double blind
geal (Charlin’s neuralgia), internal carotid (Horton’s comparison of lithium and verapamil in cluster head-
headache), internal maxillary (Vail’s neuralgia). ache prophylaxis. Headache. 1990;30:411.
PMPH_Eversole_Chapter-12.indd 622 1/20/2011 3:19:00 PM
Facial Pain and Neuromuscular Disorders 623
Evers S. Pharmacotherapy of cluster headache. Expert some patients with multiple sclerosis and
Opin Pharmacother. 2010;11(13):2121-2127. progressive systemic sclerosis (scleroderma).
Friedman A, Mikropoulos HE. Cluster headaches.
Neurology. 1958;8:63.
Kudrow L. Response of cluster headache attacks to oxy-
DIFFERENTIAL DIAGNOSIS
gen inhalation. Headache. 1981;21:1. Sharp stabbing paroxysmal pain with iden-
Mathew NT. Advances in cluster headache. Neurol Clin.
1990;8:867.
tification of a discrete trigger zone allows for
Medina JL, Diamond S, Fareed J. The nature of cluster a straightforward clinical diagnosis. Atypi-
headache. Headache. 1979;19:309. cal trigeminal neuralgias, which have no
discrete trigger zone, may be confused with
other facial pain syndromes such as midface
TRIGEMINAL NEURALGIA cluster headache and psychogenic atypical
Figure 12-9 facial pain. Eventually, a trigger zone becomes
evident in most instances. Because neoplasia
Age: Middle-aged and elderly adults may, albeit rarely, underlie the condition,
Sex: Slight female predilection both brain and CT scans are recommended.
CLINICAL FEATURES
TREATMENT
Trigeminal neuralgia or tic douloureux is
The treatment of choice is carbamazepine or
a pain syndrome involving the trigeminal
carbamazepine with phenytoin. High doses
nerve divisions and is of unknown etiology.
of carbamazepine induce bone marrow sup-
It has been speculated that this neuralgia is
the result of ganglionic compression over the
petrous ridge or by an artery or vein. Elec-
tron microscopic evidence of myelin degen-
eration of nerves is observed; these findings
support a peripheral etiology and suggest a
herpetic ganglioneuritis. The clinical symp-
toms are unique and diagnostic. The pain is
sudden, paroxysmal, severe, and stabbing; it
follows one or more divisions of the trigemi-
nal nerve. The right side of the face is most
frequently affected, and the pain is precipi-
tated by touching a specific area of the skin
or mucous membrane referred to as a “trig-
ger zone.” A patient’s trigger zone is consis-
tently in the same region, usually at the lip
commissure or the nasal ala. Local anesthetic
infiltration of the trigger zone causes the pain
to abate temporarily. During the early onset
of pain paroxysms, a discrete trigger zone
may not be apparent. In addition to pain,
many patients experience paresthesia along
the involved nerve division. Most cases are
unilateral; 5% of patients develop bilateral
involvement. The symptoms of trigeminal FIGURE 12-9
neuralgia are occasionally encountered in Trigeminal neuralgia (tic doloreau). Trigger points
association with a CNS neoplasm. Also, (yellow) and distribution of pain paroxysms along
trigeminal neuralgia is known to occur in trigeminal pathways (red).
PMPH_Eversole_Chapter-12.indd 623 1/20/2011 3:19:01 PM
624 Chapter 12
pression, thus necessitating regular blood lar eruption along sensory nerve pathways.
count monitoring. Some patients cannot toler- The virus initially infects sensory ganglia and
ate the drugs and are candidates for thermal subsequently disseminates along the sensory
nucleolysis, peripheral neurectomy, or vascu- nerve terminals in skin or mucosa. The lesions
lar decompression neurosurgical interven- persist for 2 to 3 weeks and are accompanied
tion. Surgical treatment is temporary when by a stinging pain. When the trigeminal gan-
peripheral neurectomies are performed, glion is infected, the lesions generally local-
offering, on the average, 1.5 to 2 years of pain ize in the region of the ophthalmic division;
relief. Radiofrequency thermal nucleolysis to however, both maxillary and mandibular
specific tracts within the trigeminal ganglion divisions may be involved. In older patients,
is effective, yet pain often recurs within 1 or the pain may persist after the lesions have
2 years. Because the procedure is not particu- resolved; if this symptom prevails after 6 to 8
larly invasive, it can be readministered. Vas- weeks, the condition represents postherpetic
cular decompression of the ganglion is also neuralgia. The character of the pain changes
effective, yet not universally. Gamma knife somewhat in that stinging is replaced by
surgery is effective among patients who have burning, aching, and paresthesia. This pain
not had previous surgical interventions. is usually chronic and persistent. Scarified
zones in areas of old vesicular lesions are
hypesthetic when pinched with a needle. The
Additional Reading pain may persist for months or even years
Dhople AA, Adams JR, Maggio WW, Naqvi SA, Regine after infection and, needless to say, results in
WF, Kwok Y. Long-term outcomes of Gamma Knife tremendous emotional upset. Occasionally,
radiosurgery for classic trigeminal neuralgia: impli- paroxysmal stabbing pains mimic trigeminal
cations of treatment and critical review of the lit- neuralgia, although trigger zones are lacking.
erature. Clinical article. J Neurosurg. 2009;111(2):
351-358.
Jannetta PJ. Trigeminal neuralgia and hemifacial DIFFERENTIAL DIAGNOSIS
spasm—etiology and definitive treatment. Trans Am
Neurol Assoc. 1975;100:89.
The pain of postherpetic neuralgia is limited
Peet MM, Schneider RC. Trigeminal neuralgia: a review to a single division of the trigeminal nerve in
of six hundred and eighty-nine cases with a follow-up most instances, and is restricted to the super-
study on sixty-five percent of the group. J Neurosurg. ficial skin or mucosal surfaces. Nevertheless,
1952;9:367.
it may be confused with trigeminal neural-
Quinn JH, Weil T. Trigeminal neuralgia: treatment by
repetitive peripheral neurectomy. Supplemental gia or even cluster headache. A history of
report. J Oral Maxillofac Surg. 1975;33:591. vesicular eruption (shingles) is diagnostic.
Taarhj P. Decompression of the posterior trigeminal root
in trigeminal neuralgia. A 30-year follow-up review. TREATMENT
J Neurosurg. 1982;57:14.
Zakrzewska JM. Medical management of trigeminal neu- Postherpetic neuralgia is difficult to control.
ralgia. Br Dent J. 1990;168:399. Cutaneous stimulation with an electric phys-
iologic stimulator offers some degree of pal-
liation. Other therapies that may cause relief
POSTHERPETIC NEURALGIA include the lidocaine patch, opioid analgesics,
Figure 12-10 nortriptyline, amitriptyline, and gabapentin.
Age: Middle-aged and elderly adults
Sex: No predilection
CLINICAL FEATURES
Additional Reading
Bernstein JE, Korman NJ, Bickers DR, et al. Topical
Varicella-zoster infection, causing herpes capsaicin treatment of chronic postherpetic neuralgia.
zoster or shingles, results in a painful vesicu- J Am Acad Dermatol. 1989;21:265.
PMPH_Eversole_Chapter-12.indd 624 1/20/2011 3:19:02 PM
Facial Pain and Neuromuscular Disorders 625
FIGURE 12-10
Herpes zoster vesicular lesions may be distributed along the trigeminal I, II, or III divisions preceding the
onset of postherpetic neuralgia.
Kramer PW. The management of postherpetic neuralgia a superficial component. A light touch or
with chlorprothixene. Surg Neurol. 1981;15:102. even a blast of air will provoke a hyperes-
Sugar O, Bucy PC. Postherpetic trigeminal neuralgia.
Arch Neurol Psychiatr. 1951;65:131. thetic response. The pain may be constant
Woodforde JM, Dwyer B, McEwen BW, et al. Treatment or episodic, and in some patients, cutane-
of post-herpetic neuralgia. Med J Aust. 1965;2:869. ous erythema is observed during intensity
Young L. Post-herpetic neuralgia: a review of advanc- peaks; this vasodilation phenomenon sub-
es in treatment and prevention. J Drugs Dermatol.
2006;5(10):938-941.
sequently wanes. Facial trauma or surgery
usually precedes onset of the syndrome.
The mechanism is not clearly understood;
COMPLEX REGIONAL PAIN however, mediation by the sympathetic
SYNDROME (CAUSALGIA) nervous system appears to be an impor-
Figure 12-11 tant factor. Afferent nociceptor pathways
are apparently stimulated by locally
Age: Adults released catecholamines. A stellate gan-
Sex: No predilection glion block with bupivacaine causes relief
CLINICAL FEATURES of symptoms and is therefore the most
important diagnostic tool when causalgia
Complex regional pain syndrome is now is suspected.
divided into two clinical entities: type I
is formerly identified as reflex sympathetic
DIFFERENTIAL DIAGNOSIS
dystrophy; type II is the new term for causal-
gia that always coexists with documented A variety of facial pain syndromes should
nerve injury. This rare facial pain syn- be included in the differential diagno-
drome is usually localized to the extremi- sis. Many cases of causalgia have prob-
ties after an episode of severe trauma. ably gone undiagnosed, being labeled as
Facial causalgia is characterized by atypical facial pain. Hyperesthesia, burn-
hyperesthesia of the affected skin; often, ing pain, vasodilatory cutaneous signs,
a trophic response is observed with ery- and a history of facial surgery or trauma
thema and dermatitis. The pain is burning should alert the clinician to the probability
and may be deep, yet there is invariably of causalgia. Abolition of pain subsequent
PMPH_Eversole_Chapter-12.indd 625 1/20/2011 3:19:03 PM
626 Chapter 12
FIGURE 12-11
Complex regional pain syn-
drome (Causalgia). Stellate
ganglion block (left), resul-
tant Horner’s syndrome
and pain relief (right).
to a stellate ganglion block confirms the CRANIAL BASE AND CNS
diagnosis. NEOPLASMS
Figure 12-12
TREATMENT
Biweekly stellate ganglion blocks, con- Age: Adults
firmed by initiation of Horner’s syndrome, Sex: No predilection
often are curative after 6 to 10 injections. If CLINICAL FEATURES
relief is not achieved, surgical stellate gan-
glion sympathectomy may be required. Neurologic deficits are encountered in neo-
This will, of course, result in a permanent plastic processes that encroach on cranial
hemifacial sympathetic blockade with pto- nerves above or below the exit through the
sis, miosis, and anhidrosis. cranial base foramina. Metastatic tumors to
the cranial base or middle fossa, cerebello-
pontine angle tumors, and nasopharyngeal
Additional Reading tumors often compress or invade one or two,
or all three, divisions of the trigeminal nerve,
Elfenbaum A. Causalgia in dentistry: an abandoned pain
syndrome. Oral Surg Oral Med Oral Pathol. 1954;7:594. thus resulting in paresthesia, hypesthesia,
Hanowell ST, Kennedy SF. Phantom tongue pain in and/or pain. The fact that a sensory deficit
causalgia: a case presentation and treatment. Anesth. or pain symptom is rarely encountered in
Analg. 1979;58:436. the absence of a motor deficit is significant.
Hoffmann KD, Matthews MA. Comparison of sympa-
thetic neurons in orofacial and upper extremity nerves: Although a variety of eponymic syndromes
Implications for causalgia. J Oral Maxillofac Surg. have been described depending on the local-
1990;48:720. ization of signs and symptoms, the com-
Hsu ES. Practical management of complex regional pain monality is tumor compression of nerves.
syndrome. Am J Ther. 2009;16(2):147-154.
Sakamoto E, Shiiba S, Noma N, et al. A possible case
Many of these eponymic syndromes exhibit
of complex regional pain syndrome in the orofacial overlapping features that are confusing to
region. Pain Med. 2010;11(2):274-280. the clinician; therefore, a topographic nosol-
PMPH_Eversole_Chapter-12.indd 626 1/20/2011 3:19:09 PM
Facial Pain and Neuromuscular Disorders 627
A B
FIGURE 12-12
A: CT scan illustrating a cra-
nial base chondrosarcoma
with sphenoid sinus exten-
sion. B: Site of tumor in para-
sellar syndrome in relation to
trigeminal and ocular motor
nerves. C: Site of nasopha-
ryngeal/cranial base tumor
in relation to V-3 and motor
root of the trigeminal nerve.
ogy is more practical. Malignant disease of unilateral hearing deficit resulting from
the orbit, the orbital syndrome, causes supraor- eustachian tube extension. The jugular fora-
bital pain and hypesthesia, blurred vision or men syndrome is characterized by dysphagia,
diplopia, ptosis, and/or ophthalmoplegia. hoarseness, glossopharyngeal neuralgia-like
Tumors encroaching on the cavernous sinus, pain, palate weakness, and vocal cord paral-
the parasellar syndrome, compress the first ysis. Hypoglossal weakness is also common,
division of the fifth nerve as well as nerves but it occurs more frequently in the occipital
3, 4, and 6; the result is frontal pain and condyle syndrome, which is heralded by occip-
ophthalmoplegia. The middle fossa syndrome ital pain that is exacerbated by neck flexion.
occurs in patients with neoplastic disease in
the region of the gasserian ganglion. Hypes-
DIFFERENTIAL DIAGNOSIS
thesia, paresthesia, and pain of the second
and third divisions are common; numbness Malignant neoplasia that is primary within
without pain also is encountered. Ocular the CNS, secondary to nasopharyngeal
muscle paralysis is common, and paresis of extension, or metastatic may cause facial
the masticatory muscles may be detected pain and be confused with a variety of local
(i.e., deviated mandibular opening, masse- pain syndromes. The triad of sensory deficit
teric weakness, unilateral soft palate paraly- (numbness or paresthesia), pain, and motor
sis, etc.). Foramina or intracranial extension deficit (ocular, masticatory, facial, or glossal)
by a nasopharyngeal carcinoma may cause constitutes an ominous finding. Although
similar signs and symptoms, including a routine radiographs often fail to uncover a
PMPH_Eversole_Chapter-12.indd 627 1/20/2011 3:19:16 PM
628 Chapter 12
lesion, magnetic resonance imaging (MRI) some of these patients and are discussed
or CT scans will reveal a pathologic pro- separately. The symptoms of atypical pain
cess. A history of cancer may indicate the are inconsistent from one patient to the
probability of cranial base metastasis. next. Some patients complain of localized
dull aches; others say the pain is dull and
TREATMENT wanders from one site to another; yet others
Any patient with pain, numbness, and complain of paroxysms of acute pain with-
cranial nerve motor weakness should be out a trigger zone. Many instances of atypi-
evaluated by a neurologist; a CT scan of the cal facial pain probably represent symptoms
cranium should be performed. Treatment of a psychiatric disorder, usually depression
is determined when the process has been or histrionic personality. Postherpetic gan-
definitively diagnosed. glioneuritis associated with herpes simplex
may be responsible for some instances of
atypical pain, particularly when mild par-
Additional Reading esthesia is present or motor weakness of
facial muscles is observed. No hard data are
Greenberg HS. Metastasis to the base of the skull: clini-
cal findings in 43 patients. Neurology. 1981;31:530.
available to support a viral etiology; how-
Gil Z, Fliss DM. Quality of life in patients with skull base ever, demyelinating peripheral lesions can
tumors: current status and future challenges. Skull follow herpes hominis infections and could
Base. 2010;20(1):11-18. eventuate in pain, paresthesia, and seventh-
Naheedy MH, Haag JR, Azar-Kia B, Mafee MF, Elias
DA. MRI and CT of sellar and parasellar disorders.
or fifth-nerve motor weakness. Atypical
Radial Clin North Am. 1987;25:819. odontalgia can be included as a form of atyp-
Svien HJ, Baker HL, River MH. Jugular foramen syn- ical facial pain. Patients complain of aching
drome and allied syndromes. Neurology. 1963;13:797. pain in a tooth or group of teeth in which
Thomas JE, Yoss RE. The parasellar syndrome: problems
objective pulp testing and radiographs fail
determining etiology. Mayo Clin Proc. 1970;45:617.
to show evidence of pulpal disease. These
patients are insistent and demand endodon-
ATYPICAL FACIAL PAIN tic therapy or extraction. Typically, endo-
dontic therapy is given, but pain persists;
Age: Middle-aged adults then, apicoectomy is performed, but pain
Sex: Female predilection continues. Ultimately, the tooth is removed;
CLINICAL FEATURES subsequently, the patient complains of pain
in an adjacent tooth. In these instances, psy-
Atypical facial pain occurs in the maxilla
chogenic causes should be suspected. The
or the mandible, but current evaluative and
clinician should consider depression and
diagnostic methods do not reveal an organic
conversion symptoms with secondary gain
cause. The diagnosis requires exclusion of
or guilt complex.
other known pain syndromes including the
true neuralgias, vasoactive headaches, and
DIFFERENTIAL DIAGNOSIS
myogenic pain disorders. Then one is left
with a pain patient whose signs, symptoms, The symptoms encountered in atypical
or chemical and laboratory findings do not facial pain can mimic organic, neuralgic,
allow for a definitive diagnosis. By exclusion, vasoactive, or myogenic pain syndromes.
one attaches the appellation “atypical facial The clinician is obliged to rule out odon-
pain,” which probably includes a heteroge- togenic, antrogenic, and sialogenic sources
neous constellation of disorders. Pathologic first. Secondly, muscle palpation and muscle
jawbone cavities have been identified in trigger point tenderness should be assessed
PMPH_Eversole_Chapter-12.indd 628 1/20/2011 3:19:26 PM
Facial Pain and Neuromuscular Disorders 629
with subcutaneous or intramuscular local usually sharp and severe in acute pulpitis.
anesthesia to evaluate elimination of myo- Sensitivity to heat, cold, and percussion is
genic referred pain to teeth or the jaws. characteristic. The pain often awakens the
When edentulous regions are observed, a patient or prevents sleep. In most instances,
pathologic bone cavity should be consid- clinical and radiographic examination dis-
ered; selective infiltration anesthesia is use- close a large carious lesion encroaching on
ful diagnostically. Although central neural the pulp or pulp horns. Acute pain during
or cranial base neoplasms may cause facial mastication or when firm lateral pressure is
pain, they rarely do so in the absence of par- applied to cusps and the presence of cold
esthesia or motor deficit. sensitivity are indicative of tooth fracture.
Fiberoptic light examination often uncov-
TREATMENT ers a fracture line; however, some fractures
Unfortunately, and by definition, the causal underlie restorations, thus necessitating
process is unknown. When a psychogenic removal of the material before fiberoptic
origin is suspected, patients rarely accept examination. Dull chronic aching pain is
this diagnosis and refuse psychiatric care. more often associated with periapical dis-
A 6-week trial of tricyclic antidepressant ease related to a necrotic tooth. Alterna-
therapy is recommended. This treatment tively, many patients with pulp necrosis
has been beneficial for some patients with and periapical granulomas or cysts are pain
atypical facial pain. free or have a history of pain that eventually
resolves. Radiographs uncover a periapical
radiolucency, and the tooth fails to respond
Additional Reading to electric pulp test stimulation. Most teeth
with pulp necrosis are grossly carious. A
Brooke RI. Atypical odontalgia. Oral Surg Oral Med maxillary tooth seldom refers pain to the
Oral Pathol. 1980;49:196. mandible. Furthermore, the pain, particu-
Denaley JF. Atypical facial pain as a defense against psy-
chosis. Am J Psychol. 1976;133:1151. larly in molar teeth, may be referred to the
Koopman JS, Dieleman JP, Huygen FJ, de Mos M, TMJ and ear.
Martin CG, Sturkenboom MC. Incidence of facial
pain in the general population. Pain. 2009;147
(1-3):122-127.
Kreisberg MK. Atypical odontalgia: differential diagnosis
and treatment. J Am Dent Assoc. 1982;104:852.
Marbach JJ, Hulbrock J, Hohn C, Segal AG. Incidence of
phantom tooth pain: an atypical facial neuralgia. Oral
Surg Oral Med Oral Pathol. 1982;53:190.
Mandibular Division Pain
ODONTOGENIC INFECTION
Figure 12-13
Age: No predilection
Sex: No predilection
CLINICAL FEATURES
FIGURE 12-13
The most common cause of mandibular Pain referral routes to TMJ, ear, and mandibular
pain is odontogenic infection. The pain is angle from mandibular odontogenic infection.
PMPH_Eversole_Chapter-12.indd 629 1/20/2011 3:19:26 PM
630 Chapter 12
DIFFERENTIAL DIAGNOSIS OSTEOMYELITIS
Most mandibular pains are of odontogenic Figure 12-14
origin; therefore, a dental source should be
sought before other pain syndromes involv- Age: Any age
ing the third division of the trigeminal nerve Sex: No predilection
are considered. The suspected tooth (teeth) CLINICAL FEATURES
should be tested with heat, cold, percussion, Osteomyelitis is an acute, subacute, or
electric stimulation, and fiberoptics; radio- chronic bacterial infection of the bone mar-
graphs should be obtained. When no dental row. In the jaws it usually arises from the
source can be uncovered in the mandible, the spread of infection from a necrotic tooth or
maxillary dentition should be evaluated. Peri- from a periapical infectious focus. In some
odontal probing should be undertaken, after instances an anachoretic infection may be
all dental sources are ruled out, if a periodon- responsible. Osteomyelitis of the jaws usually
tal abscess cannot be found easily. Failure to affects the mandible, and the incriminating
uncover either a dental or periodontal source tooth tends to be a posterior one. Pain may
of the pain will direct attention to other pain be dull and aching or severe and pounding
syndromes included in this section. depending on the virulence of the infectious
organisms, some of which may be anaer-
TREATMENT obes. Radiation therapy for oral carcinoma
results in vascular damage and predisposes
Restorable teeth should be treated endodon-
to osteomyelitis if an endodontic infectious
tically. In some cases, cracked teeth can be
source is extant. Another predisposing fac-
managed by full crown coverage; however,
tor is bisphosphonate therapy for osteopo-
large cracks may require extraction. When
rosis and metastatic bone cancer. Sequestra-
fever or a facial swelling is present, peni-
tion of bone and fistulous tracts may occur
cillin or erythromycin (when patients are
in all forms of osteomyelitis. Radiographs
allergic to penicillin) should be prescribed
show radiolucencies with a moth-eaten pat-
for 10 days. Response failure may indi-
tern, being poorly marginated.
cate penicillinase-producing organisms or
anaerobes. In these instances, penicillinase- MICROSCOPIC FEATURES
resistant antibiotics or clindamycin should
be used, respectively. Bony sequestra show lacunae devoid of
osteocyte nuclei and may be engulfed by
bacteria, and actinomycete colonies may
Additional Reading predominate. Marrow spaces are typically
infiltrated with inflammatory cells, neutro-
Chow AW, Roser SM, Brady FA. Oralfacial odontogenic phils if acute, round cells if chronic.
infections. Ann Intern Med. 1978;88:392.
Dodson TB, Perrott DH, Kaban LB. Pediatric maxillo- DIFFERENTIAL DIAGNOSIS
facial infections: a retrospective study of 113 patients.
J Oral Maxillofac Surg. 1989;47:327. The presence of sequestra, fistulae, and
Glick DH. Locating referred pulpal pains. Oral Surg radiolucent lesions along with elevated tem-
Oral Med Oral Pathol. 1962;15:613. perature usually clinch the diagnosis. Both
Kannangara DW, Thadepelli H, McQuiter JL.
Bacteriology and treatment of dental infections. Oral aerobic and anaerobic cultures with antibi-
Surg Oral Med Oral Pathol. 1980;50:103. otic sensitivity should be employed.
Sato FR, Hajala FA, Freire Filho FW, Moreira RW, de
Moraes M. Eight-year retrospective study of odonto- TREATMENT
genic origin infections in a postgraduation program on
oral and maxillofacial surgery. J Oral Maxillofac Surg. Antibiotic therapy should be initiated with
2009;67(5):1092-1097. a penicillin-related antibiotic or cepha-
PMPH_Eversole_Chapter-12.indd 630 1/20/2011 8:21:22 PM
Facial Pain and Neuromuscular Disorders 631
FIGURE 12-14
Moth-eaten radiolucencies seen in
the mandible on cone beam com-
puted tomography (CT) 3D recon-
structions, CT cuts and panoramic
radiographs occur in osteomyeli-
tis, bisphosphonate osteonecro-
sis, and osteoradionecrosis.
losporins until results are obtained from regeneration by the proximal axonal seg-
sensitivity testing. In severe cases, hyper- ment, which canalizes the distal nerve
baric oxygen can be administered along with sheath tract. When the severed nerve ends
analgesics. Surgical debridement should be are not readily approximated, the regener-
undertaken diligently and selectively. ating axon may, in the process of searching
for the distal sheath, become hyperplastic
Additional Reading and tortuous, creating a painful nodule.
Traumatic neuromas of soft tissue are usu-
Albuquerque MA, Melo ES, Jorge WA, Cavalcanti MG. ally detected visually as swelling, or they
Osteomyelitis of the mandible associated with autosomal are palpable. Compression initiates pain.
dominant osteopetrosis: a case report. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 2006;102(1):94-98. Occasionally, traumatic neuromas arise
Prasad KC, Prasad SC, Mouli N, Agarwal S. central in bone subsequent to tooth extrac-
Osteomyelitis in the head and neck. Acta Otolaryngol. tion or alveolar bone trauma. The pain is
2007;127(2):194-205. deep and intraosseous, and can be moder-
Santos FA, Pochapski MT, Pilatti GL, Kozlowski VA, Jr,
Goiris FA, Groppo FC. Severe necrotizing stomatitis ate or severe. The canine and mental fora-
and osteomyelitis after chemotherapy for acute leu- men areas are the most common sites; the
kaemia. Aust Dent J. 2009;54(3):262-265. pain can be triggered by denture pressure
or digital compression over the involved
area, simulating a trigger zone in trigemi-
TRAUMATIC NEUROMA
nal neuralgia. Local anesthesia eliminates
Figure 12-15 the symptoms. Occasionally, a radiolucency
Age: Middle-aged and elderly adults
can be seen on periapical films.
Sex: Male predilection DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES When compression of a palpable nodule
Severance of a nerve trunk results in axonal overlying the mental foramen or alveolus
degeneration of the distal segment with causes a pain paroxysm, traumatic neuroma
PMPH_Eversole_Chapter-12.indd 631 1/20/2011 8:21:24 PM
632 Chapter 12
Trodahl JM, Carroll GW. Traumatic neuroma of the
mandibular ridge. Oral Surg Oral Med Oral Pathol.
1967;24:563.
SUBACUTE THYROIDITIS
Age: Middle-aged adults
Sex: Female predilection
CLINICAL FEATURES
Subacute thyroiditis usually evolves subse-
quent to an upper respiratory infection; the
prevailing evidence supports a viral etiology,
FIGURE 12-15 probably coxsackievirus. The pain, which is
Small radiolucency in anterior maxilla represent- located in the thyroid region, is aggravated
ing a traumatic neuroma causing severe pain. These by swallowing or turning the head. Pain
lesions are actually more common in the mandible. radiation to the mandible, ear, and/or occipi-
tal region is a common finding; indeed, the
patient’s chief complaint may be jaw pain.
should be suspected. Alternatively, centrally
Other symptoms include nervousness, pal-
located neuromas are not palpable, and the
pitations, and lassitude. Fever may be severe.
pain episodes may mimic trigeminal neu-
Palpation of the thyroid discloses diffuse
ralgia or be classified as atypical facial pain.
swelling and acute tenderness. The overly-
Any radiolucency in the vicinity of the
ing skin is often erythematous. Occasionally,
pain should be tested for abolition of pain
the disease is asymptomatic. Most patients
by local infiltration anesthesia; pending a
are euthyroid with normal thyroid function
positive result, the area should be explored
tests. The condition usually resolves of its
surgically.
own accord within 4 to 6 weeks.
TREATMENT
DIFFERENTIAL DIAGNOSIS
Painful nodules or radiolucent foci sus-
pected of representing traumatic neuroma Acute thyroiditis with mandibular pain being
should be excised. A definitive diagnosis the primary complaint may be mistaken for
requires microscopic confirmation. Step a variety of organic and functional diseases
serial sections may be needed to identify the involving the mandibular nerve distribution.
neuromatous tissue in marrow curettings. In addition, the styloid and hyoid syndromes,
carotidynia, and cardiogenic pain may be
suspected. Elevated temperature and exqui-
Additional Reading site pain on palpation of the thyroid gland
usually suffices for the clinical diagnosis.
Chan MN, Jonsson E, Lee KM. Traumatic neuroma
following sagittal mandibular osteotomy. Int J Oral Tenderness and pain on palpation are rarely
Maxillofac Surg. 1989;18:95. featured in goiter, Graves’ disease, Hashimo-
Kallal RH, Ritto FG, Almeida LE, Crofton DJ, Thomas to’s thyroiditis, or thyroid neoplasia.
GP. Traumatic neuroma following sagittal split osteot-
omy of the mandible. Int J Oral Maxillofac Surg.
2007;36(5):453-454. TREATMENT
Rasmussen OC. Painful traumatic neuromas in the oral
cavity. Oral Surg Oral Med Oral Pathol. 1980; 49:191.
Palliative care includes the use of analge-
Robinson M, Slavkin HC. Dental amputation neuromas. sics and antipyretics. The disease is self-
J Am Dent Assoc. 1965;70:662. limited and although thyrotoxicosis has
PMPH_Eversole_Chapter-12.indd 632 1/20/2011 3:19:36 PM
Facial Pain and Neuromuscular Disorders 633
been reported to occur, most patients fail test). Anxiety is also prevalent in patients
to suffer from any residual thyrometabolic with burning mouth. Guilt, conversion
complications. reactions, and overt schizophrenia may be
encountered; many of these patients are
cancerophobic as well.
Additional Reading
DIFFERENTIAL DIAGNOSIS
Ingbar SH, Woeber KA. The thyroid gland. In:
Williams RH, eds. Textbook of Endocrinology. 6th ed. A fasting blood sugar or, preferably, a
Philadelphia, PA: W. B. Saunders; 1981:241. 2-hour postprandial glucose test should be
Papapetrou PD, Jackson I. Thyrotoxicosis due to “silent”
thyroiditis. Lancet. 1975;1:361.
performed along with a hemogram in order
Smith MJA, Myall RWT. Subacute thyroiditis as a to rule out diabetes and megaloblastic ane-
cause of facial pain. Oral Surg Oral Med Oral Pathol. mia, respectively. Negative laboratory find-
1977;43:59. ings and normal-appearing oral soft tissues
Volpe R. Acute and subacute thyroiditis. Pharmacol
Ther. 1976;1:171.
lead to a diagnosis of psychogenic stoma-
todynia. A psychiatric work-up augmented
with psychometric testing (e.g., Minnesota
Multiphasic Personality Inventory [MMPI])
STOMATODYNIA/ and a dexamethasone suppression test will
GLOSSOPYROSIS aid in establishing a diagnosis of depressive
illness.
Age: Middle-aged and elderly adults
Sex: Female predilection
TREATMENT
CLINICAL FEATURES
Once a diagnosis of depression is con-
Burning mouth or tongue (glossopyrosis) firmed, treatment with one of the tricyclic
is a common symptom and in younger antidepressants should be instituted. Dox-
patients is usually associated with one of the epin, 100 mg 2 hours before retiring, can be
vesiculo-bullous-ulcerative diseases. Older prescribed for 1 week; a final dosage of 200
patients may also present with this symp- to 250 mg per day will affect an elevation
tom in the absence of oral lesions. Rarely, in mood with resolution of pain symptoms
burning tongue is a symptom in patients for most patients. Beneficial results usu-
with organic diseases including pernicious ally require 3 or 4 weeks of therapy. Most
anemia and diabetes mellitus. In the former, patients with this symptom are postmeno-
the tongue is often beefy red and denuded pausal women, and estrogen therapy has
of papillae. In the majority of patients, no been found to alleviate the burning symp-
physical evidence of disease is encoun- toms. α-lipoic acid and gabapentin also pro-
tered. There are special sensory deficits in vide relief in some subjects. After medical
taste threshold, implicating involvement of treatment has proven efficacious, psycho-
the chorda tympani pathway. Most elderly therapy should be considered.
patients with stomatodynia suffer from
psychiatric illness, with chronic depres-
sion being the most prevalent diagnosis.
Loss of enthusiasm, sleep disturbances, loss
Additional Reading
of libido, and concurrent anxiety are often Brooke RI, Seganski DP. Aetiology and investigation of
present. Patients with long-standing endog- the sore mouth. J Canad Dent Assn. 1977;43:504.
Eliav E, Kamran B, Schaham R, Czerninski R, Gracely
enous depression usually manifest elevated RH, Benoliel R. Evidence of chorda tympani dysfunc-
blood cortisol levels after challenge with tion in patients with burning mouth syndrome. J Am
oral steroids (dexamethasone suppression Dent Assoc. 2007;138:628-633.
PMPH_Eversole_Chapter-12.indd 633 1/20/2011 3:19:37 PM
634 Chapter 12
Lamey P-J, Lamb AB. The usefulness of the HAD scale pain should arouse suspicion of coronary
in assessing anxiety and depression in patients with ischemia.
burning mouth syndrome. Oral Surg Oral Med Oral
Pathol. 1989;67:390.
López-D’alessandro E, Escovich L. Combination of TREATMENT
alpha lipoic acid and gabapentin, its efficacy in the Referral to a physician is recommended
treatment of burning mouth syndrome: a random-
ized, double-blind, placebo controlled trial. Med when cardiac origin is suspected. Rest-
Oral Patol Oral Cir Bucal. 2010 Aug 15. [Epub ahead ing and stress ECG readings then aid in
of print.] establishing the diagnosis, and appropri-
Schoenberg B, Carr AC, Kutscher AH, Zegarelli EV. ate medical management controls the jaw
Chronic idiopathic orolingual pain. Psychogenesis of
burning mouth. N Y State J Med. 1971;71:1832.
symptoms.
Ziskin DE, Moulton R. Glossodynia: a study of idiopathic
orolingual pain. J Am Dent Assoc. 1946;33:1422.
Additional Reading
Batchelder BJ, Krutchkoff DJ, Amara J. Mandibular pain
CARDIOGENIC FACIAL PAIN as the initial and sole clinical manifestation of coro-
nary insufficiency: report of case. J Am Dent Assoc.
Age: Middle-aged and elderly adults 1987;115:710.
Sex: Male predilection Franco AC, Siqueira JT, Mansur AJ. Facial pain of
cardiac origin: a case report. Sao Paulo Med J.
CLINICAL FEATURES 2006;124(3):163-164.
Although myocardial ischemia classically Matson MS. Pain in orofacial region associated with cor-
onary insufficiency. Oral Surg Oral Med Oral Pathol.
produces angina pectoris with referred 1963;16:284.
pain over the left shoulder and down the Natkin E, Harrington GW, Mandel MA. Anginal pain
arm, the pain is occasionally referred to the referred to the teeth. Oral Surg Oral Med Oral Pathol.
left mandible. Indeed, some patients may 1975;40:678.
Paine R. Ch. 4. Vascular facial pain. In: Alling CC, III,
complain of jaw pain without a substernal Mahan, PE, eds. Facial Pain. 2nd ed. Philadelphia,
component. Pain referred to the mandible PA: Lea & Febiger; 1977.
has been explained on the basis of converg-
ing nociceptor pathways from cardiac pain
fibers that ascend the cord subsequent to Otogenic Pain
synapsing in the thoracic dorsal horn and
communicate with neurons located in ACUTE OTITIS MEDIA
the subnucleus caudalis of the trigeminal Figure 12-16
nerve. Typically, the pain is precipitated by
exertion or stress and is usually described Age: Children and young adults
as an ache. Administration of a nitroglyc- Sex: No predilection
erin tablet sublingually usually, yet not CLINICAL FEATURES
invariably, relieves the symptoms. An elec- Acute inflammation of the middle ear is
trocardiogram (ECG) often displays S-T or usually bacterial in origin with β-hemolytic
T wave anomalies indicative of myocardial streptococci, Streptococcus pneumoniae, and
ischemia. Normal resting ECG results do Hemophilus influenzae being the predomi-
not rule out coronary vascular disease. nant infectious organisms. Viral agents
are rarely responsible, yet may predispose
DIFFERENTIAL DIAGNOSIS
to bacterial infection by inducing eusta-
Because many common local processes can chian tube edema and obstruction. Pain is
cause mandibular pain, a cardiogenic etiol- severe and persistent; otoscopic examina-
ogy is often overlooked. Pain on exertion or tion reveals a bulging hyperemic tympanic
left mandibular pain with concurrent chest membrane. Conductive hearing loss is a
PMPH_Eversole_Chapter-12.indd 634 1/20/2011 3:19:38 PM
Facial Pain and Neuromuscular Disorders 635
Additional Reading
Coffey JD. Otitis media in the practice of pediatrics;
bacteriologic and clinical observations. Pediatrics.
1966;38:25.
Froom J, Culpepper L, Grob P. Diagnosis and anti-
biotic treatment of acute otitis media: report from
International Primary Care Network. Br Med J.
1990;300:582.
Giebink GS, Quie PG. Otitis media: The spectrum of mid-
dle ear inflammation. Annu Rev Med. 1978;29:285.
Kalu SU, Ataya RS, McCormick DP, Patel JA, Revai
K, Chonmaitree T. Clinical spectrum of acute otitis
media complicating upper respiratory tract viral infec-
tion. Pediatr Infect Dis J. 2010 Aug 12. [Epub ahead
of print.]
Yules RB. Differential diagnosis of referred otalgia. Eye
Ear Nose Throat Mon. 1967;46:587.
FIGURE 12-16
Tympanic membrane in: normal ear (top); acute oti-
tis media with bulging drum and loss of landmarks CHRONIC OTITIS MEDIA
(bottom). Source: Reprinted by permission from Dr. Figure 12-17
R. A. Buckingham, Some Pathological Conditions of
the Eye, Ear and Throat, Abbott Laboratories, 1955. Age: Adults
Sex: No predilection
CLINICAL FEATURES
feature; the eustachian tube mucosa in the
nasopharynx is usually hyperemic. Eventu- Chronic otitis media is far more complex
ally, the patient becomes febrile and may than acute infectious otitis. The onset may
manifest an exudate with perforation of the be insidious, and pain is not common.
drum. Coalescent mastoiditis develops, and Staphylococcus aureus and Bacillus proteus
opacification of the middle ear chamber are most frequently cultured. Many factors
and mastoid air cells can be detected radio- are believed to predispose to chronic otitis,
graphically. Subsequent to perforation and including progression of acute otitis, eusta-
drainage, the lesion may resolve, or compli- chian tube obstruction, and allergy. Ear
cations such as subperiosteal abscess, dural pain, if present, is dull and usually mild to
abscess, or brain abscess may evolve. moderate. Occasionally, acute exacerbations
with sharp pain surface. Persistent otitis
DIFFERENTIAL DIAGNOSIS media of long standing is accompanied by
destructive changes within the middle ear
Acute otitis media is usually not confused and mastoid air cells. Otoscopic examina-
with other otalgic disorders because of the tion may disclose a perforation of the pars
classic clinical changes that involve the tym- tensa, and a discharge may or may not be
panic membrane along with acute severe seen. Small perforations may not interfere
persistent pain. with normal hearing; however, hearing loss
occurs with larger perforations. In chronic
TREATMENT
tubotympanic otitis, the perforation may
Penicillin or erythromycin therapy is indi- be filled with edematous polypoid mucosa.
cated; myringotomy may help to relieve pain Otitis represented by excessive middle ear
when exudation has not yet occurred. Refer- keratinization (keratoma, cholesteatoma)
ral to an otolaryngologist is recommended. is probably the result of drum perforation
PMPH_Eversole_Chapter-12.indd 635 1/20/2011 3:19:38 PM
636 Chapter 12
Additional Reading
Brook I. The role of anaerobic bacteria in chronic suppu-
rative otitis media in children: implications for medical
therapy. Anaerobe. 2008;14(6):297-300.
Freidman I. Epidermoid cholesteatoma and cholesterol
granuloma. Ann Otol Rhinol Laryngol. 1959;68:57.
Howie VW, Ploussard JH, Sloyer J. The “otitis prone”
condition. Am J Dis Child. 1975;129:676.
McGuckin F. Nonmalignant destructive ear disease.
Arch Otolaryngol Head Neck Surg. 1963;78:358.
Thomas R. The chronic ear. Renewed argument.
J Laryngol Otol. 1967;81:1071.
HERPES ZOSTER OTICUS
Age: Middle-aged and elderly adults
FIGURE 12-17 Sex: Male predilection
Tympanic membrane in: normal ear (top); bulging CLINICAL FEATURES
drum (bottom left); and perforated drum (bottom
right). Source: Reprinted by permission from Dr. R. Also known as geniculate ganglion neural-
A. Buckingham, Some Pathological Conditions of the gia or the Ramsay-Hunt syndrome, herpes
Eye, Ear and Throat, Abbott Laboratories, 1955. zoster oticus causes aural and postauricu-
lar pain. Pain is acute and burning, and
often represents a prodromal symptom
with epidermal migration from the meatus.
preceding the onset of a vesicular erup-
Retraction and pitting with loss of ossicle
tion involving the postauricular cleft. The
definition are indicative of disease. Chronic
external ear canal receives sensory inner-
otitis can become severely destructive.
vation from geniculate ganglion fibers of
the seventh nerve that innervate the aural
DIFFERENTIAL DIAGNOSIS
skin and travel with branches of the tenth
Chronic otalgia can be seen in referred pain nerve. Branches from the auriculotemporal
of odontogenic origin or in diseases of the also innervate the auditory canal anteriorly.
TMJ. Changes in the tympanic membrane Regardless of which nerves are affected
warrant a thorough otologic evaluation. In by the varicella-zoster virus, the signs and
the absence of drum changes, pain with symptoms are the same. A coexistent ipsi-
hearing loss suggests middle ear disease. lateral facial paralysis frequently follows the
Significantly, otitis media can result from vesicular eruption. Vesicles are occasionally
tubal obstruction secondary to nasopharyn- seen in the ipsilateral pharynx.
geal carcinoma. In histiocytosis, histiocytic
infiltrates involve the middle ear; however, DIFFERENTIAL DIAGNOSIS
pain is usually not a complaint. Prior to onset of the aural vesicular erup-
tion, the diagnosis may be enigmatic, simu-
TREATMENT
lating other diseases causing otalgia. Within
When clinical signs and symptoms indi- a few days, the vesicles appear; a cytologic
cate chronic otitis media, referral to an oto- smear discloses viral epithelial cell changes.
laryngologist is indicated. Surgery is often Elevated serum varicella-zoster antibody
necessary, particularly when keratoma is titers can be detected after the appearance
present. of vesicles.
PMPH_Eversole_Chapter-12.indd 636 1/20/2011 3:19:47 PM
Facial Pain and Neuromuscular Disorders 637
TREATMENT invasion by tumors arising from contiguous
The disease is self-limited and resolves of tissues of the brain, meninges, external ear,
its own accord. Facial paralysis may require nasopharynx, and parotid gland can also
4 to 6 weeks to resolve. Intravenous acyclo- cause bone destruction, otitis media, and
vir (10 mg/kg) every 8 hours has been rec- otalgia. Visual inspection of the tympanic
ommended for resolution of vesicles as well membrane often discloses drum perfora-
as paralysis. tion, a retrotympanic mass, or suppurative
otitis. Invasion of the temporal bone, inner
ear, and facial canal cause a variety of signs
Additional Reading and symptoms, including unilateral pul-
satile tinnitus, neurosensory hearing loss,
Bhupal HK. Ramsay Hunt syndrome presenting in pri- and paresis of cranial nerves VII, IX, X, XI,
mary care. Practitioner. 2010;254(1727):33-35. and XII.
Blackley B, Friedman I, Wright I. Herpes zoster auris
associated with facial palsy and auditory nerve symp-
toms: a case report with histopathological findings. DIFFERENTIAL DIAGNOSIS
Acta Otolaryngol (Stockh). 1967;63:533. Differentiation of tumor from other lesions
Dickins JR, Smith JT, Graham SS. Herpes zoster oticus:
treatment with intravenous acyclovir. Laryngoscope. causing otalgia is not always straightfor-
1988;98:776. ward on clinical grounds alone. Cranial
Harner SG, Heiny BA, Newell RC. Herpes zoster oticus. nerve deficits, hearing loss, and tinnitus
Arch Otol. 1970;92:632. should arouse suspicion of tumor. Angiog-
Jurgens EH, Jurgens PE. Syndromes involving facial
pain. In: Alling, CC, III, Mahan PE, eds. Facial pain. raphy and tomography are then employed,
2nd ed. Philadelphia, PA: Lea & Febiger; 1977:231. and if significant bony destruction is
observed, biopsy is indicated.
MIDDLE EAR NEOPLASMS
Figure 12-18
Age: Adults
Sex: Male predilection
CLINICAL FEATURES
Neoplastic and neoplasm-like prolifera-
tions of the middle ear, temporal bone, and
mastoid air cells are usually painless; how-
ever, otalgia can be a major complaint, par-
ticularly when secondary infection occurs.
Histiocytosis and granulomatous inflam-
matory diseases are the more frequently
encountered reactive lesions. Pain with
erosion of the mastoid region and acute
mastoiditis are more often encountered
in histiocytosis. Glomus jugulare tumors,
meningiomas, facial nerve neuromas, FIGURE 12-18
Normal ear drum (top); cholesteatoma middle ear
squamous cell carcinomas, and adenocarci-
with anterior polyp (bottom left); squamous cell
nomas are the common primary tumors in carcinoma filling external canal (bottom right).
this region; acute ear pain, particularly noc- Source: Reprinted by permission from Dr. R. A.
turnal, is often reported by patients with Buckingham, Some Pathological Conditions of the Eye,
squamous cancer. Metastatic lesions and Ear and Throat, Abbott Laboratories, 1955.
PMPH_Eversole_Chapter-12.indd 637 1/20/2011 3:19:58 PM
638 Chapter 12
TREATMENT process, may impinge upon nerves in their
Most middle ear complex tumors are treated vicinity, thus causing pain and discomfort.
by surgical resection. Referral to an otolar- Calcified stylohyoid ligaments are frequent
yngologist or head and neck surgeon is rec- and are usually asymptomatic.
ommended; the extent of disease along with
DIFFERENTIAL DIAGNOSIS
the specific microscopic diagnosis help to
determine the treatment. Pain associated with a calcified stylohyoid lig-
ament may simulate the pain associated with
Additional Reading other causes of TMJ and upper cervical pain.
When the pain originates in the throat or
Conley JJ, Schuller DE. Malignancies of the ear. tonsillar region, glossopharyngeal neuralgia
Laryngoscope. 1976;86:1147. must be considered in the differential diagno-
House HP. Early detection of middle ear malignancy. sis; however, a trigger zone is not present in
Ann Otol Rhinol Laryngol. 1949;58:789.
Hudson WR, Kenan PD. Otologic manifestations of his- Eagle’s syndrome and pain is elicited on man-
tiocytosis X. Laryngoscope. 1969;59:678. dibular opening. Radiographs disclose the
Spector GJ, Maisel RH, Ogura JH. Glomus tumors in the presence of a calcified stylohyoid ligament.
middle ear. I. An analysis of 46 patients. Laryngoscope.
1973;83:1652. TREATMENT
Terao K, Cureoglu S, Schachern PA, et al. Pathologic
correlations of otologic symptoms in acute lympho- Symptomatic elongated styloid processes
cytic leukemia. Am J Otolaryngol. 2009 Dec 18. [Epub can be surgically removed, using an intraoral
ahead of print.]
approach.
Neck and Throat Pain Additional Reading
STYLOHYOID SYNDROME Camarda AJ, Deschamps C, Forest D. Styloid chain ossi-
(EAGLE’S SYNDROME) fication: a discussion of etiology. Oral Surg Oral Med
Oral Pathol. 1989;67:508.
Figure 12-19 Correll RW, Jensen JL, Taylor JB, Rhyne RR.
Mineralization of the stylohyoid-stylomandibular liga-
Age: Middle-aged adults
ment complex. A radiographic incidence study. Oral
Sex: No predilection Surg Oral Med Oral Pathol. 1979;48:286.
CLINICAL FEATURES Kim E, Hansen K, Frizzi J. Eagle syndrome: case report
and review of the literature. Ear Nose Throat J.
Eagle’s syndrome is characterized by pain 2008;87(11):631-633.
during mandibular movement or twisting Odenheimer K. Symptomatic calcified stylohyoid ligaments.
of the head and neck; it is stabbing, origi- In: Archer WH, ed. Oral and Maxillofacial Surgery. 5th
ed. Philadelphia, PA: W. B. Saunders; 1975:1728.
nates in the tonsillar region, and radiates to Solfanelli SX, Braun TW, Sotereanos TC. Surgical man-
the region of the TMJ and base of the tongue. agement of a symptomatic fractured, ossified sty-
When the jaws are closed, the pain subsides. lohyoid ligament. Oral Surg Oral Med Oral Pathol.
The pain is caused by dystrophic calcifica- 1981;52:569.
tion of the stylohyoid ligament and a past
history of trauma to the area is significant.
In some instances, the ligament calcifies in HYOID SYNDROME
childhood and symptoms appear later in Age: Middle-aged and elderly adults
life. Lateral jaw or panographic radiographs Sex: Female predilection
demonstrate a slender radiopaque spicule
emanating from the region of the styloid pro- CLINICAL FEATURES
cess. Other elongated protuberances, such as The hyoid syndrome results from elonga-
the hamular process and cervical transverse tion of the greater cornu with impingement
PMPH_Eversole_Chapter-12.indd 638 1/20/2011 3:20:07 PM
Facial Pain and Neuromuscular Disorders 639
FIGURE 12-19
Calcified stylohyoid ligament
associated with upper lateral neck
pain.
on adjacent laryngeal tissues. Pain is expe- Kopstein E. Hyoid syndrome. Arch Otolaryngol Head
rienced in the lateral neck/carotid area at Neck Surg. 1975;101:484.
Lim RY. The hyoid bone syndrome. Otolaryngol Head
the tip of the greater hyoid cornu. Pain Neck Surg. 1982;90:198.
may be acute, particularly when the neck is Lim RY. Carotodynia exposed: hyoid bone syndrome.
turned or the patient swallows. Ipsilateral South Med J. 1987;80:444.
referred pain to the ear is common, and Shankland WE, 2nd. Anterior throat pain syndromes:
causes for undiagnosed craniofacial pain. Cranio.
syncope may be a feature. Many patients 2010;28(1):50-59.
experience a chronic persistent dull ache
and the sensation that a foreign body is
lodged in the throat. Lateral movement of GLOSSOPHARYNGEAL
the hyoid bone elicits pain. Significantly, NEURALGIA
radiographs may disclose an elongated
cornu, and a calcified stylohyoid ligament Age: Middle-aged adults
is usually not evident. Sex: No predilection
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS Affecting the left side of the face more often
Carotidynia, styloid syndrome, and supe- than the right, glossopharyngeal neuralgia
rior laryngeal neuralgia mimic hyoid appears to represent a disorder similar to
syndrome because they manifest pain in tic douloureux but involving cranial nerve
virtually the same location. The clinical fea- IX. Excruciating, stabbing, and paroxysmal
tures and tenderness on palpation or lateral pain develops after stimulation of a trigger
displacement of the hyoid bone allow for a zone located in the tonsil region or throat.
definitive diagnosis. Swallowing may stimulate an attack. Pain
evolves at the base of the tongue or in the
TREATMENT pharynx, radiating to the ear. Other signs,
Surgical excision of the affected greater cornu such as coughing and even syncope, may
is the treatment of choice. This procedure is appear during an attack. A few affected
usually performed through a cutaneous inci- patients also suffer from trigeminal
sion, which follows local anesthetization. neuralgia.
DIFFERENTIAL DIAGNOSIS
Additional Reading Paroxysmal pain in the throat and base of
Brown LA. Hyoid bone syndrome. South Med. J. the tongue differentiates glossopharyngeal
1954;47:1088. neuralgia from trigeminal neuralgia. Few
PMPH_Eversole_Chapter-12.indd 639 1/20/2011 3:20:08 PM
640 Chapter 12
organic lesions cause paroxysms of pain; directly below the bifurcation area. In this
however, a thorough physical examination respect, it is probably closely related to
of the pharynx and hypopharynx should the other atypical facial pain syndromes
be undertaken to rule out infection or neo- described as midface cluster headaches. The
plasm. The cocaine test is useful in making pain may be unilateral or bilateral, lasting
the diagnosis. Application of 10% cocaine for a few days or a week, with localization in
to the site of pain almost invariably elimi- the lateral neck, ear, and angle of the man-
nates the symptoms in glossopharyngeal dible. It is intense and can be accentuated
neuralgia. when the carotids are manually pressed
posterolaterally against the cervical trans-
TREATMENT verse processes. Inhalation of 100% oxygen
Phenytoin and carbamazepine are the drugs may cause pain relief, such as that encoun-
of choice; however, they are usually less tered with midface cluster headaches. In
effective in glossopharyngeal neuralgia than most instances, the disorder is self-limiting
in trigeminal neuralgia. When medical treat- with spontaneous remission of symptoms.
ment fails, surgical sectioning of the rootlets
DIFFERENTIAL DIAGNOSIS
of nerve IX may be required. Some neurosur-
geons also recommend sectioning of laryn- The localization of pain in the region of the
geal fibers from nerve X, which may also carotid artery is considered to represent
contribute to the pain paroxysms. The primary carotidynia only when all organic disease
surgical choice is vascular decompression. has been eliminated from consideration.
Neoplasms, aneurysms, and inflammatory
conditions of the lateral pharynx must be
Additional Reading ruled out, as must odontogenic inflamma-
Brzustowicz RJ. Combined trigeminal and glossopharyn- tion arising from infected mandibular teeth.
geal neuralgia. Neurology. 1955;5:1. Parotitis, sialadenitis, arteritis, and otitis may
Ferroli P, Fioravanti A, Schiariti M, et al. Microvascular all exhibit pain centered around the carotid
decompression for glossopharyngeal neuralgia: a long- bifurcation and angle of the mandible.
term retrospectic review of the Milan-Bologna experi-
ence in 31 consecutive cases. Acta Neurochir (Wien).
2009;151(10):1245-1250. TREATMENT
Laskiewicz A. Anatomical and clinical considerations on
some rare forms of glossopharyngeal neuralgias. Acta Ergotamine tartrate administered as an anal
Otolaryngol (Stockh). 1953;43:545. suppository induces transient vasoconstric-
Mairs AP, Stewart TJ. Surgical treatment of glossopha- tion and relief of pain. This drug should not
ryngeal neuralgia via the pharyngeal approach.
J Laryngol Otol. 1990;104:12.
be given to patients who are pregnant or
Rushton JG, Stevens JC, Miller RH. Glossopharyngeal hypertensive. Most cases eventually resolve
(vagoglossopharyngeal) neuralgia. A study of 217 cas- of their own accord. In recalcitrant cases, den-
es. Arch Neurol. 1981;38:201. ervation of the carotid bulb may offer relief.
CAROTIDYNIA Additional Reading
Age: Middle-aged adults Fay T. Atypical facial neuralgia, a syndrome of vascular
Sex: Female predilection pain. Ann Otol Rhinol Laryngol. 1932;41:1030.
Hemmen TM, Bettle N, Borelli Jr, AJ. Spontaneous
CLINICAL FEATURES carotidynia. Headache. 2010 Jun 21.
Roseman DM. Carotidynia. A distinct syndrome. Arch
Carotidynia is believed to represent a vaso- Otolaryngol Head Neck Surg. 1967;85:81.
dilation-mediated pain response located in Scheitler LE, Balciunas BA. Carotidynia. J Oral
the vicinity of the common carotid artery Maxillofac Surg. 1983;40:121.
PMPH_Eversole_Chapter-12.indd 640 1/20/2011 3:20:12 PM
Facial Pain and Neuromuscular Disorders 641
de Vries AC, Gender J, Riles TS. Carotidynia managed TREATMENT
by surgical denervation of the carotid bulb. Eur J Vasc
Surg. 1990;4:325. Carbamazepine (Tegretol), 200 to 1200 mg
daily, is usually adequate for control; the drug
can be withdrawn slowly. Periodic blood
SUPERIOR LARYNGEAL counts should be obtained. Surgical interven-
NEURALGIA tion with nerve resection should be reserved
for when this disorder cannot be managed
Age: Adults
Sex: No predilection medically.
CLINICAL FEATURES
Superior laryngeal neuralgia, like trigemi- Additional Reading
nal and glossopharyngeal neuralgias, is a Brownstone PK, Ballenger JJ, Vick NA. Bilateral supe-
pain syndrome of unknown etiology char- rior laryngeal neuralgia. Its successful treatment with
acterized by acute lancinating paroxysmal carbamazepine. Arch Neurol. 1980;37:525.
pain localized above the thyroid cartilage in Echols DH, Maxwell JH. Superior laryngeal neuralgia
relieved by operation. JAMA. 1934;103:2027.
the region of the hyoid bone. The disorder is Smith LA, Moersh HJ, Love JG. Superior laryngeal neu-
usually unilateral; however, bilateral cases ralgia. Mayo Clinic Proc. 1941;16:164.
have been reported. A trigger mechanism Takahashi Sato K, Suzuki M, Izuha A, Hayashi S, Isosu
prevails; an acute pain attack, which lasts a T, Murakawa M. Two cases of idiopathic superior
laryngeal neuralgia treated by superior laryngeal nerve
few seconds, can be precipitated by yawn- block with a high concentration of lidocaine. J Clin
ing, swallowing, sneezing, or touching the Anesth. 2007;19(3):237-238.
skin over the hyoid bone. During a pain
attack, the patient may exhibit uncontrolled
swallowing and belching. Local anesthesia LARYNGEAL NEOPLASMS
in the region of the hypothyroid membrane Figure 12-20
or in the pyriform sinus ablates the pain
when trigger zones are stimulated; this rep- Age: Middle-aged and elderly adults
resents an important diagnostic finding. Sex: Male predilection
CLINICAL FEATURES
DIFFERENTIAL DIAGNOSIS
Most neoplastic processes that arise in the
Superior laryngeal neuralgia may be con- larynx originate on the true or false cords
fused with glossopharyngeal neuralgia. The and pyriform recess. Benign neoplasms
former is localized to the thyrohyoid region, rarely are painful. Malignant laryngeal
whereas the latter affects the base of the tumors usually result in hoarseness with-
tongue and supraglottic region of the phar- out pain. Nevertheless, pain can be a sign of
ynx. Local disease of the larynx should be larynx cancer, particularly in large necrotic
ruled out by palpation of the neck and thyroid squamous carcinomas and in smaller
area, and laryngoscopy should be performed. tumors of the aryepiglottic fold, vallecula,
The absence of organic pathosis along with and epiglottis. The pain is often referred to
a history of acute lancinating pain with a the ear. Invasion of cartilage or contiguous
trigger mechanism is usually sufficient for a laryngeal soft tissues may produce indu-
definitive diagnosis. Nevertheless, the hyoid ration with loss of the normal laryngeal
syndrome may evince similar, if not identi- cartilage crepitus on palpation. Direct or
cal, features. The hyoid should be palpated indirect laryngoscopy should be performed
and shifted laterally; if this maneuver does in patients with hoarseness, with or without
not elicit pain, a true neuralgia of the supe- upper cervical or larynx pain. White kera-
rior laryngeal nerve is the likely diagnosis. totic, red, ulcerated, and tumefactive lesions
PMPH_Eversole_Chapter-12.indd 641 1/20/2011 3:20:12 PM
642 Chapter 12
FIGURE 12-20
Keratotic squamous cell
carninomas of the true cord
associated with hoarseness
and throat pain.
should arouse suspicion of carcinoma and
warrant biopsy. TMJ Region Pain
Figure 12-21
DIFFERENTIAL DIAGNOSIS
Pain associated with larynx cancer is usually MYOGENIC PAIN
a mild-to-moderate dull ache, yet may man- Figure 12-22
ifest occasional sharp twinges. When throat
pain is present, laryngitis or one of the other Age: Young and middle-aged adults
pain syndromes listed here is more likely Sex: Female predilection
than cancer. Regardless, cancer should be CLINICAL FEATURES
considered as a potential cause of laryngeal
Myogenic pain represents one of the most
pain, particularly among smokers.
common disorders causing facial pain. It is
included with TMJ pain because myospasm
TREATMENT
can refer pain to the joint region with or
Laryngeal carcinoma is treated according without diffuse distribution over the facial
to clinical staging and should be managed musculature. Nevertheless, localized pain
by a head and neck surgeon in conjunction from myospasm without a more diffuse
with a radiotherapist. distribution over the masseteric and tempo-
ral regions is not common in the absence of
Additional Reading joint sounds. When it does occur, the patient
complains of a dull ache in the TMJ area;
Charlin B, Brazeau-Lamontagne L, Guerrier B, Leduc it is chronic and usually persistent. Often
C. Assessment of laryngeal cancer: CT scan versus the pain is worse in the morning, in noc-
endoscopy. J Otolaryngol. 1989;18:283.
English GM. Chap. 48. Malignant neoplasms of the lar- turnal bruxism, or in the late afternoon if
ynx. In: English GM, ed. Otolaryngology, A Textbook. parafunctional clenching or bruxing habits
Hagerstown, MD: Harper and Row; 1976. are correlated with work stress. The man-
Micheau C, Luboinski B, Sancho H, Cachin Y. Modes dible may or may not deviate to the affected
of invasion of cancer of the larynx. A statistical, histo-
logical and radioclinical analysis of 120 cases. Cancer.
side; a full range of opening is observed,
1976;38:346. although maximal opening may be painful.
Ogura JH, Thawley SE. Cysts and tumors of the larynx. The patient should be evaluated for myo-
In: Paparella MM, Shumrick DA. Otolaryngology. 2nd genic TMJ pain by palpating the muscles
ed. Philadelphia, PA: W. B. Saunders; 1980:2518.
Zvrko E, Golubović M. Laryngeal adenoid cystic car-
for trigger point tenderness. The lateral
cinoma. Acta Otorhinolaryngol Ital. 2009;29(5): pterygoid is most often involved, followed
279-282. by the masseter and temporalis. Persistent
PMPH_Eversole_Chapter-12.indd 642 1/20/2011 3:20:12 PM
Facial Pain and Neuromuscular Disorders 643
FIGURE 12-21
MFP PAIN, NO CLICK Classification of functional and
internal derangements of TMJ.
(DJD, degenerative joint disease;
ID, internal derangement; MFP,
myogenic facial pain; RDN, reduc-
tion of meniscus). See text for
ID IA NOPAIN, CLICK explanation.
rdn
ID IB PAIN, CLICK
rdn
ID II PAIN, HX LOCK CLICK
II
rdn
ID III PAIN, LOCK NO CLICK
II
no rdn
DJD CREPITUS
digital pressure on the muscle trigger point are detectable and a full range of opening
usually intensifies the joint pain, and local is observed. Organic lesions such as arthri-
anesthetic infiltration of the muscle elimi- tis can be ruled out when joint swelling is
nates the pain. In uncomplicated myogenic absent or when tomograms fail to show
facial pain, clicking or popping cannot be pathologic changes indicative of arthritis.
palpated or auscultated. Rarely, facial myal- Muscle splinting secondary to a high res-
gia may be associated with generalized toration or odontogenic infection should be
myalgia and fibrositis syndromes. ruled out by conducting a thorough dental
examination. Pain of myogenic origin may
DIFFERENTIAL DIAGNOSIS also mimic toothache in which the pain
Internal derangements can be excluded symptoms are referred to the maxilla or
from the differential when no joint sounds mandible.
PMPH_Eversole_Chapter-12.indd 643 1/20/2011 3:20:18 PM
644 Chapter 12
FIGURE 12-22
Trigger points (small blue
and yellow dots) and pain
referral patterns (red
circles) in myogenic pain
of masticatory and strap
muscles.
TREATMENT Laskin DM. Etiology of pain dysfunction syndrome.
J Am Dent Assoc. 1969;79:153.
Myogenic TMJ pain can be managed in a Travell JG. Temporomandibular joint pain referred
variety of ways. All methods are directed from muscles of the head and neck. J Prosthet Dent.
toward minimizing myospasm and para- 1960;10:745.
functional activities. Electromyographic bio-
feedback with stress management behavioral TYPE I INTERNAL
medicine is highly effective. Occlusal splints
DERANGEMENT (REDUCING)
may be employed, especially for nocturnal
bruxism and clenching. Ultrasound applied Figure 12-23
over affected muscles may also relieve myo- Age: Young and middle-aged adults
genic pain. Last, trigger point injections of Sex: Female predilection
a local anesthetic without a vasoconstrictor
CLINICAL FEATURES
into affected muscle may be useful as an
adjunctive management technique. Type I derangements may be subdivided
into two variants. Type IA is characterized
by clicking or popping of the affected joint
Additional Reading without pain, whereas type 1B is charac-
terized by clicking or popping with pain.
Chesley LD, Van Gilder JW. Eosinophilia-myalgia syn-
drome masquerading as facial pain. J Oral Maxillofac Both opening and closing clicks occur, and
Surg. 1990;48:980. the fact that they are detected at different
Clark GT. Classification, causation and treatment of condylar positions is important. The pain
masticatory myogenous pain and dysfunction. Oral may be a constant dull ache in the joint
Maxillofac Surg Clin North Am. 2008;20(2): 145-157
Harness DM, Rome HP. Psychological and behavioral
area, or it may be periodic and sharp, par-
aspects of chronic facial pain. Otolaryngol Clin North ticularly when the patient eats hard or tough
Am. 1989;22:1073. foods. Notably, the patient has no history of
PMPH_Eversole_Chapter-12.indd 644 1/20/2011 3:20:20 PM
Facial Pain and Neuromuscular Disorders 645
A history of locking or a persistent closed-
lock places the derangement into type II
and III, respectively. Tomograms should
be obtained to rule out degenerative joint
disease.
TREATMENT
Evidence indicates that this type of derange-
ment may be reversible. Alternatively, some
patients become progressively worse, and
progress to type II or III derangements, and
ultimately develop degenerative joint dis-
ease. Because muscle spasm may occur in
conjunction with clicking or pain and click-
FIGURE 12-23 ing, the muscles should be palpated for trig-
Arthrogram illustrating anterior displacement of
ger point tenderness, and electromyographic
the meniscus in a type 1B internal derangement.
scanning is advisable. Splint therapy, along
with muscle relaxation and stress manage-
locking. The problem is usually unilateral, ment strategies, is the treatment of choice.
yet can be bilateral. On opening, the man- Occlusal equilibration may be performed,
dible often deviates to the affected side, the particularly if the occlusion tends to retro-
click occurs, and the mandible then shifts to pose the mandible. Alternatively, recent stud-
the midline, reaching a full open position. ies tend to minimize the role of occlusion in
The pathogenesis of this disorder is related the etiology of this disorder. Arthroscopic
to anterior displacement of the TMJ menis- intervention in recalcitrant cases is advisable
cus. The etiology has not been clarified and because fibrous adhesions may need to be
is probably multifactorial. Bruxing, clench- freed.
ing, occlusal disharmony, yawning, man-
dibular trauma, and overextension of the
joint from intubation or prolonged open-
ing have been implicated. Many patients
Additional Reading
with a type IB internal derangement may Byahatti SM, Ramamurthy BR, Mubeen M, Agnihothri
PG. Assessment of diagnostic accuracy of high-reso-
manifest concurrent myospasm with trig- lution ultrasonography in determination of temporo-
ger point tenderness of masticatory and/or mandibular joint internal derangement. Indian J Dent
strap muscles of the neck. Tomograms fail to Res. 2010;21(2):189-194.
show pathologic osseous changes; however, Farrar WB, McCarty WL, Jr. Inferior joint space
arthrography and characteristics of condylar paths in
the condyle(s) on the affected side(s) may internal derangement of the TMJ. J Prosthet Dent.
appear to be retroposed, a finding that is not 1979;41:548.
always consistent. CT and MRI may be used Helms CA, Doyle GW, Orwig D, McNeill C, Kaban L.
to confirm anterior displacement of the disc, Staging of internal derangements of the TMJ with
magnetic resonance imaging: preliminary observa-
and arthroscopic examination is useful in
tions. J Craniomand Dis. 1989;3:93.
the diagnosis and detection of fibrous adhe- Perrott DH, Alborzi A, Kaban LB, Helms CA. A pro-
sions that may limit disc function. spective evaluation of the effectiveness of temporo-
mandibular joint arthroscopy. J Oral Maxillofac Surg.
DIFFERENTIAL DIAGNOSIS 1990;48:1029.
Wilkes CH. Structural and functional alterations of
Uncomplicated myogenic pain can be ruled the temporomandibular joint. Northwest Dent.
out when no joint sounds are apparent. 1978;57:287.
PMPH_Eversole_Chapter-12.indd 645 1/20/2011 3:20:29 PM
646 Chapter 12
TYPE II INTERNAL mately achieved. Alternatively, transient
DERANGEMENT (TRANSIENT open locks may occur, presumably related
LOCK) to entrapment of a reduced disc. An open
lock should not be confused with true sub-
Figure 12-24
luxation of the condyles, which lock ante-
Age: Young and middle-aged adults rior to a steep eminence. The mandible may
Sex: Female predilection deviate laterally on opening, and in some
patients, the deviation corrects at the fully
CLINICAL FEATURES
open position. Pain is usually dull and ach-
Anterior displacement of the meniscus with ing, but sharp episodes can occur during
clicking or popping and pain in the affected transient locking or when hard foods are
joint(s) along with a history of locking char- eaten. In addition, muscle trigger points
acterize the type II internal derangement. and elevated electromyographic readings
The displaced disc in patients with a his- may be noted, as patients with type II
tory of locking may not be a reversible phe- derangements sometimes manifest coexis-
nomenon. The retrodiscal tissues (bilami- tent myogenic pain.
nar zone) have been overdistended, and
the meniscus cannot be firmly positioned DIFFERENTIAL DIAGNOSIS
over the condylar head. Fibrous adhesions The other TMJ pain syndromes listed
may be present, augmenting the displace- here usually can be eliminated with the
ment. At surgery, the entire meniscus confirmation that locking occurs, yet is
may be found to be loose (“floppy disc”). transitory.
Patients may complain of transient closed
lock whereby they are unable to open TREATMENT
more than 15 to 25 mm, yet with automa-
Splint therapy with muscle relaxation and
nipulation of the mandible they are able
stress therapy should be attempted initially.
to open full range. In these instances, the
If no progress is achieved after 6 months or
displaced disc precludes translation of the
if the patient proceeds to a type III derange-
condyle, yet reduction of the disc is ulti-
ment with persistent, nonreducing closed
lock, arthroscopic surgery with release
of adhesions is recommended or surgical
intervention with meniscus repositioning
may be necessary.
Additional Reading
Chang SW, Chuang CY, Li JR, Lin CY, Chiu CT.
Treatment effects of maxillary flat occlusal splints
for painful clicking of the temporomandibular joint.
Kaohsiung J Med Sci. 2010;26(6):299-307.
Farrar WB. Craniomandibular practice: the state of
the art: definition and diagnosis. J Craniomand Prac.
1983;1:4.
Farrar WB, McCarty WL, Jr. Inferior joint space
arthrography and characteristics of condylar paths in
internal derangement of the TMJ. J Prosthet Dent.
FIGURE 12-24 1979;41:548.
Computed tomographic scan (blink mode) showing Katzberg RW, Dolwick MF, Helms CA , Hopens T , Bales
anterior meniscus displacement in a patient with DJ , Coggs GC. Arthrotomography of the temporoman-
transient locking, a type II internal derangement. dibular joint. AJR Am J Roentgenol. 1980;134:995.
PMPH_Eversole_Chapter-12.indd 646 1/20/2011 3:20:30 PM
Facial Pain and Neuromuscular Disorders 647
Schellhas KP. Internal derangement of the temporoman- strate anterior dislocation of the disc with-
dibular joint: radiologic staging with clinical, surgi- out reduction. As with the other types of
cal, and pathologic correlation. Magn Reson Imaging.
1989;7:495. internal derangements, a myogenic pain
Westesson PL. Double-contrast arthrotomography of component may be extant. Studies have
the temporomandibular joint. J Oral Maxillofac Surg. shown that about 20% of type I or II inter-
1983;41:163. nal derangement patients progress to closed
lock within 6 months, and this progression
can be correlated with degree of pain and a
TYPE III INTERNAL deep anterior recess.
DERANGEMENT (CLOSED
LOCK) DIFFERENTIAL DIAGNOSIS
Figure 12-25 The other types of internal derangements
can be excluded from consideration when
Age: Young and middle-aged adults
Sex: Female predilection
closed lock is encountered. Other disorders
unrelated to TMJ dysfunction must be con-
CLINICAL FEATURES sidered in the differential diagnosis when
Whereas types I and II manifest pain and unilateral locking is encountered. Not all of
clicking of the affected joint(s), type III these conditions are associated with pain
derangement is characterized by locking symptoms. Postinjection trismus, infec-
with pain. Average jaw opening is 20 mm. tions, and tumors of the pterygoid space
The disc is forward and precludes transla- and lateral pharynx must be considered.
tion of the condyle; therefore, no click can These disorders are discussed in detail
be palpated or auscultated, and the jaw under the heading Limited and Deviant Man-
deviates to the affected side. In bilateral dibular Opening.
involvement, the jaw fails to deviate. Pain
is chronic with a dull ache, and may be TREATMENT
exacerbated during masticatory function. If left untreated, type III derangement will
Occasionally, the examiner can reduce the most likely progress to degenerative joint
disc with manual manipulation of the con- disease (localized osteoarthritis). Patients
dyle; however, the patient is unable to do with closed lock can be treated by menis-
so unassisted. Arthrotomograms demon- cus reattachment surgery; however, supe-
FIGURE 12-25
Arthrograms in type III internal derangement. Left: Closed with anterior disc displacement. Right: Open
without reduction, the disc remains forward. Jaw deviates on opening to affected side.
PMPH_Eversole_Chapter-12.indd 647 1/20/2011 3:20:31 PM
648 Chapter 12
rior joint space arthroscopic surgery with ing and exhibits limited opening. Ausculta-
lysis of adhesions usually relieves pain and tion reveals crepitus. During arthrographic
increases range of motion. If myogenic pain evaluation with fluoroscopy, contrast media
is a concomitant, electromyographic (EMG) introduced to the lower compartment can
biofeedback with stress management thera- be seen to flow into the upper compart-
peutic methods are recommended following ment simultaneously. Arthrotomograms
postoperative recovery. Interestingly, patients also reveal dye opacity in both joint spaces.
receiving no therapy with a follow-up of 2 Superior joint space arthroscopic examina-
years have significant diminution of symp- tion may also be diagnostic; however, some
toms despite a chronically displaced disc. false-negative results have been reported.
DIFFERENTIAL DIAGNOSIS
Additional Reading Similar findings are encountered in degen-
Abramowicz S, Dolwick MF. 20-year follow-up study erative joint disease, which, of course, may
of disc repositioning surgery for temporomandibular coexist with a perforation. Crepitus may also
joint internal derangement. J Oral Maxillofac Surg. be detected in synovial chondromatosis as
2010;68(2):239-242.
well as in other types of chronic arthritis.
Dolwick MF. Surgical treatment of anterior displace-
ment of the TMJ meniscus. Case reports and outlines
of selected scientific sessions. 62nd Annual Meeting,
TREATMENT
AAOMS; 1980:42. Surgical correction is the treatment of
Imirzalioglu P, Biler N, Agildere AM. Clinical and radio-
logical follow-up results of patients with untreated
choice. A simple retrodiscal perforation
TMJ closed lock. J Oral Rehabil. 2005;32(5):326-331. can be closed primarily. Large perforations
Westesson PL, Omnell K-Å, Rohlin M. Double contrast with adhesions may require placement of a
tomography of the temporomandibular joint: a new disc prosthesis. Any condylar osteophytes
technique based on autopsy specimen examinations.
should be eliminated by arthroplasty
Acta Radiol (Diagn). 1980;21:777.
Westesson, P-L, Lundh H. Arthrographic and clinical
characteristics of patients with disk displacement who
progressed to closed lock during a 6-month period. Additional Reading
Oral Surg Oral Med Oral Pathol. 1989;67:654.
Cholitgul W, Petersson A, Rohlin M, Akerman S. Clinical
and radiographic findings in temporomandibular
joints with disc perforation. Int J Oral Maxillofac Surg.
MENISCUS PERFORATION 1990;19:220.
Figure 12-26
Age: Young and middle-aged adults
Sex: Female predilection
CLINICAL FEATURES
Perforation of the meniscus may occur sub-
sequent to chronic anterior displacement,
whereby the condylar head articulates with
the loose connective tissues of the retrodis-
cal or bilaminar zone. Alternatively, perfora-
tions may occur in the fibrotic intermediate
zone or even anterior to the anterior band of
the meniscus. In these instances, the condyle FIGURE 12-26
has no cushion and may rub directly against Arthrogram showing contrast media in both upper
the glenoid fossa incline. Characteristically, and lower joint spaces in cases of meniscus perfora-
the patient has a history of clicking and lock- tion. A: Closed. B: Open.
PMPH_Eversole_Chapter-12.indd 648 1/20/2011 3:20:41 PM
Facial Pain and Neuromuscular Disorders 649
Helms CA, Katzberg RW, Dolwick MF, Bales DJ. referred to as Heberden’s nodes. Limita-
Arthrotomographic diagnosis of meniscus perforation in tion of motion and pain are also featured.
the temporomandibular joint. Br J Radiol. 1980;53:283.
Ireland VE. The problem of “the clicking jaw.” Proc R The TMJ is not often involved in general-
Soc Med. 1951;44:191. ized degenerative joint disease, localized
Kurita K, Bronstein SL, Westesson PL, Sternby NH. TMJ osteoarthritis being more common.
Arthroscopic diagnosis of perforation and adhesions Localized arthritis of the TMJ may evolve
of the temporomandibular joint: correlation with
postmortem morphology. Oral Surg Oral Med Oral
secondary to trauma; evidence increasingly
Pathol. 1989;68:130. implicates untreated internal derangements
Schellhas KP, Wilkes CH, Omlie MR. The diagnosis of tem- with an anterior meniscus as a precursor
poromandibular joint disease: two compartment arthrog- to degenerative disease. When the condyle
raphy and MR. AJR Am J Roentgenol. 1988;151:341.
is no longer protected by the meniscus or
when the meniscus is loosely attached,
OSTEOARTHRITIS perforation may occur, resulting in bone-to-
(DEGENERATIVE JOINT bone contact between the mandibular con-
dylar head and the articular fossa. Erosions,
DISEASE)
eburnation, and osteophyte formation
Figure 12-27 evolve with resultant chronic pain. Most
Age: Middle-aged and elderly adults patients with degenerative joint disease
Sex: Female predilection have crepitant joint sounds while opening
and closing. Tomograms reveal flatten-
CLINICAL FEATURES
ing of the condylar head, eburnation with
Generalized osteoarthritis is a degenerative deformation, erosions, and anterior or supe-
process involving, primarily, weight-bear- rior osteophytic lipping. Similar changes
ing joints and metacarpophalangeal joints. occur on the articular fossa; however, these
The latter may evince nodular excrescences changes rarely are radiographically demon-
FIGURE 12-27
Degenerative joint dis-
ease (osteoarthritis). TMJ
showing “bird break” ante-
rior osteophytes, condylar
head flattening, and Ely cyst
in condylar neck (right).
PMPH_Eversole_Chapter-12.indd 649 1/20/2011 3:20:43 PM
650 Chapter 12
strable. In chronic osteoarthritis of long RHEUMATOID ARTHRITIS
standing, the patient, despite crepitus, may Figure 12-28
be pain free. Alternatively, ankylosis may
develop, but this is unusual. Age: Young and middle-aged adults
Sex: Female predilection
DIFFERENTIAL DIAGNOSIS CLINICAL FEATURES
A diagnosis of localized TMJ degenerative Rheumatoid arthritis is a collagen disease
joint disease is based on the presence of associated with poststreptococcal immu-
crepitus on auscultation with radiographic nopathic tissue changes localized in the
confirmation of osseous changes. A history joints. This progressive disorder is variable
of trauma or of symptoms that indicate a in its regional distribution; however, there
preexistent internal derangement, in con- is a tendency for symmetric involvement.
junction with the aforementioned criteria, The second and third metacarpophalan-
provides insight into the possible patho- geal and proximal interphalangeal joints
genesis of the disease. The radiographic are most frequently involved, followed by
changes in TMJ osteoarthritis are similar if the knee, wrist, shoulder, ankle, elbow,
not identical to those encountered in rheu- and vertebrae. The chief extra-articular
matoid arthritis. The latter is a TMJ mani- manifestation of the disease is anemia. The
festation of a polyarthritic condition. affected joints are warm to the touch, swol-
len, and painful. The TMJ is frequently
TREATMENT involved; when it is, bilateral pain is accom-
When the pain is mild, management with panied by generalized joint disease. Crepi-
analgesics or nonsteroidal prostaglandin tation with stiffness is more commonly
inhibitors may be adequate. When pain is noted than pain. In rheumatic joint disease
moderate and problematic, condylar con- of childhood onset, involvement of the TMJ
touring or condylectomy with placement may result in retarded development of the
of a prosthesis may be indicated along mandible and a class II malocclusion with
with meniscoplasty. Surgical procedures open bite. Condylar destruction and TMJ
of this nature may alter the occlusion, ankylosis occur in rare instances. Transcra-
thus requiring orthodontic or restorative nial radiographs or, preferably, TMJ tomo-
correction. grams often disclose pathologic alterations,
including irregular condylar articulating
Additional Reading surfaces, flattening of the condyle, and
osteophyte formation with increased joint
Bauer WH. Osteoarthritis of the temporomandibular space dimension. Rheumatoid nodules of
joint. Am J Pathol. 1941;17:129. the preauricular soft tissues have not been
Machon V, Hirjak D, Lukas J. Therapy of the osteoarthri- encountered. Rheumatoid factor as assayed
tis of the temporomandibular joint. J Craniomaxillofac
Surg. 2010 Aug 6. [Epub ahead of print]
by latex agglutination from a serum sample
Ogus H. Degenerative disease of the temporomandibu- is the primary laboratory finding of diag-
lar joint in young persons. Br J Oral Maxillofac Surg. nostic importance.
1979;17:17.
Seligman DA, Pullinger AG. TMJ derangements and DIFFERENTIAL DIAGNOSIS
osteoarthrosis subgroups differentiated according to
active range of mandibular opening. J Craniomand The pain of TMJ rheumatoid arthritis may be
Dis. 1988;2:35. confused with that of other arthritides and
Westesson P-L, Rohlin M. Internal derangement
related to osteoarthrosis in temporomandibular joint
the myofascial pain dysfunction syndrome.
autopsy specimens. Oral Surg Oral Med Oral Pathol. The bilateral nature and association with
1984;57:17. generalized joint pain and swelling are
PMPH_Eversole_Chapter-12.indd 650 1/20/2011 3:20:55 PM
Facial Pain and Neuromuscular Disorders 651
FIGURE 12-28
Rheumatoid arthritis. Condylar
flattening, atrophy and erosion.
Hand film showing erosions of
proximal interphalangeal joints.
highly suggestive of rheumatoid arthritis, Hajati AK, Näsström K, Alstergren P, Bratt J, Kopp S.
particularly when rheumatoid nodules are Temporomandibular joint bone tissue resorption in
patients with early rheumatoid arthritis can be pre-
found over extremity joints. The rheuma- dicted by joint crepitus and plasma glutamate level.
toid factor is generally a positive finding in Mediators Inflamm. 2010;2010:627803.
the serum along with elevated glutamate. Rohlin M, Petersson A. Rheumatoid arthritis of the tem-
poromandibular joint: radiologic evaluation based on
standard reference films. Oral Surg Oral Med Oral
TREATMENT
Pathol. 1989;67:594.
Treatment for TMJ arthritis is not specific. Ronning D, Valiaho ML, Laaksonen AL. The involve-
The generalized disease should be man- ment of the temporomandibular joint in juvenile
arthritis. Scand J Rheumatol. 1974;3:89.
aged by a physician and includes the use of
steroids or other immunosuppressive drugs
along with analgesics. When fibrous anky-
losis or severe joint destruction is present, ACUTE INFECTIOUS
surgical intervention may be indicated. ARTHRITIDES
Age: Young adults
Additional Reading Sex: No predilection
Bornstein LA, Ramon Y. Bony ankylosis of the temporo- CLINICAL FEATURES
mandibular joints due to juvenile rheumatoid arthritis. Acute or suppurative TMJ arthritis is usu-
Br J Plast Surg. 1963;16:95.
Ericson S, Lundberg M. Alterations in the temporoman-
ally the result of a bacteremia with pyogenic
dibular joint at various stages of rheumatoid arthritis. organisms. Gonococcal, streptococcal, and
Acta Rheumatol Scand. 1967;13:357. staphylococcal organisms are seen most
PMPH_Eversole_Chapter-12.indd 651 1/20/2011 3:20:56 PM
652 Chapter 12
frequently in test cultures. The preauricu- recovery period prevent the development of
lar tissues are swollen and erythematous; adhesions.
they are acutely tender when palpated,
both directly and intrameatally. The patient
restricts opening; deviation of the man-
Additional Reading
dible toward the affected side is apparent. Alexander WN, Nagy WW. Gonococcal arthritis of the
Aspiration yields an exudate, and a culture temporomandibular joint. Oral Surg Oral Med Oral
Pathol. 1973;36:809.
should be obtained for specific identifica-
Cai XY, Yang C, Zhang ZY, Qiu WL, Chen MJ, Zhang
tion of the infectious agent. Acute arthritis SY. Septic arthritis of the temporomandibular joint:
is rare, but chronic granulomatous arthritis, a retrospective review of 40 cases. J Oral Maxillofac
which is usually related to tuberculosis, is Surg. 2010;68(4):731-738.
even less frequent. In tuberculosis arthritis, Goodman WS. Infections of the temporomandibular
joint. J Otolaryngol. 1979;8:250.
pain and tenderness are uncommon; how- Winters SE. Staphylococcus infection of the temporo-
ever, a preauricular swelling may be pres- mandibular joint. J Oral Maxillofac Surg. 1955;8:148.
ent. Acute arthritis causes exudate accumu- Wurman LH, Flannery JV, Jr, Sack JG. Osteomyelitis of
lation in the joint spaces, and tuberculous the mandibular condyle secondary to dental extrac-
tions. Otolaryngol Head Neck Surg. 1979;87:190.
arthritis causes granulomas; consequently,
the joint space dimensions may be enlarged
on TMJ tomograms, and a posterior open MISCELLANEOUS
bite can be seen on the affected side. ARTHRITIDES
Figure 12-29
DIFFERENTIAL DIAGNOSIS
Acute arthritis is unique in that swelling Age: Adults
and acute pain coexist with limited open- Sex: Predilection depends on specific disease
ing and deviation. In addition, joint sounds CLINICAL FEATURES
are absent. Aspiration of the periarticular On rare occasions, polyarthritic disease
area with evidence of a purulent exudate associated with hyperuricemic gout, pyro-
confirms the initial clinical impression of phosphate arthritis, psoriasis, ankylosing
acute arthritis. spondylitis, lupus erythematosus, and scle-
roderma affect the TMJ. Most patients with
TREATMENT these arthritides do not manifest signifi-
Aspiration and drainage should be per- cant TMJ signs or symptoms. In gout, the
formed initially, followed by culture and synovial tissues are the site of urate crystal
sensitivity testing of the aspirated exudate. formation, which initiates an inflammatory
An appropriate antibiotic may then be pre- reaction with hyperplasia of the periarticu-
scribed. Jaw movement exercises during the lar tissues. With progressive deposition of
FIGURE 12-29
Miscilaneous arthritides. Gout (left), psoriatic (center), erosions and osteophyte (right) in TMJ psoriatic
arthritis.
PMPH_Eversole_Chapter-12.indd 652 1/20/2011 3:21:09 PM
Facial Pain and Neuromuscular Disorders 653
urates, pain and limitation of motion may the symptoms. Most of these patients are
be observed along with osseous resorption under the care of a physician, and treatment
late in the course of the disease. A small should be pursued after medical consulta-
fraction of psoriasis patients develop arthri- tion. When unrelenting pain is a feature and
tis in the form of monoarticular or oligoar- is refractory to conservative management,
ticular symptoms. Ankylosing spondylitis surgical intervention may be indicated.
is an asymmetric oligoarthropathy that pri-
marily affects the spine, particularly the sac-
roiliac joint, while, in general, sparing small
Additional Reading
peripheral joints. In systemic lupus erythe- Bhattacharyya I, Chehal H, Gremillion H, Nair M, Odont
matosus, fibrinoid necrotic foci may occur L. Gout of the temporomandibular joint: a review of
in the articular tissue. Dystrophic calcifica- the literature. J Am Dent Assoc. 2010;141(8):979-985.
Davison C, Wojtulewski JA, Bacon PA, Winstock D.
tions and articular erosions may occur in Temporomandibular joint disease in ankylosing spon-
the later stages of systemic sclerosis (sclero- dylitis. Ann Rheum Dis. 1975;34:87.
derma). In some instances, these arthritides Koorbusch GF, Zeitler DL, Fotos PG, Doss JB. Psoriatic
affect the TMJ, and the patient may suffer arthritis of the temporomandibular joints with ankylo-
sis. Literature review and case reports. Oral Surg Oral
pain, joint swelling, and limited opening. Med Oral Pathol. 1991;71:267.
Radiographic evidence of condylar erosions Liebling MR, Gold RH. Erosions of the temporoman-
may be identified on tomograms. dibular joint in systemic lupus erythematosus. Arthritis
Rheum. 1981;24:948.
DIFFERENTIAL DIAGNOSIS Lundberg M, Ericson S. Changes in the temporomandib-
ular joint in psoriasis arthropathia. Acta Dermatovener
The jaw signs and symptoms appearing in (Stockh). 1967;47:354.
these miscellaneous arthropathies do not dif- Osial TA, Avakian A, Sassouni V, Agarwal A, Medsger TA,
fer from those encountered in rheumatoid or Jr, Rodnan GP. Resorption of the mandibular condyles
and coronoid processes in progressive systemic sclero-
degenerative TMJ arthritis. The specific diag- sis (scleroderma). Arthritis Rheum. 1981; 24:729.
nosis is based on distribution of joint symp-
toms throughout the skeleton in conjunction
with other clinical and laboratory findings. CONDYLAR FRACTURE
Figure 12-30
TREATMENT
Age: No predilection
In general, conservative therapy is indicated;
Sex: No predilection
many other joints are involved, and pain
symptoms beyond the craniomandibular CLINICAL FEATURES
articulation tend to be more troublesome. Although trauma to the mandible may
Physical therapy, ultrasound, occlusal splints, occur at any age, condylar neck and sym-
and nonnarcotic analgesics often alleviate physis fractures are commonly seen in
FIGURE 12-30
Condylar Fractures. A: Lateral
jaw showing low subcondy-
lar fracture. B: AP tomograms
showing bilateral subcondylar
fractures with medial displace-
ment. (Courtesy of Dr. William
Donlon.) C: Double condyle
occurring subsequent to nonre-
A B C ducing condylar fracture.
PMPH_Eversole_Chapter-12.indd 653 1/20/2011 3:21:15 PM
654 Chapter 12
children. The fracture may be unilateral or choice. At long-term follow-up, function is
bilateral, greenstick, complete, or commi- adequate; however, radiographs may dis-
nuted. In unilateral subcondylar fractures, close bilobed condyles.
the occlusion is altered with a shift of the
mandible toward the affected side. Palpa-
tion of the preauricular area causes pain, Additional Reading
which may be severe; in most cases, swell- Blevins C, Gores RJ. Fractures of the mandibular condy-
ing is detectable. The jaw deviates on open- loid process: results of conservative treatment in 140
ing, and movement is painful. In bilateral patients. J Oral Maxillofac Surg. 1961;19:392.
complete fractures, the patient presents Dahlstrom L, Kahnberg KE, Lindahl L. 15 years follow-
up on condylar fractures. Int J Oral Maxillofac Surg.
with a gagged occlusion that is character- 1989;18:18.
ized by retropositioning and an anterior Danda AK, Muthusekhar MR, Narayanan V, Baig MF,
open bite. Towne’s, panoramic, ramus lat- Siddareddi A. Open versus closed treatment of unilat-
eral jaw, and anteroposterior or submental eral subcondylar and condylar neck fractures: a pro-
spective, randomized clinical study. J Oral Maxillofac
vertex radiographs disclose the site of frac- Surg. 2010;68(6):1238-1241.
tures. In complete fractures, the condyle is MacLennan WD, Simpson W. Treatment of fractured
usually anteromedially displaced. Green- mandibular condyle processes in children. Br J Plast
stick fractures in children may not show Surg. 1965;18:4.
Sahm G, Witt E. Long-term results after childhood con-
any condylar displacement. dylar fractures. A computer-tomographic study. Eur J
Orthodont. 1989;11:154.
DIFFERENTIAL DIAGNOSIS
Restricted or deviant opening associated
with subcondylar fracture is, of course, SYNOVIAL CHONDROMATOSIS
preceded by a traumatic blow to the man- Figure 12-31
dible; therefore, the diagnosis is readily sus-
Age: Middle-aged adults
pected and easily confirmed by obtaining
Sex: Female predilection
radiographs.
CLINICAL FEATURES
TREATMENT Synovial chondromatosis is a reactive phe-
Most surgeons agree that open reduction is nomenon that is seldom encountered in the
rarely necessary for the treatment of condy- periarticular tissues of the TMJ. Single or
lar neck fractures. Closed reduction with multiple ovoid bodies composed of hyaline
intermaxillary fixation is the treatment of cartilage form in the subsynovial connec-
FIGURE 12-31
Synovial chondromatosis.
Computed tomography
and 3D reconstruction
showing “joint mice” ante-
rior to condyle.
PMPH_Eversole_Chapter-12.indd 654 1/20/2011 3:21:23 PM
Facial Pain and Neuromuscular Disorders 655
tive tissue; they enlarge and then become Cai XY, Yang C, Chen MJ, Jiang B, Wang BL.
detached, thus forming loose bodies within Arthroscopically guided removal of large solitary syn-
ovial chondromatosis from the temporomandibular
the joint spaces. Alternatively, it has been joint. Int J Oral Maxillofac Surg. 2010 Jul 12. [Epub
suggested that some are generated when ahead of print]
osteophytic projections in arthritic joints Herzog S, Mafee M. Synovial chondromatosis of the
become detached to form loose bodies. In TMJ: MR and CT findings. AJNR. 1990;11:742.
McCain JP, de la Rua H. Arthroscopic observation and
fact, in some cases, these cartilaginous nod- treatment of synovial chondromatosis of the tem-
ules remain in continuity with the articular poromandibular joint. Int J Oral Maxillofac Surg.
tissues, meniscus, or condylar head. They 1989;18:233.
calcify or undergo endochondral ossifica- Tasanen A, Lamberg MA, Kotilainen R. Osteochon-
dromatosis of the temporomandibular joint: report
tion and can be visualized as focal radiopac- of a case. Oral Surg Oral Med Oral Pathol. 1974;
ities radiographically. The mandible usually 38:845.
deviates toward the affected side, and the
chondroid bodies may cause cross-bite or
open-bite occlusion. Pain, particularly dur- PIGMENTED VILLONODULAR
ing mastication, is often a complaint. Larger SYNOVITIS
lesions may be palpable over the condyle,
and clicking or crepitus can be auscultated. Age: Middle-aged adults
Multiple chondroid bodies may be pres- Sex: No predilection
ent with resultant double or triple clicks on CLINICAL FEATURES
opening and closing. Synovial chondroma-
Pigmented villonodular synovitis is a reac-
tosis may occur in conjunction with reac-
tive proliferation of the synovial lining cells
tive synovial proliferation (villonodular
and underlying periarticular connective
synovitis).
tissue with a predilection for the knee joint.
DIFFERENTIAL DIAGNOSIS
The lesion is rare in the TMJ. It can be exper-
imentally induced by intra-articular injec-
Internal derangements with meniscus tions of blood and saline, thus suggesting
displacement or perforation and arthritic the possibility of traumatic hemarthrosis
joints manifest similar clinical features. in its genesis. Microscopically, villous pro-
Transcranial and TMJ tomograms disclose liferations extend into the joint space, and
the presence of joint space opacities when the supportive fibrovascular tissue contains
calcification is present. It is probable that multinucleated giant cells and hemosid-
if contrast media arthrography were used, erin pigment deposition. Many of the cases
noncalcified joint bodies would be demon- reported in the TMJ have been associated
strable in relief. with chondroid metaplasia, thus suggesting
the coexistence of synovial condromatosis.
TREATMENT In other joints, osseous erosion is uncom-
Surgical removal is the treatment of choice. mon, yet may occur. In the TMJ, radio-
Meniscus displacement, fibrous adhe- graphic and surgical evidence of condylar
sions, villonodular synovitis, and arthritic erosion may be observed. Clinical findings
changes may be present; they also require include pain, swelling, limited opening,
surgical correction. and deviation toward the affected side.
DIFFERENTIAL DIAGNOSIS
Additional Reading Pigmented villonodular synovitis is diag-
Ballard R, Weiland LH. Synovial chondromatosis of the nosed on the basis of microscopic features.
temporomandibular joint. Cancer. 1972;30:791. Clinically, the disease may mimic internal
PMPH_Eversole_Chapter-12.indd 655 1/20/2011 3:21:31 PM
656 Chapter 12
derangements, neoplasms, synovial chon- Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonod-
dromatosis, and arthritis. When condy- ular synovitis in the temporomandibular joint. A case
report. Arch Pathol Lab Med. 1941;31:730.
lar erosion is radiographically evident Takagi M, Ishikawa G. Simultaneous villonodular syno-
and when a palpable preauricular mass vitis and synovial chondromatosis of the temporoman-
can be detected, surgical intervention dibular joint: report of case. J Oral Maxillofac Surg.
with biopsy of the periarticular mass is 1981;39:699.
recommended.
TREATMENT Sialogenic Pain
Surgical excision and repair of the articular
soft tissues is the treatment of choice. Con- SIALOLITHIASIS
dylar destruction may necessitate place- Figure 12-32
ment of a joint prosthesis.
Age: Adults
Sex: Male predilection
Additional Reading CLINICAL FEATURES
Cai XY, Yang C, Chen MJ, Yun B. Simultaneous pigment- Salivary calculi are more common in the
ed villonodular synovitis and synovial chondromatosis submandibular duct than in the parotid
of the temporomandibular joint: case report. Int J Oral duct. The pain associated with salivary cal-
Maxillofac Surg. 2009;38(11):1215-1218.
Dawiskiba S, Eriksson L, Elner A, Johansen CC, Hansson culi is experienced during salivation and
LG, Westesson PL. Diffuse pigmented villonodular therefore is notable during meals. Blockage
synovitis of the temporomandibular joint diagnosed of the main excretory duct causes saliva dis-
by fine-needle aspiration cytology. Diag Cytopathol. tention throughout the duct tree, producing
1989;5:301.
Dinerman WK, Myers EN. Pigmented villonodular teno-
a drawing or stinging pain. The subman-
synovitis of the temporomandibular joint. Trans Am dibular area is often swollen during pain
Acad Ophthalmol Otolaryngol. 1977;84:132. episodes, and the swelling may be tender
FIGURE 12-32
Sialolith in submandibu-
lar duct, causing pain and
swelling at mealtimes.
Parotid duct stone (right).
PMPH_Eversole_Chapter-12.indd 656 1/20/2011 3:21:31 PM
Facial Pain and Neuromuscular Disorders 657
to palpation. Prolonged blockage may pre- Lustmann J, Regev E, Melamed Y. Sialolithiasis. A sur-
dispose to acute bacterial sialadenitis with vey on 245 patients and a review of the literature. Int J
Oral Maxillofac Surg. 1990;19:135.
constant pain. Occlusal radiographs should Pollack CV, Jr, Severance, HW, Jr. Sialolithiasis: case
be obtained in both anterior and posterior studies and review. J Emerg Med. 1990;8:561.
regions. Most stones are located anteriorly;
however, some may be found posteriorly
underlying the retromylohydoid ductal ENDEMIC PAROTITIS (MUMPS)
flexure. A panoramic radiograph or lateral Figure 12-33
skull radiograph should be obtained when
a parotid stone is suspected. When symp- Age: Children and young adults
toms indicate sialolithiasis yet radiographs Sex: No predilection
fail to uncover a stone, the gland should CLINICAL FEATURES
be milked to evaluate salivary flow. When
no flow can be elicited, a sialogram should Endemic parotitis is a paramyxovirus infec-
be ordered to evaluate for the possibility tion of the parotid glands causing bilateral
of a noncalcified blockage or focal duct parotid swelling and moderate to severe pain.
stenosis. Occasionally, the submandibular glands are
enlarged and painful. Pain increases when
DIFFERENTIAL DIAGNOSIS
sour or bitter foods are ingested. Milking
the gland often causes exudation at the ori-
Pain in the region of the submandibu-
lar gland could represent submandibu-
lar lymphadenopathy that is secondary to
odontogenic infection or is a nonspecific
sign of viral infection. The dentition should
be evaluated when radiographs are nega-
tive for a sialolith.
TREATMENT
Small stones can occasionally be manipu-
lated digitally and extruded from the duct
orifice. Surgery is required in most cases.
When duct blockage has persisted for a
long time, thus causing sclerosing sialaden-
itis, sialectomy may be required to prevent
multiple recurrent episodes of acute suppu-
rative sialadenitis.
Additional Reading
El Gehani R, Krishnan B, Shehoumi MI. Submandibular
giant sialoliths: report of two cases and review
of the literature. Ear Nose Throat J. 2010;89(6):
E1-E4.
Harrison GR. Calculi of the salivary glands and ducts.
Surg Gynecol Obstet. 1926;43:431.
Levy BM, ReMine WH, DeVine KD. Salivary gland
calculi: pain, swelling associated with eating. JAMA. FIGURE 12-33
1962;181:1115. Endemic parotitis.
PMPH_Eversole_Chapter-12.indd 657 1/20/2011 3:21:38 PM
658 Chapter 12
fice of Stensen’s duct. Constitutional signs ganisms. Two predisposing factors are asso-
and symptoms of infectious disease include ciated with nonviral sialadenitis. Surgical
malaise, fever, and cervical lymphadenopa- mumps is uncommon, representing a sup-
thy. Orchitis or oophoritis are complications. purative bacterial parotitis in elderly patients
The serum amylase level is elevated. Since recovering from surgery (usually abdomi-
development of the mumps vaccine, the dis- nal). It has also been reported to occur in
ease has become less prevalent. xerostomic patients receiving phenothiaz-
ine therapy. The parotids are enlarged and
DIFFERENTIAL DIAGNOSIS painful, and Stensen’s ducts usually have a
The swelling seen in mumps should not purulent exudate. Postobstruction sialaden-
be confused with benign lymphoepithe- itis is a suppurative bacterial infection that
lial lesion of Sjögren’s syndrome, which is develops in an occluded gland. The occlu-
painless. Acute suppurative sialadenitis is sion may be the consequence of calculus or a
encountered in elderly adults. If a bacterial focal excretory duct stricture. The involved
infection is suspected, the duct secretions gland is swollen and painful. If the obstruc-
or exudate can be cultured. tion is still present and exudate cannot
escape, draining cutaneous or oral fistulas
TREATMENT may develop. Regardless of the predispos-
ing conditions, fever and malaise are com-
Endemic parotitis resolves within 2 weeks.
mon but not invariable findings.
A bland diet, bed rest, and aspirin are rec-
ommended in conjunction with medical
DIFFERENTIAL DIAGNOSIS
consultation because of possible orchitis,
oophoritis, or meningitis. Acute suppurative sialadenitis must be
differentiated from endemic parotitis and
simple, uncomplicated sialithiasis. Pain and
Additional Reading swelling are common to all three diseases.
Both an exudate and cultivatable pathogenic
Banks P. Nonneoplastic parotid swellings: a review. Oral
Surg Oral Med Oral Pathol. 1968;25:732. organisms are required for the diagnosis.
Liang Y, Ma S, Liu L, et al. Identification and develop-
ment of a promising novel mumps vaccine candidate TREATMENT
strain. Microbes Infect. 2010 Aug 24. [Epub ahead of
print.] The exudate should be cultured, and peni-
Seibert RW, Seibert JJ. High resolution ultrasonogra- cillin should be prescibed. Pending results
phy of the parotid gland in children. Pediatr Radiol. of culture and sensitivity, an alternative
1988;19:13. antibiotic may be necessary, particularly
Wolman IJ, Evans BC, Lasker S, Jaegge K. Amylase lev-
els during mumps: the findings in blood and saliva. Am when penicillinase-producing staphylo-
J Med Sci. 1947;213:477. cocci are the predominant pathogens.
ACUTE SUPPURATIVE
SIALADENITIS
Additional Reading
Banning GL. Postoperative suppurative parotitis. Arch
Age: Middle-aged and elderly adults Surg. 1964;89:653.
Sex: Male predilection Carlson RG, Glas WE. Acute suppurative parotitis:
twenty-eight cases at a county hospital. Arch Surg.
CLINICAL FEATURES 1963;86:659.
Dance DA, Davis TM, Wattanagoon Y, et al. Acute sup-
Acute bacterial sialadenitis is usually caused purative parotitis caused by Pseudomonas pseudomal-
by streptococcal or staphylococcal microor- lei in children. J Infect Dis. 1989;159:654.
PMPH_Eversole_Chapter-12.indd 658 1/20/2011 3:21:39 PM
Facial Pain and Neuromuscular Disorders 659
Turner MD, Glickman R. Case presentations of salivary symptomatology of migraine. Furthermore,
gland infections. Oral Maxillofac Surg Clin North Am. migraine may be accompanied by tension
2009;21(3):359-362.
headache, with episodic classic attacks
being superimposed over constant dull
Temporal Pain aching pain of the frontalis and temporalis
areas.
MIGRAINE
TREATMENT
Age: Young adults
Ergotamine tartrate (with or without caf-
Sex: Female predilection
feine) suppositories or sublingual tablets
CLINICAL FEATURES usually relieve pain. Skin temperature
Migraine headache has been reported to and EMG biofeedback along with stress
affect 20% of the female population. It is not management have been highly successful.
nearly as prevalent among males. The pain Medical prophylactic management with
is usually unilateral (hemicrania), yet can propranolol has been effective, as has vera-
be bilateral. The classic form of migraine pamil (320 mg/day). For menstrual cycle–
is characterized by prodromal or concur- associated migraine, tiptan drugs have
rent symptoms including nausea, vomit- proven effective.
ing, flashing lights, scotomas, hemianopia,
and/or photophobia. Speech disorders,
paresthesias, and confusion are frequently Additional Reading
encountered. The pain is moderate to Anthony M, Hinterberger H, Lance JW. Plasma serotonin
severe, throbbing, and often incapacitat- in migraine and stress. Arch Neurol. 1967;16:544.
ing. The episodes may occur 2 or 3 times Medina JL, Diamond S, Franklin MA. Biofeedback ther-
monthly, and pain may persist for many apy for migraine. Headache. 1976;16:115.
Selby G, Lance JW. Observations on 500 cases of
hours. It is localized around the temporal migraine and allied vascular headache. J Neurol
area and often involves the frontal and ret- Neurosurg Psychiatr. 1960;23:23.
ro-orbital regions. The disorder is familial, Solomon GD. Verapamil in migraine prophylaxis—a five-
and emotional problems may precipitate an year review. Headache. 1989;29:425.
Sullivan E, Bushnell C. Management of menstrual
attack. Evidence supports a vascular source migraine: a review of current abortive and prophylac-
subsequent to vasodilation of the external tic therapies. Curr Pain Headache Rep. 2010;14(5):
carotid branches. The superficial temporal 376-384.
vessels are often dilated during an attack;
thermograms show a decrease in facial
skin temperature, presumably resulting MYOGENIC PAIN (TENSION
from shunting of blood away from the skin. HEADACHE)
Blood serotonin levels are decreased dur-
ing attacks. Age: Young and middle-aged adults
Sex: No predilection
DIFFERENTIAL DIAGNOSIS CLINICAL FEATURES
The signs and symptoms of migraine are Muscle tension headaches are the most
characteristic and usually pathognomonic. common form of headache. The pain may
Regardless, CNS neoplasms and organic be referred to the TMJ; however, diffuse
rather than functional vascular disease pain over the temporal, frontal, and masse-
must be considered in the differential diag- teric regions is more often the chief symp-
nosis, as these conditions may mimic the tom. Suboccipital, shoulder, and neck pain
PMPH_Eversole_Chapter-12.indd 659 1/20/2011 3:21:39 PM
660 Chapter 12
may occur. Myogenic pain is the result of of vasoconstrictor is also beneficial as an
prolonged and sustained muscle contrac- adjunctive procedure.
tion that is related to anxiety or stress. The
pain itself is thought to arise subsequent
to muscular accumulation of lactic acid. Additional Reading
Myogenic facial pain is characterized by
Blanchard EB, Appelbaum KA, Radnitz CL, et al.
a constant dull to moderate ache, which
Placebo controlled evaluation of abbreviated progres-
is usually poorly localized. Palpation of sive muscle relaxation and of relaxation combined with
the frontalis, temporalis, masseter, ptery- cognitive therapy in the treatment of tension head-
goids, sternomastoid, trapezius, and strap ache. J Consult Clin Psychol. 1990;58:210.
muscles of the neck locate acutely tender Carlsson SG, Gale EN. Biofeedback treatment for mus-
cle pain associated with the temporomandibular joint.
foci, referred to as muscle trigger points. J Behav Ther Exp Psychiatry. 1976;7:383.
Prolonged pressure on a trigger point Fernández-de-las-Peñas C, Caminero AB, Madeleine
often causes diffuse referred pain in the P, et al. Multiple active myofascial trigger points and
areas constituting the chief complaint. pressure pain sensitivity maps in the temporalis mus-
cle are related in women with chronic tension type
Indeed, specific muscles show predict- headache. Clin J Pain. 2009;25(6):506-512.
able routes of pain referral. Patients with Travell JG. Temporomandibular joint pain referred
uncomplicated myogenic facial pain do from muscles of the head and neck. J Prosthet Dent.
not manifest clicking or popping joints. 1960;10:745.
Travell J. Identification of myofascial trigger point syn-
Nevertheless, because of muscle spasm dromes: a case of atypical facial neuralgia. Arch Phys
and soreness, deviant jaw opening may be Med Rehabil. 1981;62:100.
a feature.
DIFFERENTIAL DIAGNOSIS GIANT CELL ARTERITIS
A diagnosis of uncomplicated myogenic Figure 12-34
facial pain is made when no joint sounds
are heard and when no palpable clicks are Age: Elderly adults
detected in the TMJ. Myospasm can develop Sex: Female predilection
secondarily if other pain disorders are CLINICAL FEATURES
extant. A newly placed high dental restora- Giant cell arteritis (GCA), also termed tem-
tion or a painful tooth may initiate muscle poral arteritis, is related to polymyalgia
guarding or splinting to protect against rheumatica (PMR), a disorder character-
occluding of the tooth in question. ized by shoulder and pelvic girdle pain
with muscular weakness, absence of joint
TREATMENT
disease, and presence of an elevated eryth-
Myogenic facial pain is a stress disorder. rocyte sedimentation rate. GCA and PMR
Treatment is directed toward breaking the often coexist. Giant cell arteritis is a gran-
myospasm pain cycle. Stress management ulomatous disease of unknown etiology
and electromyographic biofeedback are affecting the muscular-intimal layers of
extremely beneficial in this regard; when arteries, primarily cranial and facial vessels.
bruxism or clenching coexists, an occlusal The disease is characterized by episodic
splint may be employed. Short-term use of pain over the temple or temple and maxilla
muscle relaxants, anxiolytics, and analge- along with palpation tenderness of vessels,
sics are initially beneficial, yet should be fever, anorexia, and eventual blindness. The
phased out as the other forms of treatment pain is sharp or shooting with intervening
begin to achieve results. Injection of muscle periods of persistent dull ache. The tem-
trigger points with an anesthetic devoid poral artery may be prominent and visibly
PMPH_Eversole_Chapter-12.indd 660 1/20/2011 3:21:40 PM
Facial Pain and Neuromuscular Disorders 661
Mowat AG, Hazleman BL. Polymyalgia rheumatica. A
clinical study with particular reference to arterial dis-
ease. J Rheumatol. 1974;1:190.
Noshay WC, Roth RL. Giant cell (temporal) arteritis.
Henry Ford Hosp Med Bull. 1962;10:455.
Park JR, Jones JG, Hazleman BL. Relationship of the
erythrocyte sedimentation rate to acute phase proteins
in polymyalgia rheumatica and giant cell arteritis. Ann
Rheum Dis. 1981;40:493.
Paulley JW. Giant cell (temoral) arteritis-polymyalgia rheu-
matica: a critical review. Rec Prog Med. 1990;81:176.
Paresthesia
FIGURE 12-34 MENTAL PARESTHESIA
Prominent artery in giant cell (temporal) arteritis. Figure 12-35
Age: Adults
tortuous. The overlying skin is often ery- Sex: No predilection
thematous and hyperalgesic. Involvement is CLINICAL FEATURES
not confined to the temporal artery. Indeed,
many vessels supplying the head and neck Paresthesia, hypesthesia, or anesthesia
area may be involved. Cerebral infarction of the mental nerve distribution over the
is a complication. Notably, the erythrocyte lower lip usually represents a complica-
sedimentation rate and C-reactive protein tion of a mandibular fracture or third
are elevated. Ultrasonography is a first-line molar extraction with trauma of the infe-
diagnostic test and when negative, arterial rior alveolar nerve. Rarely, paresthesia may
wall biopsy is procured. occur in response to overfilling during root
canal therapy. Sensitivity to a light touch
DIFFERENTIAL DIAGNOSIS or a pinprick may be diminished or absent;
the ipsilateral mandibular teeth may fail to
The episodic or paroxysmal nature may sim- respond to vitalometer testing. When there
ulate a true neuralgia. When the patient’s is no history of trauma or tooth extraction,
age is considered in conjunction with arte- metastatic carcinoma to the jaw should be
rial tenderness and elevated sedimentation suspected. Periapical and panoramic radio-
rate, a preliminary diagnosis of temporal graphs disclose a poorly marginated or
arteritis can be made. Arterial biopsy is moth-eaten radiolucency of the mandibular
then indicated. body. Occasionally, a central or cranial base
lesion compresses the third division; when
TREATMENT this occurs, the motor trunk of the fifth
Prednisone, 20 to 30 mg daily, usually con- nerve is often compressed, resulting in soft
trols the pain associated with temporal palate paresis and/or masticatory muscle
arteritis. weakness.
DIFFERENTIAL DIAGNOSIS
Additional Reading With a documented history of trauma or
Ball EL, Walsh SR, Tang TY, Gohil R, Clarke JM. Role
third molar removal, the symptom usually
of ultrasonography in the diagnosis of temporal arteri- resolves in 6 weeks; however, some patients
tis. Br J Surg. 2010 Aug 26. [Epub ahead of print.] do not report resolution for 6 months. In
PMPH_Eversole_Chapter-12.indd 661 1/20/2011 3:21:40 PM
662 Chapter 12
FIGURE 12-35
Mental paresthesia occurs
following physical trauma
to the inferior alveolar
nerve or to malignant neo-
plasms, particularly meta-
static tumors that encroach
upon the nerve.
some instances of trauma, the paresthesia the great auricular and inferior alveolar nerve to
never resolves, but this is rare. When there restore lower lip sensation. J Oral Maxillofac Surg.
1987;45:621.
is no history of nerve injury, a panoramic Moorman WC, Shafer WG. Metastatic carcinoma of the
radiograph should be ordered; biopsy of mandible. J Oral Maxillofac Surg. 1954;12:205.
any suspicious radiolucent or mixed radio- Penarrocha Diago M, Bagán Sebastián JV, Alfaro Giner
lucent and radiopaque regions should be A, Escrig Orenga V. Mental nerve neuropathy in sys-
temic cancer. Report of three cases. Oral Surg Oral
performed. In the absence of jaw disease, Med Oral Pathol. 1990;69:48.
CT scans should be used to evaluate for von Ohle C, Elayouti A. Neurosensory impairment of
CNS or cranial base lesions. the mental nerve as a sequel of periapical periodon-
titis: case report and review. Oral Surg Oral Med
TREATMENT Oral Pathol Oral Radiol Endod. 2010;110(4):e84-
e89.
There is no treatment for posttraumatic
mental paresthesia; spontaneous resolu-
tion evolves as axis cylinders regenerate. INFRAORBITAL PARESTHESIA
When the sensory deficit persists beyond 6
Figure 12-36
months, a microsurgical nerve graft proce-
dure may be successful. Metastatic tumor Age: Adults
should be managed by an oncologist. Sex: No predilection
CLINICAL FEATURES
Additional Reading Included under this title of infraorbital
paresthesia are other forms of sensory
Goldstein NP, Gibilisco JA, Rushton JG. Trigeminal neu-
neurologic deficit, including hypesthesia
ropathy and neuritis: a study of etiology with emphasis
on dental causes. JAMA. 1963;183:458. and anesthesia of the infraorbital nerve
LaBanc JP, Epker BN, Jones DL, Milam S. Nerve shar- distribution. In instances of complete
ing by an interpositional sural nerve graft between anesthesia, light-touch and pinprick test-
PMPH_Eversole_Chapter-12.indd 662 1/20/2011 3:21:40 PM
Facial Pain and Neuromuscular Disorders 663
FIGURE 12-36
Infraorbital paresthesia
may be secondary to V-2
injury or neoplasia along
the course of the nerve.
ing over the infraorbital skin and usually The sensory deficit is usually temporary
the ipsilateral palate are not felt by the with spontaneous resolution. Some of
patient. In hypesthesia, either a pinprick, these instances may represent a viral neu-
a light touch, or both may be affected to ritis or a psychologic conversion symptom.
some degree. In other words, patients A few patients with idiopathic atypical
may detect these forms of stimulation to facial pain may also experience an attend-
a lesser degree than they would on unaf- ing paresthesia. In all instances of infraor-
fected cutaneous regions. Patients with bital paresthesia, hyperthesia, or anesthe-
paresthesias may show a normal response sia, the remaining cranial nerves should
to pinprick and light-touch tests, yet sub- be evaluated for accompanying motor defi-
jectively describe numbness and tingling cits; antral tomograms as well as CT scans
of the affected skin. In general, loss of should be used to identify a tumor.
sensation to both a pinprick and a light
touch indicates a peripheral nerve lesion, DIFFERENTIAL DIAGNOSIS
whereas differential loss suggests a cen-
As mentioned previously, loss of both pin-
tral lesion. Antral carcinoma and cranial
prick and light-touch sensation necessitates
base tumors are the more common causes
a search for a central lesion. The presence of
of infraorbital sensory deficits when the
ophthalmoplegia or other motor paresis is
second division fibers are involved after
another sign that suggests a CNS or cranial
exit from the skull. Cerebellopontine angle
base tumor. Maxillary or palatal expansion
tumors with involvement of the gasserian
implicates an antral neoplasm.
ganglion are the most prevalent central
lesions accounting for these symptoms.
TREATMENT
Other causes of sensory neuropathy in
this area are multiple sclerosis, Bell’s palsy, When the cause has been determined and
trauma, vertebrobasilar vascular disease, a biopsy diagnosis has been procured,
and connective tissue immunopathic dis- treatment must be planned according to
orders. Trigeminal (sensory) neuropathy is this diagnosis. If an antral source has been
a less frequently encountered disorder in ruled out, patients should be referred to a
which no organic source can be detected. neurologist.
PMPH_Eversole_Chapter-12.indd 663 1/20/2011 3:21:49 PM
664 Chapter 12
variety of other diseases, lesions, and trauma
Additional Reading of the temporal region, brain stem, facial
Hagen NA, Stevens JC, Michet CJ, Jr. Trigeminal sen- canal, middle ear, and infratemporal fossa
sory neuropathy associated with connective tissue dis- may produce partial, sequential, or com-
eases. Neurology. 1990;40:891. plete seventh nerve palsy. The cortical tracts
Horowitz SH. Isolated facial numbness. Clinical sig- communicating with the motor nucleus
nificance and relation to trigeminal neuropathy. Ann
Intern Med. 1974;80:49. ambiguus of the facial nerve cross over to
Sharma N, De M, Pracy P. Recurrent facial paraes- innervate the lower face musculature, while
thesia secondary to maxillary antral cyst and dehis- the upper face fibers are ipsilateral proximal
cent infraorbital canal: case report. J Laryngol Otol. to the nucleus. A cortical lesion, therefore,
2007;121(6):e6.
Tait B, Ashworth B. Trigeminal neuropathy in connec-
causes contralateral lower face palsy; a lesion
tive tissue disease. Ann Rheum Dis. 1970;29:339. of the brain stem, main trunk, or peripheral
Thrush DC, Small M. How benign a symptom is facial fibers results in a total hemifacial paralysis.
numbness? Lancet. 1970;2:851. The nervus intermedius carries parasym-
pathetic secretory fibers to the lacrimal and
Localized Motor Deficits salivary glands. Lesions of the main trunk
and facial canal are, therefore, frequently
accompanied by ipsilateral xerophthalmia;
FACIAL PARALYSIS
xerostomia may not be evident because of
Figure 12-37 normal contralateral function. Facial canal
Age: Varies according to etiology
and middle ear neoplasms are usually asso-
Sex: Varies according to etiology ciated with sensorineural hearing loss when
seventh nerve palsy is a feature. Tumors of
CLINICAL FEATURES the cranial base, parapharyngeal space, and
Seventh nerve paralysis is usually self-lim- infratemporal fossa, particularly malig-
ited, and normal function returns within nant parotid tumors, often cause seventh
2 months. Paralysis of this nature is referred nerve palsy and neuropathy of other cranial
to as Bell’s palsy. Notably, the entire distri- nerves. CT scans disclose osseous destruc-
bution of the seventh nerve is involved from tive changes in the temporal bone or a soft
the onset; therefore, the patient is unable to tissue mass, depending on the location of
raise the eyebrow, close the eye, or smile on the lesion. Lastly, neurologic involvement in
the affected side (i.e., complete hemifacial Lyme disease (Bannwarth’s syndrome) can
paralysis). Although it has been suggested result in either unilateral or bilateral facial
that Bell’s palsy is a herpesvirus neuritis, a paralysis.
FIGURE 12-37
Complete facial nerve
paralysis is seen in Bell’s
palsy and parotid adeno-
carcinomas that invade
nerve VII.
PMPH_Eversole_Chapter-12.indd 664 1/20/2011 3:21:54 PM
Facial Pain and Neuromuscular Disorders 665
DIFFERENTIAL DIAGNOSIS Greene RM, Rogers RS, III. Melkersson-Rosenthal syn-
drome: a review of 36 patients. J Am Acad Dermatol.
Evaluation of a patient with seventh nerve 1989;21:1263.
paralysis must include the following chief Neely JG. Neoplastic involvement of the facial nerve.
factors: precise muscle groups involved, Otolaryngol Clin North Am. 1974;7:385.
Sathirapanya P, Sathirapanya C. Clinical prognostic
temporal progression of muscle group pare-
factors for treatment outcome in Bell’s palsy: a pro-
sis, middle ear disease, vestibular function, spective study. J Med Assoc Thai. 2008;91(8):1182-
hearing loss, tinnitus, and presence of other 1188.
cranial nerve deficits. It should also be noted
that seventh nerve palsy accompanies cheil-
itis granulomatosa in the Melkerson-Rosen- HORNER’S SYNDROME
thal syndrome and, recently, idiopathic Figure 12-38
paresis has been observed among human
immunodeficiency virus (HIV)–positive Age: Elderly adults
patients. Special radiographic and neuro- Sex: Male predilection
logic procedures are required to secure a CLINICAL FEATURES
definitive diagnosis. Referral to an otolar- Horner’s syndrome is a neurological facial
yngologist or neurologist is recommended. sign indicative of a lesion compressing the
stellate ganglion, usually bronchogenic
TREATMENT
carcinoma arising adjacent to the apex of
Systemic steroids or corticotropin injections the lung. The sympathetic fibers emerg-
have been successful in treating Bell’s palsy. ing from the ganglion normally pass into
Even in the absence of treatment, the paral- the head and neck regions and innervate
ysis generally disappears within 2 months. the pupil dilator, smooth muscle elevator
Lesions arising along the intracranial, tem- of the upper eyelid, and periorbital sweat
poral bone, and peripheral distributions of glands. Compression of the ganglion leads
the seventh nerve are treated in accordance to miosis or contraction of the pupil, pto-
with the ultimate and definitive diagnosis. sis of the upper eyelid, and anhydrosis of
the periorbital and facial skin. In addition
to lung cancer, other neoplasms, infections,
Additional Reading or aneurysms adjacent to the cervical spine
Bateman DE, Lawton NF, White JE, Greenwood RJ,
may encroach upon the ganglion or sym-
Wright DJ. The neurological complications of Borrelia pathetic fibers arising therefrom. Lyme
burgdorferi in the New Forest area of New Hampshire. disease, and rarely CNS vascular occlusive
J Neurol Neurosurg Psychiatry. 1988;51:699. disease or aneurysms, can result in sympa-
Boone PC. Bell’s palsy. Acta Neurochir (Wien).
thetic paresis.
1959;7:16.
FIGURE 12-38
Ptosis and miosis in Horner’s syndrome
associated with carcinoma of lung apex.
PMPH_Eversole_Chapter-12.indd 665 1/20/2011 3:21:59 PM
666 Chapter 12
DIFFERENTIAL DIAGNOSIS the nuclei of III (ipsilateral) and VI (con-
The etiology of Horner’s syndrome is vari- tralateral). Internuclear ophthalmoplegia is
able and represents a medical problem. characterized by inability to move one eye
Referral to an internist or neurologist is medially while the opposite eye is directed
recommended. laterally, despite the fact that the patient is
able to converge both eyes. This apparent
TREATMENT paradox is reconciled when one realizes
that the pathway for convergence is dif-
The cause must be eliminated. Horner’s syn- ferent from the pathway for lateral conju-
drome may herald the presence of a serious gate gaze. Multiple sclerosis is usually the
illness such as cancer or an aneurysm. underlying disease involving internuclear
ophthalmoplegia. Lesions involving each
Additional Reading specific nucleus of the three nerves control-
ling eye movement manifest specific signs.
Clauser TA, Brennan PJ, Galetta SL. Reversible Bilateral involvement of the abducens
Horner’s syndrome and Lyme disease. J Clin Neuro- nuclei causes convergent gaze owing to
Ophthalmol. 1989;9:225.
Giles CL, Henderson JW. Horner’s syndrome. An analy-
defective motor supply to the lateral rec-
sis of 219 cases. Am J Ophthalmol. 1958;46:289. tus. Divergent gaze is the consequence of
Jaffee NS. Localization of lesions causing Horner’s syn- a bilateral lesion of the oculomotor nerve.
drome. Arch Ophthalmol. 1940;44:5. Compression of the peripheral nerves is
Kahraman A, Yildirim I, Kiliç MA, Okur E, Demirpolat
G. Horner’s syndrome from giant schwannoma of
caused by hemorrhage or tumor. Alterna-
the cervical sympathetic chain: case report. B-ENT. tively, entrapment of ocular muscles may
2009;5(2):111-114. occur in orbital blow-out fractures or in
Safran MJ, Greenwald MJ, Rice HC, Polin KS. Cervical localized orbital lesions. A lesion located
spine dislocation presenting as an isolated Horner’s
in the middle fossa/cavernous sinus
syndrome. Arch Ophthalmol. 1990;108:327.
region may compress one, two, or all three
motor nerves to the eye. Compression of
OPHTHALMOPLEGIA the oculomotor (CN-III) causes unilateral
Figure 12-39 gaze with pupillary dilation. The cold
caloric test confirms the finding. Involve-
Age: Varies according to disease ment of the trochlear nerve (CN-IV) causes
Sex: Varies according to disease inability to move the affected eye inferolat-
CLINICAL FEATURES erally. Unilateral paralysis of the abducens
(CN-VI) is characterized by medial gaze
Eye movement paralysis has many com- of the affected eye. Progressive supranuclear
plex origins. Lesions may arise in the cere- palsy is a primary neurologic disorder that
bral motor cortex, the nuclei of nerves III, causes paralysis of the extraocular mus-
IV, and VI, or the peripheral nerves may cles and may be due to a perturbation in
be compressed after they have exited from mitochondria.
the brain stem. A lesion of the motor cor-
tex causes a defect in contralateral con-
jugate gaze. The consequences of a left DIFFERENTIAL DIAGNOSIS
cerebral lesion are inability of both eyes to Because of the aforementioned clinical
engage in right-sided gaze and a tendency signs gleaned from cranial nerve examina-
for bilateral left deviation. In other words, tion of nerves III, IV, and VI, observation
the patient “looks toward the lesion.” The of eye position at rest, comparison of pupil
mechanism involves impairment of neural size, and use of the cold caloric test, the
pathway conduction prior to synapse with examiner will have a concept of where the
PMPH_Eversole_Chapter-12.indd 666 1/20/2011 3:22:00 PM
Facial Pain and Neuromuscular Disorders 667
A B C D
FIGURE 12-39
Ophthalmoplegia. A: Left cerebral lesion with conjugate gaze. B: Medial longitudinal fasciculus lesion
with inability to look medially when directed to look left or right, convergence intact. C: Bilateral
nuclear lesions of abducens (above) and oculomotor (below). D: Left unilateral nuclear or peripheral
nerve paresis of oculomotor (above) and abducens (below).
lesion lies. Because the etiology of ophthal- HYPOGLOSSAL PARALYSIS
moplegias is so protean, a definitive diag- Figure 12-40
nosis requires a variety of other clinical,
radiologic, and laboratory tests. A detailed Age: Adults
differential diagnosis of ophthalmoplegia is Sex: No predilection
beyond the scope of this book. CLINICAL FEATURES
The hypoglossal or twelfth nerve supplies
TREATMENT
motor fibers to the tongue and exits the
Patients with eye muscle paresis should be medulla inferior to the olive. Unilateral
examined by an ophthalmologist or a neu- injury or a lesion of the nucleus or nerve
rologist when it has been determined that
the etiology is not a maxillary or orbital
fracture.
Additional Reading
Bronstein AM, Rudge P, Gresty MA, Du Boulay G,
Morris J. Abnormalities of horizontal gaze. Clinical,
oculographic and magnetic resonance imaging find-
ings. J Neurol Neurosurg Psychiatry. 1990;53:200,
199.
Cheek CW, Simon KA, Gay AJ. Acquired cranial nerve
lesions affecting the ocular system. Am J Ophthalmol.
1965;59:13.
Goldberg S. Chap. 5. Clinical neuroanatomy made
ridiculously simple. Miami, FL: MedMaster, Inc;
1979.
Merritt HH. Textbook of Neurology. 6th ed. Philadelphia,
PA: Lea & Febiger; 1979:378.
Stamelou M, de Silva R, Arias-Carrión O, et al. Rational FIGURE 12-40
therapeutic approaches to progressive supranuclear Twelfth nerve paralysis. Tongue deviate toward the
palsy. Brain. 2010;133(Pt 6):1578-1590. affected side.
PMPH_Eversole_Chapter-12.indd 667 1/20/2011 3:22:01 PM
668 Chapter 12
causes the affected side of the tongue to Hemmings KW. Isolated hypoglossal nerve palsy as a
undergo atrophy, and on protrusion, the presenting feature of prostatic carcinoma—a case
report. Br J Oral Maxillofac Surg. 1990;28:125.
tongue deviates toward the affected side. Lieschke GJ, Davis S, Tress BM, Ebeling P. Spontaneous
Attempted movements of the protruded internal carotid artery dissection presenting as hypo-
tongue to the normal side are absent or weak. glossal nerve palsy. Stroke. 1988;19:1151.
At rest, lying in the floor of the mouth, the Merritt HH. A Textbook of Neurology. 6th ed.
Philadelphia, PA: Lea & Febiger; 1979:394.
tongue deviates slightly toward the healthy Mendes-Araújo L, Rangel C, Domingues RC, Gasparetto
side; retrusion of the tongue on the affected EL. Case report. Atlantoaxial synovial cyst causing
side is defective. A lesion may be located isolated unilateral hypoglossal nerve paralysis. Br J
within the medulla or along the peripheral Radiol. 2010;83(986):e35-e38.
course of the nerve. Basilar artery occlusion
causes a lesion of the medulla with ipsilat- SOFT PALATE PARALYSIS
eral tongue paralysis and contralateral arm
Figure 12-41
and leg paralysis. Neoplasms in the vicin-
ity of the occipital condyle frequently com- Age: Varies depending on disease
press the hypoglossal nerve with paralysis, Sex: No predilection
dysarthria, and severe pain that is wors-
CLINICAL FEATURES
ened when the neck is flexed. Neoplasms
in the lateral neck along the course of the The soft palate muscles include the tensor
nerve may also cause unilateral paresis or veli palatini, supplied by the motor root of
palsy. Bilateral twelfth nerve palsy is rare. the fifth nerve, and the levator veli pala-
Fibrillation of the tongue is seen in syrin- tini, palatoglossus, and palatopharynge-
gobulbia, amyotrophic lateral sclerosis, and ous, all supplied by branches of the tenth
chronic alcoholism. nerve from the nucleus ambiguus. Brain
stem lesions involving the nucleus or cra-
DIFFERENTIAL DIAGNOSIS nial base and parapharyngeal space lesions
Because unilateral hypoglossal paralysis may cause paralysis with resultant droop-
may be either central or peripheral in ori- ing of the palate and loss of the palatal
gin, complete neurologic examination is
required to explore other deficits indicative
of a lesion within the medulla. CT scans
should be obtained to evaluate the pos-
sibility of a cranial base primary or meta-
static tumor. Palpation of the upper lateral
neck for indurated swellings should also be
performed.
TREATMENT
Referral to a neurologist is recommended.
Treatment is determined when the source
of the lesion is located and a definitive diag-
nosis is rendered.
Additional Reading
Greenburg HS, Deck MD, Vikram B, Chu FC, Posner FIGURE 12-41
JB. Metastasis to the base of the skull: clinical findings Soft palate paralysis. Uvula deviates toward normal
in 43 patients. Neurology. 1981;31:530. side.
PMPH_Eversole_Chapter-12.indd 668 1/20/2011 3:22:05 PM
Facial Pain and Neuromuscular Disorders 669
reflex. Bilateral paralysis results in velopha- Lee MC, Resch JA. Practical clinical neurology for the
ryngeal insufficiency, thus causing nasal otolaryngologist. In: Paparella MM, Shumrick DA,
eds. Otolaryngology. 2nd ed. Philadelphia, PA: W. B.
speech and difficulty with velar sounds Saunders; 1980:871.
such as “N” and “NG.” Bilateral paralysis is
associated with poliomyelitis, diphtheritic
polyneuropathy, myasthenia gravis, and Limited and Deviant
brain stem infarction. Unilateral paralysis Mandibular Opening
is characterized by inability of the affected
side to elevate when the patient says “ah”; MUSCLE SPLINTING
the uvula deviates toward the normal side. Figure 12-42
An ipsilateral nuclear lesion, cranial base
neoplasia, nasopharyngeal carcinoma, Age: No predilection
foraminal narrowing, or varicella zoster Sex: No predilection
may be causative. When pharyngeal con- CLINICAL FEATURES
strictor paralysis and sternomastoid weak-
ness is observed, the clinical findings are When patients feel pain, they protect them-
termed Vernet syndrome, and when nerves selves by limiting motion of the associated
IV, X, and XI are involved, the term Jugular joint. For instance, wide opening may be
syndrome is used. painful; thus, the patient may consciously
maintain closure or limited opening. The
splinting may be unilateral, causing devia-
DIFFERENTIAL DIAGNOSIS tion of the mandible on opening. A variety
As previously mentioned, a variety of neu- of organic lesions may initiate this protective
rologic diseases can cause bilateral palatal phenomenon; they include trauma, fracture,
paralysis. Unilateral paralysis warrants a pericoronitis, odontogenic infection, salivary
thorough nasopharyngeal examination, gland inflammation, primary TMJ articular
which should include CT scans of the cra- disease, and avoidance of a recently placed
nial base to detect the presence of a tumor. high dental restoration. Prolonged splinting
may actually lead to myospasm, although
TREATMENT
Because a variety of neurologic and neo-
plastic disorders can cause palatal paralysis,
referral to a neurologist is recommended.
Additional Reading
Cotton R, Nuwayhid NS. The surgery of speech. In:
Paparella MM, Shumrick D. Otolaryngology. 2nd ed.
Philadelphia, PA: W. B. Saunders; 1980:2177.
Hayashi T, Murayama S, Sakurai M, Kanazawa I. Jugular
foramen syndrome caused by varicella zoster virus
infection in a patient with ipsilateral hypoplasia of the
jugular foramen. J Neurol Sci. 20001;172(1):70-72.
Kawabe K, Sekine T, Murata K, et al. A case of Vernet
syndrome with varicella zoster virus infection. J Neurol
Sci. 200815;270(1-2):209-210.
Kikuchi T, Kusakari J, Kawase T, Takasaka T.
Electrogustometry of the soft palate as a topographic
diagnostic method for facial paralysis. Acta Otolaryngol FIGURE 12-42
Suppl. 1988;458:134. Deviant jaw opening secondary to muscle splinting.
PMPH_Eversole_Chapter-12.indd 669 1/20/2011 3:22:06 PM
670 Chapter 12
this is rare. Amelioration of the problem or the patient complains of pain; however,
local anesthesia to the tissues suspected in its most patients do not experience pain unless
etiology permit the patient to fully depress they forcefully attempt full depression of
the mandible. Dystrophic calcification or the mandible. The closed-lock phenomenon
myositis ossificans of the pterygoid muscles appears 1 to 6 days after a dental procedure
also decreases ability to open. that necessitated inferior nerve block anes-
thesia. Most patients are unable to open
DIFFERENTIAL DIAGNOSIS beyond 20 mm. Although the pathogenesis
Limited opening because of muscle splint- is unknown, the condition probably occurs
ing may leave the erroneous impression because a needle has pierced a vessel and
that the problem is a primary muscle dis- caused hematoma followed by organization
order (i.e., myogenic facial pain). Physical and scar formation. Occasionally, trismus is
evaluation of teeth, occlusion, and perio- encountered in patients with acute pericoro-
dontium and perioral tissues along with nitis or alveolitis sicca. Inflammatory exten-
radiographs disclose the presence of dis- sion into the pterygomandibular space may
ease. The inflamed or traumatized tissue develop; but in most instances, pain may
can be anesthetized so that amelioration of induce muscle splinting or guarding that
the inability to open can be evaluated. prevents a full range of opening.
TREATMENT DIFFERENTIAL DIAGNOSIS
Resolution of the cause eliminates the effect. Although limited opening may be seen in
a variety of disorders, a closed-lock situa-
tion related to injection can be readily diag-
Additional Reading nosed on the basis of history. Inflammation
Bell WE. Chap. 12. Management of masticatory pain. In: of a pericoronal operculum or extraction
Alling CC, III, Mahan PE, eds. Facial Pain. 2nd ed. site accounting for trismus is also easily
Philadelphia, PA: Lea & Febiger; 1977. recognized on the basis of examination and
Bell WE. Orofacial Pains. Differential Diagnosis. 2nd ed. history.
Chicago, IL: Year Book; 1979:62.
Frost HM. Chap. 9. Musculoskeletal pain. In: Alling CC,
III, Mahan, PE, eds. Facial Pain. 2nd ed. Philadelphia, TREATMENT
PA: Lea & Febiger; 1977.
Molina OF, dos Santos Junior, Nelson SJ, Nowlin T. A
Postinjection trismus usually resolves after
clinical study of specific signs and symptoms of CMD a 3-week course of physiotherapy that
in bruxers classified by the degree of severity. Cranio. includes ultrasound to masticatory mus-
1999;17(4):268-279. cles, hot packs, and jaw opening exercises
Verma A, Tandon PN, Maheshwari MC. Trismus caused
by paradoxical activity of jaw-closing muscles in brain
3 times a week. Forced opening under gen-
stem tuberculoma. Oral Surg Oral Med Oral Pathol. eral anesthesia may be required for patients
1988;65:675. who do not respond to the aforementioned
conservative regimen. Rarely, surgical inter-
vention is required to sever a scar band that
POSTINJECTION/
may form in the pterygoid space. Pericoro-
POSTINFECTION TRISMUS nitis should be treated with hydrogen per-
Age: Middle-aged adults oxide irrigation and antibiotics when fever
Sex: No predilection and malaise are present. With resolution of
symptoms, the hyperplastic tissue should
CLINICAL FEATURES
be excised with extraction of the associated
Limitation in jaw opening may evolve from third molar. A full range of opening should
inferior alveolar nerve block. Occasionally, return within a few days.
PMPH_Eversole_Chapter-12.indd 670 1/20/2011 3:22:07 PM
Facial Pain and Neuromuscular Disorders 671
DIFFERENTIAL DIAGNOSIS
Additional Reading Because many organic disorders result in
Brooke RI. Postinjection trismus due to formation limited opening or trismus, a thorough
of fibrous band. Oral Surg Oral Med Oral Pathol. work-up for joint, muscle, and infectious dis-
1979;47:424.
ease must be pursued. Differentiation from
Brown AE. Persistent limitation of opening follow-
ing inferior alveolar nerve block injection. Br Dent J. a true closed-lock type III internal derange-
1976;141:186. ment is difficult on clinical grounds alone.
Campbell J. Trismus following inferior dental block Psychiatric consultation and MMPI testing
anaesthesia: an analysis of a personal experience. Dent should be included in the data base collec-
Rec. 1954;74:180.
tion. Restoration to normal function after
intravenous diazepam sedation with manip-
CONVERSION TRISMUS ulation of the mandible aids in establishing
the diagnosis.
Age: Young and middle-aged adults
Sex: Female predilection TREATMENT
CLINICAL FEATURES The immediate problem is easily amelio-
Conversion reactions are encountered rated by manipulation of the jaw under
among patients with hysterical or histri- general anesthesia or intravenous seda-
onic personality. The etiology is appar- tion. Long-term management rests with
ently related to an underlying emotional psychotherapy.
crisis with which the subject cannot cope,
whereby the emotional conflict is converted
to a physical sign or symptom. Motor defi- Additional Reading
cits (paralysis), sensory deficits (paresthesia
Marbach JJ. Hysterical trismus: a study of six cases. NY
or numbness), and visual loss represent the State Dent J. 1966;32:413.
more common hysterical conversion reac- Salmon TN, Tracy NH, Jr, Hiatt WR. Hysterical tris-
tions; notably, the deficits usually do not fol- mus (conversion reaction). Oral Surg Oral Med Oral
low neuroanatomic pathway distributions. Pathol. 1972;34:187.
Conversion or hysterical trismus is rare and
is characterized by inability to open the
ANKYLOSIS
mouth in the absence of organic disease in
the TMJ. Prolonged closure may, however, Figure 12-43
lead to myospasm with masticatory muscle Age: Children or adults
weakness. The personality profile is impor- Sex: No predilection
tant in the diagnosis, and psychometric
CLINICAL FEATURES
testing with the MMPI shows elevation of
the hysteria scale. Patients with histrionic Unilateral or bilateral ankylosis of the TMJ
or hysterical personalities exaggerate their is the consequence of trauma, destructive
symptoms and make multiple unfounded infectious arthritis, or rheumatoid arthritis.
organ-system somatic complaints, yet they The ankylosis may be fibrous or bony. When
maintain an indifferent attitude about their a joint lesion arises during childhood, man-
problems (belle indifference). In addition, dibular retrognathism occurs because of the
patients tend to be theatrical with overuse arrest of condylar growth on the affected
of cosmetics and adornment. The trismus side(s). The patient may be able to open the
can be reversed with restoration of normal jaw only a few millimeters or it may be com-
opening while the patient is under general pletely closed. Severe limitation of opening
anesthesia or heavy sedation. is seen even in unilateral ankylosis, and
PMPH_Eversole_Chapter-12.indd 671 1/20/2011 3:22:07 PM
672 Chapter 12
FIGURE 12-43
A: Retrognathia in bilat-
eral TMJ ankylosis. B: Skull
specimen in TMJ ankylosis.
A B
deviation of the mandible to the affected Topazian RG. Etiology of ankylosis of the temporoman-
side is generally not detected because the dibular joint: analysis of 44 cases. J Oral Maxillofac
Surg. 1964;22:227.
ankylosed joint often prevents translation Young AH. A follow-up of 12 cases of ankylosis of the
of the unaffected condyle. TMJ tomograms mandibular joint treated by condylectomy. Br J Plast
disclose an absent or anomalous-appearing Surg. 1963;16:75.
condyle without joint space radiolucency.
DIFFERENTIAL DIAGNOSIS HECHT-BEALS-WILSON
In most of the other disorders showing lim- SYNDROME
itation of opening, the restriction is incom-
Age: Childhood onset
plete. A history of trauma, acute arthritis,
Sex: No predilection
or juvenile rheumatoid arthritis and man-
dibular retrognathia, when considered in CLINICAL FEATURES
conjunction with the radiographic findings, Inherited as an autosomal dominant trait,
allows for establishment of the diagnosis. the Hecht-Beals-Wilson syndrome is char-
acterized by limited mandibular opening,
TREATMENT
campylodactyly resulting from foreshort-
Ankylosis may be corrected by surgical ened flexor tendons of the fingers and wrists,
resection, reconstruction, and/or placement shortened leg and hamstring muscles with
of a joint prosthesis. consequently short stature, and, occasionally,
foot deformities (club foot). The limitation in
Additional Reading opening is the result of bilateral abnormal lig-
aments located within the masseteric region.
Blackwood HJJ. Intra-articular fibrous ankylosis of the This fibrotic band can usually be easily pal-
temporomandibular joint. Oral Surg Oral Med Oral pated bidigitally in the buccal mucosa just
Pathol. 1957;10:634. anterior and confluent with the masseter.
Kaban LB, Perrott DH, Fisher K. A protocol for man-
agement of temporomandibular joint ankylosis. J Oral
Maxillofac Surg. 1990;48:1145. DIFFERENTIAL DIAGNOSIS
Loveless TP, Bjornland T, Dodson TB, Keith DA.
Efficacy of temporomandibular joint ankylosis surgical
This syndrome exhibits classic features
treatment. J Oral Maxillofac Surg. 2010;68(6):1276- allowing for a definitive diagnosis. Lim-
1282. ited opening in conjunction with buccal
PMPH_Eversole_Chapter-12.indd 672 1/20/2011 3:22:07 PM
Facial Pain and Neuromuscular Disorders 673
mucosal fibrous bands and flexion of the DIFFERENTIAL DIAGNOSIS
finger when the wrist is dorsiflexed con- Restricted opening without pain or devia-
firms the diagnosis. Other family members tion in a young male should arouse suspi-
may be affected. cion of coronoid hyperplasia. Although the
other entities included here must be consid-
TREATMENT ered in the differential diagnosis, they are
The masseteric fibrous bands may be sur- more common in older patients or exhibit
gically severed. Some surgeons advocate restriction of opening with deviation or
coronoidectomy to free any inhibition of pain. Radiographs confirm the diagnosis of
opening as a consequence of temporalis condylar hyperplasia.
fibrosis, which may be present.
TREATMENT
Additional Reading When patients are not bothered by their
inability to open and they are able to func-
Carlos R, Contreras E, Cabrera J. Trismus- tion adequately, no treatment is necessary.
pseudocamptodactyly syndrome (Hecht-Beals’ syn-
drome): case report and literature review. Oral Dis.
With severe limitation, bilateral coronoidec-
2005;11(3):186-189. tomy is the treatment of choice.
deJong JG. A family showing reduced ability to open
the mouth and limitation of some movements of the
extremities. Humangenetik. 1971;13:210.
Hecht F, Beals RK. Inability to open the mouth fully: Additional Reading
an autosomal dominant phenotype with faculta-
tive campylodactyly and short stature. Birth Defects. Giacomuzzi D. Bilateral enlargement of the mandibular
1969;5:96. coronoid processes: review of the literature and report
Mercuri LG. The Hecht, Beals, and Wilson syndrome: of a case. J Oral Maxillofac Surg. 1986;44:728.
report of case. J Oral Maxillofac Surg. 1981;39:53. Hall RE, Orbach S, Landesberg R. Bilateral hyperplasia
of the mandibular coronoid processes. A report of two
cases. Oral Surg Oral Med Oral Pathol. 1989;67:141.
CORONOID HYPERPLASIA Hecker R, Corwin JO. Bilateral coronoid hyperplasia:
Review of the literature and report of case. J Oral
Maxillofac Surg. 1980;38:606.
Age: Children
Rowe NL. Bilateral developmental hyperplasia of the
Sex: Males mandibular coronoid process. A report of two cases.
CLINICAL FEATURES Br J Oral Maxillofac Surg. 1963;1:90.
Yura S, Ohga N, Ooi K, Izumiyama Y. Mandibular coro-
A rare developmental disorder, coronoid noid hyperplasia: a case report. Cranio. 2009;27(4):
hyperplasia is bilateral and causes painless 275-279.
restriction of mandibular opening. Most
patients are unable to open beyond 20 mm. CONDYLAR HYPERPLASIA
The enlarged coronoids impinge upon the
Figure 12-44
posterior aspect of the zygoma, thereby
restricting translation of the condyles sec- Age: Children and young adults
ondarily. There is no deviation on opening Sex: Female predilection
as both coronoids are involved. Although
CLINICAL FEATURES
some cases are probably sporadic, others
have been reported among siblings. The Unilateral hyperplasia of the mandibu-
diagnosis must be confirmed radiographi- lar condyle is of unknown etiology yet is
cally. A lateral skull, high panoramic, or lat- considered to be a developmental defect.
eral tomograms disclose enlarged coronoid Clinically, facial asymmetry is seen and the
processes extending high above the zygo- patient exhibits either an open bite on the
matic arch. affected side or a cross bite with open bite.
PMPH_Eversole_Chapter-12.indd 673 1/20/2011 3:22:11 PM
674 Chapter 12
A B C
FIGURE 12-44
Condylar hyperplasia. A: Asymmetry with unilateral open bite on affected side. B: Hyperplastic condyle. C:
Normal condyle for comparison. (Courtesy of Dr. John Ditmer.)
The face is elongated on the affected side,
and restricted opening may or may not Additional Reading
be observed. Similarly, deviation toward Bruce RA, Hayward JR. Condylar hyperplasia and man-
the affected side is a variable finding. TMJ dibular asymmetry: a review. J Oral Maxillofac Surg.
tomograms disclose a significantly thick- 1968;26:281.
ened condyle, which may represent a two- Gruca A, Meisels E. Asymmetry of mandible from unilat-
eral hypertrophy. Ann Surg. 1926;83:755.
or threefold increase in dimension when Iannetti G, Cascone P, Belli E, Cordaro L. Condylar
compared radiographically with the normal hyperplasia: cephalometric study, treatment planning,
condyle. and surgical correction (our experience). Oral Surg
Oral Med Oral Pathol. 1989;68:673.
Jouck LM. Condylar hyperplasia. A case for early treat-
DIFFERENTIAL DIAGNOSIS
ment. Int J Oral Maxillofac Surg. 1981;10:154.
Condylar hyperplasia is easily differenti- Kawamoto HK, Kim SS, Jarrahy R, Bradley JP.
ated from the other disorders included Differential diagnosis of the idiopathic laterally devi-
ated mandible. Plast Reconstr Surg. 2009;124(5):
here with restricted or deviant mandib- 1599-1609.
ular movement. The facial asymmetry,
open bite or cross bite, and radiographic
evidence of an enlarged condyle confirm TMJ REGION NEOPLASMS
the diagnosis of condylar hyperplasia. Figure 12-45
Condylar hypoplasia is rare yet must be
considered in the differential diagnosis Age: Variable
because the normal side may be mistaken Sex: Variable
for hyperplasia. CLINICAL FEATURES
Most so-called neoplasms of the TMJ
TREATMENT region are, in actuality, represented by
Surgical correction with subcondylar hyperplastic or reactive processes includ-
osteotomy is the treatment of choice. The ing synovial chondromatosis and villonod-
case should be planned with models and ular tenosynovitis. These reactive lesions
radiographs because bilateral proce- involve the joint space or synovium and
dures may be required to obtain optimal rarely distort or erode the condylar bone.
results. Orthodontic consultation should be Nevertheless, true benign and malignant
obtained; most patients require combined neoplasms, although extremely rare, do
orthodontic and surgical therapy. arise in the region of the TMJ. The most
PMPH_Eversole_Chapter-12.indd 674 1/20/2011 3:22:11 PM
Facial Pain and Neuromuscular Disorders 675
A B C
FIGURE 12-45
TMJ neoplasms. A and B: Osteochondroma of coronoid fused to pterygoid plate. C: Osteoma overlying
condyle.
common benign tumor is osteochondroma. DIFFERENTIAL DIAGNOSIS
The lesion arises from the cortex as an exo- Submental vertex, TMJ tomograms, CT
stotic projection with a narrow neck. Actu- scans, and/or MRI should be obtained
ally, most osteochondromas arise from the when patients present with unilateral
coronoid process. Limitation of opening restricted opening and jaw deviation. Soft
with deviation toward the affected side is tissue opacification; irregular foci of resorp-
a common sign; pain usually is not a com- tion, particularly below the articular cortex;
plaint, although it certainly can be. Radio- and soft tissue swelling over the joint or in
graphs disclose a radiopaque nodular pro- the parapharyngeal region should arouse
jection emanating from either the condyle suspicion of neoplasia, and a biopsy should
or coronoid; the projection is usually ori- be obtained.
ented medially or superiorly. Other benign
neoplasms including osteomas, heman- TREATMENT
giomas, and nerve sheath neoplasms may
arise within articular tissues and cause Treatment is usually surgical, and the extent
restricted opening. Sarcomas are extremely of surgical removal depends on the micro-
rare, whereas parotid adenocarcinomas are scopic diagnosis.
not uncommon. These malignancies may
proliferate within the infratemporal space
and cause limited opening, cranial nerve
Additional Reading
deficits, and condylar or coronoid erosion Bavitz JB, Chewning LC. Malignant disease as temporo-
as evidenced radiographically. In these mandibular joint dysfunction: review of the literature
and report of case. J Am Dent Assoc. 1990;120:163.
instances, a parapharyngeal mass is usu- Goodsell JO, Hubinger HL. Benign chondroblastoma
ally palpable with deflection of the tonsillar of the mandibular condyle. J Oral Maxillofac Surg.
region or soft palate. 1964;22:355.
PMPH_Eversole_Chapter-12.indd 675 1/20/2011 3:22:18 PM
676 Chapter 12
James RB, Alexander RW, Traver JG. Osteochondroma odontal ligament spaces, loss of attached gin-
of the mandibular coronoid process. Report of a case. giva with foci of stripping, and xerostomia
Oral Surg Oral Med Oral Pathol. 1974;37:189.
Kruse AL, Luebbers HT, Obwegeser JA, Edelmann are all head and neck manifestations of the
L, Graetz KW. Temporomandibular disorders asso- disease.
ciated with metastases to the temporomandibular
joint: a review of the literature and 3 additional cases. TREATMENT
Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
2010;110(2):e21-e28. There is no effective therapy for the restricted
Thoma KH. Tumors of the condyle and temporo- opening observed in scleroderma. Plasma-
mandibular joint. Oral Surg Oral Med Oral Pathol. pheresis has been beneficial for the other
1954;7:1091.
manifestations of the disease.
SCLERODERMA
Additional Reading
Age: Adults Albilia JB, Lam DK, Blanas N, Clokie CM, Sándor GK.
Sex: Female predilection Small mouths... Big problems? A review of scleroder-
CLINICAL FEATURES ma and its oral health implications. J Can Dent Assoc.
2007;73(9):831-836.
Scleroderma or progressive systemic scle- Eversole LR, Jacobsen PL, Stone CE. Oral and gin-
rosis is grouped with the collagen diseases: gival changes in systemic sclerosis (scleroderma).
J Periodontol. 1984;55:175.
although the etiology is unknown, evidence Ramon Y, Samra H, Oberman M. Mandibular condylosis
suggests an immunopathic or autoimmune and apertognathia as presenting symptoms in progres-
mechanism. Although the onset is early sive systemic sclerosis (scleroderma). Oral Surg Oral
adult life, many years evolve before severe Med Oral Pathol. 1987;63:269.
Seiffert MH, Steigerwald JC, Cliff MM. Bone resorp-
symptoms develop. Progressive fibrosis of tion of the mandible in progressive systemic sclerosis.
the skin, lungs, and esophagus is the end Arthritis Rheum. 1975;18:507.
result with expressionless facies, board- Weisman RA, Calcaterra TC. Head and neck manifes-
like skin, sclerodactyly, and dysphagia. tations of scleroderma. Ann Otol Rhinol Laryngol.
1978;87:332.
The CREST syndrome is a variant and is
characterized by soft tissue calcinosis, Ray-
naud’s phenomenon, esophageal stricture, ORAL SUBMUCOUS FIBROSIS
sclerodactyly, and telangiectasia of the skin.
Figure 12-46
Microstomia with restricted opening occurs
late in the course of the disease. The major Age: Adults
cause is fibrosis of the perioral tissues includ- Sex: No predilection
ing the buccal mucosa. The fibrous indura-
CLINICAL FEATURES
tion is palpable and may restrict opening
severely. In addition, some patients mani- Betel nut chewing is a pervasive habit in
fest TMJ symptoms, usually crepitus, and Malaysia, Pakistan, India, Inodnesia, and
radiographs occasionally exhibit arthritic the Philipines among adults. Betel, or areca
erosive changes. is ground and chewed alone or in combi-
nation with tobacco leaves and slaked lime
(Pan). Betal nut chewing leads to mucosal
DIFFERENTIAL DIAGNOSIS changes most prominently seen in the buc-
Because scleroderma is a systemic disease cal mucosa where white scar bands form
with multisystem involvement, the diagno- causing restricted mouth opening. Diffuse
sis in a patient with restricted mandibular multifocal melanotic pigmentation, which
opening is usually straightforward. Board- is probably an expansion of physiologic
hard facial skin, microstomia, widened peri- pigmentation in this population, may also
PMPH_Eversole_Chapter-12.indd 676 1/20/2011 3:22:22 PM
Facial Pain and Neuromuscular Disorders 677
FIGURE 12-46
Restricted opening in betel nut chewer causing oral submucous fibrosis with multifocal pigmentation and
white fibrous scar bands.
occur, as may leukoplakias. The latter are Angadi PV, Rekha KP. Oral submucous fibrosis: a clini-
precancerous lesions that may become dys- copathologic review of 205 cases in Indians. Oral
Maxillofac Surg. 2010 Apr 23. [Epub ahead of print.]
plastic and progress to squamous cell car- Angadi PV, Rao SS. Areca nut in pathogenesis of oral
cinoma. It is noteworthy that oral cancer is submucous fibrosis: revisited. Oral Maxillofac Surg.
one of the most prevalent malignancies in 2010 Apr 8. [Epub ahead of print.]
India. Tumefactive indurated masses are Dagli RJ, Kumar S, Mathur A, Balasubrimanyam G,
Duraiswamy P, Kulkarni S. Prevalence of leukoplakia,
indicative of carcinoma. oral submucous fibrosis, papilloma and its relation with
stress among green marbles mine laborers, India. Med
MICROSCOPIC FEATURES Oral Patol Oral Cir Bucal. 2008;13(11):E687-E692.
Yang YH, Lee HY, Tung S, Shieh TY. Epidemiological
Oral submucous fibrosis is characterized survey of oral submucous fibrosis and leukopla-
by epithelial atrophy and marked fibrosis kia in aborigines of Taiwan. J Oral Pathol Med.
of the submucosal connective tissue. When 2001;30(4):213-219.
leukoplakia is an accompaniment, keratosis
is observed and dysplastic changes may be TETANUS
seen including foci of invasion.
Age: No predilection
DIFFERENTIAL DIAGNOSIS Sex: No predilection
Scleroderma and Hecht-Beals-Wilson syn- CLINICAL FEATURES
drome show similar clinical appearances. Tetany represents sustained tonic muscular
contraction and is seen in Clostridium tetani
TREATMENT
infection and in hypoparathyroidism sec-
Curtailing the habit of betal chewing is the ondary to hypocalcemia. Infectious tetanus
primary preventive strategy. Leukoplakias occurs primarily as a result of accidental
require close clinical monitoring. injury from fomites on which C tetani spores
reside. The organism secretes the tetanus
Additional Reading toxin that is transported to the CNS and acts
on autonomic nerves, end plates, the spinal
Angadi PV. Drug treatment for oral submucous fibrosis. cord, and the brain, where it binds to ganglio-
Evid Based Dent. 2010;11(2):56. sides. Headache is a prodromal sign followed
PMPH_Eversole_Chapter-12.indd 677 1/20/2011 3:22:22 PM
678 Chapter 12
by generalized muscle rigidity. During the etiology of parathyroid dysfunction and
early stages of the disease, masticatory mus- restitution of electrolyte balance by admin-
cle trismus occurs along with facial muscle istration of calcium and dihydrotachysterol.
spasms, producing a distorted demoniacal The care of these patients should be man-
grin referred to as risus sardonicus. This head aged by a physician.
and neck, early manifestation is sometimes
referred to as cephalic tetanus, and seventh
nerve paralysis is often an accompaniment. Additional Reading
The myotonic spasm becomes progressively Jagoda A, Riggio S, Burguieres T. Cephalic tetanus: a
generalized with dysphasia, laryngospasm, case report and review of the literature. Am J Emerg
and autonomic effects including hyperten- Med. 1988;6:128.
sion, cardiac arrythmias, elevated pulse rate, Moersch F, Woltman H. Progressive fluctuating mus-
cular rigidity and spasm (stiff-man syndrome). Mayo
and profuse perspiration. Hyperflexia is also Clinic Proc. 1956;31:421.
featured. Death may result from asphyxia. In Nusynowitz ML, Frame B, Kolb PO. The spectrum of
hypoparathyroidism, low serum calcium lev- hypoparathyroid states. Medicine. 1974;53:127.
els initiate neuromuscular electrolyte distur- Patel J, Mehta B. Tetanus: a study of 2007 cases. Indian J
Med Sci. 1963;17:791.
bances with appearance of convulsions and Smith MJA, Myall RWT. Tetanus: review of the litera-
tetanus. Jaw trismus is rarely seen alone or as ture and report of a case. Oral Surg Oral Med Oral
the chief presenting sign. Carpopedal spasm Pathol. 1976;41:451.
is the predominant finding. Latent tetany is
evaluated by trapping the preauricular skin
over the facial nerve that is followed by facial Generalized Motor
muscle contraction (Chvostek’s sign) and by Function Disorders
producing carpal spasm by reducing blood
flow to the arm by means of a blood pres- AURICULOTEMPORAL
sure cuff (Trousseau’s sign). In addition, low- SYNDROME
ered-threshold electric excitability of nerves
is observed (Erb’s sign). In addition to tetany Age: No predilection
and convulsions, other features of the dis- Sex: No predilection
ease include basal ganglia calcifications, dry CLINICAL FEATURES
skin with alopecia and atrophic nails, and
cataracts. The serum calcium level may dip A complication of conservative parotid
to 5 mg/100 mL with acalciuria; the serum surgery, the auriculotemporal syndrome
phosphate value is elevated. may also develop as a consequence of
trauma or infection of the parotid or
DIFFERENTIAL DIAGNOSIS
preauricular tissues. The syndrome, also
termed gustatory sweating, is characterized
Unlike most of the other disorders with lim- by preauricular sweating, flushing, and
ited opening, tetanus is a systemic disorder sometimes pain after ingestion of food or
involving numerous other muscle groups. visual stimulation by foods that initiate
The diagnosis is made on the basis of the salivation. These symptoms emerge after
aforementioned signs, symptoms, and labo- severance of the auriculotemporal nerve,
ratory findings. which, in addition to its sensory func-
tion, supplies parasympathetic fibers to
TREATMENT the parotid. The fibers regenerate, become
Infectious tetanus is treated by administra- misdirected, and follow the course of
tion of tetanus antitoxin. Hypoparathyroid sympathetic fibers to the skin and sweat
tetany is treated by management of the glands. Parasympathetic fibers that would
PMPH_Eversole_Chapter-12.indd 678 1/20/2011 3:22:26 PM
Facial Pain and Neuromuscular Disorders 679
ordinarily induce salivation inadvertently lar disorder is characterized by exagger-
stimulate the preauricular dermal sweat ated opening of the eye on moving of the
glands and arterioles, causing hydrosis mandible in a contralateral direction. The
and vasodilation. A similar disorder may involved eye shows ptosis at rest. The
accompany facial nerve palsy of surgical pupils of both eyes show normal reflexes
or traumatic origin in which parasympa- without miosis of the ptotic eye. One half of
thetic fibers are misdirected into the lacri- the affected patients manifest exaggerated
mal gland, causing gustatory lacrimation opening by simply abducting the jaw; the
(crocodile tears). other half show this change only when the
jaw is depressed with lateral movement to
DIFFERENTIAL DIAGNOSIS the opposite direction of the ptotic eye. The
Gustatory sweating, dysgeusia, and croco- etiology and pathogenesis are unknown. It
dile tears have been reported to occur with has been theorized that neural fiber cross-
CNS tumor. overs occur between the pterygoid inner-
vation and innervation to the upper lid.
TREATMENT Supranuclear involvement has also been
suggested as responsible.
Control of gustatory sweating may be main-
tained for up to 3 days by topical application
DIFFERENTIAL DIAGNOSIS
to the affected skin of 1% glycopyrrolate
lotion or cream. Intracutaneous injections Unilateral ptosis as seen in the jaw-wink-
of botulinum toxin A (Botox, Allergan Inc, ing phenomenon may be confused with
USA) are effective. Horner’s syndrome. In the former, miosis
with anhydrosis is lacking; conversely, the
upper lid fails to open on depression of the
Additional Reading mandible in Horner’s syndrome.
Bjerkhoel A, Trobbe O. Frey’s syndrome: treatment with
botulinum toxin. J Laryngol Otol. 1997;111(9):839-844. TREATMENT
Gardner WJ, McCubbin JW. Auriculotemporal syn-
drome; gustatory sweating due to misdirection of Surgical treatment by unilateral levator
regenerating nerve fibers. JAMA. 1956;160:272. resection and by the frontalis muscle flap
Hays LL, Novack AJ, Worsham JC. The Frey syndrome: or orbicularis oculi muscle flap results in
a simple, effective treatment. Otolaryngol Head Neck
Surg. 1982;90:419.
diminution of the anomaly.
Hemenway WG. Gustatory sweating and flushing: the
auriculo-temporal syndrome—Frey’s syndrome.
Laryngoscope. 1960;70:84.
Schnarch A, Markitziu A. Dysgeusia, gustatory sweating, Additional Reading
and crocodile tears syndrome induced by a cerebello-
pontine angle meningioma. Oral Surg. Oral Med Oral Altman, K. The Marcus-Gunn (jaw-winking) phe-
Pathol. 1990;70:711. nomenon: a case report. Br J Oral Maxillofac Surg.
1990;28:53.
Hamed LM, Dennehy PJ, Lingua RW. Synergistic
divergence and jaw-winking phenomenon. J Pediatr
JAW-WINKING PHENOMENON Ophthalmol Strabismus. 1990;27:88.
Haynes PR. A quantitative investigation of the
Age: Childhood or congenital Marcus Gunn phenomenon. Am J Optom. 1955;32:
621.
Sex: Slight male predilection
Park DH, Choi WS, Yoon SH. Treatment of the jaw-
CLINICAL FEATURES winking syndrome. Ann Plast Surg. 2008;60(4):404-
409.
The jaw-winking phenomenon is a mis- Smith EE, Gans ME. Jaw-winking (Marcus Gunn phe-
nomer in that this bizarre neuromuscu- nomenon). J Pediatr. 1957;50:52.
PMPH_Eversole_Chapter-12.indd 679 1/20/2011 3:22:27 PM
680 Chapter 12
MOTOR SYSTEM DISEASE TREATMENT
No known treatment exists. The motor sys-
Age: Varies according to subtype
tem diseases are progressive, eventually
Sex: Male predilection
resulting in death.
CLINICAL FEATURES
The motor system diseases include pro-
gressive muscular atrophy, which begins
Additional Reading
in childhood and involves the extremities; DePaul R, Abbs JH, Caligiuri M, Gracco VL, Brooks BR.
amyotrophic lateral sclerosis (ALS); and Hypoglossal, trigeminal and facial motoneuron involve-
ment in amyotrophic lateral sclerosis. Neurology.
progressive bulbar palsy. The motor sys- 1988;38:281 .
tem diseases result from degeneration of Horton WA, Eldridge R, Brody JA. Familial motor neu-
the corticospinal and anterior horn cells. ron disease. Neurology. 1976;26:460.
The latter two variants begin in adulthood Roe PF. Familial motor neuron disease. J Neurol
Neurosurg Psychiatry. 1964;27:140.
and result in bulbar signs. These two dis-
Roller NW, Garfunkel A, Nichols C, Ship II. Amyotrophic
orders may show a familial pattern or may lateral sclerosis. Oral Surg Oral Med Oral Pathol.
develop after a neurotropic infection. In 1974;37:46.
ALS, patients show ambulatory difficul- Wee CD, Kong L, Sumner CJ. The genetics of spi-
ties and weakness of the oropharyngeal nal muscular atrophies. Curr Opin Neurol. 2010;23:
450-458.
musculature evidenced by difficulty with
swallowing and speech. In progressive
bulbar palsy, deglutition and articulation MULTIPLE SCLEROSIS
defects are present in conjunction with
atrophy of masticatory and facial muscles. Age: Young adults
Fasciculation of the tongue is often present Sex: Slight female predilection
in both forms with bulbar manifestations. CLINICAL FEATURES
There are 16 distinct forms of spinal motor
atrophy, 14 of which manifest mutations Multiple sclerosis is a demyelinating dis-
in genes that encode proteins involved in ease, probably of either viral or autoim-
transcriptional regulation, RNA process- mune origin, that involves the CNS without
ing, and cytoskeletal dynamics: TRPV4, demyelinization of peripheral nerves. The
ATP7A, VRK1, and HSPB3. Genetic test- disease is chronic with periods of remission
ing is now available for many of these and exacerbation. A variety of neurologic
mutations. signs and symptoms are observed, depend-
ing on anatomic location and severity of
lesions. These signs and symptoms can
DIFFERENTIAL DIAGNOSIS
be extremely diverse; the more common
Difficulty with swallowing and articula- include spasticity, hyper-reflexia, Babin-
tion, cardinal signs of bulbar degenerative ski’s sign, absent abdominal reflexes, inten-
motor system disorders, may also be seen tion tremor, nystagmus, sensory deficits,
in organic disease such as cancer of the paresthesias, muscle weakness, ocular dis-
larynx or base of the tongue. For this rea- turbance, urinary disturbance, and ataxia.
son, a thorough physical examination is Facially, the more prevalent or noteworthy
required when these symptoms emerge. manifestations are ocular (diplopia, blur-
Bulbar lesions subsequent to cerebrovas- ring of vision, visual field defects, and sco-
cular accident may cause similar signs and toma), sensory (trigeminal paresthesia or
symptoms. neuralgia), and motor (seventh nerve pare-
PMPH_Eversole_Chapter-12.indd 680 1/20/2011 3:22:27 PM
Facial Pain and Neuromuscular Disorders 681
sis and dysarthria). Cognitive impairments MUSCULAR DYSTROPHIES
include memory, speed processing, execu-
tive function, attention, and concentration Age: Childhood onset
domains. The more significant laboratory Sex: Male predilection
abnormalities include elevated cerebrospi- CLINICAL FEATURES
nal fluid levels of immunoglobulin G and
white cells. Cortical-evoked responses from Muscular dystrophy of Duchenne is a gen-
visual, auditory, and sensorimotor stimula- eralized progressive disease of muscle with
tion have been shown to be of value in early an X-linked recessive mode of inheritance,
diagnosis. CT scans often disclose ven- occurring in males. A restricted form, fas-
tricular enlargement, cortical atrophy, and cioscapulohumeral dystrophy, shows no sex
periventricular plaques. predilection, and the disorder is restricted to
muscles of the face, neck, and shoulder. The
defective gene has been localized to chromo-
DIFFERENTIAL DIAGNOSIS
some 4. In all forms of muscular dystrophy,
Myelinoclastic infectious diseases are easily the primary defect lies in the muscle fiber;
confused with multiple sclerosis because the neural function and reflexes are not affected.
signs and symptoms can be identical. Neu- In the generalized form, which is more com-
rologic lesions in other diseases including mon, early childhood onset is characterized
lupus erythematosus, polyarteritis nodosa, by inability to ambulate, with pseudohy-
vascular malformations and gliomas of the pertrophy of the limb muscles. The increase
brain stem, syringomyelia, and lymphoma in muscle bulk is the result of fatty infiltra-
may exhibit features similar to those enu- tion so that weakness and poor function
merated for multiple sclerosis. Patients with are encountered. The muscles eventually
unexplained facial weakness, paresthesia, become atrophic. Masticatory, facial, and
or trigeminal neuralgia should be evalu- strap muscles are involved late in the course
ated for the disease. of the disease, with difficulty chewing,
swallowing, and articulating. Serum creati-
TREATMENT nine phosphokinase levels are elevated early
in the course of the disease. Fascioscapu-
Referral to a neurologist is recommended. lohumeral dystrophy spares the lower limbs
The disease may be quite mild or may and does not show pseudohypertrophic
remain in long-term remission. Alterna- enlargement. Onset may be later in life and
tively, in some instances, it is a progres- is characterized by profound weakness of
sive disease that leaves the patient severely the arms, inability to close the eyes, droop-
disabled. ing of the facies, and inability to purse the
lips (which are protuberant). Cardiac fail-
Additional Reading ure is a common complication. The various
forms of muscular dystrophy involve the
Brisman R. Trigeminal neuralgia and multiple sclerosis. complex dystrophin-associated glycopro-
Arch Neurol. 1987;44:379.
Ferreira ML. Cognitive deficits in multiple sclerosis: a
teins of the extracellular matrix: CMD with
systematic review. Arq Neuropsiquiatr. 2010;68(4): merosin deficiency (CMD1A), collagen VI-
632-641. related CMDs (Ullrich CMD and Bethlem
Mackay R, Hirano A. Forms of benign multiple sclerosis. myopathy), CMDs with abnormal glycosy-
Arch Neurol. 1967;17:588.
Poser CM. Diseases of the myelin sheath. In: Merritt HH,
lation of α-dystroglycan (Fukuyama CMD,
ed. A Textbook of Neurology. 6th ed. Philadelphia, PA: muscle-eye-brain disease, Walker-Warburg
Lea & Febiger; 1979:768. syndrome, CMD1C, CMD1D), and the much
PMPH_Eversole_Chapter-12.indd 681 1/20/2011 3:22:27 PM
682 Chapter 12
rarer CMD with integrin deficiency. Yet other major forms exist: dystrophic and congeni-
forms of CMDs are not related to the dys- tal myotonias. Myotonic contractions may
trophin/glycoproteins/extracellular matrix also be acquired after trismus, with spread
complex (rigid spine syndrome, CMD1B, of infection to muscle. This form is most
CMD with lamin A/C deficiency) common, and in the head and neck area,
myositis of the masticatory muscles gener-
DIFFERENTIAL DIAGNOSIS ally develops as a complication of odonto-
The two forms of muscular dystrophy may genic infection or pericoronitis. Myotonia
be differentiated on the basis of age and dis- congenita is the result of mutations in the
tribution of muscle involvement. Both may CLCN1 gene that controls muscle mem-
show myopathic facies, which occur in the brane hyperexcitability caused by reduced
myotonias, and myasthenia gravis. A mus- sarcolemmal chloride conductance. The
cle biopsy may be helpful in determining disorder may be transmitted as either an
whether the patient suffers from muscular autosomal dominant or recessive trait. Dys-
dystrophy. Muscle fibers show variation in trophic myotonia develops in late childhood
size with infiltration of adipose tissue, and as an autosomal dominant trait. In addition
enzyme histochemical stains are useful. to sustained contractions after voluntary
neuromuscular activity, atrophy of the mas-
TREATMENT ticatory and strap muscles occurs to yield
the so-called myopathic facies. Masticatory
No treatment is presently effective. In
weakness, malocclusion, and altered cran-
Duchenne’s muscular dystrophy, survival
iofacial morphology have been reported
beyond the second decade is rare. Fas-
among patients with myotonic dystrophy.
cioscapulohumeral muscular dystrophy
Testicular atrophy is often present. Con-
is compatible with life; however, many
genital myotonia, a familial disorder, com-
patients develop cardiac failure.
mences early in life and affects virtually all
skeletal muscles. The myotonic contractions
Additional Reading are severe but painless. The affected indi-
viduals manifest significant generalized
Black JT, Bhatt GP, Dejesus PV, Schotland DL, Rowland
LP. Diagnostic accuracy of clinical data, quantitative muscular hypertrophy so that they appear
electromyography and histochemistry in neuromuscular to be muscle bound.
disease. A study of 105 cases. J Neurol Sci. 1974;21:59.
Hanson P, Rowland LP. Möbius syndrome and fascioscapu- DIFFERENTIAL DIAGNOSIS
lo-humeral muscular dystrophy. Arch Neurol. 1971;24:31.
Lunt PW. A workshop on fascioscapulohumeral Dystrophic myotonia may resemble late
(Landouzy-Dejerine) disease, Manchester, 16 to 17 muscular dystrophy and myasthenia gravis,
November, 1988. J Med Genet. 1989;26:535. as muscular atrophy with a myopathic facies
Pearson CM. Muscular dystrophy. Am J Med. 1963;35:632.
Reed UC. Congenital muscular dystrophy. Part I: a may be seen in all three of these muscular
review of phenotypical and diagnostic aspects. Arq disorders. Characteristic myotonic contrac-
Neuropsiquiatr. 2009;67(1):144-168. tions are seen only in myotonia. The muscle
hypertrophy of congenital myotonia is also
MYOTONIAS accompanied by myotonic contraction, aid-
ing in differentiating this disorder from
Age: Children and young adults pseudohypertrophic muscular dystrophy.
Sex: No predilection
CLINICAL FEATURES TREATMENT
The myotonias are characterized by failure No treatment is available for the familial
of muscle relaxation after contraction. Two myotonias. The dystrophic form is ultimately
PMPH_Eversole_Chapter-12.indd 682 1/20/2011 3:22:27 PM
Facial Pain and Neuromuscular Disorders 683
fatal, whereas the congenital form carries musculature allow for differentiation from
a favorable prognosis. Acquired myotonia these other disorders.
may be treated by removing the source of
infection and employing antibiotics. TREATMENT
No treatment is effective. The disease is not
Additional Reading fatal.
Becker PE. Genetic approaches to the nosology of mus-
cular disease: myotonias and similar diseases. Birth
Defects. 1971;7:52.
Additional Reading
Dyken PR, Harper PS. Congenital dystrophia myotonia. Garcia Erro MI, Correale J, Arberas C, Sanz OP,
Neurology. 1973;23:465. Muchnik S, Sica RE. Familial congenital facial diple-
Kiliaridis S, Mejersjo C, Thilander B. Muscle function and gia: electrophysiologic and genetic studies. Pediatr
craniofacial morphology: a clinical study in patients with Neurol. 1989;5:262.
myotonic dystrophy. Eur J Orthodont. 1989;11:131. McDougal JJ. Möbius syndrome: a congenital facial diple-
Lossin C, George AL, Jr. Myotonia congenita. Adv Genet. gia syndrome. J Conn State Dent Assoc. 1960;34:21.
2008;63:25-55. Pedraza S, Gámez J, Rovira A, et al. MRI findings in
Thayer HH, Crenshaw J. Oral manifestations of myo- Möbius syndrome: correlation with clinical features.
tonic muscular dystrophy, report of a case. J Am Dent Neurology. 2000;55(7):1058-1060.
Assoc. 1966;72:1405. Thakkar N, O’Neil W, Duvally J, Liu C, Ambler M.
Möbius syndrome due to brainstem tegmental necro-
sis. Arch Neurol. 1977;34:124.
CONGENITAL FACIAL
DIPLEGIA
HEMIFACIAL ATROPHY
Age: Congenital
Sex: No predilection Age: Teenagers
Sex: Female predilection
CLINICAL FEATURES
CLINICAL FEATURES
The Möbius syndrome is a nonfamilial
congenital primary myopathy of the facial Unilateral progressive atrophy of the face,
muscles with secondary degeneration of known as Romberg’s syndrome, is an
the abducens and facial nerves. Alterna- uncommon disorder of unknown origin. It
tively, in utero, necrosis of brain stem nuclei begins during the second decade with slowly
has been reported and may result from an progressive atrophy of the skin, muscle, and
episode of anoxia. The paralysis is bilateral often even the maxilla and mandible on one
with expressionless facies and inability side of the face. The disease progresses for
to close the eyes. The muscles of mastica- 3 or 4 years and ultimately becomes static.
tion may also be affected, with difficulty in The teeth on the affected side may be smaller
chewing and swallowing. Drooling is often than normal, and eruption may be somewhat
uncontrollable. Patients also show a variety retarded. Contralateral epilepsy and trigem-
of other congenital defects including deaf- inal neuralgia may accompany the atrophic
ness, epilepsy, and club foot. MRI reveals changes. The condition may be the result of a
brainstem hypoplasia with straightening of trophic malformation of the cervical sympa-
the fourth ventricle floor, a finding indica- thetic nervous system secondary to trauma,
tive of an abscent facial colliculus. viral infections, heredity, endocrine distur-
bances, and autoimmunity, among others
DIFFERENTIAL DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
Congenital facial diplegia shows myopathic
facies seen in other myopathies; however, The facial asymmetry with atrophy on one
onset at birth and restriction to the facial side may be confused with hemifacial hyper-
PMPH_Eversole_Chapter-12.indd 683 1/20/2011 3:22:27 PM
684 Chapter 12
trophy. Close observation shows that the operating at the level of the neuromuscular
larger side of the face is normal, the smaller junction with interference in the release-
side is atrophic. Unilateral TMJ ankylosis binding of acetylcholine. Thymic hyperpla-
may show features similar to Romberg’s sia or thymoma is found in most patients
syndrome; however, in the former, only the with myasthenia gravis. Antiacetylcholine
mandible is atrophic, whereas in the latter, receptor antibody testing and single fiber
the entire hemiface is involved. electromyography are the more reliable
diagnostic tests.
TREATMENT
DIFFERENTIAL DIAGNOSIS
Plastic surgery may be performed once the
The myopathic facies with generalized mus-
atrophic process has stabilized.
cular weakness is seen in muscular dys-
trophy, myotonias, and Möbius syndrome.
Additional Reading The onset during midlife, predilection for
females, lack of myotonic contraction, and
Crikelair GF, Moss ML, Khuri A. Facial hemiatrophy. lack of muscle hypertrophy favor a diag-
Plast Reconstr Surg. 1962;29:5. nosis of myasthenia. A muscle biopsy may
Glass D. Hemifacial atrophy. Br J Oral Maxillofac Surg. be helpful in that perivascular lymphoid
1964;1:194.
Ong B, Chong PN, Yeo PP. Progressive hemifacial atro-
aggregates appear between muscle bundles
phy—a report of 2 cases. Singapore Med J. 1990;31:497. in this disorder, but are not featured in the
Pensler JM, Murphy GF, Mulliken JB. Clinical and ultra- aforementioned disorders. A classic diag-
structural studies of Romberg’s hemifacial atrophy. nostic finding is the ability of intramuscu-
Plast Reconstr Surg. 1990;85:669. lar injection of physostigmine to restore
Pinheiro TP, Silva CC, Silveira CS, Botelho PC, Pinheiro
MG, Pinheiro Jde J. Progressive hemifacial atro- normal functions.
phy—case report. Med Oral Patol Oral Cir Bucal.
2006;11(2):E112-E114. TREATMENT
Myasthenia gravis is treated with anticho-
linesterases such as neostigmine or related
MYASTHENIA GRAVIS drugs and should be managed by an inter-
Age: Middle-aged adults
nist or neurologist.
Sex: Female predilection
CLINICAL FEATURES Additional Reading
Myasthenia gravis is characterized by gen-
Benatar M. A systematic review of diagnostic stud-
eralized muscular weakness involving only ies in myasthenia gravis. Neuromuscul Disord.
voluntary muscle, the heart being spared. 2006;16(7):459-467.
Often the facial and masticatory muscles Chia LG. Facial weakness without ocular weakness in
are the first to show fatigue after limited myasthenia gravis. Muscle Nerve. 1988;11:185.
Gallagher DM, Erickson KL, Genkins G. Current
movement. As the disease progresses, pto- concepts in the surgical treatment of patients with
sis with an expressionless myopathic facies myasthenia gravis. J Oral Maxillofac Surg. 1981;
develops. In advanced cases, the jaw and 39:30.
head droop; eventually, the respiratory Garvin JS. Differential diagnosis of muscle weakness in
myasthenia gravis, polymyositis, and muscular dystro-
muscles become fatigued. The cause for phy. Med Clin North Am. 1965;49:189.
this condition is unknown but has been Keeling CW. Myasthenia gravis. J Oral Maxillofac Surg.
linked to immunopathologic mechanisms 1951;9:224.
PMPH_Eversole_Chapter-12.indd 684 1/20/2011 3:22:27 PM
Appendices
Appendix I. Classification of Certain Oral Cysts,
Reactive Proliferations, and Neoplasms
I. ODONTOGENIC CYSTS Thyroglossal duct cyst
Nasoalveolar (Kledstadt) cyst
Dental lamina cyst Cyst of incisive papilla
Gingival cyst True mucous cyst (sialocyst)
Primordial cyst Mucous retention cyst of the sinus
Lateral periodontal cyst C. Pseudocysts
Dentigerous (follicular) cyst Mucous retention phenomenon
Eruption cyst (mucocele)
Apical periodontal cyst Ranula (mucocele)
Calcifying cystic odontogenic tumor Traumatic (hemorrhagic) cyst
Orthokeratotic odontogenic cyst Aneurysmal bone cyst
Odontogenic keratocyst (keratocys-
tic odontogenic tumor)
Sialoodontogenic cyst III. BENIGN ODONTOGENIC
NEOPLASMS AND
HAMARTOMAS
II. DEVELOPMENTAL AND
NONODONTOGENIC A. Epithelial Group
CYSTS Ameloblastoma
Invasive type
A. Intraosseous Cysts Unicystic type
Incisive canal (nasopalatine) cyst Desmoplastic type
Median mandibular cyst Calcifying epithelial odontogenic
Surgical ciliated cyst of the maxilla tumor
B. Soft Tissue Cysts Odontogenic adenomatoid tumor
Epidermoid cyst Epithelial odontogenic hamartoma
Dermoid cyst Squamous odontogenic tumor
Lymphoepithelial (branchial cleft) B. Mixed Group
cyst Ameloblastic fibroma
Benign cystic lymph node Ameloblastic fibrodentinoma
Lingual gastric cyst (enterocystoma) Ameloblastic fibro-odontoma
PMPH_Eversole_Appendices.indd 685 1/17/2011 3:56:46 PM
686 Appendices
Odontoma Ductal epidermoid carcinoma
Odontoameloblastoma Undifferentiated carcinoma
C. Mesenchymal Group Small cell type
Odontogenic fibroma Large cell type
Odontogenic myxoma Malignant lymphoepithelial
Periapical cemental dysplasia lesion
(cementoma) Acinic cell carcinoma
Benign cementoblastoma Epithelial-myoepithelial carcinoma
Cementifying fibroma of intercalated duct
Granular cell odontogenic tumor Salivary duct carcinoma
D. Malignant Odontogenic Neoplasms Sialoblastoma
Malignant ameloblastoma Mucinous adenocarcinoma
Ameloblastic carcinoma Papillary cystadenocarcinoma
Clear cell odontogenic tumor Adenocarcinoma (not otherwise
(carcinoma) specified)
Intraosseous squamous cell
carcinoma V. ORAL EPITHELIAL
Ameloblastic fibrosarcoma
NEOPLASMS
A. Benign
IV. SALIVARY NEOPLASMS Papilloma
Verruca vulgaris
A. Benign
Condyloma acuminatum
Pleomorphic adenoma (mixed
Keratoacanthoma
tumor)
B. Malignant
Myoepithelioma
Squamous cell carcinoma
Monomorphic adenoma
Papillary exophytic squamous
Canalicular (basal cell) adenoma
cell carcinoma
Papillary cystadenoma lympho-
Verrucous carcinoma
matosum
Adenoacanthoma (pseudoglan-
Sialadenoma papilliferum
dular squamous cell carcinoma)
Oxyphilic adenoma (oncocytoma)
Spindle cell (sarcomatoid)
Intraductal papilloma
carcinoma
Ductal inverted papilloma
Sebaceous lymphadenoma
Glycogen-rich adenoma VI. NEUROECTODERMAL
Papillary cystadenoma HAMARTOMAS AND
Sclerosing polycystic adenosis NEOPLASMS
B. Malignant
Adenoid cystic carcinoma Ephilis
(cylindroma) Nevocellular nevi
Adenosquamous carcinoma Melanocytic nevi (blue nevus)
Mucoepidermoid carcinoma Spindle cells (Spitz) nevus
Polymorphous low-grade adeno- Melanotic neuroectodermal tumor
carcinoma of infancy
Malignant mixed tumor Hutchinson’s freckle (superficial
Carcinoma ex pleomorphic ade- spreading melanoma)
noma Malignant melanoma
PMPH_Eversole_Appendices.indd 686 1/17/2011 3:56:46 PM
Appendices 687
VII. MESENCHYMAL VIII. REACTIVE
NEOPLASMS OF SOFT PROLIFERATIONS
TISSUE
Pyogenic granuloma
A. Benign Traumatic fibroma
Fibroma Inflammatory fibrous hyperplasia
Giant cell fibroma (epulis fissuratum)
Collagenoma Papillomatosis
Lipoma Peripheral ossifying fibroma
Leiomyoma Peripheral giant cell granuloma
Rhabdomyoma Nodular fasciitis
Granular cell tumor Pseudosarcomatous fasciitis
Neurofibroma Myositis ossificans
Neurilemmoma (schwannoma) Proliferative myositis
Palisaded encapsulated neuroma
Solitary fibrous tumor
Osseous and cartilaginous IX. CENTRAL
choristoma NONODONTOGENIC BONE
Benign fibrous histiocytoma TUMORS OF THE JAWS
Hemangioma
Lymphangioma and cystic A. Benign
hygroma Desmoplastic fibroma (fibroma-
B. Aggressive tosis)
Hemangioendothelioma Hemangioma
Hemangiopericytoma Arteriovenous malformation
Myofibroma/myofibromatosis Neurofibroma
C. Malignant Neurilemmoma
Fibrosarcoma Leiomyoma
Liposarcoma Central ossifying fibroma
Leiomyosarcoma Osteoma
Rhabdomyosarcoma B. Malignant
Alveolar soft part sarcoma Osteogenic sarcoma
Liposarcoma Chondrosarcoma
Neurogenic sarcoma Fibrosarcoma
Malignant fibrous histiocytoma Neurogenic sarcoma
Synovial sarcoma Ewing’s sarcoma
Angiosarcoma Angiosarcoma
Kaposi’s sarcoma Non-Hodgkin’s lymphoma
Malignant lymphoma (Hodgkin’s Burkitt’s lymphoma
and non-Hodgkin’s types) Multiple myeloma
PMPH_Eversole_Appendices.indd 687 1/17/2011 3:56:46 PM
688 Appendices
Appendix II. Classification of Benign
Fibro-Osseous Lesions
I. GIANT CELL GROUP Ossifying and cementifying fibromas
Juvenile aggressive ossifying fibroma
Central giant cell granuloma (trabecular and psammomatoid)
Hyperparathyroid brown tumor Gigantiform cementoma
Aneurysmal bone cyst Periapical cemental dysplasia
Cherubism (familial fibrous dysplasia) (cementoma)
Focal sclerosing osteomyelitis
II. NONGIANT CELL GROUP Diffuse sclerosing osteomyelitis
(PURE FIBRO-OSSEOUS) Florid osseous dysplasia
Garre’s proliferative periostitis
Fibrous dysplasia
Osteitis deformans
Appendix III. Oral Lesions Associated
With HIV Infection
I. LESIONS ASSOCIATED Human papillomavirus—
WITH AIDS condylomatous papillary
lesions, Heck disease-like pap-
Kaposi’s sarcoma—red/purple ules
macules or tumefactions Fungal
Non-Hodgkin’s lymphoma— Candidiasis—pseudomembra-
ulcerated masses nous, erythematous, hyperplas-
Histoplasmosis—granulomatous tic, papillary, angular cheilitis
ulcerations Cryptococcosis—granulomatous
Herpes simplex lesions over 1 month ulcers, palatal perforation
duration—oral or labial vesiculoul- Bacterial
cerative lesions Mycobacterium avium intracel-
lular—granulomatous mass or
II. OTHER LESIONS ulcer
HIV gingivitis—erythematous
ASSOCIATED WITH band of marginal gingiva
AIDS OR PRE-AIDS HIV- HIV periodontitis—focal painful
SEROPOSITIVE SUBJECTS lesions with cementum exposure
HIV necrotizing stomatitis—
Viral progression of HIV periodonti-
Varicella zoster—shingles of the tis to adjacent tissues
trigeminal pathways Unknown etiology
Cytomegalovirus—aphthaeform HIV polycystic disease of
ulcers salivary glands
Epstein-Barr virus—oral hairy Aphthous-like ulcerations
leukoplakia
PMPH_Eversole_Appendices.indd 688 1/17/2011 3:56:46 PM
Appendices 689
Appendix IV. Clinical Laboratory
Parameters
The following diseases, which are associated with elevated or depressed values, are by
no means all inclusive. Rather, they represent the more common disease states showing
alterations in laboratory values.
I. HEMOGRAM
A. Red Blood Cell Count, Hemoglobin, and Hematocrit
1. Elevated 2. Depressed
Fluid loss Iron deficiency anemia
Polycythemia vera Pernicious anemia
Secondary polycythemia Malaria
Hemorrhage
Thalassemia
Sickle-cell anemia
Hemolytic anemias
Leukemia
Metastatic cancer
Osteopetrosis
Multiple myeloma
Pancytopenia
Erythroblastosis fetalis
Renal disease
B. White Blood Cell Count
1. Elevated 2. Depressed
Infections Certain viral infections
Leukemia Leukemia (leukopenic phase)
Agranulocytosis
Cyclic neutropenia
Hemorrhage
Pancytopenia
Typhoid fever
C. Differential White Count
1. Neutrophilic Leukocytosis
a. Pyogenic infections
b. Myelogenous leukemia
2. Lymphocytic Leukocytosis
a. Viral infections
b. Typhoid fever
c. Lymphocytic leukemia
d. Infectious mononucleosis
3. Eosinophilic Leukocytosis
a. Allergy
b. Parasitic infections, particularly helminths
PMPH_Eversole_Appendices.indd 689 1/17/2011 3:56:46 PM
690 Appendices
4. Neutrophilic Leukopenia
a. Agranulocytosis
b. Cyclic neutropenia
c. Leukemia
D. Thrombocytes
1. Depressed Count
Thrombocytopenic purpura
Secondary thrombocytopenia
Pancytopenia
Leukemia
Metastatic cancer
Multiple myeloma
Consumptive coagulopathy (DIC)
Postinfections
2. Delayed Aggregation
Thrombocytopathic purpura
von Willebrand’s disease
Salicylates and other drugs
II. COAGULATION PANEL
A. Prothrombin Time Prolonged
Alcoholic cirrhosis
Biliary cirrhosis
Hepatitis
Idiopathic steatorrhea
Hypovitaminosis K
Coumadin therapy
Afibrinogenemia
Hypoprothrombinemia
B. Partial Thromboplastin Time Prolonged
Hemophilia
Christmas disease
von Willebrand’s disease
Hageman deficiency
All disorders manifesting prolonged prothrombin time
C. Fibrin Split Products
Disseminated intravascular coagulation
III. SEROLOGY (ELEVATED OR POSITIVE TESTS)
A. VDRL, TPI, FTA—Syphilis
B. Monospot, Heterophil Antibody—Infectious Mononucleosis
C. Antistreptolysin-O—Scarlet Fever, Rheumatic Fever, Erysipelas, Streptococcal
Sore Throat
PMPH_Eversole_Appendices.indd 690 1/17/2011 3:56:47 PM
Appendices 691
D. RA Factor—Rheumatoid Arthritis
E. Antineutrophil cytoplasmic Antibody (C-ANCA, PR-3 ANCA)—Wegener’s
granulomatosis
F. Antinuclear Antibodies and Anti-DNA Antibodies—Lupus Erythematosus,
Miscellaneous Collagen Diseases
G. Antimitotic Spindle Antibody—Scleroderma
H. Coombs’ Test—Erythroblastosis Fetalis and Other Immune Hemolytic
Anemias
I. HBS-AB—Immunity to Hepatitis B
J. HBS-AG, Hepatitis Core AG—Active or Carrier Status for Hepatitis B
IV. IMMUNOFLUORESCENCE
A. Antibasal Lamina Antibodies (Smooth)—Bullous Pemphigoid, Benign Mucous
Membrane Pemphigoid
B. Antibasal Lamina Antibodies (Granular)—Lupus Erythematosus
C. Anti-Intercellular Cement Antibodies—Pemphigus Vulgaris
D. Antibasal Lamina Fibrinogen—Lichen Planus
E. Submucosal Papillae IgA Antibodies—Dermatitis Herpetiformis
F. Antiductal Salivary Antibodies—Sjögren’s Syndrome
G. Speckled Antinuclear Epithelial Antibodies- Chronic Ulcerative Stomatitis
V. COMMONLY EMPLOYED IMMUNOHISTOCHEMICAL
MARKERS IN HISTOPATHOLOGY
A. Epithelium: AE1-AE3 cytokeratins, specific cytokeratins, EMA (epithelial
membrane antigen)
B. Connective tissues: Vimentin
C. Leukocytes: CD3 T cells, CD20 B cells, CD45 common leukocyte antigen, CD56
natural killer cells
D. Myeloid cells: myeloperoxidase
E. Cell division markers: PCNA, Ki67/MIB1
F. Nerve sheath and granular cell tumors: S-100
G. Vascular walls: Factor VIII, CD34, smooth muscle actin
F. Melanocytic tumors: S-100, HMB45
G. Langerhans cells: S-100, CD1a
H. Muscle: desmin, SMA (smooth muscle actin)
I. Neuroendocrine tumors: synaptophysin, chromogranin
J. Histiocytes: CD68
K. Specific microorganisms: HPV, HSV 1 and 2, CMV, EBV
PMPH_Eversole_Appendices.indd 691 1/17/2011 3:56:47 PM
692 Appendices
VI. CLINICAL LABORATORY
Test Elevated Values Depressed Values
A. Glucose Diabetes mellitus Insulinoma
70–110 mg/100 ml Acute pancreatitis Addison’s disease
Cushing’s syndrome Liver disease
Pheochromocytoma Early diabetes
Acromegaly Glycogenosis
Anabolic hormones Renal glycosuria
Hemochromatosis
B. Total Bilirubin
0.1–1.0 mg/100 ml Biliary obstruction
Liver diseases
Hemolytic anemias
Hepatitis
Postextravasation
Dubin-Johnson syndrome
Gilbert’s disease
Crigler-Najar syndrome
Rotor’s syndrome
Malnutrition
C. Cholesterol
150–300 mg/100 ml Atherosclerosis Liver disease
Diabetes mellitus Malnutrition
Nephrotic syndrome Anemia
Hypothyroidism
Hyperlipoproteinemia
Gout
Myeloma
Biliary obstruction
D. Uric Acid
2.5–8.0 mg/100 ml Gout Cirrhosis
Malignancy Renal tubular disease
Infectious mononucleosis Various drugs
Renal disease Wilson’s disease
Tissue necrosis
Anemias
E. Creatinine
0.05–1.5 mg/100 ml Muscle necrosis
Renal disease
F. Total Protein
6–8 g/100 ml Liver disease Renal disease
Collagen disease Debilitating disease
Chronic infection Malnutrition
Myeloma Burns
Cryoglobulinemia Hypogammaglobulinemia
PMPH_Eversole_Appendices.indd 692 1/17/2011 3:56:47 PM
Appendices 693
G. Albumin
3.5–5 g/100 ml Liver disease
Nephrotic syndrome
Malnutrition
Burns
H. Calcium
8.5–10.5 mg/100 ml Hyperparathyroidism Renal disease
Milk-alkali syndrome Malnutrition
Malignancy Acute pancreatitis
Sarcoidosis Hypoparathyroidism
Hypothyroidism Vitamin D refractory
rickets
Addison’s disease
Hypophosphatasia
I. Phosphorus
2.5–4.5 mg/100 ml Malignancy in bone Hyperparathyroidism
Renal disease Malnutrition
Hypoparathyroidism Osteomalacia
Milk-alkali syndrome Renal tubular disease
Sarcoidosis Vitamin D refractory
rickets
Addison’s disease Hypophosphatasia
J. Alkaline Phosphatase
1.5–5 Bodansky U/ml Bone metastasis Hypophosphatasia
5–10 King- Hepatobiliary disease Malnutrition
Armstrong U/ml
Renal disease
Paget’s disease
Bone fractures
Fibrous dysplasia
Ulcerative colitis
Hyperthyroidism
Pancreatitis
Sarcoidosis
Rickets
Amyloidosis
K. SGOT
10–40 U/ml Acute myocardial infarction
Liver disease
Skeletal muscle disease
Congestive heart failure
Renal infarction
Pulmonary infarction
Malignancy
Burns
Certain anemias
Eclampsia
Trauma
PMPH_Eversole_Appendices.indd 693 1/17/2011 3:56:47 PM
694 Appendices
Test Elevated Values Depressed Values
L. LDH
100–225 U/ml Myocardial infarction
Liver disease
Skeletal muscle disease
Renal infarction
Pulmonary infarction
Cerebral vascular accident
Collagen vascular diseases
Acute pancreatitis
Trauma
Appendix V.Prescriptions Useful in the
Management of Oral Diseases
I. Antibiotics endocarditis prophylaxis is recommended only for high risk of adverse
outcomes from endocarditis to include: prosthetic cardiac valve, previous endocardi-
tis, select cyanotic congenital heart defects that include: 1. unrepaired cyanotic heart
disease including those with palliative shunts and conduits, 2. completely repaired
congenital heart disease with prosthetic material or device, whether placed by surgery
or catheter intervention, during the first six months after the procedure, 3. repaired
congenital heart disease with residual defects at the site or adjacent to the site of a
prosthetic patch or prosthetic device (which inhibit endothelialization). Cardiac trans-
plant recipients with valvular disease. In the above conditions, prophylactic coverage
is recommended for periodontal, endodontic and mucosal perforation (surgery).
Antibiotic Prophylactic Regimens (1 hour before procedure)
Situation Agent Adults Children
Oral Amoxicillin 2g 50 mg/kg
Unable to take oral Ampicillin 2 g IV or IM 50 mg/kg IV or IM
or
Cefazoline 1 g IV or IM 50 mg/kg IV or IM
Or Ceftriazone
Allergic to Penicillin Cephalexin* 2g 50 mg/kg
or
Clindamycin 600 mg 20 mg/kg
or
Axithromycin 500 mg 15 mg/kg
Allergic to Penicillin Clindamycin 600 mg IM or IV 20 mg/kg IM or IV
Unable to take oral or
Cefazolin 1 g IM or IV 50 mg/kg IM or IV
PMPH_Eversole_Appendices.indd 694 1/17/2011 3:56:47 PM
Appendices 695
II. ANTIBIOTICS (INFECTIONS)
Penicillin VK 500 mg
Dsp #40
Sig: 1 cap every 6 hours
Use: Odontogenic infections (i.e., abscess cellulitis), acute necrotizing ulcerative
gingivitis with fever, oral gonorrhea
Amoxycillin 500mg/Clavulanic acid 125 mg
Dsp #30
Sig: 1 or each three times per day with snack or meal.
Use: Odontogenic infections
Erythromycin stearate 500 mg
Dsp #40
Sig: 1 cap every 6 hours
Use: Odontogenic infections in the patient allergic to penicillin
Ciprofloxacin 500 mg
Dsp #20
Sig: one tablet twice a day
Use: Odontogenic infections, cellulitis
Caution: may cause tendonitis and rupture several months after use, do not use
if taking steroids
Dicloxacillin 150 mg
Dsp #40
Sig: 2 caps every 6 hours
Use: Possible drug of choice when penicillin is ineffective in 48 hours. Effective for
staphylococci or penicillinase-secreting organisms.
Clindamycin 150 mg
Dsp #40
Sig: 2 caps every 6 hours
Use: Most effective against bacteroides infections.
Caution: May cause clostridia pseudomembranous ulcerative colitis.
Cephalexin 250 mg
Dsp #40
Sig: 1 cap every 6 hours
Use: Possible drug of choice when penicillin is ineffective in 48 hours. Often inef-
fective for penicillinase-secreting organisms.
Tetracycline oral suspension 250 mg/tsp
Dsp 4 oz
Sig: 1 tsp 4 times daily, rinse orally for 5 minutes and swallow
Use: Minor and major aphthous stomatitis
III. ANTIFUNGALS
Nystatin ointment
Dsp 30 g
Sig: Apply to affected area 4 times daily
Use: Denture-related candidiasis, angular cheilitis
PMPH_Eversole_Appendices.indd 695 1/17/2011 3:56:47 PM
696 Appendices
Nystatin pastilles 200,000 U
Dsp #80
Sig: 2 tabs every 6 hours orally as lozenge
Use: Oral candidiasis
Clotrimazole troches 10 mg
Dsp #40
Sig: 1 tablet every 6 hours orally as lozenge
Use: Oral candidiasis
Ketoconazole (Nizoral) 200 mg
Dsp #10
Sig: 1 tab per day
Use: Oral candidiasis
Fluconazole 100 mg
Dsp #11
Sig: 2 tabs initial dose, 1 tab per day thereafter
Use: Oral candidiasis in HIV seropositive patients
IV. ANTIHISTAMINES AND TOPICAL ANESTHETICS
Diphenhydramine HCl (Benadryl) 50 mg
Dsp #20
Sig: 1 cap 3 times daily
Use: Allergic stomatitis of the immediate type, erythema multiforme
Promethazine (Phenergan) 12.5 mg
Dsp #20
Sig: 1 cap 3 times daily
Use: Allergic stomatitis of the immediate type, erythema multiforme
Diphenhydramine HCl (Benadryl) elixir 12.5 mg/tsp 50:50 with Kaopectate
Dsp 6 oz
Sig: 2 tsp as oral rinse 3 times daily
Use: Palliation of painful vesiculoulcerative lesions
Promethazine (Phenergan) syrup 6.25 mg/tsp 50:50 with Kaopectate
Dsp 6 oz
Sig: 2 tsp as oral rinse 3 times daily
Use: Palliation of painful vesiculoulcerative lesions
2% Xylocaine viscous
Dsp 4 oz
Sig: 3 drops with fingertip to oral sores p.r.n. for pain
Use: Palliation of painful vesiculoulcerative lesions
Caution: Instruct patient not to swallow medication to avoid anesthetizing gag
reflex
V. STEROID AND OTHER ANTI-INFLAMMATORY
PREPARATIONS
0.1% Triamcinolone in Orabase
Dsp 5-g tube
PMPH_Eversole_Appendices.indd 696 1/17/2011 3:56:47 PM
Appendices 697
Sig: Apply to oral sores 4 times daily
Use: Erosive lichen planus, bullous pemphigoid, oral lesions of pemphigus vul-
garis, contact (delayed) allergic stomatitis
0.05% fluocinonide (Lidex) ointment
Dsp 30 g
Sig: Apply to oral lesions 6 times daily
Use: Erosive lichen planus, bullous pemphigoid, pemphigus vulgaris, contact
(delayed) allergic stomatitis
0.05% Clobetasol proprionate ointment (Temovate)
Dsp 30 g
Sig: Apply to oral lesions 6 times daily
Use: Erosive lichen planus, bullous pemphigoid, pemphigus vulgaris, contact
(delayed) allergic stomatitis
Dexamethasone elixir 0.5 mg per 5 ml (Decadron)
Dsp 8 oz
Sig: 1–2 tsp as an oral rinse, expectorate.
Use: Minor aphthous ulcers, other erosive stomatitides
Dapsone 25 mg
Dsp #30
Sig: 1 tab daily for 3 days, then 2 tabs daily for 3 days, then 3 tabs daily for 3 days,
followed by 2 tabs twice daily for 3 days
Use: Benign mucous membrane pemphigoid. Maintenance dose after accelerated
schedule is between 100 and 150 mg daily.
Caution: Dapsone may cause hemolysis; red cell counts, hemoglobin, and hemat-
ocrit should be obtained regularly.
Prednisone 5 mg or dexamethasone 0.75 mg
Dsp #40
Sig: 1 tab every 6 hours for 7 days, followed by 1 tab every 12 hours for 4 days,
followed by 1/2 tab every 12 hours for 3 days
Use: Severe erosive lichen planus, major aphthous stomatitis, benign mucous
membrane pemphigoid, erythema multiforme
Caution: Do not prescribe for patients with existing infectious disease or diabetes
mellitus
Methylprednisolone Dosepak
Dsp 2 packs
Sig: Take as directed, doubling the dose (i.e.: using the two packs simultaneously
Use: Severe erosive lichen planus, major aphthous stomatitis, benign mucous
membrane pemphigoid, erythema multiforme
Caution: Do not prescribe for patients with existing infectious disease or diabetes
mellitus
Tacrolimus 0.1%
Dsp 30 g
Sig: Apply to mouth sores four times daily
Use: Erosive lichen planus, major aphthous stomatitis, benign mucous membrane
pemphigoid, erythema multiforme
Cyclosporin oral solution. 100mg/1ml
Dsp: 50 ml
PMPH_Eversole_Appendices.indd 697 1/17/2011 3:56:47 PM
698 Appendices
Sig: ½ tsp, coat lining of mouth four times daily
Use: Erosive lichen planus, major aphthous stomatitis, benign mucous membrane
pemphigoid, erythema multiforme
VI. ANTIVIRAL AGENTS
5% Acyclovir ointment
Dsp 15 g
Sig: Apply to lip sores 6 times daily
Use: Herpes labialis. Recommend application during onset of prodromal par-
esthesia if possible; otherwise apply directly over vesicles.
Acyclovir 200 mg
Dsp #120
Sig: 1 cap 4 times daily
Use: Prevention of recurrent herpes simplex and herpes-related erythema
multiforme
Famciclovir 1 g
Dsp #60
Sig: 1g twice a day
Use: Prevention of recurrent herpes simplex and herpes-related erythema
multiforme
VII. MUSCLE RELAXANTS
Chlorzoxazone (Paraflex) 250 mg
Dsp #100
Sig: 2 tabs every 4 hours
Use: Myogenic facial pain, tension headache
Chlorzoxazone and acetominophen (Parafon Forte) 500 mg
Dsp #100
Sig: 2 tabs every 4 hours
Use: Myogenic facial pain, tension headache
Baclofen (Lioresal) 10 mg
Dsp #60
Sig: 1/2 tab 3 times daily for 3 days, then 1 tab 3 times daily for 3 days, then 1 1/2
tab 3 times daily
Use: Myogenic facial pain, tension headache
VIII. ANXIOLYTICS
Diazepam (Valium) 5 mg
Dsp #20
Sig: 1–2 tabs daily
Use: Tension reduction prior to appointments, myogenic facial pain
Lorazepam (Ativan) 1 mg
PMPH_Eversole_Appendices.indd 698 1/17/2011 3:56:47 PM
Appendices 699
Dsp #20
Sig: 1 tab daily
Use: Tension reduction prior to appointments, myogenic facial pain
IX. ANTIDEPRESSANTS
Doxepin HCl (Sinequan) 25 mg
Dsp #45
Sig: 1 cap each evening for 5 days, then 2 caps each evening for 5 days, then 4 caps
each evening for 7 days
Use: Atypical facial pain of psychogenic origin and burning mouth syndrome,
most effective in depressed patients with anxiety. Dexamethasone suppres-
sion test advisable initially. Maintenance dose varies from 100–200 mg daily
Trazodone HCl (Desyrel) 50 mg
Dsp #70
Sig: 2 tabs each evening for 5 days, then 3 tabs each evening for 5 days, then 3 tabs
3 times daily for 7 days
Use: Atypical facial pain of psychogenic origin and burning mouth syndrome,
most effective in depressed patients. Dexamethasone suppression test advis-
able initially. Maintenance dose is 250–350 mg/day in divided doses.
Fluoxetine HCl 20 mg (Prozac)
Dsp #30
Sig: 1/2 cap daily
Use: Atypical facial pain of psychogenic origin and burning mouth syndrome,
most effective in depressed patients.
X. ANALGESICS
Aspirin 325 mg or Tylenol
Dsp: OTC
Sig: 2 tabs every 6 hours, p.r.n. pain
Use: Mild pain
Ibuprofen (Motrin) 600 mg
Dsp #20
Sig: 1 tab every 4 hours, p.r.n. pain
Use: Mild pain
ASA #2 (Codeine 15 mg)
_#3 (Codeine 30 mg)
_#4 (Codeine 60 mg)
Dsp #20
Sig: 1 tab every 4 hours, p.r.n. pain
Use: Mild to moderate pain
Oxycodone HCl (Percodan or Percocet)
Dsp #20
Sig: 1 tab every 4 hours, p.r.n. pain
Use: Moderate pain
PMPH_Eversole_Appendices.indd 699 1/17/2011 3:56:47 PM
700 Appendices
Meperidine HCl (Demerol) 50 mg
Dsp #12
Sig: 1 tab every 4 hours, p.r.n. pain
Use: Severe pain
Hydromorphone HCl (Dilaudid) 2 mg
Dsp #12
Sig: 1 tab every 4 hours, p.r.n. pain
Use: Severe pain
Carbamazepine (Tegretol) 100 mg
Dsp #40
Sig: 1 tab 2 times daily for 2 days, then 1 tab 3 times daily
Use: Trigeminal and glossopharyngeal neuralgias. Most patients can be main-
tained on 400–800 mg per day.
Caution: While escalating, complete blood counts should be monitored regularly
as Tegretol induces a dose-related marrow suppression.
XI. VASOACTIVE DRUGS
Nifedipine 10 mg
Dsp #42
Sig: 1 cap twice daily
Use: Short-term therapy for cluster headache (sphenopalatine neuralgia)
Ergotamine tartrate and caffeine (Cafergot) suppositories
Dsp #10
Sig: Place 1 tab rectally at onset of pain attack
Use: Migraine headache, midface cluster headache, not to exceed 5 per week.
Caution: Contraindicated in gravid women; use cautiously in hypertensive
patients.
PMPH_Eversole_Appendices.indd 700 1/17/2011 3:56:47 PM
Index
Note: Page references followed by “f” and “t” denote figures and tables, respectively.
A differential diagnosis, 105
Abrasion, of tooth structure, 575, 575f gender predilection, 105
Acanthosis, 11–12, 16, 23, 29 microscopic features, 105
Acanthosis nigricans, 278 treatment, 105
of lips, 278f Acute otitis media, otogenic pain, 634–35
Accessory cusps and roots, 566–67, 567f clinical features, 634–35
Acinic cell carcinoma, 329–30 differential diagnosis, 635
of parotid, 329f treatment, 635
Actinic cheilitis, 15f Acute sialadenitis, 316–17
affected age group, 14 purulent drainage in, 317
clinical features, 14 Acute streptococcal or staphylococcal
differential diagnosis, 14 stomatitis, 106f
gender predilection, 14 age group affected, 106
microscopic features, 14 clinical features, 106
treatment, 14 differential diagnosis, 106
Actinic prurigo, 219f microscopic features, 106
age group affected, 219 treatment, 106
clinical features, 219 Acute suppurative sialadenitis
differential diagnosis, 219 sialogenic pain, 658–59
microscopic features, 219 clinical features, 658
treatment, 219 differential diagnosis, 658
Actinomyces, 123 treatment, 658
Actinomyces israelii, 122 Acyclovir, 140, 146–47
Actinomycosis, 122f, 306–7 Addison’s disease, 84, 87–88, 87f
age group affected, 122 age group affected, 87
clinical features, 122 clinical features, 87–88
differential diagnosis, 122 differential diagnosis, 88
gender predilection, 122 gender predilection, 87
microscopic features, 122 microscopic features, 88
swollen cervical fistula in, 306f treatment, 88
treatment, 122 Adenocarcinomas, 256f
Actinomycotic microorganisms, 122 age group affected, 255
Active juvenile fibrous dysplasia, 523 clinical features, 255–56
Acute erythematous pharyngitis, 68f differential diagnosis, 256
Acute infectious arthritides, TMJ, 651–52 microscopic features, 256
Acute necrotizing ulcerative gingivitis treatment, 256
(ANUG), 96, 105f Adenocarcinomas NOS. See
age group affected, 105 Adenocarcinomas not otherwise
clinical features, 105 specified (NOS)
PMPH_Eversole_Index.indd 701 1/17/2011 3:57:40 PM
702 Index
Adenocarcinomas not otherwise specified Langerhans cell histiocytosis, 403–5
(NOS), 259f, 330–31, 330f clinical and radiographic features, 403–4
age group affected, 259 microscopic features, 404
clinical features, 259 treatment of, 405
differential diagnosis, 259 leukemia, 406–7
microscopic features, 259 Papillon-Lefevre syndrome, 401–2
treatment, 259 premature, 400f
Adenoid cystic carcinoma, 257f, 326–27 vanishing bone disease, 402–3, 403f
age group affected, 256 Amalgam and graphite tattoo, 77f
clinical features, 256–57 clinical features, 77
differential diagnosis, 257 differential diagnosis, 78
microscopic features, 257 microscopic features, 78
of parotid gland, 326f treatment, 78
treatment, 257 Ameloblastic fibrodentinoma, 496, 496f
Adenomatous hyperplasia, 208f, 253f Ameloblastic fibroma, 419–20, 419f
age group affected, 207, 252 Ameloblastic fibroodontoma, 497–98, 497f
clinical features, 207–8, 252 Ameloblastoma, 360f, 432–33
differential diagnosis, 208, 252 rising from large dentigerous cyst, 415f
gender predilection, 252 root divergence and resorption in, 432f
microscopic features, 208, 252 unicystic, 414–16
treatment, 208, 253 Amelogenesis imperfecta, 582–84, 583f
Adenomatous polyposis (APC) gene hypomaturation/hypocalcification forms,
in Gardner’s syndrome, 564 584–85, 584f
Adenosine triphosphate (ATP) calcium trans- hypoplastic forms of, 582–84, 583f
port proteins (ATP2A2), 27 Amelo-onychohypohidrotic syndrome, 586
Adjunct chemotherapy, 191 Amphotericin B, 132
Adjunct radiation, 256 Amyloidosis
Adnexal skin tumors, 347–48, 348f age group affected, 246
Aggressive juvenile ossifying fibroma, 490, 491f amyloid nodules of tongue, 247f
Agranulocytosis, 96, 98, 102 clinical features, 246–47
clinical features, 100–101 differential diagnosis, 247
differential diagnosis, 101 microscopic features, 247
immunosuppressive medications, 100 multiple tongue nodules in, 291f
microscopic features, 101 treatment, 247
treatment, 101 Anatomic localization, of tumefaction, 299
AIDS prodrome, 39 Aneurysmal bone cyst, 429–30, 430f
AIDS therapy, 73 Aneurysms, 616
Albright’s syndrome, 521 clinical features, 616
Allergic fungal sinusitis, 508–9 differential diagnosis, 616
showing bony invasion and expansion, 508f frontal area pain in, 616f
Allergic mucositis, 67, 69 treatment, 616
foreign body gingivitis, 63f Angina bullosa hemorrhagica, 159f
clinical features, 63 age group affected, 158
differential diagnosis, 64 clinical features, 158–59
microscopic features, 63–64 differential diagnosis, 159
treatment, 64 treatment, 159
Alveolar bone loss, 101, 365, 398–407 Angioneurotic edema, 218f, 356–57
chronic periodontitis, 398–99, 399f clinical features, 218
cyclic neutropenia, 405–6 differential diagnosis, 218
diabetic periodontitis, 400–401 diffuse soft swelling of lips in, 357f
juvenile periodontitis, 401–2, 401f treatment, 218–19
PMPH_Eversole_Index.indd 702 1/17/2011 3:57:40 PM
Index 703
Angular cheilitis, 119f invasive mycoses, 506–7
age group affected, 119 inverting papilloma, 516–17, 516f
clinical features, 119 maxillary sinusitis, 500–502, 501f
differential diagnosis, 119 odontogenic tumors, 512–13, 513f
microscopic features, 119 osteomas and exostoses, 513–14
treatment, 119 silent sinus syndrome, 520, 520f
Ankylosis sinus mucocele, 503–4, 504f
clinical features, 671–72 Antrolith, 511–12
treatment, 672 represent dystrophic calcifications, 512f
Anodontia, partial, 29 Aphthous stomatitis, 100
Anorexia, 88 age group affected, 96
Anorexia nervosa/bulimia, lingual erosion, 576f clinical features, 96–97
Antecedent trauma, 79 differential diagnosis, 97
Antibiotic therapy, 124, 200, 237 major, 97–98
Anti-DNA antibody, 62 microscopic features, 97
Antifungal medication, 52 treatment, 97
Antihistamines, 149 Aphthous ulcers, 96, 98f
Antihistaminic expectorant, 67 Apical periodontitis, 366–67
Antihistaminic mouth rinse, 45 associated with nonvital teeth, 366f
Antihistaminic oral suspension, 104 laterally displaced, 384
Antinuclear antibody, 62 Apical radiodensities, and focal sclerosing
Antipyretics, 141 osteomyelitis, 479f
Antistreptolysin-O titers, 68 Aspergillus mycetoma, 507–8, 507f
Antiviral therapy, 145 Aspirin, 140
Antral carcinoma, 517–18 Atrophic erythematous glossitis, 59
clinical features, 132 Atrophic glossitis, 58f, 68
differential diagnosis, 133 age group affected, 58
gender predilection, 132 clinical features, 58–59
microscopic features, 133 differential diagnosis, 59
treatment, 133 microscopic features, 59
Antral invasive mycoses, 506–7 treatment, 59
Antral neoplasms Atrophic lichen planus, 68–70, 69f
maxillary division pain and, 620–21 age group affected, 68
clinical features, 620 clinical features, 68–69
differential diagnosis, 620–21 differential diagnosis, 69
treatment, 621 gender predilection, 68
with palatal bone perforation, 621f microscopic features, 69
Antral opacities, 500–520 treatment, 70
allergic fungal sinusitis, 508–9 Atrophic nail changes, 17
showing bony invasion and expansion, 508f Attrition. See Physiologic tooth wear
antral carcinoma, 517–18 Atypia, 55
antral sarcoma, 519–20 Atypical facial pain, 628–29
antrolith/rhinolith, 511–12 clinical features, 628
represent dystrophic calcifications, 512f differential diagnosis, 628–29
augmentation materials, 510–11 treatment, 69
benign mesenchymal neoplasms, 515–16, 515f Atypical histiocytic granuloma, 110, 112f
displaced teeth, roots, and foreign bodies, age group affected, 112
509–10 clinical features, 112
fungus ball, 507–8, 507f differential diagnosis, 113
inflammatory polyps and, 502–3, 502f microscopic features, 112–13
periapical infection with, 504–6 treatment, 113
PMPH_Eversole_Index.indd 703 1/17/2011 3:57:41 PM
704 Index
Atypical lymphoproliferative disease, 260f endemic parotitis, 332, 332f
age group affected, 259 Heerfordt’s syndrome, 335–36
clinical features, 259–60 HIV salivary disease, 337–38
differential diagnosis, 261 metabolic sialadenosis, 339–40
microscopic features, 260–61 associated with diabetes, 340f
treatment, 261 Mikulicz’s disease, 334–35, 334f
Atypical verrucous hyperplasia (AVH), 32 sarcoid sialadenitis, 335–36
Augmentation materials, and antral opacities, Sjögren’s syndrome, 333–34, 333f
510–11 tuberculosis and, 336–37
Auriculotemporal syndrome, 678 Biliary atresia, 604–5
Azathioprine, 128, 151 bilirubin pigment, 605f
clinical features, 604
B differential diagnosis, 604
Bacitracin, 149 treatment, 604
Bartonella henselea, 305 Biopsy, 6, 10, 12–13, 22, 27, 32, 38, 44, 46, 54, 56,
Basal cell adenoma, 231f 64, 69–70, 89, 112–13, 115, 117, 121–22,
of parotid gland, 325f 219, 222, 230, 248, 1101
Basal cell carcinoma, 348–49 actinic cheilitis, 14
of face with central ulceration, 349f Bisphosphonate-related osteonecrosis of the
Basal cells, pleomorphism of, 14 jaws (BRONJ), 133f
B-complex deficiency, 58f age group affected, 133
Bednar’s aphthae, 110 clinical features, 133–34
Behçet’s syndrome, 97, 99f, 102 differential diagnosis, 134
age group affected, 99 inter-radicular radiopacities, 484–85, 485f
clinical features, 99 microscopic features, 134
differential diagnosis, 99 moth-eaten radiolucencies, 446–48, 447f
gender predilection, 99 clinical and radiologic features, 446–47
microscopic features, 99 microscopic features, 447
treatment, 99 treatment of, 448
Benign cementoblastoma, 370f, 371–72 treatment, 134
expansile lesions encompassing roots and, Blanching, 54
482f Blandin-Nuhn glands, 238–39, 239f
periapical radiopacities in, 481 Blastomycosis, 115
Benign leukoplakias, 13, 21 Blood chemistries, 4
Benign lymphoepithelial lesion. See Mikulicz’s Blood dyscrasia, 79
disease Blue sclera, 589f
Benign mesenchymal neoplasms BMMP. See Benign mucous membrane pemphi-
antral opacities, 515–16, 515f goid (BMMP)
Benign mesenchymal tumors, 309–10 Bohn’s nodules
Benign mucous membrane pemphigoid age group affected, 41
(BMMP), 64, 153f, 162 clinical features, 41
age group affected, 152 differential diagnosis, 42
clinical features, 152–53 microscopic features, 41–42
differential diagnosis, 153 treatment, 42
gender predilection, 152 Bone cavitation, idiopathic, 620f
treatment, 153 Bone lesions, 359–60
Benign nevi, with smooth borders, 345f enlargement of jaws due to underlying, 360f
Benign osteoblastoma, 492–93, 492f Botryoid odontogenic cyst, 424f, 425
Bilateral parotid and submandibular swellings, Branchial cleft cyst, 300, 300f
332–40 BRONJ. See Bisphosphonate-related osteone-
dysgenetic cysts of parotid, 338–39 crosis of the jaws (BRONJ)
PMPH_Eversole_Index.indd 704 1/17/2011 3:57:41 PM
Index 705
Buccal cyst, 379 microscopic features, 46, 66
Buccal mucosa, 12 of oral mucosa, 28
in focal epithelial hyperplasia, 286f treatment, 46, 66
Buccal mucosal carcinoma, 230 Carbamazepine, for superior laryngeal neural-
Bullae, 69 gia, 641
Bullous/desquamative diseases, 64–65, 65f Carcinoma in situ, 12
clinical features, 64 clinical features, 19–20
microscopic features, 65 differential diagnosis, 21
treatment, 65 microscopic features, 20–21
Bullous lesions, 69 treatment, 21
Bullous lichen planus, 154f Carcinoma-in-situ lesions, 44
age group affected, 154 Carcinoma of antrum, 262f
clinical features, 154 age group affected, 262
differential diagnosis, 154 clinical features, 262
gender predilection, 154 differential diagnosis, 262
microscopic features, 154 gender predilection, 262
treatment, 154–55 microscopic features, 262
Bullous pemphigoid, 151f treatment, 262
age group affected, 151 Carcinomatous change, in branchial cleft cyst,
clinical features, 151–52 300
differential diagnosis, 152 Cardiogenic facial pain, 634
microscopic features, 152 clinical features, 634
treatment, 152 differential diagnosis, 634
Burkitt’s lymphoma, 457–58 treatment, 634
diffuse, destructive lesion in, 457f Carotid body tumor, 311–12
causing large tumefaction, 311f
C embolization in, 312
Café-au-lait pigmentation, 86f, 87 Carotidynia, and neck and throat pain, 640–41
Caffey’s disease, 537 Caseous necrosis, 115
Calbicans species, 46 in tuberculous lymphadenitis, 304
Calcific metamorphosis, of pulp, 595 Cat-scratch fever, 305
Calcified lymph nodes cervical lymphadenopathy in, 305f
superimposed soft tissue radiopacities, Causalgia, 625–26
551–52, 552f Cause-and-effect relationship, 6, 11
Calcified stylohyoid ligament, 639f CD1a, 195
Calcifying cystic odontogenic tumor, 388–89, 389f Celiac disease, 100
Calcifying epithelial odontogenic tumor, 416f, Cellular atypia, 12
417 Cellulitis, 354–55
irregular, Ill-defined expansile radiopacities, odontogenic infection represents, 355f
542–43, 543f Central arteriovenous malformation, 436–37
pericoronal radiopacities, 494–95, 495f angiograms of, 437f
Pindborg tumor in, 543 Central giant cell granuloma, 380, 397, 428f, 429
Candida hyphae, 39, 52, 60 root divergence with, 398f
Candida infection, 46, 61 with root resorption, 381f
Candida mycelia, 26 Central hemangioma of bone, 437–38
Candida organisms, 52 Central mucoepidermoid carcinoma, 421–525
Candidiasis, 10, 45, 62, 65–66, 66f arising from lining of dentigerous cyst, 422f
age group affected, 45, 65 clinical and radiographic features, 421–22
clinical features, 45–46, 65–66 differential diagnosis, 423
differential diagnosis, 46, 66 microscopic features, 422–23
erythematous, 66 treatment of, 423
PMPH_Eversole_Index.indd 705 1/17/2011 3:57:41 PM
706 Index
Central neurogenic neoplasms, 434–35, 435f Chemodectoma. See Carotid body tumor
Central ossifying fibromas, 393–94, 393f Chemotherapy, 195, 256
inter-radicular radiopacities, 489–92 Cherubism, 427–28, 427f
clinical and radiographic features, 489–91 Chief complaint, 2
differential diagnosis, 491–92 Chlorhexidine rinses, 60–61
initiate root divergence/resorption, 490f Chondroectodermal dysplasia
microscopic features, 491 hypodontia in, 562f
treatment of, 492 missing teeth, 561–62
Cervical lymphadenitis, 302 Chondrogenic sarcoma
Cervical lymphadenopathy, in cat-scratch fever, irregular, Ill-defined expansile radiopacities,
305f 545
Cervical lymph nodes, and sinus histiocytosis, Chondrosarcoma, 453–54
308f Chromosome Xq28 IP, 29
Cervical nodes Chronic fatigue syndrome, 303
metastatic carcinoma in, 313f Chronic illnesses, 7
tuberculous lymphadenopathy of, 304f Chronic irritational habits, 11
Cervical rib and transverse process, 301, 301f Chronic otitis media, otogenic pain
Cervical vertebrae, 301f clinical features, 635–36
Chancre (primary syphilitic), 116f differential diagnosis, 636
age group affected, 115 treatment, 636
clinical features, 115–16 tympanic membrane in, 636f
differential diagnosis, 116 Chronic parotitis, with bacterial infection, 319f
microscopic features, 116 Chronic periodontitis, 398–99, 399f
treatment, 116 Chronic sialadenitis, 318–19
Cheek and tongue bite keratosis, 31f Chronic ulcerative stomatitis, 107f, 166f
age onset, 30 age group affected, 107, 165
clinical features, 30 clinical features, 107, 165–66
differential diagnosis, 30 differential diagnosis, 107, 166
microscopic features, 30 microscopic features, 107, 166
treatment, 30 treatment, 107, 166
Cheek- or lip-biting, 11 Clear-cell odontogenic tumor, 453f
Cheilitis glandularis, 217f Cleidocranial dysplasia
age group affected, 217 multiple impactions in, 564f
clinical features, 217 supernumerary teeth, 563–64, 564f
differential diagnosis, 217 Clobetasol (Temovate) ointment, 164
gender predilection, 217 Clotrimazole troches, 60
microscopic features, 217 Clotting factor deficiencies, 50
treatment, 217–18 Clouded sinuses, in chronic maxillary sinus-
Cheilitis granulomatosa, 216f itis, 618f
age group affected, 216 Cluster headache, 621–22
clinical features, 216 clinical features, 621–22
differential diagnosis, 216 differential diagnosis, 622
gender predilection, 216 treatment, 622
microscopic features, 216 vessels involved in vasodilation, 622f
treatment, 216–17 CNS neoplasms
Chemical burns, 51, 54 clinical features, 626–28
aspirin, 45f differential diagnosis, 627–28
clinical features, 44 maxillary division pain and, 626–27, 627f
differential diagnosis, 45 treatment, 628
microscopic features, 44–45 Coccidiodomycosis, 115
treatment, 45 Collagen-vascular immunopathic diseases, 38
PMPH_Eversole_Index.indd 706 1/17/2011 3:57:41 PM
Index 707
Commissural pits, 118f Conversion trismus
age of onset, 117 clinical features, 671
clinical features, 117 differential diagnosis, 671
differential diagnosis, 118 treatment, 671
Communication skills of interrogation, 2 Coronal fracture, 600–601
Complex regional pain syndrome, 625–26 clinical features, 600
clinical features, 625 differential diagnosis, 600
differential diagnosis, 625–26 incisal trauma with, 600f
Horner’s syndrome and, 626f treatment, 600–601
treatment, 626 Coronoid hyperplasia, 673
Compound complex odontoma, 489 Corps ronds, 27
Compound composite odontoma, 489 Cortical hyperostosis, generalized, 538
Computed tomography, of invasive myofibro- Cortical redundancies, 536–42
sarcoma, 459f cortical hyperostosis, generalized, 538
Concrescence, 573–74 Garré’s periostitis, 536–37
in molar teeth, 573f juxtacortical osteogenic sarcoma, 539–40
Condylar fracture, TMJ region pain, 653–54, 653f mandibular tori and exostoses, 541, 542f
clinical features, 653–54 osteoid osteoma, 540–41
differential diagnosis, 654 Cosmetic surgery, 54
treatment, 654 Cowden’s disease. See Multiple hamartoma
Condylar hyperplasia, 673–74, 674f syndrome
clinical features, 673–74 Coxsackie virus, 67
differential diagnosis, 674 Coxsackie virus infection, 284f
treatment, 674 Cranial base
Condyloma acuminatum, 269–70, 269f maxillary division pain and, 626–27, 627f
Cone beam CT, 4 Cranial base chondrosarcoma, CT scan of, 627f
Congenital cysts, 42f Crateriform papules, multiple, 283f
Congenital epulis Crohn’s disease, 166, 222f, 288–89
age of onset, 185 age group affected, 221
clinical features, 185–86 clinical features, 221–22
differential diagnosis, 186 differential diagnosis, 222
gender predilection, 185 microscopic features, 222
microscopic features, 186 multiple polypoid tumefactions, 289f
treatment, 186 polypoid masses in, 289
Congenital facial diplegia, 683 treatment, 222
Congenital lip pits, 118f Cryosurgery, 13, 44
age of onset, 118 Cryptococcosis, 115
clinical features, 118 Cushing’s syndrome, 88, 357
differential diagnosis, 118 with diffuse facial edema, 358f
gender predilection, 118 with loss of trabecular markings, 467f
treatment, 118 Cutaneous fistula, tuberculous granulomas in,
Congenital syphilis, 580 337f
screwdriver centrals and mulberry molars Cutaneous scaly papules, 285f
in, 580f Cyclic neutropenia, 102, 405–6
Conjunctivitis, recurrent, 99 age group affected, 101
Connexin 43 gene, 586 clinical features, 101–2
Contact vesicular stomatitis, 148f differential diagnosis, 102
clinical features, 148 microscopic features, 102
differential diagnosis, 148–49 treatment, 102
microscopic features, 148 Cyclophosphamide, 128
treatment, 149 and prednisone combined therapy, 199
PMPH_Eversole_Index.indd 707 1/17/2011 3:57:41 PM
708 Index
Cyclosporine, 37 hypomaturation/hypocalcification forms,
Cystic hygroma, 310–11 584–85, 584f
of neck in infant, 310f hypoplastic forms of, 582–84, 583f
Cystic parotid swelling, in HIV sialadenitis, congenital syphilis, 580, 580f
338f coronal fracture, 600–601
Cyst of incisive papilla, 251f dental caries, 577–78, 578f
age group affected, 251 dental fluorosis, 581, 581f
clinical features, 251 denticles and pulp calcification, 595
differential diagnosis, 251 dentin dysplasia type I, 589–90, 590f
microscopic features, 251 dentin dysplasia type II, 590–91, 591f
treatment, 251 dentinogenesis imperfecta, 587–88, 587f
Cystogenic carcinoma, 449–50 enamel hypoplasia, 579
Cytologic atypia, 14, 16 external root resorption, 598–99, 598f
hypophosphatasia, 593, 593f
D internal resorption, 597–98, 597f
Dapsone, 153 osteogenesis imperfecta, 588–89, 589f
Darier-White’s disease, 26–27, 42 regional odontodysplasia, 591–92
Decadron oral rinses, 164 segmental odontomaxillary dysplasia,
Definitive diagnosis, 6–7 595–96, 596f
Degenerative joint disease, 649–50, 649f snow-capped teeth, 582, 582f
Dens evaginatus, 567f subcervical resorption, 599–600, 599f
Dens invaginatus, 570, 570f syndrome-associated enamel defects, 585–86
Dental caries, 577–78, 578f vitamin d refractory rickets, 593–94, 594f
Streptococcus mutans in, 577 Dental transposition, 567–68
Dental changes, 3 of lateral incisor and canine, 568f
Dental history, 3–4 Denticles and pulp calcification, 595
Dental lamina cysts, 294–95 Dentigerous cyst, 411–12, 412f
age group affected, 41 ameloblastoma rising from large, 415f
clinical features, 41 Dentin dysplasia type I, 589–90, 590f
differential diagnosis, 42 Dentin dysplasia type II, 590–91, 591f
microscopic features, 41–42 Dentinogenesis imperfecta, 587–88
multiple alveolar ridge papules in neonate, with opalescent teeth, 587f
295f Dermal macrophages, 29
treatment, 42 Dermatitis herpetiformis (gluten enteropathy),
Dental morphology, alterations in, 565–77 161f
abrasion of tooth structure, 575, 575f age group affected, 161
accessory cusps and roots, 566–67, 567f clinical features, 161
concrescence, 573–74, 573f differential diagnosis, 161
dens invaginatus, 570, 570f gender predilection, 161
dental transposition, 567–68, 568f microscopic features, 161
dilaceration, 568–69, 569f treatment, 161
enamel pearls, 568, 569f Dermatofibrosaracoma protuberans, 352f
erosion of tooth structure, 575–76, 576f Dermoid cyst, 343–44, 344f
fusion, 572–73, 573f Desmoplastic ameloblastom
gemination, 571–72, 572f with benign fibroosseous-like pattern, 544f
hypercementosis, 576–77, 577f irregular, Ill-defined expansile radiopacities,
microdontia and macrodontia, 565–66, 566f 543–44
physiologic tooth wear, 574, 574f Desquamation, 45
taurodontism, 571, 571f Developmental oral sinuses, 124f
Dental structure, alterations in, 577–601 age of onset, 124
amelogenesis imperfecta, 582–85 clinical features, 124–25
PMPH_Eversole_Index.indd 708 1/17/2011 3:57:41 PM
Index 709
differential diagnosis, 125 chronic ulcerative stomatitis, 166
Developmental white lesions, 10 commissural pits, 118
Diabetes, metabolic sialadenosis associated congenital epulis, 186
with, 340f congenital lip pits, 118
Diabetes (juvenile, type I) Crohn’s disease, 222
age group affected, 199 cyclic neutropenia, 102
clinical features, 199–200 cyst of incisive papilla, 251
differential diagnosis, 200 dental lamina cysts, 42
hyperplastic gingivitis with abscess forma- developmental oral sinuses, 125
tion in, 200f diabetes (juvenile, type I), 200
microscopic features, 200 disontogenic cysts, 204
treatment, 200 drug-induced pigmentation, 91–92
Diabetic periodontitis, 400–401 dyskeratosis congenita, 17
Diarrhea, 88 dysplasia, 21
Differential diagnosis, 5–7, 168f ecchymosis and clotting factor deficiencies,
actinic cheilitis, 14 70
actinic prurigo, 219 ectomesenchymal chondromyxoid tumor
actinomycosis, 122 (ECT), 245
acute necrotizing ulcerative gingivitis ectopic lingual thyroid, 234
(ANUG), 105 epidermolyis bullosa (EB), 160
Addison’s disease, 88 Epstein’s pearls, 42
adenocarcinomas, 256 epulis fissurata, 185
adenocarcinomas, not otherwise specified erythema migrans (migratory stomatitis), 58
(NOS), 259 erythema multiforme, 155
adenomatous hyperplasia, 252 extranodal NK/T-cell lymphomas, 128
adenomatous or adenomatoid hyperplasia, factitial injury and trauma, 127
208 field cancerization, 71–72
agranulocytosis, 101 fissured (scrotal) tongue, 126
allergic mucositis, foreign body gingivitis, 64 Fordyce’s granules, 41
amyloidosis, 247 foreign body granuloma, 221
angina bullosa hemorrhagica, 159 geographic tongue (migratory glossitis), 57
angioneurotic edema, 218 giant cell fibroma, 178
angular cheilitis, 119 gingival cyst, 183–84
antral carcinoma, 133 gingivosis (desquamative gingivitis), 162
aphthous stomatitis, 97 granulomatous infection, specific, 248
atrophic glossitis, 59 granulomatous ulcer, specific, 115
atrophic lichen planus, 69 hairy tongue, 92
atypical histiocytic granuloma, 113 heavy metal ingestion, 90
Behçet’s syndrome, 99 hemangiomas, 53–54
bisphosphonate-related osteonecrosis of hematomas, 79
jaws, 134 hemochromatosis, 89
Bohn’s nodules, 42 hereditary benign intraepithelial dyskerato-
bullous pemphigoid, 152 sis, 26
candidiasis, 46, 66 herniated buccal fat pad, 226
carcinoma in situ, 21 herpangina, 141
carcinoma of antrum, 262 herpetic gingivostomatitis, 140
chancre (primary syphilitic), 116 HIV-associated hairy leukoplakia, 39
cheek and tongue bite keratosis, 30 HIV-associated oral pigmentation, 90
cheilitis glandularis, 217 HIV periodontitis and oral ulcerations, 109
cheilitis granulomatosa, 216 homogeneous leukoplakia, 12
chemical burns, 45 hyperplastic lingual tonsil, 236
PMPH_Eversole_Index.indd 709 1/17/2011 3:57:41 PM
710 Index
Differential diagnosis (Continued) polymorphous low-grade adenocarcinoma,
incontinentia pigmenti, 29 255
inflammatory fibrous hyperplasia, 220 proliferative verrucous leukoplakia (PVL), 32
juvenile spongiotic gingival hyperplasia, 180 puberty/pregnancy gingivitis, 201
Kaposi’s sarcoma, 73 pyogenic granuloma, 175
keratosis follicularis, 27 pyostomatitis vegetans, 167
Koplik spots of measles, 40 racial pigmentation, 84
langerhans cell histiocytosis (LCH), 195 radiation mucositis, 60
leukemia, 201 reactive lesions, 238
leukoedema, 24 reactive lymphoid hyperplasia, 227
lichenoid contact stomatitis, 165 recurrent herpes stomatitis, 145–46
lichen planus, 22, 35 retrocuspid papillae, 181
lingual abscess, 237 salivary gland tumors, 207
lingual cyst, 236 salivary neoplasms, 231–32
Ludwig’s angina, 210 sarcomas, 191, 246
lupus erythematosus, 38 scarlet fever, 68
lymphangiomas, 240 sialocysts, 214
lymphoepithelial cyst, 205 sialolithiasis, minor gland, 215
lymphonodular pharyngitis, 67 sialolithiasis with sialadenitis, 206
malignant melanoma, 83 smokeless tobacco keratoses, 16
median rhomboid glossitis, 233 soft tissue abscess, 124
mesenchymal neoplasms, 209, 225 speckled leukoplakia, 44
mesenchymal tumors, 187 squamous cell carcinoma, 21, 117, 189, 210,
metastatic carcinoma, 194 230
mucocele, 212 stomatitis nicotina, 42
mucoepidermoid carcinoma, 192, 258 suction petechiae, 74
mucous patches, 23 tertiary syphilis, 129
multiple neurofibromatosis, 87 thrombocyte disorders, 75–76
nasoalveolar (Klestadt) cyst, 215 thyroglossal duct cysts, 235
necrotizing sialometaplasia, 114 tobacco-associated leukoplakias, 12
neural sheath tumors, 242 toothpaste idiosyncratic lesions, 168
nevus, 80 torus mandibularis and exostoses, 182
non-Hodgkin’s lymphoma, 193 traumatic (amputation) neuroma, 224
nonspecific hyperplastic gingivitis, 198 traumatic granuloma with stromal eosino-
nonspecific (irritational) mucositis, 51 philia, 112
oral epithelium, carcinogenesis of, 21 uremic stomatitis, 103
oroantral fistula, 123 varices, 55
osseous or osteocartilaginous choristomas, verrucous carcinoma, 21, 34
244 Wegener’s granulomatosis, 127, 199
osteomyelitis, 120 white sponge nevus, 25
pachyonychia congenita, 28 xerostomic mucositis, 61
palatal abscess, 252 Diffuse and multifocal papillary lesions,
paraneoplastic pemphigus, 158 276–82
parulis, 174 acanthosis nigricans, 278
peripheral fibroma, 178 of lips, 278f
peripheral giant cell granuloma, 176–77 atypical verrucous leukoplakia, 278–79, 278f
peripheral odontogenic tumors, 188 focal dermal hypoplasia, 276
peripheral ossifying fibroma, 179 orolabial papillomas in, 277f
Peutz-Jeghers syndrome, 86 nevus unius lateris, 277
pigmented lichen planus, 84–85 unilateral extensive papillary proliferations
pleomorphic adenomas, 254 involving oral mucosa in, 277f
PMPH_Eversole_Index.indd 710 1/17/2011 3:57:41 PM
Index 711
papillary squamous cell carcinoma, 281–82 Disontogenic cysts, 204f
verrucous carcinoma, 280, 280f age group affected, 203
Diffuse antral opacification, 475 clinical features, 203
Diffuse facial edema, Cushing’s syndrome differential diagnosis, 204
with, 358f microscopic features, 203–4
Diffuse facial swellings, 354–61 treatment, 204
angioneurotic edema, 356–57 Displaced teeth
diffuse soft swelling of lips in, 357f antral opacities and, 509–10
bone lesions, 359–60 in sinuses, 509f
enlargement of jaws due to underlying, Downey cells, 75
360f Downey lymphocytes, atypical, 303
cellulitis and space infections, 354–55 Drug induced hyperplasia, 197f
Cushing’s syndrome, 357 clinical features, 196
with diffuse facial edema, 358f differential diagnosis, 196–97
emphysema, 355 microscopic features, 196
facial hemihypertrophy, 358–59, 359f treatment, 197
fibrous dysplasia, 359–60 Drug-induced pigmentation, 91–92
masseteric hypertrophy, 360–61, 361f clinical features, 91
Diffuse gingivitis, 50 differential diagnosis, 91–92
Diffuse infiltrative lymphocytosis syndrome, gender predilection, 91
337–38 microscopic features, 91
Diffuse papular and polypoid lesions, 282–95 treatment, 92
acute lymphonodular pharyngitis, 284 Duct blockage, with bacterial infection, 319f
oropharynx characteristic of, 284f Dysgenetic cysts, of parotid, 338–39
amyloidosis, 290–91 in adult, 339f
Crohn’s disease, 288–89, 289f Dyskeratosis congenita, 18f
dental lamina cysts, 294–95 age onset, 17
focal epithelial hyperplasia, 285–86 clinical features, 17
buccal mucosa characteristic of, 286f differential diagnosis, 17
granulomatous infections, specific, 289–90 microscopic features, 17
hemangioma/lymphangioma, 292–93 treatment, 17
hyalinosis cutis et mucosae, 291–92 Dysplasia, 7, 12, 14
keratosis follicularis, 284–85 clinical features, 19–20
multiple endocrine neoplasia, type IIb, differential diagnosis, 21
293–94 microscopic features, 20–21
multiple hamartoma syndrome, 286–87 treatment, 21
gingival papules in, 287f Dystrophic calcifications, antroliths represent,
papillary hyperplasia, 282–83 512f
pyostomatitis vegetans, 287–88
multiple papules and erosions, 288f E
stomatitis nicotina, 283–84 EB. See Epidermolyis bullosa (EB)
Diffuse pigmentations, 51 “Ebbing tide” effect, 16
Diffuse sclerosing osteomyelitis, 532 EBV molecular probe, 39
ground-glass radiopacities and chronic, 523 Ecchymosis, 50, 79
with osseous expansion, 524f Ecchymosis and clotting factor deficiencies, 70,
with periosteal onion skinning, 536f 71f
Diffuse soft swelling, of cheek, 356f clinical features, 70
Dilaceration, 568–69 differential diagnosis, 70
of roots, 569f microscopic features, 70
Diphenhydramine hydrochloride (Benadryl), 149 treatment, 70
Discomfort symptoms, 2 Ectodermal dysplasia, 561f
PMPH_Eversole_Index.indd 711 1/17/2011 3:57:41 PM
712 Index
Ectomesenchymal chondromyxoid tumor Episodic upset bowel symptoms, 100
(ECT), 245f Epithelial hyperplasia, 52
age group affected, 245 Epithelial odontogenic cyst, calcifying and
clinical features, 245 keratinizing, 486, 487f
differential diagnosis, 245 Epstein-Barr virus, 74, 303
microscopic features, 245 Epstein-Barr virus (EBV) DNA, 30
surgical excision, 245 Epstein’s pearls
treatment, 245 age group affected, 41
Ectopic lingual thyroid, 234f clinical features, 41
age group affected, 233 differential diagnosis, 42
clinical features, 233–34 microscopic features, 41–42
differential diagnosis, 234 treatment, 42
gender predilection, 233 Epulis fissurata, 185f
microscopic features, 234 age group affected, 185
treatment, 234 clinical features, 185
Elective palliative mouth rinses, 146 differential diagnosis, 185
Embolization, in carotid body tumors, 312 microscopic features, 185
Embryogenesis, 52 treatment, 185
Eminent interrogator, 2 Erosion, of tooth structure, 575–76, 576f
Emphysema, 355 Erosive lichen planus, 58, 72, 163f
Enamel hypoplasia, 420–21, 579 age group affected, 163
Enamel pearls, 568 clinical features, 163
molar teeth with, 569f differential diagnosis, 164
Encephalotrigeminal angiomatosis, 53 gender predilection, 163
Endemic parotitis, 332, 657f microscopic features, 163–64
showing diffuse parotid enlargement in treatment, 164
febrile child, 332f Eruption cyst, 184f
sialogenic pain, 657–58 age group affected, 184
clinical features, 657–58 clinical features, 184
differential diagnosis, 658 differential diagnosis, 184
treatment, 658 microscopic features, 184
Endodontic infection, 505f treatment, 184
laterally displaced, 384 Eruption/exfoliation of teeth, alterations in,
Enterococcus faecalis, 367 601–3
Enterovirus 71, 141 delayed eruption, 601–2
Enucleation, 225 impaction, 602
Eosinophilic myositis, 110 premature eruption, 601
Eosinophils, 64 premature exfoliation, 603
Ephelis Erythema migrans (migratory stomatitis), 57f,
clinical features, 81 64, 71
differential diagnosis, 82 age group affected, 57
microscopic features, 81–82 clinical features, 57–58
treatment, 82 differential diagnosis, 58
Epidermolyis bullosa (EB), 160f microscopic features, 58
age group affected, 159 treatment, 58
clinical features, 159–60 Erythema multiforme, 64, 67, 156f
differential diagnosis, 160 age group affected, 155
microscopic features, 160 clinical features, 155
treatment, 160 differential diagnosis, 155
Epilepsy, 29, 54 gender predilection, 155
Epimucous patch testing, 64 microscopic features, 155
PMPH_Eversole_Index.indd 712 1/17/2011 3:57:42 PM
Index 713
treatment, 155 seborrheic keratoses, 346–47
Erythemas of oral mucosa, 50 squamous cell carcinoma, 350
Erythematous candidiasis, 66, 72 Factitial injury and trauma
Erythematous macules, 68 clinical features, 126
Erythematous moniliasis, 58 differential diagnosis, 127
Erythroblastosis fetalis, 603–4 osseous destruction due, 126f
clinical features, 603–4 treatment, 127
differential diagnosis, 604 Familial fibrous dysplasia. See Cherubism
teeth in, 604f Familial gigantiform cementoma
Erythrogenic toxin, 67 multifocal confluent radiopacities, 534–35,
Erythromycin, 122 535f
Erythroplakia, 50, 55f Fanconi’s anemia, 19f
clinical features, 55 age onset, 18
differential diagnosis, 55–56 clinical features, 18
microscopic features, 55 differential diagnosis, 18
treatment, 56 microscopic features, 18
Erythroplakic precancerous lesions, 69 treatment, 18–19
Ewing’s sarcoma, 455, 455f Fibrinogen globular deposits, 69
Excisional biopsy, 221, 223 Fibrinous exudate, 22
Exostoses Fibrogenic sarcoma
antral opacities, 513–14 moth-eaten radiolucencies and, 458–59
cortical redundancies, 541, 542f Fibromatosis, with calcification, 307f
External root resorption, 598–99, 598f Fibromatosis gingivae, 195f
clinical features, 598–99 age of onset, 195
treatment of, 599 clinical features, 195–96
Extranodal NK/T-cell lymphomas, 128f differential diagnosis, 196
age group affected, 128 microscopic features, 196
clinical features, 128 treatment, 196
differential diagnosis, 128 Fibrosarcoma, 314f
gender predilection, 128 Fibrous dysplasia, 359–60, 360f, 442–43
microscopic features, 128 monostotic, 442f
treatment, 128 treatment of, 443
Extrinsic pigments, 50 Fibrous dysplasia, 475
Extrinsic staining, 608, 608f active juvenile, 523
ground-glass radiopacities, 521–23, 521f–522f
F Fibrous histiocytoma, of lateral neck, 307f
Facial enamel, idiopathic erosion of, 576f Field cancerization, 58, 71–72, 71f
Facial hemihypertrophy, 358–59, 359f age group affected, 71
Facial paralysis, localized motor deficits and, clinical features, 71
664f differential diagnosis, 71–72
clinical features, 664 gender predilection, 71
differential diagnosis, 665 microscopic features, 71
treatment, 665 treatment, 72
Facial skin, growths and swellings of, 344–54 Filiform papillae, 92
adnexal skin tumors, 347–48, 348f Fissured (scrotal) tongue, 125f
basal cell carcinoma, 348–49 age group affected, 125
keratoacanthoma, 351–52 clinical features, 125
malignant melanoma, 353–54, 353f differential diagnosis, 126
mesenchymal tumors, 352 gender predilection, 125
nevi, 344–45 microscopic features, 126
sebaceous cyst, 345–46 treatment, 126
PMPH_Eversole_Index.indd 713 1/17/2011 3:57:42 PM
714 Index
Flaccidness, 3 amalgam and graphite tattoo, 77–78
Flat macular superficial spreading lesions, 353f ephelis, 81–82
Florid osseous dysplasia hematomas, 79
Gardner’s syndrome, 533 mucoceles, 78–79
multifocal confluent radiopacities, 531–33, nevus, 80–81
532f oral melanotic macule, 81–82
Fluocinonide (Lidex) ointment, 153, 162, 164 Focal sclerosing osteomyelitis
Fluocinonide ointment, 70 periapical radiopacities, 479–80, 479f
Fluorescent treponemal antibody test, 23 Fordyce’s granules, 10
Fluorinated steroid gels, topical, 167 age group affected, 41
Fluorosis, dental, 581, 581f clinical features, 41
pigmentations, 606–7, 607f differential diagnosis, 41
5-fluorouracil cream, 14 histologic features, 41
Focal and umbilicated papules, 273–76 treatment, 41
keratoacanthoma, 273–74 Foreign body gingivitis, 63–64
of lip, 274f Foreign body granuloma
molluscum contagiosum, 275 clinical features, 220–21
multiple lesions, in HIV-infected patients, differential diagnosis, 221
276f microscopic features, 221
warty dyskeratoma, 274–75 treatment, 221
Focal cemento-osseous dysplasia, 369–70 Frank invasive carcinoma, 14
as apical radiolucent lesions in early stages, Frank squamous cell carcinoma, 20
369f Frictional benign keratoses
Focal cemento-osseous dysplasia clinical features, 11
opacities in edentulous areas, 483f differential diagnosis, 11–12
periapical radiopacities, 477–78, 478f due to irritation, 11f
Focal dental pigmentation, 609, 609f microscopic features, 11
Focal dermal hypoplasia, 276 treatment, 12
orolabial papillomas in, 277f Frictional keratosis, 16
Focal epithelial hyperplasia, 285–86 Frictional leukoplakias, 21
buccal mucosa characteristic of, 286f Frontal/ethmoidal sinusitis
Focal erythemas clinical features, 615
erythroplakia, 55–56 clouded, 615f
focal varix, 54–55 differential diagnosis, 615
hemangiomas, 53–54 treatment, 615
median rhomboid glossitis, 52 Functional changes, 2
nonspecific (irritational) mucositis, 51 Fungal infections, 114
Focal mucosal hemangiomas, 54 Fungus ball, 507–8, 507f
Focal papillary lesions, 267–73
condyloma acuminatum, 269–70, 269f G
giant cell fibroma, 272, 272f Gardner’s syndrome, 345, 533
papilloma, 267, 267f multifocal confluent radiopacities, 533–34, 534f
sialadenoma papilliferum, 271–72, 271f supernumerary teeth, 564–65, 565f
squamous acanthomas, 272, 272f Garré osteomyelitis, 360f
verruca vulgaris, 268, 268f Garré’s periostitis, 475
verruciform xanthoma, 270–71, 270f Cortical redundancies, 536–37
Focal periapical osteosclerosis Gemination, 571–72, 572f
idiopathic focal opacities without pulpal General health status, of patient, 3
insult, 480f Genokeratoses, 12, 38
periapical radiopacities, 480–81 hereditary benign intraepithelial
Focal pigmentations, 51 dyskeratosis, 26
PMPH_Eversole_Index.indd 714 1/17/2011 3:57:42 PM
Index 715
incontinentia pigmenti, 29 Gliadin-free diet, 100
keratosis follicularis, 27 Glossectomy, 246
pachyonychia congenita, 28 Glossopharyngeal neuralgia, 639–40
white sponge nevus, 24–25 Glossopyrosis, 633–34
Genomic assays, 4 clinical features, 633
Geographic tongue (migratory glossitis), 56f differential diagnosis, 633
age onset, 56 treatment, 633
clinical features, 56–57 Gluten enteropathy
differential diagnosis, 57 age group affected, 100
gender predilection, 56 clinical features, 100
microscopic features, 57 differential diagnosis, 100
treatment, 57 microscopic features, 100
Geotrichium, 46 treatment, 100
Ghost teeth, in regional odontodysplasia, 592f Gluten-free diet, 59
Giant cell arteritis, myogenic pain, 659–60 Goiter, 341–42
clinical features, 659–60 diffuse swelling in thyroid represents non-
differential diagnosis, 661 toxic, 342f
prominent artery in, 661f Graves’ disease and, 341
treatment, 661 Goltz syndrome. See Focal dermal hypoplasia
Giant cell fibroma, 178, 178f, 272, 272f Gonococcal stomatitis, 108f
age group affected, 178 age group affected, 107
differential diagnosis, 178 clinical features, 107–8
gender predilection, 178 differential diagnosis, 108
microscopic features, 178 microscopic features, 108
treatment, 178 treatment, 108
Giant cell granuloma, 73 Grains, 27
Gingiva, redness of, 50 Granular cell tumors, 242f
Gingival cyst, 183f clinical features, 242–43
age group affected, 183 differential diagnosis, 243
clinical features, 183 microscopic features, 243
differential diagnosis, 183–84 treatment, 243
microscopic features, 183 Granulomas, 384
treatment, 184 associated with nonvital teeth, 366f
Gingival papules Granulomatous infection, 289–90
in hyalinosis cutis et mucosae, 292f due to blastomycosis with cobblestone
in multiple hamartoma syndrome, 287f appearance, 290f
Gingivectomy, 196–97 specific, 247–48
Gingivosis (desquamative gingivitis), 162f age group affected, 247
age group affected, 161 clinical features, 247–48
clinical features, 161–62 differential diagnosis, 248
differential diagnosis, 162 microscopic features, 248
gender predilection, 161 treatment, 248
microscopic features, 162 Granulomatous inflammation, 110
treatment, 162 Granulomatous ulcer, specific, 114f
Glandular odontogenic cyst age group affected, 114
clinical and radiographic features, 425 clinical features, 114–15
expansile, loculated lucency representing, differential diagnosis, 115
426f microscopic features, 115
treatment of, 426 treatment, 115
Glandular odontogenic cyst Graves’ disease, 341
clinical and radiographic features, 425 with exophthalmos, 342f
PMPH_Eversole_Index.indd 715 1/17/2011 3:57:42 PM
716 Index
Ground-glass opacification, of alveolar bone, age onset, 53
525f clinical features, 53, 227–28, 239
Ground-glass radiopacities, 521–30 differential diagnosis, 53–54, 228, 240
chronic diffuse sclerosing osteomyelitis, 523, gender predilection, 53
524f low pressure central, 438f
fibrous dysplasia, 521–23 microscopic features, 53, 228, 239–40
ground-glass patterns in, 521f treatment, 54, 228–29, 240
mottled patterns in, 522f Hematogram, 59
hyperparathyroidism, 526–27 Hematomas, 79f
osteitis deformans, 524–26 clinical features, 79
osteopetrosis, 529 differential diagnosis, 79
opacification of teeth, 530f microscopic features, 79
segmental odontomaxillary dysplasia, treatment, 79
528–29, 528f Hemifacial atrophy, 683–84
Gummatous necrosis, 129 Hemimandibulectomy, for osteosarcoma, 454
Gustatory sweating, 678 Hemochromatosis, 88–89
age group affected, 88
H clinical features, 88–89
Hailey-Hailey disease, 27 differential diagnosis, 89
Hairy leukoplakia, 10 gender predilection, 88
Hairy tongue, 92–93 microscopic features, 89
age group affected, 92 treatment, 89
clinical features, 92 β-hemolytic streptococci, 67, 106
differential diagnosis, 92 Hemophilic pseudotumor, 439–40, 440f
gender predilection, 92 Hemorrhagic bone cyst. See Traumatic bone
microscopic features, 92 cyst
treatment, 92–93 Hemorrhagic sloughing lesions, 64
Hand-foot-and-mouth disease, 142f Hemosiderin pigment granules, 73
age group affected, 141 Hereditary benign intraepithelial dyskeratosis,
clinical features, 141–42 26f
differential diagnosis, 142 age onset, 26
microscopic features, 142 clinical features, 26
treatment, 142 differential diagnosis, 26
HBID. See Hereditary benign intraepithelial microscopic features, 26
dyskeratosis treatment, 26
Heavy metal ingestion, 90 Hereditary benign intraepithelial dyskeratosis
age group affected, 90 (HBID), 16
clinical features, 90 Hereditary ectodermal dysplasia
differential diagnosis, 90 missing teeth, 560–61
microscopic features, 90 Hereditary hemorrhagic telangiectasia, 76f
treatment, 90 age onset, 76
Hecht-Beals-Wilson syndrome, 672–73 blood-loss anemia with thrombocytopenia,
Heck’s disease. See Focal epithelial hyperplasia 77
Heerfordt’s syndrome, 335–36 clinical features, 76
Hemangioendotheliomas, 228 differential diagnosis, 76–77
Hemangioma, 352f microscopic features, 76
diffuse papular and polypoid lesions and, treatment, 77
292–93 Herniated buccal fat pad, 226f
showing grape-like clustered papules, 293f age group affected, 225
Hemangiomas, 78, 228f, 240f clinical features, 225–26
age group affected, 227, 239 differential diagnosis, 226
PMPH_Eversole_Index.indd 716 1/17/2011 3:57:42 PM
Index 717
microscopic features, 226 treatment, 109
treatment, 226 HIV salivary disease, 337–38
Herpangina, 141f HIV sialadenitis, cystic parotid swelling in,
age group affected, 140 338f
clinical features, 140–41 HLAB51, 99
differential diagnosis, 141 HLA-DRw52 antigen positive, 99
microscopic features, 141 Hodgkin’s disease, 112
treatment, 141 Hodgkin’s lymphomas, 315–16
Herpesvirus-induced lesions, 97 Homogeneous leukoplakia
Herpes zoster oticus, 636–37 age group affected, 12
Herpes zoster vesicular lesions, 625f clinical features, 12
Herpetic gingivostomatitis, 139f differential diagnosis, 12
age group affected, 139 gender predilection, 12
clinical features, 139–40 microscopic features, 12
differential diagnosis, 140 treatment, 12–13
microscopic features, 140 Horner’s syndrome, 626f
treatment, 140 localized motor deficits, 665–66
Herxheimer’s reaction, 129 clinical features, 665
Histiocytosis X, 110, 403–5 differential diagnosis, 666
localized vertical alveolar bone loss in, treatment, 666
404f ptosis and miosis in, 665f
Histoplasmosis, 114 Human immunodeficiency virus (HIV)-
Histoplasmosis of oral mucosa, 248 infected males, 72–73
Historical data base Human papillomavirus (HPV) type 16, 19,
clinical laboratory tests, 4–5 20–21
medical and dental history, 3–4 Hyalinosis cutis et mucosae, 291–92, 559
physical examination, 4 missing lateral incisors in child with, 560f
radiographic examination, 4 multiple gingival papules in, 292f
signs, 3 Hydroxychloroquine therapy, 107, 166
symptoms, 2–3 Hyoid syndrome, 638–39
HIV-associated granulomatous infections, 115 clinical features, 638–39
HIV-associated hairy leukoplakia differential diagnosis, 639
age group affected, 38 treatment, 639
clinical features, 38–39 Hyperbaric oxygen therapy, 131
differential diagnosis, 39 Hypercementosis, 576–77, 577f
gender predilection, 38 Hyperchromatism, 55
microscopic features, 39 Hyperdontia
treatment, 39 supernumerary teeth, 562–63
HIV-associated oral pigmentation, 89–90 Hyperkeratosis, 38
age group affected, 89 Hyperorthokeratosis, 11–12, 16, 29
clinical features, 89 Hyperparakeratosis, 11–12, 16, 29
differential diagnosis, 90 Hyperparathyroidism, 4, 431–32
gender predilection, 89 brown tumors and, 431f
microscopic features, 89 clinical and radiographic features, 431
treatment, 90 ground-glass radiopacities, 526–27
HIV periodontitis and oral ulcerations, 109f loss of lamina dura and secondary
age group affected, 108 renal, 527f
clinical features, 108–9 treatment of, 432
differential diagnosis, 109 Hyperparathyroidism-jaw tumor syndrome,
gender predilection, 108 393
microscopic features, 109 Hyperplastic gingivitis, 407f
PMPH_Eversole_Index.indd 717 1/17/2011 3:57:42 PM
718 Index
Hyperplastic lingual tonsil, 236f hypodontia with coronal defects in, 559f
age group affected, 236 microscopic features, 29
clinical features, 236 treatment, 29
differential diagnosis, 236 Infancy, melanotic neuroectodermal tumor,
microscopic features, 236 459–60
treatment, 236 Infectious mononucleosis, 74f, 303
Hypersensitivity-related oral red lesions, 64 age groups affected, 74
Hypertrophy, 3 clinical features, 74
Hypodontia differential diagnosis, 74–75
missing teeth, 558 lymphadenitis in patient with, 303f
in chondroectodermal dysplasia, 562f microscopic features, 74
with coronal defects in incontinentia pig- treatment, 75
menti, 559f Inflammatory cell infiltrate, 11
syndromes associated with, 586f Inflammatory fibrous hyperplasia, 220f
Hypoglossal paralysis, localized motor deficits, age group affected, 220
667–68 clinical features, 220
clinical features, 667–68 differential diagnosis, 220
differential diagnosis, 668 microscopic features, 220
tongue deviation in, 667f treatment, 220
treatment, 668 Inflammatory idiopathic disorders, 50
Hypoparathyroidism, 46 Inflammatory lesions, 10
Hypophosphatasia, 593, 593f Inflammatory polyps
antral opacities, 502–3, 502f
I periapical infection, 504–6
Idiopathic bone cavitation, 620f Inflammatory white lesions, 12
Idiopathic erosion, of facial enamel, 576f Infraorbital paresthesia
Idiopathic osteosclerosis, 483, 484f clinical features, 662–63
Idiopathic resorption, 598 differential diagnosis, 663
Idiopathic white lesions, 10, 13f. See also Homo- V-2 injury and, 663f
geneous leukoplakia Initial contact with patient, 2
IgM immunoreactants, 38 Internal resorption, 597–98
Ill-fitting dental prostheses, 11 clinical features, 597
Immunofluorescence, 38 manifesting intradental radiolucency, 597f
Immunofluorescence staining, 69 treatment of, 598
Immunosuppressive medications, 100 Interradicular radiolucencies, 383–97
Immunosuppressive therapy, 65 apical periodontal cyst, laterally displaced,
Impacted teeth, 602f 384
Impetigo, 149f calcifying cystic odontogenic tumor, 388–89,
age group affected, 149 389f
clinical features, 149 central giant cell granuloma, 397
differential diagnosis, 149 root divergence with, 398f
microscopic features, 149 central ossifying fibromas, 393–94, 393f
treatment, 149 lateral periodontal cyst, 383
Incisal trauma, with fractures interposed between vital mandibular teeth,
Incisional biopsy, 234 382f
Incisive canal cyst, 372–73, 373f odontogenic adenomatoid tumor, 394–95,
Incontinentia pigmenti, 559 395f
age onset, 29 odontogenic fibroma, 396–97, 396f
clinical features, 29 odontogenic keratocyst, 386, 387f
differential diagnosis, 29 osteoporotic bone marrow defect, 392, 392f
gender predilection, 29 primordial cysts, 386–87
PMPH_Eversole_Index.indd 718 1/17/2011 3:57:43 PM
Index 719
residual cyst, 385–86, 385f with benign fibroosseous-like pattern, 544f
squamous odontogenic tumor, 389–90, 390f metastatic carcinoma, 546–47
surgical ciliated cyst, 391, 391f osteogenic and chondrogenic sarcoma, 545,
Inter-radicular radiopacities, 482–93 545f
benign osteoblastoma, 492–93, 492f
BRONJ, 484–85 J
sequestra and surrounding radiolucency Jadassohn-Lewandowsky syndrome, 28
in, 485f Jawbone cavities, pathologic, 619–20, 620f
calcifying and keratinizing epithelial odon- clinical features, 619
togenic cyst, 486, 487f differential diagnosis, 619–20
central ossifying fibromas, 489–92 treatment, 620
clinical and radiographic features, 489–91 Jaw-winking phenomenon, 679
differential diagnosis, 491–92 Jugular foramen syndrome, 627
initiate root divergence/resorption, 490f Jugular syndrome, 669
microscopic features, 491 Junctional nevi, 80
treatment of, 492 Juvenile periodontitis, 401–2, 401f
idiopathic osteosclerosis, 483, 484f Juvenile spongiotic gingival hyperplasia, 180f
odontogenic adenomatoid tumor, 486–88 age group affected, 180
radiolucency with opaque foci in, 487f clinical features, 180
odontomas, 488f, 489 differential diagnosis, 180
residual focal osteitis and cementoma, gender predilection, 180
482–83 microscopic features, 180
Interrogation process, 2 treatment, 180
assessment of findings, 5 Juvenile spongiotic hyperplasia, 367
communication skills needed, 2 Juxtacortical osteogenic sarcoma, 539–40
definitive diagnosis, 6–7 Juxtaradicular target lesions, 478f
differential diagnosis, 5–6
formulation of treatment plan, 7 K
logical approach to, 2 Kaopectate, 45, 60, 67, 98, 103–4, 140–41
questioning process, 2 Kaposi’s sarcoma, 72–73, 72f
Intralesional steroids, 216–17 age group affected, 72
Intraosseous carcinoma, primary, 448–49, 448f clinical features, 72–73
Intraosseous leiomyoma, 439f differential diagnosis, 73
Intraosseous mucoepidermoid carcinoma, 444f gender predilection, 72
Intraosseous myofibromatosis, 441f microscopic features, 73
Intraparotid hemangioma, 320, 320f treatment, 73
Intraparotid MALT type malignant lymphoma, Kawasaki disease, 302
321f Keratin pearls, 20
Intraparotid mesenchymal tumors, 319–20 Keratoacanthoma
Intravenous antibiotic therapy, 210 of facial skin, 351f
Intrinsic pigments, 50 facial skins wellings and, 351–52
Invasive carcinoma, 13 focal and umbilicated papules, 273–74
Invasive mycoses, antral, 506–7 of lip, 274f
Invasive myofibrosarcoma, computed tomogra- Keratosis follicularis, 27f, 284–85, 285f
phy of, 459f age onset, 27
Invasive squamous cell carcinoma, 12 clinical features, 27
Irregular, Ill-defined expansile radiopacities, differential diagnosis, 27
542–47 microscopic features, 27
calcifying epithelial odontogenic tumor, treatment, 27
542–43, 543f Keratotic lesions, 45
desmoplastic ameloblastom, 543–44 Ketoconazole, 66
PMPH_Eversole_Index.indd 719 1/17/2011 3:57:43 PM
720 Index
Kikuchi-Fujimoto disease, 302 age group affected, 243
Koplik spots of measles, 40f clinical features, 243
age group affected, 40 differential diagnosis, 243
clinical features, 40 gender predilection, 243
differential diagnosis, 40 microscopic features, 243
microscopic features, 40 treatment, 244
treatment, 40 Leontiasis ossea, 526
Leukemia, 202f, 406–7
L age group affected, 201
Langerhans cell histiocytosis (LCH), 194f, clinical features, 201
403–5, 462–63 differential diagnosis, 201
age group affected, 194 microscopic features, 201
clinical and radiographic features, 403–4 treatment, 201
clinical features, 194–95 Leukoedema
differential diagnosis, 195 clinical features, 23
microscopic features, 195, 404 differential diagnosis, 24
radiolucent lesions in both jaws in patient microscopic features, 23
with, 463f treatment, 24
treatment, 195 Leukoplakias, 7, 10, 13f, 19, 38
treatment of, 405 benign, 13
Laser surgery, 13, 44 hairy, 30, 92
Lateral neck swellings, 300–316 HIV-associated hairy, 38–39
actinomycosis and, 306–7 homogenous, 12–13
benign mesenchymal tumors, 309–10 sanguinaria, 17
branchial cleft cyst, 300, 300f Leukoplakic area, 19
carotid body tumor, 311–12 Levamisole, 151
causing large tumefaction, 311f Lichenoid contact stomatitis, 165f
cat-scratch fever, 305 age group affected, 164
cervical rib and transverse process, 301, 301f clinical features, 164
cystic hygroma, 310–11 differential diagnosis, 165
of neck in infant, 310f microscopic features, 164–65
infectious mononucleosis, 303, 303f treatment, 165
malignant lymphoma, 315–16 Lichenoid dysplasia, 69
cervical masses in, 315f Lichenoid reactions, 36f
metastatic carcinoma, 312–13 age group affected, 36
in cervical nodes, 313f clinical features, 36
nonspecific lymphadenitis, 301–2 differential diagnosis, 36–37
associated with necrotic mandibular molar, gender predilection, 36
302f microscopic features, 36
reactive proliferations and, 307–8 treatment, 37
sarcomas, 314 Lichen planus, 10, 12, 21, 22f, 38, 166
sinus histiocytosis, 308–9 age group affected, 34
tuberculous lymphadenitis, 304 atrophic, 68–70
Lateral periodontal cyst, 383 clinical features, 21, 34
interposed between vital mandibular teeth, clinically mimic erosive, 64
382f differential diagnosis, 22, 35
LCH. See Langerhans cell histiocytosis (LCH) erosive, 70
Leiomyoma gender predilection, 34
central, 438–39 microscopic features, 21–22, 34–35
intraosseous, 439f plaque-form, 29
Leiomyomas, 243f stria of Wickham, 35f
PMPH_Eversole_Index.indd 720 1/17/2011 3:57:43 PM
Index 721
treatment, 22, 35 discoid and lichenoid lesions of, 37f
Limited and deviant mandibular opening, 669–78 gender predilection, 37, 61
ankylosis, 671–72 microscopic features, 38, 61–62
condylar hyperplasia, 673–74, 674f treatment, 38
conversion trismus, 671 Lupus erythematosus preparation (LE prep),
coronoid hyperplasia, 673 38, 62
Hecht-Beals-Wilson syndrome, 672–73 Lupus erythyematosus, 58
muscle splinting, 669–70 Lymphadenitis
deviant jaw opening secondary to, 669f cervical, 302
oral submucous fibrosis, 676–77 nonspecific, 301–2
postinjection/postinfection trismus, 670–71 associated with necrotic mandibular molar,
scleroderma, 676 302f
tetanus, 677–78 in patient with infectious mononucleosis, 303
TMJ region neoplasms, 674–76, 675f tuberculous, 304
Lingual abscess Lymphadenopathy, 68
age group affected, 237 Lymphangioma
clinical features, 237 age group affected, 239
differential diagnosis, 237 clinical features, 239
microscopic features, 237 differential diagnosis, 240
treatment, 237 diffuse papular and polypoid lesions and,
Lingual cyst 292–93
clinical features, 235–36 microscopic features, 239–40
differential diagnosis, 236 with pebbly surface, 293f
microscopic features, 236 treatment, 240
treatment, 236 Lymph nodes
Lingual erosion, in anorexia nervosa/bulimia, superimposed soft tissue radiopacities and
576f calcified, 551–52, 552f
Lingual hemangiomas, 240 Lymphocyte blast transformation studies, 46
Lipoid proteinosis. See Hyalinosis cutis et Lymphoepithelial cyst, 205f. See Branchial cleft
mucosae cyst
Lipomas, 310 age group affected, 204
Lipschütz bodies, 140 clinical features, 204
Lithotriptor destruction of salivary stones, 206 differential diagnosis, 205
Localized motor deficits, 664–69 microscopic features, 204–5
facial paralysis, 664–65, 664f treatment, 205
Horner’s syndrome, 665–66, 665f Lymphomas
hypoglossal paralysis, 667–68, 667f Mikulicz’s syndrome and, 321
ophthalmoplegia, 666–67, 658f and submandibular swellings, 320–21
soft palate paralysis, 668–69, 668f Lymphomatoid papulosis, 112
Ludwig’s angina, 210f Lymphonodular pharyngitis, 67, 67f
clinical features, 209 acute, 284
differential diagnosis, 210 oropharynx characteristic of, 284f
microscopic features, 209 age group affected, 67
treatment, 210 clinical features, 67
Luetic glossitis, 59 differential diagnosis, 67
Luminal ameloblastoma, 414 microscopic features, 67
Lupus erythematosus, 10, 12, 50, 61–62, 62f, 64, treatment, 67
69, 72, 107
age group affected, 37, 61 M
clinical features, 37, 61 Macrodontia, 565–66, 566f
differential diagnosis, 38, 62 Macular diffuse slate-gray pigmentation, 89
PMPH_Eversole_Index.indd 721 1/17/2011 3:57:43 PM
722 Index
Macular hemangioma, 56 Maxillary neoplasms
Maculopapular rash, 22 maxillary division pain and, 620–21
Major aphthous stomatitis clinical features, 620
age group affected, 97 differential diagnosis, 620–21
clinical features, 97–98 treatment, 621
differential diagnosis, 98 Maxillary sinusitis
microscopic features, 98 antral opacities, 500–502, 501f
treatment, 98 clouded sinuses in chronic, 618f
Malignancy, 10 maxillary division pain and, 617–19
Malignant lesions, 382f clinical features, 617–18
Malignant lymphoma, 315–16 differential diagnosis, 618–19
cervical masses in, 315f treatment, 619
Malignant melanoma, 82–83, 82f, 353–54, 353f Maxillectomy, 257–58, 262
age group affected, 82 McCune-Albright syndrome, 87
clinical features, 82–83 Median mandibular cyst, 375
differential diagnosis, 83 underlying vital teeth, 374f
gender predilection, 82 Median rhomboid glossitis, 52f, 233f
microscopic features, 83 age group affected, 52, 232
treatment, 83 clinical features, 52, 232
Malignant odontogenic tumors, 452–53 differential diagnosis, 52, 233
Mandibular division pain, 629–34 gender predilection, 232
cardiogenic facial pain, 634 microscopic features, 52, 232–33
odontogenic infection, 629–30, 629f treatment, 52, 233
osteomyelitis, 630–31, 631f Medical history, 3–4
stomatodynia/glossopyrosis, 633–34 Melanin incontinence, 82
subacute thyroiditis, 632–33 Melanoma, 51, 79
traumatic neuroma, 631–32, 632f Melanotic neuroectodermal tumor, of infancy,
Mandibular tori, 541, 542f 459–60
Mandibulo-oculo-facial dyscephaly, 560, 560f marginated radiolucency in, 460f
Manifestation of white lesions, 12 Membranous adenomas, 325
Marginal erythema, 110 Meniscus perforation, TMJ region pain, 648–49
Marked facial deformity, with multifocal mas- arthrogram of, 648f
sive lesions, 535f clinical features, 648
Marsupialization, 203 differential diagnosis, 648
Masseteric hypertrophy, 360–61, 361f treatment, 648
Massive osteolysis, 402–3, 403f Mental paresthesia, 661–62
Masticatory muscles, myositis ossificans in, clinical features, 661
553f differential diagnosis, 661–62
Maxillary dental prosthesis, 250 physical trauma, 663f
Maxillary division pain, 616–29 treatment, 662
antral and maxillary neoplasms, 620–21 Mesenchymal neoplasms, 209f, 225f
atypical facial pain, 628–29 age group affected, 208, 224
cluster headache, 621–22, 622f clinical features, 208–9, 224–25
complex regional pain syndrome, 625–26, differential diagnosis, 209, 225
626f gender predilection, 208
cranial base and CNS neoplasms, 626–28, 627f microscopic features, 209, 225
maxillary sinusitis, 617–19 treatment, 209, 225
odontogenic infection, 616–17 Mesenchymal tumors, 187f, 352, 352f
pathologic jawbone cavities, 619–20, 620f clinical features, 187
postherpetic neuralgia, 624, 625f differential diagnosis, 187
trigeminal neuralgia, 623–24, 623f microscopic features, 187
PMPH_Eversole_Index.indd 722 1/17/2011 3:57:43 PM
Index 723
treatment, 187 multiple lesions, in HIV-infected patients, 276f
Metabolic sialadenosis, 339–40 Moniliasis, 12
associated with diabetes, 340f Monomorphic adenomas
Metastasis, 240 age group affected, 230
Metastatic carcinoma, 193f, 312–13 basal cell adenoma, 231f
age group affected, 193 clinical features, 230
of breast, 382f differential diagnosis, 230
in cervical nodes, 313f gender predilection, 230
clinical and radiographic features, 380–81 microscopic features, 230–31
clinical features, 193–94 treatment, 230
differential diagnosis, 194 Mononucleosis, infectious. See Infectious
irregular, ill-defined expansile radiopacities, mononucleosis
546–47 Morsicatio mucosae oris, 30
microscopic features, 194 Moth-eaten radiolucencies, 443–60, 631f
moth-eaten radiolucencies and, 450–52 BRONJ, 446–48, 447f
osteogenic reaction in, 546f clinical and radiologic features, 446–47
periapical radiolucencies and, 380–81 microscopic features, 447
treatment, 194 treatment of, 448
Metastatic tumors, 133 Burkitt’s lymphoma, 457–58
Methyl aminolevulinic acid, 14 diffuse, destructive lesion in, 457f
Metronidazole, 109 cystogenic carcinoma, 449–50
Metronidazole therapy, 222 Ewing’s sarcoma, 455, 455f
Microbiology, 4 fibrogenic and neurogenic sarcoma, 458–59
Microcystic adenocarcinoma, 348f malignant odontogenic tumors, 452–53
Microdontia, 565–66, 566f melanotic neuroectodermal tumor of
Microvesicles, 104 infancy, 459–60
Middle ear neoplasms, otogenic pain and, metastatic carcinoma, 450–52
637–38, 637f differential diagnosis, 451
Middle fossa syndrome, 627 treatment, 452
Midline neck swellings, 340–44 osteomyelitis, 443–45
dermoid cyst, 343–44, 344f clinical and radiographic features, 443
goiter, 341–42, 342f radiolucent pattern, 444f
thyroglossal tract cyst, 340–41, 341f treatment of, 445
thyroid neoplasms, 342–43 osteoradionecrosis, 445–46
Migraine, 659 postradiation, 446f
Mikulicz’s disease, 60, 259, 334–35 osteosarcoma and chondrosarcoma, 453–54
sialogram showing lack of arborization in, 334f primary intraosseous carcinoma, 448–49,
Mikulicz’s syndrome, 321 448f
Missing teeth, 558–62 primary lymphoma of bone, 456–57, 456f
chondroectodermal dysplasia, 561–62 Mother-of-pearl appearance, 23
hereditary ectodermal dysplasia, 560–61 Motile spirochetes, 23
hyalinosis cutis et mucosae, 559, 560f Motor function disorders, generalized, 678–84
hypodontia, 558 auriculotemporal syndrome, 678–79
incontinentia pigmenti, 559 congenital facial diplegia, 683
mandibulo-oculo-facial dyscephaly, 560, 560f hemifacial atrophy, 683–84
Moh’s surgery, for squamous cell carcinoma, 350 jaw-winking phenomenon, 679
Molar teeth motor system disease, 680
concrescence in, 573f multiple sclerosis, 680–81
with enamel pearls, 569f muscular dystrophies, 681–82
Moles. See Nevi myasthenia gravis, 684
Molluscum contagiosum, 275 myotonias, 682–83
PMPH_Eversole_Index.indd 723 1/17/2011 3:57:44 PM
724 Index
Motor system disease, 680 hairy tongue, 92–93
Mouth rinses for pain relief, 37 heavy metal ingestion, 90
MPS. See Mucopolysaccharidoses (MPS) hemochromatosis, 88–89
Mucobuccal fold, 12 HIV-associated oral pigmentation, 89–90
Mucocele, 212f malignant melanoma, 82–83
age group affected, 211 multiple neurofibromatosis, 86–87
clinical features, 211–12 Peutz-Jeghers syndrome, 85–86
differential diagnosis, 212 pigmented lichen planus, 84–85
gender predilection, 211 racial pigmentation, 83–84
microscopic features, 212 Multifocal/diffuse red lesions
treatment, 212 allergic mucositis, foreign body gingivitis,
Mucoceles, 78f, 239f 63–64
age group affected, 238 atrophic glossitis, 58–59
clinical features, 78, 238–39 atrophic lichen planus, 68–70
differential diagnosis, 78–79, 239 bullous/desquamative diseases, 64–65
microscopic features, 78, 239 candidiasis, 65–66
treatment, 79, 239 ecchymosis and clotting factor deficiencies,
Mucoepidermoid carcinoma 70
intraosseous, 444f erythema migrans (migratory stomatitis),
Mucoepidermoid carcinoma, 191f, 258f, 327–29 57–58
age group affected, 191, 258 field cancerization, 71–72
clinical features, 191, 258, 327–28 geographic tongue (migratory glossitis),
differential diagnosis, 192, 258, 328 56–57
microscopic features, 192, 258 Kaposi’s sarcoma, 72–73
nodular mass of parotid representing, 328f lupus erythematosus, 61–62
treatment, 192, 258, 328–29 lymphonodular pharyngitis, 67
Mucoepidermoid or epidermoid carcinoma, 114 radiation mucositis, 59–60
Muco-oculocutaneous syndromes, 26 scarlet fever, 67–68
Mucopapillary cyst, 214 xerostomic mucositis, 60–61
Mucopolysaccharidoses (MPS), 585 Multifocal honeycomb trabeculation, in thalas-
Mucormycosis, 131f semia major, 469f
clinical features, 131 Multifocal precancerous erythroplakia, 62
differential diagnosis, 131–32 Multifocal radiolucencies, 461–65
microscopic features, 131 basal cell nevus syndrome, 461–62
with orbital floor erosion, 506f langerhans cell histiocytosis, 462–63
treatment, 132 radiolucent lesions in both jaws in patient
Mucous patches, 23f with, 463f
age group affected, 22 multiple myeloma, 463–65
clinical features, 22 multifocal punched-out lesions of jaws, 464f
differential diagnosis, 23 Multifocal red lesions, 50
microscopic features, 22–23 Multilocular keratocysts, 422f
treatment, 23 Multilocular radiolucencies, 365, 423–43
Multifocal confluent radiopacities, 530–35 ameloblastoma, 432–33
familial gigantiform cementoma, 534–35, root divergence and resorption in, 432f
535f aneurysmal bone cyst, 429–30, 430f
florid osseous dysplasia, 531–33, 532f botryoid odontogenic cyst, 424f, 425
Gardner’s syndrome, 533–34, 534f central arteriovenous malformation, 436–37
osteitis deformans, 530–31, 531f angiograms of, 437f
Multifocal/diffuse pigmentations central giant cell granuloma, 428f, 429
Addison’s disease, 87–88 central hemangioma of bone, 437–38
drug-induced pigmentation, 91–92 central leiomyoma, 438–39
PMPH_Eversole_Index.indd 724 1/17/2011 3:57:44 PM
Index 725
central neurogenic neoplasms, 434–35, 435f Myasthenia gravis, 684
cherubism, 427–28, 427f Mycobacterium avium intracellulare, 115
fibrous dysplasia, 442–43 Mycobacterium tuberculosis, 114, 304, 336
monostotic, 442f Myoepitheliomas, 325
treatment of, 443 Myofibromatosis, 440–42
glandular odontogenic cyst, 425–26 clinical and radiographic features, 440–41
clinical and radiographic features, 425 intraosseous, 441f
expansile, loculated lucency representing, treatment of, 441–42
426f Myogenic pain
treatment of, 426 temporal pain, 659–60
hyperparathyroidism, 431–32 TMJ region and, 642–44
brown tumors and, 431f clinical features, 642–43
clinical and radiographic features, 431 differential diagnosis, 643
treatment of, 432 treatment, 644
myofibromatosis, 440–42 trigger points and pain referral patterns,
clinical and radiographic features, 440–41 644f
intraosseous, 441f Myositis ossificans
treatment of, 441–42 in masticatory muscles, 553f
myxoma, 433–34 superimposed soft tissue radiopacities,
reticulated septate pattern in odontogenic, 552–53
434f Myotonias, motor function disorders, 682–83
odontogenic keratocyst, 423–24 Myxoma, 433–34
pseudotumor of hemophilia, 439–40, 440f reticulated septate pattern in odontogenic,
Multiple crateriform papules, 283f 434f
Multiple endocrine neoplasia, type IIb, 293–94
Multiple hamartoma syndrome, 286–87 N
gingival papules in, 287f Nasoalveolar (Klestadt) cyst, 215f
Multiple myeloma, 463–65 age group affected, 215
multifocal punched-out lesions of jaws, 464f clinical features, 215
Multiple neurofibromatosis differential diagnosis, 215
age of onset, 86 gender predilection, 215
clinical features, 86–87 microscopic features, 215
differential diagnosis, 87 treatment, 215
microscopic features, 87 Nasopharyngeal carcinomas, 312
treatment, 87 Neck and throat pain, 638–42
Multiple papular neuromas, of tongue, 294f carotidynia, 640–41
Multiple sclerosis, motor function disorders, glossopharyngeal neuralgia, 639–40
680–81 hyoid syndrome, 638–39
Multiple sessile papules, of lips, 286f stylohyoid syndrome, 638, 639f
Multiple tongue nodules, in amyloidosis, 291f superior laryngeal neuralgia, 641
Multiregimen chemotherapy, 193 Neck dissection, 232, 257
Mumps. See Endemic parotitis Necrotic mandibular molar, nonspecific
Mural ameloblastoma, 414 lymphadenitis and, 302f
Muscle spasm, 3 Necrotizing sialometaplasia
Muscle splinting age group affected, 113
clinical features, 669–70 clinical features, 113
deviant jaw opening secondary to, 669f differential diagnosis, 114
differential diagnosis, 670 microscopic features, 114
treatment, 670 treatment, 114
Muscular dystrophies, motor function disor- Neomycin, 149
der, 681–82 Neoplastic diseases, 7
PMPH_Eversole_Index.indd 725 1/17/2011 3:57:44 PM
726 Index
Neoplastic transformation, 19 Nonverbal communication, 2
Neural compression, in cervical rib and trans- Nonvital teeth, apical periodonttitis and granu-
verse process, 301 lomas associated with, 366f
Neural sheath tumors, 241f Noonan syndrome, 427
age group affected, 241 Nuclear hyperchromatism, 20
clinical features, 241 Nystatin cream/ointment, 66
differential diagnosis, 242
microscopic features, 241–42 O
treatment, 242 Oapilloma, antral opacities and inverting,
Neurilemmomas, 320 516–17, 516f
Neurofibroma, in NF1, 309f Objective signs, 3
Neurofibromatosis, 84 Obstructive sialadenitis, 317–18
Neurogenic sarcoma Occipital condyle syndrome, 627
moth-eaten radiolucencies and, 458–59 Oculodentodigital dysplasia, 586
Neutrophilic granulocytes, 102 Oculodento-osseous dysplasia, 586
Nevi, 344–45 OdaM. See Odontogenic ameloblastassociated
Nevocellular nevi, 80 protein (OdaM)
Nevus, 79 Odontoameloblastoma
clinical features, 80 pericoronal radiopacities, 499–500, 499f
differential diagnosis, 80 Odontodysplasia, regional, 591–92
gender predilection, 80 ghost teeth in, 592f
microscopic features, 80 Odontogenic adenomatoid tumor, 394–95, 395f,
treatment, 80–81 417–19
Nevus flammeus of facial skin, 53 clinical and radiographic features, 417–18
Nevus unius lateris, 277 impacted teeth and, 418f
unilateral extensive papillary proliferations inter-radicular radiopacities in, 486–88
involving oral mucosa in, 277f pericoronal radiopacities in, 493, 494f
NF1 gene, 87 radiolucency with opaque foci in, 487f
Nifedipine, 197 treatment, 419
Nodular invasive lesions, 353f Odontogenic ameloblastassociated protein
Nonhereditary diseases, white lesions of, 10 (OdaM), 495
Non-Hodgkin’s lymphoma, 192f, 315–16 Odontogenic fibroma, 396–97, 396f
age group affected, 192 Odontogenic fibroma/hamartoma syndrome,
clinical features, 192 420–21, 421f
differential diagnosis, 193 Odontogenic infection
extranodal, 193 mandibular division pain, 629–30
gender predilection, 192 pain referral routes and, 629f
microscopic features, 192–93 maxillary division pain, 616–17
treatment, 193 clinical features, 616–17
Non-HPV carcinomas, 21 differential diagnosis, 617
Nonspecific hyperplastic gingivitis, 198f paranasal pain and, 617f
age group affected, 197 treatment, 617
clinical features, 197–98 ophthalmic division pain, 614
differential diagnosis, 198 clinical features, 614
microscopic features, 198 differential diagnosis, 614
treatment, 198 frontal pain and anterior maxillary, 614f
Nonspecific (irritational) mucositis, 51f, 68 treatment, 614
clinical features, 51 Odontogenic keratocyst
differential diagnosis, 51 interradicular radiolucencies, 386, 387f
microscopic features, 51 multilocular radiolucencies, 423–24
treatment, 51 pericoronal radiolucencies, 413–14, 413f
PMPH_Eversole_Index.indd 726 1/17/2011 3:57:44 PM
Index 727
Odontogenic tumors treatment, 123
antral opacities, 512–13 Orolabial papillomas, in focal dermal hypopla-
in maxilla, 513f sia, 277f
Odontomas Oropharyngeal cancer, 19
inter-radicular radiopacities, 488f, 489 Orthokeratoic odontogenic cyst, 423
pericoronal radiopacities, 498–99, 498f Osseous/cartilaginous choristoma, 549–50, 550f
Oncocytoma, 324 Osseous enlargement, in fibrous dysplasia,
of parotid in elderly female, 324f 359–60
Onion-skin patterns. See Cortical redundancies Osseous expansion, diffuse sclerosing osteo-
Opacification, of antrum, 475 myelitis with, 524f
Ophthalmic division pain, 614–16 Osseous or osteocartilaginous choristomas,
frontal/ethmoidal sinusitis, 615 244f
odontogenic infection, 614, 614f age group affected, 244
vascular occlusive disease and neurysms, clinical features, 244
616, 616f differential diagnosis, 244
Ophthalmoplegia, localized motor deficits, 667f gender predilection, 244
clinical features, 666 microscopic features, 244
differential diagnosis, 666–67 treatment, 244
progressive supranuclear palsy and, 666 Osteitis circumscripta, in skul, 525f
treatment, 667 Osteitis deformans
Orabase gel, 45, 51, 61, 64, 70 ground-glass radiopacities, 524–26
Oral and maxillofacial disease processes, 2 multifocal confluent radiopacities, 530–31,
signs of, 3 531f
Oral bandage, 51 Osteitis fibrosa cystica, 431
Oral epithelium, carcinogenesis of Osteoarthritis, TMJ and, 649–50, 649f
age group affected, 19 clinical features, 649–50
clinical features, 19–20 differential diagnosis, 650
differential diagnosis, 21 treatment, 650
gender predilection, 19 Osteogenesis imperfecta, 588–89
microscopic features, 20–21 with type I dentinogenesis imperfecta, 589f
treatment, 21 Osteogenic reaction, in metastatic carcinoma,
Oral lichen simplex chronicus, 11 546f
Oral lozenge, 52 Osteogenic sarcoma
Oral macular hemangiomas, 54 irregular, ill-defined expansile radiopacities,
Oral melanotic macules, 81f 545, 545f
clinical features, 81 juxtacortical, 539–40
differential diagnosis, 82 sun burst patter, and periosteal reaction, 540f
microscopic features, 81–82 Osteoid osteoma
treatment, 82 cortical redundancies, 540–41
Oral nevi, 80 over cortex, 540f
Oral papular lesions, 285f Osteomalacia, 465–66
Oral squamous papillomas, 267, 267f diffuse granular trabeculation in, 465f
Oral submucous fibrosis, 676–77 Osteomas
Oral white lesions, 17 antral opacities, 513–14
Orbital floor erosion, mucormycosis with, 506f of antrum, 514f
Orbital syndrome, 627 Osteomyelitis, 120f, 443–45
Oroantral fistula, 123f clinical and radiographic features, 443
age group affected, 122 clinical features, 120
clinical features, 122–23 differential diagnosis, 120
differential diagnosis, 123 mandibular division pain, 630–31
microscopic features, 123 clinical features, 630
PMPH_Eversole_Index.indd 727 1/17/2011 3:57:44 PM
728 Index
Osteomyelitis (Continued) treatment, 28
differential diagnosis, 630 Paget’s disease, of bone. See Osteitis deformans
microscopic features, 630 Painful sores, diagnosis of, 6
moth-eaten radiolucencies and, 631f Palatal abscess
treatment, 630–31 clinical features, 251–52
microscopic features, 120 differential diagnosis, 252
radiolucent pattern, 444f microscopic features, 252
treatment, 120 treatment, 252
treatment of, 445 Palatal gingiva, 104
Osteopetrosis Palliative oral mouth rinse, 106
ground-glass radiopacities, 529 P-aminobenzoic acid (PABA), 14
opacification of teeth, 530f Pancytopenia, 17
Osteoporotic bone marrow defect, 392, 392f Papillary carcinoma, 343f
Osteoporotic lesions, generalized, 465– Papillary cystadenocarcinomas, 331
osteomalacia, 465–66 Papillary cystadenoma lymphomatosum,
diffuse granular trabeculation in, 465f 323–24
senile osteoporosis, 466–67 parotid nodule representing, 323f
with loss of cortical prominence and Papillary cystadenomas, 325
altered trabeculation, 466f Papillary hyperplasia, 266, 282–83
sickle cell anemia, 468 Papillary lesions
step-ladder trabeculation in, 468f focal, 267–73
steroid osteoporosis, 467 condyloma acuminatum, 269–70, 269f
thalassemia major, 469–70 giant cell fibroma, 272, 272f
multifocal honeycomb trabeculation in, 469f papilloma, 267, 267f
Osteoradionecrosis, 130f, 445–46 sialadenoma papilliferum, 271–72, 271f
age group affected, 130 squamous acanthomas, 272, 272f
clinical features, 130 verruca vulgaris, 268, 268f
differential diagnosis, 130 verruciform xanthoma, 270–71, 270f
gender predilection, 130 Papillary squamous cell carcinoma, 281–82
microscopic features, 130 Papilloma, oral squamous, 267, 267f
postradiation, 446f Papillomatosis (papillary hyperplasia), 42
treatment, 130–31 in vault, 282f
Osteosarcoma, 410, 411f Papillon-lefevre syndrome, 401–2
hemimandibulectomy for, 454 Paradental cyst, 379
moth-eaten radiolucencies and, 453–54, 454f lies buccal to vital tooth roots, 378f
Otitis media, 101 Parakeratosis, 22–23, 30
Otogenic pain, 634–38 surface, 46
acute otitis media, 634–35 Paralysis, 3
chronic otitis media, 635–36 Paraneoplastic pemphigus, 158f
herpes zoster oticus, 636–37 age group affected, 157
middle ear neoplasms, 637, 638f clinical features, 157–58
differential diagnosis, 158
P microscopic features, 158
P16, 21 treatment, 158
Pachyonychia, 17 Parasellar syndrome, 627
Pachyonychia congenita, 28f Paresthesia, 661–64
age onset, 28 infraorbital, 662–64, 663f
bilateral mucosal white lesions, 28 mental, 661–62, 663f
clinical features, 28 Parotid duct stone, 656f
differential diagnosis, 28 Parotid gland
microscopic features, 28 acinic cell carcinoma of, 329f
PMPH_Eversole_Index.indd 728 1/17/2011 3:57:44 PM
Index 729
basal cell adenoma of, 325f microscopic features, 381
dysgenetic cysts of, 338–39 treatment of, 383
oncocytoma in elderly female, 324f paradental cyst, 379
pleomorphic adenoma of, 322f lies buccal to vital tooth roots, 378f
Parotid lymph nodes periapical cemental dysplasia, 367–69
tuberculous granulomas in, 337f clinical and radiographic features, 367–68
Parotid swelling, in sarcoidosis, 335f microscopic features, 368
Parotitis, after abdominal surgery, 316f multiple apical radiolucencies underlying
Paroxysmal hematologic disorder, 102 vital teeth, 368f
Parulis, 174f treatment, 369
clinical features, 173–74 static bone cyst, 376f, 377
differential diagnosis, 174 sublingual gland depression, 377–79, 378f
microscopic features, 174 clinical and radiographic features, 378
treatment, 174 treatment of, 379
PAS-positive mycelia, 46 traumatic bone cyst, 375–76
Patch testing, 64 appears as nonexpansile periapical radiolu-
Pathologic tooth wear, 575, 575f cency, 374f
Pemphigus vulgaris, 64, 150f Periapical radiopacities, 475–82
age group affected, 150 benign cementoblastoma, 481
clinical features, 150 focal cemento-osseous dysplasia, 477–78, 478f
differential diagnosis, 151 focal periapical osteosclerosis, 480–81, 480f
microscopic features, 151 focal sclerosing osteomyelitis, 479–80, 479f
treatment, 151 periapical cemental dysplasia, 475–77, 476f
Penicillin, 23, 68, 105–6, 108, 116, 120, 122, 149 Pericoronal radiolucencies, 411–23
Periadenitis mucosae necrotica, 97 ameloblastic fibroma, 419–20, 419f
Periapical abscess, 120 calcifying epithelial odontogenic tumor, 416f,
Periapical cemental dysplasia, 367–69 417
clinical and radiographic features, 367–68 central mucoepidermoid carcinoma, 421–525
microscopic features, 368 arising from lining of dentigerous cyst,
multiple apical radiolucencies underlying 422f
vital teeth, 368f clinical and radiographic features, 421–22
opacities in edentulous areas, 483f differential diagnosis, 423
periapical radiopacities, 475–77, 476f microscopic features, 422–23
treatment, 369 treatment of, 423
Periapical infection, with antral polyps, 504–6 dentigerous cyst, 411–12, 412f
Periapical radiolucencies, 366–81 odontogenic adenomatoid tumor, 417–19
apical periodontitis, 366–67 clinical and radiographic features, 417–18
associated with nonvital teeth, 366f impacted teeth and, 418f
benign cementoblastoma, 371–72 treatment, 419
central giant cell granuloma, 380 odontogenic fibroma/hamartoma syndrome,
with root resorption, 381f 420–21, 421f
focal cemento-osseous dysplasia, 369–70 odontogenic keratocyst, 413–14, 413f
as apical radiolucent lesions in early stages, unicystic ameloblastoma, 414–16
369f with inferiorly displaced molars, 415f
focal sclerosing osteomyelitis, 370f, 371 Pericoronal radiopacities, 493–500
incisive canal cyst, 372–73, 373f ameloblastic fibrodentinoma, 496, 496f
median mandibular cyst, 375 ameloblastic fibroodontoma, 497–98, 497f
underlying vital teeth, 374f calcifying epithelial odontogenic tumor,
metastatic carcinoma, 380–81 494–95, 495f
of breast, 382f odontoameloblastoma, 499–500, 499f
clinical and radiographic features, 380–81 odontogenic adenomatoid tumor, 493, 494f
PMPH_Eversole_Index.indd 729 1/17/2011 3:57:44 PM
730 Index
Pericoronal radiopacities (Continued) thrombocyte disorders, 75–76
odontomas, 498–99 Petechial lesions, 51, 303
arise in dental follicles of impacted teeth, 498f Peutz-Jeghers syndrome, 85f, 88
Periodic acid-Schiff (PAS) staining, 26, 52, 115 age of onset, 85
Periodontal abscesses clinical features, 85–86
age group affected, 121 differential diagnosis, 86
clinical features, 121 microscopic features, 86
differential diagnosis, 121 treatment, 86
microscopic features, 121 Pharyngeal ulceration, in infectious mono-
oral fistula associated with, 121f nucleosis, 303
treatment, 121 Pharyngitis, 68
Periodontal bone loss. See Alveolar bone loss Phlebolithiasis
Periodontal maintenance therapy, 197 superimposed soft tissue radiopacities,
Periodontal therapy, 121, 201 548–49, 549f
Periodontic-endodontic inflammation, 407–8, 408f Photoactivated dye treatments, 147
Peripheral fibroma, 177f Photodynamic therapy, 14
age group affected, 177 Physiologic tooth wear, 574, 574f
clinical features, 177 Pigmentations, 603–9
differential diagnosis, 178 biliary atresia, 604–5, 605f
gender predilection, 177 dental fluorosis, 606–7, 607f
microscopic features, 178 erythroblastosis fetalis, 603–4, 604f
treatment, 178 extrinsic staining, 608, 608f
Peripheral giant cell granuloma, 176f focal, 609, 609f
clinical features, 176 porphyria, 605–6, 606f
differential diagnosis, 176–77 postmortem pink teeth, 605
gender predilection, 176 tetracycline staining, 607
microscopic features, 176 Pigmented lichen planus
treatment, 177 age group affected, 84
Peripheral odontogenic tumors, 188f clinical features, 84
age group affected, 188 differential diagnosis, 84–85
clinical features, 188 gender predilection, 84
differential diagnosis, 188 microscopic features, 84
microscopic features, 188 treatment, 85
treatment, 188–89 Pigmented nevi, 80, 80f
Peripheral ossifying fibroma, 179f Pigmented villonodular synovitis, 655–56
age group affected, 179 clinical features, 655
clinical features, 179 differential diagnosis, 655–56
differential diagnosis, 179 treatment, 656
gender predilection, 179 Pindborg tumor, 543
microscopic features, 179 Plaque-like white lesion, 21
treatment, 180 Plaque-related inflammatory disease, 50
Pernicious anemia, 59, 68 Plasmacytosis gingivae, 63
Pesidual focal osteitis Pleomorphic adenomas, 254f, 322–23
inter-radicular radiopacities, 482–83 age group affected, 253
Petechiae clinical features, 253
hereditary hemorrhagic telangiectasia, 76–77 differential diagnosis, 254
infectious mononucleosis, 74–75 gender predilection, 253
onset of “itchiness,” 73 microscopic features, 253–54
palatal, 74 of parotid gland, 322f
soft-palate, 73 treatment, 254
suction, 73–74 Pleomorphism, 20, 55, 73
PMPH_Eversole_Index.indd 730 1/17/2011 3:57:44 PM
Index 731
Plummer-Vinson syndrome, 19 Prussian blue iron stain, 89
Podophyllum resin, 92 Pseudohypoparathyroidism, 586
Polymorphous low-grade adenocarcinoma, 255f Pseudotumor, of hemophilia, 439–40, 440f
age group affected, 254 Puberty/pregnancy gingivitis, 201f
clinical features, 254 age group affected, 200
differential diagnosis, 255 clinical features, 200
gender predilection, 254 differential diagnosis, 201
microscopic features, 254–55 gender predilection, 200
treatment, 255 microscopic features, 201
Polymyxin, 149 treatment, 201
Polyps with calcification, in localized aspergil- Pulmonary disease, 115
losis, 507f Pulpal inflammation, and focal sclerosing
Poorly differentiated carcinoma, 20 osteomyelitis, 479f
Porphyria, 605–6 Pulp stones, 595f
clinical features, 605–6 Purulent drainage, in acute sialadenitis, 317
differential diagnosis, 606 Pyodermatitis vegetans of Hallopeau, 287
porphyrin deposits in, 606f Pyogenic granuloma, 73, 175f
treatment, 606 age group affected, 175
Porphyromonas gingivalis, 367 clinical features, 175
Postherpetic neuralgia, 624 differential diagnosis, 175
clinical features, 624 gender predilection, 175
differential diagnosis, 624 microscopic features, 175
herpes zoster vesicular lesions, 624f treatment, 175
treatment, 624 Pyostomatitis vegetans, 167f, 287–88
Postinjection/postinfection trismus, 670–71 age group affected, 166
Postmortem pink teeth, 605 associated with ulcerative colitis, 288f
Powdered calcifications, augmentation materi- clinical features, 166
als and, 511f differential diagnosis, 167
Precancerous leukoplakia, 12 microscopic features, 167
Prednisone, 153 multiple papules and erosions, 288f
Premalignant leukoplakias, 10 treatment, 167
Premature aging, 17
Primary intraosseous carcinoma, 448–49, 448f Q
Primary lymphoma, of bone, 456–57, 456f Questioning process, 2
Primary varicella-zoster (chickenpox), 143f
age group affected, 143 R
clinical features, 143 Racial melanosis, 84f
differential diagnosis, 143 Racial pigmentation
microscopic features, 143 age of onset, 83
treatment, 143 clinical features, 83–84
Primordial cysts, 386–87, 388f differential diagnosis, 84
Progressive supranuclear palsy, 666 gender predilection, 83
Proliferative verrucous leukoplakia (PVL) microscopic features, 84
age group affected, 31 treatment, 84
clinical features, 31 Radiation mucositis, 59f, 69, 72
differential diagnosis, 32 age group affected, 59
gender predilection, 31 clinical features, 59
microscopic features, 31–32 differential diagnosis, 60
treatment, 32 gender predilection, 59
Promethazine hydrochloride (Phenergan), 149 microscopic features, 59–60
Prophylactic neck dissection, 83, 189 treatment, 60
PMPH_Eversole_Index.indd 731 1/17/2011 3:57:45 PM
732 Index
Radiation therapy, 32, 34, 60, 189, 191, 193, 210, microscopic features, 181
261–62 Retromolar swellings, 192
with chemotherapy, 128 Rhabdomyosarcoma, 314f
Radical excision, 232 Rheumatoid arthritis, TMJ and, 650–51, 651f
Radical neck dissection, 207 clinical features, 650
Radical surgery, 83, 191 differential diagnosis, 650–51
Radiographic examination, 4 treatment, 651
radiographs in oral and maxillofacial medi- Rieger’s syndrome, 586
cine, 5t Risus sardonicus, 678
Radiotherapy, 117 Root resorption, central giant cell granuloma,
Ramon syndrome, 427 381f
Ranula, 203f Rubeola infection, 40
clinical features, 202
differential diagnosis, 202–3 S
microscopic features, 202 Sagliker syndrome, 526
treatment, 203 Salicylates, 40
Reactive lesions, 238f Salivary gland tumors, 207f
age group affected, 237 age group affected, 207
clinical features, 237–38 clinical features, 207
differential diagnosis, 238 differential diagnosis, 207
microscopic features, 238 gender predilection, 207
of palatal gingival. See Gingival microscopic features, 207
tumefactions treatment, 207
treatment, 238 Salivary neoplasms
Reactive lymphoid hyperplasia age group affected, 231
clinical features, 226–27 clinical features, 231
differential diagnosis, 227 differential diagnosis, 231–32
microscopic features, 227 gender predilection, 231
treatment, 227 microscopic features, 231
Recurrent herpes labialis, 148f treatment, 232
age group affected, 146 Salivary squamous cell carcinomas, 331
clinical features, 146–47 Sanguinaria (blood root), 16
differential diagnosis, 147 Sanguinaria-induced keratoses, 17f
microscopic features, 147 clinical features, 16
treatment, 147–48 differential diagnosis, 17
Recurrent herpes stomatitis, 146f microscopic features, 16
age group affected, 145 treatment, 17
clinical features, 145 Sanguinaria leukoplakia, 17
differential diagnosis, 145–46 Sarcoidosis, 335–36
microscopic features, 145 parotid swelling in, 335f
treatment, 146 Sarcoid sialadenitis, 335–36
Referral to a specialist, 7 Sarcomas, 133, 191f, 314
Reflex sympathetic dystrophy, 625 age group affected, 190
Reiter’s syndromes, 99 clinical features, 190, 245–46
Residual cyst, 385–86, 385f differential diagnosis, 191, 246
Retinoid preparations, 35 microscopic features, 190–91, 246
Retinoids, 27 rhabdomyosarcoma of tongue, 246f
Retrocuspid papillae, 181f treatment, 191, 246
age group affected, 181 Scarlet fever, 67–68
clinical features, 181 age group affected, 67
differential diagnosis, 181 clinical features, 67–68
PMPH_Eversole_Index.indd 732 1/17/2011 3:57:45 PM
Index 733
differential diagnosis, 68 treatment, 214
microscopic features, 68 Sialogenic pain, 656–59
treatment, 68 acute suppurative sialadenitis, 658–59
Schirmer strips, 60 endemic parotitis, 657–58
Scleroderma, 409–10, 409f sialolithiasis, 656–57, 656f
limited and deviant mandibular opening, 676 Sialolithiasis, 317–18, 656–57
clinical features, 676 and calcified submandibular gland, 547f
differential diagnosis, 676 clinical features, 656–57
treatment, 676 differential diagnosis, 657
Sclerostosis minor gland, 214f
bilateral, 539f age group affected, 214
Scrofula. See Tuberculous lymphadenitis clinical features, 214
Sebaceous cell carcinoma, 348f differential diagnosis, 215
Sebaceous cyst, 345–46 gender predilection, 214
Sebaceous lymphadenomas, 323, 325 microscopic features, 215
Seborrheic keratoses, 346–47 treatment, 215
of cheek, 346f with sialadenitis, 206f
scaly nodule of scalp in elderly male, 347f age group affected, 205
Secondary varicellazoster (shingles), 144f clinical features, 205–6
clinical features, 144 differential diagnosis, 206
differential diagnosis, 145 gender predilection, 205
microscopic features, 145 microscopic features, 206
treatment, 145 treatment, 206
Segmental odontomaxillary dysplasia, 528–29, sialolith in submandibular duct, 656f
528f, 595–96, 596f superimposed soft tissue radiopacities,
clinical features, 595–96 547–48
differential diagnosis, 596 treatment, 658
microscopic features, 596 Sickle cell anemia, 468
treatment of, 596 step-ladder trabeculation in, 468f
Senile elastosis, 14 Signs
Senile osteoporosis, 466–67 characterization of, 3
with loss of cortical prominence and altered hard-tissue changes (clinical), 3
trabeculation, 466f hard-tissue changes (radiographic), 3
Sensory deficits, 3 neuromuscular functional changes, 3
Sequestrectomy with gentle nonaggressive of oral and maxillofacial disease processes, 3
debridement, 134 soft-tissue changes, 3
Serology, 4–5 Silent sinus syndrome, 520, 520f
Shelterin (TINF2), 17 Silver nitrate, 97
Sialadenitis Sinonasal undifferentiated carcinoma (SNUC),
acute, 316–17 518f
chronic, 318–19 Sinus histiocytosis, 308–9
obstructive, 317–18 with massive lymphadenopathy, 308f
sarcoid, 335–36 Sinus mucocele
submandibular swelling in, 318f antral opacities, 503–4, 504f
Sialadenoma papilliferum, 271–72, 271f, 325 Sjögren’s syndrome, 60, 60f, 259, 333–34, 333f
Sialectomy, 207 Smokeless tobacco-associated white lesions, 16
Sialocysts, 202, 213f Smokeless tobacco keratoses
age group affected, 213 clinical features, 14–16
clinical features, 213 differential diagnosis, 16
differential diagnosis, 214 microscopic features, 16
microscopic features, 213–14 treatment, 16
PMPH_Eversole_Index.indd 733 1/17/2011 3:57:45 PM
734 Index
Snow-capped teeth, 582, 582f treatment, 21, 117, 189, 211, 230, 249
SNUC. See Sinonasal undifferentiated carci- Squamous odontogenic tumor, 389–90, 390f
noma (SNUC) Static bone cyst, 376f, 377
Snuff keratosis, 16 Stensen’s ducts, 60, 226
Soft palate paralysis, localized motor deficits Step-ladder trabeculation, in sickle cell anemia,
clinical features, 668–69 468f
differential diagnosis, 669 Steroid osteoporosis, 467
treatment, 669 Steroid therapy, 37–38, 88, 147, 157, 161, 164–65,
uvula deviation in, 668f 167, 219
Vernet syndrome and, 669 Stevens-Johnson syndrome, 157f
Soft-palate petechiae, 73 age group affected, 156
Soft tissue abscess, 124f clinical features, 156
clinical features, 123 differential diagnosis, 156–57
differential diagnosis, 124 gender predilection, 156
microscopic features, 123–24 microscopic features, 155
treatment, 124 treatment, 157
Solar cheilitis, 14 Stomatitis nicotina, 43f, 283–84, 283f
Soothing oral rinse, 104 clinical features, 42
Space infections, 354–55, 355f differential diagnosis, 42
Speckled leukoplakia, 20 microscopic features, 42
age group affected, 43 treatment, 42–43
clinical features, 43 Stomatodynia, 633–34
differential diagnosis, 44 clinical features, 633
gender predilection, 43 differential diagnosis, 633
microscopic features, 43 treatment, 633
treatment, 44 Strabismus with nystagmus, 29
velvety red lesions with white punctate pap- Strawberry tongue, 68
ules in dysplastic, 44f Streptococcus mutans, 577
Spindle cell nevi, 80 Sturge-Weber syndrome, 53–54
Spindle cell proliferation, 73 Stylohyoid ligament, calcified, 639f
Spindle cells Stylohyoid syndrome, 638, 639f
in fibroproliferative reactions, 307 Subacute thyroiditis, 632
Spirochete, 23 Subcervical resorption, 599–600, 599f
Spongiosis, 23 clinical features, 599
S-100 protein, 195 differential diagnosis, 599
Squamous acanthomas, 272, 272f microscopic features, 599
Squamous cell carcinoma, 12, 17, 117f, 130f, 190f, treatment, 599–600
211f, 229f, 249f, 350, 518f Submandibular gland depression, 376f, 377
age group affected, 116, 189, 210, 229, 248 Submucosal macrophages, 29
clinical features, 19–20, 116, 189, 210, 229, Suction petechiae, 73f
248–49 clinical features, 73
differential diagnosis, 21, 117, 189, 210, 230, differential diagnosis, 74
249 microscopic features, 74
of facial skin, 350f treatment, 74
gender predilection, 116, 189, 210, 229, 248 Sulfa drugs, 157
hoarseness and throat pain and keratotic, Sulfapyridine therapy, 161
642f Sulfasalazine, 222
microscopic features, 20–21, 116–17, 189, 210, Sun screen, 219
230, 249 Superimposed soft tissue radiopacities, 547–53
papillary, 281–82 calcified lymph nodes, 551–52, 552f
papillary exophytic, 281f foreign bodies and, 550–51, 550f
PMPH_Eversole_Index.indd 734 1/17/2011 3:57:45 PM
Index 735
myositis ossificans, 552–53 Telangiectatic pigmented reticular lesions, 17
osseous/cartilaginous choristoma, 549–50, Telomerase complex, 17
550f Temporal pain, 659–61
phlebolithiasis, 548–49, 549f giant cell arteritis, 660–61, 661f
sialolithiasis, 547–48, 547f migraine, 659
Superior laryngeal neuralgia, 641 myogenic pain, 659–60
clinical features, 641 Temporo-mandibular joint (TMJ), 613
differential diagnosis, 641 mandibular odontogenic infection and,
treatment, 641 629f
Supernumerary teeth, 562–65 Tension headache, 255
cleidocranial dysplasia, 563–64, 564f Tertiary syphilis, 129f
Gardner’s syndrome, 564–65, 565f age group affected, 129
hyperdontia, 562–63 clinical features, 129
Surgery, 13, 117, 123, 210 differential diagnosis, 129
Surgical biopsy, 60 gender predilection, 129
Surgical ciliated cyst, 391, 391f microscopic features, 129
Surgical excision, 177–78, 180, 184, 186, 209, treatment, 129
212, 215, 220, 224–25, 229, 231, 235–39, Tetanus, limited and deviant mandibular
242–44, 251, 254, 259 opening
Surgical mumps. See Acute sialadenitis clinical features, 677–78
Surgical stripping, 44 differential diagnosis, 678
Sutton’s disease, 97–98 treatment, 678
Swollen cervical fistula, in actinomycosis, 306f Tetracycline, 98, 109
Symptoms Tetracycline oral suspension, 97, 106
discomfortness, 2 Tetracycline staining, 607
functional changes, 2 Textural changes, 2
interrogation post identification of, 3 Thalassemia major, 469–70
textural changes, 2 multifocal honeycomb trabeculation in,
Syndrome-associated enamel defects, 585–86 469f
Synovial chondromatosis, TMJ region pain, Thrombocyte disorders, 75f
654–55 age groups affected, 75
clinical features, 654–55 clinical features, 75
computed tomography and 3D reconstruc- differential diagnosis, 75–76
tion, 654f microscopic features, 75
differential diagnosis, 655 treatment, 76
treatment, 655 Thyroglossal duct cysts, 235f
Synthetic penicillin, 106 age of onset, 234
Syphilis, 19, 248 clinical features, 234
Syringoma, 348f differential diagnosis, 235
Systemic antibiotics, 105, 134 microscopic features, 235
Systemic corticosteroid therapy, short-term, 107, treatment, 235
166 Thyroglossal tract cyst, 340–41, 341f
Systemic immunosuppressant therapy, 62 Thyroid adenoma, 343f
Systemic prednisone, 222 Thyroid neoplasms, 342–43
Systemic steroid therapy, 153 T lymphocytes, 97
TMJ. See Temporo-mandibular joint (TMJ)
T TMJ psoriatic arthritis, 652f
Tacrolimus, 37 TMJ region neoplasms, 674–75, 675f
Taurodontism, 571, 571f clinical features, 674–75
T-cell lymphomas, 113 differential diagnosis, 675
Telangiectasia, 258 treatment, 675
PMPH_Eversole_Index.indd 735 1/17/2011 3:57:45 PM
736 Index
TMJ region pain, 642–56 Traumatic bone cyst, 375–76
acute infectious arthritides, 651–52 appears as nonexpansile periapical radiolu-
condylar fracture, 653–54, 653f cency, 374f
meniscus perforation, 648–49, 648f Traumatic fibroma, 223f
and miscellaneous arthritides, 652–53, 652f clinical features, 222–23
myogenic pain, 642–44 differential diagnosis, 223
osteoarthritis, 649–50, 649f microscopic features, 223
pigmented villonodular synovitis, 655–56 treatment, 223
rheumatoid arthritis, 650–51, 651f Traumatic granuloma, 110
synovial chondromatosis, 654–55, 654f Traumatic granuloma with stromal eosino-
type III internal derangement, 647–48, 647f philia (TUGSE), 111f
type II internal derangement, 646–47, 646f age group affected, 111
type I internal derangement, 644–45, 645f clinical features, 111
Tobacco-associated leukoplakias, 10 differential diagnosis, 112
differential diagnosis, 12 microscopic features, 111–12
microscopic features, 12 treatment, 112
Tobacco-associated white lesions, 10 Traumatic neuroma, 631–32
Tobacco-induced leukokeratosis, 16 clinical features, 631
Tobacco-specific nitrosamines, 16 differential diagnosis, 631–32
Toluidine blue, 22 radiolucency in anterior maxilla and, 632f
Tongue papillae, 59 treatment, 632
Tonsillar enlargement, in infectious mono- Traumatic ulcer, 110f
nucleosis, 303 clinical features, 109–10
Toothpaste idiosyncratic lesions differential diagnosis, 110
clinical features, 168 microscopic features, 110
differential diagnosis, 168 treatment, 110
microscopic features, 168 Treatment plan, formulation of, 7
treatment, 168 Treponema denticola, 367
Topical steroid, 37 Treponema pallidum, 115
Torus mandibularis and exostoses, 182f Triamcinolone, 64, 70, 216
age group affected, 181 Trichodento-osseous syndrome, 586
clinical features, 181–82 Trigeminal neuralgia, 623–24
differential diagnosis, 182 clinical features, 623
gender predilection, 181 differential diagnosis, 623
microscopic features, 182 treatment, 623–24
treatment, 182 trigger points and pain paroxysms of, 623f
Torus palatinus, 250f Tuberculosis, 115, 336–37
age group affected, 250 Tuberculous granulomas, 337f
clinical features, 250 Tuberculous lymphadenitis, 304
differential diagnosis, 250 Tuberculous lymphadenopathy, of cervical
gender predilection, 250 nodes, 304f
microscopic features, 250 Tuberous sclerosis, 586
treatment, 250 TUGSE. See Traumatic granuloma with stromal
Tourniquet test, 76 eosinophilia (TUGSE)
Toxoplasma lymphadenitis, 227 Tumefaction, 19
Traumatic (amputation) neuroma, 224f anatomic localization of, 299
clinical features, 224 carotid body tumor causing large, 311f
differential diagnosis, 224 Turner’s hypoplasia, of centrals, 579f
microscopic features, 224 Twelfth nerve paralysis, 667–68, 668f
treatment, 224 Tympanic membrane
PMPH_Eversole_Index.indd 736 1/17/2011 3:57:45 PM
Index 737
in acute otitis media, 635f Uremic oral ulcers, 103
in chronic otitis media, 636f Uremic stomatitis
Type III internal derangement, TMJ region age group affected, 102
pain, 647–39648 clinical features, 102–3
arthrograms in, 648f differential diagnosis, 103
clinical features, 647 microscopic features, 103
differential diagnosis, 647 treatment, 103
treatment, 647–48 Urinalysis, 4
Type II internal derangement, TMJ region pain,
646–47, 646f V
Type I internal derangement, TMJ region pain, Vanishing bone disease, 402–3, 403f
644–45, 645f Varicella-zoster virus infections, 145
Varices, 79, 228f
U age group affected, 227
Ulceration, 14, 99 blue/purple lesions, multiple confluent, 54
Ulcerative colitis, pyostomatitis vegetans asso- clinical features, 54, 227–28
ciated with, 288f differential diagnosis, 55, 228
Ulcerative lesions, of oral cavity, 96 microscopic features, 54, 228
Unicystic ameloblastoma, 414–16 treatment, 55, 228–29
clinical and radiographic features, 414 Vascular occlusive disease, 616
with inferiorly displaced molars, 415f clinical features, 616
treatment of, 416 differential diagnosis, 616
Unilateral parotid and submandibular swell- frontal area pain in, 616f
ings, 316–31 treatment, 616
acinic cell carcinoma, 329–30 Vasodilation, 68
of parotid, 329f Velvety-red macules, 71
acute sialadenitis, 316–17 Venereal Disease Research Laboratory
purulent drainage in, 317 test, 23
adenocarcinomas NOS, 330–31, 330f Venous aneurysms, 319
adenoid cystic carcinoma, 326–27 Vernet syndrome, 669
of parotid gland, 326f Verruca vulgaris, 268, 268f
chronic sialadenitis, 318–19 Verruciform xanthoma, 270–71, 270f
intraparotid mesenchymal tumors, 319–20 Verrucous carcinoma, 280, 280f
lymphomas, 320–21 age group affected, 33
miscellaneous adenomas and, 325–26 clinical features, 19–20, 33
mucoepidermoid carcinoma, 327–29 differential diagnosis, 21, 34
clinical features, 327–28 microscopic features, 20–21, 33
differential diagnosis, 328 treatment, 21, 34
nodular mass of parotid representing, 328f Verrucous leukoplakia, atypical, 278–79, 278f
treatment, 328–29 Vesiculo-bullousulcerative diseases
oncocytoma, 324 clinical features, 47
papillary cystadenoma lymphomatosum, Vinca alkaloids, 195
323–24 Vincent’s disease, 105
pleomorphic adenoma, 322–23 Viral vesicular stomatitis
of parotid gland, 322f age group affected, 103
sialolithiasis and obstructive sialadenitis, clinical features, 103–4
317–18 differential diagnosis, 104
Urbach-Wiethe syndrome. See Hyalinosis cutis microscopic features, 104
et mucosae treatment, 104
Uremia, 96 Viscous lidocaine, 143
PMPH_Eversole_Index.indd 737 1/17/2011 3:57:45 PM
738 Index
Vitamin D refractory rickets, 593–94, 594f age onset, 24
Vomiting, 88 clinical features, 24–25
Von Recklinghausen’s disease, 87–88 differential diagnosis, 25
microscopic features, 25
W treatment, 25
Warthin-Starry spirochete stain, 116 Widened periodontal ligament space, 407–10
Warthin’s tumor. See Papillary cystadenoma osteogenic sarcoma, 410, 411f
lymphomatosum periodontic-endodontic inflammation, 407–8,
Warty dyskeratoma, 274–75 408f
Water’s sinus, 132 scleroderma, 409–10, 409f
Wegener’s granulomatosis, 126f, 199f
age group affected, 127, 198 X
clinical features, 127, 198–99 Xerostomic mucositis, 60f
differential diagnosis, 127, 199 age group affected, 60
gender predilection, 127 clinical features, 60–61
microscopic features, 127, 199 differential diagnosis, 61
treatment, 127, 199 gender predilection, 60
Well-circumscribed radiolucency, in posterior microscopic features, 61
maxilla, 391f treatment, 61
Well-differentiated carcinomas, 20 X-linked or autosomal dominant disorder, 17
Wharton’s ducts, 60
White necrotic surface, 45 Z
White papular eruption, 27 Zidovudine, 90
White plaques, 12 Zinsser-Engman-Cole syndrome, 17
White sponge nevus, 25f Zone of erythema, 51
PMPH_Eversole_Index.indd 738 1/17/2011 3:57:45 PM
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- 1000 MCQS - ORAL MEDICINE & PATHOLOGY Plus September 2014 MCQsDocument31 pages1000 MCQS - ORAL MEDICINE & PATHOLOGY Plus September 2014 MCQsHarjotBrar100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Diagnosis List IcdDocument7 pagesDiagnosis List IcdNaimi WahyuniNo ratings yet
- Handbook Oral Medicine PDFDocument217 pagesHandbook Oral Medicine PDFpretty100% (1)
- Prayer of St. Ephraim BookmarkDocument1 pagePrayer of St. Ephraim BookmarkTNo ratings yet
- TheLifeOfStAntony TextDocument119 pagesTheLifeOfStAntony TextTNo ratings yet
- Minute TakingDocument11 pagesMinute TakingTNo ratings yet
- Taking Board Meeting Minutes - Step by StepDocument2 pagesTaking Board Meeting Minutes - Step by StepTNo ratings yet
- Denture StomatitisDocument28 pagesDenture StomatitisAmalorNo ratings yet
- Orofacial Complications of Non Surgical Cancer TherapyDocument59 pagesOrofacial Complications of Non Surgical Cancer TherapyKassim OboghenaNo ratings yet
- Current Perspectives On Use of Aloe Vera in DentistryDocument12 pagesCurrent Perspectives On Use of Aloe Vera in DentistrysevattapillaiNo ratings yet
- Biopsy TechniquesDocument31 pagesBiopsy Techniqueschouchou124No ratings yet
- Nicotin Stomatitis in Smokers-Case ReportDocument3 pagesNicotin Stomatitis in Smokers-Case Reportsri afriyanti muntheNo ratings yet
- Vitamins: Ghubaya College of Pharmacy 9485500085Document2 pagesVitamins: Ghubaya College of Pharmacy 9485500085Ghubaya CopNo ratings yet
- White LesionsDocument53 pagesWhite Lesionsmmali5853No ratings yet
- Stomatitis - AHNDocument22 pagesStomatitis - AHNZimran SalimNo ratings yet
- Gingival and PeriodontalDocument57 pagesGingival and PeriodontalPhanQuangHuyNo ratings yet
- Aphthous Stomatitis - WikipediaDocument69 pagesAphthous Stomatitis - WikipediaAtul MhetreNo ratings yet
- Oral Manifestations of Nutritional Disorders2Document33 pagesOral Manifestations of Nutritional Disorders2Yeoh Wen LiNo ratings yet
- Krok 2 Stomatology: Test Items For Licensing ExaminationDocument30 pagesKrok 2 Stomatology: Test Items For Licensing ExaminationjimmyNo ratings yet
- Epidemiology and Etiology of Denture Stomatitis: KeywordsDocument10 pagesEpidemiology and Etiology of Denture Stomatitis: Keywordsluthfia choirunnisaNo ratings yet
- Cinnamon Chewing Gum Induced Oral Allergic Contact StomatitisDocument4 pagesCinnamon Chewing Gum Induced Oral Allergic Contact Stomatitisfitri dwi123No ratings yet
- Tissue Response To Complete DentureDocument7 pagesTissue Response To Complete DentureEVA MONSERRATNo ratings yet
- White, Red, and Mixed Lesions of Oral Mucosa A Clinicopathologic Approach To DiagnosisDocument17 pagesWhite, Red, and Mixed Lesions of Oral Mucosa A Clinicopathologic Approach To DiagnosisAlexandra LupuleasaNo ratings yet
- Fateema Priyam Second Yr P.GDocument163 pagesFateema Priyam Second Yr P.GSahana RangarajanNo ratings yet
- Osmf-Classification Systems PDFDocument6 pagesOsmf-Classification Systems PDFporkodi sudhaNo ratings yet
- Handbook of Oral Pathology and Oral Medicine S R Prabhu Full ChapterDocument51 pagesHandbook of Oral Pathology and Oral Medicine S R Prabhu Full Chapterjessica.mulligan539100% (4)
- Modern Approaches To The Treatment of Viral Stomatitis in ChildrenDocument5 pagesModern Approaches To The Treatment of Viral Stomatitis in ChildrenCentral Asian StudiesNo ratings yet
- Textbook of Oral Medicine Oral DiagnosisDocument924 pagesTextbook of Oral Medicine Oral DiagnosisSonal100% (1)
- Asia Pacific Dental Students Association Journal - APDSJV3N2Document117 pagesAsia Pacific Dental Students Association Journal - APDSJV3N2APDSANo ratings yet
- 2 Oral UlcersDocument27 pages2 Oral UlcersAhmed Abdelhady Mahmoud AbdelwahedNo ratings yet
- Tschauner - S Guide To Small Animal ClinicsDocument408 pagesTschauner - S Guide To Small Animal ClinicsRagil Angga Prastiya83% (6)
- 26 MethylmethacrylateDocument3 pages26 MethylmethacrylateDaniela CapitanuNo ratings yet
- Third Year Paper 2020 - 1999 by DENTOWESOMEDocument60 pagesThird Year Paper 2020 - 1999 by DENTOWESOMENeeraja VeerisettyNo ratings yet
- Autoimmunity Reviews: SciencedirectDocument10 pagesAutoimmunity Reviews: SciencedirectYeni PuspitasariNo ratings yet