Professional Documents
Culture Documents
Fundamentals of Anatomy & Physiology-1 PDF
Fundamentals of Anatomy & Physiology-1 PDF
Uploaded by
Novely MerlynOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fundamentals of Anatomy & Physiology-1 PDF
Fundamentals of Anatomy & Physiology-1 PDF
Uploaded by
Novely MerlynCopyright:
Available Formats
20 The Heart
Learning Outcomes
These Learning Outcomes correspond by number to this chapter’s sections and
indicate what you should be able to do after completing the chapter.
20-1 ■ Describe the anatomy of the heart, including vascular supply and
pericardium structure, and trace the flow of blood through the heart,
identifying the major blood vessels, chambers, and heart valves. p. 689
20-2 ■ Explain the events of an action potential in cardiac muscle, indicate
the importance of calcium ions to the contractile process, describe
the conducting system of the heart, and identify the electrical events
associated with a normal electrocardiogram. p. 702
20-3 ■ Explain the events of the cardiac cycle, including atrial and ventricular
systole and diastole, and relate the heart sounds to specific events
in the cycle. p. 711
20-4 ■ Define cardiac output,
describe the factors
that influence heart
rate and stroke
volume, and explain
how adjustments in
stroke volume and
cardiac output are
coordinated at
different levels
of physical
activity. p. 716
M20_MART6026_11_SE_C20_pp688-726.indd 688 28/10/16 3:35 pm
+ CLINICAL CASE A Needle to the Chest
It has been a slow night in the emergency Dr. Jim instructs the EMTs to take the
room. Dr. Jim is reading an emergency victim directly into Trauma Room 1. The patient
medicine journal and nodding off. He is loaded supine on the trauma cart and Dr. Jim
perks up when he hears the speakerphone quickly introduces himself to the barely con-
crackle. scious man. A chest x-ray shows a fractured
“We have a male, mid-40s, driver of a sternum and several fractured ribs, but the
vehicle involved in a head-on collision with a heart shadow (outline on the x-ray) appears
truck,” reports an EMT. “He was unconscious normal. The heart sounds are distant and
at the scene, but is now semi-alert, complain- muffled through a stethoscope. After a rapid
ing of severe chest pain. His respirations are bedside ultrasound, Dr. Jim puts on sterile
30 and shallow. His blood pressure is 80/58. Pulse 130. Carotid gloves, does a skin prep of the patient’s anterior chest, and sticks
pulses in the neck are present, but barely palpable (able to be felt). a large-bore needle with a 100-mL syringe attached into the man’s
He has massive jugular venous distension (the veins in his neck sub-xiphoid space, directing the needle toward his left shoulder.
are backed up with blood). The seat belt was broken and he has a The syringe fills with dark blood twice. What is Dr. Jim doing?
steering wheel contusion on his anterior chest.” To find out, turn to the Clinical Case Wrap-Up on p. 726.
An Introduction to the Heart as Part arteries, and oxygen-poor blood through systemic veins back to
of the Cardiovascular System the heart’s upper right chamber (right atrium). Let’s start with
an overview of heart function.
The heart, along with the blood and blood vessels, is part of the
cardiovascular system, as we introduced in Chapter 19. This Overview of Heart Function: The Pulmonary
system functions to distribute oxygen and nutrients to the cells and Systemic Circuits
of the body, and to take away carbon dioxide and other wastes.
In the cardiovascular system, blood flows through a network of
In this chapter we consider the structure and function of the
blood vessels that extend between the heart and peripheral tis-
heart, a small organ about the size of your clenched fist. This
sues. Those blood vessels make up a pulmonary circuit, which
extraordinary organ beats approximately 100,000 times each
carries blood to and from the gas exchange surfaces of the 20
day. Each day the heart pumps about 8000 liters of blood—
lungs, and a systemic circuit, which transports blood to and
enough to fill forty 55-gallon drums, or 8800 quart-sized milk
from the rest of the body (Figure 20–1). Each circuit begins and
cartons. Try transferring a gallon of water with a cooking baster,
ends at the heart, and blood travels through these circuits in
and you’ll appreciate just how hard the heart has to work to
sequence. Thus, blood returning to the heart from the systemic
keep you alive. Let’s look first at the structure of this organ, and
circuit must complete the pulmonary circuit before reentering
then at several important aspects of its function.
the systemic circuit.
The blood vessels of both circuits include arteries, capil-
20-1 The heart is a four-chambered laries, and veins. Arteries carry blood away from the heart,
organ that pumps blood through the and veins return blood to the heart. The great vessels are the
systemic and pulmonary circuits largest veins and arteries in the body, those connected to the
Learning Outcome Describe the anatomy of the heart, including heart. Microscopic thin-walled vessels called capillaries inter-
vascular supply and pericardium structure, and trace the flow connect the smallest arteries and the smallest veins. Capillaries
of blood through the heart, identifying the major blood vessels, are called exchange vessels, because their thin walls permit the
chambers, and heart valves.
exchange of nutrients, dissolved gases (called gas exchange), and
The heart is a hollow muscular organ that pumps oxygen-poor wastes between the blood and surrounding tissues.
blood to the lungs within the pulmonary circuit and oxygen-rich The heart has four muscular chambers, two associated with
blood to the rest of the body within the systemic circuit. The each circuit—in essence, the heart is two side-by-side pumps.
.
pulmonary circuit carries oxygen-poor blood from the heart’s The right atrium (A-tre-um; entry chamber; plural, atria) receives
.
lower right chamber (right ventricle), through the pulmonary blood from the systemic circuit and passes it to the right ven-
arteries, to the lungs, and oxygen-rich blood back through tricle (VEN-tri-kul; little belly), which then pumps blood into
the pulmonary veins to the heart’s upper left chamber (left the pulmonary circuit. The left atrium collects blood from the
atrium). The systemic circuit carries oxygen-rich blood from the pulmonary circuit and empties it into the left ventricle, which
heart’s lower left chamber (left ventricle), through the systemic pumps blood into the systemic circuit. When the heart beats,
689
M20_MART6026_11_SE_C20_pp688-726.indd 689 04/11/16 11:02 pm
690 UNIT 4 Fluids and Transport
first the atria contract, and then the ventricles contract. The two
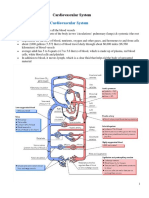
Figure 20–1 An Overview of the Cardiovascular Sys- ventricles contract at the same time and eject equal volumes of
tem. Driven by the pumping of the heart, blood flows through the blood into the pulmonary and systemic circuits.
pulmonary and systemic circuits in sequence. Each circuit begins
and ends at the heart and contains arteries, capillaries, and veins. Heart Location and Position
The heart is located in the thoracic cavity near the anterior chest
Systemic wall, directly posterior to the sternum (Figure 20–2a,b). The
Circuit
great vessels, both veins and arteries, are connected to the supe-
Capillaries rior end of the heart at its base. The base sits posterior to the
in head and sternum at the level of the third costal cartilage, centered about
Pulmonary neck
Circuit 1.2 cm (0.5 in.) to the left side (Figure 20–3a). The inferior,
pointed tip of the heart is the apex (A-peks). Standard measure-
.
Pulmonary ments for determining heart size take into account age, height,
Systemic
arteries
arteries weight, and sex. A midsagittal section through the trunk does
Capillaries Left not divide the heart into two equal halves. Note that the center
in lungs atrium
of the base lies slightly to the left of the midline.
Pulmonary Left
ventricle The heart sits in the anterior portion of the mediasti-
veins
Capillaries in num, the region between the two pleural cavities. The medias-
abdominal tinum contains the great vessels, which are attached at the base
Right atrium organs
of the heart, as well as the thymus, esophagus, and trachea.
Right Figure 20–2b is a superior view that shows the position of the
ventricle
Systemic heart relative to other structures in the mediastinum.
veins
Heart Superficial Anatomy, Heart Wall, and
Cardiac Skeleton
The walls of the heart, from deep to superficial, are the endocar-
dium (inner layer whose simple squamous epithelium is con-
tinuous with the endothelial lining of blood vessels), myocardium
20 (spiral bundles of cardiac muscle cells), and pericardium (fibrous
Pulmonary Circuit Capillaries in pericardium and serous pericardium that protect, anchor, and
upper limbs
Pulmonary prevent overfilling). The two-layered serous pericardium is made
arteries up of a parietal layer and a visceral layer (epicardium). These
Pulmonary layers are separated by a fluid-filled pericardial cavity. Another
veins structure, the cardiac skeleton, is a crisscrossing, interlacing layer
Capillaries
in trunk and of dense connective tissue that anchors muscle fibers, supports
lower limbs
the great vessels and heart valves, and limits the spread of action
potentials. Our discussion begins with the pericardium.
Systemic Circuit
Outer Covering of the Heart: The Pericardium
Systemic
arteries The pericardium (pehr-ih-KAR-de-um) surrounds the heart
.
Systemic and consists of an outer fibrous pericardium and an inner serous
veins pericardium. The fibrous pericardium contains a dense network
of collagen fibers that stabilize the position of the heart and
associated vessels within the mediastinum.
The inner serous pericardium is a two-layered membrane
composed of an outer parietal layer and an inner visceral
layer. The visceral layer is also known as the epicardium. The
? The ___________ side of the heart supplies blood to the potential, fluid-filled space between these two serous layers is
systemic circuit, while the ___________ side of the heart the pericardial cavity.
supplies blood to the pulmonary circuit.
The pericardial cavity normally contains 15–50 mL of
pericardial fluid, secreted by the pericardial membranes.
This fluid acts as a lubricant, reducing friction between the oppos-
ing visceral and parietal surfaces as the heart beats. To visualize
M20_MART6026_11_SE_C20_pp688-726.indd 690 24/10/16 8:13 PM
Chapter 20 The Heart 691
Figure 20–2 The Location of the Heart in the Thoracic Cavity. ATLAS: Plates 47a,b
Trachea
Thyroid gland
First rib (cut)
Base of heart
Right lung Left lung
Apex of heart
a An anterior view of the chest, showing Diaphragm
the position of the heart and major blood
vessels relative to the ribs, lungs, and diaphragm.
Posterior mediastinum
Esophagus Aorta (arch segment removed)
Left pulmonary artery
Right pleural cavity
Left pleural cavity
Right Left
lung lung
Left pulmonary vein
Bronchus of lung
Right pulmonary artery Pulmonary trunk
Aortic 20
arch Left atrium
Right pulmonary vein
Left ventricle
Superior vena cava
Pericardial cavity
Right atrium
Visceral layer (epicardium)
Right ventricle
Pericardium
Anterior mediastinum Sternum
b A superior view of the organs in the mediastinum; portions of the lungs have been removed to reveal blood vessels
and airways. The heart is located in the anterior part of the mediastinum, immediately posterior to the sternum.
Cut edge of parietal layer Wrist (corresponds
Base of heart
to base of heart)
Fibrous pericardium
Inner wall (visceral layer
Parietal Layer of of serous pericardium)
Serous Pericardium
Air space (corresponds
Areolar tissue
to pericardial cavity)
Mesothelium
Outer wall (parietal layer
Cut edge of visceral layer of of serous pericardium)
serous pericardium (epicardium)
Fibrous attachment
to diaphragm Apex of heart Balloon
c The relationship between the heart and the pericardial cavity; compare with the fist-and-balloon example.
M20_MART6026_11_SE_C20_pp688-726.indd 691 24/10/16 8:13 PM
692 UNIT 4 Fluids and Transport
Figure 20–3 The Position and Superficial Anatomy of the Heart.
Left common Left subclavian artery
carotid artery
Brachiocephalic Ligamentum
Arch of arteriosum
trunk
Base of heart aorta
Descending
aorta
1 1 Ascending
aorta Left pulmonary
artery
Ribs Superior
2 2 vena cava Pulmonary
trunk
3 3 Auricle
Auricle of
of right Right left atrium
atrium atrium
4 4
Right Fat and vessels
5 5 in anterior
ventricle
interventricular
6
6 sulcus
Fat and
7 7 Apex of Left
vessels in
heart coronary ventricle
8 8
9 sulcus
9
10 10
a Heart position relative to the rib cage. b Major anatomical features on the anterior surface.
Left subclavian artery
Left common carotid Arch of aorta
artery Left pulmonary artery
Ligamentum Right pulmonary
Brachiocephalic trunk arteriosum Left pulmonary veins artery
Left pulmonary Fat and vessels
Ascending artery Superior
aorta in coronary vena cava
Left
Pulmonary sulcus
Superior atrium
20 trunk
vena cava Coronary Right
Auricle of left atrium sinus pulmonary
Auricle of Left coronary artery veins
right atrium (LCA) Right (superior
Left atrium and inferior)
Right atrium Anterior ventricle
interventricular
Right Right sulcus
coronary ventricle Right Inferior
artery Left ventricle vena cava
ventricle
Coronary sulcus
Anterior
interventricular Fat and vessels in posterior
Marginal branch branch of LCA interventricular sulcus
of right coronary artery
d Major anatomical features on the posterior surface.
Coronary arteries (which supply the heart itself) are
c Anterior surface of the heart, cadaver dissection. shown in red; coronary veins are shown in blue.
the relationship between the heart and the pericardial cavity, scratching sound (called a friction rub) that can be heard through
imagine pushing your fist toward the center of a large, partially an instrument called a stethoscope that is placed on the chest. The
inflated balloon. The balloon represents the pericardium, and pericardial inflammation also commonly results in increased
your fist is the heart. Your wrist, where the balloon folds back on production of pericardial fluid. Fluid then collects in the peri-
itself, corresponds to the base of the heart (Figure 20–2c). cardial cavity, restricting the movement of the heart. This condi-
tion, called cardiac tamponade (tam-po-NAD; tampon, plug),
.
Pathogens can infect the pericardium, producing inflam-
.
mation and the condition pericarditis. The inflamed peri- can also result from traumatic injuries (such as stab wounds)
cardial surfaces rub against one another, making a distinctive that produce bleeding into the pericardial cavity.
> Go to > Study Area > Menu > Lab Tools > 3.0 > Anatomical Models > Cardiovascular System > Heart
M20_MART6026_11_SE_C20_pp688-726.indd 692 02/11/16 2:35 pm
Chapter 20 The Heart 693
Superficial Anatomy of the Heart endocardium (Figure 20–4a). The details of these three layers,
The four chambers of the heart can be identified in a superficial from superficial to deep, are covered in the following list.
view (see Figure 20–3). The two atria have relatively thin mus- 1. The visceral layer of serous pericardium (epicardium)
cular walls and are highly expandable. When not filled with covers the surface of the heart. This serous membrane consists
blood, the outer portion of each atrium deflates and becomes a of an exposed mesothelium and an underlying layer of areo-
lumpy, wrinkled flap. This expandable extension of an atrium is lar connective tissue that is attached to the myocardium. The
called an auricle (AW-rih-kul; auris, ear), because it reminded parietal layer of serous pericardium consists of an outer
early anatomists of the external ear (Figure 20–3b). dense fibrous layer, an areolar layer, and an inner mesothelium.
The coronary sulcus, a deep groove, marks the border
2. The myocardium is cardiac muscle tissue that forms the atria
between the atria and the ventricles. The anterior interven-
and ventricles. This muscular layer contains cardiac muscle
tricular sulcus and the posterior interventricular sulcus
cells, connective tissues, blood vessels, and nerves. The atrial
are shallower depressions that mark the boundary between the
myocardium contains muscle bundles that wrap around
left and right ventricles (Figure 20–3b–d). Substantial amounts
the atria and form figure eights that encircle the great vessels
of fat generally lie in the coronary and interventricular sulci.
(Figure 20–4b). Superficial ventricular muscles wrap around
In fresh or preserved hearts, this fat must be stripped away to
both ventricles, and deeper muscle layers spiral around and
expose the underlying grooves. These sulci also contain the
between the ventricles toward the apex in a figure-eight pattern.
arteries and veins that carry blood to and from the cardiac
muscle. 3. The endocardium covers the inner surfaces of the heart,
including those of the heart valves. It is made up of a sim-
The Heart Wall ple squamous epithelium and underlying areolar tissue.
A section through the wall of the heart reveals three distinct lay- This simple squamous epithelium, or endothelium, is con-
ers: the outer epicardium, a middle myocardium, and an inner tinuous with the endothelium of the attached great vessels.
Figure 20–4 The Heart Wall.
Pericardial cavity Parietal Layer of
Myocardium Serous Pericardium
Cardiac Dense fibrous layer
muscle cells
Areolar tissue
20
Connective
tissues Mesothelium
Artery
Vein
Endocardium
Endothelium Visceral Layer of
Serous Pericardium
Areolar tissue
Mesothelium
Areolar tissue
all
rt w
Atrial musculature Hea
forms bands that wrap
around the atria in a
figure-eight pattern
a A diagrammatic section through the heart wall, showing the
relative positions of the myocardium, pericardium, and
Ventricular endocardium. The proportions are not to scale; the
musculature forms thickness of the myocardial wall has been greatly reduced.
bands that spiral
around the ventricles
b Cardiac muscle tissue forms concentric
layers that wrap around the atria or spiral
within the walls of the ventricles.
M20_MART6026_11_SE_C20_pp688-726.indd 693 24/10/16 8:13 PM
694 UNIT 4 Fluids and Transport
Connective Tissues and the Cardiac Skeleton From the fifth week of embryonic development until birth,
The connective tissues of the heart include large numbers of an oval opening called the foramen ovale penetrates the inter-
collagen and elastic fibers. Each cardiac muscle cell is wrapped atrial septum and connects the two atria of the fetal heart. Before
in a strong, but elastic, sheath. Adjacent cells are tied together birth, the foramen ovale permits blood to flow from the right
by fibrous cross-links, or “struts.” These fibers are, in turn, inter- atrium to the left atrium while the lungs are developing. At birth,
woven into sheets that separate the superficial and deep muscle the foramen ovale closes, and the opening is permanently sealed
layers. The connective tissue fibers (1) provide physical sup- off within 3 months of delivery. (If the foramen ovale does not
port for the cardiac muscle fibers, blood vessels, and nerves of close, serious cardiovascular problems may result. We consider
the myocardium; (2) help distribute the forces of contraction; these in Chapter 21.) A small, shallow depression called the fossa
(3) add strength and prevent overexpansion of the heart; and ovalis remains at this site in the adult heart (see Figure 20–5a).
(4) provide elasticity that helps return the heart to its original ATLAS: Embryology Summary 15: The Development of the Heart
size and shape after a contraction. The posterior walls of the right atrium and the interatrial sep-
The cardiac skeleton (sometimes called the fibrous skel- tum have smooth surfaces. In contrast, the anterior atrial wall and
eton) of the heart consists of four dense bands of tough elastic the inner surface of the auricle contain prominent muscular ridges
tissue that encircle the heart valves and the bases of the pulmo- called the pectinate muscles (pectin, comb) (see Figure 20–5a).
nary trunk and aorta (look ahead to Figure 20–7). These bands Blood travels from the right atrium into the right ventricle
stabilize the positions of the heart valves and ventricular muscle through a broad opening bordered by three fibrous flaps. These
flaps, called cusps, are part of the tricuspid (trı-KUS-pid; tri,
.
cells. They also electrically insulate the ventricular cells from
the atrial cells. three) valve, also known as the right atrioventricular (AV) valve.
The free edge of each cusp is attached to connective tissue
fibers called the chordae tendineae (KOR-de TEN-dih-ne-e;
. . .
Heart Chambers, Valves, and Great Vessels
tendinous cords). The fibers originate at the papillary (PAP-ih-
Next let’s examine the major landmarks and structures visible lehr-e) muscles, conical muscular projections that arise from
.
on the interior surface of the heart. In a sectional view, you can the inner surface of the right ventricle (Figure 20–5c).
see that the right atrium communicates with the right ventricle,
and the left atrium with the left ventricle (Figure 20–5a,b). Tips & Tools
The chambers of the heart are separated by muscular partitions
called septa (singular septum, wall). The atria are separated by The saying “To tug on your heartstrings” may help you
remember the functions of the papillary muscles and the
the interatrial septum, and the ventricles are separated by
20 the much thicker interventricular septum. The heart also has chordae tendineae: Contractions of the papillary muscles pull
on the chordae tendineae, which “tug” on your heart’s valves.
valves, covered openings that direct the flow of blood between
chambers and vessels. The cardiac skeleton stabilizes the posi-
tions of these valves. The two atrioventricular (AV) valves The Right Ventricle, Pulmonary Valve, and
(tricuspid and mitral) are folds of fibrous tissue that extend Pulmonary Trunk
into the openings between the atria and ventricles. These valves The internal surface of the right ventricle contains a series
permit blood to flow only in one direction: from the atria to of muscular ridges: the trabeculae carneae (trah-BEK-yu-
.
the ventricles. There are also two semilunar valves (pulmonary le KAR-ne-e; carneus, fleshy). The moderator band is a muscular
. . .
and aortic) between the ventricles and their great vessels, which ridge that extends horizontally from the inferior portion of the
ensure blood flows into these vessels. interventricular septum and connects to the anterior papillary
muscle. The moderator band delivers the stimulus for contrac-
The Vena Cavae, Right Atrium, and tion to the papillary muscles. As a result, they begin tensing the
Tricuspid Valve chordae tendineae before the rest of the ventricle contracts.
The right atrium receives blood from the systemic circuit The superior end of the right ventricle tapers to the conus
through the two great veins: the superior vena cava (VE-nah arteriosus, a cone-shaped pouch that ends at the pulmonary
.
KA-vuh; venae cavae, plural) and the inferior vena cava. The valve, or pulmonary semilunar valve. The pulmonary valve consists
.
superior vena cava opens into the posterior and superior por- of three semilunar (half-moon shaped) cusps of thick connec-
tion of the right atrium. It delivers blood to the right atrium tive tissue. Blood flowing from the right ventricle passes through
from the head, neck, upper limbs, and chest. The inferior vena this valve into the pulmonary trunk, the start of the pulmonary
cava opens into the posterior and inferior portion of the right circuit. Once in the pulmonary trunk, blood flows into the left
atrium. It carries blood to the right atrium from the rest of the pulmonary arteries and the right pulmonary arteries. These
trunk, the viscera, and the lower limbs. Note there are no valves vessels branch repeatedly within the lungs before supplying the
between the venae cavae and the right atrium. capillaries, where gas exchange occurs.
M20_MART6026_11_SE_C20_pp688-726.indd 694 24/10/16 8:13 PM
Chapter 20 The Heart 695
Figure 20–5 The Sectional Anatomy of the Heart.
Left common carotid artery
Left subclavian artery
Brachiocephalic trunk
Ligamentum arteriosum
Aortic arch Pulmonary trunk
Superior
vena cava Pulmonary valve
Right pulmonary Left pulmonary arteries
arteries
Ascending aorta Left pulmonary veins
Fossa ovalis Left
atrium
Opening of coronary sinus Interatrial septum
Aortic valve
Right atrium
Cusp of mitral valve
Pectinate muscles
Chordae tendineae
Conus arteriosus
Left ventricle
Cusp of tricuspid valve
Interventricular septum
Papillary muscle
Trabeculae carneae
Right ventricle
Inferior vena cava
Moderator band
a A diagrammatic frontal section through the heart, showing Descending aorta
anatomical features and the path of blood flow (marked by
arrows) through the atria, ventricles, and associated vessels.
20
Left subclavian artery
Left common carotid artery
Brachiocephalic trunk
Superior vena cava
Ascending aorta
Pulmonary trunk
Cusp of
pulmonary valve
Auricle of left atrium
Right atrium
Cusp of mitral valve
Chordae tendineae
Cusp of
Papillary muscles tricuspid valve
Right ventricle
Left ventricle
b Papillary muscles and chordae c Anterior view of a
Trabeculae carneae
tendineae support the mitral valve frontally sectioned
and tricuspid valve. heart showing internal Interventricular
features and valves. septum
? Beginning with the right atrium, what is the order of the valves through which blood will pass?
M20_MART6026_11_SE_C20_pp688-726.indd 695 24/10/16 8:13 PM
696 UNIT 4 Fluids and Transport
The Pulmonary Veins, Left Atrium, Anatomical differences between the left and right ventricles
and Mitral Valve are easiest to see in a three-dimensional view (Figure 20–6a).
From the respiratory capillaries, blood collects into small veins The lungs are close to the heart, and the pulmonary blood ves-
that ultimately unite to form the four pulmonary veins. The sels are relatively short and wide. For these reasons, the right
posterior wall of the left atrium receives blood from two ventricle normally does not need to work very hard to push
left and two right pulmonary veins. Again there is no valve blood through the pulmonary circuit. Accordingly, the muscu-
between the pulmonary veins and the left atrium. Like the right lar wall of the right ventricle is relatively thin. In sectional view,
atrium, however, the left atrium has an auricle. it resembles a pouch attached to the massive wall of the left ven-
A valve, the mitral (MI-tral; mitre, a bishop’s hat) valve tricle. When the right ventricle contracts, it acts like a bellows,
.
(also called the left atrioventricular [AV] valve, or bicuspid valve) squeezing the blood against the thick wall of the left ventricle.
guards the entrance to the left ventricle (see Figure 20–5a,c). As This action moves blood very efficiently with minimal effort,
the name bicuspid implies, the left AV valve contains two cusps, but it develops relatively low pressures.
not three. The mitral valve permits blood to flow from the left A comparable pumping arrangement would not work well
atrium into the left ventricle. for the left ventricle. Four to six times as much pressure must
be exerted to push through the systemic circuit as through the
Tips & Tools pulmonary circuit. The left ventricle has an extremely thick
To remember the locations of the tricuspid and bicuspid
try to be right” for the tricuspid, and
(mitral) valves, think “try Figure 20–6 Structural Differences between the Left and
associate the l in mitral with the l in left. Right Ventricles. ATLAS: Plate 45d
Posterior Left
The Left Ventricle, Aortic Valve, and Ascending Aorta
interventricular sulcus ventricle
The internal organization of the left ventricle resembles
that of the right ventricle, but it has no moderator band (see
Figure 20–5a). The trabeculae carneae are prominent. A pair
of large papillary muscles tenses the chordae tendineae that
anchor the cusps of the mitral valve and prevent blood from
flowing back into the left atrium.
20 Blood leaves the left ventricle through the aortic valve, Right
or aortic semilunar valve, and enters the ascending aorta. The ventricle
arrangement of cusps in the aortic valve is the same as that in the
pulmonary valve. Adjacent to each cusp of the aortic valve are
saclike expansions of the base of the ascending aorta called aortic
sinuses. From the ascending aorta, blood flows through the aor-
tic arch and into the descending aorta (see Figure 20–5a). The
pulmonary trunk is attached to the aortic arch by the ligamentum
Fat in anterior
arteriosum, a fibrous band left over from an important fetal blood interventricular sulcus
vessel that once linked the pulmonary and systemic circuits.
a A diagrammatic sectional view through the heart,
Structural and Functional Differences between showing the relative thicknesses of the two ventricular
the Left and Right Ventricles walls. Note the pouchlike shape of the right ventricle
The function of the atria is to collect blood that is returning to the and the greater thickness of the left ventricular muscle.
heart and to convey it to the ventricles. The demands on the right
and left atria are similar, and the two chambers look almost identi- Right Left
cal. The demands on the right and left ventricles, however, are very ventricle ventricle
different, and the two have significant structural differences. Even
though the two ventricles hold and pump equal amounts of blood,
the left ventricle is much larger than the right ventricle. What’s the
reason? It has thicker walls. These thick, muscular walls enable the Dilated Contracted
left ventricle to push blood through the body’s extensive systemic b Diagrammatic views of the ventricles just before a
circuit. In contrast, the right ventricle needs to pump blood, at contraction (dilated) and just after a contraction
lower pressure, only about 15 cm (6 in.) to and from the lungs. (contracted).
M20_MART6026_11_SE_C20_pp688-726.indd 696 24/10/16 8:13 PM
Chapter 20 The Heart 697
muscular wall and is round in cross section (see Figure 20–6a). The Semilunar Valves: Ventricles to Great Vessels
When this ventricle contracts, it shortens and narrows. In other The pulmonary and aortic semilunar valves prevent the backflow
words, (1) the distance between the base and apex decreases, and of blood from the pulmonary trunk and aorta into the right and
(2) the diameter of the ventricular chamber decreases. The effect left ventricles, respectively. Unlike the AV valves, the semilunar
is similar to simultaneously squeezing and rolling up the end of valves do not need muscular braces, because the arterial walls
a toothpaste tube. The pressure generated is more than enough do not contract and the relative positions of the cusps are stable.
to open the aortic valve and eject blood into the ascending aorta. When the semilunar valves close, the three symmetrical cusps
As the powerful left ventricle contracts, it bulges into the support one another like the legs of a tripod (see Figure 20–7a).
right ventricular cavity (Figure 20–6b). This action increases the When the aortic valve opens, the aortic sinuses prevent the individ-
pumping efficiency of the right ventricle. Individuals with severe ual cusps from sticking to the wall of the aorta (see Figure 20–7b).
damage to the right ventricle may survive, because the contrac- Serious valve problems can interfere with the working of
tion of the left ventricle helps push blood into the pulmonary the heart. If valve function deteriorates to the point at which
circuit. We return to this topic in Chapter 21, where we consider the heart cannot maintain adequate circulatory flow, symptoms
the integrated functioning of the cardiovascular system. of valvular heart disease (VHD) appear. Congenital malfor-
mations may be responsible, but in many cases the condition
Blood Flow through the Heart Valves develops after carditis, an inflammation of the heart, occurs.
As we have seen, the heart has two pairs of one-way valves. One important cause of carditis is rheumatic (ru-MAT-ik)
.
These valves prevent the backflow of blood as the chambers fever, an inflammatory autoimmune response to an infection
contract. Let’s look at the function of these heart valves, and the by streptococcal bacteria. It most often occurs in children.
path of blood flow through each half of the heart.
The Blood Supply to the Heart
The AV Valves: Atria to Ventricles
The heart works continuously, so cardiac muscle cells need reli-
The atrioventricular (AV) valves prevent the backflow of blood
able supplies of oxygen and nutrients. A great volume of blood
from the ventricles to the atria when the ventricles are con-
flows through the chambers of the heart, but the myocardium
tracting. The chordae tendineae and papillary muscles play
has its own, separate blood supply. The coronary circulation
important roles in the normal function of the AV valves. When
supplies blood to the muscle tissue of the heart. During maxi-
the ventricles are relaxed, the chordae tendineae are loose, and
mum exertion, the heart’s demand for oxygen rises consider-
the AV valves offer no resistance as blood flows from the atria
ably. The blood flow to the myocardium may then increase to
into the ventricles (Figure 20–7a). When the ventricles contract, 20
nine times that of the resting level. The coronary circulation
blood moving back toward the atria swings the cusps together,
includes an extensive network of coronary blood vessels, both
closing the valves (Figure 20–7b). At the same time, the con-
arteries and veins (Figure 20–8).
traction of the papillary muscles tenses the chordae tendineae,
stopping the cusps before they swing into the atria. If the chor-
The Coronary Arteries
dae tendineae were cut or the papillary muscles were damaged,
backflow, called regurgitation, of blood into the atria would The left and right coronary arteries originate at the base of
occur each time the ventricles contracted. the ascending aorta, at the aortic sinuses (Figure 20–8a). Blood
pressure here is the highest in the systemic circuit. When the
left ventricle contracts and forces blood into the aorta, the high
+ Clinical Note Faulty Heart Valves pressure of this blood stretches the elastic walls of the aorta.
When the left ventricle relaxes, blood no longer flows into the
aorta, pressure declines, and the walls of the aorta recoil. This
Each of the four heart valves must open and close crisply and recoil, called elastic rebound, pushes blood both forward, into
precisely to permit the proper flow of blood through the heart.
the systemic circuit, and backward, through the left and right
The most common valve to falter is the mitral valve. One
aortic sinuses and then into the respective coronary arteries.
scenario responsible for mitral malfunction is an untreated bac-
terial or viral infection that infiltrates the valve cusps. The cusps
In this way, the combination of elevated blood pressure and
become inflamed and later scar, resulting in a faulty valve. elastic rebound ensures a continuous flow of blood to meet the
A valve can malfunction in one of three ways: (1) It can demands of active cardiac muscle tissue.
become rigid (a stenotic valve) so that it does not open fully, The right and left coronary arteries, which deliver blood to
(2) it can fail to close properly (a regurgitant valve), or (3) it can the myocardium, originate at the right and left aortic sinuses.
actually flop backwards (a prolapsed valve). Faulty valves are The right coronary artery follows the coronary sulcus around
heard as heart murmurs with a stethoscope. the heart (see Figure 20–8). It supplies blood to (1) the right
atrium, (2) portions of both ventricles, and (3) portions of the
M20_MART6026_11_SE_C20_pp688-726.indd 697 24/10/16 8:13 PM
698 UNIT 4 Fluids and Transport
Figure 20–7 Valves of the Heart and Blood Flow. Red (oxygenated) and blue (deoxygenated) arrows indicate
blood flow into or out of a ventricle, smaller red arrows show blood flow into an atrium, and green arrows indicate
contraction of the ventricles.
Transverse Sections, Superior View, Frontal Sections through Left Atrium and Ventricle
Atria and Vessels Removed
POSTERIOR
Cardiac Mitral
skeleton valve (open) Pulmonary
veins
Right Left
ventricle ventricle Left
atrium
Mitral valve
Relaxed ventricles
(open)
Chordae
Aortic valve
tendineae (loose)
(closed)
Tricuspid Papillary muscles
valve (open) (relaxed)
Left ventricle
Aortic valve (relaxed and filling
(closed) with blood)
Pulmonary
ANTERIOR
valve (closed)
a When the ventricles are relaxed, the tricuspid and mitral valves are
open and the aortic and pulmonary valves are closed. The chordae
Aortic valve closed tendineae are loose, and the papillary muscles are relaxed.
20
Tricuspid valve Cardiac Mitral valve
(closed) skeleton (closed)
Right Left Left
Aorta
ventricle ventricle atrium
Contracting ventricles
Aortic sinus Mitral valve
(closed)
Aortic valve
(open) Chordae tendineae
(tense)
Papillary muscles
(contracted)
Aortic valve Left ventricle
(open) (contracted)
Pulmonary
valve (open)
b When the ventricles are contracting, the tricuspid and mitral
valves are closed and the aortic and pulmonary valves are open.
In the frontal section, note the attachment of the mitral valve to
Aortic valve open the chordae tendineae and papillary muscles.
M20_MART6026_11_SE_C20_pp688-726.indd 698 24/10/16 8:13 PM
Chapter 20 The Heart 699
Figure 20–8 The Coronary Circulation. ATLAS: Plates 45b,c
Coronary sinus
Circumflex artery
Aortic Left coronary
arch artery Great cardiac vein
Marginal artery
Ascending Posterior
Pulmonary
aorta interventricular
trunk
artery
Right Circumflex
coronary artery Posterior
artery vein of left
Anterior ventricle
interventricular
Atrial Left
artery
arteries ventricle
Great Small
Right cardiac cardiac
Anterior ventricle vein vein
cardiac
veins Right
coronary
Small artery
cardiac Middle cardiac vein Marginal artery
vein
b Coronary vessels supplying and draining
Marginal
artery a Coronary vessels supplying the posterior surface of the heart.
and draining the anterior
surface of the heart. Left pulmonary
Left pulmonary
Auricle of veins artery
left atrium
electrical conducting system of the heart. Inferior to the right Right
Circumflex pulmonary
atrium, the right coronary artery generally gives rise to one artery artery
or more marginal arteries, which extend across the surface
Great cardiac Superior
of the right ventricle. The right coronary artery then contin- vein vena cava
ues across the posterior surface of the heart. It supplies the Marginal 20
posterior interventricular artery, or posterior descend- artery Right
pulmonary
ing artery, which runs toward the apex within the posterior Posterior vein veins
interventricular sulcus. The posterior interventricular artery of left ventricle
Left atrium
supplies blood to the interventricular septum and adjacent
portions of the ventricles. Right atrium
The left coronary artery supplies blood to the left
ventricle, left atrium, and interventricular septum (see Inferior
Figure 20–8). As it reaches the anterior surface of the heart, vena cava
it gives rise to a circumflex branch and an anterior inter- Coronary sinus
ventricular branch. The circumflex artery curves to the left
Middle cardiac vein
around the coronary sulcus. It eventually meets and fuses
with small branches of the right coronary artery. Right ventricle
The much larger anterior interventricular artery, or Posterior interventricular artery
left anterior descending artery (LAD), swings around the pul- c A posterior view of the heart; the vessels have been
monary trunk and runs along the surface within the anterior injected with colored latex (liquid rubber).
interventricular sulcus. The anterior interventricular artery
supplies small tributaries continuous with those of the pos- Coronary artery disease is characterized by interrupted
terior interventricular artery. Such interconnections between blood flow to the myocardium. Spotlight Figure 20–9 describes
arteries are called arterial anastomoses (ah-nas-to-MO-
.
this condition, along with myocardial infarction.
sez; anastomosis, outlet). Because the arteries are intercon-
.
nected in this way, the blood supply to the cardiac muscle The Cardiac Veins
remains relatively constant despite pressure fluctuations in The various cardiac veins are also shown in Figure 20–8.
the left and right coronary arteries as the heart beats. The great cardiac vein begins on the anterior surface of the
M20_MART6026_11_SE_C20_pp688-726.indd 699 24/10/16 8:13 PM
SPOTLIGHT
Figure 20–9
Heart Disease and Heart Attacks
Coronary Artery Disease
HEART DISEASE
The term coronary artery disease (CAD) refers to
areas of partial or complete blockage of coronary
circulation. Cardiac muscle cells need a constant supply
of oxygen and nutrients, so any reduction in blood flow to
the heart muscle produces a corresponding reduction in
cardiac performance. Such reduced circulatory supply,
known as coronary ischemia (iss-KĒ-mē-uh), generally
results from partial or complete blockage of the coronary
arteries. The usual cause is the formation of a fatty
deposit, or atherosclerotic plaque, in the wall of a
coronary vessel. The plaque, or an associated thrombus
(clot), then narrows the passageway and reduces blood
flow. Spasms in the smooth muscles of the vessel wall Advanced
C
A color-enha oronary Artery Dise
can further decrease or even stop blood flow. One of the coronary ar
nced DSA
scan show se
a
Normal Heart te ing
first symptoms of CAD is commonly angina pectoris A color-enhanced digital ventricular ry disease. Blood flow advanced
myocardium to the
(an-JĪ-nuh PEK-tor-is; angina, pain spasm + pectoris, of subtraction angiography is severely
restricted.
the chest). In its most common form, a temporary (DSA) scan of a normal heart.
ischemia develops when the workload of the heart
increases. Although the individual may feel comfortable Plaques may be visible by angiography or high-resolution
at rest, exertion or emotional stress can produce a ultrasound, and the effects on coronary blood flow can be
sensation of pressure, chest constriction, and pain that detected in digital subtraction angiography (DSA) scans of
may radiate from the sternal area to the arms, back, the heart as shown above.
and neck.
Normal Artery Narrowing of Artery
Tunica Atherosclerotic
externa plaque
Tunica
media
Cross section Cross section
Left: Chest pain or discomfort is a common symptom
of angina pectoris. Although similar symptoms may
accompany a heart attack, during a heart attack, pain
often radiates down the left arm.
Below: The presence of any two of these coronary risk
factors more than doubles the risk of heart attack.
Risk Factors for CAD and Myocardial Infarction
M20_MART6026_11_SE_C20_pp688-726.indd 700 24/10/16 8:13 PM
Myocardial Infarction
HEART ATTACK
Occluded
coronary Treatment of CAD and Myocardial Infarction
artery
About 25% of MI patients die before obtaining medical assistance,
and 65% of MI deaths among those under age 50 occur within an
hour after the initial infarction.
Damaged
heart Risk Factor Modification
muscle Stop smoking, treat high blood pressure, adjust diet
to lower cholesterol and promote weight loss, reduce
stress, and increase physical activity.
Drug Treatment
In a myocardial (mī-ō-KAR-dē-al) infarction (MI), or • Drugs that reduce coagulation and therefore the risk
heart attack, part of the coronary circulation becomes of thrombosis, such as aspirin and coumadin
• Drugs that block sympathetic stimulation
blocked, and cardiac muscle cells die from lack of oxygen. (propranolol or metoprolol)
The death of affected tissue creates a nonfunctional area • Drugs that cause vasodilation, such as nitroglycerin
known as an infarct. Heart attacks most commonly result (nī-trō-GLIS-er-in)
from severe coronary artery disease (CAD). The conse- • Drugs that block calcium ion movement into the
quences depend on the site and nature of the circulatory cardiac and vascular smooth muscle cells (calcium
ion channel blockers)
blockage. If it occurs near the start of one of the coronary • In a myocardial infarction, drugs to relieve pain,
arteries, the damage will be widespread and the heart fibrinolytic agents to help dissolve clots, and oxygen
may stop beating. If the blockage involves one of the
smaller arterial branches, the individual may survive the Noninvasive Surgery
immediate crisis but may have many complications such • Atherectomy. Blockage by a single, soft plaque may
as reduced contractility and cardiac arrhythmias. be reduced with the aid of a long, slender catheter
A crisis often develops as a result of thrombus (KATH-e-ter) inserted into a coronary artery to the
formation at a plaque (the most common cause of an MI), plaque. A variety of surgical tools can be slid into the
catheter, and the plaque can then be removed.
a condition called coronary thrombosis. A vessel already • Balloon angioplasty (AN-jē-ō-plas-tē; angeion,
narrowed by plaque formation may also become blocked by vessel). In balloon angioplasty, the tip of the catheter
a sudden spasm in the smooth muscles of the vascular wall. contains an inflatable balloon. Once in position, the
Individuals having an MI experience intense pain, similar balloon is inflated, pressing the plaque against the
to that felt in angina, but persisting even at rest. However, vessel walls. Because plaques commonly redevelop
after angioplasty, a fine tubular wire mesh called a
pain does not always accompany a heart attack, and silent stent may be inserted into the vessel, holding it open.
heart attacks may be even more dangerous than more
apparent attacks, because the condition may go undiag- Coronary Artery Bypass Graft (CABG)
nosed and may not be treated before a fatal MI occurs. A In a coronary artery bypass graft, a small section is
myocardial infarction can usually be diagnosed with an removed from either a small artery or a peripheral vein
electrocardiogram (ECG) and blood studies. Damaged and is used to create a detour around the obstructed
myocardial cells release enzymes into the circulation, and portion of a coronary artery. As many as four coronary
arteries can be rerouted this way during a single
these elevated enzymes can be measured in diagnostic operation. The procedures are named according to the
blood tests. The enzymes include cardiac troponin T, number of vessels repaired, so we speak of single,
cardiac troponin I, and a special form of creatinine phos- double, triple, or quadruple coronary bypasses.
phokinase, CK-MB.
M20_MART6026_11_SE_C20_pp688-726.indd 701 24/10/16 8:13 PM
702 UNIT 4 Fluids and Transport
Next we start to look at how the heart works—cardiac physiol-
+ Clinical Note Broken-Heart Syndrome ogy. Then we examine the structure and function of the dif-
ferent types of cardiac muscle cells. Some form the conducting
The popular notion that grief can “break your heart” finds system, an internal network that uses electrical signals to coor-
support in the novel diagnosis of broken-heart syndrome, dinate the contractions of cardiac muscle cells. The electrical
also called stress-induced cardiomyopathy. First noted in events of the heart can then be recorded in an electrocardiogram
Japan in the early 2000s, elderly women were presenting (ECG). Finally we discuss the contraction of the heart at the
with apparent heart attacks. The precipitating event was an cellular level.
acute emotional stress, such as the death of a loved one.
The women’s ECGs were abnormal; their left ventricles
Cardiac Physiology: Electrical Impulses
were significantly dilated. But their coronary arteries—the
Leading to the Contractions Making Up a
site of the lesions responsible for heart attacks—were clear!
All of these changes reverted to normal within a month of
Heartbeat
supportive care. In a single cardiac contraction, or heartbeat, all of the cham-
bers of the heart contract in series—first the atria and then the
ventricles. Two types of cardiac muscle cells are involved in a
normal heartbeat: (1) Specialized autorhythmic cells (pacemaker
ventricles, along the interventricular sulcus. This vein drains
and conducting) of the conducting system control and coordi-
blood from the region supplied by the anterior interventricular
nate the heartbeat, and (2) contractile cells produce the power-
artery, a branch of the left coronary artery. The great cardiac vein
ful contractions that propel blood. The electrical impulses of
reaches the level of the atria and then curves around the left side
the conducting system initiate the contraction of the heart
of the heart within the coronary sulcus.
chambers.
The cardiac veins draining the myocardium return blood to
Each heartbeat begins with an action potential gener-
the coronary sinus, a large, thin-walled vein. The coronary sinus
ated by cells of the conducting system. Other cells of this
opens into the right atrium near the base of the inferior vena cava.
system then propagate and distribute this electrical impulse
Other cardiac veins empty into the great cardiac vein or the
to stimulate contractile cells to push blood in the right direc-
coronary sinus. These veins include (1) the posterior vein of
tion at the proper time. The arrival of an electrical impulse
left ventricle, draining the area served by the circumflex artery;
at a cardiac contractile cell’s plasma membrane produces an
(2) the middle cardiac vein, draining the area supplied by the
action potential that is comparable to an action potential in a
posterior interventricular artery; and (3) the small cardiac vein,
20 skeletal muscle fiber. As in a skeletal muscle fiber, this action
which receives blood from the posterior surfaces of the right
potential triggers the contraction of the cardiac contractile
atrium and ventricle. The anterior cardiac veins (also called the
cell. The actual contraction lags behind the beginning of the
anterior veins of right ventricle), which drain the anterior surface of
action potential. Because of the coordination provided by
the right ventricle, empty directly into the right atrium.
the conducting system, the atria contract first, driving blood
into the ventricles through the AV valves, and the ventricles
Checkpoint
contract next, driving blood out of the heart through the
1. Damage to the semilunar valve of the right ventricle semilunar valves.
would affect blood flow into which vessel? A heartbeat lasts only about 370 milliseconds (msec).
2. What prevents the AV valves from swinging into the atria? Although brief, it is a very busy period! Let’s follow the steps
3. Why is the left ventricle more muscular than the right that produce a single heartbeat.
ventricle?
See the blue Answers tab at the back of the book. The Conducting System: Pacemaker and
Conducting Cells
20-2 The cells of the conducting Unlike skeletal muscle, cardiac muscle tissue contracts on
its own, without neural or hormonal stimulation; this prop-
system distribute electrical impulses
erty is called autorhythmicity. The cells that initiate and
through the heart, causing cardiac distribute the stimulus to contract are part of the heart’s
contractile cells to contract conducting system. This system is a network of specialized
Learning Outcome Explain the events of an action potential cardiac muscle cells, called pacemaker cells and conducting
in cardiac muscle, indicate the importance of calcium ions to cells, that initiates and distributes electrical impulses. Let’s
the contractile process, describe the conducting system of the
heart, and identify the electrical events associated with a normal look at these types of cells, and how they function in the
electrocardiogram. conducting system.
> Go to > Study Area > Menu > Lab Tools > Bone and Dissection Videos > Sheep Heart: External
M20_MART6026_11_SE_C20_pp688-726.indd 702 24/10/16 8:13 PM
Chapter 20 The Heart 703
Figure 20–10 The Conducting System of the Heart and the Pacemaker Potential
+20 mV
Sinoatrial
(SA) node 0 mV
–20 mV
Internodal
pathways Threshold
–40 mV
Atrioventricular –60 mV Pacemaker
(AV) node potential
AV bundle
0 0.8 1.6
Time (sec)
Bundle b Changes in the membrane potential of a pacemaker cell in the SA
branches node that is establishing a heart rate of 72 beats per minute. Note
Purkinje the pacemaker potential, a gradual spontaneous depolarization.
fibers
a Components of the conducting system.
Components of the Conducting System and the bundle branches that run between the ventricles,
as well as the Purkinje (pur-KIN-je) fibers, which distribute
.
The specialized cardiac cells of the conducting system are col-
lected in various locations. This section introduces the compo- the stimulus to the ventricular myocardium.
nents of this system (Figure 20–10a). Most of the cells of the conducting system are smaller than
the contractile cells of the myocardium and contain very few
Pacemaker Cells in the Sinoatrial and Atrioventricular
myofibrils. Purkinje fibers, however, are much larger in diam-
Nodes. Pacemaker cells are essential to establishing the nor-
eter than the contractile cells.
mal heart rate. They are also called nodal cells because they are
found in two nodes, or locations: 20
Pacemaker Cells and Heart Rate
The sinoatrial (sı-no-A-tre-al) (SA) node is embedded
.
. . .
■
Pacemaker cells of the SA and AV nodes share a special charac-
in the posterior wall of the right atrium, near the entrance
teristic: Their excitable membranes do not have a stable resting
of the superior vena cava. Because the SA node is the pri-
membrane potential. Each time a pacemaker cell repolarizes, its
mary driver of the heart rate, it is also known as the cardiac
membrane potential drifts toward threshold. This gradual depo-
pacemaker.
larization is called a pacemaker potential (Figure 20–10b).
■ The relatively large atrioventricular (AV) node is located The pacemaker potential results from a slow inflow of Na+
at the junction between the atria and ventricles, near the without a compensating outflow of K+ .
opening of the coronary sinus. The pacemaker cells of this The rate of spontaneous depolarization differs in various
node send on signals from the cells of the SA node, and act parts of the conducting system. It is fastest at the SA node. With-
as backup to the SA node pacemaker cells. out neural or hormonal stimulation, the SA node generates
action potentials at a rate of 60–100 per minute. Isolated cells
Conducting Cells in the Internodal Pathways, AV Bun-
of the AV node depolarize more slowly, generating 40–60 action
dles, Bundle Branches, and Purkinje Fibers. Conducting
potentials per minute. Because the SA node reaches threshold
cells interconnect the SA and AV nodes, and distribute the con-
first, it establishes the basic heart rhythm, or sinus rhythm.
tractile stimulus throughout the myocardium. These cells are
(While heart rhythm is essential to heart rate, the heart rate is the
found in two main locations:
number of beats per minute.) In other words, the impulse gener-
■ In the atria, conducting cells are found in internodal ated by the SA node brings the AV pacemaker cells to threshold
pathways in the atrial walls. These pathways distribute the faster than does the pacemaker potential of the AV pacemaker
contractile stimulus to atrial muscle cells as this electrical cells. The normal resting heart rate is somewhat slower than
impulse travels from the SA node to the AV node. 80–100 beats per minute (bpm), however, due to the effects of
■ In the ventricles, conducting cells include those in the parasympathetic innervation. (We discuss the influence of auto-
atrioventricular (AV) bundle (also called the bundle of His) nomic innervation on heart rate in Section 20–4.)
M20_MART6026_11_SE_C20_pp688-726.indd 703 24/10/16 8:13 PM
704 UNIT 4 Fluids and Transport Figure 20–11 Impulse Conduction through the Heart and Accompanying ECG
Tracings. The ECG tracings are explained in the next section and in Figure 20–12 on page 706.
The pacemaker cells of the AV After reading about the electrocardiogram, come back to this figure to integrate the electrical activity
node can conduct impulses at a of the heart and atrial and ventricular contractions.
maximum rate of 230 per minute.
Because each impulse results in a 1 SA node activity and ECG Tracing
ventricular contraction, this value atrial activation begin SA node
(60–100 action
is the maximum normal heart potentials per minute
rate. Even if the SA node generates at rest).
impulses at a faster rate, the ventri-
cles will still contract at 230 bpm.
This limitation is important, because
mechanical factors (discussed later) Time = 0
begin to decrease the pumping effi-
ciency of the heart at rates above
approximately 180 bpm. Rates above 2 Stimulus spreads across the P wave: atrial
230 bpm occur only when the heart atrial surfaces and reaches depolarization
the AV node.
or the conducting system has been
AV node
damaged or stimulated by drugs.
As ventricular rates increase toward
their theoretical maximum limit of P
300–400 bpm, pumping effective-
ness becomes dangerously, if not Elapsed time = 50 msec
fatally, reduced.
3 There is a 100-msec delay P–R interval:
Impulse Conduction through conduction through
at the AV node. Atrial
the Heart contraction begins. AV node and AV
bundle
Now let’s trace the path of an
AV
impulse from its initiation at the bundle
SA node, examining its effects on
20 the surrounding myocardium as we Bundle P
branches
proceed.
Elapsed time = 150 msec
Functions of the Pacemaker
Cells. An action potential pro-
duced by the pacemaker cells of the 4 The impulse travels along the Q wave:
interventricular septum within beginning of ventricular
SA node (Figure 20–11 1 ) takes depolarization
the AV bundle and the bundle
approximately 50 msec to travel to branches to the Purkinje fibers
the AV node along the internodal and, by the moderator band,
to the papillary muscles of the
pathways. Along the way, the con- right ventricle.
ducting cells pass the stimulus to P
Moderator
contractile cells of both atria. The band
action potential then spreads across Q
Elapsed time = 175 msec
the atrial surfaces by cell-to-cell con-
tact (Figure 20–11 2 ). The stimulus QRS complex:
affects only the atria, because the 5 The impulse is distributed by completion of ventricular
cardiac skeleton isolates the atrial Purkinje fibers and relayed depolarization
throughout the ventricular R
myocardium from the ventricular myocardium. Atrial contraction
myocardium. is completed, and ventricular
The impulse slows as it leaves contraction begins.
the internodal pathways and enters P
the AV node, because the nodal cells
are smaller in diameter than the con- Elapsed time = 225 msec Purkinje fibers QS
ducting cells. (Chapter 12 discussed
? What happens to the electrical impulse when it reaches the AV node?
M20_MART6026_11_SE_C20_pp688-726.indd 704 24/10/16 8:13 PM
Chapter 20 The Heart 705
the relationship between axon diameter and propagation generation of an impulse at the SA node to the complete
speed. p. 416) In addition, the connections between pace- depolarization of the ventricular myocardium, normally takes
maker cells are less efficient than those between conducting around 225 msec.
cells at relaying the impulse from one cell to another. As a
result, the impulse takes about 100 msec to pass through the Disturbances in Heart Rhythm
AV node (Figure 20–11 3 ). This delay is important because it
A number of clinical problems result from abnormal pace-
allows the atria to contract before the ventricles do. (The delay
maker function. Bradycardia (brad-e-KAR-de-uh; bradys, slow)
. . .
is a result of the time it takes for calcium ions to enter the sar-
is a condition in which the heart rate is slower than normal.
coplasm and activate the contraction process, as described in
Tachycardia (tak-e-KAR-de-uh; tachys, swift) is a faster-than-
. .
Chapter 10. p. 306) Otherwise, contraction of the powerful
normal heart rate. These terms are relative, and in clinical
ventricles would close the AV valves and prevent blood flow
practice the definitions vary with the normal resting heart rate
from the atria into the ventricles.
of the individual.
Damage to the conducting pathways disturbs the normal
Functions of the Conducting Cells. After the brief delay at
rhythm of the heart. The resulting problems are called conduc-
the AV node, the impulse is conducted along the AV bundle
tion deficits. If the SA node or any of the internodal pathways
and the bundle branches to the Purkinje fibers and the pap-
becomes damaged, the heart continues to beat, but at a slower
illary muscles (Figure 20–11 4 ). The connection between
rate, usually 40–60 bpm, as dictated by the AV node. Certain
the AV node and the AV bundle is normally the only electrical
cells in the Purkinje fiber network depolarize spontaneously
connection between the atria and the ventricles. Once an
at an even slower rate. If the rest of the conducting system is
impulse enters the AV bundle, it travels to the interventricular
damaged, these cells can stimulate a heart rate of 20–40 bpm.
septum and enters the right and left bundle branches. The
Under normal conditions, cells of the AV bundle, the bundle
left bundle branch, which supplies the massive left ventricle,
branches, and most Purkinje fibers do not depolarize spontane-
is much larger than the right bundle branch. Both branches
ously. If, due to damage or disease, these cells do begin depo-
extend toward the apex of the heart, turn, and fan out deep to
larizing spontaneously, the heart may no longer pump blood
the endocardial surface.
effectively. Death can result if the problem persists.
As the bundle branches diverge, they conduct the impulse
If an abnormal conducting cell or ventricular contractile cell
to both the Purkinje fibers and, through the moderator band,
begins generating action potentials at a higher rate, the impulses
to the papillary muscles of the right ventricle. Because the
can override those of the SA or AV node. The origin of these
impulse is delivered to the papillary muscles directly, these
abnormal signals is called an ectopic (ek-TOP-ik; out of place) 20
muscles begin contracting before the rest of the ventricu-
pacemaker. The activity of an ectopic pacemaker partially or
lar musculature does. Contraction of the papillary muscles
completely bypasses the conducting system, disrupting the tim-
applies tension to the chordae tendineae, bracing the AV
ing of ventricular contraction. The result may be a dangerous
valves. This tension limits the movement of the cusps, pre-
reduction in the pumping efficiency of the heart. Such conditions
venting the backflow of blood into the atria when the ven-
are commonly diagnosed with the aid of an electrocardiogram.
tricles contract.
The Purkinje fibers then distribute the impulse to the ven-
tricular myocardium (Figure 20–11 5 ). Purkinje fibers, which
The Electrocardiogram (ECG)
radiate from the apex toward the base of the heart, conduct The electrical events in the heart are powerful enough to be
action potentials very rapidly—as fast as small myelinated detected by electrodes on the body. A procedure known as
axons. Within about 75 msec, the signal to begin a contrac- electrocardiography can monitor the electrical events of the con-
tion has reached all the ventricular cardiac contractile cells, ducting system. A recording of these events is an electrocardio-
and ventricular contraction begins. By this time, the atria have gram (e-lek-tro-KAR-de-o-gram), also called an ECG, or EKG
. . . .
completed their contractions and ventricular contraction can (from the German term). Clinicians can use an ECG to assess
safely occur. Because of the location of the Purkinje fibers, the the functions of specific pacemaker, conducting, and contrac-
ventricles contract in a wave that begins at the apex of the heart tile cells. When a portion of the heart has been damaged by a
and spreads toward the base. The contraction pushes blood heart attack, for example, the ECG reveals an abnormal pattern
toward the base, into the aorta and pulmonary trunk. of impulse conduction.
In summary, each time the heart beats, a wave of depolar- The monitoring electrodes for an ECG are placed at dif-
ization spreads through the atria, pauses at the AV node, then ferent locations on the body surface. The appearance of the
travels down the interventricular septum to the apex, turns, ECG varies with the placement of the monitoring electrodes,
and spreads through the ventricular myocardium toward or leads. Figure 20–12a shows the leads in one of the standard
the base (see Figure 20–11). The entire process, from the configurations. Figure 20–12b depicts the important features of
M20_MART6026_11_SE_C20_pp688-726.indd 705 24/10/16 8:13 PM
706 UNIT 4 Fluids and Transport
Figure 20–12 An Electrocardiogram (ECG).
800 msec
R R +1
a Electrode placement for
recording a standard ECG. P wave
(atria T wave S–T
depolarize) (ventricles repolarize) P – R segment segment +0.5
0 Millivolts
Q S S –T
P–R
interval
interval
–0.5
Q –T QRS complex
interval (ventricles depolarize)
0 0.2 0.4 0.6 0.8 1.0 1.2 1.4
20 Time (sec)
b An ECG printout is a strip of graph paper containing a record of the electrical events monitored
by the electrodes. The placement of electrodes on the body surface affects the size and shape
of the waves recorded. The example is a normal ECG; the enlarged section indicates the major
components of the ECG and the measurements most often taken during clinical analysis.
an ECG recorded with that configuration. Note the following To analyze an ECG, you must measure the size of the
ECG features: voltage changes and determine the durations and temporal
(time) relationships of the various components. The amount
■ The small P wave, which accompanies the depolarization
of depolarization during the P wave and the QRS complex is
of the atrial contractile cells. Depolarization of these cells
particularly important in making a diagnosis. For example, an
causes atrial contraction. (Also see Figure 20–11 2 .)
excessively large QRS complex often indicates that the heart has
■ The QRS complex, which appears as the ventricle con- become enlarged. A smaller-than-normal electrical signal may
tractile cells depolarize. This electrical signal is relatively mean that the mass of the heart muscle has decreased (although
strong, because the ventricular muscle is much more monitoring problems are more often responsible). The size
massive than that of the atria. It is also a complex signal, and shape of the T wave may also be affected by any condition
largely because of the complex pathway that the spread of that slows ventricular repolarization. For example, starvation
depolarization takes through the ventricles. The ventricles and low cardiac energy reserves, coronary ischemia (inadequate
begin contracting shortly after the peak of the R wave. blood flow to cardiac cells), or abnormal ion concentrations
Atrial repolarization takes place while the ventricles are reduce the size of the T wave.
depolarizing and it is obscured by the more powerful QRS The times between waves are reported as segments and
complex. (Also see Figure 20–11 4 and 5 .) intervals. Segments generally extend from the end of one wave
■ The smaller T wave, which indicates repolarization of the to the start of another. Intervals are more variable, but always
ventricular contractile cells. include at least one entire wave. Commonly used segments and
M20_MART6026_11_SE_C20_pp688-726.indd 706 24/10/16 8:13 PM
Chapter 20 The Heart 707
intervals are labeled in Figure 20–12b. The names, however, can ventricular walls. These cells account for about 99 percent of
be somewhat misleading. For example: the muscle cells in the heart. As noted in Chapter 10, cardiac
contractile cells are interconnected by intercalated (in-TER-
■■ The P–R interval extends from the start of atrial depolar-
kah-la-ted) discs (Figure 20–14a). Intercalated discs transfer
.
ization to the start of the QRS complex (ventricular depo-
the force of contraction from cell to cell and propagate action
larization) rather than to R, because in abnormal ECGs the
potentials. At an intercalated disc, the interlocking membranes
peak at R can be difficult to determine. Extension of the
of adjacent cells are held together by desmosomes and linked
P–R interval to more than 200 msec can indicate damage to
by gap junctions (Figure 20–14b,c). The desmosomes prevent
the AV node or conducting pathways.
cells from separating during contraction, while the gap junc-
■■ The Q–T interval indicates the time required for the
tions allow ions to pass and electrically couple adjacent cells.
ventricles to undergo a single cycle of depolarization and
This allows the heart muscle to behave as a functional syncytium
repolarization. It is usually measured from the end of the
(sin-SI-she-um), a mechanically, chemically, and electrically
.
P–R interval rather than from the bottom of the Q wave.
coupled, multinucleate tissue.
The Q–T interval can be lengthened by electrolyte distur-
bances, some medications, conduction problems, coronary
Tips & Tools
ischemia, or myocardial damage. A congenital heart defect
that can cause sudden death without warning may be The term intercalated means “inserted between other ele-
detectable as a prolonged Q–T interval. ments.” So, intercalated discs appear to have been inserted
between cardiac muscle cells.
An arrhythmia (a-RITH-me-uh) is an irregularity in the nor-
. .
mal rhythm or force of the heartbeat. Serious arrhythmias may
indicate damage to the myocardium, injuries to the pacemaker Cardiac Contractile Cells Compared with Skeletal
cells or conducting cell pathways, exposure to drugs, or abnor- Muscle Fibers
malities in the electrolyte composition of extracellular fluids. Table 20–1 provides a review of the structural and functional
Spotlight Figure 20–13 describes cardiac arrhythmias. differences between cardiac contractile cells and skeletal mus-
cle fibers. Histological characteristics that distinguish cardiac
contractile cells from skeletal muscle fibers include (1) small
Cardiac Contractions: Contractile Cells size; (2) a single, centrally located nucleus; (3) branching
The Purkinje fibers distribute the stimulus to the cardiac interconnections between cells; and (4) the presence of inter-
contractile cells, which form the bulk of the atrial and calated discs.
20
Table 20–1 Structural and Functional Differences between Cardiac Contractile Cells and Skeletal Muscle Fibers
Feature Cardiac Contractile Cells Skeletal Muscle Fibers
Size 10920 µm * 509100 µm 100 µm * up to 40 cm
Nuclei Typically 1 (rarely 2–5) Multiple (hundreds)
Contractile proteins Sarcomeres along myofibrils Sarcomeres along myofibrils
Internal membranes Short T tubules; no triads formed with Long T tubules form triads with cisternae of the
sarcoplasmic reticulum sarcoplasmic reticulum
Mitochondria Abundant (25% of cell volume) Much less abundant
Inclusions Myoglobin, lipids, glycogen Little myoglobin, few lipids, but extensive glycogen reserves
Blood supply Very extensive More extensive than in most connective tissues, but sparse
compared with supply to cardiac muscle cells
Metabolism (resting) Not applicable Aerobic, primarily lipid based
Metabolism (active) Aerobic, primarily using lipids and carbohydrates Anaerobic, through breakdown of glycogen reserves
Contractions Twitches with brief relaxation periods; long refractory period Usually sustained contractions
prevents tetanic contractions
Stimulus for contraction Autorhythmicity of pacemaker cells generates action Activity of somatic motor neuron generates action potentials
potentials in sarcolemma
Trigger for contraction Calcium ion entry from the extracellular fluid and calcium ion Calcium ion release from the sarcoplasmic reticulum
release from the sarcoplasmic reticulum
Intercellular connections Branching network with plasma membranes locked together Adjacent fibers tied together by connective tissue fibers
at intercalated discs; connective tissue fibers tie adjacent
layers together
M20_MART6026_11_SE_C20_pp688-726.indd 707 02/11/16 2:35 pm
SPOTLIGHT
Figure 20–13
Cardiac Arrhythmias
Despite the variety of sophisticated equipment available to assess or
visualize cardiac function, in the majority of cases the ECG provides the
most important diagnostic information. ECG analysis is especially useful
in detecting and diagnosing cardiac arrhythmias (ā-RITH-mē-uz)—
abnormal patterns of cardiac electrical activity. Momentary arrhythmias
are not inherently dangerous, but clinical problems appear when
arrhythmias reduce the pumping efficiency of the heart.
Premature Atrial Contractions (PACs) Premature atrial contractions (PACs) increase the incidence of PACs, presumably
often occur in healthy individuals. In a PAC, by increasing the permeabilities of the SA
the normal atrial rhythm is momentarily pacemakers. The impulse spreads along the
P P P
interrupted by a “surprise” atrial contraction. conduction pathway, and a normal ventricular
Stress, caffeine, and various drugs may contraction follows the atrial beat.
Paroxysmal Atrial Tachycardia (PAT) In paroxysmal (par-ok-SIZ-mal) atrial tachy-
cardia, or PAT, a premature atrial contraction
triggers a flurry of atrial activity. The ventricles
P P P P P P are still able to keep pace, and the heart rate
jumps to about 180 beats per minute.
Atrial Fibrillation (AF) During atrial fibrillation (fib-ri-LĀ-shun), the limits. Even though the atria are now
impulses move over the atrial surface at rates nonfunctional, their contribution to ventricular
of perhaps 500 beats per minute. The atrial end-diastolic volume (the maximum amount
wall quivers instead of producing an organized of blood the ventricles can hold at the end of
contraction. The ventricular rate cannot follow atrial contraction) is so small that the condition
the atrial rate and may remain within normal may go unnoticed in older individuals.
Premature Ventricular Contractions (PVCs) Premature ventricular contractions responsible is called an ectopic pacemaker.
(PVCs) occur when a Purkinje cell or ventricu- The frequency of PVCs can be increased by
lar myocardial cell depolarizes to threshold and exposure to epinephrine, to other stimulatory
P T P T P T triggers a premature contraction. Single PVCs drugs, or to ionic changes that depolarize
are common and not dangerous. The cell cardiac muscle plasma membranes.
Ventricular Tachycardia (VT) Ventricular tachycardia is defined as four
or more PVCs without intervening normal
beats. It is also known as VT or V-tach.
P Multiple PVCs and VT may indicate that
serious cardiac problems exist.
Ventricular Fibrillation (VF) Ventricular fibrillation (VF) is responsible
for the condition known as cardiac arrest.
VF is rapidly fatal, because the ventricles
quiver and stop pumping blood.
708
M20_MART6026_11_SE_C20_pp688-726.indd 708 24/10/16 8:13 PM
Chapter 20 The Heart 709
Figure 20–14 Cardiac Contractile Cells.
Intercalated Disc
Gap junction
Cardiac contractile cell Z-lines bound to
facing plasma
Mitochondria membranes
Intercalated Desmosomes
disc (sectioned)
b Structure of an intercalated disc
Nucleus
Cardiac contractile
cell (sectioned)
Bundles of
myofibrils
Intercalated discs
a Cardiac contractile cells
Cardiac muscle tissue LM × 575
20
c Cardiac muscle tissue
The functions of cardiac contractile cells and skeletal mus- reached in a portion of the membrane next to an interca-
cle cells are similar but have some differentiating characteris- lated disc. The typical stimulus is the excitation of an adjacent
tics. In both types of cells, (1) an action potential leads to the contractile cell. Once threshold has been reached, the action
appearance of Ca2+ among the myofibrils, and (2) the binding potential proceeds in three basic steps (Figure 20–15a):
of Ca2+ to troponin on the thin filaments initiates the contrac-
1 Rapid Depolarization. The stage of rapid depolarization in a
tion. But cardiac contractile cells and skeletal muscle fibers dif-
cardiac contractile cell resembles that in a skeletal muscle fiber.
fer in terms of the nature of the action potential, the source of
At threshold, voltage-gated sodium ion channels open, and the
the Ca2+ , and the duration of the resulting contraction. p. 331
membrane suddenly becomes permeable to Na+ . A massive in-
flux of sodium ions rapidly depolarizes the sarcolemma. The
The Action Potential in Cardiac Contractile Cells
channels involved are called fast sodium channels, because
The resting membrane potential of a ventricular contractile cell
they open quickly and remain open for only a few milliseconds.
is approximately -90 mV, comparable to that of a resting skel-
2 The Plateau. A partial repolarization takes place as some
etal muscle fiber 1 -85 mV2. (The resting membrane potential
potassium ions 1K+ 2 leave the cell before most K+ channels
of an atrial contractile cell is about -80 mV, but the basic prin-
close. Voltage-gated calcium channels then open and extracel-
ciples described here apply to atrial cells as well.)
lular calcium ions 1Ca2+ 2 enter the cytosol. The slow calcium
Process of the Action Potential. An action potential begins channels remain open for a relatively long period—roughly
when the membrane of the ventricular contractile cell reaches 175 msec. The inflow of positive charges 1Ca2+ 2 and reduced
threshold, usually at about -75 mV. Threshold is normally outflow of K+ delay repolarization, causing the membrane
M20_MART6026_11_SE_C20_pp688-726.indd 709 24/10/16 8:13 PM
710 UNIT 4 Fluids and Transport
Figure 20–15 Action Potentials in Cardiac Contractile Cells and Skeletal Muscle Fibers.
1 Rapid Depolarization 2 The Plateau 3 Repolarization +30 Skeletal
Cause: Na+ entry Action muscle
Cause: Ca2+ entry Cause: K+ loss 0
Duration: 3–5 msec potential fiber
Duration: ~175 msec Duration: 75 msec
Ends with: Closure of mV
Ends with: Closure Ends with: Closure
voltage-gated fast of slow calcium of slow potassium
sodium channels channels channels –85
Tension Contraction
+30
0 100 200 300
2
0
Time (msec)
1
mV Relative
3 refractory
period +30 Cardiac
Absolute refractory
contractile
–90 period KEY 0
cell
Absolute refractory
mV Action potential
period
0 100 200 300
Stimulus Time (msec) Relative refractory
period –90
a Events in an action potential in a ventricular contractile cell.
Tension
Contraction
0 100 200 300
Time (msec)
20
b Action potentials and twitch contrac-
tions in a skeletal muscle fiber (above)
and cardiac contractile cell (below).
The shaded areas indicate the
durations of the absolute (blue) and
relative (beige) refractory periods.
? Which ion’s entry causes rapid depolarization? Which ion’s entry causes
the plateau? Which ion’s exit causes repolarization?
potential to remain near 0 mV for an extended period. This The Refractory Period. As with skeletal muscle fiber contrac-
portion of the action potential is called the plateau. The extra- tions, the membrane of a cardiac contractile cell will not respond
cellular calcium ions initiate contraction and also delay repo- normally to a second stimulus for some time after an action poten-
larization. Their increased concentration within the cell also tial begins. This time is called the refractory period. Initially, in
triggers the release of Ca2+ from reserves in the sarcoplasmic the absolute refractory period, the membrane cannot respond at
reticulum (SR), which continues the contraction. all, because the sodium ion channels are either already open or
3 Repolarization. As the plateau continues, slow calcium chan- closed and inactivated. In a ventricular contractile cell, the abso-
nels begin closing, and slow potassium channels begin open- lute refractory period lasts approximately 200 msec. It includes the
ing. As these channels open, potassium ions 1K + 2 rush out of plateau and the initial period of rapid repolarization.
the cell, and the net result is a period of rapid repolarization The absolute refractory period is followed by a shorter
that restores the resting membrane potential. (50-msec) relative refractory period. During this period, the
M20_MART6026_11_SE_C20_pp688-726.indd 710 24/10/16 8:13 PM
Chapter 20 The Heart 711
voltage-gated sodium ion channels are closed, but can open. In addition to obtaining oxygen from the coronary cir-
The membrane will respond to a stronger-than-normal stimu- culation, cardiac contractile cells maintain their own sizable
lus by initiating another action potential. In total, an action reserves of oxygen. In these cells, oxygen molecules are bound
potential in a ventricular contractile cell lasts 250–300 msec, to the heme units of myoglobin molecules. (We discussed this
about 30 times as long as a typical action potential in a skel- globular protein, which reversibly binds oxygen molecules, and
etal muscle fiber. its function in skeletal muscle fibers in Chapter 10.) p. 323
Normally, the combination of circulatory supplies plus myo-
The Role of Calcium Ions in Cardiac or Skeletal globin reserves is enough to meet the oxygen demands of the
Muscle Contractions heart, even when it is working at maximum capacity.
The appearance of an action potential in the cardiac contractile
cell plasma membrane produces a contraction by causing an Checkpoint
increase in the concentration of Ca2+ around the myofibrils.
4. Define autorhythmicity.
This process takes place in two steps:
5. Which structure of the heart is known as the cardiac
1. Extracellular calcium ions crossing the plasma mem- pacemaker?
brane during the plateau phase of the action potential 6. If the cells of the SA node did not function, how would
provide roughly 20 percent of the Ca2+ required for a the heart rhythm change and the heart rate be affected?
contraction. 7. Why is it important for impulses from the atria to be
delayed at the AV node before they pass into the ventricles?
2. The arrival of extracellular Ca2+ triggers the release of addi-
tional Ca2+ from reserves in the sarcoplasmic reticulum (SR). See the blue Answers tab at the back of the book.
Extracellular calcium ions thus have both direct and indirect
effects on cardiac contractile cell contraction. For this reason, 20-3 The contraction–relaxation events
cardiac muscle tissue is highly sensitive to changes in the Ca2+ that occur during a complete heartbeat
concentration of the extracellular fluid. make up a cardiac cycle
In a skeletal muscle fiber, the action potential is rela-
Learning Outcome Explain the events of the cardiac cycle,
tively brief and ends as the resulting twitch contraction begins including atrial and ventricular systole and diastole, and relate the
(Figure 20–15b). The twitch contraction is short and ends as heart sounds to specific events in the cycle.
the SR reclaims the Ca2+ it released. In a cardiac contractile cell,
The electrical events of the conducting system initiate the mechan-
as we have seen, the action potential is prolonged, and calcium
ical events of heart contraction. A brief resting phase follows each 20
ions continue to enter the cell throughout the plateau. As a
heartbeat, allowing time for the chambers to relax and prepare
result, the cell actively contracts until the plateau ends. As the
for the next heartbeat. The period between the start of one heart-
slow calcium channels close, the intracellular calcium ions are
beat and the beginning of the next is a single cardiac cycle. It
pumped back into the SR or out of the cell, and the contractile
includes alternating periods of contraction and relaxation. For
cell relaxes.
any one chamber in the heart, the cardiac cycle can be divided
In skeletal muscle fibers, the refractory period ends before
into two phases: systole and diastole. During systole (SIS-to-le),
. .
peak tension develops. As a result, twitches can summate and
or contraction, the chamber contracts and pushes blood into an
tetanus can occur. In cardiac contractile cells, the absolute refrac-
adjacent chamber or into an arterial trunk. Systole is followed by
tory period continues until relaxation is under way. Because
diastole (dı-AS-to-le), or relaxation. During diastole, the cham-
. . .
summation is not possible, tetanic contractions cannot occur in
ber fills with blood and prepares for the next cardiac cycle.
a normal cardiac contractile cell, regardless of the frequency or
intensity of stimulation. This feature is vital: A heart in tetany
An Introduction to Pressure and Flow
could not pump blood. With a single twitch lasting 250 msec or
in the Heart
longer, a normal cardiac contractile cell could reach 300–400
contractions per minute under maximum stimulation. This rate Fluids flow from an area of higher pressure to an area of lower
is not reached in a normal heart, due to limitations imposed by pressure. In the cardiac cycle, the blood pressure within each
the conducting system. chamber rises during systole and falls during diastole. Valves
between adjacent chambers help ensure that blood flows in
The Energy for Cardiac Contractions the required direction, but blood flows from one chamber to
When a normal heart is beating, it gets energy as the mito- another only if the pressure in the first chamber exceeds that
chondria break down fatty acids (stored as lipid droplets) and in the second. This basic principle governs the movement of
glucose (stored as glycogen). These aerobic reactions can occur blood between atria and ventricles, between ventricles and arte-
only when oxygen is readily available. p. 320 rial trunks, and between major veins and atria.
M20_MART6026_11_SE_C20_pp688-726.indd 711 24/10/16 8:13 PM
712 UNIT 4 Fluids and Transport
Figure 20–16 Phases of the Cardiac Cycle. Thin black arrows indicate blood flow, green arrows indicate
contractions, and the red-hued areas indicate which heart chambers are in systole.
SmartArt
Atrial systole
Start
a Atrial systole begins:
Atrial contraction forces a small amount
of additional blood into relaxed ventricles.
b Atrial systole
ends, atrial
diastole begins
tole
0
dias
800 msec
msec 100
msec
lar
Ventricu
Ventricular systole
Cardiac
f Ventricular c Ventricular systole—
diastole—late: cycle first phase: Ventricular
All chambers are contraction exerts
relaxed. Ventricles enough pressure on
fill passively. the blood to close AV
valves but not enough
370 to open semilunar
20 msec valves.
d Ventricular systole—second
phase: As ventricular
pressure rises and exceeds
pressure in the arteries,
e Ventricular diastole—early: the semilunar valves
As ventricles relax, pressure in open and blood is
ventricles drops; blood flows back ejected.
against cusps of semilunar valves
and forces them closed. Blood
flows into the relaxed atria. le
iasto
ld
Atria
The correct pressure relationships depend on the careful Phases of the Cardiac Cycle
timing of contractions. For example, blood could not move The phases of the cardiac cycle—atrial systole, atrial diastole,
in the proper direction if an atrium and its attached ventricle ventricular systole, and ventricular diastole—are diagrammed in
contracted at precisely the same moment. The heart’s elabo- Figure 20–16 for a representative heart rate of 75 bpm. At this
rate pacemaking and conducting systems normally provide the heart rate, a sequence of systole and diastole in either the atria
required spacing between atrial systole and ventricular systole. or the ventricles lasts 800 msec. When the cardiac cycle begins,
M20_MART6026_11_SE_C20_pp688-726.indd 712 04/11/16 8:52 pm
Chapter 20 The Heart 713
all four chambers are relaxed, and the ventricles are partially ventricles is less than that through the smaller, angled open-
filled with blood. ings of the large veins.
Let’s start by focusing on the atria. During atrial systole, At the end of atrial systole, each ventricle contains the
the atria contract, filling the ventricles completely with blood maximum amount of blood that it will hold in this cardiac
(Figure 20–16a,b). Atrial systole lasts 100 msec. The atria next cycle. That quantity is called the end-diastolic volume (EDV). In
enter atrial diastole, which continues until the start of the next an adult who is standing at rest, the end-diastolic volume is
cardiac cycle. typically about 130 mL (about 4.4 oz).
Ventricular systole begins at the same time as atrial dias-
tole. Ventricular systole lasts 270 msec. During this period, the Ventricular Systole and Atrial Diastole
ventricles push blood through the systemic and pulmonary In ventricular systole:
circuits and toward the atria (Figure 20–16c,d). The heart then 3 Atrial systole ends; AV valves close. As atrial systole ends,
enters ventricular diastole (Figure 20–16e,f), which lasts ventricular systole begins. As the pressures in the ventricles rise
530 msec (the 430 msec remaining in this cardiac cycle, plus above those in the atria, the AV valves are pushed closed.
the first 100 msec of the next, when the atria are again contract-
4 Isovolumetric ventricular contraction occurs. During the early
ing). For the rest of this cycle, filling occurs passively, and both the
stage of ventricular systole, the ventricles are contracting, but
atria and the ventricles are relaxed. The next cardiac cycle begins
blood flow has yet to occur. Ventricular pressures are not yet
with atrial systole, which completes the filling of the ventricles.
high enough to force open the semilunar valves and push
When the heart rate increases, all the phases of the cardiac
blood into the pulmonary or aortic trunk. Over this period, the
cycle are shortened. The greatest reduction occurs in the length of
ventricles contract isometrically; in other words, they generate
time spent in diastole. When the heart rate climbs from 75 bpm
tension and pressures rise inside them, but blood does not flow
to 200 bpm, the time spent in systole drops by less than 40 per-
out. The ventricles are in isovolumetric contraction: All the
cent, but the duration of diastole is reduced by almost 75 percent.
heart valves are closed, the volumes of the ventricles do not
change, and ventricular pressures are rising.
Pressure and Volume Changes 5 Ventricular ejection occurs. Once pressure in the ventricles
in the Cardiac Cycle exceeds that in the arterial trunks, the semilunar valves are
Figure 20–17 plots the pressure and volume changes during the pushed open and blood flows into the pulmonary and aor-
cardiac cycle. It also shows an ECG for the cardiac cycle. The tic trunks. This point marks the beginning of ventricular
circled numbers in the figure correspond to numbered para- ejection. The ventricles now contract isotonically: The muscle
20
graphs in the text. The figure shows pressure and volume within cells shorten, and tension production remains relatively con-
the left atrium and left ventricle, but our discussion applies to stant. (To review isotonic versus isometric contractions, look
both sides of the heart. Although pressures are lower in the right back at Figure 10–18, p. 317.)
atrium and right ventricle, both sides of the heart contract at the During ventricular ejection, each ventricle ejects 70–80 mL
same time, and they eject equal volumes of blood. of blood, the stroke volume (SV) of the heart. The stroke volume
at rest is roughly 60 percent of the end-diastolic volume.
After reaching a peak, ventricular pressures gradually decline
Atrial Systole
near the end of ventricular systole. Figure 20–17 shows values
In atrial systole:
for the left ventricle and aorta. The right ventricle also undergoes
1 Atrial contraction begins. At the start of atrial systole, the ven- periods of isovolumetric contraction and ventricular ejection.
tricles are already filled to about 70 percent of their normal 6 Semilunar valves close. As the end of ventricular systole
capacity, due to passive blood flow during the end of the previ- approaches, ventricular pressures fall rapidly. Blood in the
ous cardiac cycle. aorta and pulmonary trunk now starts to flow back toward the
2 Atria eject blood into the ventricles. As the atria contract, ris- ventricles, and this movement closes the semilunar valves. As
ing atrial pressures provide the remaining 30 percent by push- the backflow begins, pressure decreases in the aorta. When the
ing blood into the ventricles through the open right and left semilunar valves close, pressure rises again as the elastic arterial
AV valves. Atrial systole essentially “tops off” the ventricles. walls recoil. This small, temporary rise produces a valley in the
Over this period, blood cannot flow into the atria from the aortic pressure tracing, called a dicrotic (dı-KROT-ik; dikrotos,
.
veins because atrial pressure exceeds venous pressure. Yet double beating) notch.
there is very little backflow into the veins, even though the The amount of blood remaining in the ventricle when the
connections with the venous system lack valves. The reason semilunar valve closes is the end-systolic volume (ESV). At rest,
is that blood takes the path of least resistance. Resistance to the end-systolic volume is 50 mL, about 40 percent of the end-
blood flow through the wide opening between the atria and diastolic volume.
M20_MART6026_11_SE_C20_pp688-726.indd 713 24/10/16 8:13 PM
714 UNIT 4 Fluids and Transport
Figure 20–17 Pressure and Volume Relationships in the Cardiac Cycle. Major features of the cardiac cycle
are shown for a heart rate of 75 bpm. The circled numbers correspond to those in the associated box. For further details,
see the numbered list in the text (pp. 713–715).
ONE CARDIAC CYCLE
QRS
QRS complex
complex
Electro-
cardiogram
P T
(ECG) P
ATRIAL ATRIAL ATRIAL
ATRIAL DIASTOLE
DIASTOLE SYSTOLE SYSTOLE
VENTRICULAR VENTRICULAR
VENTRICULAR DIASTOLE
DIASTOLE SYSTOLE
120 5 Aortic valve
closes
Aortic valve
opens
6
Aorta
90
Dicrotic
notch
1 Atrial contraction begins.
2 Atria eject blood into ventricles.
Pressure
(mm Hg)
60 3 Atrial systole ends; AV valves close.
Left 4 Isovolumetric ventricular contraction occurs.
ventricle 4
7 5 Ventricular ejection occurs.
6 Semilunar valves close.
Left AV 7 Isovolumetric relaxation occurs.
20 30 Left AV
Left atrium valve opens
valve closes 8 AV valves open; passive ventricular
filling occurs.
2
1
3 8
0
130 End-diastolic
3 volume
2
volume (mL)
ventricular
1
Left
Stroke
volume End-systolic
volume
6
50
0 100 200 300 400 500 600 700 800
Time (msec)
Ventricular Diastole
ventricular pressures are still higher than atrial pressures, blood
The period of ventricular diastole lasts for the remainder of the
cannot flow into the ventricles. This is isovolumetric relax-
current cardiac cycle and continues through atrial systole in the
ation. Ventricular pressures drop rapidly over this period,
next cycle.
because the elasticity of the connective tissues of the heart and
7 Isovolumetric relaxation occurs. All the heart valves are now cardiac skeleton helps re-expand the ventricles toward their
closed, and the ventricular myocardium is relaxing. Because resting dimensions.
M20_MART6026_11_SE_C20_pp688-726.indd 714 24/10/16 8:13 PM
Chapter 20 The Heart 715
8 AV valves open; passive ventricular filling occurs. When
stethoscope is placed depends on which valve is under exami-
nation (Figure 20–18a). Valve sounds must pass through the
ventricular pressures fall below those of the atria, the atrial
pericardium, surrounding tissues, and the chest wall, and some
pressures force the AV valves open. Blood now flows from
tissues muffle sounds more than others. For this reason, the
the atria into the ventricles. Both the atria and the ventricles
placement of the stethoscope differs somewhat from the posi-
are in diastole, but the ventricular pressures continue to fall
tion of the valve under review.
as the ventricular chambers expand. Throughout this period,
There are four heart sounds, named S1 through S4
pressures in the ventricles are so far below those in the major
(Figure 20–18b). If you listen to your own heart with a stetho-
veins that blood pours through the relaxed atria and on
scope, you will clearly hear the first and second heart sounds.
through the open AV valves into the ventricles. This passive
These sounds accompany the closing of your heart valves. The
flow of blood is the primary method of ventricular filling.
first heart sound (S1), known as “lubb,” lasts a little longer than
The ventricles become nearly three-quarters full before the
the second (S2), called “dupp.” S1 marks the start of ventricular
cardiac cycle ends.
contraction, when the AV valves close and the semilunar valves
The relatively minor contribution that atrial systole makes open. S2 occurs at the beginning of ventricular filling, when the
to ventricular volume explains why individuals can survive semilunar valves close and the AV valves open. The third and
quite normally when their atria have been so severely damaged fourth heart sounds are usually very faint and are seldom audible
that they can no longer function. In contrast, damage to one in healthy adults. These sounds are associated with blood flow-
or both ventricles can leave the heart unable to pump enough ing into the ventricles (S3) and atrial contraction (S4), rather
blood through peripheral tissues and organs. A condition of than with valve action.
heart failure then exists. If the valve cusps are malformed or there are problems with
the papillary muscles or chordae tendineae, the heart valves
Heart Sounds may not close properly. AV valve regurgitation then occurs
Listening to the heart, a technique called auscultation (aws-
.
during ventricular systole. The surges, swirls, and eddies of tur-
kul-TA-shun), is a simple and effective method of cardiac bulent blood flow that accompany regurgitation create a rush-
assessment. Clinicians use an instrument called a stethoscope ing, gurgling sound known as a heart murmur. Minor heart
to listen for normal and abnormal heart sounds. Where the murmurs are common and inconsequential.
20
Figure 20–18 Heart Sounds.
120
Valve Valve Semilunar Semilunar
location location valves open valves close
Aortic Pulmonary
valve Sounds Sounds valve 90
heard heard Aorta
Pressure
(mm Hg)
60
Left
Valve Valve ventricle
Right location location Left
AV AV Left AV valves
AV valves
valve Sounds Sounds valve 30 atrium
close open
heard heard
0
S1
S2
S4 S3 S4
Heart
sounds
“Lubb” “Dupp”
a Placements of a stethoscope for
listening to the different sounds b The relationship between heart sounds
produced by individual valves and key events in the cardiac cycle
M20_MART6026_11_SE_C20_pp688-726.indd 715 24/10/16 8:14 PM
716 UNIT 4 Fluids and Transport
Figure 20–19 Factors Affecting Cardiac Output.
Checkpoint
8. Give the technical terms for heart contraction and heart
relaxation. Factors Affecting Factors Affecting
Heart Rate (HR) Stroke Volume (SV)
9. List the phases of the cardiac cycle.
10. Is the heart always pumping blood when pressure in the Autonomic End-diastolic End-systolic
Hormones
left ventricle is rising? Explain. innervation volume (EDV) volume (ESV)
11. What could cause an increase in the size of the QRS
complex in an electrocardiogram?
HEART RATE (HR) STROKE VOLUME (SV) = EDV — ESV
See the blue Answers tab at the back of the book.
20-4 Cardiac output is determined by SmartArt
heart rate and stroke volume
CARDIAC OUTPUT (CO) = HR x SV
Learning Outcome Define cardiac output, describe the factors
that influence heart rate and stroke volume, and explain how
adjustments in stroke volume and cardiac output are coordinated
at different levels of physical activity.
When considering cardiac function over time, physicians gen-
erally are most interested in the cardiac output (CO), the
amount of blood pumped by the left ventricle in 1 minute. of the handle (Figure 20–20). Where you stop when you lift
In essence, cardiac output is an indication of the blood flow the handle determines how much water the pump contains—
through peripheral tissues—and without adequate blood flow, the EDV. How far down you push the handle determines how
homeostasis cannot be maintained. The cardiac output pro- much water remains in the pump at the end of the cycle—the
vides a useful indication of ventricular efficiency over time. ESV. You pump the maximum amount of water when you pull
Figure 20–19 summarizes the factors involved in the nor- the handle all the way to the top and then push it all the way to
mal regulation of cardiac output. Cardiac output can be adjusted the bottom. In other words, you get the largest stroke volume
by changes in either heart rate or stroke volume. The heart rate when the EDV is as large as it can be and the ESV is as small as
(HR), the number of heartbeats per minute, can be adjusted by it can be.
20 the activities of the autonomic nervous system or by circulat- The body precisely adjusts cardiac output to supply periph-
ing hormones. Stroke volume (SV) is the amount of blood eral tissues with enough blood as conditions change. When
pumped out of a ventricle during each contraction. necessary, the heart rate can increase by 250 percent, and stroke
We can calculate cardiac output by multiplying the heart volume in a normal heart can almost double. (In addition,
rate by the average stroke volume: a variety of other factors can influence cardiac output under
abnormal circumstances.) For convenience, the discussions in
CO = HR * SV this section consider heart rate and stroke volume indepen-
cardiac heart stroke dently. However, changes in cardiac output generally reflect
output rate volume changes in both factors.
1mL>min2 1beats>min2 1mL>beat2
For example, if the heart rate is 75 bpm and the stroke volume Factors Affecting the Heart Rate
is 80 mL per beat, the cardiac output is
Under normal circumstances, autonomic activity and circu-
75 bpm * 80 mL>beat = 6000 mL>min 16 L>min2 CO lating hormones make homeostatic adjustments to the heart
Let’s look more into stroke volume, as it is the most impor- rate as cardiovascular demands change, thereby adjusting car-
tant factor in an examination of a single cardiac cycle. Stroke diac output. These factors act by modifying the autorhythmic-
volume can be expressed as SV = EDV - ESV, where EDV is ity of the heart. Even a heart removed for a heart transplant
end-diastolic volume and ESV is end-systolic volume. EDV is continues to beat unless it is kept chilled in a preservation
the amount of blood in each ventricle at the end of ventricular solution.
diastole, while ESV is the amount of blood remaining in each
ventricle at the end of ventricular systole. The ejection fraction is the Autonomic Innervation
percentage of EDV that is ejected during a ventricular contraction. The sympathetic and parasympathetic divisions of the auto-
If the heart were a simple hand pump, the stroke volume nomic nervous system innervate the heart by means of the
would be the amount of water pumped in one up–down cycle nerve network known as the cardiac plexus (Figure 16–6,
> Go to > Study Area > > Cardiovascular System: Cardiac Cycle
M20_MART6026_11_SE_C20_pp688-726.indd 716 02/11/16 6:18 pm
Chapter 20 The Heart 717
Figure 20–20 A Simple Model of Stroke Volume. The stroke volume of the heart can be compared to the
amount of water ejected from a simple pump. The amount of water ejected varies with the amount of movement of the
pump handle.
Filling
Start When the pump handle is
raised, pressure within the
cylinder decreases, and
water enters through a
one-way valve. This
corresponds to passive
filling during ventricular At the start of the pumping
diastole. cycle, the amount of water in
the cylinder corresponds to
the amount of blood in a
ventricle at the end of
ventricular diastole. This
amount is known as the
end-diastolic volume (EDV).
Ventricular
diastole
End-systolic
volume
(ESV) End-diastolic
volume (EDV)
Stroke
volume
Pumping
When the handle is depressed as 20
far as it will go, some water will
remain in the cylinder. That amount
corresponds to the end-systolic
volume (ESV) remaining in the
ventricle at the end of ventricular
systole. The amount of water As the pump handle is pushed
pumped out corresponds to the down, water is forced out of
stroke volume of the heart; the the cylinder. This corresponds
stroke volume is the difference to the period of ventricular
between the EDV and the ESV. ejection.
Ventricular
systole
p. 549, and Figure 20–21). Postganglionic sympathetic neu- The cardiac centers of the medulla oblongata contain the
rons are located in the cervical and upper thoracic ganglia. autonomic headquarters for cardiac control. p. 474 The
The vagus nerves (CN X) carry parasympathetic preganglionic cardioacceleratory center controls sympathetic neurons that
fibers to small ganglia in the cardiac plexus. Both ANS divi- increase the heart rate. The adjacent cardioinhibitory center
sions innervate the SA and AV nodes and the atrial contrac- controls the parasympathetic neurons that slow the heart rate.
tile cells. Both divisions also innervate ventricular contractile Reflex pathways regulate the cardiac centers. They also receive
cells, but sympathetic fibers far outnumber parasympathetic input from higher centers, especially from the parasympathetic
fibers there. and sympathetic centers in the hypothalamus.
M20_MART6026_11_SE_C20_pp688-726.indd 717 24/10/16 8:14 PM
718 UNIT 4 Fluids and Transport
The cardiac centers respond to changes in
Figure 20–21 Autonomic Innervation of the Heart. blood pressure as reported by baroreceptors, and
to changes in arterial concentrations of dissolved
Vagal nucleus
oxygen and carbon dioxide as reported by chemo-
Cardioinhibitory
center receptors. For example, a decline in the blood pres-
sure or oxygen concentration or an increase in the
Cardioacceleratory carbon dioxide level generally means that the heart
center must work harder to meet the demands of periph-
Medulla
eral tissues. The cardiac centers then call for an
oblongata
increase in cardiac activity. We detail these reflexes
and their effects on the heart and peripheral vessels
Vagus nerve (X)
in Chapter 21.
Spinal cord
Autonomic Tone. Like other organs with dual
innervation, the heart has a resting autonomic tone.
Both autonomic divisions are normally active at a
Sympathetic Parasympathetic steady background level, releasing acetylcholine
(ACh) and norepinephrine (NE) at the nodes and
Parasympathetic into the myocardium. For this reason, cutting the
preganglionic vagus nerves increases the heart rate, and sympa-
Sympathetic fiber thetic blocking agents slow the heart rate.
preganglionic Synapses in Parasympathetic effects dominate in a healthy,
fiber cardiac plexus
resting individual. Without autonomic innerva-
Sympathetic ganglia
Parasympathetic tion, the pacemaker cells of the SA node estab-
(cervical ganglia and
postganglionic
superior thoracic
fibers
lish the heart rate. Such a heart beats at a rate of
ganglia [ T1–T4 ]) 80–100 bpm. At rest, a typical adult heart with nor-
Sympathetic mal innervation beats more slowly, at 70–80 bpm,
postganglionic fiber due to activity in the parasympathetic nerves
Cardiac nerve innervating the SA node. If parasympathetic activ-
20 ity increases, the heart rate declines further. Con-
versely, the heart rate increases if parasympathetic
activity decreases, or if sympathetic activation
occurs. Through dual innervation and adjustments
in autonomic tone, the ANS can make very delicate
adjustments in cardiovascular function to meet the
? Which division of the autonomic nervous system would increase heart rate?
demands of other systems.
Effects on the Pacemaker Cells of the SA Node. How do
the sympathetic and parasympathetic divisions alter the heart
Tips & Tools rate? They do so by changing the ionic permeabilities of cells
To remember the effect of the sympathetic nervous system in the conducting system. The most dramatic effects take place
on cardiac performance, remember that sympathetic input at the SA node, which affects the heart rate through changes in
speeds and strengthens the heartbeat. the rate at which impulses are generated.
Consider the SA node of a resting individual whose heart is
Cardiac Reflexes. Information about the status of the car- beating at 75 bpm (Figure 20–22a). Any factor that changes the
diovascular system arrives over visceral sensory fibers accom- rate of spontaneous depolarization or the duration of repolar-
panying the vagus nerve and the sympathetic nerves of the ization in pacemaker cells will alter the heart rate by changing
cardiac plexus. The cardiac centers monitor baroreceptors the time required for these cells to reach threshold. Acetyl-
and chemoreceptors innervated by the glossopharyngeal (IX) choline released by parasympathetic neurons opens chemically
and vagus (X) nerves. pp. 502, 503 On the basis of the gated K + channels in the plasma membrane. Then K + leaves the
information received, the cardiac centers adjust the heart’s pacemaker cells, dramatically slowing their rate of spontaneous
activity to maintain adequate circulation to vital organs, such depolarization and also slightly extending their duration of
as the brain. repolarization (Figure 20–22b). As a result, heart rate declines.
M20_MART6026_11_SE_C20_pp688-726.indd 718 24/10/16 8:14 PM
Chapter 20 The Heart 719
Figure 20–22 Autonomic Regulation of Pacemaker Cell Function. Venous Return and the Bainbridge Reflex
Venous return is the amount of blood returning to
Normal (resting) Spontaneous the heart through veins. Venous return directly affects
+20
depolarization pacemaker cells. When venous return increases, the
Membrane 0
potential atria receive more blood and the walls are stretched.
(mV) Stretching of the cardiac pacemaker cells of the SA node
–30
Threshold
leads to more rapid depolarization and an increase in
the heart rate.
–60 Venous return also has an indirect effect on heart
Heart rate: 75 bpm
rate. The Bainbridge reflex, or atrial reflex, involves
0.8 1.6 2.4 adjustments in heart rate in response to an increase in
a Pacemaker cells have membrane potentials closer to the venous return. When the walls of the right atrium
threshold than those of cardiac contractile cells (–60 mV are stretched, stretch receptors there trigger a reflexive
versus –90 mV). Their plasma membranes spontane-
increase in heart rate by stimulating sympathetic activ-
ously depolarize to threshold, producing action poten-
tials at a frequency determined by (1) the membrane ity (see Figure 20–22). Thus, when the rate of venous
potential and (2) the rate of depolarization. return to the heart increases, so does the heart rate, and
for this reason the cardiac output increases as well.
Parasympathetic stimulation
+20
Hormones and Factors Affecting Heart Rate
Membrane
0
potential Epinephrine (E), norepinephrine (NE), and thyroid hor-
(mV) mone (T3,) increase heart rate by their effects on the
–30
SA node. The effects of E on the pacemaker cells of the SA
Threshold
Hyperpolarization node are similar to those of NE. Epinephrine also affects
–60 the cardiac contractile cells. After massive sympathetic
Heart rate: 40 bpm Slower depolarization stimulation of the adrenal medullae, the myocardium
may become so excitable that abnormal contractions
0.8 1.6 2.4
occur. Factors that increase the heart rate are positively
b Parasympathetic stimulation releases ACh, which
chronotropic (chrono-, time) and factors that decrease the
extends repolarization and decreases the rate of
spontaneous depolarization. The heart rate slows. heart rate are negatively chronotropic. 20
Sympathetic stimulation Factors Affecting the Stroke Volume
+20
Membrane Changes in either EDV or ESV can change the stroke
potential 0 volume, and thus cardiac output. The factors involved
(mV) in the regulation of stroke volume are indicated in
–30
Threshold Figure 20–23.
Reduced repolarization
–60 The End-Diastolic Volume (EDV)
More rapid
Heart rate: 120 bpm depolarization
Two factors affect the EDV, the amount of blood in a
0.8 1.6 2.4 ventricle at the end of diastole: the filling time and the
Time (sec) venous return. Filling time is the duration of ventricu-
c Sympathetic stimulation releases NE, which shortens lar diastole. It depends entirely on the heart rate: The
repolarization and accelerates the rate of spontaneous faster the heart rate, the shorter the filling time. Venous
depolarization. As a result, the heart rate increases. return is variable over this period. It varies in response
to changes in cardiac output, blood volume, peripheral
Norepinephrine released by sympathetic neurons binds circulation, skeletal muscle activity, and other factors that affect
to beta-1 receptors, leading to the opening of sodium ion the rate of blood flow back to the heart. (We explore these fac-
and calcium ion channels. Then an influx of positively tors in Chapter 21.)
charged ions increases the rate of depolarization and
shortens the period of repolarization. The pacemaker cells Preload. The degree of stretching in ventricular muscle cells
reach threshold more quickly, and the heart rate increases during ventricular diastole is called the preload. The preload
(Figure 20–22c ). is directly proportional to the EDV: The greater the EDV,
M20_MART6026_11_SE_C20_pp688-726.indd 719 24/10/16 8:14 PM
720 UNIT 4 Fluids and Transport
Figure 20–23 Factors Affecting Stroke Volume.
Factors Affecting Stroke Volume (SV)
KEY
Venous return (VR) Filling time (FT) Sympathetic Parasympathetic E, NE, glucagon, = increased
VR = EDV FT = EDV stimulation stimulation thyroid hormones = decreased
VR = EDV FT = EDV
increases decreases increases
Contractility (Cont)
of muscle cells
Preload Cont = ESV
Cont = ESV Vasoconstriction Vasodilation
increases decreases
Afterload (AL)
End-diastolic End-systolic AL = ESV
volume (EDV) volume (ESV) AL = ESV
EDV = SV ESV = SV
STROKE VOLUME (SV)
EDV = SV ESV = SV
the larger the preload. Preload matters because it affects the increase in the stroke volume. This general rule of “more in =
ability of muscle cells to produce tension. As sarcomere length more out” is known as the Frank–Starling principle.
increases past resting length, the amount of force produced Autonomic adjustments to cardiac output normally make
during systole increases. the effects of the Frank–Starling principle difficult to see. How-
The amount of preload, and hence the degree of myocar- ever, we can see the effects more clearly in heart transplant
20 dial stretching, varies with the demands on the heart. When you patients, because the implanted heart is not innervated by the
are standing at rest, your EDV is low. The ventricular muscle ANS. So, the outputs of the left and right ventricles remain bal-
is stretched very little, and the sarcomeres are relatively short. anced under a variety of conditions.
During ventricular systole, the cardiac contractile cells develop Consider, for example, a person at rest, with the two
little power, and the ESV (the amount of blood in the ventricle ventricles ejecting equal volumes of blood. Although the ven-
after contraction) is relatively high because the contractile cells tricles contract together, they work in series: When the heart
contracted only a short distance. If you begin exercising, venous contracts, blood leaving the right ventricle heads to the lungs.
return increases and more blood flows into your heart. Your During the next ventricular diastole, that volume of blood
EDV increases, and the myocardium stretches further. As the passes through the left atrium, to be ejected by the left ven-
sarcomeres approach optimal lengths, the ventricular contrac- tricle at the next contraction. If the venous return decreases,
tile cells can contract more efficiently and produce more force- the EDV of the right ventricle will decrease. During ventricular
ful contractions. They also shorten more, and more blood is systole, the right ventricle will then pump less blood to the
pumped out of your heart. lungs. In the next cardiac cycle, the EDV of the left ventricle
will be reduced, and that ventricle will eject a smaller vol-
The EDV and Stroke Volume: The Frank–Starling
ume of blood. The output of the two ventricles will again be
Principle. In general, the greater the EDV, the larger the stroke
in balance, but both will have smaller stroke volumes than
volume. Stretching the cardiac contractile cells past their opti-
they did initially.
mal length would reduce the force of contraction, but this
degree of stretching does not normally take place. Myocardial
connective tissues, the cardiac skeleton, and the pericardium all The End-Systolic Volume (ESV)
limit the expansion of the ventricles. After the ventricle has contracted and ejected the stroke volume,
The relationship between the amount of ventricular stretch- the amount of blood that remains in the ventricle at the end
ing and the contractile force means that, within normal physi- of ventricular systole is the ESV. Three factors that influence the
ological limits, increasing the EDV results in a corresponding ESV are preload, ventricular contractility, and afterload.
M20_MART6026_11_SE_C20_pp688-726.indd 720 24/10/16 8:14 PM
Chapter 20 The Heart 721
Contractility. Contractility is the amount of force produced Many of the drugs used to treat hypertension (high blood
during a contraction, at a given preload. Under normal circum- pressure) are negatively inotropic. Beta-blocking drugs such as
stances, autonomic innervation or circulating hormones can propranolol, metoprolol, atenolol, and labetalol block beta recep-
alter contractility. Under special circumstances, drugs or abnor- tors, alpha receptors, or both, and prevent sympathetic stimula-
mal ion concentrations in the extracellular fluid can alter con- tion of the heart. Calcium-channel blockers such as nifedipine or
tractility. verapamil are negatively inotropic.
Factors that strengthen heart contraction are positively ino-
.
Afterload. The afterload is the amount of tension that the
tropic (I-no-tro-pik) (ino-, fiber). Factors that weaken heart
. .
contracting ventricle must produce to force open the semilu-
contraction are negatively inotropic. Positive inotropic agents
nar valve and eject blood. Afterload increases with increased
typically stimulate Ca2+ entry into cardiac contractile cells, thus
resistance to blood flow out of the ventricle. The greater the
increasing the force and duration of ventricular contractions.
afterload, the longer the period of isovolumetric contraction,
Negative inotropic agents may block Ca2+ movement or depress
the shorter the duration of ventricular ejection, and the larger
cardiac muscle metabolism. Positive and negative inotropic
the ESV. In other words, as the afterload increases, the stroke
factors include ANS activity, hormones, and changes in extracel-
volume decreases.
lular ion concentrations.
Any factor that restricts blood flow through the arterial sys-
Effects of Autonomic Activity on Contractility. Autonomic tem increases afterload. For example, either the constriction of
activity alters the degree of contraction and changes the ESV in peripheral blood vessels or a circulatory blockage elevates arterial
the following ways: blood pressure and increases the afterload. If the afterload is too
great, the ventricles cannot eject blood. Such a high afterload is
■ Sympathetic stimulation has a positive inotropic effect. It
rare in a normal heart. However, damage to the heart muscle
causes the release of norepinephrine (NE) by postganglionic
can weaken the myocardium enough that even a modest rise in
fibers of the cardiac nerves and the secretion of epinephrine
arterial blood pressure can decrease the stroke volume to a dan-
(E) and NE by the adrenal medullae. These hormones affect
gerously low level, producing heart failure. Damage to the semi-
heart rate. They also stimulate alpha and beta receptors in
lunar valve that restricts blood flow will also increase afterload.
cardiac contractile cell plasma membranes. This stimulation
increases the metabolism of these cells. The net effect is that
the ventricles contract more forcefully, increasing the ejec- Summary: The Control of Cardiac Output
tion fraction and decreasing the ESV.
Figure 20–24 summarizes the factors that regulate heart rate
■ Parasympathetic stimulation from the vagus nerves has a and stroke volume, which interact to determine cardiac output. 20
negative inotropic effect. The primary effect of acetylcho- The heart rate is influenced by the autonomic nervous system,
line (ACh) is at the cardiac contractile cell membrane sur- circulating hormones, and venous return.
face, where it produces hyperpolarization and inhibition.
■ Sympathetic stimulation increases the heart rate, and para-
As a result, the force of cardiac contractions is reduced.
sympathetic stimulation decreases it. Under resting condi-
The atria show the greatest changes in contractile force
tions, parasympathetic tone dominates, and the heart rate
because the ventricles are not extensively innervated by
is slightly slower than the intrinsic heart rate. When the
the parasympathetic division. However, under strong para-
activity level rises, venous return increases and triggers the
sympathetic stimulation or with drugs that mimic ACh,
Bainbridge reflex. The result is an increase in sympathetic
the ventricles contract less forcefully, the ejection fraction
tone and an increase in heart rate.
decreases, and the ESV becomes larger.
■ Circulating hormones, specifically E, NE, and T3, accelerate
Hormones Affecting Contractility. Many hormones affect heart rate.
heart contractility. For example, epinephrine, norepineph- ■ An increase in venous return stretches the pacemaker cells
rine, glucagon, and thyroid hormones are positively inotropic. and increases heart rate.
Before synthetic inotropic drugs were available, glucagon was
■ The stroke volume (SV) is the difference between the end-
used to stimulate cardiac function. It is still used in cardiac
diastolic volume (EDV) and the end-systolic volume (ESV).
emergencies and to treat some forms of heart disease.
The drugs isoproterenol, dopamine, and dobutamine mimic E ■ The EDV is determined by the available filling time and the
and NE by stimulating beta-1 receptors on cardiac contractile rate of venous return.
cells. Dopamine (at high doses) and dobutamine also stimu- ■ The ESV is determined by the amount of preload (the degree
late Ca2+ entry through alpha-1 receptor stimulation. Digitalis of myocardial stretching), the degree of contractility (adjusted
elevates the intracellular Ca2+ concentration by interfering with by hormones and autonomic innervation), and the afterload
Ca2+ removal from the cytosol of cardiac contractile cells. (the arterial resistance to blood flow out of the heart).
M20_MART6026_11_SE_C20_pp688-726.indd 721 24/10/16 8:14 PM
722 UNIT 4 Fluids and Transport
Figure 20–24 A Summary of the Factors Affecting Cardiac Output.
Maximum for
trained athletes
40 exercising at Factors affecting Factors affecting
peak levels
heart rate (HR) stroke volume (SV)
35
Skeletal Blood Changes in
muscle volume peripheral
activity circulation
30
Bainbridge
Venous Filling Autonomic
(atrial) Hormones
return time innervation
reflex
Normal range
Cardiac output (L/min)
25 of cardiac
output during Vasodilation
heavy exercise Preload Contractility
or
vasoconstriction
20
Autonomic End-diastolic End-systolic
Hormones Afterload
innervation volume volume
15
10 HEART RATE (HR) STROKE VOLUME (SV) = EDV – ESV
Average resting
cardiac output
5
Heart failure
CARDIAC OUTPUT (CO) = HR x SV
20 0
a Cardiac output varies widely b Factors affecting cardiac output
to meet metabolic demands
? What is considered a “normal” cardiac output when resting? Please provide units.
During exercise, increasing both the stroke volume and the The Heart and the Vessels of the
heart rate can increase the cardiac output by 300–500 percent, Cardiovascular System
to 18–30 L/min. The difference between resting and maximal
The purpose of cardiovascular regulation is to maintain ade-
cardiac outputs is the cardiac reserve. Trained athletes exercis-
quate blood flow to all body tissues. The heart cannot accom-
ing at maximal levels may increase cardiac output by nearly
plish this by itself, and it does not work in isolation. For
700 percent, to 40 L/min.
example, when blood pressure changes, the cardiac centers
Cardiac output cannot increase indefinitely, primarily
adjust not only the heart rate but also the diameters of periph-
because the available filling time shortens as the heart rate
eral blood vessels. These adjustments work together to keep
increases. At heart rates up to 160–180 bpm, the combination
the blood pressure within normal limits and to maintain cir-
of increased venous return rate and increased contractility com-
culation to vital tissues and organs. In Chapter 21 we complete
pensates for the reduced filling time. Over this range, cardiac
this story by detailing the cardiovascular responses to chang-
output and heart rate increase together. But if the heart rate
ing activities and circulatory emergencies. We then conclude
continues to climb, the stroke volume begins to drop. Cardiac
our discussion of the cardiovascular system by examining the
output first plateaus and then declines.
anatomy of the pulmonary and systemic circuits.
> Go to > Study Area > Menu > > Cardiovascular System: Cardiac Output
M20_MART6026_11_SE_C20_pp688-726.indd 722 02/11/16 6:18 pm
Chapter 20 The Heart 723
15. What effect would stimulating the acetylcholine receptors
Checkpoint of the heart have on cardiac output?
12. Define cardiac output. 16. What effect would an increase in venous return have on
13. Caffeine has effects on cardiac conducting cells and the stroke volume?
contractile cells that are similar to those of NE. What effect 17. Joe’s end-systolic volume is 40 mL, and his end-diastolic
would drinking large amounts of caffeinated drinks have volume is 125 mL. What is Joe’s stroke volume?
on the heart?
14. Why is it a potential problem if the heart beats too rapidly? See the blue Answers tab at the back of the book.
20 Chapter Review
Study Outline
An Introduction to the Heart as Part of the Cardiovascular > Access more chapter study tools online
System p. 689 in the MasteringA&P Study Area:
■ Chapter Quizzes, Chapter Practice Test, MP3 Tutor Sessions,
1. The blood vessels can be subdivided into the pulmonary
and Clinical Case Studies
circuit (which carries blood to and from the lungs) and the
■ Practice Anatomy Lab 3.0 ■ A&P Fli
™
systemic circuit (which transports blood to and from the rest
of the body). ■ Interactive Physiology ■ PhysioEx
2. Arteries carry blood away from the heart; veins return blood
to the heart. Capillaries, or exchange vessels, are thin-walled,
narrow-diameter vessels that connect the smallest arteries and by the chordae tendineae, which are connected to papillary
veins. (Figure 20–1) muscles. (Figure 20–5)
3. The heart has four chambers: the right atrium and right 10. Blood leaving the right ventricle enters the pulmonary
ventricle, and the left atrium and left ventricle. trunk after passing through the pulmonary valve. The
pulmonary trunk divides to form the left and right
20-1 The heart is a four-chambered organ that pulmonary arteries. The left and right pulmonary veins
pumps blood through the pulmonary and systemic return blood from the lungs to the left atrium. Blood leav-
circuits p. 689 ing the left atrium flows into the left ventricle through the
4. The heart is surrounded by the pericardium and lies within mitral valve (left atrioventricular valve or bicuspid valve).
the anterior portion of the mediastinum, which separates the Blood leaving the left ventricle passes through the aortic
two pleural cavities. (Figure 20–2) valve and into the systemic circuit by the ascending aorta.
5. The pericardial cavity is lined by the pericardium. The visceral (Figure 20–5)
layer of serous pericardium (epicardium) covers the heart’s 11. Anatomical differences between the ventricles reflect the func-
outer surface, and the parietal layer of serous pericardium tional demands placed on them. The wall of the right ventricle
lines the inner surface. (Figure 20–2) is relatively thin, whereas the left ventricle has a massive mus-
6. The coronary sulcus, a deep groove, marks the boundary cular wall. (Figure 20–6)
between the atria and the ventricles. Other surface markings 12. The connective tissues of the heart (mainly collagen and elas-
also provide useful reference points in describing the heart tic fibers) and the cardiac skeleton support the heart’s valves
and associated structures. (Figure 20–3) and ventricular muscle cells. (Figure 20–7)
7. The bulk of the heart consists of the muscular myocardium. 13. Valves normally permit blood flow in only one direction, pre-
The endocardium lines the inner surfaces of the heart, venting the regurgitation (backflow) of blood. (Figure 20–7)
and the visceral layer of serous pericardium covers the 14. The coronary circulation meets the high oxygen and
outer surface. The endothelium of the endocardium is con- nutrient demands of cardiac muscle cells. The coronary
tinuous with the endothelium of the attached great vessels. arteries originate at the base of the ascending aorta. Inter-
(Figure 20–4) connections between arteries, called arterial anastomoses,
8. The atria are separated by the interatrial septum, and the ensure a constant blood supply. The great, posterior, small,
ventricles are divided by the interventricular septum. The anterior, and middle cardiac veins are epicardial vessels
right atrium receives blood from the systemic circuit via two that carry blood from the coronary capillaries to the coro-
large veins, the superior vena cava and the inferior vena nary sinus. (Figure 20–8)
cava. (The atrial walls contain the pectinate muscles, promi- 15. In coronary artery disease (CAD), portions of the coronary
nent muscular ridges.) (Figure 20–5) circulation undergo partial or complete blockage. A myocardial
9. Blood flows from the right atrium into the right ventricle infarction (MI), or heart attack, occurs when part of the coro-
by the tricuspid valve (right atrioventricular valve). This nary circulation becomes blocked and muscle tissue dies when
opening is bounded by three cusps of fibrous tissue braced it cannot be oxygenated. (Spotlight Figure 20–9)
M20_MART6026_11_SE_C20_pp688-726.indd 723 24/10/16 8:14 PM
724 UNIT 4 Fluids and Transport
20-2 The cells of the conducting system distribute 24. When the heart beats, the two ventricles eject equal volumes of
electrical impulses through the heart, causing cardiac blood. (Figure 20–17)
contractile cells to contract p. 702 25. The closing of valves and rushing of blood through the heart
cause characteristic heart sounds, which can be heard during
16. Two general classes of cardiac muscle cells are involved in the
auscultation. (Figure 20–18)
normal heartbeat: autorhythmic cells and contractile cells.
17. The conducting system is composed of the sinoatrial node,
the atrioventricular node, and conducting cells. The conducting
20-4 Cardiac output is determined by heart rate and
stroke volume p. 716
system initiates and distributes electrical impulses within
the heart. Nodal cells establish the rate of cardiac contrac- 26. Cardiac output can be adjusted by changes in either heart rate
tion, and conducting cells distribute the contractile stimulus or stroke volume. (Figure 20–19)
from the SA node to the atrial myocardium and the AV node 27. The amount of blood ejected by a ventricle during a single
(along internodal pathways), and from the AV node to the beat is the stroke volume (SV). The amount of blood
ventricular myocardium. (Figure 20–10) pumped by a ventricle each minute is the cardiac output
18. Unlike skeletal muscle, cardiac muscle contracts without neu- (CO). (Figure 20–20)
ral or hormonal stimulation. Pacemaker cells in the sino- 28. The cardioacceleratory center in the medulla oblongata
atrial (SA) node (cardiac pacemaker) normally establish the activates sympathetic neurons; the cardioinhibitory center
rate of contraction. From the SA node, the stimulus travels to controls the parasympathetic neurons that slow the heart rate.
the atrioventricular (AV) node, and then to the AV bundle, These cardiac centers receive inputs from higher centers and
which divides into bundle branches. From there, Purkinje from receptors monitoring blood pressure and the concentra-
fibers convey the impulses to the ventricular myocardium. tions of dissolved gases. (Figure 20–21)
(Figures 20–10, 20–11) 29. The basic heart rate is established by the pacemaker cells
19. A recording of electrical activities in the heart is an electro- of the SA node, but it can be modified by the autonomic
cardiogram (ECG or EKG). Important landmarks of an ECG nervous system. The Bainbridge reflex (atrial reflex) accel-
include the P wave (atrial depolarization), the QRS complex erates the heart rate when the walls of the right atrium are
(ventricular depolarization), and the T wave (ventricular repo- stretched. (Figure 20–22)
larization). (Figure 20–12) 30. Sympathetic activity increases the force of contraction
20. Cardiac arrhythmias are abnormal patterns of electrical activ- (contractility), which reduces the ESV. Parasympathetic
ity in the heart. (Spotlight Figure 20–13) stimulation slows the heart rate, reduces contractility, and
21. Cardiac contractile cells are interconnected by intercalated raises the ESV.
discs, which convey the force of contraction from cell to cell 31. Cardiac output is affected by various factors, including auto-
and conduct action potentials. (Figure 20–14; Table 20–1) nomic innervation and hormones. (Figure 20–22)
22. Contractile cells form the bulk of the atrial and ventricular 32. The stroke volume is the difference between the end-diastolic
walls. Cardiac contractile cells have a long refractory period, so volume (EDV) and the end-systolic volume (ESV). The
20 rapid stimulation produces twitches rather than tetanic con- filling time and venous return interact to determine the
tractions. (Figure 20–15) EDV. Normally, the greater the EDV, the more powerful
the succeeding contraction (the Frank–Starling principle).
20-3 The contraction–relaxation events that occur during (Figure 20–23)
a complete heartbeat make up a cardiac cycle p. 711 33. The difference between resting and maximal cardiac outputs is
23. The cardiac cycle includes periods of atrial and ventricular the cardiac reserve. (Figure 20–24)
systole (contraction) and atrial and ventricular diastole 34. The heart does not work in isolation in maintaining adequate
(relaxation). (Figure 20–16) blood flow to all tissues.
Review Questions See the blue Answers tab at the back of the book.
LEVEL 1 Reviewing Facts and Terms 5. The heart is surrounded by the (a) pleural cavity, (b) peritoneal
1. The great cardiac vein drains blood from the heart muscle to the cavity, (c) abdominopelvic cavity, (d) mediastinum, (e) abdominal
(a) left ventricle, (b) right ventricle, (c) right atrium, (d) left atrium. cavity.
2. The autonomic centers for cardiac function are located in (a) the 6. The cardiac skeleton of the heart has which two of the following func-
myocardial tissue of the heart, (b) the cardiac centers of the medulla tions? (a) It physically isolates the muscle fibers of the atria from
oblongata, (c) the cerebral cortex, (d) all of these structures. those of the ventricles. (b) It maintains the normal shape of the heart.
3. The serous membrane covering the outer surface of the heart is the (c) It helps distribute the forces of cardiac contraction. (d) It allows
(a) parietal layer of the serous pericardium, (b) endocardium, more rapid contraction of the ventricles. (e) It strengthens and helps
(c) myocardium, (d) visceral layer of the serous pericardium. prevent overexpansion of the heart.
4. The simple squamous epithelium covering the heart valves is the 7. Cardiac output is equal to the (a) difference between the end-diastolic
(a) epicardium, (b) endocardium, (c) myocardium, (d) endothelium. volume and the end-systolic volume, (b) product of heart rate and
M20_MART6026_11_SE_C20_pp688-726.indd 724 24/10/16 8:14 PM
Chapter 20 The Heart 725
stroke volume, (c) difference between the stroke volume at rest 10. During diastole, a chamber of the heart (a) relaxes and fills with
and the stroke volume during exercise, (d) stroke volume less blood, (b) contracts and pushes blood into an adjacent chamber,
the end-systolic volume, (e) product of heart rate and blood (c) experiences a sharp increase in pressure, (d) reaches a pressure of
pressure. approximately 120 mm Hg.
8. Identify the superficial structures in the following diagram of the 11. During the cardiac cycle, the amount of blood ejected from the left
heart. ventricle when the semilunar valve opens is the (a) stroke volume
(SV), (b) end-diastolic volume (EDV), (c) end-systolic volume (ESV),
(d) cardiac output (CO).
e
12. What role do the chordae tendineae and papillary muscles play in the
normal function of the AV valves?
13. Describe the three distinct layers that make up the heart wall.
14. What are the valves in the heart, and what is the function of each?
f 15. Trace the normal pathway of an electrical impulse through the con-
a ducting system of the heart.
g
16. What is the cardiac cycle? What phases and events are necessary to
b h complete a cardiac cycle?
17. What three factors regulate stroke volume to ensure that the left and
right ventricles pump equal volumes of blood?
c LEVEL 2 Reviewing Concepts
18. The cells of the conducting system differ from the contractile cells of
d the heart in that (a) conducting cells are larger and contain more
myofibrils, (b) contractile cells exhibit pacemaker potentials, (c) con-
tractile cells do not normally exhibit autorhythmicity, (d) both a and b
are correct.
19. Which of the following is longer? (a) the refractory period of a
cardiac contractile cell, (b) the refractory period of skeletal
(a) ___________ (b) ___________ muscle fiber.
(c) ___________ (d) ___________ 20. If the papillary muscles fail to contract, (a) the ventricles will not
(e) ___________ (f) ___________ pump blood, (b) the atria will not pump blood, (c) the semilunar
(g) ___________ (h) ___________ valves will not open, (d) the AV valves will not close properly,
(e) none of these happen.
9. Identify the structures in the following diagram of a sectional view of 21. Cardiac output cannot increase indefinitely because (a) the available
the heart. filling time becomes shorter as the heart rate increases, (b) the car-
diovascular centers adjust the heart rate, (c) the rate of spontaneous
depolarization decreases, (d) the ion concentrations of pacemaker
plasma membranes decrease.
22. Describe the function of the SA node in the cardiac cycle. How does 20
this function differ from that of the AV node?
g
23. What are the sources and significance of the four heart sounds?
24. Differentiate between stroke volume and cardiac output. How is
cardiac output calculated?
a
h 25. What factors influence cardiac output?
26. What effect does sympathetic stimulation have on the heart? What
b i effect does parasympathetic stimulation have on the heart?
j 27. Describe the effects of epinephrine, norepinephrine, glucagon, and
c
k thyroid hormones on the contractility of the heart.
l LEVEL 3 Critical Thinking and Clinical Applications
d 28. Vern is suffering from cardiac arrhythmias and is brought into the
emergency room of a hospital. In the emergency room he begins to ex-
e m hibit tachycardia and as a result loses consciousness. Explain why Vern
lost consciousness.
f 29. Harvey has a heart murmur in his left ventricle that produces a loud
“gurgling” sound at the beginning of systole. Which valve is probably
faulty?
30. The following measurements were made on two individuals (the val-
ues recorded remained stable for 1 hour):
Person 1: heart rate, 75 bpm; stroke volume, 60 mL
Person 2: heart rate, 90 bpm; stroke volume, 95 mL
(a) ___________ (b) ___________ (c) ___________ Which person has the greater venous return? Which person has the
(d) ___________ (e) ___________ (f) ___________ longer ventricular filling time?
(g) ___________ (h) ___________ (i) ___________ 31. Karen is taking the medication verapamil, a drug that blocks the cal-
(j) ___________ (k) ___________ (l) ___________ cium channels in cardiac muscle cells. What effect should this medica-
(m) ___________ tion have on Karen’s stroke volume?
M20_MART6026_11_SE_C20_pp688-726.indd 725 24/10/16 8:14 PM
726 UNIT 4 Fluids and Transport
+ CLINICAL CASE Wrap-Up A Needle to the Chest
With the force of the head-on collision, the patient’s with a narrow difference between the systolic blood
chest first broke the seat belt and then collided pressure and the diastolic blood pressure. The ultra-
with the steering wheel. This caused fractures of sound confirmed fluid in the pericardial cavity that
the anterior chest wall, including the sternum was compressing the heart.
and ribs. Dr. Jim knew this victim was suffering from
The heart, located just deep to the sternum, then cardiac tamponade due to blood in the pericardial
hit the steering wheel hard enough to cause bleeding space. He also knew the problem was severe
into the pericardial cavity. As the delicate parietal and enough that with the decreasing stroke volume,
visceral pericardial linings bled into the pericardial cavity, the tough, the heart could not pump adequate blood to the patient’s brain.
fibrous connective tissue of the parietal layer itself did not expand. So he removed the blood from the pericardial space with a
The blood in the pericardial cavity compressed the heart, needle, a procedure known as pericardiocentesis, and saved
squeezing the atria and ventricles. During atrial diastole, the atria this patient’s life.
could not fill. This caused a backup of the venous system that was 1. Why do you think the heart sounds were muffled and distant?
obvious in the veins of the patient’s neck. The compressed ven-
2. What other cardiac structures were likely to be injured by this
tricles could not fill with blood during ventricular diastole. Because
collision?
the end-diastolic volume (EDV) was so low, the stroke volume (SV)
was also very low. This was evident in the blood pressure of 80/58, See the blue Answers tab at the back of the book.
Related Clinical Terms
artificial pacemaker: A small, battery-operated device that keeps maintain adequate blood circulation in the peripheral tissues and
one’s heart beating in a regular rhythm. It may be permanently the lungs.
implanted or temporarily placed externally. cor pulmonale: Weakness of the right ventricle of the heart due
asystole: The absence of cardiac activity with no contraction and to prolonged high blood pressure in the pulmonary artery and
20 no output. right ventricle; or any disease or malfunction that affects the pul-
automated external defibrillator (AED): A device that, when monary circuit in the lungs.
applied, automatically checks the function of the heart. Upon echocardiography: A noninvasive diagnostic test that uses
detecting a condition that may respond to an electric shock, it ultrasound to make images of the heart chambers, valves, and
delivers a shock to restore normal heartbeat rhythm. surrounding structures. This diagnostic tool can also measure
automatic implantable cardioverter defibrillator (AICD): cardiac output, detect inflammation around the heart, identify
A surgically implanted battery-operated device that monitors abnormal anatomy, and detect infections of the heart valves.
the function of the heart. Upon detecting a condition that may endocarditis: Inflammation or infection of the endocardium, the
respond to an electric shock, such as a disorganized heartbeat, inner lining of the heart muscle.
the device delivers a shock to restore normal heartbeat rhythm. fibrillation: Fast twitching of the heart muscle fibers with little or no
cardiac arrest: Sudden stopping of the pumping action of the movement of the muscle as a whole. Atrial fibrillation occurs in
heart causing the loss of arterial blood pressure. the atria of the heart and is characterized by chaotic quivers and
cardiology: The branch of medicine dealing with the diagnosis and irregular ventricular beating with both atria and ventricles being
treatment of heart disorders and related conditions. out of sync.
cardiomegaly: An enlarged heart, which is a sign of some other heart block: Delay in the normal electrical pulses that cause the
condition such as stress, weakening of the heart muscle, coro- heart to beat.
nary artery disease, heart valve problems, or abnormal heart mitral valve prolapse: A condition in which the mitral (bicuspid)
rhythms. valve cusps do not close properly and are pushed back toward
cardiomyoplasty: A surgical procedure that uses stimulated latis- the left atrium.
simus dorsi muscle to assist with cardiac function. The latissimus myocarditis: Inflammation of the myocardium, the middle layer of
dorsi muscle is relocated and wrapped around the left and right the heart wall tissue.
ventricles and stimulated to contract during cardiac systole by palpitation: Irregular and rapid beating of the heart.
means of an implanted burst-stimulator. percutaneous transluminal coronary angioplasty (PTCA): The sur-
commotio cordis: Sudden cardiac arrest as the result of a blunt hit gical use of a balloon-tipped catheter to enlarge a narrowed artery.
or impact to the chest. sick sinus syndrome: A group of heart rhythm disorders or prob-
congestive heart failure: The heart condition of weakness, edema, lems in which the sinoatrial node does not work properly to
and shortness of breath caused by the inability of the heart to regulate the heart rhythms.
M20_MART6026_11_SE_C20_pp688-726.indd 726 24/10/16 8:14 PM
You might also like
- EKG Exam Study Guide PDFDocument31 pagesEKG Exam Study Guide PDFmeb100% (1)
- Basic Life Support: Practice Test QuestionsDocument6 pagesBasic Life Support: Practice Test QuestionsDay Moreno100% (3)
- Case Study - PneumoniaDocument14 pagesCase Study - Pneumonianeil garcia89% (36)
- Lecture 4 Properties of Myocardium and Cardiac Cycle 2020-2021Document43 pagesLecture 4 Properties of Myocardium and Cardiac Cycle 2020-2021badarbhai222No ratings yet
- Lecture Notes NCM 102: Union Christian College College of NursingDocument77 pagesLecture Notes NCM 102: Union Christian College College of Nursingnarswiponshistoryan100% (1)
- CCN CardioDocument5 pagesCCN CardioSofia P. PanlilioNo ratings yet
- Lesson 3Document71 pagesLesson 3Angel joyce ValenciaNo ratings yet
- The Circulatory SystemDocument53 pagesThe Circulatory SystemVera June RañesesNo ratings yet
- Body Fluids & CirculationDocument29 pagesBody Fluids & CirculationAyaan AshrafNo ratings yet
- Digital Heart Beat Counter: Project Report ONDocument76 pagesDigital Heart Beat Counter: Project Report ONlkosumdecNo ratings yet
- Ecg InterpretationDocument82 pagesEcg InterpretationROMULO NU�EZ JR.No ratings yet
- الجهاز الدوريDocument16 pagesالجهاز الدوريHUAWEI HUAWEINo ratings yet
- Regulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowDocument20 pagesRegulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowShveta MahajanNo ratings yet
- Cardiovascular System - Electrical SystemDocument5 pagesCardiovascular System - Electrical SystemRashid DayaoNo ratings yet
- The Mammalian Circulatory SystemDocument58 pagesThe Mammalian Circulatory Systemirisgoldcaster100% (1)
- Structure and Function of The Cardiovascular System PDFDocument9 pagesStructure and Function of The Cardiovascular System PDFteuuuuNo ratings yet
- Heart & Hemodynamics NotesDocument8 pagesHeart & Hemodynamics NotesBrandice BradleyNo ratings yet
- Cardiovascular SystemDocument9 pagesCardiovascular SystemMayim LouiseNo ratings yet
- Heart ChambersDocument14 pagesHeart Chambersberniebernie20No ratings yet
- Components of The Cardiovascular SystemDocument23 pagesComponents of The Cardiovascular SystemMr. DummyNo ratings yet
- Cardiac PhysiologyDocument102 pagesCardiac PhysiologyPeter Larsen100% (1)
- Lecture - 3 Properties of Cardiac MuscleDocument35 pagesLecture - 3 Properties of Cardiac MuscleMRM7MDNo ratings yet
- Circulatory System ReadingDocument4 pagesCirculatory System ReadingAlejandro PabonNo ratings yet
- Clinical PaperDocument18 pagesClinical Paperapi-356406300No ratings yet
- Cardiovascular System - Transportation 1Document28 pagesCardiovascular System - Transportation 1Louise Mica Lee100% (1)
- Heart 2018 - Part IDocument57 pagesHeart 2018 - Part Iwww.hudevaa6No ratings yet
- Cardiovascular System - Lecture 3-2018-2019 PDFDocument27 pagesCardiovascular System - Lecture 3-2018-2019 PDFMary100% (1)
- Lecture 3 Cardiovascular System 1Document54 pagesLecture 3 Cardiovascular System 1hafiz patah100% (1)
- The Heart and CirculationDocument7 pagesThe Heart and CirculationsaframikdarhafisNo ratings yet
- Physiology of ExerciseDocument25 pagesPhysiology of ExerciseTedy Friyadi100% (1)
- Circulatory SystemDocument8 pagesCirculatory SystemDany MonteroNo ratings yet
- Technical DefinitionDocument3 pagesTechnical DefinitionErin BarnesNo ratings yet
- Cardiac Ana & DxticsDocument3 pagesCardiac Ana & Dxticsjames garciaNo ratings yet
- Circulation NotesDocument2 pagesCirculation NotesBhkti MittalNo ratings yet
- EKG Study Guide RevisedDocument29 pagesEKG Study Guide Revisedflashyboy506No ratings yet
- The Heart and Circulation: The Tissues and Structures of The Heart Make It An Efficient PumpDocument4 pagesThe Heart and Circulation: The Tissues and Structures of The Heart Make It An Efficient PumpMaya SwailemNo ratings yet
- Module Cardiovascular SystemDocument14 pagesModule Cardiovascular SystemVynz Morales CosepNo ratings yet
- SB0024 Transport in Animals and Plant (DFN)Document80 pagesSB0024 Transport in Animals and Plant (DFN)jmyphjmrdnNo ratings yet
- Lecture 5 (Heart)Document10 pagesLecture 5 (Heart)Άγγελος ΧαβέλαςNo ratings yet
- Physio Individual CardioDocument4 pagesPhysio Individual CardioAyunie ZulkeflyNo ratings yet
- Cardiovascular Structure and Function: OutlineDocument1 pageCardiovascular Structure and Function: OutlineMskola KarlovacNo ratings yet
- Cardiovascular System - Lecture IDocument4 pagesCardiovascular System - Lecture IpragantraNo ratings yet
- WEEK 1 MEDSURG AsynchDocument12 pagesWEEK 1 MEDSURG AsynchLeigh Angelika Dela CruzNo ratings yet
- Medical Surgical Nursing: Anatomy HeartDocument8 pagesMedical Surgical Nursing: Anatomy HeartRoyce Vincent TizonNo ratings yet
- A. MODUL PDP 8Document29 pagesA. MODUL PDP 8Suraya Eiman ZafiraNo ratings yet
- Salcedo ANPH111 The Cardiovascular System23Document46 pagesSalcedo ANPH111 The Cardiovascular System23ajline.esto23No ratings yet
- Common Cardiac Anomalies Seen Within The Cardiac Catheterization LabDocument23 pagesCommon Cardiac Anomalies Seen Within The Cardiac Catheterization Labapi-356406300No ratings yet
- Chapter 19 Heart Marie BDocument29 pagesChapter 19 Heart Marie BomarNo ratings yet
- CARDIOVASCULARDocument41 pagesCARDIOVASCULARNor Jeannah PolaoNo ratings yet
- ISL PJM Anatomi Fisiologi Minggu 11 - JantungDocument4 pagesISL PJM Anatomi Fisiologi Minggu 11 - Jantungcuksam27No ratings yet
- Cardiovascular System 3Document28 pagesCardiovascular System 3Kris Adrian MallillinNo ratings yet
- Cardiovascular System (Heart) : o o o o oDocument5 pagesCardiovascular System (Heart) : o o o o okayaldrNo ratings yet
- 2300 - Module 5 - Basic Cardiovascular PathophysiologyDocument14 pages2300 - Module 5 - Basic Cardiovascular Pathophysiologymegan.abbinkNo ratings yet
- Circulation and Cardiovascular SystemDocument12 pagesCirculation and Cardiovascular SystemSatria MandalaNo ratings yet
- Ekg Ecg Interpretation by DR Jason Lowe PDF Bb3 DR NotesDocument79 pagesEkg Ecg Interpretation by DR Jason Lowe PDF Bb3 DR NotesGuru RewriNo ratings yet
- PALMA, LYCA D. - CARDIOVASCULAR SYSTEM (Heart and Blood Vessels)Document6 pagesPALMA, LYCA D. - CARDIOVASCULAR SYSTEM (Heart and Blood Vessels)G-Palma, Lyca D.No ratings yet
- NCM Responses To Altered Oxygenation Cardiac FunctionDocument14 pagesNCM Responses To Altered Oxygenation Cardiac FunctionJeson Vien GuerraNo ratings yet
- Week 9 CVS WorkbookDocument24 pagesWeek 9 CVS Workbooksupriyakunwar2019No ratings yet
- Anatomy Central Nervous System - AapDocument6 pagesAnatomy Central Nervous System - AapLinsha BerylNo ratings yet
- NCMMSN Notes - Sacramento, Karl SebastianDocument96 pagesNCMMSN Notes - Sacramento, Karl SebastianRHEA MAY CAPORNo ratings yet
- Chapter 5 Care of The Clients With Cardiovascular DisordersDocument226 pagesChapter 5 Care of The Clients With Cardiovascular DisordersDon Felicisimo EbronNo ratings yet
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisFrom EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisRating: 5 out of 5 stars5/5 (1)
- Emerg 6 E5 PDFDocument6 pagesEmerg 6 E5 PDFNovely MerlynNo ratings yet
- Daftar PustakaDocument5 pagesDaftar PustakaNovely MerlynNo ratings yet
- A New Coumarin Derivative, 4-Acetatecoumarin, With Antifungal Activity and Association Study Against SPPDocument7 pagesA New Coumarin Derivative, 4-Acetatecoumarin, With Antifungal Activity and Association Study Against SPPNovely MerlynNo ratings yet
- Antifungal Activity of CoumarinsDocument8 pagesAntifungal Activity of CoumarinsNovely MerlynNo ratings yet
- Usp Uniformity of Dosage Units PDFDocument3 pagesUsp Uniformity of Dosage Units PDFMilonhgNo ratings yet
- 1 INTRODUÇÃO - Pt.enDocument11 pages1 INTRODUÇÃO - Pt.enSozinho JoséNo ratings yet
- Human SexualityDocument11 pagesHuman Sexualitylanilyn aquinoNo ratings yet
- Session 5 Presentation Cleaning DisinfectionDocument22 pagesSession 5 Presentation Cleaning DisinfectionPrincess Anne ChavezNo ratings yet
- Essay About Your CommunityDocument6 pagesEssay About Your Communitynhbtoxwhd100% (2)
- NCRP 160 PDFDocument81 pagesNCRP 160 PDFmarkNo ratings yet
- Prot SAP 000 PDFDocument20 pagesProt SAP 000 PDFGrozny GroznyNo ratings yet
- Customized NQAS Checklist For Non FRU CHC of OdishaDocument130 pagesCustomized NQAS Checklist For Non FRU CHC of OdishaqaNo ratings yet
- EhrDocument4 pagesEhrapi-608465780No ratings yet
- Addison's Disease: Dexter DawsonDocument7 pagesAddison's Disease: Dexter DawsonDexter DawsonNo ratings yet
- Pizeta Pharma Corporate Profile 2022Document73 pagesPizeta Pharma Corporate Profile 2022Faruk HossainNo ratings yet
- Principle of ImmunologyDocument89 pagesPrinciple of ImmunologyAslen Postanes BañosNo ratings yet
- Mhpss and Remote Psychological First Aid: During The COVID-19 OutbreakDocument18 pagesMhpss and Remote Psychological First Aid: During The COVID-19 OutbreakARLENE MARASIGANNo ratings yet
- Proposal FiadetaDocument4 pagesProposal Fiadetajose suni100% (1)
- Dental WorkforceDocument18 pagesDental Workforcesobiaarshad2004No ratings yet
- SIMULASI+UAS+D3+KEP+2021 - Hikmah FitriaDocument6 pagesSIMULASI+UAS+D3+KEP+2021 - Hikmah FitriaHikmah FitriaNo ratings yet
- Roles and Responsibilities of Geriatric Nurse in CommunityDocument4 pagesRoles and Responsibilities of Geriatric Nurse in CommunityAKHILA PKNo ratings yet
- Siaga US Bahasa Inggris XII SMADocument9 pagesSiaga US Bahasa Inggris XII SMADayinta GayuhNo ratings yet
- Psychosis: Compton 2020 Jcompton@health - Ucsd.eduDocument33 pagesPsychosis: Compton 2020 Jcompton@health - Ucsd.eduJason ComptonNo ratings yet
- Rhode Island Kids Count: Disparities Maternal Infant ChildDocument16 pagesRhode Island Kids Count: Disparities Maternal Infant ChildNBC 10 WJARNo ratings yet
- Herbal Infused Oils & Salves 2Document8 pagesHerbal Infused Oils & Salves 2Chelsea McGowanNo ratings yet
- Echocardiography English GifDocument77 pagesEchocardiography English GifAlexandra StancuNo ratings yet
- Inpatient Pocket Card SetDocument10 pagesInpatient Pocket Card SetMuhammad Ahmad bin makruf syammakuNo ratings yet
- Nursing Care Plan Sample 5Document13 pagesNursing Care Plan Sample 5GEN ERIGBUAGASNo ratings yet
- Healthcare Impact of Covid-19 Epidemic in IndiaDocument2 pagesHealthcare Impact of Covid-19 Epidemic in IndiaAnupam GuptaNo ratings yet
- Drug StudyDocument3 pagesDrug StudyPsalms Aubrey Domingo AcostaNo ratings yet
- Cancer IncorporatedDocument253 pagesCancer IncorporatedRebekah RuizNo ratings yet
- Formulasi Sediaan Sabun Cair Kombinasi Ekstrak Etanol DAUN KERSEN (Muntingia Calabura L.) DAN DAUN KEMANGI (OcymumDocument9 pagesFormulasi Sediaan Sabun Cair Kombinasi Ekstrak Etanol DAUN KERSEN (Muntingia Calabura L.) DAN DAUN KEMANGI (Ocymumちかお 千春No ratings yet
- 1 - NCD in MalaysiaDocument17 pages1 - NCD in Malaysiaedkktm pkdmNo ratings yet