Professional Documents
Culture Documents
Long-Term (5-Year) Effects of A Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance
Long-Term (5-Year) Effects of A Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance
Uploaded by
Miguel Martinez GamboaCopyright:
Available Formats
You might also like
- Devitt AA Et Al. J Diabetes Res Clin Metab. 2012 1 20Document9 pagesDevitt AA Et Al. J Diabetes Res Clin Metab. 2012 1 20Teresa100% (1)
- Kpop Body Challenge Round2 PDFDocument6 pagesKpop Body Challenge Round2 PDFAlessandraAbigailHuamanPalacios100% (1)
- A Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialDocument10 pagesA Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialvicenteNo ratings yet
- Dietary Strategies For Patients With TypDocument8 pagesDietary Strategies For Patients With TypMalal QuechuaNo ratings yet
- Obesity&ExerciseDocument12 pagesObesity&ExerciseJacob LuttrellNo ratings yet
- Effect of A Low-Glycaemic Index - Low-Fat - High Protein Diet On The Atherogenic Metabolic Risk Profile of Abdominally Obese MenDocument12 pagesEffect of A Low-Glycaemic Index - Low-Fat - High Protein Diet On The Atherogenic Metabolic Risk Profile of Abdominally Obese MenAmida OaxacaNo ratings yet
- 2022 - JCEM - Metabolic Efficacy of Time-Restricted Eating in AdultsDocument14 pages2022 - JCEM - Metabolic Efficacy of Time-Restricted Eating in AdultsLuiz Fernando Fonseca VieiraNo ratings yet
- Diabetes MellitusDocument8 pagesDiabetes Mellitusi_anitaNo ratings yet
- Fat Vs Carb RestrictedDocument4 pagesFat Vs Carb RestrictedGiolla HijabNo ratings yet
- Am J Clin Nutr 2016 Valsesia Ajcn.116.137646Document10 pagesAm J Clin Nutr 2016 Valsesia Ajcn.116.137646kasabeNo ratings yet
- ArticleDocument9 pagesArticlernvisNo ratings yet
- Esfahani Et al-2011-IUBMB Life PDFDocument7 pagesEsfahani Et al-2011-IUBMB Life PDFLisiane PerinNo ratings yet
- Calorie Restriction With or Without Exercise On Insulin Sensitivity Beta Cell Functions Ectopic LipidDocument8 pagesCalorie Restriction With or Without Exercise On Insulin Sensitivity Beta Cell Functions Ectopic Lipidadibahfauzi85No ratings yet
- Moderate CarbohydrateDocument9 pagesModerate CarbohydrateAndrea TorrealdayNo ratings yet
- Randomized Controlled Trial of The Medifast 5 & 1 Plan For Weight LossDocument8 pagesRandomized Controlled Trial of The Medifast 5 & 1 Plan For Weight Losszainab asalNo ratings yet
- 1743 7075 7 17 PDFDocument10 pages1743 7075 7 17 PDFmarquelia.jardonNo ratings yet
- The Effect of High-Protein, Low-Carbohydrate Diets in The Treatment of Type 2 Diabetes: A 12 Month Randomised Controlled TrialDocument10 pagesThe Effect of High-Protein, Low-Carbohydrate Diets in The Treatment of Type 2 Diabetes: A 12 Month Randomised Controlled TrialFirda Rizky KhoerunnissaNo ratings yet
- dc14-0018 FullDocument8 pagesdc14-0018 FullLo RakNo ratings yet
- ASs 2 OriginalDocument13 pagesASs 2 OriginalArushi GuptaNo ratings yet
- Art 3A10.1186 2Fs40795 017 0152 4Document9 pagesArt 3A10.1186 2Fs40795 017 0152 4NurfadhilahNo ratings yet
- JCM 08 01645 PDFDocument11 pagesJCM 08 01645 PDFFranklin Howley-Dumit SerulleNo ratings yet
- Ntrs 513-Final PaperDocument8 pagesNtrs 513-Final Paperapi-203339953No ratings yet
- 1 s2.0 S0002916522004385 MainDocument11 pages1 s2.0 S0002916522004385 Maincarlos santamariaNo ratings yet
- Lundgreen Healthy Weight Loss Maintenance With Exercise 12Document12 pagesLundgreen Healthy Weight Loss Maintenance With Exercise 12Ricardo Parra ArangoNo ratings yet
- Effect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesDocument8 pagesEffect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesFajar AgNo ratings yet
- May Focus DeedDocument5 pagesMay Focus DeedEgy SunandaNo ratings yet
- Diet and Diabetes: Australian Family Physician June 2015Document6 pagesDiet and Diabetes: Australian Family Physician June 2015a3llamNo ratings yet
- 1 s2.0 S0026049511003404 MainDocument8 pages1 s2.0 S0026049511003404 MainFrankis De Jesus Vanegas RomeroNo ratings yet
- Wiliam Yancy PDFDocument7 pagesWiliam Yancy PDFDeaz Fazzaura PutriNo ratings yet
- Final 4Document11 pagesFinal 4api-722911357No ratings yet
- Meta AnalysisDocument7 pagesMeta AnalysisAliyahRajutButikNo ratings yet
- Ketogenic DietsDocument23 pagesKetogenic DietsNorma Edith López DíazGuerreroNo ratings yet
- Comparison of High-Fat and High-Protein Diets With A High-Carbohydrate Diet in Insulin-Resistant Obese WomenDocument9 pagesComparison of High-Fat and High-Protein Diets With A High-Carbohydrate Diet in Insulin-Resistant Obese WomenDanielle AliceNo ratings yet
- Kheniser, K Et Al (2021) Long-Term Weight Loss Strategies For ObesityDocument13 pagesKheniser, K Et Al (2021) Long-Term Weight Loss Strategies For Obesityasdrubal5martinezNo ratings yet
- Effects of A Ketogenic Diet On Muscle Fatigue in Healthy, Young, Normal-Weight Women A Randomized Controlled Feeding TrialDocument15 pagesEffects of A Ketogenic Diet On Muscle Fatigue in Healthy, Young, Normal-Weight Women A Randomized Controlled Feeding TrialRubinhoNo ratings yet
- Dietary Protein Effect On Body CompositionDocument8 pagesDietary Protein Effect On Body CompositionAllisa RufaedahNo ratings yet
- Example 6Document4 pagesExample 6Tutor BlairNo ratings yet
- Dietary Fiber Intake and Glycemic Control: Coronary Artery Calcification in Type 1 Diabetes (CACTI) StudyDocument8 pagesDietary Fiber Intake and Glycemic Control: Coronary Artery Calcification in Type 1 Diabetes (CACTI) StudyLeonardo AzevedoNo ratings yet
- Jurnal Tugas 3Document7 pagesJurnal Tugas 3Yuan Zhi YiNo ratings yet
- Effects of A Meal Replacement On Body CompositionDocument10 pagesEffects of A Meal Replacement On Body CompositionGiffariNo ratings yet
- 2014 - Johansson - Neovius - Hemmingsson - Effects of Anti Obesity Drugs Diet and Exercise On Weight LossDocument10 pages2014 - Johansson - Neovius - Hemmingsson - Effects of Anti Obesity Drugs Diet and Exercise On Weight LossPatricioNo ratings yet
- Asemi 2015Document7 pagesAsemi 2015ahmad azhar marzuqiNo ratings yet
- Scientific Evidence of Diets For Weight Loss Different Macronutrient... (BITAN ČLANAK)Document11 pagesScientific Evidence of Diets For Weight Loss Different Macronutrient... (BITAN ČLANAK)mirkoNo ratings yet
- Nejmoa2032183 - STEP 1Document14 pagesNejmoa2032183 - STEP 1นันทสิทธิ์ ศิริวิชญ์ไมตรีNo ratings yet
- Ajcn 9530614Document12 pagesAjcn 9530614Mateo TamayoNo ratings yet
- Human Nutrition and MetabolismDocument7 pagesHuman Nutrition and MetabolismMisyani MisyaniNo ratings yet
- Nuevas Terapias para La Obesidad - Euro Soc Cardiol 2023Document18 pagesNuevas Terapias para La Obesidad - Euro Soc Cardiol 2023endobariatryNo ratings yet
- Restricao Diaria Ou Intermitente PDFDocument9 pagesRestricao Diaria Ou Intermitente PDFAna Carolina Basso MorenoNo ratings yet
- Research Open Access: Antonio Paoli, Lorenzo Cenci and Keith A GrimaldiDocument8 pagesResearch Open Access: Antonio Paoli, Lorenzo Cenci and Keith A Grimaldipainah sumodiharjoNo ratings yet
- Tan, 2022Document8 pagesTan, 2022Mirilláiny AnacletoNo ratings yet
- PDF Philippine-CONSENSUS-STATEMENT-FINAL-BJMeditsDocument21 pagesPDF Philippine-CONSENSUS-STATEMENT-FINAL-BJMeditsElly JoyNo ratings yet
- ZVJZ Volume 49 Issue 1 Pages 56-66Document11 pagesZVJZ Volume 49 Issue 1 Pages 56-66Arbaz PatelNo ratings yet
- A Low-Fat Vegan Diet and A Conventional Diabetes Diet in The Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-wk Clinical TrialDocument9 pagesA Low-Fat Vegan Diet and A Conventional Diabetes Diet in The Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-wk Clinical TrialSheldon SilvaNo ratings yet
- Semaglutide in Obesity NEJM 2021 02Document13 pagesSemaglutide in Obesity NEJM 2021 02Eashaa Kumar100% (1)
- Differential Gene Expression in Adipose Tissue From Obese Human Subjects During Weight Loss and Weight MaintenanceDocument12 pagesDifferential Gene Expression in Adipose Tissue From Obese Human Subjects During Weight Loss and Weight Maintenancesergiuosan96No ratings yet
- Obesity Update AACE 2019 M AlvaradoDocument40 pagesObesity Update AACE 2019 M AlvaradonutoswaldoNo ratings yet
- Colberg 2009 2511457365Document8 pagesColberg 2009 2511457365fedelarru9No ratings yet
- Intermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese WomenDocument9 pagesIntermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese Womenpriya1832No ratings yet
- Long-Term Effects of A Ketogenic Diet in Obese PatientsDocument10 pagesLong-Term Effects of A Ketogenic Diet in Obese Patientsrobertofca2266No ratings yet
- 10 FullDocument9 pages10 Fullraksneck23No ratings yet
- Bmi Grade10 Jan.Document34 pagesBmi Grade10 Jan.Berith Grace Magcalas-GallardoNo ratings yet
- (Ivy Academia) Obesity PresentationDocument21 pages(Ivy Academia) Obesity PresentationWendell SenerpidaNo ratings yet
- BMI For AgeDocument2 pagesBMI For AgeNeil AtanacioNo ratings yet
- Final Physical Medical-Dental Examination ReportDocument1 pageFinal Physical Medical-Dental Examination ReportmillerNo ratings yet
- Meena Photo EssayDocument17 pagesMeena Photo Essayapi-533348723No ratings yet
- A Fast Way To Loss Weight 2021-Weight Loss Method - Effective Weight LossDocument2 pagesA Fast Way To Loss Weight 2021-Weight Loss Method - Effective Weight LossShahil NewarNo ratings yet
- Nutritional Status SF8 by Teacher TechDocument8 pagesNutritional Status SF8 by Teacher TechJONATHAN GARGANERANo ratings yet
- GUMAMELA Nutritional Status Baseline 2018 2019Document1 pageGUMAMELA Nutritional Status Baseline 2018 2019Sheryll PortuguesNo ratings yet
- Obesity and Physical Activity: John M. Jakicic,, Kelliann K. DavisDocument12 pagesObesity and Physical Activity: John M. Jakicic,, Kelliann K. Davispedro juanNo ratings yet
- Buce DebeljDocument2 pagesBuce DebeljSunčica DronjakNo ratings yet
- Deped Memo No. 165, S 2010: WastedDocument6 pagesDeped Memo No. 165, S 2010: WastedJayne InoferioNo ratings yet
- Nutritional Status Report EndlineDocument3 pagesNutritional Status Report EndlineOliva Cabrales Cabornay100% (2)
- Protap PenakibDocument1 pageProtap Penakibsiti marfu'atin100% (1)
- Body Mass Index Calculator: Your BMIDocument7 pagesBody Mass Index Calculator: Your BMIConstantin CosoiuNo ratings yet
- BMI-NS Grade Six Rizal 2014Document18 pagesBMI-NS Grade Six Rizal 2014Dhan BunsoyNo ratings yet
- Unit 9: Global Epidemic: Causes of ObesityDocument3 pagesUnit 9: Global Epidemic: Causes of ObesityNguyen Hoai ThuongNo ratings yet
- Activ 3 BMI DeterminationDocument4 pagesActiv 3 BMI DeterminationLovelyNo ratings yet
- Physical Fitness Test FormDocument3 pagesPhysical Fitness Test FormAnthony Gerarld TalainNo ratings yet
- Energy Balance PPT 1114he2Document10 pagesEnergy Balance PPT 1114he2Inthira SanmugamNo ratings yet
- Nutritional Status TemplateDocument1 pageNutritional Status TemplateShangkiee Amora-TamborNo ratings yet
- Consolidated BmiDocument2 pagesConsolidated BmiSARAH JEAN CABUGNASONNo ratings yet
- The Weight Debate With QuestionsDocument3 pagesThe Weight Debate With QuestionsAmna AlshehhiNo ratings yet
- FormulasDocument1 pageFormulasmgilmerNo ratings yet
- SF8 Grade 1 PreDocument5 pagesSF8 Grade 1 PreIrishNo ratings yet
- Metabolic Syndrome - Symptoms, Diagnosis, and CausesDocument7 pagesMetabolic Syndrome - Symptoms, Diagnosis, and CausesdrmuratNo ratings yet
- BibliographyDocument4 pagesBibliographyDr-GauravPantNo ratings yet
- Nutritional Status SEC. ConsolDocument1 pageNutritional Status SEC. ConsolRhea FerrerNo ratings yet
- Growth Scale (0-23 Mos Boys and Girls)Document2 pagesGrowth Scale (0-23 Mos Boys and Girls)Lester Paul Sivila100% (1)
- Script Forum - Impact of Obesity To ChildrenDocument6 pagesScript Forum - Impact of Obesity To ChildrenHaziq ThaqifNo ratings yet
Long-Term (5-Year) Effects of A Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance
Long-Term (5-Year) Effects of A Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance
Uploaded by
Miguel Martinez GamboaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Long-Term (5-Year) Effects of A Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance
Long-Term (5-Year) Effects of A Reduced-Fat Diet Intervention in Individuals With Glucose Intolerance
Uploaded by
Miguel Martinez GamboaCopyright:
Available Formats
Clinical Care/Education/Nutrition
O R I G I N A L A R T I C L E S
Long-Term (5-Year) Effects of a Reduced-
Fat Diet Intervention in Individuals With
Glucose Intolerance
BOYD A. SWINBURN, MD, FRACP1 has minor effects on suppressing appetite
PATRICIA A. METCALF, PHD1 and stimulating fat oxidation, and it is
SARAH J. LEY, MSC1 readily stored by the body as fat (9). A
high-fat diet results in passive overcon-
sumption of total energy (10), and simple
reduction of dietary fat alone has been
shown to cause weight loss (11,12). How-
OBJECTIVE — To determine whether reducing dietary fat would reduce body weight and ever, there has been much debate about
improve long-term glycemia in people with glucose intolerance. the long-term impact of reducing total fat
RESEARCH DESIGN AND METHODS — A 5-year follow-up of a 1-year randomized
in the diet. Some suggest that it should be
controlled trial of a reduced-fat ad libitum diet versus a usual diet. Participants with glucose a central strategy; others believe that the
intolerance (2-h blood glucose 7.0 –11.0 mmol/l) were recruited from a Workforce Diabetes effect of reducing total fat is weak and that
Survey. The group that was randomized to a reduced-fat diet participated in monthly small- a diet high in monounsaturated fatty acid
group education sessions on reduced-fat eating for 1 year. Body weight and glucose tolerance should be recommended (13,14).
were measured in 136 participants at baseline, 6 months, and 1 year (end of intervention), with We previously reported a 1-year ran-
follow-up at 2 years (n ⫽ 104), 3 years (n ⫽ 99), and 5 years (n ⫽ 103). domized controlled trial of a reduced-
dietary-fat intervention (15). The reduced-
RESULTS — Compared with the control group, weight decreased in the reduced-fat– diet fat-diet group significantly decreased its
group (P ⬍ 0.0001); the greatest difference was noted at 1 year (–3.3 kg), diminished at mean daily fat intake and total energy intake
subsequent follow-up (⫺3.2 kg at 2 years and ⫺1.6 kg at 3 years), and was no longer present by
5 years (1.1 kg). Glucose tolerance also improved in patients on the reduced-fat diet; a lower
compared with the control group without
proportion had type 2 diabetes or impaired glucose tolerance at 1 year (47 vs. 67%, P ⬍ 0.05), affecting micronutrient intake. We now re-
but in subsequent years, there were no differences between groups. However, the more compli- port on the 5-year follow-up of that study to
ant 50% of the intervention group maintained lower fasting and 2-h glucose at 5 years (P ⫽ 0.041 examine the long-term impact of the re-
and P ⫽ 0.026, respectively) compared with control subjects. duced-fat-diet program on body weight,
glucose tolerance, and conversion to type 2
CONCLUSIONS — The natural history for people at high risk of developing type 2 diabetes diabetes.
is weight gain and deterioration in glucose tolerance. This process may be ameliorated through
adherence to a reduced fat intake. RESEARCH DESIGN AND
METHODS
Diabetes Care 24:619 – 624, 2001
Participants were selected from a previous
Workforce Diabetes Survey (16) in which
oral glucose tolerance tests (OGTT) were
I
mpaired glucose tolerance (IGT) is a and/or saturated fat also seems to have an performed in 4,833 workers, aged 40
major risk factor in the development of important effect on the risk of developing years and older, from 41 work sites
type 2 diabetes (1) with conversion type 2 diabetes, independent of weight around Auckland between 1988 and
rates ranging from 3.6 – 8.7% per year (2). gain (4,5). Combined diet and physical 1990. Of those participants surveyed,
Any measures that can reduce the pro- activity interventions have been found to 162 (2.8%) were classified as having IGT
gression to diabetes in such high-risk be successful in reducing the rate of con- by 1985 World Health Organization
populations will have major health bene- version from IGT to type 2 diabetes (6 – criteria (2-h blood glucose 7.8 –11.0
fits. Weight gain is a critical factor in this 8). mmol/l) (17), and another 114 workers
progression, increasing the risk ⬃2- to Decreasing fat intake is a central part (2%) had high normal blood glucose con-
12-fold, depending on the amount of of the dietary approach to weight reduc- centrations (7.0 –7.8 mmol/l). In this
weight gained (3). Long-term intake of fat tion. Because fat is very energy dense, it combined “glucose intolerant” group
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● (i.e., 2-h blood glucose 7.0 –11.0 mmol/l,
From the 1Department of Community Health, University of Auckland, Auckland, New Zealand.
n ⫽ 276), 237 participants could be con-
Address correspondence and reprint requests to Boyd A. Swinburn, MD, FRACP, Professor, School of tacted (⬃2 years after the original survey);
Health Sciences, Deakin University, 221 Burwood Hwy., Victoria 3125, Australia. E-mail: swinburn@deakin. 176 participants entered the intervention,
edu.au. and 136 (77%) completed the 1-year in-
Received for publication 25 April 2000 and accepted in revised form 30 November 2000. tervention period. Of these 136 partici-
Abbreviations: CD, control diet; IGT, impaired glucose tolerance; OGTT, oral glucose tolerance test; RF,
reduced fat. pants, we were able to reassess 104 (76%)
A table elsewhere in this issue shows conventional and Système International (SI) units and conversion at 2 years, 99 (73%) at 3 years, and 103
factors for many substances. (76%) at 5 years.
DIABETES CARE, VOLUME 24, NUMBER 4, APRIL 2001 619
Reduced-fat diet and glucose intolerance
Before randomization, participants Measurements not the case, because weight change over
underwent repeat OGTT for redefinition Height and weight were recorded with time is nonlinear.
of glucose tolerance status, which, in participants wearing lightweight clothing
many cases, had changed since the origi- and no shoes using a Seca 2000 scale with RESULTS
nal testing in the Workforce Diabetes Sur- attached stadiometer (Seca, Hamburg,
vey ⬃2 years prior. The participants were Germany). Participants in both groups Participants
then individually assigned by simple ran- completed a comprehensive 3-day food The baseline characteristics of partici-
domization using an unmarked envelope diary before randomization and after 1 pants who completed the 1-year interven-
system to an intervention group, the year. Foods were measured using stan- tion are presented in Table 1. There were
members of which were asked to con- dard measuring cups and spoons and no significant differences between the
sume a reduced-fat (RF) but otherwise ad- weight-approximation diagrams. Diaries groups. The 40 participants who did not
libitum diet, or to a control-diet (CD) were analyzed for nutrients using Nutri- complete the 1-year intervention (4 died,
group, the members of which continued tionist III software (Version 6; N-Squared 1 became pregnant, 7 developed serious
with their usual diet. Six participants from Computing, Silverton, OR), to which the illnesses, 4 moved out of Auckland, and
one work site, all of whom were women nutrient values of ⬃600 New Zealand 24 dropped out of the study) were of sim-
from the Pacific Islands, were assigned to foods had been added. ilar age to those who did complete the
the RF group, because individual random- A standard 75-g OGTT was per- 1-year intervention but had a significantly
ization may have caused some contamina- formed at each review. Diabetes, IGT, and (P ⬍ 0.05) higher BMI (30.7 ⫾ 0.7 vs.
tion of the CD-group participants. All impaired fasting glycemia were defined 29.1 ⫾ 0.4 kg/m2) and included a higher
participants found to have diabetes on re- using the revised World Health Organiza- proportion of women (42 vs. 27%) and
testing were referred to their general practi- tion criteria and classification of diabetes individuals of Maori or Pacific descent (40
tioners for management but were still mellitus (18). Measurements were taken vs. 24%). The baseline characteristics of
randomized for the study. All participants at randomization and at 0.5, 1, 2, 3, and 5 the participants who were lost to 5-year
provided informed consent, and the study years. Insulin was not measured at years follow-up (n ⫽ 33) were not significantly
was approved by the Auckland Hospital Re- 2, 3, and 5. different from the rest of the participants,
search Ethics Committee. except that they were older (53.5 vs. 49.9
years, P ⫽ 0.029).
Statistical analyses There were no differences in sex or
Dietary intervention Mean (SE) values, adjusted for age, sex, glucose tolerance status between those
Participants in the RF group entered a ethnicity, and baseline measurement, participants in the RF group classified as
1-year structured program aimed solely at were calculated using SAS PROC MIXED compliers or noncompliers, but Europe-
reducing the total amount of fat in their (SAS Institute, Cary, NC) (19). The re- ans were more likely to be compliers (66
usual diet. The program involved educa- peated-measures model included time vs. 18%, P ⬍ 0.001). Interestingly, at the
tion on reducing dietary fat intake, per- since baseline for each of the time points, end of year 1, there was no difference in
sonal goal-setting, and self-monitoring treatment group, and the time by treat- fat intake between compliers and non-
(food diaries) through a series of monthly ment interaction and used an unstruc- compliers.
small-group sessions as previously de- tured variance-covariance matrix to model
scribed (15). Briefly, the education ses- the correlations between time points. The
sions detailed the reasons for reducing Satherthwaite option was used to approx- Lifestyle changes
dietary fat, showed participants how to imate the correct denominator degrees of The dietary changes over the intervention
identify high-fat foods (including reading freedom for the tests of fixed effects. A year are shown in Table 2. The total energy
labels), and identified a variety of strate- linear model was assumed from time 0 –5 intake and the absolute intake (gram/day)
gies for reducing fat intake. The food di- years. Analyses were performed using of fat decreased in the RF group, where-
aries counted dietary fat intake for 2 days random coefficients models, which allow as changes in the other macronutrients
each week on a rotating schedule of days the slopes and intercepts to vary ran- and fiber were not different between the
to capture weekdays and weekends. Par- domly for each participant. groups. As a percentage of total energy, fat
ticipants used a simple fat-counter book- Categorical variables were compared decreased, whereas carbohydrate and
let to estimate the fat content of foods. using the 2 test, and Student’s t test was protein increased in the RF group com-
Those in the CD group received only gen- used for continuous variables. All statisti- pared with the CD group.
eral dietary advice about healthy food cal analyses were performed using SAS At the end of year 1, 20% of the RF
choices upon entering the trial. (19). Participants who dropped out be- group reported an increase in recreational
Compliance with the program was as- fore the end of the 12-month intervention exercise over the previous year compared
sessed by attendance at the monthly period were not included in the analysis with 9% in the CD group (P ⫽ 0.002). At
meetings and completion of the diet dia- because if their last observation had been the end of year 2, 21% of the RF group
ries (compliance score ⫽ mean of the per- carried forward, the differences between reported that they were exercising as a
centage of meetings attended and the the two groups would have been artifi- means to lose weight compared with 12%
percentage of diaries filled). Those with cially maintained over the follow-up pe- of the control group (P ⫽ 0.087), but by
compliance scores above the median for riod. Carrying the last observation for- the end of year 3, these percentages had
the group were classified as compliers for ward assumes that assigning a no-change reversed (13 vs. 21%, P ⫽ 0.13). By the
the analysis. status is a conservative analysis, which is end of year 1, four participants in the RF
620 DIABETES CARE, VOLUME 24, NUMBER 4, APRIL 2001
Swinburn and Associates
Table 1—Baseline characteristics of participants who completed the 1-year intervention Fig. 1. There were no significant differ-
ences between the RF and CD groups at
RF group CD group baseline and 0.5 years, but the interven-
tion showed a significant effect on glucose
n 66 70 tolerance status (P ⫽ 0.015) at 1 year. A
Age (years) 52.5 ⫾ 0.8 52.0 ⫾ 0.8 smaller proportion of participants had
Sex (M:F) 45:21 56:14 type 2 diabetes or IGT in the RF group (47
Ethnicity compared with 67%). No intervention ef-
European 44 (66.7) 53 (75.7) fect was present at 2, 3, or 5 years.
Maori 7 (10.6) 5 (7.1)
Pacific Islander 13 (19.7) 9 (12.9) Effects with greater compliance
Other 2 (3.0) 3 (4.3) The RF group was subdivided in half
Anthropometry according to compliance (as described in
Weight (kg) 85.46 ⫾ 1.80 84.33 ⫾ 1.55 RESEARCH DESIGN AND METHODS). The compli-
BMI (kg/m2) 29.08 ⫾ 0.55 29.17 ⫾ 0.48 ers showed a significantly lower blood
Waist circumference (cm) 100.48 ⫾ 1.42 101.60 ⫾ 1.28 glucose level (after adjustment for age,
Waist to hip ratio 0.944 ⫾ 0.008 0.954 ⫾ 0.008 sex, and ethnicity) at fasting (P ⫽ 0.041)
Glucose tolerance test and 2 h (P ⫽ 0.024) at 5 years compared
Fasting glucose (mmol/l) 6.7 ⫾ 0.2 6.6 ⫾ 0.2 with the CD group (Fig. 2). In contrast,
2-h glucose (mmol/l) 7.5 ⫾ 0.3 7.9 ⫾ 0.3 noncompliers showed no significant
Fasting insulin (mIU/l) 16.0 ⫾ 1.1 15.8 ⫾ 0.9 changes versus the CD group. The com-
2-h insulin (mIU/l) 50.2 ⫾ 4.2 47.0 ⫾ 3.8 pliers showed a significantly lower
Glucose tolerance status weight in the first 3 years, but at 5 years,
Normal 24 (36.4) 23 (32.9) there were no significant differences be-
Impaired fasting glucose 11 (16.6) 15 (21.4) tween the groups (Fig. 2). Compliers also
Impaired glucose tolerance 10 (15.1) 9 (12.9) showed significantly lower fasting and
Diabetes 21 (31.8) 23 (32.9) 2-h insulin levels at 1 year (P ⫽ 0.023 and
Data are means ⫾ SEM or n (%) unless otherwise indicated. 0.018, respectively) compared with the
CD group (data not shown) but were not
group had quit smoking compared with riod, and this was sustained for 3 years. By tested subsequently.
two participants in the CD group. 5 years, however, the mean weight of the
RF group was not significantly different CONCLUSIONS — What are the
Changes in weight and glucose from that measured before the interven- long-term effects of promoting reductions
tolerance tion (1.1 kg) or from the CD group. in total dietary fat? That question is cur-
The mean changes in weight, BMI, and There was no overall effect of diet on rently under debate, and we have exam-
glucose tolerance at 0.5, 1, 2, 3, and 5 fasting glucose, but there was a signifi- ined the effects of a 1-year intervention to
years (Table 3) were adjusted for age, sex, cant effect on 2-h glucose over the period reduce dietary fat on body weight and
ethnicity, and baseline measurements. (P ⬍ 0.0001) (Table 3). There was a signif- glucose tolerance. Participants were not
The RF group lost weight and achieved a icantly lower 2-h insulin at 1 year. Changes expecting to lose weight during the inter-
lower BMI during the intervention pe- in glucose tolerance status are shown in vention, because they were told that the
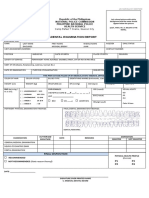
Table 2—Daily energy, macronutrient, and fiber intakes determined by 3-day diet diaries
RF group (n ⫽ 49) CD group (n ⫽ 61)
Baseline 1 year Change Baseline 1 year Change
Mean ⫾ SD Mean ⫾ SD Mean ⫾ SEM Mean ⫾ SD Mean ⫾ SD Mean ⫾ SEM P*
Energy (kcal) 2,195 (610) 1,832 (481) ⫺362 (92) 2,366 (693) 2,307 (856) ⫺59 (93) 0.016
Fat (g) 86.1 (32.6) 52.1 (24.5) ⫺34.0 (4.8) 96.5 (35.7) 90.0 (43.6) ⫺6.6 (4.5) ⬍0.0001
% Energy 34.6 (6.5) 25.9 (8.8) ⫺8.7 (1.3) 36.1 (6.6) 33.8 (7.2) ⫺2.3 (1.0) ⬍0.0001
Carbohydrate (g) 250 (74) 251 (90) 1.0 (14) 261 (80) 250 (73) ⫺11 (9) 0.49
% Energy 46.2 (8.3) 54.5 (11.7) 8.3 (1.5) 45.0 (9.1) 45.6 (10.1) 0.6 (1.2) ⬍0.0001
Protein (g) 91.3 (27.3) 83.6 (25.6) ⫺7.7 (3.7) 96.1 (31.1) 95.1 (45.3) ⫺1.0 (4.3) 0.25
% Energy 16.9 (3.3) 18.6 (4.1) 1.7 (0.6) 16.7 (4.1) 16.5 (3.8) ⫺0.2 (0.6) 0.025
Alcohol† (g) 14.6 (21.1) 10.0 (14.4) ⫺4.6 (20.5) 17.5 (29.2) 22.1 (34.0) 4.6 (25.8) 0.21
% Energy 4.4 (6.2) 3.5 (4.7) ⫺0.9 (0.8) 4.5 (6.7) 5.8 (7.9) 1.3 (0.7) 0.19
Fiber (g) 20.9 (8.1) 20.5 (10.1) ⫺0.4 (1.3) 19.4 (7.8) 18.4 (6.6) ⫺1.0 (1.2) 0.73
g/1,000 kcal 9.9 (3.9) 11.2 (4.8) 1.3 (0.6) 8.7 (3.7) 8.8 (3.2) 0.1 (0.5) 0.061
*Difference in changes between the groups; Student’s t test; †distribution not normal, Wilcoxon rank-sum test.
DIABETES CARE, VOLUME 24, NUMBER 4, APRIL 2001 621
Reduced-fat diet and glucose intolerance
Table 3—Mean changes in anthropometrical and biochemical measurements (SEM) from baseline over 5 years in the RF and CD groups
adjusted for baseline measurements
Time (years)
Intervention period
Overall effect
0.5 1.0 2.0 3.0 5.0 of diet (P)*
n (RF/CD) 66/70 66/70 47/57 48/51 51/52 —
Weight (kg)
RF ⫺2.97 ⫾ 0.54† ⫺3.32 ⫾ 0.68† ⫺3.15 ⫾ 0.78† ⫺1.60 ⫾ 0.78† 1.06 ⫾ 0.64 ⬍0.0001
CD ⫺0.08 ⫾ 0.43 0.59 ⫾ 1.61 1.06 ⫾ 0.46 2.13 ⫾ 0.70 1.26 ⫾ 0.68
BMI (kg/m2)
RF ⫺0.99 ⫾ 0.18† ⫺1.09 ⫾ 0.24† ⫺1.01 ⫾ 0.28‡ ⫺0.46 ⫾ 0.28‡ 0.72 ⫾ 0.28 ⬍0.0001
CD ⫺0.01 ⫾ 0.15 0.22 ⫾ 0.15 0.38 ⫾ 0.15 0.75 ⫾ 0.24 0.59 ⫾ 0.27
Fasting glucose (mmol/l)
RF 0.04 ⫾ 0.17 0.08 ⫾ 0.16 ⫺0.17 ⫾ 0.26 ⫺0.04 ⫾ 0.18 0.02 ⫾ 0.18 NS
CD 0.11 ⫾ 0.16 0.17 ⫾ 0.13 0.05 ⫾ 0.24 0.09 ⫾ 0.22 0.29 ⫾ 0.30
2-h glucose (mmol/l)
RF ⫺0.36 ⫾ 0.36 0.01 ⫾ 0.33 ⫺0.76 ⫾ 0.42 0.20 ⫾ 0.37 1.02 ⫾ 0.40 ⬍0.0001
CD 0.13 ⫾ 0.37 0.74 ⫾ 0.35 0.01 ⫾ 0.49 0.48 ⫾ 0.45 2.30 ⫾ 0.54
Fasting insulin (mIU/l)
RF ⫺3.71 ⫾ 1.58 ⫺4.87 ⫾ 1.09 — — — ⬍0.0001
CD ⫺4.31 ⫾ 0.86 ⫺3.80 ⫾ 0.83 — — —
2-h insulin (mIU/l)
RF ⫺12.01 ⫾ 6.16 ⫺14.94 ⫾ 4.20‡ — — — 0.0103
CD ⫺6.20 ⫾ 3.64 ⫺1.90 ⫾ 3.75 — — —
Significant difference between RF and CD groups at each time point. *Effect of diet assessed by the interaction term group time (i.e., does the time course of the
changes over the 5 years differ with time); †P ⬍ 0.01; ‡0.01 ⫽ P ⬍ 0.05.
study was testing the effect of fat intake on (6) and 6 years (7), suggesting that a the effectiveness of lifestyle modifications
blood glucose levels. In the medium term, higher level of compliance was reached (24). These studies, together with our
up to 3 years, significant weight loss oc- during that length of intervention. Sus- findings, suggest that to be successful, in-
curred that was not sustained at 5 years. tained therapeutic contact was consid- terventions should probably be multifac-
Glucose tolerance also improved initially ered an important factor in maintaining torial and longer in duration. Otherwise,
with the diet but was not significantly dif-
ferent at 5 years. However, the partici-
pants who were most compliant with the
program did show lower fasting and 2-h
blood glucose levels at 5 years.
The amount of weight loss in our
study (3.3 kg at 1 year) was similar to
other reduced-fat ad libitum intervention
trials (12,20,21), and also like most inter-
ventions for weight loss, weight was re-
gained in the long term (22). Greater
compliance to the intervention resulted in
greater weight loss and more lasting ef-
fects on glucose tolerance, consistent with
other studies showing that compliance
with the intervention, long-term mainte-
nance of low-fat eating patterns, and
weight loss were all strongly interrelated
(23). Similarly, more intensive, longer-
term interventions that combined exer-
cise with diet modification in individuals
with IGT showed significant health gains
of sustained weight reduction and im- Figure 1—Changes in glucose tolerance status over time in the RF and CD groups. A significant
provements in glucose tolerance over 5 difference is shown between the RF and CD participants at 1 year. *P ⬍ 0.015.
622 DIABETES CARE, VOLUME 24, NUMBER 4, APRIL 2001
Swinburn and Associates
the initial efforts and enthusiasm for
healthier lifestyles become eroded by the
external obesogenic environmental forces
(25). If, on the other hand, the lifestyles
can be maintained, they will probably re-
duce the amount of weight gain and the
risk of diabetes.
Our results may have implications for
other studies of diabetes prevention in
high-risk groups. The dietary interven-
tions in the large Diabetes Prevention Pro-
gram (26) will be sustained over the
5-year period of the trial, and the “dose” is
high in the intensive lifestyle group. Phys-
ical activity is also included, but no envi-
ronmental interventions are planned.
Interestingly, in our study, the partici-
pants randomized to the RF group also
seemed to increase their levels of physical
activity; therefore, promoting healthy be-
haviors through dietary changes may
have stimulated the participants to exer-
cise more.
Our study was limited by the number
of people, particularly of Maori and Pa-
cific Island ethnicity, who were either lost
to follow-up (n ⫽ 24, 17.6%) or who had
low compliance to the intervention. These
ethnic groups are at higher risk of devel-
oping diabetes than Europeans. The man-
ner of recruitment into the study may also
have limited participation. People who
learn from a work-site survey that their
blood glucose level is somewhat elevated
may not be as ready or willing to change
their lifestyle behaviors as people who al-
ready have known health problems such
as diabetes.
In conclusion, an intervention aimed
at reducing dietary fat alone improved
body weight and glucose tolerance over a
2- to 3-year period but was only sustained
in more compliant participants.
Acknowledgments — This study was sup-
ported by funding from the Auckland Medical
Research Foundation, the National Heart
Foundation of New Zealand, and the Lotteries
Medical Board. P.A.M. was supported by the
Health Research Council of New Zealand.
We thank Michael Wilson for assistance
with data collection and with the intervention.
Figure 2—Long-term changes in weight, fasting glucose, and 2-h blood glucose concentrations in References
the CD group (– – – –), the least compliant RF group (- - - -), and the most compliant RF group 1. Tuomilehto J, Knowler WC, Zimmet P:
(——–). Significant differences are shown between the most compliant RF and CD groups (*P ⬍ Primary prevention of non-insulin depen-
0.05, **P ⬍ 0.01) and between the least compliant RF and CD groups (aP ⬍ 0.05). dent diabetes. Diabetes Metab Rev 8:339 –
353, 1992
2. Edelstein SL, Knowler WC, Bain RP, An-
DIABETES CARE, VOLUME 24, NUMBER 4, APRIL 2001 623
Reduced-fat diet and glucose intolerance
dres R, Barrett-Connor EL, Dowse GK, ercise. Diabetologia 41:1010 –1016, 1998 sis and classification of diabetes mellitus:
Haffner SM, Pettitt DJ, Sorkin JD, Muller 9. Ravussin E, Tataranni PA: Dietary fat and provisional report of a WHO consulta-
DC, Collins VR, Hamman RF: Predictors human obesity. J Am Diet Assoc (Suppl. tion. Diabet Med 15:539 –553, 1998
of progression from impaired glucose in- 97):S42–S46, 1997 19. SAS Institute: SAS/STAT Software: Changes
tolerance to NIDDM: an analysis of six 10. Blundell JE, Macdiarmid JI: Fat as a risk and Enhancements Through Release 6.12.
prospective studies. Diabetes 46:701–710, factor for overconsumption: satiation, sa- Cary, NC: SAS Institute Inc, 1997, p. 1167
1997 tiety, and patterns of eating. J Am Diet As- 20. Singh RB, Rastogi SS, Verma R, Laxmi B,
3. Colditz GA, Willett WC, Rotnitzky A, soc (Suppl. 97):S63–S69, 1997 Singh R, Ghosh S, Niaz MA: Randomised
Manson JE: Weight gain as a risk factor for 11. Carmichael HE, Swinburn BA, Wilson controlled trial of cardioprotective diet in
clinical diabetes mellitus in women. Ann MR: Lower fat intake as a predictor of ini- patients with recent acute myocardial in-
Intern Med 122:481– 486, 1998 tial and sustained weight loss in obese farction: results of one year follow-up.
4. Feskens EJ, Virtanen SM, Rasanen L, Tuo- subjects consuming an otherwise ad libi- BMJ 304:1015–1019, 1992
milehto J, Stengard J, Pekkanen J, Nissi- tum diet. J Am Diet Assoc 98:35–39, 1998 21. Kasim SE, Martino S, Kim PN, Khilnani S,
nen A, Kromhout D: Dietary factors de- 12. Sheppard L, Kristal AR, Kushi LH: Weight Boomer A, Depper J, Reading BA, Heil-
termining diabetes and impaired glu- loss in women participating in a random- brun LK: Dietary and anthropometric de-
cose tolerance: a 20-year follow-up of the ized trial of low-fat diets. Am J Clin Nutr terminants of plasma lipoproteins during
Finnish and Dutch cohorts of the Seven 54:821– 828, 1991 a long-term low-fat diet in healthy wom-
Countries Study. Diabetes Care 18:1104 – 13. Bray GA, Popkin BM: Dietary fat intake
en. Am J Clin Nutr 57:146 –153, 1993
1112, 1995 does affect obesity. Am J Clin Nutr 68:
22. NIH Assessment Conference Panel: Meth-
5. Marshall JA, Hoag S, Shetterly S, Hamman 1157–1173, 1998
ods for voluntary weight loss and control.
RF: Dietary fat predicts conversion from 14. Willett WC: Dietary fat and obesity: an
Ann Intern Med 119:764 –770, 1993
impaired glucose tolerance to NIDDM: unconvincing relation. Am J Clin Nutr 68:
the San Luis Valley Diabetes Study. Dia- 1149 –1150, 1998 23. Urban N, White E, Anderson GV, Curry
betes Care 17:50 –56, 1994 15. Swinburn BA, Woollard GA, Chang EC, S, Kristal AR: Correlates of maintenance
6. Eriksson KF, Lindgarde F: Prevention of Wilson MR: Reduced-fat, ad libitum diets: of a low-fat diet among women in the
type 2 (non-insulin-dependent) diabetes effects on nutrient intake, micronutrient Women’s Health Trial. Prev Med 21:279 –
mellitus by diet and physical activity. Dia- intake, antioxidant vitamins. J Am Diet 291, 1992
betologia 34:891– 898, 1991 Assoc 99:1400 –1405, 1999 24. Perri MG, McAllister DA, Gange JJ, Jordan
7. Pan XR, Li GW, Hu YH, Wang JX, Yang 16. Scragg R, Baker J, Metcalf P, Dryson E: R, McAdoo G, Nezu AM: Effects of four
WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao Prevalence of diabetes mellitus and im- maintenance programs on the long-term
HB, Liu PA, Jiang XG, Jiang YY, Wang JP, paired glucose tolerance in a New Zealand management of obesity. J Consult Clin Psy-
Zheng H, Zhang H, Bennett PH, Howard multiracial workforce. N Z Med J 104:395– chol 56:529 –534, 1988
BV: Effects of diet and exercise in prevent- 397, 1991 25. Egger G, Swinburn B: An “ecological” ap-
ing NIDDM in people with impaired glu- 17. World Health Organization: Diabetes Mel- proach to the obesity pandemic. BMJ 315:
cose tolerance: the Da Qing IGT and dia- litus: Report of a WHO Study Group. Gene- 477– 480, 1997
betes study. Diabetes Care 20:537–544, 1997 va, World Health Org., 1985 (Tech. Rep. 26. Diabetes Prevention Program Research
8. Eriksson KF, Lindgarde F: No excess 12- Ser., no. 727) Group: The Diabetes Prevention Program:
year mortality in men with impaired glu- 18. Alberti KG, Zimmet PZ: Definition, diag- design and methods for a clinical trial in
cose tolerance who participated in the nosis and classification of diabetes melli- the prevention of type 2 diabetes. Diabetes
Malmo Preventive Trial with diet and ex- tus and its complications. Part 1: Diagno- Care 22:623– 634, 1999
624 DIABETES CARE, VOLUME 24, NUMBER 4, APRIL 2001
You might also like
- Devitt AA Et Al. J Diabetes Res Clin Metab. 2012 1 20Document9 pagesDevitt AA Et Al. J Diabetes Res Clin Metab. 2012 1 20Teresa100% (1)
- Kpop Body Challenge Round2 PDFDocument6 pagesKpop Body Challenge Round2 PDFAlessandraAbigailHuamanPalacios100% (1)
- A Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialDocument10 pagesA Very Low Carbohydrate, Low Saturated Fat Diet For Type 2 Diabetes Management: A Randomized TrialvicenteNo ratings yet
- Dietary Strategies For Patients With TypDocument8 pagesDietary Strategies For Patients With TypMalal QuechuaNo ratings yet
- Obesity&ExerciseDocument12 pagesObesity&ExerciseJacob LuttrellNo ratings yet
- Effect of A Low-Glycaemic Index - Low-Fat - High Protein Diet On The Atherogenic Metabolic Risk Profile of Abdominally Obese MenDocument12 pagesEffect of A Low-Glycaemic Index - Low-Fat - High Protein Diet On The Atherogenic Metabolic Risk Profile of Abdominally Obese MenAmida OaxacaNo ratings yet
- 2022 - JCEM - Metabolic Efficacy of Time-Restricted Eating in AdultsDocument14 pages2022 - JCEM - Metabolic Efficacy of Time-Restricted Eating in AdultsLuiz Fernando Fonseca VieiraNo ratings yet
- Diabetes MellitusDocument8 pagesDiabetes Mellitusi_anitaNo ratings yet
- Fat Vs Carb RestrictedDocument4 pagesFat Vs Carb RestrictedGiolla HijabNo ratings yet
- Am J Clin Nutr 2016 Valsesia Ajcn.116.137646Document10 pagesAm J Clin Nutr 2016 Valsesia Ajcn.116.137646kasabeNo ratings yet
- ArticleDocument9 pagesArticlernvisNo ratings yet
- Esfahani Et al-2011-IUBMB Life PDFDocument7 pagesEsfahani Et al-2011-IUBMB Life PDFLisiane PerinNo ratings yet
- Calorie Restriction With or Without Exercise On Insulin Sensitivity Beta Cell Functions Ectopic LipidDocument8 pagesCalorie Restriction With or Without Exercise On Insulin Sensitivity Beta Cell Functions Ectopic Lipidadibahfauzi85No ratings yet
- Moderate CarbohydrateDocument9 pagesModerate CarbohydrateAndrea TorrealdayNo ratings yet
- Randomized Controlled Trial of The Medifast 5 & 1 Plan For Weight LossDocument8 pagesRandomized Controlled Trial of The Medifast 5 & 1 Plan For Weight Losszainab asalNo ratings yet
- 1743 7075 7 17 PDFDocument10 pages1743 7075 7 17 PDFmarquelia.jardonNo ratings yet
- The Effect of High-Protein, Low-Carbohydrate Diets in The Treatment of Type 2 Diabetes: A 12 Month Randomised Controlled TrialDocument10 pagesThe Effect of High-Protein, Low-Carbohydrate Diets in The Treatment of Type 2 Diabetes: A 12 Month Randomised Controlled TrialFirda Rizky KhoerunnissaNo ratings yet
- dc14-0018 FullDocument8 pagesdc14-0018 FullLo RakNo ratings yet
- ASs 2 OriginalDocument13 pagesASs 2 OriginalArushi GuptaNo ratings yet
- Art 3A10.1186 2Fs40795 017 0152 4Document9 pagesArt 3A10.1186 2Fs40795 017 0152 4NurfadhilahNo ratings yet
- JCM 08 01645 PDFDocument11 pagesJCM 08 01645 PDFFranklin Howley-Dumit SerulleNo ratings yet
- Ntrs 513-Final PaperDocument8 pagesNtrs 513-Final Paperapi-203339953No ratings yet
- 1 s2.0 S0002916522004385 MainDocument11 pages1 s2.0 S0002916522004385 Maincarlos santamariaNo ratings yet
- Lundgreen Healthy Weight Loss Maintenance With Exercise 12Document12 pagesLundgreen Healthy Weight Loss Maintenance With Exercise 12Ricardo Parra ArangoNo ratings yet
- Effect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesDocument8 pagesEffect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesFajar AgNo ratings yet
- May Focus DeedDocument5 pagesMay Focus DeedEgy SunandaNo ratings yet
- Diet and Diabetes: Australian Family Physician June 2015Document6 pagesDiet and Diabetes: Australian Family Physician June 2015a3llamNo ratings yet
- 1 s2.0 S0026049511003404 MainDocument8 pages1 s2.0 S0026049511003404 MainFrankis De Jesus Vanegas RomeroNo ratings yet
- Wiliam Yancy PDFDocument7 pagesWiliam Yancy PDFDeaz Fazzaura PutriNo ratings yet
- Final 4Document11 pagesFinal 4api-722911357No ratings yet
- Meta AnalysisDocument7 pagesMeta AnalysisAliyahRajutButikNo ratings yet
- Ketogenic DietsDocument23 pagesKetogenic DietsNorma Edith López DíazGuerreroNo ratings yet
- Comparison of High-Fat and High-Protein Diets With A High-Carbohydrate Diet in Insulin-Resistant Obese WomenDocument9 pagesComparison of High-Fat and High-Protein Diets With A High-Carbohydrate Diet in Insulin-Resistant Obese WomenDanielle AliceNo ratings yet
- Kheniser, K Et Al (2021) Long-Term Weight Loss Strategies For ObesityDocument13 pagesKheniser, K Et Al (2021) Long-Term Weight Loss Strategies For Obesityasdrubal5martinezNo ratings yet
- Effects of A Ketogenic Diet On Muscle Fatigue in Healthy, Young, Normal-Weight Women A Randomized Controlled Feeding TrialDocument15 pagesEffects of A Ketogenic Diet On Muscle Fatigue in Healthy, Young, Normal-Weight Women A Randomized Controlled Feeding TrialRubinhoNo ratings yet
- Dietary Protein Effect On Body CompositionDocument8 pagesDietary Protein Effect On Body CompositionAllisa RufaedahNo ratings yet
- Example 6Document4 pagesExample 6Tutor BlairNo ratings yet
- Dietary Fiber Intake and Glycemic Control: Coronary Artery Calcification in Type 1 Diabetes (CACTI) StudyDocument8 pagesDietary Fiber Intake and Glycemic Control: Coronary Artery Calcification in Type 1 Diabetes (CACTI) StudyLeonardo AzevedoNo ratings yet
- Jurnal Tugas 3Document7 pagesJurnal Tugas 3Yuan Zhi YiNo ratings yet
- Effects of A Meal Replacement On Body CompositionDocument10 pagesEffects of A Meal Replacement On Body CompositionGiffariNo ratings yet
- 2014 - Johansson - Neovius - Hemmingsson - Effects of Anti Obesity Drugs Diet and Exercise On Weight LossDocument10 pages2014 - Johansson - Neovius - Hemmingsson - Effects of Anti Obesity Drugs Diet and Exercise On Weight LossPatricioNo ratings yet
- Asemi 2015Document7 pagesAsemi 2015ahmad azhar marzuqiNo ratings yet
- Scientific Evidence of Diets For Weight Loss Different Macronutrient... (BITAN ČLANAK)Document11 pagesScientific Evidence of Diets For Weight Loss Different Macronutrient... (BITAN ČLANAK)mirkoNo ratings yet
- Nejmoa2032183 - STEP 1Document14 pagesNejmoa2032183 - STEP 1นันทสิทธิ์ ศิริวิชญ์ไมตรีNo ratings yet
- Ajcn 9530614Document12 pagesAjcn 9530614Mateo TamayoNo ratings yet
- Human Nutrition and MetabolismDocument7 pagesHuman Nutrition and MetabolismMisyani MisyaniNo ratings yet
- Nuevas Terapias para La Obesidad - Euro Soc Cardiol 2023Document18 pagesNuevas Terapias para La Obesidad - Euro Soc Cardiol 2023endobariatryNo ratings yet
- Restricao Diaria Ou Intermitente PDFDocument9 pagesRestricao Diaria Ou Intermitente PDFAna Carolina Basso MorenoNo ratings yet
- Research Open Access: Antonio Paoli, Lorenzo Cenci and Keith A GrimaldiDocument8 pagesResearch Open Access: Antonio Paoli, Lorenzo Cenci and Keith A Grimaldipainah sumodiharjoNo ratings yet
- Tan, 2022Document8 pagesTan, 2022Mirilláiny AnacletoNo ratings yet
- PDF Philippine-CONSENSUS-STATEMENT-FINAL-BJMeditsDocument21 pagesPDF Philippine-CONSENSUS-STATEMENT-FINAL-BJMeditsElly JoyNo ratings yet
- ZVJZ Volume 49 Issue 1 Pages 56-66Document11 pagesZVJZ Volume 49 Issue 1 Pages 56-66Arbaz PatelNo ratings yet
- A Low-Fat Vegan Diet and A Conventional Diabetes Diet in The Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-wk Clinical TrialDocument9 pagesA Low-Fat Vegan Diet and A Conventional Diabetes Diet in The Treatment of Type 2 Diabetes: A Randomized, Controlled, 74-wk Clinical TrialSheldon SilvaNo ratings yet
- Semaglutide in Obesity NEJM 2021 02Document13 pagesSemaglutide in Obesity NEJM 2021 02Eashaa Kumar100% (1)
- Differential Gene Expression in Adipose Tissue From Obese Human Subjects During Weight Loss and Weight MaintenanceDocument12 pagesDifferential Gene Expression in Adipose Tissue From Obese Human Subjects During Weight Loss and Weight Maintenancesergiuosan96No ratings yet
- Obesity Update AACE 2019 M AlvaradoDocument40 pagesObesity Update AACE 2019 M AlvaradonutoswaldoNo ratings yet
- Colberg 2009 2511457365Document8 pagesColberg 2009 2511457365fedelarru9No ratings yet
- Intermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese WomenDocument9 pagesIntermittent Fasting Combined With Calorie Restriction Is Effective For Weight Loss and Cardio-Protection in Obese Womenpriya1832No ratings yet
- Long-Term Effects of A Ketogenic Diet in Obese PatientsDocument10 pagesLong-Term Effects of A Ketogenic Diet in Obese Patientsrobertofca2266No ratings yet
- 10 FullDocument9 pages10 Fullraksneck23No ratings yet
- Bmi Grade10 Jan.Document34 pagesBmi Grade10 Jan.Berith Grace Magcalas-GallardoNo ratings yet
- (Ivy Academia) Obesity PresentationDocument21 pages(Ivy Academia) Obesity PresentationWendell SenerpidaNo ratings yet
- BMI For AgeDocument2 pagesBMI For AgeNeil AtanacioNo ratings yet
- Final Physical Medical-Dental Examination ReportDocument1 pageFinal Physical Medical-Dental Examination ReportmillerNo ratings yet
- Meena Photo EssayDocument17 pagesMeena Photo Essayapi-533348723No ratings yet
- A Fast Way To Loss Weight 2021-Weight Loss Method - Effective Weight LossDocument2 pagesA Fast Way To Loss Weight 2021-Weight Loss Method - Effective Weight LossShahil NewarNo ratings yet
- Nutritional Status SF8 by Teacher TechDocument8 pagesNutritional Status SF8 by Teacher TechJONATHAN GARGANERANo ratings yet
- GUMAMELA Nutritional Status Baseline 2018 2019Document1 pageGUMAMELA Nutritional Status Baseline 2018 2019Sheryll PortuguesNo ratings yet
- Obesity and Physical Activity: John M. Jakicic,, Kelliann K. DavisDocument12 pagesObesity and Physical Activity: John M. Jakicic,, Kelliann K. Davispedro juanNo ratings yet
- Buce DebeljDocument2 pagesBuce DebeljSunčica DronjakNo ratings yet
- Deped Memo No. 165, S 2010: WastedDocument6 pagesDeped Memo No. 165, S 2010: WastedJayne InoferioNo ratings yet
- Nutritional Status Report EndlineDocument3 pagesNutritional Status Report EndlineOliva Cabrales Cabornay100% (2)
- Protap PenakibDocument1 pageProtap Penakibsiti marfu'atin100% (1)
- Body Mass Index Calculator: Your BMIDocument7 pagesBody Mass Index Calculator: Your BMIConstantin CosoiuNo ratings yet
- BMI-NS Grade Six Rizal 2014Document18 pagesBMI-NS Grade Six Rizal 2014Dhan BunsoyNo ratings yet
- Unit 9: Global Epidemic: Causes of ObesityDocument3 pagesUnit 9: Global Epidemic: Causes of ObesityNguyen Hoai ThuongNo ratings yet
- Activ 3 BMI DeterminationDocument4 pagesActiv 3 BMI DeterminationLovelyNo ratings yet
- Physical Fitness Test FormDocument3 pagesPhysical Fitness Test FormAnthony Gerarld TalainNo ratings yet
- Energy Balance PPT 1114he2Document10 pagesEnergy Balance PPT 1114he2Inthira SanmugamNo ratings yet
- Nutritional Status TemplateDocument1 pageNutritional Status TemplateShangkiee Amora-TamborNo ratings yet
- Consolidated BmiDocument2 pagesConsolidated BmiSARAH JEAN CABUGNASONNo ratings yet
- The Weight Debate With QuestionsDocument3 pagesThe Weight Debate With QuestionsAmna AlshehhiNo ratings yet
- FormulasDocument1 pageFormulasmgilmerNo ratings yet
- SF8 Grade 1 PreDocument5 pagesSF8 Grade 1 PreIrishNo ratings yet
- Metabolic Syndrome - Symptoms, Diagnosis, and CausesDocument7 pagesMetabolic Syndrome - Symptoms, Diagnosis, and CausesdrmuratNo ratings yet
- BibliographyDocument4 pagesBibliographyDr-GauravPantNo ratings yet
- Nutritional Status SEC. ConsolDocument1 pageNutritional Status SEC. ConsolRhea FerrerNo ratings yet
- Growth Scale (0-23 Mos Boys and Girls)Document2 pagesGrowth Scale (0-23 Mos Boys and Girls)Lester Paul Sivila100% (1)
- Script Forum - Impact of Obesity To ChildrenDocument6 pagesScript Forum - Impact of Obesity To ChildrenHaziq ThaqifNo ratings yet