Professional Documents
Culture Documents
Filarial Nematodes: Wuchereria Bancrofti
Filarial Nematodes: Wuchereria Bancrofti
Uploaded by
Megumi TadokoroCopyright:
Available Formats
You might also like
- Nursing Care Plan-AscitesDocument10 pagesNursing Care Plan-AscitesKayki Louise75% (4)
- Vaccine Debate by Jennifer MargulisDocument21 pagesVaccine Debate by Jennifer Margulisv2vreader100% (1)
- FILARIASISDocument57 pagesFILARIASISadekayo100% (6)
- Lesson 2 Extraintestinal NematodesDocument5 pagesLesson 2 Extraintestinal NematodesCDNo ratings yet
- BN Filarial WormDocument137 pagesBN Filarial WormCherenet TomaNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- Parasitology - Blood & Tissue - W Bancrofti B Malayi - PresentationDocument43 pagesParasitology - Blood & Tissue - W Bancrofti B Malayi - PresentationNicole ManogNo ratings yet
- Filarial NematodeDocument18 pagesFilarial NematodeHawre NajmaddinNo ratings yet
- FilariaDocument85 pagesFilariaRajkishor YadavNo ratings yet
- 3 - Loa Loa and Onchocerca VolvolusDocument29 pages3 - Loa Loa and Onchocerca VolvolusayaamrsharfNo ratings yet
- Helemnth ReportDocument15 pagesHelemnth ReportHawre NajmaddinNo ratings yet
- Filariasis Report (NCM 55 - B3)Document21 pagesFilariasis Report (NCM 55 - B3)Jette Charmae OlboNo ratings yet
- Blood and Tissue NematodesDocument60 pagesBlood and Tissue NematodesDanielle Pecson100% (1)
- PARA NematodesDocument23 pagesPARA Nematodes12 Newton - Cayetano, Arafe Nicole A.No ratings yet
- Wuchereria Bancrofti: Aby Elijah L. BernardinoDocument22 pagesWuchereria Bancrofti: Aby Elijah L. BernardinoAby Brr100% (1)
- Unit - 4-3 - Blood and Tissue NematodesDocument130 pagesUnit - 4-3 - Blood and Tissue NematodesDembalu NuguseNo ratings yet
- Wuchereria BancroftiDocument19 pagesWuchereria BancroftiMayuri VohraNo ratings yet
- Microbiology - ParasitologyDocument34 pagesMicrobiology - ParasitologySasi Dharan100% (1)
- Lect 2Document11 pagesLect 2Sara AliNo ratings yet
- Blood and Tissue NematodesDocument37 pagesBlood and Tissue NematodesjelenaNo ratings yet
- Blood and Tissue Nematods 2015Document109 pagesBlood and Tissue Nematods 2015sinte beyuNo ratings yet
- 4.3. Blood and Tissue NematodesDocument89 pages4.3. Blood and Tissue NematodesRediat GossayeNo ratings yet
- Filariasis: Tropmed Block Faculty Medicine USU 2016Document26 pagesFilariasis: Tropmed Block Faculty Medicine USU 2016Tiurma SibaraniNo ratings yet
- Blood and Tissue Nematodes WipDocument6 pagesBlood and Tissue Nematodes WipHemloNo ratings yet
- Parasitology NotesDocument5 pagesParasitology NotesAndriaNo ratings yet
- Filaria - A Comprehensive StudyDocument63 pagesFilaria - A Comprehensive StudyDayledaniel SorvetoNo ratings yet
- Medical Parasitology A Self Instructional Text PDFDriveDocument60 pagesMedical Parasitology A Self Instructional Text PDFDriveDenise Sta. AnaNo ratings yet
- Filariasis 2015Document56 pagesFilariasis 2015ChandraNo ratings yet
- Blood and Tissue Nematodes BiologiDocument47 pagesBlood and Tissue Nematodes BiologiAxzchiuu :vNo ratings yet
- Revision: Types of Life Cycle in Trematoda and CestodaDocument54 pagesRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekNo ratings yet
- Midterm ParasitologyDocument18 pagesMidterm ParasitologyAngelic AngelesNo ratings yet
- Lecture 10 - Phylum Nematoda and Nematode FilarioideaDocument12 pagesLecture 10 - Phylum Nematoda and Nematode FilarioideaBHEKUMUSA MASEKONo ratings yet
- Dracunculus Medinensis and Filarial WormsDocument19 pagesDracunculus Medinensis and Filarial WormsAnastasiaNo ratings yet
- Habronemose em Um CameloDocument4 pagesHabronemose em Um CameloTais SenaNo ratings yet
- Tissue Nematodes: 49.1 IntoductionDocument8 pagesTissue Nematodes: 49.1 IntoductionAileen LuzonNo ratings yet
- 11 Parasitology - Phasmids 4Document4 pages11 Parasitology - Phasmids 4maqmmNo ratings yet
- Clinical Parasitology-Module 9Document10 pagesClinical Parasitology-Module 9Geresh MagsinoNo ratings yet
- Micropara Lab Parasites Gr123456Document99 pagesMicropara Lab Parasites Gr123456Mary Jane TiangsonNo ratings yet
- Merge AbDocument17 pagesMerge AbEricsson CarabbacanNo ratings yet
- Wu C Here Ria Bancroft IDocument3 pagesWu C Here Ria Bancroft IMariamNo ratings yet
- Wuchereria BancroftiDocument13 pagesWuchereria Bancroftiumeshchandralenka09No ratings yet
- General Parasitology L6Document13 pagesGeneral Parasitology L6kayse abtidoonNo ratings yet
- W - BancroftiDocument19 pagesW - BancroftiALLISON PAMITTANNo ratings yet
- Blood and Tissue Roundworms (Filaria Worms)Document5 pagesBlood and Tissue Roundworms (Filaria Worms)nge257No ratings yet
- Parasitology Day 9 FilariaeDocument4 pagesParasitology Day 9 Filariaeniczdelosreyes8No ratings yet
- NematodaDocument30 pagesNematodaTagonna Di RaizelNo ratings yet
- Report PARA Lymphatic Filarial Nematodes Group 2 Adalid Asug AustriaDocument28 pagesReport PARA Lymphatic Filarial Nematodes Group 2 Adalid Asug AustriaDaniel AustriaNo ratings yet
- FilariasisDocument13 pagesFilariasissarguss14100% (3)
- FilariaDocument16 pagesFilariaJessa MayNo ratings yet
- Merged PDF 2021 11 16T12 - 01 - 01Document15 pagesMerged PDF 2021 11 16T12 - 01 - 01Ericsson CarabbacanNo ratings yet
- Loa Loa, OnchocercaDocument28 pagesLoa Loa, Onchocercabindu dhanapalNo ratings yet
- 9 BIO3243 Lecturer4 RiverblindnessDocument18 pages9 BIO3243 Lecturer4 RiverblindnessNGOGA NISINGIZWE NESTORNo ratings yet
- Wuchereria Bancrofti, Brugia Malayi, Brugia TimoriDocument3 pagesWuchereria Bancrofti, Brugia Malayi, Brugia TimoriJurel GaoatNo ratings yet
- Section 4: Vector Biology and ProfileDocument7 pagesSection 4: Vector Biology and ProfilenurotuljanahNo ratings yet
- Blood Borne Helminths - Wucherelia BancroftiDocument15 pagesBlood Borne Helminths - Wucherelia BancroftiCLEMENTNo ratings yet
- Phylum NematodaDocument11 pagesPhylum NematodaKristine Aranna ConcepcionNo ratings yet
- Worm Tissue Infestation: Umar Zein FK - UisuDocument77 pagesWorm Tissue Infestation: Umar Zein FK - UisuAmalul MukmininNo ratings yet
- Mansonella StreptocercaDocument14 pagesMansonella StreptocercaALLISON PAMITTANNo ratings yet
- Filariasis: Causes, Tests, and Treatment OptionsFrom EverandFilariasis: Causes, Tests, and Treatment OptionsRating: 5 out of 5 stars5/5 (2)
- Bontoc National High School - Senior High School Bontoc, Hindang, LeyteDocument32 pagesBontoc National High School - Senior High School Bontoc, Hindang, LeyteLianne SanchezNo ratings yet
- Identicifation of Hookworm Species in Stool by Harada Mori CultureDocument2 pagesIdenticifation of Hookworm Species in Stool by Harada Mori CultureMeenachi ChidambaramNo ratings yet
- Glycemic Targets 2022Document14 pagesGlycemic Targets 2022Tom BiusoNo ratings yet
- Nacker - 2011 - The-Impact-Of-Climate-Change-And-Other-Factors-On-Zoonotic-DiseasesDocument6 pagesNacker - 2011 - The-Impact-Of-Climate-Change-And-Other-Factors-On-Zoonotic-Diseasesrodrigocamiloo97No ratings yet
- Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) A ReviewDocument13 pagesPathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) A ReviewBryan Diaz LopezNo ratings yet
- Vaccination CertificateDocument1 pageVaccination Certificatemansoor 31 shaikhNo ratings yet
- Republic of The Philippines: NO YESDocument1 pageRepublic of The Philippines: NO YESInchic MirandaNo ratings yet
- Paediatric Symptoms SorterDocument3 pagesPaediatric Symptoms SorterPrasetya Ismail PermadiNo ratings yet
- Study Literatur: Pengkajian Luka Kaki DiabetesDocument15 pagesStudy Literatur: Pengkajian Luka Kaki DiabetesoctaviamayvikaNo ratings yet
- Pcap FinalDocument51 pagesPcap FinalThomas joshua QuiñonesNo ratings yet
- IPL Client History v1 - 7Document8 pagesIPL Client History v1 - 7Karen Dodd100% (1)
- Treatment and Prevention of Meningococcal InfectionDocument18 pagesTreatment and Prevention of Meningococcal InfectionMárcius SilvaNo ratings yet
- Must Have OkoubakaDocument2 pagesMust Have Okoubakaambertje12No ratings yet
- Core Epidemiologic FunctionsDocument6 pagesCore Epidemiologic FunctionsEvans MogakaNo ratings yet
- 15 Virusne Infekcije U Trudnoci - PrevedenoDocument7 pages15 Virusne Infekcije U Trudnoci - PrevedenoVelibor StankovićNo ratings yet
- 1 - MCCDDocument26 pages1 - MCCDAnupam SarkarNo ratings yet
- Fist Bump BillDocument2 pagesFist Bump BillJo InglesNo ratings yet
- Hasil Pemeriksaan Laboratorium: Laboratory Test ResultDocument1 pageHasil Pemeriksaan Laboratorium: Laboratory Test ResultDwi SaputroNo ratings yet
- Master Excel-2Document2 pagesMaster Excel-2Anonymous 7AKb61QyS4No ratings yet
- AnthraxDocument5 pagesAnthraxSaman SarKoNo ratings yet
- Understanding Blood Tests PDFDocument2 pagesUnderstanding Blood Tests PDFKishor SinghNo ratings yet
- 2 PPT Introduction To Epidemiology 18Document21 pages2 PPT Introduction To Epidemiology 18JMCDUFFIENo ratings yet
- DR ZauteaDocument56 pagesDR Zauteadvo aizawlNo ratings yet
- (A) Visitor's Health Declaration Form Dd. 10.05.2020 - GTVIDocument4 pages(A) Visitor's Health Declaration Form Dd. 10.05.2020 - GTVIamwin bizNo ratings yet
- Indovax CD Poultry DiseasesDocument78 pagesIndovax CD Poultry DiseasesSuraj_Subedi100% (3)
- Plant ProtectionDocument9 pagesPlant ProtectionPooja BhusalNo ratings yet
- Infection Control - Bron HenebryDocument28 pagesInfection Control - Bron HenebryGhazali Ahmad SiregarNo ratings yet
Filarial Nematodes: Wuchereria Bancrofti
Filarial Nematodes: Wuchereria Bancrofti
Uploaded by
Megumi TadokoroOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Filarial Nematodes: Wuchereria Bancrofti
Filarial Nematodes: Wuchereria Bancrofti
Uploaded by
Megumi TadokoroCopyright:
Available Formats
Wuchereria bancrofti
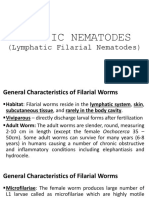
Filarial Nematodes
Common Name: ___________________________________________________________________________________
General Characteristics Associated Diseases: _____________________________________________________________________________
Filariae or filarial nematodes Mode of Transmission: __________________________________________________________________________
Adult worms live in tissue or the lymphatic system (thus rarely seen) Habitat: ____________________________________________________________________________________________
Microfilarie (larvae) that are usually detected in the blood; they may exhibit periodicity Infective stage: ___________________________________________________________________________________
Morphologic forms: ____________________ and ________________________
Diagnostic stage: _________________________________________________________________________________
Adults usually appear creamy white and assume a threadlike appearance
Two key characteristics of speciating the microfilariae: distribution of nuclei within
the tip of the tail and the presence/absence of a delicate transparent covering (sheath) W. bancrofti is responsible for 90% of lymphatic filariasis. Recently, 120 million
worldwide cases of lymphatic filariasis were estimated.
It largely affects areas across the broad equatorial belt (Africa, the Nile Delta, Turkey,
Life Cycle
India, the East Indies, Southeast Asia, Philippines, Oceanic Islands, and parts of South
Only one to four infective larvae, injected by an arthropod at the feeding site, are
America.)
required to initiate human infection
The mosquito vectors of W. bancrofti have a preference for human blood; humans are
Once inside the body, the larvae migrate to the tissues, where they complete their
apparently the only animals naturally infected with W. bancrofti.
development (a process that may take up to 1 year)
Adult worms may reside in the lymphatics, subcutaneous tissue, or internal body
Morphology
cavities.
Microfilariae
Fertilized adult female worms lay live microfilariae, which take up residence in the blood
Appear as minute snake-like organisms constantly moving among the RBCs
or dermis.
Measures 270-290µm and is enclosed in hyaline sheath
The microfilarie exit the body via a blood meal by the appropriate arthropod vector
The column of nuclei is arranged in two or three rows and is distinctly
Intermediate host: arthropod; where the larvae development into the infective stage
conspicuous
takes place
The cephalic or anterior end is blunt and round
The posterior tail end culminates in a point that is free of nuclei
Laboratory Diagnosis
Periodicity – a phenomenon whereby the parasites are present in the bloodstream
during a specific time period (thus helping a technologist in selecting the appropriate
time for specimen collection); it depends to the arthropods feeding schedule
o Nocturnal – occurring at night
o Diurnal – occurring during the day Adult worms
o Subperiodic – timing of occurrences not clear-cut Long hair-like transparent nematodes; creamy white in
Giemsa-stained blood smear / tissue scraping of an infected nodule – primary color
method of filarial diagnosis Filiform in shape, both ends are tapering
Knott’s technique – lysing cells followed by concentrating and examining the sample Male: 2.5-4cm in length and 0.1 mm thick; tail is curved
for microfilariae ventrally containing 2 spicules
Female: 8-10 cm in length and 0.2-0.3 mm thick
Review Notes in Clinical Parasitology by RMDM 26
Life Cycle Clinical Manifestation
Intermediate host: Culex, Aedes, and Anopheles spp. Asymptomatic
Definitive host: humans (live in the lymphatics where adults lay their microfilariae. Infections of this type are self-limiting because the adult worms eventually die and
These microfilariae live in the blood and lymphatics) there are no signs of microfilariae being present.
Once blood is collected, eosinophilia may be noted; physical examination reveals only
enlarged lymph nodes, particularly the inguinal region, the groin area.
Symptomatic Bancroftian Filariasis
General: fever, shaking chills, body aches, and swollen lymph nodes
Invasion of larvae: formation of granulomatous lesions, lymphangitis, and
lymphadenopathy
Lymphaginitis: episodes of acute inflammation of the lymphatic vessels
Lymphadenopathy: chronic lymph node swelling
Elephantiasis (swelling of the lower extremities) develop due to obstruction of the
lymphatics
Genitals and breast may also be involved
▪ Orchitis, funiculitis, and epididymitis
On the death of the adult worms, calcification or the formation of abscesses may
occur.
Laboratory Diagnosis and Treatment
Wuchereria bancrofti exhibits nocturnal periodicity, therefore, blood for the test should
be taken at night
Collect blood specimen from 8pm to 4am - Thick Smear (Giemsa or H&E)
Knott’s test
Serologic tests such as immunofluorescence be done by identifying positive antibody
1. During a blood meal, an infected mosquito introduces third-stage filarial larvae onto the titers
skin of the human host, where they penetrate into the bite wound. Others: PCR, Ultrasonography, and X-ray examinations
2. They develop in adults that commonly reside in the lymphatics. Gold standard: Antigen-detection (ELISA) to detect CFA (Circulating Filarial Antigen)
3. Adult worms produce microfilariae which are sheathed and have nocturnal periodicity. Alternative method: filtering heparinized blood through a special filter, known as
The microfilariae migrate into lymph and blood channels moving actively through lymph nuclepore filter, and then staining and examining the filter contents
and blood Drug of Choice: Diethylcarbamazine (DEC)
4. A mosquito ingests the microfilariae during a blood meal. Alternatice drugs: Ivermectin and Albendazole
5. After ingestion, the microfilariae lose their sheaths and some of them work their way
through the wall of the proventriculus and cardiac portion of the mosquito’s midgut and
Prevention and Control
reach the thoracic muscles.
Prevention involves mosquito control with insecticides
6. There, the microfilariae develop into first-stage larvae and subsequently into third-stage Use of protective clothing to prevent mosquito bites
infective larvae. Use of mosquito netting for sleeping and on windows of houses
7. The third-stage infective larvae migrate through the hemocoel to the mosquito’s Use of mosquito repellent cream
proboscis and can infect another human when the mosquito takes a blood meal. Clearing of bushes around residential houses and clearing of drainages to ensure there is
no breeding place for mosquitoes.
Review Notes in Clinical Parasitology by RMDM 27
Brugia malayi Life Cycle
Intermediate host: Aedes, Anopheles, or Mansonia
Common Name: ___________________________________________________________________________________ Definitive host: man, felines and monkeys
Associated Diseases: _____________________________________________________________________________ Since Anopheles mosquito also transmits W. bancrofti, coinfection is possible.
Mode of Transmission: __________________________________________________________________________ Similar life cycle with W. bancrofti
Habitat: ____________________________________________________________________________________________
Infective stage: ___________________________________________________________________________________
Diagnostic stage: _________________________________________________________________________________
Lymphatic filariasis affects over 120 million people in 73 countries throughout the tropics
and sub-tropics of Asia, Africa, the Western Pacific, and parts of the Caribbean and South
America.
In the Americas, only four countries are currently known to be endemic: Haiti, the
Dominican Republic, Guyana and Brazil.
In the United States, Charleston, South Carolina, was the last known place with lymphatic
filariasis. The infection disappeared early in the 20th century. Currently, you cannot get
infected in the U.S.
Morphology
Microfilariae
Slightly smaller than those of W. bancrofti
Sheathed and measures about 200-275µm
Possess a sheath, rounded anterior end, and numerous nuclei
Presence of two distinct nuclei in the tip of the somewhat pointed tail (these two
nuclei are distinct and separated from the other nuclei present)
Clinical Manifestation
Often asymptomatic
Fevers may take months to years to develop after initial infection
Formation of granulomatous lesions following microfilarial invasion into the lymphatics,
Adult worms chills, lymphadenopathy, lymphangitis, and eosinophilia
Male and female adult worms of B. malayi and W. bancrofti are indistinguishable Elephentiasis of the legs; elephantiasis of the genitals may also be possible but less
Male: 13-23 mm in length common
Female: 43-55 mm in length
Review Notes in Clinical Parasitology by RMDM 28
Laboratory Diagnosis and Treatment Morphology
Blood Microfilariae
Thin and thick blood smear Sheathed and measures about 0.25 mm long and 6-8µm thick
Wet preparations and concentrations (Knott’s) posterior extremity of the microfilaria showing a column of five nuclei (nu) reaching
PCR the extremity of the tail excluding the sheath.
Serologic testing: Antigen and antibody detection Exhibits diurnal periodicity
Ultrasonography
Drug of Choice: Diethylcarbamazine (DEC)
Alternatice drugs: Ivermectin
Since inflammatory reactions are more common, anti-inflammatory drugs may be
necessary
Adult worms
Prevention and Control White in color and exhibit a cylindrical threadlike
The best way to prevent lymphatic filariasis is to avoid mosquito bites. The mosquitoes appearance
that carry the microscopic worms usually bite between the hours of dusk and dawn. Male: 30-34 mm long
sleep in an air-conditioned room or Female: 40-70 mm long
sleep under a mosquito net ▪ With narrow straight buccal canal and muscular
wear long sleeves and trousers and esophagus
use mosquito repellent on exposed skin. ▪ Extremities contain anus and posterior uterine loop of the posterior uterus
Another approach to prevention includes giving entire communities medicine that kills
the microscopic worms — and controlling mosquitoes.
Life Cycle
Intermediate host: Chrysops fly
Definitive host: man
Loa loa Adult worms take up residence and multiply throughout the subcutaneous tissues.
The microfilariae are present in the blood but not until years after the initial infection
Common Name: ___________________________________________________________________________________
making the diagnosis more difficult.
Associated Diseases: _____________________________________________________________________________
Mode of Transmission: __________________________________________________________________________
1. During a blood meal, an infected fly introduces third-stage filarial larvae onto the skin of
Habitat: ____________________________________________________________________________________________ the human host, where they penetrate into the bite wound.
Infective stage: ___________________________________________________________________________________ 2. The larvae develop into adults that commonly reside in subcutaneous tissue.
Diagnostic stage: _________________________________________________________________________________ 3. Adults produce microfilariae, which are sheathed and have diurnal periodicity.
4. The fly ingests microfilariae during a blood meal. After ingestion, the microfilariae lose
their sheaths and migrate from the fly’s midgut through the hemocoel to the thoracic
Loa loa parasites are found in West and Central Africa (more than 40% of the people who
muscles of the arthropod.
live in that area report that they have had eye worm in the past)
5. There, the microfilariae develop into first-stage larvae and subsequently into third-stage
In the case of L. loa, the Chrysops fly inhabits Africa especially the rainforest belt region. infective larvae.
It is estimated that infection rates may be over 70% in the areas in which a large vector 6. The third-stage infective larvae migrate to the fly’s proboscis and can infect another
population exists. A less than 10% infection rate occurs in regions in which minimal human when the fly takes a blood meal.
numbers of vectors reside.
Review Notes in Clinical Parasitology by RMDM 29
Laboratory Diagnosis and Treatment
The main methods of diagnosis include:
The presence of microfilariae in the blood
The presence of a worm in the eye; and
The presence of skin swelling
Specimen of choice: Giemsa-stained blood
Knott technique and other serologic testing may also be performed
Time of collection: 10:15am and 2:15pm (diurnal periodicity)
The migrating adult worms may be extracted from a variety of body locations, including
the eye.
Other methods:
Blood count
Urine and saliva testing
Drug of Choice: Diethylcarbamazine (DEC) (one side effect is encephalitis; it should be
used with caution)
Prevention and Control
Avoiding areas where the deerflies are found
Clinical Manifestation You may reduce your risk of bites by using insect repellants that contain DEET (N,N-
Pruritus or itchiness and localized pain usually near the joints Diethyl-meta-toluamide)
Calabar swelling (localized subcutaneous edema) at the site of discomfort follows Wearing long sleeves and long pants during the day, which is when deerflies bite
Muscle and joint pain, tiredness and fatigue Treating your clothes with permethrin may also help.
Adult worms may only be noticeable when seen migrating in the conjunctiva of the eye /
under the skin of the bridge of the nose.
CNS involvement
Onchocerca volvulus
Occasional intense swelling can cause nerve compression and subsequent
neuropathies Common Name: ___________________________________________________________________________________
Can lead to carpal tunnel syndrome developmentt Associated Diseases: _____________________________________________________________________________
Meningoencephalitis (increase in microfilarial burden 2,500 microfilaria/ml) Mode of Transmission: __________________________________________________________________________
Microfilaria can be found in CSF with high organism burden Habitat: ____________________________________________________________________________________________
Renal failure
Infective stage: ___________________________________________________________________________________
Glomerular damage
Diagnostic stage: _________________________________________________________________________________
Rarely, microfilariae are evident in urine
Infrequent complications
Lymphadenitis, pulmonary infiltrates, hydroceles, scrotal swelling, and joint The World Health Organization (WHO) estimates that at least 25 million people are
involvement infected with O. volvulus worldwide; of these people 300,000 are blind and 800,000 have
Endomyocardial fibrosis some sort of visual impairment. Some 123 million people are at risk for becoming infected
with the parasite.
Review Notes in Clinical Parasitology by RMDM 30
Morphology 5. There the microfilariae develop into first-stage larvae and subsequently into third-stage
Microfilariae infective larvae. The third-stage infective larvae migrate to the blackfly’s proboscis and
Unsheathed, non-periodic and measure 220-360mm can infect another human when the fly takes a blood meal.
The body contains numerous nuclei that extend from the rounded anterior end,
almost to but not including the tip of the somewhat pointed tail
Normally found in dermis, rarely in the blood, sputum or urine
Adult worms
are long and slender, have a smooth cuticle, and have blunt anterior and posterior
ends.
no lips or buccal capsule, and the mouth is surrounded by 2 circles made up of four
papillae each
White, opalescent and transparent with traverse striation in the muscle
Male: 1.9-4.2 cm
Female: 33-50 cm
Adult worms have a longevity of 10-15 years
Life Cycle
Intermediate host: blackfly genus Simulium
Definitive host: man
The microfilariae are rarely seen in the peripheral blood making this a poor specimen for
Clinical Manifestation
diagnosis.
Symptoms may not appear for months to years
Adults can live in the nodules for approximately 15 years. Some nodules may contain
Early signs include raised nodules that can be seen under the skin around areas over body
numerous male and female worms.
prominence
Symptoms: skin changes, itching, nodules, and alterations in vision
1. During a blood meal, an infected blackfly (genus Simulium) introduces third-stage filarial Onchocerciasis (River blindness)
larvae onto the skin of the human host, where they penetrate into the bite wound. When the eye becomes involved, lesions, due to the body’s reaction to the
2. In subcutaneous tissues the larvae develop into adult filariae, which commonly reside in microfilariae, may lead to blindness. Blindness has proven to be a significant
nodules in subcutaneous connective tissues. complication for many infected adults.
3. In the subcutaneous nodules, the female worms are capable of producing microfilariae for
approximately 9 years.
4. A blackfly ingests the microfilariae during a blood meal. After ingestion, the microfilariae
migrate from the blackfly’s midgut through the hemocoel to the thoracic muscles.
Review Notes in Clinical Parasitology by RMDM 31
Laboratory Diagnosis and Treatment Mansonella perstans
Specimen of choice: Multiple Giemsa-stained slides of tissue biopsies, known as skin
snips (should be collected with as little blood as possible to avoid contamination) Common Name: ___________________________________________________________________________________
Skin snip: most common method of diagnosis Associated Diseases: _____________________________________________________________________________
Infections in the eye can be diagnosed with a slit-lamp examination of the anterior part of Mode of Transmission: __________________________________________________________________________
the eye where the larvae or the lesions they cause are visible. Habitat: ____________________________________________________________________________________________
Drug of Choice: Ivermectin Infective stage: ___________________________________________________________________________________
In patients with nodules in the skin, the nodule can be surgically removed and examined Diagnostic stage: _________________________________________________________________________________
for adult worms.
M. perstans is widely distributed in Africa, with the exception of the most northern
Prevention and Control (Mauritania, Morocco, Algeria, Tunisia, Libya, Egypt), southern (South Africa, Botswana,
There are no vaccines or medications available to prevent becoming infected with O. Lesotho, Swaziland, Namibia) and western (Eritrea, Ethiopia, Djibouti, Somalia) parts and
volvulus. some of the island countries (Madagascar, Comoros, Mauritius, Seychelles, Cape Verde)
The best prevention efforts include personal protection measures against biting insects. from which indigenous cases have not been reported.
This includes wearing insect repellant such as N,N-Diethyl-meta-toluamide (DEET) on A total of 33 countries in Sub-Saharan Africa, with a total of about 580 million inhabitants,
exposed skin,
appear to be endemic for transmission.
Wearing long sleeves and long pants during the day when blackflies bite, and wearing
permethrin- treated clothing.
Morphology
Microfilariae
Unsheathed and measure 190-200 µm in stained blood smears and 180-225 µm in
Parasite Disease Geographic Location of Location of Vector 2% formalin.
genus distribution adult worms microfilariae The tail is blunt, and nuclei extend to the tip of the tail. Microfilariae circulate in the
Onchocerca river blindness, Africa, Central subcutaneous tissues black-fly
skin lesions America blood.
Wuchereria Bancroftian Africa, Asia, lymphatics blood mosquito Adult worms
filariasis South America are cylindrical in shape
(elephantiasis)
Male: 35-45 mm by 50-60 μm
Brugia Malayan/Timorian Malaya/Timor lymphatics blood mosquito
filariasis Female: 50-80 mm by 80-120 μm
(elephantiasis)
Loa Calabar swellings Central/West subcutaneous blood tabanids Life Cycle
Africa
Intermediate host: Culicoides
Definitive host: man
Vector: Culicoides (biting midges)
1. During a blood meal, an infected midge (genus Culicoides) introduces third-stage filarial
larvae onto the skin of the human host, where they penetrate into the bite wound .
2. They develop into adults that reside in body cavities, most commonly the peritoneal cavity
or pleural cavity, but less frequently in the pericardium.
Review Notes in Clinical Parasitology by RMDM 32
3. Adults produce unsheathed and subperiodic microfilariae, measuring 200 by 4.5 µm that Combination of DEC and mebendazole: A combination of the aforementioned drugs has
reach the blood stream. proven to be effective in clinical trials towards reducing the amounts of circulating M.
4. A midge ingests microfilariae during a blood meal. After ingestion, the microfilariae perstans microfilariae and adult M. perstans
migrate from the midge’s midgut through the hemocoel to the thoracic muscles of the
arthropod. Prevention and Control
5. There the microfilariae develop into first-stage larvae and subsequently into third-stage The best way to prevent Mansonella Perstans Infection is through the use of an insect
infective larvae. The third-stage infective larvae migrate to the midge’s proboscis and can repellent.
infect another human when the midge takes a blood meal. Mosquito nets are mostly ineffective because the midges that transmit the M. perstans are
small enough to fly through the net/mesh.
Eliminating the swamp-like areas where Culicoides midges breed is proven to be more
effective in prevention.
Avoiding travel to the endemic areas can also help eliminate the risk of contracting the
infection.
Additional Notes :
Clinical Manifestation
It is a rather mild infection in comparison to similar types of filarial worm infections. Many
individuals do not have any signs and symptoms, but those that do, typically present with
the following:
Itchiness, red, itchy swelling on the arms or underneath the eye, hives, headaches,
fever, pain in the abdomen, and neurologic abnormalities
Laboratory Diagnosis and Treatment
Diagnosed by the finding of microfilariae circulating in blood.
Identification of microfilariae in a blood smear by microscopic examination.
Specimen of Choice: Giemsa-stained blood smear
Review Notes in Clinical Parasitology by RMDM 33
You might also like
- Nursing Care Plan-AscitesDocument10 pagesNursing Care Plan-AscitesKayki Louise75% (4)
- Vaccine Debate by Jennifer MargulisDocument21 pagesVaccine Debate by Jennifer Margulisv2vreader100% (1)
- FILARIASISDocument57 pagesFILARIASISadekayo100% (6)
- Lesson 2 Extraintestinal NematodesDocument5 pagesLesson 2 Extraintestinal NematodesCDNo ratings yet
- BN Filarial WormDocument137 pagesBN Filarial WormCherenet TomaNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- Man Bahadur Rana BPH, Acas, NepalDocument34 pagesMan Bahadur Rana BPH, Acas, NepalDipankar NathNo ratings yet
- Parasitology - Blood & Tissue - W Bancrofti B Malayi - PresentationDocument43 pagesParasitology - Blood & Tissue - W Bancrofti B Malayi - PresentationNicole ManogNo ratings yet
- Filarial NematodeDocument18 pagesFilarial NematodeHawre NajmaddinNo ratings yet
- FilariaDocument85 pagesFilariaRajkishor YadavNo ratings yet
- 3 - Loa Loa and Onchocerca VolvolusDocument29 pages3 - Loa Loa and Onchocerca VolvolusayaamrsharfNo ratings yet
- Helemnth ReportDocument15 pagesHelemnth ReportHawre NajmaddinNo ratings yet
- Filariasis Report (NCM 55 - B3)Document21 pagesFilariasis Report (NCM 55 - B3)Jette Charmae OlboNo ratings yet
- Blood and Tissue NematodesDocument60 pagesBlood and Tissue NematodesDanielle Pecson100% (1)
- PARA NematodesDocument23 pagesPARA Nematodes12 Newton - Cayetano, Arafe Nicole A.No ratings yet
- Wuchereria Bancrofti: Aby Elijah L. BernardinoDocument22 pagesWuchereria Bancrofti: Aby Elijah L. BernardinoAby Brr100% (1)
- Unit - 4-3 - Blood and Tissue NematodesDocument130 pagesUnit - 4-3 - Blood and Tissue NematodesDembalu NuguseNo ratings yet
- Wuchereria BancroftiDocument19 pagesWuchereria BancroftiMayuri VohraNo ratings yet
- Microbiology - ParasitologyDocument34 pagesMicrobiology - ParasitologySasi Dharan100% (1)
- Lect 2Document11 pagesLect 2Sara AliNo ratings yet
- Blood and Tissue NematodesDocument37 pagesBlood and Tissue NematodesjelenaNo ratings yet
- Blood and Tissue Nematods 2015Document109 pagesBlood and Tissue Nematods 2015sinte beyuNo ratings yet
- 4.3. Blood and Tissue NematodesDocument89 pages4.3. Blood and Tissue NematodesRediat GossayeNo ratings yet
- Filariasis: Tropmed Block Faculty Medicine USU 2016Document26 pagesFilariasis: Tropmed Block Faculty Medicine USU 2016Tiurma SibaraniNo ratings yet
- Blood and Tissue Nematodes WipDocument6 pagesBlood and Tissue Nematodes WipHemloNo ratings yet
- Parasitology NotesDocument5 pagesParasitology NotesAndriaNo ratings yet
- Filaria - A Comprehensive StudyDocument63 pagesFilaria - A Comprehensive StudyDayledaniel SorvetoNo ratings yet
- Medical Parasitology A Self Instructional Text PDFDriveDocument60 pagesMedical Parasitology A Self Instructional Text PDFDriveDenise Sta. AnaNo ratings yet
- Filariasis 2015Document56 pagesFilariasis 2015ChandraNo ratings yet
- Blood and Tissue Nematodes BiologiDocument47 pagesBlood and Tissue Nematodes BiologiAxzchiuu :vNo ratings yet
- Revision: Types of Life Cycle in Trematoda and CestodaDocument54 pagesRevision: Types of Life Cycle in Trematoda and CestodaMicroscopeGeekNo ratings yet
- Midterm ParasitologyDocument18 pagesMidterm ParasitologyAngelic AngelesNo ratings yet
- Lecture 10 - Phylum Nematoda and Nematode FilarioideaDocument12 pagesLecture 10 - Phylum Nematoda and Nematode FilarioideaBHEKUMUSA MASEKONo ratings yet
- Dracunculus Medinensis and Filarial WormsDocument19 pagesDracunculus Medinensis and Filarial WormsAnastasiaNo ratings yet
- Habronemose em Um CameloDocument4 pagesHabronemose em Um CameloTais SenaNo ratings yet
- Tissue Nematodes: 49.1 IntoductionDocument8 pagesTissue Nematodes: 49.1 IntoductionAileen LuzonNo ratings yet
- 11 Parasitology - Phasmids 4Document4 pages11 Parasitology - Phasmids 4maqmmNo ratings yet
- Clinical Parasitology-Module 9Document10 pagesClinical Parasitology-Module 9Geresh MagsinoNo ratings yet
- Micropara Lab Parasites Gr123456Document99 pagesMicropara Lab Parasites Gr123456Mary Jane TiangsonNo ratings yet
- Merge AbDocument17 pagesMerge AbEricsson CarabbacanNo ratings yet
- Wu C Here Ria Bancroft IDocument3 pagesWu C Here Ria Bancroft IMariamNo ratings yet
- Wuchereria BancroftiDocument13 pagesWuchereria Bancroftiumeshchandralenka09No ratings yet
- General Parasitology L6Document13 pagesGeneral Parasitology L6kayse abtidoonNo ratings yet
- W - BancroftiDocument19 pagesW - BancroftiALLISON PAMITTANNo ratings yet
- Blood and Tissue Roundworms (Filaria Worms)Document5 pagesBlood and Tissue Roundworms (Filaria Worms)nge257No ratings yet
- Parasitology Day 9 FilariaeDocument4 pagesParasitology Day 9 Filariaeniczdelosreyes8No ratings yet
- NematodaDocument30 pagesNematodaTagonna Di RaizelNo ratings yet
- Report PARA Lymphatic Filarial Nematodes Group 2 Adalid Asug AustriaDocument28 pagesReport PARA Lymphatic Filarial Nematodes Group 2 Adalid Asug AustriaDaniel AustriaNo ratings yet
- FilariasisDocument13 pagesFilariasissarguss14100% (3)
- FilariaDocument16 pagesFilariaJessa MayNo ratings yet
- Merged PDF 2021 11 16T12 - 01 - 01Document15 pagesMerged PDF 2021 11 16T12 - 01 - 01Ericsson CarabbacanNo ratings yet
- Loa Loa, OnchocercaDocument28 pagesLoa Loa, Onchocercabindu dhanapalNo ratings yet
- 9 BIO3243 Lecturer4 RiverblindnessDocument18 pages9 BIO3243 Lecturer4 RiverblindnessNGOGA NISINGIZWE NESTORNo ratings yet
- Wuchereria Bancrofti, Brugia Malayi, Brugia TimoriDocument3 pagesWuchereria Bancrofti, Brugia Malayi, Brugia TimoriJurel GaoatNo ratings yet
- Section 4: Vector Biology and ProfileDocument7 pagesSection 4: Vector Biology and ProfilenurotuljanahNo ratings yet
- Blood Borne Helminths - Wucherelia BancroftiDocument15 pagesBlood Borne Helminths - Wucherelia BancroftiCLEMENTNo ratings yet
- Phylum NematodaDocument11 pagesPhylum NematodaKristine Aranna ConcepcionNo ratings yet
- Worm Tissue Infestation: Umar Zein FK - UisuDocument77 pagesWorm Tissue Infestation: Umar Zein FK - UisuAmalul MukmininNo ratings yet
- Mansonella StreptocercaDocument14 pagesMansonella StreptocercaALLISON PAMITTANNo ratings yet
- Filariasis: Causes, Tests, and Treatment OptionsFrom EverandFilariasis: Causes, Tests, and Treatment OptionsRating: 5 out of 5 stars5/5 (2)
- Bontoc National High School - Senior High School Bontoc, Hindang, LeyteDocument32 pagesBontoc National High School - Senior High School Bontoc, Hindang, LeyteLianne SanchezNo ratings yet
- Identicifation of Hookworm Species in Stool by Harada Mori CultureDocument2 pagesIdenticifation of Hookworm Species in Stool by Harada Mori CultureMeenachi ChidambaramNo ratings yet
- Glycemic Targets 2022Document14 pagesGlycemic Targets 2022Tom BiusoNo ratings yet
- Nacker - 2011 - The-Impact-Of-Climate-Change-And-Other-Factors-On-Zoonotic-DiseasesDocument6 pagesNacker - 2011 - The-Impact-Of-Climate-Change-And-Other-Factors-On-Zoonotic-Diseasesrodrigocamiloo97No ratings yet
- Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) A ReviewDocument13 pagesPathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) A ReviewBryan Diaz LopezNo ratings yet
- Vaccination CertificateDocument1 pageVaccination Certificatemansoor 31 shaikhNo ratings yet
- Republic of The Philippines: NO YESDocument1 pageRepublic of The Philippines: NO YESInchic MirandaNo ratings yet
- Paediatric Symptoms SorterDocument3 pagesPaediatric Symptoms SorterPrasetya Ismail PermadiNo ratings yet
- Study Literatur: Pengkajian Luka Kaki DiabetesDocument15 pagesStudy Literatur: Pengkajian Luka Kaki DiabetesoctaviamayvikaNo ratings yet
- Pcap FinalDocument51 pagesPcap FinalThomas joshua QuiñonesNo ratings yet
- IPL Client History v1 - 7Document8 pagesIPL Client History v1 - 7Karen Dodd100% (1)
- Treatment and Prevention of Meningococcal InfectionDocument18 pagesTreatment and Prevention of Meningococcal InfectionMárcius SilvaNo ratings yet
- Must Have OkoubakaDocument2 pagesMust Have Okoubakaambertje12No ratings yet
- Core Epidemiologic FunctionsDocument6 pagesCore Epidemiologic FunctionsEvans MogakaNo ratings yet
- 15 Virusne Infekcije U Trudnoci - PrevedenoDocument7 pages15 Virusne Infekcije U Trudnoci - PrevedenoVelibor StankovićNo ratings yet
- 1 - MCCDDocument26 pages1 - MCCDAnupam SarkarNo ratings yet
- Fist Bump BillDocument2 pagesFist Bump BillJo InglesNo ratings yet
- Hasil Pemeriksaan Laboratorium: Laboratory Test ResultDocument1 pageHasil Pemeriksaan Laboratorium: Laboratory Test ResultDwi SaputroNo ratings yet
- Master Excel-2Document2 pagesMaster Excel-2Anonymous 7AKb61QyS4No ratings yet
- AnthraxDocument5 pagesAnthraxSaman SarKoNo ratings yet
- Understanding Blood Tests PDFDocument2 pagesUnderstanding Blood Tests PDFKishor SinghNo ratings yet
- 2 PPT Introduction To Epidemiology 18Document21 pages2 PPT Introduction To Epidemiology 18JMCDUFFIENo ratings yet
- DR ZauteaDocument56 pagesDR Zauteadvo aizawlNo ratings yet
- (A) Visitor's Health Declaration Form Dd. 10.05.2020 - GTVIDocument4 pages(A) Visitor's Health Declaration Form Dd. 10.05.2020 - GTVIamwin bizNo ratings yet
- Indovax CD Poultry DiseasesDocument78 pagesIndovax CD Poultry DiseasesSuraj_Subedi100% (3)
- Plant ProtectionDocument9 pagesPlant ProtectionPooja BhusalNo ratings yet
- Infection Control - Bron HenebryDocument28 pagesInfection Control - Bron HenebryGhazali Ahmad SiregarNo ratings yet