Professional Documents
Culture Documents
Central Nervous System Infection in The Pediatric
Central Nervous System Infection in The Pediatric
Uploaded by
Jeriz Marie GamboaCopyright:
Available Formats
You might also like
- Defuse Project Drastic Analysis 1Document25 pagesDefuse Project Drastic Analysis 1Zerohedge Janitor100% (17)
- Chastity Before Marriage - A Fresh Perspective PDFDocument18 pagesChastity Before Marriage - A Fresh Perspective PDFJeriz Marie GamboaNo ratings yet
- CNS InfectionsDocument92 pagesCNS InfectionsWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- 12 Cns Infection 2 LecturesDocument18 pages12 Cns Infection 2 LecturesZain AlAbideen AlTaeeNo ratings yet
- Clinical MicrobiologyDocument16 pagesClinical MicrobiologyArthur YanezNo ratings yet
- Host-Pathogen Interactions in Bacterial MeningitisDocument25 pagesHost-Pathogen Interactions in Bacterial MeningitisEugen TarnovschiNo ratings yet
- بحث نموذج 2Document9 pagesبحث نموذج 2asakingofhNo ratings yet
- Meningitis - StatPearls - NCBI BookshelfDocument13 pagesMeningitis - StatPearls - NCBI Bookshelfaslan tonapaNo ratings yet
- Ppat 1010234hhDocument9 pagesPpat 1010234hhChairulanisaNo ratings yet
- Bacterial Meningitis and Brain Abscess: Key PointsDocument7 pagesBacterial Meningitis and Brain Abscess: Key PointsMartha OktaviaNo ratings yet
- Managing Meningoencephalitis in Indian ICU: Neurocritical CareDocument5 pagesManaging Meningoencephalitis in Indian ICU: Neurocritical CareerikafebriyanarNo ratings yet
- Cshperspectmed BAC A012393Document14 pagesCshperspectmed BAC A012393RaffaharianggaraNo ratings yet
- Meningitis ResearchDocument9 pagesMeningitis ResearchasakingofhNo ratings yet
- Suthar 2018Document10 pagesSuthar 2018CARLOS MONCAYO DIAZNo ratings yet
- Meningitis Bacteriana y Viral 3Document15 pagesMeningitis Bacteriana y Viral 3María Nurys Acevedo CerchiaroNo ratings yet
- Neuroinfección Rosen's Emergency Medicine - Concepts and Clinical Practice 10th Edition 2022Document13 pagesNeuroinfección Rosen's Emergency Medicine - Concepts and Clinical Practice 10th Edition 2022fyqmk4q8pkNo ratings yet
- Meningitis and Acute MeningococcemiaDocument16 pagesMeningitis and Acute Meningococcemiaalfaz lakhaniNo ratings yet
- Upload 2Document10 pagesUpload 2zendah123No ratings yet
- 13 Management and Prevention of Cranioplasty InfectionsDocument8 pages13 Management and Prevention of Cranioplasty InfectionsCatarine OttobeliNo ratings yet
- MSD Pro DocumentDocument6 pagesMSD Pro DocumentMuhammedNo ratings yet
- Epidemic Cerebrospinal MeningitisDocument76 pagesEpidemic Cerebrospinal MeningitisAngie LawrenceNo ratings yet
- Central Nervous System Tuberculosis: John M. LeonardDocument10 pagesCentral Nervous System Tuberculosis: John M. LeonardMarcela Catalina Fandiño VargasNo ratings yet
- Research Review - Term PaperDocument12 pagesResearch Review - Term PaperTania RiazNo ratings yet
- InfectiousmeningitisDocument10 pagesInfectiousmeningitisHow ToNo ratings yet
- Pathogenesis Infection of CnsDocument4 pagesPathogenesis Infection of CnshadiNo ratings yet
- Crum Cianflone2016Document24 pagesCrum Cianflone2016chemistpl420No ratings yet
- TB MeningitisDocument10 pagesTB MeningitisEveline YuniartiNo ratings yet
- Meningitis 2Document28 pagesMeningitis 2Mehveen KashifNo ratings yet
- Intracranial Infection - Prof SunartiniDocument12 pagesIntracranial Infection - Prof SunartiniFranciscus BuwanaNo ratings yet
- Diagnostic and Terapi in Infection in Solid TransplantDocument19 pagesDiagnostic and Terapi in Infection in Solid TransplantretnoNo ratings yet
- Nej MR A 0804573Document9 pagesNej MR A 0804573saabNo ratings yet
- CNS Fungal InfectionDocument12 pagesCNS Fungal InfectionMuhammad Yusuf HanifNo ratings yet
- Neuroinfections Presentation Diagnosis and Treatment of Meningitis and EncephalitisDocument10 pagesNeuroinfections Presentation Diagnosis and Treatment of Meningitis and EncephalitisZarick SaenzNo ratings yet
- Treatment of Extrapulmonary Nontuberculous MycobacDocument11 pagesTreatment of Extrapulmonary Nontuberculous Mycobacjoao pereiraNo ratings yet
- Pathophysiology of Bacterial Meningitis: Mechanism(s) of Neuronal InjuryDocument9 pagesPathophysiology of Bacterial Meningitis: Mechanism(s) of Neuronal InjuryMedranoReyesLuisinNo ratings yet
- Bacterial Meningitis: EpidemiologyDocument4 pagesBacterial Meningitis: EpidemiologykapilNo ratings yet
- 5.infecciones Micóticas Del Sistema Nervioso CentralDocument13 pages5.infecciones Micóticas Del Sistema Nervioso CentralLiz NuñezNo ratings yet
- CNs InfectionDocument6 pagesCNs InfectionChefera AgaNo ratings yet
- Neisseria Meningitidis: General ConceptsDocument16 pagesNeisseria Meningitidis: General Conceptssomebody_maNo ratings yet
- 55 61 Brain AbscessDocument7 pages55 61 Brain AbscessNadia OktarinaNo ratings yet
- Chapter1: Introduction: E Coli and Other Gram-Negative Enteric Bacilli Such AsDocument6 pagesChapter1: Introduction: E Coli and Other Gram-Negative Enteric Bacilli Such AsAhmed RashadNo ratings yet
- Parikh2019 240528 175409Document5 pagesParikh2019 240528 175409cakepbanget1252No ratings yet
- Acutebacterialmeningitis: Current Review and Treatment UpdateDocument11 pagesAcutebacterialmeningitis: Current Review and Treatment UpdateWidya Niendy PrameswariiNo ratings yet
- Bacterial MeningitisDocument2 pagesBacterial MeningitisyanNo ratings yet
- Severe Meningoccal InfectionDocument17 pagesSevere Meningoccal Infectionmatias cisternaNo ratings yet
- Murray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryDocument17 pagesMurray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryAndi Karwana CiptaNo ratings yet
- Invasive Cryptococcal Meningitis Presenting As A Skull Base Mass in An Immunocompetent Host: A Case ReportDocument5 pagesInvasive Cryptococcal Meningitis Presenting As A Skull Base Mass in An Immunocompetent Host: A Case ReportAsep RiswandiNo ratings yet
- Presentation, Diagnosis, and Treatment of Meningitis and Encephalitis A Detailed ReviewDocument7 pagesPresentation, Diagnosis, and Treatment of Meningitis and Encephalitis A Detailed Reviewfitri dwiyantiNo ratings yet
- First Page PDFDocument1 pageFirst Page PDFMay Edogawa SuramuthNo ratings yet
- Roos, Karen L. Greenlee, John E. - Meningitis and EncephalitisDocument14 pagesRoos, Karen L. Greenlee, John E. - Meningitis and EncephalitisNadila Nur PratiwiNo ratings yet
- 2962-Article Text-9149-1-10-20230822Document7 pages2962-Article Text-9149-1-10-20230822Ragil Putri FritriyantiNo ratings yet
- The Importance of Mucormycosis Infections On Example of Rhino Orbital Cerebral MucormycosisDocument6 pagesThe Importance of Mucormycosis Infections On Example of Rhino Orbital Cerebral MucormycosisAlex OprisanNo ratings yet
- MeninigtisDocument5 pagesMeninigtisCatalina Constanza Mujica CovarrubiasNo ratings yet
- Meningococcemia Without Meningitis, Starting With Gastrointestinal Symptoms - Case ReportDocument5 pagesMeningococcemia Without Meningitis, Starting With Gastrointestinal Symptoms - Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Meningitis IN PDF PEDIATRICDocument14 pagesMeningitis IN PDF PEDIATRICCruz Roelia Ruiz SanchezNo ratings yet
- Preprints202309 0487 v1Document23 pagesPreprints202309 0487 v1Saul EstrellaNo ratings yet
- Imaging of Intracranial InfectionsDocument12 pagesImaging of Intracranial Infectionsrafael rocha novaesNo ratings yet
- Mold Infections of The Central Nervous SystemDocument15 pagesMold Infections of The Central Nervous SystemJohn TusselNo ratings yet
- Tuberculous Meningitis: A Narrative ReviewDocument10 pagesTuberculous Meningitis: A Narrative ReviewVyom BuchNo ratings yet
- Bacterial Infections of The Central Nervous System: Paul A. Lapenna, Do Karen L. Roos, MDDocument9 pagesBacterial Infections of The Central Nervous System: Paul A. Lapenna, Do Karen L. Roos, MDOver HidalgoNo ratings yet
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensFrom EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNo ratings yet
- Peptic Ulcer Disease: by Ntr/Jevr/Djs/AjisDocument14 pagesPeptic Ulcer Disease: by Ntr/Jevr/Djs/AjisJeriz Marie GamboaNo ratings yet
- Source For EcolecDocument35 pagesSource For EcolecJeriz Marie GamboaNo ratings yet
- Office of The Secretary: FirstDocument12 pagesOffice of The Secretary: FirstJeriz Marie GamboaNo ratings yet
- International Conference On Physical Activity and Obesity in Children: Summary Statement and RecommendationsDocument18 pagesInternational Conference On Physical Activity and Obesity in Children: Summary Statement and RecommendationsJeriz Marie GamboaNo ratings yet
- Hepatocellular Carcinoma (HCC)Document37 pagesHepatocellular Carcinoma (HCC)Jeriz Marie GamboaNo ratings yet
- The Human Body: An Orientation: Chapter 1Document88 pagesThe Human Body: An Orientation: Chapter 1Jeriz Marie GamboaNo ratings yet
- USTFMS ERB F01 Application FormDocument2 pagesUSTFMS ERB F01 Application FormJeriz Marie GamboaNo ratings yet
- Dating and CourtshipDocument12 pagesDating and CourtshipJeriz Marie GamboaNo ratings yet
- Chapter 12. BloodDocument23 pagesChapter 12. BloodJeriz Marie GamboaNo ratings yet
- Make Health Your "New High" Life Not DrugsDocument1 pageMake Health Your "New High" Life Not DrugsJeriz Marie GamboaNo ratings yet
- Human Genetic VariationDocument35 pagesHuman Genetic VariationJeriz Marie GamboaNo ratings yet
- Mitosis and Meiosis: Higher BiologyDocument16 pagesMitosis and Meiosis: Higher BiologyJeriz Marie GamboaNo ratings yet
- Mitosis New Cells: Results in 2 Identical Daughter CellsDocument26 pagesMitosis New Cells: Results in 2 Identical Daughter CellsJeriz Marie GamboaNo ratings yet
- Xoxo GossipDocument2 pagesXoxo GossipJeriz Marie GamboaNo ratings yet
- Environmental and Experimental Botany: R. Cruz de Carvalho, A. Bernardes Da Silva, C. Branquinho, J. Marques Da SilvaDocument5 pagesEnvironmental and Experimental Botany: R. Cruz de Carvalho, A. Bernardes Da Silva, C. Branquinho, J. Marques Da SilvaJeriz Marie GamboaNo ratings yet
- Ekonomiks: Maxine Yosobelle P. Cruz 10-Righteousness Ms - SardonDocument5 pagesEkonomiks: Maxine Yosobelle P. Cruz 10-Righteousness Ms - SardonJeriz Marie Gamboa0% (1)
- Lesson 28 Using The Internet and The World Wide Web: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument39 pagesLesson 28 Using The Internet and The World Wide Web: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Lesson 27 Communications and Collaboration: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument39 pagesLesson 27 Communications and Collaboration: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Lesson 26 Communication Services: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument36 pagesLesson 26 Communication Services: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Lesson 25 Network Fundamentals: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument45 pagesLesson 25 Network Fundamentals: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Typhidot TestDocument1 pageTyphidot TestPre Cadet AcademyNo ratings yet
- Microbiology ReviewerDocument3 pagesMicrobiology ReviewerWendy Escalante100% (6)
- Animal Health and Livestock Services Act 2055 NepalDocument13 pagesAnimal Health and Livestock Services Act 2055 NepalSuraj SubediNo ratings yet
- (Libribook - Com) Introduction To Clinical Infectious Diseases A Problem-Based Approach 1st EditionDocument465 pages(Libribook - Com) Introduction To Clinical Infectious Diseases A Problem-Based Approach 1st EditionDaoud IssaNo ratings yet
- Rajiv Gandhi University: of Health SciencesDocument40 pagesRajiv Gandhi University: of Health SciencesAnirudhGopalNo ratings yet
- Bioterrorism and Biowarfare BTH 1Document6 pagesBioterrorism and Biowarfare BTH 1Akshita JainNo ratings yet
- ميكرو دبيDocument30 pagesميكرو دبيMohsen Haleem0% (1)
- HIV 1&2 Ab Cass Z09742 Rev01Document6 pagesHIV 1&2 Ab Cass Z09742 Rev01werther666No ratings yet
- UntitledDocument103 pagesUntitledjana whiteNo ratings yet
- Science of MicrobiologyDocument11 pagesScience of MicrobiologyJamaica M DanguecanNo ratings yet
- Bacteriocin Production by Lactic Acid Bacteria Encapsulated in Calcium Alginate BeadsDocument8 pagesBacteriocin Production by Lactic Acid Bacteria Encapsulated in Calcium Alginate BeadsangelicaaragonNo ratings yet
- Arbovirus Flash CardsDocument11 pagesArbovirus Flash CardsmfabzakNo ratings yet
- How To Transfer A Mobilizable Plasmid From A Cell Without A Conjugative Plasmid?Document14 pagesHow To Transfer A Mobilizable Plasmid From A Cell Without A Conjugative Plasmid?m86544422No ratings yet
- Virulence Factors MycoplasmDocument9 pagesVirulence Factors MycoplasmAlan GarcíaNo ratings yet
- Limitations Results: Congenital Syphilis: Management Dilemmas Using Reverse ScreeningDocument1 pageLimitations Results: Congenital Syphilis: Management Dilemmas Using Reverse ScreeningFaye Cabotaje LinganNo ratings yet
- Gabinete - 2A - Module 1 AssessmentDocument3 pagesGabinete - 2A - Module 1 AssessmentNathaniel GABINETENo ratings yet
- Biggy AgarDocument2 pagesBiggy AgarMatei BogdanNo ratings yet
- Intestinal and Commensal AmoebaDocument9 pagesIntestinal and Commensal AmoebaFuture TrekingNo ratings yet
- BurnettDocument4 pagesBurnettJean CotteNo ratings yet
- Principles of Antimicrobial Therapy 2022Document33 pagesPrinciples of Antimicrobial Therapy 2022Puteri Nursyamimi Mohd SabilanNo ratings yet
- Rev 6. DAFTAR PUSTAKA 19novDocument8 pagesRev 6. DAFTAR PUSTAKA 19novSams SriningsihNo ratings yet
- Microbiology Laboratory PrelimsDocument8 pagesMicrobiology Laboratory PrelimsMARIA ISABILLE DUALLO MUSONGNo ratings yet
- Literature ReviewDocument2 pagesLiterature ReviewFaith Arpon AbogandaNo ratings yet
- Deferrals For Blood DonationDocument2 pagesDeferrals For Blood DonationShane AñoNo ratings yet
- Reference: Product: Technical Data Sheet: Legionella GVPC Supplement IsoDocument2 pagesReference: Product: Technical Data Sheet: Legionella GVPC Supplement IsoSLN TESTING LABORATORYNo ratings yet
- Basic ParasitologiDocument23 pagesBasic ParasitologiNur'Azmi AyuningtyasNo ratings yet
- Pathogenesis TBDocument39 pagesPathogenesis TBGede Eka Putra NugrahaNo ratings yet
- Philippine Adult Immunization Recommendation 2017 PDFDocument2 pagesPhilippine Adult Immunization Recommendation 2017 PDFLinius CruzNo ratings yet
- CDC's HIV Infection Through Oral Sex, Fact SheetDocument2 pagesCDC's HIV Infection Through Oral Sex, Fact SheetCésar E. ConcepciónNo ratings yet
Central Nervous System Infection in The Pediatric
Central Nervous System Infection in The Pediatric
Uploaded by
Jeriz Marie GamboaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Central Nervous System Infection in The Pediatric
Central Nervous System Infection in The Pediatric
Uploaded by
Jeriz Marie GamboaCopyright:
Available Formats
[Downloaded free from http://www.pediatricneurosciences.com on Monday, April 2, 2018, IP: 176.212.163.
5]
Review Article
Central nervous system infection in the
pediatric population
Rabi Narayan Sahu, Raj Kumar, A. K. Mahapatra
Department of Neurosurgery, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India.
Address for Correspondence: Dr. Rabi Narayan Sahu, Department of Neurosurgery, Sanjay Gandhi Postgraduate Institute of Medical
Sciences, Rae Bareli Road, Lucknow, Uttar Pradesh-226 014, India. E-mail: drrnsahu@gmail.com
ABSTRACT
Infection of the central nervous system is a life-threatening condition in the pediatric population. Almost all
agents can cause infection within the central nervous system and the extent of infection ranges from diffuse
involvement of the meninges, brain, or the spinal cord to localized involvement presenting as a space-occupying
lesion. Modern imaging techniques define the anatomic region infected, the evolution of the disease, and help
in better management of these patients. Acute bacterial meningitis remains a major cause of mortality and
long-term neurological disability. Fortunately, the incidence of infection after clean craniotomy is < 5%, but it
leads to significant morbidity as well as fiscal loss. The most significant causative factor in postcraniotomy
infections is postoperative CSF leak. Cerebral abscess related to organic congenital heart disease is one of
the leading causes of morbidity and mortality in the pediatric population. The administration of prophylactic
antibiotics is indicated for contaminated and clean-contaminated wounds.
Key words: Cerebral abscess, meningitis, pediatric, post-craniotomy infection, prophylactic antibiotics
Introduction of potent newer antibiotics, the mortality rate due to acute
bacterial meningitis remains significantly high (16–32%) in
Infection of the central nervous system is a life-threatening India and other developing countries.[1-4]
condition, especially in children, that demands immediate
attention from the attending physician or surgeon and the
clinical pathologist as well as the microbiologist. Almost Bacteriology of Infection and
all agents can cause infection within the central nervous Host Defenses
system and the extent of infection ranges from diffuse
involvement of the meninges, brain, or the spinal cord to Almost every infective agent can cause infections within
localized involvement presenting as a space-occupying the CNS, although agents vary in their tendency to do so.
lesion. Epidemiological considerations, appreciation of the
Infective agents generally gain access to the CNS either
presenting clinical syndrome (acute bacterial meningitis,
by the hematogenous route or by direct extensions. Most
acute aseptic meningitis, chronic meningitis or space-
agents that can invade the blood stream can be carried to
occupying lesions) and cerebrospinal fluid analysis facilitates
the CNS. The rare exceptions include rabies virus, herpes
diagnosis. Modern imaging techniques define the anatomic
region that has been infected and the evolution of the disease, simplex virus 1, and Naegleria fowleri. In rabies, the virus
help to evaluate the treatment efficacy, and can frequently travels along the peripheral nerves from the site of infection
help to determine extra-central nervous system sources of to the CNS. However, in herpes and Naegleria infections,
infection, such as sinusitis or mastoiditis. Acute bacterial the inoculation occurs directly through the olfactory bulbs.
meningitis remains a major worldwide cause of mortality Bacterial agents commonly cause infection of the CNS in
and long-term neurological sequelae. Despite the availability infants and children. By far, the most common presentation of
such infection is meningitis. Less often, intracranial abscesses
are found in the epidural, subdural, or intracerebral tissues.
DOI: 10.4103/1817-1745.49102 The incidence of bacterial meningitis is high in the first few
Online full text at months of life and continues to be high until two years of age,
http://www.pediatricneurosciences.com after which it declines considerably.[5,6] Neonates usually
20 / J Pediatr Neurosci / Volume 4 / Jan-Jun / 2009
[Downloaded free from http://www.pediatricneurosciences.com on Monday, April 2, 2018, IP: 176.212.163.5]
Sahu, et al.: Infection in pediatric population
derive their colonization from the maternal gastrointestinal Specific CNS Infections
or genitourinary tracts. In the first two weeks of life, group
B Streptococci and Escherichia coli are the most common Craniotomy infections
infective agents, accounting for approximately 80–85% In most hospitals, the incidence of infection after clean
of all cases.[7] The bulk of the remaining cases are caused craniotomy is < 5%. There are several contributing factors
by other coliforms such as Enterobacter cloacae, Proteus such as the duration of surgery, re-exploration surgery, age
mirabilis, Citrobacter freundii, Klebsiella pneumoniae, and of the patient, and postoperative CSF leaks.[12,13] However,
Salmonella enteritidis. Group B Streptococci type-I are still the most significant causative factor in postcraniotomy
the most frequent cause of bacterial meningitis in infants infections is the postoperative CSF leak.[14] CSF fistulae
between three and six weeks of age. [8] A comprehensive offer routes for bacterial entry and should be treated
age-wise etiology of meningitis is given in the Table 1.[9] promptly.[12] A few stitches in time when the skin is healthy,
solve the problem in most cases. Sometimes, repeated
Fortunately, the central nervous system is well protected lumber punctures or a spinal drain help and enables the
against most micro-organisms because of its unique location CSF fistula to scar.
deep in the body where it is protected by skin, muscle, bone,
and tough fibrous tissue. Surgical interventions transcend Amongst the further complications of craniotomy infections are
these barriers and directly expose the CNS to the possibility postoperative meningitis, empyema, abscess formation, wound
of microbiological attacks. However, the body executes a gap, and bone flap infections. Postoperative meningitis is not
complex series of host defenses to reduce the likelihood very common but it is a potentially lethal complication[15] with
that such microbiologic contaminations will proceed to Staphylococci sp. being common pathogens in such meningitis.
frank infection. Whether a bacterial inoculum in a wound Lumber puncture should be done to exclude meningitis in the
will proceed to a frank infection can be predicted by many postoperative period if the patients show signs of meningismus
factors such as the size and virulence of the inoculum and with fever. Choosing a proper antibiotic is as important as
the level of the host defense present. administering these antibiotics in proper doses.[16]
Bone flap infection
Imaging in Infection The incidence of bone flap infection following craniotomy is
greater when the bone is devascularized. Bone flap infections
Imaging is extremely important in the diagnosis and are characterized by a local inflammation and a nonhealing
management of intracranial infections. It defines the fistula. The standard treatment is removal of the infected
anatomic region affected: the epidural or subdural bone flap and cranioplasty at a later date.[17,18]
spaces, the pia-arachnoid, the cerebral parenchyma, or
the ventricles. It also helps to define the evolution of the CSF shunt infection
process, i.e., the transitions from meningitis to cerebritis
CSF shunt infections are one of the most important infections
to abscess formation. The primary imaging techniques for
encountered by neurosurgeons. According to several studies,
demonstrating the presence of inflammation and their
the incidence varies from 5–39% of all shunts [19,20] and
effects are computerized tomography (CT) and magnetic
the infective etiology is responsible for hydrocephalus in
resonance imaging (MRI). The intravenous injection of a significant number of children (36%).[20] The possibility
an iodinated contrast agent is essential in the CT-assisted of TORCH infection as a cause of hydrocephalus should
diagnosis of cerebritis, cerebral abscess, and ventriculitis. be considered during antenatal check-up even among the
Similarly magnetic resonance contrast agents such as children of screened mothers. As colonization of shunt
gadolinium-DTPA cross the blood brain barrier in areas tubing occurs most frequently during surgery, the organisms
of cerebritis or abscess.[10,11] MRI is superior to CT scans in are usually skin pathogens, especially Staphylococci sp., both
showing meningeal enhancement from meningitis because coagulase-positive and coagulase-negative types. Staphylococci
of the absence of bony artifacts of adjacent skull bones epidermidis, (coagulase-negative) makes up the largest group
seen with CT scans. However, evidence of bony erosion of microorganisms that colonize shunts.[21] There is some
or abnormalities due to inflammation is more clearly controversy about whether antibiotic-impregnated shunts
demarcated in CT scans than in MRI. help in preventing infection.[22,23] Sometimes, brain abscess
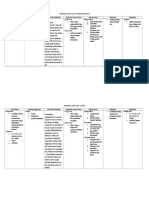
Table 1: Age-wise etiology of meningitis
Within 2 weeks 3 to 6 weeks 7 weeks to 15 years > 15 years
Group B Streptococcus Group B Streptococcus Haemophilus inßuenzae b Streptococcus pneumoniae
Escherichia coli Haemophilus inßuenzae b Streptococcus pneumoniae Neisseria meningitides
Enterococcus Streptococcus pneumoniae Neisseria meningitides Streptococcus
Listeria monocytogenes Neisseria meningitides Staphylococcus
Escherichia coli Listeria monocytogenes
Listeria monocytogenes
2009 / Jan-Jun / Volume 4 / J Pediatr Neurosci / 21
[Downloaded free from http://www.pediatricneurosciences.com on Monday, April 2, 2018, IP: 176.212.163.5]
Sahu, et al.: Infection in pediatric population
and other uncommon complications can occur due to shunt begins subsequently with capsulation consolidating around
insertion.[24,25] the necrotic center. The late capsule phase occurs around
14 days with dense collagen capsulation surrounded by a
gliotic pseudocapscule.[33] The treatment of the brain abscess
Intracranial Abscess is usually nonsurgical, but surgical aspiration or excision of
the whole abscess in necessary in most cases.[34] Occasionally,
The incidence of brain abscess is higher in India. Bhatia et spontaneous evacuation of intracranial abscesses has been
al, reported that abscess comprised 8% of all intracranial reported through normal or abnormal pathways.[35]
spinal space-occupying lesions.[25] Brain abscess is initiated
when micro-organisms are introduced as a result of trauma,
contiguous infection, or hematogenous dissemination. Neurosurgical Infections in the
Sometimes, the abscess confines itself to subdural spaces
and is then known as subdural empyema [Figure 1]. The
Immunocompromised Host
source of infection is frequently found and the cause
Infection involving the CNS is often devastating in patients
remains obscure in 10–37% of patients. [26] Suppurative
with compromised immune function. The incidence of
infections of the paranasal sinus, middle ear, and mastoid
CNS infection in immunocompromised patients is 0.6–14%
are the most common sources of underlying infection in
with a mortality rate of 42–77%. Sometimes, intracranial
most clinical series.[27-29] Metastatic abscesses occur through
infections harbor unusual organisms such as Nocardia sp.
hematogenous dissemination of micro-organisms from a
etc. [36] Meningitis and encephalitis represent most CNS
remote site of infection. Common primary foci include skin
infections in immunocompromised patients and do not usually
pustules, pulmonary infections (empyema, bronchiectasis,
require neurosurgical attention. The developments of brain
abscess and pneumonia), osteomyelitis, dental abscess, and
abscess in the compromised host signals a neurosurgical
subacute bacterial endocarditis. Metastatic abscesses occur in
emergency. Organ transplantation and cancer patients
multiples and tend to occur at the cortico-medullary junction
comprise the majority of immunocompromised patients
where the blood flow is slowest.[30] Cerebral abscess related to
who are prone to brain abscess formation.[37] The duration
organic congenital heart disease is one of the leading causes
of immunosuppressant therapy is a major determining
of morbidity and mortality in the pediatric population.[31]
factor for the development of CNS infection. After organ
Tubercular brain abscess (TBA) is a rare manifestation of
transplantation, the maximal risk of CNS infection for
CNS tuberculosis. It is characterized by an encapsulated
transplants recipients is for the first four months. Potential
collection of pus containing viable tubercular bacilli without
infections including Pseudomonas sp, E. coli, and Proteus sp
any evidence of tubercular granuloma.[32] Britt et al, divided
are more common. Among fungal infections, Aspergillus sp
abscess formation into four stages based on histopathologic
is common.[38,39]
data.[33] The early celebrities (days one to three) stage is
characterized by the presence of a necrotic center accompanied Tubercular abscess formation has been described in some
by a local inflammatory response surrounding the adventitia cases.[40]
of blood vessels [Figure 2]. In the late celebrities phase
(days four to nine), pus formation occurs leading to the
enlargement of the necrotic center, which is surrounded by Antibiotic Prophylaxis in Neurosurgery
a zone of inflammatory cells and macrophages; maximum
edema occurs during this phase. Early encapsulation phase Due to a low risk of infection (2–3%), prophylactic use of
Figure 1: Brain abscess in contrast-enhanced CT scan Figure 2: Interhemispheric subdural empyema
22 / J Pediatr Neurosci / Volume 4 / Jan-Jun / 2009
[Downloaded free from http://www.pediatricneurosciences.com on Monday, April 2, 2018, IP: 176.212.163.5]
Sahu, et al.: Infection in pediatric population
antibiotics in neurosurgery is a controversial issue. Some References
neurosurgeons believe that there are strong arguments
against the use of antimicrobials (promotion of antibiotic- 1. Kabra SK, Kumar P, Verma IC, Mukherjee D, Chowdhary BH, Sengupta
resistant strains of bacteria, superinfection, and adverse S, et al. Bacterial meningitis in India: An IJP survey. Indian J Pediatr
drug reactions) and meticulous aseptic techniques could 1991;58:505-11.
2. Tang LM, Chen ST, Hsu WC, Lyu RK. Acute bacterial meningitis
be more useful than prophylactic antibiotics. On the
in adults: A hospital-based epidemiological study. Q J Med 1999;92:
other hand, despite being rare, the consequences of a 719-25.
neurosurgical infection can be dramatic and may result 3. Celal A, Faruk GM, Salih H, Kemal CM, Serife A, Faruk KO.
in rapid death caused by meningitis, cerebritis, abscess Characteristics of acute bacterial meningitis in Southeast Turkey. Indian
formation, or sepsis.[41,42] Ideally, a prophylactic antibiotic J Med Sci 2004;58:327-33.
should achieve high peak tissue concentrations at the site of 4. Chinchankar N, Mane M, Bhave S, Bapat S, Bavdekar A, Pandit A,
the wound before the first incision and should be maintained et al. Diagnosis and outcome of acute bacterial meningitis in early
childhood. Indian Pediatr 2002;39:914-21.
until the time of closure. Currently, the administration of
5. Wubbel L, McCracken GH Jr. Management of bacterial meningitis.
prophylactic antibiotics is indicated for contaminated and Pediatr Rev 1998;19:78-84.
clean-contaminated wounds. Clinical studies emphasized 6. Sáez-Llorens X, McCracken GH Jr. Bacterial meningitis in neonates
that the most important factors influencing the choice of and children. Infect Dis Clin North Am 1990;4:623-44.
antibiotic prophylaxis in neurosurgery is the patient’s immune 7. Barker FG 2nd. Efficacy of prophylactic antibiotics against meningitis
status, virulence of the pathogens, and the type of surgery after craniotomy: A meta-analysis. Neurosurgery 2007;60:887-94;
discussion 887-94.
(“clean contaminated”--procedure that crosses the cranial
8. Feigin RD, Dodge PR. Bacterial meningitis: newer concepts of
sinuses, “clean nonimplant”--procedure that does not cross pathophysiology and neurologic sequelae. Pediatr Clin North Am
the cranial sinuses, CSF shunt surgery, skull fracture). Despite 1976;23:541-56.
the proven effectiveness of antibiotic prophylaxis, many 9. Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld
researchers would argue that contemporary dosing regimens WM, et al. Practice guidelines for the management of bacterial
should be re-evaluated. The debates concerning the dosage meningitis. Clin Infect Dis 2004;39:1267-84.
and timing of ideal prophylactic administration are likely to 10. Haimes AB, Zimmerman RD, Morgello S, Weingarten K, Becker RD,
Jennis R, et al. MR imaging of brain abscesses. AJR Am J Roentgenol
continue.[42]
1989;152:1073-85.
11. Mathews VP, Kuharik MA, Edwards MK, D’Amour PG, Azzarelli
B, Dreesen RG. Dyke award. Gd-DTPA-enhanced MR imaging of
Discussion experimental bacterial meningitis: Evaluation and comparison with
CT. AJR Am J Roentgenol 1989;152:131-6.
Almost all agents can cause infection within the central 12. Mollman HD, Haines SJ. Risk factors for postoperative neurosurgical
nervous system and the extent of infection ranges from wound infection: A case-control study. J Neurosurg 1986;64:902-6.
13. Wright RL. A survey of possible etiologic agents in postoperative
diffuse involvement of the meninges, brain, or the spinal
craniotomy infections. J Neurosurg 1966;25:125-32.
cord to localized involvement presenting as a space- 14. Blomstedt GC. Craniotomy infections. Neurosurg Clin N Am
occupying lesion. Infection of the central nervous system 1992;3:375-85.
is a life-threatening condition in the pediatric population. 15. Blomstedt GC. Infections in neurosurgery: A retrospective study
Modern imaging techniques define the anatomic region of 1143 patients and 1517 operations. Acta Neurochir (Wien)
that has been infected, the evolution of the disease, and 1985;78:81-90.
help in improved management of these patients. Acute 16. De Bels D, Korinek AM, Bismuth R, Trystram D, Coriat P, Puybasset L.
Empirical treatment of adult postsurgical nosocomial meningitis. Acta
bacterial meningitis remains a major cause of mortality and
Neurochir (Wien) 2002;144:989-95.
long-term neurological disability. Fortunately, the incidence 17. Dashti SR, Baharvahdat H, Spetzler RF, Sauvageau E, Chang SW,
of infection after clean craniotomy is < 5%, but it leads Stiefel MF, et al. Operative intracranial infection following craniotomy.
to significant morbidity as well as fiscal loss. The most Neurosurg Focus 2008;24:E10.
significant causative factor in postcraniotomy infections is 18. McClelland S 3rd, Hall WA. Postoperative central nervous system
the postoperative CSF leak. CSF shunt infection is one of infection: incidence and associated factors in 2111 neurosurgical
procedures. Clin Infect Dis 2007;45:55-9.
the most important infections encountered by neurosurgeons.
19. Conen A, Walti LN, Merlo A, Fluckiger U, Battegay M, Trampuz A.
Staphylococci epidermidis (coagulase-negative) makes up the Characteristics and treatment outcome of cerebrospinal fluid shunt-
largest group of microorganisms colonizing shunts. Cerebral associated infections in adults: A retrospective analysis over an 11-year
abscess related to organic congenital heart disease is one of period. Clin Infect Dis 2008;47:73-82.
the leading causes of morbility and mortality in the pediatric 20. Kumar R, Singh V, Kumar MV. Shunt revision in hydrocephalus. Indian
population. The administration of prophylactic antibiotics J Pediatr 2005;72:843-7.
is indicated for contaminated and clean-contaminated 21. Kontny U, Höfling B, Gutjahr P, Voth D, Schwarz M, Schmitt HJ. CSF
shunt infections in children. Infection 1993;21:89-92.
wounds. The most important factors influencing the choice 22. Sciubba DM, Stuart RM, McGirt MJ, Woodworth GF, Samdani A,
of antibiotic prophylaxis in neurosurgery are the patient’s Carson B, et al. Effect of antibiotic-impregnated shunt catheters
immune status, the virulence of the pathogens, and the type in decreasing the incidence of shunt infection in the treatment of
of surgery performed. hydrocephalus. J Neurosurg 2005;103:131-6.
2009 / Jan-Jun / Volume 4 / J Pediatr Neurosci / 23
[Downloaded free from http://www.pediatricneurosciences.com on Monday, April 2, 2018, IP: 176.212.163.5]
Sahu, et al.: Infection in pediatric population
23. Kan P, Kestle J. Lack of efficacy of antibiotic-impregnated shunt 972-89.
systems in preventing shunt infections in children. Childs Nerv Syst 35. Moorthy RK, Rajshekhar V. Management of brain abscess: An overview.
2007;23:773-7. Neurosurg Focus 2008;24:E3.
24. Pandey P, Suri A, Singh AK, Mahapatra AK. Brain abscess: An 36. Kumar R, Sharma R, Tyagi I. Spontaneous evacuation of cerebellar
unusual complication of ventriculo-peritoneal shunt. Indian J Pediatr abscess through the middle ear: A case report. Neurosurg Rev
2003;70:833-4. 1998;21:66-8.
25. Kumar R. Uncommon manifestations of shunt infection. Indian J 37. Mukhopadhyay C, Sahu RN, Ayyagari A. Nocardial brain abscesses
Pediatr 2003;70:21-4. in a HIV positive patient misinterpreted as tubercular brain abscesses.
26. Bhatia R. Brain abscess in children. Indian J Pediatr 1983;50:591-7. Nepal Med Coll J 2005;7:74-6.
27. Carpenter J, Stapleton S, Holliman R. Retrospective analysis of 49 38. Rodríguez-Granger J, Olivares G, Turiño JD, Camacho-Muñoz E.
cases of brain abscess and review of the literature. Eur J Clin Microbiol Cerebral abscess in an immunosuppressed patient. Enferm Infecc
Infect Dis 2007;26:1-11. Microbiol Clin 2005;23:41-2.
28. Bradley PJ, Manning KP, Shaw MD. Brain abscess secondary to paranasal 39. Polo JM, Fábrega E, Casafont F, Fariñas MC, Salesa R, Vázquez A,
sinusitis. J Laryngol Otol 1984;98:719-25. et al. Treatment of cerebral aspergillosis after liver transplantation.
29. Papanagiotou P, Grunwald IQ, Politi M, Reith WJ. Cerebral abscess due Neurology 1992;42:1817-9.
to sinusitis. Arch Neurol 2008;65:668-9. 40. Proca E, Popescu A. Tuberculous cerebral abscess 8 years after renal
30. Gallagher RM, Gross CW, Phillips CD. Suppurative intracranial transplantation. Br J Urol 1991;68:205.
complications of sinusitis. Laryngoscope 1998;108:1635-42. 41. Korinek AM, Baugnon T, Golmard JL, van Effenterre R, Coriat
31. Goodkin HP, Harper MB, Pomeroy SL. Intracerebral abscess in P, Puybasset L. Risk factors for adult nosocomial meningitis after
children: Historical trends at Children’s Hospital Boston. Pediatrics craniotomy: role of antibiotic prophylaxis. Neurosurgery 2006;59:126-
2004;113:1765-70. 33; discussion 126-33.
32. Kumar R, Pandey CK, Bose N, Sahay S. Tuberculous brain abscess: 42. Dempsey R, Rapp RP, Young B, Johnston S, Tibbs P. Prophylactic
Clinical presentation, pathophysiology and treatment (in children). parenteral antibiotics in clean neurosurgical procedures: A review. J
Childs Nerv Syst 2002;18:118-23. Neurosurg 1988;69:52-7.
33. Sharma BS, Gupta SK, Khosla VK. Current concepts in the management
of pyogenic brain abscess. Neurol India 2000;48:105-11.
34. Britt RH, Enzmann DR. Clinical stages of human brain abscesses on
serial CT scans after contrast infusion. Computerized tomographic, Source of Support: Nil, Conflict of Interest: None declared.
neuropathological and clinical correlations. J Neurosurg 1983;59:
Author Help: Sending a revised article
1) Include the referees’ remarks and point to point clarification to those remarks at the beginning, in the revised article file itself. In
addition, mark the changes as underlined or coloured text in the article. Please include in a single file
a. referees’ comments
b. point to point clarifications on the comments
c. revised article with text highlighting the changes done
2) Include the original comments of the reviewers/editor with point to point reply, at the beginning of the article in the ‘Article File’. To
ensure that the reviewer can assess the revised paper in timely fashion, please reply to the comments of the referees/editors in the
following manner:
• There is no data on follow-up of these patients.
Authors’ Reply: The follow up of patients has been included in the results section [Page 3, para 2]
• Authors should highlight the relation of complication to duration of diabetes.
Authors’ Reply: The complications as seen in our study group has been included in the results section [Page 4, Table]
24 / J Pediatr Neurosci / Volume 4 / Jan-Jun / 2009
You might also like
- Defuse Project Drastic Analysis 1Document25 pagesDefuse Project Drastic Analysis 1Zerohedge Janitor100% (17)
- Chastity Before Marriage - A Fresh Perspective PDFDocument18 pagesChastity Before Marriage - A Fresh Perspective PDFJeriz Marie GamboaNo ratings yet
- CNS InfectionsDocument92 pagesCNS InfectionsWaaqoo Guutuu Waaqoo GuutuuNo ratings yet
- 12 Cns Infection 2 LecturesDocument18 pages12 Cns Infection 2 LecturesZain AlAbideen AlTaeeNo ratings yet
- Clinical MicrobiologyDocument16 pagesClinical MicrobiologyArthur YanezNo ratings yet
- Host-Pathogen Interactions in Bacterial MeningitisDocument25 pagesHost-Pathogen Interactions in Bacterial MeningitisEugen TarnovschiNo ratings yet
- بحث نموذج 2Document9 pagesبحث نموذج 2asakingofhNo ratings yet
- Meningitis - StatPearls - NCBI BookshelfDocument13 pagesMeningitis - StatPearls - NCBI Bookshelfaslan tonapaNo ratings yet
- Ppat 1010234hhDocument9 pagesPpat 1010234hhChairulanisaNo ratings yet
- Bacterial Meningitis and Brain Abscess: Key PointsDocument7 pagesBacterial Meningitis and Brain Abscess: Key PointsMartha OktaviaNo ratings yet
- Managing Meningoencephalitis in Indian ICU: Neurocritical CareDocument5 pagesManaging Meningoencephalitis in Indian ICU: Neurocritical CareerikafebriyanarNo ratings yet
- Cshperspectmed BAC A012393Document14 pagesCshperspectmed BAC A012393RaffaharianggaraNo ratings yet
- Meningitis ResearchDocument9 pagesMeningitis ResearchasakingofhNo ratings yet
- Suthar 2018Document10 pagesSuthar 2018CARLOS MONCAYO DIAZNo ratings yet
- Meningitis Bacteriana y Viral 3Document15 pagesMeningitis Bacteriana y Viral 3María Nurys Acevedo CerchiaroNo ratings yet
- Neuroinfección Rosen's Emergency Medicine - Concepts and Clinical Practice 10th Edition 2022Document13 pagesNeuroinfección Rosen's Emergency Medicine - Concepts and Clinical Practice 10th Edition 2022fyqmk4q8pkNo ratings yet
- Meningitis and Acute MeningococcemiaDocument16 pagesMeningitis and Acute Meningococcemiaalfaz lakhaniNo ratings yet
- Upload 2Document10 pagesUpload 2zendah123No ratings yet
- 13 Management and Prevention of Cranioplasty InfectionsDocument8 pages13 Management and Prevention of Cranioplasty InfectionsCatarine OttobeliNo ratings yet
- MSD Pro DocumentDocument6 pagesMSD Pro DocumentMuhammedNo ratings yet
- Epidemic Cerebrospinal MeningitisDocument76 pagesEpidemic Cerebrospinal MeningitisAngie LawrenceNo ratings yet
- Central Nervous System Tuberculosis: John M. LeonardDocument10 pagesCentral Nervous System Tuberculosis: John M. LeonardMarcela Catalina Fandiño VargasNo ratings yet
- Research Review - Term PaperDocument12 pagesResearch Review - Term PaperTania RiazNo ratings yet
- InfectiousmeningitisDocument10 pagesInfectiousmeningitisHow ToNo ratings yet
- Pathogenesis Infection of CnsDocument4 pagesPathogenesis Infection of CnshadiNo ratings yet
- Crum Cianflone2016Document24 pagesCrum Cianflone2016chemistpl420No ratings yet
- TB MeningitisDocument10 pagesTB MeningitisEveline YuniartiNo ratings yet
- Meningitis 2Document28 pagesMeningitis 2Mehveen KashifNo ratings yet
- Intracranial Infection - Prof SunartiniDocument12 pagesIntracranial Infection - Prof SunartiniFranciscus BuwanaNo ratings yet
- Diagnostic and Terapi in Infection in Solid TransplantDocument19 pagesDiagnostic and Terapi in Infection in Solid TransplantretnoNo ratings yet
- Nej MR A 0804573Document9 pagesNej MR A 0804573saabNo ratings yet
- CNS Fungal InfectionDocument12 pagesCNS Fungal InfectionMuhammad Yusuf HanifNo ratings yet
- Neuroinfections Presentation Diagnosis and Treatment of Meningitis and EncephalitisDocument10 pagesNeuroinfections Presentation Diagnosis and Treatment of Meningitis and EncephalitisZarick SaenzNo ratings yet
- Treatment of Extrapulmonary Nontuberculous MycobacDocument11 pagesTreatment of Extrapulmonary Nontuberculous Mycobacjoao pereiraNo ratings yet
- Pathophysiology of Bacterial Meningitis: Mechanism(s) of Neuronal InjuryDocument9 pagesPathophysiology of Bacterial Meningitis: Mechanism(s) of Neuronal InjuryMedranoReyesLuisinNo ratings yet
- Bacterial Meningitis: EpidemiologyDocument4 pagesBacterial Meningitis: EpidemiologykapilNo ratings yet
- 5.infecciones Micóticas Del Sistema Nervioso CentralDocument13 pages5.infecciones Micóticas Del Sistema Nervioso CentralLiz NuñezNo ratings yet
- CNs InfectionDocument6 pagesCNs InfectionChefera AgaNo ratings yet
- Neisseria Meningitidis: General ConceptsDocument16 pagesNeisseria Meningitidis: General Conceptssomebody_maNo ratings yet
- 55 61 Brain AbscessDocument7 pages55 61 Brain AbscessNadia OktarinaNo ratings yet
- Chapter1: Introduction: E Coli and Other Gram-Negative Enteric Bacilli Such AsDocument6 pagesChapter1: Introduction: E Coli and Other Gram-Negative Enteric Bacilli Such AsAhmed RashadNo ratings yet
- Parikh2019 240528 175409Document5 pagesParikh2019 240528 175409cakepbanget1252No ratings yet
- Acutebacterialmeningitis: Current Review and Treatment UpdateDocument11 pagesAcutebacterialmeningitis: Current Review and Treatment UpdateWidya Niendy PrameswariiNo ratings yet
- Bacterial MeningitisDocument2 pagesBacterial MeningitisyanNo ratings yet
- Severe Meningoccal InfectionDocument17 pagesSevere Meningoccal Infectionmatias cisternaNo ratings yet
- Murray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryDocument17 pagesMurray A.d., Meyers A.D. Deep Neck Infections. Otolaryngology and Facial Plastic SurgeryAndi Karwana CiptaNo ratings yet
- Invasive Cryptococcal Meningitis Presenting As A Skull Base Mass in An Immunocompetent Host: A Case ReportDocument5 pagesInvasive Cryptococcal Meningitis Presenting As A Skull Base Mass in An Immunocompetent Host: A Case ReportAsep RiswandiNo ratings yet
- Presentation, Diagnosis, and Treatment of Meningitis and Encephalitis A Detailed ReviewDocument7 pagesPresentation, Diagnosis, and Treatment of Meningitis and Encephalitis A Detailed Reviewfitri dwiyantiNo ratings yet
- First Page PDFDocument1 pageFirst Page PDFMay Edogawa SuramuthNo ratings yet
- Roos, Karen L. Greenlee, John E. - Meningitis and EncephalitisDocument14 pagesRoos, Karen L. Greenlee, John E. - Meningitis and EncephalitisNadila Nur PratiwiNo ratings yet
- 2962-Article Text-9149-1-10-20230822Document7 pages2962-Article Text-9149-1-10-20230822Ragil Putri FritriyantiNo ratings yet
- The Importance of Mucormycosis Infections On Example of Rhino Orbital Cerebral MucormycosisDocument6 pagesThe Importance of Mucormycosis Infections On Example of Rhino Orbital Cerebral MucormycosisAlex OprisanNo ratings yet
- MeninigtisDocument5 pagesMeninigtisCatalina Constanza Mujica CovarrubiasNo ratings yet
- Meningococcemia Without Meningitis, Starting With Gastrointestinal Symptoms - Case ReportDocument5 pagesMeningococcemia Without Meningitis, Starting With Gastrointestinal Symptoms - Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Meningitis IN PDF PEDIATRICDocument14 pagesMeningitis IN PDF PEDIATRICCruz Roelia Ruiz SanchezNo ratings yet
- Preprints202309 0487 v1Document23 pagesPreprints202309 0487 v1Saul EstrellaNo ratings yet
- Imaging of Intracranial InfectionsDocument12 pagesImaging of Intracranial Infectionsrafael rocha novaesNo ratings yet
- Mold Infections of The Central Nervous SystemDocument15 pagesMold Infections of The Central Nervous SystemJohn TusselNo ratings yet
- Tuberculous Meningitis: A Narrative ReviewDocument10 pagesTuberculous Meningitis: A Narrative ReviewVyom BuchNo ratings yet
- Bacterial Infections of The Central Nervous System: Paul A. Lapenna, Do Karen L. Roos, MDDocument9 pagesBacterial Infections of The Central Nervous System: Paul A. Lapenna, Do Karen L. Roos, MDOver HidalgoNo ratings yet
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensFrom EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNo ratings yet
- Peptic Ulcer Disease: by Ntr/Jevr/Djs/AjisDocument14 pagesPeptic Ulcer Disease: by Ntr/Jevr/Djs/AjisJeriz Marie GamboaNo ratings yet
- Source For EcolecDocument35 pagesSource For EcolecJeriz Marie GamboaNo ratings yet
- Office of The Secretary: FirstDocument12 pagesOffice of The Secretary: FirstJeriz Marie GamboaNo ratings yet
- International Conference On Physical Activity and Obesity in Children: Summary Statement and RecommendationsDocument18 pagesInternational Conference On Physical Activity and Obesity in Children: Summary Statement and RecommendationsJeriz Marie GamboaNo ratings yet
- Hepatocellular Carcinoma (HCC)Document37 pagesHepatocellular Carcinoma (HCC)Jeriz Marie GamboaNo ratings yet
- The Human Body: An Orientation: Chapter 1Document88 pagesThe Human Body: An Orientation: Chapter 1Jeriz Marie GamboaNo ratings yet
- USTFMS ERB F01 Application FormDocument2 pagesUSTFMS ERB F01 Application FormJeriz Marie GamboaNo ratings yet
- Dating and CourtshipDocument12 pagesDating and CourtshipJeriz Marie GamboaNo ratings yet
- Chapter 12. BloodDocument23 pagesChapter 12. BloodJeriz Marie GamboaNo ratings yet
- Make Health Your "New High" Life Not DrugsDocument1 pageMake Health Your "New High" Life Not DrugsJeriz Marie GamboaNo ratings yet
- Human Genetic VariationDocument35 pagesHuman Genetic VariationJeriz Marie GamboaNo ratings yet
- Mitosis and Meiosis: Higher BiologyDocument16 pagesMitosis and Meiosis: Higher BiologyJeriz Marie GamboaNo ratings yet
- Mitosis New Cells: Results in 2 Identical Daughter CellsDocument26 pagesMitosis New Cells: Results in 2 Identical Daughter CellsJeriz Marie GamboaNo ratings yet
- Xoxo GossipDocument2 pagesXoxo GossipJeriz Marie GamboaNo ratings yet
- Environmental and Experimental Botany: R. Cruz de Carvalho, A. Bernardes Da Silva, C. Branquinho, J. Marques Da SilvaDocument5 pagesEnvironmental and Experimental Botany: R. Cruz de Carvalho, A. Bernardes Da Silva, C. Branquinho, J. Marques Da SilvaJeriz Marie GamboaNo ratings yet
- Ekonomiks: Maxine Yosobelle P. Cruz 10-Righteousness Ms - SardonDocument5 pagesEkonomiks: Maxine Yosobelle P. Cruz 10-Righteousness Ms - SardonJeriz Marie Gamboa0% (1)
- Lesson 28 Using The Internet and The World Wide Web: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument39 pagesLesson 28 Using The Internet and The World Wide Web: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Lesson 27 Communications and Collaboration: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument39 pagesLesson 27 Communications and Collaboration: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Lesson 26 Communication Services: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument36 pagesLesson 26 Communication Services: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Lesson 25 Network Fundamentals: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionDocument45 pagesLesson 25 Network Fundamentals: Computer Literacy Basics: A Comprehensive Guide To IC, 5 EditionJeriz Marie GamboaNo ratings yet
- Typhidot TestDocument1 pageTyphidot TestPre Cadet AcademyNo ratings yet
- Microbiology ReviewerDocument3 pagesMicrobiology ReviewerWendy Escalante100% (6)
- Animal Health and Livestock Services Act 2055 NepalDocument13 pagesAnimal Health and Livestock Services Act 2055 NepalSuraj SubediNo ratings yet
- (Libribook - Com) Introduction To Clinical Infectious Diseases A Problem-Based Approach 1st EditionDocument465 pages(Libribook - Com) Introduction To Clinical Infectious Diseases A Problem-Based Approach 1st EditionDaoud IssaNo ratings yet
- Rajiv Gandhi University: of Health SciencesDocument40 pagesRajiv Gandhi University: of Health SciencesAnirudhGopalNo ratings yet
- Bioterrorism and Biowarfare BTH 1Document6 pagesBioterrorism and Biowarfare BTH 1Akshita JainNo ratings yet
- ميكرو دبيDocument30 pagesميكرو دبيMohsen Haleem0% (1)
- HIV 1&2 Ab Cass Z09742 Rev01Document6 pagesHIV 1&2 Ab Cass Z09742 Rev01werther666No ratings yet
- UntitledDocument103 pagesUntitledjana whiteNo ratings yet
- Science of MicrobiologyDocument11 pagesScience of MicrobiologyJamaica M DanguecanNo ratings yet
- Bacteriocin Production by Lactic Acid Bacteria Encapsulated in Calcium Alginate BeadsDocument8 pagesBacteriocin Production by Lactic Acid Bacteria Encapsulated in Calcium Alginate BeadsangelicaaragonNo ratings yet
- Arbovirus Flash CardsDocument11 pagesArbovirus Flash CardsmfabzakNo ratings yet
- How To Transfer A Mobilizable Plasmid From A Cell Without A Conjugative Plasmid?Document14 pagesHow To Transfer A Mobilizable Plasmid From A Cell Without A Conjugative Plasmid?m86544422No ratings yet
- Virulence Factors MycoplasmDocument9 pagesVirulence Factors MycoplasmAlan GarcíaNo ratings yet
- Limitations Results: Congenital Syphilis: Management Dilemmas Using Reverse ScreeningDocument1 pageLimitations Results: Congenital Syphilis: Management Dilemmas Using Reverse ScreeningFaye Cabotaje LinganNo ratings yet
- Gabinete - 2A - Module 1 AssessmentDocument3 pagesGabinete - 2A - Module 1 AssessmentNathaniel GABINETENo ratings yet
- Biggy AgarDocument2 pagesBiggy AgarMatei BogdanNo ratings yet
- Intestinal and Commensal AmoebaDocument9 pagesIntestinal and Commensal AmoebaFuture TrekingNo ratings yet
- BurnettDocument4 pagesBurnettJean CotteNo ratings yet
- Principles of Antimicrobial Therapy 2022Document33 pagesPrinciples of Antimicrobial Therapy 2022Puteri Nursyamimi Mohd SabilanNo ratings yet
- Rev 6. DAFTAR PUSTAKA 19novDocument8 pagesRev 6. DAFTAR PUSTAKA 19novSams SriningsihNo ratings yet
- Microbiology Laboratory PrelimsDocument8 pagesMicrobiology Laboratory PrelimsMARIA ISABILLE DUALLO MUSONGNo ratings yet
- Literature ReviewDocument2 pagesLiterature ReviewFaith Arpon AbogandaNo ratings yet
- Deferrals For Blood DonationDocument2 pagesDeferrals For Blood DonationShane AñoNo ratings yet
- Reference: Product: Technical Data Sheet: Legionella GVPC Supplement IsoDocument2 pagesReference: Product: Technical Data Sheet: Legionella GVPC Supplement IsoSLN TESTING LABORATORYNo ratings yet
- Basic ParasitologiDocument23 pagesBasic ParasitologiNur'Azmi AyuningtyasNo ratings yet
- Pathogenesis TBDocument39 pagesPathogenesis TBGede Eka Putra NugrahaNo ratings yet
- Philippine Adult Immunization Recommendation 2017 PDFDocument2 pagesPhilippine Adult Immunization Recommendation 2017 PDFLinius CruzNo ratings yet
- CDC's HIV Infection Through Oral Sex, Fact SheetDocument2 pagesCDC's HIV Infection Through Oral Sex, Fact SheetCésar E. ConcepciónNo ratings yet