Professional Documents
Culture Documents
2022 Clinthera S1T4 Copd PDF
2022 Clinthera S1T4 Copd PDF
Uploaded by
medicoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2022 Clinthera S1T4 Copd PDF
2022 Clinthera S1T4 Copd PDF
Uploaded by
medicoCopyright:
Available Formats
CHRONIC OBSTRUCTIVE
PULMONARY DISEASE CLINICAL THERAPEUTICS| PRELIMS (1st Sem)
Dr. Magnolia Reyes
OUTLINE C. WHAT ARE THE ACCESSORY MUSCLES OF
I. Case RESPIRATION?
II. Case Discussion It refers to those that assist, but do not play a primary
III. Sample Interview and Patient’s Picture
IV. Case Questions role, in breathing. Use of these while at rest is often interpreted
V. Comprehension Questions as a sign of respiratory distress.
VI. Clinical Pearls
VII. References
The accessory inspiratory muscles are the
VIII. Appendix sternocleidomastoid*, the scalenus anterior, medius, and
posterior*, the pectoralis major and minor, the inferior fibres of
I. CASE serratus anterior and latissimus dorsi, the serratus posterior
A 55-year-old male comes to the clinic because of superior may help in inspiration, also the iliocostalis cervicis.
shortness of breath. He has experienced mild dyspnea on Technically. any muscle attached to the upper limb and the
exertion for a few years but more recently he has noted thoracic cage can act as an accessory muscle of inspiration
worsening SOB with minimal exercise and onset of dyspnea at through reverse muscle action (muscle work from distal to
rest. He has difficulty of reclining as a result, he spends the proximal).
night sitting up in a chair trying to sleep. He reports a cough The accessory expiratory muscles are the abdominal
with production of yellowish-brown sputum every morning muscles: rectus abdominis, external oblique, internal oblique,
throughout the year. He denies chest pain, fever, chills or lower and transversus abdominis. And in the thoracolumbar region;
extremity edema. He has smoked about 2 packs of cigarette the lowest fibres of iliocostalis and longissimus, the serratus
per day since age 15. He does not drink alcohol. posterior inferior, and quadratus lumborum.
A few months ago, he went to a clinic for evaluation of D. WHY IS THE PATIENT USING HIS ACCESSORY
his symptoms and received prescriptions for some inhalers MUSCLES?
which names he cannot remember. In emphysema, the alveoli are dilated, increasing their
oxygen demand. Thus, accessory muscles of respiration are
PE: BP 136/86, HR 96bpm, RR 28bpm, T 37℃
used.
He is sitting in a chair, leaning forward with his arms
braced on his knees. He appears uncomfortable with labored E. WHAT WAS HEARD ON HIS CHEST EXAM?
respirations and cyanotic lips. He is using accessory muscles “… wheezes and rhonchi bilaterally with no crackles”
of respiration, and chest exam reveals wheezed and rhonchi Rhonchi?
bilaterally, but no crackles. The AP diameter of the chest wall o Continuous low pitched, rattling lung sounds
appears increased and inward movement of the lower rib cage. that often resemble snoring. Obstruction or
Heart is normal but with distant heart sounds. Normal jugular secretions in larger airways are frequent
venous pressure of his extremities shows no cyanosis, edema causes of rhonchi.
or clubbing. o Heard on expiration
Wheezes?
II. CASE DISCUSSION o Wheezing is a high-pitched, coarse whistling
A. WHAT ARE THE SALIENT POINTS OF THIS CASE? sound when you breathe. The whistling
Mild dyspnea on exertion sound happens when air moves through
Shortness of breath with minimal exercise narrowed airways, much like the way a
Onset of dyspnea at rest whistle or flute makes music.
Difficulty of reclining o The most common causes are COPD and
Cough with production of yellowish-brown sputum asthma.
every morning throughout the year o Heard during inspiration and/or expiration,
2 packs of cigarette per day since age 15 usually louder on the latter
Crackles? “Rales”
B. WHAT IS THE PICTURE OF THE PATIENT?
o Occur when airway contains fluid
Has a difficulty in breathing
o Heard on inspiration
In “tripod position”: sitting leaning forward with hands
supported anteriorly on the knees, a posture F. WHAT IS THE PATHOPHYSIOLOGY THERE?
frequently assumed by patients in respiratory distress When emphysema develops, the alveoli and lung
RR: 28 bmp (Normal: 12-20 bmp) tissue are destroyed. With this damage, the alveoli cannot
Chest exam reveals wheezes and rhonchi bilaterally support the bronchial tubes. The tubes collapse and cause an
The AP diameter of the chest wall appears increased “obstruction” (a blockage), which traps air inside the lungs. Too
and inward movement of the lower rib cage. “barrel much air trapped in the lungs can give some patients a barrel-
chest” *can be a sign of underlying condition like chested appearance.
COPD
o What does it denote? Emphysema G. LUNG LOBES
Right – 3; (superior) upper, middle, (inferior) lower
lobes
Left – 2; (superior) upper, (inferior) lower lobes
FALSIS / ROJO / SALAGUBANG / QUIGAO 1 of 5
Prelims (1st Sem) Chronic Obstructive Pulmonary DIsease
Dr. Magnolia Reyes
CLINICAL THERAPEUTICS· September 17, 2020
H. WHAT IS IN THE PATIENT’S HISTORY THAT IS VERY time, α1-antitrypsin, a plasma protein that normally
IMPORTANT? inactivates elastase and other proteases, is itself
The patient is a smoker since he was 15 years old inhibited. The α1-antitrypsin is inactivated by oxygen
How many packs per day? (in pack years) radicals, and these are released by the leukocytes.
The final result is a protease antiprotease imbalance
Formula:
with increased destruction of lung tissue.
C. WHAT IS PFT? SPIROMETRY?
Pulmonary function tests (PFTs)
o Group of tests that measure breathing and
how well the lungs are functioning. Complete
PFTs comprise respiratory tests of
Computation: spirometry, lung volumes, and diffusion
o 1 pack of cigarette contains 20 sticks which evaluates respiratory flow volumes
o 40 sticks per day x 40 years of smoking and flow rates to assess pulmonary function.
20 (see appendices A and B)
o 1600/ 20 = 80 pack years Spirometry
Smoking is a risk factor of having his current condition o Method of evaluating respiratory flow
volumes and flow rates to assess pulmonary
III. SAMPLE INTERVIEW AND PATIENT’S PICTURE function. It is the most basic, inexpensive,
Doctor: Ano ho bang nangyari sa inyo? 55 years old na ho widely valuable pulmonary function test to
kayo. Ano po ba ang trabaho niyo noon? Kailan po nag- diagnose pulmonary diseases.
umpisa iyan?
D. WHAT IS FORCED VITAL CAPACITY, FORCED
Patient: Madali lang po akong mapagod pag may EXPIRATORY VOLUME IN 1 SECONDS, FEV/FVC1?
ginagawa. Pagkatapos po ngayon, kahit FVC – Forced vital capacity
naglalakad nahihirapan na po ako. Ngayon po, hindi Total volume of air expired after full inspiration. FVC is
reduced in restrictive lung disease. Patients with
na ako makahinga kahit na wala akong ginagawa.
obstructive lung disease usually have normal FVC.
Note the progression of the disease process – from
SOB to mild dyspnea on exertion to dyspnea at rest. Try to FEV1 – Forced expiratory volume in one second
picture what is happening to the patient, not only at that Volume of air expired in the first second during
maximal expiratory effort.
present moment.
FEV1 is reduced in
Where does he sleep? Sa chair kasi hindi both obstructive lung disease (increased airway
nakakahinga „pag diretso. resistance) and restrictive lung disease (low vital
capacity)
What medicine was given? Unrecalled inhalers
Did the patient get well with the medicine given? No, FEV1/ FVC ratio – Percentage of the vital capacity that is
because the patient returned for consultation expired during the first second
What was noted on the heart exam? Normal heart but of maximal effort, reduced in obstructive lung disease.
with distant heart sound
What if JVP is normal? Case might be a respiratory E. WHAT IS OBSTRUCTIVE LUNG DISEASE?
problem, not cardiac RESTRICTIVE LUNG DISEASE?
What if JVP is high, there could be CHF Obstructive lung Restrictive lung disease
disease
What was seen on the extremities? No cyanosis,
Increase in resistance Reduced expansion of
edema, and clubbing
to airflow due to lung parenchyma and decreased
Findings only include the pulmonary but is the case partial or complete total lung capacity (there is
compensated? Yes, because there is no cyanosis on obstruction at any difficulty in taking air inside the
the extremities, only on the lips level from the lungs d/t loss of elasticity)
trachea and larger
IV. CASE QUESTIONS bronchi to the terminal
A. WHAT IS YOUR DIAGNOSIS? and respiratory
COPD (Emphysema) with acute exacerbations bronchioles (px
experience shortness
B. WHAT IS THE ETIOLOGY OF YOUR DIAGNOSIS? of breath d/t difficulty
Inhalation injury like prolonged cigarette smoking in exhaling air from the
o Airflow limitation due to chronic inflammation lungs
noxious particles of cigarette Decreased FEV Decreased lung volumes
The smoke causes an increase in the number of 1 <80% of Decreased VC
pulmonary alveolar macrophages, and these predicted Decreased TLC
macrophages release a chemical substance that FEV1/FVC <0.7 FEV1/FVC is normal
attracts leukocytes to the lungs. The leukocytes in TLC usually
turn release proteases including elastase, which normal or
attacks the elastic tissue in the lungs. At the same increased
FALSIS / ROJO / SALAGUBANG / QUIGAO 2 of 5
Prelims (1st Sem) Chronic Obstructive Pulmonary DIsease
Dr. Magnolia Reyes
CLINICAL THERAPEUTICS· September 17, 2020
Diffusion capacity
decreased I. WHAT IS YOUR DIAGNOSTICS?
Bronchiectasis (ie, Extrapulmonary: Pulmonary: ABG to assess oxygenation and acid-base status.
cystic fibrosis) poor breathing poor lung
Asthma mechanics expansion J. WHAT IS YOUR TREATMENT AND RECOMMENDED
Bronchitis (chronic) Poliomyelitis Pneumonia MANAGEMENT AT THIS POINT?
Emphysema Myasthenia gravis ARDS Ensure adequate oxygenation with target oxygenation
Scoliosis Pulmonary of 90-92% (watch out for CO2 retention), via nasal
edema cannula
Interstitial Bronchodilators (beta-agonist and anticholinergic
fibrosis agents) administered via
Obstructive lung disease: Chronic pulmonary disorder handheld nebulizers
that is characterized by a disproportional decrease in Steroids for airway inflammation
maximal airflow from the lung in relation to maximal Systemic glucocorticoids to accelerate the rate of
volume that can be displaced from the lung. Most common improvement in lung function
types of obstructive lung disease are asthma and COPD. Antibiotics if suspicious of respiratory infection
Restrictive lung disease: Chronic pulmonary disorder *Consider surgical treatments like lung reduction
characterized by low lung volumes because of alterations surgery and segmentectomy/lobectomy
of either the lung parenchyma (intrinsic), or chest wall,
pleura, or respiratory muscles (extrinsic). V. COMPREHENSION QUESTIONS
1. Which of the following is the most likely physical examination
F. WHAT IS COPD? findings in a patient with COPD?
COPD is a chronic airflow obstruction caused by A. Diffuse expiratory wheezing
chronic bronchitis or emphysema characterized by persistent B. Clubbing of the fingers
airflow limitation that is usually progressive and associated with C. Bibasilar inspiratory crackles with increased jugular venous
enhanced chronic inflammatory response in the lungs to the pressure (JVP)
noxious particles and gases. D. Inspiratory stridor
FEV1/ FVC ratio of less than 70 E. Third heart sound
Severity on spirometry is based on FEV 1/ FEV1 ratio
vs. predicted 2. A 56-year-old woman admits to a 60-pack-year smoking
o >80% = mild disease history. She complains of fatigue and dyspnea with minimal
o 50% to 80% = moderate exertion, and a cough that is productive each morning. Which
o 30% to 50% = severe of the following is the most likely finding in this patient?
o < 30% = very severe disease A. Higher diffusing capacity of lung for carbon monoxide
(DLCO)
G. WHAT IS RESPIRATORY DISTRESS? B. Decreased residual volume
It is a clinical syndrome of progressive respiratory C. Normal to slightly increased FEV1
insufficiency caused by diffuse alveolar damage with damage D. Decreased FEV1/ FVC
to hyaline membrane lining the walls, edema, scattered E. Decreased FVC
neutrophils and macrophages, and epithelial necrosis.
This occurs when fluid builds up in the tiny, elastic air 3. Which of the following therapies is most likely to provide the
sacs (alveoli) in your lungs keeping it from filling with enough greatest benefit to a patient with chronic stable emphysema
air causing less oxygen to reach the bloodstream. and a resting oxygen saturation of 86%?
A. Inhaled tiotropium daily
H. WHAT IS YOUR EMPHYSEMA? CHRONIC B. Inhaled albuterol as needed
BRONCHITIS? C. Oral prednisone daily
Emphysema Chronic bronchitis D. Supplemental oxygen used at night
COPD component that is COPD component that is E. Supplemental oxygen used continuously
diagnosed pathologically with diagnosed clinically. It
irreversible enlargement of characterized by excessive VI. CLINICAL PEARLS
the airspaces distal to the secretion of bronchial mucus Patients with obstructive lung disease have air flow
terminal bronchiole, and productive cough for limitation on expiration (reduced FEV1/FVC), whereas
accompanied by destruction 3 months or more in at least 2 patients with restrictive lung disease have difficulty in
of their walls without obvious consecutive years in the expanding their lung volumes in response to exercise
fibrosis. absence of any other disease (reduced TLC).
that might account for this The mainstay for treatment of chronic obstructive
symptom pulmonary disease exacerbations includes
Smoking and inhaled Dominant pathologic features bronchodilators, oxygen, and glucocorticoids, as well
pollutants cause ongoing are mucus hypersecretion as antibiotics if infection is suspected.
accumulations of and persistent inflammation. Controlled supplemental oxygen along with positive-
inflammatory cells, releasing pressure mask ventilation (bilevel positive airway
elastases and oxidants, which pressure) may prevent respiratory failure requiring
destroy the alveolar walls endotracheal intubation.
*most patients with emphysema also have some degree of Smoking cessation and supplemental oxygen to treat
chronic bronchitis, which is to be expected since cigarette chronic hypoxemia are the only medical therapies
smoking is an underlying risk factor for both
FALSIS / ROJO / SALAGUBANG / QUIGAO 3 of 5
Prelims (1st Sem) Chronic Obstructive Pulmonary DIsease
Dr. Magnolia Reyes
CLINICAL THERAPEUTICS· September 17, 2020
shown to decrease mortality among persons with
chronic obstructive pulmonary disease.
In both obstructive and restrictive lung disease, the
FEV1 is decreased, the FEV1/FVC is decreased in
obstructive processes and normal in restrictive
processes.
The hallmark of restrictive lung disease is decreased
lung capacities, particularly the TLC but also the VC.
References
Case Files Ⓡ Internal Medicine (5 Edition)
th
Doc Reyes’ ppt and lecture notes
th
Moore’s Clinically Oriented Anatomy (7 Edition)
FALSIS / ROJO / SALAGUBANG / QUIGAO 4 of 5
Prelims (1st Sem) Chronic Obstructive Pulmonary DIsease
Dr. Magnolia Reyes
CLINICAL THERAPEUTICS· September 17, 2020
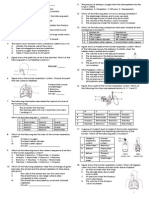
Appendix A
Appendix B
FALSIS / ROJO / SALAGUBANG / QUIGAO 5 of 5
You might also like
- Normal Physical Changes in Older AdultDocument47 pagesNormal Physical Changes in Older AdultBushra EjazNo ratings yet
- Jarvis Chapter 18 Study GuideDocument5 pagesJarvis Chapter 18 Study GuideEmily Cheng100% (2)
- Thoracic Radiology For The Small Animal PractitionerDocument149 pagesThoracic Radiology For The Small Animal PractitionerPaulo Matias Filho100% (10)
- Respiratory Assessment & DiagnosticsDocument9 pagesRespiratory Assessment & DiagnosticsAngellene GraceNo ratings yet
- NCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsDocument7 pagesNCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsViviene Faye FombuenaNo ratings yet
- Chest and Lungs ExaminationDocument75 pagesChest and Lungs Examinationdhainey100% (10)
- Final Death Note - Compre NotesDocument1,550 pagesFinal Death Note - Compre NotesSteph TabasaNo ratings yet
- Lungs and ThoracicDocument66 pagesLungs and ThoracicJoyce Jacobe0% (1)
- Chest and LungsDocument49 pagesChest and LungsChala KeneNo ratings yet
- Topics:: A. Upper Airways B. Lower AirwaysDocument10 pagesTopics:: A. Upper Airways B. Lower AirwaysAya CalauToNo ratings yet
- 316 RevalidaDocument14 pages316 RevalidaPAOLA LUZ CRUZNo ratings yet
- A.Chest Wall Abnormalities: 1.) Respiratory SystemDocument6 pagesA.Chest Wall Abnormalities: 1.) Respiratory SystemAlhadzra AlihNo ratings yet
- Chest ExaminationDocument14 pagesChest Examinationsajad abasewNo ratings yet
- Decompression Pulmonary Barotrauma DPBDocument19 pagesDecompression Pulmonary Barotrauma DPBRicardoNo ratings yet
- Respiratory Sounds: by Oluwaseun OlaiyaDocument16 pagesRespiratory Sounds: by Oluwaseun OlaiyaOlaiya OluwaseunNo ratings yet
- Respiratory Disorders & TB in Children (Part I and Ii) - Dr. MendozaDocument17 pagesRespiratory Disorders & TB in Children (Part I and Ii) - Dr. MendozaRea Dominique CabanillaNo ratings yet
- Block B Overview of Respiratory Exam PresentationDocument5 pagesBlock B Overview of Respiratory Exam PresentationKim Adarem Joy ManimtimNo ratings yet
- Pi Is 0960982216310557Document2 pagesPi Is 0960982216310557Ridski D. MiruNo ratings yet
- NCM 112 NotesDocument6 pagesNCM 112 NotesKatrina Jhane MercadoNo ratings yet
- Ha Lab ReviewerDocument3 pagesHa Lab ReviewerzabalaiiirogeliopaclibarNo ratings yet
- Physical Assessment Part 2Document19 pagesPhysical Assessment Part 2Isabel DizonNo ratings yet
- Respiratory SystemDocument38 pagesRespiratory Systemjsreyes.402No ratings yet
- Assignment No 4Document7 pagesAssignment No 4Ana Belle BautistaNo ratings yet
- Respiratory Examination - Protected 1Document4 pagesRespiratory Examination - Protected 1anirudh811100% (1)
- Ncma113-Respiratory and Nursing CareDocument5 pagesNcma113-Respiratory and Nursing Careroldanmarygrace023No ratings yet
- MVS Pulmonary AuscultationDocument8 pagesMVS Pulmonary Auscultationvashini9151No ratings yet
- Shortness of Breath NotesDocument7 pagesShortness of Breath NotesChananNo ratings yet
- Respiratory System Assessment: Other SystemsDocument4 pagesRespiratory System Assessment: Other SystemsChetan KumarNo ratings yet
- Respiratory, Assessment, Diseases.Document4 pagesRespiratory, Assessment, Diseases.ninoNo ratings yet
- 8 Lung Auscultation Points and SoundsDocument11 pages8 Lung Auscultation Points and SoundsCHARIEMAE CA�AZARES100% (1)
- COPD - Case PresentationDocument68 pagesCOPD - Case PresentationJaslir MendozaNo ratings yet
- The Respiratory System and Its DisordersDocument16 pagesThe Respiratory System and Its DisordersZea Leyan J. LopezNo ratings yet
- K14 - Sesak Dan Pneumonia Pada AnakDocument125 pagesK14 - Sesak Dan Pneumonia Pada AnakBintang FortunaNo ratings yet
- Pediatric Respiratory Anatomy: Course Tak 5 Dula Stephanie PDocument5 pagesPediatric Respiratory Anatomy: Course Tak 5 Dula Stephanie PSteph DulaNo ratings yet
- Respiratory ENT Assessment GuideDocument3 pagesRespiratory ENT Assessment GuidepriyaNo ratings yet
- 3 RespDocument81 pages3 RespashuNo ratings yet
- DR Amsalu Bekele Ass - Professor of Medicine Head of Chest Unit Department of Internal Medicine Addis Ababa University, School of Medicine Addis Ababa, EthiopiaDocument81 pagesDR Amsalu Bekele Ass - Professor of Medicine Head of Chest Unit Department of Internal Medicine Addis Ababa University, School of Medicine Addis Ababa, EthiopiaBethelhem BirhanuNo ratings yet
- AnapiDocument4 pagesAnapianastaziaarcayeraNo ratings yet
- Bronchial Asthma Case Pres ExplanationDocument6 pagesBronchial Asthma Case Pres ExplanationYoongiNo ratings yet
- Cardio AssessementDocument9 pagesCardio AssessementPoonam soniNo ratings yet
- RESPIRATIONDocument7 pagesRESPIRATIONnjayrestNo ratings yet
- The Respiratory SystemDocument61 pagesThe Respiratory SystemLuna JadeNo ratings yet
- Thoracic and Lung Assessment: Physical Examination of The Thorax and The LungsDocument16 pagesThoracic and Lung Assessment: Physical Examination of The Thorax and The Lungsshannon c. lewis100% (1)
- Breath Sounds: ConsiderationsDocument10 pagesBreath Sounds: ConsiderationsKarl RobleNo ratings yet
- Respiratory EmergenciesDocument30 pagesRespiratory EmergenciesNovriefta NugrahaNo ratings yet
- Lecture 3 RS12015 PDFDocument136 pagesLecture 3 RS12015 PDFDaniel AshooriNo ratings yet
- Respiratory AssessmentDocument54 pagesRespiratory Assessmentraima ayazNo ratings yet
- PL1263Document28 pagesPL1263Mirjana MandićNo ratings yet
- Assessment of Lung and ChestDocument50 pagesAssessment of Lung and ChestAbdurehman Ayele100% (1)
- Unit 5.2 RespirationsDocument5 pagesUnit 5.2 RespirationsAssasination ClassroomNo ratings yet
- Michigan EMS Expo 2004: Bob Page, AAS, NREMT-P, CCEMT-P, I/CDocument16 pagesMichigan EMS Expo 2004: Bob Page, AAS, NREMT-P, CCEMT-P, I/CJefferson FloresNo ratings yet
- Michigan EMS Expo 2004: Bob Page, AAS, NREMT-P, CCEMT-P, I/CDocument15 pagesMichigan EMS Expo 2004: Bob Page, AAS, NREMT-P, CCEMT-P, I/Cbash021No ratings yet
- The Respiratory SystemDocument5 pagesThe Respiratory SystemRyan TimogNo ratings yet
- STUDY GUIDE 2 OXYGENATION Operaña EllayzaDocument5 pagesSTUDY GUIDE 2 OXYGENATION Operaña EllayzaOPERAñA ELLAYZA RB DECANONo ratings yet
- Physiological Overview in Relation To PracticeDocument52 pagesPhysiological Overview in Relation To PracticedrkhaledassemNo ratings yet
- Physical Diagnoses: Respiratory SystemDocument72 pagesPhysical Diagnoses: Respiratory SystemAmanuel MaruNo ratings yet
- BLS CPR Part 2Document30 pagesBLS CPR Part 2yhunabbyNo ratings yet
- Oxygenation 1Document155 pagesOxygenation 1Khatlen BagaresNo ratings yet
- Diagnosis of Dyspnea 2011 VTDocument77 pagesDiagnosis of Dyspnea 2011 VTRovanNo ratings yet
- Physical Examinations Respiratory System: InspectionDocument5 pagesPhysical Examinations Respiratory System: InspectionAzizan HannyNo ratings yet
- Iyengar Yoga For The Respiratory System-2020 PDFDocument13 pagesIyengar Yoga For The Respiratory System-2020 PDFSlice LeNo ratings yet
- AbortionDocument39 pagesAbortionmedico100% (1)
- Pediatric History and PE - Dr. LeonesDocument4 pagesPediatric History and PE - Dr. LeonesmedicoNo ratings yet
- Case 5Document28 pagesCase 5medicoNo ratings yet
- Early Pregnancy Complications: Ectopic Pregnancy Gestational Trophoblastic Disease Ji Aggasid, JanniecelDocument60 pagesEarly Pregnancy Complications: Ectopic Pregnancy Gestational Trophoblastic Disease Ji Aggasid, JanniecelmedicoNo ratings yet
- 2022 Ob2 s1t17 Fetal Growth DisordersDocument10 pages2022 Ob2 s1t17 Fetal Growth DisordersmedicoNo ratings yet
- 2022 Anesth s1t10 Local AnestheticsDocument4 pages2022 Anesth s1t10 Local AnestheticsmedicoNo ratings yet
- 2022 Anesth s1t8 Intravenous Anesthesia and OpioidsDocument10 pages2022 Anesth s1t8 Intravenous Anesthesia and OpioidsmedicoNo ratings yet
- 2022 Clinthera S1T5 Aki PDFDocument4 pages2022 Clinthera S1T5 Aki PDFmedicoNo ratings yet
- 2022 Ob2 s1t15 Preterm Labor and BirthDocument12 pages2022 Ob2 s1t15 Preterm Labor and BirthmedicoNo ratings yet
- 2022 Clinthera S1T2 Hypercholesterolemia PDFDocument7 pages2022 Clinthera S1T2 Hypercholesterolemia PDFmedicoNo ratings yet
- 2022 Clinthera S1T3 Ami PDFDocument6 pages2022 Clinthera S1T3 Ami PDFmedicoNo ratings yet
- Chest Pyhsiotherapy - 052329Document12 pagesChest Pyhsiotherapy - 052329Ahmed MansourNo ratings yet
- JUNE 2017: Gauteng Department of Education Provincial ExaminationDocument14 pagesJUNE 2017: Gauteng Department of Education Provincial ExaminationGoce KuzeskiNo ratings yet
- 2011 Krok Bank TherapyDocument32 pages2011 Krok Bank TherapyRahul PatilNo ratings yet
- 02 2018 Biomedical Instrumentation - Measurement of RespirationDocument28 pages02 2018 Biomedical Instrumentation - Measurement of Respirationviki mikiNo ratings yet
- 1406 IAL Biology WBI05 01 Scientific ArticleDocument8 pages1406 IAL Biology WBI05 01 Scientific ArticleMohamed NaaifNo ratings yet
- Cambridge International AS & A Level: Biology 9700/13Document20 pagesCambridge International AS & A Level: Biology 9700/13shabanaNo ratings yet
- Pedia Reporting 2ND Yr 2ND SemDocument109 pagesPedia Reporting 2ND Yr 2ND SemWenalyn Grace Abella LlavanNo ratings yet
- 1.1 Human Breathing MechanismDocument2 pages1.1 Human Breathing Mechanismieya_yNo ratings yet
- Pulmonary Function TestsDocument38 pagesPulmonary Function TestsMohamedSalahNo ratings yet
- The Respiratory SystemDocument147 pagesThe Respiratory SystemAya SobhiNo ratings yet
- Stress and Strain Within The Lung: ReviewDocument6 pagesStress and Strain Within The Lung: ReviewdanielNo ratings yet
- Measurement of Respiratory Compliance - Deranged PhysiologyDocument9 pagesMeasurement of Respiratory Compliance - Deranged PhysiologyJose Morato E FlavianeNo ratings yet
- Grade 9 Science 1st Quarter 2016Document9 pagesGrade 9 Science 1st Quarter 2016Yang PoreberNo ratings yet
- Permissive Hypercapnia: What To Remember: ReviewDocument12 pagesPermissive Hypercapnia: What To Remember: ReviewNataly Osorio MarínNo ratings yet
- Case Presentation Final2Document36 pagesCase Presentation Final2zerpthederpNo ratings yet
- Chicken Anatomy & PhysiologyDocument26 pagesChicken Anatomy & PhysiologySanjeev ChaudharyNo ratings yet
- Course Task 3Document2 pagesCourse Task 3Geraldine MaeNo ratings yet
- Exploring The Science of Marma - An Ancient Healing Technique - Part 4: Marma TherapyDocument17 pagesExploring The Science of Marma - An Ancient Healing Technique - Part 4: Marma TherapyIrina MartelNo ratings yet
- CPL Human Performance and Limitations ManualDocument150 pagesCPL Human Performance and Limitations ManualChina LalaukhadkaNo ratings yet
- Bronchial Asthma Case Write UpDocument5 pagesBronchial Asthma Case Write UpEry FarishNo ratings yet
- 3rd Year Cardio Lesson Plan 1Document139 pages3rd Year Cardio Lesson Plan 1Jeffery Samuel100% (2)
- Chemical Toxicology-OKDocument93 pagesChemical Toxicology-OKScott PilgrimNo ratings yet
- Recurrent/Persistent Pneumonia Among Children in Upper EgyptDocument14 pagesRecurrent/Persistent Pneumonia Among Children in Upper EgyptLaila Ninda ShofiaNo ratings yet
- Oxygen InsufficiencyDocument35 pagesOxygen InsufficiencyTINJU12345673% (11)
- Bony ThoraxDocument6 pagesBony ThoraxKaren LaureanoNo ratings yet
- Cardiovascular System NotesDocument9 pagesCardiovascular System NotesMeleen ConstantinoNo ratings yet
- Chest and Lungs - Supplementary Handout - Laboratory SessionDocument7 pagesChest and Lungs - Supplementary Handout - Laboratory SessionPaul AculladorNo ratings yet
- Interpretando RX PediatricoDocument10 pagesInterpretando RX PediatricosuzukishareNo ratings yet