Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
90 viewsAntiamoebic & Other Antiprotozoal Drugs
Antiamoebic & Other Antiprotozoal Drugs
Uploaded by
Amit ShahThis document discusses drugs used to treat protozoal infections, specifically amoebiasis and giardiasis. It provides details on the mechanisms of action, pharmacokinetics, clinical uses, dosages and adverse effects of various antiamebic and antiparasitic drugs. The main drugs discussed are metronidazole, tinidazole, emetine, diloxanide furoate, nitazoxanide, and tetracyclines for treating amoebiasis. For giardiasis, the recommended first-line treatments include metronidazole, tinidazole, secnidazole, nitazoxanide and quiniodochlor. Guidelines
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Quiz PharmaDocument6 pagesQuiz PharmaMary Grace Bañes100% (1)
- Anti Amoebic DrugsDocument17 pagesAnti Amoebic DrugsSaurabh Gautam100% (2)
- Treatment of A Moe Bias Is Giardia SisDocument27 pagesTreatment of A Moe Bias Is Giardia SisLuthfi Hilman TaufikNo ratings yet
- Treatment of Amoebiasis & GiardiasisDocument27 pagesTreatment of Amoebiasis & GiardiasisElda LizmaNo ratings yet
- ANTIAMUBADocument20 pagesANTIAMUBAAspar RafiqNo ratings yet
- Farmakologi Obat Kusta Dan Antiparasit 2015Document84 pagesFarmakologi Obat Kusta Dan Antiparasit 2015Alex FerdinandNo ratings yet
- (Udah) AntiamubaDocument20 pages(Udah) AntiamubaMohammad Rizki PratamaNo ratings yet
- Antiprotozoal Drugs: DR Manik GhadlingeDocument63 pagesAntiprotozoal Drugs: DR Manik GhadlingeEscitalopram 5mgNo ratings yet
- Anti-Protozoal DrugsDocument38 pagesAnti-Protozoal DrugsMahnoor AbidNo ratings yet
- Keterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugDocument7 pagesKeterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugEm Hernandez AranaNo ratings yet
- PROBLEM 2B - VarlaDocument50 pagesPROBLEM 2B - VarlavarlavarleyNo ratings yet
- Chemotherapy of Helminth Infections: DR - Rathnakar U.PDocument39 pagesChemotherapy of Helminth Infections: DR - Rathnakar U.PDr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- Anti Parasites Blok 3.2Document46 pagesAnti Parasites Blok 3.2Alda Herlen Kalkarina BangunNo ratings yet
- 1 Final Drug Study Gastro Jan26-27, 2023Document13 pages1 Final Drug Study Gastro Jan26-27, 2023Wynne GriffinNo ratings yet
- Ameobiasis and Giardiasis: S.Ravindra Babu Associate ProfessorDocument38 pagesAmeobiasis and Giardiasis: S.Ravindra Babu Associate Professorkamsu JyothsnaNo ratings yet
- Antiproto & AnthelminticsDocument57 pagesAntiproto & AnthelminticsDrMohan GuptaNo ratings yet
- Metronidazole: (Me Troe Ni' Da Zole)Document4 pagesMetronidazole: (Me Troe Ni' Da Zole)Wino SantosNo ratings yet
- Domperidone Uses:: Nausea and Vomiting BreastDocument6 pagesDomperidone Uses:: Nausea and Vomiting BreastAnna Charissa Arcales HoraNo ratings yet
- Pharmacotherapy of Peptic Ulcer: DR ZareenDocument50 pagesPharmacotherapy of Peptic Ulcer: DR ZareenGareth BaleNo ratings yet
- Pharmacotherapy of Peptic Ulcer: DR ZareenDocument50 pagesPharmacotherapy of Peptic Ulcer: DR ZareenGareth BaleNo ratings yet
- L 1+2 - Urinary Tract InfectinsDocument33 pagesL 1+2 - Urinary Tract InfectinsMunibaNo ratings yet
- Urinary Germicides PharmaDocument11 pagesUrinary Germicides PharmaMaria Pina Barbado PonceNo ratings yet
- Pharma - Drugs Affecting Git MotilityDocument6 pagesPharma - Drugs Affecting Git MotilityBobet ReñaNo ratings yet
- Chemotherapy of Protozoal InfectionsDocument34 pagesChemotherapy of Protozoal InfectionsSri RamNo ratings yet
- Group-3-Ward-Class 20240213 182023 0000Document31 pagesGroup-3-Ward-Class 20240213 182023 0000Hanna CarsanoNo ratings yet
- CefaclorDocument3 pagesCefaclorAyah PaasaNo ratings yet
- Anti DiarrhoealsDocument37 pagesAnti DiarrhoealsCrome operatorNo ratings yet
- Anti-Protozoal Drugs: Dr. Mozna TalpurDocument25 pagesAnti-Protozoal Drugs: Dr. Mozna TalpurShahid Hameed100% (1)
- Farmakologi AntiparasitDocument119 pagesFarmakologi AntiparasitFitri Sri WulandariNo ratings yet
- DrugsDocument8 pagesDrugsShizuka Marycris AmaneNo ratings yet
- Pharmacological SheetDocument21 pagesPharmacological SheetScribdTranslationsNo ratings yet
- Anthelmintic DrugsDocument16 pagesAnthelmintic Drugsthanh ba matNo ratings yet
- ) Pharmacology Drug StudyDocument8 pages) Pharmacology Drug StudyFatima KateNo ratings yet
- A Drug Study On: Monaliza J. Lee, RN, MNDocument6 pagesA Drug Study On: Monaliza J. Lee, RN, MNJeah Bearl AbellarNo ratings yet
- Pharmacology of Antiparasit DrugsDocument40 pagesPharmacology of Antiparasit Drugsakun scribNo ratings yet
- Urinary Tract Infection in Children: DR Nada Qawasmi Alquds Faculty of MedicineDocument25 pagesUrinary Tract Infection in Children: DR Nada Qawasmi Alquds Faculty of Medicineولاء إبراهيمNo ratings yet
- Drug Study 408Document13 pagesDrug Study 408Jheryck SabadaoNo ratings yet
- Drug Study Gentamicin Sulfate and SalbutamolDocument7 pagesDrug Study Gentamicin Sulfate and SalbutamolEduardNo ratings yet
- Antiemetic Drugs: Dr. Jatin DhananiDocument31 pagesAntiemetic Drugs: Dr. Jatin DhananiRiddhi JainNo ratings yet
- Pharmacology Lab DrugsDocument14 pagesPharmacology Lab DrugszzNo ratings yet
- Aminoglycosides: Dr. Amit ShahDocument29 pagesAminoglycosides: Dr. Amit ShahAmit ShahNo ratings yet
- Class Indications: MetronidazoleDocument3 pagesClass Indications: MetronidazoleDwi WulandariNo ratings yet
- Baby Katzung Second Shifting Reviewer PDFDocument13 pagesBaby Katzung Second Shifting Reviewer PDFJoanne Aluzan100% (1)
- Drugs For Constipation and DiarrheaDocument40 pagesDrugs For Constipation and Diarrheagirgray100% (1)
- Drug Therapy For GI Disorders PDFDocument5 pagesDrug Therapy For GI Disorders PDFmeeraNo ratings yet
- Antidiarrhoeal DrugsDocument15 pagesAntidiarrhoeal DrugsJyoti SidhuNo ratings yet
- Pharmacology of The Gastrointestinal Drugs (I)Document12 pagesPharmacology of The Gastrointestinal Drugs (I)anaNo ratings yet
- Antiemetics AmoebiasisDocument5 pagesAntiemetics AmoebiasisEaint BoNo ratings yet
- Anthelmintic DrugsDocument28 pagesAnthelmintic DrugsAmit ShahNo ratings yet
- Loperamide - Pharma Online UstadDocument1 pageLoperamide - Pharma Online UstadF ParikhNo ratings yet
- Sample - Drug Index DatabaseDocument12 pagesSample - Drug Index DatabaseEubert John VenturinaNo ratings yet
- MetronidazoleDocument3 pagesMetronidazoleAvigale Arcillas BasilioNo ratings yet
- 9 - Antiprotozoal DrugsDocument29 pages9 - Antiprotozoal Drugsمهند الرحيليNo ratings yet
- Clostridium Difficile Guideline - UMMCDocument5 pagesClostridium Difficile Guideline - UMMCdamondouglas100% (3)
- Antiprotozoal Agents: PHR SangitaDocument21 pagesAntiprotozoal Agents: PHR SangitaCurex QANo ratings yet
- Obat Antijamur Dan Antihistamin: Dr. Elly Usman, M.Si, AptDocument17 pagesObat Antijamur Dan Antihistamin: Dr. Elly Usman, M.Si, AptChindyNo ratings yet
- Anti Amoebic DrugsDocument35 pagesAnti Amoebic DrugsAlishba MushtaqNo ratings yet
- Management of GoutDocument6 pagesManagement of GoutSeanHong TanNo ratings yet
- Drugs Acting On The GitDocument29 pagesDrugs Acting On The GitIsheanesu MugwisiNo ratings yet
- COTRIMOXAZOLE +FQsDocument62 pagesCOTRIMOXAZOLE +FQsHussein AlhaddadNo ratings yet
- Factors Responsible For Noncompliance To Drug Therapy in The Elderly and The Impact of Patient Education On Improving ComplianceDocument9 pagesFactors Responsible For Noncompliance To Drug Therapy in The Elderly and The Impact of Patient Education On Improving ComplianceAmit ShahNo ratings yet
- Cost Burden of Inappropriate Peri-Operative Antibacterial Use in A Teaching Tertiary-Care Rural Hospital in IndiaDocument8 pagesCost Burden of Inappropriate Peri-Operative Antibacterial Use in A Teaching Tertiary-Care Rural Hospital in IndiaAmit ShahNo ratings yet
- Trends of Articles Published in National Journal of Physiology, Pharmacy and Pharmacology (NJPPP)Document7 pagesTrends of Articles Published in National Journal of Physiology, Pharmacy and Pharmacology (NJPPP)Amit ShahNo ratings yet
- Apti Apti Ijopp IjoppDocument5 pagesApti Apti Ijopp IjoppAmit ShahNo ratings yet
- Antiseptics & DisinfectantsDocument26 pagesAntiseptics & DisinfectantsAmit ShahNo ratings yet
- Antiretroviral DrugsDocument26 pagesAntiretroviral DrugsAmit ShahNo ratings yet
- Aminoglycosides: Dr. Amit ShahDocument29 pagesAminoglycosides: Dr. Amit ShahAmit ShahNo ratings yet
- Adrenoceptor AntagonistsDocument72 pagesAdrenoceptor AntagonistsAmit ShahNo ratings yet
- Adrenergic AgentsDocument45 pagesAdrenergic AgentsAmit ShahNo ratings yet
- Medication Exercise Treatment Hygiene Outpatient Diet: C (Classification)Document3 pagesMedication Exercise Treatment Hygiene Outpatient Diet: C (Classification)Carla Tongson MaravillaNo ratings yet
- Supply of DD: Cheza May Baldado Francose Marie EstradaDocument10 pagesSupply of DD: Cheza May Baldado Francose Marie EstradaKathleen B BaldadoNo ratings yet
- Essential Drug List PharmacyDocument26 pagesEssential Drug List PharmacyIchigo ShoonNo ratings yet
- Chemo ExtravasationDocument12 pagesChemo Extravasationlanka007No ratings yet
- Iv Computation QuestionsDocument4 pagesIv Computation QuestionsJasmine YntigNo ratings yet
- WC500020164 PDFDocument29 pagesWC500020164 PDFNeicu Marius-RăzvanNo ratings yet
- Misoprostol Indications: PharmacologyDocument2 pagesMisoprostol Indications: PharmacologyPatricia Marie BuenafeNo ratings yet
- Acetylcysteine (Fluimucil)Document2 pagesAcetylcysteine (Fluimucil)Chelsy MurielNo ratings yet
- Infliximab ProtDocument5 pagesInfliximab ProtQusay AbdohNo ratings yet
- Gajanan CirtificateDocument1 pageGajanan CirtificateLearn easy By Gajanan topaleNo ratings yet
- Drug Study (Alnix)Document2 pagesDrug Study (Alnix)julesubayubay5428No ratings yet
- PONV Prophylaxis Guidelines: Risk Factor OR 95% CIDocument4 pagesPONV Prophylaxis Guidelines: Risk Factor OR 95% CIHerly NurrahmaNo ratings yet
- Bud - Labeling PrescriptionsDocument15 pagesBud - Labeling PrescriptionsUsna AprilianaNo ratings yet
- Antiemetic Drugs: What To Prescribe and When: GastroenteritisDocument8 pagesAntiemetic Drugs: What To Prescribe and When: GastroenteritisSejal MishraNo ratings yet
- Parts of PrescriptionDocument12 pagesParts of PrescriptionEmpanology GamesNo ratings yet
- 2 2 Bioaivers ExperienceDocument80 pages2 2 Bioaivers Experienceblashyrkh_79No ratings yet
- NO Nama Produk Beta Kemasan Per Box HNA Hna + PPN Disc Harga Jadi Sales Sm. I OLD NEW JAN FEB MAR APR MEI JUNDocument4 pagesNO Nama Produk Beta Kemasan Per Box HNA Hna + PPN Disc Harga Jadi Sales Sm. I OLD NEW JAN FEB MAR APR MEI JUNtoko berkat istiqomahNo ratings yet
- Antipsychotics - AMBOSS PDFDocument7 pagesAntipsychotics - AMBOSS PDFOpio Isaac100% (1)
- HolyFamilyHospital Standardcharges 0Document1,596 pagesHolyFamilyHospital Standardcharges 0CCRNo ratings yet
- Public Assessment Report Scientific DiscussionDocument19 pagesPublic Assessment Report Scientific DiscussionTaki JuveNo ratings yet
- Obesity 1Document12 pagesObesity 1ANOOPVANo ratings yet
- Translate 5Document22 pagesTranslate 5Dahliawati MohiNo ratings yet
- Ghid Astm BronsicDocument11 pagesGhid Astm BronsicLeonard D100% (1)
- High-Priority Drugedrug Interactions For Use inDocument9 pagesHigh-Priority Drugedrug Interactions For Use inProfessor DeividNo ratings yet
- 2nd yDocument9 pages2nd yPrashant DhakadNo ratings yet
- Cefalexin (Cephalexin) Monograph - Paediatric: DescriptionDocument5 pagesCefalexin (Cephalexin) Monograph - Paediatric: Descriptioneinas omerNo ratings yet
- Editorial: Dental Caries and OsteoporosisDocument2 pagesEditorial: Dental Caries and OsteoporosisBagis Emre GulNo ratings yet
- Daftar Obat - Obatan Klinik Kunci Sehat (Poli Umum, Poli Gigi)Document4 pagesDaftar Obat - Obatan Klinik Kunci Sehat (Poli Umum, Poli Gigi)rain st.markNo ratings yet
- Neutropenic Fever Empiric TherapyDocument5 pagesNeutropenic Fever Empiric TherapyRominaPulvermüllerSalvatierraNo ratings yet
Antiamoebic & Other Antiprotozoal Drugs
Antiamoebic & Other Antiprotozoal Drugs
Uploaded by
Amit Shah0 ratings0% found this document useful (0 votes)
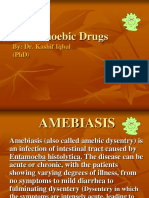
90 views47 pagesThis document discusses drugs used to treat protozoal infections, specifically amoebiasis and giardiasis. It provides details on the mechanisms of action, pharmacokinetics, clinical uses, dosages and adverse effects of various antiamebic and antiparasitic drugs. The main drugs discussed are metronidazole, tinidazole, emetine, diloxanide furoate, nitazoxanide, and tetracyclines for treating amoebiasis. For giardiasis, the recommended first-line treatments include metronidazole, tinidazole, secnidazole, nitazoxanide and quiniodochlor. Guidelines
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses drugs used to treat protozoal infections, specifically amoebiasis and giardiasis. It provides details on the mechanisms of action, pharmacokinetics, clinical uses, dosages and adverse effects of various antiamebic and antiparasitic drugs. The main drugs discussed are metronidazole, tinidazole, emetine, diloxanide furoate, nitazoxanide, and tetracyclines for treating amoebiasis. For giardiasis, the recommended first-line treatments include metronidazole, tinidazole, secnidazole, nitazoxanide and quiniodochlor. Guidelines
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
90 views47 pagesAntiamoebic & Other Antiprotozoal Drugs
Antiamoebic & Other Antiprotozoal Drugs
Uploaded by
Amit ShahThis document discusses drugs used to treat protozoal infections, specifically amoebiasis and giardiasis. It provides details on the mechanisms of action, pharmacokinetics, clinical uses, dosages and adverse effects of various antiamebic and antiparasitic drugs. The main drugs discussed are metronidazole, tinidazole, emetine, diloxanide furoate, nitazoxanide, and tetracyclines for treating amoebiasis. For giardiasis, the recommended first-line treatments include metronidazole, tinidazole, secnidazole, nitazoxanide and quiniodochlor. Guidelines
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 47
DR.
AMIT M SHAH
ANTIAMOEBIC & OTHER
ANTIPROTOZOAL DRUGS
ANTIAMOEBIC DRUGS
INTRODUCTION
Protozoal infection of the intestinal tract that
occurs due to ingestion of foods or water
contaminated with Entameba Histolytica cysts
A worldwide distribution (over 50 million people
are infected)
Endemic in most parts of India
LIFE CYCLE
CLINICAL PRESENTATIONS
Asymptomatic Intestinal infection (Carriers,
passing cysts)
Mild to moderate intestinal disease
(Nondysenteric Colitis)
Severe Intestinal infection (Dysentery)
Hepatic abscess, ameboma (localized
granulomatous lesion of colon) and other
extraintestinal disease
ANTIAMOEBIC DRUGS
Tissue amoebicides
o For both intestinal and extraintestinal amoebiasis:
• Nitroimidazoles: Metronidazole, Tinidazole
• Alkaloids: Emetine, Dehydroemetine
o For extraintestinal amoebiasis only: Chloroquine
Luminal amoebicides
o Amide: Diloxanide furoate, Nitazoxanide
o 8-Hydroxyquinolines: Iodochlorohydroxyquin,
Clioquinol, Iodoquinol
o Antibiotics: Tetracyclines
METRONIDAZOLE
Broad-spectrum cidal activity against protozoa,
including E. histolytica, Giardia, T. vaginalis
Also active against many anaerobic bacteria, e.g.
o B. fragilis
o Fusobacterium
o Cl. perfringens, Cl. Difficile
o H. pylori
o Campylobacter
o Anaerobic Streptococci
MECHANISM OF ACTION
Reduced product that binds to DNA, proteins and
cell membrane resulting into parasite death
PHARMACOKINETICS
Given orally or IV
Absorption is rapid and complete
Due to rapid absorption from GIT, not reliably
effective against luminal parasites
Wide distribution to all tissues and body fluids
(Vaginal secretion, CSF, saliva, milk).
Metabolized in liver by oxidation and glucuronide
conjugation
Plasma half life is 8 h
CLINICAL USES
Amoebiasis:
o 1st line drug for all forms of amoebic infection
o Invasive dysentery and liver abscess: 800 mg TDS
(children 30–50 mg/kg/day) for 7–10 days
o Serious cases of liver abscess 1 g i.v. slowly followed by
0.5 g every 8–12 hr till oral therapy is instituted
o Mild intestinal disease: 400 mg TDS for 5–7 days
o Less effective in eradicating amoebic cysts from the
colon
Giardiasis: 400 mg TDS X 7 days OR 2 g/day X 3 days
Trichomonas vaginitis: 400 mg TDS for 7 days
Anaerobic bacterial infections:
o After colorectal or pelvic surgery, appendicectomy
o Brain abscesses and endocarditis
o Combination with gentamicin or cephalosporins
o IV 15 mg/kg infused over 1 hr ⇒ 7.5 mg/kg every 6 hrs
till oral therapy can be instituted with 400–800 mg TDS
o Prophylactic use in high risk situations (colorectal
surgery)
Pseudomembranous enterocolitis: due to Cl. Difficile;
Oral metronidazole 800 mg TDS
Ulcerative gingivitis, trench mouth: 200–400 mg TDS
Helicobacter pylori gastritis/peptic ulcer:
Metronidazole 400 mg TDS along with
amoxicillin/clarithromycin and a proton pump
inhibitor in triple drug 2 week regimens
ADVERSE EFFECTS
Frequent and unpleasant, but mostly nonserious.
MOST COMMON: Anorexia, nausea, metallic taste and
abdominal cramps, looseness of stool
LESS FREQUENT: Headache, glossitis, dryness of
mouth, dizziness, rashes and transient neutropenia.
PROLONGED ADMINISTRATION may cause peripheral
neuropathy and Seizures
Thrombophlebitis of the injected vein
CONTRAINDICATIONS
Neurological disease
Blood dyscrasias
First trimester of pregnancy
Chronic alcoholism
INTERACTIONS
Disulfiram-like reaction to alcohol
Enzyme inducers (phenobarbitone, rifampin)
reduce its therapeutic effect
Cimetidine reduce metronidazole metabolism
Enhances warfarin action by inhibiting its
metabolism
Decrease renal elimination of lithium
TINIDAZOLE
Similar to metronidazole but,
o Metabolism is slower ⇒ long duration of action (t½
~12 hr) ⇒ single dose or once daily therapy
o Some trials in amoebiasis have reported higher cure
rates
o Better tolerated
CLINICAL USES
Amoebiasis: 2 g OD for 3 days (children 30–50 mg/
kg/day) OR 0.6 g BD for 5–10 days
Trichomoniasis and giardiasis: 2 g single dose OR 0.6
g OD for 7 days
Anaerobic infections:
o Prophylactic: 2 g single dose before colorectal surgery
o Therapeutic: 2 g followed by 0.5 g BD for 5 days
H. pylori: 500 mg BD for 2 weeks in triple combination
SECNIDAZOLE: Rapid & complete oral absorption;
t½ of 17–29 hours
ORNIDAZOLE: longer t½ (12–14 hr)
SATRANIDAZOLE: longer t½ (14 hr); better
tolerability
EMETINE
Alkaloid from Cephaelis ipecacuanha
Potent and directly acting amoebicide: kills
trophozoites; no effect on cysts (not curative)
Inhibiting intraribosomal translocation of tRNA-
amino acid complex ⇒ Inhibit protein synthesis
Rapidly clearance of the trophozoites from stool
(1–3 days) – even faster than metronidazole
Highly efficacious in amoebic liver abscess also.
Cannot be given orally because it will be vomited
out
Administered by s.c. or i.m.: 60 mg OD
Concentrated in liver, kidney, spleen and lungs ⇒
should not be given more than 10 days
Very slowly excreted in urine taking 1–2 months
Cumulative toxicity ⇒ 2nd course should not be
repeated within 6 weeks
ADVERSE EFFECTS: High
Local: Pain, stiffness and eczematous lesions at the site
of injection
Nausea and vomiting: Parenteral and oral route
Abdominal cramps and diarrhoea
Weakness and stiffness of muscles
Hypotension, tachycardia, ECG changes and
myocarditis
CONTRAINDICATED: Cardiac or renal dz & pregnancy.
CLINICAL USES: Reserve Drug
Severe intestinal or extraintestinal amoebiasis
Patients not responding to or not tolerating
metronidazole
A luminal amoebicide must always follow to eradicate
the cyst
Also effective in liver fluke infestation
DEHYDROEMETINE
Semisynthetic derivative of emetine
Equally effective
Less cumulative and less toxic to the heart
Preferred over emetine
CHLOROQUINE
Kills trophozoites of E. histolytica
Completely absorbed from the upper GIT and not
so highly concentrated in the intestinal wall ⇒ Not
effective in invasive dysentery nor in cyst passers
Highly concentrated in liver ⇒ Used in hepatic
amoebiasis
Longer duration of treatment
Relapses are relatively more frequent
Relative safe to Emetine
Only when metronidazole is not effective or not
tolerated
Given concurrently or immediately after a course
of metronidazole to ensure complete eradication of
the trophozoites in liver
A luminal amoebicide must always be given
Dose: 600 mg (base) for 2 days ⇒ 300 mg for 2-3
weeks
DILOXANIDE FUROATE
Highly effective luminal amoebicide
Directly kills trophozoites
Furoate ester is hydrolysed in intestine and the
released diloxanide is largely absorbed
Diloxanide is a weaker amoebicide than its ester
Metabolized by glucuronidation and excreted in urine
No antibacterial action
Less effective in invasive amoebic dysentery, because
of poor tissue amoebicidal action
High (80–90%) cure rate with single course
Drug of choice for mild intestinal/asymptomatic
amoebiasis (500 mg TDS for 5–10 days)
Given after any tissue amoebicide to eradicate cysts
Combined with metronidazole/tinidazole
Some chronic cases require repeat courses for
eradication
Very well tolerated
ADR: flatulence, nausea, itching and urticarial
NITAZOXANIDE
Congener of the anthelmintic niclosamide
Active against Giardia, E. histolytica, T. vaginalis,
Cryptosporidium, H. pylori, Ascaris, H. nana
Prodrug (active form tizoxanide)
Inhibitor of PFOR enzyme that is an essential pathway
of electron transport energy metabolism
Active against metronidazole-resistant Giardia
Indicated in giardiasis, cryptosporidiasis, amoebic
dysentery as luminal amoebicide
Abdominal pain, vomiting and headache
8-HYDROXYQUINOLINES
Quiniodochlor (Iodochlorohydroxyquin, Clioquinol),
Diiodohydroxyquin (Iodoquinol)
Active against Entamoeba, Giardia, Trichomonas, some
fungi (dermatophytes, Candida) and some bacteria
Mechanism of action - Unknown
Effective against organisms in GIT only Not intestinal
wall or liver
Absorption is poor (90%), excreted in feces
Used as lumen amoebicide for eradication of infection
given along with tissue amoebicide (metronidazole)
Adverse Effects
o Peripheral neuropathy [Quiniodochlor - Subacute Myelo-
optic Neuropathy (SMON)]
o GIT: Nausea, vomiting, diarrhoea
o Agranulocytosis
o Enlargement of the thyroid gland & interference with
thyroid function tests
o Iodism (furunculosis, inflammation of mucous
membranes)
TETRACYCLINES
Older Tetracyclines
Very weak direct amoebicidal action.
Mainly act indirectly on bacterial flora
Used in severe cases of amoebic dysentery not
responding to metronidazole combined with
dehydroemetine
Clinical Setting Drugs of Choice
Asymptomatic Diloxanide furoate 500 mg orally TDS for 7-10 days
intestinal infection OR
Iodoquinol, 650 mg orally TDS for 21 days
Mild to moderate Metronidazole, 400 mg orally TDS for 7-10 days
intestinal infection OR
Tinidazole, 2 g orally daily for 3 days
PLUS
Luminal agent
Severe intestinal Metronidazole 800 mg orally TDS (500 mg IV every
infection, hepatic 8-12 hours) for 7-10 days
abscess, and other OR
extraintestinal Tinidazole, 2 g orally daily for 3 days
disease PLUS
Luminal agent
DRUGS FOR GIARDIASIS
Metronidazole: 200 mg TDS (15 mg/kg/day) for 7 days
or 2 g daily for 3 days
Tinidazole: 0.6 g daily for 7 days or 2 g single dose
Secnidazole: 2 g single dose
Nitazoxanide: 500 mg (7.5 mg/kg) BD daily for 3 days
Quiniodochlor: 250 mg TDS for 7 days
Furazolidone:
o Nitrofuran compound
o Active against gram-negative bacilli (Salmonella and
Shigella), Giardia and Trichomonas
o Inferior to metronidazole or tinidazole
o Dose: 100 mg TDS for 5–7 days
o Also used in bacterial enteritis, food poisoning
diarrhoeas and bacillary dysentery
o ADR: mild & infrequent—nausea, headache, dizziness
DRUGS FOR
TRICHOMONIASIS
DRUGS USED ORALLY
Metronidazole: 400 mg TDS for 7 days or 2 g daily for 3
days
Tinidazole: 0.6 g daily for 7 days or 2 g single dose
Secnidazole: 2 g single dose
Nimorazole: 2 g single dose
Additional intravaginal treatment is required only in
refractory cases
DRUGS USED INTRAVAGINALLY
Diiodohydroxyquin: 200 mg at bed time for 1–2 weeks
Quiniodochlor: 200 mg at bed time for 1–3 weeks
Clotrimazole: 100 mg inserted highup in vagina every
night for 6–12 days
Hamycin: 4–8 lac U daily for 15 days
Natamycin: 25 mg at bed time for 10 days
Povidone-iodine: 400 mg daily at night for 2 weeks
DRUGS FOR LEISHMANIASIS
(KALA-AZAR)
Available Drugs
Antimonial: Sodium stibogluconate (SSG)
Diamide: Pentamidine
Antifungal: Amphotericin B (AMB), Ketoconazole
(KTZ)
Others: Miltefosine, Paromomycin, Allopurinol
SODIUM STIBOGLUCONATE
The drug of choice in Leishmaniasis – resistance
Water soluble pentavalent antimonial compound –
1/3rd antimony by weight
MOA: Not clear
o -SH dependent enzymes are inhibited – bioenergetics of
the parasite
o Blocks glycolytic and fatty acid oxidation pathways
o Enzyme in leishmania converts SSG to trivalent
compound – causes efflux of glutathione and thiols –
oxidative damage
Dose: 20-30 mg/kg (max. 850 mg)deep IM or IV daily
in buttock for 20-30 days or more – depends on
response in bone marrow and splenic aspirates
Adverse Effects: All antimonials are toxic
o Nausea, vomiting, metallic taste, cough and pain
abdomen
o Stiffness and abscess in injected muscles
o Pancreatitis, liver and kidney damage etc.
o Rarely shock and death
PENTAMIDINE
MOA: Not clear, inhibits Topoisomerase II or interferes
with aerobic glycolysis
Not metabolized but stored in kidneys and liver –
slowly released
USES:
o SSG failure cases - AMB is preferred now
o Trypanosomiasis - CNS involvement
o Pneumocystis jiroveci pneumonia in AIDS patients
Dose: 4 mg/kg IM or slow IV for 1 Hr on alternate days
for 5-15 weeks
Adverse Effects:
o Histamine release – acute reactions – Sharp fall in BP,
dyspnoea, palpitation, fainting, vomiting and rigor etc.
o Other reactions - rashes, mental confusion, kidney and
liver damage
o Cytolysis of pancreatioc beta cells – initially insulin
release – hypoglycaemia, but later IDDM
MILTEFOSINE
First oral antileishmania drug approved in 2002
Interfere with lipid metabolism
≥ 95% cure rate with 4 week course
1st line agent under NVBDCP
Vomiting and diarrhoea occur in over ½ of the patients
Reversible derangement of liver and kidney function
Teratogenic ⇒ C/I in pregnant women
Dose: 100 mg/day for 4 weeks
Visceral (L Miltefosine 100 mg/day for 4 weeks
donovani, L chagasi, OR
L infantum) Sodium stibogluconate, 20 mg/kg/d IV or IM
or mucosal (L for 28 days
braziliensis) OR
Pentamidine 4 mg/kg deep i.m. or slow i.v.
(over 1 hr) on alternate days for 5–15 weeks
OR
Amphotericin-B 0.5–1.0 mg/kg/day slow i.v.
infusion till 15–20 mg/kg
OR
Paromomycin 10–15 mg/kg/day i.m. × 21 days
Cutaneous Sodium stibogluconate: Infiltrate 2 ml of the
(L major, L tropica, L solution (100 mg antimony/ml) round the sore
mexicana, L OR
braziliensis) Paromomycin ointment
DID YOU SLEEP DURING LAST 45 MIN?
If yes, no problem – just have to go and
read Metronidazole and SSG
If No, enjoy today - for knowing
Metronidazole and SSG
You might also like
- Quiz PharmaDocument6 pagesQuiz PharmaMary Grace Bañes100% (1)
- Anti Amoebic DrugsDocument17 pagesAnti Amoebic DrugsSaurabh Gautam100% (2)
- Treatment of A Moe Bias Is Giardia SisDocument27 pagesTreatment of A Moe Bias Is Giardia SisLuthfi Hilman TaufikNo ratings yet
- Treatment of Amoebiasis & GiardiasisDocument27 pagesTreatment of Amoebiasis & GiardiasisElda LizmaNo ratings yet
- ANTIAMUBADocument20 pagesANTIAMUBAAspar RafiqNo ratings yet
- Farmakologi Obat Kusta Dan Antiparasit 2015Document84 pagesFarmakologi Obat Kusta Dan Antiparasit 2015Alex FerdinandNo ratings yet
- (Udah) AntiamubaDocument20 pages(Udah) AntiamubaMohammad Rizki PratamaNo ratings yet
- Antiprotozoal Drugs: DR Manik GhadlingeDocument63 pagesAntiprotozoal Drugs: DR Manik GhadlingeEscitalopram 5mgNo ratings yet
- Anti-Protozoal DrugsDocument38 pagesAnti-Protozoal DrugsMahnoor AbidNo ratings yet
- Keterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugDocument7 pagesKeterolax Trometamol Classification: Nonsteroidal Anti-Inflamatory DrugEm Hernandez AranaNo ratings yet
- PROBLEM 2B - VarlaDocument50 pagesPROBLEM 2B - VarlavarlavarleyNo ratings yet
- Chemotherapy of Helminth Infections: DR - Rathnakar U.PDocument39 pagesChemotherapy of Helminth Infections: DR - Rathnakar U.PDr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- Anti Parasites Blok 3.2Document46 pagesAnti Parasites Blok 3.2Alda Herlen Kalkarina BangunNo ratings yet
- 1 Final Drug Study Gastro Jan26-27, 2023Document13 pages1 Final Drug Study Gastro Jan26-27, 2023Wynne GriffinNo ratings yet
- Ameobiasis and Giardiasis: S.Ravindra Babu Associate ProfessorDocument38 pagesAmeobiasis and Giardiasis: S.Ravindra Babu Associate Professorkamsu JyothsnaNo ratings yet
- Antiproto & AnthelminticsDocument57 pagesAntiproto & AnthelminticsDrMohan GuptaNo ratings yet
- Metronidazole: (Me Troe Ni' Da Zole)Document4 pagesMetronidazole: (Me Troe Ni' Da Zole)Wino SantosNo ratings yet
- Domperidone Uses:: Nausea and Vomiting BreastDocument6 pagesDomperidone Uses:: Nausea and Vomiting BreastAnna Charissa Arcales HoraNo ratings yet
- Pharmacotherapy of Peptic Ulcer: DR ZareenDocument50 pagesPharmacotherapy of Peptic Ulcer: DR ZareenGareth BaleNo ratings yet
- Pharmacotherapy of Peptic Ulcer: DR ZareenDocument50 pagesPharmacotherapy of Peptic Ulcer: DR ZareenGareth BaleNo ratings yet
- L 1+2 - Urinary Tract InfectinsDocument33 pagesL 1+2 - Urinary Tract InfectinsMunibaNo ratings yet
- Urinary Germicides PharmaDocument11 pagesUrinary Germicides PharmaMaria Pina Barbado PonceNo ratings yet
- Pharma - Drugs Affecting Git MotilityDocument6 pagesPharma - Drugs Affecting Git MotilityBobet ReñaNo ratings yet
- Chemotherapy of Protozoal InfectionsDocument34 pagesChemotherapy of Protozoal InfectionsSri RamNo ratings yet
- Group-3-Ward-Class 20240213 182023 0000Document31 pagesGroup-3-Ward-Class 20240213 182023 0000Hanna CarsanoNo ratings yet
- CefaclorDocument3 pagesCefaclorAyah PaasaNo ratings yet
- Anti DiarrhoealsDocument37 pagesAnti DiarrhoealsCrome operatorNo ratings yet
- Anti-Protozoal Drugs: Dr. Mozna TalpurDocument25 pagesAnti-Protozoal Drugs: Dr. Mozna TalpurShahid Hameed100% (1)
- Farmakologi AntiparasitDocument119 pagesFarmakologi AntiparasitFitri Sri WulandariNo ratings yet
- DrugsDocument8 pagesDrugsShizuka Marycris AmaneNo ratings yet
- Pharmacological SheetDocument21 pagesPharmacological SheetScribdTranslationsNo ratings yet
- Anthelmintic DrugsDocument16 pagesAnthelmintic Drugsthanh ba matNo ratings yet
- ) Pharmacology Drug StudyDocument8 pages) Pharmacology Drug StudyFatima KateNo ratings yet
- A Drug Study On: Monaliza J. Lee, RN, MNDocument6 pagesA Drug Study On: Monaliza J. Lee, RN, MNJeah Bearl AbellarNo ratings yet
- Pharmacology of Antiparasit DrugsDocument40 pagesPharmacology of Antiparasit Drugsakun scribNo ratings yet
- Urinary Tract Infection in Children: DR Nada Qawasmi Alquds Faculty of MedicineDocument25 pagesUrinary Tract Infection in Children: DR Nada Qawasmi Alquds Faculty of Medicineولاء إبراهيمNo ratings yet
- Drug Study 408Document13 pagesDrug Study 408Jheryck SabadaoNo ratings yet
- Drug Study Gentamicin Sulfate and SalbutamolDocument7 pagesDrug Study Gentamicin Sulfate and SalbutamolEduardNo ratings yet
- Antiemetic Drugs: Dr. Jatin DhananiDocument31 pagesAntiemetic Drugs: Dr. Jatin DhananiRiddhi JainNo ratings yet
- Pharmacology Lab DrugsDocument14 pagesPharmacology Lab DrugszzNo ratings yet
- Aminoglycosides: Dr. Amit ShahDocument29 pagesAminoglycosides: Dr. Amit ShahAmit ShahNo ratings yet
- Class Indications: MetronidazoleDocument3 pagesClass Indications: MetronidazoleDwi WulandariNo ratings yet
- Baby Katzung Second Shifting Reviewer PDFDocument13 pagesBaby Katzung Second Shifting Reviewer PDFJoanne Aluzan100% (1)
- Drugs For Constipation and DiarrheaDocument40 pagesDrugs For Constipation and Diarrheagirgray100% (1)
- Drug Therapy For GI Disorders PDFDocument5 pagesDrug Therapy For GI Disorders PDFmeeraNo ratings yet
- Antidiarrhoeal DrugsDocument15 pagesAntidiarrhoeal DrugsJyoti SidhuNo ratings yet
- Pharmacology of The Gastrointestinal Drugs (I)Document12 pagesPharmacology of The Gastrointestinal Drugs (I)anaNo ratings yet
- Antiemetics AmoebiasisDocument5 pagesAntiemetics AmoebiasisEaint BoNo ratings yet
- Anthelmintic DrugsDocument28 pagesAnthelmintic DrugsAmit ShahNo ratings yet
- Loperamide - Pharma Online UstadDocument1 pageLoperamide - Pharma Online UstadF ParikhNo ratings yet
- Sample - Drug Index DatabaseDocument12 pagesSample - Drug Index DatabaseEubert John VenturinaNo ratings yet
- MetronidazoleDocument3 pagesMetronidazoleAvigale Arcillas BasilioNo ratings yet
- 9 - Antiprotozoal DrugsDocument29 pages9 - Antiprotozoal Drugsمهند الرحيليNo ratings yet
- Clostridium Difficile Guideline - UMMCDocument5 pagesClostridium Difficile Guideline - UMMCdamondouglas100% (3)
- Antiprotozoal Agents: PHR SangitaDocument21 pagesAntiprotozoal Agents: PHR SangitaCurex QANo ratings yet
- Obat Antijamur Dan Antihistamin: Dr. Elly Usman, M.Si, AptDocument17 pagesObat Antijamur Dan Antihistamin: Dr. Elly Usman, M.Si, AptChindyNo ratings yet
- Anti Amoebic DrugsDocument35 pagesAnti Amoebic DrugsAlishba MushtaqNo ratings yet
- Management of GoutDocument6 pagesManagement of GoutSeanHong TanNo ratings yet
- Drugs Acting On The GitDocument29 pagesDrugs Acting On The GitIsheanesu MugwisiNo ratings yet
- COTRIMOXAZOLE +FQsDocument62 pagesCOTRIMOXAZOLE +FQsHussein AlhaddadNo ratings yet
- Factors Responsible For Noncompliance To Drug Therapy in The Elderly and The Impact of Patient Education On Improving ComplianceDocument9 pagesFactors Responsible For Noncompliance To Drug Therapy in The Elderly and The Impact of Patient Education On Improving ComplianceAmit ShahNo ratings yet
- Cost Burden of Inappropriate Peri-Operative Antibacterial Use in A Teaching Tertiary-Care Rural Hospital in IndiaDocument8 pagesCost Burden of Inappropriate Peri-Operative Antibacterial Use in A Teaching Tertiary-Care Rural Hospital in IndiaAmit ShahNo ratings yet
- Trends of Articles Published in National Journal of Physiology, Pharmacy and Pharmacology (NJPPP)Document7 pagesTrends of Articles Published in National Journal of Physiology, Pharmacy and Pharmacology (NJPPP)Amit ShahNo ratings yet
- Apti Apti Ijopp IjoppDocument5 pagesApti Apti Ijopp IjoppAmit ShahNo ratings yet
- Antiseptics & DisinfectantsDocument26 pagesAntiseptics & DisinfectantsAmit ShahNo ratings yet
- Antiretroviral DrugsDocument26 pagesAntiretroviral DrugsAmit ShahNo ratings yet
- Aminoglycosides: Dr. Amit ShahDocument29 pagesAminoglycosides: Dr. Amit ShahAmit ShahNo ratings yet
- Adrenoceptor AntagonistsDocument72 pagesAdrenoceptor AntagonistsAmit ShahNo ratings yet
- Adrenergic AgentsDocument45 pagesAdrenergic AgentsAmit ShahNo ratings yet
- Medication Exercise Treatment Hygiene Outpatient Diet: C (Classification)Document3 pagesMedication Exercise Treatment Hygiene Outpatient Diet: C (Classification)Carla Tongson MaravillaNo ratings yet
- Supply of DD: Cheza May Baldado Francose Marie EstradaDocument10 pagesSupply of DD: Cheza May Baldado Francose Marie EstradaKathleen B BaldadoNo ratings yet
- Essential Drug List PharmacyDocument26 pagesEssential Drug List PharmacyIchigo ShoonNo ratings yet
- Chemo ExtravasationDocument12 pagesChemo Extravasationlanka007No ratings yet
- Iv Computation QuestionsDocument4 pagesIv Computation QuestionsJasmine YntigNo ratings yet
- WC500020164 PDFDocument29 pagesWC500020164 PDFNeicu Marius-RăzvanNo ratings yet
- Misoprostol Indications: PharmacologyDocument2 pagesMisoprostol Indications: PharmacologyPatricia Marie BuenafeNo ratings yet
- Acetylcysteine (Fluimucil)Document2 pagesAcetylcysteine (Fluimucil)Chelsy MurielNo ratings yet
- Infliximab ProtDocument5 pagesInfliximab ProtQusay AbdohNo ratings yet
- Gajanan CirtificateDocument1 pageGajanan CirtificateLearn easy By Gajanan topaleNo ratings yet
- Drug Study (Alnix)Document2 pagesDrug Study (Alnix)julesubayubay5428No ratings yet
- PONV Prophylaxis Guidelines: Risk Factor OR 95% CIDocument4 pagesPONV Prophylaxis Guidelines: Risk Factor OR 95% CIHerly NurrahmaNo ratings yet
- Bud - Labeling PrescriptionsDocument15 pagesBud - Labeling PrescriptionsUsna AprilianaNo ratings yet
- Antiemetic Drugs: What To Prescribe and When: GastroenteritisDocument8 pagesAntiemetic Drugs: What To Prescribe and When: GastroenteritisSejal MishraNo ratings yet
- Parts of PrescriptionDocument12 pagesParts of PrescriptionEmpanology GamesNo ratings yet
- 2 2 Bioaivers ExperienceDocument80 pages2 2 Bioaivers Experienceblashyrkh_79No ratings yet
- NO Nama Produk Beta Kemasan Per Box HNA Hna + PPN Disc Harga Jadi Sales Sm. I OLD NEW JAN FEB MAR APR MEI JUNDocument4 pagesNO Nama Produk Beta Kemasan Per Box HNA Hna + PPN Disc Harga Jadi Sales Sm. I OLD NEW JAN FEB MAR APR MEI JUNtoko berkat istiqomahNo ratings yet
- Antipsychotics - AMBOSS PDFDocument7 pagesAntipsychotics - AMBOSS PDFOpio Isaac100% (1)
- HolyFamilyHospital Standardcharges 0Document1,596 pagesHolyFamilyHospital Standardcharges 0CCRNo ratings yet
- Public Assessment Report Scientific DiscussionDocument19 pagesPublic Assessment Report Scientific DiscussionTaki JuveNo ratings yet
- Obesity 1Document12 pagesObesity 1ANOOPVANo ratings yet
- Translate 5Document22 pagesTranslate 5Dahliawati MohiNo ratings yet
- Ghid Astm BronsicDocument11 pagesGhid Astm BronsicLeonard D100% (1)
- High-Priority Drugedrug Interactions For Use inDocument9 pagesHigh-Priority Drugedrug Interactions For Use inProfessor DeividNo ratings yet
- 2nd yDocument9 pages2nd yPrashant DhakadNo ratings yet
- Cefalexin (Cephalexin) Monograph - Paediatric: DescriptionDocument5 pagesCefalexin (Cephalexin) Monograph - Paediatric: Descriptioneinas omerNo ratings yet
- Editorial: Dental Caries and OsteoporosisDocument2 pagesEditorial: Dental Caries and OsteoporosisBagis Emre GulNo ratings yet
- Daftar Obat - Obatan Klinik Kunci Sehat (Poli Umum, Poli Gigi)Document4 pagesDaftar Obat - Obatan Klinik Kunci Sehat (Poli Umum, Poli Gigi)rain st.markNo ratings yet
- Neutropenic Fever Empiric TherapyDocument5 pagesNeutropenic Fever Empiric TherapyRominaPulvermüllerSalvatierraNo ratings yet