Professional Documents
Culture Documents
Using Diode Laser For Soft Tissue Incision of Oral Cavity: Case Report
Using Diode Laser For Soft Tissue Incision of Oral Cavity: Case Report
Uploaded by
Andhika GilangCopyright:
Available Formats
You might also like
- Cockney MonologuesDocument2 pagesCockney MonologuesLaReceHawkins86% (7)
- Samhita SarangadharaDocument4 pagesSamhita SarangadharavatsalabaluNo ratings yet
- 5897 PDFDocument8 pages5897 PDFMohamad BasofiNo ratings yet
- 7 TH JC PDF - SindhuDocument5 pages7 TH JC PDF - SindhuDadi SindhuNo ratings yet
- Correcting Labial Thick and High ATTACHED FRENUM (Clinical Observation)Document3 pagesCorrecting Labial Thick and High ATTACHED FRENUM (Clinical Observation)NisatriaNo ratings yet
- Dentistry Oraldisorders Therapy30Document6 pagesDentistry Oraldisorders Therapy30muhammadNo ratings yet
- Idjsr Se 0168Document4 pagesIdjsr Se 0168Alfan MaulanaNo ratings yet
- Epulis 34465Document4 pagesEpulis 34465Ismail YusufNo ratings yet
- Scalpel Versus Diode Laser For Gingival Depigmentation: A Case ReportDocument8 pagesScalpel Versus Diode Laser For Gingival Depigmentation: A Case ReportIJAR JOURNALNo ratings yet
- 28 Tripty RahangdaleDocument16 pages28 Tripty RahangdaleDrShweta SainiNo ratings yet
- Chen DT Reprint1Document2 pagesChen DT Reprint1Dr.O.R.GANESAMURTHINo ratings yet
- J Lasers Med Sci 2012 3 1 26 32Document7 pagesJ Lasers Med Sci 2012 3 1 26 32Muhammad AbazaNo ratings yet
- اخيرDocument40 pagesاخيرAbas HamzaNo ratings yet
- Application of Lasers in Dentistry 22 25Document4 pagesApplication of Lasers in Dentistry 22 25SkAliHassanNo ratings yet
- Diode Laser Assisted For The Excision of Focal Epithelial Hyperplasia. Case ReportDocument5 pagesDiode Laser Assisted For The Excision of Focal Epithelial Hyperplasia. Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Lasers in Dental ImplantologyDocument18 pagesLasers in Dental ImplantologyErty TyuuNo ratings yet
- Lasers in Prosthetic Dentistry: Medical ScienceDocument3 pagesLasers in Prosthetic Dentistry: Medical Science2oclockNo ratings yet
- Contentserver - AspDocument7 pagesContentserver - AspcasillarodrigoNo ratings yet
- Lasers in Dental ImplantologyDocument17 pagesLasers in Dental ImplantologyIulian CosteanuNo ratings yet
- High-Power Diode Laser Use On Fordyce Granule Excision: A Case ReportDocument4 pagesHigh-Power Diode Laser Use On Fordyce Granule Excision: A Case ReportPauly JinezNo ratings yet
- Research ArticleDocument5 pagesResearch ArticleAtul ScNo ratings yet
- Lasers in Oral and Maxillofacial Surgery.Document28 pagesLasers in Oral and Maxillofacial Surgery.Sukhvinder Singh Rana0% (1)
- Maxillary Labial Frenectomy by Using ConDocument6 pagesMaxillary Labial Frenectomy by Using ConShinta rahma MansyurNo ratings yet
- 9685 40464 1 PBDocument3 pages9685 40464 1 PBTri Sakti Sunda RomdhoniNo ratings yet
- Laser Applications in DentistryDocument13 pagesLaser Applications in DentistryrubytrangtoNo ratings yet
- Laser in Conservative DentistryDocument39 pagesLaser in Conservative DentistryAiluul AlmaaNo ratings yet
- Laser in Proctology: A New Hope in Treating The Distressing Anal Diseases EditorialDocument1 pageLaser in Proctology: A New Hope in Treating The Distressing Anal Diseases EditorialAmit MalikNo ratings yet
- Unusual Radiopacities Spotted in A Dental Radiograph: Case ReportDocument3 pagesUnusual Radiopacities Spotted in A Dental Radiograph: Case ReportlilaNo ratings yet
- Telaah THTDocument3 pagesTelaah THTila chaeruniNo ratings yet
- Piezoelectrico 2020 PDFDocument13 pagesPiezoelectrico 2020 PDFLucy Lobato RomeroNo ratings yet
- Anitua 2013Document9 pagesAnitua 2013Paul CerdaNo ratings yet
- Future of Laser Pediatric Dentistry PDFDocument5 pagesFuture of Laser Pediatric Dentistry PDFsnehasthaNo ratings yet
- Laser Assisted Crown Lengthening - A Multidisciplinary Approach: A ReviewDocument7 pagesLaser Assisted Crown Lengthening - A Multidisciplinary Approach: A ReviewpoojaNo ratings yet
- Morphology of Plans MCQDDocument8 pagesMorphology of Plans MCQDAneesa TafheemNo ratings yet
- Orthodntics MicroimplantsDocument11 pagesOrthodntics Microimplantsdruzair007No ratings yet
- Root Canal Treatment of A 32-mm Length Maxillary Canine - A Case ReportDocument4 pagesRoot Canal Treatment of A 32-mm Length Maxillary Canine - A Case ReportAndre ManaroinsongNo ratings yet
- Endo Don TicDocument8 pagesEndo Don TicArmareality Armareality100% (1)
- Lasers in Endodontics-A Review of Literature: P.A.Vasishta, K Anjaneyalu, Vinay Sivaswamy, K AnjaneyaluDocument7 pagesLasers in Endodontics-A Review of Literature: P.A.Vasishta, K Anjaneyalu, Vinay Sivaswamy, K AnjaneyaluKalpanaNo ratings yet
- Management of Limited Interocclusal Distance With The Aid of A Modified Surgical Guide: A Clinical ReportDocument5 pagesManagement of Limited Interocclusal Distance With The Aid of A Modified Surgical Guide: A Clinical ReporttovarichNo ratings yet
- Surgical Extrusion With An Atraumatic Extraction System: A Clinical StudyDocument7 pagesSurgical Extrusion With An Atraumatic Extraction System: A Clinical StudyFebri YolandaNo ratings yet
- Endodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarDocument6 pagesEndodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarGunjan GargNo ratings yet
- Laser in ProsthodonticsDocument84 pagesLaser in ProsthodonticsmarwaNo ratings yet
- Frenectomy1 PDFDocument5 pagesFrenectomy1 PDFEdi NugrohoNo ratings yet
- Laser in Fixed ProsthodonticsDocument6 pagesLaser in Fixed Prosthodontics2oclock0% (1)
- Comparison of Techniques of Closed Reduction - Arch Bar VersusDocument3 pagesComparison of Techniques of Closed Reduction - Arch Bar Versus6hd6mnrzw2No ratings yet
- Leukoplakia Removal by Carbon Dioxide Laser (CO) Laser: Case ReportDocument3 pagesLeukoplakia Removal by Carbon Dioxide Laser (CO) Laser: Case ReportDeasireeNo ratings yet
- Cap 4Document16 pagesCap 4Elena DimitriuNo ratings yet
- Recent Advances in Laser TechnologyDocument5 pagesRecent Advances in Laser TechnologyIOSRjournalNo ratings yet
- Cirugía EndodonticaDocument23 pagesCirugía Endodonticajaimerendon0978No ratings yet
- Radiation Prosthesis For Improving The Life of Cancer PatientsDocument2 pagesRadiation Prosthesis For Improving The Life of Cancer PatientsDr FarhatNo ratings yet
- 1 s2.0 S001185322200012XDocument19 pages1 s2.0 S001185322200012XDANTE DELEGUERYNo ratings yet
- 10 1016@j Oooo 2020 03 048Document11 pages10 1016@j Oooo 2020 03 048Arthur CésarNo ratings yet
- 03 DB 05Document3 pages03 DB 05manikantatssNo ratings yet
- Photobio-Root ResorptionDocument9 pagesPhotobio-Root Resorptionhassankhan9849No ratings yet
- FrenectomiaDocument5 pagesFrenectomiasilpayNo ratings yet
- pg70-71 Periodontal ManagementDocument2 pagespg70-71 Periodontal ManagementJackie CooperNo ratings yet
- Jurnal Laser GingivectomyDocument6 pagesJurnal Laser GingivectomyFajar RamadhanNo ratings yet
- Yu 그리고 Qiu - 2018 - Efficacy of the split-thickness labial flap methodDocument6 pagesYu 그리고 Qiu - 2018 - Efficacy of the split-thickness labial flap methodsupercool0120No ratings yet
- Exito de mt y complicaciones (2019).pdfDocument7 pagesExito de mt y complicaciones (2019).pdfNicolás ValenzuelaNo ratings yet
- Successful Management of Lip and Oral Venous VaricDocument5 pagesSuccessful Management of Lip and Oral Venous VaricAna BarbosaNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- The Hand Test FinalDocument22 pagesThe Hand Test Finaltaylor alison swiftNo ratings yet
- Digital Image Processing - S. Jayaraman, S. Esakkirajan and T. VeerakumarDocument4 pagesDigital Image Processing - S. Jayaraman, S. Esakkirajan and T. VeerakumarBenedict IsaacNo ratings yet
- Portfolio Output No. 17: Reflections On Personal RelationshipsDocument3 pagesPortfolio Output No. 17: Reflections On Personal RelationshipsKatrina De VeraNo ratings yet
- Nes D2188Document6 pagesNes D2188prasannaNo ratings yet
- Perfecto Floresca Vs Philex Mining CorporationDocument11 pagesPerfecto Floresca Vs Philex Mining CorporationDelsie FalculanNo ratings yet
- The Madmullah of Somaliland 1916 1921Document386 pagesThe Madmullah of Somaliland 1916 1921Khadar Hayaan Freelancer100% (1)
- B412 TM Vol 1 Bell 412 EPDocument288 pagesB412 TM Vol 1 Bell 412 EPAri100% (1)
- Hanson Uk Cracked ConcreteDocument1 pageHanson Uk Cracked ConcreteAhmed Daahir AdenNo ratings yet
- Waterfront Regeneration As A Sustainable Approach To City Development in MalaysiaDocument10 pagesWaterfront Regeneration As A Sustainable Approach To City Development in MalaysiaРадоњић МајаNo ratings yet
- Assessment of Digestive and GI FunctionDocument23 pagesAssessment of Digestive and GI FunctionSandeepNo ratings yet
- Explore (As) : Types of Commission and InterestsDocument4 pagesExplore (As) : Types of Commission and InterestsTiffany Joy Lencioco GambalanNo ratings yet
- Swelling Properties of Chitosan Hydrogels: David R Rohindra, Ashveen V Nand, Jagjit R KhurmaDocument4 pagesSwelling Properties of Chitosan Hydrogels: David R Rohindra, Ashveen V Nand, Jagjit R KhurmaSeptian Perwira YudhaNo ratings yet
- Hemispheric Structure and FuctionDocument4 pagesHemispheric Structure and FuctionDebby RizkyNo ratings yet
- 2022421593543深圳大学成人高等教育本科生学士学位英语水平考试样卷Document9 pages2022421593543深圳大学成人高等教育本科生学士学位英语水平考试样卷nova yiNo ratings yet
- Kawng - Ha Leh Kawng Hlunte: Kristian - Halai Pawl ThiltumteDocument4 pagesKawng - Ha Leh Kawng Hlunte: Kristian - Halai Pawl ThiltumteChanmari West Branch KtpNo ratings yet
- The Masonic ManualDocument9 pagesThe Masonic ManualCrispin M. KaikaiNo ratings yet
- Of Mice and Men EssayDocument7 pagesOf Mice and Men Essayjon782No ratings yet
- Gayatri MantraDocument2 pagesGayatri MantraAnandh ShankarNo ratings yet
- MAN0019215 - TaqPathCOVID-19 - CE-IVD - RT-PCR Kit - IFUDocument27 pagesMAN0019215 - TaqPathCOVID-19 - CE-IVD - RT-PCR Kit - IFUFe LipeNo ratings yet
- GE 8-Ethics-Study-Guide-for-Module-2-Updated - 09192022Document12 pagesGE 8-Ethics-Study-Guide-for-Module-2-Updated - 09192022Baybayan, Alyssa MaeNo ratings yet
- Resource AllocationDocument10 pagesResource AllocationZoe NyadziNo ratings yet
- Ruq Abdominal PainDocument55 pagesRuq Abdominal PainriphqaNo ratings yet
- Mod Jeemain - GuruDocument31 pagesMod Jeemain - Guruparamarthasom1974No ratings yet
- Capr-Iii En4115 PDFDocument49 pagesCapr-Iii En4115 PDFYT GAMERSNo ratings yet
- Gauss Contest: Canadian Mathematics CompetitionDocument4 pagesGauss Contest: Canadian Mathematics CompetitiongzboyzoneNo ratings yet
- Goetic Spells by SkipDocument3 pagesGoetic Spells by SkipPhil DanielsNo ratings yet
- Better Get 'It in Your SoulDocument4 pagesBetter Get 'It in Your SoulJeremiah AnnorNo ratings yet
- Renesas Application Note AN1340Document6 pagesRenesas Application Note AN1340Rip_BarNo ratings yet
Using Diode Laser For Soft Tissue Incision of Oral Cavity: Case Report
Using Diode Laser For Soft Tissue Incision of Oral Cavity: Case Report
Uploaded by
Andhika GilangOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Using Diode Laser For Soft Tissue Incision of Oral Cavity: Case Report
Using Diode Laser For Soft Tissue Incision of Oral Cavity: Case Report
Uploaded by
Andhika GilangCopyright:
Available Formats
Case Report
Using Diode Laser for Soft Tissue Incision of Oral Cavity
1 1 1 2
Reza Amid , Mahdi Kadkhodazadeh , Mohammad Reza Talebi Ardakani , Somayeh Hemmatzadeh
2 2 2
Soheil Refoua , Parastoo Iranparvar , Anahita Shahi
1
Dental Research Center, Department of Periodontics, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2
School of Dentistry, Department of Periodontics, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract:
Introduction: The purpose of this case report is to analyze the results of vestibuleplasty
around an over-denture based on dental implants to determine the evidence on the
effectiveness of laser-assisted surgery and soft tissue management in implant dentistry. Case
Report: The patient in this case report was a 57 year- old male who was completely
edentulous, with a mandibular over denture based on 4 standard implants suffering from pain
on chewing, and a general discomfort, especially in anterior segment. He received a standard
gingival augmentation surgery which failed to create sufficient vestibular depth. A laser-
assisted vestibuloplasty was done to make the environment suitable for making a new
overdenture.
Conclusions: There were clinically significant improvements in vestibular depth and peri
implant soft tissue situation by laser. Also, bleeding during surgery was well controlled; the
patient’s discomfort and pain were less than the first operation done with gingival graft.
Based on our clinical data and review of the literature, an evidence- based approach to the
use of lasers for the management of soft tissue in oral surgery is necessary. Simply, there is
insufficient evidence to suggest that any specific wavelength of laser is superior to the
traditional modalities of therapy. However, improved hemostasis and patient’s satisfaction
can be considered as advantages of adjunctive laser therapy in some clinical situations like
vestibuloplasty.
Keywords: diode Laser; overdenture; vestibuloplasties
Please cite this article as follows:
Amid R, Kadkhodazadeh M, Talebi MR, Hemmatzadeh S, Refoua S, Iranparvar P, Shahi A. Using Diode Laser for Soft Tissue
Incision of Oral Cavity: J Lasers Med Sci 2012; 3(1):36-43
*Corresponding Author: Mahdi Kadkhodazadeh, DDS, MS; Department of Periodontics, Shahid Beheshti University of Medical
Sciences, Tehran, Iran; Tel: +98-912-760-8346; Fax: +98-21-2219-0224; Email: kadkhodazadehmahdi@yahoo.com
location or the fear of the noises coming from devices,
Introduction
such as scaling instruments. On the other hand, using
Dentistry has seen many great improvements in the scalpels is easy, but these instruments fail to make
field of instruments through years. Many instruments hemostasis in the surgical site (1). More or less,
have been invented for performing incisions, scaling, different lasers may be able to reduce patients’ fear
root planning, etc. However, there has always been a and pain and also can make great hemostasis in the
concern in patients regarding these instruments. For surgery field besides many other benefits.
example, fear of the pain from incision by scalpel in
spite of anesthesia in The first laser was introduced by Maiman in
36 Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012
Diode Laser for Oral Cavity Soft Tissue Incision
1960 (2), who used ruby to make laser. After a implants which were constructed by O’ball abutments.
while,(Carbon Dioxide Laser) CO2 and Neodymium- He was suffering from pain on chewing and a general
Doped Yttrium Aluminium Garnet(Nd: YAG) lasers discomfort, especially in the anterior segment. He
were developed. In medical field, laser was first used could not use his prosthesis for the past three months,
for photocoagulation of retina in 1960 (3). Goldman and was only able to wear it during mastication and in
used lasers in dentistry in 1964 for the first time (3) . public. It was found that peri mucositis was present
In 1989, Myers published the first article about using around the soft tissue of two implants inserted in right
laser in periodontal surgery side; the area also showed bleeding on probing and
(3). However, in those years studies suggested that the tenderness (Figure 1a).The patient received a gingival
laser devices used for incision and ablation of soft augmentation surgery that was performed with free
tissues were not suitable for dental hard tissues and gingival graft obtained from keratinized palatal
finally Food and Drug Administration (FDA) allowed mucosa(Figure 1b). Searching in patient’s file
CO2, Nd: YAG, and diode lasers only for soft tissues documented in our department showed that the result
(3). Today, there are different types of lasers available was not acceptable, and the procedure had totally
for using in dentistry: CO2, Nd: YAG, Holmium failed to gain the sufficient vestibular depth. The
Yttrium Aluminium Garnet (Ho: YAG), (Erbium, colleagues working in prosthetic phase recommended
Chromium doped Yttrium Scandium Gallium Garnet) another operation to create sufficient space for the
Er,Cr: YSGG, Neodymium doped Yttrium Aluminum next overdenture (Figure 1c).
Perovskite (Nd: YAP), Gallium arsenide (GaAs)
(diode), and Argon(4).
Considering all aspects like his age, fear of surgery,
hypersensitivity, need for fast healing to prepare the
soft tissue as soon as possible, it was decided to
Soft Tissue Surgical Applications of Lasers
perform vestibuloplasty with soft tissue laser (14).
In comparison with conventional scalpel, laser has The laser wavelength was 810 nm and it was set in a
many benefits, such as ease of soft tissue ablation, continuous wave mode at a power output of 2.5 watt
hemostasis (5), instant sterilization, reduced with a 0.3-mm diameter fiber tip (Doctor Smile Diode
bacteremia, little wound contraction, reduced edema, Laser, Italy). The tip was directed at an angle of 10 to
minimal scar, reduced mechanical trauma, less 15 degrees to the tissue; and was applied continuously
operative and post-operative pain (6-8), increased for 5 minutes till the approvable vestibular depth was
patients’ acceptance (6), no or few sutures, no need achieved. There was no significant bleeding during, or
for topical anesthesia (9). Thus, different dental lasers immediately after the surgery (Figure 2).
are being widely used for gingival soft tissue
procedures including gingivectomy, frenectomy, The local anesthesia used before laser irradiation
gingivoplasty, epulis, or benign tumor removal (5), was minimal, and the patient’s discomfort after
gingival depigmentation, second stage exposure of surgery was limited and managed with mouthwash
dental implants, irradiation of aphtus ulcers, chlorhexidine. No additional analgesic or antibiotic
coagulation of free gingival graft donor sites (6), and was recommended. Suturing was done at the apical
soft tissue crown-lengthening part of margin in order to prevent from muscular
(5) . Vascular lesions, such as hemangioma, should be reattachment. We used periosteal penetration
approached with caution. Incisional biopsies are not technique and sutures to reduce the muscle tension
allowed, but smaller lesions, particularly those during the healing phase. In most clinical cases,
affecting the lip are best ablated with either laser or sutures would not be used, because of excellent
cryosurgery (10). hemostasis achieved with dental lasers. The secondary
wound closure was covered with sponge gauze soaked
in tetracycline ointment. Two weeks later, a new
Case Report
overdenture was made and delivered to the patient.
The patient presented here was a 57 year- old male The patient was satisfied, and the retention of final
who was completely edentulous, with a mandibular prosthesis was great well due to deep vestibule.
over denture based on 4 screw type
Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012 37
Diode Laser for Oral Cavity Soft Tissue Incision
B
Figure 1 . (A) Insufficient keratinized soft tissue and narrow vestibule
around dental implants supporting an overdenture. Peri impant
mucositis apparently exist. (B) Using free gingival graft to create some
attached and keratinized soft tissue. (C) Early healing of soft tissue
graft seems acceptable results. However, narrow vestibular depth made
the prosthesis phase difficult.
clinics. In some cases like in the patient described
Discussion
here, conventional augmentation procedures cannot be
Usages of lasers in periodontics include initial efficient enough to solve the problem. Excessive
periodontal therapy, implant therapy, root surface vestibuloplasty alone, or in combination with gingival
modification, osseous surgery and soft tissue surgery graft is recommended in order to prevent recurrent
(4). Need for creating a reasonable band of high muscle attachment. Narrow vestibular depth is
keratinized gingival/soft tissue around natural one of the most complicated situations for successful
teeth/dental implants is not a rare condition in gingival augmentation.
38 Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012
Diode Laser for Oral Cavity Soft Tissue Incision
A B
C D
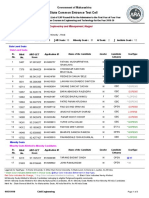
Figure 2. (A) Clinical situation exactly before second operation. (B) Laser-assisted vestibuloplasty using diode laser immediately after irradiation.
Excellent hemostasis can be observed. (C) Healing of the tissue around dental implants two weeks later. (D) Final overdenture could be made in an
easy way due to sufficient depth of vestibule in anterior segment.
Using dental lasers for vestibuloplasty has some of each tissue is specific, so the wavelength of the
clinical benefits during surgery like little bleeding outcome laser beam should be designed for each
with better access and less discomfort. Understanding tissue separately (3). A comprehensive review of
of the mechanisms and different effects of routine available data in soft tissue surgery by different dental
dental lasers is necessary before clinical use. By lasers is calculated in Table 1.
striking the laser beam to a material, four results may In brief, CO2 laser was effective in achieving
occur for the laser beam: absorption, reflection, hemostasis by vessel coagulation. (34). Less wound
scattering, and transmission. When striking the laser contraction occurs, because the CO2 laser does not
beam to living tissues, the beam is absorbed unless
remove the tissue collagen (8). Thus, the CO2 laser is
the penetration is so deep. In that situation the beam a useful instrument, which provides control of the
will be scattered. Conceiving many factors, the surgical field, esthetic and functional results (35). For
absorbed energy can cause heating, coagulation and CO2 laser, histological effects are related to the beam
incision. These factors include emitted wavelength, characteristics, rather than wavelength; greater
power (Watts), wave form (i.e. continues or pulsed), damage has been observed with the use of the
pulse duration, energy per pulse, energy density, constant wave mode (1) . The least risk of unwanted
duration of exposure, peak power of pulse, angulation thermal damage can be achieved with very short
of energy delivery to the target surface, and optical pulses at the highest power density for the shortest
properties of tissue (e.g. factors such as pigmentation, time possible (11).
water content, mineral content, etc.). The energy In the case presented here, we used laser beam
absorption degree around dental implants. Some clinicians have
considerations for side effects of irradiation of
Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012 39
Diode Laser for Oral Cavity Soft Tissue Incision
Table 1. Review of published data in using dental lasers for different kinds of soft tissue incisions.
Author/year Method/clinical application Laser type Conclusion
1 Wilder-Smith Soft tissue incision (oral mucosa CO2 Thermal and histologic results were related to
et al 1995 (11) of pig’s mandible) parameters and beam characteristics rather than
wavelength.
2 Rizoiu et al 1996 mucocutanous soft tissues Er,Cr:YSGG Minimal edge coagulation artifact observed. minimal
(12) incision to no hemorrhage and re-epithelialization and
collagenization were found to occur by day 7 in both
laser and conventional groups.
3 White et al 1998 Excision of oral mucosa CO2 and Nd:YAG Laser excision was well tolerated by patients, All
(9) lesions(leukoplakia,lichen patients healed post surgically with no loss of
planus, squamous papilloma, function, minimal postoperative pain, conservative
pyogenic granuloma,…) site-specific minimally invasive surgeries, and
elimination of need for sutures.
4 Goharkhay et al Soft tissue incision Diode laser (810 nm/0.5- Remarkable cutting ability and the tolerable damage
1999 (1) 15 w/pulse rate of 2-32 zone. Excellent coagulation ability, useful alternative
msec/1.5-250 Hz) in soft-tissue surgery of the oral cavity.
5 Neiburger et al gingival flap incisions 1.4 mw helium-neon (670 helium-neon diode lasers, at the mentioned energy
1999 (13) nm) diode laser for 30 level, increase the rate of gingival wound healing in
seconds (fluence = 0.34 69 percent of patients, without any side effects.
J/cm2).
6 Wilcox et al Use of electrosurgery and lasers a unipolar electrosurgical Use of the unipolar electrosurgical unit should be
2001 (14) in the presence of dental unit, a bipolar avoided, while judicious use of both the bipolar unit
implants (in vitro study) electrosurgical unit, and or the laser unit should produce temperature profiles
Nd:YAG. well within clinical limits.
7 Gontijo et al labial frenectomy in infant diode (810 nm) and a combined technique is suggested: using the diode
2005 (15) patients. Er:YAG laser in soft tissues and the Er:YAG laser in
periosteal bone tissues and for removal of final
collagen fibers.
8 Haytac et al 2006 frenectomy CO2 Compared with scalpel technique it shows
(16) less postoperative pain and fewer functional
complications (speaking and chewing). required
fewer analgesics. safe, effective, acceptable, and
impressive alternative for frenectomy operations.
9 Boj et al 2007 Squamous cell papilloma Er,Cr:YSGG laser No pain medication was required after surgery, wound
(17) removal in the pediatric dental healing was excellent and rapidly achieved. The oral
office. pathology report confirmed the pre surgical clinical
diagnosis.
10 D’Arcangelo et incisions in rat oral tissue diode (808 nm) Diode laser tends to produce more pronounced
al 2007 (18) changes than conventional scalpel surgical procedure
(due to tissue thermal damage), with corresponding
greater inflammatory reaction and delay in tissue
organization only at the initial stage.
11 Shetty et al2008 Maxillary frenectomy in a CO2 A successful case of a maxillary labial frenectomy in a
(19) pediatric patient. pediatric patient .
12 Capodiferro S et excision of fibrolipoma of the Diode the diode laser is undoubtedly a good alternative to
al 2008 (20) lip conventional surgery. possibility of avoiding direct
suture is surely helpful in aesthetic areas.
13 Boj et al 2009 Lower lip mucocele treatment Er:YAG The wound healed excellently and rapidly without
(21) sutures. No relapse was observed a year after the
surgery.
14 Iseri et al 2009 Treatment of epulis fissuratum CO2 Minimal damage to surrounding tissue.
(22) and prosthetic rehabilitation in
patients with vesiculobullous
disease.
15 De Arruda Paes- Treatment of epulis fissuratum CO2 Good haemostasis, no infection, post-operative
Junior et al comfort, esthetic and functional aspects immediately
2010 (23) reestablished.
16 Tuncer et al 2010 Intra oral soft tissue excisional CO2 Minimal interoperative and postoperative
(24) biopsies complications , good pain control.
40 Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012
Diode Laser for Oral Cavity Soft Tissue Incision
Table 1. (Continue)
Author/year Method/clinical application Laser type Conclusion
17 Cercadillo- In vitro study on porcine oral CO2 (1w, 2w, 10w, 20w)- The wavelength of each laser determines the
Ibarquren et al mucosa samples, evaluation of Diode(2w, 5w, 10w absorption rate of every tissue and the thermal effect
2010 (25) thermal damage pulsed)-Er,Cr:YSGG
(1w with & without
water/air spray, )
18 Vescovi et al Hyperplastic fibroepithelial Nd:YAG (3.5 w, 60 Hz) Better incision quality and less width of overall tissue
2010(26) lesions excision.(buccal and Nd:YAG (5w, 30 injuries in use of higher frequency and lower power.
mucosa) Hz)
19 Jin et al 2010 Wound healing following Diode laser Er,Cr:YSGG Diode laser is considered a good cutting device for
(27) incision in guinea pig oral laser oral mucosa.
mucosa
20 Gomez-Santos et Irradiation of different implant CO2 (4 W) and an The acid-etched and sandblasted surfaces were those
al 2010 (28) surfaces ErCr:YSGG laser (1.5 most affected by the thermal changes.
W, pulsed mode)
21 De Oliveira Drug-induced gingival gallium-aluminum- A diode laser was used as an effective and safe method
Guare et al enlargement treatment arsenide (GaAlAs) to remove the patient’s overgrown gingival tissue in
2010 (29) (gingivectomy) diode laser a two year follow up.
22 Pedron et al 2010 Excision of mucocele of the high-intensity diode laser rapid, bloodless, and well accepted by patients.
(30) lower lip. Postoperative problems, discomfort, and scarring
were minimal.
23 Lee et al 2010 laser-aided circumferential Er:YAG laser ( 100 mJ, laser-aided procedures, when used at appropriate
(31) supracrestal fiberotomy 10 Hz); diode laser (808 laser settings, preserve the original morphology and
nm, 1.2 W,continuous chemical composition of cementum.
wave); and CO2 laser
(10.6 mm, 3 W).
24 Arnabat- second-stage implant surgery Er,Cr:YSGG laser minimized postoperative pain, and the time
Dominguez et in patients with insufficient to prosthetic rehabilitation was also shortened.
al 2010 (32) gingival attachment. The esthetic results were far superior, and no
complications were recorded.
25 Boj et al 2011 Crown lengthening, exposure Er,Cr:YSGG laser All cases healed satisfactorily and were followed up
(33) of an unerupted molar, lingual for 3 to 4 years.
and maxillary frenectomies,…
implant surfaces. According to Arnabat-Dominguez et damage were those irradiated with Er, Cr: YSGG laser
al application of Erbium, Chromium doped Yttrium using water/air spray, followed by CO2 and diode
Scandium Gallium Garnet (Er, Cr: YSGG) laser in the lasers (25). In addition, Vescovi et al showed that Nd:
nd
2 stage of implant surgery in patients, minimized YAG laser induced serious thermal effects in small
postoperative pain, and the time to prosthetic specimens (mean size < 7 mm) independently from
rehabilitation was also shortened. The esthetic results the frequency and power employed. Better incision
were far superior, and no complications were quality and less width of overall tissue injuries were
recorded (32). When the Er, Cr: YSGG was used with observed in the use of higher frequency and lower
a water spray, a decrease in temperature was observed power (26).
in all implants. The acid- etched and sandblasted There are different findings about the healing
surfaces were those most affected by the thermal process after using different dental lasers. Jin et al
changes. Er, Cr: YSGG laser with a water spray showed that CO 2 laser leads to less tissue damage
applied to the sealing cap, or the coronal zone of the than a scalpel or Er,Cr:YSGG laser. (27) D’Arcangelo
implants does not generate thermal increments in the et al. evaluated that diode laser at a power output of 6
apical surface capable of adversely affecting W showed the worst results of tissue repair, especially
osseointegration and the integrity of the peri-implant after 7 days. On the contrary, the extent of epithelial
bone tissue (28). damage lateral to the wound edge and the extent of
Cercadillo _Ibarguren et al histologically evaluated collagen denaturation were near equal with scalpel
the thermal damage produced in soft tissue by CO2, incision and laser irradiation at 4 W after 14 days.
Er, Cr: YSGG and diode lasers and showed that the There was a greater concentration of endothelial nitric
samples with lowest thermal
Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012 41
Diode Laser for Oral Cavity Soft Tissue Incision
oxide synthase (eNOS) and inducible nitric oxide 8. Luomanen M, Meurman JH, Lehto VP. Extracellular matrix
synthase (iNOS) after 7 days of laser surgical in healing co2 laser incision wound. J Oral Pathol.
1987;16(6):322-31.
procedure. Diode laser tends to produce more
9. White JM, Goodis HE, Rose CL. Use of pulsed Nd;YAG
pronounced changes than conventional scalpel
laser for intraoral soft tissue surgery. Lasers Surg Med.
surgical procedure (due to tissue thermal damage), 1991;11(5):455-61.
with corresponding greater inflammatory reaction and 10. Oliver RJ, Sloan P, Pemberton MN. Oral Biopsies: methods
delay in tissue organiza tion only at the initial stage and applications. Br Dent J. 2004; 196(6):329-33.
(18). 11. Wilder-Smith P, Arrastia AM, Liaw LH, Berns M. Incision
properties and thermal effects of three CO2 lasers in soft
tissue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
Conclusion 1995;79(6):685-91.
Because of their rapid operations and regular 12. Rizoiu IM, Eversole LR, Kimmel AI. Effects of an erbium,
chromium: yttrium, scandium, gallium, garnet laser on
wound healing without sutures, lasers apply a great
mucocutanous soft tissues. Oral Surg Oral Med Oral Pathol
technology and are useful for soft tissue surgery in Oral Radiol Endod. 1996;82(4):386-95.
modern dentistry. In spite of all these advantages of 13. Neiburger EJ. Rapid healing of gingival incisions by the
using lasers in soft tissue incisions, there are not helium-neon diode laser. J Mass Dent Soc. 1999;48(1):8-13,
enough data to support the theory of reducing the 40.
healing time using lasers. Cost and the site of the laser 14. Wilcox CW, Wilwerding TM, Watson P, Morris JT. Use of
device may be the biggest obstacles for its routine electrosurgery and lasers in the presence of dental implants.
Int J Oral Maxillofac Implants. 2001;16(4):578-82.
application.
15. Gontijo I, Navarro RS, Haypek P, Ciamponi AL, Haddad
Acknowledgments AE. The applications of diode and Er:YAG lasers in labial
frenectomy in infant patients. J Dent Child (Chic).
The study was supported by a grant from the 2005;72(1):10-5.
Dental Research Center, Shahid Beheshti University 16. Haytac MC, Ozcelik O. Evaluation of patient perceptions
of Medical Sciences. after frenectomy operations: a comparison of carbon dioxide
laser and scalpel techniques. J Periodontol.
2006;77(11):1815-9.
Conflicts of Interest and Source of Funding: 17. Boj JR, Hernandez M, Espasa E, Poirier C. Laser treatment
of an oral papilloma in the pediatric dental office: a case
none declared report. Quintessence Int. 2007;38(4):307-12.
18. D’Arcangelo C, Di Nardo Di Maio F, Prosperi GD, Conte E,
Baldi M, Caputi S. A preliminary study of healing of diode
References laser versus scalpel incisions in rat oral tissue: a comparison
of clinical, histological, and immunohistochemical results.
1. Goharkhay K, Moritz A, Wilder-Smith P, Schoop U, Kluger Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
W, Jakolitsch S, et al. Effects on oral soft tissue produced by 2007;103(6):764-73.
a diode laser in vitro. Lasers Surg Med. 1999;25(5):401-6.
19. Shetty K, Trajtenberg C, Patel C, Streckfus C. Maxillary
frenectomy using a carbon dioxide laser in a pediatric
2. Maiman TH. Stimulated optical radiation in ruby. Nature.
patient: a case report. Gen Dent. 2008;56(1):60-3.
1960;187:493-4.
20. Capodiferro S, Maiorano E, Scarpelli F, Favia G.
3. Mahajan A. Lasers in periodontics-a review. Eur J Dent Fibrolipoma of the lip treated by diode laser surgery: a case
Med. 2011;3:1-11. report. J Med Case Reports. 2008;2:301.
4. Bains VK, Gupta S, Bains R. Lasers in periodontics: An 21. Boj JR, Poirier C, Espasa E, Hernandez M, Espanya A.
Overview. J Oral Health Community Dent. 2010;4:29-34. Lower lip mucocele treated with an erbium laser. Pediatr
5. Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM, Dent. 2009;31(3):249-52.
Izumi Y. Application of laser in periodontics: true 22. Işeri U, Ozçakir-Tomruk C, Gürsoy-Mert H. Treatment
innovation or myth? Periodontol 2000. 2009;50:90-126. of epulis fissuratum with CO2 laser and prosthetic
6. Cobb CM. Lasers in peroidontics:a review of the literature. J rehabilitation in patients with vesiculobullous disease.
Peridontol. 2006;77(4):545-64. Photomed Laser Surg. 2009;27(4):675-81.
7. Wigdor HA, Walsh JT Jr, Featherstone JDB, Virsuri SR, 23. de Arruda Paes-Junior TJ, Cavalcanti SC, Nascimento DF,
Fried D, Waldvogel JL. Lasers in dentistry. Lasers Surg Saavedra Gde S, Kimpara ET, Borges AL, et al. CO(2) laser
Med. 1995;16(2):103-33. surgery and prosthetic management for the treatment
42 Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012
Diode Laser for Oral Cavity Soft Tissue Incision
of epulis fissuratum. ISRN Dent. 2011;2011:282361. enlargement: biofilm control and surgical therapy with
24. Tuncer I, Ozçakir-Tomruk C, Sencift K, Cöloğlu S. gallium-aluminum- arsenide (GaAlAs) diode laser-A 2-year
Comparison of conventional surgery and CO2 laser on follow-up. Spec Care Dentist. 2010;30(2):46-52.
intraoral soft tissue pathologies and evaluation of the 30. Pedron IG, Galletta VC, Azevedo LH, Corrêa L. Treatment
collateral thermal damage. Photomed Laser Surg. of mucocele of the lower lip with diode laser in pediatric
2010;28(1):75-9. patients: presentation of 2 clinical cases. Pediatr Dent.
25. Cercadillo-Ibarguren I, Espana Tost A, Arnabat-Dominguez 2010;32(7):539-41.
J, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. 31. Lee JW, Park KH, Chung JH, Kim SJ. Effects of laser-aided
Histologic evaluation of thermal damage produced on soft circumferential supracrestal fiberotomy on root surfaces.
tissues by CO2, Er,Cr: YSGG and diode lasers. Med Oral Angle Orthod. 2011;81(6):1021-7.
Patol Oral Cir Bucal. 2010;15(6):912-8. 32. Arnabat-Domínguez J, Bragado-Novel M, España-Tost AJ,
26. Vescovi P, Corcione L, Meleti M, Merigo E, Fornaini C, Berini-Aytés L, Gay-Escoda C. Advantages and esthetic
Manfredi M, et al. Nd:YAG laser versus traditional scalpel. results of erbium, chromium:yttrium-scandium-gallium-
A preliminary histological analysis of specimens from the garnet laser application in second-stage implant surgery in
human oral mucosa. Lasers Med Sci. 2010;25(5):685-91. patients with insufficient gingival attachment: a report of
27. Jin JY, Lee SH, Yoon HJ. A comparative study of wound three cases. Lasers Med Sci. 2010;25(3):459-64.
healing following incision with a scalpel, diode laser or 33. Boj JR, Poirier C, Hernandez M, Espassa E, Espanya A.
Er,Cr:YSGG laser in guinea pig oral mucosa: A histological Case series: laser treatments for soft tissue problems in
and immunohistochemical analysis. Acta Odontol Scand. children. Eur Arch Paediatr Dent. 2011;12(2):113-7.
2010;68(4):232-8. 34. Kardos TB, Holt T, Ferguson MM. Histological evaluation
28. Gómez-Santos L, Arnabat-Domínguez J, Sierra-Rebolledo of the effect of a miniature CO2 laser on oral mucosa. Int J
A, Gay-Escoda C. Thermal increment due to ErCr:YSGG Oral Maxillofac surg. 1989;18(2):117-20.
and CO2 laser irradiation of different implant surfaces. A 35. Niccoli-Filho W, Murilo-Santos L, Schubert M, Morosolli
pilot study. Med Oral Patol Oral Cir Bucal.
AC. Treatment of developmental defect of upper lip with
2010;15(5):e782-7.
CO2 laser radiation: First surgical time. J Cosmet Laser
29. De Oliveira Guaré R, Costa SC, Baeder F, de Souza Merli Ther. 2005;7(2):97-100.
LA, Dos Santos MT. Drug-induced gingival
Journal of Lasers in Medical Sciences Volume 3 Number 1 Winter 2012
PDF to Word 43
You might also like
- Cockney MonologuesDocument2 pagesCockney MonologuesLaReceHawkins86% (7)
- Samhita SarangadharaDocument4 pagesSamhita SarangadharavatsalabaluNo ratings yet
- 5897 PDFDocument8 pages5897 PDFMohamad BasofiNo ratings yet
- 7 TH JC PDF - SindhuDocument5 pages7 TH JC PDF - SindhuDadi SindhuNo ratings yet
- Correcting Labial Thick and High ATTACHED FRENUM (Clinical Observation)Document3 pagesCorrecting Labial Thick and High ATTACHED FRENUM (Clinical Observation)NisatriaNo ratings yet
- Dentistry Oraldisorders Therapy30Document6 pagesDentistry Oraldisorders Therapy30muhammadNo ratings yet
- Idjsr Se 0168Document4 pagesIdjsr Se 0168Alfan MaulanaNo ratings yet
- Epulis 34465Document4 pagesEpulis 34465Ismail YusufNo ratings yet
- Scalpel Versus Diode Laser For Gingival Depigmentation: A Case ReportDocument8 pagesScalpel Versus Diode Laser For Gingival Depigmentation: A Case ReportIJAR JOURNALNo ratings yet
- 28 Tripty RahangdaleDocument16 pages28 Tripty RahangdaleDrShweta SainiNo ratings yet
- Chen DT Reprint1Document2 pagesChen DT Reprint1Dr.O.R.GANESAMURTHINo ratings yet
- J Lasers Med Sci 2012 3 1 26 32Document7 pagesJ Lasers Med Sci 2012 3 1 26 32Muhammad AbazaNo ratings yet
- اخيرDocument40 pagesاخيرAbas HamzaNo ratings yet
- Application of Lasers in Dentistry 22 25Document4 pagesApplication of Lasers in Dentistry 22 25SkAliHassanNo ratings yet
- Diode Laser Assisted For The Excision of Focal Epithelial Hyperplasia. Case ReportDocument5 pagesDiode Laser Assisted For The Excision of Focal Epithelial Hyperplasia. Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Lasers in Dental ImplantologyDocument18 pagesLasers in Dental ImplantologyErty TyuuNo ratings yet
- Lasers in Prosthetic Dentistry: Medical ScienceDocument3 pagesLasers in Prosthetic Dentistry: Medical Science2oclockNo ratings yet
- Contentserver - AspDocument7 pagesContentserver - AspcasillarodrigoNo ratings yet
- Lasers in Dental ImplantologyDocument17 pagesLasers in Dental ImplantologyIulian CosteanuNo ratings yet
- High-Power Diode Laser Use On Fordyce Granule Excision: A Case ReportDocument4 pagesHigh-Power Diode Laser Use On Fordyce Granule Excision: A Case ReportPauly JinezNo ratings yet
- Research ArticleDocument5 pagesResearch ArticleAtul ScNo ratings yet
- Lasers in Oral and Maxillofacial Surgery.Document28 pagesLasers in Oral and Maxillofacial Surgery.Sukhvinder Singh Rana0% (1)
- Maxillary Labial Frenectomy by Using ConDocument6 pagesMaxillary Labial Frenectomy by Using ConShinta rahma MansyurNo ratings yet
- 9685 40464 1 PBDocument3 pages9685 40464 1 PBTri Sakti Sunda RomdhoniNo ratings yet
- Laser Applications in DentistryDocument13 pagesLaser Applications in DentistryrubytrangtoNo ratings yet
- Laser in Conservative DentistryDocument39 pagesLaser in Conservative DentistryAiluul AlmaaNo ratings yet
- Laser in Proctology: A New Hope in Treating The Distressing Anal Diseases EditorialDocument1 pageLaser in Proctology: A New Hope in Treating The Distressing Anal Diseases EditorialAmit MalikNo ratings yet
- Unusual Radiopacities Spotted in A Dental Radiograph: Case ReportDocument3 pagesUnusual Radiopacities Spotted in A Dental Radiograph: Case ReportlilaNo ratings yet
- Telaah THTDocument3 pagesTelaah THTila chaeruniNo ratings yet
- Piezoelectrico 2020 PDFDocument13 pagesPiezoelectrico 2020 PDFLucy Lobato RomeroNo ratings yet
- Anitua 2013Document9 pagesAnitua 2013Paul CerdaNo ratings yet
- Future of Laser Pediatric Dentistry PDFDocument5 pagesFuture of Laser Pediatric Dentistry PDFsnehasthaNo ratings yet
- Laser Assisted Crown Lengthening - A Multidisciplinary Approach: A ReviewDocument7 pagesLaser Assisted Crown Lengthening - A Multidisciplinary Approach: A ReviewpoojaNo ratings yet
- Morphology of Plans MCQDDocument8 pagesMorphology of Plans MCQDAneesa TafheemNo ratings yet
- Orthodntics MicroimplantsDocument11 pagesOrthodntics Microimplantsdruzair007No ratings yet
- Root Canal Treatment of A 32-mm Length Maxillary Canine - A Case ReportDocument4 pagesRoot Canal Treatment of A 32-mm Length Maxillary Canine - A Case ReportAndre ManaroinsongNo ratings yet
- Endo Don TicDocument8 pagesEndo Don TicArmareality Armareality100% (1)
- Lasers in Endodontics-A Review of Literature: P.A.Vasishta, K Anjaneyalu, Vinay Sivaswamy, K AnjaneyaluDocument7 pagesLasers in Endodontics-A Review of Literature: P.A.Vasishta, K Anjaneyalu, Vinay Sivaswamy, K AnjaneyaluKalpanaNo ratings yet
- Management of Limited Interocclusal Distance With The Aid of A Modified Surgical Guide: A Clinical ReportDocument5 pagesManagement of Limited Interocclusal Distance With The Aid of A Modified Surgical Guide: A Clinical ReporttovarichNo ratings yet
- Surgical Extrusion With An Atraumatic Extraction System: A Clinical StudyDocument7 pagesSurgical Extrusion With An Atraumatic Extraction System: A Clinical StudyFebri YolandaNo ratings yet
- Endodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarDocument6 pagesEndodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarGunjan GargNo ratings yet
- Laser in ProsthodonticsDocument84 pagesLaser in ProsthodonticsmarwaNo ratings yet
- Frenectomy1 PDFDocument5 pagesFrenectomy1 PDFEdi NugrohoNo ratings yet
- Laser in Fixed ProsthodonticsDocument6 pagesLaser in Fixed Prosthodontics2oclock0% (1)
- Comparison of Techniques of Closed Reduction - Arch Bar VersusDocument3 pagesComparison of Techniques of Closed Reduction - Arch Bar Versus6hd6mnrzw2No ratings yet
- Leukoplakia Removal by Carbon Dioxide Laser (CO) Laser: Case ReportDocument3 pagesLeukoplakia Removal by Carbon Dioxide Laser (CO) Laser: Case ReportDeasireeNo ratings yet
- Cap 4Document16 pagesCap 4Elena DimitriuNo ratings yet
- Recent Advances in Laser TechnologyDocument5 pagesRecent Advances in Laser TechnologyIOSRjournalNo ratings yet
- Cirugía EndodonticaDocument23 pagesCirugía Endodonticajaimerendon0978No ratings yet
- Radiation Prosthesis For Improving The Life of Cancer PatientsDocument2 pagesRadiation Prosthesis For Improving The Life of Cancer PatientsDr FarhatNo ratings yet
- 1 s2.0 S001185322200012XDocument19 pages1 s2.0 S001185322200012XDANTE DELEGUERYNo ratings yet
- 10 1016@j Oooo 2020 03 048Document11 pages10 1016@j Oooo 2020 03 048Arthur CésarNo ratings yet
- 03 DB 05Document3 pages03 DB 05manikantatssNo ratings yet
- Photobio-Root ResorptionDocument9 pagesPhotobio-Root Resorptionhassankhan9849No ratings yet
- FrenectomiaDocument5 pagesFrenectomiasilpayNo ratings yet
- pg70-71 Periodontal ManagementDocument2 pagespg70-71 Periodontal ManagementJackie CooperNo ratings yet
- Jurnal Laser GingivectomyDocument6 pagesJurnal Laser GingivectomyFajar RamadhanNo ratings yet
- Yu 그리고 Qiu - 2018 - Efficacy of the split-thickness labial flap methodDocument6 pagesYu 그리고 Qiu - 2018 - Efficacy of the split-thickness labial flap methodsupercool0120No ratings yet
- Exito de mt y complicaciones (2019).pdfDocument7 pagesExito de mt y complicaciones (2019).pdfNicolás ValenzuelaNo ratings yet
- Successful Management of Lip and Oral Venous VaricDocument5 pagesSuccessful Management of Lip and Oral Venous VaricAna BarbosaNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- The Hand Test FinalDocument22 pagesThe Hand Test Finaltaylor alison swiftNo ratings yet
- Digital Image Processing - S. Jayaraman, S. Esakkirajan and T. VeerakumarDocument4 pagesDigital Image Processing - S. Jayaraman, S. Esakkirajan and T. VeerakumarBenedict IsaacNo ratings yet
- Portfolio Output No. 17: Reflections On Personal RelationshipsDocument3 pagesPortfolio Output No. 17: Reflections On Personal RelationshipsKatrina De VeraNo ratings yet
- Nes D2188Document6 pagesNes D2188prasannaNo ratings yet
- Perfecto Floresca Vs Philex Mining CorporationDocument11 pagesPerfecto Floresca Vs Philex Mining CorporationDelsie FalculanNo ratings yet
- The Madmullah of Somaliland 1916 1921Document386 pagesThe Madmullah of Somaliland 1916 1921Khadar Hayaan Freelancer100% (1)
- B412 TM Vol 1 Bell 412 EPDocument288 pagesB412 TM Vol 1 Bell 412 EPAri100% (1)
- Hanson Uk Cracked ConcreteDocument1 pageHanson Uk Cracked ConcreteAhmed Daahir AdenNo ratings yet
- Waterfront Regeneration As A Sustainable Approach To City Development in MalaysiaDocument10 pagesWaterfront Regeneration As A Sustainable Approach To City Development in MalaysiaРадоњић МајаNo ratings yet
- Assessment of Digestive and GI FunctionDocument23 pagesAssessment of Digestive and GI FunctionSandeepNo ratings yet
- Explore (As) : Types of Commission and InterestsDocument4 pagesExplore (As) : Types of Commission and InterestsTiffany Joy Lencioco GambalanNo ratings yet
- Swelling Properties of Chitosan Hydrogels: David R Rohindra, Ashveen V Nand, Jagjit R KhurmaDocument4 pagesSwelling Properties of Chitosan Hydrogels: David R Rohindra, Ashveen V Nand, Jagjit R KhurmaSeptian Perwira YudhaNo ratings yet
- Hemispheric Structure and FuctionDocument4 pagesHemispheric Structure and FuctionDebby RizkyNo ratings yet
- 2022421593543深圳大学成人高等教育本科生学士学位英语水平考试样卷Document9 pages2022421593543深圳大学成人高等教育本科生学士学位英语水平考试样卷nova yiNo ratings yet
- Kawng - Ha Leh Kawng Hlunte: Kristian - Halai Pawl ThiltumteDocument4 pagesKawng - Ha Leh Kawng Hlunte: Kristian - Halai Pawl ThiltumteChanmari West Branch KtpNo ratings yet
- The Masonic ManualDocument9 pagesThe Masonic ManualCrispin M. KaikaiNo ratings yet
- Of Mice and Men EssayDocument7 pagesOf Mice and Men Essayjon782No ratings yet
- Gayatri MantraDocument2 pagesGayatri MantraAnandh ShankarNo ratings yet
- MAN0019215 - TaqPathCOVID-19 - CE-IVD - RT-PCR Kit - IFUDocument27 pagesMAN0019215 - TaqPathCOVID-19 - CE-IVD - RT-PCR Kit - IFUFe LipeNo ratings yet
- GE 8-Ethics-Study-Guide-for-Module-2-Updated - 09192022Document12 pagesGE 8-Ethics-Study-Guide-for-Module-2-Updated - 09192022Baybayan, Alyssa MaeNo ratings yet
- Resource AllocationDocument10 pagesResource AllocationZoe NyadziNo ratings yet
- Ruq Abdominal PainDocument55 pagesRuq Abdominal PainriphqaNo ratings yet
- Mod Jeemain - GuruDocument31 pagesMod Jeemain - Guruparamarthasom1974No ratings yet
- Capr-Iii En4115 PDFDocument49 pagesCapr-Iii En4115 PDFYT GAMERSNo ratings yet
- Gauss Contest: Canadian Mathematics CompetitionDocument4 pagesGauss Contest: Canadian Mathematics CompetitiongzboyzoneNo ratings yet
- Goetic Spells by SkipDocument3 pagesGoetic Spells by SkipPhil DanielsNo ratings yet
- Better Get 'It in Your SoulDocument4 pagesBetter Get 'It in Your SoulJeremiah AnnorNo ratings yet
- Renesas Application Note AN1340Document6 pagesRenesas Application Note AN1340Rip_BarNo ratings yet