Professional Documents
Culture Documents
Clonidine: Imidazoline Derivative, Partial
Clonidine: Imidazoline Derivative, Partial
Uploaded by
Asma Alfaouri0 ratings0% found this document useful (0 votes)
9 views2 pagesThis document summarizes different types of antiadrenergic drugs that are used to treat hypertension by inhibiting the sympathetic nervous system. It describes alpha blockers that work by blocking alpha-1 receptors to dilate blood vessels. It also discusses centrally-acting drugs like clonidine and methyldopa that work in the brain. Finally, it provides details on different types of beta blockers, including cardioselective beta blockers that preferentially block beta-1 receptors and nonselective beta blockers that block both receptor types.
Original Description:
Original Title
alphabeta
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes different types of antiadrenergic drugs that are used to treat hypertension by inhibiting the sympathetic nervous system. It describes alpha blockers that work by blocking alpha-1 receptors to dilate blood vessels. It also discusses centrally-acting drugs like clonidine and methyldopa that work in the brain. Finally, it provides details on different types of beta blockers, including cardioselective beta blockers that preferentially block beta-1 receptors and nonselective beta blockers that block both receptor types.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
9 views2 pagesClonidine: Imidazoline Derivative, Partial
Clonidine: Imidazoline Derivative, Partial
Uploaded by
Asma AlfaouriThis document summarizes different types of antiadrenergic drugs that are used to treat hypertension by inhibiting the sympathetic nervous system. It describes alpha blockers that work by blocking alpha-1 receptors to dilate blood vessels. It also discusses centrally-acting drugs like clonidine and methyldopa that work in the brain. Finally, it provides details on different types of beta blockers, including cardioselective beta blockers that preferentially block beta-1 receptors and nonselective beta blockers that block both receptor types.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 2
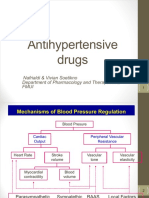
Antiadrenergics
• Inhibit activity of the sympathetic nervous system
• Effective in decreasing heart rate,force of myocardial contraction, cardiac output, and blood pressure
Alpha
• Alpha 1 adrenergics receptor blocking agents dilate vessels and Antiadrenergics-Alpha 1
decrease peripheral vascular resistance • Cardura (doxazosin)
• Can experience first dose phenomenon with orthostatic • Minipress (prazosin)
hypotension, dizziness, syncope,possible sodium and fluid retentin • Hytrin (terazosin)
Centrally-Acting Drugs
Alpha-Methyldopa: a prodrug Clonidine: Imidazoline derivative, partial
• Precursor of Dopamine and NA agonist of central alpha-2 receptor
• Methyldopa in adrenergic nerve • Not frequently used now because of tolerance and withdrawal
endings to α-methylNE, which stimulates α2-adrenoceptors receptors hypertension
in brain and causes inhibition of adrenergic discharge in medulla – fall • Clonidine rebound hypertension if suddenly withdrawn
in PVR and fall in BP
• in the medulla and decr sympathetic outflow.
Side-effect: drowsiness, hemolytic anemia.
cognitive impairement, postural hypotension
β
β-Blockers β-Blockers β-Receptors Cardioselective β-Blockers
• Inhibit renin release • Adverse effects: • Distributed throughout the • Greater affinity for β1 than β2
◦ weak association with ◦ bradycardia body ◦ concentrate differently in receptors ◦ inhibit β1 receptors at
antihypertensive effect ◦ atrioventricular conduction certain organs & low to moderate dose ◦ higher
• Negative chronotropic & abnormalities tissues doses block β2 receptors
inotropic cardiac effects reduce ◦ acute heart failure • β1 receptors: • Safer in patients with
CO ◦ abrupt discontinuation may ◦ heart, kidney ◦ stimulation bronchospastic
◦ β-blockers with intrinsic cause unstable increases HR, contractility, renin disease, peripheral arterial
sympathomimetic angina, myocardial infarction, & Release disease,diabetes ◦ may
at high enough doses activity death in patients with high • β2 receptors: exacerbate bronchospastic
(ISA) coronary disease risk ◦ lungs, liver, pancreas, arteriolar disease when selectivity lost at
do not reduce CO lower BP ◦ bronchospastic pulmonary smooth high doses
decrease peripheral resistance disease muscle ◦ dose where selectivity lost
◦ Membrane-stabilizing action on ◦ stimulation causes varies from patientto patient
cardiac cells bronchodilation
β-Blockers Nonselective β-Blockers
• Cardioselective • Inhibit β1 & β2 receptors at all doses
a ◦ atenolol, betaxolol, bisoprolol, metoprolol,nebivolol • Can exacerbate bronchospastic disease
• Nonselective • Additional benefits in:
◦ nadolol, propranolol, timolol ◦ essential tremor ◦ migraine headache ◦ thyrotoxicosis
• Intrinsic sympathomimetic activity ◦ acebutolol, carteolol,penbutolo • Nadolol, Propranolol
l, pindolol • Avoid in patients with reactive airways disease
• Mixed α- and β-blockers
◦ carvedilol, labetolol
Beta Blockers Side Effects
• Bronchospasm
• Diminished exercise capacity
• Negative inotropy
• Sexual dysfunction
• Bradyarrhythmia
• Masking of hypoglycemia
• Hair loss
You might also like
- MKSAP 17 Cardiovascular SystemDocument237 pagesMKSAP 17 Cardiovascular SystemFiaz medico80% (5)
- Test Bank CardioDocument16 pagesTest Bank CardioLudwigJayBarayuga86% (7)
- Dha & Scfhs ExamsDocument115 pagesDha & Scfhs Examsrayooona88100% (4)
- OA Case #Q1Document6 pagesOA Case #Q1Asma AlfaouriNo ratings yet
- Part 3: Pharmacology Antihypertensives: SympatholyticsDocument13 pagesPart 3: Pharmacology Antihypertensives: SympatholyticsJovelyn BandiolaNo ratings yet
- Anti HypertensivesDocument23 pagesAnti HypertensivesLeena AlateeqNo ratings yet
- Adrenergic AntagonistDocument30 pagesAdrenergic AntagonistOmar AlaamNo ratings yet
- Antihypertensive Drugs (2) - 092019Document33 pagesAntihypertensive Drugs (2) - 092019muntadhar5000No ratings yet
- 13 Beta Adrenoceptor BlockersDocument35 pages13 Beta Adrenoceptor BlockersanojanNo ratings yet
- 2.Ghafez-Adrenergic Antagonists 2023Document29 pages2.Ghafez-Adrenergic Antagonists 2023yasmin.rahmany03No ratings yet
- Terapi Farmakologi Gagal Jantung - Sept - 2020Document58 pagesTerapi Farmakologi Gagal Jantung - Sept - 2020FAUZAN ILHAM PRATAMANo ratings yet
- Antihypertensive Agents: Ayman Khdair Ph.D. Pharmaceutical Sciences Wayne State University, Michigan, USADocument15 pagesAntihypertensive Agents: Ayman Khdair Ph.D. Pharmaceutical Sciences Wayne State University, Michigan, USAJalil HaddadinNo ratings yet
- Cardiac Inotropes in Treatment of Heart Failure Fight (Autosaved)Document32 pagesCardiac Inotropes in Treatment of Heart Failure Fight (Autosaved)Insan IlmanNo ratings yet
- Week 5-14 Notes 2Document1 pageWeek 5-14 Notes 2navkkirangillNo ratings yet
- Pharma Unit 8 - Anti - Adrenergic Drugs - 2 of 2Document21 pagesPharma Unit 8 - Anti - Adrenergic Drugs - 2 of 2MIbrahimNo ratings yet
- Pharma Unit 1-2 Anti - Adrenergic DrugsDocument21 pagesPharma Unit 1-2 Anti - Adrenergic DrugsMIbrahimNo ratings yet
- Week 4 Cardiovascular and Renal Systems Ed 6-20-22Document117 pagesWeek 4 Cardiovascular and Renal Systems Ed 6-20-22sultanmsajidmNo ratings yet
- 1CVS-2. ACEIs 1435 PDFDocument19 pages1CVS-2. ACEIs 1435 PDFMuath AlqarniNo ratings yet
- SUMMARY Drugs Used in HypertensionDocument11 pagesSUMMARY Drugs Used in HypertensionPAULINE ANGELI DIEGONo ratings yet
- PH 1.13:BETA Blockers: Dr. Lavakumar S Professor Dept of Pharmacology SssmcriDocument31 pagesPH 1.13:BETA Blockers: Dr. Lavakumar S Professor Dept of Pharmacology SssmcriBeena ShajimonNo ratings yet
- Narsum 1. Peran Vasodilator Beta BlockerFinalDocument45 pagesNarsum 1. Peran Vasodilator Beta BlockerFinalTony RamirezNo ratings yet
- Cvs DrugsDocument106 pagesCvs DrugsIkoona ivanNo ratings yet
- Drug ClassDocument13 pagesDrug ClassEdfren Salazar Colon100% (1)
- Adrenergic Nervous System Drugs 2023 104DDocument36 pagesAdrenergic Nervous System Drugs 2023 104Djudd wilsonNo ratings yet
- Propranolol Drug StudyDocument1 pagePropranolol Drug Studycarbon.mariaauroraisabel.cNo ratings yet
- 41.antihypertensive DrugsDocument75 pages41.antihypertensive DrugspradeephdNo ratings yet
- Antihypertensive Drugs.Document35 pagesAntihypertensive Drugs.Abdul WahabNo ratings yet
- Adrenergics & Adrenergic BlockersDocument5 pagesAdrenergics & Adrenergic Blockersapi-3739910100% (4)
- Cardiac Medications TemplateDocument5 pagesCardiac Medications TemplateErinNo ratings yet
- Adrenergic Drugs: S. Parasuraman, M.Pharm., PH.D.Document25 pagesAdrenergic Drugs: S. Parasuraman, M.Pharm., PH.D.Zakaria salimNo ratings yet
- Antihypertensive AgentsDocument41 pagesAntihypertensive AgentsRwapembe StephenNo ratings yet
- Adrenergic DrugsDocument26 pagesAdrenergic DrugsManish ChoudharyNo ratings yet
- CVD and HTNDocument60 pagesCVD and HTNZsazsa100% (1)
- Antiadrenergic Drugs - II 24.07.018 PDFDocument25 pagesAntiadrenergic Drugs - II 24.07.018 PDFHitesh karnNo ratings yet
- PharmacologyDocument21 pagesPharmacologySophia Kyla AcerNo ratings yet
- Lecture 8 Heart FailureDocument38 pagesLecture 8 Heart Failureukashazam19No ratings yet
- β - BlockersDocument12 pagesβ - Blockersmohavi8169No ratings yet
- Vas Opressor 233Document55 pagesVas Opressor 233songsokalinNo ratings yet
- Drugs Acting On The Cardiovascular SystemDocument12 pagesDrugs Acting On The Cardiovascular Systemcleahis cruzNo ratings yet
- Vasoactive DrugsDocument14 pagesVasoactive DrugsTushar GhuleNo ratings yet
- 4 Adrenergic and Anti-Adrenergic DrugsDocument51 pages4 Adrenergic and Anti-Adrenergic DrugsLoai Mohammed IssaNo ratings yet
- ANS2Document16 pagesANS2yaya mohaNo ratings yet
- Antihypertensive Drugs: Loretta Walker, PH.DDocument11 pagesAntihypertensive Drugs: Loretta Walker, PH.DAdrian Jake LiuNo ratings yet
- Antihypertensives: Dr. Lucy ClunesDocument45 pagesAntihypertensives: Dr. Lucy ClunesZaqueo Gutierrez FajardoNo ratings yet
- ShockDocument19 pagesShockNitesh TiwariNo ratings yet
- Anoosha Roll#21Document19 pagesAnoosha Roll#21Anusha ZubairNo ratings yet
- Peripheral Vascular DisordersDocument4 pagesPeripheral Vascular DisordersDawnmurph Dharlene Wag-eNo ratings yet
- Penatalaksanaan Penyulit Gagal JantungDocument17 pagesPenatalaksanaan Penyulit Gagal JantungarumNo ratings yet
- Drugs of CvsDocument32 pagesDrugs of CvsAgus HaryantoNo ratings yet
- Chapter 11 Antihypertensive AgentsDocument11 pagesChapter 11 Antihypertensive AgentsChristine Annmarie TapawanNo ratings yet
- Antihypertensive DrugsDocument56 pagesAntihypertensive Drugssultan khabeebNo ratings yet
- Cardiovascular Pharmacology: Ana Sharmaine S. Uera, MD DR PJGMRMC Anesthesiology Department 1st Year ResidentDocument68 pagesCardiovascular Pharmacology: Ana Sharmaine S. Uera, MD DR PJGMRMC Anesthesiology Department 1st Year ResidentLalay CabanagNo ratings yet
- AntihipertensiDocument39 pagesAntihipertensiHarri HardiNo ratings yet
- Antianginal DrugsDocument19 pagesAntianginal DrugsAnusha ZubairNo ratings yet
- HTN JmiDocument39 pagesHTN Jmink999999No ratings yet
- HypertensionDocument43 pagesHypertensionAbin PNo ratings yet
- Pharm 3 eDocument3 pagesPharm 3 eravi2likeNo ratings yet
- Jake Drug StudyDocument9 pagesJake Drug StudyJake Yvan Dizon0% (1)
- Beta-Adrenergic Receptor AntagonistsDocument5 pagesBeta-Adrenergic Receptor AntagonistsKabwe BrandonNo ratings yet
- Antianginals Drugs DSDocument6 pagesAntianginals Drugs DSMademoiselle KayettyNo ratings yet
- Sympatholytic AgentsDocument17 pagesSympatholytic AgentsofficialdanieladejumoNo ratings yet
- Sympathetic Agonist and Antagonist 23Document12 pagesSympathetic Agonist and Antagonist 23PNo ratings yet
- Treatment of CHF: Therapeutic UsesDocument2 pagesTreatment of CHF: Therapeutic UsesAsma AlfaouriNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- AgonistDocument1 pageAgonistAsma AlfaouriNo ratings yet
- Antiplatelet Drugs Cyclooxygenase Inhibitors Aspirin: MOA Clinical UsesDocument3 pagesAntiplatelet Drugs Cyclooxygenase Inhibitors Aspirin: MOA Clinical UsesAsma AlfaouriNo ratings yet
- First Generation Agents Self-Injectables Drug Brand Name MOADocument1 pageFirst Generation Agents Self-Injectables Drug Brand Name MOAAsma AlfaouriNo ratings yet
- Treatment of CHF: Therapeutic UsesDocument2 pagesTreatment of CHF: Therapeutic UsesAsma AlfaouriNo ratings yet
- Lecture1-SystemsAnalysis 2 PDFDocument71 pagesLecture1-SystemsAnalysis 2 PDFAsma AlfaouriNo ratings yet
- Nclex NotesDocument12 pagesNclex NotesMary Rose Albior PaquibotNo ratings yet
- Antihypertensive Drug InteractionsDocument8 pagesAntihypertensive Drug InteractionsNur AzimahNo ratings yet
- التدريب الصيفي محلولهDocument129 pagesالتدريب الصيفي محلولهMohamed MosawiNo ratings yet
- Antihypertensive DrugsDocument5 pagesAntihypertensive DrugsAiman TymerNo ratings yet
- Lecture 24-25 - Antihypertensive AgentsDocument30 pagesLecture 24-25 - Antihypertensive AgentsJedoNo ratings yet
- Approach To Patient With HypertensionDocument64 pagesApproach To Patient With HypertensionAndrassy Twinkle AlineaNo ratings yet
- Chronic Renal Failure Lecture 3Document44 pagesChronic Renal Failure Lecture 3Toqa ElmansouryNo ratings yet
- Week 6 Hypertenesion and Heart FailureDocument86 pagesWeek 6 Hypertenesion and Heart Failureعزالدين الطيارNo ratings yet
- Pharmacology McqNEW 2Document7 pagesPharmacology McqNEW 2Ayman Ragab100% (2)
- Cardiovascular Medications NCLEX Practice QuizDocument8 pagesCardiovascular Medications NCLEX Practice QuizAngie MandeoyaNo ratings yet
- Module 8 PharmaDocument34 pagesModule 8 PharmaGin MananganNo ratings yet
- Autonomic DrugsDocument107 pagesAutonomic DrugsMaria Mercedes LeivaNo ratings yet
- SWT Pharmacology DamsDocument84 pagesSWT Pharmacology DamsvamshidhNo ratings yet
- Rational Drug Prescribing Training CourseDocument78 pagesRational Drug Prescribing Training CourseAhmadu Shehu MohammedNo ratings yet
- Medical Management of Symptomatic Aortic StenosisDocument10 pagesMedical Management of Symptomatic Aortic StenosisDAT TRANNo ratings yet
- CPG Management of Heart Failure (4th Ed) 2019Document161 pagesCPG Management of Heart Failure (4th Ed) 2019Muaz AbdullahNo ratings yet
- Drug Profile (Bisoprolol)Document16 pagesDrug Profile (Bisoprolol)Maryam KhushbakhatNo ratings yet
- Passmedicine 2021 Key Notes MRCP IIDocument79 pagesPassmedicine 2021 Key Notes MRCP IIzehra khowajaNo ratings yet
- Antiglaucoma DrugDocument18 pagesAntiglaucoma DrugFoungZanz D. LuffyzNo ratings yet
- Ainul Haq Report 2Document27 pagesAinul Haq Report 2Mohd AliNo ratings yet
- Questions PharmcologyDocument17 pagesQuestions Pharmcologylalitrajindolia100% (2)
- Wiysonge Et Al-2017-The Cochrane LibraryDocument97 pagesWiysonge Et Al-2017-The Cochrane LibraryAsmaa LabibNo ratings yet
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Document47 pagesPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageNo ratings yet
- Principles of Treatment of IhdDocument3 pagesPrinciples of Treatment of IhdArvinth Guna SegaranNo ratings yet
- Drugs Acting On CVS-2014Document36 pagesDrugs Acting On CVS-2014كسلان اكتب اسميNo ratings yet
- Isoprenaline Infusion 2016Document3 pagesIsoprenaline Infusion 2016Glory Claudia KarundengNo ratings yet
- Baveno 6Document29 pagesBaveno 6José Pepo Apey Reinoso100% (1)