Professional Documents
Culture Documents
Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!
Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!
Uploaded by
ayesha FalakCopyright:
Available Formats
You might also like
- Atlas of Gynecologic Surgical PathologyDocument581 pagesAtlas of Gynecologic Surgical PathologySandu Alexandra100% (4)
- Student Cell CommunicationDocument11 pagesStudent Cell Communicationapi-2620290510% (1)
- From Blue Nines and Red WordsDocument6 pagesFrom Blue Nines and Red Wordsabunour50% (4)
- List of Medicinal Plants and Their UsesDocument6 pagesList of Medicinal Plants and Their Usesshangiri75% (4)
- Original Research Abstract AFCC ASMIHA 2019Document82 pagesOriginal Research Abstract AFCC ASMIHA 2019Program Studi Kardiologi100% (1)
- Chughtai Lab Rate ListDocument33 pagesChughtai Lab Rate ListHassan Gill67% (9)
- Obstetrics and Gynaecology History Taking TemplateDocument4 pagesObstetrics and Gynaecology History Taking TemplateMaruti100% (3)
- Impact of Atropine and Aminophylline On TAVB With Inferior Wall MIDocument2 pagesImpact of Atropine and Aminophylline On TAVB With Inferior Wall MIRakhmat RamadhaniNo ratings yet
- Outcomes of Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction at Tehran Heart CenterDocument6 pagesOutcomes of Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction at Tehran Heart CenterHamiNo ratings yet
- 62 2020 Article 898Document7 pages62 2020 Article 898sinamirjaniNo ratings yet
- Ischemic 19Document8 pagesIschemic 19Adina Alexandra CNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofahmadto80No ratings yet
- F QRSDocument9 pagesF QRSaisyah hamzakirNo ratings yet
- Abstrak IsicamDocument22 pagesAbstrak IsicambgusjklNo ratings yet
- AggarwalDocument7 pagesAggarwalSuryaNo ratings yet
- Stenoza MitralaDocument7 pagesStenoza MitralaVerginia OnofreiNo ratings yet
- Manual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceDocument9 pagesManual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceArdiana FirdausNo ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDocument6 pagesPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- Therapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticDocument8 pagesTherapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticNITACORDEIRONo ratings yet
- Study 3Document7 pagesStudy 3OstazNo ratings yet
- Synopsis For DissertationDocument9 pagesSynopsis For DissertationahmedNo ratings yet
- 1 s2.0 S1933171109001302 MainDocument7 pages1 s2.0 S1933171109001302 MainRizky BafadhalNo ratings yet
- Stem Cell Research - COPD, Diabetes, Heart Disease-Abstracts From Dr. Fernandez VinaDocument5 pagesStem Cell Research - COPD, Diabetes, Heart Disease-Abstracts From Dr. Fernandez VinaDon Margolis Scam100% (1)
- Pi Is 0007091217540015Document10 pagesPi Is 0007091217540015Yoga WibowoNo ratings yet
- Goyal Et Al-2015-Annals of NeurologyDocument7 pagesGoyal Et Al-2015-Annals of NeurologyWinda Wahyu IkaputriNo ratings yet
- 1 s2.0 S1071916423003068 MainDocument13 pages1 s2.0 S1071916423003068 Mainevelyn.minichNo ratings yet
- Art 02Document8 pagesArt 02Paula Milla TorresNo ratings yet
- Department of Pharmacy Practice Sultan Ul Uloom College of Pharmacy (Approved by AICTE & PCI, A Liated To JNTUH) Mount Pleasant, Road No.3, Banjara Hills, Hyderabad 500 034Document14 pagesDepartment of Pharmacy Practice Sultan Ul Uloom College of Pharmacy (Approved by AICTE & PCI, A Liated To JNTUH) Mount Pleasant, Road No.3, Banjara Hills, Hyderabad 500 034sufiya fatimaNo ratings yet
- s12872 019 1096 1Document9 pagess12872 019 1096 1sarahNo ratings yet
- 1 s2.0 S0929664617300487 MainDocument8 pages1 s2.0 S0929664617300487 MainSuryati HusinNo ratings yet
- Ptca AGE RangeDocument4 pagesPtca AGE RangetanviNo ratings yet
- Graft Patency After Off-Pump Versus On-Pump Coronary Artery Surgery in High-Risk PatientsDocument8 pagesGraft Patency After Off-Pump Versus On-Pump Coronary Artery Surgery in High-Risk PatientsZul FikarNo ratings yet
- HRT 09000902Document6 pagesHRT 09000902boynextdoorpkyNo ratings yet
- 1 s2.0 S0735109719300956 MainDocument9 pages1 s2.0 S0735109719300956 MainAlberto PolimeniNo ratings yet
- Nikolsky2007 PDFDocument7 pagesNikolsky2007 PDFPicha PichiNo ratings yet
- Ni Hms 725829Document19 pagesNi Hms 725829SabariaNo ratings yet
- Percutaneous Transluminal Coronary Angioplasty (PTCA) and Stenting - Study of 100 CasesDocument7 pagesPercutaneous Transluminal Coronary Angioplasty (PTCA) and Stenting - Study of 100 CasesLuqy Luqman EffendyNo ratings yet
- Uhr Ve MortaliteDocument8 pagesUhr Ve MortalitealitrnfbNo ratings yet
- Intracoronary Autologous CD34+ Stem Cell Therapy For Intractable AnginaDocument8 pagesIntracoronary Autologous CD34+ Stem Cell Therapy For Intractable Anginaasep mahmudNo ratings yet
- Yeshwant 2018Document16 pagesYeshwant 2018StevenSteveIIINo ratings yet
- Factores para FNRDocument10 pagesFactores para FNRPOMYNo ratings yet
- NEJM 2019 Early or Delayed Cardioversion in Recent-Onset Atrial FibrillationDocument10 pagesNEJM 2019 Early or Delayed Cardioversion in Recent-Onset Atrial Fibrillationsl duoNo ratings yet
- Elaxim ResearchDocument6 pagesElaxim ResearchMayukh BanerjeeNo ratings yet
- Pan 2017Document1 pagePan 2017Arhip CojocNo ratings yet
- Cardiac CTDocument7 pagesCardiac CTdaniel7pintiliiNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- Carotid UltrasoundDocument9 pagesCarotid UltrasoundLora LefterovaNo ratings yet
- Prediction of Failed Fibrinolytic Using Scoring System in ST Elevation Myocardial Infarction PatientsDocument8 pagesPrediction of Failed Fibrinolytic Using Scoring System in ST Elevation Myocardial Infarction Patientsicurshm17No ratings yet
- Effect of chronic intercurrent medication with β-adrenoceptor blockade or calcium channel entry blockade on postoperative silent myocardial ischaemia†Document5 pagesEffect of chronic intercurrent medication with β-adrenoceptor blockade or calcium channel entry blockade on postoperative silent myocardial ischaemia†Taufik HidayatNo ratings yet
- 634-Article Text-2665-1-10-20190914 PDFDocument8 pages634-Article Text-2665-1-10-20190914 PDFhayaNo ratings yet
- Anaesthesia 1Document9 pagesAnaesthesia 1Sreekanth JangamNo ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- Brain Natriuretic Peptide in Acute Ischemic StrokeDocument6 pagesBrain Natriuretic Peptide in Acute Ischemic Strokesalma rachidiNo ratings yet
- Ija 18 4 168Document8 pagesIja 18 4 168Erika KennedyNo ratings yet
- Scot TrialDocument10 pagesScot TrialGP MHTGNo ratings yet
- Ing 5Document11 pagesIng 5Farida MufidatiNo ratings yet
- Eci 12222Document9 pagesEci 12222Andikaputra Brahma WidiantoroNo ratings yet
- Troponina Guided Coronary ComputedDocument11 pagesTroponina Guided Coronary ComputedafFNo ratings yet
- Admission Inferior Vena Cava Measurements Are Associated With Mortality After Hospitalization For Acute Decompensated Heart FailureDocument18 pagesAdmission Inferior Vena Cava Measurements Are Associated With Mortality After Hospitalization For Acute Decompensated Heart FailurePuja Nastia LubisNo ratings yet
- Transcatheter Closure of Patent Ductus ArteriosusDocument5 pagesTranscatheter Closure of Patent Ductus Arteriosusbagas rachmadiNo ratings yet
- Detection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloreDocument8 pagesDetection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloresubramanianNo ratings yet
- Terapia de Resincronización en Pacientes Con Insuficiencia Cardiaca Experiencia Acumulada de 10 AñosDocument9 pagesTerapia de Resincronización en Pacientes Con Insuficiencia Cardiaca Experiencia Acumulada de 10 AñosKevin Alegre AguileraNo ratings yet
- Full RevascDocument10 pagesFull RevascfelipeNo ratings yet
- Parental Consent and Waiver Form: Bogo Central School IiDocument2 pagesParental Consent and Waiver Form: Bogo Central School IiMhërvžž CatarataNo ratings yet
- Placenta and Amniotic Fluid Structure FunctionDocument66 pagesPlacenta and Amniotic Fluid Structure FunctionmadyNo ratings yet
- Perdev Q3 M4Document17 pagesPerdev Q3 M4Carl Laura Climaco100% (2)
- Terra Rosa Emagazine Issue 1Document45 pagesTerra Rosa Emagazine Issue 1Terra RosaNo ratings yet
- VetriDocument5 pagesVetrihari karanNo ratings yet
- By Dr. AlabastroDocument9 pagesBy Dr. Alabastro2013SecBNo ratings yet
- Nurse Patient Nurse: Tugas Sir Jon. Admission Patient DialogueDocument7 pagesNurse Patient Nurse: Tugas Sir Jon. Admission Patient DialogueIndry LabungasaNo ratings yet
- Untitled DocumentDocument121 pagesUntitled DocumentNur SanaaniNo ratings yet
- What Is Vicarious Trauma 2018 05 20Document2 pagesWhat Is Vicarious Trauma 2018 05 20api-546034011No ratings yet
- Narrative Lyphedema and ElephantiasisDocument1 pageNarrative Lyphedema and ElephantiasisKim SunooNo ratings yet
- Long Term Care Facilities Final ReportDocument157 pagesLong Term Care Facilities Final ReportPeter YankowskiNo ratings yet
- Chilhood2.0 AnalysisAndCritiqueDocument2 pagesChilhood2.0 AnalysisAndCritiqueYukaNo ratings yet
- Emergency Nursing 5 Tier Triage Protocols Second Edition Julie K Briggs Online Ebook Texxtbook Full Chapter PDFDocument69 pagesEmergency Nursing 5 Tier Triage Protocols Second Edition Julie K Briggs Online Ebook Texxtbook Full Chapter PDFdavid.shallenberger255100% (13)
- List of Members of Person's With Disability - Gulod (APWD-Gulod) Barangay Gulod, District 5, Quezon CityDocument33 pagesList of Members of Person's With Disability - Gulod (APWD-Gulod) Barangay Gulod, District 5, Quezon CityJurryNo ratings yet
- Liu004 Healthy LifestyleDocument2 pagesLiu004 Healthy LifestyleElena MHNo ratings yet
- Nitta Erlinda: Seminar Keperawatan RS Jantung Dan Pembuluh Darah "Harapan Kita" Jakarta 2019Document18 pagesNitta Erlinda: Seminar Keperawatan RS Jantung Dan Pembuluh Darah "Harapan Kita" Jakarta 2019Duas JourgieNo ratings yet
- Drug Study: AmoxicillinDocument3 pagesDrug Study: AmoxicillinKrzia TehNo ratings yet
- URC Form Lactation Clinic Final 2Document14 pagesURC Form Lactation Clinic Final 2muhammad zubair khanNo ratings yet
- Prostaglandins and Other Lipid Mediators: Prevent The Cause, Not Just The SymptomsDocument4 pagesProstaglandins and Other Lipid Mediators: Prevent The Cause, Not Just The SymptomsMaria Camila Ramírez GutiérrezNo ratings yet
- Operasi Dakriosistorhinostomi DCR Pada Pasien Dengan Dakriosistitis Kronis - Novaqua YandiDocument13 pagesOperasi Dakriosistorhinostomi DCR Pada Pasien Dengan Dakriosistitis Kronis - Novaqua YandiIDI Bangka BaratNo ratings yet
- Principles of Microbial Alchemy - Insights From The Streptomyces Coelicolor Genome Sequence PDFDocument5 pagesPrinciples of Microbial Alchemy - Insights From The Streptomyces Coelicolor Genome Sequence PDFCaesar VranceanuNo ratings yet
- RenalDocument60 pagesRenalEdmalyn Dela CruzNo ratings yet
- Accumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaDocument5 pagesAccumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaJana NgNo ratings yet
- Decoding Cancer Educator Guide - Lesson 5 - Updated8.18Document63 pagesDecoding Cancer Educator Guide - Lesson 5 - Updated8.18NisrinNo ratings yet
Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!
Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!
Uploaded by
ayesha FalakOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!
Heart J: Outcome of Primary Percutaneous Coronary Intervention With Early and Late ST Resolution - Earlier Is Better!
Uploaded by
ayesha FalakCopyright:
Available Formats
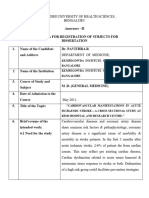
ORIGINAL ARTICLE
Pak Heart J
OUTCOME OF PRIMARY PERCUTANEOUS CORONARY
INTERVENTION WITH EARLY AND LATE ST
RESOLUTION - EARLIER IS BETTER!
Muhammad Tariq Farman1, Abdul Malik2, Qurban Ali Rahu3, Jawaid Akbar Sial4,
Naveedullah Khan5, Waheed Murad Shaikh6, Tahir Saghir7, Khan Shah Zaman8
1
Department of Cardiology, Jinnah
Medical College Hospital (JMCH), ABSTRACT
Karachi, Pakistan
2 Objective: To compare the outcome of Primary PCI in patients presenting with
Depar tment of Cardiovascular
Surgery, Lady Reading Hospital, early ST resolution versus those presenting late ST resolution after the procedure.
Peshawar Methodology: This observational prospective study was conducted in the
3
Department of Cardiology, People Catheterization Laboratory of a Tertiary Care Cardiovascular Centre of Pakistan.
Medical University, Nawabshah, Those patients who under went primary PCI were enrolled. All patients were pre
Pakistan treated with Aspirin 300 mg, and Clopidogrel 600mg. Platelet glycoprotein IIb IIIa
4
Department of Cardiology, Chandka inhibitor was given in the Catheterization Laboratory before the commencement
Medical College Hospital, Larkana,
Pakistan of procedure. Primary PCI was done in a standard fashion. Procedural details,
5-8 angiographic and electrocardiographic signs were recorded after PCI and clinical
Department of Cardiology, NICVD,
Karachi, Pakistan follow up was documented up to 1 year.
Address for Correspondence: Results: A total of 150 consecutive patients underwent primary PCI. 112 patients
Dr. Muhammad Tariq Farman, showed ST resolution within 60 minutes while 38 patients showed ST resolution
after 60 minutes. Patients with early ST resolution showed significant procedural
C-45, Block-2, KAECHS, Karachi, success (100 % vs. 94.7 %; P=0.014), and stable follow up at 30 days (92 % vs.
Pakistan 50 %; P= <0.001) and one year (88.3 % vs. 60.6 %; P=< 0.001). Mortality at
E-Mail: tariqfarman@yahoo.com 30 days was significantly lower (0.9% vs. 7.9 %; P=0.019) in patients with early
ST resolution while coronary artery bypass surgery was also significantly lower
Date Received: November 17, 2014
at 30 days (1.7 % vs. 15.8 %; P=0.001) and one year (2.7 % vs. 15.8 %;
Date Revised: December 23, 2014
P=0.004). Patients with late ST resolution were significantly aged (54.5±8.1 vs.
Date Accepted:December 26, 2014
50.4±12.9; P=0.023), more diabetic (39.5 % vs. 19.6 %; P=0.014), having
Contribution longer (>120 minutes) chest pain to ER time (34.2 % vs. 17.9%; P=0.03), and
All the authors contributed significantly having diffusely diseased vessels (73.7% vs. 52.7%; P=0.023). Three vessel
to the research that resulted in the disease was also more frequently seen in patients with late ST resolution (36.9%
submitted manuscript. vs. 17.9%; P=0.015).
All authors declare no conflict of Conclusion: Outcome of patients showing early ST resolution is significantly
interest. better than those showing late ST resolution. Elderly, diabetes, longer chest pain
This article may be cited as: Farman to ER time and diffuse three vessel disease are associated with late ST resolution.
MT, Malik A, Rahu QA, Sial JA, Khan N, Key Words: Outcome, Primary Percutaneous Coronary Intervention, ST
Shaikh WM, et al. Outcome of primary Resolution
percutaneous coronary intervention
with early and late ST resolution -
earlier is better! Pak Hear t J
2014;48(01):42-47.
Pak Heart J 2015 Vol. 48 (01) : 42-47 42
OUTCOME OF PRIMARY PCI WITH EARLY AND LATE ST RESOLUTION - EARLIER IS BETTER!
INTRODUCTION of hospital admission, those who were diagnosed as Non ST
elevation Myocardial Infarction (NSTEMI) and those
Primary Percutaneous coronary intervention (PCI) is presenting beyond 24 hours with resolved symptoms were
considered a preferable treatment of acute ST elevation excluded from the study. Patients with history of MI in the
myocardial infarction (STEMI).1,2 It is now being done same territory and those whose surface ECG could not be
successfully in many tertiary care centers of Pakistan.3,4 evaluated due to persistent electrical problem like left bundle
Although the restoration of epicardial coronary flow with branch block, paced or ventricular rhythm, WPW syndrome
primary PCI is achieved in majority of patients and it is far etc were also excluded from the study.
better than the pharmacological revascularization.1,2
Primary PCI was performed in standard method using a
However, considerable number of patients showed
variety of guiding catheters, coronary wires, balloons and
suboptimal and unsatisfactory results manifested by
stents. The majority of interventions were performed
unstable hemodynamic status, persistence of symptoms,
through the femoral route. However, the choice of access
abnormal myocardial blush and incomplete or absent ST
was on discretion of operators and considerable number
resolution on surface electrocardiogram (ECG).5-8
(18 %) of interventions was performed through radial route.
Absent or incomplete ST resolution after PCI is a strong All patients received 5000-10,000 units of intravenous
predictor for adverse events and abnormal left ventricular unfractionated heparin, Aspirin 300 mg, clopidogrel 600 mg
function. In contrast, patients with early ST resolution show (loading dose), and Platelet glycoprotein IIb IIIa inhibitor.
smaller infarct size and lower incidence of cardiac death at Thrombus extraction catheter (Export catheter 6-F;
one year. These differences remained significant even after Medtronic Corporation, USA) was used when obvious clot
adjustment of myocardial blush grade (MBG).5-9 was visible in the infarct related artery (thrombus class 2-5).
Intracoronary nitroprusside and adenosine use were at the
In our resource limited country, the average age of patients
discretion of operators. All patients were prescribed Aspirin
suffering STEMI is younger than the western population.3,4
300 mg, Clopidogrel 75 mg and Atorvastatin 20-40 mg /
Moreover, overall risk profile is poorer considering the fact of
Rosuvastatin 10-20 mg daily at the time of discharge from
having more uncontrolled diabetes and hypertension.10 In
the hospital.
addition, due to lack of awareness and poor education,
patients are usually used to present late after having The prospective information on variables including age,
symptoms of acute MI.11 This complicates the management gender, history of diabetes, hypertension, hyperlipidemia,
and the results may not be the same as shown by the smoking, angiographic and procedural details (number of
western studies. Therefore, in addition to outcome we also vessels, segment of vessel, use of aspiration catheter, clot
evaluated the predictors of late ST resolution in this study. retrieval, use of stents, GP IIb IIIa inhibitors, Thrombolysis in
We believe that the local data is scarcely available in this Myocardial Infarction (TIMI) flow, and Tissue Myocardial
regard and our study not only adds on the available data but perfusion (TMP) grade and Electrocardiogram (ECG)
also provides the new piece of information regarding the findings were recorded.
above mentioned issue.
TIMI flow, TMP grades and ST resolution (on 12- lead ECG
The aim of our study was to compare the outcome of strips) were visually determined and documented by two
Primary PCI in patients presenting with early ST resolution independent observers before and after PCI and in case of
versus those presenting late ST resolution after the controversy third expert opinion was taken as final.
procedure.
Intracoronary thrombus was classified as: zero - No
thrombus, 1 - reduced contrast density / possible thrombus,
METHODOLOGY 2 - small size thrombus / greatest dimension ≤ ½ of vessel
This observational, prospective, single centre study was diameter, 3 - moderate size thrombus / greatest dimension
conducted at a tertiary care cardiovascular teaching > ½ and < 2 vessel diameter, 4 - large size thrombus / ≥ 2
hospital (National Institute of Cardiovascular Diseases, vessel diameter, 5 - total occlusion. 12
Karachi-Pakistan) from January 1st 2011 to October 31st
PCI success was defined as achievement of vessel patency
2012. All adult patients (≥ 18 years old) with chest pain
to a residual ≤ 30 %. Major bleeding was defined as a
lasting > 30 minutes and ST elevation of ≥ 1 mm in ≥ 2
hematoma ≥ 10 cm in diameter or bleeding requiring
contiguous leads were included in this study. In case of
transfusion, vascular surgery or resulting in major
posterior MI, ST depression of ≥ 2 mm in ≥ 2 precordial morbidity.
leads were also considered eligible for the study. Informed
consent was taken and detailed questionnaire was filled of TIMI flow grades were defined as: Zero - total occlusion
those patients who underwent primary PCI. resulting in no antegrade flow, 1 - minimal penetration of
contrast across the obstruction but fails to opacify the
Patients who received Thrombolytic therapy within 24 hours vessel, 2 - contrast opacifies the vessel beyond the
Pak Heart J 2015 Vol. 48 (01) : 42-47 43
OUTCOME OF PRIMARY PCI WITH EARLY AND LATE ST RESOLUTION - EARLIER IS BETTER!
occlusion but with delay, 3 - normal complete perfusion of ST resolution was defined as any resolution or no resolution
entire vessel without any delay. 13 after 60 minutes of Primary PCI. Complete ST resolution
was defined as ≥ 70% ST resolution compared to baseline
TMP grades were defined as: Zero - minimal or no
ECG. No ST segment resolution was defined as persistent
myocardial blush, 1 - dye stains the myocardium and this
ST segment elevation or ≤ 30 % resolution of ST segment.15
stain persists on the next injection, 2 - dye enters the
myocardium but washes out slowly and strongly persists at Patients were followed in outpatient department (OPD) after
the end of injection, 3 - normal entrance and exit of dye in the one month, and at 1 year. Those patients who could not
myocardium.14 come in OPD, they were contacted through telephone and
follow up documented.
Early ST resolution was defined as ≥ 50% ST segment
resolution within 60 minutes of primary PCI, whereas, late All the data was entered and analyzed through SPSS
version17. Categorical variables like gender, diabetes,
Table 1: Baseline Demographic and Angiographic features hypertension, smoking, history of previous MI, cardiogenic
of Patients Underwent Primary PCI within 60 and shock, inotropic support, IABP, infarction territory, route of
after 60 Minutes of ST Resolution access etc were presented in frequencies and percentages.
ST Resolution ST Resolution Whereas continuous variables like age, height, weight, BMI,
Variables within 60 mins after 60 mins P-value symptom onset to ER and door to balloon time were
n=112 n=38 presented as mean ± SD. Chi square test was used for
Age in years [Mean ±SD] 50.4 +12.9 54.5 +8.1 0.023 significant association. Independent t-test for normally
Gender Male 103 (92%) 32 (84%) 0.169
distributed data and Mann Whitney U test were used for not
normally distributed data to compare mean (±SD) values of
Height in cm [Mean ±SD] 172.2 +7.1 170 +7.2 0.093
with and without aspiration of thrombus. P-value < 0.05
Weight in Kg [Mean ±SD] 77.8 +12.2 75.8 +8.4 0.281 was considered as statistically significant.
Diabetes 22 (19.6%) 15 (39.5%) 0.014
RESULTS
Hypertension 54 (48%) 16 (42%) 0.514
Smoking 46 (41%) 10 (26%) 0.104
Out of 150 patients enrolled, 112 (74.6 %) showed ST
resolution within 60 minutes. Table 1 is showing baseline
History of previous MI 22 (19.6%) 12 (31.6%) 0.129 demographic, clinical and angiographic features of both
Symptom onset to ER time 113.9 +137.5 141.4 +128.5 0.074 groups. Patients who showed ST resolution after 60 minutes
in minutes [Mean ±SD]*
were significantly elder than those revealed early ST
resolution. Diabetes, Multivessel disease and type C lesions
Door to Balloon time 101.6 +54.3 105.6 +72.0 0.586 were also more common in patients with late ST resolution
in minutes; [Mean ±SD]* (Table 1). Procedural characteristics were almost same in
≤ 90 minutes 55 (49%) 23 (60.5%) 0.223
both groups except the TIMI III flow that was significantly
more commonly seen in patients with early ST resolution
> 90 minutes 57 (51%) 15 (39.5%) (Table 2).
Infarction territory
Table 3 is showing the difference of outcomes of both
AWMI 76 (68%) 25 (66%) 0.814 groups underwent primary PCI. 100% immediate success
IWMI 36 (32%) 13 (34%) was achieved in patients showing early ST resolution, while
it was ~95% in patients with late ST resolution. At 30 days
Culprit Artery
and 1 year of follow up 103(90%) and 99(88.3%) were
LAD, Diagonal 72 (64.3%) 25 (65.8%) 0.875 stable, respectively, in patients with early ST resolution.
RCA 23 (20.5%) 10 (26.3%) 0.469 While only 19(50%) and 23(60.6 %) were stable in the other
group. Similarly, CABG and death were significantly more
LCx, Ramus 17 (15.2%) 03 (7.9%) 0.247
common in patients with late ST resolution (Table 3). Table 4
Lesion Risk is showing the comparison of group of patients with early
Type A, B 53 (47.3%) 10 (26.3%) 0.023 and late ST resolution whom DBT is ≤ 90 minutes.
Prolonged symptom onset to ER time (91.9±59.6 vs.
Type C 59 (52.7%) 28 (73.7%)
167.8±156.7 minutes; p=0.02) was significantly related to
Number of Diseased vessels late ST resolution.
SVD 70 (62.5%) 23 (60.5%) 0.816
2VD 22 (19.6%) 01 (2.6%) 0.012
DISCUSSION
3VD 20 (17.9%) 14 (36.9) 0.015 It is evident by our study that outcome of the patients
Pak Heart J 2015 Vol. 48 (01) : 42-47 44
OUTCOME OF PRIMARY PCI WITH EARLY AND LATE ST RESOLUTION - EARLIER IS BETTER!
Table 2: Procedural Characteristics of the Groups of Patients STR group was worse than the early STR group. They were
Underwent Primary PCI Showing ST Resolution aged and majority of them having diabetes, multivessel
within 60 and After 60 Minutes disease and type C lesions. As a result this was not
surprising when they demonstrated a poor prognosis and
ST Resolution ST Resolution quite a few of them showed a suboptimal TIMI flow grades
Variables within 60 mins after 60 mins P-value immediately after PCI (Table 2). It is a well known fact that
n=112 n=38
aged population has got worse atherosclerotic
Grade of stenosis cardiovascular disease. They have poor microvasculature,
Total (100 %) 66 (59%) 26 (68.4%) 0.298 and badly diseased endothelium that may not be responded
well even following the restoration of coronary blood flow
Sub-total (91-99%) 11 (10%) 04 (10.5%) 0.900
after the primary PCI.16, 17 Similarly, diabetes badly damages
Severe (70-90%) 35 (31%) 08 (21.1%) 0.229 the vascular system in general and microvasculature in
Lesion length particular. Therefore, even after the restoration of coronary
vessel myocardium may not be well perfused due to
≤ 20 mm 71 (63.4%) 22 (58%) 0.546 diseased microvasculature and hence, late STR ensued.18
> 20 mm 41 (36.6%) 16 (42%) Recent studies have shown the increased risk of major
Size of culprit artery adverse cardiovascular events after primary PCI in case of
multivessel disease if the other vessels are not
≤ 3 mm 36 (32%) 10 (26.3%) 0.501
intervened.19,20 Therefore recently published landmark
> 3 mm 73 (68%) 28 (73.7%) Complete versus Lesion-only Primary PCI Trial (CvLPRIT)
Clot retrieved 38 (34%) 14 (37%) 0.752 study have shown a 55% reduction in major adverse
cardiovascular events in those patients presenting for
Adenosine used 23 (20.5%) 09 (23.7%) 0.682 primary percutaneous coronary interventions when the non-
Size of stent deployed
Table 3: Outcomes of the Patients Underwent
≤ 20 mm 49 (43.7%) 13 (34.2%) 0.303
Primary PCI within 60 and After
> 20 mm 48 (42.9%) 16 (42.1%) 0.939 60 Minutes of ST Resolution
> one stent 09 (8%) 07 (18.4%) 0.079 ST Resolution ST Resolution
06 (5.4%) 02 (5.3%) 0.999
Variables within 60 mins after 60 mins P-value
stenting not done n=112 n=38
TIMI flow Immediate after Procedure
Zero – I 0 01 (2.6%) 0.125 Successful PCI 112 (100%) 36 (94.7%) 0.014
II 03 (2.7%) 04 (10.5%) 0.051 Major bleeding 0 01 (2.6%) 0.125
III 109 (97.3%) 33 (86.9%) 0.012 Death 0 01 (2.6%) 0.125
TMP Grade Follow up after 30 days
Zero – I 67 (59.8%) 25 (65.8%) 0.514 Stable 103 (92%) 19 (50%) < 0.001
II & III 45 (40.2%) 13 (34.2%) 0.514 CABG 02 (1.7%) 06 (15.8%) 0.001
showing late or no STR after primary PCI is dismal. This MACE 03 (2.7%) 01 (2.6%) 0.999
group did not show stable follow up and encountered more Death 01 (0.9%) 03 (7.9%) 0.019
frequent adverse cardiac events like CABG and death. This
Lost follow up 03 (2.7%) 09 (23.7%) < 0.001
finding is consistent with previous studies in which the same
issue of STR was addressed. It was previously reported that Follow up after 1 year
patients with early STR had more preserved LVEF and Stable 99 (88.3%) 23 (60.6%) < 0.001
smaller infarct size compared to patients with late or no
STR.9 Therefore it is understandable if the patients with late CABG 03 (2.7%) 06 (15.8%) 0.004
STR showed poor outcome results in our study. MACE 05 (4.5%) 01 (2.6%) 0.630
Within 60 minutes of time window three fourths (74.7%) of Death 04 (3.6%) 04 (10.5%) 0.093
our patients showed satisfactory STR. While 28 (18.7%)
Lost follow up 01 (0.9%) 04 (10.5%) 0.005
patients showed STR after 60 minutes and 10 (6.7%)
patients did not show any resolution. The risk profile of late PCI=Percutaneous coronary intervention; CABG=Coronary artery bypass grafting;
MACE=Major adverse cardiovascular events
Pak Heart J 2015 Vol. 48 (01) : 42-47 45
OUTCOME OF PRIMARY PCI WITH EARLY AND LATE ST RESOLUTION - EARLIER IS BETTER!
Table 4: Comparison Between ST Resolution between the government and health care authorities.
within & after 60 Mins Who's Door to
Balloon Time < 90 mins CONCLUSION
Outcome of patients showing early ST resolution is
ST Resolution ST Resolution significantly better than those showing late ST resolution.
Variables within 60 mins after 60 mins P-value Elderly age, diabetes, longer chest pain to ER time and
n=55 n=23
diffuse three vessel disease are associated with late ST
Age in years [Mean ±SD] 50.1 ± 12.6 53.6 ± 8.8 0.165
resolution. Outcome of late presenter (patients who have
Gender Male 49 (89%) 20 (87%) 0.999 longer chest pain to ER time) remains poor even after
achieving standard DBT of 90 minutes.
Height in cm [Mean ±SD] 172.1 ± 7.3 168.8 ± 7.3 0.072
Weight in Kg [Mean ±SD] 78.3 ± 14.7 75.5 ± 8.9 0.309
ACKNOWLEDGMENT
Diabetes 11 (20%) 08 (35%) 0.165 Authors wish to thanks Mr. Jaffer Bin Baqar for his help in
data management and analysis.
Hypertension 26 (47%) 10 (43.5%) 0.759
Smoking 23 (42%) 05 (22%) 0.092 REFERENCES
History of previous MI 10 (18%) 06 (26%) 0.540 1. Keeley EC, Boura JA, Grines CL. Priamry angioplasty
Symptom onset to ER time versus intravenous thrombolytic therapy for acute
myocardial infarction: a quantitative review of 23
in minutes [Mean ±SD]* 91.9 ± 59.6 167.8 ± 156.7 0.022 randomized trials. Lancet 2003;361:13-20.
*Man-Whitney U test was used
2. Silber S, Albertsson P, Aviles FF, Camici PG, Colombo
infarct-related artery is treated on the index admission. In 21, 22 A, Hamm C, et al. Guidelines for percutaneous
our study although we strictly followed the recent guidelines coronary interventions: the Task Force for
and did not intervene the non infarct related arteries during Percutaneous Coronary Interventions of the European
the index admission unless the patient was in shock. Society of Cardiology. Eur Heart J 2005;26:804-47.
However, by viewing our data it may be said that patients 3. Farman MT, Sial JA, Khan NU, Rizvi SNH, Saghir T,
with multivessel disease have poorer outcome after primary Zaman KS. Outcome of primary percutaneous
PCI as compare to those having single vessel disease. Thus, coronary intervention at public sector tertiary care
our data further support the argument in favor of complete hospital in Pakistan. J Pak Med Assoc 2011;61:575-
revascularization at the time of primary PCI during index 81.
admission.
4. Shaikh AH, Siddiqui MS, Hanif B, Malik F, Hasan K, Adhi
The another interesting fact that we found in our data that F. Outcomes of Primary percutaneous coronary
despite of achieving optimum DTB time of 90 minutes, STR intervention in a tertiary care cardiac centre. J Pak Med
was significantly different between early presenter versus Assoc 2009;59:426-9
late presenter to ER. STR within 60 minutes was achieved
more frequently in patients who presented to ER within 90 5. Santoro GM, Antoniucci D, Valenti R, Bolognese L,
minutes after symptoms onset. There was remarkable Buonamici P, Trapani M, et al. Rapid reduction of ST-
difference of presentation time to ER between both the segment elevation after successful direct angioplasty
groups. None of the other factors like age, DM, in acute myocardial infarction. Am J Cardiol
hypertension, smoking etc. turned significant in this 1997;80:685-9.
perspective. Hence, it further strengthens the famous saying 6. Brodie BR, Stuckey TD, Hansen C, VerSteeg DS, Muncy
“Time is Muscle”, that means more you waste the time more DB, Moore S, et al. Relation between
you lose the muscle.23, 24 Thus, it is not enough to achieve the electrocardiographic ST-segment resolution and early
optimal DTB to get the better outcome. We must try hard to and late outcomes after primary percutaneous
lessen the symptom onset to ER time to achieve the better coronary intervention for acute myocardial infarction.
outcome. Therefore, increasing awareness about the Am J Cardiol 2005;95:343-8.
ischemic symptoms among the patients on the mass level is
important at the one end. At the other end development of 7. Buller CE, Fu Y, Mahaffey KW, Todaro TG, Adams P,
effective social and health care system is equally necessary Westerhout CM, et al. ST-segment recovery and
that must ensure the early transport of the poor patient of outcome after primary percutaneous coronary
STEMI to the tertiary health care facility without wasting intervention for ST-elevation myocardial infarction:
time. This needs effective communication and political will insights from the Assessment of Pexelizumab in Acute
Myocardial Infarction (APEX-AMI) trial. Circulation
Pak Heart J 2015 Vol. 48 (01) : 42-47 46
OUTCOME OF PRIMARY PCI WITH EARLY AND LATE ST RESOLUTION - EARLIER IS BETTER!
2008;118:1335-46. do with it? A review of contemporary revascularization
in the elderly. Curr Cardiol Rev 2014;[Epub ahead of
8. McLaughlin MG, Stone GW, Aymong E, Gardner G,
print].
Mehran R, Lansky AJ, et al. Prognostic utility of
comparative methods for assessment of ST-segment 17. Odden MC, Coxson PG, Moran A, Lightwood JM,
resolution after primary angioplasty for acute Goldman L, Bibbins-Domingo K. The Impact of the
myocardial infarction: the Controlled Abciximab and aging population on coronary heart disease in the
Device Investigation to Lower Late Angioplasty United States. Am J Med 2011;24:827-33.
Complications (CADILLAC) trial. J Am Coll Cardiol
18. Brener SJ, Mehran R, Dressler O, Cristea E, Stone GW.
2004;44:1215-23.
Diabetes mellitus, myocardial reperfusion, and
9. Haeck JD, Verouden NJ, Kuijt WJ, Koch KT, Majidi M, outcome in patients with acute ST-elevation myocardial
Hirsch A, et al. Impact of early, late, and no ST-segment infarction treated with primary angioplasty (from
resolution measured by continuous ST Holter HORIZONS AMI). Am J Cardiol 2012;109:1111-6.
monitoring on left ventricular ejection fraction and
19. Harries I, Ramcharitar S. Total revascularization of
infarct size as determined by cardiovascular magnetic
coronary disease at the time of primary percutaneous
resonance imaging. J Electrocardiol 2011;44:36-41.
coronary intervention. Future Cardiol 2014;10:451-5.
10. Farman MT, Saghir T, Rizvi NH, Sial JA, Khan NU, Malik
20. Iqbal MB, Ilsley C, Kabir T, Smith R, Lane R, Mason M,
A, et al. Safety of primary percutaneous coronary
et al. Culprit vessel versus multivessel intervention at
intervention with and without (selective) thrombus
the time of primary percutaneous coronary intervention
aspiration. J Pak Med Assoc 2014;64:653-9.
in patients with ST-segment-elevation myocardial
11. Khan MS, Jafary FH, Faruqui AM, Rasool SI, Hatcher J, infarction and multivessel disease: real-world analysis
Chatervedi N, et al. High prevalence of lack of of 3984 patients in London. Circ Cardiovasc Qual
knowledge of symptoms of acute myocardial infarction Outcomes 2014;7:936-43.
in Pakistan and its contribution to delayed presentation
21. Bainey KR, Mehta SR, Lai T, Welsh RC. Complete vs
to the hospital. BMC Public Health 2007;7:284.
culprit-only revascularization for patients with
12. Sianos G, Papafaklis MI, Serruys PW. Angiographic multivessel disease undergoing primary percutaneous
thrombus burden classification in patients with ST coronary intervention for ST-segment elevation
segment elevation myocardial infarction treated with myocardial infarction: a systematic review and meta-
percutaneous coronary intervention. J Invasive Cardiol analysis. Am Heart J 2014;167:1-14.
2010;22:6B-14B.
22. Kelly DJ, McCann GP, Blackman D, Curzen NP, Dalby M,
13. The TIMI study group. The Thrombolysis in Myocardial Greenwood JP, et al . Complete Versus culprit-Lesion
Infarction (TIMI) Trial Phase I findings. N Eng J Med only Primary PCI Trial (CVLPRIT): a multicentre trial
1985;312:932-6. testing management strategies when multivessel
disease is detected at the time of primary PCI: rationale
14. Van't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de
and design. Eurointervention 2013;8:1190-8.
Boer MJ. Zajistra F. Angiographic assessment of
myocardial reperfusion in patients treated primary 23. Gibson CM, de Lemos JA, Antman EM. Time is muscle
angioplasty for acute myocardial infarctiopn. in primary PCI: the strength of the evidence grows. Eur
Myocardial blush grade. Zwolle myocardial infarction Heart J 2004;25:1001-2.
study group. Circulation 1998;97:2302-6.
24. De Luca G, Van't Hof WJA, De Boer MJ, Ottervanger JP,
15. Van't Hof AW, Liem A, de Boer MJ, Zijlstra F. Clinical Hoorntje JCA, Gosselink ATM, et al. Time-to-treatment
value of 12-lead electrocardiogram after successful significantly affects the extent of ST-segment resolution
reperfusion therapy for acute myocardial infarcton. and myocardial blush in patients with acute myocardial
Lancet 1997;350:615-9. infarction treated by primary angioplasty. Eur Heart J
2004;25:1009-13.
16. Vandermolen S, Abbott J, De Silva K. What's age got to
Pak Heart J 2015 Vol. 48 (01) : 42-47 47
You might also like
- Atlas of Gynecologic Surgical PathologyDocument581 pagesAtlas of Gynecologic Surgical PathologySandu Alexandra100% (4)
- Student Cell CommunicationDocument11 pagesStudent Cell Communicationapi-2620290510% (1)
- From Blue Nines and Red WordsDocument6 pagesFrom Blue Nines and Red Wordsabunour50% (4)
- List of Medicinal Plants and Their UsesDocument6 pagesList of Medicinal Plants and Their Usesshangiri75% (4)
- Original Research Abstract AFCC ASMIHA 2019Document82 pagesOriginal Research Abstract AFCC ASMIHA 2019Program Studi Kardiologi100% (1)
- Chughtai Lab Rate ListDocument33 pagesChughtai Lab Rate ListHassan Gill67% (9)
- Obstetrics and Gynaecology History Taking TemplateDocument4 pagesObstetrics and Gynaecology History Taking TemplateMaruti100% (3)
- Impact of Atropine and Aminophylline On TAVB With Inferior Wall MIDocument2 pagesImpact of Atropine and Aminophylline On TAVB With Inferior Wall MIRakhmat RamadhaniNo ratings yet
- Outcomes of Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction at Tehran Heart CenterDocument6 pagesOutcomes of Primary Percutaneous Coronary Intervention in Acute Myocardial Infarction at Tehran Heart CenterHamiNo ratings yet
- 62 2020 Article 898Document7 pages62 2020 Article 898sinamirjaniNo ratings yet
- Ischemic 19Document8 pagesIschemic 19Adina Alexandra CNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofahmadto80No ratings yet
- F QRSDocument9 pagesF QRSaisyah hamzakirNo ratings yet
- Abstrak IsicamDocument22 pagesAbstrak IsicambgusjklNo ratings yet
- AggarwalDocument7 pagesAggarwalSuryaNo ratings yet
- Stenoza MitralaDocument7 pagesStenoza MitralaVerginia OnofreiNo ratings yet
- Manual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceDocument9 pagesManual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceArdiana FirdausNo ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDocument6 pagesPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- Therapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticDocument8 pagesTherapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticNITACORDEIRONo ratings yet
- Study 3Document7 pagesStudy 3OstazNo ratings yet
- Synopsis For DissertationDocument9 pagesSynopsis For DissertationahmedNo ratings yet
- 1 s2.0 S1933171109001302 MainDocument7 pages1 s2.0 S1933171109001302 MainRizky BafadhalNo ratings yet
- Stem Cell Research - COPD, Diabetes, Heart Disease-Abstracts From Dr. Fernandez VinaDocument5 pagesStem Cell Research - COPD, Diabetes, Heart Disease-Abstracts From Dr. Fernandez VinaDon Margolis Scam100% (1)
- Pi Is 0007091217540015Document10 pagesPi Is 0007091217540015Yoga WibowoNo ratings yet
- Goyal Et Al-2015-Annals of NeurologyDocument7 pagesGoyal Et Al-2015-Annals of NeurologyWinda Wahyu IkaputriNo ratings yet
- 1 s2.0 S1071916423003068 MainDocument13 pages1 s2.0 S1071916423003068 Mainevelyn.minichNo ratings yet
- Art 02Document8 pagesArt 02Paula Milla TorresNo ratings yet
- Department of Pharmacy Practice Sultan Ul Uloom College of Pharmacy (Approved by AICTE & PCI, A Liated To JNTUH) Mount Pleasant, Road No.3, Banjara Hills, Hyderabad 500 034Document14 pagesDepartment of Pharmacy Practice Sultan Ul Uloom College of Pharmacy (Approved by AICTE & PCI, A Liated To JNTUH) Mount Pleasant, Road No.3, Banjara Hills, Hyderabad 500 034sufiya fatimaNo ratings yet
- s12872 019 1096 1Document9 pagess12872 019 1096 1sarahNo ratings yet
- 1 s2.0 S0929664617300487 MainDocument8 pages1 s2.0 S0929664617300487 MainSuryati HusinNo ratings yet
- Ptca AGE RangeDocument4 pagesPtca AGE RangetanviNo ratings yet
- Graft Patency After Off-Pump Versus On-Pump Coronary Artery Surgery in High-Risk PatientsDocument8 pagesGraft Patency After Off-Pump Versus On-Pump Coronary Artery Surgery in High-Risk PatientsZul FikarNo ratings yet
- HRT 09000902Document6 pagesHRT 09000902boynextdoorpkyNo ratings yet
- 1 s2.0 S0735109719300956 MainDocument9 pages1 s2.0 S0735109719300956 MainAlberto PolimeniNo ratings yet
- Nikolsky2007 PDFDocument7 pagesNikolsky2007 PDFPicha PichiNo ratings yet
- Ni Hms 725829Document19 pagesNi Hms 725829SabariaNo ratings yet
- Percutaneous Transluminal Coronary Angioplasty (PTCA) and Stenting - Study of 100 CasesDocument7 pagesPercutaneous Transluminal Coronary Angioplasty (PTCA) and Stenting - Study of 100 CasesLuqy Luqman EffendyNo ratings yet
- Uhr Ve MortaliteDocument8 pagesUhr Ve MortalitealitrnfbNo ratings yet
- Intracoronary Autologous CD34+ Stem Cell Therapy For Intractable AnginaDocument8 pagesIntracoronary Autologous CD34+ Stem Cell Therapy For Intractable Anginaasep mahmudNo ratings yet
- Yeshwant 2018Document16 pagesYeshwant 2018StevenSteveIIINo ratings yet
- Factores para FNRDocument10 pagesFactores para FNRPOMYNo ratings yet
- NEJM 2019 Early or Delayed Cardioversion in Recent-Onset Atrial FibrillationDocument10 pagesNEJM 2019 Early or Delayed Cardioversion in Recent-Onset Atrial Fibrillationsl duoNo ratings yet
- Elaxim ResearchDocument6 pagesElaxim ResearchMayukh BanerjeeNo ratings yet
- Pan 2017Document1 pagePan 2017Arhip CojocNo ratings yet
- Cardiac CTDocument7 pagesCardiac CTdaniel7pintiliiNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- Carotid UltrasoundDocument9 pagesCarotid UltrasoundLora LefterovaNo ratings yet
- Prediction of Failed Fibrinolytic Using Scoring System in ST Elevation Myocardial Infarction PatientsDocument8 pagesPrediction of Failed Fibrinolytic Using Scoring System in ST Elevation Myocardial Infarction Patientsicurshm17No ratings yet
- Effect of chronic intercurrent medication with β-adrenoceptor blockade or calcium channel entry blockade on postoperative silent myocardial ischaemia†Document5 pagesEffect of chronic intercurrent medication with β-adrenoceptor blockade or calcium channel entry blockade on postoperative silent myocardial ischaemia†Taufik HidayatNo ratings yet
- 634-Article Text-2665-1-10-20190914 PDFDocument8 pages634-Article Text-2665-1-10-20190914 PDFhayaNo ratings yet
- Anaesthesia 1Document9 pagesAnaesthesia 1Sreekanth JangamNo ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- Brain Natriuretic Peptide in Acute Ischemic StrokeDocument6 pagesBrain Natriuretic Peptide in Acute Ischemic Strokesalma rachidiNo ratings yet
- Ija 18 4 168Document8 pagesIja 18 4 168Erika KennedyNo ratings yet
- Scot TrialDocument10 pagesScot TrialGP MHTGNo ratings yet
- Ing 5Document11 pagesIng 5Farida MufidatiNo ratings yet
- Eci 12222Document9 pagesEci 12222Andikaputra Brahma WidiantoroNo ratings yet
- Troponina Guided Coronary ComputedDocument11 pagesTroponina Guided Coronary ComputedafFNo ratings yet
- Admission Inferior Vena Cava Measurements Are Associated With Mortality After Hospitalization For Acute Decompensated Heart FailureDocument18 pagesAdmission Inferior Vena Cava Measurements Are Associated With Mortality After Hospitalization For Acute Decompensated Heart FailurePuja Nastia LubisNo ratings yet
- Transcatheter Closure of Patent Ductus ArteriosusDocument5 pagesTranscatheter Closure of Patent Ductus Arteriosusbagas rachmadiNo ratings yet
- Detection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloreDocument8 pagesDetection of Myocardial Infraction Monisha C M - 17bei0092: Select, Vit VelloresubramanianNo ratings yet
- Terapia de Resincronización en Pacientes Con Insuficiencia Cardiaca Experiencia Acumulada de 10 AñosDocument9 pagesTerapia de Resincronización en Pacientes Con Insuficiencia Cardiaca Experiencia Acumulada de 10 AñosKevin Alegre AguileraNo ratings yet
- Full RevascDocument10 pagesFull RevascfelipeNo ratings yet
- Parental Consent and Waiver Form: Bogo Central School IiDocument2 pagesParental Consent and Waiver Form: Bogo Central School IiMhërvžž CatarataNo ratings yet
- Placenta and Amniotic Fluid Structure FunctionDocument66 pagesPlacenta and Amniotic Fluid Structure FunctionmadyNo ratings yet
- Perdev Q3 M4Document17 pagesPerdev Q3 M4Carl Laura Climaco100% (2)
- Terra Rosa Emagazine Issue 1Document45 pagesTerra Rosa Emagazine Issue 1Terra RosaNo ratings yet
- VetriDocument5 pagesVetrihari karanNo ratings yet
- By Dr. AlabastroDocument9 pagesBy Dr. Alabastro2013SecBNo ratings yet
- Nurse Patient Nurse: Tugas Sir Jon. Admission Patient DialogueDocument7 pagesNurse Patient Nurse: Tugas Sir Jon. Admission Patient DialogueIndry LabungasaNo ratings yet
- Untitled DocumentDocument121 pagesUntitled DocumentNur SanaaniNo ratings yet
- What Is Vicarious Trauma 2018 05 20Document2 pagesWhat Is Vicarious Trauma 2018 05 20api-546034011No ratings yet
- Narrative Lyphedema and ElephantiasisDocument1 pageNarrative Lyphedema and ElephantiasisKim SunooNo ratings yet
- Long Term Care Facilities Final ReportDocument157 pagesLong Term Care Facilities Final ReportPeter YankowskiNo ratings yet
- Chilhood2.0 AnalysisAndCritiqueDocument2 pagesChilhood2.0 AnalysisAndCritiqueYukaNo ratings yet
- Emergency Nursing 5 Tier Triage Protocols Second Edition Julie K Briggs Online Ebook Texxtbook Full Chapter PDFDocument69 pagesEmergency Nursing 5 Tier Triage Protocols Second Edition Julie K Briggs Online Ebook Texxtbook Full Chapter PDFdavid.shallenberger255100% (13)
- List of Members of Person's With Disability - Gulod (APWD-Gulod) Barangay Gulod, District 5, Quezon CityDocument33 pagesList of Members of Person's With Disability - Gulod (APWD-Gulod) Barangay Gulod, District 5, Quezon CityJurryNo ratings yet
- Liu004 Healthy LifestyleDocument2 pagesLiu004 Healthy LifestyleElena MHNo ratings yet
- Nitta Erlinda: Seminar Keperawatan RS Jantung Dan Pembuluh Darah "Harapan Kita" Jakarta 2019Document18 pagesNitta Erlinda: Seminar Keperawatan RS Jantung Dan Pembuluh Darah "Harapan Kita" Jakarta 2019Duas JourgieNo ratings yet
- Drug Study: AmoxicillinDocument3 pagesDrug Study: AmoxicillinKrzia TehNo ratings yet
- URC Form Lactation Clinic Final 2Document14 pagesURC Form Lactation Clinic Final 2muhammad zubair khanNo ratings yet
- Prostaglandins and Other Lipid Mediators: Prevent The Cause, Not Just The SymptomsDocument4 pagesProstaglandins and Other Lipid Mediators: Prevent The Cause, Not Just The SymptomsMaria Camila Ramírez GutiérrezNo ratings yet
- Operasi Dakriosistorhinostomi DCR Pada Pasien Dengan Dakriosistitis Kronis - Novaqua YandiDocument13 pagesOperasi Dakriosistorhinostomi DCR Pada Pasien Dengan Dakriosistitis Kronis - Novaqua YandiIDI Bangka BaratNo ratings yet
- Principles of Microbial Alchemy - Insights From The Streptomyces Coelicolor Genome Sequence PDFDocument5 pagesPrinciples of Microbial Alchemy - Insights From The Streptomyces Coelicolor Genome Sequence PDFCaesar VranceanuNo ratings yet
- RenalDocument60 pagesRenalEdmalyn Dela CruzNo ratings yet
- Accumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaDocument5 pagesAccumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaJana NgNo ratings yet
- Decoding Cancer Educator Guide - Lesson 5 - Updated8.18Document63 pagesDecoding Cancer Educator Guide - Lesson 5 - Updated8.18NisrinNo ratings yet